Professional Documents
Culture Documents
P ('t':'3', 'I':'3054456811') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)
P ('t':'3', 'I':'3054456811') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)
Uploaded by
fraditayyunusCopyright:
Available Formats
You might also like
- (ASRA) Guidelines Neuraxial and AnticoagulationDocument6 pages(ASRA) Guidelines Neuraxial and Anticoagulationfraditayyunus82% (11)
- KUKA Programming NotesDocument13 pagesKUKA Programming Notes92dalliNo ratings yet
- Jurnal 5Document4 pagesJurnal 5MFWPNo ratings yet
- Glycated Haemoglobin As A Stable Indicator Of: Hba C Type 2 DiabetesDocument4 pagesGlycated Haemoglobin As A Stable Indicator Of: Hba C Type 2 DiabetesfamtaluNo ratings yet
- Correlation of Fasting and Postprandial Plasma Glucose With Hba1C in Assessing Glycemic Control Systematic Review and Meta-AnalysisDocument9 pagesCorrelation of Fasting and Postprandial Plasma Glucose With Hba1C in Assessing Glycemic Control Systematic Review and Meta-AnalysisRodas GetachewNo ratings yet
- Schwingshackl2013 PDFDocument8 pagesSchwingshackl2013 PDFLisiane PerinNo ratings yet
- Glyca AlbuminDocument8 pagesGlyca AlbuminElang SudewaNo ratings yet
- Association of Coagulation Profile With Microvascular Complications and Glycemic Control in Type 2 Diabetes Mellitus - A Study ADocument1 pageAssociation of Coagulation Profile With Microvascular Complications and Glycemic Control in Type 2 Diabetes Mellitus - A Study Aseneh17198No ratings yet
- Glycemic Variability June 12 2014Document42 pagesGlycemic Variability June 12 2014Hemant GaurkarNo ratings yet
- Glucose Variability - FullDocument12 pagesGlucose Variability - FullAlina PopaNo ratings yet
- Bismillah Fix Hba1c1Document23 pagesBismillah Fix Hba1c1NsafifahNo ratings yet
- tmp2475 TMPDocument7 pagestmp2475 TMPFrontiersNo ratings yet
- GA, 1,5 AG and HbA1cDocument7 pagesGA, 1,5 AG and HbA1cLegina AdityaNo ratings yet
- Clinical Study: The Effects of Glucose Fluctuation On The Severity of Coronary Artery Disease in Type 2 Diabetes MellitusDocument6 pagesClinical Study: The Effects of Glucose Fluctuation On The Severity of Coronary Artery Disease in Type 2 Diabetes MellitusEgi Dwi SatriaNo ratings yet
- 7 FFCDocument8 pages7 FFCHow to youNo ratings yet
- DiabetesDocument8 pagesDiabetesDanielValenciaNo ratings yet
- Diabetes Care Glucosa Promedio EstimadaDocument6 pagesDiabetes Care Glucosa Promedio EstimadaGemeneza GonzalesNo ratings yet
- HBA1CVARIABILITYDocument17 pagesHBA1CVARIABILITYThanisha SanthoshNo ratings yet
- Translating The A1C Assay Into Estimated Average Glucose ValuesDocument6 pagesTranslating The A1C Assay Into Estimated Average Glucose ValuesFaryalBalochNo ratings yet
- Nutritional Status in Patients With Diabetes and Chronic Kidney Disease: A Prospective StudyDocument6 pagesNutritional Status in Patients With Diabetes and Chronic Kidney Disease: A Prospective StudyHenry HadiantoNo ratings yet
- Research ArticleDocument12 pagesResearch ArticleRodas GetachewNo ratings yet
- Bismillah Fix Hba1c2Document7 pagesBismillah Fix Hba1c2NsafifahNo ratings yet
- Hba1c VariabilityDocument5 pagesHba1c Variabilityruruh_wibowoNo ratings yet
- DZ Tip II CancerDocument7 pagesDZ Tip II CancerAndreeaGheorgheNo ratings yet
- Relationship Between Hba1c and Complete Blood Count Parameters in Adult Patients With Type 2 Diabetes in Saudi ArabiaDocument7 pagesRelationship Between Hba1c and Complete Blood Count Parameters in Adult Patients With Type 2 Diabetes in Saudi ArabiaIJAR JOURNALNo ratings yet
- Mia Now Ska 2010Document8 pagesMia Now Ska 2010Anonymous 2AiYmQ1dNo ratings yet
- Estudio NICE - Sugar (2009)Document11 pagesEstudio NICE - Sugar (2009)Trt CamargoNo ratings yet
- Dietary Fiber DMDocument8 pagesDietary Fiber DMAnnisa SavitriNo ratings yet
- Relationship Between C-Reactive Protein, White Blood Cell Count and Metabolic Syndrome in Nigerians With Type 2 Diabetes MellitusDocument11 pagesRelationship Between C-Reactive Protein, White Blood Cell Count and Metabolic Syndrome in Nigerians With Type 2 Diabetes MellitusPaul Gesswein FonatabaNo ratings yet
- Optimal Hba1C Cutoff For Detecting Diabetic RetinopathyDocument6 pagesOptimal Hba1C Cutoff For Detecting Diabetic RetinopathyLacazette AubameyangNo ratings yet
- Full TextDocument8 pagesFull TextJeNeth RevilNo ratings yet
