Professional Documents
Culture Documents
Polymyalgia Rheumatica: Fast Facts
Polymyalgia Rheumatica: Fast Facts
Uploaded by
ハルァン ファ烏山Copyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Otc Advisor PainDocument24 pagesOtc Advisor Painfarzad100% (2)
- Onicomicosis y Laser 2020. 3 Long de Onda.Document15 pagesOnicomicosis y Laser 2020. 3 Long de Onda.Luis Angel Díaz MarínNo ratings yet
- Signs of Mental Retardation in ChildrenDocument6 pagesSigns of Mental Retardation in ChildrenShine 2009No ratings yet
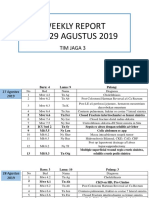
- WR Tim Jaga 3Document285 pagesWR Tim Jaga 3VincentiusNo ratings yet
- Amniotic Fluid and ItDocument8 pagesAmniotic Fluid and ItSaman SarKoNo ratings yet
- Cognitive-Behavioral Therapies For Personality DisordersDocument8 pagesCognitive-Behavioral Therapies For Personality DisordersTeodor CiobanuNo ratings yet
- Chlorpheniramine MaleateDocument3 pagesChlorpheniramine Maleateapi-3797941100% (1)
- 155 PenyakitDocument112 pages155 Penyakitpuskesmas kedungdoroNo ratings yet
- Thesis PoDocument5 pagesThesis PoJane SandovalNo ratings yet
- Duloxetine PDFDocument4 pagesDuloxetine PDFscribdseewalNo ratings yet
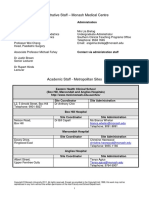
- DR Ashfaq ResumeDocument1 pageDR Ashfaq Resumedidoba7635No ratings yet
- What Is PresbycusisDocument4 pagesWhat Is PresbycusisNisa UcilNo ratings yet
- dm2020 0123Document47 pagesdm2020 0123Franchise AlienNo ratings yet
- Emedica MRCGP AKT Curriculum ChecklistDocument42 pagesEmedica MRCGP AKT Curriculum ChecklistSana Mustafa100% (1)
- Resume - Hamid Kermani MoakharDocument2 pagesResume - Hamid Kermani Moakharmohammadrezahajian12191No ratings yet
- HSD Sept22 Clin Chem Saqs Essay and Case Studies Exam PapersDocument10 pagesHSD Sept22 Clin Chem Saqs Essay and Case Studies Exam PapersYusuph MipawaNo ratings yet
- Ohmega: Ambulatory Impedance-pH RecorderDocument4 pagesOhmega: Ambulatory Impedance-pH RecorderMoas GabrounNo ratings yet
- Neoplasias Cisticas Do PancreasDocument37 pagesNeoplasias Cisticas Do PancreasMoises BitencourtNo ratings yet
- Dress Syndrome A Review and UpdateDocument5 pagesDress Syndrome A Review and UpdateCarlos Alberto Torres LópezNo ratings yet
- YCYSt DocumentDocument24 pagesYCYSt DocumentDodo AlsunaidiNo ratings yet
- Ulse Ximetry: Steven J. BarkerDocument17 pagesUlse Ximetry: Steven J. BarkerBRYAN RAFAEL ALEMAN HERNANDEZNo ratings yet
- Treating Vulvovaginal Atrophy Genitourinary Syndrome of Menopause How Important Is Vaginal Lubricant and Moisturizer CompositionDocument12 pagesTreating Vulvovaginal Atrophy Genitourinary Syndrome of Menopause How Important Is Vaginal Lubricant and Moisturizer CompositionPELVIC ANGELNo ratings yet
- Childrens Health Discipline GuideDocument41 pagesChildrens Health Discipline GuidegurkibajwaNo ratings yet
- BronchopneumoniaDocument11 pagesBronchopneumoniaDesiree GuerraNo ratings yet
- Immunopathology of Vesicular Cutaneous Lupus Erythematosus in The Rough Collie and Shetland Sheepdog - A Canine Homologue of SubacuteDocument10 pagesImmunopathology of Vesicular Cutaneous Lupus Erythematosus in The Rough Collie and Shetland Sheepdog - A Canine Homologue of SubacutejenNo ratings yet
- Product Monograph - Zoledronic Acid For Injection ConcentrateDocument58 pagesProduct Monograph - Zoledronic Acid For Injection ConcentrateMisgi Candra DasaNo ratings yet
- Incisions and ClosuresDocument14 pagesIncisions and ClosuresSalazar ÁngelNo ratings yet
- 342 FullDocument9 pages342 FulldrdevvratNo ratings yet
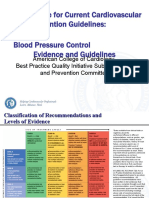
