Professional Documents
Culture Documents
Odontogenic Myxoma in A Child: Diagnostic and Treatment Dilemmas
Odontogenic Myxoma in A Child: Diagnostic and Treatment Dilemmas
Uploaded by
thedocperuOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Odontogenic Myxoma in A Child: Diagnostic and Treatment Dilemmas
Odontogenic Myxoma in A Child: Diagnostic and Treatment Dilemmas
Uploaded by
thedocperuCopyright:
Available Formats
68
J Indian Sot
Pedo Prev Dent June 2002
Odontogenic myxoma in a child : Diagnostic and treatment dilemmas.
Sarode.T. NAIR Pa, Malik N.A.b, Mumbai.
* ; _ .; Y,
. : : .- ..: : -;-! .r I
HOSPITAL DENTAL COLLEGE.
(A rare case of odontogenic myxoma of the mandible in a 10 year old child has been reported and an attempt has been made to critically analyze the case as well as the diagnostic dilemmas related to myxomatous tumours to improve our knowledge and skills in their management. ~7 J Indian Sot Pedo Prev Dent 2002 ; 20 : 2 : 68-72 Keywords : Odontogenic myxoma, J Mandible, ; Child, Myxomatous tumours
Radiologically,its
appearance ranges from a unilocular peri-
coronal radiolucency to multilocular radiolucency with variable trabecular pattern giving rise to a Honey-comb, Soap bubble or Tennis racket appearance14. burst appearence The sunray or sunhas also been reported in literature. Dis-
placement of teeth rather than resorption is more common Often displacement of tooth follicles may take place. Mandibular lesions cross the midline while maxillary do not. A lot of controversy regarding the borders of the lesions have been mentioned in literature6. They range from well defined to diffused marginsThe not typical. cyst radiological features of myxoma are
yxomatous tumors of the jaw bones have always been
a subject of discussion as the controversies regarding the origin, clinical and radiological features, treatment and recurrence rate associated with the tumors still prevail. Odontogenic myxoma is a rare benign neoplasm. Various theories regarding the origin of the tumor have been pro-
The differential diagnoses for myxoma are as below:
??
Dentigerous Periapical
??
cyst
??
posed as follows: 1. Dental papilla 2. Dental follicle 3. Periodontal ligament
?? ??
Lateral periodontal cyst Ameloblastoma lntraosseous Hemangioma Cherubism Giant cell lesions Metastatic tumours
I . ,_ :.
??
??
??
4. Degeneration of fibroma 5. Non-Odontogenic mesenchyme Myxoid tissue is not a native tissue in children or adults. It is only found in the umbilical cord of the foetus2. Recent ultra structural studies have proved the that myxoblasts mucoid i.e. modified fibroblasts secrete intracellular matrix
Macroscopically, the lesion appears to be a soft gelatinous yellowish grey mass which is often non-encapsulated. Cut surface of the lesion exhibits characteristic slimy appearance. Histopathologically, it consists of triangular stellate cells with long processes intermeshing with each other. The intercellular matrix is mucoid and the cytoplasm is slightly basophillic, finely granular and with a well defined nucleus Mitotrc figures are few. Cells may show pleomorphism. Tiny caprllanes are often seen. Variable amount of collagen fiepibres are presentbased on which it is designated as myxofibroma or fibromyxoma. Islands or nests of odontogenrc thelium are often present. Bone may be rarely present I. Recent ultrastructural studies8 have proved that myxoma is a tumor of fibroblasts, modified in such a way that they form
to form the myxoid tissuez3. Clinically, odontogenic myxoma is a benign invasive, slowly enlarging mass causing marked asymmetry of the face. It commonly involves the mandibular premolar and molar regions. Females have a higher predilection than males It usually occurs in second or third decades of life and causes expansion of the bony cortices, displacement and loosen_. i :. ing of teeth. Pain is a rare feature.
a. b
Former Professor
Post-graduate and Head
Student, . I
a matrix composed of glycosaminoglycans and do not form collagen fibrils designated as myxoblasts.
Dept. of Oral and Maxillofacial Surgery
Sar0de.T. P, Malik N.A.