- The Association Between Estimated Average Glucose Levels and Fasting Plasma Glucose LevelsDocument4 pagesThe Association Between Estimated Average Glucose Levels and Fasting Plasma Glucose LevelsRina MachdalenaNo ratings yet
- Effects of A High-Protein Diet On Cardiometabolic Health, Vascular Function, and Endocannabinoids - A Preview StudyDocument9 pagesEffects of A High-Protein Diet On Cardiometabolic Health, Vascular Function, and Endocannabinoids - A Preview Studysiti lestariNo ratings yet
- 1595 FullDocument7 pages1595 FullHerly Maulida SurdhawatiNo ratings yet
- Glycemic Index, Glycemic Load, and Blood Pressure: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsDocument15 pagesGlycemic Index, Glycemic Load, and Blood Pressure: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsLisiane PerinNo ratings yet
- Hypertension Management Algorithm For Type 2 Diabetic Patients Applied in Primary CareDocument5 pagesHypertension Management Algorithm For Type 2 Diabetic Patients Applied in Primary CareMarco Free-MindNo ratings yet
- Changes in Glycemic Control From 1996 To 2006 Among Adults With Type 2 Diabetes: A Longitudinal Cohort StudyDocument6 pagesChanges in Glycemic Control From 1996 To 2006 Among Adults With Type 2 Diabetes: A Longitudinal Cohort StudyReny NapitupuluNo ratings yet
- Effect of Increasing Duration of Diabetes Mellitus Type 2 On Glycated Hemoglobin and Insulin SensitivityDocument5 pagesEffect of Increasing Duration of Diabetes Mellitus Type 2 On Glycated Hemoglobin and Insulin SensitivityAlifLaelaNo ratings yet
- 881 Full PDFDocument5 pages881 Full PDFRizki GiofaniNo ratings yet
- Jurnal TerbaruDocument5 pagesJurnal TerbaruSuci Ramadhani PutriNo ratings yet
- 64 Ej16-0546Document8 pages64 Ej16-0546jzhongg91No ratings yet
- Mean Platelet Volume in Type 2 Diabetic Patients.: J Diabetes ComplicationsDocument1 pageMean Platelet Volume in Type 2 Diabetic Patients.: J Diabetes ComplicationsummibarchiaNo ratings yet
- Introduction: Diabetes Mellitus (DM) Is The Most Common Endocrine ProblemDocument6 pagesIntroduction: Diabetes Mellitus (DM) Is The Most Common Endocrine ProblemHeribertus Andi WidagdoNo ratings yet
- Assessment and Treatment of Hyperglycemia in Critically IllDocument6 pagesAssessment and Treatment of Hyperglycemia in Critically IllYousif ElmasryNo ratings yet
- An Evaluation of The Accuracy of A Flash Glucose Monitoring System in Children With Diabetes in Comparison With Venous Blood GlucoseDocument8 pagesAn Evaluation of The Accuracy of A Flash Glucose Monitoring System in Children With Diabetes in Comparison With Venous Blood GlucosesovalaxNo ratings yet
- Wang 2020Document10 pagesWang 2020DR VENKATARAMANA MurthyNo ratings yet
- Obsgyn Referat FullDocument3 pagesObsgyn Referat FullasdaadNo ratings yet
- 2021 Journal of Personalized Medicine. 11 (8) 799Document14 pages2021 Journal of Personalized Medicine. 11 (8) 799Sofa ChaNo ratings yet
- Jurnal Proposal7Document14 pagesJurnal Proposal7ArjunaPamungkasNo ratings yet
- Nutrients: Dietary Salt Restriction in Chronic Kidney Disease: A Meta-Analysis of Randomized Clinical TrialsDocument15 pagesNutrients: Dietary Salt Restriction in Chronic Kidney Disease: A Meta-Analysis of Randomized Clinical TrialsMutiara Putri UtamiNo ratings yet
- Gornik 2007Document6 pagesGornik 2007Sintya RadhayantiNo ratings yet
- Implications of The United Kingdom Prospective Diabetes StudyDocument5 pagesImplications of The United Kingdom Prospective Diabetes StudyAgustin MendezNo ratings yet
- Articulo Chingon E.FDocument4 pagesArticulo Chingon E.FRuggery LeonNo ratings yet
- 1 s2.0 S0168822703002201 MainDocument7 pages1 s2.0 S0168822703002201 MainaasdaNo ratings yet
- tmpFF74 TMPDocument2 pagestmpFF74 TMPFrontiersNo ratings yet
- Insulin Detemir and Basal Insulin TherapyDocument7 pagesInsulin Detemir and Basal Insulin Therapymayrapp16No ratings yet
- Research ArticleDocument8 pagesResearch ArticlebegumbahceciNo ratings yet
- The Effects of High Haematocrit Levels On Glucose Metabolism DisordersDocument5 pagesThe Effects of High Haematocrit Levels On Glucose Metabolism DisordersTsegay AsefawNo ratings yet
- 881 Full PDFDocument5 pages881 Full PDFrizki giofaniNo ratings yet
- DSPN ResearchFormDocument5 pagesDSPN ResearchFormThanisha SanthoshNo ratings yet
