Professional Documents
Culture Documents
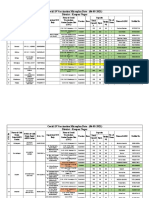
Atropine Sulfate Injection
Atropine Sulfate Injection
Uploaded by
IrawanMarlyOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Atropine Sulfate Injection
Atropine Sulfate Injection
Uploaded by
IrawanMarlyCopyright:
Available Formats
Atropine Sulfate Injection BP MIMS Abbreviated Prescribing Information
Atropine sulfate
CSL Section: 16(c) Cholinergic and anticholinergic agents - Surgical Preparations Pregnancy Category: A Permitted in sport Use: Severe bradycardia, bradyarrhythmias, 1st degree A-V block; pre-op salivary and bronchial secretion reduction, vagal inhibition; with neostigmine in muscle relaxant reversal; anticholinesterase poisoning Contraindications: Prostatic hypertrophy; bladder neck, pyloric obstruction; glaucoma; unstable cardiac rhythm; myasthenia gravis; reflux oesophagitis; severe ulcerative colitis, toxic megacolon complicating ulcerative colitis; obstructive GI disease; cardiospasm; paralytic ileus; intestinal atony Precautions: Hyperthyroidism; hypertension; renal, hepatic impairment; fever; high ambient temp; autonomic neuropathy; chronic pulmonary disease; coronary heart disease, CHF; mild to moderate ulcerative colitis; GI disorders; elderly, debilitated; lactation, children; see full PI Adverse Reactions: Drowsiness; anticholinergic effects; see full PI Interactions: Other anticholinergics Atropine Sulfate Injection BP (Injection) Rx (S4) Atropine sulfate; Min-I-Jet (single use vial) Pack 0.1 mg/mL 5 mL [1] Pack 0.1 mg/mL 10 mL [1] Dose Complex, see full PI MIMS Full Prescribing Information MIMS revision date: 1/05/97 Composition Active. Atropine sulfate. Inactive. Water for injections; sodium chloride, sodium citrate, citric acid monohydrate. Description Atropine is an odourless, bitter tasting, crystalline powder and an alkaloid which is widely distributed in nature, especially in the deadly nightshade plant, Atropa belladonna. Chemical name: (1R,3r,5S,8r)-tropan-3-yl-(+/-)-tropate sulfate monohydrate. Molecular formula: (C17H23NO3)2H2SO4.H2O. CAS: 5908-99-6. Actions Antimuscarinic agent. Pharmacology. Atropine is an antimuscarinic agent which competitively antagonises acetylcholine at postganglionic nerve endings, thus affecting receptors of the exocrine glands, smooth muscle, cardiac muscle and the central nervous system. Peripheral effects include tachycardia, decreased production of saliva, sweat and bronchial, nasal, lacrimal and gastric secretions, decreased intestinal motility and inhibition of micturition. Atropine increases sinus rate and sinoatrial and atrioventricular conduction by blocking vagal tone. The heart rate is usually increased but is sometimes preceded by an initial bradycardia. Atropine inhibits secretions throughout the respiratory tract and relaxes bronchial smooth muscle, producing bronchodilatation. Pharmacokinetics. Peak plasma concentrations of atropine after intramuscular administration are reached within 30 minutes. The elimination half-life varies between two and five hours. Plasma levels after intramuscular and intravenous injection are comparable after one hour. Atropine is distributed widely throughout the body and crosses the blood-brain barrier and placenta. Up to 50% of the dose is protein bound. Peak effects on the heart occur within four minutes of intravenous and about one hour after intramuscular administration. Atropine is metabolised in the liver by oxidation and conjugation to give inactive metabolites. About 50% of the dose is excreted within four hours and 90% in 24 hours in the urine, about 30 to 50% as unchanged drug. Indications Cardiac. In the management of patients with severe bradycardia and bradyarrhythmias, to increase the heart rate, and patients with type I atrioventricular conduction deficits, to lessen the degree of atrioventricular heart block.