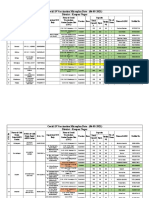
Fig.3:Preoperative Mandible
- Right Lateral Oblique View of
Fig.1 :Preoperative
- Frontal View
Fig.2: Preoperative - Intraoral View ,I_
Fig.4: Axial CT scans - showing expansion of buccal and ligual cortices with areas of erosion ,*,-. f
70
J Indian Sot Pedo Prev Dent June 2002
Fig.8:Tumour
Specimen
Fig.5 3 D CT Scan
Fig.9:Photomicrograph
of the specimen
Fig.G:lntraoperative - Exposure of tumour mass by intraoral approach
Fig.7:Surgical
; ?
defect after excision of tumour mass
. . 4
Fig. ,l 0:Postoperative
- Frontal View
Sar0de.T. P, Malik N.A.
71
Fig.ll:Postoperative - Intraoral wound healing
Fig.13: 4 months, Postoperative - Right Lateral Oblique View of Mandible
Fig.14: 6 months, P o s t o p e r a t i v e regeneration of bone Fig.1 2: Immediate Postoperative - Right Lateral Oblique View of Mandible
OPG
showing
. I
72
J Indian Sot Pedo Prev Dent June 2002
,
CASE REPORT A 10 year old child reported to the Maxillofacial OPD, N.H.D.C. with swelling of right side of face involving the body and ramus mandible since 30-35 days. The swelling was diffuse, firm, non-fluctuant, hard and tender on palpation. lntraorally the swelling presented as an exophytic growth on the distolingual aspect of right first molar and was firm in consistency, tender and lobulated. The mucosa overlying the swelling was pale pink in colour. Expansion of buccal and lingual cortical plates of ramus and body of the mandible was also evident. Preoperative right lateral oblique view of mandible showed a well defined unilocular pericoronal radiolucent lesion extending from the right ascending ramus till lower right first molar. The developing tooth follicle of lower right second molar was seen and the condyle was uninvolved. 3D CT scans showed expansion of both the buccal and lingual cortical plates with a focal area of erosion. The coronoid process and condyle were uninvolved. The inferior border of the mandible and posterior border of ramus showed no evidence of expansion. An incisional biopsy of the patient was done and the overall histopathological picture was suggestive of Non-odontogenit fibroma.The patient was taken up for surgery under gen3. 4.
I. Though the tumour is locally aggressive, the tumor mass excised in toto was well encapsulated. 2. Considering the age of the patient, the deformity caused by mandibular resection would be more. 3. The recurrence rate in children has not been detected. 4. The post operative radiographs taken after4 and 6 months showed regeneration of bone. Keeping in mind the high recurrence rate 2 associated with odontogenic myxoma, regular follow up visits are required. Moreover, because of rarity of occurrence of the myxoma, it is not possible to speculate whether the recurrence is more frequent in adults or in children. However, a surgeon must always make an attempt to critically analyse the features such as diagnostic dilemmas related to these tumors to improve our knowledge and skills in management of myxomatus tumors of the jaw bones. REFERENCES : 1. Shaefer WG, Hine M K. Levy B M. A Textbook of Oral Pathology, Philadelphia, P.A. Saunders, 1983. pp 160-161, 295297.
2.
David L. Schneck, Gross, Tabor Odontogenrc Myxoma: Report of
two cases with Reconstruction Consrderatrons. J. Oral Maxillofacial Surgery,199351 :935-940 MC Clure D K. Dahlin D C. Myxoma of Bone: Report of three cases Mayo Clinic Proc 1977:52:249 Chuchurru J.A, Luberti R, Cornicehi J C Dominguez F.Y. Myxoma of mandrble with unusual Radiographic Appearances J Oral Maxillofacial Surgery, 1985:43:987-990
eral anaesthesia. An intraoral approach was taken and the tumour mass was excised in toto The teeth 47,46,85,84.83 were extracted. Dental follicles of 45, 44 and right inferior alveolar nerve were protected Peripheral ostectomy was completed. The excised tumor was ivory in colour, well encapsulated and firm with lobulated surface. Cut surface was slimy and gelatinous. The tissue mass was sent for histopathological examination and was reported to be a Odontogenic myxoma. Post operative wound healing was satisfactory and patient has been regularly followed up since 1 year. DISCUSSION The typical myxoma of the jaw bones, though benign, is locally aggressive and the lack of encapsulation produces a lesion difficult to eradicate and requires a more radical form of treatment. Reports of surgical treatment of odontogenie myxoma range from conservative enucleation curettage to peripheral resectior?. Considering the incisional biopsy report, the tumor was excised and peripheral ostectomy was done. There was no evidence of involvement of inferior border of mandible and posterior border of ramus and hence, left intact. The conservative line of treatment followed by us is justified as : and
5.
