Professional Documents
Culture Documents
Uid 1776
Uid 1776
Uploaded by
IsaacJ22Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Uid 1776
Uid 1776
Uploaded by
IsaacJ22Copyright:
Available Formats
WOUND CULTURES PURPOSE Routine wound culture will be performed to isolate mainly aerobic and facultative anaerobic organisms
in superficial lesions and body fluids. Anaerobic bacteria that are isolated will be reported. If an anaerobic process is suspected, the procedures described in the anaerobic culture section must be followed to prevent loss of anaerobic organisms in transit. Various specimens will be considered. Wound cultures are from various body sites (arm, leg, etc), gastric aspirates, body fluids (other than CSF), tissues and ears. PRINCIPLE Wound infections may be caused by one or several organisms. Post operative wounds are most often caused by a mixture of aerobes and anaerobes. Superficial wounds are usually caused by aerobes only. Drainage, exudates, infections in closed body cavities, internal body fluids and visceral organ infections, and other deep seated infections can be caused by one or several aerobes and/or anaerobes. The most common wound pathogens include Staph aureus, Streptococci, Enterobacteriaceae, Pseudomonas, Bacteroides, Clostridia, and anaerobic cocci. Staph epidermidis can be found as a pathogen in wounds associated with a foreign body. Specimen choice depends on the extent and character of the infection rather than the organism suspected. A significant problem in collecting specimens and interpreting cultures arises from the ease with which most open lesions are colonized with microflora which can be pathogenic. Attention should be given to removing as much superficial material as possible before specimen collection is attempted. Types of Wounds are as follows: A. Superficial Wounds - Impetigo B. Pyogenic Skin Infections 1. Folliculitis 2. Furunculosis 3. Carbuncles C. Traumatic Wounds 1. Bite Wounds - Human and Animal 2. Soil Contaminated Wounds 3. Water Contaminated Wounds
4. 5. 6. 7.
Erysipelas Cellulitis Necrotizing Wounds Stab Wounds
D. Surgical Wounds 1. Clean Surgical Wound - Result of Clean Surgical Procedure 2. Contaminated Wound - Infections Mirror the Microbiota of the Particular Anatomical Site E. Musculoskeletal Infections 1. Bacterial Arthritis 2. Osteomyelitis F. Closed Body Cavity Infections (Ex. Peritoneal, Pericardial, Joints) G. Ear Infections 1. Otitis externa is a superficial infection of the external auditory canal. It is frequently initiated by moisture and occasionally occurs as a secondary manifestation of a chronically draining middle ear infection. Pseudomonas and Staph aureus are the organisms most frequently involved. 2. Acute bacterial otitis media (middle ear infection) is the most common illness in children that requires antibiotics. Highest attack rates occur during winter months in children 6-24 months old. Adolescents and adults are rarely affected. Hemophilus influenzae, Strep. pneumonia and Strep. pyogenes cause most of the cases of bacterial otitis media. H. Autopsy Cultures Autopsy cultures can yield valuable information. If more than 6 hours has elapsed between death and examination, the heart, blood and tissues will reflect post mortem on perimortem contamination by organisms from the large intestines. I. Staph Screen These cultures are routinely performed in the Neonatal Intensive Care Unit to control the amount of Staph aureus associated nosocomial infection. J Bone Marrow Surveillance cultures These cultures are performed on patients undergoing bone marrow transplantation. The results represent when the patient's endogenous flora has been suppressed after a radiation and/or chemotherapeutic conditioning regiment. The recolonization of the patient can also be displayed in these cultures after successful transplantation has occurred. The results can also represent colonization of the patient with potential pathogens.
