Professional Documents
Culture Documents
Psoriasis Vulgaris DG Kortikosteroid
Psoriasis Vulgaris DG Kortikosteroid
Uploaded by
Nurmaniar MajidOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Psoriasis Vulgaris DG Kortikosteroid
Psoriasis Vulgaris DG Kortikosteroid
Uploaded by
Nurmaniar MajidCopyright:
Available Formats
CASE REPORT
PSORIASIS VULGARIS TREATED WITH TOPICAL CORTICOSTEROIDS
Solecha Setiawati1, Dirmawati Kadir1, Wiwiek Dewiyanti1, Ni Ketut Sungowati2
1
Department of Dermatovenereology Medical Faculty of Hasanuddin University / Wahidin Sudirohusodo Hospital Makassar 2 Department of Phatology Anatomy Medical Faculty of Hasanuddin University / Wahidin Sudirohusodo Hospital Makassar
ABSTRACT
Psoriasis vulgaris is a chronic papulosquamous disease and is associated with genetic and environmental factors. Clinical manifestations in the form of red plaques with thick silvery-white squama and demarcated, predilection on the scalp and extensor extremities. Various therapeutic modalities for psoriasis vulgaris include corticosteroid topical, derivatives of vitamin D, tar preparations, biological agents and systemic agents. Reported one case of psoriasis vulgaris in a male patient aged 26 years who were treated with topical corticosteroids, seem significant improvement as measured by PASI scores (Psoriasis Area and Saverity Index). Keywords:, psoriasis vulgaris,PASI scores,topical corticosteroids.
Address for correspondence : Solecha Setiawati, dr., Department of Dermatovenereology Medical Faculty of Hasanuddin University / Wahidin Sudirohusodo Hospital Makassar Blok B/12 Jl. Poros Makassar Maros Griya Azikrul Toaha Makassar, South Sulawesi, Indonesia dr.ikasolecha@gmail.com
66
Solecha Setiawati
psoriasis vulgaris treated with topical corticosteroids
INTRODUCTION Psoriasis is a chronic inflammatory skin disease that has a close relationship with genetic factors, characterized by complex changes in the growth and differentiation of epidermal abnormalities and various biochemical, immunological, and vascular. Psoriasis is considered as a primary disorder of keratinocytes. [1] Having a form of patches lesion demarcated erythema with squama rough, layered and transparent with wax drip phenomenon, the phenomenon kobner , and Auspitz sign. (2,3,4) Psoriasis can be found all over the world. although the frequency varies in some ethnic. According to published reports, the prevalence varies among populations ranging from 0.1% to 11.8%. Highest incidence in Europe, in Denmark (2.9%) and the Faeroe Islands (2.8%), with the northern European average is around 2%. In the United States the prevalence ranged from 2.2% to 2.6% with about 150000 new cases are diagnosed each year. (1) The incidence of psoriasis appears to be lower in Asia, with a prevalence of about 0.4% . Psoriasis can affect all ages, both children and adults. But, rarely occurs in people under 10 years old. More common in the age 15 to 30 years. (1) The incidence of the same in men and women. (4) Underlying cause of psoriasis remains unclear. (1) According to Gunnar Lomholt in 1963 said that the genetically induced psoriasis. (1.2) Some risk factors that can increase the development of psoriasis in addition to family history (genetics), is the presence of trauma, infection, drugs, metabolic factors, physiogenic factors, smoking, and alcohol consumption. (1,2,7,9,11) There are several types of psoriasis include plaque psoriasis, pustular psoriasis, psoriasis guttata, 67
psoriasis erythroderma, and in certain locations such as scalp psoriasis, flexural psoriasis, psoriasis of the oral mucosa, nail psoriasis, and psoriatic arthritis. Plaque psoriasis is the most common type, found about 80-90% of patients with psoriasis. Plaque psoriasis (also known as psoriasis vulgaris or chronic stable plaque psoriasis or psoriasis chronic stationair).