Peltola J, Magnusson B. Happonen RP. Borrman H. Odontogenic Myxoma- A Radiographic study of 21 Tumors. Br J Oral Maxillofacial Surgery 1994 :32:298-302
6.
Kaffe I, Naor H, Buchner A Clinical and Radiological features of Odontogenrc Myxoma of the Jaws Dentomaxrllofacial Radiology 1997:26:299-303
7.
Keszler A, Dominguez F V. Giannunzio G Myxoma in Childhood, An analysis of 10 cases J Oral Maxillofacral Surgery, 1995:53:518521
8.
Stootweg P J, van den Bos T. Straks W Glycosaminoglycans in
myxoma of the jaw. A biochemical study. J Oral Pathology 1985:14:299
Reprint requests to: Dept. of Oral and Maxillofacial Surgery, Nair Hospital Dental College, Mumbai Central, Mumbai- 400008, Maharashtra.
You might also like
- 057608komatsu Hydraulic Oil HO 46-HMDocument5 pages057608komatsu Hydraulic Oil HO 46-HMrolex21No ratings yet
- HK I 05 Set A Cleaning CaddyDocument10 pagesHK I 05 Set A Cleaning CaddysamismithNo ratings yet
- Mixoma 9Document4 pagesMixoma 9Nicolás MedinaNo ratings yet
- Ameloblastic Fibroma: Report of A Case: Su-Gwan Kim, DDS, PHD, and Hyun-Seon Jang, DDS, PHDDocument3 pagesAmeloblastic Fibroma: Report of A Case: Su-Gwan Kim, DDS, PHD, and Hyun-Seon Jang, DDS, PHDdoktergigikoeNo ratings yet
- Odontogenic FibromaDocument5 pagesOdontogenic FibromaGowthamChandraSrungavarapuNo ratings yet
- Peripheral Ameloblastic FibromaDocument3 pagesPeripheral Ameloblastic FibromadoktergigikoeNo ratings yet
- Lucrare Stiintifica ParodontologieDocument4 pagesLucrare Stiintifica ParodontologieReduceriAvonNo ratings yet
- Peripheral Cemento-Ossifying Fibroma - A Case Report With A Glimpse On The Differential DiagnosisDocument5 pagesPeripheral Cemento-Ossifying Fibroma - A Case Report With A Glimpse On The Differential DiagnosisnjmdrNo ratings yet
- PlasmacytomaDocument8 pagesPlasmacytomaSowmya ManthaNo ratings yet
- Marsupialization With Enucleation of Mandibular Lateral Periodontal CystDocument1 pageMarsupialization With Enucleation of Mandibular Lateral Periodontal CystSkyeNo ratings yet
- IJRID28Document10 pagesIJRID28Saurabh SatheNo ratings yet
- CA LS Bướu Nhiều Hốc - Multilocular Radiolucency in the Body of MandibleDocument4 pagesCA LS Bướu Nhiều Hốc - Multilocular Radiolucency in the Body of MandibleThành Luân NguyễnNo ratings yet
- Bony Ankylosis Mimicking Benign ChondromaDocument4 pagesBony Ankylosis Mimicking Benign ChondromaAnumita DekaNo ratings yet
- Odontogenickeratocyst Clinically Mimicking Osteomyelitis - A Rare Case ReportDocument4 pagesOdontogenickeratocyst Clinically Mimicking Osteomyelitis - A Rare Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Adenoid Cystic Carcinoma of Hard Palate: A Case ReportDocument5 pagesAdenoid Cystic Carcinoma of Hard Palate: A Case ReportHemant GuptaNo ratings yet
- Follicular With Plexiform Ameloblastoma in Anterior Mandible: Report of Case and Literature ReviewDocument6 pagesFollicular With Plexiform Ameloblastoma in Anterior Mandible: Report of Case and Literature Reviewluckytung07No ratings yet
- CarcinomaDocument5 pagesCarcinomaLori SimmonsNo ratings yet
- 1-s2.0-S2214541921000055-mainDocument8 pages1-s2.0-S2214541921000055-mainreyesivangarciacuevasNo ratings yet
