Professional Documents
Culture Documents
Novel p53 Splicing Site Mutation in Li-Fraumeni-like Syndrome With Osteosarcoma
Novel p53 Splicing Site Mutation in Li-Fraumeni-like Syndrome With Osteosarcoma
Uploaded by
Missy MishaCopyright:
Available Formats
You might also like
- The Every Other Day DietDocument33 pagesThe Every Other Day DietDrGyenes Zsuzsanna0% (2)
- A Novel Somatic K-Ras Mutation in Juvenile Myelomonocytic LeukemiaDocument2 pagesA Novel Somatic K-Ras Mutation in Juvenile Myelomonocytic LeukemiamahanteshNo ratings yet
- Oncogenic Osteomalacia - A Complex Dance of Factors: Thomas O. Carpenter, M.DDocument4 pagesOncogenic Osteomalacia - A Complex Dance of Factors: Thomas O. Carpenter, M.DAsticha Erlianing SariNo ratings yet
- Late Onset Thrombosis in A Case of Severe Protein S Deficiency Due To Compound Heterozygosity For PROS1 MutationsDocument3 pagesLate Onset Thrombosis in A Case of Severe Protein S Deficiency Due To Compound Heterozygosity For PROS1 Mutationsgabriela ciolpanNo ratings yet
- A Novel Fibrillin-1 Gene Missense Mutation Associated With Neonatal Marfan Syndrome - A Case Report and Review of The Mutation SpectrumDocument6 pagesA Novel Fibrillin-1 Gene Missense Mutation Associated With Neonatal Marfan Syndrome - A Case Report and Review of The Mutation SpectrumeduardoperezagonzalezNo ratings yet
- La Mellarin D2Document2 pagesLa Mellarin D2JESUS DAVID BOLA‹O JIMENEZNo ratings yet
- Storti Foundation: Clinical Relevance ofDocument4 pagesStorti Foundation: Clinical Relevance ofNimra AwaisNo ratings yet
- SF3B1 and Other Novel Cancer Genes: in Chronic Lymphocytic LeukemiaDocument10 pagesSF3B1 and Other Novel Cancer Genes: in Chronic Lymphocytic LeukemiaRafael ColinaNo ratings yet
- (Sici) 1520 6823 (1997) 5:3 93::aid Roi1 3.0.co 2 DDocument4 pages(Sici) 1520 6823 (1997) 5:3 93::aid Roi1 3.0.co 2 DRashmeeta ThadhaniNo ratings yet
- Karen A. Gelmon: Desmoplastic Small Round-Cell Tumor of The PancreasDocument3 pagesKaren A. Gelmon: Desmoplastic Small Round-Cell Tumor of The PancreasAdam HartonoNo ratings yet
- Microscopy Res Technique - 2001 - Southwood - Molecular Pathways of Oligodendrocyte Apoptosis Revealed by Mutations inDocument9 pagesMicroscopy Res Technique - 2001 - Southwood - Molecular Pathways of Oligodendrocyte Apoptosis Revealed by Mutations inAnglia LopesNo ratings yet
- Targetable Kinase-Activating Lesions in Ph-Like Acute Lymphoblastic LeukemiaDocument11 pagesTargetable Kinase-Activating Lesions in Ph-Like Acute Lymphoblastic LeukemiaseverinNo ratings yet
- 2016 Article 70Document8 pages2016 Article 70sawantleena62No ratings yet
- Angelman Syndrome Phenotype Associated With Mutations in Mecp2, A Gene Encoding A Methyl CPG Binding ProteinDocument6 pagesAngelman Syndrome Phenotype Associated With Mutations in Mecp2, A Gene Encoding A Methyl CPG Binding ProteinAkmal NugrahaNo ratings yet
- Jurnal OM TransleteDocument7 pagesJurnal OM TransleterisjunNo ratings yet
- Gene Expression Differences Between Thyroid Carcinoma, Thyroid Adenoma and Normal Thyroid TissueDocument11 pagesGene Expression Differences Between Thyroid Carcinoma, Thyroid Adenoma and Normal Thyroid TissueArtha MahulaeNo ratings yet
- Pancytopenia As Initial Presentation of Acute Lymphoblastic Leukemia and Its Associationwith Bone MarrowresponseDocument6 pagesPancytopenia As Initial Presentation of Acute Lymphoblastic Leukemia and Its Associationwith Bone MarrowresponseIJAR JOURNALNo ratings yet
- Anemia Aplastic JournalDocument13 pagesAnemia Aplastic JournalGenoveva Maditias Dwi PertiwiNo ratings yet
- Campbell 1992Document3 pagesCampbell 1992Pilar AufrastoNo ratings yet
- 439 2007 Article 362Document6 pages439 2007 Article 362Zinik EşanuNo ratings yet
- 1 s2.0 S0016508515013104 MainDocument16 pages1 s2.0 S0016508515013104 MainMaria PalNo ratings yet
- Genomic Mutations of Primary and Metastatic LungDocument9 pagesGenomic Mutations of Primary and Metastatic LungDiana AyuNo ratings yet
- Abnormalities of RUNX1, CBFB, CEBPA, and NPM1 Genes in Acute Myeloid LeukemiaDocument10 pagesAbnormalities of RUNX1, CBFB, CEBPA, and NPM1 Genes in Acute Myeloid LeukemiaAndikhaNo ratings yet
- European Journal of Medical GeneticsDocument7 pagesEuropean Journal of Medical GeneticsAdam NowakNo ratings yet
- 1500 Pac MNewDocument6 pages1500 Pac MNewBioq. GallegosNo ratings yet
- Management of Iron Overload With A Disposable Multi-Day Delivery SystemDocument1 pageManagement of Iron Overload With A Disposable Multi-Day Delivery SystemEloy Guillermo Mijares EchezuríaNo ratings yet
- Primary Midgut VolvulusDocument2 pagesPrimary Midgut VolvulusNihal S KiranNo ratings yet
- Letter: Mutations in UBQLN2 Cause Dominant X-Linked Juvenile and Adult-Onset ALS and ALS/dementiaDocument7 pagesLetter: Mutations in UBQLN2 Cause Dominant X-Linked Juvenile and Adult-Onset ALS and ALS/dementiaGarzo ZardofskyNo ratings yet
- Multiple Lipomas Linked To An RB1 Gene Mutation in A Large Pedigree With Low Penetrance RetinoblastomaDocument5 pagesMultiple Lipomas Linked To An RB1 Gene Mutation in A Large Pedigree With Low Penetrance RetinoblastomaMaria Burke-ChaussonNo ratings yet
- On The Horizon From The ORS: WNT, Osteosarcoma, and Future TherapyDocument2 pagesOn The Horizon From The ORS: WNT, Osteosarcoma, and Future TherapyEbetWasuwayNo ratings yet
- Slater Case Presentation Issue 1 Article For WebsiteDocument2 pagesSlater Case Presentation Issue 1 Article For Websiteapi-400507461No ratings yet
