Professional Documents
Culture Documents
Assesment Stroke Without CT Scan (Greek Score, Alen Score
Assesment Stroke Without CT Scan (Greek Score, Alen Score
Uploaded by
Missing ManCopyright:
Available Formats
You might also like
- MR Clean Late LancetDocument10 pagesMR Clean Late LancetLetícia JanuziNo ratings yet
- Journal 4Document5 pagesJournal 4dr. Nadia Salsabila100% (1)
- Boysen-Osborn (2018) PDFDocument11 pagesBoysen-Osborn (2018) PDFBryan TorresNo ratings yet
- Acute Stroke Treatment - CPM 8th EdDocument22 pagesAcute Stroke Treatment - CPM 8th EdSuresh ShresthaNo ratings yet
- 3046-Article Text-5935-1-10-20200724Document7 pages3046-Article Text-5935-1-10-20200724Kirubel DeribNo ratings yet
- Siriraj Stroke ScoreDocument3 pagesSiriraj Stroke ScoreHendy SetiawanNo ratings yet
- The Recognition of Stroke in The Emergency Room ROSIERDocument8 pagesThe Recognition of Stroke in The Emergency Room ROSIERcristian viretto100% (1)
- Absen Kelas X - 2020-2021 RNDocument10 pagesAbsen Kelas X - 2020-2021 RNZickra Awla0% (1)
- An Introduction DTIDocument23 pagesAn Introduction DTIAliceNo ratings yet
- Cardiac Radiosurgery (CyberHeart™) For Treatment of Arrhythmia: Physiologic and Histopathologic Correlation in The Porcine ModelDocument28 pagesCardiac Radiosurgery (CyberHeart™) For Treatment of Arrhythmia: Physiologic and Histopathologic Correlation in The Porcine ModelCureusNo ratings yet
- Special Investigation in RadiographyDocument76 pagesSpecial Investigation in RadiographyOluseyiNo ratings yet
- Abdominal RadiographDocument36 pagesAbdominal RadiographLarasati FadhlenNo ratings yet
- Computerized Tomography (CT) Scan: Indication Abnormal ResultsDocument7 pagesComputerized Tomography (CT) Scan: Indication Abnormal ResultsVanessa VillanuevaNo ratings yet
- Hysterosalpingography A Re - Emerging Study With CDocument7 pagesHysterosalpingography A Re - Emerging Study With CTuyul Yelsi 1No ratings yet
- Bishop Rehabilitation and Nursing Center Inspection ReportDocument117 pagesBishop Rehabilitation and Nursing Center Inspection ReportJames MulderNo ratings yet
- Medical Malpractice and Compensation in The UKDocument33 pagesMedical Malpractice and Compensation in The UKgun rayNo ratings yet
- Analisis Efisiensi Celah Shutter Kolimator Tabung Sinar X Di Tiga Instalasi Radiologi Lahan PKL Prodi D3 Radiologi Unisa YogyakartaDocument7 pagesAnalisis Efisiensi Celah Shutter Kolimator Tabung Sinar X Di Tiga Instalasi Radiologi Lahan PKL Prodi D3 Radiologi Unisa YogyakartaNoveliaNo ratings yet
- RS CoachingDocument201 pagesRS CoachingHalia MalicNo ratings yet
- Modified Rankin Scale How To PDFDocument15 pagesModified Rankin Scale How To PDFKNI Maret 2023No ratings yet
- Allreports PDFDocument2 pagesAllreports PDFNeena SinghNo ratings yet
- Coronary Artery Diseases - Ilham PDocument43 pagesCoronary Artery Diseases - Ilham PKeputrian FKUPNo ratings yet
- Medel SonataDocument54 pagesMedel Sonatamaclab macNo ratings yet
- Dual Source CT Imaging PDFDocument275 pagesDual Source CT Imaging PDFAnisa SetiawatiNo ratings yet
- General-Mrcs-Recalls-Paper-2-From-Previous-Exams .Document79 pagesGeneral-Mrcs-Recalls-Paper-2-From-Previous-Exams .Victor FabunmiNo ratings yet
- Loopography Examination For Colon Cancer 7c394e77Document11 pagesLoopography Examination For Colon Cancer 7c394e77N. Camelya FirdausNo ratings yet
- Laboratory Blood Request FormDocument2 pagesLaboratory Blood Request FormIsaac AgbemafleNo ratings yet
- Practicing Medicine in FinlandDocument12 pagesPracticing Medicine in FinlandDr Richard AnekweNo ratings yet
- 1.1. Pocus en Emg y Critical Care 2018 PDFDocument8 pages1.1. Pocus en Emg y Critical Care 2018 PDFEmergencias RebagliatiNo ratings yet
- Abstracts From The Global Embolization Sympo 2021 Journal of Vascular and inDocument21 pagesAbstracts From The Global Embolization Sympo 2021 Journal of Vascular and infreedy freedyNo ratings yet
- Anaesthesia For Hepatic Resection SurgeryDocument15 pagesAnaesthesia For Hepatic Resection SurgeryDianita P Ñáñez VaronaNo ratings yet
- Perioperative Risk Stratification and ModificationDocument23 pagesPerioperative Risk Stratification and ModificationDianita P Ñáñez VaronaNo ratings yet
- Review Jurnal RadiologiDocument10 pagesReview Jurnal RadiologiM Benni KadapihNo ratings yet
- A Thesis ProtocolDocument29 pagesA Thesis ProtocolMelvin JohnNo ratings yet
- Jay Ushin 2018Document92 pagesJay Ushin 2018Puneet367No ratings yet
- SKB Radiografer & Aipri I (93 Soal) - Beserta Jawaban PDFDocument55 pagesSKB Radiografer & Aipri I (93 Soal) - Beserta Jawaban PDFiwan hardiansyahNo ratings yet
- Compilation Questions of Theory Part One 04-1Document34 pagesCompilation Questions of Theory Part One 04-1Rebecca WongNo ratings yet
- Medical Ethics Principles, 14 Januari 2018Document16 pagesMedical Ethics Principles, 14 Januari 2018Adji SuwandonoNo ratings yet
- Siriraj 1Document5 pagesSiriraj 1Winda MelatiNo ratings yet
- Lack of Clinical Utility of The Siriraj Stroke Score: Riginal RticleDocument4 pagesLack of Clinical Utility of The Siriraj Stroke Score: Riginal RticleWinda MelatiNo ratings yet
- Siriraj 2Document4 pagesSiriraj 2Winda MelatiNo ratings yet
- Siriraj Stroke Score PDFDocument11 pagesSiriraj Stroke Score PDFGalant Lefebvre 戈蓝No ratings yet
- Stroke Score 2004Document4 pagesStroke Score 2004Pebrian SyahNo ratings yet
- IL 6 and StrokeDocument7 pagesIL 6 and StrokeDian Laras SuminarNo ratings yet
- A Three-Item Scale For The Early Prediction of Stroke RecoveryDocument5 pagesA Three-Item Scale For The Early Prediction of Stroke RecoverydoktergigikoeNo ratings yet
