Professional Documents
Culture Documents
Antibodies and Neuronal Autoimmune Disorders of The CNS: Ó Springer-Verlag 2009
Antibodies and Neuronal Autoimmune Disorders of The CNS: Ó Springer-Verlag 2009
Uploaded by
deadcorpsesOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antibodies and Neuronal Autoimmune Disorders of The CNS: Ó Springer-Verlag 2009
Antibodies and Neuronal Autoimmune Disorders of The CNS: Ó Springer-Verlag 2009
Uploaded by
deadcorpsesCopyright:
Available Formats
J Neurol (2010) 257:509517 DOI 10.
1007/s00415-009-5431-9
REVIEW
Antibodies and neuronal autoimmune disorders of the CNS
Francesc Graus Albert Saiz Josep Dalmau
Received: 14 December 2009 / Accepted: 14 December 2009 / Published online: 25 December 2009 Springer-Verlag 2009
Abstract We review the neuronal antibodies described in CNS disorders in order to clarify their diagnostic value, emphasize potentials pitfalls and limitations in the diagnosis of paraneoplastic neurological syndromes (PNS), and examine the current evidence for a possible pathogenic role. We propose to classify the neuronal antibodies associated with syndromes resulting from CNS neuronal dysfunction into two groups according to the location of the antigen: inside the neuron or in the cell membrane. Group I includes antibodies which target intracellular antigens and probably are not pathogenic. They are further subdivided into three groups. Group Ia comprises well-characterized onconeural antibodies (Hu (ANNA1), Yo (PCA1), Ri (ANNA2), CV2 (CRMP5), amphiphysin, Ma2) that are useful for the diagnosis of PNS. Group Ib antibodies (SOX and ZIC) are cancer-specic but there is no evidence that the immune response is in any way pathogenically related to the PNS. Antibodies in group Ic (glutamic acid decarboxylase (GAD), adenylate kinase 5 and Homer 3) identify non-PNS: stiff-person syndrome (SPS), cerebellar ataxia, and limbic encephalitis (LE). Group II antibodies recognize neuronal surface antigens. Antibodies in group IIa associate with characteristic CNS syndromes but their detection does not indicate that the disorder is paraneoplastic. Antibodies to potassium channels, AMPA and GABAB receptors are associated with LE, NMDA receptor antibodies
F. Graus (&) A. Saiz Servei de Neurologia, Hospital Clinic, Institut d Investigacio ` dica August Pi i Sunyer (IDIBAPS), Villarroel 170, Biome 08036 Barcelona, Spain e-mail: fgraus@clinic.ub.es J. Dalmau Department of Neurology, University of Pennsylvania, Philadelphia, PA, USA
identify a well-dened encephalitis, and antibodies against glycine receptors associate with SPS with encephalitis. A pathogenic role of the antibodies is suggested by the response of symptoms to immunotherapy and the correlation between antibody titers and neurological outcome. Lastly, Group IIb includes antibodies that are found in patients with paraneoplastic cerebellar ataxia associated with lung cancer (P/Q type calcium channels antibodies) or Hodgkin disease (metabotropic glutamate receptor type 1 antibodies). Keywords Antibodies Autoimmunity Paraneoplastic neurological syndromes Encephalitis Cerebellar degeneration Epilepsy
Introduction The idea that neurons can be the target of an autoimmune attack mediated by antibodies still is not well-acknowledged in the medical community. Initial evidence that this may occur was reported more that 20 years ago when Hu and Yo antibodies were described in some paraneoplastic neurological syndromes (PNS) and glutamic acid decarboxylase (GAD) antibodies in stiff-person syndrome (SPS) [13]. However, failure to model these disorders in animals prevented clarication of the immunological mechanisms involved in the neuronal damage, and the fact that the antigens were intracellular questioned the pathogenic role of the antibodies. Nevertheless, these antibodies and others described in the next decades were found useful in the diagnosis of PNS [4]. In recent years, the description of antibodies against neuronal surface antigens in patients with paraneoplastic and idiopathic encephalitis has bolstered the concept that antibodies against CNS antigens can
123
510
J Neurol (2010) 257:509517
be pathogenic, indicating that the autoimmune hypothesis of neuronal damage should not be limited to the PNS [5]. On a practical level, the constant description of novel neuronal antibodies and the expanding spectrum of associated symptoms make it difcult for neurologists to decide which antibody or set of antibodies is important for the diagnosis of a given syndrome and which antibodies are markers of PNS or non-cancer related disorders. The aim of this study is to review the neuronal antibodies described in CNS disorders in order to clarify their diagnostic value, emphasize potential pitfalls and limitations in the diagnosis of PNS, and examine the current evidence for a possible pathogenic role. In addition, we propose a classication of neuronal antibodies that may help neurologists in the diagnosis of these disorders. The study is focused only on neuronal antibodies with wellcharacterized target antigens.
as paraneoplastic or non-paraneoplastic markers of CNS syndromes.
Group I: Antibodies against intracellular antigens Group Ia: PNS-related onconeuronal antibodies The term onconeural antibodies was introduced by tumor immunologists to designate antibodies that target antigens present in neuroectodermal tissues and tumors [6]. Concerning PNS, well-characterized onconeural antibodies were dened as those that, in addition to reacting with neural antigens, also present in tumors, served to establish the associated neurological disorder as denite PNS (Table 1). These antibodies are unambiguously demonstrated by standardized tests, associate with limited subsets of tumors, and are present in several CNS syndromes. Some of these syndromes, such as limbic encephalitis, had been known to occur as PNS long before the discovery of onconeural antibodies. However, the discovery of these antibodies facilitates the prompt diagnosis of these disorders and has been crucial for the identication of new PNS. Two examples are chorea associated with CV2 antibodies and the mesodiencephalic encephalitis of patients with Ma2 antibodies [12, 13]. An important issue is that a positive report for any wellcharacterized onconeural antibody has to be assessed
Antineuronal antibodies and CNS autoimmunity We propose to classify the neuronal antibodies associated with syndromes resulting from CNS neuronal dysfunction into two groups according to the location of the antigen: inside the neuron or in the cell membrane. This classication provides an indication of the potential pathogenic role of the antibodies. Additionally, each group of antibodies is further classied according to its diagnostic value
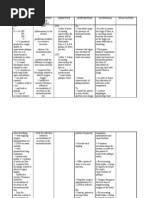
Table 1 Well-characterized onconeuronal antibodies and CNS paraneoplastic neurological syndromes (PNS) Antibody Hu (ANNA1) [7] Predominant tumors Small cell lung cancer (SCLC) CNS syndromes Encephalomyelitis Paraneoplastic cerebellar degeneration (PCD) Limbic encephalitis Brainstem encephalitis CV2 (CRMP5) [8] SCLC, thymoma Encephalomyelitis Chorea PCD Limbic encephalitis Amphiphysin [9] Breast, SCLC Stiff-person syndrome Myelopathy and myoclonus Ri (ANNA2) [10] Yo (PCA1) [11] Ma2 [12]
a
Antibody positive patients without cancera (%) 2
Frequency in cancer without PNSa (%) 16
Breast, SCLC Ovary, breast Testicular
Encephalomyelitis Brainstem encephalitis Opsoclonus myoclonus PCD Limbic encephalitis Brainstem encephalitis
3 2 4
4 1 0
For review see reference [4]
123
J Neurol (2010) 257:509517
511
