Professional Documents
Culture Documents
Prp-Soft Tissue Coverage
Prp-Soft Tissue Coverage
Uploaded by
Partha Saradhi0 ratings0% found this document useful (0 votes)
29 views11 pagesGingival recession can compromise esthetics and function of dental treatment. This article reviews the current evidence on the role of platelet-rich plasma. Clinical evidence on the use of PRP in root-coverage procedures is extremely limited.
Original Description:
Original Title
Prp-soft Tissue Coverage
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentGingival recession can compromise esthetics and function of dental treatment. This article reviews the current evidence on the role of platelet-rich plasma. Clinical evidence on the use of PRP in root-coverage procedures is extremely limited.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
29 views11 pagesPrp-Soft Tissue Coverage
Prp-Soft Tissue Coverage
Uploaded by
Partha SaradhiGingival recession can compromise esthetics and function of dental treatment. This article reviews the current evidence on the role of platelet-rich plasma. Clinical evidence on the use of PRP in root-coverage procedures is extremely limited.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 11
VOLUME 39 NUMBER 6 JUNE 2008 473
QUI NTESSENCE I NTERNATI ONAL
Patients are placing increasing value on
esthetic and functional outcomes of dental
treatment. Gingival recession can compro-
mise both esthetics and function and is a
common condition, with reported prevalence
as high as 50% to 88% in adults.
1
Traditional
root-coverage procedures include the sub-
epithelial connective tissue graft,
2
coronally
advanced flap,
3
semilunar flap,
4
laterally posi-
tioned flap,
5
double papilla flap,
6
and the
epithelialized gingival graft.
7
Recently, dermal allografts
8,9
and guided
tissue regeneration (GTR)
1012
have been
introduced as alternative treatment options.
Today, the subepithelial connective tissue
graft procedure is still considered the gold
standard for root coverage with mean per-
cent root coverage varying between 65%
and 98% and complete root coverage
achieved in 0% to 90% of cases.
13,14
The
Role of platelet-rich plasma in soft tissue
root-coverage procedures: A review
Jill D. Bashutski, DDS
1
/Hom-Lay Wang, DDS, MSD
2
The aim of this article was to review the current evidence on the role of platelet-rich plasma
(PRP) in enhancing root-coverage techniques and discuss the rationale for its use in these
applications. Sound biologic rationale and a multitude of basic science research support
the use of PRP to promote soft tissue healing, although evidence of its role in enhancing
periodontal applications, especially root coverage, is limited. Current scientific research
has yet to elucidate all of the mechanisms by which PRP can affect soft tissue healing and
assess its capacity to stimulate regeneration. Furthermore, clinical evidence on the use of
PRP in root-coverage procedures is extremely limited, with only 2 randomized controlled
trials published as of May 2007. A pertinent review of medical and dental literature relating
to PRP and its role in wound healing and enhancement of root-coverage procedures was
performed. Preliminary reports in this area suggest that the potential benefits of PRP in
root-coverage procedures may be improved esthetics, decreased patient morbidity, and
accelerated wound healing. An appropriate assessment of the effects of PRP and its pos-
sible use in enhancing root-coverage procedures cannot be made at this time because of
inadequate clinical evidence. (Quintessence Int 2008;39:473483)
Key words: platelet-rich plasma, regeneration, root coverage, soft tissue grafts
1
Resident, Department of Periodontics and Oral Medicine,
School of Dentistry, University of Michigan, Ann Arbor,
Michigan.
2
Professor and Director of Graduate Periodontics, Department
of Periodontics and Oral Medicine, School of Dentistry,
University of Michigan, Ann Arbor, Michigan.
Correspondence: Dr Hom-Lay Wang, Professor and Director of
Graduate Periodontics, Department of Periodontics and Oral
Medicine, University of Michigan School of Dentistry, 1011
North University Avenue, Ann Arbor, MI 48109-1078. Fax: 734-
936-0374. E-mail: homlay@umich.edu
Bashutski.qxd 4/15/08 2:13 PM Page 473
COPYRIGHT 2008 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO
PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER
474 VOLUME 39 NUMBER 6 JUNE 2008
QUI NTESSENCE I NTERNATI ONAL
Bashut ski /Wang
disadvantages of this technique include the
need for a donor site and occasional unsatis-
factory tissue contour and esthetics.
1315
In
addition, complications that may arise using
this technique include excessive bleeding at
the donor site and infection and/or slough-
ing at the receptor site.
1315
The coronally advanced flap procedure
has a wide range of clinical success, with an
average root coverage of 75% to 99% and
complete root coverage in 23% to 95% of
cases.
1619
The coronally advanced flap proce-
dure has an advantage over the subepithelial
connective tissue graft in that it does not
require a second surgical site; however, this is
at the expense of gaining tissue thickness.
Similarly, root-coverage procedures utilizing
GTR can achieve an average of 74% reces-
sion depth coverage, with complete coverage
in 41% of cases.
20
Providing soft tissue coverage of denuded
root surfaces presents a unique challenge in
that these surfaces are avascular, which com-
plicates the healing process. Also, if soft tis-
sue grafting is employed, it can be difficult to
stabilize the graft against the tooth surface,
resulting in sloughing and even occasional
failure of the graft.
15
While traditional root-
coverage procedures have adequately
addressed the challenge of covering exposed
roots, other factors such as esthetic accept-
ability, patient morbidity, and postsurgical
healing time for these grafts are sometimes
suboptimal. More important, root coverage
using these techniques primarily results in tis-
sue repair, not regeneration.
21
As a result, new
approaches to root coverage currently involve
incorporating growth factors into previously
employed techniques to enhance the healing
response and possibly promote regeneration.
Most recently, enamel matrix derivative,
platelet-derived growth factor, and platelet-rich
plasma (PRP) have been studied for these
purposes. Although data are emerging on the
ability of these factors to affect wound healing
and root coverage, more long-term research is
needed to fully evaluate their clinical utility.
This article reviews current information on the
use of PRP in soft tissue healing and root-cov-
erage procedures, focusing on the biologic
rationale behind its use and summarizing per-
tinent studies on the subject.
