Professional Documents
Culture Documents
Jop 2005 03 s0189
Jop 2005 03 s0189
Uploaded by
Herpika DianaCopyright:
Available Formats
You might also like
- F 16 CLINNeurologicalObservationChartDocument2 pagesF 16 CLINNeurologicalObservationChartRani100% (1)
- Mechanism of Pain Generation For Endometriosis-Associated Pelvic PainDocument9 pagesMechanism of Pain Generation For Endometriosis-Associated Pelvic PainDwi CahyaNo ratings yet
- Halpern 2016Document25 pagesHalpern 2016SAYDE ILEANA NAJERA DOMINGUEZNo ratings yet
- Alphabetized BibsDocument33 pagesAlphabetized Bibsapi-512426092No ratings yet
- Ami FM SummariesDocument3 pagesAmi FM SummariesDimple PatelNo ratings yet
- Vulnerabilidade A Dor 2014Document9 pagesVulnerabilidade A Dor 2014Ellen AmaralNo ratings yet
- Management BMSDocument16 pagesManagement BMSMega RafikaNo ratings yet
- Panic DisorderDocument10 pagesPanic Disorderandikaagus13No ratings yet
- Tinitus y TTM EcaDocument25 pagesTinitus y TTM EcaFernando Espada SalgadoNo ratings yet
- Sleep Disorders and Their Association With Laboratory Pain Sensitivity in Temporomandibular Joint DisorderDocument12 pagesSleep Disorders and Their Association With Laboratory Pain Sensitivity in Temporomandibular Joint DisorderAlba de la BarreraNo ratings yet
- Epigenetics Insights Into Chronic Pain: DNA Hypomethylation in Fibromyalgia-A Controlled Pilot-StudyDocument8 pagesEpigenetics Insights Into Chronic Pain: DNA Hypomethylation in Fibromyalgia-A Controlled Pilot-StudyChofi SaezNo ratings yet
- Sarlanietal JOrofac Pain 2004Document16 pagesSarlanietal JOrofac Pain 2004soylahijadeunvampiroNo ratings yet
- Dissertation Chronic PainDocument4 pagesDissertation Chronic PainWriteMyCollegePaperForMeSingapore100% (1)
- Fischer2008 1 PDFDocument8 pagesFischer2008 1 PDFRenas HajiNo ratings yet
- S180886941530673XDocument8 pagesS180886941530673XErick PiñerosNo ratings yet
- Sleep Apnea Symptoms and Risk of Temporomandibular Disorder: OPPERA CohortDocument8 pagesSleep Apnea Symptoms and Risk of Temporomandibular Disorder: OPPERA CohortGabrielle RodriguesNo ratings yet
- The Influence of Cranio-Cervical Posture On Maximal Mouth Opening and Pressure Pain Threshold in Patients With Myofascial Temporomandibular Pain DisordersDocument8 pagesThe Influence of Cranio-Cervical Posture On Maximal Mouth Opening and Pressure Pain Threshold in Patients With Myofascial Temporomandibular Pain DisordersFelipeVidalNo ratings yet
- Art 21Document9 pagesArt 21Mirek SzNo ratings yet
- MTDDocument10 pagesMTDmajid mirzaeeNo ratings yet
- Vocal Ped Article Short Essay Extrinsic Laryngeal Muscular Tension in Patients With Voice Disorders - Document - Gale OneFile: Health and MedicineDocument18 pagesVocal Ped Article Short Essay Extrinsic Laryngeal Muscular Tension in Patients With Voice Disorders - Document - Gale OneFile: Health and MedicinelorenaNo ratings yet
- 1 s2.0 S1526590017304881 Main PDFDocument9 pages1 s2.0 S1526590017304881 Main PDFmuthiaNo ratings yet
- Neural Mechanisms Underlying Changes (2010)Document9 pagesNeural Mechanisms Underlying Changes (2010)maria paula brenesNo ratings yet
- Orofacial Musculoskeletal Pain. An Evidence-Based Bio-Psycho-Social Matrix ModelDocument27 pagesOrofacial Musculoskeletal Pain. An Evidence-Based Bio-Psycho-Social Matrix ModelAMBAR JOSEFA ALEJANDRA MORAGA VALENZUELANo ratings yet
- SAQ GenDocument1 pageSAQ GenJaka PataftaNo ratings yet
- Orofacial Pain: From Basic Science to Clinical Management, Second EditionFrom EverandOrofacial Pain: From Basic Science to Clinical Management, Second EditionNo ratings yet
- The Use The Use of Metformin Is Associated With Decreased Lumbar Radiculopathy Painof Metformin Is Associated With Decreased Lumbar Rad 120613Document9 pagesThe Use The Use of Metformin Is Associated With Decreased Lumbar Radiculopathy Painof Metformin Is Associated With Decreased Lumbar Rad 120613เพียงแค่ แอนโทนี่No ratings yet
- Apa Ajaapa AjaDocument7 pagesApa Ajaapa AjaMeidi RaniNo ratings yet