(2,7,9)
Psoriasis vulgaris diagnosis is established through clinical picture, also by histopathological examination. Histopathological picture of psoriasis vulgaris varies, depending on the stage of the lesion, namely: the initial lesion; fully developed lesions, or lesions further / final
(2)
There are a variety of safe and effective treatment, such treatment can improve skin condition and reduce complaints of itch. The main goal of treatment is to reduce the severity and extensive skin lesions that the disease no longer interfere with work, personal life / social, and the livelihoods of people, as well as reduce the symptoms of psoriasis. (10) There are three basic therapeutic modalities available are topical agents, phototherapy and systemic agents, to achieve therapeutic success it is necessary to understanding the mechanism of action, toxicity, and side effects of therapy . (10) CASE REPORTS A man, 26 years old, Bugis, the Honorary Governor's office in Mamuju, went to the clinic of skin and venereal Wahidin Sudirohusodo hospital on March 11, 2013, with complaints of red and scaly skin over most of the body, which was experienced approximately 1 year ago, and was advancing from 3 months, originally appeared on the legs, appeared red and scaly patches of itchy lesions, especially
IJDV
Vol.2 No.2 2013
on the head but not with pain. Patients complaining of skin lesions spread almost throughout the body. Complaint is not found on the face and nails. History of treatment in clinical practice dermatologist in Mamuju, given ointment and oral medication, but felt no change, so it was given a referral to the clinic of skin and venereal Wahidin Sudirohusodo hospital. Family history of suffering from the same disease exist (aunt), history had previously the same disease denied. Smoking history until now. History consume alcoholic beverages 2 years ago. 68
Physical examination showed the patient's general condition is good and vital signs within normal limits. Physical examination of the heart, lungs, liver, spleen and kidney abnormalities not found. Dermatologist status obtained in the region of thoracic, abdominal, trunk posterior et anterior, glutea, extremities superior et inferior. Skin lesions are found in the form of plaques erythematous , demarcated, varied forms, from round, oval, irregular, and vary in size with a diameter of about 1-10cm, above there squama psoriasiform, dry and white. The
Solecha Setiawati
psoriasis vulgaris treated with topical corticosteroids
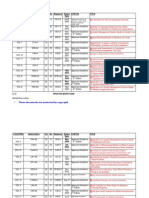
phenomenon of wax droplets (+), the phenomenon auspitz (+). PASI score (Psoriasis Area and Saverity Index) in these patients was 11.7 (Figure 1) From the results of laboratory tests of blood and urine complete in normal limit. Examination test of skin scraping with 10% KOH (Potassium Hydroxide) is negative. The differential diagnosis of this disease is psoriasis vulgaris, pityriasis rubra pilaris, and seborrheic dermatitis. Working diagnosis was psoriasis vulgaris or chronic plaque psoriasis. Then performed on the skin biopsy for histopathological examination. Patients were assigned topical treatment desoximetasone 0.25% ointment , salicyl acid 3%, 3% LCD, and vaseline. Cetirizine 10mg once a day. Antibiotics and analgesics, given after biopsy was done ciprofloxacin 500 mg twice a day, mefenamic acid 500 mg three times a day. Histopathological examination showed epidermal hyperplasia, psoriasiform, hyperkeratosis, parakeratosis, spongiosis, suprapapillary plate thinning, blood vessels dilated dermal papilla contains erythrocytes, upper dermis are pretty solid inflammatory cells infiltrates, limphohistiositic with some neutrophils, abscess munro, conclusions support psoriasis vulgaris (figure 3). Control during three days later, the patient showed improvement, plaques erythema thinning, and itching started skuama reduced and reduced. PASI score 10.3. Therapy with desoximetasone 0:25% ointment 20 grams, 3% Salicyl acid, Lcd 3%, and vaseline. Cetirizine 10mg 1x1 tablet per day. Control day 7, showed better results; plaques erythema thinning and fine scales. PASI score of 6.3.