The microbiota of wounds reflect their anatomical site, mode of infliction, the environment in which the wounds were inflicted, and the degree of microbial contamination of the adjacent areas which were perforated in the process. The most dominant organism in a wound infection is usually the most clinically significant. The Gram stain result (i.e. presence of PMNs) will also aid the clinician in evaluating the results of the culture and correlating it to the clinical picture of the patient. The most common contaminating flora is usually cutaneous flora which consists of: Staph. sp. coag negative Corynebacterium sp. Alpha hemolytic strep Non-hemolytic strep not Enterococcus Small # Staph aureus However, the anatomical site of the wound will play an important role in discerning whether or not the organisms isolated are pathogens or contaminating flora (Ex. Abdominal wounds, Contaminated with fecal flora). It is not medically relevant to identify and perform susceptibility on any more than 3 pathogens from a wound infection. Cultures from decubiti can yield a multitude of organisms. Full identification and susceptibility testing is usually not clinically useful due to the nature of the wound and the treatment of the wound. Many hospitalized and chronically ill patients become colonized very rapidly with organisms (especially Gram negative rods). Most of these are just colonizers and are not representative of the true infection. The Gram stain smear will aid the microbiologist and clinician in evaluating the culture result in these cases. SPECIMEN COLLECTION 1. Specimens Collected on Swabs a. Examples - Superficial wounds, boils, incision sites, Staph screens, bone marrow surveillance b. Collect specimen on Culturette swab, sampling the deepest portion or active margin of the wound. Do not sample areas of healing. Try to avoid touching contaminating skin with the swab. c. Replace swab into culturette holder and crush ampule at base of culturette. d. Transport to Lab ASAP. 2. Drainages, exudates and/or abscess where there is enough pus to aspirate by syringe. a. Clean surface with antiseptic. b. Aspirate with needle and syringe, being careful to sample deepest portion or active margin of the wound.
c. Expel air from the syringe. d. Replace needle sheath or place needle in a cork. e. Transport to the Lab ASAP. 3. Body Fluids a. Disinfect skin b. Collect fluid via percutaneous aspiration with a syringe. c. Expel air from syringe. d. Replace needle sheath or place needle in a cork, or express fluid into a sterile tube. If the fluid is in danger of clotting, ie. high WBCs and/or high, the fluid should be placed in a SPS tube. If a cell count was ordered the fluid should also be placed in an EDTA tube. e. Transport to Lab ASAP. NOTE: Body fluids can also be collected in blood culture bottles. See Blood Culture Procedure for collection and processing. 4 Tissue (including autopsy) a. The tissues are collected by a physician according to standard medical procedures. b. The tissue should be placed in a sterile container. c. Transport to the Lab ASAP. d. If Helicobacter pylori is requested, see the procedures in this manual. 5. Ears a. Ear canal, outer ear. 1. Collect specimen with a swab from a culturette. 2. Sample the active margin or deepest portion of the infected site. 3. As much as possible, avoid sampling areas of healing and non-infected tissue. 4. Use a swab or gauze pad to remove cerumen. b. Middle Ear 1. If perforation of the eardrum has not occurred, the specimen may be obtained by the physician by aspiration through the tympanic membrane with a needle and syringe or a suction device. 2. If perforation has occurred, use a swab to remove and aseptically discard in the upper ear canal and earwax. With a second swab, collect discharge nearest the eardrum. c. Mastoid processes 1. These are collected during surgery. 2. Place specimen in a sterile tube and transport immediately. STORAGE AND TRANSPORT The specimen should be transported to the Laboratory as soon as possible. The maximum amount of time between collection and processing of the specimen should not exceed two hours. If more than 2 hours will elapse, place the specimen in the
refrigerator for no more than 8-10 hours. If a fluid was collected the specimen should be stored at room temperature. SPECIAL HANDLING When a specimen is received, it is charged to the patient according to protocol. The following test codes are used for wounds: TEST CODE M240 M269 M269 M020 M262 M270* M175 M170 M180 M192* M272* M235* CULTURE Routine Wound Actinomyces culture (see anaerobic wound) Amniotic Fluid (see anaerobic wound) Anaerobic Wound (see anaerobic wound) Body Fluid Culture** Ear Culture Joint Fluid Culture** Peritoneal Fluid Culture** Pleural Fluid Culture** Staphylococcal Screen Bone Marrow Surveillance Quantitative Wound (see Quantitative Wound)
The test code is entered and the appropriate specimen code is entered in the specimen slot. Any further identifying characteristics should be entered in the "IDENT". A Gram stain is charged, test code "M110" with the exception of the test codes marked with an "*" and autopsy cultures. The appropriate specimen code should be entered in the specimen slot. **If a cell count is requested on a sterile body fluid charge a test code "M050". See cell count procedure in this manual. CRITERIA FOR REJECTION OF SPECIMENS The following specimens are unacceptable: Mislabeled specimens Leaking specimens Grossly contaminated specimens Specimens received in non-sterile containers If a specimen is rejected, call the physician/nurse in charge of the patient and explain the reason for the rejection. Record the date, time, patient name, unit number, reason for the rejection and the name of the person contacted in the Quality Assurance Book. If an improper specimen must be processed, the final result should indicate that the specimen quality was compromised.