- An Integer-Based Score To PredictDocument21 pagesAn Integer-Based Score To PredictMichael BentonNo ratings yet
- Comparison of Neurological Clinical Manifestation in Patients With Hemorrhagic and Ischemic StrokeDocument5 pagesComparison of Neurological Clinical Manifestation in Patients With Hemorrhagic and Ischemic StrokeDessy FarwasNo ratings yet
- Serum CytokinesDocument7 pagesSerum CytokinesEvy Yulia KusmayantiNo ratings yet
- Antiagregacion Vs Anticoagulacion en DiseccionDocument4 pagesAntiagregacion Vs Anticoagulacion en DiseccionCarlos Alberto CorredorNo ratings yet
- Early Prediction of Severity StrokeDocument11 pagesEarly Prediction of Severity StrokeainihanifiahNo ratings yet
- Main 51 ???Document5 pagesMain 51 ???pokharelriwaj82No ratings yet
- Medip, IJAM-2391 ODocument4 pagesMedip, IJAM-2391 OalitrnfbNo ratings yet
- Missed Ischemic Stroke Diagnosis in The Emergency Department by Emergency Medicine and Neurology ServicesDocument7 pagesMissed Ischemic Stroke Diagnosis in The Emergency Department by Emergency Medicine and Neurology ServicesReyhansyah RachmadhyanNo ratings yet
- Comparison of Clinical Diagnosis With Computed Tomography in Ascertaining Type of StrokeDocument3 pagesComparison of Clinical Diagnosis With Computed Tomography in Ascertaining Type of StrokeDyah Wulan RamadhaniNo ratings yet
- Efecto de Estatinas en RecurrencaDocument4 pagesEfecto de Estatinas en RecurrencaLeonela Ramirez Almanza y Lina Maria Ossa HerreraNo ratings yet
- Role of Interleukin-6 in Ischemic Stroke OutcomeDocument7 pagesRole of Interleukin-6 in Ischemic Stroke OutcomeSalma SalmaNo ratings yet
- NIHSS Cut-Point For Predicting Outcome in Supra-Vs Infratentorial Acute Ischemic StrokeDocument8 pagesNIHSS Cut-Point For Predicting Outcome in Supra-Vs Infratentorial Acute Ischemic StrokePutri NurdiyantiNo ratings yet
- Accuracy of Physical Signs For Detecting Meningitis - A Hospital-Based Diagnostic Accuracy StudyDocument7 pagesAccuracy of Physical Signs For Detecting Meningitis - A Hospital-Based Diagnostic Accuracy StudyNanda AlvionitaNo ratings yet
- Mathematics 10 02049 v3Document17 pagesMathematics 10 02049 v3Dhavala Shree B JainNo ratings yet
- Flat-Head Positioning Increases Cerebral Blood Flow in Anterior Circulation Acute Ischemic Stroke. A Cluster Randomized Phase Iib TrialDocument12 pagesFlat-Head Positioning Increases Cerebral Blood Flow in Anterior Circulation Acute Ischemic Stroke. A Cluster Randomized Phase Iib TrialNaufal HilmiNo ratings yet
- Glyceryl Trinitrate For Acute Intracerebral HemorrhageDocument21 pagesGlyceryl Trinitrate For Acute Intracerebral HemorrhageAhmad Al-atthosNo ratings yet
- Unit3&4 Network TheoramsDocument73 pagesUnit3&4 Network TheoramsBALAKRISHNA PERALANo ratings yet
- Attach 8 - CPDS Type 2ADocument401 pagesAttach 8 - CPDS Type 2AGlenn Adalia BonitaNo ratings yet
- PFI ES-5-1993 Cleaning of Fabricated PipingDocument4 pagesPFI ES-5-1993 Cleaning of Fabricated PipingRodrigo Chambilla VernazaNo ratings yet
- PhilosophyDocument4 pagesPhilosophyJudalineNo ratings yet
- Excel Project AssignmentDocument5 pagesExcel Project AssignmentJayden RinquestNo ratings yet
- VBA Water 6.09 Temperature Pressure Relief Valve Drain LinesDocument2 pagesVBA Water 6.09 Temperature Pressure Relief Valve Drain LinesgaryNo ratings yet
- The Decline of The WestDocument3 pagesThe Decline of The Westyasminbahat80% (5)
- Vijaya DairyDocument65 pagesVijaya DairyAjay KumarNo ratings yet
- Immuno DiffusionDocument3 pagesImmuno DiffusionSai SridharNo ratings yet
- Catalogue 2019Document450 pagesCatalogue 2019AntonNo ratings yet
- Terms of Use: Thank You For Respecting My Work!Document11 pagesTerms of Use: Thank You For Respecting My Work!Tammy Reyes VélizNo ratings yet
- Visvesvaraya Technological University, BELGAUM-590 014: "Online Movie Ticket Management System"Document53 pagesVisvesvaraya Technological University, BELGAUM-590 014: "Online Movie Ticket Management System"Ashutosh pandeyNo ratings yet
- Title Business Partner Number Bus Part Cat Business Partner Role Category Business Partner GroupingDocument16 pagesTitle Business Partner Number Bus Part Cat Business Partner Role Category Business Partner GroupingRanjeet KumarNo ratings yet
- Activities Guide and Evaluation Rubric - Unit 1 - Task 2 - Attacking and DefendingDocument9 pagesActivities Guide and Evaluation Rubric - Unit 1 - Task 2 - Attacking and Defendingsteven alvarezNo ratings yet
- Disaster Mana BooksDocument20 pagesDisaster Mana BooksSupraja_Prabha_8353No ratings yet
- METRIX AUTOCOMP - Company ProfileDocument2 pagesMETRIX AUTOCOMP - Company ProfileVaibhav AggarwalNo ratings yet
- 04 Control of Reactive PowerDocument30 pages04 Control of Reactive PowersulemankhalidNo ratings yet
- Lubricattng Oil For Marine EnginesDocument5 pagesLubricattng Oil For Marine Enginesemmsh71No ratings yet
- FAKRO Technical Specification DRF DU6 PDFDocument2 pagesFAKRO Technical Specification DRF DU6 PDFthomasNo ratings yet
- 7 - Simulations and PFDsDocument23 pages7 - Simulations and PFDsIslam SolimanNo ratings yet
- (1142) Grade XI Admissions 2016-17Document7 pages(1142) Grade XI Admissions 2016-17Naveen ShankarNo ratings yet
- Bluetooth Car Using ArduinoDocument13 pagesBluetooth Car Using ArduinoRainy Thakur100% (1)
- Research GR 2 Pinaka Final 1Document36 pagesResearch GR 2 Pinaka Final 1Richeille JoshNo ratings yet
- Selection & Applications of Power Factor Correction Capacitor For Industrial and Large Commercial Users Ben Banerjee Power Quality Solution GroupDocument61 pagesSelection & Applications of Power Factor Correction Capacitor For Industrial and Large Commercial Users Ben Banerjee Power Quality Solution Groupraghav4life8724No ratings yet
