Professional Documents
Culture Documents
Differential Count
Differential Count
Uploaded by
Mohsen HaleemCopyright:
Available Formats
You might also like
- CST Interview Guide PDFDocument159 pagesCST Interview Guide PDFTaha Haq100% (1)
- Manual of Clinical Microbiology 10th Edition MurrayDocument3 pagesManual of Clinical Microbiology 10th Edition MurrayMohsen Haleem15% (20)
- User Manual: Catalog # 001000Document222 pagesUser Manual: Catalog # 001000Kingson WongNo ratings yet
- How To Run A Sample On Vitros XT 7600Document1 pageHow To Run A Sample On Vitros XT 7600rlab49716No ratings yet
- Cairo: Pilbeam's Mechanical Ventilation, 6th EditionDocument6 pagesCairo: Pilbeam's Mechanical Ventilation, 6th Editionفاتن المطيريNo ratings yet
- Basic Infection Control Skills License BICSL Training Guide 2023Document99 pagesBasic Infection Control Skills License BICSL Training Guide 2023Mohsen HaleemNo ratings yet
- Saudi Council ExaminationDocument15 pagesSaudi Council Examinationdedxdreamth95% (41)
- Sedivue Urine Sediment GuideDocument3 pagesSedivue Urine Sediment GuideyanamabrurNo ratings yet
- Draft - Recommended Methods For Blood Grouping Reagents Evaluation PDFDocument55 pagesDraft - Recommended Methods For Blood Grouping Reagents Evaluation PDFwidya astutiNo ratings yet
- MCQDocument85 pagesMCQyasser95% (20)
- Hematology 1 Lab - The Reticulocyte CountDocument17 pagesHematology 1 Lab - The Reticulocyte CountCIRILO MABBORANGNo ratings yet
- Lab AboDocument5 pagesLab Aboclower112No ratings yet
- Manual Platelet CountDocument14 pagesManual Platelet CountMiyo SobremisanaNo ratings yet
- Erythrocyte Sedimentation RateDocument16 pagesErythrocyte Sedimentation Rateapi-3823785100% (2)
- The Clinical LaboratoryDocument24 pagesThe Clinical LaboratoryRomar DurianNo ratings yet
- Exercise 6 Cheek Cell DNA Extraction: Cell and Molecular Biology LaboratoryDocument9 pagesExercise 6 Cheek Cell DNA Extraction: Cell and Molecular Biology LaboratoryDham DoñosNo ratings yet
- Methods of Studying Fungi: Dr. Alice Alma C. BungayDocument74 pagesMethods of Studying Fungi: Dr. Alice Alma C. BungayKaycee Gretz LorescaNo ratings yet
- Preparing A Blood SmearDocument10 pagesPreparing A Blood Smearalan_kadirNo ratings yet
- Final Sop Manual-1-1Document62 pagesFinal Sop Manual-1-1Dianne JoyNo ratings yet
- RBC AnomalyDocument38 pagesRBC AnomalyTorillo KimNo ratings yet
- BloodDocument44 pagesBloodBabak BarghyNo ratings yet
- ABO Blood Group SystemDocument117 pagesABO Blood Group SystemShemiza BalmacoonNo ratings yet
- Gel TechnologyDocument2 pagesGel TechnologyJai Carungay100% (1)
- Antibody TitrationDocument14 pagesAntibody Titrationalibayaty1No ratings yet
- Clinical MicrosDocument14 pagesClinical MicrosKRISTINE JOY PANGAHINNo ratings yet
- 4 - HemoglobinopathiesDocument19 pages4 - HemoglobinopathiesHamzehNo ratings yet
- Capillarys Immunotyping NorestrictionDocument24 pagesCapillarys Immunotyping Norestrictionabbhyasa5206100% (2)
- RCS PreparationDocument3 pagesRCS PreparationMaria Charlene OrpillaNo ratings yet
- Laboratory Evaluation of PlateletsDocument5 pagesLaboratory Evaluation of PlateletsDennis ValdezNo ratings yet
- GPHT1 Lab 3 Shift Reviewer Pap's Smear Prepared By: C Papanicolau'S MethodDocument5 pagesGPHT1 Lab 3 Shift Reviewer Pap's Smear Prepared By: C Papanicolau'S MethodCatherine MerillenoNo ratings yet
- Post Lab 01-09Document7 pagesPost Lab 01-09Patrick ParconNo ratings yet
- Hematology Recall QuestionsDocument4 pagesHematology Recall QuestionsMai RodrigoNo ratings yet
- Hematology PDFDocument85 pagesHematology PDFammarNo ratings yet
- ABO Blood Group SystemDocument26 pagesABO Blood Group SystemFahimNo ratings yet
- Aubf Case Study AbcdefDocument9 pagesAubf Case Study AbcdefChiara Kate CodillaNo ratings yet
- Hematology (Ferrokinetics HemoglobinometryDocument3 pagesHematology (Ferrokinetics HemoglobinometryAbby TorresNo ratings yet
- Anti-Globulin Test AGT (Coomb's Test) Direct, IndirectDocument26 pagesAnti-Globulin Test AGT (Coomb's Test) Direct, Indirectlubna aloshibiNo ratings yet
- Difference Between Precipitation and AgglutinationDocument22 pagesDifference Between Precipitation and AgglutinationMuhammad Awais ZahoorNo ratings yet
- Hematology BMLS 103Document88 pagesHematology BMLS 103harpreetNo ratings yet
- Hematology 2 Topic 2 Prelim2222Document73 pagesHematology 2 Topic 2 Prelim2222Mary Lyka ReyesNo ratings yet