REAGENTS AND SUPPLIES 1. BBL Media, Available from General Medical a. TSA with 5% sheep blood (BAP), Cat# 21261 b. Chocolate II Agar ( CHOC ), Cat # 21267 c. MacConkey Agar (MAC), Cat # 21270 d. Thioglycollate Medium (THIO), Cat # 21200 e. Mannitol Salt Agar (MSA), Cat # 21173 2. Culturette (Marion), available from Medical Warehouse, Cat # 00830 3. Tissue Grinder (Sage), available from Baxter Scientific, Cat. # T4031 STORAGE All media is kept refrigerated with the exception of the thioglycollate media. Small volumes of media are kept at room temperature and replenished as needed. QUALITY CONTROL All media is quality controlled by the Manufacturer according to NCCLS Guidelines. PROCEDURE Inoculation and Incubation A. Routine Wound Culture collected on a culturette 1. Inoculate the following media a. Two Blood Agar Plates (BAP) b. Chocolate Agar Plate (CHOC) c. MacConkey Plate (MAC) d. Mannitol Salt Agar Plate (MSA) e. Thioglycollate Media (THIO) 2. The plates are inoculated by rolling the swab onto the agar surface. 3. A Gram stain is made next by rolling the swab on the glass slide, making a a thin film. Place the slide on the slide warmer to dry. 4. Inoculate the THIO by breaking the swab off into the broth. 5. Incubate one BAP in the Anaerobic Jar at 35C. Incubate the other BAP and CHOC in 5% C02 at 35C. Incubate the MAC, MSA and THIO in the aerobic incubator at 35C.
B. Drainages, exudates, pus in syringes. Inoculate the same media as above using the actual pus instead of a swab. C. Body Fluids 1. Inoculate the following media: a. Two Blood Agar Plates (BAP) b. Chocolate Agar Plate (CHOC) c. Thioglycollate Media (THIO) 2. The Plates and broth are inoculated by using the syringe if the specimen came in a syringe or a sterile pipet if the fluid came in a sterile container. 3. A Gram stain is made using the cytospin centrifuge (see Cytospin Procedure). 4. Incubate one BAP in the Anaerobic Jar at 35C. Incubate the other BAP and CHOC in 5% C02 at 35C. Incubate the THIO in the Aerobic Incubator at 35C. D. Tissues 1. If there is enough tissue, cut the tissue with a sterile scalpel and make a touch prep for a Gram stain. 2. Place tissue in sterile disposable tissue grinder. 3. Add small volume of Thioglycollate broth to tissue grinder. 4. Grind tissue. 5. Using sterile Pasteur pipette, inoculate the following media: a. Two Blood Agar Plate (BAP) b. Chocolate Agar Plate (CHOC) c. MacConkey Plate (MAC) d. Mannitol Salt Agar Plate (MSA) e. Thioglycollate Media (THIO) 6. A Gram stain is made, if a touch prep has not already been made, by placing a drop of the ground specimen on a glass slide. Place the slide on the slide warmer to dry. 7. Incubate one BAP in the Anaerobic Jar at 35C. Incubate the other BAP and CHOC in 5% C02 at 35C. Incubate the MAC, MSA, and THIO in the Aerobic Incubator at 35C. E. Ears 1. Inoculate the following: a. Blood Agar Plate (BAP)
b. Chocolate Agar Plate (CHOC) c. MacConkey Plate (MAC) d. Thioglycollate Media (THIO) 2. The plates are inoculated by rolling the swab on the surface of the agar plate. 3. A gram stain is made if requested by rolling the swab on the glass slide, making a thin film. Place the slide on the slide warmer to dry. 4. Inoculate the THIO by breaking the swab off into the broth. 5. Incubate the BAP and CHOC in 5% C02 at 35C. Incubate the MAC and THIO in the Aerobic incubator at 35C. F. Staphylococcal Screens 1. Using the culturette swab inoculate a Blood Agar Plate 2. Incubate the BAP in 5% C02 at 35C. G. Bone Marrow Surveillance 1. Using the culture swab inoculate a Chocolate Agar Plate. 2. Inoculate the THIO by breaking the swab off into the broth. 3. Incubate the THIO in the aerobic incubator at 35C and the CHOC in 5% C02 at 35C. Gram Stain Examination A. After the slide has been stained, examine the slide for cells and bacteria under the oil immersion objective. B. Cells: Polys, Mononuclear, and Epithelial Cells, if seen, should be enumerated and reported. If no cells seen, report "No Cells Seen". C. Bacteria: All organisms seen should be reported and quantitated (rare, small, mod and large). If no bacteria is seen, report "No Organisms Seen". If Gram positive thin, branching rods are seen, the culture should be covered for Actinomycetes. CULTURE WORKUP (Routine Wounds, Exudates, Ears, Body Fluid, and Tissues) DAY 1 (18 -24 hours incubation) 1. All plates and broths are examined at 24 hours. 2. If no growth on plates or in broth, reincubate plates and broth for an additional 24 hours.