- Ovarian Granulocytic Sarcoma in A Patient With Philadelphia Chromosome-Positive Acute Biphenotypic Leukemia - Case ReportDocument5 pagesOvarian Granulocytic Sarcoma in A Patient With Philadelphia Chromosome-Positive Acute Biphenotypic Leukemia - Case ReportOoAldoONo ratings yet
- Myeloid NeoplasiaDocument10 pagesMyeloid NeoplasiaivssonNo ratings yet
- AMM V 27.07Document138 pagesAMM V 27.07Anonymous 5cHdazK6b100% (1)
- Jack 2Document5 pagesJack 2Josue BarralNo ratings yet
- AMM V 27.07Document138 pagesAMM V 27.07paul_calburean7899No ratings yet
- Steroid Resistant NephroticS YndromeDocument42 pagesSteroid Resistant NephroticS YndromeSholihatul AmaliyaNo ratings yet
- 66 68 PBDocument89 pages66 68 PBAyesha FatimaNo ratings yet
- Jurnal InternaDocument3 pagesJurnal InternaIndahNo ratings yet
- Pancreatic CancerDocument13 pagesPancreatic CancerFA MonterNo ratings yet
- Acute Pyelonephritis in Adults: A Case Series of 223 PatientsDocument6 pagesAcute Pyelonephritis in Adults: A Case Series of 223 PatientsshiaNo ratings yet
- Paper Comparativa Sobrevida de PV, TE y MFPDocument7 pagesPaper Comparativa Sobrevida de PV, TE y MFPDani HaindlNo ratings yet
- McKinnis Bone Marrow Transplantation Hunter Syndrome The Journal of PediatricsDocument17 pagesMcKinnis Bone Marrow Transplantation Hunter Syndrome The Journal of PediatricsBoNo ratings yet
- How I Treat Polycythemia VeraDocument11 pagesHow I Treat Polycythemia Veraayu_cicuuNo ratings yet
- PIIS0085253815551752Document6 pagesPIIS0085253815551752Ignacio TabuadaNo ratings yet
- Adult Acute Lymphoblastic Leukemia: Concepts and StrategiesDocument12 pagesAdult Acute Lymphoblastic Leukemia: Concepts and StrategiesdrravesNo ratings yet
- Adult Minimal-Change Disease: Clinical Characteristics, Treatment, and OutcomesDocument9 pagesAdult Minimal-Change Disease: Clinical Characteristics, Treatment, and OutcomesMutiara RizkyNo ratings yet
- Psu 50318Document4 pagesPsu 50318Dr Venkatachalapathy T S Ped SurgeonNo ratings yet
- Cancers 14 01120 v4Document21 pagesCancers 14 01120 v4ABCNo ratings yet
- Mar FanDocument5 pagesMar FanLav DehcNo ratings yet
- Neuroendocrine Tumors: Surgical Evaluation and ManagementFrom EverandNeuroendocrine Tumors: Surgical Evaluation and ManagementJordan M. CloydNo ratings yet
- HDF Pre y Post Dilución 8 AnexoDocument7 pagesHDF Pre y Post Dilución 8 AnexoPamelaNo ratings yet
- Artigo B1Document6 pagesArtigo B1José Eduardo AdelinoNo ratings yet
- Cell Cycle and Cancer - Unit I IV/IDocument6 pagesCell Cycle and Cancer - Unit I IV/IManoj GourojuNo ratings yet
- Cystic Fibrosis Article - RCCADocument9 pagesCystic Fibrosis Article - RCCAAndleeb ImranNo ratings yet
- Bremer 1995Document5 pagesBremer 1995samuel ZhangNo ratings yet
- Fisiopatologia de La FiebreDocument3 pagesFisiopatologia de La FiebreLINA MARIA AVILA PEÑANo ratings yet
- Blastic Plasmacytoid Dendritic Cell NeoplasmeCurrent InsightsDocument10 pagesBlastic Plasmacytoid Dendritic Cell NeoplasmeCurrent InsightsPaúl Otañez MolinaNo ratings yet
- Papillary Microcarcinoma of The Thyroid-Prognostic Significance of Lymph Node Metastasis and MultifocalityDocument10 pagesPapillary Microcarcinoma of The Thyroid-Prognostic Significance of Lymph Node Metastasis and MultifocalityAZ RPNo ratings yet
- Literature Review On Sickle Cell DiseaseDocument8 pagesLiterature Review On Sickle Cell Diseaseafmzwflmdnxfeb100% (1)
- Connective Support, Binding, Locomotion Co-Ordination AbsorptionDocument3 pagesConnective Support, Binding, Locomotion Co-Ordination AbsorptionSatvik MohantyNo ratings yet
- Cushing's SyndromeDocument24 pagesCushing's SyndromeUdtjeVanDerJeyk100% (1)
- Pedigree SymbolsDocument30 pagesPedigree SymbolsJoshi SabinaNo ratings yet
- Jurnal Oogenesis Int'l 1Document8 pagesJurnal Oogenesis Int'l 1Iqval AnggiNo ratings yet
- Bacterial Kidney Disease (Renibacterium Salmoninarum) : G.D. Wiens and S.L. KaattariDocument34 pagesBacterial Kidney Disease (Renibacterium Salmoninarum) : G.D. Wiens and S.L. KaattariLiana QuinnNo ratings yet
- Planaria Lab ReportDocument3 pagesPlanaria Lab Reportapi-194648534No ratings yet
- PDF Essentials of Modern Neuroscience Lange 1St Edition Erik Roberson Ebook Full ChapterDocument53 pagesPDF Essentials of Modern Neuroscience Lange 1St Edition Erik Roberson Ebook Full Chapterdaniel.keller545100% (3)
- Nexus Magazine - August 2018 PDFDocument100 pagesNexus Magazine - August 2018 PDFmarsalg100% (3)
- Filtracion GlomerularDocument18 pagesFiltracion GlomerularNicole Jheny Raraz SosaNo ratings yet
- Anatomy and Physiology SDL 1Document3 pagesAnatomy and Physiology SDL 1Faatoots FatsNo ratings yet
- ANGIOEDEMADocument11 pagesANGIOEDEMAromimedNo ratings yet
- Scopus - All Journal Titles - Scopus - Academic Database Assessment Tool PDFDocument270 pagesScopus - All Journal Titles - Scopus - Academic Database Assessment Tool PDFSiva Kumar ReddyNo ratings yet
- Haem. Notes (MBCHB) ProperDocument162 pagesHaem. Notes (MBCHB) ProperKelvinTMaikanaNo ratings yet
- Ganoderma Lucidum Against Candida AlbicansDocument8 pagesGanoderma Lucidum Against Candida AlbicansCsikós IlonaNo ratings yet
- Final Paper 110218Document156 pagesFinal Paper 110218Bien Carlos Esteves ViaNo ratings yet
- Faculty 363 Histotechnique Lectures - 2Document27 pagesFaculty 363 Histotechnique Lectures - 2einsteinspy100% (1)
- MARK SCHEME For The June 2005 Question PaperDocument10 pagesMARK SCHEME For The June 2005 Question PaperequatorloungeNo ratings yet
- Science 9 Lesson 2 Non Mendelian Patterns of InheritanceDocument30 pagesScience 9 Lesson 2 Non Mendelian Patterns of InheritanceIts RxsgNo ratings yet
- Biology TRIPLE SCIENCE 1 2023 PREDICTEDDocument15 pagesBiology TRIPLE SCIENCE 1 2023 PREDICTEDjayakantharushanNo ratings yet
