Professional Documents
Culture Documents
Pathophysiology of Fracture
Pathophysiology of Fracture
Uploaded by
Lawrence Espinosa82%(11)82% found this document useful (11 votes)
9K views2 pagesWhen a bone fractures, it disrupts the continuity of the bone and surrounding soft tissues like muscles and blood vessels. This causes bleeding and the formation of a hematoma in the marrow canal. The bone tissue near the fracture site dies, stimulating an inflammatory response. Within 48 hours, new blood vessels invade the fracture site and bone-forming cells begin creating callus, or woven bone, to repair the fracture.
Original Description:
Pathophysiology of fracture
Original Title
44135497 Pathophysiology of Fracture
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentWhen a bone fractures, it disrupts the continuity of the bone and surrounding soft tissues like muscles and blood vessels. This causes bleeding and the formation of a hematoma in the marrow canal. The bone tissue near the fracture site dies, stimulating an inflammatory response. Within 48 hours, new blood vessels invade the fracture site and bone-forming cells begin creating callus, or woven bone, to repair the fracture.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
82%(11)82% found this document useful (11 votes)
9K views2 pagesPathophysiology of Fracture
Pathophysiology of Fracture
Uploaded by
Lawrence EspinosaWhen a bone fractures, it disrupts the continuity of the bone and surrounding soft tissues like muscles and blood vessels. This causes bleeding and the formation of a hematoma in the marrow canal. The bone tissue near the fracture site dies, stimulating an inflammatory response. Within 48 hours, new blood vessels invade the fracture site and bone-forming cells begin creating callus, or woven bone, to repair the fracture.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 2
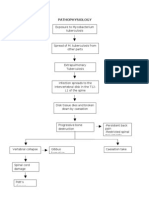
PATHOPHYSIOLOGY OF FRACTURE
Stress placed on a bone,
exceeds the bone ability to absorb it
Injury in the bone
Disruption in the continuity of bone
Disruption of muscle and blood vessels attached
to the ends of the bone
Soft tissue damage
Bleeding
Hematoma forms in medullary canal
Bone tissue surround the fractured site dies
Inflammatory response
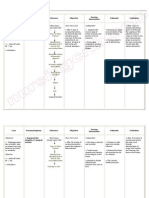
When a bone is broken, the periosteum and blood vessels in the cortex,
marrow, and surrounding soft tissues are disrupted. Bleeding occurs
from the damaged ends of the bone and from the neighboring soft tissue.
A clot (hematoma) forms within the medullary canal, between the
fractured ends of the bone, and beneath the periosteum. Bone tissue
immediately adjacent to the fracture dies. This necrotic tissue along with
any debris in the fracture area stimulates an intense inflammatory
response characterized by vasodilation, exudation of plasma and
leukocytes, and infiltration by inflammatory leukocytes and mast cells.
Within 48 hours after the injury, vascular tissue invades the fracture area
from surrounding soft tissue and the marrow cavity, and blood flow to
the entire bone is increased. Bone-forming cells in the periosteum,
endosteum, and marrow are activated to produce subperiosteal procallus
along the outer surface of the shaft and over the broken ends of the bone.
Osteoblasts within the procallus synthesize collagen and matrix, which
becomes mineralized to form callus (woven bone). As the repair process
continues, remodeling occurs, during which unnecessary callus is
resorbed and trabeculae are formed along lines of stress. Except for the
liver, bone is unique among all body tissues in that it will form new
bone, not scar tissue, when it heals after a fracture."
