Professional Documents
Culture Documents
55 To 61
55 To 61
Uploaded by
Dgek LondonCopyright:
Available Formats
You might also like
- Study Guide - Basic Medication Administration ExamDocument2 pagesStudy Guide - Basic Medication Administration ExamChanelle HusbandsNo ratings yet
- Formula Ambroxol JurnalDocument3 pagesFormula Ambroxol Jurnalrd_al_snrNo ratings yet
- Formulasi Sediaan FarmasiDocument11 pagesFormulasi Sediaan FarmasiKukuh PermadiNo ratings yet
- Formulation and In-Vitro Characterization of Risperidone Nanosuspensions For The Enhancement of Drug Release RateDocument16 pagesFormulation and In-Vitro Characterization of Risperidone Nanosuspensions For The Enhancement of Drug Release RateSiva PrasadNo ratings yet
- PR 15003Document6 pagesPR 15003Satvika AdhiNo ratings yet
- Preparation and Evaluation of Wound Healing Activity of Ursolic Acid Nanoemulgel Formulations in RatsDocument11 pagesPreparation and Evaluation of Wound Healing Activity of Ursolic Acid Nanoemulgel Formulations in RatsRAPPORTS DE PHARMACIENo ratings yet
- Formulation and Evaluation of Niosome-Encapsulated Levofloxacin For Ophthalmic Controlled DeliveryDocument11 pagesFormulation and Evaluation of Niosome-Encapsulated Levofloxacin For Ophthalmic Controlled Deliverynurbaiti rahmaniaNo ratings yet
- Experiment KumudDocument8 pagesExperiment KumudSudeep KothariNo ratings yet
- Formulation and in - Vitro Evaluation of Baclofen Gastroretentive Microballoons For Sustained Drug DeliveryDocument10 pagesFormulation and in - Vitro Evaluation of Baclofen Gastroretentive Microballoons For Sustained Drug DeliveryIJRASETPublicationsNo ratings yet
- MY Rsearch Publication 1Document14 pagesMY Rsearch Publication 1Samuel UzonduNo ratings yet
- Uv Spectroscopic Method For Estimation Ofamlodipine Besylate in TabletsDocument5 pagesUv Spectroscopic Method For Estimation Ofamlodipine Besylate in Tabletsk44xpj4zqkNo ratings yet
- 11 ArticleDocument10 pages11 ArticleBaru Chandrasekhar RaoNo ratings yet
- Development and Evaluation of Mucoadhesive Vaginal Tablet of Sertaconazole For Vaginal CandidiasisDocument8 pagesDevelopment and Evaluation of Mucoadhesive Vaginal Tablet of Sertaconazole For Vaginal CandidiasisAnugrah ElfaNo ratings yet
- Formulation and Evaluation of Thermosensitive Intranasal in Situ Gel of Sumatriptan Succinate by Using A Blend of PolymersDocument9 pagesFormulation and Evaluation of Thermosensitive Intranasal in Situ Gel of Sumatriptan Succinate by Using A Blend of PolymersabikeshNo ratings yet
- Etoposide JurnalDocument6 pagesEtoposide JurnalShalie VhiantyNo ratings yet
- Formulation and Evaluation of Sustained Release Sodium Alginate Microbeads of CarvedilolDocument8 pagesFormulation and Evaluation of Sustained Release Sodium Alginate Microbeads of CarvedilolDelfina HuangNo ratings yet
- 4.1 2 PDFDocument6 pages4.1 2 PDFNela SharonNo ratings yet
- Preparation and Evaluation of Sustained Release Microbeads of Norfloxacin Using Sodium AlginateDocument5 pagesPreparation and Evaluation of Sustained Release Microbeads of Norfloxacin Using Sodium AlginateRajesh KumarNo ratings yet
- Jurnal Simultaneous Determination of Reservatives in SucralfateDocument8 pagesJurnal Simultaneous Determination of Reservatives in SucralfateLia EleaNo ratings yet
- Development of Microemulsion For Solubility Enhancement of Poorly Water Soluble Drug ValsartanDocument6 pagesDevelopment of Microemulsion For Solubility Enhancement of Poorly Water Soluble Drug Valsartandini hanifaNo ratings yet
- Pilocarpine Hydrochloride-Loaded NiosomesDocument14 pagesPilocarpine Hydrochloride-Loaded NiosomesĐủ PhạmNo ratings yet
- EJCHEM - Volume 65 - Issue 11 - Pages 155-162Document8 pagesEJCHEM - Volume 65 - Issue 11 - Pages 155-162Gustavo D.B.No ratings yet
- Development and Optimization of Floating Microspheres in AmethopterinDocument6 pagesDevelopment and Optimization of Floating Microspheres in AmethopterinDr Sharique AliNo ratings yet
- Actra 2018 034Document11 pagesActra 2018 034EnggerianiNo ratings yet
- DESIGN AND EVALUATION OF MUCOADHESIVE MICROCAPSULES OF ACECLOFENAC BY SOLVENT EMULSIFICATION METHOD Gangotri Yadav, Resma Jadhav, Vaishali Jadhav, Ashish JainDocument7 pagesDESIGN AND EVALUATION OF MUCOADHESIVE MICROCAPSULES OF ACECLOFENAC BY SOLVENT EMULSIFICATION METHOD Gangotri Yadav, Resma Jadhav, Vaishali Jadhav, Ashish JainiajpsNo ratings yet
- Development and Evaluation of Nanoemulsion of RepaglinideDocument8 pagesDevelopment and Evaluation of Nanoemulsion of Repaglinidevikrantkadam12No ratings yet
- Nano Emulsion Production by Sonication and Microfluidization A ComparisonDocument13 pagesNano Emulsion Production by Sonication and Microfluidization A ComparisonOsama MoussaNo ratings yet
- AJPS - Author TemplateDocument16 pagesAJPS - Author TemplateAdityaNo ratings yet
- AJPS - Author TemplateDocument15 pagesAJPS - Author TemplatePatmasariNo ratings yet
- Formulation and Evaluation of Egg Albumin Based Controlled Release Microspheres of MetronidazoleDocument5 pagesFormulation and Evaluation of Egg Albumin Based Controlled Release Microspheres of MetronidazoleSachin BagewadiNo ratings yet
- NANOPARTICLESDocument8 pagesNANOPARTICLESutdtud jtursNo ratings yet
- Kesharvani 2019Document9 pagesKesharvani 2019RiyanNo ratings yet
- 2 51 1588072528 6.ijmpsapr20206Document14 pages2 51 1588072528 6.ijmpsapr20206TJPRC PublicationsNo ratings yet
- A C A D e M I C S C I e N C e SDocument7 pagesA C A D e M I C S C I e N C e SMSKNo ratings yet
- Salbutamol Sulphate-Ethylcellulose Microparticles: Formulation and In-Vitro Evaluation With Emphasis On Mathematical ApproachesDocument8 pagesSalbutamol Sulphate-Ethylcellulose Microparticles: Formulation and In-Vitro Evaluation With Emphasis On Mathematical ApproachesThiiwiie'thiiwiie PrathiiwiieNo ratings yet
- Article WJPR 1399543685Document14 pagesArticle WJPR 1399543685Nafi Hasan ZahidNo ratings yet
- Chemistry Prject ReportDocument35 pagesChemistry Prject ReportAJ ONLINENo ratings yet
- Spectrophotometric Method Development and ValidatiDocument7 pagesSpectrophotometric Method Development and ValidatiEVELYN SOLANHS ACERO RODRIGUEZNo ratings yet
- Dokumen PDFDocument8 pagesDokumen PDFnadia julisaNo ratings yet
- ASSAY METHOD DEVELOPMENT AND VALIDATION FOR THE ESTIMATION OF SOLIFENACIN SUCCINATE IN TABLETS BY UV SPECTROPHOTOMETRY N.J.R. Hepsebah, A. Ashok KumarDocument6 pagesASSAY METHOD DEVELOPMENT AND VALIDATION FOR THE ESTIMATION OF SOLIFENACIN SUCCINATE IN TABLETS BY UV SPECTROPHOTOMETRY N.J.R. Hepsebah, A. Ashok KumariajpsNo ratings yet
- Composition: 1/26 EMEA 2005Document26 pagesComposition: 1/26 EMEA 2005Argun WidarsaNo ratings yet
- Formulation and Evaluation of in Situ Ophthalmic Gels of Diclofenac SodiumDocument8 pagesFormulation and Evaluation of in Situ Ophthalmic Gels of Diclofenac Sodiumsunaina agarwalNo ratings yet
- Design and Characterization of Zaltoprofen Nanosuspension by Precipitation MethodDocument8 pagesDesign and Characterization of Zaltoprofen Nanosuspension by Precipitation Methodsunaina agarwalNo ratings yet
- Formulation and Evaluation of Mucoadhesive Microcapsules of RifampicinDocument5 pagesFormulation and Evaluation of Mucoadhesive Microcapsules of RifampicinIOSR Journal of PharmacyNo ratings yet