- 3 ACC Prevention Blood PressureDocument69 pages3 ACC Prevention Blood PressureMelissa Delgado100% (1)
- Jan 24 Skeletal Embryology and Limb Growth Stanmore Dr. Riego de Dios CPT TiongsonDocument3 pagesJan 24 Skeletal Embryology and Limb Growth Stanmore Dr. Riego de Dios CPT TiongsonMarlon MejiaNo ratings yet
Polymyalgia Rheumatica: Fast Facts
Polymyalgia Rheumatica: Fast Facts
Uploaded by
ハルァン ファ烏山Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Polymyalgia Rheumatica: Fast Facts
Polymyalgia Rheumatica: Fast Facts
Uploaded by
ハルァン ファ烏山Copyright:
Available Formats
Polymyalgia Rheumatica Page 1
Polymyalgia Rheumatica
Polymyalgia rheumatica (sometimes referred to as PMR) is a common cause of widespread aching and
stiffness in older adults. Because PMR does not often cause swollen joints, it may be hard to recognize.
PMR may occur with another health problem, giant cell arteritis.
Fast facts
PMR affects only adults over the age of 50.
Aching and stiffness in PMR affect the upper arms, neck, buttocks and thighs, and are most
severe in the morning.
These symptoms respond quickly and completely to low doses of corticosteroids.
What is polymyalgia rheumatica?
The typical symptoms (what you feel) of PMR are aching and stiffness about the upper arms, neck, lower
back and thighs. Symptoms tend to come on quickly, over a few days or weeks, and sometimes even
overnight. Both sides of the body are equally affected. Involvement of the upper arms, with trouble
raising them above the shoulders, is common. Sometimes, aching occurs at joints such as the hands and
wrists.
Achiness is always worse in the morning and improves as the day goes by. Yet inactivity, such as a long
car ride or sitting too long in one position, may cause stiffness to return. Stiffness may be so severe that
it causes any of these problems:
Disturbed sleep
Trouble getting dressed in the morning (for instance, putting on a jacket or bending over to pull
on socks and shoes)
Problems getting up from a sofa or in and out of a car
What causes polymyalgia rheumatica?
The cause of PMR is unknown. PMR does not result from side effects of medications. The abrupt onset
of symptoms suggests the possibility of an infection but, so far, none has been found. Myalgia comes
Polymyalgia Rheumatica Page 2
from the Greek word for muscle pain. However, specific tests of the muscles, such as a blood test for
muscle enzymes or a muscle biopsy (surgical removal of a small piece of muscle for inspection under a
microscope), are all normal.
Recent research suggests that inflammation in PMR involves the shoulder and hip joints themselves, and
the bursae (or sacs) around these joints. So pains at the upper arms and thighs, in fact, start at the
nearby shoulder and hip joints. This is what doctors call referred pain.
PMR should not be confused with fibromyalgia, a poorly understood health problem that affects mainly
younger adults.
Who gets polymyalgia rheumatica?
PMR affects older adults over the age of 50. The
average age at onset (start) of symptoms is 70, so
people who have PMR may be in their 80s or even
older. The disease affects women somewhat more
often than men. It is more frequent in whites than
nonwhites, but all races can get PMR.
How is polymyalgia rheumatica diagnosed?
In PMR, results of blood tests to detect inflammation
are most often abnormally high. One such test is the
erythrocyte sedimentation rate, also called sed rate.
Another test is the C-reactive protein, or CRP. Both
tests may be very elevated in PMR but, in some
patients, these tests may have normal or only slightly
high results.