You might also like
- Bone Fracture PathophysiologyDocument1 pageBone Fracture PathophysiologyRay Mahawi100% (2)
- Pathophysiology of FractureDocument1 pagePathophysiology of FractureShayne Jessemae Almario100% (3)
- Pathophysiology of FractureDocument2 pagesPathophysiology of FractureAnne Lorraine Bringas93% (27)
- Pathophysiology of OsteosarcomaDocument5 pagesPathophysiology of Osteosarcomafanvicfay100% (9)
- Pathophysiology of Spinal Cord Injury 1Document1 pagePathophysiology of Spinal Cord Injury 1kristel_nicole18yaho67% (6)
- Hernia PathophysiologyDocument1 pageHernia PathophysiologyIvan Louise Fajardo Maniquiz86% (7)
- Pathophysiology OsteosarcomaDocument4 pagesPathophysiology OsteosarcomaGladys Barcelona0% (1)
- Case Study - FractureDocument35 pagesCase Study - FractureJo-anne Cordero100% (4)
- Pott's DiseaseDocument30 pagesPott's DiseaseLucila Lugo100% (1)
- Pathophysiology of POTT's DiseaseDocument1 pagePathophysiology of POTT's DiseaseLeLi CortezNo ratings yet
- Nursing Care of Patients Undergoing Orthopedic SurgeryDocument27 pagesNursing Care of Patients Undergoing Orthopedic SurgeryKwabena Amankwa100% (5)
- Fracture PathophysiologyDocument1 pageFracture PathophysiologyIrene Joy Gomez100% (2)
- Pathophysiology of FractureDocument1 pagePathophysiology of FractureMarion Mendez100% (1)
- Pathophysiology of FractureDocument2 pagesPathophysiology of FractureVenus Tagaan UcatNo ratings yet
- Pott's DiseaseDocument17 pagesPott's DiseaseRheegell Ellar-Fuertes100% (1)
- PathophysiologyDocument1 pagePathophysiologyRj MagpayoNo ratings yet
- NCP OrthoDocument5 pagesNCP OrthoMyluck Elaine Wailan100% (4)
- Nursing Care Plan - Posterior Hip Dislocation LeftDocument1 pageNursing Care Plan - Posterior Hip Dislocation LeftJasmin Jacob100% (7)
- Balance Skeletal TractionDocument4 pagesBalance Skeletal TractionIris BalinoNo ratings yet
- Pott's DiseaseDocument8 pagesPott's DiseaseBij HilarioNo ratings yet
- Nursing Care Plan Impaire Physical MobilityDocument2 pagesNursing Care Plan Impaire Physical Mobilityderic90% (10)
- Case of OsteosarcomaDocument25 pagesCase of Osteosarcomadocs2009100% (3)
- Osteomyelitis Case StudyDocument41 pagesOsteomyelitis Case StudyJohn Bernard Ting Tizon100% (2)
- Fracture Healing in Cortical and Cancellous BoneDocument63 pagesFracture Healing in Cortical and Cancellous BonePramod Thottimane0% (1)
- Pathophysiology FracturesDocument2 pagesPathophysiology FracturesSewyel Garburi71% (7)
- Pathophysiology Bone Fracture (Tibia)Document1 pagePathophysiology Bone Fracture (Tibia)Brainan Aquino0% (2)
- Iii. Clinical Discussion of The Disease A. Pathophysiology of Fracture I. (Book Based)Document4 pagesIii. Clinical Discussion of The Disease A. Pathophysiology of Fracture I. (Book Based)Lemuel GuevarraNo ratings yet
- Post Open Reduction Internal Fixation PathophysiologyDocument3 pagesPost Open Reduction Internal Fixation PathophysiologyRizalyn QuindipanNo ratings yet
- Pathophysiology OsteosarcomaDocument2 pagesPathophysiology OsteosarcomaVernadeth Dumagat50% (2)
- NCP: FracturesDocument21 pagesNCP: FracturesJavie100% (1)
- Potts DiseaseDocument5 pagesPotts Diseasemyla-elmarie100% (1)
- Pa Tho Physiology of Ovarian New GrowthDocument2 pagesPa Tho Physiology of Ovarian New Growthhaniellan100% (5)
