Professional Documents
Culture Documents
8
8
Uploaded by
Aurora KumikoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
8
8
Uploaded by
Aurora KumikoCopyright:
Available Formats
Clinical, Cosmetic and Investigational Dermatology
Open Access Full Text Article
Dovepress
open access to scientic and medical research
R apid C omm U N icatio N
Application and tolerability of Herpotherm in the treatment of genital herpes
This article was published in the following Dove Press journal: Clinical, Cosmetic and Investigational Dermatology 4 June 2013 Number of times this article has been viewed
Gerrit Schlippe 1 Werner Voss 1 Lars Christian Brenn 2
Dermatest Medical Research Company, Mnster, Germany; 2 RIEMSER Pharma GmbH, Greifswald, Germany
1
Abstract: Genital herpes is the manifestation of a herpes simplex virus 2infection. Standard treatment uses both local and systemic approaches. Here, we report on the results of a local therapy approach with 31 female patients at a gynecological practice. In the here-described approach, established genital herpes infection was treated with the medical device Herpotherm, with or without virostatic drugs. Herpotherm is a certied medical device operating on the basis of local heat application. Parameters evaluated during the approach were (i) subjective patient assessments and (ii) objective assessment of the physician. In the described therapy approach a positive effect in terms of nature and severity in the course of the disease using Herpotherm could be demonstrated. It could be shown that Herpotherm can also be used for genital herpes and that it is well tolerated. In relation to other therapies using topical treatment for genital herpes, an extremely rapid reduction of pain and herpetic symptoms could be observed. Intolerances or discontinued use as a result of complications were not observed. Keywords: herpes simplex virus, local heat, virostatic
Introduction
Herpes simplex virus (HSV) and human herpes virus (HHV) infections are very common among the general population. With a prevalence of up to 95%, HSV type 1 infection is more common than HSV type 2 infection. The latter is the principal pathogenic cause of genital herpes, which has a prevalence of approx. 3%60%, depending on the patient cohort examined.13 In industrial nations, however, genital herpes infection is increasingly triggered by HSV type 1infection. HSV is transmitted by droplet infection, via micro-lesions. It is then absorbed into epithelial cells, where the virus replicates. By destroying the host cells, virions are released and the disease is spread. Once the virus reaches the nerve endings of sensory neurons, it is endocytosed and transported to the cell body via cellular transport mechanisms.4 The virus persists lifelong in the ganglia, and even after symptoms have completely disappeared it can trigger a relapse of the HSV infection through factors such as impairment of the immune system due to febrile infection.5 Initial infection may be symptom-free. Over the course of time blisters and ulcers can appear, indicating tissue destruction and an inflammatory reaction. In immunosuppressed patients and occasionally in healthy patients, the viruses can spread via the lymphatic system and affect organs, which is often fatal.3 The exudate from the blisters contains an extremely high concentration of the virus.6 A relapse of genital herpes can manifest itself clinically in the form of unnoticed, small red spots up to extremely painful blistering of genital skin and mucous membranes.
Clinical, Cosmetic and Investigational Dermatology 2013:6 163166 163 2013 Schlippe etal, publisher and licensee Dove Medical Press Ltd. This is an Open Access article which permits unrestricted noncommercial use, provided the original work is properly cited.