- Formulation and Evaluation of Mefenamic Acid Ointment Using Penetration EnhancersDocument5 pagesFormulation and Evaluation of Mefenamic Acid Ointment Using Penetration EnhancersIndradewiNo ratings yet
- Component Screening of Miconazole Nitrate Nanoemulsion: Research ArticleDocument8 pagesComponent Screening of Miconazole Nitrate Nanoemulsion: Research ArticleSiddhant YadavNo ratings yet
- Claudio Müller, Gloria Godoy, Marta de Diego.: Chemical Stability of Prednisone Oral Suspension and Drug SubstanceDocument5 pagesClaudio Müller, Gloria Godoy, Marta de Diego.: Chemical Stability of Prednisone Oral Suspension and Drug SubstanceGitanti Rohmanda HolaholaNo ratings yet
- Tds 4Document4 pagesTds 4Neha YadavNo ratings yet
- Diltizem MicrosphereDocument11 pagesDiltizem MicrospheredoddadineshNo ratings yet
- Micro EmulsionDocument7 pagesMicro EmulsionIndustrial OilsNo ratings yet
- .Trashed 1662592588 NanoemulsionDocument22 pages.Trashed 1662592588 NanoemulsionRajat KadyanNo ratings yet
- Mucoadhesive MicrospheresDocument20 pagesMucoadhesive MicrospheresRam C DhakarNo ratings yet
- Ashraf M. Mahmoud, Saad A. Alqahtani: American Journal of Analytical Chemistry, 2016, 7, 179-191Document13 pagesAshraf M. Mahmoud, Saad A. Alqahtani: American Journal of Analytical Chemistry, 2016, 7, 179-191DrGajanan VaishnavNo ratings yet
- Design and Evaluation of Sustained Release Microcapsules Containing Diclofenac SodiumDocument4 pagesDesign and Evaluation of Sustained Release Microcapsules Containing Diclofenac SodiumLia Amalia UlfahNo ratings yet
- Formulation and Evaluation of Multiple Emulation of Diclofenac SodiumDocument7 pagesFormulation and Evaluation of Multiple Emulation of Diclofenac SodiumIJRASETPublicationsNo ratings yet
- Nanoparticulas EmulsionesDocument6 pagesNanoparticulas EmulsionesDavid Leonardo CañasNo ratings yet
- Jurnal Uv Vis 8Document3 pagesJurnal Uv Vis 8UnsaniaNo ratings yet
- Optimization of Finasteride Nano-Emulsion Preparation Using Chemometric ApproachDocument5 pagesOptimization of Finasteride Nano-Emulsion Preparation Using Chemometric ApproachNurul Hikmah12No ratings yet
- New Polymers for Encapsulation of Nutraceutical CompoundsFrom EverandNew Polymers for Encapsulation of Nutraceutical CompoundsJorge Carlos Ruiz RuizNo ratings yet
- A Comprehensive Book on Experimental PharmaceuticsFrom EverandA Comprehensive Book on Experimental PharmaceuticsRating: 5 out of 5 stars5/5 (1)
- 10 Intraoperative RadiotherapyDocument11 pages10 Intraoperative RadiotherapyDgek LondonNo ratings yet
- 5-Scanned Ion Beam TherapyDocument17 pages5-Scanned Ion Beam TherapyDgek LondonNo ratings yet
- 7-The Stopping Power ofDocument21 pages7-The Stopping Power ofDgek LondonNo ratings yet
- Quickly Dissolving Amylose Indicator in Cadmium Iodide-Linear Starch Colorimetric ReagentDocument3 pagesQuickly Dissolving Amylose Indicator in Cadmium Iodide-Linear Starch Colorimetric ReagentDgek LondonNo ratings yet
- λ-modulation absorption spectraDocument7 pagesλ-modulation absorption spectraDgek LondonNo ratings yet
- Midterm Examination: N N N NDocument2 pagesMidterm Examination: N N N NDgek LondonNo ratings yet
- An Overview of Recycling of Electronic WasteDocument4 pagesAn Overview of Recycling of Electronic WasteDgek LondonNo ratings yet
- Name - Homework Assignment #5 Angular Kinetics Due 3/13/2014 1) If F (1.67, - 8.5, 4.7) N and R (0.49, 0.12, 0.6) M. Find R X FDocument2 pagesName - Homework Assignment #5 Angular Kinetics Due 3/13/2014 1) If F (1.67, - 8.5, 4.7) N and R (0.49, 0.12, 0.6) M. Find R X FDgek LondonNo ratings yet
- Recovery and Refining of Precious Metals Alloys by Oxi-Nitrogen LeachingDocument9 pagesRecovery and Refining of Precious Metals Alloys by Oxi-Nitrogen LeachingDgek LondonNo ratings yet
- E WasteDocument6 pagesE WasteDgek LondonNo ratings yet
- Leaching of Gold and Silver From Crushed Au-Ag Wastes: Jana Ficeriová, Peter Balá, Erika Dutková and Eberhard GockDocument4 pagesLeaching of Gold and Silver From Crushed Au-Ag Wastes: Jana Ficeriová, Peter Balá, Erika Dutková and Eberhard GockDgek LondonNo ratings yet
- e Waste GoldDocument115 pagese Waste GoldDgek LondonNo ratings yet
- 10 5923 J Ijmee 20120102 02EWASTEDocument5 pages10 5923 J Ijmee 20120102 02EWASTEDgek LondonNo ratings yet
- Lucas vs. TuañoDocument17 pagesLucas vs. TuañoJenny ButacanNo ratings yet
- OBAT2Document12 pagesOBAT2AuliaHadiningratNo ratings yet
- Chewable Lozenges Larry L. Augsburger, Stephen W.Document6 pagesChewable Lozenges Larry L. Augsburger, Stephen W.Faris M ZidiqNo ratings yet
- Oral MoniliasisDocument16 pagesOral MoniliasisMel Izhra N. MargateNo ratings yet
- PiroxicamDocument2 pagesPiroxicamVirginia Aira Lara MarquezNo ratings yet
- Types of Racks For Pharmacy Store by Instor IndiaDocument11 pagesTypes of Racks For Pharmacy Store by Instor IndiaRoshni SharmaNo ratings yet
- Common Medical AbbreviationsDocument4 pagesCommon Medical AbbreviationsJustine DicksonNo ratings yet
- Harga ObatDocument44 pagesHarga ObatFreddy ApotekerNo ratings yet
- ParvezDocument43 pagesParvezShobhit GoswamiNo ratings yet
- Community Pharmacy InternshipDocument8 pagesCommunity Pharmacy InternshipKenny TuanNo ratings yet
- Perioperative Nursing (PreOp)Document51 pagesPerioperative Nursing (PreOp)jessamariesabio100% (1)
- Daftar PustakaDocument4 pagesDaftar PustakaNuryanti RokhmanNo ratings yet
- Nmims India Pharma MarketDocument36 pagesNmims India Pharma MarketAjay SainiNo ratings yet
- Parenteral Administration of DrugsDocument3 pagesParenteral Administration of DrugspauchanmnlNo ratings yet
- Babe 2Document17 pagesBabe 2Sathish SizzyNo ratings yet
- AcetylcysteineDocument2 pagesAcetylcysteineMeriLyn Parayno83% (6)
- Classification of Dangerous DrugsDocument3 pagesClassification of Dangerous Drugsjinmenchie0% (1)
- Zentel Tablets: What Is in This LeafletDocument3 pagesZentel Tablets: What Is in This LeafletLadyKahluaNo ratings yet
- KRATOM 101 - BEGINNER - S GUIDE VENDORS (2) WORD FINALShannon (2) 10 - 14 - 2015 PDFDocument3 pagesKRATOM 101 - BEGINNER - S GUIDE VENDORS (2) WORD FINALShannon (2) 10 - 14 - 2015 PDFDiego CastroNo ratings yet
- Medical Administration RecordDocument1 pageMedical Administration RecorddemereNo ratings yet
- DRUG STUDY: Rocephin - Ceftriaxone SodiumDocument1 pageDRUG STUDY: Rocephin - Ceftriaxone SodiumYum C100% (1)
- Contact Dermatitis 2015parameterDocument39 pagesContact Dermatitis 2015parameterSaniya Ilma ArifaNo ratings yet
- CC3 Finals Toxicology of The Drugs of Abuse-1Document4 pagesCC3 Finals Toxicology of The Drugs of Abuse-1Gabriel QuillNo ratings yet
- Bam Slam Drug CardDocument4 pagesBam Slam Drug CardLeticia GonzalezNo ratings yet
- Mercy Health-Eastgate Medical Center Dedicated: Ensure The Safety of Your Home While You're AwayDocument6 pagesMercy Health-Eastgate Medical Center Dedicated: Ensure The Safety of Your Home While You're AwayDonNo ratings yet
- Jurnal AnestesiDocument8 pagesJurnal AnestesiFaidh HusnanNo ratings yet
- FArmasi RS Dan Klinik KomprehensifDocument8 pagesFArmasi RS Dan Klinik Komprehensifklinik dktNo ratings yet
- Who Uhc Sds 2019.10 EngDocument50 pagesWho Uhc Sds 2019.10 EngChristian ObandoNo ratings yet
