Professional Documents
Culture Documents
Paraplegia Types Causes and Diagnosis
Paraplegia Types Causes and Diagnosis
Uploaded by
mudzungCopyright:
Available Formats
You might also like
- Body by RingsDocument6 pagesBody by RingsDenis Osmenaj100% (2)
- Jivamukti Spitirual Warrior ScriptDocument17 pagesJivamukti Spitirual Warrior ScriptvaleriyappvNo ratings yet
- Wasting of Small Muscles of HandDocument38 pagesWasting of Small Muscles of HandSumit Khare75% (4)
- Chapter 26 Guyton and HallDocument5 pagesChapter 26 Guyton and HallSanna Asila AkramNo ratings yet
- Myofascial Trigger PointsDocument17 pagesMyofascial Trigger PointsVera Belchior100% (3)
- Paraplegia-Types, Causes and DiagnosisDocument59 pagesParaplegia-Types, Causes and Diagnosiskashmala afzalNo ratings yet
- Spastic ParaplegiaDocument7 pagesSpastic ParaplegiaDio ResnaNo ratings yet
- ParaplegiaDocument51 pagesParaplegiaChuah Wei HongNo ratings yet
- Neuromuscular DisordersDocument73 pagesNeuromuscular Disordersnurwahidah100% (1)
- Cardiorespiratory Assesment of Tetralogy of Fallot and Physiotherapy Management of Tetralogy of FallotDocument7 pagesCardiorespiratory Assesment of Tetralogy of Fallot and Physiotherapy Management of Tetralogy of FallotAyusa PradhanNo ratings yet
- Diagnosis and Management of Ulnar Nerve PalsyDocument20 pagesDiagnosis and Management of Ulnar Nerve PalsyamaliafarahNo ratings yet
- Cranial Nerves 7-12Document62 pagesCranial Nerves 7-12jangyNo ratings yet
- ASIA Impairment ScaleDocument10 pagesASIA Impairment Scaleazimahzainal211No ratings yet
- Cns ExaminationDocument17 pagesCns ExaminationJuana Maria Garcia Espinoza100% (1)
- MusculoskeletalDocument35 pagesMusculoskeletalZeeshan SiddiquiNo ratings yet
- Scoliosis PPT B IngDocument11 pagesScoliosis PPT B IngSyifa Anindya100% (1)
- LBP in Pregnancy: OMT For The MDDocument23 pagesLBP in Pregnancy: OMT For The MDOkimi Suyi JuliusNo ratings yet
- What Is PolymyositisDocument24 pagesWhat Is PolymyositisAshraf MobyNo ratings yet
- Covid19 - Physiotherapy - Management - Information - GuidanceDocument13 pagesCovid19 - Physiotherapy - Management - Information - GuidanceMasrov TukirovNo ratings yet
- 26 Chronic Pelvic Pain - LR PDFDocument132 pages26 Chronic Pelvic Pain - LR PDFersand2002No ratings yet
- Chvostek's Sign and Carpopedal Spasm NEJM APRIL 2009 PDFDocument1 pageChvostek's Sign and Carpopedal Spasm NEJM APRIL 2009 PDFAnonymous uVinWXfo4No ratings yet
- ORTHO Booklet 427-B1 FinalDocument226 pagesORTHO Booklet 427-B1 FinalMandisa Ndlovu Tenego0% (1)
- Cervical Radiculopathy Part 1 - Clinical Presentation - Rayner & Smale PDFDocument9 pagesCervical Radiculopathy Part 1 - Clinical Presentation - Rayner & Smale PDFItai IzhakNo ratings yet
- Approach To Movement Disorders ..Document54 pagesApproach To Movement Disorders ..Ihda ParidahNo ratings yet
- Congenital Muscular TorticollisDocument29 pagesCongenital Muscular Torticolliskashmala afzal100% (1)
- EndocarditisDocument24 pagesEndocarditisamyNo ratings yet
- Upper and Lower Motor NeuronDocument22 pagesUpper and Lower Motor NeuronJoshua Henrina100% (2)
- Pronator Teres Syndrome FixDocument11 pagesPronator Teres Syndrome FixNUR ZAMZAM AZIZAHNo ratings yet
- Motor Neuron Disease: Amyotrophic Lateral Sclerosis (ALS)Document2 pagesMotor Neuron Disease: Amyotrophic Lateral Sclerosis (ALS)james cordenNo ratings yet
- Brachial Plexus InjuryDocument14 pagesBrachial Plexus InjuryYugaraj ThangaveluNo ratings yet
- Cardiorespiratory AssessmentDocument7 pagesCardiorespiratory AssessmentmalarvelykNo ratings yet
- Arthrokinematics of Body Joints FinalDocument3 pagesArthrokinematics of Body Joints FinalnmahpbooksNo ratings yet
- Peripheral NerveDocument6 pagesPeripheral NerveNur Atiqah ZainalNo ratings yet
- Psoriatic ArthritisDocument12 pagesPsoriatic ArthritisSelvia RosadiNo ratings yet
- Juvenile Rheumatoid ArthritisDocument8 pagesJuvenile Rheumatoid ArthritisDhanNie CenitaNo ratings yet
- LungsDocument16 pagesLungsJoher100% (1)
- Shoulder Joint AssessmentDocument92 pagesShoulder Joint Assessmentsonali tushamerNo ratings yet
- LMNL Vs UmnlDocument49 pagesLMNL Vs UmnlLohshini ManickavasagamNo ratings yet
- CTEVDocument27 pagesCTEVJevisco LauNo ratings yet
- Radial NerveDocument47 pagesRadial NerveFadilla PermataNo ratings yet