- Akinlo and Asaolo, 2012 PDFDocument9 pagesAkinlo and Asaolo, 2012 PDFJason KurniawanNo ratings yet
- Questions Energy Surfaces and Spontaneous ReactionsDocument2 pagesQuestions Energy Surfaces and Spontaneous Reactionshernys NietoNo ratings yet
- AP06-EV04 - Taller en Idioma Inglés Sobre Sistema de Distribución.Document8 pagesAP06-EV04 - Taller en Idioma Inglés Sobre Sistema de Distribución.juanze rodriguezNo ratings yet
- Critical Analysis of Story Number 2Document12 pagesCritical Analysis of Story Number 2David MorganNo ratings yet
- Checklist Information Security Policy ImplementationDocument18 pagesChecklist Information Security Policy Implementationbaye omar SoceNo ratings yet
- 13 B 2 NDocument7 pages13 B 2 NRay Ramilo100% (1)
Assesment Stroke Without CT Scan (Greek Score, Alen Score
Assesment Stroke Without CT Scan (Greek Score, Alen Score
Uploaded by
Missing ManOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Assesment Stroke Without CT Scan (Greek Score, Alen Score
Assesment Stroke Without CT Scan (Greek Score, Alen Score
Uploaded by
Missing ManCopyright:
Available Formats
137
Indian Journal of Medical Sciences, Vol. 67, No. 5 and 6, May and June 2013
BEDSIDE UTILITY OF CLINICAL SCORING SYSTEMS IN
CLASSIFYING STROKE
RUDRA PROSAD GOSWAMI, PARTHA SARATHI KARMAKAR, ALAKENDU GHOSH
ABSTRACT
BACKGROUND: The study aimed to validate and compare the Siriraj score,
Guys hospital score, Greek score, and Besson score in a group of stroke
patients. MATERIALS AND METHODS: We assessed the stroke scores and compared
them to computed tomography (CT) scan of brain. RESULTS: Two hundred stroke
patients (129 ischemic stroke) were included. For ischemic stroke, sensitivity and
specificity were 71% and 92% (Siriraj score), 73% and 98% (Greek score), 59% and 87%
(Guys hospital score), and 65% and 98% (Besson score), respectively. For intracranial
hemorrhage, sensitivity and specificity were 84% and 89% (Siriraj score), 80% and 99%
(Greek score), and 63% and 95% (Guys hospital score), respectively. Using receptor
operating characteristic curve, the greatest area under the curve was obtained for
Greek score (0.973). For bedside accurate and safe diagnosis of ischemic stroke, the
best cut off was for Greek score (1.5) which identified 47% of ischemic stroke patients.
CONCLUSIONS: The Greek score appears as the single best score. Using the newly
developed discriminant cut off value; a substantial number of patients may be started
with anti-platelet therapy while awaiting CT scan of brain.
Key words: Allen score, besson score, greek score, siriraj score, stroke
Department of Medicine, Institute of Post Graduate Medical
Education and Research, Kolkata, West Bengal, India
Address for correspondence:
Dr. Rudra Prosad Goswami,
Department of Medicine,
Abhyudoy Housing, Flat - 18/14, ECTP, Ph-IV,
Type-B, EM Bypass, Kolkata, West Bengal - 700 107, India.
E-mail: rudra.goswami@gmail.com
INTRODUCTION
Bedside diagnosis of subtype of stroke is often
lifesaving. But the subtleties and nuances of
overlap of clinical features make this distinction
diffcult. The greatest impact is on the ischemic
stroke, early identifcation of which renders the
physician use a powerful weapon of thrombolysis
or anti-platelet therapy which have been
shown to have mortality beneft.
[1]
Computed
tomography (CT) scan of brain is invaluable
in this regard and is considered an important
measure to exclude hemorrhagic stroke. But
in rural India, where CT scan has not gained
its access, physically and financially, clinical
determinism becomes the most important factor.
Access this article online
Quick Response Code:
Website:
www.indianjmedsci.org
DOI:
10.4103/0019-5359.122745
PMID:
*****************************
ORIGINAL ARTICLE
138 INDIAN JOURNAL OF MEDICAL SCIENCES
Indian Journal of Medical Sciences, Vol. 67, No. 5 and 6, May and June 2013
There are two famous stroke scores which can
guide the treating physician in such situations,
namely Siriraj score (SS)
[2]
and the Guys hospital
score (GHS) or the Allen score.
[3]
Recently, a
new score proposed by a team from Athens
claimed that the sensitivity, specifcity, positive
predictive value, and negative predictive value
were much better as compared to the previous
scores.
[4]
This Greek score (GS) was only once
tested in Indian population in a relatively small
study.
[5]
Besson, et al. also proposed a scoring
system (Besson score or BS) that could be used
to identify a fairly good proportion of ischemic
stroke patients at the bedside, with good safety
margin for appropriate therapy.
[6]
This score is yet
to be tested in India. Recently another scoring
system (Kurashiki Pre-hospital Stroke Subtyping
Score) has been published, but we could not get
enough information on this system to incorporate
it in our study.
[7]
We therefore aimed to validate and compare
the SS, GHS, GS, and BS in a moderately
large, independently selected group of Indian
patients in a tertiary care referral center in
eastern India.
MATERIALS AND METHODS
All cases with a diagnosis of stroke admitted in
the Department of Medicine, Institute of Post
Graduate Medical Education and Research and
Seth Sukhlal Karnani Memorial Hospital, were
consecutively recruited from October 2010 to
July 2011. We defned stroke according to the
World Health Organization criteria as rapidly
developing signs of focal (or global) disturbance
of cerebral function, leading to death or lasting
longer than 24 h, with no apparent cause other
than vascular.
