Professional Documents
Culture Documents
S0002870311X00248 S000287031200662X Main
S0002870311X00248 S000287031200662X Main
Uploaded by
Juan Camilo MoralesCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- 14-Rights of Drug AdministrationDocument4 pages14-Rights of Drug AdministrationFernandez, Florence Nicole100% (2)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Celtic Reiki Level 2Document0 pagesCeltic Reiki Level 2Enlazador de Mundos100% (2)
- Cialis Case PDFDocument4 pagesCialis Case PDFinterpon07No ratings yet
- 1 An Evolutionary Perspective On The Origin REVIEWDocument9 pages1 An Evolutionary Perspective On The Origin REVIEWJuan Camilo MoralesNo ratings yet
- J10 - T3 Criterios de Cotton ColedocolitiasisDocument7 pagesJ10 - T3 Criterios de Cotton ColedocolitiasisJuan Camilo MoralesNo ratings yet
- Fisiopato NCPHDocument12 pagesFisiopato NCPHJuan Camilo MoralesNo ratings yet
- Radiological Investigation in Acute Diverticulitis: ReviewDocument6 pagesRadiological Investigation in Acute Diverticulitis: ReviewJuan Camilo MoralesNo ratings yet
- Book Reviews: R e N A L Disease in Children - Clinical Evaluation and DiagnosisDocument1 pageBook Reviews: R e N A L Disease in Children - Clinical Evaluation and DiagnosisJuan Camilo MoralesNo ratings yet
- Bleeding and HemorrhagesDocument3 pagesBleeding and HemorrhagesJehanzeb ZebNo ratings yet
- Comparative Evaluation of Antimicrobial Efficacy of Various Herbal Root Canal Irrigants Against Enterococcus Faecalis - An in Vitro StudyDocument6 pagesComparative Evaluation of Antimicrobial Efficacy of Various Herbal Root Canal Irrigants Against Enterococcus Faecalis - An in Vitro StudyIJAR JOURNALNo ratings yet
- Argan Vitalisation of Dermal Stem Cells For Skin Rejuvenation Personal Care 07 2011Document3 pagesArgan Vitalisation of Dermal Stem Cells For Skin Rejuvenation Personal Care 07 2011Steve D'HamsNo ratings yet
- Rehabilitation Centre: Accepting, Embracing and Making Change." "Document3 pagesRehabilitation Centre: Accepting, Embracing and Making Change." "Manasvini KarthihaNo ratings yet
- Anesthesia-Assessing Depth PDFDocument1 pageAnesthesia-Assessing Depth PDFAvinash Technical ServiceNo ratings yet
- Clinical Leadership Doc by MckinseyAug08Document32 pagesClinical Leadership Doc by MckinseyAug08Tyka Asta AmaliaNo ratings yet
- A Disease, Disorder, Illness or Condition: How To Label Epilepsy?Document5 pagesA Disease, Disorder, Illness or Condition: How To Label Epilepsy?HaniNo ratings yet
- Human HerpesvirusesDocument498 pagesHuman HerpesvirusesCeleste Sánchez RomeroNo ratings yet
- Chronic Itp - Karen Nina Ocampo 09012008Document61 pagesChronic Itp - Karen Nina Ocampo 09012008LIMRA ALAMNo ratings yet
- Important Notice 38-2021 Dated 24-03-2021 Available Seats Foreign National Spon INI CET PG Courses July 2021Document3 pagesImportant Notice 38-2021 Dated 24-03-2021 Available Seats Foreign National Spon INI CET PG Courses July 2021Priyobrata KonjengbamNo ratings yet
- Formularium PDFDocument16 pagesFormularium PDFDewayu NanaNo ratings yet
- SK-600II Operator's Manual PDFDocument90 pagesSK-600II Operator's Manual PDFdian100% (1)
- Food Safety PDFDocument178 pagesFood Safety PDFarunNo ratings yet
- Characteristics of NewbornDocument102 pagesCharacteristics of NewbornSusan HepziNo ratings yet
- Glatt Production of Liquid DrugsDocument16 pagesGlatt Production of Liquid Drugsteatoom75% (4)
- Basic Hara Diagnosis An Introduction To Kiiko Style The Avi Way"Document90 pagesBasic Hara Diagnosis An Introduction To Kiiko Style The Avi Way"sillypolo100% (1)
- How To Cure A Skin Disease VitiligoDocument85 pagesHow To Cure A Skin Disease VitiligoSurendra PadhanNo ratings yet
- CP 100 Module 10 14.editedDocument24 pagesCP 100 Module 10 14.editedKhyla AmorNo ratings yet
- Difficult Airway Management in The Intensive Care UnitDocument10 pagesDifficult Airway Management in The Intensive Care UnitcedivadeniaNo ratings yet
- 14.ergonomic Workstation Design For Science Laboratory (Norhafizah Rosman) PP 93-102Document10 pages14.ergonomic Workstation Design For Science Laboratory (Norhafizah Rosman) PP 93-102upenapahangNo ratings yet
- 11-First Aid PDFDocument33 pages11-First Aid PDFSaizul Baharudin100% (1)
- Overview of HemostasisDocument21 pagesOverview of Hemostasis黄資元100% (1)
- NLE 05-2015 Laoag Room AssignmentDocument17 pagesNLE 05-2015 Laoag Room AssignmentPRC BaguioNo ratings yet
- Orthognathic Surgery RonalDocument56 pagesOrthognathic Surgery Ronaldrghempik100% (2)
- Cancers: Cell Origins of High-Grade Serous Ovarian CancerDocument28 pagesCancers: Cell Origins of High-Grade Serous Ovarian CancerAlfonso AnggriawanNo ratings yet
- DEATH IN THE FREEZER ActivitiesDocument5 pagesDEATH IN THE FREEZER ActivitiesLaura Alicia TerragnoNo ratings yet
- Drug-Study HydrocortisoneDocument4 pagesDrug-Study HydrocortisoneChristian Neil PonceNo ratings yet
S0002870311X00248 S000287031200662X Main
S0002870311X00248 S000287031200662X Main
Uploaded by
Juan Camilo MoralesOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
S0002870311X00248 S000287031200662X Main
S0002870311X00248 S000287031200662X Main
Uploaded by
Juan Camilo MoralesCopyright:
Available Formats
Vitamin D reduces left atrial volume in patients with left ventricular hypertrophy and chronic kidney disease
Hector Tamez, MD, MPH, a Carmine Zoccali, MD, d David Packham, MD, e,f Julia Wenger, MPH, a Ishir Bhan, MD, MPH, a Evan Appelbaum, MD, MM, Sci, g Yili Pritchett, PhD, i Yuchiao Chang, PhD, b Rajiv Agarwal, MD, j Christoph Wanner, MD, k Donald Lloyd-Jones, MD, ScD, l Jorge Cannata, MD, m B. Taylor Thompson, MD, c Dennis Andress, MD, i Wuyan Zhang, PhD, i Bhupinder Singh, MD, n Daniel Zehnder, MD, o Ajay Pachika, MD, p Warren J. Manning, MD, g,h Amil Shah, MD, p Scott D. Solomon, MD, p and Ravi Thadhani, MD, MPH a Boston, MA; Reggio Calabria, Italy; Victoria, Australia; Abbott Park, and Chicago, IL; Indianapolis, IN; Wuerzburg, Germany; Oviedo, Spain; Tempe, AZ; and Coventry, United Kingdom