3. If growth on plates, identify all significant isolates according to "Guidelines" for the workup of organisms". Reincubate plates and broth for an additional 24 hours. 4. If no growth on plates and broth appears to have growth, Gram stain THIO. Based on the Gram stain result, transfer THIO to the appropriate media. Reincubate all plates and THIO for an additional 24 hours. (Incubate anaerobic BAP in all transfers). DAY 2 1. All plates and broths are examined. 2. If no growth on plates or in broth, discard plates and report "No Growth". The THIO is placed in the THIO rack for an additional 5 days. It is placed in the forward portion of the rack so it can be examined daily. 3. If growth on plates, identify all significant isolates, according to the "Guidelines for the workup of organisms". Save any relevant plates and discard the rest. Place the THIO in the THIO rack in the back portion of the rack. By placing it here the THIO will be held for 5 additional days but will not be examined daily. 4. If no growth on plates and THIO appears to have growth follow #4 on Day 1, however, the original plates can be discarded. DAY 3-7 1. The negative THIOs are examined daily for signs of growth (i.e., puff balls, turbidity, gas formation, etc). 2. The technologist will discard the 7 day THIOs writing the date and his/her initials on the THIO sheet (see Figure 1). 3. The technologist will then move Day 6 THIOs to the Day 7 rack, examining them for growth, and recording date and initials on the THIO sheet. Next Day 5 to Day 6 , etc. and Day 4 to Day 5 etc. and Day 3 to Day 4, etc. 4. All new THIOs (48 hr old cultures) are placed in day 3 rack. The accession numbers for the broth are logged in on the THIO sheet. STAPHYLOCOCCAL SCREENS 1. Examine plates at 24 hours for the presence or absence of Staph aureus only. A staphaurex is done on all suspected colonies. No susceptibility testing is done. 2. If the specimen came in before 4:30 p.m. the culture can be reported out. If the specimen came in after 4:30, the plates have to be reincubated for an additional 24 hours.
BONE MARROW SURVEILLANCE CULTURE 1. Examine the plates and broth at 24 hours for growth. All organisms should be reported generically. No susceptibility testing is done. 2. Reincubate plates and broth for an additional 24 hours. 3. Reexamine plates and broth for growth. Report out culture and discard plate. If nothing significant, place THIO in THIO rack . If positive for growth, place in back of rack on Day 3. If negative for growth place THIO in front and log accession number onto THIO rack sheet. 4. Follow Day 3-7 under Routine Wounds for examination of THIO rack. REPORTING OF RESULTS Report all results on Worksheet #550 ROUTINE WOUNDS, ETC 1. If culture is sterile after 48 hours, report "No Growth" (code 101) 2. If a significant organism is isolated, report the organism, its quantitation and susceptibility testing (if appropriate) first, using the appropriate codes. Report any other insignificant isolates next. Example: Large # Staph aureus (code "307") with sensitivities. 3. If an organism is isolated from the broth only: If significant, report with susceptibility, and "Isolated from broth culture only" Code "153". Also, add the number of days incubation before being isolated using one of the following: CODE 154 155 156 157 158 Isolated after 3 days incubation Isolated after 4 days incubation Isolated after 5 days incubation Isolated after 6 days incubation Isolated after 7 days incubation CODE 400 153 157
Example: Staph. sp. coag negative Isolated from broth culture only Isolated after 6 days incubation