- Trima PharmaceuticalsDocument1 pageTrima PharmaceuticalsIsrael ExporterNo ratings yet
55 To 61
55 To 61
Uploaded by
Dgek LondonOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
55 To 61
55 To 61
Uploaded by
Dgek LondonCopyright:
Available Formats
Indian Journal of Pharmaceutical Education and Research
Association of Pharmaceutical Teachers of India
Preparation and In Vitro Characterization of Mucoadhesive Polyvinyl Alcohol Microspheres Containing Amlodipine Besylate for Nasal Administration
N.G.N. Swamy* and Z. Abbas
Department of Pharmaceutics, Government College of Pharmacy, Subbaiah Circle, Bangalore 560027, India
ABSTRACT
Submitted: 23/4/2011
Revised: 21/5/2011
Accepted: 28/6/2011
Amlodipine Besylate microspheres for intranasal administration were prepared with an aim to avoid first-pass metabolism, to achieve controlled blood level profiles and to improve therapeutic efficacy. Polyvinyl Alcohol, a water soluble synthetic polymer, was used in the preparation of microspheres by employing phase separation emulsification technique. The formulation variables were drug concentration, emulsifier concentration, temperature, agitation speed and polymer concentration. All the formulations were evaluated for particle size, particle shape and surface morphology by Scanning Electron Microscopy, percentage yield, drug entrapment efficiency, in vitro mucoadhesion test, degree of swelling and in vitro drug diffusion through sheep nasal mucosa. The microspheres obtained were free flowing, spherical and had a mean particle size of 10.2 3.08 m to 37.2 1.52 m very much suitable for nasal delivery. Increasing the polymer concentration resulted in increased drug entrapment efficiency and increased particle size. Amlodipine Besylate was entrapped into the microspheres with an efficiency of 64.5 2.08 % to 83.6 1.05 %. The prepared microspheres revealed good mucoadhesion properties, swellability and sustained the release of the drug over a period of 8 h. The data obtained were analysed by fitment into various kinetic models; it was observed that the drug release was matrix diffusion controlled and the release mechanism was found to be non-Fickian. Stability studies were carried out on select formulations at 50C 30C, 250C 20C / 60% RH 5% RH and 400C 20C / 75% RH 5% RH for 90 days. The drug content was observed to be within permissible limits and there were no significant deviations in the in vitro mucoadhesion and in vitro drug diffusion characteristics. Keywords: Mucoadhesive microspheres, Amlodipine Besylate, Phase separation emulsification technique, Drug entrapment efficiency, Degree of swelling, In vitro mucoadhesion studies, Nasal drug delivery INTRODUCTION The nasal route is conventionally used for drug delivery for treatment of local diseases1. In the recent years, this route has received special attention as a convenient and reliable method for the systemic delivery of drugs, especially those that are ineffective by oral route due to their metabolism in the gastrointestinal tract being prone to first-pass effect and must be administered by injection2. The nasal cavity as a site for systemic absorption of drugs has advantages such as relatively large surface area, porous endothelial membrane, highly vascularized epithelial layer, enhanced blood flow, avoidance of first-pass metabolism due to lack of gastric and pancreatic enzymatic activity, neutral pH of the nasal mucus and ready accessibility3-4. However, the major limitation of the nasal drug delivery is the mucociliary clearance that provides a limited time available for adsorption within the nasal cavity5.
*Address for Correspondence: Dr. N G N Swamy, Government College of Pharmacy, No.2, P. Kalinga Rao Road, Subbaiah Circle, Bangalore 560 027, Karnataka. E-mail: ngnswami@yahoo.co.in
Nasal mucociliary clearance is one of the most important limiting factor for nasal drug delivery6. It severely limits the time allowed for drug absorption to occur and effectively rules out sustained nasal drug administration. However, mucoadhesive preparations have been developed to achieve the increased contact time of the dosage form with mucosal layers of nasal cavities resulting in enhanced drug absorption7. Amongst the various approaches available to enhance the transnasal delivery of drugs, the mucoadhesive microsphere drug delivery system is an attractive concept that has the ability to control the rate of drug clearance from the nasal cavity as well as to protect the drug from enzymatic degradation. The microspheres form a gel-like layer, which is cleared relatively slowly from the nasal cavity, resulting in prolonged residence time of the drug formulation, thereby increasing the systemic bioavailability of drugs8. Amlodipine Besylate (AB), a calcium channel blocker, is a drug of choice in the treatment of hypertension and angina pectoris. AB on oral administration undergoes first-pass metabolism and exhibits 60-65% bioavailability9. The present investigation was aimed at avoidance of first-pass
52
Ind J Pharm Edu Res, Jan-Mar, 2012/ Vol 46/ Issue 1
N.G.N Swamy et al Preparation and In Vitro Characterization of Mucoadhesive Polyvinyl Alcohol Microspheres Containing Amlodipine Besylate for Nasal Administration
metabolism of AB by preparing Polyvinyl Alcohol (PVA) microspheres for nasal administration. PVA is a water soluble synthetic polymer, used as a viscosity-increasing agent for ophthalmic products, in sustained release formulations for oral administration 10 , in transdermal patches 11 and microspheres for controlled oral drug delivery12. The purpose of this study is to investigate the suitability of PVA microspheres as nasal drug delivery system and also to study the influence of the process variables in the preparation of the microspheres. MATERIALS AND METHODS AB was obtained as a gift sample from Micro labs limited, Bangalore. PVA and Span 80 were purchased from Himedia Laboratories Private limited (Mumbai). Liquid Paraffin (light & heavy) were purchased from Qualigens fine chemicals, All other reagents used were of analytical grade. Preparation of Microspheres Mucoadhesive PVA microspheres containing AB were prepared by Phase separation emulsification technique13. A 1 %w/v aqueous PVA dispersion was prepared using a magnetic stirrer. Pure AB was added to the aqueous polymeric dispersion and it was heated to 800C for 15 minutes by agitation. The resultant dispersion was extruded through a syringe (Needle no. 20) into 100 ml of liquid paraffin (heavy and light 1:1 ratio) previously warmed to the same temperature. This two phase system with 0.5 %w/v span 80 as emulsifying agent was stirred at 1200 rpm for 10 minutes and temperature was maintained at 800C. The resulting water in oil emulsion was then cooled to 50C for 30 minutes by keeping it in an ice water bath. Dehydration was carried out by adding 50 ml of acetone. The mineral oil was decanted and the microspheres obtained were washed three times with 100 ml aliquots of petroleum ether, filtered through Whatman filter paper and then dried in a hot air oven at 500C for 2 h and preserved in a desiccator at room temperature.