- The Neonate: Eugenia K. Pallotto, MDDocument17 pagesThe Neonate: Eugenia K. Pallotto, MDSamNo ratings yet
- History of HLA PDFDocument17 pagesHistory of HLA PDFeseNo ratings yet
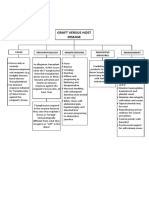
- Graft Versus Host DiseaseDocument1 pageGraft Versus Host DiseaseIzhra MargateNo ratings yet
- تجميع اسئله الاخصائين 1Document36 pagesتجميع اسئله الاخصائين 1Osama BakheetNo ratings yet
- Bio TherapyDocument18 pagesBio TherapyChino RamirezNo ratings yet
- Prenatal Diagnosis On The Use of Non Invasive Prenatal Testing For The Detection of Fetal Chromosomal Conditions in Singleton Pregnanciesprenatal Diagnosis - 2023 - HuiDocument15 pagesPrenatal Diagnosis On The Use of Non Invasive Prenatal Testing For The Detection of Fetal Chromosomal Conditions in Singleton Pregnanciesprenatal Diagnosis - 2023 - HuiYến ĐàoNo ratings yet
- Biomedik 2Document22 pagesBiomedik 2Fergi ListiawanNo ratings yet
- Case Report Polyhydramions: Created By: Febiena ID. 61111005Document3 pagesCase Report Polyhydramions: Created By: Febiena ID. 61111005febienaNo ratings yet
- PIC-Seq Dissecting Cellular Crosstalk by Sequencing Physically Interacting CellsDocument16 pagesPIC-Seq Dissecting Cellular Crosstalk by Sequencing Physically Interacting CellsNiv SabathNo ratings yet
- 1 s2.0 S0022391313603583 MainDocument50 pages1 s2.0 S0022391313603583 MainDANTE DELEGUERYNo ratings yet
Novel p53 Splicing Site Mutation in Li-Fraumeni-like Syndrome With Osteosarcoma
Novel p53 Splicing Site Mutation in Li-Fraumeni-like Syndrome With Osteosarcoma
Uploaded by
Missy MishaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Novel p53 Splicing Site Mutation in Li-Fraumeni-like Syndrome With Osteosarcoma
Novel p53 Splicing Site Mutation in Li-Fraumeni-like Syndrome With Osteosarcoma
Uploaded by
Missy MishaCopyright:
Available Formats
bs_bs_banner
R254Q AQP-2 gene mutation in NDI
could concentrate urine above 500 mOsm/Kg water. Thus, it may be possible that the further identication of new patients with genetic disease conrmation will provide a wider clinical picture of NDI. In this context, gene mutation analysis should be considered even in patients with mild NDI symptoms. Fortunately, both AVPR2 and AQP2 genes are small and can be easily analyzed. As patients with autosomal dominant mutations of the AQP2 gene are likely to demonstrate more mild clinical manifestations than recessive form, the NDI seen in this case is likely to be the autosomal dominant form rather than the recessive form. All mutations in dominant NDI are found in the coding region of the C-terminal tail of AQP2, which plays an important role in AQP2 trafcking to the apical plasma membrane. Thus, AQP2 mutants in dominant NDI are sorted to other subcellular locations in the cells than wt-AQP2.
107
References
1 Fujiwara TM, Bichet DG. Molecular biology of hereditary diabetes insipidus. J. Am. Soc. Nephrol. 2005; 16: 283646. 2 Kuwahara M, Iwai K, Ooeda T et al. Three families with autosomal dominant nephrogenic diabetes insipidus caused by aquaporin-2
8
ped_3641 107..134
mutations in the C-terminus. Am. J. Hum. Genet. 2001; 69: 738 48. Hochberg Z, Lieburg AV, Even L et al. Autosomal recessive nephrogenic diabetes insipidus caused by an aquaporin-2 mutation. J. Clin. Endocrinol. Metab. 1997; 82: 6869. Miyakoshi M, Kamoi K, Uchida S, Sasaki S. A case of a novel mutant vasopressin receptor-dependent nephrogenic diabetes insipidus with bilateral non-obstructive hydronephrosis in a middle aged man: differentiation from aquaporin-dependent nephrogenic diabetes insipidus by response of factor VII and von Willebrand factor to 1-diamino-8-arginine vasopressin administration. Endocr. J. 2003; 50: 80914. Moon SS, Kim HJ, Choi YK et al. Novel mutation of aquaporin-2 gene in a patient with congenital nephrogenic diabetes insipidus. Endocr. J. 2009; 56: 90510. Mattia FD, Savelkoul PJM, Kamsteeg EJ et al. Lack of arginine vasopressin-induced phosphorylation of aquaporin-2 mutant explains dominant nephrogenic diabetes insipidus. J. Am. Soc. Nephrol. 2005; 16: 287280. Savelkoul PJM, Mattia FD, Li Y et al. p.R254Q mutation in the aquaporin-2 water channel causing dominant nephrogenic diabetes insipidus is due to a lack of arginine vasopressin-induced phosphorylation. Hum. Mutat. 2009; 30: E891E903. Sasaki S. Nephrogenic diabetes insipidus: update of genetic and clinical aspects. Nephrol. Dial. Transplant. 2004; 19: 13513.
Novel p53 splicing site mutation in Li-Fraumeni-like syndrome with osteosarcoma
Naoto Sakurai,1 Shotaro Iwamoto,1 Yoshihiro Miura,2 Tomoki Nakamura,2 Akihiko Matsumine,2 Junji Nishioka,3 Kaname Nakatani3 and Yoshihiro Komada1 Departments of 1Pediatrics and Developmental Science and 2Orthopaedic Surgery, Mie University Graduate School of Medicine and 3Division of Personalized Medicine, Mie University Hospital, Tsu, Mie, Japan
Abstract We describe a 15-year-old girl with a novel germline p53 splice site mutation who developed an osteosarcoma. She received several cycles of chemotherapy with complete resection of the primary tumor without amputation, and has maintained remission for 18 months. Li-Fraumeni-like syndrome was suspected based on familial history. Sequence analysis revealed the presence of a novel germline p53 gene mutation resulting in a G to A transition at position +1 at the donor splice site of intron 6, creating a 6 amino acid insertion. This case provides interesting insight into the phenotype-genotype correlation in LFL syndrome with a TP53 splicing mutation.