4. If multiple organisms are isolated, they can be listed generically or using the code "105" - "Multiple species of organisms isolated". If this is suggestive of contamination flora based on the site of the specimen, you can use the comment section to note this. Example: Abdominal Wound Grew out - 3 types Gram Negative Rods Staph. sp. Coag Negative Alpha Haemolytic Strep. Report: "Multiple species of organisms isolated - "code" "105". Add under comments: "Suggestive of Fecal Flora"
5. If a single organism isolated, but is not significant, report out generically without susceptibility profile. 6. For Staphylococcal Screens report No growth No Staph aureus isolated _____# Staph aureus isolated PROCEDURAL NOTES 1. Any significant isolates from bone, tissues, body fluids, etc, should be saved on TSA slants or frozen at -70C. These isolates may require further testing such as serum bacteriacidal levels. 2. Isolates from autopsy cultures do not require susceptibility testing. 3. Generally speaking, wound infections will show the growth of limited numbers of pathogens. One expects the gram stain to show moderate or more polymorphonuclear cells and a limited number of bacterial morphotypes. Organisms colonizing a wound are expected to be present in small numbers. Cultures of colonized wounds, especially postoperative wounds, show growth of several morphotypes. Gram stains show few or no polymorphs and mixed flora. 4. Microbiology must allow for the fact that a wound which is colonized today and gives culture and Gram stain results that correspond to this picture, may become infected tomorrow. Therefore, if clinical information to this effect is relayed to Microbiology, the approaches to identification and sensitivity testing must be modified accordingly. LIMITATIONS 1. The use of antibiotics, before specimen collection, can cause false negative cultures. Code 101 160 397
2. Specimen collection and transport is critical. Death of fragile organisms and overgrowth of irrelevant bacteria may occur in a short period of time. 3. When one sample of the deepest portion of the infected site, it may be impossible to avoid collection of organisms of lesser significance. Hopefully, these will be present in smaller numbers on both the culture and the Gram stain. REFERENCES ASM. Manual of Clinical Microbiology, 4th ED. Washington, DC, 1985. Finegold, SM, et al. Baily and Scott's Diagnostic Microbiology, 5th ED. CV Mosby Company, St. Louis, Mo pp 100-109. 1978. Mandell G, et al ED. Principles and Practice of Infectious Disease (2nd ED). John Wiley and sons, New York. 1985.
You might also like
- 3.6.9 SOP - Urine CultureDocument3 pages3.6.9 SOP - Urine CultureSemeeeJunior100% (2)
- Microbiology Lab Manual - Revised Spring 2013Document117 pagesMicrobiology Lab Manual - Revised Spring 2013Mbiko SabeyoNo ratings yet
- Fitzpatricks Dermatology in General Medicine 8ed 1Document10 pagesFitzpatricks Dermatology in General Medicine 8ed 1ANTINNo ratings yet
- Common Microorganisms Cause Wound Infections: Possible Pathogens Gram Positive ExamplesDocument8 pagesCommon Microorganisms Cause Wound Infections: Possible Pathogens Gram Positive Examplesعبدالحكيم النهديNo ratings yet
- Appropriate Specimens For Anaerobic Cultures: (Phil J Microbiol Infect Dis 1998 27 (2) :71-73)Document4 pagesAppropriate Specimens For Anaerobic Cultures: (Phil J Microbiol Infect Dis 1998 27 (2) :71-73)u_niz_058038No ratings yet
- Isolation IDof StrepDocument13 pagesIsolation IDof Strepidris rabiluNo ratings yet