The search strategy included an electronic
search of the Medline (PubMed) database for
medical and dental literature published in the
English language through May 2007. Key
search terms included root coverage, coronal-
ly advanced flap, connective tissue graft, gin-
gival recession, platelet-rich plasma, and PRP.
In addition, the bibliographies of several key
papers
2224
were also reviewed and pertinent
references included. The search resulted in a
total of 4 clinical studies, all of which are pre-
sented in the body of this article.
PLATELET-RICH PLASMA
Platelet-rich plasma is essentially an increased
concentration of autologous platelets sus-
pended in a small amount of plasma after
centrifugation. Several systems have been
developed to isolate PRP, all with varying
platelet and growth factor yields (for a detailed
review, see Roukis et al
25
). Briefly, a small vol-
ume (about 50 mL) of the patients blood is
obtained and centrifuged at varying speeds
until it separates into 3 layers: platelet-poor
plasma, platelet-rich plasma, and red blood
cells. The PRP is isolated and stored with a cit-
rate-based anticoagulant until the end of the
surgical procedure. Immediately before appli-
cation, topical bovine thrombin and 10% cal-
cium chloride are added to activate the clot-
ting cascade, producing a platelet gel. The
whole process takes approximately 12 min-
utes
26
and produces a platelet concentration
of 3 to 5 times that of native plasma.
26,27
Because the platelets are autologous, they
are able to secrete bioactive growth factors
upon activation and subsequent degranulation
of their alpha granules. These growth factors
are also present at increased concentrations in
PRP and are involved in key stages of wound
healing and regenerative processes including
chemotaxis, proliferation, differentiation, and
angiogenesis.
28
In addition to growth factors,
platelets release numerous other substances
that are important in wound healing. Table 1
summarizes these substances and describes
the specific role of each in wound healing.
Bashutski.qxd 4/15/08 2:13 PM Page 474
COPYRIGHT 2008 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO
PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER
VOLUME 39 NUMBER 6 JUNE 2008 475
QUI NTESSENCE I NTERNATI ONAL
Bashut ski /Wang
BIOLOGIC RATIONALE
PRP contains a plethora of substances
involved in the wound healing process that
have the potential to greatly enhance soft tis-
sue healing. Table 2 summarizes these
mechanisms. In addition, Table 3 and Fig 1
list proposed advantages and disadvantages
for the use of PRP in root-coverage applica-
tions, which are elucidated forthwith.
VASCULARITY
Because PRP contains many growth factors
that stimulate angiogenesis and increase
granulation tissue formation, using PRP in
combination with root-coverage procedures
may be particularly advantageous (see Table
1). Vascular endothelial growth factor and
platelet-derived growth factor are perhaps
the most widely characterized growth factors
Secreted factor Function
Platelet-derived growth factor (PDGF) Accelerates deposition of wound matrix
(-AA, -BB, -AB) Promotes chemotaxis of polymorphonuclear leukocytes,
macrophages, fibroblasts, and smooth muscle cells
Increases fibroblast and endothelial cell differentiation
Enhances angiogenesis
16,39,72,73
Transforming growth factor (TGF) (-1, -2) Accelerates deposition and maturation of collagen
Promotes hemotaxis of fibroblasts
Stimulates collagen and fibronectin production
Inhibits collagen degradation
16,39,72
Vascular endothelial growth factor (VEGF) Enhances angiogenesis
16,39,73
Fibroblast growth factor (FGF) Enhances angiogenesis
73
Epithelial cell growth factor (ECGF) Stimulates endothelial chemotaxis and promotes angiogenesis
16,39
Platelet-derived angiogenic factor (PDAF) Promotes mitogenesis of endothelial cells
Enhances angiogenesis
39
Platelet factor 4 (PF4) Promotes chemotaxis for fibroblasts and monocytes
Inhibits collagenase
39
Platelet-derived endothelial growth factor Stimulates mitogenesis of endothelial cells and keratinocytes
39
(PDEGF)
Hepatocyte growth factor (HGF) Enhances angiogenesis
Inhibits fibrosis
73
Insulin-like growth factor (IGF) Stimulates osteoblast proliferation
Enhances matrix synthesis
39,72
Fibrin Cell adhesion
Fibronectin Thrombus formation
Vitronectin Mitogenesis
Thrombospondin-1 (TSP-1) Hemostasis
39,74
Osteocalcin (Oc) Mineralization
39
Osteonectin (On)
Interleukin-1 (IL-1) Activates growth factor expression in macrophages, fibroblasts,
and keratinocytes
24,31
Complement Antimicrobial
74
Serotonin Primary hemostasis
74
Fibrinogen
Catecholamines
Adenosine Diphosphate (ADP)
Adenosine Triphosphate (ATP)
Factor V
Von Willebrand factor VIII
Thromboxane A2
Calcium
Tabl e 1 Growth factors and other components
of platelet-rich plasma that contribute to wound healing
Bashutski.qxd 4/15/08 2:13 PM Page 475
COPYRIGHT 2008 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO
PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER
QUI NTESSENCE I NTERNATI ONAL
Bashut ski /Wang
secreted by platelets. Both play key roles in
angiogenesis and fibroblast cell differentia-
tion and are consequently very important in
the wound healing process. Optimizing the
blood supply to the newly covered root sur-
face could theoretically allow for a greater
percentage of root coverage and better soft
tissue graft acceptance rates. Attaining an
adequate blood supply could be particularly
useful in gaining coverage of deep and wide
recession defects or in minimizing sloughing
where a large soft tissue graft is being
placed.
15
GRAFT ACCEPTANCE
AND WOUND STABILITY
PRP may play a particularly important role in
soft tissue grafting procedures. Compellingly,
the addition of PRP improves graft adhesion
and minimizes micromovement, providing
the most advantageous environment for graft
acceptance.