- The Efficacy and Safety of Triple Vs Dual Combination of ARB, CCB, and DiureticsDocument9 pagesThe Efficacy and Safety of Triple Vs Dual Combination of ARB, CCB, and DiureticsLucky PratamaNo ratings yet
- Continuous Glucose MonitoringFrom EverandContinuous Glucose MonitoringWeiping JiaNo ratings yet
- Pediatric Notes: Nutrition and Metabolic DiseaseDocument33 pagesPediatric Notes: Nutrition and Metabolic DiseasefraditayyunusNo ratings yet
- Igd ManDocument1 pageIgd ManfraditayyunusNo ratings yet
- AanDocument1 pageAanfraditayyunusNo ratings yet
- Poed APN: Jadwal Jaga Kepaniteraan Klinik Rsud Labuang Baji Periode 7 - 14 Desember 2014Document2 pagesPoed APN: Jadwal Jaga Kepaniteraan Klinik Rsud Labuang Baji Periode 7 - 14 Desember 2014fraditayyunusNo ratings yet
- Victoria Secret Body (A Month On December !) : Step 1 60 Dumbell Side LungesDocument5 pagesVictoria Secret Body (A Month On December !) : Step 1 60 Dumbell Side LungesfraditayyunusNo ratings yet
- Morning Report: Emergency Room Wahidin Sudirohusodo General Hospital Makassar July 9th, 2014Document20 pagesMorning Report: Emergency Room Wahidin Sudirohusodo General Hospital Makassar July 9th, 2014fraditayyunusNo ratings yet
- Mechanism of Trauma Lauge-Hansen Classification: Acute Fractures and Dislocations in Netter's and Sport MedicineDocument4 pagesMechanism of Trauma Lauge-Hansen Classification: Acute Fractures and Dislocations in Netter's and Sport MedicinefraditayyunusNo ratings yet
- P ('t':'3', 'I':'3054456811') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Document4 pagesP ('t':'3', 'I':'3054456811') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)fraditayyunusNo ratings yet
- Guidelines For Mini Research Projects/ Programmes: BackgroundDocument4 pagesGuidelines For Mini Research Projects/ Programmes: BackgroundSurya Singh TiwariNo ratings yet
- NanotechnologyDocument32 pagesNanotechnologyAshwin KumarNo ratings yet
- Chapter 1: Exploring Data: Section 1.2Document16 pagesChapter 1: Exploring Data: Section 1.2张书No ratings yet
- Electrical Machines and EquipmentDocument76 pagesElectrical Machines and EquipmentsirageldeenNo ratings yet
- Class 7 Integers Word Problems: C C C CDocument1 pageClass 7 Integers Word Problems: C C C CAnjali SainiNo ratings yet
- Nalanda Modern Public School: Unit Test-1 (July) DATE SHEET (2022-23) Timing - 40 Minutes (1 Period)Document1 pageNalanda Modern Public School: Unit Test-1 (July) DATE SHEET (2022-23) Timing - 40 Minutes (1 Period)Vansh GoelNo ratings yet
- Ef3e Int Filetest 07bDocument5 pagesEf3e Int Filetest 07bCarlos Daniel Lupaca ChipanaNo ratings yet
- List of Computer Sindh Board of Technical EducationDocument17 pagesList of Computer Sindh Board of Technical Educationmuhamedshuaibbhai50% (2)
- Quantum Compatibility RulesDocument4 pagesQuantum Compatibility RulesAbel AndradaNo ratings yet
- Lec 3 - AssumptionsDocument13 pagesLec 3 - AssumptionsPriyadharshan BobbyNo ratings yet
- Bourdieu, Pierre & Angela Zanott-Karp. 1968. Structuralism & Theory of Sociological KnowledgeDocument27 pagesBourdieu, Pierre & Angela Zanott-Karp. 1968. Structuralism & Theory of Sociological KnowledgeDrew HopkinsNo ratings yet
- DR Giron 1 K To 12 Enhanced Edited PATEF 2 August 22 2013 1 PDFDocument80 pagesDR Giron 1 K To 12 Enhanced Edited PATEF 2 August 22 2013 1 PDFJaquelyn Dela Victoria100% (3)
- Uel Secondary Standards Tracker 2012Document13 pagesUel Secondary Standards Tracker 2012api-229636179No ratings yet
- DLP in Science 3 Day 1Document6 pagesDLP in Science 3 Day 1Wilmar MondidoNo ratings yet
- Activity Guide For JuniorsDocument2 pagesActivity Guide For JuniorsMELISSA PANAGANo ratings yet
- Magazine CoverDocument2 pagesMagazine Coverapi-330469878No ratings yet
- Momentum TransferDocument40 pagesMomentum TransferDecien Dee Ferraren-De CagalitanNo ratings yet
- ROD REYES LAC Form-4 Module 1Document3 pagesROD REYES LAC Form-4 Module 1Rodrigo Reyes88% (8)
- SWDD TemplateDocument6 pagesSWDD TemplateSulthonul MubarokNo ratings yet
- Producing Clinical Laboratory Shift Tables From Adam Data: Rao Bingi, Octagon Research Solutions, Wayne, PADocument12 pagesProducing Clinical Laboratory Shift Tables From Adam Data: Rao Bingi, Octagon Research Solutions, Wayne, PAlenithNo ratings yet
- Data Domain DD OS 5.4 Hardware Installation: Student GuideDocument83 pagesData Domain DD OS 5.4 Hardware Installation: Student GuideLouis Thierry Ekwa Bekok0% (1)