Correspondence: Lars Christian Brenn RIEMSER Pharma GmbH, An der Wiek 7, 17493 Greifswald Insel Riems, Germany Tel+49 38 3517 6677 Fax+49 38 3517 6778 Email brenn@riemser.com
submit your manuscript | www.dovepress.com
Dovepress
http://dx.doi.org/10.2147/CCID.S41145
Schlippe etal
Dovepress
The blisters are typically round in shape, vary in their size, and appear either alone or in groups.3 The overall healing time for a genital herpes relapse has a large interindividual variability with 5 to 10days on average.3,7 The affected skin and mucous membrane areas are particularly stressed during the various stages of the blister-forming process (blistering/vesicular phase, wound/ulceration phase, incrustation and healing). Up to now, treatment of genital herpes involves the systemic administration of antiviral substances such as aciclovir, famciclovir or valaciclovir.812 Since it was shown that Herpotherm can shorten the duration of lip herpes and prevent recurrences when used early in the course of the disease,13 a local therapy approach was conducted at a gynecological practice in order to see whether this holds true for genital herpes infections also. The treatment of herpes with Herpotherm takes place with the help of a concentrated heat in the range of 51C53C which, when applied at the proper time, prevents the formation of the blisters and allows further symptoms (prickly sensation, burns, itchiness, feeling of tightness, pain) to subside quickly. Through the heating of the cells infected with the herpes virus, a total or partial denaturing of the enzymes or proteins can be achieved. The reproduction of the virus is thereby prevented and the development of the lip
blisters can be stopped. In dermatological testing the formation of lip blisters was totally prevented in the test subjects by means of the correctly timed use of Herpotherm. When used later, Herpotherm causes a less serious cycle and/or an earlier subsidence of the symptoms.13
Patients and methods
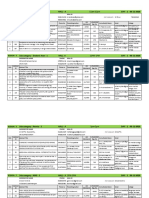
The local therapy approach was conducted at a single medical practice (Dr EN Kondrateva, Russia) from January 2007 to December 2008. Thirty-one female patients with established HSV infection aged 2349 years (mean 35) were treated in the therapy. All patients had, at baseline, signicant clinically detectable genital herpes symptoms. Twenty-one (68%) patients received Herpotherm (RIEMSER Pharma GmbH, Greifswald, Germany) treatment plus virostatic medication (aciclovir, [Valenta Pharmaceutica JSC, Russia] and Cycloferon, [NTFF Polysan, St Petersburg, Russia]). Ten (32%) patients were treated with Herpotherm only. Treatment was based on the decision of the attending physician and assessed using questionnaires lled in by patients and the physician in each visit. Five visits were individually scheduled in order to assess the genital herpes outbreaks over time (Figure1). Therapy starting point was dened by initial application of the Herpotherm after physical examination on
100
Days
II III IV
10
V Relapse
1 0 5 10 15 20 25 30
Patients
Figure1 Five visits were individually scheduled. Notes: Roman numbers indicate visits 2 to 5. Visit 1 (day 0) is not shown, treatment started on day 1. Visit 2 was scheduled on day 1; visit 3 on day 2 to 3; visit 4 on day 3 to 17 and visit 5 on day 8270. The four relapses are indicated. Arrows indicate patients treated with Herpotherm only; all other patients received Herpotherm plus virostatic treatment.
164
submit your manuscript | www.dovepress.com
Clinical, Cosmetic and Investigational Dermatology 2013:6
Dovepress
Dovepress
Herpotherm in the treatment of genital herpes
day 1 (visit 2). Herpotherm was used either once or several times a day. Treatment (Herpotherm and virostatic medication) was self-administered until condition had improved, or for about 5days. The mode of action of Herpotherm is based on a local and time-limited thermal stress of a defined skin area, by applying a microprocessor controlled temperature of 51C53C for 4seconds.
Results
Diagnosis of the genital herpes was conrmed during the rst visit (day 0). Vesicles and/or ulcers of varying intensity were already evident in all of the patients at that time. Accordingly, the disease had already broken out. Treatment was started irrespective of disease stage. The second visit took place one day after the rst visit (day 1). At this time, 28 patients (90%) had vesicles, 24 (77%) had ulcers, and one patient (3%) had incrustation. Treatment began with this visit. At the third visit (day 23), vesicles had already broken down in 25 of the patients (81%), tissue inltration was reduced in two patients (6%) and exudate was reduced in one patient (3%). Incrustation was already evident in 29 patients (94%) and ulcers in 18 patients (58%). Twenty-nine patients reported a signicant reduction of pain, and one patient reported relief of an unpleasant feeling. One patient provided no information. At the fourth visit (day 3 to 17), pink consolidation in 30 patients (97%) was evident where the vesicles/ulcers had been, to be equated with wound-healing. One patient (3%) treated with Herpotherm and cycloferon still had scabs (Figure 2). Thirty patients said that they were no longer suffering from any complaints and only one patient reported continued discomfort. Visit ve took place at day 8 to 270. Relapse occurred in only four patients (13%), three of them were treated
30
with Herpotherm plus virostatic medication and one with Herpotherm only. All other patients were symptom-free at visit ve (Figure1). Subjective assessment through patients using Herpotherm plus virostatics revealed that eight patients (67%) observed immediate, three (25%) rapid, and one (8%) quick improvement of HPV symptoms. Patients treated with Herpotherm only reported in four cases (67%) an immediate and in two cases (33%) a rapid improvement of herpetic symptoms. Thirteen patients provided no information (Figure3). Only nine patients (29%) reported adverse events; four (13%) reported pain when they rst started using Herpotherm, and the other ve (16%) a general feeling of pain. The remaining 22 patients (71%) reported no adverse events. The physician rated treatment with Herpotherm in 28 (90%) patients as good and in the remaining three patients (10%) as satisfactory. Two of these three patients were treated with Herpotherm plus virostatic medication and one with Herpotherm only, all three of these patients suffered from a relapse of symptoms.