Background Left atrial enlargement, a sensitive integrator of left ventricular diastolic function, is associated with increased cardiovascular morbidity and mortality. Vitamin D is linked to lower cardiovascular morbidity, possibly modifying cardiac structure and function; however, firm evidence is lacking. We assessed the effect of an activated vitamin D analog on left atrial volume index (LAVi) in a post hoc analysis of the PRIMO trial (clinicaltrials.gov: NCT00497146). Methods and results One hundred ninety-six patients with chronic kidney disease (estimated glomerular filtration rate 15-60 mL/min per 1.73m 2), mild to moderate left ventricular hypertrophy, and preserved ejection fraction were randomly assigned to 2 g of oral paricalcitol or matching placebo for 48 weeks. Two-dimensional echocardiography was obtained at baseline and at 24 and 48 weeks after initiation of therapy. Over the study period, there was a significant decrease in LAVi (2.79 mL/m 2, 95% CI 4.00 to 1.59 mL/m 2) in the paricalcitol group compared with the placebo group (0.70 mL/m 2 [95% CI 1.93 to 0.53 mL/m 2], P = .002). Paricalcitol also attenuated the rise in levels of brain natriuretic peptide (10.8% in paricalcitol vs 21.3% in placebo, P = .02). For the entire population, the change in brain natriuretic peptide correlated with change in LAVi (r = 0.17, P = .03). Conclusions Forty-eight weeks of therapy with an active vitamin D analog reduces LAVi and attenuates the rise of BNP. In a population where only few therapies alter cardiovascular related morbidity and mortality, these post hoc results warrant further confirmation. (Am Heart J 2012;164:902-909.e2.)
Left atrial (LA) enlargement is a common early finding associated with increase left ventricular (LV) mass and elevated cardiovascular risk. 1-3 Left atrial volume is directly influenced by the LV diastolic filling pressure through the open mitral orifice. 4,5 In contrast to Doppler
measurements of LV diastolic functionaffected by acute hemodynamic changesLA volume indexed to body surface area (LAVi) is a more stable parameter, and it is a sensitive indicator of diastolic dysfunction severity. 6-8 Patients with increased LAVi have a higher risk for
From the aDepartment of Medicine (Division of Nephrology), Massachusetts General Hospital, Boston, MA, bDepartment of Medicine (Division of General Medicine), Massachusetts General Hospital, Boston, MA, cDepartment of Medicine (Division of Pulmonary and Critical Care Unit), Massachusetts General Hospital, Boston, MA, d Nephrology, Dialysis and Transplantation Unit and CNR-IBIM Clinical Epidemiology and Pathophysiology of Renal Diseases and Hypertension, Reggio Calabria, Italy, e Melbourne Renal Research Group, Reservoir Private Hospital, Department of Nephrology, Royal Melbourne Hospital, Melbourne, Victoria, Australia, fDepartment of Nephrology, Austin Hospital, Melbourne, Victoria, Australia, gPERFUSE CMR Core Laboratory and Department of Medicine (Cardiovascular Division), Beth Israel Deaconess Medical Center, Boston, MA, hDepartment of Radiology, Beth Israel Deaconess Medical Center, Boston, MA, iAbbott Laboratories, Abbott Park, IL, j Department of Medicine, Indiana University School of Medicine, Indianapolis, IN, k Department of Medicine, Division of Nephrology, University Hospital, University of
Wuerzburg, Wuerzburg, Germany, lDepartment of Preventive Medicine, Northwestern University Feinberg School of Medicine, Chicago, IL, mServicio de Metabolismo seo y Mineral, Instituto Reina Sofia de Investigacin, Hospital Universitario Central de Asturias, RedinRen, Instituto Carlos III, Oviedo, Spain, nSouthwest Kidney Institute, Tempe, AZ, oClinical Sciences Research Institute, Warwick Medical School, The University of Warwick, Coventry, United Kingdom, and pDepartment of Medicine, Cardiovascular Division, Brigham and Women's Hospital, Boston, MA. Submitted June 28, 2012; accepted September 19, 2012. Reprint requests: Ravi Thadhani, MD, MPH, Massachusetts General Hospital, 55 Fruit Street, Bulfinch 127, Boston, MA 02114. E-mail: thadhani.r@mgh.harvard.edu 0002-8703/$ - see front matter 2012, Mosby, Inc. All rights reserved. http://dx.doi.org/10.1016/j.ahj.2012.09.018
American Heart Journal Volume 164, Number 6
Tamez et al 903
cardiovascular events, heart failure hospitalization, atrial arrhythmia, and stroke, 9-12 independently of other risk factors. 13,14 Importantly, in patients with chronic kidney disease (CKD), LAVi has added prognostic value above LV morphology and function. 8,15 Although primarily recommended for bone health, vitamin D has been linked to decreasing cardiovascular diseases, but the mechanisms involved remain unknown. 16-18 The vitamin D receptor is present in vascular smooth muscle, endothelial cells, and possibly cardiac tissue. 16,19 Animal studies have shown that vitamin D improves LV diastolic dysfunction, heart failure, cardiac morphology, and reduces natriuretic peptides. 20-23 In humans, observational studies, small clinical trials, and meta-analyses suggest that vitamin D reduces cardiovascular events. 17,18 Patients with low 25-hydroxy vitamin D levels have a higher prevalence of heart failure. 24 Patients with CKD tend to have low levels of 25-hydroxy vitamin D and of 1,25-dihydroxyvitamin D3, which have been linked to higher cardiac morbidity and mortality. 25 There are few proven therapies to reduce cardiovascular morbidity and mortality in CKD patients, although vitamin D has been suggested to be among them. In the recently completed PRIMO trial, a multinational double-blinded, placebocontrolled, randomized trial, we assessed the effect of paricalcitol on LV mass in patients with LV hypertrophy and CKD (www.clinicaltrials.gov NCT00497146). 26 We found no change in LV mass index assessed by cardiac magnetic resonance imaging in patients treated with paricalcitol over 48 weeks compared with those who received placebo. However, paricalcitol decreased the number of cardiovascular hospitalizations. In addition, exploratory analyses suggested an effect of paricalcitol on LA size. 26 Herein, we perform a detailed analysis to assess the effect of paricalcitol on LAVi.