- Daily Lesson Log School Grade Level Teacher Learning Area MATHEMATICS Dates and Time November 15, 2022 QuarterDocument7 pagesDaily Lesson Log School Grade Level Teacher Learning Area MATHEMATICS Dates and Time November 15, 2022 QuarterRydan MinorNo ratings yet
- 2Nd Generation Cpted: An Antidote To The Social Y2K Virus of Urban DesignDocument19 pages2Nd Generation Cpted: An Antidote To The Social Y2K Virus of Urban DesignFábio SalvadorNo ratings yet
- QMM Assignment 2Document2 pagesQMM Assignment 2Ambika Sharma0% (1)
- Link L6 U1 Writing ProjectDocument1 pageLink L6 U1 Writing ProjectAlexNo ratings yet
- Binary To DecimalDocument13 pagesBinary To DecimalCyrus R. FloresNo ratings yet
- Policy Review: Myanmar Migrants To Thailand and Implications ToDocument9 pagesPolicy Review: Myanmar Migrants To Thailand and Implications ToKo NgeNo ratings yet
- IKOS Ability Test June 2009Document6 pagesIKOS Ability Test June 2009cocoNo ratings yet
- Core Java PDFDocument177 pagesCore Java PDFpratikshaNo ratings yet
P ('t':'3', 'I':'3054456811') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)
P ('t':'3', 'I':'3054456811') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)
Uploaded by
fraditayyunusOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
P ('t':'3', 'I':'3054456811') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)
P ('t':'3', 'I':'3054456811') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)
Uploaded by
fraditayyunusCopyright:
Available Formats
SHORT COMMUNICATION
HbA
1c
and mean blood glucose show stronger
associations with cardiovascular disease risk factors
than do postprandial glycaemia or glucose variability
in persons with diabetes: the A1C-Derived Average Glucose
(ADAG) study
R. Borg & J. C. Kuenen & B. Carstensen & H. Zheng &
D. M. Nathan & R. J. Heine & J. Nerup &
K. Borch-Johnsen & D. R. Witte &
on behalf of the ADAG Study Group
Received: 9 March 2010 / Accepted: 16 August 2010 / Published online: 1 October 2010
# The Author(s) 2010. This article is published with open access at Springerlink.com
Abstract
Aims Increased glucose excursions and postprandial hyper-
glycaemia have been suggested as unique risk factors for
cardiovascular disease (CVD) and mortality in patients with
diabetes mellitus. Much of the evidence is based on a single
2 h glucose value after oral glucose tolerance testing in
epidemiological studies. We examined the association
between various indices of glycaemia measured during
everyday activities and metabolic CVD risk factors in the
A1C-Derived Average Glucose (ADAG) study.
Methods Participants (268 with type 1 diabetes, 159 with
type 2 diabetes) completed 16 weeks of intensive continuous
glucose monitoring (CGM) and self-monitoring of blood
glucose (SMBG). From these data, common indices of
postprandial glycaemia, overall hyperglycaemia, glucose
variability and HbA
1c
were derived. The associations
between glycaemic indices and known CVD risk factors
(lipids, high-sensitivity C-reactive protein and blood pres-
sure) were explored in linear regression models.
Results For both diabetes types, the overall strongest
associations with CVD risk factors were seen for the
measures of average glycaemia (mean blood glucose and
HbA
1c
). Associations between self-monitored postprandial
and fasting glucose and CVD risk factors were weaker, but
significant. Measurements of blood glucose variability
showed non-significant associations. Overall, calculations
based on CGM were not more informative than those based
on frequent SMBG.
Conclusions/interpretation Mean glycaemia and HbA
1c
show consistent and stronger associations with CVD risk
factors than fasting glucose or postprandial glucose levels
or measures of glucose variability in patients with diabetes.
Keywords ADAG study
.
CVD risk
.
Glucose monitoring
.
Glucose variability
.
HbA
1c
.
Postprandial glycaemia
.
z score
Abbreviations
ADAG A1C-Derived Average Glucose study
BG Blood glucose
CGM Continuous glucose monitoring
The Electronic supplementary material (ESM) contains a list of
members of the ADAG Study Group
Electronic supplementary material The online version of this article
(doi:10.1007/s00125-010-1918-2) contains supplementary material,
which is available to authorised users.