- Chondrosarcome MandiDocument8 pagesChondrosarcome MandiKarim OuniNo ratings yet
- Odontogenic Myxoma A Rare Case ReportDocument3 pagesOdontogenic Myxoma A Rare Case Reportvictorubong404No ratings yet
- DMFR 52088107Document4 pagesDMFR 52088107Roisah Yunan NegariNo ratings yet
- Gingival Squamous Cell Carcinoma: A Case Report: Dr. P.S.Rakhewar, Dr. Vrunda Kanjalkar, DR - Ruby SyedDocument3 pagesGingival Squamous Cell Carcinoma: A Case Report: Dr. P.S.Rakhewar, Dr. Vrunda Kanjalkar, DR - Ruby SyedGrecia SunurNo ratings yet
- 2019 Article 867Document8 pages2019 Article 867Reyes Ivan García CuevasNo ratings yet
- PMR 2 1 6Document4 pagesPMR 2 1 6Adrian PermadiNo ratings yet
- Benign Cementoblastoma - A Case ReportDocument3 pagesBenign Cementoblastoma - A Case ReportArafat Masud NiloyNo ratings yet
- Myoepithelioma of The Hard Palate: A Rare Case Report: 10.5005/jp-Journals-00000-0000Document4 pagesMyoepithelioma of The Hard Palate: A Rare Case Report: 10.5005/jp-Journals-00000-0000Ade primayudiNo ratings yet
- Case Report: Langerhans Cell Histiocytosis of The Mandible in A Six-Year-Old ChildDocument0 pagesCase Report: Langerhans Cell Histiocytosis of The Mandible in A Six-Year-Old ChildElvina Agnestin HarianjaNo ratings yet
- Giant CellDocument5 pagesGiant CellTamimahNo ratings yet
- Ameloblastic Fibro-Odontoma: A Case ReportDocument4 pagesAmeloblastic Fibro-Odontoma: A Case Reportoral pathNo ratings yet
- Ijcmr 692 Jun 14Document2 pagesIjcmr 692 Jun 14Jeyachandran MariappanNo ratings yet
- JournalDocument24 pagesJournalLydia OctaviaNo ratings yet
- Adult Langerhans Cell Histiocytosis With A Rare BRAF - 2022 - Advances in Oral ADocument3 pagesAdult Langerhans Cell Histiocytosis With A Rare BRAF - 2022 - Advances in Oral Ag.abdulrhmanNo ratings yet
- Pindborg Tumor Presenting in Early Adolescent - A Rare Case ReportDocument7 pagesPindborg Tumor Presenting in Early Adolescent - A Rare Case ReportIJAR JOURNALNo ratings yet
- Juvenile Ossifying Fibroma: ASE EportDocument3 pagesJuvenile Ossifying Fibroma: ASE Eportsagarjangam123No ratings yet
- Cementoblastoma Journal PDFDocument3 pagesCementoblastoma Journal PDFBayu Indra LesmanaNo ratings yet
- Unusual Large and Abiding Fibroepithelial Polyp in Oral Cavity: A Case ReportDocument4 pagesUnusual Large and Abiding Fibroepithelial Polyp in Oral Cavity: A Case ReportmuharrimahNo ratings yet
- Posterior Auricular Mass: Interesting Case SeriesDocument5 pagesPosterior Auricular Mass: Interesting Case SeriesMaria EsterNo ratings yet
- Solid Multicystic Ameloblastoma Misdiagnosed Radiographically AsDocument5 pagesSolid Multicystic Ameloblastoma Misdiagnosed Radiographically AsFury JanuarioNo ratings yet
- Primary Ameloblastic Carcinoma of The Maxilla A CaDocument9 pagesPrimary Ameloblastic Carcinoma of The Maxilla A CaMuhammad Avicenna AdjiNo ratings yet
- Case PresentationDocument46 pagesCase PresentationCareer Guide with Dr ShahzadNo ratings yet
- Ameloblastic Fibro-Dentinoma of Mandible: A Case ReportDocument3 pagesAmeloblastic Fibro-Dentinoma of Mandible: A Case ReportBrutusRexNo ratings yet