- Bleeding Time, Clotting Time, PT, Aptt, Platelet IndicesDocument59 pagesBleeding Time, Clotting Time, PT, Aptt, Platelet Indicespriya madhooliNo ratings yet
- Reticulocyte CountDocument10 pagesReticulocyte CountNeo Mervyn MonahengNo ratings yet
- Automated Cell Counts HB Estimation MethodsDocument10 pagesAutomated Cell Counts HB Estimation Methodsjohn mwambuNo ratings yet
- M6 Histopath ImpregantionAndEmbeddingDocument4 pagesM6 Histopath ImpregantionAndEmbeddingninaNo ratings yet
- Antihuman GlobulinDocument18 pagesAntihuman GlobulinChariss Pacaldo ParungaoNo ratings yet
- AIMS Professional Exam PackDocument18 pagesAIMS Professional Exam PackDESSA JOY ALVAREZNo ratings yet
- Hematology Week 1 CBCDocument4 pagesHematology Week 1 CBCMICHELLE RAPELONo ratings yet
- Normal Haemopoiesis: Dr. Tariq M. Roshan Department of Hematology PPSPDocument29 pagesNormal Haemopoiesis: Dr. Tariq M. Roshan Department of Hematology PPSPyamanassafNo ratings yet
- Coombs TestDocument6 pagesCoombs TestjnsenguptaNo ratings yet
- Micro 1Document6 pagesMicro 1JOSSHUWA CASISNo ratings yet
- LN Hematology MLT FinalDocument549 pagesLN Hematology MLT FinalMahfuzur Rahman100% (3)
- Lesson 07 PDFDocument14 pagesLesson 07 PDFIhsan UllahNo ratings yet
- Antistreptolysin o (Aso) Latex Slide TestDocument5 pagesAntistreptolysin o (Aso) Latex Slide Testkiedd_04100% (1)
- Basic Clinical Chemistry TestsDocument49 pagesBasic Clinical Chemistry TestsMegbaru100% (1)
- Immunohematology Handout PDFDocument9 pagesImmunohematology Handout PDFTanveerNo ratings yet
- PROTOZOAN Part 1Document1 pagePROTOZOAN Part 1Meccar Moniem H. Elino100% (1)
- Hematology II Notes - MagtalasDocument12 pagesHematology II Notes - MagtalasAbhugz VosotrosNo ratings yet
- Blood Bank ProceduresDocument33 pagesBlood Bank Procedures99noname100% (1)
- Abs Elu HandoutDocument6 pagesAbs Elu HandoutSiti Fadhilla TsabithaNo ratings yet
- Procedures WBC CountDocument2 pagesProcedures WBC CountAlfred ChowNo ratings yet
- Tietz's Applied Laboratory MedicineFrom EverandTietz's Applied Laboratory MedicineMitchell G. ScottRating: 3 out of 5 stars3/5 (1)
- Laboratory Quality Control A Complete Guide - 2020 EditionFrom EverandLaboratory Quality Control A Complete Guide - 2020 EditionNo ratings yet
- 68th AACC Annual Scientific Meeting Abstract eBookFrom Everand68th AACC Annual Scientific Meeting Abstract eBookNo ratings yet
- Practical Haematology GazaDocument86 pagesPractical Haematology GazaTophe DiqiNo ratings yet
- Brochure of ABGDocument4 pagesBrochure of ABGMohsen HaleemNo ratings yet
- ED-60D Control EH0523Document3 pagesED-60D Control EH0523Mohsen HaleemNo ratings yet
- The Api 20E Microtube System For Rapid Identification of Gram NegativeDocument4 pagesThe Api 20E Microtube System For Rapid Identification of Gram NegativeMohsen HaleemNo ratings yet
- Aramco World 2023 CalendarDocument28 pagesAramco World 2023 CalendarMohsen HaleemNo ratings yet
- Requirements For Quality, Safety and Effectiveness of Medical Devices at Healthcare FacilitiesDocument16 pagesRequirements For Quality, Safety and Effectiveness of Medical Devices at Healthcare FacilitiesMohsen HaleemNo ratings yet
- تصحيح النماذج الاربعه للاختبار البرومتركDocument37 pagesتصحيح النماذج الاربعه للاختبار البرومتركMohsen HaleemNo ratings yet
- HIVcomb - Ce Insert Rev.3 0911 EngDocument11 pagesHIVcomb - Ce Insert Rev.3 0911 EngMohsen HaleemNo ratings yet
- ملارياDocument6 pagesملارياMohsen HaleemNo ratings yet
- Sample MCQ's of Bacteriology (M PDFDocument2 pagesSample MCQ's of Bacteriology (M PDFMohsen Haleem74% (23)
- نماذج اختبار الهيئة بالاجااباااتDocument68 pagesنماذج اختبار الهيئة بالاجااباااتjawish81% (48)
- Microbiology Questions PDFDocument5 pagesMicrobiology Questions PDFMohsen HaleemNo ratings yet
- Ø Ø Ù Ùšø Ø Ø Ø Ù Ù 2011Document35 pagesØ Ø Ù Ùšø Ø Ø Ø Ù Ù 2011Farooq MohammadNo ratings yet
- Microbiology Questions PDFDocument5 pagesMicrobiology Questions PDFMohsen HaleemNo ratings yet
- اسئلة هيئه نموذج 1Document12 pagesاسئلة هيئه نموذج 1Mohsen HaleemNo ratings yet
- نماذج اختبار الهيئة بالاجااباااتDocument68 pagesنماذج اختبار الهيئة بالاجااباااتjawish81% (48)
- تصحيح النماذج الاربعه للاختبار البرومتركDocument37 pagesتصحيح النماذج الاربعه للاختبار البرومتركMohsen HaleemNo ratings yet
- اسئلة الهيئه 2010Document6 pagesاسئلة الهيئه 2010Mohsen HaleemNo ratings yet
- StreptococcusDocument22 pagesStreptococcusMohsen HaleemNo ratings yet
- Gram Negative Rods: Lactose Ferments Non Lactose FermentsDocument1 pageGram Negative Rods: Lactose Ferments Non Lactose FermentsMohsen HaleemNo ratings yet