R. Borg (*)
:
B. Carstensen
:
J. Nerup
:
K. Borch-Johnsen
:
D. R. Witte
Steno Diabetes Center A/S,
Niels Steensens Vej 2-4,
DK-2820 Gentofte, Denmark
e-mail: RBrg@steno.dk
J. C. Kuenen
:
R. J. Heine
VU University Medical Center,
Amsterdam, the Netherlands
H. Zheng
:
D. M. Nathan
Diabetes Center and Biostatistics Department,
Massachusetts General Hospital and Harvard Medical School,
Boston, MA, USA
R. J. Heine
Eli Lilly and Company,
Indianapolis, IN, USA
Diabetologia (2011) 54:6972
DOI 10.1007/s00125-010-1918-2
CVD Cardiovascular disease
hs-CRP High-sensitivity C-reactive protein
PPG Postprandial glucose concentration
SMBG Self-monitored blood glucose concentration
Introduction
The role of postprandial hyperglycaemia and glucose
variability in relation to the risk of cardiovascular disease
(CVD) is heavily debated [14]. Treatment regimens and
guidelines have increasingly focused on the control of
postprandial glucose concentration (PPG) as an additional
target beyond average glucose (HbA
1c
) control. Much of
the evidence is based on single glucose concentration
values after oral glucose tolerance testing [5, 6]. Direct
evidence for an additional effect of controlling PPG
excursions, over and above an effect on reduced average
glucose levels, on relevant diabetic endpoints is limited.
The objective of this study was to examine the association
between different indices of glycaemia, monitored inten-
sively during daily life activities, and CVD risk factors in the
A1C-Derived Average Glucose (ADAG) study.
Methods
The ADAG study (20062008) defined the mathematical
relationship between HbA
1c
and average glucose levels,
and included 268 individuals with type 1 diabetes mellitus
and 159 with type 2 diabetes mellitus. A full description of
the ADAG study has been published previously [7]. The
study was approved by the human studies committees at the
participating institutions and informed consent was obtained
from all participants.
Continuous glucose monitoring (CGM) (Medtronic
Minimed, Northridge, CA, USA) was performed at baseline
and three times at 4 week intervals during the 12 week
study period. Monitoring lasted at least 48 h, during which
glucose levels were assessed every 5 min. Furthermore,
participants performed an eight-point profile of self-
monitored blood glucose (SMBG) (preprandial, 90 min
postprandial, bedtime and 03:00 hours) with a Hemocue
Glucose 201 Plus meter (Hemocue, Angelholm, Sweden)
during the days of CGM. During the weeks when CGM
was not performed, participants performed a seven-point
SMBG (preprandial, postprandial and bedtime) (OneTouch
Ultra; Lifescan, Milpitas, CA, USA) for at least 3 days per
week. All BG values stated are plasma equivalents.
The average BG concentration and SD were calculated
based on CGM data and the seven-point SMBG (Lifescan)
data. A combined average BG was calculated from CGM
and SMBG [7].
Two validated indices of intraday glucose variability
were calculated based on CGM: the mean amplitude of
glycaemic excursions (MAGE) and the continuous over-
lapping net glycaemic action (CONGA) [8, 9].
As an indicator of overall hyperglycaemia, the area under
the CGM curve (AUC) above levels of 7.8 or 11.1 mmol/l
(140 or 200 mg/dl) was calculated for the first 24 h of each
CGM monitoring period. Also, a postprandial AUC was
calculated for periods of 2 h after meals (without thresholds),
and a postprandial increment was calculated from the
preprandial glucose level to the highest peak within 2 h after
meals. Pre- and postprandial measurements from SMBG
(HemoCue) were used to calculate mean pre- and postprandial
BG, as well as pre- and post-breakfast, lunch and dinner values.
The pre-breakfast BG was used as fasting BG. All indices
based on CGM were calculated after exclusion of the initial 2 h
of monitoring, considered to be the unstable calibration period.
HbA
1c
samples were analysed by DCCT-aligned assays;
the mean value at the end of the 12 week study period was
used [7]. Samples for lipids and high-sensitivity C-reactive
protein (hs-CRP) analyses were obtained at baseline (not
necessarily fasting) and analysed by validated methods at a
central laboratory (for details, see Electronic supplementary
material [ESM] Methods).
The associations of the calculated glycaemic indices
with the CVD risk factors were explored in separate linear
regression models adjusted for sex, age, smoking and
diabetes type. To facilitate comparison of associations,
glycaemic variables were standardised by the study popu-
lation SD. Each regression estimate represents the change
in the individual CVD risk factor per population SD change
in the explanatory variable. Non-standardised estimates are
given as examples in clinically relevant units.
In order to assess the combined cardiovascular risk, a
summed z score was calculated. CVD risk factors were
standardised (based on the distribution within each diabetes
type), and combined within the groups of lipids, blood
pressure, inflammation and anthropometrics (for details, see
ESM Methods). The z score was used as an additional
outcome variable in regression analyses with and without
stratification by diabetes type. The stratified estimates were
tested for interaction.
Results
Glucose monitoring was completed by 427 participants
with diabetes, leading to approximately 2,700 glucose
values per participant. We excluded one participant (type
1 diabetes mellitus) due to erroneous pre- and postprandial
Hemocue measurements.
Characteristics of the study population are summarised
in ESM Table 1.
70 Diabetologia (2011) 54:6972
When examining the associations between different
glycaemic indices and known CVD risk factors, HbA
1c
and mean BG consistently showed statistically significant
associations with the different risk factors with a larger
magnitude than most of the associations of the self-
monitored PPG measurements (ESM Table 2). PPG based
on CGM, fasting BG and overall hyperglycaemia also
showed statistically significant associations with CVD risk
factors, albeit at a lower level. Indices of glucose variability
and postprandial increment did not show significant
associations. A similar pattern of associations was present
for the various lipid measures, blood pressure and hs-CRP.