Key words Li-Fraumeni syndrome, Li-Fraumeni-like syndrome, osteosarcoma, p53, splicing site mutation.
Li-Fraumeni syndrome (LFS) is a rare genetic disease with autosomal-dominant inheritance. LFS patients and their family members have a higher risk of developing multiple neoplasms during their lifetime, especially breast cancer, leukemia, sarcoma,
Correspondence: Shotaro Iwamoto, MD PhD, Department of Pediatrics and Developmental Science, Mie University Graduate School of Medicine, 2-174 Edobashi, Tsu, Mie 514-8507, Japan. Email: siwamoto@clin.medic.mie-u.ac.jp Received 1 March 2011; revised 17 February 2012; accepted 16 March 2012. doi: 10.1111/j.1442-200X.2012.03641.x
and other neoplasms, in children and young adults. LFS is classied into two disease types: classic LFS and Li-Fraumeni-like (LFL) syndrome. Classic LFS is dened as a diagnosis of sarcoma before 45 years of age, a rst-degree relative with cancer before 45 years of age, and another rst- or second-degree relative with any cancer diagnosed by 45 years of age or with a sarcoma at any age.1,2 Li-Fraumeni-like syndrome is characterized by the diagnosis of any childhood cancer or sarcoma, brain tumor, or adrenocortical carcinoma before 45 years of age, a rst- or second-degree relative with a typical LFS-related cancer diagnosed at any age,
2013 The Authors Pediatrics International 2013 Japan Pediatric Society
bs_bs_banner
108
N Sakurai et al.
tenderness of the left knee. Laboratory blood tests indicated no abnormalities. Radiography of the knee showed ne geographic osteosclerosis and a periosteal reaction in the medulla of the proximal metaphysis of the left tibia. A bone tumor was suspected, and magnetic resonance imaging (MRI) was performed. MRI showed a 31 mm 87 mm lesion with low signal intensity on T1-weighted and T2-weighted images at the medulla of the proximal metaphysic of the left tibia with marked gadolinium enhancement (Fig. 2). Whole-body computed tomography (CT) showed no metastatic lesions, except for a 96 mm 72 mm cystic lesion in the pelvis. MRI suggested this cystic lesion might be a teratoma of the right ovary. Because a malignant bone tumor was highly suspected based on the imaging, open biopsy of the left knee was performed. A pathological diagnosis of conventional osteosarcoma was conrmed. Treatment was performed based on the Mie Osteosarcoma Study Protocol. After two cycles of neoadjuvant chemotherapy using adriamycin, and cisplatin, curative resection of the tumor was performed. The left knee joint was replaced by a prosthesis. Histopathology of the resected specimen showed 5060% necrosis, and thus the response to the neoadjuvant therapy was classied as grade II based on the Rosen and Huvos grading system. After limb-salvage surgery, the patient was given two cycles of adjuvant chemotherapy consisting of adriamycin, cisplatin, methotrexate and ifosfamide. Right ovarian torsion occurred due to the ovarian tumor on the third day of the rst course of neoadjuvant chemotherapy. Emergency right oophorectomy was performed. Pathology showed that the ovarian tumor was a dermoid cyst with areas of necrosis. As at the time of writing, the patient has been alive and free of disease for 18 months since completion of the therapy.
Molecular genetic analysis
d.76 years Liver cancer
d.46 years Breast cancer (Onset 42y)
d.70 years Lung cancer
d.57 years Uterus cancer (Onset 55y)
50 years
52 years
22 years
15 years Osteosarcoma
Fig. 1 Family chart of the () present patient. () male; () female.
and a rst- or second-degree relative in the same genetic lineage with any cancer diagnosed before the age of 60 years.3,4 A germline mutation in the p53 tumor-suppressor gene is present in 5670% of families with classical LFS and 1620% of families with LFL. Most mutations identied in LFS have been located between exons 5 and 8 of the gene. The majority of p53 mutations are missense substitutions (73.6%). Other alterations include frameshift insertions and deletions (8.65%), nonsense mutations (7.67%), silent mutations (4.37%), splice site mutations (1.84%) and other infrequent alterations (IARC TP53 Database, http:// www-p53.iarc.fr/). Splice site mutations are considered to be rare in the p53 gene, and only a few studies have described genetic changes that resulted in splicedonor or spliceacceptor regions and nonsense mutations (IARC TP53 Database).5
Case report
A 15-year-old girl presented with a 1 month history of left knee pain and swelling. Her family had a history of cancer, notably her paternal grandmother developed breast cancer at 42 years of age (Fig. 1). Physical examination showed swelling and point Li-Fraumeni-like syndrome was suspected in the present case because the familial history and type of tumor satised both the Eeles and the Birch et al. LFL criteria.3,4 This study was approved
Fig. 2 (a) T1-weighted and (b) T2-weighted magnetic resonance imaging of the medulla of the proximal metaphysis of the left tibia.
2013 The Authors Pediatrics International 2013 Japan Pediatric Society
bs_bs_banner
Novel p53 splicing site mutation in LFL
by Mie Universitys ethics committee. We performed genetic analysis after obtaining informed consent, and the patient was offered genetic counseling. Genomic DNA was puried from peripheral blood lymphocytes, oral mucosa and tumor tissue. Exons 59 of the p53 gene were analyzed on polymerase chain reaction (PCR), followed by direct sequencing with an automated DNA sequencer. The direct sequencing showed a G to A heterozygous transition at position +1 in the donor splice site of intron 6 of the p53 gene (c.672 + 1G>A; Fig. 3a). Subsequent reverse transcriptionPCR (RTPCR) of the region encompassing exons 57 of the p53 cDNA sequence showed that this nucleotide substitution created an 18-nucleotide (6 amino acids) in-frame insertion between exons 6 and 7 (Fig. 3b). Next, we investigated the expression frequency of this mutant cDNA by direct sequencing of plasmids isolated from individual colonies after transformation of TA-cloned PCR products. Interestingly, only one mutant cDNA was detected from 10 independent colonies. Then real-time quantitative RT-PCR was performed, which showed that mutant p53 mRNA expression was 10-fold lower than wild-type mRNA expression (Fig. 3c). These results suggest that expression of mutant p53 is lower than wild-type p53 expression. Sequencing of the promoter region of the p53 gene did not identify any nucleotide
109
substitutions (data not shown). Analysis of the resected tumor tissue showed loss of heterozygosity (LOH) of the wild-type p53 allele (Fig. 3d). Although we wished to investigate the germline p53 status of the patients family members, we were unable to obtain consent.