- Bacteriology SummaryDocument38 pagesBacteriology SummaryMohsen HaleemNo ratings yet
- The Panama Aging Research Initiative Longitudinal Study: Lessons From The FieldDocument5 pagesThe Panama Aging Research Initiative Longitudinal Study: Lessons From The FieldMiguel Ángel DominguezNo ratings yet
- Lichen PlanusDocument2 pagesLichen PlanusKunal TejaniNo ratings yet
- Breast Cancer Epidemiology, StellaDocument32 pagesBreast Cancer Epidemiology, StellaLamchabbek NajouaNo ratings yet
- CH 2Document88 pagesCH 2Saurabh JorwalNo ratings yet
- India Immunization Chart 2010Document1 pageIndia Immunization Chart 2010Sarath Nageshwaran SujathaNo ratings yet
- Test Questions GRADE 9 NAIL CAREDocument2 pagesTest Questions GRADE 9 NAIL CARESharmaine ManigosNo ratings yet
- DM GestasionalDocument22 pagesDM GestasionalAditya Arya PutraNo ratings yet
- Abstract Book FinalDocument45 pagesAbstract Book Finalapi-200029530No ratings yet
- HALLOCINOGENDocument43 pagesHALLOCINOGENChinnu ChinnuNo ratings yet
- SequiseZ 70000ON210156 2022 11 11Document19 pagesSequiseZ 70000ON210156 2022 11 11Vipul SinghNo ratings yet
- Neuropsychological Deficits in Disordered Screen Use Behaviours - A Systematic Review and Meta-AnalysisDocument32 pagesNeuropsychological Deficits in Disordered Screen Use Behaviours - A Systematic Review and Meta-AnalysisBang Pedro HattrickmerchNo ratings yet
- Nursing Clinical QuestionsDocument8 pagesNursing Clinical QuestionsMrinalini BakshiNo ratings yet
- hs486 Document OSHA Recording Work-Related Injuries and IllnessesDocument13 pageshs486 Document OSHA Recording Work-Related Injuries and Illnessesfatmata koromaNo ratings yet
- On LeukemiaDocument28 pagesOn LeukemiaMeena Koushal100% (1)
- MIA 22nd July 22Document17 pagesMIA 22nd July 22mn nandaniNo ratings yet
- Bhatia and Speed Grand Test McqsDocument10 pagesBhatia and Speed Grand Test McqsRavi RajaNo ratings yet
- Principles and Practice of Phytotherapy 2013 Calculos BiliaresDocument8 pagesPrinciples and Practice of Phytotherapy 2013 Calculos BiliaresJose Antonio VenacostaNo ratings yet
- Tingkat Pengetahuan TB Paru Mempengaruhi Penggunaan Masker Pada Penderita TB ParuDocument17 pagesTingkat Pengetahuan TB Paru Mempengaruhi Penggunaan Masker Pada Penderita TB ParuDesak PratiwiNo ratings yet
- Bab 7Document27 pagesBab 7bangarudaugtherNo ratings yet
- Anesthesia: Essays and Researches General Anesthesia in Tetanus Patient Undergoing Emergency Surgery: A Challenge For AnesthesiologistDocument4 pagesAnesthesia: Essays and Researches General Anesthesia in Tetanus Patient Undergoing Emergency Surgery: A Challenge For AnesthesiologistEnrico StefanelliNo ratings yet
- Welcome To California Connections Academy!: Log in To Connexus Today-And Often!Document10 pagesWelcome To California Connections Academy!: Log in To Connexus Today-And Often!lesleyNo ratings yet
- Nursing DiagnosisDocument3 pagesNursing DiagnosisPuspita DiahNo ratings yet
- Copy-Of-Chapter 38 Medical Gas TherapyDocument29 pagesCopy-Of-Chapter 38 Medical Gas TherapyMaxinne GorospeNo ratings yet
- Chapter 13 - Diseases of White Blood Cells, Lymph Nodes, Spleen, and ThymusDocument10 pagesChapter 13 - Diseases of White Blood Cells, Lymph Nodes, Spleen, and ThymusAgnieszka WisniewskaNo ratings yet
- RISE CEP Workshop - RISE Tanzania VMMC Project Overview - Handout - September 2022Document2 pagesRISE CEP Workshop - RISE Tanzania VMMC Project Overview - Handout - September 2022munna shabaniNo ratings yet
- Specialized Cells: Sperm Cell Oocyte Stem CellDocument45 pagesSpecialized Cells: Sperm Cell Oocyte Stem CellShiro MisakiNo ratings yet
- Pediatric Assessment TriangleDocument31 pagesPediatric Assessment TriangleblairNo ratings yet
- 10: Use Contextto Determine Meanings of Difficult Words: SkillDocument16 pages10: Use Contextto Determine Meanings of Difficult Words: SkillyusianaNo ratings yet
Differential Count
Differential Count
Uploaded by
Mohsen HaleemOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Differential Count
Differential Count
Uploaded by
Mohsen HaleemCopyright:
Available Formats
GHOR ALSAFI LAB.
Differential Count
A.KAREEM AL-AJOURI 1
White Blood Cells
Differential Count
1. Introduction:
To small laboratories, white blood cell differential becomes a high complexity test
if:
not performed as a direct readout from an automated analyzer
and / or atypical cells are identified.