- Management of Juvenile Ossifying Fibroma in The MaDocument6 pagesManagement of Juvenile Ossifying Fibroma in The Maabeer alrofaeyNo ratings yet
- Article in Press: Journal of Oral and Maxillofacial Surgery, Medicine, and PathologyDocument6 pagesArticle in Press: Journal of Oral and Maxillofacial Surgery, Medicine, and PathologyOMFS FKG UnimusNo ratings yet
- JOFBJMSDocument5 pagesJOFBJMSabeer alrofaeyNo ratings yet
- ورقه بروف احمد سليمانDocument6 pagesورقه بروف احمد سليمانdr.m.m.yousifNo ratings yet
- Australian Dental Journal - 2008 - Spencer - Odontogenic Myxoma Case Report With Reconstructive ConsiderationsDocument4 pagesAustralian Dental Journal - 2008 - Spencer - Odontogenic Myxoma Case Report With Reconstructive ConsiderationsMarkNo ratings yet
- 40 Vinuta EtalDocument5 pages40 Vinuta EtaleditorijmrhsNo ratings yet
- Issn 2 Issn 2 Issn 2 ISSN 2073 073 073 073 - 9990 East Cent. Afr. J. S 9990 East Cent. Afr. J. S 9990 East Cent. Afr. J. S 9990 East Cent. Afr. J. SDocument7 pagesIssn 2 Issn 2 Issn 2 ISSN 2073 073 073 073 - 9990 East Cent. Afr. J. S 9990 East Cent. Afr. J. S 9990 East Cent. Afr. J. S 9990 East Cent. Afr. J. SAngga Witra NandaNo ratings yet
- 2 51 1647598330 5ijmpsjun202205Document10 pages2 51 1647598330 5ijmpsjun202205TJPRC PublicationsNo ratings yet
- Benign Extrapleural Solitary Fibrous Tumorofthe Headand NeckDocument7 pagesBenign Extrapleural Solitary Fibrous Tumorofthe Headand NeckCara Danielle PabellanoNo ratings yet
- Peripheral Squamous Odontogenic Tumor: Hort OmmunicationDocument4 pagesPeripheral Squamous Odontogenic Tumor: Hort OmmunicationGreisy Saym Cruz FelixNo ratings yet
- JIndianSocPedodPrevDent302179-1553084 041850Document4 pagesJIndianSocPedodPrevDent302179-1553084 041850NiNis Khoirun NisaNo ratings yet
- 47 Case ReportDocument4 pages47 Case Reportsusanti bulanNo ratings yet
- Keratocystic Odontogenic Tumor - A Case Report and Review of LiteratureDocument4 pagesKeratocystic Odontogenic Tumor - A Case Report and Review of Literaturearbi123No ratings yet
- Odontogenic Keratocyst Tumor: Report of Two CasesDocument6 pagesOdontogenic Keratocyst Tumor: Report of Two CasesAnibal FuentesNo ratings yet
- Traumatic Bone Cyst of Idiopathic Origin? A Report of Two CasesDocument5 pagesTraumatic Bone Cyst of Idiopathic Origin? A Report of Two CasesjulietNo ratings yet
- Tumor Odontogenico EscamosoDocument4 pagesTumor Odontogenico Escamosoメカ バルカNo ratings yet
- Journal of Oral and Maxillofacial Surgery, Medicine, and PathologyDocument7 pagesJournal of Oral and Maxillofacial Surgery, Medicine, and PathologyOMFS FKG UnimusNo ratings yet
- Prognostic Influence of Bio Markers in Oral Cancer IJMOS 2011 - v5n3 - 014Document7 pagesPrognostic Influence of Bio Markers in Oral Cancer IJMOS 2011 - v5n3 - 014lucineioliveiraNo ratings yet
- Case Report: Palatal Swelling: A Diagnostic EnigmaDocument6 pagesCase Report: Palatal Swelling: A Diagnostic EnigmaPrince AhmedNo ratings yet
- Pseudo-Ankylosis Caused by Osteoma of The Coronoid Process: Case Report - Tumors/CystsDocument3 pagesPseudo-Ankylosis Caused by Osteoma of The Coronoid Process: Case Report - Tumors/CystsSaurabh SatheNo ratings yet