Patients were randomly assigned in a 1:1 ratio to receive paricalcitol 2 g/d capsules or placebo. Randomization was stratified with respect to country, gender, and RAAS inhibitor use. Transthoracic echocardiograms were obtained at baseline, week 24, and week 48 after randomization. For the current analysis, all patients with at least 2 echocardiographic measurements were included (baseline and either 24 or 48 weeks).
Outcomes
Our main outcome of interest was the change from baseline in LA volume indexed to body surface area over the study duration (48 weeks) on echocardiography. Other parameters evaluated were LA area (apical 4-chamber), measures of LV diastolic function (early [E] and late [A] mitral inflow wave velocities, peak lateral mitral annular relaxation velocity [E'], isovolumetric relaxation time [IVRT], and E-wave deceleration time), and brain natriuretic peptide (BNP).
Echocardiographic measurements. Eligible candidates underwent transthoracic echocardiogram to establish baseline, week 24, and week 48 LAVi. Left atrial volume was assessed by the biplane area-length method from apical 4- and 2chamber views at end systole from the frame preceding mitral valve opening. Left atrial volume index was calculated as LA volume to body surface area (mL/m 2). 12 Echocardiographic parameters were measured by a single sonographer at each center according to established American Society of Echocardiography protocols 27 and subsequently sent to the echocardiographic core laboratory at the Brigham and Women's Hospital. From 2-dimensional M-mode and Doppler (spectral, color, tissue) images, E (cm/s), A (cm/s), IVRT (s 1000), and transmitral E-wave deceleration time (s) were measured. 28 Left ventricular volumes were derived as previously described, 21 and LV mass, estimated from linear dimensions according to published formulae. 27 Left atrial volumes were measured by Simpson's method of discs in the apical 4-chamber view. 27 Mitral regurgitation was graded according to standard criteria. 27 Laboratory measurements. Details of all laboratory measurements have been previously published. 26 In brief, we measured BNP (normal b100 pg/mL; Abbott Diagnostics, Abbott Park, IL) at baseline, week 24, and week 48. The modification of diet in renal disease formula was used to calculate eGFR. 29
Methods
Study population
The PRIMO study enrolled 227 patients from 60 centers in 11 countries between July 2008 and September 2010. Details of the protocol and primary results have been reported previously. 26 In brief, patients were 18 to 75 years old with LV hypertrophy on 2-dimensional transthoracic echocardiography (septal wall thickness of 1.1-1.7 cm in females, 1.2-1.8 cm in males), 27 LV ejection fraction (LVEF) N50%, and estimated glomerular filtration rate (eGFR) of 15 to 60 mL/minute per 1.73m 2. Patients on renin-angiotensin-aldosterone-system (RAAS) inhibitors were on stable doses for N1 month. Patients with asymmetric septal hypertrophy, valvular disease, clinically significant coronary artery disease, cerebrovascular accident within 3 months, receiving active vitamin D therapy, and uncontrolled blood pressure at screening were excluded. Cholecalciferol and ergocalciferol were limited to 400 IU/d. The institutional review board/ethics committee at each site approved the protocol, and all patients provided written informed consent.
Statistical analysis
Means (SDs) or number (percentages) was used to summarize baseline characteristics aside from laboratory measures, which were summarized using medians (quartile 1quartile 3). We created binary variables based on the reference range for troponin T. Longitudinal analyses were conducted in all randomized patients with at least 2 measures (baseline and either 24 or 48 week follow-up) using a maximum-likelihood, mixed-effect repeated-measures model (MMRM) of all observations. The models included terms for treatment, visit, and treatment by visit interaction; baseline value; gender; RAAS use; country; and baseline eGFR (strong association with LAVi). Means and 95% CIs from the MMRMs are presented. Overall P values represent the significance level for the overall treatment group effect (24 and 48 weeks combined). The same models were used to investigate treatment effect pattern among subgroups.
904 Tamez et al
American Heart Journal December 2012
Table I. Baseline characteristics by treatment group
Characteristics Paricalcitol (n = 103) Placebo (93)
Table II. Baseline transthoracic echocardiogram measures by treatment group
Measures Paricalcitol (n = 103) 32.8 9.8 20 4 126 37 51 17 60 5 53 12 78 20 86 23 0.9 0.3 8.3 2.4 105 16 0.22 0.03 3.0 1.7 Placebo(93) 35.4 11.4 21 5 125 31 50 14 60 5 55 14 79 21 86 24 1.0 0.3 8.4 2.5 109 18 0.23 0.03 2.8 2.0
Age, mean (SD), y 64 11 65 12 Male, n (%) 72 (70) 65 (70) Race, n (%) White 77 (75) 68 (73) African American 11 (11) 11 (12) Other 15 (14) 14 (15) Cardiovascular history, n (%) Hypertension 100 (97) 88 (95) Smoking 52 (50) 45 (48) Peripheral vascular 12 (12) 13 (14) disease, arterial Diabetes mellitus 55 (53) 47 (51) RAAS medication 81 (79) 74 (80) Diuretics 37 (36) 32 (34) Weight, mean (SD), kg 86 21 84 18 Body surface area, 2.0 0.3 2.0 0.2 mean (SD), m2 Vital signs, mean (SD) Systolic blood pressure, 135 16 135 18 mm Hg Diastolic blood 75 12 75 10 pressure, mm Hg Heart rate, per min 70 10 68 13 Laboratory values, median (quartile 1-quartile 3) Albumin, g/dL 4.40 (4.20-4.60) 4.40 (4.20-4.60) Calcium, mg/dL 9.60 (9.22-9.80) 9.58 (9.34-9.90) Phosphate, mg/dL 3.70 (3.30-4.10) 3.53 (3.19-4.00) Parathyroid hormone, 98 (64-163) 105 (71-145) pg/mL Hemoglobin level, g/dL 12.50 (11.45-13.75) 12.60 (11.30-13.90) Blood urea nitrogen, 37 (29-48) 35 (26-42) mg/dL Creatinine, mg/dL 2.10 (1.60-2.70) 1.90 (1.61-2.40) eGFR, mL/min 31 (26-43) 36 (26-42) Brain natriuretic 68 (35-132) 81 (33-177) peptide, pg/mL Troponin T 0.01 ng/mL, 24 (25) 24 (26) No. (%) Cholesterol, mg/dL 179 (145-219) 171 (146-206) High-density lipoprotein, 45 (38-59) 46 (38-55) mg/dL Low-density lipoprotein, 95 (68-119) 90 (72-111) mg/dL Urine albumin 240 (54-855) 118 (26-782) creatinine ratio, mg/g
LAVi, mL/m 2 Left atrial area, cm 2 Left ventricular end-diastolic volume (4-chamber), mL Left Ventricular end-systolic volume (4-chamber), mL Ejection fraction (4-chamber), % Left ventricular mass index, g/m 2.7 Early mitral inflow wave velocity (E), cm/s Late mitral inflow wave velocity (A), cm/s Early / late mitral inflow wave velocity ratio (E/A) Early diastolic mitral annular velocity (E'), cm/s Isolvolumetric relaxation time, s 1000 Transmitral E-wave deceleration time, s Mitral regurgitation jet area, cm 2
Values represent mean and SD.