- Specimen Collections in The Medical Microbiology and parasitologyNOTESDocument43 pagesSpecimen Collections in The Medical Microbiology and parasitologyNOTESPrincewill SeiyefaNo ratings yet
- Lecture11 MicrobiologyDocument62 pagesLecture11 MicrobiologyVenomNo ratings yet
- Lab Policies Culture Wounds Lab 3115Document7 pagesLab Policies Culture Wounds Lab 3115Marj MendezNo ratings yet
- Anaerobic Culture .: Ahmed GomaaDocument42 pagesAnaerobic Culture .: Ahmed Gomaaah7510No ratings yet
- Ear Cultures Principle: 3.6.12 Sop: Ear Culture Page 1 of 2Document2 pagesEar Cultures Principle: 3.6.12 Sop: Ear Culture Page 1 of 2SemeeeJuniorNo ratings yet
- HML 316 Notes 2021Document39 pagesHML 316 Notes 2021nessa nimoNo ratings yet
- Clinical PathologyDocument37 pagesClinical PathologyVincent ReyesNo ratings yet
- Principles of Diagnostic Medical MicrobiologyDocument4 pagesPrinciples of Diagnostic Medical MicrobiologyTarequl Islam NishadNo ratings yet
- Wound Swabs, BasicsDocument26 pagesWound Swabs, Basicstummalapalli venkateswara raoNo ratings yet
- Diagnostic Tissue Microbiology Methods: Nelson S. Brewer, M.D., Aml Lyle A. Weed, M.D.Document9 pagesDiagnostic Tissue Microbiology Methods: Nelson S. Brewer, M.D., Aml Lyle A. Weed, M.D.JimenoNo ratings yet
- Week 7-8Document13 pagesWeek 7-8Glaiza Dalayoan FloresNo ratings yet
- BacteDocument13 pagesBacteJhanver Joel AldosNo ratings yet
- Microbiology Lab Manual and GuideDocument117 pagesMicrobiology Lab Manual and GuideSelvaraju Parthibhan100% (2)
- Specimen Collection 2Document70 pagesSpecimen Collection 2Sakura Di Musim Semi100% (2)
- Role of Specimen CollectionDocument72 pagesRole of Specimen Collectiontummalapalli venkateswara rao100% (4)
- Microbiology Lab Manual - Spring 2012Document114 pagesMicrobiology Lab Manual - Spring 2012occbuzi100% (3)
- Handwashing Is The Single Most Important Measure To Reduce The Risks of TransmittingDocument3 pagesHandwashing Is The Single Most Important Measure To Reduce The Risks of TransmittingMaria OgabangNo ratings yet
- Lauren R. Pinchbeck, DVM, MS, DACVD South Texas Veterinary Allergy & Dermatology, San Antonio, TX, USADocument4 pagesLauren R. Pinchbeck, DVM, MS, DACVD South Texas Veterinary Allergy & Dermatology, San Antonio, TX, USADonny ArtikaNo ratings yet
- Surgical Infections PDFDocument9 pagesSurgical Infections PDFJohn Christopher LucesNo ratings yet
- Blood Specimen Collection: Elaine M. KeohaneDocument15 pagesBlood Specimen Collection: Elaine M. KeohanePrince Guevara100% (1)
- PL-Microbiology Specimen Collection Guidelines (2020.07.22)Document14 pagesPL-Microbiology Specimen Collection Guidelines (2020.07.22)Anonymous fgRHAEIMrHNo ratings yet
- 3.6.6 SOP - Wound CultureDocument3 pages3.6.6 SOP - Wound CultureSemeeeJunior100% (1)
- Specimen Collection in Infectious DiseasesDocument72 pagesSpecimen Collection in Infectious DiseasesFadi KhaizaranNo ratings yet
- Last WorksheetDocument4 pagesLast WorksheetMusa WinxNo ratings yet
- Procedure For Taking A Wound SwabDocument15 pagesProcedure For Taking A Wound Swabchloemeriel100% (1)
- Micro NoeDocument63 pagesMicro NoejoseNo ratings yet
- Eye Culture 1. Principle: 3.6.11 SOP: Eye Cultures Page 1 of 2Document2 pagesEye Culture 1. Principle: 3.6.11 SOP: Eye Cultures Page 1 of 2SemeeeJuniorNo ratings yet
- 3 Wound InfectionDocument4 pages3 Wound InfectionSRO oONo ratings yet
- MicrobesDocument6 pagesMicrobesemms meNo ratings yet
- Basic Mycology: Deanna A. SuttonDocument14 pagesBasic Mycology: Deanna A. SuttonGURJEET SINGHNo ratings yet
- Bact##Document16 pagesBact##lawobi5622No ratings yet