Anaesthesia. As an antisialogogue in anaesthetic premedication, to reduce or prevent secretions in the respiratory tract. During anaesthesia, atropine may be used to prevent reflex bradycardia and restore cardiac rate and arterial pressure resulting from the increased vagal activity associated with laryngoscopy, tracheal intubation and intra-abdominal manipulation, and for the prevention of the oculocardiac reflex during ophthalmic surgery. Atropine may also be used to block muscarinic effects when neostigmine is used to counter the action of muscle relaxants. Anticholinesterase poisoning. Treatment of cardiovascular collapse following poisoning from cholinesterase inhibitors such as the organophosphorous insecticides parathion and malathion, the nerve gases and from mushroom poisoning. Contraindications Known hypersensitivity to atropine. Prostatic hypertrophy, bladder neck obstruction, pyloric obstruction, reflux oesophagitis, unstable cardiac rhythm, narrow angle glaucoma and myasthenia gravis (unless used to treat the adverse effects of an anticholinesterase agent). Severe ulcerative colitis or toxic megacolon complicating ulcerative colitis, obstructive disease of the gastrointestinal tract (e.g. pyloroduodenal stenosis, achalasia) cardiospasm, paralytic ileus or intestinal atony (especially in elderly or debilitated patients). Precautions Antimuscarinic agents should be used with caution in the elderly and in children since these patients may be more susceptible to adverse events. Atropine should also be used with caution in patients with hyperthyroidism, hepatic or renal disease or hypertension. Use with caution in febrile patients or when ambient temperature is high since antimuscarinics may cause an increase in temperature. Antimuscarinics block v agal inhibition of the sinoatrial nodal pacemaker and should thus be used with caution in patients with tachyarrhythmias, congestive cardiac failure or coronary heart disease. Atropine should be used with extreme caution in patients with mild to moderate ulcerative colitis. Parenterally administered atropine should be used cautiously in patients with chronic pulmonary disease, since a reduction in bronchial secretions may lead to the formation of bronchial plugs. Antimuscarinics should be used with extreme caution in patients with autonomic neuropathy. Antimuscarinics decrease gastric motility, relax the lower oesophageal sphincter and may delay gastric emptying; they should therefore be used with caution in patients with gastric ulcer, oesophageal reflux, pyloric stenosis, diarrhoea or gastrointestinal infection. Systemic administration of conventional doses of atropine may precipitate acute glaucoma in susceptible individuals. Tachycardia may result from vagal inhibition and induce angina pectoris in patients with coronary heart disease. Infants, patients with Down syndrome and children with spastic paralysis or brain damage may be hypersensitive to atropine's effect. Use in pregnancy. (Category A) Atropine has been given to a large number of pregnant women and women of childbearing age without any proven increase in the frequency of malformation or other direct or indirect harmful effects on the fetus having been observed. Atropine crosses the placenta and may cause tachycardia in the fetus. Use in lactation. Trace amounts of atropine appear in the breast milk and may cause antimuscarinic effects in the infant. Lactation may be inhibited. Effect on ability to drive or operate machinery. As atropine may affect eyesight and cause drowsiness, patients should not be allowed to drive cars or operate machinery.