[8]
Detailed clinical history, physical examination,
and routine tests including electrocardiography,
complete blood count, and CT scan of brain
within 24 h of presentation, but later than 6 h
of onset were performed on each patient. Any
patient presenting later than 24 h of symptom
onset was excluded from this study. Patients
with pure subarachnoid or intraventricular
hemorrhage were excluded.
The stroke scores were calculated from
this data. The scoring systems are adapted
from existing literature and are detailed in
Table 1.
[2-4,6]
The inferences of the scoring
systems were ischemic stroke, hemorrhagic
stroke, or uncertain, except in the BS where
the inferences were ischemic stroke and
non-ischemic stroke. All statistical calculations
were done with SPSS version 16.
RESULTS
Data comprised those of 200 consecutive
eligible patients, which included 129 ischemic
strokes (64.5%) and 71 hemorrhagic strokes
(35.5%). Average age of the popul ati on
was 57.09 years (standard deviation 12.67),
ranging from 26 to 80 years. There were
90 f emal e (45%) and 110 mal e (55%)
participants.
Table 2 shows the sensitivity, specificity,
positive and negative likelihood ratios for
the SS, GS, GHS, and BS for the diagnosis
of ischemic stroke. Table 3 shows these
values of the tests (except BS, which was
originally devised to screen ischemic strokes
onl y) for i ntracrani al hemorrhage. Al l of
the systems have better specificity than
sensitivity in any stroke subtype. The GS has
139 UTILITY OF STROKE SCORING SYSTEMS
Indian Journal of Medical Sciences, Vol. 67, No. 5 and 6, May and June 2013
Table 1: Scoring systems utilized in the study
Scoring system Variable Clinical feature Score Diagnosis
Siriraj scoring system Consciousness (2.5) Alert 0 <-1=Ischemic stroke
>1=Hemorrhagic stroke
Drowsy, stupor 1
Semicoma, coma 2
Vomiting (2) No 0
Yes 1
Headache within 2 h (2) No 0
Yes 1
Diastolic blood
pressure (0.1)
Atheroma markers (3) None 0
Diabetes, angina, intermittent
claudication
One or more 1
Constant 12
Guys hospital scoring
system
Apoplectic onset <4=Ischemic stroke
>24=Hemorrhagic stroke
Loss of consciousness None or one 0
Headache within 2 h Two or more 21.9
Vomiting
Neck stiffness
Level of consciousness
(24 h after admission)
Alert 0
Drowsy 7.3
Unconscious 14.6
Plantar responses Both fexor or single
extensor
0
Both extensor 7.1
Diastolic blood pressure
(24 h after admission) (0.17)
0.17
Atheroma markers
Diabetes, angina, intermittent None 0
Claudication One or more 3.7
History of hypertension Not present 0
Present 4.1
Previous event None 0
Transient ischemic attack Any number of
previous events
6.7
Heart disease None 4.3
Aortic or mitral
murmur
4.3
Cardiac failure 4.3
Cardiomyopathy 4.3
Atrial fbrillation 4.3
Cardiomegaly 4.3
Myocardial infarct
within 6 months 4.3
Constant 12
(Contd...)
140 INDIAN JOURNAL OF MEDICAL SCIENCES
Indian Journal of Medical Sciences, Vol. 67, No. 5 and 6, May and June 2013
acceptable sensitivity (around 80%) and good
specifcity (>95%) in both subgroups. The GHS
appears to be worst of the four. The BS is
particularly specifc for ischemic stroke (>95%).
The test results were uncertain in 29 cases
(14.5%) using SS, in 46 cases (23%) using
the GS, and in 63 cases (31.5%) using the
GHS.
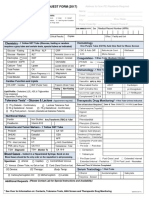
Next we pr epar ed r ecept or oper at i ng
characteristic (ROC) curves for all the four
data sets using CT diagnosis as the criterion
val ue [Fi gure 1]. We generated Youden
Table 1: Contd...
Scoring system Variable Clinical feature Score Diagnosis
Greek score Neurological deterioration
within 3 h of admission
6 <3=Ischemic stroke
>11=Hemorrhagic stroke
Vomiting 4
Total leukocyte count in
peripheral blood >12,000/l
4
Decreased level of
consciousness at admission
3
Besson score Alcohol consumption Absent 0 <1=Ischemic stroke
Present 2
Plantar response (1.5) Bilateral fexor 0
Extensor ipsilateral to
defcit
1
Extensor contralateral
to defcit
2
Both extensors 3
Headache Absent 0
Present 3
History of transient
neurological defcit
Absent
Present
0
5
Hyperlipidemia Absent
Present 1.5
Atrial fbrillation at admission Absent
Present 2.5
Table 2: Comparison of SS, GHS, GS, and BS against CT scan of brain for the diagnosis of ischemic stroke
Diagnosis CT diagnosis Sensitivity % (CI) Specifcity % (CI) Positive likelihood ratio
(CI)
Negative likelihood ratio
(CI)
IS Not IS
SS
IS 92 5 71.32 (62.58-78.06) 92.96 (83.65-7.37) 10.12 (4.32-23.74) 0.31 (0.23-0.41)
Not IS 37 66
GS
IS 95 1 73.64 (65.02-80.82) 98.59 (91.35-99.92) 52.28 (7.45-367.08) 0.27 (0.20-0.35)
Not IS 34 70
GHS
IS 77 9 59.69 (50.67-68.12) 87.32 (76.80-93.68) 4.71 (2.52-8.81) 0.46 (0.37-0.57)
Not IS 62 52
BS
IS 85 1 65.89 (56.96-73.86) 98.59 (91.35-99.92) 46.78 (6.655-328.84) 0.34 (0.27-0.44)
Not IS 44 70
SS=Siriraj score, GS=Greek score, GHS=Guys hospital score, BS=Besson score
141 UTILITY OF STROKE SCORING SYSTEMS
Indian Journal of Medical Sciences, Vol. 67, No. 5 and 6, May and June 2013
index for each cut off value of each test and
the cut off value with the highest Youden
index was taken as optimum. The cut off
values and the respective sensitivities and
specifcities are detailed in Table 4. The area
under the curve (AUC) was also estimated
for each test. These are also summarized
in Table 4. The highest AUC was that of
GS (0.973), followed by SS (0.929), BS (0.911),
and GHS (0.873) [P val ue: SS vs. GS
(two tailed) = 0.03].