Discussion
We report here the results of molecular analysis of a 15-year-old girl who had osteosarcoma of the left tibia. Her family had a history of cancer. The clinical phenotype of the patient was suggestive of LFL syndrome. Sequence analysis of the patients p53 gene identied a unique splicing mutation that created a 6-amino-acid insertion between exons 6 and 7. Interestingly, expression of the mutant p53 was less than that of the wild-type p53. Although there is no clear explanation for that, we would like to offer three hypotheses that might explain our observations. One possibility was the presence of an as yet unidentied single nucleotide polymorphism (SNP) in the promoter or enhancer region of the mutant p53 gene allele that affects gene expression. But no nucleotide substitution was detected in the 1 kb region upstream of exon 1, including the promoter region. Another possibility was that the affected sequence contains the binding site for a transcription factor, but analysis of the exonintron boundaries using TFSEARCH (http://www.cbrc.jp/research/
Fig. 3 Sequencing analysis of the p53 gene in the present patient. (a) Sequence electropherogram of polymerase chain reaction (PCR) products amplied using peripheral blood lymphocyte-derived genomic DNA. Red arrow, splice donor site; blue arrow, novel cryptic acceptor site. (b) Sequence electropherogram of cDNA. (c) Mutant specic real- time quantitative PCR. Left: real copy numbers of mutant (mt) and wild-type (WT) p53 mRNA; right: relative ratio of expression. Expression of wild-type p53 mRNA is standardized as 10. The mutation-specic primer is TAT GAG CCG CCT GAG atc t (c.658672_NM_000546.4) with a 4-nucleotide intronic sequence (g.7578177-7578173) (lower case letters), and the wild-type specic primer is TGC CCT ATG AGC CGC CTG AGG (c.653673). These primers were combined with the wild-type antisense primer CCA GTG TGA TGA TGG TGA GG (c.753772) for PCR amplication. The primer designations are provided in the supplemental data (Figure S1). (d) Sequence electropherogram of PCR products amplied using tumor tissue from the patient. 2013 The Authors Pediatrics International 2013 Japan Pediatric Society
bs_bs_banner
110
N Sakurai et al.
Table 1 Donor splicing score of target boundary Sequence CTGAGGTCTGGTTTG CTGAGATCTGGTTTG CTGGGGTCTCTGGGA Donor score 3.30114183111706 -0.698858168882942 -1.42800608982695
Normal exon 5intron 6 boundary Mutant exon 5intron 6 boundary Cryptic donor site
Underline, exon 5; non-underline, intron 6; bold, splice donor site. Alternative splicing database workbench donor score analysis http:// www.ebi.ac.uk/asd/index.html.
db/TFSEARCH.html) identied the AML1 (RUNX1) binding site as the potential wild-type sequence, but the c.672 + 1G>A mutation attenuated this consensus sequence. The preferred explanation is that the splicing strength upon creation of a novel cryptic site at +19 of intron 6 is not strong enough (donor splicing score: -1.428) compared to the G to A transition of +1 at the donor splice site of intron 6 (donor splicing score: -0.69; Table 1). p53 splicing mutations are relatively rare, representing <2% of cases based on database entries.6 The reported frequency of germline splicing mutations shows some variation. While some believe they occur in <3% of germline mutations, Varley et al. estimated a frequency of 18%.7 To our knowledge, this particular splice donor site mutation (c.672 + 1G>A) has been reported in only one case of LFL syndrome.8 Most splice site mutations cause exon skipping or deletion. Loss of p53 function occurs because the mutation results in either a large conformational change in the p53 protein or a null phenotype due to nonsense-mediated RNA decay induced by premature codon termination. Deletion involving the entire p53 gene appears to confer phenotypes consistent with classic LFS rather than LFL syndrome. It was interesting that tumor tissue showed LOH. It is known that most tumors in LFS patients retain wild-type p53. This may be explained by the dominant-negative effect of mutant p53. We speculate that in the present case selection pressure to remove the wild-type allele is required for tumor development, because the dominant-negative effect of the mutant p53 is weaker, or because expression of the mutant p53 allele is lower. Patients with LFS who have germline p53 mutations are at risk for multiple cancers, including osteosarcoma. Interestingly, germline p53 mutations were identied in seven of 235 children (3.0%) with osteosarcoma.9 Four of these mutations were found in patients who did not have rst-degree relatives with cancer. That study proves the signicance of screening for germline changes in the p53 gene of pediatric osteosarcoma cases because the result could be of predictive value for a second malignancy during the long-term clinical course. Screening could also provide some information on possible cancer predisposition for other family members.9 LFS family members have a 50% likelihood of developing cancer by 30 years of age. Most of the tumors associated with the syndrome do not have a high cure rate, with the exception of early breast cancer, rare germ cell tumors of the testis, and childhood acute lymphocytic leukemia. The prognosis of patients with the syndrome who have solid tumors, however, is generally improved by earlier-stage
2013 The Authors Pediatrics International 2013 Japan Pediatric Society
diagnosis, and screening for breast cancer has been proven to reduce mortality. The difcult ethical problem for genetic testing for this syndrome is that the cancers occur with high frequency among children. Cancer morbidity and mortality may be reduced by genetic testing of these children rather than waiting until young adulthood. As children mature, it becomes appropriate to consider their assent or dissent to testing as well as their parents permission. Parents and investigators should develop a plan regarding the timing and the person to convey test results to children. Although genetic testing has several potentially benecial aspects, predictive testing for p53 mutations should be guided by the four ethical principles of respect for autonomy, benecence, condentiality, and justice. Predictive testing for germ-line p53 mutations should be initiated only after counseling and support services have been established. Mutations of the p53 gene have been associated with resistance to chemotherapy as well as a poor prognosis in many different malignancies. TP53 mutation is identied in approximately 20% of de novo osteosarcomas, but in the case of de novo osteosarcoma, the p53 mutation status is not associated with prediction of the prognosis, or the risk of systemic relapse, metastasis or chemotherapy sensitivity.10 No convincing studies have compared the prognosis, or chemotherapy sensitivity between de novo osteosarcoma and osteosarcoma that developed in LFS patients. Further studies of those issues are required. The present patient has remained in complete remission for 18 months. Because the response to the neoadjuvant chemotherapy was poor, the present patient is being carefully monitored to ensure early identication of recurrent osteosarcoma or any second unrelated tumors.
Acknowledgment
We thank Dr Masatoshi Takagi for his helpful comments regarding the manuscript.