DISCUSSION Psoriasis is a chronic skin disease that commonly occurs, and attack the 15% of the world population (5). According to Henseler and Christopherm psoriasis split in two, type I and type II. Where the prevalence of type I before the age of 40 years, and type II after the age of 40. years. (1.6,7) In this case, patients aged 26 years and there is a family history of the same disease, so it can be included in psoriasis type I. Diagnosis in these patients is psoriasis vulgaris, based on history, clinical features, histopathologic examination support. In this patient , lesions found in the form of plaques erythematous, varied forms, from round, oval, irregular, and vary in size with a diameter of about 1-10cm, squama psoriasiform, dry and shiny white, which is found on the area back, chest, abdomen, superior and inferior extremities, neck and head. Lesions characteristic of psoriasis vulgaris is erythematous plaques, demarcated, symmetrical, accompanied layered squama and shiny on scalp, extensor arms, legs, knees, elbows, back, and body .2.8) Are also perceived complaint of itchy especially on the head, there were a history of stress, smoke and drinking alcohol. Itching is an additional symptom that usually occurs in patients with psoriasis, especially scalp and anogenital regions. (4.8) As for the allegation that is considered the factors that can trigger psoriasis are: physical trauma (Koebner phenomenon), streptococuss infection, stress, drugs & alcohol. (2,4,8) Physical examination found the phenomenon of wax droplets and Auspitz mark and score Pasi 11.7. Phenomenon that is scratch squama on the lesion wax droplets so it looks uneven and tangled white lines. 69
IJDV
Vol.2 No.2 2013
Auspitz sign is a characteristic feature of psoriasis lesions, made with sloughing squama hyperkeratotic lesions in the picture and found a small bleeding spots caused by 'beheading' papillary dermis and dilation and winding blood vessels. This Auspitz sign has greater (1,2,7,12) diagnostic value. Accurate assessment of psoriasis severity is essential in clinic and research. PASI (psoriasis area severity index) is one of indicators to assess the severity of lesions of psoriasis and response to treatment. PASI assessment was first formulated by Fredricksson and Pettersson, is the most widely used method for measuring the severity of psoriasis in clinical trials. This method is a practical and fast with PASI score ranged from 0.0 to 72.0. (7,8,12) Histopathological picture of psoriasis vulgaris varies, depending on the stage of the lesion, the initial lesions, lesions that developed, and advanced lesions. (1.7) In the literature, the results of histopathologic examination is hyperkeratosis, focal parakeratosis there are heaps of neutrophils (munro micro abscesses), and focal hyperplasia psoriasiformis hypogranulosis. Suprapapillary plate area looks thinner. Some dilated capillaries at the papilla, infiltration of inflammatory cells are lymphocytes found in the dermis layer (1) The results of histopathological examination of biopsy specimens of this case, obtained with epidermal hyperplasia, psoriasisform, hyperkeratosis, parakeratosis, hypogranulosis, spongiosis, suprapapillary plate thinning, blood vessels dilated dermal papilla contains erythrocytes, upper dermis inflammatory cells infiltrates are dense enough, limphohistiositic with some neutrophils, microabscesses munro, which support a conclusion of psoriasis vulgaris. The appeal case was diagnosed 70
with seborrheic dermatitis, pityriasis rubra pilaris, linear psoriasis, and tinea corporis. Seborrheic dermatitis can be distinguished with psoriasis vulgaris seborrheic dermatitis where the color is pale patches of erythema, ill defined and covered white - yellow squama and greasy. Some cases of psoriasis overlap with seborrheic dermatitis. Seborrheic lesions can be found on the face, retroauricular, scalp, flexura, axilla and breast crease. Erythematous lesions on the area and a bit wet with smooth squama, but more dominant yellow dry squama than oily. (1,2,7,9) In Pityriasis rubra pilaris is a chronic disease, characterized by redness squama characterized by follicular keratotic papules and plaques reddish orange color that often form between the islands of normal skin (1, 9) In the linear psoriasis, a rare form of psoriasis. Psoriatic lesions appear as lesions especially on the extremities and trunk, likely nevus that covered, it's just the same linear ILVEN (inflammatory linear (1.15) verrucous epidermal nevus) Therefore resembles psoriasis in clinical and histologinya linearbaik. (1). Tinea Corporis can be excluded with KOH examination, presence of hyphae and arthrospora were obtained in skin scraping lesion, (1.4) whereas in this case KOH examination result was negative. Management of psoriasis vary widely and include broad based, severity of lesions, location of psoriasis, type of psoriasis (1.7) In mild psoriasis with PASI <8 or extensive lesions <5%, treated with topical therapy; moderate to severe psoriasis with a PASI score> 8; treated with topical therapy, phototherapy. While on severe psorisis, can be treated systematically. (1,2,6,7,10) In this patient body surface area of> 5%, or PASI score> 8, so that is treated with topical therapy.