- Neuroendocrine Derangement in Chronic Migraine (Pages 1309-1310)Document2 pagesNeuroendocrine Derangement in Chronic Migraine (Pages 1309-1310)Massio MaxNo ratings yet
- Personality Traits According To HormonesDocument23 pagesPersonality Traits According To HormonesTakudzwa Raphael MuzaNo ratings yet
- Small Fiber Neuropathy and Related Syndromes: Pain and NeurodegenerationFrom EverandSmall Fiber Neuropathy and Related Syndromes: Pain and NeurodegenerationSung-Tsang HsiehNo ratings yet
- 10 1016@j Jpsychores 2016 03 001Document16 pages10 1016@j Jpsychores 2016 03 001Adimas DewanggaNo ratings yet
- Depresi Dan KankerDocument10 pagesDepresi Dan KankernigoNo ratings yet
- Artigos Coderre1997Document65 pagesArtigos Coderre1997JonasMarçaloNo ratings yet
- 10 1016@j Jpain 2009 04 017Document9 pages10 1016@j Jpain 2009 04 017Carlos Martín De RosasNo ratings yet
- HyfvDocument5 pagesHyfvAgusNo ratings yet
- OPERATORIA. Henry A. Gremillion Multidisciplinary Diagnosis and Management of Orofacial PainDocument13 pagesOPERATORIA. Henry A. Gremillion Multidisciplinary Diagnosis and Management of Orofacial PainKenigal14No ratings yet
- 10.1007@s00737 018 0933 ZDocument11 pages10.1007@s00737 018 0933 ZFernandoNo ratings yet
- PMT 11 88Document3 pagesPMT 11 88Sri RamadhaniNo ratings yet
- Estados de Humor Asociados Con Cambios Transitorios en Síntomas en Asma y Peak de Flujo Espiratorio 2000Document8 pagesEstados de Humor Asociados Con Cambios Transitorios en Síntomas en Asma y Peak de Flujo Espiratorio 2000Sara FarrellNo ratings yet
- Lower Placebo Responses After Long-Term Exposure To Fibromyalgia PainDocument9 pagesLower Placebo Responses After Long-Term Exposure To Fibromyalgia PainmuthiaNo ratings yet
- 2011 Van Wingen Gonadal Hormone Emotional CircutsDocument8 pages2011 Van Wingen Gonadal Hormone Emotional CircutserrrorerNo ratings yet
- Headache Tension - Neuro ClinicsDocument11 pagesHeadache Tension - Neuro ClinicsDian Ayu Permata SandiNo ratings yet
- Epigenetics and NeuroendocrinologyDocument280 pagesEpigenetics and NeuroendocrinologyArianPedroza100% (4)
- Ursin, H. (1998) The Psychology in PsychoneuroendocrinologyDocument16 pagesUrsin, H. (1998) The Psychology in PsychoneuroendocrinologyCristian jimènezNo ratings yet
- Effect of Application of Transcutaneous Electrical Nerve Stimulation and Laryngeal Manual Therapy in Dysphonic Women: Clinical TrialDocument9 pagesEffect of Application of Transcutaneous Electrical Nerve Stimulation and Laryngeal Manual Therapy in Dysphonic Women: Clinical TrialFrancisca Carrasco LavadoNo ratings yet
- Children: Acupuncture For Pediatric PainDocument15 pagesChildren: Acupuncture For Pediatric PainRachel GreeneNo ratings yet
- NIH Public Access: Author ManuscriptDocument25 pagesNIH Public Access: Author ManuscriptsoylahijadeunvampiroNo ratings yet
- Sex Differences in Anxiety and Depression Role of TestosteroneDocument35 pagesSex Differences in Anxiety and Depression Role of Testosteronepopa.irinaNo ratings yet
- Nss 10 271Document16 pagesNss 10 271杨钦杰No ratings yet
- International Journal of Pediatric Research Ijpr 9 110Document9 pagesInternational Journal of Pediatric Research Ijpr 9 110VsbshNo ratings yet
- 4 U1.0 B978 0 7216 9654 6..50177 6..DOCPDFDocument5 pages4 U1.0 B978 0 7216 9654 6..50177 6..DOCPDFgilmeraf2000No ratings yet
- University of Groningen: Document VersionDocument23 pagesUniversity of Groningen: Document VersionLailaNo ratings yet
- Bar Shalita 2019 SMD and Pain in SUD-handoutDocument3 pagesBar Shalita 2019 SMD and Pain in SUD-handoutMariana FidelesNo ratings yet
- The Role of Operant Conditioning in Chronic Pain: An Experimental InvestigationDocument8 pagesThe Role of Operant Conditioning in Chronic Pain: An Experimental InvestigationMaRiA dAnIeLaNo ratings yet
- Human Brain Mechanisms of Pain PerceptionDocument22 pagesHuman Brain Mechanisms of Pain Perceptionnynaeve_almeeraNo ratings yet