- Fractures of The Upper LimbDocument3 pagesFractures of The Upper LimbJim Jose AntonyNo ratings yet
- Nerve InjuryDocument19 pagesNerve Injurybhavesh jain100% (2)
- Blood Supply of BrainDocument2 pagesBlood Supply of BrainvmagtotoNo ratings yet
- Altered Level of ConsciousnessDocument11 pagesAltered Level of ConsciousnessRamji PaudelNo ratings yet
- Male GU ExamDocument5 pagesMale GU ExamOmar Farid ElgebalyNo ratings yet
- Middle Cerebral ArteryDocument4 pagesMiddle Cerebral Arterykat9210No ratings yet
- Nerve Injuries of Upper Limb: Dr. Mujahid KhanDocument41 pagesNerve Injuries of Upper Limb: Dr. Mujahid KhanElton Ndhlovu100% (1)
- Neurological Aspect in Musculoskeletal Diseases Entrapment and CompressionDocument38 pagesNeurological Aspect in Musculoskeletal Diseases Entrapment and CompressionBakingpancakesNo ratings yet
- False Localising SignsDocument46 pagesFalse Localising SignsVarun B RenukappaNo ratings yet
- Lesions of Upper Motor Neurons and Lower Motor NeuronsDocument9 pagesLesions of Upper Motor Neurons and Lower Motor NeuronsAdhitya Rama Jr.No ratings yet
- Pituitary AdenomaDocument20 pagesPituitary AdenomaAbdulaziz Al-TaisanNo ratings yet
- History and Examination: GIT System: Ahmed Laving Paediatric GastroenterologistDocument27 pagesHistory and Examination: GIT System: Ahmed Laving Paediatric Gastroenterologistokwadha simionNo ratings yet
- Knee Special Test FinallllllDocument19 pagesKnee Special Test FinallllllElijah QuianoNo ratings yet
- Back Pain: Group 4Document71 pagesBack Pain: Group 4Cesar Guico Jr.No ratings yet
- Hernia AbdominalisDocument45 pagesHernia AbdominalisFAIRUZ RIFANINo ratings yet
- Spinal Cord InjuryDocument37 pagesSpinal Cord InjuryArfian Deny PNo ratings yet
- Brachial Plexus: MusculocutaneousDocument5 pagesBrachial Plexus: Musculocutaneousashdmb217No ratings yet
- Motor Neuron DiseaseDocument8 pagesMotor Neuron DiseaseyigoNo ratings yet
- Gullaine-Barré SyndromeDocument13 pagesGullaine-Barré SyndromeOnieBoy CurayagNo ratings yet
- Biomechanics of Peripheral and Spinal Nerve RootsDocument86 pagesBiomechanics of Peripheral and Spinal Nerve RootsJawad HassanNo ratings yet
- Cervical Radiculopathy, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandCervical Radiculopathy, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- 19 Spinal CordDocument8 pages19 Spinal Cordkarar AhmedNo ratings yet
- Spinal Cord Disease by GadisaDocument128 pagesSpinal Cord Disease by GadisaGadisa DejeneNo ratings yet
- ParaplegiaDocument56 pagesParaplegiarashid38No ratings yet
- Sensory-Motor Development in The First Year: By:Yohannes PurwantoDocument39 pagesSensory-Motor Development in The First Year: By:Yohannes PurwantoAndrew Aland100% (1)
- Natrum MuriaticumDocument10 pagesNatrum MuriaticumvasgarNo ratings yet
- LegendsDocument2 pagesLegendsEnrique Serrano VelazquezNo ratings yet
- Yoga For DiabetesDocument43 pagesYoga For DiabetesSubramanya SeshagiriNo ratings yet
- The Tibiofibular JointsDocument7 pagesThe Tibiofibular JointsVictor Espinosa BuendiaNo ratings yet
- Assessment of The Ear and Hearing AcuityDocument3 pagesAssessment of The Ear and Hearing AcuityJay Debby RuizoNo ratings yet
- Beginnings Kill ListsDocument16 pagesBeginnings Kill ListsHENRY SINGCOLNo ratings yet
- Training ExercisesDocument197 pagesTraining ExercisesYasir ButtNo ratings yet
- 5:2 Clinical Patterns in ShoulderDocument3 pages5:2 Clinical Patterns in Shoulder莉涵邱No ratings yet
- PIIS0022522317311571Document3 pagesPIIS0022522317311571Juan David Arboleda LopezNo ratings yet
- PancreasDocument2 pagesPancreasSam TagardaNo ratings yet
- 12.basal Nuclei PDFDocument3 pages12.basal Nuclei PDFadiNo ratings yet
- Chapter 1 - Stimuli and ResponsesDocument3 pagesChapter 1 - Stimuli and ResponsesIzz ZiqryNo ratings yet
- Mcu Test Micturating CystourethrogramDocument1 pageMcu Test Micturating CystourethrogramSudharsanNo ratings yet
- Discrepancy Index Scoring SystemDocument26 pagesDiscrepancy Index Scoring SystemJohn PulgarinNo ratings yet
- The Endocrine Systems How The Body WorksDocument3 pagesThe Endocrine Systems How The Body Worksapi-441462208No ratings yet
- Knee Meniscus InjuryDocument6 pagesKnee Meniscus InjuryHazel Aikulola GriffithNo ratings yet