PMR can be hard to diagnose. Your health care
providers should rule out other health problems, such
as rheumatoid arthritis.
How is polymyalgia rheumatica treated?
If your doctor strongly suspects PMR, you will receive a
trial of low-dose corticosteroids. Often, the dose is 10
15 milligrams per day of prednisone (Deltasone,
Orasone, etc.). If PMR is present, the medicine quickly
relieves stiffness. The response to corticosteroids can
be dramatic. Sometimes patients are better after only one dose. Improvement can be slower, though.
But, if symptoms do not go away after 2 or 3 weeks of treatment, the diagnosis of PMR is not likely, and
your doctor will consider other causes of your illness.
Nonsteroidal anti-inflammatory drugs (commonly called NSAIDs), such as ibuprofen (Advil, Motrin,
etc.) and naproxen (Naprosyn, Aleve), are not effective in treating PMR.
When your symptoms are under control, your doctor will slowly decrease (taper) the dose of
corticosteroid medicine. The goal is to find the lowest dose that keeps you comfortable. Some people
can stop taking corticosteroids within a year. Others, though, will need a small amount of this medicine
In PMR, the aching is located primarily around
the shoulders and hips.
Polymyalgia Rheumatica Page 3
for 23 years, to keep aching and stiffness under control. Symptoms can recur. Because the symptoms
of PMR are sensitive to even small changes in the dose of corticosteroids, your doctor should direct the
gradual decrease of this medicine.
Living with polymyalgia rheumatica
Once stiffness has gone away, you can resume all normal activities, including exercise.
Even low doses of corticosteroids can cause side effects. These include higher blood sugar, weight gain,
sleeplessness, osteoporosis (bone loss), cataracts, thinning of the skin and bruising. Checking for these
problems, including bone density testing, is an important part of follow-up visits with your doctor. Older
patients may need medicine to prevent osteoporosis.
PMR can occur with a more serious condition, giant cell arteritis. Thus, see your doctor right away if you
have PMR and you get symptoms of headache, changes in vision or fever.
Points to remember
Aching and stiffness develop quickly in PMR, and are most
common about the shoulders and upper arms.
Symptoms are worse in the morning.
Symptoms respond promptly to low doses of
corticosteroids, but may recur as the dose is lowered.
The rheumatologist's role in the treatment of polymyalgia
rheumatica
PMR may be hard to diagnose. Because rheumatologists are
experts in diseases of the joints, muscles and bones. they can
recognize the diagnosis of PMR, and expertly manage its
treatment .
To find a rheumatologist
For more information about rheumatologists, click here.
Learn more about rheumatologists and rheumatology health professionals.
For more information
The American College of Rheumatology has compiled this list to give you a starting point for your own
additional research. The ACR does not endorse or maintain these Web sites, and is not responsible for
any information or claims provided on them. It is always best to talk with your rheumatologist for more
information and before making any decisions about your care.
The Arthritis Foundation
www.arthritis.org
National Library of Medicine
www.nlm.nih.gov/medlineplus/polymyalgiarheumatica.html
Once stiffness has gone away, you
can resume normal activities.
Polymyalgia Rheumatica Page 4
National Institute of Arthritis and Musculoskeletal and Skin Diseases Information Clearinghouse
www.niams.nih.gov/Health_Info/Polymyalgia
Updated February 2013
Written by William P. Docken, MD, and reviewed by the American College of Rheumatology Communications and
Marketing Committee.
This patient fact sheet is provided for general education only. Individuals should consult a qualified health care
provider for professional medical advice, diagnosis and treatment of a medical or health condition.