Interactions The effects of atropine may be enhanced by the concomitant administration of other drugs with anticholinergic activity, e.g. tricyclic antidepressants, antispasmodics, antiparkinsonian drugs, some antihistamines, phenothiazines, disopyramide and quinidine. By delaying gastric emptying, atropine may alter the absorption of other drugs. Adverse Reactions Adverse events are dose related and usually reversible when therapy is discontinued. In relatively small doses, atropine reduces salivary, bronchial and sweat secretions; dryness of the mouth and anhidrosis may develop, these effects being intensified as dosage is increased. Reduced bronchial secretion may cause dehydration of residual secretion and consequent formation of thick bronchial plugs that are difficult to eject from the respiratory tract. Larger doses dilate the pupil and inhibit accommodation of the eye, and block vagal impulses with consequent increase in heart rate with possible atrial arrhythmias, atrioventricular dissociation, multiple ventricular ectopics and angina; parasympathetic control of the urinary bladder and gastrointestinal tract is inhibited, causing urinary retention and constipation. Further increase in dosage inhibits gastric secretion. Anaphylaxis, urticaria and rash, occasionally progressing to exfoliation, may develop in some patients. Other effects include increased ocular tension, loss of taste, headache, nervousness, drowsiness, weakness, dizziness, flushing, insomnia, nausea, vomiting and bloated feeling. Mental confusion and/or excitement may occur, especially in the elderly. Dosage and Administration Adults. The usual adult dose is 0.4 to 0.6 mg intravenously, intramuscularly or subcutaneously to a total of 2 mg. Anaesthetic premedication. 0.2 to 0.6 mg intramuscularly or subcutaneously half to one hour before surgery or the same dose intravenously immediately before surgery. To control muscarinic side effects of neostigmine. 0.6 to 1.2 mg intravenously for each 0.5 to 2.5 mg of neostigmine. Anticholinesterase poisoning. 1 to 2 mg intramuscularly or intravenously, repeated every five to 60 minutes until signs and symptoms disappear. Up to 50 mg may be needed in the first 24 hours. Children. The usual paediatric dose is 0.01 mg/kg or 0.3 mg/m2 body surface intravenously, intramuscularly or subcutaneously. The dose should not exceed 0.4 mg. If necessary, it can be repeated every four to six hours. Cardiac. For advanced cardiac life support the dose is 0.02 mg/kg with a minimum of 0.1 mg and a maximum of 1 mg in children and 2 mg in adolescents. Anaesthetic premedication. Subcutaneous doses, as follows. Up to 3 kg: 0.1 mg; 7 to 9 kg: 0.2 mg; 12 to 16 kg: 0.3 mg; over 20 kg: adult dose. Anticholinesterase poisoning. Intramuscularly or intravenously, 0.05 mg/kg every ten to 30 minutes until signs and symptoms disappear. Note. The atropine is in a single use Min-I-Jet prefilled syringe. Once the unit is assembled and used, any remaining portion of the solution must be discarded with the entire unit. Overdosage Symptoms. Marked dryness of the mouth accompanied by a burning sensation, difficulty in swallowing, pronounced photophobia, flushing and dryness of the skin, raised body temperature (very high in infants), rash, leucocytosis, nausea, vomiting, tachycardia and hypertension. Restlessness, tremor, confusion, excitement, hallucinations and delirium may result from CNS stimulation. This may be followed by increasing drowsiness, stupor and general central depression, terminating in death from circulatory and respiratory failure. Treatment. In severe cases, physostigmine 1 to 4 mg should be administered intravenously, intramuscularly or subcutaneously. The dose may be repeated as necessary since it is rapidly eliminated from the body. Diazepam may be administered for sedation of the delirious patient but the risk of central depression occurring late in the course of atropine poisoning contraindicates large doses of sedative. An adequate airway should be maintained and respiratory failure may be treated with oxygen and carbon