Effect of process variables on microsphere properties PVA microspheres were prepared with different drug to polymer ratio (0.5:3, 1:3, 1.5:3 and 2:3) at emulsifier concentrations of 0.2, 0.3, 0.4 and 0.5 % w/v, at temperatures of 60, 70, 80 and 900C, at agitation speeds of 800, 1000, 1200 and 1400 rpm and with varying PVA to drug ratios of 1:1, 2:1, 3:1 and 4:1. The effect of process variables on the properties of the resulting microspheres is depicted in Table 1, 2 and 3. Characterization of Microspheres Percentage Yield: The practical percentage yield14 was calculated from the weight of dried microspheres recovered from each batch in relation to the sum of the initial weight of starting materials. The percentage yield was calculated using the following formula: Practical mass of Microspheres % yield = -------------------------------------------------- X100 Theoretical mass (Polymer + Drug) Drug Entrapment Efficiency: Microspheres equivalent to 5 mg of AB were crushed using a glass mortar and pestle and the powdered microspheres were suspended in 25 ml of phosphate buffer pH 6.4. After 24 h, the solution was filtered; 1 ml of the filtrate was pipetted out and diluted to 10 ml and analyzed for the drug content using Elico SL-159 UV Visible spectrophotometer at 366 nm15. The drug entrapment efficiency16 was calculated using the following formula: Practical Drug content % Drug entrapment efficiency = ------------------------------------- X100 Theoretical Drug content
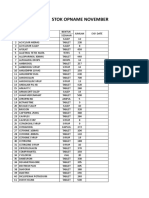
Table 1: Effect of drug to polymer ratio on % drug entrapment efficiency and particle size of microspheres Formula Drug to Emulsifier Temperature % Drug Particle tion polymer concentration (0C) entrapment size code ratio (% w/v) efficiency* (m) PM-1 0.5:3 0.5 80 85.6 1.32 22.62 1.93 PM-2 1:3 0.5 80 81.8 1.52 31.67 2.73 PM-3 1.5:3 0.5 80 77.6 2.01 43.72 2.41 PM-4 2:3 0.5 80 71.2 2.21 51.93 2.38 In all the formulations, agitation speed of 1200 rpm, was kept constant, *Data are expressed as mean SD., n = 3
Ind J Pharm Edu Res, Jan-Mar, 2012/ Vol 46/ Issue 1
53
N.G.N Swamy et al Preparation and In Vitro Characterization of Mucoadhesive Polyvinyl Alcohol Microspheres Containing Amlodipine Besylate for Nasal Administration
Table 2: Effect of emulsifier concentration, temperature and agitation speed on particle size of microspheres Formulation Emulsifier Temperature Agitation speed Particle size code concentration (0C) (rpm) (m)* (% w/v) PM-5 0.2 80 1200 113.2 2.32 PM-6 0.3 80 1200 84.3 2.87 PM-7 0.4 80 1200 58.5 2.44 PM-8 0.5 80 1200 36.2 2.71 PM-9 0.5 60 1200 61.4 2.69 PM-10 0.5 70 1200 45.4 3.11 PM-11 0.5 80 1200 37.4 3.71 PM-12 0.5 90 1200 29.1 4.29 PM-13 0.5 80 800 86.9 4.29 PM-14 0.5 80 1000 58.7 4.21 PM-15 0.5 80 1200 38.1 3.31 PM-16 0.5 80 1400 24.6 3.34 In all the formulations, drug to polymer ratio of 1:4 was maintained constant. *Data are expressed as mean SD., n = 3 Table 3: Influence of polymer to drug ratio on % yield, % drug entrapment efficiency, particle size, degree of swelling and % mucoadhesion Formulation Polymer to % % Drug Particle size Degree of % code drug ratio Yield entrapment (m)* swelling* Mucoadhesion efficiency* PAM-1 1:1 74.65 64.5 2.08 10.2 3.08 0.758 0.012 76.90 0.063 PAM-2 2:1 79.20 76.8 1.42 16.0 2.27 0.873 0.014 79.40 0.098 PAM-3 3:1 83.95 80.4 1.64 27.1 2.41 0.986 0.007 81.40 0.070 PAM-4 4:1 90.14 83.6 1.05 37.2 1.52 1.103 0.019 83.10 0.110 In all the formulations, emulsifier concentration of 0.5% w/v, temperature of 800C and agitation speed of 1200 rpm was maintained constant. *Data are expressed as mean SD., n = 3
Particle Size Analysis
Particle size of the microspheres was determined by optical microscopy. The eye piece micrometer was calibrated with the help of a stage micrometer. The particle diameters of more than 300 microspheres were measured randomly. The average particle size17 was determined by using Edmundson's equation. � � � � � � � � � �nd Dmean = -------------�n Where, n = Number of microspheres checked; d = Mean size range Shape and Surface Morphology The shape and surface characteristics18 of the microspheres were evaluated by means of scanning electron microscopy (JEOL JSM - 840A, Japan). The samples were prepared by
Ind J Pharm Edu Res, Jan-Mar, 2012/ Vol 46/ Issue 1
gently sprinkling the microspheres on a double adhesive tape, which is stuck to an aluminium stub. The stubs were then coated with gold using a sputter coater (JEOL Fine coat JFC 1100E, ion sputtering device) under high vacuum and high voltage to achieve a film thickness of 30 nm. The samples were then imaged using a 20 KV electron beam. Degree of Swelling The Swellability19 of microspheres in physiological media was determined by allowing the microspheres to swell in the phosphate buffered saline pH 6.4. 100 mg of accurately weighed microspheres were immersed in little excess of phosphate buffered saline of pH 6.4 for 24 h and washed thoroughly with deionised water. The degree of swelling was arrived at using the following formula; Ws - Wo � = --------------WO
54
N.G.N Swamy et al Preparation and In Vitro Characterization of Mucoadhesive Polyvinyl Alcohol Microspheres Containing Amlodipine Besylate for Nasal Administration
Where, is the degree of swelling; Wo is the weight of microspheres before swelling and Ws is the weight of microspheres after swelling In Vitro Mucoadhesion Studies: The in vitro mucoadhesion study of microspheres was assessed using Falling liquid film technique20. A strip of sheep nasal mucosa was mounted on a glass slide and 50 mg of accurately weighed microspheres were sprinkled on the nasal mucosa. This glass slide was incubated for 15 min in a desiccator at 90% relative humidity to allow the polymer to interact with the membrane and finally placed on the stand at an angle of 450. Phosphate buffered saline of pH 6.4 previously warmed to 37 0.50C was allowed to flow over the microspheres and membrane at the rate of 1 ml/min for 5 min with the help of a peristaltic pump. At the end of this process, the detached particles were collected and weighed. Weight of Sample - Weight of detached particles % Mucoadhesion = ---------------------------------------------------- X 100 weight of sample In Vitro Drug Diffusion Studies: Preparation of nasal mucosa: Fresh sheep nasal mucosa was collected from a nearby slaughter house. The nasal mucosa of sheep was separated from sub layer bony tissues and stored in distilled water containing few drops of Gentamycin injection21. After complete removal of blood from mucosal surface, it was attached to the donor chamber tube. In vitro nasal diffusion study22 was done using nasal diffusion cell, having three openings each for sampling, thermometer and donor tube chamber. The receptor compartment with a capacity of 60 ml was used in the study in which Phosphate buffered saline of pH 6.4 was taken. Within 80 min of removal, the nasal mucosa measuring an area of 3 cm2 was carefully cut with a scalpel and tied to the donor tube chamber and it was placed in contact with the diffusion medium in the recipient chamber. Microspheres equivalent to 5 mg of AB were spread on the sheep nasal mucosa. At hourly intervals, 1 ml of the diffusion sample was withdrawn with the help of a hypodermic syringe, diluted to 10 ml and absorbance was read at 366 nm. Each time, the sample withdrawn was replaced with 1 ml of pre-warmed Phosphate buffered saline (pH 6.4) to maintain a constant volume of the receptor compartment vehicle. In Vitro Drug Release Kinetics: For understanding the mechanism of drug release and release rate kinetics23 of the drug from the dosage form, the data obtained was analysed with software (PCP - Disso V2.08)24 equipped with zero order, first order, Higuchi matrix and