according to the clinical setting. All these antibodies, particularly those associated with SCLC (Hu, CV2, amphiphysin), can be found in patients with cancer without PNS [14]. Therefore, one should still rule out other potential causes of the neurological syndrome that is being evaluated. This concern increases when the presence of a cancer is already known or when the antibody titers are low. Up to 16% of patients with SCLC without PNS have low titers of Hu antibodies, whereas in patients with PNS and Hu antibodies the titers are substantially higher [15]. A typical example is a patient with SCLC treated with cisplatinum who develops a delayed sensory neuropathy [16]. In this case, the detection of low titer Hu or other onconeural antibody probably reects the presence of the cancer and it cannot be used to support the paraneoplastic origin of the neuropathy, unless other clinical clues exclude a toxic origin. Well-characterized onconeural antibodies are markers of specic subsets of tumors, usually SCLC, breast, ovarian and testicular cancer (Table 1). If another tumor is diagnosed, one cannot establish that the tumor is the cause of the PNS unless the antigen recognized by the onconeural antibody is found expressed in the tumor. If this is not the case, the search for a second neoplasm, directed by the type of onconeural antibody, is warranted. In some PNS, the clinical signicance of the antibodies is difcult to establish. One can argue that the antibodies are unrelated to the PNS and simply indicate a tumorinduced immune response [17]. In this scenario, the PNS could be caused by additional, pathogenically more relevant antibodies against cell surface antigens (see below) [18] or other immunological mechanisms. However, there are at least two important ndings indicating that wellcharacterized onconeural antibodies are not just biological markers of cancer. First, the frequency of these antibodies is much higher in patients with some PNS than in those with isolated cancer (Table 1). For example, the frequency of Yo antibodies is much higher in patients with PCD and ovarian cancer that in patients with ovarian cancer alone or with other PNS associated with ovarian cancer, such as dermatomyositis. Second, and most important, specic intrathecal synthesis has been demonstrated for all types of well-characterized onconeural antibodies associated with PNS of the CNS [19]. This should not occur unless a specic immunologic activation against neuronal antigens operates in the CNS. Despite these data, the direct role of well-characterized onconeural antibodies in the pathogenesis of PNS is unclear. The intracellular location of the antigen and multiple failed attempts to produce an animal model by passive transfer experiments or active vaccination with the antigen strongly suggest these antibodies are not pathogenic [20, 21]. A possible exception is amphiphysin
antibodies. In one study, rats injected with IgG from a patient with SPS and amphiphysin antibodies developed transient spasms and rigidity. Although one cannot rule that other IgG antibodies caused the symptoms, amphiphysin is a protein involved in the recycling of synaptic vesicles, and perhaps it is transiently exposed on the cell membrane to the binding of antibodies [22]. Well-characterized onconeural antibodies probably represent the humoral component of a complex immune response, likely mediated by cytotoxic T cell mechanisms against the same onconeural antigens. This is supported by several lines of evidence: First, postmortem studies demonstrate prominent perivascular and parenchymatous inammatory inltrates [23]. Second, immunophenotyping of the inammatory cells show cytotoxic CD8? T cells in close contact with neurons [24]. Third, Yo- and Hu-specic CD8? cytotoxic T cells are present in the blood of PNS patients, and they can kill target cells in an HLA-restricted manner [25, 26]. Taken together, these data suggest that PNS associated with well-characterized onconeural antibodies resulting from a T cell immune attack against neuronal antigens, probably the same that are targeted by antibodies. This hypothesis awaits conrmation in an animal model. Group Ib: Cancer-related onconeural antibodies Antibodies of this group share with well-characterized onconeural antibodies the recognition of tumor antigens also expressed in the CNS. However, there is no evidence that the immune response (antibodies or associated T cell response) is in any way pathogenically related with the PNS. At present only two antibodies would t in this group, and both recognize antigens (ZIC and SOX families) expressed in SCLC [27, 28]. We do not have evidence of intrathecal synthesis of SOX or ZIC antibodies in patients with PNS. Moreover, the frequency of these antibodies is not higher in patients with PNS than in those with SCLC alone, with the exception of SOX1 antibodies in patients with paraneoplastic Lambert-Eaton myasthenic syndrome (LEMS) (see below), a syndrome caused by antibodies against VGCC [28]. The ZIC genes encode proteins that contain ve zincnger domains. Antibodies against ZIC2 were initially detected by serological analysis of cDNA expression libraries derived from SCLC lines [29]. Antibodies to ZIC4 were subsequently identied in a patient with subacute, severe cerebellar ataxia without cancer [30]. Antibodies against ZIC proteins were found in 15% of patients with PCD and SCLC, an incidence similar (16%) to that of patients with isolated SCLC, and in 29% of patients with different PNS and SCLC [27]. Unlike patients with PCD, many of those with other PNS and ZIC antibodies also had
123
512
J Neurol (2010) 257:509517
Hu or CV2 antibodies [27]. Positive sera of PCD patients reacted with ZIC2, and some also with ZIC1 and ZIC4, suggesting that the immunoreactivity of ZIC antibodies is directed primarily against the conserved zinc-nger domains of ZIC proteins [31]. Although intrathecal synthesis of ZIC4 antibodies was detected in the rst reported case with subacute cerebellar ataxia without cancer, similar studies have not been carried out in patients with PCD and SCLC. Like ZIC antibodies, SOX antibodies were initially detected by serological analysis of cDNA expression libraries derived from SCLC lines [29]. In patients with PNS, SOX antibodies had been rst immunohistochemically described with the term anti-glial nuclear antibody (AGNA), dened by the immunoreaction with the nuclei of the Bergmann glia of the cerebellum [32]. We found a robust association between AGNA and the presence of an underlying SCLC. However, the frequency of AGNA found was higher than expected, for the simple presence of SCLC, in paraneoplastic LEMS (43 vs. 11%) [32]. Because AGNA reactivity is widely expressed in the developing nervous system, we screened a fetal brain library with AGNA positive sera and identied the AGNA antigen as SOX1. SOX1 belongs to a large family of developmental transcription factors that share a highly conserved DNAbinding domain known as the HMG-box, dened by 79 aminoacids [33]. The human SOX gene family is classied in groups from A to H. SOX1 belongs to group B1 along with SOX2 and SOX3 [34]. Patients with SOX1 antibodies may also react with SOX2 and SOX3 proteins, suggesting that the immunoreactivity is directed against epitopes of the conserved HGM box. However, some sera react only against SOX1, indicating that assays that use SOX1 as antigen are the most sensitive to detected antibodies against SOX proteins of the group B1 [35]. Using this strategy, SOX1 antibodies were detected in 64% of patients with LEMS and SCLC but in none of the 50 with idiopathic LEMS [28]. These data indicate that the detection of SOX1 antibodies in patients with LEMS predicts the presence of SCLC and may be used to follow more closely those LEMS patients with no evidence of cancer at the initial work-up. Patients with SCLC and PNS do not have intrathecal synthesis of SOX1 antibodies, indicating that SOX autoimmunity is not involved in the pathogenesis of the PNS. SOX antibodies are found in 36% of patients with isolated SCLC and no difference in survival was observed between SOX positive and SOX negative SCLC patients [36]. Group Ic: Non-paraneoplastic antibodies associated with CNS syndromes Antibodies to GAD, adenylate kinase 5 (AK5), and Homer 3 are representative of this group. GAD antibodies were initially identied in the serum and CSF of patients with