dioxide inhalation. Fever is reduced by the application of cold packs or sponging with tepid water. Adequate fluid intake is essential. Urethral catherisation may be necessary. A darkened room is essential because of photophobia. Presentation Injection (sterile solution), 0.1 mg/mL (Min-I-Jet: single use vial and vial injector): 5 mL, 10 mL. Storage Store below 25 deg. C. Protect from light; keep in carton until ready for use. Poison Schedule S4; except 0.6 mg/mL or less; 5's (for organophosphorous poisoning): S2. Date of TGA approval or last amendment 29/04/1996
You might also like
- Hesi Maternity Ob PDFDocument32 pagesHesi Maternity Ob PDFcclaire197% (37)
- Drug Study TramadolDocument14 pagesDrug Study TramadolBianca Freya Porral85% (13)
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (3)
- Case Write Up-DengueDocument16 pagesCase Write Up-DengueSyafi'ie Syukri100% (1)
- Free Preview - The Stall Slayer PDFDocument9 pagesFree Preview - The Stall Slayer PDFRohit RumadeNo ratings yet
- Side Effects:: AtropineDocument7 pagesSide Effects:: AtropinekletadaNo ratings yet
- Drug RationaleDocument77 pagesDrug RationaleYolanda WilliamsNo ratings yet
- Therapeutic: Urinary Tract Stimulants Pharmacologic: CholinergicDocument37 pagesTherapeutic: Urinary Tract Stimulants Pharmacologic: CholinergicApple MaeNo ratings yet
- Anesthetic DrugsDocument7 pagesAnesthetic DrugsAJ DalawampuNo ratings yet
- Atropine SulfateDocument6 pagesAtropine SulfateManelle SingzonNo ratings yet
- Drug Study ArvinDocument6 pagesDrug Study ArvinArvin BeltranNo ratings yet
- Drug StudyDocument22 pagesDrug StudyColleen Fretzie Laguardia NavarroNo ratings yet
- Drug StudyDocument9 pagesDrug StudyJannefer HernandezNo ratings yet
- Drug Study FORTDocument3 pagesDrug Study FORTLysa Mae EleazarNo ratings yet
- Respiratory Medications ReviewerDocument4 pagesRespiratory Medications ReviewerKevin VillaranteNo ratings yet
- Drug Study 2Document8 pagesDrug Study 2rey_tengNo ratings yet
- Drug Book On EmergencyDocument21 pagesDrug Book On EmergencyDimpal Choudhary100% (4)
- Drug Study ShenDocument12 pagesDrug Study ShenLass KazeNo ratings yet
- Drug StudyDocument6 pagesDrug StudyChickz HunterNo ratings yet
- Drug Action Indication Adverse Effects Contraindications Nursing Considerations Ketorolac TromethamineDocument8 pagesDrug Action Indication Adverse Effects Contraindications Nursing Considerations Ketorolac TromethamineAiryn CanonNo ratings yet
- Atropine SulfateDocument5 pagesAtropine Sulfateapi-3797941100% (1)
- CefuroximeDocument11 pagesCefuroximeAlmira Ballesteros CestonaNo ratings yet
- MM MM MM MM MMM MMMMM M MM M MMMM MMMMM MMM MM MMM MM!M M!"M#MM MM M $M M %MMM MM "M "MM M MMM MDocument9 pagesMM MM MM MM MMM MMMMM M MM M MMMM MMMMM MMM MM MMM MM!M M!"M#MM MM M $M M %MMM MM "M "MM M MMM M배기숭No ratings yet
- Drug Study - LeptospirosisDocument19 pagesDrug Study - LeptospirosisCamille PinedaNo ratings yet
- 5 MG Iv BidDocument17 pages5 MG Iv BidhanzreinherNo ratings yet
- Labs Drug Study 1Document17 pagesLabs Drug Study 1Drei LanuzoNo ratings yet
- 24 Emergency DrugsDocument7 pages24 Emergency DrugsApple BelicanNo ratings yet
- Drug StudyDocument9 pagesDrug StudyShiara Ruth EdrosoloNo ratings yet
- AnalgesicDocument3 pagesAnalgesicAnnaMaeVelosoNo ratings yet
- NCP DrugDocument13 pagesNCP DrugMhar CamposanoNo ratings yet