By including the white blood cell differential in the test menu, the laboratory will
need:
Increased level of necessary staff training
Quality control
Continuing education
An efficient strategy would be to refer blood specimens outside when the white
blood cell count is abnormal initially or significantly changed.
2. Definition:
The white blood cell differential count is performed to determine the relative
number of each type of white blood cell present in the blood.
3. The Normal Reference Ranges:
3.1. Normal Ranges for WBC Differential Count; values expressed in percentages:
3.1. Normal Ranges for WBC Differential Count; values expressed in percentages:
Age
Neutrophils Lymphocytes Monocytes
Neonates & Children
10% - 25% 75% 90% 0% 8%
Adults 25% 75 % 25% 60% 0% 8%
GHOR ALSAFI LAB. Differential Count
A.KAREEM AL-AJOURI 2
3.2. Normal Ranges for WBC Differential Count; values expressed cells X 10
9
/L:
Table 3.2 Normal Ranges for WBC Differential Count (cells X 10
9
/L)
Age
Neutrophils
Eosinophils Basophils Lympho-
cytes
Mono-
cytes
Total
WBC
Count
Total Band Segmented
Birth
6.0-
26
1.0-
1.6
9-11 0.02-0.85 0-0.64 2.0-11.0 0.4-3.1 9-30
7 Days 1.5-
10.0
0-
0.83
2.0-4.7 0.07-1.1 0-0.25 2.0-17.0 0.3-2.7 5.0-
21.0
14
Days
1.0-
9.5
0-
0.63
0-3.9 0.07-1.0 0-0.23 2.0-17.0 0.2-2.4 5.0-
20.0
12
Month
1.5-
8.5
3 1.0- 8.5 0.05- 0.70 0.0- 10.5 4.0-10.5 6.0-
17.5
4
Years
1.5-
8.5
0- 1.0 1.5-7.5 0.02-0.65 0.0-2.0 2.0-8.0 0-0.8 5.5-
15.5
6
Years
1.5-
8.0
0-10 1.5-7.0 0-0.65 0-0.2 1.5-7.0 0-0.8 5.0-
14.5
10
Years
1.8-
8.0
0-1.0 1.8-7.0 0-0.6 0-0.2 1.5-6.5 0-0.8 4.5-
13.5
21
Years
&
above
1.8-
7.7
0-0.7 1.8-7.0 0-0.45 0-0.2 1.0-4.8 0-0.08 4.5-
11.0
4. Clinical Significance:
In certain disease states, a particular white blood cell type may show an absolute
increase in number in the blood.
Common diseases showing an increased number of a specified cell type are listed
bellow:
Absolute increase in the number of neutrophils (neutrophilia):
o Appendicitis
o Myelogenous leukemia
o Bacterial infection
Absolute increase in the number of eosinophils (eosinphilia):
o Allergies
o Scarlet fever
o Parasitic infection
o Eosinophilic leukemia
Absolute increase in the number of basophils (basophilia):
o Allergic reactions
o Chronic myelogenous leukemia
o Basophilic leukemia
o Polycythemia vera
o Following irradiation (transient basophilia)
GHOR ALSAFI LAB. Differential Count
A.KAREEM AL-AJOURI 3
Absolute increase in the number of lymphocytes (lymphocytosis):
o Viral infection
o Whooping cough
o Infectious mononucleosis
o Lymphocytic leukemia
Absolute increase in the number of monocytes (monocytosis):
o Brucellosis
o Tuberculosis
o Monocytic leukemia
o Subacute bacterial endocarditis
o Typhoid
o Ricketsial disease
o Hodgkins disease
o Gauchers disease
5. Preanalytical Conditions:
5.1. Preparation of Patient:
Child and Adult: no special procedure to follow.
5.2. Collection of Specimen:
Morning rested state collection of EDTA blood is recommended.
5.3. Storage Considerations:
Sample is stored at room temperature and is analyzed within 4 hours.
6. Reagents:
6.1 Preparation of the Wright Stain:
6.1.1 Mix the following in a large, tightly stoppered brown bottle:
Wright stain powder 10 grams
Glycerin 90 mL
Methanol 2,910 mL
6.1.2. The stain should be allowed to age for approximately 30 days prior to use. During this
time the stain should be shaken once a day. Incubation at 37C speeds the aging process.
6.1.3. The stain must be freshly filtered before use (only filter 1- or 2- day supply at a time).
GHOR ALSAFI LAB. Differential Count
A.KAREEM AL-AJOURI 4
6.1.4. After the stain is ready to use, use it for a maximum of one month, then discard and
prepare a fresh stain.
6.2. Preparation of the Phosphate Buffer
6.2.1. Mix the following in a large, volumetric flask:
Anhydrous monobasic potassium phosphate (KH2PO4) 6.63 grams
Anhydrous dibasic sodium phosphate (Na2HPO4) 2.56 grams
Distilled water 1000 mL
6.2.2. The pH of the buffer solution should be within a pH range of 6.4 to 6.7, depending on
the staining times and the type of Wright stain used.
7. Procedure:
Table 7. Procedure for Blood Films
Step Procedure
7.1. Manual preparation of the blood smear:
7.1.1. Obtain two clean and dust-free glass slides and a microhematocrit tube.
If using anticoagulated blood, use a plain microhematocrit tube.
One of the slides will be used as a spreader slide. The spreader slide is a glass slide with
specially ground ends to ensure even spreading of the blood. The spreader slide should
be clean and dry.
7.1.2. Fill the microhematocrit tube with the anticoagulated blood.
Carefully place a small drop of blood (2-3 mm in diameter) about 1 cm from the end of
the slide.
7.1.3. Place the slide on a flat table top with the drop of blood on the right.
For left-handed people, the technique is reversed to the opposite hand.