Next we tried to determine the discriminant cut
off vale of each test defned as the value of the
system which provides no false-negative results
with maximum achievable specifcity when applied
to diagnose ischemic stroke patients. These are
summarized in Table 4. At the given cut off values
for optimal discrimination, the proportions of
ischemic stroke patients identifed are 40 (31%),
61 (47.28%), 13 (10%), and 47 (36.43%) for SS,
GS, GHS, and BS, respectively (P values: GS vs.
BS = 0.07; GS vs. SS = 0.007).
DISCUSSION
Management of stroke largely depends on
differentiation of hemorrhagic from ischemic
stroke. Clinical stroke score can help in this
direction. The ideal score to predict stroke type
Table 3: Comparison of SS, GHS, GS, and BS against CT scan of brain for the diagnosis of hemorrhagic stroke
Diagnosis CT diagnosis Sensitivity % (CI) Specifcity % (CI) Positive likelihood ratio
(CI)
Negative likelihood ratio
(CI)
ICH Not ICH
SS
ICH 60 14 84.51 (73.54-91.65) 89.15 (82.15-93.72) 4.28 (2.64-6.96) 0.09 (0.05-0.17)
Not ICH 11 115
GS
ICH 57 1 80.28 (68.80-88.42) 99.22 (95.12-99.95) 103.56 (14.64-732.11) 0.19 (0.12-0.32)
Not ICH 14 128
GHS
ICH 45 6 63.38 (51.05-74.05) 95.35 (89.72-98.09) 13.62 (6.11-30.36) 0.38 (0.28-0.52)
Not ICH 26 123
ICH= Intracranial haemorrhage, SS=Siriraj score, GS=Greek score, GHS=Guys hospital score
Table 4: ROC curve analysis of all the scoring systems
Scoring system AUC (standard error) Optimal cut off Sensitivity/specifcity Discriminant cut off Specifcity (%)
SS 0.929 (0.019) 1 84.5/91.4 3.2 30.5
GS 0.973 (0.013) 6.5 97.2/87.8 1.5 47.9
GHS 0.873 (0.029) 13.2 76.1/87.5 5 10.9
BS 0.911 (0.020) 3.25 85.9/84.4 0 35.9
SS=Siriraj score, GS=Greek score, GHS=Guys hospital score, BS=Besson score
Figure 1: Comparison of diagnostic accuracy of the
stroke scoring systems (ROC method)
142 INDIAN JOURNAL OF MEDICAL SCIENCES
Indian Journal of Medical Sciences, Vol. 67, No. 5 and 6, May and June 2013
should have a good balance between validity,
simplicity, and utility.
[9]
With these qualities, a
scoring system might become an important
tool for timely decision making in rural areas
of developing countries where facilities like CT
scanning are sparse.
Amongst the available four systems, the SS
and GHS have been tested in the past decade
many times against each other and against the
gold standard test (CT scan of brain).
[5,10-15]
The results have varied widely from one
researcher to another, but overall they have
been shown to have acceptable sensitivity
and fair specifcity [Table 5]. In this regard,
it is to be noted that the Indian studies have
found fairly consistent sensitivity (80%) and
specifcity (7080%) of SS.
[5,14,15]
GS has been
evaluated in only one study and was found to
be highly specifc (94%) but with disappointing
sensitivity (42%).
[5]
Our results are in agreement
with the previous studies. The sensitivities
calculated in the present study are all in the
range of 70-80% except that for GHS. But the
specifcities of GS and GHS in our data are
excellent (98.59%) for diagnosing ischemic
stroke. Though all the systems in the present
study have good specificities to diagnose
hemorrhagic stroke, GS has the most satisfying
value of 99.22%. SS has consistently been
shown to be superior to GHS. There are only
two studies which show GHS to be superior to
SS, one from New Zealand
[11]
and another from
Turkey.
[16]
Our results are in agreement with the
majority of the studies and we conclude that
GHS is inferior to SS in this regard.
The superiority of the SS over the Allen score
is related to its better discrimination, evident
in statistical analysis, simplicity in application,
and the fact that the score can be applied at
presentation of the patient unlike that for GHS
which requires 24 h to be calculated.
[9]
All these
criteria are shared by GS. The fact that GS
is superior to all other scoring systems as an
early screening tool is also augmented by the
ROC curve analysis in which the AUC for GS
is signifcantly higher than any other system.
This is the first Indian study which utilized
the BS to specifcally discriminate ischemic
stroke from non-ischemic ones. BS was
originally devised for this express purpose.
[6]
We have successfully validated the said
utility of BS through our data. BS had a high
specificity and high positive likelihood ratio
for identifying ischemic strokes though the
sensitivity of the system was somewhat less.
Table 5: Literature review of population application of the scoring systems
Scoring
systems
South Africa
[10]
(222)
New Zealand
[11]
(485)
UK
[12]
(482)
Italy
[13]
(193)
India 1
[5]
(91)
India 2
[14]
(139)
India 3
[15]
(159 for SS and 147 for GHS)
SS
Sensitivity 60 48 67 61 75 78 85
Specifcity 88 85 71 94 81 71 73
GHS
Sensitivity 34 31 78 98 50 81 91
Specifcity 95 95 81 71 94 76 60
GS
Sensitivity 42
Specifcity 94
SS=Siriraj score, GS=Greek score, GHS=Guys hospital score
143 UTILITY OF STROKE SCORING SYSTEMS
Indian Journal of Medical Sciences, Vol. 67, No. 5 and 6, May and June 2013
Using the original cut off (1), a large number of
ischemic stroke patients could be diagnosed at
bedside (65.89%), but with the risk of wrongly
classifying 1.41% hemorrhagic stroke patients
as ischemic stroke patients.
It has been suggested that these scoring
systems should be used as rule-out measures
rather than rule-in measures for methodical
evaluation of stroke patients.
[9]
Indeed for
the majority of our patients, thrombolytics
are not a therapeutic option, either due to
logistic or fnancial reasons. Using a score that
could exclude intracranial hemorrhage with a
reasonable degree of medical certainty would
encourage physicians in remote areas to initiate
an early aspirin therapy.
Previous literature has shown that at a cut off
value of 4 for SS, nearly 38% of all stroke
patients could be treated safely without the
need for CT scan which could be an immensely
important costbenefit advantage.
[10]
In the
original work, Besson, et al. claimed to identify
43% of ischemic stroke patients at bedside safely
without the need of CT scan.