Ind J Pharm Edu Res, Jan-Mar, 2012/ Vol 46/ Issue 1
Krosmeyer Peppas model kinetics. By analyzing the R values, the best fit model was arrived at. Stability studies: Stability studies were carried out at 50C 30C, 250C 20C / 60% RH 5% RH and 400C 20C / 75% RH 5% RH for three months using Programmable environmental test chambers 25 (REMI Instruments ltd.). The selected formulations were packed in amber coloured glass containers and closed with air tight closures and stored for 90 days. Samples were analyzed at the end of 30, 60 and 90 days and they were evaluated for % Drug entrapment efficiency, in vitro mucoadhesion test and in vitro drug diffusion studies. RESULTS AND DISCUSSION The mucoadhesive microspheres of PVA were prepared by phase separation emulsification technique. Preliminary trials were carried out to optimize the process of preparation. Batches PM-1 to PM-16 were prepared to study the effect of drug to polymer ratio, emulsifier concentration, temperature and agitation speed on the % drug entrapment efficiency and Particle size. As the drug to polymer concentration was varied from 0.5:3 to 2:3, it was observed that the particle size increased, whereas, entrapment efficiency decreased. The increase in particle size could be attributed to the increased drug content of the emulsion droplet at higher drug concentration. The decrease in entrapment efficiency with increase in drug concentration could be related to the increased extent of drug diffusion to the external phase due to greater flux at higher drug content during the emulsification and microsphere formation process. Hence, further trials were carried out with a drug to polymer ratio of 1:3. Increasing the surfactant concentration from 0.2 to 0.5% w/v exhibited a reversal in trend between particle sizes. Microspheres fabricated with 0.2% w/v Span 80 showed the largest particle size while those fabricated with 0.5% w/v showed lowest particle size. When the surfactant is added in small concentrations, it may not have been able to cover the entire droplet surface. Thus some of the droplets would tend to aggregate till the surface area was decreased to such a point that the available amount of surfactant was able to coat the entire surface of the agglomerate and form a stable emulsion resulting in a larger microparticle size. When the concentration of emulsifier is increased, it will allow the emulsion to stabilize to a greater interfacial surface area, thus leading to smaller particle size. Based on these observations, concentration of emulsifier was optimized to 0.5% w/v. Increase in the temperature from 600C to 900C led to a decrease in the mean particle size. However, further increase
55
N.G.N Swamy et al Preparation and In Vitro Characterization of Mucoadhesive Polyvinyl Alcohol Microspheres Containing Amlodipine Besylate for Nasal Administration
in temperature above 900C did not produce any significant change in the mean particle size. Increase in temperature from 600C to 900C increases the degree of congealing or rigidization of the polymer, which ultimately results in shrinking of the particles, leading to a decrease in particle size. Hence for the final formulation design, a temperature of 800C was optimized. The results were in general agreement with the general theory of microspheres that the particle size of microspheres prepared at 1400 rpm were smaller than those prepared at 800, 1000 and 1200 rpm. Since the microspheres obtained at 1200 rpm were in the size range of 30-40 m, suitable for nasal delivery, 1200 rpm was chosen to obtain microspheres. It was observed that as the polymer to drug ratio increases, the product yield also increases. The low percentage yield in some formulations may be due to microspheres lost during the washing process. The percentage yield was found to be in the range of 74.65 to 90.14%. Percentage drug entrapment efficiency of AB ranged from 64.5 2.08 % to 83.6 1.05 % for PVA microspheres. Increase in the polymer concentration resulted in increased viscosity of the dispersed phase. The particle size increases exponentially with viscosity. The higher viscosity of the polymer solution at the highest polymer concentration would be expected to decrease the diffusion of the drug into the external phase which would obviously result in higher entrapment efficiency. The prepared microspheres were in a size range suitable for nasal drug delivery. The mean microsphere size increased with increasing polymer concentration due to a significant increase in the viscosity, thus leading to an increased aqueous droplet size resulting in an increased microsphere size. PVAAB microspheres in the size range of 10.2 3.08 m to 37.2 1.52 m were obtained. The photographs of the optimized formulation taken by scanning electron microscope are depicted in the Figure 1 and 2. The SEM photographs revealed that the microspheres of PVA (PAM-4) were discrete and spherical in shape with a rough outer surface morphology which could be because of the surface association of the drug with the polymer. The pores on microsphere surface could help in drug release by diffusion mechanism. Swellability is an indicative parameter for rapid availability of drug solution for diffusion with greater flux. Swellability data revealed that the amount of polymer plays an important role in solvent transfer. It can be concluded from the data shown in Table 3 that, with an increase in polymer concentration, the degree of swelling also increases ranging from 0.758 0.012 to 1.103 0.019. Thus, we can say that the amount of polymer directly affects the degree of swelling. As the polymer to drug ratio is increased, PVA microspheres
Ind J Pharm Edu Res, Jan-Mar, 2012/ Vol 46/ Issue 1
Fig. 1: SEM microphotograph of optimized formulation (Low magnification)
Fig. 2: SEM microphotograph of optimized formulation (High magnification)
exhibited an increase in % mucoadhesion ranging from 76.90 0.063 to 83.10 0.110; the results of in vitro mucoadhesion test are compiled in Table 3. The in vitro diffusion of AB from the prepared microspheres exhibited a biphasic mechanism. The release of AB from the microspheres was characterized by an initial phase of burst effect due to the presence of drug particles on the surface of the microspheres followed by a second phase of moderate release. The initial bursting phenomenon is an effect very much desired to achieve initial therapeutic plasma concentration of the drug. The initial burst effect was considerably reduced with increase in polymer concentration. The increase in the polymer concentration resulting in better drug entrapment
56
N.G.N Swamy et al Preparation and In Vitro Characterization of Mucoadhesive Polyvinyl Alcohol Microspheres Containing Amlodipine Besylate for Nasal Administration
efficiency could be the reason for the observed decrease in burst effect. As the polymer to drug ratio (PAM-1 to PAM-4) was increased, the extent of drug release decreased from 98.85 81.77%. A significant decrease in the rate and extent of drug release is attributed to the increase in density of polymer matrix that results in increased diffusion path length which the drug molecules have to traverse. The release of the drug has been controlled by swelling control release mechanism. Additionally, the larger particle size at higher polymer concentration also restricts the total surface area thus resulting in slower drug release over a span of 8 h. The comparative in vitro drug diffusion profile from the PVA microspheres is depicted in Figure 3.