36,37
PRP also increases early wound
strength
34,35
through a variety of mecha-
nisms, which would help stabilize the posi-
tion of a coronally advanced flap or ensure
476 VOLUME 39 NUMBER 6 JUNE 2008
Promote angiogenesis
32
Stimulate granulation tissue formation
33
Decrease inflammatory phase of wound healing
34
Increase collagen content
34,32
Increase early glycosaminoglycan (GAG) and fibronectin deposition
34
Increase early wound strength
34,35
Enhance initial epithelial migration
15
Improve hemostasis
36,37
Tabl e 2 Mechanisms by which PRP may enhance soft tissue healing
Increased time of procedure
Increased cost for equipment
Knowledge of phlebotomy required
Technique sensitive
38
A platelet count within a narrow range must be achieved for optimal results
39
Lack of long-term data and controlled trials to support efficacy
Tabl e 3 Disadvantages of PRP in root-coverage procedures
Platelet-rich plasma
Increased
vascularity
Increased
wound stability
Increased
esthetics
42
Increased
regeneration
potiential
40,43,45
Decreased
patient morbidity
Reduced tissue
sloughing
26
Improved
healing
26,40
Improved wound
closure
15,34,36,41
Enhanced graft
adhesion
37
Reduced micro-
movement of graft
36
Increased tissue
thickness
26
Reduced
scarring
22,40,43,44
Increased healing
rate
27,40,46,47
Improved
hemostasis
36,37
Minimized immune
response
26,49
Decreased infections
Fig 1 Advantages of PRP in root-coverage procedures.
Bashutski.qxd 4/15/08 2:13 PM Page 476
COPYRIGHT 2008 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO
PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER
VOLUME 39 NUMBER 6 JUNE 2008 477
QUI NTESSENCE I NTERNATI ONAL
Bashut ski /Wang
soft tissue graft acceptance. This early
wound strength results from the ability of
PRP to decrease the inflammatory phase of
wound healing and to increase collagen con-
tent and early deposition of glycosaminoglycan
and fibronectin.
34
ESTHETIC OUTCOMES
Increased graft acceptance rates, a greater
percentage of root coverage, decreased
healing time, and less sloughing of grafts
would all contribute to better esthetics, both
short term and long term. It has been sug-
gested that PRP can also increase tissue
thickness after root coverage,
15,38
thereby
improving esthetics and preventing relapse
of the recession since increased flap thick-
ness has been correlated with better out-
comes in root-coverage procedures.
50
One
study comparing a coronally advanced flap
to a coronally advanced flap with PRP
showed a trend toward greater tissue thick-
ness in the presence of PRP, although the
study lacked sufficient power to detect a sig-
nificant difference (P = .1).
38
To date, the abil-
ity of PRP to enhance tissue thickness in soft
tissue grafting procedures has not been eval-
uated, nor has any mechanism been pro-
posed for the observed increase in tissue
thickness in the above study. This potential
benefit of PRP in root-coverage procedures
requires further investigation, although it
shows promise. The present authors have
experienced and shown
38
that PRP can
enhance vascularity (due to release of vascu-
lar endothelial growth factors
24
) and promote
graft adhesion and wound stability.
Nonetheless, these clinical effects do not
translate in enhancing percentage of root
coverage or in promoting esthetic outcome
when compared to sites treated without PRP.
If vertical incisions are used during root-
coverage procedures, potential scarring of
the mucosa can be an esthetic concern,
especially in patients with a high lip line. PRP
may contribute to improved esthetics by min-
imizing this scar formation.
22,4244
Monteleone
assessed the ability of PRP to accelerate soft
tissue wound healing and epithelialization of
a split-thickness skin graft donor site.
44
In this
study, 20 patients with side-by-side split-thick-
ness graft donor sites were treated with either
topical bovine thrombin or PRP in addition
to an occlusive dressing. Wounds were eval-
uated by direct observation, photographic
morphometry, and some histopathology
specimens; patient pain was also evaluated
using a discomfort scale. Accelerated wound
maturity and epithelialization and decreased
scar formation were noted in the PRP group
compared to the control group. Furthermore,
patients in the PRP group reported less pain
and annoyance.
The possible mechanism behind de-
creased scarring may be twofold. First, accel-
erated wound maturation minimizes the
amount of time granulation tissue is present
in the surgical site. Granulation tissue forma-
tion occurs in the proliferative stage of
wound healing and contains collagen that is
less organized and thinner than uninjured tis-
sue.
51
It is necessary for wound healing, but
unless the collagen reorganizes, an unsightly
scar will form. Platelet-derived growth factor
and epidermal growth factor, which are both
present in PRP, are the main growth factors
involved in fibroblast migration, proliferation,
and collagen synthesis. Increased concen-
trations of these growth factors are likely the
reason for the accelerated wound healing,
which is suggested to be at least 2 to 3 times
faster than that of normal healing.
27
Second,
PRP contains hepatocyte growth factor,
which has powerful antifibrotic effects.
Hepatocyte growth factor has been shown to
reduce scar formation in various animal and
human studies.
5256
Furthermore, 1 study
suggested that hepatocyte growth factor may
even enhance dermal regeneration in addi-
tion to decreasing scar formation.
52
PRP con-
tains a higher concentration of all these
growth factors, which would explain the
increased rate of maturation and antifibrotic
effects leading to decreased scar formation.
Although the biologic rationale for decreas-
ing scar formation in root-coverage proce-
dures exists, this has yet to be proven in stud-
ies on gingival tissue.
Bashutski.qxd 4/15/08 2:13 PM Page 477
COPYRIGHT 2008 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO
PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER
478 VOLUME 39 NUMBER 6 JUNE 2008
QUI NTESSENCE I NTERNATI ONAL
Bashut ski /Wang
PATIENT MORBIDITY
Patient morbidity is also an important issue to
consider with root-coverage procedures.
There are several reports of PRP increasing
healing rates and decreasing postoperative
bleeding and pain.
23,27,42,44,46,47,48
Many of the
growth factors present in PRP enhance initial
epithelial migration, creating a more pre-
dictable soft tissue seal than with primary clo-
sure alone.
15,36
One author suggests that the
wound-healing process is accelerated with the
use of PRP, minimizing postoperative healing
time for patients and decreasing their morbid-
ity.
27
However, studies utilizing PRP for other
applications have revealed that PRP could not
enhance wound healing, bone remodeling, or
sinus augmentation.
57,58
Given that PRP has
failed to show promise in other applications,
the initially promising results reported in soft
tissue healing during root-coverage proce-
dures should be interpreted with caution until
more rigorous trials are conducted.