This study was funded by an investigator-initiated grant from Abbott Laboratories, and no additional funding was received for this analysis. The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the manuscript, and its final contents.
Results
Baseline characteristics A total of 196 (86%) of the 227 enrolled patients in the PRIMO study had available longitudinal echocardiographic data; 103 were randomly assigned to paricalcitol; and 93, to placebo. Baseline characteristics were similar between groups (Table I). Participants were mostly white males with hypertension. Other cardiovascular risk factors, such as obesity and diabetes mellitus, were highly prevalent in both groups. Most participants were receiving RAAS inhibitors (79% in paricalcitol vs 80% in placebo). Diuretic use was also similar between groups (36% in paricalcitol vs 34% in placebo) as were plasma BNP levels (median 68 ng/mL in paricalcitol vs 81 ng/mL in placebo). Estimated glomerular filtration rate was lower in the paricalcitol group (31 mL/min) compared with the placebo group (36 mL/min), and the paricalcitol group had a higher urinary albumin to creatinine ratio (240 mg/g paricalcitol vs 118 mg/g placebo). Echocardiographic measurements showed similar moderate LAVi enlargement in both groups (Table II). In addition, patients had a similar degree of left ventricular hypertrophy. The early diastolic lateral mitral annular velocity (E) was below normal, and the IVRT was prolonged consistent with impaired diastolic function. Mitral regurgitation was minimal in both groups.
Subgroups were stratified by natural groupings for categorical variables and median values for continuous variables. The MMRM models excluding eGFR were used for vital sign and continuous laboratory values comparisons. Medication use and categorical laboratory values at 48 weeks were compared using 2 test. Brain natriuretic peptide values were log transformed (positive skewness). Brain natriuretic peptide models included same variables as LAVi models, plus age and baseline weight (known confounders). All correlations used Spearman coefficients. Analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC).
American Heart Journal Volume 164, Number 6
Tamez et al 905
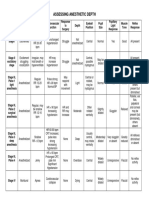
Table III. Repeated-measures analysis of change in transthoracic echocardiography measures from baseline to 24 and 48 weeks
24 wk Paricalcitol (n = 98) 1.49 (2.66 to 0.32) 0.98 (1.52 to 0.45) 2.05 (5.68 to 1.57) 0.88 (3.10 to 1.34) 0.03 (1.13 to 1.06) 1.28 (2.64 to 0.09) 6.01 (10.10 to 1.93) 1.38 (4.95 to 2.19) 0.08 (0.14 to 0.02) 0.31 (0.88 to 0.25) 0.41 (3.63 to 4.45) 0.006 (0.003 to 0.014) 1.68 (2.59 to 0.77) Placebo (n = 88) 0.46 (1.68 to 0.76) 0.24 (0.80 to 0.31) 0.07 (3.83 to 3.69) 0.55 (1.77 to 2.87) 0.27 (1.41 to 0.86) 1.55 (2.97 to 0.14) 5.60 (9.87 to 1.34) 1.10 (4.82 to 2.62) 0.05 (0.11 to 0.01) 0.05 (0.65 to 0.56) 1.78 (5.89 to 2.34) 0.001 (0.009 to 0.010) 1.59 (2.53 to 0.66) Paricalcitol (n = 82) 2.79 (4.00 to 1.59) 1.09 (1.62 to 0.56) 0.09 (0.16 to 0.01) 4.13 (8.02 to 0.24) 2.22 (4.61 to 0.18) 1.34 (2.96 to 0.29) 4.59 (8.84 to 0.34) 0.47 (4.44 to 3.50) 0.08 (0.14 to 0.02) 0.05 (0.58 to 0.69) 0.92 (3.42 to 5.26) 0.008 (0.001 to 0.018) 2.03 (3.23 to 0.82) 48 wk Placebo (n = 80) 0.70 (1.93 to 0.53) 0.40 (0.94 to 0.15) 0.07 (0.14 to 0.01) 0.87 (4.87 to 3.13) 0.06 (2.41 to 2.54) 1.18 (2.84 to 0.49) 5.91 (10.28 to 1.55) 2.53 (1.56 to 6.62) 0.12 (0.18 to 0.06) 0.27 (0.93 to 0.38) 1.16 (5.65 to 3.33) 0.001 (0.011 to 0.008) 1.03 (2.10 to 0.05) Overall P value 0.006 0.004 0.14 0.09 0.52 0.94 0.81 0.37 0.81 0.92 0.29 0.08 0.17
Measures LAVi, mL/m 2 Left atrial area, cm 2 Left ventricular end diastolic volume (4-chamber), mL Left ventricular end systolic volume (4-chamber), mL Left ventricular ejection fraction (4-chamber), % Left ventricular mass index, g/m 2.7 Early mitral inflow wave velocity, cm/s Late mitral inflow wave velocity, cm/s Early / late mitral inflow wave velocity ratio Early diastolic mitral annular velocity Isolvolumetric relaxation time, ms Transmitral E-wave deceleration time, s Mitral regurgitation jet area, cm 2
P .11 .01 .29 .22 .68 .69 .85 .88 .40 .39 .31 .27 .84
P .002 .02 .66 .13 .09 .87 .58 .18 .22 .38 .40 .06 .12
Values are adjusted least-squares means and 95% CIs estimated from the models. Test of significance of treatment group differences by visit from the mixed-effects model. Test of significance between treatment groups for the overall effect (24 and 48 weeks combined) from the mixed-effects models.
Left atrial volume change. Serial echocardiographic data are summarized in Table III. The main outcome of interest, change in LAVi over the study period, demonstrated a significant decrease in the paricalcitol group (2.79 mL/m 2 [95% CI 4.00 to 1.59 mL/m 2]) (Table III) (Figure 1) compared with the placebo group (0.70 mL/m 2 [95% CI 1.93 to 0.53 mL/m 2], P = .002). Results were similar when LA volume was not indexed by body surface area (paricalcitol 5.14 mL [95% CI 7.47 to 2.82 mL] vs placebo 1.07 mL [95% CI 3.45 to 1.30 mL], P = .002). Left ventricular mass, LVEF, and LV volumes did not significantly change throughout the study duration. Doppler measurements of diastolic function (E/A, E, IVRT, DT) and mitral regurgitation did not significantly differ between groups throughout the study. Weight and blood pressure were similar in the paricalcitol and placebo groups throughout the 48 weeks of treatment (Supplemental Table I). Diuretic use did not differ between groups (Supplemental Table II, P = .30). Left atrial volume change by subgroups. The paricalcitol effect was homogeneous across baseline characteristics with greater reduction in LA volume
Figure 1
Adjusted mean LAVi at baseline, week 24, and week 48 by treatment group. Values are adjusted least-square means and 95% CIs estimated from the models.