Discussion
In previous studies it could be shown that the medical device Herpotherm can prevent recurrences of lip herpes (appearance of prodromes) and have a positive effect on further symptoms (tingling, burning, itching, tightness, pain) when used at an early stage of the disease. It was shown that herpetic symptoms could be attenuated and disease duration shortened from typically 99.7 days to 1.85 days when applying local heat.13 The present local therapy approach indicates that Herpotherm can also be used for genital herpes and that it is well tolerated. In relation to other therapies using topical treatment for genital herpes, an extremely rapid reduction of pain on day 1 after the start of treatment as opposed to day 3414,15 can be highlighted.
70
Number of patients
25 20 15 10 5 0 Visit 2 Visit 3 Visit 4
Vesicles Ulcers Incrustation
60
% of each group
50 40 30 20 10 0 Immediate Rapid Quick
Herpotherm + virostatics Herpotherm only
Figure2 Improvement of herpetic symptoms from visit 2 to 4. Notes: The bars show the number of patients suffering from indicated herpetic symptoms, according to physicians assessment, n=31.
Figure3 Onset of improvement of herpetic symptoms. Notes: The bars show the percentage of patients who provided information about their subjective assessment of the time to onset of improvement, n=18.
submit your manuscript | www.dovepress.com
Clinical, Cosmetic and Investigational Dermatology 2013:6
Dovepress
165
Schlippe etal
Dovepress
The statements of the affected patients on the efcacy of Herpotherm support the conclusion that symptoms can be reduced; even at the stage of an existing relapse. According to the physician, the healing process of the patients treated with Herpotherm only was not protracted or subject to discomfort. The patients receiving virostatic therapy in addition to Herpotherm treatment appeared to have no therapeutic advantage. In general, shortening the course of the disease was not expected, since even an antiviral therapy can be expected to shorten the duration of illness by only one day on average (from 6 to 5 days) when administered after an outbreak.1012 In principle, it can be assumed that the application of Herpotherm upon the onset of prodromes and before symptoms appear, achieves results similar to those of lip herpes treatment, as both the disease course and the pathophysiology of genital herpes matches that of lip herpes. The underlying molecular biological mechanism of the physical therapy with Herpotherm remains unclear. Typical for herpes is the fact that relapse always occurs within the same areas of skin/mucosa innervated by the virus-infested nerves.3 The application of a local treatment therefore makes sense. Possible explanations for the mechanism of action refer, for example, to the activation of heat shock proteins (eg, HSP60), which are involved in regulating a number of proteins, including immunomodulatory proteins.16 It is thought that heat therapy possibly leads to accelerated local immune reactions, which counteract the intensity of a HSV relapse. It is also conceivable that, through heat therapy, a certain degree of denaturation in the affected cells prevents the formation of new virions. Based on the existing approach, further studies should be conducted in order to substantiate the results obtained from using Herpotherm in genital herpes.
Disclosure
G Schlippe and W Voss have received honoraria for consulting activities from RIEMSER Pharma GmbH. LC Brenn is an employee of RIEMSER Pharma GmbH. The authors report no other conicts of interest in this work.