PRP has a pH of 6.5 to 6.7, which is low
compared to the pH of a mature blood clot
(7.0 to 7.2).
23
This lowered pH may inhibit
bacterial growth and therefore decrease
infection rates. Furthermore, several growth
factors present in PRP are chemotactic for
neutrophils, which would enhance the
bodys ability to combat a developing infec-
tion. However, Marx reported from his experi-
ence that there was no difference in infection
rates of PRP-treated bone grafts and skin
wounds compared with controls.
23
The inci-
dence of infection ranged between 2.0% and
3.5% for both groups.
Since PRP is autologous, there is a rela-
tively low risk of a negative immune reaction
and disease transmission in patients who
receive this product.
23,49
The only potential
concern with PRP is the bovine thrombin that
is frequently used to activate it. Several reports
of bleeding coagulopathies exist in the litera-
ture that were attributed to interactions with
bovine and human factor Va, a clotting factor
that binds activated platelets and is critical for
prothrombin activation, after PRP applica-
tion.
5961
However, within the past 10 years, the
amount of bovine factor Va has been signifi-
cantly reduced from 50.0 mg/mL to less than
0.2 mg/mL, thus reducing this complication.
61
REGENERATION
In the field of periodontics, tissue regenera-
tion is much preferred over tissue repair.
While PRP has been shown to accelerate the
wound-healing process and hasten repair, lit-
tle is known about its ability to regenerate the
soft tissues of the periodontium, although
some authors suggest that it may have this
potential.
27,28
Unfortunately, studies evaluat-
ing the ability of PRP to promote regenera-
tion in bone have shown that PRP actually
has a low regenerative potential.
62,63
A signif-
icant amount of data exists for the potential
of growth factors found in PRP to promote
regeneration.
40,6469
However, most of these
studies were performed using the growth
factors in isolation or in pairs, so it remains
unclear what modifying effects these factors
will have on each other.
Some evidence of synergistic effects of
different components of PRP has already
been reported in the literature.
70
One recent
study evaluated the effect of PRP itself on
human cell lines.
71
In this in vitro study, PRP
caused a marked increase in periodontal lig-
ament cell proliferation, a minor increase in
gingival fibroblast growth, and inhibition of
keratinocyte proliferation. Also, collagen and
alkaline phosphatase activity levels increased
in the presence of PRP, leading the authors
to conclude that PRP may promote regener-
ation by differentially regulating the cell types
of the periodontium. It is also important to
note that platelets may secrete many other
as-yet-unknown growth factors, which have
an unknown effect on the regenerative
potential of cells in the periodontium.
An advantage of using PRP is that numer-
ous growth factors are available in one product.
However, this also creates a disadvantage in
that the concentration of each growth factor
cannot be individually customized. In addi-
tion, the maximum concentration of growth
factors that can be obtained in a PRP prepa-
ration is not necessarily the most optimal
concentration. One recent study found that
fibroblast and osteoblast proliferation was
optimized using a 2.5 concentration of
PRP, but that further increases in concentra-
tion actually reduced this proliferative effect.
39
Similar observations were found by Weibrich
Bashutski.qxd 4/15/08 2:13 PM Page 478
COPYRIGHT 2008 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO
PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER
VOLUME 39 NUMBER 6 JUNE 2008 479
QUI NTESSENCE I NTERNATI ONAL
Bashut ski /Wang
and coworkers, who found that regeneration
of bone around implants placed into rabbit
femurs occurred only within a narrow, inter-
mediate range of PRP concentration.
72
Thus,
while further studies are still needed to
assess the ability of PRP to stimulate regen-
eration, it is already acknowledged that the
inherent nature of PRP may present chal-
lenges in this area because of the inability to
achieve optimal levels of each growth factor
with a single PRP concentration.
HUMAN ROOT-COVERAGE
STUDIES
Evaluation of PRP and its role in augmenting
root-coverage procedures is limited to 4 pub-
lished reports to date (Table 4). The first case
report using this technique was published in
2001, when Petrungaro used PRP as an
adjunct to traditional treatment of gingival
recession in 3 patients.
15
Two patients were
treated using connective tissue grafts, and 1
patient was treated using a barrier mem-
brane. Although complete root coverage was
only obtained in 1 case, the author acknowl-
edged that the gingival recession defects
were difficult to treat and that complete root
coverage was not an intended goal. Based
on the authors clinical observations, PRP
provided additional benefit to root-coverage
procedures by decreasing pain and bleed-
ing, increasing tissue thickness, enhancing
stabilization of the graft, decreasing infection
and graft sloughing, decreasing healing time,
and promoting revascularization. However, it
is important to note that this publication is a
case report and that the clinical observations
were subjective and nonquantitative. There-
fore, the evidence-based conclusions that
can be obtained from this study are limited
since no quantitative data was presented.
Griffin and Cheung used platelet-concen-
trate gel in a collagen sponge carrier as an
adjunct to a coronally advanced flap in the
treatment of gingival recession in 2 patients.
43
Author and year Study design Results Critique
Petrungaro, 2001
15
3 patients with multiple recession defects: 1/3 complete coverage, faster healing, Case report
2 PRP + SCTG less bleeding/pain, increased KG
1 PRP + GTR
Griffin and 2 patients PRP + CAF Complete root coverage at 6 m, faster Case report
Cheung, 2004
43
Platelet concentrate gel in sponge carrier healing, decreased inflammation, KG gain
Cheung and Randomized controlled trial 80% root coverage (60% CRC) in test 2/3 examiners were
Griffin, 2004
42
Miller Class I or II buccal recession in compared to 95% (65.5% CRC ) in inconsistent in
15 patients control color match test
Split-mouth design
SCTG or PCG
8-m follow-up
Huang et al, 2005
38
Randomized controlled trial 81.0% root coverage in CAF + PRP Only Miller Class 1
23 Miller Class I buccal recession defects group (63.6% CRC) compared to recessions used
CAF + PRP or CAF alone 83.5% (58.3% CRC) in the control Insufficient power to
24-w follow-up Trend toward lower WHI and GI scores detect a difference
in PRP group
(PRP) Platelet-rich plasma; (SCTG) subepithelial connective tissue graft; (GTR) guided tissue regeneration; (KG) keratinized gingiva; (CAF) coronally
advanced flap; (PCG) platelet-concentrate grafts; (CRC) complete root coverage; (WHI) Wound Healing Index; (GI) Gingival Index.