- NCP OsteomyelitisDocument3 pagesNCP OsteomyelitisClariss Alota100% (2)
- Nursing Care Plan Orthopedic Philipine CenterDocument4 pagesNursing Care Plan Orthopedic Philipine CenterAnonymous NZTQVgjaNo ratings yet
- OsteomyelitisDocument1 pageOsteomyelitisJohara Mae De RamaNo ratings yet
- Pott's DiseaseDocument8 pagesPott's DiseaseLorebell100% (2)
- Balanced Suspension Skeletal TractionDocument4 pagesBalanced Suspension Skeletal Tractionfegerilene100% (1)
- Common Cause or Etiology of Pott's DiseaseDocument5 pagesCommon Cause or Etiology of Pott's DiseaseStan Aves GarciaNo ratings yet
- Pott's Disease NCPDocument7 pagesPott's Disease NCPkristel_nicole18yahoNo ratings yet
- Pa Tho Physiology of Open FractureDocument2 pagesPa Tho Physiology of Open FracturegiffersonbNo ratings yet
- OsteomyelitisDocument11 pagesOsteomyelitisLorebell100% (7)
- Pathophysiology of OsteomyelitisDocument3 pagesPathophysiology of OsteomyelitisJhon Jerric Pante Aguinaldo100% (1)
- Casts. Braces. TractionDocument3 pagesCasts. Braces. TractionClancy Anne Garcia Naval100% (1)
- Case Study 1Document3 pagesCase Study 1api-481780857No ratings yet
- Handout - Bone Anatomy and Healing - Nlogo - HighDocument11 pagesHandout - Bone Anatomy and Healing - Nlogo - HighlevimacoNo ratings yet
- Fracture Healing and BonegraftingDocument76 pagesFracture Healing and BonegraftingJio AmurNo ratings yet
- Topic 5. Bone Microscopic Anatomy and Devt 1Document24 pagesTopic 5. Bone Microscopic Anatomy and Devt 1Janine Jerica JontilanoNo ratings yet
- Bone Healing ProcessDocument21 pagesBone Healing ProcessWing YenNo ratings yet
- Femur in Lower Limb) .: Ankle)Document2 pagesFemur in Lower Limb) .: Ankle)Pekeng IlokanoNo ratings yet
- 3 Bone Injury InflammationDocument24 pages3 Bone Injury InflammationGwyneth Koleen LopezNo ratings yet
- Bone Formation & GrowthDocument3 pagesBone Formation & GrowtherinNo ratings yet
- Chapter 6 Content Review Questions 1-8Document3 pagesChapter 6 Content Review Questions 1-8Rhonique MorganNo ratings yet
- Bone Formation - Ossification 2 PDFDocument35 pagesBone Formation - Ossification 2 PDFalan100% (1)
- Lecture: Histology of Cartilage and BoneDocument49 pagesLecture: Histology of Cartilage and BonevictorNo ratings yet
- Skeletal SystemDocument104 pagesSkeletal Systemsyafi zulNo ratings yet
- Bones and Skeletal Tissues Skeletal CartilagesDocument7 pagesBones and Skeletal Tissues Skeletal CartilagesChelsey ReaumeNo ratings yet
- Bone Development: Osteogenesis (Ossification) Endochondral OssificationDocument2 pagesBone Development: Osteogenesis (Ossification) Endochondral OssificationVanshika SethiNo ratings yet
- Histogenesis of BoneDocument6 pagesHistogenesis of BoneAlya Putri KhairaniNo ratings yet
- BonesDocument2 pagesBonesDDNo ratings yet
- 1) - Bone As An OrganDocument3 pages1) - Bone As An OrganSofia LoveNo ratings yet
- Mbol CHNDocument38 pagesMbol CHNLawrence EspinosaNo ratings yet
- Theme Resource Changer InstructionsDocument1 pageTheme Resource Changer InstructionsLawrence EspinosaNo ratings yet
- Mark Jetro Bondad AboDocument3 pagesMark Jetro Bondad AboLawrence EspinosaNo ratings yet
- FNCP Barefooted (Revised)Document2 pagesFNCP Barefooted (Revised)Lawrence Espinosa50% (2)