References
Acknowledgments
We thank Florian Losch for revising the manuscript and Franziska Vo for expert assistance in preparing the manuscript.
1. Hellenbrand W, Thierfelder W, Mller-Pebody B, Hamouda O, Breuer T. Seroprevalence of herpes simplex virus type 1 (HSV-1) and type 2 (HSV-2) in former East and West Germany, 19971998. Eur J Clin Microbiol Infec Dis. 2005;24:131135. 2. Halioua B, Malkin JE. Epidemiology of genital herpes recent advances. Eur J Dermatol. 1999;9:177184. 3. Gupta R, Warren T, Wald A. Genital herpes. Lancet. 2007;370: 21272137. 4. Connolly SA, Jackson JO, Jardetzky TS, Longnecker R. Fusing structure and function: a structural view of the herpesvirus entry machinery. Nat Rev Microbiol. 2009;9:369381. 5. Steiner I, Kennedy PG. Herpes simplex virus latent infection in the nervous system. J Neurovirol. 1995;1:1929. 6. Daniels C, Legoff S, Notkins A. Shedding of infectious virus/antibody complexes from vesicular lesions of patients with recurrent herpes labialis. Lancet. 1975;306:524528. 7. Gross G. Herpes-simplex-Virus infektionen. Hautarzt. 2004;55: 818830. German. 8. Patel R, Alderson S, Geretti A, et al. European guideline for the management of genital herpes, 2010, International Journal of STD and AIDS 22, 2011:110. 9. Clinical Effectiveness Group (British Association for Sexual Health and HIV). National Guideline for the Management of Genital Herpes (2007). BASSH, Cheshire, UK. Available at http://www.bashh.org/ documents/115/115.pdf. Accessed May 9, 2012. 10. Chosidow O, Drouault Y, Garraffo R, Veyssier P. Valaciclovir as a single dose during prodrome of herpes facialis: a pilot randomized double-blind clinical trial. Br J Dermatol. 2003;148:142146. 11. Chosidow O, etal. Famciclovir vs aciclovir in immunocompetent patients with recurrent genital herpes infections: a parallel-groups, randomized, double-blind clinical trial. Br J Dermatol. 2001;144:818824. 12. Bavaro JB, Drolette L, Koelle DM, et al. One-day regimen of valacyclovir for treatment of recurrent genital herpes simplex virus 2infection. Sex Transm Dis. 2008;35:383386. 13. Schlippe G, Voss W, Bayer M, Bunge I. Neue Behandlungsmethode bei einem Herpes-labialis-Rezidiv. [New method of treatment for a herpes labialis recurrence]. derm Praktische Dermatologie. 2011;17:340342. German. 14. Kinghorn GR, Turner EB, Barton, Potter CW, Burke CA, Fiddian AP. Efcacy of topical acyclovir cream in rst and recurrent episodes of genital herpes. Antiviral Res. 1983;3:291301. 15. Corey L, Benedetti JK, Critchlow CW, etal. Double-blind controlled trial of topical acyclovir in genital herpes simplex virus infections. Am J Med. 1982;73:326334. 16. Quintana FJ, Cohen IR. The HSP60 immune system network. Trends Immunol. 2011;32:8995.
Clinical, Cosmetic and Investigational Dermatology
Publish your work in this journal
Clinical, Cosmetic and Investigational Dermatology is an international, peer-reviewed, open access, online journal that focuses on the latest clinical and experimental research in all aspects of skin disease and cosmetic interventions. All areas of dermatology will be covered; contributions will be welcomed from all clinicians and
Dovepress
basic science researchers globally. This journal is indexed on CAS. The manuscript management system is completely online and includes a very quick and fair peer-review system, which is all easy to use. Visit http://www.dovepress.com/testimonials.php to read real quotes from published authors.