- PEDocument44 pagesPEArifoden AcatoNo ratings yet
- Anatomy and Physiology of The EarDocument46 pagesAnatomy and Physiology of The EarRoni Ananda Perwira HarahapNo ratings yet
- Lesiones Del Rodete GlenoideoDocument6 pagesLesiones Del Rodete Glenoideobarbara liuva chia policarpoNo ratings yet
- Unit 1Document6 pagesUnit 1Mahesh PatilNo ratings yet
- 1.2.3 The Nervous System WorksheetDocument4 pages1.2.3 The Nervous System WorksheetTavon FloydNo ratings yet
- Activity in Digestive System I.: Name of Structure Description No. of Structure (Answer)Document2 pagesActivity in Digestive System I.: Name of Structure Description No. of Structure (Answer)Lainie ZefiahNo ratings yet
- Aries: Head, Brain, & EyesDocument7 pagesAries: Head, Brain, & EyesAtul Chauhan100% (1)
- Accessory LigamentsDocument10 pagesAccessory LigamentsWidy AnniNo ratings yet
- Ossicles: The Malleus, The Incus, and The StapesDocument6 pagesOssicles: The Malleus, The Incus, and The StapesLili M.No ratings yet
Paraplegia Types Causes and Diagnosis
Paraplegia Types Causes and Diagnosis
Uploaded by
mudzungOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Paraplegia Types Causes and Diagnosis
Paraplegia Types Causes and Diagnosis
Uploaded by
mudzungCopyright:
Available Formats
1
PARAPLEGIA- TYPES, CAUSES AND DIAGNOSIS
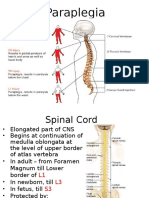
DEFINITION: Paraplegia is impairment in motor and or sensory functions of the lower extremities often including lower part of the trunk. Paraplegia; total paralysis Paraperesis: partial paralysis The area of spinal canal affected-either thoracic or lumbar or sacral region
Most common causes of Paraplegia
Trauma Tumor Tuberculosis Transverse myelitis
CLASSIFICATION OF ETIOLOGY
Figure 1.PARAPLEGIA MAJOR CAUSES
SPINAL CORD LESIONS: COMPRESSIVE MYELOPATHY. Destruction of spinal cord tissue caused by pressure. ( from spinal cord compression by degenerative spinal disease /neoplasms /hematoma or other masses.) Pathogenesis of cord involvement: 1. Direct involvement of roots and cords causing dysfunction.
2. Lesions can interfere with longitudinal and radicular spinal arteries causing ischemia of the segment, which they supply. This vascular disturbance causes local edema of the cord which results in degeneration of the white matter- areas of softening occur.( called compressive myelitis.)
3. Compression can cause pressure effect upon ascending longitudinal spinal vein, which leads to edema of the cord below the site of compression e.g. If there is compression at high cervical level edema can occur at C8T1 level resulting in small muscle wasting. Order of compression of the tracts: 1st Pyramidal tract, then Posterior column, lastly Spinothalamic tract. But exception can occur to this rule.
Explanation for the above; Pyramidal tract is supplied by the terminal branches of spinal arteries and hence most susceptible to compressive ischemia. Another explanation offered: Pyramidal tract is lying closest to denticulate ligament This ligament is subject to traction in spinal cord compression. So pyramidal, tract is most involved. Obstruction of subarachnoid space,
4 below the level of the tumor. causes loculation of CSF -causing the characteristic changes in its composition.
Cause of compression of spinal cord: Classified as 1.Intra medullary and 2Extra medullary
2.Extra medullary causes divisible into Intra dural & Extra dural 2a.Intra dural arise from the dura and compress the cord and roots-typical e.g.meningioma
2b.Extra dural i. Arising from vertebra invading spinal canal and compressing intra spinal structures typical e.g.2ndries of spine from primaries breast, lung, prostate Disc lesions;disc prolapse /spondylosis act similarly ii. Through intervertebral foramina,mass can invade spinal canal e.g Schwanoma,neurofibroma iii. Paravertebral masses of diverse pathologies- can compress roots,their arteries autonomic ,dorsal root ganglia
Elsberg phenomenon; Order of involvement of limbs: In cervical myelopathy first there is weakness of ipsilateral arm,then ipsilstersl leg then contralateral leg and lastly contra lateral arm occurs. This U shaped involvement of the limbs is called Elsberg phenomenon.Occurs in Extradural intra medullary compression.