- Temporal Bone CancerFrom EverandTemporal Bone CancerPaul W. GidleyNo ratings yet
- Maternity Nursing ReviewDocument37 pagesMaternity Nursing Reviewshenric16No ratings yet
- Aim Global TieupsDocument84 pagesAim Global Tieupsjhorgecruz18No ratings yet
- Applied PsychologyDocument362 pagesApplied Psychologyprajjwal100% (1)
- ACE Personal Trainer Manual, 4 Edition - Ning PDFDocument112 pagesACE Personal Trainer Manual, 4 Edition - Ning PDFbasuthker raviNo ratings yet
- Deep Fat FryingDocument2 pagesDeep Fat FryingalinawidagdoNo ratings yet
- 1574-Article Text-2641-1-10-20181107Document5 pages1574-Article Text-2641-1-10-20181107Faraz HaiderNo ratings yet
- Readings On Human Development of NepalDocument310 pagesReadings On Human Development of NepalBirkha B PunNo ratings yet
- Medicare Enrollment TipsDocument34 pagesMedicare Enrollment TipsdaringdreuNo ratings yet
- The Effects of Emotion On Short-Term Power Spectrum Analysis of Heart RateDocument5 pagesThe Effects of Emotion On Short-Term Power Spectrum Analysis of Heart RateManuel Guerrero GómezNo ratings yet
- Trojan Battery Company Valve Regulated Lead Acid Battery Safety Data SheetDocument12 pagesTrojan Battery Company Valve Regulated Lead Acid Battery Safety Data SheetNels OdrajafNo ratings yet
- Tratament Diuretic in Insuficienta CardiacaDocument19 pagesTratament Diuretic in Insuficienta CardiacaOlga HMNo ratings yet
- Qdoc - Tips - Prometric Practice Exam For Nurses Test 1Document6 pagesQdoc - Tips - Prometric Practice Exam For Nurses Test 1Ponnudev100% (1)
- Margaret Paul - Taking The Lid Off Your FeelingsDocument4 pagesMargaret Paul - Taking The Lid Off Your FeelingspapetologeneNo ratings yet
- Substance AbuseDocument54 pagesSubstance AbuseCharles CastilloNo ratings yet
- Ing GrisDocument4 pagesIng GrisaniNo ratings yet
- Clinical AssignmentDocument9 pagesClinical AssignmentkomalNo ratings yet
- Mt. Olive - August 2012-FINALDocument52 pagesMt. Olive - August 2012-FINALjoe9783No ratings yet
- ალერგიული რინიტი=20Document31 pagesალერგიული რინიტი=20Dali KochalidzeNo ratings yet
- 16012019FV4Q6RWBAnnexure documentofEIAEMP PDFDocument400 pages16012019FV4Q6RWBAnnexure documentofEIAEMP PDFJainam Shah100% (1)
- Soal D3 Bidan HermanDocument2 pagesSoal D3 Bidan HermanMidwifeDeviFadhaNo ratings yet
- Rabbit KeepingDocument12 pagesRabbit KeepingMoses NdwaruNo ratings yet
- Your AnswersDocument5 pagesYour AnswersHa TranNo ratings yet
- An Appraisal On Occlusal Philosophies in Full-Mouth Rehabilitation A Literature ReviewDocument4 pagesAn Appraisal On Occlusal Philosophies in Full-Mouth Rehabilitation A Literature ReviewaggrolNo ratings yet
- A Review On Various Uses of N-Acetyl CysteineDocument7 pagesA Review On Various Uses of N-Acetyl CysteineMudrikaNo ratings yet
- Orphan Drugs Doctoral SeminarDocument21 pagesOrphan Drugs Doctoral SeminarDr RC Mishra100% (1)
- Case StudiesDocument5 pagesCase StudiesPou PunzalanNo ratings yet
- Covid-19 Vaccination Microplan Date - (06-05-2021) District: Kanpur NagarDocument4 pagesCovid-19 Vaccination Microplan Date - (06-05-2021) District: Kanpur NagarAditi GuptaNo ratings yet
- Ultrarunning MagDocument60 pagesUltrarunning MagLynseyNo ratings yet