Tabl e 4 Publications evaluating the effects of PRP in root-coverage procedures
Bashutski.qxd 4/15/08 2:13 PM Page 479
COPYRIGHT 2008 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO
PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER
480 VOLUME 39 NUMBER 6 JUNE 2008
QUI NTESSENCE I NTERNATI ONAL
Bashut ski /Wang
The authors reported strikingly mature soft
tissue healing at 1 week, and decreased
inflammation, excellent tissue contour and
color, and complete root coverage at 6
months. In 1 patient, there was a 1.5-mm
gain in keratinized tissue. A lack of scar for-
mation was reported, despite vertical releas-
ing incisions in both cases. Again, the major
drawback to this publication is that it is a
case report where many of the observations
were not quantified.
A randomized controlled trial compared
the use of platelet-concentrate grafts (PCGs)
with subepithelial connective tissue grafts
(SCTGs) in Miller Class I or II buccal reces-
sion defects in 15 patients.
42
At 8 months,
80% root coverage (60% complete root
coverage) was achieved in the PCG group
compared to 95% (65.5% complete root cov-
erage) in the SCTG group, although this dif-
ference was not statistically significant.
Notably, the control group outperformed the
PCG group by 15%. In contrast, the PCG
group resulted in significantly shallower
probing depths (1.05 mm versus 1.79 mm).
Postsurgical discomfort levels were evaluat-
ed using a visual analog scale from 0 (no
pain) to 10 (most pain). The group treated
using PCGs had significantly less pain at 3
weeks, with a pain rating of 0.15 0.34 com-
pared to 0.59 0.78 in the SCTG group,
although it is questionable whether this dif-
ference is clinically significant. Finally, the
PCG group exhibited significant improve-
ments in soft tissue contour and texture com-
pared to controls. These findings were based
on the observations of 3 blinded examiners
who reviewed slides of the cases and scored
them twice using a subjective esthetic rating
of 1 (most favorable esthetics) to 4 (least
favorable esthetics).
Another study evaluated the effect of PRP
on the coronally advanced flap procedure.
38
In this randomized controlled trial, 23
patients with Miller Class I buccal recession
defects were treated with either PRP plus
coronally advanced flap or coronally
advanced flap alone and followed for 24
weeks postsurgery. Mean root coverage was
81.0% (63.6% complete root coverage) in the
coronally advanced flap plus PRP group
compared to 83.5% (58.3% complete root
coverage) in the control group, which was not
significantly different. PRP-treated recession
defects resulted in lower Gingival Index
73
scores, although this was not statistically sig-
nificant. A Wound Healing Index
38
was devel-
oped for this study, which scored the tissue
healing on a scale from 1 (uneventful healing)
to 3 (poor wound healing). At 2 weeks, the
PRP group had lower Wound Healing Index
scores than did controls, although this also
was not statistically significant and this effect
was no longer seen at 1 month. However, the
authors suggested that this lack of signifi-
cance may be due to small sample sizes and
the fact that only Miller Class I recession
defects were studied and these respond well
to most root-coverage techniques.
CONCLUSION
Using PRP as an adjunct to root-coverage pro-
cedures is a relatively new phenomenon,
although PRP has been used to promote
wound healing and hemostasis in medical
and dental applications for many years.
Specifically, PRP has been used most com-
monly in sinus augmentation procedures,
74
esthetic plastic surgery,
75
and spinal surgery.
76
Preliminary reports suggest that the potential
benefits of PRP in root-coverage procedures
may be improved esthetics, decreased patient
morbidity, and accelerated wound healing.
Further investigation of this technique is war-
ranted with larger sample sizes, more chal-
lenging defects, and histologic data to better
determine the value of PRP as an adjunct to
traditional root-coverage procedures. At this
point, sufficient long-term evidence and rigor-
ous clinical studies to support the use of PRP
for this purpose are lacking. Although PRP
may show promise in this area, there is insuffi-
cient evidence to support its use at this time.
ACKNOWLEDGMENT
This work was partially supported by the University of
Michigan Periodontal Graduate Student Research Fund.
Bashutski.qxd 4/15/08 2:13 PM Page 480
COPYRIGHT 2008 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO
PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER
VOLUME 39 NUMBER 6 JUNE 2008 481
QUI NTESSENCE I NTERNATI ONAL
Bashut ski /Wang
REFERENCES
1. Kassab MM, Cohen RE. The etiology and prevalence
of gingival recession. J Am Dent Assoc 2003;134:
220225.
2. Langer B, Langer L. Subepithelial connective tissue
graft technique for root coverage. J Periodontol
1985;56:715720.
3. Restrepo OJ. Coronally repositioned flap: Report of
four cases. J Periodontol 1973;44:564567.
4. Tarnow DP. Semilunar coronally repositioned flap. J
Clin Periodontol 1986;13:182185.
5. Grupe H, Warren R. Repair of gingival defects by a
sliding flap operation. J Periodontol 1956;27:
290295.
6. Cohen DW, Ross SE. The double papillae reposi-
tioned flap in periodontal therapy. J Periodontol
1968;39:6570.
7. Nabers JM. Free gingival grafts. Periodontics 1966;
4:243245.
8. Mahn DH. Esthetic correction of gingival recession
using a modified tunnel technique and an acellular
dermal connective tissue allograft. J Esthet Restor
Dent 2002;14:1823.
9. Harris RJ. Cellular dermal matrix used for root cov-
erage: 18-month follow-up observation. Int J
Periodontics Restorative Dent 2002;22:156163.
10. Pini Prato G, Clauser C, Cortellini P,Tinti C, Vincenzi G,
Pagliaro U. Guided tissue regeneration versus
mucogingival surgery in the treatment of human
buccal recessions. A 4-year follow-up study. J
Periodontol 1996;67:12161223.
11. Tinti C, Vincenzi G, Cortellini P, Pini Prato G, Clauser
C. Guided tissue regeneration in the treatment of
human facial recession. A 12-case report. J
Periodontol 1992;63:554560.