- Dance/movement Therapy and Changes in Stress-Related Hormones: A Study of Fibromyalgia Patients With Video-InterpretationDocument1 pageDance/movement Therapy and Changes in Stress-Related Hormones: A Study of Fibromyalgia Patients With Video-InterpretationShirley ValvelNo ratings yet
- Balance Problems With Parkinson'S Disease: Are They Anxiety-Dependent?Document9 pagesBalance Problems With Parkinson'S Disease: Are They Anxiety-Dependent?Vasile MuratNo ratings yet
- Temporomandibular Disorders - A Review of Current Concepts inDocument24 pagesTemporomandibular Disorders - A Review of Current Concepts inAlba Letícia MedeirosNo ratings yet
- TTH TMD SleepDocument8 pagesTTH TMD SleepDudeperfect666No ratings yet
- Esuizorenia e InsonmioDocument32 pagesEsuizorenia e InsonmioVictor CarrenoNo ratings yet
- Handbook of Methadone Prescribing and Buprenorphine TherapyFrom EverandHandbook of Methadone Prescribing and Buprenorphine TherapyNo ratings yet
- Stress and The Periodontium: Review Article 10.5005/jp-Journals-10031-1005Document3 pagesStress and The Periodontium: Review Article 10.5005/jp-Journals-10031-1005Herpika DianaNo ratings yet
- Dr. Nikita AgrawalDocument4 pagesDr. Nikita AgrawalHerpika DianaNo ratings yet
- Caffeine Bone CalciumDocument8 pagesCaffeine Bone CalciumHerpika DianaNo ratings yet
- Understanding Stress and TMJ Dysfunction: What Causes TMJ Problems? How Can Physical Therapy Help TMJ Sufferers?Document2 pagesUnderstanding Stress and TMJ Dysfunction: What Causes TMJ Problems? How Can Physical Therapy Help TMJ Sufferers?Herpika DianaNo ratings yet
- A Comparative Study of Acidogenic Potential of Milk and Commonly Used Milk FormulaeDocument3 pagesA Comparative Study of Acidogenic Potential of Milk and Commonly Used Milk FormulaeHerpika DianaNo ratings yet
- Green Tea Extract For Periodontal Health: Review ArticleDocument5 pagesGreen Tea Extract For Periodontal Health: Review ArticleHerpika DianaNo ratings yet
- Effects of Self-Ligating and Conventional Brackets On Halitosis and Periodontal ConditionsDocument6 pagesEffects of Self-Ligating and Conventional Brackets On Halitosis and Periodontal ConditionsHerpika DianaNo ratings yet
- The Cariostatic Potential of Cheese: Cooked Cheese-Containing Meals Increase Plaque Calcium ConcentrationDocument4 pagesThe Cariostatic Potential of Cheese: Cooked Cheese-Containing Meals Increase Plaque Calcium ConcentrationHerpika DianaNo ratings yet
- Dr. Karam Abu Shakra 42-10Document8 pagesDr. Karam Abu Shakra 42-10Herpika DianaNo ratings yet
- Effect of Mastication On Human Brain Activity: Kiwako Sakamoto, Hiroki Nakata, Masato Yumoto, Ryusuke KakigiDocument8 pagesEffect of Mastication On Human Brain Activity: Kiwako Sakamoto, Hiroki Nakata, Masato Yumoto, Ryusuke KakigiHerpika DianaNo ratings yet
- Evaluation of Temporomandibular Joint in Stress-Free PatientsDocument5 pagesEvaluation of Temporomandibular Joint in Stress-Free PatientsHerpika DianaNo ratings yet
- An Expanded Odontogenic Myxoma in MaxillaDocument7 pagesAn Expanded Odontogenic Myxoma in MaxillaHerpika DianaNo ratings yet
- Investigation On Two-Body Abrasive Wear Behavior of Silicon Carbide Filled Glass Fabric-Epoxy CompositesDocument16 pagesInvestigation On Two-Body Abrasive Wear Behavior of Silicon Carbide Filled Glass Fabric-Epoxy CompositesHerpika DianaNo ratings yet
- Osteoma 1Document3 pagesOsteoma 1Herpika DianaNo ratings yet
- Midterm Practice 2011Document53 pagesMidterm Practice 2011Marina ChengNo ratings yet
- Tugas 10 Toksikologi Klinik Jurnal KonvensionalDocument7 pagesTugas 10 Toksikologi Klinik Jurnal KonvensionalFitrah assagafNo ratings yet
- Primary Vaginal TumorsDocument3 pagesPrimary Vaginal TumorsEngra CiaNo ratings yet
- 33-Nursing Care PlanDocument3 pages33-Nursing Care Planakositabon100% (1)
- Clotting TimeDocument26 pagesClotting TimeMalliga SundareshanNo ratings yet
- Clearing Clutter With EFT BonusDocument10 pagesClearing Clutter With EFT BonusKristen Hammer75% (4)
- SnakesDocument13 pagesSnakesDiya laljyNo ratings yet