6 Differences between Extradural and Intradural lesions. Extra dural {Mnemonic- (3Ps) } Pain-present -(root pain and spinal tenderness) Pyramidal involvement early. Proteins in CSF-High.(Froins syndrome) Asymmetrical Intra dural Dissociated anesthesia. Bladder involvement early. Not so high. Symmetrical involvement Trophic Ulcers common
Points, which help in determining level of lesion in spinal cord -compression: 1. Sensory level 2. Motor level 3. Reflex level 4. Root pain-shows dermatome involved. 5. Type of bladder involvement. 6. Autonomic disturbances. Sensory level: Below that level, sensory loss or impairement. Motor level: 1.Beevors sign:- indicates T10 lesion; In positive Beevors sign, umbilicus moves up on raising the head,because lower abdominal muscles are weak. The upper abdominal muscles supplied by T8-T10 pull the umbilicus up. Reflex level: Inverted supinator reflex indicates C5level. If upper abdominal reflexes are preserved & lower abdominal are lostthe level of the lesion is T10. Autonomic disturbances: Below a certain level there will be autonomic disturbances like loss of sweating or excessive sweating, loss of temperature or pilo erection.
DIFFERENCES BETWEEN CORD, NERVE AND ROOT LESIONS
CORD NERVE ROOT
Adjoining area involvement can affect the ascending and descending long tracts
Formed by many roots; supplies definite area. Hence sensory and /motor loss will be confined to that area 2.Can be motor ,sensory or mixed In motor nerve muscles supplied by that motor nerve are wasted after 3wks. In sensory nerve-all types of superficial sensations are lost
2.Cord lesion may be partial; physical findings depend upon that particular area; and long tracts involvement below the lesion UMN paralysis occurs. Below the lesion long sensory tracts( like spinothalamic
Forms apart of nerve or nerves Area supplied by one root ,there is considerable overlapping.Hence the loss is minimal 2.Antr.root-motor atrophy- a part of the muscle;partial wasting postr.root area of sensory loss is minimal ;most marked for pin prick e.g.In S1 lesion area of
7 /posterior column) deficit may be seen. over of distribution of the nerve area In mixed verve lesion combination of both . sensory loss is confined to lateral border of foot.
DIAGNOSIS OF LEVEL OF THE LESION IN COMPRESSIVE MYELOPATHY Upper cervical region& foramen magnum: 1. Severe pain in the occiput &neck. 2. In hands loss of posterior column sensation is early symptom &severe tingling &numbness. Pain & weakness in the limbs & wasting may occur in the upper limb. 3. Movements of diaphragm reduced because of compression of phrenic nerve. 4. Lower cranial nerve involvement &medullary involvement can occur. 5. Descending tract of trigeminal can be involved. C5C6 segment lesion: 1. INVERTED SUPINATOR REFLEX 2. wasting of muscles supplied byC5C6 namely deltoid,biceps, brachioradialis,infra & suprasinators&rhomboids 3. Paraplegia
C8T1 Level: 1. WASTING OF SMALL MUSCLES OF THE HAND. 2. Wasting of flexors of wrist & fingers. 3. Horners syndrome. 4. DTR of upper limbs preserved. 5. Spastic paralysis of trunk & lower limbs. Cervical spondylosis never involves C8& so small muscle wasting rules out cervical spondylosis. Mid Thoracic region of spinal cord:
8 1. Upper limb normal. 2. Wasting of intercostals muscles (those supplied by involved segments) 3. .Movements of diaphragm normal. 4. Spastic paralysis of abdominal muscles &lower limbs. 5. 9th &10th thoracic segments: 1. BEEVORS SIGN (when patient raises the head against resistance umbilicus is drawn upwards). T12L1 segments: Abdominal reflexes preserved Cremastric lost. Paraplegia Wasting of internal oblique & transverse abdominal muscle. L3 L4 segmental lesion: 1. Flexion of hip is preserved. 2. Cremastric preserved. 3. But Quadriceps & adductors of hip are wasted 4. KNEE JERK IS LOST or diminished. 5. BUT ANKLE JERK IS EXAGGERATED. 6. Plantar-extensor. 7. Foot drop S1S2 segments; 1. Wasting & paralysis of intrinsic muscles of feet. 2. Wasting & paralysis of calf muscles Plantor flexion impaired. 3. But dorsi flexion of foot is preserved. 4. In the hip all muscles of hip are preserved except flexors & adductors. 5. In the knee flexors of knee are wasted. 6. KNEE JERK IS PRESERVED 7. ANKLE JERK IS LOST. 8. Plantar reflex is lost. 9. No foot drop. 10. Anal & Bulbocavernous reflexes are preserved. S3S4 segments: 1 .Large bowel & bladder are paralysed. 2. There is RETENSION OF URINE & FEACES due to unopposed action of internal sphincters. 1. The external sphincters are paralyzed. 2. ANAL & BULBO CAVERNOUS REFLEXES ARE LOST. 3. SADDLE SHAPED ANESTHESIA occurs. 4. but no paraplegia Calculating segments involved: from vertebral level For cervical vertebra Add1