12. Wang HL, Pappert TD, Castelli WA, Chiego DJ Jr, Shyr
Y, Smith BA. The effect of platelet-derived growth
factor on the cellular response of the periodontium:
An autoradiographic study on dogs. J Periodontol
1994;65:429436.
13. Roccuzzo M, Bunino M, Needleman I, Sanz M.
Periodontal plastic surgery for treatment of local-
ized gingival recessions: A systematic review. J Clin
Periodontol 2002;29(suppl 3):178194.
14. Clauser C, Nieri M, Franceschi D, Pagliaro U, Pini-
Prato G. Evidence-based mucogingival therapy. Part
2: Ordinary and individual patient data meta-analy-
ses of surgical treatment of recession using com-
plete root coverage as the outcome variable. J
Periodontol 2003;74:741756.
15. Petrungaro PS. Using platelet-rich plasma to accel-
erate soft tissue maturation in esthetic periodontal
surgery. Compend Contin Educ Dent 2001;22:
729732, 734, 736 passim.
16. de Sanctis M, Zucchelli G. Coronally advanced flap:
A modified surgical approach for isolated reces-
sion-type defects: Three-year results. J Clin
Periodontol 2007;34:262268.
17. Spahr A, Haegewald S, Tsoulfidou F, et al. Coverage
of Miller class I and II recession defects using enam-
el matrix proteins versus coronally advanced flap
technique: A 2-year report. J Periodontol 2005;76:
18711880.
18. Wennstrom JL. Mucogingival therapy. Ann Perio-
dontol 1996;1:671701.
19. Greenwell H, Bissada NF, Henderson RD, Dodge JR.
The deceptive nature of root coverage results. J
Periodontol 2000;71:13271337.
20. Al-Hamdan K, Eber R, Sarment D, Kowalski C, Wang
HL. Guided tissue regeneration-based root coverage:
Meta-analysis. J Periodontol 2003;74:15201533.
21. Trombelli L. Periodontal regeneration in gingival
recession defects. Periodontol 2000 1999;19:
138150.
22. Anitua E, Sanchez M, Nurden AT, Nurden P, Orive G,
Andia I. New insights into and novel applications for
platelet-rich fibrin therapies. Trends Biotechnol
2006;24:227234.
23. Marx RE. Platelet-rich plasma: Evidence to support
its use. J Oral Maxillofac Surg 2004;62:489496.
24. Pietrzak WS, Eppley BL. Platelet rich plasma: Biology
and new technology. J Craniofac Surg 2005;16:
10431054.
25. Roukis TS, Zgonis T, Tiernan B. Autologous platelet-
rich plasma for wound and osseous healing: A
review of the literature and commercially available
products. Adv Ther 2006;23:218237.
26. Petrungaro P. Platelet-rich plasma for dental
implants and soft-tissue grafting. Interview by Arun
K. Garg. Dent Implantol Update 2001;12:4146.
27. Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR,
Strauss JE, Georgeff KR. Platelet-rich plasma: Growth
factor enhancement for bone grafts. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod 1998;85:638646.
28. Cochran DL, Wozney JM. Biological mediators for
periodontal regeneration. Periodontol 2000 1999;
19:4058.
29. Grageda E. Platelet-rich plasma and bone graft
materials: A review and a standardized research
protocol. Implant Dent 2004;13:301309.
30. Distler JH, Hirth A, Kurowska-Stolarska M, Gay RE,
Gay S, Distler O. Angiogenic and angiostatic factors
in the molecular control of angiogenesis. Q J Nucl
Med 2003;47:149161.
31. Broughton G 2nd, Janis JE, Attinger CE. Wound heal-
ing: An overview. Plast Reconstr Surg 2006;117
(suppl):1e-S32e-S.
32. Green DM, Klink B. Platelet gel as an intraoperative-
ly procured platelet-based alternative to fibrin glue.
Plast Reconstr Surg 1998;101:11611162.
33. Mustoe TA, Pierce GF, Morishima C, Deuel TF. Growth
factorinduced acceleration of tissue repair
through direct and inductive activities in a rabbit
dermal ulcer model. J Clin Invest 1991;87:694703.
Bashutski.qxd 4/15/08 2:13 PM Page 481
COPYRIGHT 2008 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO
PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER
482 VOLUME 39 NUMBER 6 JUNE 2008
QUI NTESSENCE I NTERNATI ONAL
Bashut ski /Wang
34. Pierce GF, Tarpley JE, Yanagihara D, Mustoe TA, Fox
GM,Thomason A. Platelet-derived growth factor (BB
homodimer), transforming growth factor-beta 1,
and basic fibroblast growth factor in dermal wound
healing. Neovessel and matrix formation and cessa-
tion of repair. Am J Pathol 1992;140:13751388.
35. Murray MM, Spindler KP, Devin C, et al. Use of a col-
lagenplatelet rich plasma scaffold to stimulate
healing of a central defect in the canine ACL. J
Orthop Res 2006;24:820830.
36. Whitman DH, Berry RL, Green DM. Platelet gel: An
autologous alternative to fibrin glue with applica-
tions in oral and maxillofacial surgery. J Oral
Maxillofac Surg 1997;55:12941299.
37. Carlson NE, Roach RB Jr. Platelet-rich plasma: Clinical
applications in dentistry. J Am Dent Assoc 2002;
133:13831386.
38. Huang LH, Neiva RE, Soehren SE, Giannobile WV,
Wang HL. The effect of platelet-rich plasma on the
coronally advanced flap root coverage procedure: A
pilot human trial. J Periodontol 2005;76:17681777.
39. Graziani F, Ivanovski S, Cei S, Ducci F, Tonetti M,
Gabriele M. The in vitro effect of different PRP con-
centrations on osteoblasts and fibroblasts. Clin Oral
Implants Res 2006;17:212219.
40. Park JB, Matsuura M, Han KY, et al. Periodontal
regeneration in class III furcation defects of beagle
dogs using guided tissue regenerative therapy with
platelet-derived growth factor. J Periodontol 1995;
66:462477.
41. Anitua E. Plasma rich in growth factors: Preliminary
results of use in the preparation of future sites for
implants. Int J Oral Maxillofac Implants 1999;14:
529535.