- Meat Eating Predicts Diabetes DevelopmentDocument2 pagesMeat Eating Predicts Diabetes DevelopmentQ429ma6No ratings yet
- IM - Facts From Case Files CRCDocument80 pagesIM - Facts From Case Files CRCridin007No ratings yet
- Management of Dry SocketDocument4 pagesManagement of Dry SocketFakhrul ImamNo ratings yet
- Write Up TutorialDocument22 pagesWrite Up Tutorialballer0417100% (1)
- Membrane FiltrationDocument30 pagesMembrane Filtrationsupravietuire100% (1)
- Gestational Trophoblastic DiseaseDocument25 pagesGestational Trophoblastic Diseaseapi-3705046100% (1)
- Spine Oncology, An Issue of Orthopedic Clinics PDFDocument168 pagesSpine Oncology, An Issue of Orthopedic Clinics PDFThanh Le DangNo ratings yet
- Web Amc Cat MCQ Information SheetDocument3 pagesWeb Amc Cat MCQ Information SheetMuhammad Tawfiik Mathure100% (1)
- Acute Gastroenteritis (AGE) PDFDocument37 pagesAcute Gastroenteritis (AGE) PDFAries Chandra AnandithaNo ratings yet
- B1 1 HowIBeatEmphysemaandCOPDinSixWeeks PDFDocument130 pagesB1 1 HowIBeatEmphysemaandCOPDinSixWeeks PDFGreg DaymondNo ratings yet
- Learning ReflectionDocument11 pagesLearning ReflectionTran GatesNo ratings yet
- DRUG STUDY - AmoxicillinDocument7 pagesDRUG STUDY - AmoxicillinFaye Gatchalian100% (1)
- Platelet Rich Plasma in OrthopaedicsDocument269 pagesPlatelet Rich Plasma in OrthopaedicsBelinda Azhari SiswantoNo ratings yet
- Patient Adm NoteDocument4 pagesPatient Adm NoteTraceyNo ratings yet
- H S PPLDocument13 pagesH S PPLPablo Berardo67% (3)
- Esophagus, TearDocument36 pagesEsophagus, Tearapi-19641337No ratings yet
- Katalog Cook Gynekologie PDFDocument70 pagesKatalog Cook Gynekologie PDFHari_Shankar_G_7847No ratings yet
- (MIKROBIOLOGI) IT 20 - Orthomyxovirus, Paramyxovirus - KHSDocument37 pages(MIKROBIOLOGI) IT 20 - Orthomyxovirus, Paramyxovirus - KHSRessy FelisaNo ratings yet
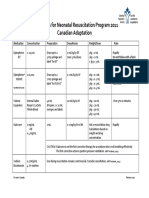
- Medications For Neonatal Resuscitation Program 2011 Canadian AdaptationDocument1 pageMedications For Neonatal Resuscitation Program 2011 Canadian AdaptationrubymayNo ratings yet
- Lab Report - BodDocument11 pagesLab Report - BodZack MalikNo ratings yet
- Dialysis SkillsDocument2 pagesDialysis Skillssheelaaku100% (1)
- Kinesiology 8 - PJJ Assgnment Movement AnalysisDocument64 pagesKinesiology 8 - PJJ Assgnment Movement AnalysispaegyoNo ratings yet
Jop 2005 03 s0189
Jop 2005 03 s0189
Uploaded by
Herpika DianaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jop 2005 03 s0189
Jop 2005 03 s0189
Uploaded by
Herpika DianaCopyright:
Available Formats
C
o
pyr
i
g
h
t
b
y
N
o
t
f o
r
Q
u
i
n
t
e
s
s
en
c
e
N
o
t
f
o
r
P
u
b
l
i
c
a
t
i
o
n
Journal of Orofacial Pain 189
A
variety of factors ranging from psychologi-
cal stress and occlusal variables to gender
and sleep may be related to the expression
of chronic orofacial pain conditions such as
temporomandibular disorders (TMD) or atypical
odontalgia. Several articles in this issue of the
Journal of Orofacial Pain report on studies that
have explored some of these possible associations
or risk factors. Although the article by
Yoshihara et al does not set out to address
whether stress is the cause or effect of TMD, it
does document that TMD patients are more
reactive to psychological stress than healthy
controls, as reflected in significantly higher levels
of and more prolonged elevation of plasma
cortisol, adrenaline, and nonadrenaline. Of related
interest is LeResche et als article, which presents
the results of the first prospective study of TMD
pain during pregnancy. The authors show that
psychological distress changes little over the course
of pregnancy in female TMD patients, while signs
and symptoms of TMD improve over this period.
They attribute the TMD improvements to the
marked sex hormone changes during pregnancy,
which is interesting in light of earlier studies
reporting that use of oral contraceptives and
hormone replacement therapy increases the risk
for TMD. Other TMD risk factors suggested in
the literature include occlusal factors and smoking.