SPS [3, 37]. This syndrome often occurs in association with other autoimmune diseases, mainly type 1 diabetes mellitus (DM1) [38]. This is important, because GAD antibodies are present in about 80% of newly diagnosed DM1 patients, although the levels are usually 100-fold higher in SPS than in DM1 [37]. GAD antibodies were also reported in a subgroup of patients with late onset isolated cerebellar ataxia [39], and a few patients with epilepsy, limbic encephalitis, downbeat nystagmus, palatal tremor, and brainstem dysfunction [40]. In a study focused in 50 patients with high levels of GAD antibodies ([2,000 U/ml by radioimmunoassay), 22 had SPS, 17 cerebellar ataxia, and 11 other neurological disorders (epilepsy 4, PNS 4, limbic encephalitis 2, myasthenia gravis 1) [40]. The frequency of increased intrathecal synthesis of GAD antibodies was 85% in SPS, 100% in cerebellar ataxia, and 86% in other neurological disorders. However, similar serum levels of GAD antibodies were found in 11 patients with DM1 without neurological manifestations. Although the presence of high GAD antibody levels probably suggests that the underlying neurological syndrome may be immunomediated, the observed high frequency of specic intrathecal synthesis support that this analysis should be done to conrm that the GAD autoimmunity is related to the neurological syndrome. This evaluation is particularly important when there is a concomitant DM1 or other autoimmune endocrine syndrome where GAD antibodies could just reect the presence of the associated endocrine disorder. GAD antibodies have been described in a few patients with paraneoplastic SPS associated with thymoma and other solid tumors [41], but their occurrence in patients with classical PNS is less known. Two patients with paraneoplastic encephalomyelitis and PCD had intrathecal synthesis of GAD antibodies, and the tumors expressed GAD. This nding suggests that the immunity raised against the neoexpression of GAD by the tumor may cause a PNS as occurs with classical onconeuronal antibodies [40]. Overall, these data indicate that in patients without DM1 who develop neurological syndromes suggesting a PNS, detection of GAD antibodies does not exclude a paraneoplastic etiology, and therefore cancer screening is warranted. In patients with limbic encephalitis, the signicance of GAD antibodies is unclear for two reasons: [42] the small number of cases reported despite the fact that GAD autoimmunity is relatively common, and the frequent presence of antibodies against cell surface antigens [43], one of them, the GABA(B) receptor, recently reported (see below) [44]. Antibodies to AK5 were identied in two patients with idiopathic LE refractory to immunotherapy [45]. AK5 is specically expressed in the brain, located in the neuronal cytosolic fraction, and has critical neuronal-specic metabolic functions. The absence of theses antibodies in patients with other PNS, or breast cancer or SCLC without
123
J Neurol (2010) 257:509517
513
PNS, suggests that AK5 antibodies are associated with an immune response not related to cancer. As occurs with other immune responses to intracellular antigens, the LE of patients with AK5 antibodies is poorly responsive to treatment. Antibodies to Homer 3 were identied in a patient with cerebellar ataxia of subacute onset and CSF pleocytosis [46]. No cancer has been found after more than 5 years of followup. Homer 3 is predominantly expressed in the dendritic spines of the Purkinje cells. Homer 3 specically binds to the C-termini of mGluR1 and to inositol 1,4,5 triphosphate receptors. This complex is physiologically important for postsynaptic calcium responses to mGluR1 stimulation. The frequency of Homer 3 antibodies in patients with idiopathic subacute cerebellar ataxia is unknown, but they seem to be associated with this clinical prole because they were not detected in other autoimmune cerebellar ataxias, including PCD and lung cancer or Hodgkin disease, and chronic sporadic cerebellar ataxia with or without GAD antibodies [46].
Group II: Antibodies against neuronal surface antigens Group IIa: Markers of the CNS syndrome The antibodies of this group share several characteristics (Table 2). They associate with characteristic CNS
Table 2 Antibodies against neuronal surface antigens Antibody VGKC Tumors (%) Small cell lung cancer (SCLC), thymoma (31) Neurological syndrome Limbic encephalitis Morvans syndrome Creutzfeldt-Jakob disease like syndrome[54] Encephalitis with initial psychiatric features followed by catatonia, dystonia, aphasia and hypoventilation Limbic encephalitis Atypical psychosis Limbic encephalitis
syndromes but their detection does not indicate that the disorder is paraneoplastic. Indeed, the frequency of an underlying tumor varies among the antibody type and is never higher that 70%. The antibodies recognize antigenic epitopes located in the external surface of the neuronal membrane, usually at pre- or post-synaptic sites. Moreover, a pathogenic role of the antibodies is suggested by the response of symptoms to immunotherapy and the correlation between antibody titers and neurological outcome. Antibodies to voltage-gated potassium channels (VGKC) have been associated with non-paraneoplastic limbic encephalitis [47] and case reports of Morvan syndrome [48] or isolated epilepsy [49]. The VGKC antibodyassociated LE is more prevalent in men and usually presents as a classical picture of LE. Rapid eye movement sleep behavior disorder develops at the onset of LE [50]. Hyponatremia is a frequent nding, whereas CSF analysis shows mild pleocytosis in only 41% of the patients (median white cell count 6, range 516 cells) [51]. Serum VGKC antibody levels are high without intrathecal synthesis of the antibody [51]. Probably, the clinical spectrum of CNS disorders associated with VGKC antibodies is wider than previously expected. A recent study showed that 10% of patients had neurological symptoms different from those of LE or diffuse encephalitis and 31% had an underlying tumor, usually lung cancer or thymoma [52].
CSF pleocytosis (%)/IT synthesis 41/no
Method of detection RIAa
Comments Male predominance; associated rapid eye movement (REM) sleep behavior disorder; frequent hiponatremia ([70%) Female predominance; MRI normal in 45%, frequency of tumor higher in patients [18 years old. Female predominance; frequent relapses (60%) Seizures in 86%. Concurrent GAD antibodies in 3 patients Only one patient published. Series published in abstract form [65]
NMDA receptor
Ovarian teratoma (956)
91/yes
Cell based assay
AMPA receptor GABAB receptor
SCLC, breast, thymoma (70) SCLC (47)
90/yes 80/yes
Cell based assay Cell based assay
Glycine receptor
Lung cancer (3)
Progressive encephalomyelitis with rigidity, stiff person syndrome
Unknown
Cell based assay
Cut-off value: 100 pM
However, values between 100 and 400 pM may be seen in 5% of patients without autoimmune neurological disorder [47] VGKC voltage-gated potassium channel
123
514
J Neurol (2010) 257:509517
Unlike other antibodies to cell surface antigens described below, the target antigen of VGKC antibodies has never been directly precipitated by patients antibodies. Moreover, antibodies do not react with cells transfected with the putative antigen (e.g., Kv1 subunit of the VGKC) suggesting that the radioimmunoassay used for antibody detection could in fact be showing antibodies against antigens that coprecipitate with the VGKC, but not against the VGKC themselves. For example, the antibodies of patients with Morvans syndrome and thymoma are directed against contactin-associated protein 2 (CASPR2) a VGKCassociated protein [53]. Whether patients with LE and VGKC antibodies have antibodies to similar proteins is presently unknown. Until recently, only 50% of patients with LE and SCLC were considered antibody positive, usually harbouring Hu or, less frequently, other onconeural antibodies [55]. Recent studies indicate that most cases previously considered seronegative have, in fact, antibodies against neuronal surface antigens [56]. Two of these antibodies have been identied: the GluR1/2 subunits of the AMPA receptor, and the B1 subunit of the GABAB receptor [44, 57]. These two antibodies have in common the association with idiopathic or paraneoplastic LE. Seven of 15 (47%) patients with LE associated with GABAB receptor antibodies had an underlying tumor, usually an SCLC [44]. In LE associated with AMPAR antibodies, the frequency of cancer was 64%, with SCLC being the most common type, followed by thymomas and breast cancer [57]. Some clinical and immunological clues may suggest the type of antibody associated with LE. AMPA receptor antibodies have been almost exclusively identied in women and the LE has a tendency to relapse [57]. Patients with LE and GABABR antibodies present with early and prominent seizures and frequently have other concurrent autoantibodies, particularly against GAD [44]. This overlap is intriguing, as it suggests that some patients with LE attributed to GAD antibodies may have GABAB receptor antibodies as a more plausible cause of the disorder. A severe but treatment-responsive encephalitis has been associated with antibodies to NR1, a crucial subunit of the NMDA receptors [58]. Most patients are children or young women who do not develop the classical picture of LE [59, 60]. They are initially seen or admitted to psychiatric wards for acute anxiety, behavioral change, or psychosis followed in a few days by seizures, decline of consciousness, aphasia, and abnormal movements. Patients may develop hypoventilation and autonomic imbalance that requires admission to intensive care units [59]. The frequency of ovarian teratomas is higher (56%) in women older than 18 years than girls under the age of 14 years (9%). High titers of antibodies signicantly associated with the