References
1 Li FP, Fraumeni JF, Mulvihill JJ et al. A cancer family syndrome in twenty-four kindreds. Cancer Res. 1988; 48: 535862. 2 Tinat J, Bougeard G, Baert-Desurmont S et al. 2009 version of the Chompret criteria for Li Fraumeni syndrome. J. Clin. Oncol. 2009; 27: e1089. 3 Eeles RA. Germline mutations in the TP53 gene. Cancer Surv. 1995; 25: 10124. 4 Birch JM, Hartley AL, Tricker KJ et al. Prevalence and diversity of constitutional mutations in the p53 gene among 21 Li-Fraumeni families. Cancer Res. 1994; 54: 1298304.
bs_bs_banner
Novel p53 splicing site mutation in LFL
5 Varley JM, Attwooll C, White G et al. Characterization of germline TP53 splicing mutations and their genetic and functional analysis. Oncogene 2001; 20: 264754. 6 Petitjean A, Achatz MI, Borresen-Dale AL, Hainaut P, Olivier M. TP53 mutations in human cancers: Functional selection and impact on cancer prognosis and outcomes. Oncogene 2007; 26: 2157 65. 7 Varley JM, Evans DG, Birch JM. Li-Fraumeni syndrome: A molecular and clinical review. Br. J. Cancer 1997; 76: 114. 8 Achatz MI, Olivier M, Le Calvez F et al. The TP53 mutation, R337H, is associated with Li-Fraumeni and Li-Fraumeni-Like syndromes in Brazilian families. Cancer Lett. 2007; 245: 96 102. 9 McIntyre JF, Smith-Sorensen B, Friend SH et al. Germline mutations of the p53 tumor suppressor gene in children with osteosarcoma. J. Clin. Oncol. 1994; 12: 92530.
111
10 Wunder JS, Gokgoz N, Parkes R et al. TP53 mutations and outcome in osteosarcoma: A prospective, multicenter study. J. Clin. Oncol. 2005; 23: 148390.
Supporting information
Additional Supporting Information may be found in the online version of this article: Figure S1. The primer designations for the target sequence. Please note: Wiley-Blackwell are not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
ped_3631 111..138
T-cell large granular lymphocyte leukemia in a child with anemia and Crohns disease
Kensuke Kondoh,1 Mizuho Morimoto,1 Dai Keino,1 Ryo Oyama,1 Chiai Nagae,1 Tomoko Ashikaga,1 Katsuhiro Arai,2 Atsuko Nakazawa3 and Akitoshi Kinoshita1 1 Department of Pediatrics, St Marianna University School of Medicine, Kanagawa, 2Division of Gastroenterology, Department of Medical Specialties and 3Department of Pathology, National Center for Child Health and Development, Tokyo, Japan
Abstract T-LGL leukemia has been rarely reported in children. We report a child with T-LGL leukemia who presented with anemia and went on to develop Crohns disease. Although prednisolone treatment proved effective in the treatment of anemia, large granular lymphocyte counts increased as the doses were tapered. T-cell rearrangement studies revealed a clonal rearrangement of the TCR Vb/jb2 gene. Concurrently, the patient developed severe diarrhea. Inammatory changes across the upper and lower intestines led to the diagnosis of Crohns disease. This case highlights that T-LGL leukemia could be occurred in children. Flow cytometry and/or T-cell gene rearrangement studies are recommend in patients of anemia and various kind of autoimmune diseases including Crohns disease, even in children.
Key words anemia, autoimmune disease, Crohns disease, parvovirus B19, T-cell large granular lymphocyte leukemia.
Large granular lymphocyte (LGL) leukemia is a lymphoproliferative disorder characterized by a persistent increase in LGL cells in the blood or bone marrow.1 On the basis of clonal proliferation, LGL cells have been classied into either CD3-positive T-cell LGL (T-LGL) or CD3-negative natural killer (NK)-LGL. The former demonstrates clonal rearrangement of the T-cell receptor (TCR) gene. Clinical manifestations of this group include cytopenia,2 rheumatoid arthritis, various constitutional symptoms,3 and
Correspondence: Kensuke Kondoh, MD, Department of Pediatrics, St Marianna University, School of Medicine, 2-16-1 Sugao Miyamaeku, Kawasaki 216-8511, Japan. Email: kensuke-k@marianna-u.ac.jp Received 22 July 2011; revised 1 February 2012; accepted 16 March 2012. doi: 10.1111/j.1442-200X.2012.03631.x
no clinical signs.4 The disease, however, is indolent and does not progress to a more aggressive disorder.3 Although a few pediatric cases have been reported, the median age of onset is 55 years with equal gender distribution. Herein, we report the case of a 2-yearold boy with T-LGL leukemia who initially presented with anemia and later developed Crohns disease.
Case report
A 28-month-old Japanese male patient was referred to St Marianna University School of Medicine Hospital after he received red blood cell transfusion at a previous hospital, where his hemoglobin level was found to be 2.7 g/dL. He had a history of erythema infectosum, which was diagnosed when he was 19 months old. Physical examination indicated a relatively comfortableappearing child, except for facial pallor. His height ranged
2013 The Authors Pediatrics International 2013 Japan Pediatric Society
You might also like
- The Every Other Day DietDocument33 pagesThe Every Other Day DietDrGyenes Zsuzsanna0% (2)
- A Novel Somatic K-Ras Mutation in Juvenile Myelomonocytic LeukemiaDocument2 pagesA Novel Somatic K-Ras Mutation in Juvenile Myelomonocytic LeukemiamahanteshNo ratings yet
- Oncogenic Osteomalacia - A Complex Dance of Factors: Thomas O. Carpenter, M.DDocument4 pagesOncogenic Osteomalacia - A Complex Dance of Factors: Thomas O. Carpenter, M.DAsticha Erlianing SariNo ratings yet
- Late Onset Thrombosis in A Case of Severe Protein S Deficiency Due To Compound Heterozygosity For PROS1 MutationsDocument3 pagesLate Onset Thrombosis in A Case of Severe Protein S Deficiency Due To Compound Heterozygosity For PROS1 Mutationsgabriela ciolpanNo ratings yet