9 For T1-T6 - vertebrae Add2 ForT6-T9- vertebrae Add3 T10 vertebra corresponds to L1L2 segments T11 vertebra corresponds to L3L4 segments T12 vertebra corresponds to L5 segment L1 vertebra overlies Sacral and coccygeal segments
Other conditions which produce symptoms similar to Cord compression Pain may be referred pain as in gastritis angina, pleural pain cholycystitis renal calculus To avoid errors thoroughly examine CNS.;usually there will be signs implicating spinal cord; signs of other visceral involvement will be absent. Diagnosis of causes of Paraplegia I. Vertebral Disease-pain,rigidspine,Angular deformity Common cause TB osteitis(young patient,raised ESR,Evidence of Tb focus anywherelse II. 2ndry Carcinoma: middle age,rapid onset,severe pain,h/o surgery for carcinoma,primary detection. III. Cervical Sponylosis: detected by Xray;but can be coincidental finding IV. Spinal tumor:insidious onset,slowly progressive,no evidence of vertebral disease Under general exam look for neurofibroma,pigmentation It is difficult to guess the nature of spinal tumor V. Meningitis: impossible to differentiate pachy meningitis and arachnoiditis: Multiple levels of lesion and patchy and streky arrest of contrast medium indicates -arachnoiditis VI. Myeloma/Pagets:Only by investigations VII. Other rare causes: lymphoma,leukemia,parasitic cyst,extra dural metastasis: Diagnosis-on clinical grounds,evidence of disease elsewhereand investigations
Certain special types of paraplegia
Pure motor paraplegia without sensory loss Hereditary spastic paraplegia Lathyrism Amyotropiclateral sclerosis Flurosis Gullain Barre syndrome
10
Acute paraplegia :
Trauma-fracture dislocationof vertebra Infection:Epidural Abscess\ Vascular:
Thrombosis of Anterior spinal artery Endarteritis(tuberculous,Syphilitic) Hematomyelia(AV malformation,Angioma)
Transverse Myelitis
Cord Compression at multiple levels Arachnoiditis Multiple secondaries Multiple sclerosis Neurofibramatosis Spondylosis-cervical and lumbar level Paraplegia in flexion; Paralysed legs are fixed in flexed posture.occurs in partial transaction of the spinal cord.Extensors are more paralysed than flexors Paraplegia in extension: Occurs in complete transaction of spinal cord,where extra pyramidal tract also is affected and hence no voluntary movements of the limb is possible resulting in paraplegia in extension Mass reflex In severe injury of spinal cord, stimulation below the level of the lesion produces flexion reflexes of the lower limb ,evacuation of bowel and bladder and sweating of the skin below the level of the lesion. NON-COMPRESSIVE MYELOPATHY. Infective Causes: Bacterial: Acute: Staphylococcal (extramural or intradural) Chronic: Tuberculous, Syphilitic. Parasitic: Hydatid, cysticercosis, Schistosomiasis, falciparum malaria. Viral: Polio, Rabies, Herpes zoster,HIV Rickettsial: Typhus fever, spotted fever Fungal: Cryptococcus, Actinomycosis, and coccidiomycosis Immuno Allergic causes: Post vaccinial-Rabies, tetanus, and polio Post exanthematous-Chicken pox, Herpes zoster Demyelinating: Multiple sclerosis, Neuromyelitis optica, Sub acute combined degeneration. TRANSVERSE MYELITIS CAN BE DUE TO INFECTIVE OR IMMUNO ALLERGIC OR DEMYELINATING CAUSES.
11
Heredo familial, Degenerative: Spinocerebellar degeneration. Familial spastic paraplegia Motor neuron Disease Toxic myelopathy: Lathyrism TOCP Arsenic Contrast media used in radiology Intra thecal penicillin Spinal anesthesia SMON-Sub acute myelo opotic neuropathy (long term enteroquinol, large dose; Myelopotic and peripheral neuropathy. Abdominal symptoms. Vascular Disorder: Arteriosclerosis-Anterior spinal artery thrombosis Dissecting aneurysm of aorta AV malformation in spinal cord 2ndry to surgery on aorta Metabolic /Nutrional; B12 deficiency. Pellagra, Myelopathy of chronic liver disease Tropical; Tropical spastic paraplegia Para Neoplastic Syndrome: Physical agents; Irradiation Electric shock to spinal cord Caissons disease. Manifestations of cord /root lesion depends upon 1. Level of lesion 2. Speed of onset 3. Vascular involvement 4. Site Level of the lesion: AboveL1 vertebra- Damage to both cord and roots. Below L1 vertebra- only roots are involved. Speed of the lesion: A rapidly progressive cord lesion produces flaccid paralysis and absent reflexes and extensor plantar. This is similar to spinal shock in trauma. After weeks or days tone becomes hypertonic. Vascular involvement: In cord compression damage may be due to mechanical stretching or ischemia.In certain cases clinical findings indicate cord damage well beyond the site of compression. This shows vessel compression at the site of lesion is causing distant ischemic effect.