presence of a tumor. Despite the severity of the syndrome, often requiring prolonged intensive care support, 75% of patients fully recover or have mild residual decits. Antibody titers (mainly those in the CSF) vary according the clinical outcome [59]. Patients whose tumors are treated promptly (usually along with immunotherapy) have faster and more complete neurological recovery, without relapses, than those who are not treated or only receive immunotherapy either because no tumor is found or it is initially missed [59]. Application of patients NMDA or AMPA receptor antibodies into cultures of rat hippocampal neurons signicantly decreases the number of specic receptor clusters in synapses, an effect that is reversed when patients antibodies are removed or replaced by control human IgG. Moreover, recent studies showed a correlation between antibody titers and the decrease of clusters of NMDA receptors in cultured neurons, as well as in the hippocampus of rats infused with patients antibodies [61]. Overall, these data and the detection of deposits of IgG in the brain of autopsied patients with NMDA receptor encephalitis strongly suggest that these antibodies are probably responsible for the neurological syndrome [62]. Antibodies against the glycine receptor have been reported in a patient with progressive encephalomyelitis with rigidity [63]. This syndrome is considered a variant of stiff-person syndrome characterized by subacute onset of limb and trunk rigidity, muscle spasms, brainstem dysfunction, hyperekplexia, and encephalopathy [64]. This is a severe encephalopathy that may be reversed with immunotherapy. Preliminary work suggests that glycine receptor antibodies could be associated with this rare disorder; the antibodies have also been identied in some patients with isolated hyperekplexia, and a few cases with SPS [65]. Group IIb: Markers of a CNS paraneoplastic syndrome There are two antibodies that can be placed in this group because their presence in a patient with cerebellar ataxia suggest a paraneoplastic origin. Antibodies against the metabotropic glutamate receptor type 1 (mGLuR1) have been described in only two patients with cerebellar ataxia 2 and 9 years after the diagnosis of Hodgkin disease [66]. Intrathecal injection of the IgG of one of the patients into rats caused a transient cerebellar ataxia, suggesting a pathogenic role of the antibody [66, 67]. The long delay between the tumor diagnosis and the cerebellar ataxia suggests mGluR1 antibodies are linked to the neurological syndrome rather than to the tumor. This impression must be conrmed with the description of more patients with mGluR1 antibodies, cerebellar ataxia, and no cancer. If more cases are described, this antibody will likely be reclassied in group Ib.
123
J Neurol (2010) 257:509517
515
Antibodies to P/Q type voltage-gated calcium channels (VGCC) are associated with Lambert-Eaton myasthenic syndrome (LEMS) and are responsible for the syndrome [68]. The clinical observation that some LEMS patients also have cerebellar ataxia and the demonstration of P/Q type VGCC in Purkinje cells raised the question of whether these antibodies could be involved in cases of isolated cerebellar ataxia. Increased levels of P/Q type VGCC antibodies were found in 16 (41%) of 39 patients with paraneoplastic cerebellar degeneration (PCD) and lung cancer. Only seven of the 16 patients had an associated LEMS [69]. In contrast, patients with non-paraneoplastic cerebellar ataxia usually do not harbor VGCC antibodies or do so at low levels [70]. Therefore, the detection of P/Q type VGCC antibodies in a patient with cerebellar ataxia, associated or not with LEMS, strongly indicates the presence of an underlying lung cancer. The pathogenic role of VGCC antibodies in PCD is unclear despite the observation of loss of P/Q type VGCC in postmortem studies of cerebellums of patients with PCD and LEMS [71]. Unlike other syndromes associated with neuronal surface receptor antibodies, the cerebellar ataxia does not improve with immunotherapy either because the Purkinje cells are irreversibly damaged at early stage of the syndrome, or because the treatments used are unable to remove the pathogenic antibodies.
Experience with the recently described antibodies, with exception of those against NMDAR, is still relatively small. Therefore, their inclusion in one particular group of the proposed classication must we viewed with caution until more cases are described. Good clinical-immunological correlations are crucial to dene the clinical syndrome that most likely associates with a particular antibody. Researchers in this eld must provide good clinical descriptions of the case series associated with the antibody they study. This approach will help clinicians to identify the clinical syndromes and to make a rational decision on which antibodies to request.
Acknowledgments This study was supported in part by grant PS09/ 00193 Fondo de Investigaciones Sanitarias, Madrid, Spain. Conict of interest statement None.
References
1. Greenlee JE, Brashear HR (1983) Antibodies to cerebellar Purkinje cells in patients with paraneoplastic cerebellar degeneration and ovarian carcinoma. Ann Neurol 14:609613 2. Graus F, Cordon-Cardo C, Posner JB (1985) Neuronal antinuclear antibody in sensory neuronopathy from lung cancer. Neurology 35:538543 3. Solimena M, Folli F, Denis-Donini S, Comi GC, Pozza G, De Camilli P, Vicari AM (1988) Autoantibodies to glutamic acid decarboxylase in a patient with stiff-man syndrome, epilepsy, and Type I diabetes mellitus. N Engl J Med 318:10121020 4. Graus F, Delattre JY, Antoine JC, Dalmau J, Giometto B, Grisold W, Honnorat J, Smitt PS, Vedeler Ch, Verschuuren JJ, Vincent A, Voltz R (2004) Recommended diagnostic criteria for paraneoplastic neurological syndromes. J Neurol Neurosurg Psychiatry 75:11351140 5. Dalmau J, Rosenfeld MR (2008) Paraneoplastic syndromes of the CNS. Lancet Neurol 7:327340 6. Seeger RC, Zeltzer PM, Rayner SA (1979) Onco-neural antigen: a new neural differentiation antigen expressed by neuroblastoma, oat cell carcinoma, Wilms tumor, and sarcoma cells. J Immunol 722:15481555 e R, Benyahia B, Ribalta T, 7. Graus F, Keime-Guibert F, Ren Ascaso C, Escaramis G, Delattre JY (2001) Anti-Hu-associated paraneoplastic encephalomyelitis: analysis of 200 patients. Brain 124:11381148 8. Honnorat J, Antoine JC, Derrington E, Aguera M, Belin MF (1996) Antibodies to a subpopulation of glial cells and a 66 kDa developmental protein in patients with paraneoplastic neurological syndromes. J Neurol Neurosurg Psychiatry 61:270 278 9. Pittock SJ, Lucchinetti CF, Parisi JE, Benarroch EE, Mokri B, Stephan CL, Kim KK, Kilimann MW, Lennon VA (2005) Amphiphysin autoimmunity: paraneoplastic accompaniments. Ann Neurol 58:96107 10. Pittock SJ, Lucchinetti CF, Lennon VA (2003) Anti-neuronal nuclear autoantibody type 2: paraneoplastic accompaniments. Ann Neurol 53:580587 11. Peterson K, Rosenblum MK, Posner JB (1992) Paraneoplastic cerebellar degeneration: a clinical analysis of 55 anti-Yo antibody-positive patients. Neurology 42:19311937
Final comments In a few years the number of antineuronal antibodies described in CNS disorders has increased dramatically. There are two important features that differentiate most of the novel antibodies from previous antineuronal antibodies: rst, they are directed against cell surface or synaptic proteins, and second, the target antigens are relevant receptors involved in wellknown mechanisms of synaptic transmission or plasticity. Screening by immunohistochemistry on rat brain sections may detect most of these antibodies, but these studies do not confer specicity. This is based on direct immunoprecipitation of the antigen and, once it is characterized, the development of cell based assays specically expressing the antigen. Indirect immunoprecipitation techniques, such as those used for the VGKC antibodies, although may be useful as a diagnostic test do not necessarily provide the main target antigen. Future studies must address the sensitivity and specicity of immunohistochemistry to screen these novel antibodies in a way similar to what has been done with anti-aquaporin-4 (NMO-IgG) antibodies [72] and to conrm by the specic cell based assays only the positive samples. This approach, if feasible, would be more practical and cheaper than to initially analyze all the samples by the different cell based assays.