[6]
Our cut off values
for this discrimination were 3.2 for SS, 1.5 for
GS, 5 for GHS, and 0 for BS. GS (47%) and
BS (36%) identifed signifcantly greater number
of ischemic stroke patients compared to the
other two systems, who could be started with
anti-platelet therapy before a CT scan of brain
could be performed safely. This is a considerable
improvement in identifcation of such patients
compared to previous data which used SS.
CONCLUSIONS
The scores have moderate sensitivity and
good specifcity for the diagnosis of subtypes
of stroke. The GS appears as the single best
score. Using the newly developed discriminant
cut off value, a substantial number of patients
may be started with anti-platelet therapy while
awaiting CT scan of brain.
REFERENCES
1. Adams HP Jr, del Zoppo G, Alberts MJ, et al.
Guidelines for the early management of adults with
ischemic stroke: A guideline from the American
Heart Association/American Stroke Association
Stroke Council, Clinical Cardiology Council,
Cardiovascular Radiology and Intervention
Council, and the Atherosclerotic Peripheral
Vascular Disease and Quality of Care Outcomes
in Research Interdisciplinary Working Groups:
The American Academy of Neurology affrms the
value of this guideline as an educational tool for
neurologists. Stroke 2007;38:1655-711.
2. Poungvarin N, Viriyavejakul A, Komontri C. Siriraj
stroke score and validation study to distinguish
supratentorial intracerebral hemorrhage from
infarction. BMJ 1991;302:1565.
3. Allen CMC. Clinical diagnosis of the acute stroke
syndrome. Q J Med 1983;52:515-23.
4. Efstathiou SP, Tsioulos DI, Zacharos ID. A new
classification tool for clinical differentiation
between haemorrhagic and ischaemic stroke.
J Intern Med 2002;252:121.
5. Soman A, Joshi SR, Tarvade S, Jayaram S.
Greek stroke score, Siriraj score and Allen score
in clinical diagnosis of intracerebral hemorrhage
and infarct: Validation and comparison study.
Indian J Med Sci 2004;58:417-22.
6. Besson G, Robert C, Hommel M, Perret J. Is it
clinically possible to distinguish nonhemorrhagic
i nfarct from hemorrhagi c stroke? Stroke
1995;26:1205-9.
7. Yamashita S, Kimura K, Iguchi Y, Shibazaki K,
Watanabe M, Iwanaga T. Kurashiki Prehospital
Stroke Subtyping Score (KP3S) as a means of
144 INDIAN JOURNAL OF MEDICAL SCIENCES
Indian Journal of Medical Sciences, Vol. 67, No. 5 and 6, May and June 2013
distinguishing ischemic from hemorrhagic stroke
in emergency medical services. Eur Neurol
2011;65:233-8
8. Hatano S. Experience from a multicentre stroke
register: A preliminary report. Bull World Health
Organ 1976;54:541-53.
9. Nouira S, Boukef R, Bouida W, Marghli S,
Dridi Z, Benamou S, et al. Accuracy of two
scores in the diagnosis of stroke subtype in
a multicenter cohort study. Ann Emerg Med
2009;53:373-8.
10. Connor MD, Modi G, Warlow CP. Accuracy of the
Siriraj and Guys Hospital Stroke Scores in urban
South Africans. Stroke 2007;38:62-8.
11. Hawkins GC, Bonita R, Broad JB, Anderson NE.
Inadequacy of clinical scoring systems to
differentiate stroke subtypes in population-based
studies. Stroke 1995;26:1338-42.
12. Sandercock PA, Al l en CM, Corst on RN,
Harrison MJ, Warlow CP. Clinical diagnosis of
intracranial haemorrhage using Guys Hospital
score. BMJ (Clin Res Ed) 1985;291:1675-7.
13. Celani MG, Righetti E, Migliacci R, Zampolini M,
Antoniutti L, Grandi FC, et al. Comparability
and validity of two clinical scores in the early
differential diagnosis of acute stroke. BMJ
1994;308:1674-6.
14. Badam P, Solao V, Pai M, Kalantri SP. Poor
accuracy of the Siriraj and Guys hospital stroke
scores in distinguishing haemorrhagic from
ischaemic stroke in a rural, tertiary care hospital.
Natl Med J India 2003;16:8-12.
15. Kochar DK, Joshi A, Agarwal N, Aseri S,
Sharma BV, Agarwal TD. Poor diagnostic
accuracy and applicability of Siriraj stroke score,
Allen score and their combination in differentiating
acute haemorrhagic and thrombotic stroke.
J Assoc Physicians India 2000;48:584-8.
16. Ozeren A, Bicakci S, Burgut R, Sarica Y,
Bozdemir H. Accuracy of bedside diagnosis
versus Allen and Siriraj stroke scores in Turkish
patients. Eur J Neurol 2006;13:611-5.
How to cite this article: Goswami RP, Karmakar PS, Ghosh A.
Bedside utility of clinical scoring systems in classifying stroke.
Indian J Med Sci 2013;67:137-45.
Source of Support: Nil. Confict of Interest: None declared.