Adjustment for antihypertensive treatment or lipid lowering
medication, or exclusion of all participants with these
treatments, did not substantially alter the results.
Overall, the indices based on CGM were not more
informative than those based on frequent SMBG.
Higher levels of HbA
1c
were associated with higher
systolic blood pressure (2.2 mmHg per percentage unit
HbA
1c),
higher total cholesterol (0.1 mmol/l per percentage
unit HbA
1c
), higher hs-CRP (0.39 mg/ml per percentage
unit HbA
1c
) and lower HDL-cholesterol (0.04 mmol/l per
percentage unit HbA
1c
) (ESM Table 3)
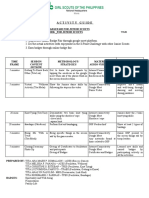
The associations of the different glycaemic indices with
the combined CVD z score are illustrated in Fig. 1. Both for
the total group (in grey) and for the two diabetes types (in
black), the strongest associations were seen with the
measures of average glycaemia (mean BG and HbA
1c
)
and with the mean of all self-monitored postprandial BG
values. The difference between estimates for the two
diabetes types was not statistically significant (p values
between 0.15 and 0.92). The associations of the variability
indices with the CVD z score were not statistically
significant.
Discussion
We found that average glucose and HbA
1c
showed the
strongest associations with CVD risk factors among a wide
set of indicators of glycaemia and variability. Indices of
glycaemic variability showed no significant associations
with CVD risk factors.
Elevated postprandial glucose levels and/or glucose
variability have been suggested to increase the risk of CVD
beyond their effect on overall hyperglycaemia. Only a few
studies have tested this hypothesis directly or compared the
effect with that of overall glucose exposure (HbA
1c
) and
shown postprandial glucose levels and/or glucose variability
to be independent mechanisms. One single-blind randomised
trial comparing the effects of two insulin secretagogues with
different effects on PPG found that control of postprandial
hyperglycaemia led to a reduction in carotid intimamedia
thickness in patients with type 2 diabetes compared with the
control group [1]. Therapy with lower PPG levels was
associated with significant reductions in the concentrations
of the inflammatory markers IL6 and hs-CRP. However, a
recent randomised clinical trial in patients with type 2
diabetes mellitus and CVD did not support an added benefit
of targeting control of PPG for subsequent CVD events [4].
In our study, glucose variability and postprandial hyper-
glycaemia did not have a stronger association with known
metabolic CVD risk factors than measures of average
glucose. This suggests that the impact of PPG on cardio-
vascular risk is likely to be captured by the assessment of
average blood glucose or HbA
1c
.
Several of the epidemiological studies demonstrating an
association between post-OGTT hyperglycaemia and in-
creased CVD and mortality did not take an average glucose
measurement (for example HbA
1c
) into account [2, 5].
In type 1 diabetes mellitus, glucose variability has not
been shown to be associated with the development of
complications. In the DCCT, BG variability (from seven-
point profiles) did not appear to be a factor in the
development of microvascular complications, and pre- and
postprandial glucose values contributed equally to small-
vessel complications [10].
The strength of this study is the analysis of glycaemia
under real-life circumstances in a large number of individ-
uals with diabetes. Intensive glucose monitoring using
several methods allowed us to compare several approaches
for defining PPG, and provided sufficient measurements to
reliably assess the different features of glycaemia.
0.2 0.1 0.0 0.1 0.2 0.3
CVD risk factor z score
Variability: Mage (CGM)
Variability: Conga4 (CGM)
Variability: SD (CGM)
Variability: SD (SMBG)
Postprandial increment (CGM)
Postprandial BG (SMBG)
Postprandial BG (AUC2h CGM)
Fasting BG (SMBG)
Overall hyperglycaemia (AUC >11.1 mmol/l)
Overall hyperglycaemia (AUC >7.8 mmol/l)
HbA
1c
Mean BG
Fig. 1 Standardised associations between different glycaemic indices
and the z score derived from the CVD risk factors (associations per 1
population SD with 95% CI). Upper and lower black bars are for
patients with type 1 and type 2 diabetes mellitus, respectively; middle
grey bars are for both groups together (controlling for diabetes type).
Postprandial BG (AUC 2hpp CGM), area under the continuous
glucose monitoring curve 2 h postprandially; CONGA
4
, continuous
overlapping net glycaemic action (n=4 h); MAGE, mean amplitude of
glycaemic excursions
Diabetologia (2011) 54:6972 71
The main limitation of the study is its cross-sectional
character. While it has a very high resolution, glucose
monitoring is short term and our outcomes are CVD risk
factors rather than actual CVD events. Therefore, although
we cannot reach direct conclusions regarding the impact of
postprandial glucose levels or glucose variability on CVD
endpoints, our results show that, if such an effect exists, it
is likely to be mediated through mechanisms other than
those examined in our study. The CVD risk factors we
chose are well-validated risk factors for CVD (lipids, blood
pressure and hs-CRP). Treatment to lower these CVD risk
factors might have confounded our findings.
The participants had stable HbA
1c
at baseline (defined as
a <1 percentage unit change in HbA
1c
during the 6 months
prior to the study), and were relatively stable during the
study. We may therefore have limited the range of glucose
variability as seen in a diabetic population. However, high
levels of glucose variability were seen among our individ-
uals despite stable HbA
1c
levels.