12
Site of lesion: Intra medullary lesion produces only segmental signs &symptoms. Extra dural lesions on the other hand produce both signs of root lesion cord lesion. i.e. At the site of lesion LMN segmental lesion with segmental sensory loss & below that levelUMN Lesion & sensory loss plus root pain. . Difference between Cauda equina and Conus lesion. Differentiation is often difficult. Also there can be isolated conus lesion, isolated cauda lesion or a combination. Cauda equina is a bundle of spinal nerve roots arising from lower end of spinal cord. Cauda equina lesion :produces Asymmetric, Atonic, Areflexic, Paraperisis; With bladder & bowel disturbance Plus sensory loss, Saddle shaped anesthesia Pain is common & is referred to perineum & thigh. Conus lesion Conus medullaris is terminal end of spinal cord which occurs at L1L2 level. In spite of paralysis of bladder &rectum if bulbocavernous and anal reflexes are preserved and If there is dissociated sensory loss (over S2S3S4), it is likely that the lesion is in conus. If the lesion extends above S1 then plantar can be extensor, which is never the case with cauda lesion.
13
Features Pain
Cauda lesions Pain in lower limbs is characteristic. Often absent Present only in the involvement of lower sacral roots-usually late. Often asymmetrical or unilateral for a long time. All forms of sensation impaired.
Conus lesions(S3,S4,S5,C1) Often absent or limited to buttocks &perineum. Always present
Bladder and rectal symptoms.
Symmetry
Practically always bilateral.
Sensation
May be dissociated.
14 DTR Both knee & ankle jerk Lost. Flaccid paralysis of legs &feet characteristic of cauda lesion. Absent Present. Only ankle jerk affected/or even that may be spared.
Tone
Trophic changes
Investigations in a case of paraplegia
Plain Xray Spine Myelogram CT scan CSF analysis Plain Xray Spine Lateral and oblique view: Signs of degeneration of spines Reduction of intervertebral space Narrowing of intervertebral foramina Osteophyte formation. Widening of IV foramina-Neuro fibroma Widening of inter peduncular distance:-long standing intramedullary, intradural lesion. Secondaries,myeloma,tuberculous infection: Destruction of vertebra/collapse of vertebra.. AP view: Erosion of the pedicle-extra medullary tumor Para spinal mass; -extra medullary tumor /cold abscess. Myelogram (Must specify at which level lesion is suspected.) A. Extradural: Complete block shows with ragged edge. At times even with complete block contrast can be coaxed beyond the block to determine its upper extent otherwise a cervical puncture may be required. Partial block; Extra dural; Dura mater is lifted away from the vertebral body. B. Intra dural; Intra medullary; contrast is splayed around dilated cord. Extramedullary; cord displaced to one side.
15 CSF Analysis;Lumbar puncture can worsen neurological disease, because of the pressure gradient it creates.So when a compressive lesion is suspected lumbar puncture &CSF analysis can be done at the time of Myelography. CSF protein is increased often especially below the block,more so in extra medullary. Cell count; Increase in Leukocytoes indicates infections like Abcess/TB. CT scan: Plain CT; Can diagnose narrowing of disc disease of lu8mbar region. Can identify narrowing of lumbar canal& thickening of facet joint. Contrast CT is required to show Cord compression.: Best done 6-12 hrs after myelography. Can show amount of compression & delineate neurofibroma likeintraspinal lesions.. MRI: Saggital views are to be taken., not axial views as in case of CT scan. Can differentiate Syringomyelia from intramedullary tumors.
Other investigations; Xray chest: May show P.T,Lymphomaor malignancy. C.S.F.-Electrophoresis to show oligoclonal bands of multiple sclerosis. Serological tests for Syphilis. IgG/Albumin ratio-to diagnose multiple sclerosis. Routine blood test;hematological,biochemical Routine urine exam,urine for culture and sensitivity
Complications of paraplegia:
Bed sores Contractures Urinary tract infection Pneumonia Deep venous thrombosis
---------------------
You might also like
- Body by RingsDocument6 pagesBody by RingsDenis Osmenaj100% (2)
- Jivamukti Spitirual Warrior ScriptDocument17 pagesJivamukti Spitirual Warrior ScriptvaleriyappvNo ratings yet
- Wasting of Small Muscles of HandDocument38 pagesWasting of Small Muscles of HandSumit Khare75% (4)
- Chapter 26 Guyton and HallDocument5 pagesChapter 26 Guyton and HallSanna Asila AkramNo ratings yet