123
516 12. Dalmau J, Graus F, Villarejo A, Posner JB, Blumenthal D, Thiessen B, Saiz A, Meneses P, Rosenfeld MR (2004) Clinical analysis of anti-Ma2-associated encephalitis. Brain 127:1831 1844 13. Vernino S, Tuite P, Adler CH, Meschia JF, Boeve BF, Boasberg P, Parisi JE, Lennon VA (2002) Paraneoplastic chorea associated with CRMP-5 neuronal antibody and lung carcinoma. Ann Neurol 51:625630 14. Monstad SE, Knudsen A, Salvesen HB, Aarseth JH, Vedeler CA (2009) Onconeural antibodies in sera from patients with various types of tumours. Cancer Immunol Immunother 58:17951800 R, Tora M, Malats N, Verschuuren JJ, e 15. Graus F, Dalmau J, Ren olas N, Garcia del Muro J, Vadell C, Mason WP, Cardenal F, Vin Rosell R, Posner JB, Real FX (1997) Anti-Hu antibodies in patients with small-cell lung cancer: association with complete response to therapy and improved survival. J Clin Oncol 15:28662872 16. Mollman JE, Hogan WM, Glover DJ, McCluskey LF (1988) Unusual presentation of cis-platinum neuropathy. Neurology 38:488490 17. Pittock SJ, Kryzer TJ, Lennon VA (2004) Paraneoplastic antibodies coexist and predict cancer, not neurological syndrome. Ann Neurol 56:715719 18. Zuliani L, Saiz A, Tavolato B, Giometto B, Vincent A, Graus F (2007) Paraneoplastic limbic encephalitis associated with potassium channel antibodies: value of anti-glial nuclear antibodies in identifying the tumour. J Neurol Neurosurg Psychiatry 78:204205 19. Stich O, Jarius S, Kleer B, Rasiah C, Voltz R, Rauer S (2007) Specic antibody index in cerebrospinal uid from patients with central and peripheral paraneoplastic neurological syndromes. J Neuroimmunol 183:220224 20. Graus F, Illa I, Agusti M, Ribalta T, Cruz-Sanchez F, Juarez C (1991) Effect of intraventricular injection of an anti-Purkinje cell antibody (anti-Yo) in a guinea pig model. J Neurol Sci 106:8287 21. Carpentier AF, Rosenfeld MR, Delattre JY, Whalen RG, Posner JB, Dalmau J (1998) DNA vaccination with HuD inhibits growth of a neuroblastoma in mice. Clin Cancer Res 4:28192824 22. Sommer C, Weishaupt A, Brinkhoff J, Biko L, Wessig C, Gold R, Toyka KV (2005) Paraneoplastic stiff-person syndrome: passive transfer to rats by means of IgG antibodies to amphiphysin. Lancet 365:14061411 23. Jean WC, Dalmau J, Ho A, Posner JB (1994) Analysis of the IgG subclass distribution and inammatory inltrates in patients with anti-Hu-associated paraneoplastic encephalomyelitis. Neurology 44:140147 A, Saiz A, Benyahia B, Ribalta T 24. Bernal F, Graus F, Pifarre (2002) Immunohistochemical analysis of anti-Hu-associated paraneoplastic encephalomyelitis. Acta Neuropathol 103:509 515 25. Albert ML, Austin LM, Darnell RB (2000) Detection and treatment of activated T cells in the cerebrospinal uid of patients with paraneoplastic cerebellar degeneration. Ann Neurol 47:917 26. Roberts WK, Deluca IJ, Thomas A, Fak J, Williams T, Buckley N, Dousmanis AG, Posner JB, Darnell RB (2009) Patients with lung cancer and paraneoplastic Hu syndrome harbor HuD-specic type 2 CD8? T cells. J Clin Invest 119:20422051 27. Bataller L, Wade DF, Graus F, Stacey HD, Rosenfeld MR, Dalmau J (2004) Antibodies to Zic4 in paraneoplastic neurologic disorders and small-cell lung cancer. Neurology 62:778782 re AO, Graus F 28. Sabater L, Titulaer M, Saiz A, Verschuuren J, Gu (2008) SOX1 antibodies are markers of paraneoplastic LambertEaton myasthenic syndrome. Neurology 70:924928 ger D, Altorki re AO, Stockert E, Scanlan MJ, Keresztes RS, Ja 29. Gu NK, Old LJ, Chen YT (2000) Serological identication of embryonic neural proteins as highly immunogenic tumor antigens in small cell lung cancer. Proc Natl Acad Sci USA 97:41984203
J Neurol (2010) 257:509517 30. Bataller L, Wade DF, Fuller GN, Rosenfeld MR, Dalmau J (2002) Cerebellar degeneration and autoimmunity to zinc-nger proteins of the cerebellum. Neurology 59:19851987 rez-Calvet M, Saiz A, Dalmau J, Graus 31. Sabater L, Bataller L, Sua F (2008) ZIC antibodies in paraneoplastic cerebellar degeneration and small cell lung cancer. J Neuroimmunol 201202:163165 32. Graus F, Vincent A, Pozo-Rosich P, Sabater L, Saiz A, Lang B, Dalmau J (2005) Anti-glial nuclear antibody: marker of lung cancer-related paraneoplastic neurological syndromes. J Neuroimmunol 165:166171 33. Wegner M, Stolt CC (2005) From stem cells to neurons and glia: a Soxists view of neural development. Trends Neurosci 28:583588 34. Schepers GE, Teasdale RD, Koopman P (2002) Twenty pairs of Sox: extent, homology, and nomenclature of the mouse and human Sox transcriptor factor gene families. Dev Cell 3:167170 35. Vural B, Chen LC, Saip P, Chen YT, Ustuner Z, Gonen M, Simpson AJ, Old LJ, Ozbek U, Gure AO (2005) Frequency of SOX Group B (SOX1, 2, 3) and ZIC2 antibodies in Turkish patients with small cell lung carcinoma and their correlation with clinical parameters. Cancer 103:25752583 36. Titulaer MJ, Klooster R, Potman M, Sabater L, Graus F, Hegeman IM, Thijssen PE, Wirtz PW, Twijnstra A, Smitt PA, van der Maarel SM, Verschuuren JJ (2009) SOX antibodies in small-cell lung cancer and Lambert-Eaton myasthenic syndrome: frequency and relation with survival. J Clin Oncol 27:42604267 37. Solimena M, Folli F, Aparisi R, Pozza G, De Camilli P (1990) Autoantibodies to GABA-ergic neurons and pancreatic beta cells in stiff-man syndrome. N Engl J Med 322:15501560 38. Baekkeskov S, Aanstoot HJ, Christgau S, Reetz A, Solimena M, Cascalho M, Folli F, Richter-Olesen H, De Camilli P (1990) Identication of the 64K autoantigen in insulin-dependent diabetes as the GABA-synthesizing enzyme glutamic acid decarboxylase. Nature 347:151156 s 39. Honnorat J, Saiz A, Giometto B, Vincent A, Brieva L, de Andre C, Maestre J, Fabien N, Vighetto A, Casamitjana R, Thivolet C, Tavolato B, Antoine CA, Graus F (2001) Cerebellar ataxia with anti-glutamic acid decarboxylase antibodies. Arch Neurol 58:225230 40. Saiz A, Blanco Y, Sabater L, Gonzalez F, Bataller L, Casamitjana -Torrenta ` L, Graus F (2008) Spectrum of neurological R, Ramio syndromes associated with glutamic acid decarboxylase antibodies: diagnostic clues for this association. Brain 131:2553 2563 41. McHugh JC, Murray B, Renganathan R, Connolly S, Lynch T (2007) GAD antibody positive paraneoplastic stiff person syndrome