- A Novel Fibrillin-1 Gene Missense Mutation Associated With Neonatal Marfan Syndrome - A Case Report and Review of The Mutation SpectrumDocument6 pagesA Novel Fibrillin-1 Gene Missense Mutation Associated With Neonatal Marfan Syndrome - A Case Report and Review of The Mutation SpectrumeduardoperezagonzalezNo ratings yet
- La Mellarin D2Document2 pagesLa Mellarin D2JESUS DAVID BOLA‹O JIMENEZNo ratings yet
- Storti Foundation: Clinical Relevance ofDocument4 pagesStorti Foundation: Clinical Relevance ofNimra AwaisNo ratings yet
- SF3B1 and Other Novel Cancer Genes: in Chronic Lymphocytic LeukemiaDocument10 pagesSF3B1 and Other Novel Cancer Genes: in Chronic Lymphocytic LeukemiaRafael ColinaNo ratings yet
- (Sici) 1520 6823 (1997) 5:3 93::aid Roi1 3.0.co 2 DDocument4 pages(Sici) 1520 6823 (1997) 5:3 93::aid Roi1 3.0.co 2 DRashmeeta ThadhaniNo ratings yet
- Karen A. Gelmon: Desmoplastic Small Round-Cell Tumor of The PancreasDocument3 pagesKaren A. Gelmon: Desmoplastic Small Round-Cell Tumor of The PancreasAdam HartonoNo ratings yet
- Microscopy Res Technique - 2001 - Southwood - Molecular Pathways of Oligodendrocyte Apoptosis Revealed by Mutations inDocument9 pagesMicroscopy Res Technique - 2001 - Southwood - Molecular Pathways of Oligodendrocyte Apoptosis Revealed by Mutations inAnglia LopesNo ratings yet
- Targetable Kinase-Activating Lesions in Ph-Like Acute Lymphoblastic LeukemiaDocument11 pagesTargetable Kinase-Activating Lesions in Ph-Like Acute Lymphoblastic LeukemiaseverinNo ratings yet
- 2016 Article 70Document8 pages2016 Article 70sawantleena62No ratings yet
- Angelman Syndrome Phenotype Associated With Mutations in Mecp2, A Gene Encoding A Methyl CPG Binding ProteinDocument6 pagesAngelman Syndrome Phenotype Associated With Mutations in Mecp2, A Gene Encoding A Methyl CPG Binding ProteinAkmal NugrahaNo ratings yet
- Jurnal OM TransleteDocument7 pagesJurnal OM TransleterisjunNo ratings yet
- Gene Expression Differences Between Thyroid Carcinoma, Thyroid Adenoma and Normal Thyroid TissueDocument11 pagesGene Expression Differences Between Thyroid Carcinoma, Thyroid Adenoma and Normal Thyroid TissueArtha MahulaeNo ratings yet
- Pancytopenia As Initial Presentation of Acute Lymphoblastic Leukemia and Its Associationwith Bone MarrowresponseDocument6 pagesPancytopenia As Initial Presentation of Acute Lymphoblastic Leukemia and Its Associationwith Bone MarrowresponseIJAR JOURNALNo ratings yet
- Anemia Aplastic JournalDocument13 pagesAnemia Aplastic JournalGenoveva Maditias Dwi PertiwiNo ratings yet
- Campbell 1992Document3 pagesCampbell 1992Pilar AufrastoNo ratings yet
- 439 2007 Article 362Document6 pages439 2007 Article 362Zinik EşanuNo ratings yet
- 1 s2.0 S0016508515013104 MainDocument16 pages1 s2.0 S0016508515013104 MainMaria PalNo ratings yet
- Genomic Mutations of Primary and Metastatic LungDocument9 pagesGenomic Mutations of Primary and Metastatic LungDiana AyuNo ratings yet
- Abnormalities of RUNX1, CBFB, CEBPA, and NPM1 Genes in Acute Myeloid LeukemiaDocument10 pagesAbnormalities of RUNX1, CBFB, CEBPA, and NPM1 Genes in Acute Myeloid LeukemiaAndikhaNo ratings yet
- European Journal of Medical GeneticsDocument7 pagesEuropean Journal of Medical GeneticsAdam NowakNo ratings yet
- 1500 Pac MNewDocument6 pages1500 Pac MNewBioq. GallegosNo ratings yet
- Management of Iron Overload With A Disposable Multi-Day Delivery SystemDocument1 pageManagement of Iron Overload With A Disposable Multi-Day Delivery SystemEloy Guillermo Mijares EchezuríaNo ratings yet
- Primary Midgut VolvulusDocument2 pagesPrimary Midgut VolvulusNihal S KiranNo ratings yet
- Letter: Mutations in UBQLN2 Cause Dominant X-Linked Juvenile and Adult-Onset ALS and ALS/dementiaDocument7 pagesLetter: Mutations in UBQLN2 Cause Dominant X-Linked Juvenile and Adult-Onset ALS and ALS/dementiaGarzo ZardofskyNo ratings yet
- Multiple Lipomas Linked To An RB1 Gene Mutation in A Large Pedigree With Low Penetrance RetinoblastomaDocument5 pagesMultiple Lipomas Linked To An RB1 Gene Mutation in A Large Pedigree With Low Penetrance RetinoblastomaMaria Burke-ChaussonNo ratings yet
- On The Horizon From The ORS: WNT, Osteosarcoma, and Future TherapyDocument2 pagesOn The Horizon From The ORS: WNT, Osteosarcoma, and Future TherapyEbetWasuwayNo ratings yet
- Slater Case Presentation Issue 1 Article For WebsiteDocument2 pagesSlater Case Presentation Issue 1 Article For Websiteapi-400507461No ratings yet
- Ovarian Granulocytic Sarcoma in A Patient With Philadelphia Chromosome-Positive Acute Biphenotypic Leukemia - Case ReportDocument5 pagesOvarian Granulocytic Sarcoma in A Patient With Philadelphia Chromosome-Positive Acute Biphenotypic Leukemia - Case ReportOoAldoONo ratings yet
- Myeloid NeoplasiaDocument10 pagesMyeloid NeoplasiaivssonNo ratings yet
- AMM V 27.07Document138 pagesAMM V 27.07Anonymous 5cHdazK6b100% (1)
- Jack 2Document5 pagesJack 2Josue BarralNo ratings yet
- AMM V 27.07Document138 pagesAMM V 27.07paul_calburean7899No ratings yet
- Steroid Resistant NephroticS YndromeDocument42 pagesSteroid Resistant NephroticS YndromeSholihatul AmaliyaNo ratings yet
- 66 68 PBDocument89 pages66 68 PBAyesha FatimaNo ratings yet
- Jurnal InternaDocument3 pagesJurnal InternaIndahNo ratings yet
- Pancreatic CancerDocument13 pagesPancreatic CancerFA MonterNo ratings yet
- Acute Pyelonephritis in Adults: A Case Series of 223 PatientsDocument6 pagesAcute Pyelonephritis in Adults: A Case Series of 223 PatientsshiaNo ratings yet
- Paper Comparativa Sobrevida de PV, TE y MFPDocument7 pagesPaper Comparativa Sobrevida de PV, TE y MFPDani HaindlNo ratings yet
- McKinnis Bone Marrow Transplantation Hunter Syndrome The Journal of PediatricsDocument17 pagesMcKinnis Bone Marrow Transplantation Hunter Syndrome The Journal of PediatricsBoNo ratings yet