2013 American College of Rheumatology
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Otc Advisor PainDocument24 pagesOtc Advisor Painfarzad100% (2)
- Onicomicosis y Laser 2020. 3 Long de Onda.Document15 pagesOnicomicosis y Laser 2020. 3 Long de Onda.Luis Angel Díaz MarínNo ratings yet
- Signs of Mental Retardation in ChildrenDocument6 pagesSigns of Mental Retardation in ChildrenShine 2009No ratings yet
- WR Tim Jaga 3Document285 pagesWR Tim Jaga 3VincentiusNo ratings yet
- Amniotic Fluid and ItDocument8 pagesAmniotic Fluid and ItSaman SarKoNo ratings yet
- Cognitive-Behavioral Therapies For Personality DisordersDocument8 pagesCognitive-Behavioral Therapies For Personality DisordersTeodor CiobanuNo ratings yet
- Chlorpheniramine MaleateDocument3 pagesChlorpheniramine Maleateapi-3797941100% (1)
- 155 PenyakitDocument112 pages155 Penyakitpuskesmas kedungdoroNo ratings yet
- Thesis PoDocument5 pagesThesis PoJane SandovalNo ratings yet
- Duloxetine PDFDocument4 pagesDuloxetine PDFscribdseewalNo ratings yet
- DR Ashfaq ResumeDocument1 pageDR Ashfaq Resumedidoba7635No ratings yet
- What Is PresbycusisDocument4 pagesWhat Is PresbycusisNisa UcilNo ratings yet
- dm2020 0123Document47 pagesdm2020 0123Franchise AlienNo ratings yet
- Emedica MRCGP AKT Curriculum ChecklistDocument42 pagesEmedica MRCGP AKT Curriculum ChecklistSana Mustafa100% (1)
- Resume - Hamid Kermani MoakharDocument2 pagesResume - Hamid Kermani Moakharmohammadrezahajian12191No ratings yet
- HSD Sept22 Clin Chem Saqs Essay and Case Studies Exam PapersDocument10 pagesHSD Sept22 Clin Chem Saqs Essay and Case Studies Exam PapersYusuph MipawaNo ratings yet
- Ohmega: Ambulatory Impedance-pH RecorderDocument4 pagesOhmega: Ambulatory Impedance-pH RecorderMoas GabrounNo ratings yet
- Neoplasias Cisticas Do PancreasDocument37 pagesNeoplasias Cisticas Do PancreasMoises BitencourtNo ratings yet
- Dress Syndrome A Review and UpdateDocument5 pagesDress Syndrome A Review and UpdateCarlos Alberto Torres LópezNo ratings yet
- YCYSt DocumentDocument24 pagesYCYSt DocumentDodo AlsunaidiNo ratings yet
- Ulse Ximetry: Steven J. BarkerDocument17 pagesUlse Ximetry: Steven J. BarkerBRYAN RAFAEL ALEMAN HERNANDEZNo ratings yet
- Treating Vulvovaginal Atrophy Genitourinary Syndrome of Menopause How Important Is Vaginal Lubricant and Moisturizer CompositionDocument12 pagesTreating Vulvovaginal Atrophy Genitourinary Syndrome of Menopause How Important Is Vaginal Lubricant and Moisturizer CompositionPELVIC ANGELNo ratings yet
- Childrens Health Discipline GuideDocument41 pagesChildrens Health Discipline GuidegurkibajwaNo ratings yet
- BronchopneumoniaDocument11 pagesBronchopneumoniaDesiree GuerraNo ratings yet
- Immunopathology of Vesicular Cutaneous Lupus Erythematosus in The Rough Collie and Shetland Sheepdog - A Canine Homologue of SubacuteDocument10 pagesImmunopathology of Vesicular Cutaneous Lupus Erythematosus in The Rough Collie and Shetland Sheepdog - A Canine Homologue of SubacutejenNo ratings yet
- Product Monograph - Zoledronic Acid For Injection ConcentrateDocument58 pagesProduct Monograph - Zoledronic Acid For Injection ConcentrateMisgi Candra DasaNo ratings yet
- Incisions and ClosuresDocument14 pagesIncisions and ClosuresSalazar ÁngelNo ratings yet
- 342 FullDocument9 pages342 FulldrdevvratNo ratings yet
- 3 ACC Prevention Blood PressureDocument69 pages3 ACC Prevention Blood PressureMelissa Delgado100% (1)
- Jan 24 Skeletal Embryology and Limb Growth Stanmore Dr. Riego de Dios CPT TiongsonDocument3 pagesJan 24 Skeletal Embryology and Limb Growth Stanmore Dr. Riego de Dios CPT TiongsonMarlon MejiaNo ratings yet