The latter is addressed in Wnmans article report-
ing that smoking is not an important element
influencing the development or maintenance of
TMD, while no causal relationships were found in
the study reported by Hirsch et al between over-
bite or overjet and temporomandibular joint
(TMJ) sounds defined according to the Research
Diagnostic Criteria for TMD. Their study suggests
that normal functioning of the TMJ is associated
with wide ranges of overbite or overjet. Joint
sounds were also the subject of a study by Baba et
al. Since they report that joint sounds, as well as
gender, are significantly associated with the dura-
tion of masseter muscle activity during sleep, it
will be interesting to investigate this association
further, given the frequently cited view that muscle
hyperactivity is a factor in sleep bruxism and that
sleep bruxism is causally related to TMD. Sleep
bruxism is also the focus of the article by Ommer-
born et al, who report on the utility of a recently
developed computer-based approach to the assess-
ment of sleep bruxism.
One of the remaining articles is a case report by
Mourouzis et al of occipital neuralgia associated
with respiratory tract infection. The other 2 papers
in this issue focus on dental pain and possible
mechanisms. The study by Baad-Hansen et al
utilized the blink reflex, which a recent review
article in the Journal indicates may be useful in the
diagnosis of orofacial pain conditions.
1
No differ-
ence in blink reflexes was found between the
painful and nonpainful sides of patients with
atypical odontalgia. The blink reflex also was not
significantly modulated by experimental pain
induced by the intraoral application of capsaicin,
the chemical in hot peppers that acts as an irritant
on the vanilloid receptor TRPV1 in peripheral
tissues. As the authors indicate, further studies are
needed to clarify the potential role of peripheral as
well as central mechanisms, including sensitiza-
tion, in atypical odontalgia. The TRPV1 receptor
is also the focus of the article by Morgan et al who
document that TRPV1 is present in the dental pulp
and that TRPV1 expression in pulpal nerve fibers
and vascular cells is greater in carious and painful
teeth, respectively. Since TRPV1 has been shown
elsewhere in the body to be an important signaling
mechanism in the responses of nociceptive afferent
fibers to heat and irritant chemicals such as
capsaicin and in the sensitization of the fibers, it
offers a novel therapeutic target to control pain,
and so it will be important to study further the
role of these receptor mechanisms in acute and
chronic orofacial pain conditions.
Barry J. Sessle
Editor-in-Chief
Reference
1. Jskelinen SK. Clinical neurophysiology and quantitative
sensory testing in the investigation of orofacial pain and sen-
sory function. J Orofac Pain 2004;18:85107.
Stress, Sex, Smoking, Sounds, Sleep, and Sensitization
Studies on Associations, Risk Factors, and Mechanisms
in Orofacial Pain
Editorial
You might also like
- F 16 CLINNeurologicalObservationChartDocument2 pagesF 16 CLINNeurologicalObservationChartRani100% (1)
- Mechanism of Pain Generation For Endometriosis-Associated Pelvic PainDocument9 pagesMechanism of Pain Generation For Endometriosis-Associated Pelvic PainDwi CahyaNo ratings yet
- Halpern 2016Document25 pagesHalpern 2016SAYDE ILEANA NAJERA DOMINGUEZNo ratings yet
- Alphabetized BibsDocument33 pagesAlphabetized Bibsapi-512426092No ratings yet
- Ami FM SummariesDocument3 pagesAmi FM SummariesDimple PatelNo ratings yet
- Vulnerabilidade A Dor 2014Document9 pagesVulnerabilidade A Dor 2014Ellen AmaralNo ratings yet
- Management BMSDocument16 pagesManagement BMSMega RafikaNo ratings yet
- Panic DisorderDocument10 pagesPanic Disorderandikaagus13No ratings yet
- Tinitus y TTM EcaDocument25 pagesTinitus y TTM EcaFernando Espada SalgadoNo ratings yet
- Sleep Disorders and Their Association With Laboratory Pain Sensitivity in Temporomandibular Joint DisorderDocument12 pagesSleep Disorders and Their Association With Laboratory Pain Sensitivity in Temporomandibular Joint DisorderAlba de la BarreraNo ratings yet
- Epigenetics Insights Into Chronic Pain: DNA Hypomethylation in Fibromyalgia-A Controlled Pilot-StudyDocument8 pagesEpigenetics Insights Into Chronic Pain: DNA Hypomethylation in Fibromyalgia-A Controlled Pilot-StudyChofi SaezNo ratings yet