You might also like
- MR Clean Late LancetDocument10 pagesMR Clean Late LancetLetícia JanuziNo ratings yet
- Journal 4Document5 pagesJournal 4dr. Nadia Salsabila100% (1)
- Boysen-Osborn (2018) PDFDocument11 pagesBoysen-Osborn (2018) PDFBryan TorresNo ratings yet
- Acute Stroke Treatment - CPM 8th EdDocument22 pagesAcute Stroke Treatment - CPM 8th EdSuresh ShresthaNo ratings yet
- 3046-Article Text-5935-1-10-20200724Document7 pages3046-Article Text-5935-1-10-20200724Kirubel DeribNo ratings yet
- Siriraj Stroke ScoreDocument3 pagesSiriraj Stroke ScoreHendy SetiawanNo ratings yet
- The Recognition of Stroke in The Emergency Room ROSIERDocument8 pagesThe Recognition of Stroke in The Emergency Room ROSIERcristian viretto100% (1)
- Absen Kelas X - 2020-2021 RNDocument10 pagesAbsen Kelas X - 2020-2021 RNZickra Awla0% (1)
- An Introduction DTIDocument23 pagesAn Introduction DTIAliceNo ratings yet
- Cardiac Radiosurgery (CyberHeart™) For Treatment of Arrhythmia: Physiologic and Histopathologic Correlation in The Porcine ModelDocument28 pagesCardiac Radiosurgery (CyberHeart™) For Treatment of Arrhythmia: Physiologic and Histopathologic Correlation in The Porcine ModelCureusNo ratings yet
- Special Investigation in RadiographyDocument76 pagesSpecial Investigation in RadiographyOluseyiNo ratings yet
- Abdominal RadiographDocument36 pagesAbdominal RadiographLarasati FadhlenNo ratings yet
- Computerized Tomography (CT) Scan: Indication Abnormal ResultsDocument7 pagesComputerized Tomography (CT) Scan: Indication Abnormal ResultsVanessa VillanuevaNo ratings yet
- Hysterosalpingography A Re - Emerging Study With CDocument7 pagesHysterosalpingography A Re - Emerging Study With CTuyul Yelsi 1No ratings yet
- Bishop Rehabilitation and Nursing Center Inspection ReportDocument117 pagesBishop Rehabilitation and Nursing Center Inspection ReportJames MulderNo ratings yet
- Medical Malpractice and Compensation in The UKDocument33 pagesMedical Malpractice and Compensation in The UKgun rayNo ratings yet
- Analisis Efisiensi Celah Shutter Kolimator Tabung Sinar X Di Tiga Instalasi Radiologi Lahan PKL Prodi D3 Radiologi Unisa YogyakartaDocument7 pagesAnalisis Efisiensi Celah Shutter Kolimator Tabung Sinar X Di Tiga Instalasi Radiologi Lahan PKL Prodi D3 Radiologi Unisa YogyakartaNoveliaNo ratings yet
- RS CoachingDocument201 pagesRS CoachingHalia MalicNo ratings yet
- Modified Rankin Scale How To PDFDocument15 pagesModified Rankin Scale How To PDFKNI Maret 2023No ratings yet
- Allreports PDFDocument2 pagesAllreports PDFNeena SinghNo ratings yet
- Coronary Artery Diseases - Ilham PDocument43 pagesCoronary Artery Diseases - Ilham PKeputrian FKUPNo ratings yet
- Medel SonataDocument54 pagesMedel Sonatamaclab macNo ratings yet
- Dual Source CT Imaging PDFDocument275 pagesDual Source CT Imaging PDFAnisa SetiawatiNo ratings yet
- General-Mrcs-Recalls-Paper-2-From-Previous-Exams .Document79 pagesGeneral-Mrcs-Recalls-Paper-2-From-Previous-Exams .Victor FabunmiNo ratings yet
- Loopography Examination For Colon Cancer 7c394e77Document11 pagesLoopography Examination For Colon Cancer 7c394e77N. Camelya FirdausNo ratings yet
- Laboratory Blood Request FormDocument2 pagesLaboratory Blood Request FormIsaac AgbemafleNo ratings yet
- Practicing Medicine in FinlandDocument12 pagesPracticing Medicine in FinlandDr Richard AnekweNo ratings yet
- 1.1. Pocus en Emg y Critical Care 2018 PDFDocument8 pages1.1. Pocus en Emg y Critical Care 2018 PDFEmergencias RebagliatiNo ratings yet
- Abstracts From The Global Embolization Sympo 2021 Journal of Vascular and inDocument21 pagesAbstracts From The Global Embolization Sympo 2021 Journal of Vascular and infreedy freedyNo ratings yet
- Anaesthesia For Hepatic Resection SurgeryDocument15 pagesAnaesthesia For Hepatic Resection SurgeryDianita P Ñáñez VaronaNo ratings yet
- Perioperative Risk Stratification and ModificationDocument23 pagesPerioperative Risk Stratification and ModificationDianita P Ñáñez VaronaNo ratings yet
- Review Jurnal RadiologiDocument10 pagesReview Jurnal RadiologiM Benni KadapihNo ratings yet
- A Thesis ProtocolDocument29 pagesA Thesis ProtocolMelvin JohnNo ratings yet
- Jay Ushin 2018Document92 pagesJay Ushin 2018Puneet367No ratings yet
- SKB Radiografer & Aipri I (93 Soal) - Beserta Jawaban PDFDocument55 pagesSKB Radiografer & Aipri I (93 Soal) - Beserta Jawaban PDFiwan hardiansyahNo ratings yet
- Compilation Questions of Theory Part One 04-1Document34 pagesCompilation Questions of Theory Part One 04-1Rebecca WongNo ratings yet
- Medical Ethics Principles, 14 Januari 2018Document16 pagesMedical Ethics Principles, 14 Januari 2018Adji SuwandonoNo ratings yet
- Siriraj 1Document5 pagesSiriraj 1Winda MelatiNo ratings yet
- Lack of Clinical Utility of The Siriraj Stroke Score: Riginal RticleDocument4 pagesLack of Clinical Utility of The Siriraj Stroke Score: Riginal RticleWinda MelatiNo ratings yet
- Siriraj 2Document4 pagesSiriraj 2Winda MelatiNo ratings yet
- Siriraj Stroke Score PDFDocument11 pagesSiriraj Stroke Score PDFGalant Lefebvre 戈蓝No ratings yet
- Stroke Score 2004Document4 pagesStroke Score 2004Pebrian SyahNo ratings yet
- IL 6 and StrokeDocument7 pagesIL 6 and StrokeDian Laras SuminarNo ratings yet
- A Three-Item Scale For The Early Prediction of Stroke RecoveryDocument5 pagesA Three-Item Scale For The Early Prediction of Stroke RecoverydoktergigikoeNo ratings yet
- An Integer-Based Score To PredictDocument21 pagesAn Integer-Based Score To PredictMichael BentonNo ratings yet
- Comparison of Neurological Clinical Manifestation in Patients With Hemorrhagic and Ischemic StrokeDocument5 pagesComparison of Neurological Clinical Manifestation in Patients With Hemorrhagic and Ischemic StrokeDessy FarwasNo ratings yet
- Serum CytokinesDocument7 pagesSerum CytokinesEvy Yulia KusmayantiNo ratings yet
- Antiagregacion Vs Anticoagulacion en DiseccionDocument4 pagesAntiagregacion Vs Anticoagulacion en DiseccionCarlos Alberto CorredorNo ratings yet