- How I Treat Polycythemia VeraDocument11 pagesHow I Treat Polycythemia Veraayu_cicuuNo ratings yet
- PIIS0085253815551752Document6 pagesPIIS0085253815551752Ignacio TabuadaNo ratings yet
- Adult Acute Lymphoblastic Leukemia: Concepts and StrategiesDocument12 pagesAdult Acute Lymphoblastic Leukemia: Concepts and StrategiesdrravesNo ratings yet
- Adult Minimal-Change Disease: Clinical Characteristics, Treatment, and OutcomesDocument9 pagesAdult Minimal-Change Disease: Clinical Characteristics, Treatment, and OutcomesMutiara RizkyNo ratings yet
- Psu 50318Document4 pagesPsu 50318Dr Venkatachalapathy T S Ped SurgeonNo ratings yet
- Cancers 14 01120 v4Document21 pagesCancers 14 01120 v4ABCNo ratings yet
- Mar FanDocument5 pagesMar FanLav DehcNo ratings yet
- Neuroendocrine Tumors: Surgical Evaluation and ManagementFrom EverandNeuroendocrine Tumors: Surgical Evaluation and ManagementJordan M. CloydNo ratings yet
- HDF Pre y Post Dilución 8 AnexoDocument7 pagesHDF Pre y Post Dilución 8 AnexoPamelaNo ratings yet
- Artigo B1Document6 pagesArtigo B1José Eduardo AdelinoNo ratings yet
- Cell Cycle and Cancer - Unit I IV/IDocument6 pagesCell Cycle and Cancer - Unit I IV/IManoj GourojuNo ratings yet
- Cystic Fibrosis Article - RCCADocument9 pagesCystic Fibrosis Article - RCCAAndleeb ImranNo ratings yet
- Bremer 1995Document5 pagesBremer 1995samuel ZhangNo ratings yet
- Fisiopatologia de La FiebreDocument3 pagesFisiopatologia de La FiebreLINA MARIA AVILA PEÑANo ratings yet
- Blastic Plasmacytoid Dendritic Cell NeoplasmeCurrent InsightsDocument10 pagesBlastic Plasmacytoid Dendritic Cell NeoplasmeCurrent InsightsPaúl Otañez MolinaNo ratings yet
- Papillary Microcarcinoma of The Thyroid-Prognostic Significance of Lymph Node Metastasis and MultifocalityDocument10 pagesPapillary Microcarcinoma of The Thyroid-Prognostic Significance of Lymph Node Metastasis and MultifocalityAZ RPNo ratings yet
- Literature Review On Sickle Cell DiseaseDocument8 pagesLiterature Review On Sickle Cell Diseaseafmzwflmdnxfeb100% (1)
- Connective Support, Binding, Locomotion Co-Ordination AbsorptionDocument3 pagesConnective Support, Binding, Locomotion Co-Ordination AbsorptionSatvik MohantyNo ratings yet
- Cushing's SyndromeDocument24 pagesCushing's SyndromeUdtjeVanDerJeyk100% (1)
- Pedigree SymbolsDocument30 pagesPedigree SymbolsJoshi SabinaNo ratings yet
- Jurnal Oogenesis Int'l 1Document8 pagesJurnal Oogenesis Int'l 1Iqval AnggiNo ratings yet
- Bacterial Kidney Disease (Renibacterium Salmoninarum) : G.D. Wiens and S.L. KaattariDocument34 pagesBacterial Kidney Disease (Renibacterium Salmoninarum) : G.D. Wiens and S.L. KaattariLiana QuinnNo ratings yet
- Planaria Lab ReportDocument3 pagesPlanaria Lab Reportapi-194648534No ratings yet
- PDF Essentials of Modern Neuroscience Lange 1St Edition Erik Roberson Ebook Full ChapterDocument53 pagesPDF Essentials of Modern Neuroscience Lange 1St Edition Erik Roberson Ebook Full Chapterdaniel.keller545100% (3)
- Nexus Magazine - August 2018 PDFDocument100 pagesNexus Magazine - August 2018 PDFmarsalg100% (3)
- Filtracion GlomerularDocument18 pagesFiltracion GlomerularNicole Jheny Raraz SosaNo ratings yet
- Anatomy and Physiology SDL 1Document3 pagesAnatomy and Physiology SDL 1Faatoots FatsNo ratings yet
- ANGIOEDEMADocument11 pagesANGIOEDEMAromimedNo ratings yet
- Scopus - All Journal Titles - Scopus - Academic Database Assessment Tool PDFDocument270 pagesScopus - All Journal Titles - Scopus - Academic Database Assessment Tool PDFSiva Kumar ReddyNo ratings yet
- Haem. Notes (MBCHB) ProperDocument162 pagesHaem. Notes (MBCHB) ProperKelvinTMaikanaNo ratings yet
- Ganoderma Lucidum Against Candida AlbicansDocument8 pagesGanoderma Lucidum Against Candida AlbicansCsikós IlonaNo ratings yet
- Final Paper 110218Document156 pagesFinal Paper 110218Bien Carlos Esteves ViaNo ratings yet
- Faculty 363 Histotechnique Lectures - 2Document27 pagesFaculty 363 Histotechnique Lectures - 2einsteinspy100% (1)
- MARK SCHEME For The June 2005 Question PaperDocument10 pagesMARK SCHEME For The June 2005 Question PaperequatorloungeNo ratings yet
- Science 9 Lesson 2 Non Mendelian Patterns of InheritanceDocument30 pagesScience 9 Lesson 2 Non Mendelian Patterns of InheritanceIts RxsgNo ratings yet
- Biology TRIPLE SCIENCE 1 2023 PREDICTEDDocument15 pagesBiology TRIPLE SCIENCE 1 2023 PREDICTEDjayakantharushanNo ratings yet
- The Neonate: Eugenia K. Pallotto, MDDocument17 pagesThe Neonate: Eugenia K. Pallotto, MDSamNo ratings yet
- History of HLA PDFDocument17 pagesHistory of HLA PDFeseNo ratings yet
- Graft Versus Host DiseaseDocument1 pageGraft Versus Host DiseaseIzhra MargateNo ratings yet
- تجميع اسئله الاخصائين 1Document36 pagesتجميع اسئله الاخصائين 1Osama BakheetNo ratings yet
- Bio TherapyDocument18 pagesBio TherapyChino RamirezNo ratings yet
- Prenatal Diagnosis On The Use of Non Invasive Prenatal Testing For The Detection of Fetal Chromosomal Conditions in Singleton Pregnanciesprenatal Diagnosis - 2023 - HuiDocument15 pagesPrenatal Diagnosis On The Use of Non Invasive Prenatal Testing For The Detection of Fetal Chromosomal Conditions in Singleton Pregnanciesprenatal Diagnosis - 2023 - HuiYến ĐàoNo ratings yet
- Biomedik 2Document22 pagesBiomedik 2Fergi ListiawanNo ratings yet
- Case Report Polyhydramions: Created By: Febiena ID. 61111005Document3 pagesCase Report Polyhydramions: Created By: Febiena ID. 61111005febienaNo ratings yet
- PIC-Seq Dissecting Cellular Crosstalk by Sequencing Physically Interacting CellsDocument16 pagesPIC-Seq Dissecting Cellular Crosstalk by Sequencing Physically Interacting CellsNiv SabathNo ratings yet
- 1 s2.0 S0022391313603583 MainDocument50 pages1 s2.0 S0022391313603583 MainDANTE DELEGUERYNo ratings yet