Solecha Setiawati
psoriasis vulgaris treated with topical corticosteroids
Topical glucocorticoids are generally the mainstay of therapy in mild to moderate psoriasis. Improvement is usually achieved within 2 to 4 weeks. Mechanism of action of topical corticosteroids by binding to glucocorticoid receptors, gene transcription inhibit Ap-1 and NF-B, including IL-1 and TNF-. This therapy will suppress the hypothalamicpituitary-adrenal (high risk in children), making epidermis and dermis atrophy, striae, and tachiphylaxis This treatment is contraindicated hipersensitive to steroids, active infection skin. (1) This patient was given desoximetasone ointment 0.25%, which is a potent corticosteroid potency (class 2). Expected effectiveness is thinning plaque, a reduction in symptoms and get a repair lesions (7,8). State of lesions in this patient showed improvement, namely erythema plaques thinning, and squama reduced (PASI score 8). Plaque effectively treated if induration was lost . Topical corticosteroid therapy desoximetason 0.25% ointment forwarded. If the lesions respond better circumstances again, it is replaced with a less potent corticosteroid. Tend to fast remission when corticosteroid therapy was stopped. (1) Prognosis of the disease in this case good because lesion showed improvement after topical corticosteroids therapy. But psoriasis is a chronic skin disease and frequent recurrence, disease can be rapidly improved, but one day could be worse. [1-3]. Education should be given to patient that this disease can be recurrent, it is important to avoid the trigger factors and the treatment given and its effectiveness should be monitored to prevent adverse effects the drug.
(1,2,4,13,14)
REFERENCES
1. Gudjonsson JE, Elder JT. Psoriasis. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatricks Dermatology in General Medicine. 7 ed. New York: Mc Graw Hill; 2008. p.169-89 James WD, Berger TG, Elston DM. Psoriasis. Andrews Disease of The Skin, Clinical Dermatology. 11 ed. New York: Saunders Elsevier; 2007. p.190-198 Griffiths CEM, Barker JNWN. Psoriasis. In: Burns T, Breathnach S, Cox N, Griffits C, editors. Rook's Textbook of Dermatology. eighth ed: Wiley Blackwell; 2008. p. 20.1-.42 Wolff K, Johnson R A, Psoriasi, in klauff, R A Johnson, Editor. Fitzpatrick Color atlas & Synopsis of clinical Dermatology. Sixth edition. New York: McGrawHill Medical; 2009. p. 54-1. Gottileb A.B, Langley R.G,.Strober B.E,et all ,BJD.A.randomized,double-blind, placebo-controlled study to evaluated the addition of methotrexate to etanercept in patients with moderate to severe plaque psoriasis, British associaction of dermatology 20012;1;649-53. Mrowietz U,Reich K.DAI,Psoriasis-new insight into pathogenesis and treatment, Medicine,2009;106; p:11-19 TjatraA,Sularsito AS,Kurniati DD,Rihatmaja R,Bagian Ilmu Kesehatan Kulit dan Kelamin FK UI. Psoriasis vulgaris .Metode Diagnostik dan penatalaksanaan Psoriasis dan Dermatitis Seboroik.JakartaUI pres 2003, p: 1-53 FinalyY, Andrew L,Jv, Inflamatory Skin diseases,Edinburgh ;2006;4;47-75. http://www.bad.org.uk/publick/leaflests/
th
2.
3. 4.
5.
6.
7.
8.
9.