- Myofascial Trigger PointsDocument17 pagesMyofascial Trigger PointsVera Belchior100% (3)
- Paraplegia-Types, Causes and DiagnosisDocument59 pagesParaplegia-Types, Causes and Diagnosiskashmala afzalNo ratings yet
- Spastic ParaplegiaDocument7 pagesSpastic ParaplegiaDio ResnaNo ratings yet
- ParaplegiaDocument51 pagesParaplegiaChuah Wei HongNo ratings yet
- Neuromuscular DisordersDocument73 pagesNeuromuscular Disordersnurwahidah100% (1)
- Cardiorespiratory Assesment of Tetralogy of Fallot and Physiotherapy Management of Tetralogy of FallotDocument7 pagesCardiorespiratory Assesment of Tetralogy of Fallot and Physiotherapy Management of Tetralogy of FallotAyusa PradhanNo ratings yet
- Diagnosis and Management of Ulnar Nerve PalsyDocument20 pagesDiagnosis and Management of Ulnar Nerve PalsyamaliafarahNo ratings yet
- Cranial Nerves 7-12Document62 pagesCranial Nerves 7-12jangyNo ratings yet
- ASIA Impairment ScaleDocument10 pagesASIA Impairment Scaleazimahzainal211No ratings yet
- Cns ExaminationDocument17 pagesCns ExaminationJuana Maria Garcia Espinoza100% (1)
- MusculoskeletalDocument35 pagesMusculoskeletalZeeshan SiddiquiNo ratings yet
- Scoliosis PPT B IngDocument11 pagesScoliosis PPT B IngSyifa Anindya100% (1)
- LBP in Pregnancy: OMT For The MDDocument23 pagesLBP in Pregnancy: OMT For The MDOkimi Suyi JuliusNo ratings yet
- What Is PolymyositisDocument24 pagesWhat Is PolymyositisAshraf MobyNo ratings yet
- Covid19 - Physiotherapy - Management - Information - GuidanceDocument13 pagesCovid19 - Physiotherapy - Management - Information - GuidanceMasrov TukirovNo ratings yet
- 26 Chronic Pelvic Pain - LR PDFDocument132 pages26 Chronic Pelvic Pain - LR PDFersand2002No ratings yet
- Chvostek's Sign and Carpopedal Spasm NEJM APRIL 2009 PDFDocument1 pageChvostek's Sign and Carpopedal Spasm NEJM APRIL 2009 PDFAnonymous uVinWXfo4No ratings yet
- ORTHO Booklet 427-B1 FinalDocument226 pagesORTHO Booklet 427-B1 FinalMandisa Ndlovu Tenego0% (1)
- Cervical Radiculopathy Part 1 - Clinical Presentation - Rayner & Smale PDFDocument9 pagesCervical Radiculopathy Part 1 - Clinical Presentation - Rayner & Smale PDFItai IzhakNo ratings yet
- Approach To Movement Disorders ..Document54 pagesApproach To Movement Disorders ..Ihda ParidahNo ratings yet
- Congenital Muscular TorticollisDocument29 pagesCongenital Muscular Torticolliskashmala afzal100% (1)
- EndocarditisDocument24 pagesEndocarditisamyNo ratings yet
- Upper and Lower Motor NeuronDocument22 pagesUpper and Lower Motor NeuronJoshua Henrina100% (2)
- Pronator Teres Syndrome FixDocument11 pagesPronator Teres Syndrome FixNUR ZAMZAM AZIZAHNo ratings yet
- Motor Neuron Disease: Amyotrophic Lateral Sclerosis (ALS)Document2 pagesMotor Neuron Disease: Amyotrophic Lateral Sclerosis (ALS)james cordenNo ratings yet
- Brachial Plexus InjuryDocument14 pagesBrachial Plexus InjuryYugaraj ThangaveluNo ratings yet
- Cardiorespiratory AssessmentDocument7 pagesCardiorespiratory AssessmentmalarvelykNo ratings yet
- Arthrokinematics of Body Joints FinalDocument3 pagesArthrokinematics of Body Joints FinalnmahpbooksNo ratings yet
- Peripheral NerveDocument6 pagesPeripheral NerveNur Atiqah ZainalNo ratings yet
- Psoriatic ArthritisDocument12 pagesPsoriatic ArthritisSelvia RosadiNo ratings yet
- Juvenile Rheumatoid ArthritisDocument8 pagesJuvenile Rheumatoid ArthritisDhanNie CenitaNo ratings yet
- LungsDocument16 pagesLungsJoher100% (1)
- Shoulder Joint AssessmentDocument92 pagesShoulder Joint Assessmentsonali tushamerNo ratings yet
- LMNL Vs UmnlDocument49 pagesLMNL Vs UmnlLohshini ManickavasagamNo ratings yet
- CTEVDocument27 pagesCTEVJevisco LauNo ratings yet
- Radial NerveDocument47 pagesRadial NerveFadilla PermataNo ratings yet
- Fractures of The Upper LimbDocument3 pagesFractures of The Upper LimbJim Jose AntonyNo ratings yet
- Nerve InjuryDocument19 pagesNerve Injurybhavesh jain100% (2)
- Blood Supply of BrainDocument2 pagesBlood Supply of BrainvmagtotoNo ratings yet
- Altered Level of ConsciousnessDocument11 pagesAltered Level of ConsciousnessRamji PaudelNo ratings yet
- Male GU ExamDocument5 pagesMale GU ExamOmar Farid ElgebalyNo ratings yet
- Middle Cerebral ArteryDocument4 pagesMiddle Cerebral Arterykat9210No ratings yet
- Nerve Injuries of Upper Limb: Dr. Mujahid KhanDocument41 pagesNerve Injuries of Upper Limb: Dr. Mujahid KhanElton Ndhlovu100% (1)
- Neurological Aspect in Musculoskeletal Diseases Entrapment and CompressionDocument38 pagesNeurological Aspect in Musculoskeletal Diseases Entrapment and CompressionBakingpancakesNo ratings yet