in a patient with renal cell carcinoma. Mov Disord 22:13431346 ` S, Muscas GC, Naldi I, Rosati E, Paladini S, Cruciatti B, 42. Mata Bisulli F, Paganini M, Mazzi G, Sorbi S, Tinuper P (2008) Nonparaneoplastic limbic encephalitis associated with anti-glutamic acid decarboxylase antibodies. J Neuroimmunol 199:155159 43. Ances BM, Vitaliani R, Taylor RA, Liebeskind DS, Voloschin A, Houghton DJ, Galetta SL, Dichter M, Alavi A, Rosenfeld MR, Dalmau J (2005) Treatment-responsive limbic encephalitis identied by neuropil antibodies: MRI and PET correlates. Brain 128:17641777 44. Lancaster E, Lai M, Peng X, Hughes E, Contastinescu R, Raizer J, Friedman D, Skeen MB, Grisold W, Kimura A, Ohta K, Iizuka n M, Graus F, Moss SJ, Balice-Gordon R, Dalmau J T, Guzma (2010) The GABAB receptor is a novel autoantigen of limbic encephalitis with prominent seizures: a case series and characterization of the antigen. Lancet Neurol 9:6776 zun E, Rossi JE, Karner SF, Centurion AF, Dalmau J (2007) 45. Tu Adenilate kinase 5 autoimmunity in treatment refractory limbic encephalitis. J Neuroimmunol 186:177180
123
J Neurol (2010) 257:509517 46. Zuliani L, Sabater L, Saiz A, Baiges JJ, Giometto B, Graus F (2007) Homer 3 autoimmunity in subacute idiopathic cerebellar ataxia. Neurology 68:239240 47. Vincent A, Buckley C, Schott JM, Baker I, Dewar BK, Detert N, Clover L, Parkinson A, Bien CG, Omer S, Lang B, Rossor MN, Palace J (2004) Potassium channel antibody-associated encephalopathy: a potentially immunotherapy-responsive form of limbic encephalitis. Brain 127:701712 48. Liguori R, Vincent A, Clover L, Avoni P, Plazzi G, Cortelli P, Baruzzi A, Carey T, Gambetti P, Lugaresi E, Montagna P (2001) Morvans syndrome: peripheral and central nervous system and cardiac involvement with antibodies to voltage-gated potassium channels. Brain 124:24172426 49. Irani SR, Buckley C, Vincent A, Cockerell OC, Rudge P, Johnson MR, Smith S (2008) Immunotherapy-responsive seizure-like episodes with potassium channel antibodies. Neurology 71:16471648 50. Iranzo A, Graus F, Clover L, Morera J, Bruna J, Vilar C, nez-Rodriguez JE, Vincent A, Santamar a J (2006) Rapid Mart eye movement sleep behavior disorder and potassium channel antibody-associated limbic encephalitis. Ann Neurol 59:178181 51. Jarius S, Hoffmann L, Clover L, Vincent A, Voltz R (2008) CSF ndings in patients with voltage gated potassium channel antibody associated limbic encephalitis. J Neurol Sci 268:7477 52. Tan KM, Lennon VA, Klein CJ, Boeve BF, Pittock SJ (2008) Clinical spectrum of voltage-gated potassium channel autoimmunity. Neurology 70:18831890 53. Vincent A (2009) Antibodies to contactin-associated protein 2 (CASPR2) in thymoma and Morvans syndrome. Ann Neurol 66(suppl 13): S3(abstract) 54. Geschwind MD, Tan KM, Lennon VA, Barajas RF Jr, Haman A, Klein CJ, Josephson SA, Pittock SJ (2008) Voltage-gated potassium channel autoimmunity mimicking Creutzfeldt-Jakob disease. Arch Neurol 65:13411346 R, Bescansa E, Delattre e 55. Alamowitch S, Graus F, Uchuya M, Ren JY (1997) Limbic encephalitis and small cell lung cancer. Clinical and immunological features. Brain 120:923928 pez F, Sabater L, Blanco Y, 56. Graus F, Saiz A, Lai M, Bruna J, Lo Rey MJ, Ribalta T, Dalmau J (2008) Neuronal surface antigen antibodies in limbic encephalitis: clinical-immunologic associations. Neurology 71:930936 ` 57. Lai M, Hughes EG, Peng X, Zhou L, Gleichman AJ, Shu H, Mata S, Kremens D, Vitaliani R, Geschwind MD, Bataller L, Kalb RG, Davis R, Graus F, Lynch DR, Balice-Gordon R, Dalmau J (2009) AMPA receptor antibodies in limbic encephalitis alter synaptic receptor location. Ann Neurol 65:424434 zu n E, Wu HY, Masjuan J, Rossi JE, Voloschin A, 58. Dalmau J, Tu Baehring JM, Shimazaki H, Koide R, King D, Mason W, Sansing LH, Dichter MA, Rosenfeld MR, Lynch DR (2007) Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol 61:2536 59. Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M, Dessain SK, Rosenfeld MR, Balice-Gordon R, Lynch DR (2008) Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 7:10911098
517 60. Florance NR, Davis RL, Lam C, Szperka C, Zhou L, Ahmad S, Campen CJ, Moss H, Peter N, Gleichman AJ, Glaser CA, Lynch DR, Rosenfeld MR, Dalmau J (2009) Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis in children and adolescents. Ann Neurol 66:1118 61. Hughes BA, Peng X, Gleichman AJ, Lai M, Zhou L, Tsou R, Parsons TD, Lynch DR, Dalmau J, Balice-Gordon R (2009) Cellular and synaptic mechanisms underlying anti-NMDA receptor encephalitis. Ann Neurol 66(Suppl 13):S63S64 zu n E, Zhou L, Baehring JM, Bannykh S, Rosendfeld MR, 62. Tu Dalmau J (2009) Evidence for antibody-mediated pathogenesis in anti-NMDAR encephalitis associated with ovarian teratoma. Acta Neuropathol. doi:10.1007/s00401-009-0582-4 63. Hutchinson M, Waters P, McHugh J, Gorman G, ORiordan S, Connolly S, Hager H, Yu P, Becker CM, Vincent A (2008) Progressive encephalomyelitis, rigidity, and myoclonus: a novel glycine receptor antibody. Neurology 71:12911292 64. Whiteley AM, Swash M, Urich H (1976) Progressive encephalomyelitis with rigidity. Brain 99:2742 65. Vincent A, Leite MI, Waters P, Jacobi Ch, Becker CM, Meinck HM (2009) Glycine receptor antibodies in progressive encephalomyelitis with rigidity and myoclonus, hyperekplexia and stiff person syndrome. Ann Neurol 66(suppl 13):S50(abstract) 66. Sillevis Smitt P, Kinoshita A, De Leeuw B, Moll W, Coesmans M, Jaarsma D, Henzen-Logmans S, Vecht C, De Zeeuw C, Sekiyama N, Nakanishi S, Shigemoto R (2000) Paraneoplastic cerebellar ataxia due to autoantibodies against a glutamate receptor. N Engl J Med 342:2127 67. Coesmans M, Smitt PA, Linden DJ, Shigemoto R, Hirano T, Yamakawa Y, van Alphen AM, Luo C, van der Geest JN, Kros JM, Gaillard CA, Frens MA, de Zeeuw CI (2003) Mechanisms underlying cerebellar motor decits due to mGluR1-autoantibodies. Ann Neurol 53:325336 68. Motomura M, Lang B, Johnston I, Palace J, Vincent A, NewsomDavis J (1997) Incidence of serum anti-P/O-type and anti-N-type calcium channel autoantibodies in the Lambert-Eaton myasthenic syndrome. J Neurol Sci 147:3542 69. Graus F, Lang B, Pozo-Rosich P, Saiz A, Casamitjana R, Vincent A (2002) P/Q type calcium-channel antibodies in paraneoplastic cerebellar degeneration with lung cancer. Neurology 59:764766 rk K, Wick M, Roth G, Decker P, Voltz R (2009) Antineuronal 70. Bu antibodies in sporadic late-onset cerebellar ataxia. J Neurol. doi: 10.1007/s00415-009-5262-8 71. Fukuda T, Motomura M, Nakao Y, Shiraishi H, Yoshimura T, Iwanaga K, Tsujihata M, Eguchi K (2003) Reduction of P/Q-type calcium channels in the postmortem cerebellum of paraneoplastic cerebellar degeneration with Lambert-Eaton myasthenic syndrome. Ann Neurol 53:2128 72. McKeon A, Fryer JP, Apiwattanakul M, Lennon VA, Hinson SR, Kryzer TJ, Lucchinetti CF, Weinshenker BG, Wingerchuk DM, Shuster EA, Pittock SJ (2009) Diagnosis of neuromyelitis spectrum disorders: comparative sensitivities and specicities of immunohistochemical and immunoprecipitation assays. Arch Neurol 66:11341138