Our results do not support a unique role of postprandial
hyperglycaemia in CVD. Monitoring PPG and glucose
variability may be important in adjusting treatment to
achieve target mean glycaemia and to avoid daily excur-
sions, but our results suggest that interventions to reduce
the risk of CVD are best aimed at controlling mean glucose
and HbA
1c
.
We conclude that mean glycaemia and HbA
1c
show
stronger and consistent associations with CVD risk factors
than fasting glucose and most measures of postprandial
glucose and glucose variability. The previously observed
associations between glucose variability and postprandial
hyperglycaemia (often OGTT-based) and CVD events
cannot be explained by an association with CVD risk factors.
Acknowledgements The ADAG study was supported by research
grants from the ADA and EASD. Financial support was provided by
Abbott Diabetes Care, Bayer Healthcare, GlaxoSmithKline, sanofi-
aventis Netherlands, Merck, Lifescan and Medtronic Minimed, and
supplies and equipment were provided by Medtronic Minimed,
Lifescan and Hemocue. The assessment of CVD risk factor analyses
was supported by research grants from the Sehested Hansen Founda-
tion, Steno Diabetes Center and the Danish Diabetes Association.
Duality of interest R. J. Heine is employed by and owns stocks of
Eli Lilly. K. Borch-Johnsen is head of the Steno Diabetes Center, a
hospital integrated in the Danish National Healthcare Service but
owned by Novo Nordisk. K. Borch-Johnsen holds shares in Novo
Nordisk. The other authors have no duality of interest associated with
this manuscript.
Open Access This article is distributed under the terms of the
Creative Commons Attribution Noncommercial License which per-
mits any noncommercial use, distribution, and reproduction in any
medium, provided the original author(s) and source are credited.
References
1. Esposito K, Giugliano D, Nappo F, Marfella R (2004) Regression
of carotid atherosclerosis by control of postprandial hyperglycemia
in type 2 diabetes mellitus. Circulation 110:214219
2. Hanefeld M, Fischer S, Julius U et al (1996) Risk factors for
myocardial infarction and death in newly detected NIDDM: the
Diabetes Intervention Study, 11-year follow-up. Diabetologia 39:
15771583
3. Lefebvre P, Scheen AJ (1998) The postprandial state and risk of
cardiovascular disease. Diabet Med 15:S63S68
4. Raz I, Wilson PWF, Strojek K et al (2009) Effects of prandial vs
fasting glycemia on cardiovascular outcomes in type 2 diabetes:
the HEART2D trial. Diabetes Care 32:381386
5. Glucose tolerance and mortality: comparison of WHO and
American Diabetes Association diagnostic criteria. The DECODE
study group. European Diabetes Epidemiology Group. Diabetes
Epidemiology: Collaborative analysis Of Diagnostic criteria in
Europe (1999). Lancet 354:617621
6. Barrett-Connor E, Ferrara A (1998) Isolated postchallenge
hyperglycemia and the risk of fatal cardiovascular disease in
older women and men: the Rancho Bernardo study. Diabetes Care
21:12361239
7. Nathan DM, Kuenen J, Borg R et al (2008) Translating the A1C
assay into estimated average glucose values. Diabetes Care 31:
14731478
8. Service FJ, Molnar GD, Rosevear JW, Ackerman E, Gatewood
LC, Taylor WF (1970) Mean amplitude of glycemic excursions, a
measure of diabetic instability. Diabetes 19:644655
9. McDonnell CM, Donath SM, Vidmar SI, Werther GA, Cameron
FJ (2005) A novel approach to continuous glucose analysis
utilizing glycemic variation. Diabetes Technol Ther 7:253263
10. Kilpatrick ES, Rigby AS, Atkin SL (2006) The effect of glucose
variability on the risk of microvascular complications in type 1
diabetes. Diabetes Care 29:14861490
72 Diabetologia (2011) 54:6972
You might also like
- (ASRA) Guidelines Neuraxial and AnticoagulationDocument6 pages(ASRA) Guidelines Neuraxial and Anticoagulationfraditayyunus82% (11)
- KUKA Programming NotesDocument13 pagesKUKA Programming Notes92dalliNo ratings yet
- Jurnal 5Document4 pagesJurnal 5MFWPNo ratings yet
- Glycated Haemoglobin As A Stable Indicator Of: Hba C Type 2 DiabetesDocument4 pagesGlycated Haemoglobin As A Stable Indicator Of: Hba C Type 2 DiabetesfamtaluNo ratings yet
- Correlation of Fasting and Postprandial Plasma Glucose With Hba1C in Assessing Glycemic Control Systematic Review and Meta-AnalysisDocument9 pagesCorrelation of Fasting and Postprandial Plasma Glucose With Hba1C in Assessing Glycemic Control Systematic Review and Meta-AnalysisRodas GetachewNo ratings yet
- Schwingshackl2013 PDFDocument8 pagesSchwingshackl2013 PDFLisiane PerinNo ratings yet