- False Localising SignsDocument46 pagesFalse Localising SignsVarun B RenukappaNo ratings yet
- Lesions of Upper Motor Neurons and Lower Motor NeuronsDocument9 pagesLesions of Upper Motor Neurons and Lower Motor NeuronsAdhitya Rama Jr.No ratings yet
- Pituitary AdenomaDocument20 pagesPituitary AdenomaAbdulaziz Al-TaisanNo ratings yet
- History and Examination: GIT System: Ahmed Laving Paediatric GastroenterologistDocument27 pagesHistory and Examination: GIT System: Ahmed Laving Paediatric Gastroenterologistokwadha simionNo ratings yet
- Knee Special Test FinallllllDocument19 pagesKnee Special Test FinallllllElijah QuianoNo ratings yet
- Back Pain: Group 4Document71 pagesBack Pain: Group 4Cesar Guico Jr.No ratings yet
- Hernia AbdominalisDocument45 pagesHernia AbdominalisFAIRUZ RIFANINo ratings yet
- Spinal Cord InjuryDocument37 pagesSpinal Cord InjuryArfian Deny PNo ratings yet
- Brachial Plexus: MusculocutaneousDocument5 pagesBrachial Plexus: Musculocutaneousashdmb217No ratings yet
- Motor Neuron DiseaseDocument8 pagesMotor Neuron DiseaseyigoNo ratings yet
- Gullaine-Barré SyndromeDocument13 pagesGullaine-Barré SyndromeOnieBoy CurayagNo ratings yet
- Biomechanics of Peripheral and Spinal Nerve RootsDocument86 pagesBiomechanics of Peripheral and Spinal Nerve RootsJawad HassanNo ratings yet
- Cervical Radiculopathy, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandCervical Radiculopathy, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- 19 Spinal CordDocument8 pages19 Spinal Cordkarar AhmedNo ratings yet
- Spinal Cord Disease by GadisaDocument128 pagesSpinal Cord Disease by GadisaGadisa DejeneNo ratings yet
- ParaplegiaDocument56 pagesParaplegiarashid38No ratings yet
- Sensory-Motor Development in The First Year: By:Yohannes PurwantoDocument39 pagesSensory-Motor Development in The First Year: By:Yohannes PurwantoAndrew Aland100% (1)
- Natrum MuriaticumDocument10 pagesNatrum MuriaticumvasgarNo ratings yet
- LegendsDocument2 pagesLegendsEnrique Serrano VelazquezNo ratings yet
- Yoga For DiabetesDocument43 pagesYoga For DiabetesSubramanya SeshagiriNo ratings yet
- The Tibiofibular JointsDocument7 pagesThe Tibiofibular JointsVictor Espinosa BuendiaNo ratings yet
- Assessment of The Ear and Hearing AcuityDocument3 pagesAssessment of The Ear and Hearing AcuityJay Debby RuizoNo ratings yet
- Beginnings Kill ListsDocument16 pagesBeginnings Kill ListsHENRY SINGCOLNo ratings yet
- Training ExercisesDocument197 pagesTraining ExercisesYasir ButtNo ratings yet
- 5:2 Clinical Patterns in ShoulderDocument3 pages5:2 Clinical Patterns in Shoulder莉涵邱No ratings yet
- PIIS0022522317311571Document3 pagesPIIS0022522317311571Juan David Arboleda LopezNo ratings yet
- PancreasDocument2 pagesPancreasSam TagardaNo ratings yet
- 12.basal Nuclei PDFDocument3 pages12.basal Nuclei PDFadiNo ratings yet
- Chapter 1 - Stimuli and ResponsesDocument3 pagesChapter 1 - Stimuli and ResponsesIzz ZiqryNo ratings yet
- Mcu Test Micturating CystourethrogramDocument1 pageMcu Test Micturating CystourethrogramSudharsanNo ratings yet
- Discrepancy Index Scoring SystemDocument26 pagesDiscrepancy Index Scoring SystemJohn PulgarinNo ratings yet
- The Endocrine Systems How The Body WorksDocument3 pagesThe Endocrine Systems How The Body Worksapi-441462208No ratings yet
- Knee Meniscus InjuryDocument6 pagesKnee Meniscus InjuryHazel Aikulola GriffithNo ratings yet
- PEDocument44 pagesPEArifoden AcatoNo ratings yet
- Anatomy and Physiology of The EarDocument46 pagesAnatomy and Physiology of The EarRoni Ananda Perwira HarahapNo ratings yet
- Lesiones Del Rodete GlenoideoDocument6 pagesLesiones Del Rodete Glenoideobarbara liuva chia policarpoNo ratings yet
- Unit 1Document6 pagesUnit 1Mahesh PatilNo ratings yet
- 1.2.3 The Nervous System WorksheetDocument4 pages1.2.3 The Nervous System WorksheetTavon FloydNo ratings yet
- Activity in Digestive System I.: Name of Structure Description No. of Structure (Answer)Document2 pagesActivity in Digestive System I.: Name of Structure Description No. of Structure (Answer)Lainie ZefiahNo ratings yet
- Aries: Head, Brain, & EyesDocument7 pagesAries: Head, Brain, & EyesAtul Chauhan100% (1)
- Accessory LigamentsDocument10 pagesAccessory LigamentsWidy AnniNo ratings yet
- Ossicles: The Malleus, The Incus, and The StapesDocument6 pagesOssicles: The Malleus, The Incus, and The StapesLili M.No ratings yet