906 Tamez et al
American Heart Journal December 2012
Figure 2
Forest plots for difference in adjusted LAVi change between treatment groups. Values are the difference in adjusted mean percent LAVi and 95% CIs from the models.
in all paricalcitol subgroups compared with placebo (Figure 2) (Supplemental Table III). Paricalcitol appeared to have a larger effect on patients less than 65 years of age, males, without peripheral vascular disease or diabetes mellitus, lower renal function, RAAS inhibitor use, and blood pressure N133 mm Hg. All interactions were nonsignificant, except RAAS inhibitor use (P = .03). Patients in the paricalcitol group using a RAAS inhibitor had a reduction in LAVi of 2.82 mL/m 2 (95% CI 4.00 to 1.65 mL/m 2) compared with 2.58 mL/m 2 (95% CI 4.75 to 0.40 mL/m 2) in those not on RAAS inhibitors. In contrast, patients in the placebo group using a RAAS inhibitor had a reduction in LAVi of 0.50 mL/m 2 (95% CI 1.72 to 0.72 mL/m 2) compared with 1.18 mL/m 2 (95% CI 3.39 to 1.02 mL/m 2) in those not on a RAAS inhibitor. Cardiac biomarkers. Plasma levels of BNP increased throughout the study in both groups; however, the rise was attenuated in the paricalcitol group (Figure 3). The adjusted rise in BNP from baseline to week 48 was 8.4 pg/ mL in the paricalcitol group compared with 18.5 pg/mL in the placebo group (10.8% in paricalcitol vs 21.3% in placebo, P = .02). The change in LAVi was correlated with log-transformed BNP change (r = 0.17, P = .03). Patients in the paricalcitol group with the highest decrease in BNP from baseline to week 48 (lowest quartile) had a change in LAVi of 3.7 ml/m 2 (95% CI 5.8 to 1.6 mL/m 2) compared with patients in the highest
Figure 3
Adjusted mean BNP at baseline, week 24, and week 48 by treatment group. Values are adjusted least-square means and 95% CIs estimated from the models.
BNP change quartile who demonstrated an decrease in LAVi of 0.8 mL/m 2 (95% CI 3.0 to 1.4 mL/m 2, P = .05, Figure 4). In the placebo group, there was no significant difference in LAVi change between patients in the lowest
American Heart Journal Volume 164, Number 6
Tamez et al 907
Figure 4
Adjusted change in LAVi by brain natriuretic peptide change quartile in the paricalcitol group. Values are adjusted least-square means and 95% CIs estimated from the models.
BNP change quartile and the patients in the highest BNP change quartile (1.2 mL/m 2 [95% CI 3.9 to 1.4 mL/m 2] vs 0.005 mL/m 2 [95% CI 2.0 to 2.0 mL/m 2], P = .43).
Discussion
The nephrology community has long sought interventions to modify cardiac structure and function given the marked elevation in risk for cardiovascular disease and the almost universal findings of altered cardiac structure and function in this population. In this post hoc analysis of the PRIMO trial, we demonstrate that paricalcitol therapy over 48 weeks was associated with a significant decrease in LAVi in patients with CKD, despite similar
blood pressure control and superimposed RAAS inhibitor medication use. In addition, reduction in LAVi was further augmented between the 24th and 48th week, leading us to speculate the potential for further benefit with longer therapy. These changes paralleled corresponding attenuation in the rise in plasma levels of BNP. The effect of vitamin D on LAVi reduction may operate through several mechanisms. First, paricalcitol can directly inhibit the RAAS axis. 21,30 Interestingly, there was a synergistic effect between paricalcitol and RAAS inhibitors, with the largest decline in LAVi in patients receiving both medications. Vitamin D can also affect cardiac remodeling by regulating extracellular matrix metalloproteinases expression such as tissue inhibitors of metalloproteinases 1 and 3 leading to attenuation of collagen deposition and oxidation. 31 Moreover, the vitamin D receptor is located in the sarcolemma and likely regulates myocyte relaxation. 32 Similarly, in animal models, paricalcitol increased lusitropy and regulated myocyte growth. 20,33 Diuretic use and body weight changes were similar between both groups suggesting that paricalcitol effect in LAVi was independent of extracellular fluid volume. However, paricalcitol can augment the number of natriuretic peptide receptors in the kidney and enhance BNP-mediated natriuresis. 34,35 In addition, paricalcitol can increase urinary calcium concentration, which could lead to a net volume loss. 36 The possibility remains that paricalcitol alters the dose-response relationship and causes subtle reduction in extracellular fluid undetected by body weight. Brain natriuretic peptide rise was attenuated by paricalcitol, despite the lower eGFR in this group. Left atrial volume index and BNP changes suggest improved LV filling pressures and attenuated myocardial stretch. However, Doppler measurements of diastolic function (E, E/A, IVRT, and transmitral E-wave deceleration time) did not significantly change throughout the study. 26 A possible explanation for the discrepancy between change in BNP, LAVi, and the lack of evident changes in diastolic dysfunction measurements is that our sample size was too small to account for the well-known variability of Doppler measurements. 6,7 Another possibility is that the 48-week follow-up was not long enough to uncover a difference; changes in natriuretic peptides are known to precede improvement of structural echocardiographic parameters. 37 Our study has limitations. All post hoc analyses inherently carry a higher risk of false-positive results. However, the effect of paricalcitol was homogeneous across all subgroups defined by baseline characteristics. This monotonic effect is consistent with a drug effect. In addition, changes in LAVi paralleled the attenuation of plasma BNP. Our study excluded patients with severe renal dysfunction (eGFR b15 mL/min), LV dysfunction (LVEF b50%), and severe LV hypertrophy. Nevertheless,
908 Tamez et al
American Heart Journal December 2012
the baseline LA size was similar to those of patients with advanced heart failure, mitral regurgitation, or atrial fibrillation, 38 and there is no known biologic reason why these patients would respond differently. Furthermore, our results indicate that the patients with a larger baseline LA size are more likely to respond. Lastly, the number of cardiovascular events was small, which prevented us from evaluating the relationship between change in LAVi and cardiovascular hospitalizations and heart failure in more detail. In CKD where alterations of cardiac structure and function are common and interventions limited, these results warrant further investigation.
Disclosures
Dr. Thadhani received a coordinating grant from Abbot Laboratories to the Massachusetts General Hospital, speaker's fees and travel support from Abbot Laboratories. Drs. Pritchett, Andress, and Zhang are employees of Abbott Laboratories and may own Abbott stock or options. Drs. Agarwal, Zoccali, Wanner and Zehnder received honoraria from Abbott Laboratories for lectures or for participation in steering committee. Dr. Manning received travel support for a CMR meeting from Abbott Laboratories. Dr. Solomon is supported by a research grant from Abbott Laboratories to the Brigham and Womens Hospital.