- Pentazine, Phenazine, Phencen,, Phenoject-50, Prometh, Prorex, Prothazine, V-GanDocument34 pagesPentazine, Phenazine, Phencen,, Phenoject-50, Prometh, Prorex, Prothazine, V-GankotonashiNo ratings yet
- AmbroxolDocument4 pagesAmbroxoldiannuryandaNo ratings yet
- Drug 25Document17 pagesDrug 25carol_gigliotti24100% (1)
- Name of Drug Indications Action Contraindication Side Effects Adverse Side Effects Nursing ManagementDocument3 pagesName of Drug Indications Action Contraindication Side Effects Adverse Side Effects Nursing Managementjhappo31No ratings yet
- Drug StudyDocument5 pagesDrug StudyBea Andrea LarismaNo ratings yet
- Drug Study Format Ready To PrintDocument2 pagesDrug Study Format Ready To Printmay_hisolerNo ratings yet
- OB Med SheetDocument12 pagesOB Med SheetSam DanaNo ratings yet
- Generic Name: Albuterol Brand Name: Salbutamol, Proventil, Ventolin, Accuneb, Airet, Novo-SalbutamolDocument26 pagesGeneric Name: Albuterol Brand Name: Salbutamol, Proventil, Ventolin, Accuneb, Airet, Novo-SalbutamolAnna Joy Antone100% (1)
- Drug StudyDocument9 pagesDrug StudyShane Arroyo100% (1)
- FINAL Drug StudyDocument9 pagesFINAL Drug StudyKristen Leigh MarianoNo ratings yet
- Fluimucil 300mg / 3mlDocument3 pagesFluimucil 300mg / 3mlRezti PratiwiNo ratings yet
- Pedia Ward Drug Study...Document12 pagesPedia Ward Drug Study...Sheena Arnoco ToraynoNo ratings yet
- Diazepam, Lanoxin, Hemostan, NaprexDocument6 pagesDiazepam, Lanoxin, Hemostan, NaprexRene John Francisco100% (1)
- Summary of Product CharacteristicDocument5 pagesSummary of Product Characteristicresearch universalNo ratings yet
- HyosDocument8 pagesHyosAngie MandeoyaNo ratings yet
- Drug StudyDocument11 pagesDrug StudyKaloy KamaoNo ratings yet
- Drug Study HydralazineDocument10 pagesDrug Study HydralazineLuige AvilaNo ratings yet
- Emergency Drugs Crash CartDocument14 pagesEmergency Drugs Crash CartEricson SomeraNo ratings yet
- Drug StudyDocument6 pagesDrug StudyNajmah Saaban100% (1)
- 06 2014 Anticholinergic Agents - AtropineDocument6 pages06 2014 Anticholinergic Agents - AtropinemodayearNo ratings yet
- Drug Study..DokcyDocument7 pagesDrug Study..DokcyPeArl Peralta0% (1)
- Name of Drug/ Therapeutic Class Action Indications Side Effect Nursing Considerations ParacetamolDocument7 pagesName of Drug/ Therapeutic Class Action Indications Side Effect Nursing Considerations ParacetamolAnne Monique Moran OngjocoNo ratings yet
- DrugsDocument5 pagesDrugsVal Ian Palmes SumampongNo ratings yet
- Atropine Sulfate (Drug Study)Document3 pagesAtropine Sulfate (Drug Study)Franz.thenurse6888100% (1)
- Amphotericin B Deoxycholate (Conventional) - Drug Information - UpToDate-4Document4 pagesAmphotericin B Deoxycholate (Conventional) - Drug Information - UpToDate-4Vh TRNo ratings yet
- Drugs Acting On Respiratory SystemDocument15 pagesDrugs Acting On Respiratory SystemQusai BassamNo ratings yet
- Propranolol Hydro ChlorideDocument4 pagesPropranolol Hydro Chlorideapi-3797941No ratings yet
- Drug Study (Mefenamic Acid, Beetab, Esomeprazole Aspirin, Citicoline Plavix)Document6 pagesDrug Study (Mefenamic Acid, Beetab, Esomeprazole Aspirin, Citicoline Plavix)Patricia LuceroNo ratings yet
- Critical Care Medications: Anti-Arrhythmics Study Guide: Critical Care EssentialsFrom EverandCritical Care Medications: Anti-Arrhythmics Study Guide: Critical Care EssentialsNo ratings yet
- Winning against Prostatitis in the Elderly. Insider’s View of a Medical Worker.From EverandWinning against Prostatitis in the Elderly. Insider’s View of a Medical Worker.No ratings yet
- EthicsDocument10 pagesEthicsMadhubala JNo ratings yet
- IELTS Cause-Problem and Effect-Solution Model EssayDocument17 pagesIELTS Cause-Problem and Effect-Solution Model EssaySayaf RashadNo ratings yet