7.1.4. With the thumb and forefinger of the left hand, hold the two left edges of the slide. With
the right hand, hold the spreader slide with the thumb on the edge of one side end and
the forefinger on the edge of the other side. Place the end of the spreader slide slightly
in front of the drop of blood on the other slide, at an angle of 30
0
C to 45
0
C between the
two slides.
7.1.5. Draw the spreader slide back toward the drop of blood. As soon as the spreader slide
comes in contact with the drop of blood, the blood begins to spread to the edge of the
spreader slide. If this does not occur, wiggle the spreader slide a little until it does so. Be
careful that no blood gets in front of the slide.
7.1.6. Keeping the spreader slide at a 30
0
C to 45
0
C angle and the edge of the spreader slide
firmly against the horizontal slide, push the spreader slide at a moderate speed forward
until all the blood has been spread into a moderately thin film.
7.1.7. The blood smears should be dried quickly by waving them rapidly in the air; this
prevents distortion of the red blood cells. The blood smears are now ready for Wrights
stain.
7.1.8. The slide may be labeled by writing the identification with a lead pencil, wax pencil or
diamond pen on the frosted end or directly on the thicker end of the blood film.
GHOR ALSAFI LAB. Differential Count
A.KAREEM AL-AJOURI 5
7.2. Staining of the prepared blood smear:
7.2.1. Place the air dried blood smears on a level staining rack, with the smear side up.
7.2.2. Fix the smears by flooding the slides with methanol for 1-2 minutes. Drain the excess
methanol off the slide. Alternatively, dip the smears into a coplin jar containing
methanol and then place the slides on the staining rack.
7.2.3. Flood the slides with the Wrights stain and time for 4 minutes.
7.2.4. Without removing the Wrights stain add an equal volume of phosphate buffer to the
slide. Mix the two reagents on the slide by gently blowing back and forth over the
solution. A metallic green sheen should now form on top of this mixture. Time 7
minutes.
7.2.5. Rinse the slide off thoroughly with a stream of tap water.
7.2.6. Wipe the back of the slide with a piece of gauze to remove any stain.
7.2.7. Allow the slides to air-dry in a tilted position. Never blot the smears dry.
7.3 Examination of the stained blood smear:
7.3.1. Examine the blood smear using the low-power (10x) objective:
The white blood cells should be evenly distributed over the smear.
Estimate the white blood cell count (by noting the number of white blood cell in relation
to the number or red blood cells).
Examine the thin peripheral edge of the smear, if there is an increased number of white
blood cells in this area, the differential cell count is inaccurate. Most of the cells at the
edge of the smear are the larger white blood cells, namely, neutrophils and monocytes.
This, therefore, shows poor distribution of white blood cell types in this area of the
smear.
7.3.2. Choose the portion of the blood smear where there is only a slight overlapping of the
red blood cells. Place a drop of oil on the slide and carefully change to the oil
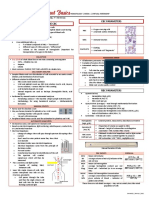
immersion objective (100x).
7.3.3. Begin in the thin area of the slide where the red cells are slightly overlapping. Gradually
move the slide as shown in Figure 1. (Also see Figure 2). Count each white blood cell
seen and record on a differential cell counter until 100 white blood cells have been
counted. If any nucleated red blood cells are seen during the differential count,
enumerate them on a separate counter. These cells are not to be included in the 100-cell
differential count.
7.3.4. While counting the white blood cells, make a note of any abnormalities present in the
cells.
8. Technical Notes:
8.1. Technical Notes on Preparing the Blood Smear:
Table 8.1. Technical notes on preparing the blood smear:
Note Reason
The glass slides must be very clean Any trace of dirt will distort the blood
smear
As soon as the drop of blood is placed on the glass
slide, the smear should be made without delay
Any delay whatsoever results in an
abnormal distribution of WBCs cells, with
many of the larger WBCs accumulating at
thin edge of the smear
GHOR ALSAFI LAB. Differential Count
A.KAREEM AL-AJOURI 6
8.1.1. Common Causes of a Poor Blood Smear:
The drop of blood too large or too small.
The spreader slide pushed across the slide in a jerky manner.
Failure to keep the entire edge of the spreader slide against the slide while making
the smear.
Failure to keep the spreader slide at a 25 angle with the slide (increasing the
angle results in a thicker smear, whereas a smaller angle gives a thin smear).
Failure to push the spreader slide completely across the slide.
8.2. Technical Notes on Staining the Blood Smear:
Table 8.2. Technical notes on staining the blood smear
Problem Reason
Distorted white blood cells Water in the Fixative (methanol). Care must be
taken to change the methanol in the coplin jar
several times a day and to keep the jar covered
when not in use because methanol readily takes
up water. You can place 100-200 mg of
anhydrous copper sulfite in the coplin jar
containing 50 mL methanol to minimize water
uptake by methanol
Uneven staining The staining rack is not exactly leveled.
Precipitate on the smear Insufficient washing of the smear when
removing the stain and buffer mixture
Stain fading - Leaving water on the smear after
rinsing
- Prolonged rinsing
8.2.1. Restaining:
If it is desirable to re-stain a slide, the original Wrights stain may be
removed with methanol. Flood the smear with methanol and rinse
with tap water as many time as necessary to remove the stain and
then re-stain the slide according to the previously described
procedure.