42. Cheung WS, Griffin TJ. A comparative study of root
coverage with connective tissue and platelet con-
centrate grafts: 8-month results. J Periodontol 2004;
75:16781687.
43. Griffin TJ, Cheung WS. Treatment of gingival reces-
sion with a platelet concentrate graft: A report of
two cases. Int J Periodontics Restorative Dent 2004;
24:589595.
44. Monteleone K, Marx RE, Ghurani R. Wound
repair/Cosmetic surgery healing enhancement of
skin graft donor sites with platelet-rich plasma
(PRP). Presented at the 82nd Annual American
Academy of Oral and Maxillofacial Surgery Meeting,
San Francisco, 2000.
45. Anitua E, Sanchez M, Nurden AT, et al. Autologous
fibrin matrices: A potential source of biological
mediators that modulate tendon cell activities. J
Biomed Mater Res A 2006;77:285293.
46. Anitua E, Andia I, Ardanza B, Nurden P, Nurden AT.
Autologous platelets as a source of proteins for
healing and tissue regeneration. Thromb Haemost
2004;91:415.
47. Garg AK. The use of platelet-rich plasma to enhance
the success of bone grafts around dental implants.
Dent Implantol Update 2000;11:1721.
48. Mancuso JD, Bennion JW, Hull MJ, Winterholler BW.
Platelet-rich plasma: A preliminary report in routine
impacted mandibular third molar surgery and the
prevention of alveolar osteitis. J Oral Maxillofac
Surg 2003;61:40.
49. Ogino Y, Ayukawa Y, Tsukiyama Y, Koyano K. The
effect of platelet-rich plasma on the cellular
response of rat bone marrow cells in vitro. Oral Surg
Oral Med Oral Pathol Oral Radiol Endod 2005;100:
302307.
50. Hwang D, Wang HL. Flap thickness as a predictor of
root coverage: A systematic review. J Periodontol
2006;77:16251634.
51. Forrest L. Current concepts in soft connective tissue
wound healing. Br J Surg 1983;70:133140.
52. Ono I, Yamashita T, Hida T, et al. Local administration
of hepatocyte growth factor gene enhances the
regeneration of dermis in acute incisional wounds.
J Surg Res 2004;120:4755.
53. Ha X, Li Y, Lao M, Yuan B, Wu CT. Effect of human
hepatocyte growth factor on promoting wound
healing and preventing scar formation by aden-
ovirus-mediated gene transfer. Chin Med J (Engl)
2003;116:10291033.
54. Herrero-Fresneda I, Torras J, Franquesa M, et al. HGF
gene therapy attenuates renal allograft scarring by
preventing the profibrotic inflammatory-induced
mechanisms. Kidney Int 2006;70:265274.
55. Tarnawski AS. Cellular and molecular mechanisms
of gastrointestinal ulcer healing. Dig Dis Sci 2005;50
(suppl 1):S2433.
56. Tarnawski A. Molecular mechanisms of ulcer heal-
ing. Drug News Perspect 2000;13:158168.
57. Thor A, Wannfors K, Sennerby L, Rasmusson L.
Reconstruction of the severely resorbed maxilla
with autogenous bone, platelet-rich plasma, and
implants: 1-year results of a controlled prospective
5-year study. Clin Implant Dent Relat Res 2005;
7:209220.
58. Raghoebar GM, Schortinghuis J, Liem RS, Ruben JL,
van der Wal JE, Vissink A. Does platelet-rich plasma
promote remodeling of autologous bone grafts
used for augmentation of the maxillary sinus floor?
Clin Oral Implants Res 2005;16:349356.
59. Cmolik BL, Spero JA, Magovern GJ, Clark RE. Redo
cardiac surgery: Late bleeding complications from
topical thrombin-induced factor V deficiency. J
Thorac Cardiovasc Surg 1993;105:222227.
60. Muntean W, Zenz W, Finding K, Zobel G, Beitzke A.
Inhibitor to factor V after exposure to fibrin sealant
during cardiac surgery in a two-year-old child. Acta
Paediatr 1994;83:8487.
61. Christie RJ, Carrington L, Alving B. Postoperative
bleeding induced by topical bovine thrombin:
Report of two cases. Surgery 1997;121:708710.
62. Sanchez AR, Sheridan PJ, Eckert SE, Weaver AL.
Regenerative potential of platelet-rich plasma
added to xenogenic bone grafts in peri-implant
defects: A histomorphometric analysis in dogs. J
Periodontol 2005;76:16371644.
Bashutski.qxd 4/15/08 2:13 PM Page 482
COPYRIGHT 2008 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO
PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER
VOLUME 39 NUMBER 6 JUNE 2008 483
QUI NTESSENCE I NTERNATI ONAL
Bashut ski /Wang
63. Casati MZ, de Vasconcelos Gurgel BC, Goncalves PF,
et al. Platelet-rich plasma does not improve bone
regeneration around peri-implant bone defectsA
pilot study in dogs. Int J Oral Maxillofac Surg
2007;36:132136.
64. Lynch SE, Buser D, Hernandez RA, et al. Effects of the
platelet-derived growth factor/insulin-like growth
factor-I combination on bone regeneration around
titanium dental implants. Results of a pilot study in
beagle dogs. J Periodontol 1991;62:710716.
65. Lynch SE, Williams RC, Polson AM, et al. A combina-
tion of platelet-derived and insulin-like growth fac-
tors enhances periodontal regeneration. J Clin
Periodontol 1989;16:545548.
66. Rutherford RB, Niekrash CE, Kennedy JE, Charette
MF. Platelet-derived and insulin-like growth factors
stimulate regeneration of periodontal attachment
in monkeys. J Periodontal Res 1992;27:285290.
67. Cho MI, Lin WL, Genco RJ. Platelet-derived growth
factormodulated guided tissue regenerative ther-
apy. J Periodontol 1995;66:522530.
68. Giannobile WV, Hernandez RA, Finkelman RD, et al.
Comparative effects of platelet-derived growth
factor-BB and insulin-like growth factor-I, individu-
ally and in combination, on periodontal regenera-
tion in Macaca fascicularis. J Periodontal Res 1996;
31:301312.