- Sarlanietal JOrofac Pain 2004Document16 pagesSarlanietal JOrofac Pain 2004soylahijadeunvampiroNo ratings yet
- Dissertation Chronic PainDocument4 pagesDissertation Chronic PainWriteMyCollegePaperForMeSingapore100% (1)
- Fischer2008 1 PDFDocument8 pagesFischer2008 1 PDFRenas HajiNo ratings yet
- S180886941530673XDocument8 pagesS180886941530673XErick PiñerosNo ratings yet
- Sleep Apnea Symptoms and Risk of Temporomandibular Disorder: OPPERA CohortDocument8 pagesSleep Apnea Symptoms and Risk of Temporomandibular Disorder: OPPERA CohortGabrielle RodriguesNo ratings yet
- The Influence of Cranio-Cervical Posture On Maximal Mouth Opening and Pressure Pain Threshold in Patients With Myofascial Temporomandibular Pain DisordersDocument8 pagesThe Influence of Cranio-Cervical Posture On Maximal Mouth Opening and Pressure Pain Threshold in Patients With Myofascial Temporomandibular Pain DisordersFelipeVidalNo ratings yet
- Art 21Document9 pagesArt 21Mirek SzNo ratings yet
- MTDDocument10 pagesMTDmajid mirzaeeNo ratings yet
- Vocal Ped Article Short Essay Extrinsic Laryngeal Muscular Tension in Patients With Voice Disorders - Document - Gale OneFile: Health and MedicineDocument18 pagesVocal Ped Article Short Essay Extrinsic Laryngeal Muscular Tension in Patients With Voice Disorders - Document - Gale OneFile: Health and MedicinelorenaNo ratings yet
- 1 s2.0 S1526590017304881 Main PDFDocument9 pages1 s2.0 S1526590017304881 Main PDFmuthiaNo ratings yet
- Neural Mechanisms Underlying Changes (2010)Document9 pagesNeural Mechanisms Underlying Changes (2010)maria paula brenesNo ratings yet
- Orofacial Musculoskeletal Pain. An Evidence-Based Bio-Psycho-Social Matrix ModelDocument27 pagesOrofacial Musculoskeletal Pain. An Evidence-Based Bio-Psycho-Social Matrix ModelAMBAR JOSEFA ALEJANDRA MORAGA VALENZUELANo ratings yet
- SAQ GenDocument1 pageSAQ GenJaka PataftaNo ratings yet
- Orofacial Pain: From Basic Science to Clinical Management, Second EditionFrom EverandOrofacial Pain: From Basic Science to Clinical Management, Second EditionNo ratings yet
- The Use The Use of Metformin Is Associated With Decreased Lumbar Radiculopathy Painof Metformin Is Associated With Decreased Lumbar Rad 120613Document9 pagesThe Use The Use of Metformin Is Associated With Decreased Lumbar Radiculopathy Painof Metformin Is Associated With Decreased Lumbar Rad 120613เพียงแค่ แอนโทนี่No ratings yet
- Apa Ajaapa AjaDocument7 pagesApa Ajaapa AjaMeidi RaniNo ratings yet
- Neuroendocrine Derangement in Chronic Migraine (Pages 1309-1310)Document2 pagesNeuroendocrine Derangement in Chronic Migraine (Pages 1309-1310)Massio MaxNo ratings yet
- Personality Traits According To HormonesDocument23 pagesPersonality Traits According To HormonesTakudzwa Raphael MuzaNo ratings yet
- Small Fiber Neuropathy and Related Syndromes: Pain and NeurodegenerationFrom EverandSmall Fiber Neuropathy and Related Syndromes: Pain and NeurodegenerationSung-Tsang HsiehNo ratings yet
- 10 1016@j Jpsychores 2016 03 001Document16 pages10 1016@j Jpsychores 2016 03 001Adimas DewanggaNo ratings yet
- Depresi Dan KankerDocument10 pagesDepresi Dan KankernigoNo ratings yet
- Artigos Coderre1997Document65 pagesArtigos Coderre1997JonasMarçaloNo ratings yet
- 10 1016@j Jpain 2009 04 017Document9 pages10 1016@j Jpain 2009 04 017Carlos Martín De RosasNo ratings yet
- HyfvDocument5 pagesHyfvAgusNo ratings yet
- OPERATORIA. Henry A. Gremillion Multidisciplinary Diagnosis and Management of Orofacial PainDocument13 pagesOPERATORIA. Henry A. Gremillion Multidisciplinary Diagnosis and Management of Orofacial PainKenigal14No ratings yet
- 10.1007@s00737 018 0933 ZDocument11 pages10.1007@s00737 018 0933 ZFernandoNo ratings yet
- PMT 11 88Document3 pagesPMT 11 88Sri RamadhaniNo ratings yet
- Estados de Humor Asociados Con Cambios Transitorios en Síntomas en Asma y Peak de Flujo Espiratorio 2000Document8 pagesEstados de Humor Asociados Con Cambios Transitorios en Síntomas en Asma y Peak de Flujo Espiratorio 2000Sara FarrellNo ratings yet
- Lower Placebo Responses After Long-Term Exposure To Fibromyalgia PainDocument9 pagesLower Placebo Responses After Long-Term Exposure To Fibromyalgia PainmuthiaNo ratings yet