GHOR ALSAFI LAB. Differential Count
A.KAREEM AL-AJOURI 7
8.3. Technical Notes on Differential White Blood Count:
Table 8.3. Technical Notes on differential white blood count:
Problem
What to do
White blood count below 1,000 per L
(difficult to find many white blood cell on the
stained smear)
The differential is usually performed by
counting 50 white blood cells. A notation on
the report must then be made that only 50
white blood cells were counted
In a differential showing one or more of the
following:
- Over 10% eosinophils
- Over 3% basophils
- Over 12% monocytes
- More lymphocytes than neutrophils
200 white blood cells should be counted. The
results are then divided by 2 and a note made
on the report that 200 white blood cells were
counted
Presence of immature white blood cells - Note that there is a left shift (found in
infection and Leukemia)
- Refer the slide for consultation
- Be sure to add a comment that
Immature cells seen
- Phone the physician to bring this matter to his
attention
Presence of increased number of
hypersegmentated neutrophils
Note that there is a right shift
Technical Error Rate 10% to 15%
You might also like
- CST Interview Guide PDFDocument159 pagesCST Interview Guide PDFTaha Haq100% (1)
- Manual of Clinical Microbiology 10th Edition MurrayDocument3 pagesManual of Clinical Microbiology 10th Edition MurrayMohsen Haleem15% (20)
- User Manual: Catalog # 001000Document222 pagesUser Manual: Catalog # 001000Kingson WongNo ratings yet
- How To Run A Sample On Vitros XT 7600Document1 pageHow To Run A Sample On Vitros XT 7600rlab49716No ratings yet
- Cairo: Pilbeam's Mechanical Ventilation, 6th EditionDocument6 pagesCairo: Pilbeam's Mechanical Ventilation, 6th Editionفاتن المطيريNo ratings yet
- Basic Infection Control Skills License BICSL Training Guide 2023Document99 pagesBasic Infection Control Skills License BICSL Training Guide 2023Mohsen HaleemNo ratings yet
- Saudi Council ExaminationDocument15 pagesSaudi Council Examinationdedxdreamth95% (41)
- Sedivue Urine Sediment GuideDocument3 pagesSedivue Urine Sediment GuideyanamabrurNo ratings yet
- Draft - Recommended Methods For Blood Grouping Reagents Evaluation PDFDocument55 pagesDraft - Recommended Methods For Blood Grouping Reagents Evaluation PDFwidya astutiNo ratings yet
- MCQDocument85 pagesMCQyasser95% (20)
- Hematology 1 Lab - The Reticulocyte CountDocument17 pagesHematology 1 Lab - The Reticulocyte CountCIRILO MABBORANGNo ratings yet
- Lab AboDocument5 pagesLab Aboclower112No ratings yet
- Manual Platelet CountDocument14 pagesManual Platelet CountMiyo SobremisanaNo ratings yet
- Erythrocyte Sedimentation RateDocument16 pagesErythrocyte Sedimentation Rateapi-3823785100% (2)
- The Clinical LaboratoryDocument24 pagesThe Clinical LaboratoryRomar DurianNo ratings yet
- Exercise 6 Cheek Cell DNA Extraction: Cell and Molecular Biology LaboratoryDocument9 pagesExercise 6 Cheek Cell DNA Extraction: Cell and Molecular Biology LaboratoryDham DoñosNo ratings yet
- Methods of Studying Fungi: Dr. Alice Alma C. BungayDocument74 pagesMethods of Studying Fungi: Dr. Alice Alma C. BungayKaycee Gretz LorescaNo ratings yet
- Preparing A Blood SmearDocument10 pagesPreparing A Blood Smearalan_kadirNo ratings yet
- Final Sop Manual-1-1Document62 pagesFinal Sop Manual-1-1Dianne JoyNo ratings yet
- RBC AnomalyDocument38 pagesRBC AnomalyTorillo KimNo ratings yet
- BloodDocument44 pagesBloodBabak BarghyNo ratings yet
- ABO Blood Group SystemDocument117 pagesABO Blood Group SystemShemiza BalmacoonNo ratings yet
- Gel TechnologyDocument2 pagesGel TechnologyJai Carungay100% (1)
- Antibody TitrationDocument14 pagesAntibody Titrationalibayaty1No ratings yet
- Clinical MicrosDocument14 pagesClinical MicrosKRISTINE JOY PANGAHINNo ratings yet
- 4 - HemoglobinopathiesDocument19 pages4 - HemoglobinopathiesHamzehNo ratings yet
- Capillarys Immunotyping NorestrictionDocument24 pagesCapillarys Immunotyping Norestrictionabbhyasa5206100% (2)
- RCS PreparationDocument3 pagesRCS PreparationMaria Charlene OrpillaNo ratings yet
- Laboratory Evaluation of PlateletsDocument5 pagesLaboratory Evaluation of PlateletsDennis ValdezNo ratings yet
- GPHT1 Lab 3 Shift Reviewer Pap's Smear Prepared By: C Papanicolau'S MethodDocument5 pagesGPHT1 Lab 3 Shift Reviewer Pap's Smear Prepared By: C Papanicolau'S MethodCatherine MerillenoNo ratings yet
- Post Lab 01-09Document7 pagesPost Lab 01-09Patrick ParconNo ratings yet
- Hematology Recall QuestionsDocument4 pagesHematology Recall QuestionsMai RodrigoNo ratings yet
- Hematology PDFDocument85 pagesHematology PDFammarNo ratings yet