References
1. Miller JT, O'Rourke RA, Crawford MH. Left atrial enlargement: an early sign of hypertensive heart disease. Am Heart J 1988;116(4): 1048-51. 2. Pearson AC, Gudipati C, Nagelhout D, et al. Echocardiographic evaluation of cardiac structure and function in elderly subjects with isolated systolic hypertension. J Am Coll Cardiol 1991;17(2):422-30. 3. Ristow B, Ali S, Whooley MA, et al. Usefulness of left atrial volume index to predict heart failure hospitalization and mortality in ambulatory patients with coronary heart disease and comparison to left ventricular ejection fraction (from the Heart and Soul Study). Am J Cardiol 2008;102(1):70-6. 4. Appleton CP, Galloway JM, Gonzalez MS, et al. Estimation of left ventricular filling pressures using two-dimensional and Doppler echocardiography in adult patients with cardiac disease. Additional value of analyzing left atrial size, left atrial ejection fraction and the difference in duration of pulmonary venous and mitral flow velocity at atrial contraction. J Am Coll Cardiol 1993;22(7):1972-82. 5. Basnight MA, Gonzalez MS, Kershenovich SC, et al. Pulmonary venous flow velocity: relation to hemodynamics, mitral flow velocity and left atrial volume, and ejection fraction. J Am Soc Echocardiogr 1991;4(6):547-58. 6. Tsang TSM, Barnes ME, Gersh BJ, et al. Left atrial volume as a morphophysiologic expression of left ventricular diastolic dysfunction and relation to cardiovascular risk burden. Am J Cardiol 2002; 90(12):1284-9. 7. Simek CL, Feldman MD, Haber HL, et al. Relationship between left ventricular wall thickness and left atrial size: comparison with other measures of diastolic function. J Am Soc Echocardiogr 1995;8(1): 37-47.
8. Tripepi G, Benedetto FA, Mallamaci F, et al. Left atrial volume in endstage renal disease: a prospective cohort study. J Hypertens 2006; 24(6):1173-80. 9. Leung DY, Chi C, Allman C, et al. Prognostic implications of left atrial volume index in patients in sinus rhythm. Am J Cardiol 2010; 105(11):1635-9. 10. Tamura H, Watanabe T, Nishiyama S, et al. Increased left atrial volume index predicts a poor prognosis in patients with heart failure. J Card Fail 2011;17(3):210-6. 11. Benjamin EJ, D'Agostino RB, Belanger AJ, et al. Left atrial size and the risk of stroke and death. The Framingham Heart Study. Circulation 1995;92(4):835-41. 12. Meris A, Amigoni M, Uno H, et al. Left atrial remodelling in patients with myocardial infarction complicated by heart failure, left ventricular dysfunction, or both: the VALIANT Echo study. Eur Heart J 2009;30(1):56-65. 13. Gerdts E, Wachtell K, Omvik P, et al. Left atrial size and risk of major cardiovascular events during antihypertensive treatment: losartan intervention for endpoint reduction in hypertension trial. Hypertension 2007;49(2):311-6. 14. Quiones MA, Greenberg BH, Kopelen HA, et al. Echocardiographic predictors of clinical outcome in patients with left ventricular dysfunction enrolled in the SOLVD registry and trials: significance of left ventricular hypertrophy. Studies of Left Ventricular Dysfunction. J Am Coll Cardiol 2000;35(5):1237-44. 15. Patel RK, Jardine AGM, Mark PB, et al. Association of left atrial volume with mortality among ESRD patients with left ventricular hypertrophy referred for kidney transplantation. Am J Kidney Dis 2010;55(6):1088-96. 16. Holick MF. Vitamin D, deficiency. N Engl J Med 2007;357(3): 266-81. 17. Autier P, Gandini S. Vitamin D supplementation and total mortality: a meta-analysis of randomized controlled trials. Arch Intern Med 2007; 167(16):1730-7. 18. Wang TJ, Pencina MJ, Booth SL, et al. Vitamin D deficiency and risk of cardiovascular disease. Circulation 2008;117(4):503-11. 19. Levin A, Djurdjev O, Thompson C, et al. Canadian randomized trial of hemoglobin maintenance to prevent or delay left ventricular mass growth in patients with CKD. Am J Kidney Dis 2005;46(5):799-811. 20. Bodyak N, Ayus JC, Achinger S, et al. Activated vitamin D attenuates left ventricular abnormalities induced by dietary sodium in Dahl salt-sensitive animals. Proc Natl Acad Sci U S A 2007; 104(43):16810-5. 21. Bae S, Yalamarti B, Ke Q, et al. Preventing progression of cardiac hypertrophy and development of heart failure by paricalcitol therapy in rats. Cardiovasc Res 2011;91(4):632-9. 22. Chen S, Wu J, Hsieh JC, et al. Suppression of ANP gene transcription by liganded vitamin D receptor: involvement of specific receptor domains. Hypertension 1998;31(6):1338-42. 23. Li Q, Gardner DG. Negative regulation of the human atrial natriuretic peptide gene by 1,25-dihydroxyvitamin D3. J Biol Chem 1994; 269(7):4934-9. 24. Kim DH, Sabour S, Sagar UN, et al. Prevalence of hypovitaminosis D in cardiovascular diseases (from the National Health and Nutrition Examination Survey 2001 to 2004). Am J Cardiol 2008;102(11):1540-4. 25. Drechsler C, Pilz S, Obermayer-Pietsch B, et al. Vitamin D deficiency is associated with sudden cardiac death, combined cardiovascular events, and mortality in haemodialysis patients. Eur Heart J 2010; 31(18):2253-61. 26. Thadhani RI, Appelbaum E, Pritchett Y, et al. Vitamin D therapy and cardiac structure and function in patients with chronic kidney disease: the PRIMO randomized controlled trial. JAMA 2012;307(7):674-84.
American Heart Journal Volume 164, Number 6
Tamez et al 909
27. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 2005; 18(12):1440-63. 28. Ho CY, Solomon SD. A clinician's guide to tissue Doppler imaging. Circulation 2006;113(10):e396-8. 29. Stevens LA, Coresh J, Greene T, et al. Assessing kidney function measured and estimated glomerular filtration rate. N Engl J Med 2006;354(23):2473-83. 30. Li YC, Kong J, Wei M, et al. 1,25-Dihydroxyvitamin D(3) is a negative endocrine regulator of the renin-angiotensin system. J Clin Invest 2002;110(2):229-38. 31. Rahman A, Hershey S, Ahmed S, et al. Heart extracellular matrix gene expression profile in the vitamin D receptor knockout mice. J Steroid Biochem Mol Biol 2007;103(35):416-9. 32. Tishkoff DX, Nibbelink KA, Holmberg KH, et al. Functional vitamin D receptor (VDR) in the t-tubules of cardiac myocytes: VDR knockout cardiomyocyte contractility. Endocrinology 2008;149(2): 558-64.