10. Travers,BJ,Papulo skuamos Skin Eruption. . In: Fitzpatricks JE,Morelli JG,Wolff, editors. Fitzpatricks Dermatology Secrets in General Medicine. 3 ed. New York: Mc Graw Hill; 20087 p.57-75
71
IJDV
Vol.2 No.2 2013
11. Shimizu H, Shimizuss Textbook of dermatology.Treatmen of skin diseases.Nsb,Capter 6.p:73-89 12. Patel VR,Shelling ML,Prodanovich S, Federman GD, Kirsner RS.Psoriasis and vascular diseases risc factors and outcomes:a systemic review of the literature;JGIM; 2011p:1036-1047 13. Mrowietz u,kragballe k, reich k,et all;Defenition of treatment goals for moderate to severe psoriasis a European Consensus;springer-verlag 2011;p:1-10 14. Aldeen T,basra M;Management of psoriasis and its comorbidities in primary care;BJN ;2011;p:1186 - 1192 15. Parissh l.Psoriasis : symptoms,treatments and its impact on quality of life; BJ 2012;p:524-528 16. Brinca A,Santiago F,Serra D, Andrade P,Vieira A,Linear psoriasis-two case report; Figueiredo;ISSN-2011;p:1-5
72
You might also like
- Janeway's Immunobiology 8thDocument892 pagesJaneway's Immunobiology 8thSergio Falcon Rivera92% (13)
- Childhood PsioriasisDocument6 pagesChildhood PsioriasisYuliana DaisongNo ratings yet
- Psoriasis: A Comprehensive Review: Nternational Ournal OF Harmacy & IFE CiencesDocument21 pagesPsoriasis: A Comprehensive Review: Nternational Ournal OF Harmacy & IFE Ciences24hintheghettoworkoutNo ratings yet
- Psoriasis: Epidemiology, Clinical and Histological Features, Triggering Factors, Assessment of Severity and Psychosocial AspectsDocument21 pagesPsoriasis: Epidemiology, Clinical and Histological Features, Triggering Factors, Assessment of Severity and Psychosocial AspectsMapsNo ratings yet
- Psoriasis - Systemic DiseaseDocument225 pagesPsoriasis - Systemic DiseaseShengping LUONo ratings yet
- Psoriasis: Incurable But Manageable: Luke Clews Principles of NaturopathyDocument3 pagesPsoriasis: Incurable But Manageable: Luke Clews Principles of Naturopathyglenn johnstonNo ratings yet
- 582 880 1 SMDocument11 pages582 880 1 SMJupiter CarlNo ratings yet
- Ethnopharmacological Studies of Argemone Mexicana For The Management of Psoriasis 300Document5 pagesEthnopharmacological Studies of Argemone Mexicana For The Management of Psoriasis 300Jitesh Kumar MaharanaNo ratings yet
- Homoeopathy in A Case of Palmo-Plantar Psoriasis: A Case ReportDocument5 pagesHomoeopathy in A Case of Palmo-Plantar Psoriasis: A Case ReportHomoeopathic PulseNo ratings yet
- SolDocument10 pagesSolTsigereda AberaNo ratings yet
- Behcet Disease AND Toxoplasmosis: by DR Shahzada Khan Tmo Eye A Ward HMCDocument67 pagesBehcet Disease AND Toxoplasmosis: by DR Shahzada Khan Tmo Eye A Ward HMCShahzada KhanNo ratings yet
- Psoriasis: Epidemiology, Clinical and Histological Features, Triggering Factors, Assessment of Severity and Psychosocial AspectsDocument21 pagesPsoriasis: Epidemiology, Clinical and Histological Features, Triggering Factors, Assessment of Severity and Psychosocial AspectsOktavianti Prisilia SoumokilNo ratings yet
- Case Report: Xanthoma Disseminatum With Tumor-Like Lesion On FaceDocument5 pagesCase Report: Xanthoma Disseminatum With Tumor-Like Lesion On FaceAgus SyaifudinNo ratings yet