- ABO Blood Group SystemDocument26 pagesABO Blood Group SystemFahimNo ratings yet
- Aubf Case Study AbcdefDocument9 pagesAubf Case Study AbcdefChiara Kate CodillaNo ratings yet
- Hematology (Ferrokinetics HemoglobinometryDocument3 pagesHematology (Ferrokinetics HemoglobinometryAbby TorresNo ratings yet
- Anti-Globulin Test AGT (Coomb's Test) Direct, IndirectDocument26 pagesAnti-Globulin Test AGT (Coomb's Test) Direct, Indirectlubna aloshibiNo ratings yet
- Difference Between Precipitation and AgglutinationDocument22 pagesDifference Between Precipitation and AgglutinationMuhammad Awais ZahoorNo ratings yet
- Hematology BMLS 103Document88 pagesHematology BMLS 103harpreetNo ratings yet
- Hematology 2 Topic 2 Prelim2222Document73 pagesHematology 2 Topic 2 Prelim2222Mary Lyka ReyesNo ratings yet
- Bleeding Time, Clotting Time, PT, Aptt, Platelet IndicesDocument59 pagesBleeding Time, Clotting Time, PT, Aptt, Platelet Indicespriya madhooliNo ratings yet
- Reticulocyte CountDocument10 pagesReticulocyte CountNeo Mervyn MonahengNo ratings yet
- Automated Cell Counts HB Estimation MethodsDocument10 pagesAutomated Cell Counts HB Estimation Methodsjohn mwambuNo ratings yet
- M6 Histopath ImpregantionAndEmbeddingDocument4 pagesM6 Histopath ImpregantionAndEmbeddingninaNo ratings yet
- Antihuman GlobulinDocument18 pagesAntihuman GlobulinChariss Pacaldo ParungaoNo ratings yet
- AIMS Professional Exam PackDocument18 pagesAIMS Professional Exam PackDESSA JOY ALVAREZNo ratings yet
- Hematology Week 1 CBCDocument4 pagesHematology Week 1 CBCMICHELLE RAPELONo ratings yet
- Normal Haemopoiesis: Dr. Tariq M. Roshan Department of Hematology PPSPDocument29 pagesNormal Haemopoiesis: Dr. Tariq M. Roshan Department of Hematology PPSPyamanassafNo ratings yet
- Coombs TestDocument6 pagesCoombs TestjnsenguptaNo ratings yet
- Micro 1Document6 pagesMicro 1JOSSHUWA CASISNo ratings yet
- LN Hematology MLT FinalDocument549 pagesLN Hematology MLT FinalMahfuzur Rahman100% (3)
- Lesson 07 PDFDocument14 pagesLesson 07 PDFIhsan UllahNo ratings yet
- Antistreptolysin o (Aso) Latex Slide TestDocument5 pagesAntistreptolysin o (Aso) Latex Slide Testkiedd_04100% (1)
- Basic Clinical Chemistry TestsDocument49 pagesBasic Clinical Chemistry TestsMegbaru100% (1)
- Immunohematology Handout PDFDocument9 pagesImmunohematology Handout PDFTanveerNo ratings yet
- PROTOZOAN Part 1Document1 pagePROTOZOAN Part 1Meccar Moniem H. Elino100% (1)
- Hematology II Notes - MagtalasDocument12 pagesHematology II Notes - MagtalasAbhugz VosotrosNo ratings yet
- Blood Bank ProceduresDocument33 pagesBlood Bank Procedures99noname100% (1)
- Abs Elu HandoutDocument6 pagesAbs Elu HandoutSiti Fadhilla TsabithaNo ratings yet
- Procedures WBC CountDocument2 pagesProcedures WBC CountAlfred ChowNo ratings yet
- Tietz's Applied Laboratory MedicineFrom EverandTietz's Applied Laboratory MedicineMitchell G. ScottRating: 3 out of 5 stars3/5 (1)
- Laboratory Quality Control A Complete Guide - 2020 EditionFrom EverandLaboratory Quality Control A Complete Guide - 2020 EditionNo ratings yet
- 68th AACC Annual Scientific Meeting Abstract eBookFrom Everand68th AACC Annual Scientific Meeting Abstract eBookNo ratings yet
- Practical Haematology GazaDocument86 pagesPractical Haematology GazaTophe DiqiNo ratings yet
- Brochure of ABGDocument4 pagesBrochure of ABGMohsen HaleemNo ratings yet
- ED-60D Control EH0523Document3 pagesED-60D Control EH0523Mohsen HaleemNo ratings yet
- The Api 20E Microtube System For Rapid Identification of Gram NegativeDocument4 pagesThe Api 20E Microtube System For Rapid Identification of Gram NegativeMohsen HaleemNo ratings yet
- Aramco World 2023 CalendarDocument28 pagesAramco World 2023 CalendarMohsen HaleemNo ratings yet
- Requirements For Quality, Safety and Effectiveness of Medical Devices at Healthcare FacilitiesDocument16 pagesRequirements For Quality, Safety and Effectiveness of Medical Devices at Healthcare FacilitiesMohsen HaleemNo ratings yet
- تصحيح النماذج الاربعه للاختبار البرومتركDocument37 pagesتصحيح النماذج الاربعه للاختبار البرومتركMohsen HaleemNo ratings yet
- HIVcomb - Ce Insert Rev.3 0911 EngDocument11 pagesHIVcomb - Ce Insert Rev.3 0911 EngMohsen HaleemNo ratings yet
- ملارياDocument6 pagesملارياMohsen HaleemNo ratings yet
- Sample MCQ's of Bacteriology (M PDFDocument2 pagesSample MCQ's of Bacteriology (M PDFMohsen Haleem74% (23)
- نماذج اختبار الهيئة بالاجااباااتDocument68 pagesنماذج اختبار الهيئة بالاجااباااتjawish81% (48)
- Microbiology Questions PDFDocument5 pagesMicrobiology Questions PDFMohsen HaleemNo ratings yet
- Ø Ø Ù Ùšø Ø Ø Ø Ù Ù 2011Document35 pagesØ Ø Ù Ùšø Ø Ø Ø Ù Ù 2011Farooq MohammadNo ratings yet