- 2011 Van Wingen Gonadal Hormone Emotional CircutsDocument8 pages2011 Van Wingen Gonadal Hormone Emotional CircutserrrorerNo ratings yet
- Headache Tension - Neuro ClinicsDocument11 pagesHeadache Tension - Neuro ClinicsDian Ayu Permata SandiNo ratings yet
- Epigenetics and NeuroendocrinologyDocument280 pagesEpigenetics and NeuroendocrinologyArianPedroza100% (4)
- Ursin, H. (1998) The Psychology in PsychoneuroendocrinologyDocument16 pagesUrsin, H. (1998) The Psychology in PsychoneuroendocrinologyCristian jimènezNo ratings yet
- Effect of Application of Transcutaneous Electrical Nerve Stimulation and Laryngeal Manual Therapy in Dysphonic Women: Clinical TrialDocument9 pagesEffect of Application of Transcutaneous Electrical Nerve Stimulation and Laryngeal Manual Therapy in Dysphonic Women: Clinical TrialFrancisca Carrasco LavadoNo ratings yet
- Children: Acupuncture For Pediatric PainDocument15 pagesChildren: Acupuncture For Pediatric PainRachel GreeneNo ratings yet
- NIH Public Access: Author ManuscriptDocument25 pagesNIH Public Access: Author ManuscriptsoylahijadeunvampiroNo ratings yet
- Sex Differences in Anxiety and Depression Role of TestosteroneDocument35 pagesSex Differences in Anxiety and Depression Role of Testosteronepopa.irinaNo ratings yet
- Nss 10 271Document16 pagesNss 10 271杨钦杰No ratings yet
- International Journal of Pediatric Research Ijpr 9 110Document9 pagesInternational Journal of Pediatric Research Ijpr 9 110VsbshNo ratings yet
- 4 U1.0 B978 0 7216 9654 6..50177 6..DOCPDFDocument5 pages4 U1.0 B978 0 7216 9654 6..50177 6..DOCPDFgilmeraf2000No ratings yet
- University of Groningen: Document VersionDocument23 pagesUniversity of Groningen: Document VersionLailaNo ratings yet
- Bar Shalita 2019 SMD and Pain in SUD-handoutDocument3 pagesBar Shalita 2019 SMD and Pain in SUD-handoutMariana FidelesNo ratings yet
- The Role of Operant Conditioning in Chronic Pain: An Experimental InvestigationDocument8 pagesThe Role of Operant Conditioning in Chronic Pain: An Experimental InvestigationMaRiA dAnIeLaNo ratings yet
- Human Brain Mechanisms of Pain PerceptionDocument22 pagesHuman Brain Mechanisms of Pain Perceptionnynaeve_almeeraNo ratings yet
- Dance/movement Therapy and Changes in Stress-Related Hormones: A Study of Fibromyalgia Patients With Video-InterpretationDocument1 pageDance/movement Therapy and Changes in Stress-Related Hormones: A Study of Fibromyalgia Patients With Video-InterpretationShirley ValvelNo ratings yet
- Balance Problems With Parkinson'S Disease: Are They Anxiety-Dependent?Document9 pagesBalance Problems With Parkinson'S Disease: Are They Anxiety-Dependent?Vasile MuratNo ratings yet
- Temporomandibular Disorders - A Review of Current Concepts inDocument24 pagesTemporomandibular Disorders - A Review of Current Concepts inAlba Letícia MedeirosNo ratings yet
- TTH TMD SleepDocument8 pagesTTH TMD SleepDudeperfect666No ratings yet
- Esuizorenia e InsonmioDocument32 pagesEsuizorenia e InsonmioVictor CarrenoNo ratings yet
- Handbook of Methadone Prescribing and Buprenorphine TherapyFrom EverandHandbook of Methadone Prescribing and Buprenorphine TherapyNo ratings yet
- Stress and The Periodontium: Review Article 10.5005/jp-Journals-10031-1005Document3 pagesStress and The Periodontium: Review Article 10.5005/jp-Journals-10031-1005Herpika DianaNo ratings yet
- Dr. Nikita AgrawalDocument4 pagesDr. Nikita AgrawalHerpika DianaNo ratings yet
- Caffeine Bone CalciumDocument8 pagesCaffeine Bone CalciumHerpika DianaNo ratings yet
- Understanding Stress and TMJ Dysfunction: What Causes TMJ Problems? How Can Physical Therapy Help TMJ Sufferers?Document2 pagesUnderstanding Stress and TMJ Dysfunction: What Causes TMJ Problems? How Can Physical Therapy Help TMJ Sufferers?Herpika DianaNo ratings yet
- A Comparative Study of Acidogenic Potential of Milk and Commonly Used Milk FormulaeDocument3 pagesA Comparative Study of Acidogenic Potential of Milk and Commonly Used Milk FormulaeHerpika DianaNo ratings yet
- Green Tea Extract For Periodontal Health: Review ArticleDocument5 pagesGreen Tea Extract For Periodontal Health: Review ArticleHerpika DianaNo ratings yet