- A Study of Work Life Balance of Female Employee With Refrence To HDFC Bank at MoradabadDocument72 pagesA Study of Work Life Balance of Female Employee With Refrence To HDFC Bank at MoradabadbuddysmbdNo ratings yet
- Name: Rank: Date: Quiz On IMO Conventions 1. Write True or FalseDocument3 pagesName: Rank: Date: Quiz On IMO Conventions 1. Write True or FalseBisratNo ratings yet
- Chun-Hung Chen Kun-Cheng ChouDocument38 pagesChun-Hung Chen Kun-Cheng ChoutwnationNo ratings yet
- 4-CGC 1D1 Unit 3 Changing Populations - INDIGENOUS PEOPLE - Brief LookDocument46 pages4-CGC 1D1 Unit 3 Changing Populations - INDIGENOUS PEOPLE - Brief LookMichael KeNo ratings yet
- HOLANDA ALEX CFE103 Module4 ContextEngageActivitiesDocument4 pagesHOLANDA ALEX CFE103 Module4 ContextEngageActivitiesAsus LaptopNo ratings yet
- Practice 9-10-11Document12 pagesPractice 9-10-11cheplit123No ratings yet
- "After All, There Is Nothing As Interesting As People, and One Can Never Study Them Enough" Vincent Van GoghDocument38 pages"After All, There Is Nothing As Interesting As People, and One Can Never Study Them Enough" Vincent Van GoghAnonymous 1gH7ra9ANo ratings yet
- SynopsisDocument8 pagesSynopsisarunNo ratings yet
- Emergency Animal Hospital in Clifton Veterinary Emergency GroupDocument1 pageEmergency Animal Hospital in Clifton Veterinary Emergency Group6kqznycbyzNo ratings yet
- Technical Datasheet DHFFMDocument2 pagesTechnical Datasheet DHFFMSamerNo ratings yet
- Covid-19 Vaccination Microplan Date - (06-05-2021) District: Kanpur NagarDocument4 pagesCovid-19 Vaccination Microplan Date - (06-05-2021) District: Kanpur NagarAditi GuptaNo ratings yet
- BHS InggrisDocument5 pagesBHS InggrisDeajeng Febby AyuNo ratings yet
- ANALISIS PENERAPAN SISTEM LOCKOUTTAGOUT (LOTO) PADA BAGIAN OPERASI DAN PEMELIHARAAN DI PT. X TANJUNG EMAS KOTA SEMARANG (Berdasarkan Standar OSHA 29 CFR Part 1910.147 Dan Part 1910.333) PDFDocument11 pagesANALISIS PENERAPAN SISTEM LOCKOUTTAGOUT (LOTO) PADA BAGIAN OPERASI DAN PEMELIHARAAN DI PT. X TANJUNG EMAS KOTA SEMARANG (Berdasarkan Standar OSHA 29 CFR Part 1910.147 Dan Part 1910.333) PDFAfif Fayadh VictoryNo ratings yet
- Effective Leg Workout Exercises To Prevent Varicose Veins or Spider VeinsDocument2 pagesEffective Leg Workout Exercises To Prevent Varicose Veins or Spider VeinsLaser Vein ClinicNo ratings yet
- PREGNANCYDocument4 pagesPREGNANCYShaileeNo ratings yet
- Chapter 21 Muscle Blood FlowDocument17 pagesChapter 21 Muscle Blood Flowelmedina omeragicNo ratings yet
- FREE 8 Week Program For AthletesDocument13 pagesFREE 8 Week Program For AthletesHydra StortoNo ratings yet
- Betz Rebecca ResumeDocument2 pagesBetz Rebecca Resumeapi-316054946No ratings yet
- Future Biotechnology: The Eurobiotech JournalDocument4 pagesFuture Biotechnology: The Eurobiotech JournalsaraNo ratings yet
- Literature Review - Ashton Hyllengren 1Document4 pagesLiterature Review - Ashton Hyllengren 1api-549132151No ratings yet
- Impact of Covid19 On The Indian Stock MarketDocument6 pagesImpact of Covid19 On The Indian Stock MarketB31 Viraj PatilNo ratings yet
- Helping Children With Learning DisabilitiesDocument10 pagesHelping Children With Learning DisabilitiesUni KartikasariNo ratings yet
- Speed ManagementDocument284 pagesSpeed ManagementAdel AhmedNo ratings yet
- Synthesis of The Work of Enderlein, Etc PDFDocument3 pagesSynthesis of The Work of Enderlein, Etc PDFpaulxe100% (1)
- ICO-Ophthalmology Surgical Competency Assessment Rubric-SICS (ICO-OSCAR: SICS)Document3 pagesICO-Ophthalmology Surgical Competency Assessment Rubric-SICS (ICO-OSCAR: SICS)Andi Akhmad FaisalNo ratings yet
- Catlist MMDocument19 pagesCatlist MMWilfredVincentNo ratings yet