- Lab 9. Sample CollectionDocument23 pagesLab 9. Sample CollectionSuzan AbdNo ratings yet
- Methods of Specimen Collection For Diagnosis of Superficial and Subcutaneous Fungal InfectionsDocument5 pagesMethods of Specimen Collection For Diagnosis of Superficial and Subcutaneous Fungal InfectionssaadmcsNo ratings yet
- Microbiology Lab #1 - StainingDocument85 pagesMicrobiology Lab #1 - StainingAmanda PachecoNo ratings yet
- Asepsis and Infection ControlDocument6 pagesAsepsis and Infection ControlgilissaNo ratings yet
- 5 Cardinal Signs of Infection (Classical Signs Latin-Based Naming)Document7 pages5 Cardinal Signs of Infection (Classical Signs Latin-Based Naming)Ianne MerhNo ratings yet
- Lab Dept/Section: Microbiology/Virology Test Name: Sputum Culture and Gram StainDocument4 pagesLab Dept/Section: Microbiology/Virology Test Name: Sputum Culture and Gram StainAdn crnNo ratings yet
- 3-The Risk of Doing An Autopsy and High-Risk AutopsiesDocument8 pages3-The Risk of Doing An Autopsy and High-Risk Autopsiestherese_ticNo ratings yet
- PATH505PDocument11 pagesPATH505PMohsin SialNo ratings yet
- Tell Me and I Will Forget. Show Me and I Might Remember. Involve Me and I Will UnderstandDocument36 pagesTell Me and I Will Forget. Show Me and I Might Remember. Involve Me and I Will UnderstandChandrashekhar UnakalNo ratings yet
- Infection Prevention and Safety Measures Including HivDocument37 pagesInfection Prevention and Safety Measures Including HivRipunjoy KalitaNo ratings yet
- Abdul CadarDocument4 pagesAbdul CadarVitta Kusma WijayaNo ratings yet
- Wound Culture and Gram StainDocument4 pagesWound Culture and Gram StainNicodeme SodeaNo ratings yet
- Diagnostic MicrobiologyDocument7 pagesDiagnostic MicrobiologyadebomojoodunayoNo ratings yet
- Articulo 1Document14 pagesArticulo 1galovinicioNo ratings yet
- Idea ? 1 Mini ProposalDocument5 pagesIdea ? 1 Mini ProposalThompson GukwaNo ratings yet
- Sputum CollectionDocument4 pagesSputum CollectionBELIGANIO JOHANNANo ratings yet
- Abcess PeritonsillarDocument21 pagesAbcess PeritonsillarribeetleNo ratings yet
- Collection and Storage of Pecimen in The Lab: Expired ContainersDocument5 pagesCollection and Storage of Pecimen in The Lab: Expired ContainersClick QuantumNo ratings yet
- MLS 422 Diagnostic MicrobiologyDocument50 pagesMLS 422 Diagnostic MicrobiologyMayowa OgunmolaNo ratings yet
- Bacteriology HandoutsDocument30 pagesBacteriology HandoutsMarco Tolentino100% (8)
- Surgical Site InfectionsDocument78 pagesSurgical Site InfectionsBashiru AminuNo ratings yet
- Practical Manual for Detection of Parasites in Feces, Blood and Urine SamplesFrom EverandPractical Manual for Detection of Parasites in Feces, Blood and Urine SamplesNo ratings yet
- Vitamins 091027012332 Phpapp01Document83 pagesVitamins 091027012332 Phpapp01IsaacJ22No ratings yet
- Fluidsandelectrolytes 090224074347 Phpapp02Document102 pagesFluidsandelectrolytes 090224074347 Phpapp02IsaacJ22No ratings yet
- Endocrine Glands & Their Functions: Anatomy & Physiology II Georgia Perimeter College K. Donaldson, InstructorDocument55 pagesEndocrine Glands & Their Functions: Anatomy & Physiology II Georgia Perimeter College K. Donaldson, InstructorIsaacJ22No ratings yet
- Basic Virus Structure: Capsid Protein Nucleocapsid Naked Capsid Virus DNA or +Document47 pagesBasic Virus Structure: Capsid Protein Nucleocapsid Naked Capsid Virus DNA or +IsaacJ22No ratings yet
- Clinicalchemistryreviewsheetformltcertificationandascp 131203172703 Phpapp02Document299 pagesClinicalchemistryreviewsheetformltcertificationandascp 131203172703 Phpapp02IsaacJ22No ratings yet