123
You might also like
- PLAB 2 List of PhrasesDocument4 pagesPLAB 2 List of Phrasesshuvo786100% (4)
- A Case of Vasa Previa Diagnosed PrenatallyDocument5 pagesA Case of Vasa Previa Diagnosed PrenatallydeadcorpsesNo ratings yet
- English TaskDocument6 pagesEnglish Taskwa ode wulanNo ratings yet
- In Vitro Bacterial Penetration of Coronally UnsealedDocument4 pagesIn Vitro Bacterial Penetration of Coronally UnsealedAlejandro Junior GarayNo ratings yet
- Paraneoplastic Neurologic Syndromes: Myrna R. Rosenfeld, MD, PHD A, Josep Dalmau, MD, PHD BDocument25 pagesParaneoplastic Neurologic Syndromes: Myrna R. Rosenfeld, MD, PHD A, Josep Dalmau, MD, PHD Banton MDNo ratings yet
- Jurnal CA SarafDocument13 pagesJurnal CA SarafAydhing Nathasya JapNo ratings yet
- PARANEOPLASTICDocument8 pagesPARANEOPLASTICMuhammad Imran MirzaNo ratings yet
- Encefalitis Autoinmune 2022Document18 pagesEncefalitis Autoinmune 2022Pablo Sebastián SaezNo ratings yet
- 2022 Article 1184Document16 pages2022 Article 1184Muhammad Imran MirzaNo ratings yet
- Encefalitis AutoinmuneDocument18 pagesEncefalitis AutoinmunealmarazneurologiaNo ratings yet
- APT 2014 Rickards 92 100Document10 pagesAPT 2014 Rickards 92 100Karam Ali ShahNo ratings yet
- Autoimmune Encephalitis Review (Lancet 2016)Document14 pagesAutoimmune Encephalitis Review (Lancet 2016)tjelongNo ratings yet
- Pembrolizumab Treatment For Progressive Multifocal LeukoencephalopathyDocument8 pagesPembrolizumab Treatment For Progressive Multifocal LeukoencephalopathyAnonymous Kv0sHqFNo ratings yet
- Encefalite AutoimuneDocument14 pagesEncefalite AutoimuneAlina AndreiNo ratings yet
- The Management of Encephalitis: Clinical Practice Guidelines by The Infectious Diseases Society of AmericaDocument25 pagesThe Management of Encephalitis: Clinical Practice Guidelines by The Infectious Diseases Society of AmericaomartorigalNo ratings yet
- Management of EncephalitisDocument25 pagesManagement of EncephalitisOWintero OWarmoNo ratings yet
- Antibodies and Neuronal Autoimmune Disorders of The CNS.: Gra1uus F Saiz A Dalmau JDocument3 pagesAntibodies and Neuronal Autoimmune Disorders of The CNS.: Gra1uus F Saiz A Dalmau JAlejandro Guerrero LeónNo ratings yet
- Encephalitis and Aseptic Meningitis: Short-Term and Long-Term Outcome, Quality of Life and Neuropsychological FunctioningDocument9 pagesEncephalitis and Aseptic Meningitis: Short-Term and Long-Term Outcome, Quality of Life and Neuropsychological FunctioningRoberto SoehartonoNo ratings yet
- MOG Antibody-Associated DiseasesDocument3 pagesMOG Antibody-Associated DiseasesYassmin ElNazerNo ratings yet
- HHS Public Access: Autoimmune EncephalopathiesDocument33 pagesHHS Public Access: Autoimmune EncephalopathiesLink BuiNo ratings yet
- Autoimmune EncephalitisDocument10 pagesAutoimmune EncephalitisMagda CabralesNo ratings yet
- Paraneoplastic Syndromes of The Peripheral NervesDocument6 pagesParaneoplastic Syndromes of The Peripheral NervesValen RoldánNo ratings yet
- The Management of Encephalitis: Clinical Practice Guidelines by The Infectious Diseases Society of AmericaDocument25 pagesThe Management of Encephalitis: Clinical Practice Guidelines by The Infectious Diseases Society of AmericaVictor Euclides Briones MoralesNo ratings yet
- The Management of Encephalitis: Clinical Practice Guidelines by The Infectious Diseases Society of AmericaDocument25 pagesThe Management of Encephalitis: Clinical Practice Guidelines by The Infectious Diseases Society of AmericaJosephNo ratings yet
- Birnbaum 2018 - Sdr. Sjogren - AnticorpiDocument17 pagesBirnbaum 2018 - Sdr. Sjogren - AnticorpiSimina BarbuNo ratings yet
- Encefaliti AutoimmuniDocument12 pagesEncefaliti AutoimmuniLallo CuluNo ratings yet
- Sindrome Paraneoplasico Neurologico NejmDocument12 pagesSindrome Paraneoplasico Neurologico NejmFernando Rodriguez BayonaNo ratings yet
- Autoimmune Encephalitis With Antibodies 2023Document14 pagesAutoimmune Encephalitis With Antibodies 2023ctsakalakisNo ratings yet
- Armangue2014Document8 pagesArmangue2014etiyaNo ratings yet
- Diagnostic CriteriaDocument12 pagesDiagnostic CriteriaBenjamin NgNo ratings yet
- Immune Mediated Pediatric Encephalitis - Need For Comprehensive Evaluation and Consensus GuidelinesDocument8 pagesImmune Mediated Pediatric Encephalitis - Need For Comprehensive Evaluation and Consensus GuidelinesJudit SzamosujvariNo ratings yet
- Autoimmune Encephalitis: Proposed Best Practice Recommendations For Diagnosis and Acute ManagementDocument12 pagesAutoimmune Encephalitis: Proposed Best Practice Recommendations For Diagnosis and Acute ManagementSafitri MuhlisaNo ratings yet
- 19 Full-1Document15 pages19 Full-1Dionisio Garcia AlvarezNo ratings yet
- Encefalite Autoimune Soronegativa - June 2023Document12 pagesEncefalite Autoimune Soronegativa - June 2023FernandoNo ratings yet
- Journal ReadingDocument15 pagesJournal ReadingUsmel RamadhaniaNo ratings yet
- 2019 Autoimmune EncephalitidesDocument23 pages2019 Autoimmune EncephalitidesNeurologia homicNo ratings yet
- Nihms 202712Document16 pagesNihms 202712siddhi divekarNo ratings yet
- Clin Infect Dis.-2008-Tunkel-ENCEFALITISDocument25 pagesClin Infect Dis.-2008-Tunkel-ENCEFALITISJizus GonzalezNo ratings yet
- Autoimmune EncephalitisDocument9 pagesAutoimmune EncephalitisDini Fajriah OmariNo ratings yet
- Jarius 2014Document16 pagesJarius 2014ezradamanikNo ratings yet