Submit your manuscript here: http://www.dovepress.com/clinical-cosmetic-and-investigational-dermatology-journal
166
submit your manuscript | www.dovepress.com
Clinical, Cosmetic and Investigational Dermatology 2013:6
Dovepress
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5822)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Amlodipine Drug StudyDocument2 pagesAmlodipine Drug StudyJoseph Dann Enero Jr.100% (3)
- HIV - Begining of The End - SawleshwarkarDocument52 pagesHIV - Begining of The End - SawleshwarkarStevanus Bob Arvianto AlwieNo ratings yet
- Congenital Heart Surgery: The Appropriate Diagnosis Is Achieved byDocument9 pagesCongenital Heart Surgery: The Appropriate Diagnosis Is Achieved byprofarmahNo ratings yet
- 2EMT Wuchereriabancroft&BrugiamalayiDocument3 pages2EMT Wuchereriabancroft&BrugiamalayiMAKI REYESNo ratings yet
- Dermoscopy of Disorders of HypopigmentationDocument5 pagesDermoscopy of Disorders of HypopigmentationIJAR JOURNALNo ratings yet
- The English PresentationDocument16 pagesThe English PresentationKhalid QahtaniNo ratings yet
- Effective Hemodynamic Monitoring 2Document10 pagesEffective Hemodynamic Monitoring 2Shirley castañedaNo ratings yet
- Animal Viruses and HumansDocument201 pagesAnimal Viruses and HumansPetrisor GheorghiuNo ratings yet
- PeripheralDocument25 pagesPeripheralMans FansNo ratings yet
- Final Bio IADocument8 pagesFinal Bio IAVictor SERRANO100% (1)
- Procedure On Lumber PunctureDocument8 pagesProcedure On Lumber PunctureDimpal ChoudharyNo ratings yet
- UK Patient Metoclopramide Medication LeafletDocument3 pagesUK Patient Metoclopramide Medication Leafletmarisa apriliaNo ratings yet
- DOMINGO - OB RequirmentsDocument10 pagesDOMINGO - OB RequirmentsJick Esteva de VicenteNo ratings yet
- NCM-112-RESP (Sanaani, Nur-Fatima, M.) (Drug Study)Document2 pagesNCM-112-RESP (Sanaani, Nur-Fatima, M.) (Drug Study)Nur SetsuNo ratings yet
- Abdominal Distension: Common Causes: - (Five F'S) 1. 2. 3. 4. 5. History of Present Illness 1Document3 pagesAbdominal Distension: Common Causes: - (Five F'S) 1. 2. 3. 4. 5. History of Present Illness 1Maxamed DananNo ratings yet
- Acetaminophen Drug StudyDocument7 pagesAcetaminophen Drug StudyHugh Klied ItuhatNo ratings yet
- Boy With No BrainDocument3 pagesBoy With No BrainbdamitaNo ratings yet
- Ho Densium KuretaseDocument36 pagesHo Densium KuretaseGifford Adiel SantosoNo ratings yet
- HPE 113X - First Aid (Choking)Document6 pagesHPE 113X - First Aid (Choking)Doreen MasikaNo ratings yet
- ABSLI Income Shield Plan BrochureDocument8 pagesABSLI Income Shield Plan BrochureAlroy RajNo ratings yet
- Diabetic Foot UlcersDocument13 pagesDiabetic Foot UlcersShanmuga SundaramNo ratings yet
- Cornea PBLDocument15 pagesCornea PBLThomas ChapelNo ratings yet
- ETDRSDocument16 pagesETDRSAna Cecy AvalosNo ratings yet
- 2023 10 1 451 PDFDocument16 pages2023 10 1 451 PDFBeatriz Melo de Almeida100% (1)
- Free Paper Programme FinalDocument18 pagesFree Paper Programme FinalShiwali SinghNo ratings yet
- Elution and Adsorption TechniquesDocument23 pagesElution and Adsorption TechniquesBromance H.No ratings yet
- Clinical Practice Guidelines GS PIMSDocument86 pagesClinical Practice Guidelines GS PIMSDrvikash Singh100% (1)
- Clinical Examination and Management of Impairments in VariousDocument34 pagesClinical Examination and Management of Impairments in Variousmukesh pokharelNo ratings yet
- Physical Examination Related NutritionDocument40 pagesPhysical Examination Related NutritionYohan SamudraNo ratings yet
- Dinesh RamDocument1 pageDinesh RamchandanNo ratings yet