33. Wu J, Garami M, Cheng T, et al. 1,25(OH)2 vitamin D3, and retinoic acid antagonize endothelin-stimulated hypertrophy of neonatal rat cardiac myocytes. J Clin Invest 1996;97(7): 1577-88. 34. Chen S, Olsen K, Grigsby C, et al. Vitamin D activates type A natriuretic peptide receptor gene transcription in inner medullary collecting duct cells. Kidney Int 2007;72(3):300-6. 35. Chen S, Ni X-P, Humphreys MH, et al. 1,25 dihydroxyvitamin d amplifies type a natriuretic peptide receptor expression and activity in target cells. J Am Soc Nephrol 2005;16(2):329-39. 36. Wang W, Kwon T-H, Li C, et al. Reduced expression of Na-K-2Cl cotransporter in medullary TAL in vitamin D-induced hypercalcemia in rats. Am J Physiol Renal Physiol 2002;282(1):F34-44. 37. Gackowski A, Isnard R, Golmard J-L, et al. Comparison of echocardiography and plasma B-type natriuretic peptide for monitoring the response to treatment in acute heart failure. Eur Heart J 2004;25(20):1788-96. 38. Shah AM, Hung C-L, Shin SH, et al. Cardiac structure and function, remodeling, and clinical outcomes among patients with diabetes after myocardial infarction complicated by left ventricular systolic dysfunction, heart failure, or both. Am Heart J 2011;162(4): 685-91.
American Heart Journal Volume 164, Number 6
Tamez et al 909.e1
Appendix
Supplemental Table I. Change from baseline to week 48 in vital signs and laboratory values by treatment group
Change at 48 wk Characteristic Vital signs, mean (95% CI) Weight, kg Body surface area, m 2 Systolic blood pressure, mm Hg Diastolic blood pressure, mm Hg Heart rate, per min Laboratory value, mean (95% CI) Hemoglobin level, g/dL Blood urea nitrogen, mg/dL Creatinine, mg/dL eGFR, mL/min Calcium, mg/dL Urine albumin creatinine ratio, mg/g Paricalcitol Placebo P Overall P value
0.3 (0.6, 1.1) 0.003 (0.01, 0.01) 0 (4, 4) 0 (2, 2) 3 (0, 5) 0.3 (0.6, 0.0) 5 (2, 8) 0.6 (0.5, 0.8) 4 (6, 2) 0.3 (0.2, 0.4) 18 (168, 31)
0.8 0.01 2 2 1
(0.1, 1.7) (0.002, 0.02) (2, 5) (0, 5) (1, 4)
.33 .41 .46 .10 .36 .09 .01 b.001 b.001 b.001 .20
.18 .77 .93 .45 .29 .24 .01 b.001 b.001 .39 .20
0.0 (0.3, 0.2) 1 (2, 4) 0.1 (0.0, 0.3) 1 (1, 2) 0.3 (0.4, 0.2) 98 (45, 241)
Values are adjusted least-square means and 95% CIs estimated from models. Models include treatment, visit, treatment by visit interaction, country, baseline and week 24 values. The test of significance treatment group differences by visit from the mixed effects model. The test of significance between treatment groups for the overall effect (24 and 48 weeks combined) from the mixed effect models.
Supplemental Table II. Medication use at week 48 by treatment group
Characteristic Medication, n (%) RAAS Diuretic
Obtained using v2-test.
Supplemental Table III (continued ) Pa Characteristic Difference in adjusted LAVi between paricalcitol and placebo over 48 wk (mL/m 2) 2.1 (3.7 to 0.4) 1.8 (3.6 to 0.1) 2.6 (4.5 to 0.7) 1.7 (3.6 to 0.2) 2.5 (4.3 to 0.6) 1.6 (3.5 to 0.2) 2.6 (4.5 to 0.7)
Paricalcitol
Placebo
84 (82) 42 (41)
72 (77) 31 (33)
.48 .30
Supplemental Table III. Difference in adjusted LAVi between paricalcitol and placebo over 48 weeks by subgroup
Difference in adjusted LAVi between paricalcitol and placebo over 48 wk (mL/m 2) 2.4 1.7 2.2 1.8 (4.3 (3.6 (3.8 (4.1 to 0.5) to 0.2) to 0.6) to 0.5)
Characteristic Age 65 y Age N65 y Male Female Race White Black Asian Cardiovascular history Peripheral vascular disease No peripheral vascular disease Diabetes mellitus No diabetes mellitus Renin-angiotensin-aldosterone antagonist No renin-angiotensin-aldosterone antagonist Diuretic
2.0 (3.5 to 0.5) 2.3 (6.1 to 1.5) 3.6 (7.4 to 0.1) 3.2 (7.1 to 0.6) 1.9 (3.3 to 0.5) 1.1 (2.9 to 0.7) 3.2 (5.1 to 1.3) 2.3 (3.8 to 0.8) 1.4 (4.3 to 1.5) 2.2 (4.4 to 0.1)
No diuretic Body mass index 29 kg/m 2 Body mass index N29 kg/m 2 Vital signs Systolic blood pressure 133 mm Hg Systolic blood pressure N133 mm Hg Diastolic blood pressure 75 mm Hg Diastolic blood pressure N75 mm Hg Laboratory values Albumin 4.4 g/dL Albumin b4.4 g/dL Calcium 9.6 mg/dL Calcium N9.6 mg/dL Phosphate 3.6 mg/dL Phosphate N3.6 mg/dL Parathyroid hormone 99 pg/mL Parathyroid hormone N99 pg/mL Hemoglobin 12.5 g/dL Hemoglobin N12.5 g/dL Blood urea nitrogen 36 mg/dL Blood urea nitrogen N36 mg/dL Creatinine 2 mg/dL Creatinine N2 mg/dL eGFR 33 mL/min eGFR N33 mL/min Brain natriuretic peptide 100 pg/mL Brain natriuretic peptide N100 pg/mL Troponin T 0.01 ng/mL
2.2 2.1 2.7 1.2 2.8 1.4 1.6 2.5 2.4 1.9 1.6 2.5 1.4 2.8 3.0 1.0 2.9
(3.9 (4.2 (4.5 (3.2 (4.7 (3.3 (3.5 (4.4 (4.3 (3.9 (3.5 (1.5 (3.2 (4.7 (4.9 (2.9 (4.8
to 0.4) to 0.1) to 1.0) to 0.8) to 1.0) to 0.5) to 0.2) to 0.6) to 0.5) to 0.0) to 0.3) to 0.6) to 0.4) to 0.8) to 1.1) to 0.9) to 0.9)
1.4 (3.2 to 0.5) 1.6 (3.1 to 0.1)
909.e2 Tamez et al
American Heart Journal December 2012
Supplemental Table III (continued ) Difference in adjusted LAVi between paricalcitol and placebo over 48 wk (mL/m 2) 3.6 1.8 2.3 1.1 (6.8 (3.6 (4.2 (3.1 to 0.4) to 0.1) to 0.4) to 0.8)
Characteristic Troponin T N0.01 ng/mL Cholesterol 175 mg/dL Cholesterol N175 mg/dL High-density lipoprotein 45 mg/dL High-density lipoprotein N45 mg/dL Low-density lipoprotein 92 mg/dL Low-density lipoprotein N92 mg/dL Urine albumin creatinine ratio 165 mg/g Urine albumin creatinine ratio N165 mg/g LAVi tertile 1 LAVi tertile 2 LAVi tertile 3
2.9 (4.8 to 1.0) 2.3 (4.2 to 0.4) 1.7 (3.6 to 0.2) 1.7 (3.8 to 0.3) 2.0 (4.1 to 0.2) 1.0 (3.3 to 1.2) 2.8 (5.1 to 0.5) 2.6 (5.0 to 0.1)
Values are the difference in adjusted least-square mean percent LAVi and 95% CIs from the models. Models include treatment, visit, treatment-visit interaction, gender, RAAS inhibitor use, country, baseline eGFR, and baseline LAVi. Negative values represent lower LAVi in paricalcitol compared with placebo. Estimated glomerular filtration rate (modification diet renal disease).