- Early Prediction of Severity StrokeDocument11 pagesEarly Prediction of Severity StrokeainihanifiahNo ratings yet
- Main 51 ???Document5 pagesMain 51 ???pokharelriwaj82No ratings yet
- Medip, IJAM-2391 ODocument4 pagesMedip, IJAM-2391 OalitrnfbNo ratings yet
- Missed Ischemic Stroke Diagnosis in The Emergency Department by Emergency Medicine and Neurology ServicesDocument7 pagesMissed Ischemic Stroke Diagnosis in The Emergency Department by Emergency Medicine and Neurology ServicesReyhansyah RachmadhyanNo ratings yet
- Comparison of Clinical Diagnosis With Computed Tomography in Ascertaining Type of StrokeDocument3 pagesComparison of Clinical Diagnosis With Computed Tomography in Ascertaining Type of StrokeDyah Wulan RamadhaniNo ratings yet
- Efecto de Estatinas en RecurrencaDocument4 pagesEfecto de Estatinas en RecurrencaLeonela Ramirez Almanza y Lina Maria Ossa HerreraNo ratings yet
- Role of Interleukin-6 in Ischemic Stroke OutcomeDocument7 pagesRole of Interleukin-6 in Ischemic Stroke OutcomeSalma SalmaNo ratings yet
- NIHSS Cut-Point For Predicting Outcome in Supra-Vs Infratentorial Acute Ischemic StrokeDocument8 pagesNIHSS Cut-Point For Predicting Outcome in Supra-Vs Infratentorial Acute Ischemic StrokePutri NurdiyantiNo ratings yet
- Accuracy of Physical Signs For Detecting Meningitis - A Hospital-Based Diagnostic Accuracy StudyDocument7 pagesAccuracy of Physical Signs For Detecting Meningitis - A Hospital-Based Diagnostic Accuracy StudyNanda AlvionitaNo ratings yet
- Mathematics 10 02049 v3Document17 pagesMathematics 10 02049 v3Dhavala Shree B JainNo ratings yet
- Flat-Head Positioning Increases Cerebral Blood Flow in Anterior Circulation Acute Ischemic Stroke. A Cluster Randomized Phase Iib TrialDocument12 pagesFlat-Head Positioning Increases Cerebral Blood Flow in Anterior Circulation Acute Ischemic Stroke. A Cluster Randomized Phase Iib TrialNaufal HilmiNo ratings yet
- Glyceryl Trinitrate For Acute Intracerebral HemorrhageDocument21 pagesGlyceryl Trinitrate For Acute Intracerebral HemorrhageAhmad Al-atthosNo ratings yet
- Unit3&4 Network TheoramsDocument73 pagesUnit3&4 Network TheoramsBALAKRISHNA PERALANo ratings yet
- Attach 8 - CPDS Type 2ADocument401 pagesAttach 8 - CPDS Type 2AGlenn Adalia BonitaNo ratings yet
- PFI ES-5-1993 Cleaning of Fabricated PipingDocument4 pagesPFI ES-5-1993 Cleaning of Fabricated PipingRodrigo Chambilla VernazaNo ratings yet
- PhilosophyDocument4 pagesPhilosophyJudalineNo ratings yet
- Excel Project AssignmentDocument5 pagesExcel Project AssignmentJayden RinquestNo ratings yet
- VBA Water 6.09 Temperature Pressure Relief Valve Drain LinesDocument2 pagesVBA Water 6.09 Temperature Pressure Relief Valve Drain LinesgaryNo ratings yet
- The Decline of The WestDocument3 pagesThe Decline of The Westyasminbahat80% (5)
- Vijaya DairyDocument65 pagesVijaya DairyAjay KumarNo ratings yet
- Immuno DiffusionDocument3 pagesImmuno DiffusionSai SridharNo ratings yet
- Catalogue 2019Document450 pagesCatalogue 2019AntonNo ratings yet
- Terms of Use: Thank You For Respecting My Work!Document11 pagesTerms of Use: Thank You For Respecting My Work!Tammy Reyes VélizNo ratings yet
- Visvesvaraya Technological University, BELGAUM-590 014: "Online Movie Ticket Management System"Document53 pagesVisvesvaraya Technological University, BELGAUM-590 014: "Online Movie Ticket Management System"Ashutosh pandeyNo ratings yet
- Title Business Partner Number Bus Part Cat Business Partner Role Category Business Partner GroupingDocument16 pagesTitle Business Partner Number Bus Part Cat Business Partner Role Category Business Partner GroupingRanjeet KumarNo ratings yet
- Activities Guide and Evaluation Rubric - Unit 1 - Task 2 - Attacking and DefendingDocument9 pagesActivities Guide and Evaluation Rubric - Unit 1 - Task 2 - Attacking and Defendingsteven alvarezNo ratings yet
- Disaster Mana BooksDocument20 pagesDisaster Mana BooksSupraja_Prabha_8353No ratings yet
- METRIX AUTOCOMP - Company ProfileDocument2 pagesMETRIX AUTOCOMP - Company ProfileVaibhav AggarwalNo ratings yet
- 04 Control of Reactive PowerDocument30 pages04 Control of Reactive PowersulemankhalidNo ratings yet
- Lubricattng Oil For Marine EnginesDocument5 pagesLubricattng Oil For Marine Enginesemmsh71No ratings yet
- FAKRO Technical Specification DRF DU6 PDFDocument2 pagesFAKRO Technical Specification DRF DU6 PDFthomasNo ratings yet
- 7 - Simulations and PFDsDocument23 pages7 - Simulations and PFDsIslam SolimanNo ratings yet
- (1142) Grade XI Admissions 2016-17Document7 pages(1142) Grade XI Admissions 2016-17Naveen ShankarNo ratings yet
- Bluetooth Car Using ArduinoDocument13 pagesBluetooth Car Using ArduinoRainy Thakur100% (1)
- Research GR 2 Pinaka Final 1Document36 pagesResearch GR 2 Pinaka Final 1Richeille JoshNo ratings yet
- Selection & Applications of Power Factor Correction Capacitor For Industrial and Large Commercial Users Ben Banerjee Power Quality Solution GroupDocument61 pagesSelection & Applications of Power Factor Correction Capacitor For Industrial and Large Commercial Users Ben Banerjee Power Quality Solution Groupraghav4life8724No ratings yet
- Akinlo and Asaolo, 2012 PDFDocument9 pagesAkinlo and Asaolo, 2012 PDFJason KurniawanNo ratings yet
- Questions Energy Surfaces and Spontaneous ReactionsDocument2 pagesQuestions Energy Surfaces and Spontaneous Reactionshernys NietoNo ratings yet
- AP06-EV04 - Taller en Idioma Inglés Sobre Sistema de Distribución.Document8 pagesAP06-EV04 - Taller en Idioma Inglés Sobre Sistema de Distribución.juanze rodriguezNo ratings yet
- Critical Analysis of Story Number 2Document12 pagesCritical Analysis of Story Number 2David MorganNo ratings yet
- Checklist Information Security Policy ImplementationDocument18 pagesChecklist Information Security Policy Implementationbaye omar SoceNo ratings yet
- 13 B 2 NDocument7 pages13 B 2 NRay Ramilo100% (1)