69. Giannobile WV, Finkelman RD, Lynch SE.
Comparison of canine and non-human primate ani-
mal models for periodontal regenerative therapy:
Results following a single administration of PDGF/
IGF-I. J Periodontol 1994;65:11581168.
70. Strayhorn CL, Garrett JS, Dunn RL, Benedict JJ,
Somerman MJ. Growth factors regulate expression
of osteoblast-associated genes. J Periodontol 1999;
70:13451354.
71. Annunziata M, Oliva A, Buonaiuto C, et al. In vitro
cell-type specific biological response of human
periodontally related cells to platelet-rich plasma. J
Periodontal Res 2005;40:489495.
72. Weibrich G, Hansen T, Kleis W, Buch R, Hitzler WE.
Effect of platelet concentration in platelet-rich plas-
ma on peri-implant bone regeneration. Bone
2004;34:665671.
73. Loe H. The Gingival Index, the Plaque Index and the
Retention Index Systems. J Periodontol 1967;38
(suppl):610616.
74. Boyapati L, Wang HL. The role of platelet-rich plas-
ma in sinus augmentation: A critical review. Implant
Dent 2006;15:160170.
75. Bhanot S, Alex JC. Current applications of platelet
gels in facial plastic surgery. Facial Plast Surg
2002;18:2733.
76. Bose B, Balzarini MA. Bone graft gel: Autologous
growth factors used with autograft bone for lumbar
spine fusions. Adv Ther 2002;19:170175.
Bashutski.qxd 4/15/08 2:13 PM Page 483
COPYRIGHT 2008 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO
PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- NCP Cholecystectomy RevisedDocument7 pagesNCP Cholecystectomy RevisedMariquita Buenafe100% (4)
- Subdural HematomaDocument52 pagesSubdural HematomaanjarwatiNo ratings yet
- Health System Nutrition and DietDocument2 pagesHealth System Nutrition and DietMikaela LaoNo ratings yet
- Test Bank For Laboratory Manual For Seeleys Anatomy Physiology 11th Edition Eric Wise 3 DownloadDocument69 pagesTest Bank For Laboratory Manual For Seeleys Anatomy Physiology 11th Edition Eric Wise 3 Downloadcaseyyoungtoekwmcfdi100% (30)
- Denoising of ECG Signal For Detection and Classification of Arrhythmia in On-Line Patient MonitoringDocument31 pagesDenoising of ECG Signal For Detection and Classification of Arrhythmia in On-Line Patient MonitoringPratik SinghNo ratings yet
- Saudi Board of General Surgery Final Exam, November 2009 PDFDocument47 pagesSaudi Board of General Surgery Final Exam, November 2009 PDFRahmah Shah Bahai100% (2)
- The Nasal Septum PDFDocument18 pagesThe Nasal Septum PDFalit100% (1)
- Kimia KlinikDocument1 pageKimia KlinikOldi JunizarNo ratings yet
- Presentation CVADocument43 pagesPresentation CVAHenk Kraaijenhof100% (3)
- CollagenaseDocument3 pagesCollagenaseThivia RajNo ratings yet
- 20 Literasi Bahasa InggrisDocument14 pages20 Literasi Bahasa Inggriskeysakeysa739No ratings yet
- Use and Limitations of in Vitro Dissolution Testing: Topic Introduction and OverviewDocument114 pagesUse and Limitations of in Vitro Dissolution Testing: Topic Introduction and OverviewMuthu Venkatesh100% (1)
- ThrombocytopeniaDocument49 pagesThrombocytopeniaMaria EnjelinaNo ratings yet
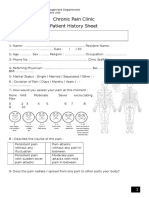
- Chronic Pain Clinic Patient History SheetDocument4 pagesChronic Pain Clinic Patient History SheetBelal N. MahfouzNo ratings yet
- Alpina, Eurycoma Longifolia, and Curcuma Xanthorrhiza) Increases Number and ImprovesDocument6 pagesAlpina, Eurycoma Longifolia, and Curcuma Xanthorrhiza) Increases Number and ImprovesedwardNo ratings yet
- Gordon's FormDocument6 pagesGordon's FormHarry AglugobNo ratings yet
- Breathing TheoryDocument3 pagesBreathing TheoryNicolás LowryNo ratings yet
- Central DogmaDocument50 pagesCentral DogmaIvilyn ManguladNo ratings yet
- Drop MethodDocument2 pagesDrop MethodCharlene Bularan100% (2)
- Pancuronium: "Pavulon - Bromurex"Document33 pagesPancuronium: "Pavulon - Bromurex"Bahaa ShaabanNo ratings yet
- The Healing Power of HumorDocument3 pagesThe Healing Power of HumorJuan Daniel Yanqui GuerreroNo ratings yet
- BP201TPDocument1 pageBP201TPDarshanNo ratings yet
- 5ykgogrgmtd3pwbpedotjsidDocument10 pages5ykgogrgmtd3pwbpedotjsidKartik SharmaNo ratings yet
- Flow Sheet TemplateDocument4 pagesFlow Sheet TemplateIulia Tania AndronacheNo ratings yet
- Heart MurmursDocument7 pagesHeart MurmursOffvb MednuNo ratings yet
- Silverthorne 2018-Learning by Osmosis An Approach To Teaching Osmolarity and TonicityDocument10 pagesSilverthorne 2018-Learning by Osmosis An Approach To Teaching Osmolarity and TonicityIlham NugrohoNo ratings yet
- Adrenocortical AgentsDocument14 pagesAdrenocortical AgentsFredie O HadjimudinNo ratings yet
- Answers: CHAPTER 1 Stimuli and ResponsesDocument22 pagesAnswers: CHAPTER 1 Stimuli and Responses林柄洲No ratings yet
- Citrate Anticoagulation During CRRTDocument12 pagesCitrate Anticoagulation During CRRTpmunizNo ratings yet
- IronGAINS How To Get Strong & Muscular - Ebook 1st Edition - CompressedDocument289 pagesIronGAINS How To Get Strong & Muscular - Ebook 1st Edition - CompressedJames Khanso100% (1)