- Ayurvedic Management of Psoriasis (Ek Kustha) - A Case StudyDocument8 pagesAyurvedic Management of Psoriasis (Ek Kustha) - A Case Studybhavana NandakumarNo ratings yet
- Ahri Proposal 2Document28 pagesAhri Proposal 2Tsigereda AberaNo ratings yet
- Psoriasis Case Presentation 2Document9 pagesPsoriasis Case Presentation 2conterNo ratings yet
- Dermatology D. Azr Lec2 Mon 18.10.2010: Papulosquamous DiseasesDocument9 pagesDermatology D. Azr Lec2 Mon 18.10.2010: Papulosquamous DiseasesMohamed Al-zichrawyNo ratings yet
- Thesis PsoriasisDocument4 pagesThesis PsoriasisDereck Downing100% (2)
- Case Report of Acne Vulgaris Edit 1Document18 pagesCase Report of Acne Vulgaris Edit 1Irwin FitriansyahNo ratings yet
- Psoriasis and Dermatitis AtopicDocument11 pagesPsoriasis and Dermatitis AtopicsayasajaNo ratings yet
- Ijms 20 01475 With CoverDocument29 pagesIjms 20 01475 With CoverJemini PereraNo ratings yet
- Psoriasis: PathophysiologyDocument23 pagesPsoriasis: PathophysiologyImran KhanNo ratings yet
- Psoriasis A Case StudyDocument14 pagesPsoriasis A Case StudyYayin PestañoNo ratings yet
- Staphylococcal Scalded Skin Syndrome in Child A CADocument6 pagesStaphylococcal Scalded Skin Syndrome in Child A CAsalshabilaNo ratings yet
- Stevens-Johnson Syndrome Induced by Carbamazepine: PharmacologyDocument4 pagesStevens-Johnson Syndrome Induced by Carbamazepine: PharmacologyginNo ratings yet
- Case ReportDocument12 pagesCase ReportRimueng GhuenNo ratings yet
- Psoriasis A Comprehensive Review On The AetiopathoDocument29 pagesPsoriasis A Comprehensive Review On The AetiopathoGregorius HocevarNo ratings yet
- 170 FullDocument4 pages170 FullRegita LatuihamalloNo ratings yet
- Systemic Lupus Erythematosus Discoid in Dog CanisDocument4 pagesSystemic Lupus Erythematosus Discoid in Dog CanisAlina BlondaNo ratings yet
- Psoriasis: Psoriasis Type of PsoriasisDocument18 pagesPsoriasis: Psoriasis Type of PsoriasisDeepikaNo ratings yet
- Psoriasis A Biological and Behavioral Management ApproachDocument5 pagesPsoriasis A Biological and Behavioral Management ApproachAthenaeum Scientific PublishersNo ratings yet
- Oral Manifestations of Behcet's Syndrome: Case ReportDocument6 pagesOral Manifestations of Behcet's Syndrome: Case Report24 februaryNo ratings yet
- Sjogren Syndrome A Case ReportDocument3 pagesSjogren Syndrome A Case ReportEditor IJTSRDNo ratings yet
- Psoriasis - StatPearls - NCBI BookshelfDocument8 pagesPsoriasis - StatPearls - NCBI BookshelfMehmet TaşçıNo ratings yet
- LuciophenomenonDocument6 pagesLuciophenomenonAdniana NareswariNo ratings yet
- Pathology Outlines - PsoriasisDocument1 pagePathology Outlines - PsoriasisCaryl DagamiNo ratings yet
- Faculty of Medicine: DR Archianda Arsad HakimDocument8 pagesFaculty of Medicine: DR Archianda Arsad HakimnikfarisNo ratings yet
- Papules On The Back: Figure 1a, BDocument3 pagesPapules On The Back: Figure 1a, BDwi Tantri SPNo ratings yet
- Herpes OdontalgiaDocument5 pagesHerpes OdontalgiaBramita Beta ArnandaNo ratings yet
- Erythroderma Caused Drug Allergies: Case ReportDocument7 pagesErythroderma Caused Drug Allergies: Case Report568563No ratings yet