that diffusion was the main mechanism of drug release from the mucoadhesive microspheres. Further, the observed diffusion coefficient values are indicative of the fact that the drug release from the formulation follows non-Fickian transport mechanism. The stability data showed that there was no change in the appearance of the microspheres indicating that the formulations were stable at different conditions of storage. It was observed that there was slight reduction in the drug content of the microspheres which were stored at 400C 20C / 75% RH 5% RH at the end of 90 days and no significant change in drug content were observed for formulations stored at room temperature and at 50C 30C. The extent of mucoadhesion of the formulations did not show any significant change after the microspheres were subjected to stability studies. In vitro drug diffusion studies for all the four formulations were carried out at the end of 90 days and did not reveal any significant change in drug release from all the formulations. Thus, we may conclude that, the drug does not undergo degradation on storage. Fig. 4: Higuchi Plot
The drug release kinetic data is compiled in Table 4. In all the cases, the R values of Higuchi matrix model were close to 1. The diffusion coefficient (n) values ranged between 0.4886 to 0.6606. Since the R values of Higuchi matrix were close to 1, the drug release follows matrix diffusion kinetics and the plot shown in Figure 4 revealed linearity; hence it was concluded
Fig. 3: In vitro diffusion profile of PVA microspheres
Table 4: In vitro release data fitment into various mathematical models PAM-1 PAM-2 PAM-3 PAM-4 Zero order R 0.8104 0.8140 0.8618 0.9013 k 0.1470 0.1361 0.1273 0.1192 First order R 0.8120 0.8154 0.8629 0.9021 k -0.0015 -0.0014 -0.0013 -0.0012 Matrix R 0.9910 0.9880 0.9918 0.9920 k 0.3591 0.3324 0.3091 0.2872 Hixon- Crowell R 0.8115 0.8149 0.8626 0.9019 k -0.0005 -0.0005 -0.0004 -0.0004 Peppas R 0.9775 0.9622 0.9644 0.9660 k 0.3700 0.3209 0.2721 0.2266 n 0.4886 0.5330 0.5910 0.6606
Ind J Pharm Edu Res, Jan-Mar, 2012/ Vol 46/ Issue 1 57
N.G.N Swamy et al Preparation and In Vitro Characterization of Mucoadhesive Polyvinyl Alcohol Microspheres Containing Amlodipine Besylate for Nasal Administration
CONCLUSION The Phase separation emulsification technique for obtaining PVA microspheres has proved to be a useful tool in the preparation of microspheres for nasal drug delivery. By virtue of prolonged drug residence at the site of absorption, improved bioavailability can be achieved in contrast to oral dosage form prone for first-pass metabolism. ACKNOWLEDGEMENTS The authors wish to thank Messrs Micro Labs limited, Bangalore, for sparing gift sample of Amlodipine Besylate. The authors are thankful to the Principal, Government College of Pharmacy, Bangalore for extending the laboratory facilities to carry out the Research work. REFERENCES 1. Gavini E, Hegge AB, Rassu G, Sanna V, Testa C et al. Nasal administration of Carbamazepine using chitosan microspheres: in vitro/in vivo studies. Int J Pharm 2006; 307: 915. Mainardes RM, Cocenza urban MC, Cinto PO, Chaud MV, Evangelista RC et al. Liposomes and micro / nanoparticles as colloidal carriers for nasal drug delivery. Curr Drug Delivery 2006; 3: 275-85. Jadhav KR, Gambhire MN, Shaikh IM, Kadam VJ and Pisal SS. Nasal drug delivery system factors affecting and applications. Current Drug Therapy 2007; 2: 27-38. Krishnamoorthy R, Mitra AK.Prodrugs for nasal drug delivery. Advanced drug delivery reviews 1998; 29: 135 46. Soane RJ, Frier M, perkins AC, Jones NS, Davis SS et al. Evaluation of the clearance characteristics of bioadhesive systems in humans. Int J pharm 1999; 178: 55-65. Canan Hascicek, Nursin Gonul, Nevin Erk. Mucoadhesive microspheres containing gentamicin sulfate for nasal administration: preparation and in vitro characterization. IL Farmaco 2003; 58: 11-6. Vidgren P, Vidgren M, Vainio P, Nuutinen J, Paronen P. Doublelabelling technique in the evaluation of disodium cromoglycate microspheres. Int J Pharm 1991;73: 131-6. Chein YW. Nasal drug delivery and drug delivery systems, In: Novel Drug Delivery Systems. 2nded. New York:Marcel Dekker Inc.; 1992. P. 229 - 68. Patil SB, Murthy RSR. Preparation and in vitro evaluation of mucoadhesive chitosan microspheres of Amlodipine Besylate for Nasal Administration. Indian J Pharm Sci 2006; 68(1): 64 7.
11. Wan LSC, Lim LY. Drug release from heat-treated polyvinyl alcohol films. Drug Dev Ind pharm 1992; 18: 1895 - 906. 12. Thanoo BC, Sunny MC, Jayakrishnan A. Controlled release of oral drugs from crosslinked polyvinyl alcohol microspheres. J Pharm Pharmacol 1993; 45: 16 20. 13. Muthuswamy K, Shibi KP, Ravi TK. Preparation and Evaluation of Albumin Chitosan microspheres containing Theophylline. Indian J Pharm Sci 2004; 245 8. 14. Mahajan HS, Gattani SG. Gellan gum based microparticles of Metoclopromide hydrochloride for Intranasal delivery: Development and Evaluation.Chem Pharm Bull 2009; 57(4): 388-92. 15. British Pharmacopoeia, Medicinal and Health care products Regulatory Agency (MHRA): London; 2005, Vol. 2, 126-8. 16. Dubey RR, Parikh RH. Two-stage optimization process for formulation of Chitosan microspheres. AAPS PharmSciTech 2004; 5(1): 1-9. 17. Dandagi PM, Mastiholimath VS, Gadad AP, Iliger SR. Mucoadhesive microspheres of Propranolol Hydrochloride for Nasal Delivery. Indian J Pharm Sci 2007; 69(3): 402-7. 18. Chaurasia M, Chourasia MK, Jain NK, Jain A, Soni V, et al. Cross-Linked Guar Gum Microspheres: A viable approach for improved delivery of Anticancer Drugs for the treatment of Colorectal Cancer. AAPS PharmSciTech 2006; 7 (3): E1-E9. 19. Jain SK, Jain NK, Gupta Y, Jain A, Jain D, et al. Mucoadhesive chitosan microspheres for non-invasive and improved nasal delivery of Insulin. Indian J Pharm Sci 2007; 69(4): 498-504. 20. Ascentiis AD, Grazia JL, Bowman CN, Colombo P, Peppas NA. Mucoadhesion of poly (2-hydroxyethyl methacrylate) is improved when linear poly (ethylene oxide) chains are added to the polymer network. J Controlled Release 1995; 33: 197-201. 21. Chaudhari PD, Pramod Kolsure, Amit Ajab, Nishant Vari. Recent trends in nasal drug delivery systems An overview. Pharmaceutical Reviews 2006; 4(5): www.pharmainfo.net. 22. Pisal S, Shelke V, Mahadik K, Kadam S. Effect of Organogel components on in vitro nasal delivery of Propranolol hydrochloride. AAPS PharmSciTech 2004; 4: 1-9. 23. Costa P, Lobo JMS. Modeling and Comparision of dissolution profiles. Eur J Pharm Sci 2001; 13: 123-33. 24. Swamy NGN, Rupa V, Abbas Z, Dasankoppa FS. Formulation and evaluation of Nanosuspensions for enhancing the dissolution of poorly soluble Mebendazole. Indian Drugs 2010; 47(9): 47-54. 25. Tamizharasi S, Rathi JC, Rathi V. Formulation and evaluation of Pentoxifylline-loaded poly (-caprolactone) microspheres. Indian J Pharm Sci 2008; 70(3): 333-7.
58
2.
3.
4. 5.
6.
7.
8.
9.
10. Raymond C.R., Sheskey P.J., Owen S.C.; (editors) Handbook of Pharmaceutical Excipients. 5th edition. Pharmaceutical Press and the American Pharmacists Association., 2006, 592 3.