- Effects of Self-Ligating and Conventional Brackets On Halitosis and Periodontal ConditionsDocument6 pagesEffects of Self-Ligating and Conventional Brackets On Halitosis and Periodontal ConditionsHerpika DianaNo ratings yet
- The Cariostatic Potential of Cheese: Cooked Cheese-Containing Meals Increase Plaque Calcium ConcentrationDocument4 pagesThe Cariostatic Potential of Cheese: Cooked Cheese-Containing Meals Increase Plaque Calcium ConcentrationHerpika DianaNo ratings yet
- Dr. Karam Abu Shakra 42-10Document8 pagesDr. Karam Abu Shakra 42-10Herpika DianaNo ratings yet
- Effect of Mastication On Human Brain Activity: Kiwako Sakamoto, Hiroki Nakata, Masato Yumoto, Ryusuke KakigiDocument8 pagesEffect of Mastication On Human Brain Activity: Kiwako Sakamoto, Hiroki Nakata, Masato Yumoto, Ryusuke KakigiHerpika DianaNo ratings yet
- Evaluation of Temporomandibular Joint in Stress-Free PatientsDocument5 pagesEvaluation of Temporomandibular Joint in Stress-Free PatientsHerpika DianaNo ratings yet
- An Expanded Odontogenic Myxoma in MaxillaDocument7 pagesAn Expanded Odontogenic Myxoma in MaxillaHerpika DianaNo ratings yet
- Investigation On Two-Body Abrasive Wear Behavior of Silicon Carbide Filled Glass Fabric-Epoxy CompositesDocument16 pagesInvestigation On Two-Body Abrasive Wear Behavior of Silicon Carbide Filled Glass Fabric-Epoxy CompositesHerpika DianaNo ratings yet
- Osteoma 1Document3 pagesOsteoma 1Herpika DianaNo ratings yet
- Midterm Practice 2011Document53 pagesMidterm Practice 2011Marina ChengNo ratings yet
- Tugas 10 Toksikologi Klinik Jurnal KonvensionalDocument7 pagesTugas 10 Toksikologi Klinik Jurnal KonvensionalFitrah assagafNo ratings yet
- Primary Vaginal TumorsDocument3 pagesPrimary Vaginal TumorsEngra CiaNo ratings yet
- 33-Nursing Care PlanDocument3 pages33-Nursing Care Planakositabon100% (1)
- Clotting TimeDocument26 pagesClotting TimeMalliga SundareshanNo ratings yet
- Clearing Clutter With EFT BonusDocument10 pagesClearing Clutter With EFT BonusKristen Hammer75% (4)
- SnakesDocument13 pagesSnakesDiya laljyNo ratings yet
- Meat Eating Predicts Diabetes DevelopmentDocument2 pagesMeat Eating Predicts Diabetes DevelopmentQ429ma6No ratings yet
- IM - Facts From Case Files CRCDocument80 pagesIM - Facts From Case Files CRCridin007No ratings yet
- Management of Dry SocketDocument4 pagesManagement of Dry SocketFakhrul ImamNo ratings yet
- Write Up TutorialDocument22 pagesWrite Up Tutorialballer0417100% (1)
- Membrane FiltrationDocument30 pagesMembrane Filtrationsupravietuire100% (1)
- Gestational Trophoblastic DiseaseDocument25 pagesGestational Trophoblastic Diseaseapi-3705046100% (1)
- Spine Oncology, An Issue of Orthopedic Clinics PDFDocument168 pagesSpine Oncology, An Issue of Orthopedic Clinics PDFThanh Le DangNo ratings yet
- Web Amc Cat MCQ Information SheetDocument3 pagesWeb Amc Cat MCQ Information SheetMuhammad Tawfiik Mathure100% (1)
- Acute Gastroenteritis (AGE) PDFDocument37 pagesAcute Gastroenteritis (AGE) PDFAries Chandra AnandithaNo ratings yet
- B1 1 HowIBeatEmphysemaandCOPDinSixWeeks PDFDocument130 pagesB1 1 HowIBeatEmphysemaandCOPDinSixWeeks PDFGreg DaymondNo ratings yet
- Learning ReflectionDocument11 pagesLearning ReflectionTran GatesNo ratings yet
- DRUG STUDY - AmoxicillinDocument7 pagesDRUG STUDY - AmoxicillinFaye Gatchalian100% (1)
- Platelet Rich Plasma in OrthopaedicsDocument269 pagesPlatelet Rich Plasma in OrthopaedicsBelinda Azhari SiswantoNo ratings yet
- Patient Adm NoteDocument4 pagesPatient Adm NoteTraceyNo ratings yet
- H S PPLDocument13 pagesH S PPLPablo Berardo67% (3)
- Esophagus, TearDocument36 pagesEsophagus, Tearapi-19641337No ratings yet
- Katalog Cook Gynekologie PDFDocument70 pagesKatalog Cook Gynekologie PDFHari_Shankar_G_7847No ratings yet
- (MIKROBIOLOGI) IT 20 - Orthomyxovirus, Paramyxovirus - KHSDocument37 pages(MIKROBIOLOGI) IT 20 - Orthomyxovirus, Paramyxovirus - KHSRessy FelisaNo ratings yet
- Medications For Neonatal Resuscitation Program 2011 Canadian AdaptationDocument1 pageMedications For Neonatal Resuscitation Program 2011 Canadian AdaptationrubymayNo ratings yet
- Lab Report - BodDocument11 pagesLab Report - BodZack MalikNo ratings yet
- Dialysis SkillsDocument2 pagesDialysis Skillssheelaaku100% (1)
- Kinesiology 8 - PJJ Assgnment Movement AnalysisDocument64 pagesKinesiology 8 - PJJ Assgnment Movement AnalysispaegyoNo ratings yet