- Patterns of Skin Disease and Prescribing Trends in Rural India Juno J. Joel, Neethu Jose, Shastry C.SDocument6 pagesPatterns of Skin Disease and Prescribing Trends in Rural India Juno J. Joel, Neethu Jose, Shastry C.SHabibur RahmanNo ratings yet
- Muco-Cutaneous & Aphthous UlcerDocument7 pagesMuco-Cutaneous & Aphthous Ulcerربيد احمد مثنى يحيى كلية طب الاسنان - جامعة عدنNo ratings yet
- Case Report: Lepra Reaction With Lucio Phenomenon Mimicking Cutaneous VasculitisDocument5 pagesCase Report: Lepra Reaction With Lucio Phenomenon Mimicking Cutaneous VasculitisadibahtiarNo ratings yet
- Herpes Zoster Thorakalis Th9Document13 pagesHerpes Zoster Thorakalis Th9Roby Syah Putra FirmansyahNo ratings yet
- Tugas Behcet SyndromDocument6 pagesTugas Behcet SyndromIsmy HoiriyahNo ratings yet
- 2545-Article Text-7661-1-10-20190414 PDFDocument6 pages2545-Article Text-7661-1-10-20190414 PDFClariza ZulyanNo ratings yet
- Therapy Selection For Tinea Corporis and Cruris With CommorbidityDocument9 pagesTherapy Selection For Tinea Corporis and Cruris With CommorbidityShimie Shimie KokobopNo ratings yet
- Background: Aphthous Ulcers UveitisDocument19 pagesBackground: Aphthous Ulcers UveitisCupris23No ratings yet
- Comorbidities in Psoriasis PDFDocument9 pagesComorbidities in Psoriasis PDFbogdansoroNo ratings yet
- Recent Insights Into The Immunopathogenesis of Psoriasis Provide New Therapeutic OpportunitiesDocument13 pagesRecent Insights Into The Immunopathogenesis of Psoriasis Provide New Therapeutic Opportunitiesraudhatul muttaqinNo ratings yet
- Psoriasis Research PaperDocument4 pagesPsoriasis Research Papervvjrpsbnd100% (1)
- 1 PBDocument6 pages1 PBdamayantiwenny24No ratings yet
- Case Report - PsoriasisDocument7 pagesCase Report - Psoriasisnathalia gabriellaNo ratings yet
- Serbian Association of Dermatovenereologists Guidelines For The Diagnosis and Treatment of PsoriasisDocument18 pagesSerbian Association of Dermatovenereologists Guidelines For The Diagnosis and Treatment of PsoriasisAndjela KosticNo ratings yet
- Jurnal Reading Glorivy Regita 112021072Document5 pagesJurnal Reading Glorivy Regita 112021072Regita LatuihamalloNo ratings yet
- Psoriasis NATURE AYFinlayDocument48 pagesPsoriasis NATURE AYFinlayMelly SyafridaNo ratings yet
- Behc Et's Disease Physiopathology: A Contemporary Review: DescriptionDocument12 pagesBehc Et's Disease Physiopathology: A Contemporary Review: Descriptionerma gusmayantiNo ratings yet
- Kuliah 4 B - PSORIASISDocument30 pagesKuliah 4 B - PSORIASISTimothy TobiasNo ratings yet
- Basic of AutoimmunityDocument13 pagesBasic of Autoimmunitymahadevabhu07100% (1)
- Presentation 3 (Information) Major Descending (Motor) Pathway and Spinal Cord Tracts March 25, 2012Document23 pagesPresentation 3 (Information) Major Descending (Motor) Pathway and Spinal Cord Tracts March 25, 2012bsittNo ratings yet
- Antigen - Antibody Reactions: Dr.D.BinduDocument46 pagesAntigen - Antibody Reactions: Dr.D.Bindubindu dhanapalNo ratings yet
- Molecules 28 05624Document30 pagesMolecules 28 05624Sayed Newaj ChowdhuryNo ratings yet
- Alphabetical Listing of CLSI Books0309Document15 pagesAlphabetical Listing of CLSI Books0309glodovichiNo ratings yet