Ind J Pharm Edu Res, Jan-Mar, 2012/ Vol 46/ Issue 1
You might also like
- Study Guide - Basic Medication Administration ExamDocument2 pagesStudy Guide - Basic Medication Administration ExamChanelle HusbandsNo ratings yet
- Formula Ambroxol JurnalDocument3 pagesFormula Ambroxol Jurnalrd_al_snrNo ratings yet
- Formulasi Sediaan FarmasiDocument11 pagesFormulasi Sediaan FarmasiKukuh PermadiNo ratings yet
- Formulation and In-Vitro Characterization of Risperidone Nanosuspensions For The Enhancement of Drug Release RateDocument16 pagesFormulation and In-Vitro Characterization of Risperidone Nanosuspensions For The Enhancement of Drug Release RateSiva PrasadNo ratings yet
- PR 15003Document6 pagesPR 15003Satvika AdhiNo ratings yet
- Preparation and Evaluation of Wound Healing Activity of Ursolic Acid Nanoemulgel Formulations in RatsDocument11 pagesPreparation and Evaluation of Wound Healing Activity of Ursolic Acid Nanoemulgel Formulations in RatsRAPPORTS DE PHARMACIENo ratings yet
- Formulation and Evaluation of Niosome-Encapsulated Levofloxacin For Ophthalmic Controlled DeliveryDocument11 pagesFormulation and Evaluation of Niosome-Encapsulated Levofloxacin For Ophthalmic Controlled Deliverynurbaiti rahmaniaNo ratings yet
- Experiment KumudDocument8 pagesExperiment KumudSudeep KothariNo ratings yet
- Formulation and in - Vitro Evaluation of Baclofen Gastroretentive Microballoons For Sustained Drug DeliveryDocument10 pagesFormulation and in - Vitro Evaluation of Baclofen Gastroretentive Microballoons For Sustained Drug DeliveryIJRASETPublicationsNo ratings yet
- MY Rsearch Publication 1Document14 pagesMY Rsearch Publication 1Samuel UzonduNo ratings yet
- Uv Spectroscopic Method For Estimation Ofamlodipine Besylate in TabletsDocument5 pagesUv Spectroscopic Method For Estimation Ofamlodipine Besylate in Tabletsk44xpj4zqkNo ratings yet
- 11 ArticleDocument10 pages11 ArticleBaru Chandrasekhar RaoNo ratings yet
- Development and Evaluation of Mucoadhesive Vaginal Tablet of Sertaconazole For Vaginal CandidiasisDocument8 pagesDevelopment and Evaluation of Mucoadhesive Vaginal Tablet of Sertaconazole For Vaginal CandidiasisAnugrah ElfaNo ratings yet
- Formulation and Evaluation of Thermosensitive Intranasal in Situ Gel of Sumatriptan Succinate by Using A Blend of PolymersDocument9 pagesFormulation and Evaluation of Thermosensitive Intranasal in Situ Gel of Sumatriptan Succinate by Using A Blend of PolymersabikeshNo ratings yet
- Etoposide JurnalDocument6 pagesEtoposide JurnalShalie VhiantyNo ratings yet
- Formulation and Evaluation of Sustained Release Sodium Alginate Microbeads of CarvedilolDocument8 pagesFormulation and Evaluation of Sustained Release Sodium Alginate Microbeads of CarvedilolDelfina HuangNo ratings yet
- 4.1 2 PDFDocument6 pages4.1 2 PDFNela SharonNo ratings yet
- Preparation and Evaluation of Sustained Release Microbeads of Norfloxacin Using Sodium AlginateDocument5 pagesPreparation and Evaluation of Sustained Release Microbeads of Norfloxacin Using Sodium AlginateRajesh KumarNo ratings yet
- Jurnal Simultaneous Determination of Reservatives in SucralfateDocument8 pagesJurnal Simultaneous Determination of Reservatives in SucralfateLia EleaNo ratings yet
- Development of Microemulsion For Solubility Enhancement of Poorly Water Soluble Drug ValsartanDocument6 pagesDevelopment of Microemulsion For Solubility Enhancement of Poorly Water Soluble Drug Valsartandini hanifaNo ratings yet
- Pilocarpine Hydrochloride-Loaded NiosomesDocument14 pagesPilocarpine Hydrochloride-Loaded NiosomesĐủ PhạmNo ratings yet
- EJCHEM - Volume 65 - Issue 11 - Pages 155-162Document8 pagesEJCHEM - Volume 65 - Issue 11 - Pages 155-162Gustavo D.B.No ratings yet
- Development and Optimization of Floating Microspheres in AmethopterinDocument6 pagesDevelopment and Optimization of Floating Microspheres in AmethopterinDr Sharique AliNo ratings yet
- Actra 2018 034Document11 pagesActra 2018 034EnggerianiNo ratings yet
- DESIGN AND EVALUATION OF MUCOADHESIVE MICROCAPSULES OF ACECLOFENAC BY SOLVENT EMULSIFICATION METHOD Gangotri Yadav, Resma Jadhav, Vaishali Jadhav, Ashish JainDocument7 pagesDESIGN AND EVALUATION OF MUCOADHESIVE MICROCAPSULES OF ACECLOFENAC BY SOLVENT EMULSIFICATION METHOD Gangotri Yadav, Resma Jadhav, Vaishali Jadhav, Ashish JainiajpsNo ratings yet
- Development and Evaluation of Nanoemulsion of RepaglinideDocument8 pagesDevelopment and Evaluation of Nanoemulsion of Repaglinidevikrantkadam12No ratings yet
- Nano Emulsion Production by Sonication and Microfluidization A ComparisonDocument13 pagesNano Emulsion Production by Sonication and Microfluidization A ComparisonOsama MoussaNo ratings yet
- AJPS - Author TemplateDocument16 pagesAJPS - Author TemplateAdityaNo ratings yet
- AJPS - Author TemplateDocument15 pagesAJPS - Author TemplatePatmasariNo ratings yet
- Formulation and Evaluation of Egg Albumin Based Controlled Release Microspheres of MetronidazoleDocument5 pagesFormulation and Evaluation of Egg Albumin Based Controlled Release Microspheres of MetronidazoleSachin BagewadiNo ratings yet
- NANOPARTICLESDocument8 pagesNANOPARTICLESutdtud jtursNo ratings yet
- Kesharvani 2019Document9 pagesKesharvani 2019RiyanNo ratings yet
- 2 51 1588072528 6.ijmpsapr20206Document14 pages2 51 1588072528 6.ijmpsapr20206TJPRC PublicationsNo ratings yet
- A C A D e M I C S C I e N C e SDocument7 pagesA C A D e M I C S C I e N C e SMSKNo ratings yet
- Salbutamol Sulphate-Ethylcellulose Microparticles: Formulation and In-Vitro Evaluation With Emphasis On Mathematical ApproachesDocument8 pagesSalbutamol Sulphate-Ethylcellulose Microparticles: Formulation and In-Vitro Evaluation With Emphasis On Mathematical ApproachesThiiwiie'thiiwiie PrathiiwiieNo ratings yet
- Article WJPR 1399543685Document14 pagesArticle WJPR 1399543685Nafi Hasan ZahidNo ratings yet
- Chemistry Prject ReportDocument35 pagesChemistry Prject ReportAJ ONLINENo ratings yet
- Spectrophotometric Method Development and ValidatiDocument7 pagesSpectrophotometric Method Development and ValidatiEVELYN SOLANHS ACERO RODRIGUEZNo ratings yet
- Dokumen PDFDocument8 pagesDokumen PDFnadia julisaNo ratings yet
- ASSAY METHOD DEVELOPMENT AND VALIDATION FOR THE ESTIMATION OF SOLIFENACIN SUCCINATE IN TABLETS BY UV SPECTROPHOTOMETRY N.J.R. Hepsebah, A. Ashok KumarDocument6 pagesASSAY METHOD DEVELOPMENT AND VALIDATION FOR THE ESTIMATION OF SOLIFENACIN SUCCINATE IN TABLETS BY UV SPECTROPHOTOMETRY N.J.R. Hepsebah, A. Ashok KumariajpsNo ratings yet
- Composition: 1/26 EMEA 2005Document26 pagesComposition: 1/26 EMEA 2005Argun WidarsaNo ratings yet
- Formulation and Evaluation of in Situ Ophthalmic Gels of Diclofenac SodiumDocument8 pagesFormulation and Evaluation of in Situ Ophthalmic Gels of Diclofenac Sodiumsunaina agarwalNo ratings yet
- Design and Characterization of Zaltoprofen Nanosuspension by Precipitation MethodDocument8 pagesDesign and Characterization of Zaltoprofen Nanosuspension by Precipitation Methodsunaina agarwalNo ratings yet
- Formulation and Evaluation of Mucoadhesive Microcapsules of RifampicinDocument5 pagesFormulation and Evaluation of Mucoadhesive Microcapsules of RifampicinIOSR Journal of PharmacyNo ratings yet