- Autoimmune EncephalitisDocument14 pagesAutoimmune EncephalitisMarco Antonio KoffNo ratings yet
- Profound Olfactory Dysfunction in Myasthenia GravisDocument5 pagesProfound Olfactory Dysfunction in Myasthenia GravisAngie Sidney Naranjo GarciaNo ratings yet
- Leypoldt2014Document21 pagesLeypoldt2014etiyaNo ratings yet
- Neuromyelitisoptica: Sarah L. Patterson,, Sarah E. GoglinDocument13 pagesNeuromyelitisoptica: Sarah L. Patterson,, Sarah E. GoglinErji K.No ratings yet
- 1 s2.0 S0169500220303986 Main PDFDocument10 pages1 s2.0 S0169500220303986 Main PDFsandra rojas ducuaraNo ratings yet
- Autoimmunemeningitisand Encephalitis: Megan B. RichieDocument20 pagesAutoimmunemeningitisand Encephalitis: Megan B. RichieJuan Felipe Quintero MorenoNo ratings yet
- Steiner2010 PDFDocument14 pagesSteiner2010 PDFLilisNo ratings yet
- Seizure in SLE PatientDocument7 pagesSeizure in SLE PatientdivisiimunNo ratings yet
- Ref 14Document8 pagesRef 14Tiago BaraNo ratings yet
- Autoimmune Encephalitis Best PracticeDocument12 pagesAutoimmune Encephalitis Best PracticeKatrina San GilNo ratings yet
- NLR Bells PalsyDocument4 pagesNLR Bells PalsyIskandar HasanNo ratings yet
- Autoimmune Encephalitis: Frequency and Prognosis: A. Al Ansari N. P. RobertsonDocument3 pagesAutoimmune Encephalitis: Frequency and Prognosis: A. Al Ansari N. P. RobertsonNathaly CantorNo ratings yet
- Nej MR A 1216008Document11 pagesNej MR A 1216008guillosarahNo ratings yet
- Antibody-Mediated EncephalitisDocument12 pagesAntibody-Mediated EncephalitisOlga Manco GuzmánNo ratings yet
- Encefalitis AutoinmuneDocument8 pagesEncefalitis AutoinmuneRoosevelt Santibañez Dla TorreNo ratings yet
- 757 FullDocument16 pages757 FullDara Purnamasari DersyaNo ratings yet
- Encef Limbica 5Document10 pagesEncef Limbica 5Carolina MuñozNo ratings yet
- Ref 12Document12 pagesRef 12Tiago BaraNo ratings yet
- Neuroinmunidad y tb10.1007@s12264-019-00403-7Document13 pagesNeuroinmunidad y tb10.1007@s12264-019-00403-7fededelveliNo ratings yet
- The Diagnosis and Treatment of Autoimmune Encephalitis JCN 2016Document13 pagesThe Diagnosis and Treatment of Autoimmune Encephalitis JCN 2016Alex Del PieroNo ratings yet
- KBM0701 Stern 21Document6 pagesKBM0701 Stern 21Agus WijataNo ratings yet
- Ref 9Document25 pagesRef 9Tiago BaraNo ratings yet
- Paraneoplastic Syndromes in Small Cell Lung CancerDocument11 pagesParaneoplastic Syndromes in Small Cell Lung CancerFebri Dwi HaryonoNo ratings yet
- Neuroimmunology: Multiple Sclerosis, Autoimmune Neurology and Related DiseasesFrom EverandNeuroimmunology: Multiple Sclerosis, Autoimmune Neurology and Related DiseasesAmanda L. PiquetNo ratings yet
- Cell Tracking in Cardiac RepairDocument16 pagesCell Tracking in Cardiac RepairdeadcorpsesNo ratings yet
- Dual Energy CTDocument11 pagesDual Energy CTdeadcorpsesNo ratings yet
- Organizing PneumoniaDocument11 pagesOrganizing PneumoniadeadcorpsesNo ratings yet
- Breast Tomosynthesis in Clinical PracticeDocument9 pagesBreast Tomosynthesis in Clinical PracticedeadcorpsesNo ratings yet
- P ('t':'3', 'I':'669333659') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Document6 pagesP ('t':'3', 'I':'669333659') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)deadcorpsesNo ratings yet
- What Is Depression in Epilepsy?: Christian E. Elger and Christian HoppeDocument3 pagesWhat Is Depression in Epilepsy?: Christian E. Elger and Christian HoppedeadcorpsesNo ratings yet
- Twin Force Bite CorrectorDocument26 pagesTwin Force Bite CorrectorMohammed ElgendyNo ratings yet
- Asthma & COPDDocument26 pagesAsthma & COPDraheenbushNo ratings yet
- D.T.max The Secrets of SleepDocument23 pagesD.T.max The Secrets of Sleepbritties69No ratings yet
- Core Procedures - Guidance For Assessors and Foundation DoctorsDocument10 pagesCore Procedures - Guidance For Assessors and Foundation DoctorsadybutucNo ratings yet
- Skill 103 Administering A Large-Volume Cleansing EnemaDocument3 pagesSkill 103 Administering A Large-Volume Cleansing EnemaHarley Justiniani Dela CruzNo ratings yet
- Visual FieldsDocument86 pagesVisual FieldsoptorameshgpNo ratings yet
- Sandeep Patterns of NursingDocument12 pagesSandeep Patterns of NursingKamlesh Kalal100% (1)
- Medical IdiomsDocument14 pagesMedical IdiomsLeidy RodriguezNo ratings yet
- Umbilical Cord ProlapseDocument19 pagesUmbilical Cord ProlapsedenekeNo ratings yet
- Don't Hope, Decide!: 191 Comments Marriage Motivational StoriesDocument10 pagesDon't Hope, Decide!: 191 Comments Marriage Motivational StoriesDwiNo ratings yet
- ThyroidectomyDocument52 pagesThyroidectomyWindelyn Gamaro100% (4)
- (Current Clinica (Current - Clinical - Strategies) - Gynecology - and - Obstetrics - 2004l Strategies) - Gynecology and Obstetrics 2004Document125 pages(Current Clinica (Current - Clinical - Strategies) - Gynecology - and - Obstetrics - 2004l Strategies) - Gynecology and Obstetrics 2004Eliza Stochita100% (1)
- ContractedDocument15 pagesContractedswapnil3250No ratings yet
- CRRT Guidelines RenalDocument5 pagesCRRT Guidelines Renalanon_361066654100% (1)
- 563 Methotrexate AlertDocument4 pages563 Methotrexate AlertKenef CheungNo ratings yet
- NCP-Dengue Hemorrhagic FeverDocument8 pagesNCP-Dengue Hemorrhagic Feverjunrey1990No ratings yet
- The Effect of Late Pregnancy Consumption of Date Fruit On Labour andDocument3 pagesThe Effect of Late Pregnancy Consumption of Date Fruit On Labour andnindya100% (1)
- AAnch HospitalDocument8 pagesAAnch HospitalAANCH hospitalNo ratings yet
- IntJPedodRehabil2260-4247839 114758Document6 pagesIntJPedodRehabil2260-4247839 114758anna handayaniNo ratings yet
- Patient Education PlanDocument4 pagesPatient Education Planapi-248022066No ratings yet
- Medicine NuggetsDocument12 pagesMedicine NuggetsFiaz medicoNo ratings yet
- Book Understanding PainDocument44 pagesBook Understanding PainsnaggletooothNo ratings yet
- Jawaban Latihan Soal Bahasa InggrisDocument12 pagesJawaban Latihan Soal Bahasa InggrisErlianaMargaLena0% (1)
- Norton Presure Sore Risk Assessment Scale PDFDocument1 pageNorton Presure Sore Risk Assessment Scale PDFchrisyenNo ratings yet
- NCP For Ineffective Airway ClearanceDocument3 pagesNCP For Ineffective Airway ClearanceJennelyn BayleNo ratings yet
- Document PDFDocument12 pagesDocument PDFEviNo ratings yet