- Microbiology Questions PDFDocument5 pagesMicrobiology Questions PDFMohsen HaleemNo ratings yet
- اسئلة هيئه نموذج 1Document12 pagesاسئلة هيئه نموذج 1Mohsen HaleemNo ratings yet
- نماذج اختبار الهيئة بالاجااباااتDocument68 pagesنماذج اختبار الهيئة بالاجااباااتjawish81% (48)
- تصحيح النماذج الاربعه للاختبار البرومتركDocument37 pagesتصحيح النماذج الاربعه للاختبار البرومتركMohsen HaleemNo ratings yet
- اسئلة الهيئه 2010Document6 pagesاسئلة الهيئه 2010Mohsen HaleemNo ratings yet
- StreptococcusDocument22 pagesStreptococcusMohsen HaleemNo ratings yet
- Gram Negative Rods: Lactose Ferments Non Lactose FermentsDocument1 pageGram Negative Rods: Lactose Ferments Non Lactose FermentsMohsen HaleemNo ratings yet
- Bacteriology SummaryDocument38 pagesBacteriology SummaryMohsen HaleemNo ratings yet
- The Panama Aging Research Initiative Longitudinal Study: Lessons From The FieldDocument5 pagesThe Panama Aging Research Initiative Longitudinal Study: Lessons From The FieldMiguel Ángel DominguezNo ratings yet
- Lichen PlanusDocument2 pagesLichen PlanusKunal TejaniNo ratings yet
- Breast Cancer Epidemiology, StellaDocument32 pagesBreast Cancer Epidemiology, StellaLamchabbek NajouaNo ratings yet
- CH 2Document88 pagesCH 2Saurabh JorwalNo ratings yet
- India Immunization Chart 2010Document1 pageIndia Immunization Chart 2010Sarath Nageshwaran SujathaNo ratings yet
- Test Questions GRADE 9 NAIL CAREDocument2 pagesTest Questions GRADE 9 NAIL CARESharmaine ManigosNo ratings yet
- DM GestasionalDocument22 pagesDM GestasionalAditya Arya PutraNo ratings yet
- Abstract Book FinalDocument45 pagesAbstract Book Finalapi-200029530No ratings yet
- HALLOCINOGENDocument43 pagesHALLOCINOGENChinnu ChinnuNo ratings yet
- SequiseZ 70000ON210156 2022 11 11Document19 pagesSequiseZ 70000ON210156 2022 11 11Vipul SinghNo ratings yet
- Neuropsychological Deficits in Disordered Screen Use Behaviours - A Systematic Review and Meta-AnalysisDocument32 pagesNeuropsychological Deficits in Disordered Screen Use Behaviours - A Systematic Review and Meta-AnalysisBang Pedro HattrickmerchNo ratings yet
- Nursing Clinical QuestionsDocument8 pagesNursing Clinical QuestionsMrinalini BakshiNo ratings yet
- hs486 Document OSHA Recording Work-Related Injuries and IllnessesDocument13 pageshs486 Document OSHA Recording Work-Related Injuries and Illnessesfatmata koromaNo ratings yet
- On LeukemiaDocument28 pagesOn LeukemiaMeena Koushal100% (1)
- MIA 22nd July 22Document17 pagesMIA 22nd July 22mn nandaniNo ratings yet
- Bhatia and Speed Grand Test McqsDocument10 pagesBhatia and Speed Grand Test McqsRavi RajaNo ratings yet
- Principles and Practice of Phytotherapy 2013 Calculos BiliaresDocument8 pagesPrinciples and Practice of Phytotherapy 2013 Calculos BiliaresJose Antonio VenacostaNo ratings yet
- Tingkat Pengetahuan TB Paru Mempengaruhi Penggunaan Masker Pada Penderita TB ParuDocument17 pagesTingkat Pengetahuan TB Paru Mempengaruhi Penggunaan Masker Pada Penderita TB ParuDesak PratiwiNo ratings yet
- Bab 7Document27 pagesBab 7bangarudaugtherNo ratings yet
- Anesthesia: Essays and Researches General Anesthesia in Tetanus Patient Undergoing Emergency Surgery: A Challenge For AnesthesiologistDocument4 pagesAnesthesia: Essays and Researches General Anesthesia in Tetanus Patient Undergoing Emergency Surgery: A Challenge For AnesthesiologistEnrico StefanelliNo ratings yet
- Welcome To California Connections Academy!: Log in To Connexus Today-And Often!Document10 pagesWelcome To California Connections Academy!: Log in To Connexus Today-And Often!lesleyNo ratings yet
- Nursing DiagnosisDocument3 pagesNursing DiagnosisPuspita DiahNo ratings yet
- Copy-Of-Chapter 38 Medical Gas TherapyDocument29 pagesCopy-Of-Chapter 38 Medical Gas TherapyMaxinne GorospeNo ratings yet
- Chapter 13 - Diseases of White Blood Cells, Lymph Nodes, Spleen, and ThymusDocument10 pagesChapter 13 - Diseases of White Blood Cells, Lymph Nodes, Spleen, and ThymusAgnieszka WisniewskaNo ratings yet
- RISE CEP Workshop - RISE Tanzania VMMC Project Overview - Handout - September 2022Document2 pagesRISE CEP Workshop - RISE Tanzania VMMC Project Overview - Handout - September 2022munna shabaniNo ratings yet
- Specialized Cells: Sperm Cell Oocyte Stem CellDocument45 pagesSpecialized Cells: Sperm Cell Oocyte Stem CellShiro MisakiNo ratings yet
- Pediatric Assessment TriangleDocument31 pagesPediatric Assessment TriangleblairNo ratings yet
- 10: Use Contextto Determine Meanings of Difficult Words: SkillDocument16 pages10: Use Contextto Determine Meanings of Difficult Words: SkillyusianaNo ratings yet