- Formulation and Evaluation of Mefenamic Acid Ointment Using Penetration EnhancersDocument5 pagesFormulation and Evaluation of Mefenamic Acid Ointment Using Penetration EnhancersIndradewiNo ratings yet
- Component Screening of Miconazole Nitrate Nanoemulsion: Research ArticleDocument8 pagesComponent Screening of Miconazole Nitrate Nanoemulsion: Research ArticleSiddhant YadavNo ratings yet
- Claudio Müller, Gloria Godoy, Marta de Diego.: Chemical Stability of Prednisone Oral Suspension and Drug SubstanceDocument5 pagesClaudio Müller, Gloria Godoy, Marta de Diego.: Chemical Stability of Prednisone Oral Suspension and Drug SubstanceGitanti Rohmanda HolaholaNo ratings yet
- Tds 4Document4 pagesTds 4Neha YadavNo ratings yet
- Diltizem MicrosphereDocument11 pagesDiltizem MicrospheredoddadineshNo ratings yet
- Micro EmulsionDocument7 pagesMicro EmulsionIndustrial OilsNo ratings yet
- .Trashed 1662592588 NanoemulsionDocument22 pages.Trashed 1662592588 NanoemulsionRajat KadyanNo ratings yet
- Mucoadhesive MicrospheresDocument20 pagesMucoadhesive MicrospheresRam C DhakarNo ratings yet
- Ashraf M. Mahmoud, Saad A. Alqahtani: American Journal of Analytical Chemistry, 2016, 7, 179-191Document13 pagesAshraf M. Mahmoud, Saad A. Alqahtani: American Journal of Analytical Chemistry, 2016, 7, 179-191DrGajanan VaishnavNo ratings yet
- Design and Evaluation of Sustained Release Microcapsules Containing Diclofenac SodiumDocument4 pagesDesign and Evaluation of Sustained Release Microcapsules Containing Diclofenac SodiumLia Amalia UlfahNo ratings yet
- Formulation and Evaluation of Multiple Emulation of Diclofenac SodiumDocument7 pagesFormulation and Evaluation of Multiple Emulation of Diclofenac SodiumIJRASETPublicationsNo ratings yet
- Nanoparticulas EmulsionesDocument6 pagesNanoparticulas EmulsionesDavid Leonardo CañasNo ratings yet
- Jurnal Uv Vis 8Document3 pagesJurnal Uv Vis 8UnsaniaNo ratings yet
- Optimization of Finasteride Nano-Emulsion Preparation Using Chemometric ApproachDocument5 pagesOptimization of Finasteride Nano-Emulsion Preparation Using Chemometric ApproachNurul Hikmah12No ratings yet
- New Polymers for Encapsulation of Nutraceutical CompoundsFrom EverandNew Polymers for Encapsulation of Nutraceutical CompoundsJorge Carlos Ruiz RuizNo ratings yet
- A Comprehensive Book on Experimental PharmaceuticsFrom EverandA Comprehensive Book on Experimental PharmaceuticsRating: 5 out of 5 stars5/5 (1)
- 10 Intraoperative RadiotherapyDocument11 pages10 Intraoperative RadiotherapyDgek LondonNo ratings yet
- 5-Scanned Ion Beam TherapyDocument17 pages5-Scanned Ion Beam TherapyDgek LondonNo ratings yet
- 7-The Stopping Power ofDocument21 pages7-The Stopping Power ofDgek LondonNo ratings yet
- Quickly Dissolving Amylose Indicator in Cadmium Iodide-Linear Starch Colorimetric ReagentDocument3 pagesQuickly Dissolving Amylose Indicator in Cadmium Iodide-Linear Starch Colorimetric ReagentDgek LondonNo ratings yet
- λ-modulation absorption spectraDocument7 pagesλ-modulation absorption spectraDgek LondonNo ratings yet
- Midterm Examination: N N N NDocument2 pagesMidterm Examination: N N N NDgek LondonNo ratings yet
- An Overview of Recycling of Electronic WasteDocument4 pagesAn Overview of Recycling of Electronic WasteDgek LondonNo ratings yet
- Name - Homework Assignment #5 Angular Kinetics Due 3/13/2014 1) If F (1.67, - 8.5, 4.7) N and R (0.49, 0.12, 0.6) M. Find R X FDocument2 pagesName - Homework Assignment #5 Angular Kinetics Due 3/13/2014 1) If F (1.67, - 8.5, 4.7) N and R (0.49, 0.12, 0.6) M. Find R X FDgek LondonNo ratings yet
- Recovery and Refining of Precious Metals Alloys by Oxi-Nitrogen LeachingDocument9 pagesRecovery and Refining of Precious Metals Alloys by Oxi-Nitrogen LeachingDgek LondonNo ratings yet
- E WasteDocument6 pagesE WasteDgek LondonNo ratings yet
- Leaching of Gold and Silver From Crushed Au-Ag Wastes: Jana Ficeriová, Peter Balá, Erika Dutková and Eberhard GockDocument4 pagesLeaching of Gold and Silver From Crushed Au-Ag Wastes: Jana Ficeriová, Peter Balá, Erika Dutková and Eberhard GockDgek LondonNo ratings yet
- e Waste GoldDocument115 pagese Waste GoldDgek LondonNo ratings yet
- 10 5923 J Ijmee 20120102 02EWASTEDocument5 pages10 5923 J Ijmee 20120102 02EWASTEDgek LondonNo ratings yet
- Lucas vs. TuañoDocument17 pagesLucas vs. TuañoJenny ButacanNo ratings yet
- OBAT2Document12 pagesOBAT2AuliaHadiningratNo ratings yet
- Chewable Lozenges Larry L. Augsburger, Stephen W.Document6 pagesChewable Lozenges Larry L. Augsburger, Stephen W.Faris M ZidiqNo ratings yet
- Oral MoniliasisDocument16 pagesOral MoniliasisMel Izhra N. MargateNo ratings yet
- PiroxicamDocument2 pagesPiroxicamVirginia Aira Lara MarquezNo ratings yet
- Types of Racks For Pharmacy Store by Instor IndiaDocument11 pagesTypes of Racks For Pharmacy Store by Instor IndiaRoshni SharmaNo ratings yet
- Common Medical AbbreviationsDocument4 pagesCommon Medical AbbreviationsJustine DicksonNo ratings yet
- Harga ObatDocument44 pagesHarga ObatFreddy ApotekerNo ratings yet
- ParvezDocument43 pagesParvezShobhit GoswamiNo ratings yet
- Community Pharmacy InternshipDocument8 pagesCommunity Pharmacy InternshipKenny TuanNo ratings yet
- Perioperative Nursing (PreOp)Document51 pagesPerioperative Nursing (PreOp)jessamariesabio100% (1)
- Daftar PustakaDocument4 pagesDaftar PustakaNuryanti RokhmanNo ratings yet
- Nmims India Pharma MarketDocument36 pagesNmims India Pharma MarketAjay SainiNo ratings yet
- Parenteral Administration of DrugsDocument3 pagesParenteral Administration of DrugspauchanmnlNo ratings yet
- Babe 2Document17 pagesBabe 2Sathish SizzyNo ratings yet
- AcetylcysteineDocument2 pagesAcetylcysteineMeriLyn Parayno83% (6)
- Classification of Dangerous DrugsDocument3 pagesClassification of Dangerous Drugsjinmenchie0% (1)
- Zentel Tablets: What Is in This LeafletDocument3 pagesZentel Tablets: What Is in This LeafletLadyKahluaNo ratings yet
- KRATOM 101 - BEGINNER - S GUIDE VENDORS (2) WORD FINALShannon (2) 10 - 14 - 2015 PDFDocument3 pagesKRATOM 101 - BEGINNER - S GUIDE VENDORS (2) WORD FINALShannon (2) 10 - 14 - 2015 PDFDiego CastroNo ratings yet
- Medical Administration RecordDocument1 pageMedical Administration RecorddemereNo ratings yet
- DRUG STUDY: Rocephin - Ceftriaxone SodiumDocument1 pageDRUG STUDY: Rocephin - Ceftriaxone SodiumYum C100% (1)
- Contact Dermatitis 2015parameterDocument39 pagesContact Dermatitis 2015parameterSaniya Ilma ArifaNo ratings yet
- CC3 Finals Toxicology of The Drugs of Abuse-1Document4 pagesCC3 Finals Toxicology of The Drugs of Abuse-1Gabriel QuillNo ratings yet
- Bam Slam Drug CardDocument4 pagesBam Slam Drug CardLeticia GonzalezNo ratings yet
- Mercy Health-Eastgate Medical Center Dedicated: Ensure The Safety of Your Home While You're AwayDocument6 pagesMercy Health-Eastgate Medical Center Dedicated: Ensure The Safety of Your Home While You're AwayDonNo ratings yet
- Jurnal AnestesiDocument8 pagesJurnal AnestesiFaidh HusnanNo ratings yet
- FArmasi RS Dan Klinik KomprehensifDocument8 pagesFArmasi RS Dan Klinik Komprehensifklinik dktNo ratings yet
- Who Uhc Sds 2019.10 EngDocument50 pagesWho Uhc Sds 2019.10 EngChristian ObandoNo ratings yet
- Trima PharmaceuticalsDocument1 pageTrima PharmaceuticalsIsrael ExporterNo ratings yet