- Intervenciones en Dermatitis Atópica CaninaDocument16 pagesIntervenciones en Dermatitis Atópica CaninaMaka.ibanezNo ratings yet
- Cellular AberrationsDocument94 pagesCellular AberrationsridzkhaNo ratings yet
- Brugia MalayiDocument8 pagesBrugia MalayiROn Ace DancelNo ratings yet
- Oms BookDocument292 pagesOms BookLUisNo ratings yet
- Carlos Simon, Antonio Pellicer-Stem Cells in Human Reproduction_ Basic Science and Therapeutic Potential, 2nd Edition (Reproductive Medicine & Assisted Reproductive Techniques)-Informa Healthcare (200Document273 pagesCarlos Simon, Antonio Pellicer-Stem Cells in Human Reproduction_ Basic Science and Therapeutic Potential, 2nd Edition (Reproductive Medicine & Assisted Reproductive Techniques)-Informa Healthcare (200yasirhistoNo ratings yet
- Textbook Therapy For Severe Psoriasis Jashin J Wu Ebook All Chapter PDFDocument53 pagesTextbook Therapy For Severe Psoriasis Jashin J Wu Ebook All Chapter PDFcalvin.price163100% (2)
- Report Regarding DepressionDocument18 pagesReport Regarding Depressiontech masterNo ratings yet
- Antimicrobial DrugsDocument20 pagesAntimicrobial Drugsmaria adventia martinNo ratings yet
- Stress Management Thru Sahaja Yoga (Always Free)Document19 pagesStress Management Thru Sahaja Yoga (Always Free)Vinay Singh100% (5)
- HCV Treatment RevolutionDocument3 pagesHCV Treatment RevolutionMai NabiehNo ratings yet
- Cells vs. Viruses Venn Diagram Sort: Interactive Notebooking ActivityDocument2 pagesCells vs. Viruses Venn Diagram Sort: Interactive Notebooking ActivityNellyRdzNo ratings yet
- MCQs From All Subjects For Medical PG EntranceDocument16 pagesMCQs From All Subjects For Medical PG EntranceEMIN3MNo ratings yet
- Protein BiosynthesisDocument33 pagesProtein BiosynthesisLucy WijayaNo ratings yet
- Vitamin DeficiencyDocument43 pagesVitamin DeficiencyAathi Pathmanathan100% (1)
- Cellometer Via Stain CS1 0108 5ML Product Insert Rev A PDFDocument4 pagesCellometer Via Stain CS1 0108 5ML Product Insert Rev A PDFDimasPrasetiantoWicaksonoNo ratings yet
- Dwnload Full Wheaters Basic Pathology A Text Atlas and Review of Histopathology 5th Edition Young Test Bank PDFDocument36 pagesDwnload Full Wheaters Basic Pathology A Text Atlas and Review of Histopathology 5th Edition Young Test Bank PDFasherharrisgdo3100% (12)
- Intraocular Pressure and Aqueous Humor DynamicsDocument36 pagesIntraocular Pressure and Aqueous Humor DynamicsIntan EkarulitaNo ratings yet
- Vitamin ChartDocument3 pagesVitamin ChartSrivani MamidishettyNo ratings yet
- Mesenchymal Stem Cells: From Biology To Clinical UseDocument10 pagesMesenchymal Stem Cells: From Biology To Clinical UseroyNo ratings yet
- The Regeneration of Human Limbs PDFDocument21 pagesThe Regeneration of Human Limbs PDFKeke MauroNo ratings yet
- Thirteenth Course "Clinical Cytogenetics", Goldrain Castle (BZ), ItalyDocument2 pagesThirteenth Course "Clinical Cytogenetics", Goldrain Castle (BZ), ItalyDoina Ababii UrsanNo ratings yet
- Muscle & MalocclusionDocument57 pagesMuscle & MalocclusionRazeev Mishra100% (1)
- DNADocument23 pagesDNAMuneeb Jan100% (1)
- Lung Cancer Presentation: DR Richard Sullivan and Ms Anne FraserDocument24 pagesLung Cancer Presentation: DR Richard Sullivan and Ms Anne FraseranggiNo ratings yet