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- 14-Rights of Drug AdministrationDocument4 pages14-Rights of Drug AdministrationFernandez, Florence Nicole100% (2)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Celtic Reiki Level 2Document0 pagesCeltic Reiki Level 2Enlazador de Mundos100% (2)
- Cialis Case PDFDocument4 pagesCialis Case PDFinterpon07No ratings yet
- 1 An Evolutionary Perspective On The Origin REVIEWDocument9 pages1 An Evolutionary Perspective On The Origin REVIEWJuan Camilo MoralesNo ratings yet
- J10 - T3 Criterios de Cotton ColedocolitiasisDocument7 pagesJ10 - T3 Criterios de Cotton ColedocolitiasisJuan Camilo MoralesNo ratings yet
- Fisiopato NCPHDocument12 pagesFisiopato NCPHJuan Camilo MoralesNo ratings yet
- Radiological Investigation in Acute Diverticulitis: ReviewDocument6 pagesRadiological Investigation in Acute Diverticulitis: ReviewJuan Camilo MoralesNo ratings yet
- Book Reviews: R e N A L Disease in Children - Clinical Evaluation and DiagnosisDocument1 pageBook Reviews: R e N A L Disease in Children - Clinical Evaluation and DiagnosisJuan Camilo MoralesNo ratings yet
- Bleeding and HemorrhagesDocument3 pagesBleeding and HemorrhagesJehanzeb ZebNo ratings yet
- Comparative Evaluation of Antimicrobial Efficacy of Various Herbal Root Canal Irrigants Against Enterococcus Faecalis - An in Vitro StudyDocument6 pagesComparative Evaluation of Antimicrobial Efficacy of Various Herbal Root Canal Irrigants Against Enterococcus Faecalis - An in Vitro StudyIJAR JOURNALNo ratings yet
- Argan Vitalisation of Dermal Stem Cells For Skin Rejuvenation Personal Care 07 2011Document3 pagesArgan Vitalisation of Dermal Stem Cells For Skin Rejuvenation Personal Care 07 2011Steve D'HamsNo ratings yet
- Rehabilitation Centre: Accepting, Embracing and Making Change." "Document3 pagesRehabilitation Centre: Accepting, Embracing and Making Change." "Manasvini KarthihaNo ratings yet
- Anesthesia-Assessing Depth PDFDocument1 pageAnesthesia-Assessing Depth PDFAvinash Technical ServiceNo ratings yet
- Clinical Leadership Doc by MckinseyAug08Document32 pagesClinical Leadership Doc by MckinseyAug08Tyka Asta AmaliaNo ratings yet
- A Disease, Disorder, Illness or Condition: How To Label Epilepsy?Document5 pagesA Disease, Disorder, Illness or Condition: How To Label Epilepsy?HaniNo ratings yet
- Human HerpesvirusesDocument498 pagesHuman HerpesvirusesCeleste Sánchez RomeroNo ratings yet
- Chronic Itp - Karen Nina Ocampo 09012008Document61 pagesChronic Itp - Karen Nina Ocampo 09012008LIMRA ALAMNo ratings yet
- Important Notice 38-2021 Dated 24-03-2021 Available Seats Foreign National Spon INI CET PG Courses July 2021Document3 pagesImportant Notice 38-2021 Dated 24-03-2021 Available Seats Foreign National Spon INI CET PG Courses July 2021Priyobrata KonjengbamNo ratings yet
- Formularium PDFDocument16 pagesFormularium PDFDewayu NanaNo ratings yet
- SK-600II Operator's Manual PDFDocument90 pagesSK-600II Operator's Manual PDFdian100% (1)
- Food Safety PDFDocument178 pagesFood Safety PDFarunNo ratings yet
- Characteristics of NewbornDocument102 pagesCharacteristics of NewbornSusan HepziNo ratings yet
- Glatt Production of Liquid DrugsDocument16 pagesGlatt Production of Liquid Drugsteatoom75% (4)
- Basic Hara Diagnosis An Introduction To Kiiko Style The Avi Way"Document90 pagesBasic Hara Diagnosis An Introduction To Kiiko Style The Avi Way"sillypolo100% (1)
- How To Cure A Skin Disease VitiligoDocument85 pagesHow To Cure A Skin Disease VitiligoSurendra PadhanNo ratings yet
- CP 100 Module 10 14.editedDocument24 pagesCP 100 Module 10 14.editedKhyla AmorNo ratings yet
- Difficult Airway Management in The Intensive Care UnitDocument10 pagesDifficult Airway Management in The Intensive Care UnitcedivadeniaNo ratings yet
- 14.ergonomic Workstation Design For Science Laboratory (Norhafizah Rosman) PP 93-102Document10 pages14.ergonomic Workstation Design For Science Laboratory (Norhafizah Rosman) PP 93-102upenapahangNo ratings yet
- 11-First Aid PDFDocument33 pages11-First Aid PDFSaizul Baharudin100% (1)
- Overview of HemostasisDocument21 pagesOverview of Hemostasis黄資元100% (1)
- NLE 05-2015 Laoag Room AssignmentDocument17 pagesNLE 05-2015 Laoag Room AssignmentPRC BaguioNo ratings yet
- Orthognathic Surgery RonalDocument56 pagesOrthognathic Surgery Ronaldrghempik100% (2)
- Cancers: Cell Origins of High-Grade Serous Ovarian CancerDocument28 pagesCancers: Cell Origins of High-Grade Serous Ovarian CancerAlfonso AnggriawanNo ratings yet
- DEATH IN THE FREEZER ActivitiesDocument5 pagesDEATH IN THE FREEZER ActivitiesLaura Alicia TerragnoNo ratings yet
- Drug-Study HydrocortisoneDocument4 pagesDrug-Study HydrocortisoneChristian Neil PonceNo ratings yet