- Diagnosis of Important Bacterial DiseasesDocument41 pagesDiagnosis of Important Bacterial DiseasesIsaacJ22No ratings yet
- Wound Cultures Culture SetupDocument3 pagesWound Cultures Culture SetupIsaacJ22No ratings yet
- Biochemical: ReactionsDocument62 pagesBiochemical: ReactionsIsaacJ22No ratings yet
- Denaturation of ProteinsDocument16 pagesDenaturation of ProteinsLineah Untalan100% (2)
- M.Sc. Foods and Nutrition PDFDocument43 pagesM.Sc. Foods and Nutrition PDFRajaDeepak VermaNo ratings yet
- Immune Response To Mycobacterium Tuberculosis: A Narrative ReviewDocument8 pagesImmune Response To Mycobacterium Tuberculosis: A Narrative ReviewBrenda RamirezNo ratings yet
- Biology RespirationDocument10 pagesBiology RespirationArmanai KhamzinaNo ratings yet
- MalariaDocument83 pagesMalariasarguss1467% (3)
- Blast Pre LabDocument2 pagesBlast Pre Labapi-373344212No ratings yet
- Jawapan: Kertas 1 BiologyDocument9 pagesJawapan: Kertas 1 BiologyNang Maizana Megat YahyaNo ratings yet
- 1st August (Porifera)Document7 pages1st August (Porifera)tayyabuetlhrNo ratings yet
- Aids 8-12-2013Document6 pagesAids 8-12-2013giancarlo_luzziNo ratings yet
- Hayden Crump - Student - LeesvilleRdHS - Lamberth Fall22 Academic Evolution SlidesDocument18 pagesHayden Crump - Student - LeesvilleRdHS - Lamberth Fall22 Academic Evolution SlidesHayden CrumpNo ratings yet
- Chapter 7Document4 pagesChapter 7MALTI MAHESH VASHISTHNo ratings yet
- Protein Engineering-Methods and ProtocolsDocument347 pagesProtein Engineering-Methods and Protocolslzy100% (1)
- General Pathology NotesDocument29 pagesGeneral Pathology NotesMohd Syaiful Mohd ArisNo ratings yet
- Cell Defense WorksheetDocument2 pagesCell Defense WorksheetDana Fransen0% (1)
- MicrobiologyDocument2 pagesMicrobiologynguyenhoh100% (1)
- Earth and Life Science Week 14 (Perpetuation of Life) : DECEMBER 1-4, 2020Document9 pagesEarth and Life Science Week 14 (Perpetuation of Life) : DECEMBER 1-4, 2020Ann Kyla ManrezaNo ratings yet
- Physiology of Growth: Arlan L. RosenbloomDocument12 pagesPhysiology of Growth: Arlan L. Rosenbloomانجمن بدنسازی ایرانNo ratings yet
- Analogy Ad HomologyDocument5 pagesAnalogy Ad HomologyNeelamNo ratings yet
- Vigneshwar ResumeDocument2 pagesVigneshwar ResumeelanthamizhmaranNo ratings yet
- Biochemistry Review Notes: MembraneDocument18 pagesBiochemistry Review Notes: MembraneRanielle Samson100% (1)
- Foot and Mouth DiseaseDocument444 pagesFoot and Mouth DiseaseAdil razaNo ratings yet
- Respiration Chapter 7 Biology Form 4Document90 pagesRespiration Chapter 7 Biology Form 4edain84No ratings yet
- 1 6 Regulation of Blood Glucose PDFDocument3 pages1 6 Regulation of Blood Glucose PDFtiaraNo ratings yet
- Glycolysis: Biochemistry. 5th Edition. Berg JM, Tymoczko JL, Stryer L. New York: 2002Document7 pagesGlycolysis: Biochemistry. 5th Edition. Berg JM, Tymoczko JL, Stryer L. New York: 2002api-550381747No ratings yet
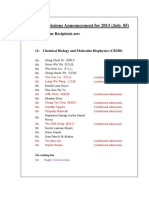
- TIGP Admissions Announcement For 2013Document6 pagesTIGP Admissions Announcement For 2013WinataWahyuFajarNo ratings yet
- Histopathology Report GuideDocument2 pagesHistopathology Report GuidejkNo ratings yet
- Signs and SymptomsDocument8 pagesSigns and SymptomsGehla TumananNo ratings yet
- Juan Diego Pacheco-Polanco, Lenin E. Oviedo-Correa, David Herra Miranda and Maria Gabriela SilvaDocument1 pageJuan Diego Pacheco-Polanco, Lenin E. Oviedo-Correa, David Herra Miranda and Maria Gabriela SilvaCentro de Investigación de Cetáceos (CEIC) - Costa RicaNo ratings yet
- Cells of The Immune SystemDocument2 pagesCells of The Immune Systemhasbiallah1306100% (1)