- Glyca AlbuminDocument8 pagesGlyca AlbuminElang SudewaNo ratings yet
- Association of Coagulation Profile With Microvascular Complications and Glycemic Control in Type 2 Diabetes Mellitus - A Study ADocument1 pageAssociation of Coagulation Profile With Microvascular Complications and Glycemic Control in Type 2 Diabetes Mellitus - A Study Aseneh17198No ratings yet
- Glycemic Variability June 12 2014Document42 pagesGlycemic Variability June 12 2014Hemant GaurkarNo ratings yet
- Glucose Variability - FullDocument12 pagesGlucose Variability - FullAlina PopaNo ratings yet
- Bismillah Fix Hba1c1Document23 pagesBismillah Fix Hba1c1NsafifahNo ratings yet
- tmp2475 TMPDocument7 pagestmp2475 TMPFrontiersNo ratings yet
- GA, 1,5 AG and HbA1cDocument7 pagesGA, 1,5 AG and HbA1cLegina AdityaNo ratings yet
- Clinical Study: The Effects of Glucose Fluctuation On The Severity of Coronary Artery Disease in Type 2 Diabetes MellitusDocument6 pagesClinical Study: The Effects of Glucose Fluctuation On The Severity of Coronary Artery Disease in Type 2 Diabetes MellitusEgi Dwi SatriaNo ratings yet
- 7 FFCDocument8 pages7 FFCHow to youNo ratings yet
- DiabetesDocument8 pagesDiabetesDanielValenciaNo ratings yet
- Diabetes Care Glucosa Promedio EstimadaDocument6 pagesDiabetes Care Glucosa Promedio EstimadaGemeneza GonzalesNo ratings yet
- HBA1CVARIABILITYDocument17 pagesHBA1CVARIABILITYThanisha SanthoshNo ratings yet
- Translating The A1C Assay Into Estimated Average Glucose ValuesDocument6 pagesTranslating The A1C Assay Into Estimated Average Glucose ValuesFaryalBalochNo ratings yet
- Nutritional Status in Patients With Diabetes and Chronic Kidney Disease: A Prospective StudyDocument6 pagesNutritional Status in Patients With Diabetes and Chronic Kidney Disease: A Prospective StudyHenry HadiantoNo ratings yet
- Research ArticleDocument12 pagesResearch ArticleRodas GetachewNo ratings yet
- Bismillah Fix Hba1c2Document7 pagesBismillah Fix Hba1c2NsafifahNo ratings yet
- Hba1c VariabilityDocument5 pagesHba1c Variabilityruruh_wibowoNo ratings yet
- DZ Tip II CancerDocument7 pagesDZ Tip II CancerAndreeaGheorgheNo ratings yet
- Relationship Between Hba1c and Complete Blood Count Parameters in Adult Patients With Type 2 Diabetes in Saudi ArabiaDocument7 pagesRelationship Between Hba1c and Complete Blood Count Parameters in Adult Patients With Type 2 Diabetes in Saudi ArabiaIJAR JOURNALNo ratings yet
- Mia Now Ska 2010Document8 pagesMia Now Ska 2010Anonymous 2AiYmQ1dNo ratings yet
- Estudio NICE - Sugar (2009)Document11 pagesEstudio NICE - Sugar (2009)Trt CamargoNo ratings yet
- Dietary Fiber DMDocument8 pagesDietary Fiber DMAnnisa SavitriNo ratings yet
- Relationship Between C-Reactive Protein, White Blood Cell Count and Metabolic Syndrome in Nigerians With Type 2 Diabetes MellitusDocument11 pagesRelationship Between C-Reactive Protein, White Blood Cell Count and Metabolic Syndrome in Nigerians With Type 2 Diabetes MellitusPaul Gesswein FonatabaNo ratings yet
- Optimal Hba1C Cutoff For Detecting Diabetic RetinopathyDocument6 pagesOptimal Hba1C Cutoff For Detecting Diabetic RetinopathyLacazette AubameyangNo ratings yet
- Full TextDocument8 pagesFull TextJeNeth RevilNo ratings yet
- The Association Between Estimated Average Glucose Levels and Fasting Plasma Glucose LevelsDocument4 pagesThe Association Between Estimated Average Glucose Levels and Fasting Plasma Glucose LevelsRina MachdalenaNo ratings yet
- Effects of A High-Protein Diet On Cardiometabolic Health, Vascular Function, and Endocannabinoids - A Preview StudyDocument9 pagesEffects of A High-Protein Diet On Cardiometabolic Health, Vascular Function, and Endocannabinoids - A Preview Studysiti lestariNo ratings yet
- 1595 FullDocument7 pages1595 FullHerly Maulida SurdhawatiNo ratings yet
- Glycemic Index, Glycemic Load, and Blood Pressure: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsDocument15 pagesGlycemic Index, Glycemic Load, and Blood Pressure: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsLisiane PerinNo ratings yet
- Hypertension Management Algorithm For Type 2 Diabetic Patients Applied in Primary CareDocument5 pagesHypertension Management Algorithm For Type 2 Diabetic Patients Applied in Primary CareMarco Free-MindNo ratings yet
- Changes in Glycemic Control From 1996 To 2006 Among Adults With Type 2 Diabetes: A Longitudinal Cohort StudyDocument6 pagesChanges in Glycemic Control From 1996 To 2006 Among Adults With Type 2 Diabetes: A Longitudinal Cohort StudyReny NapitupuluNo ratings yet
- Effect of Increasing Duration of Diabetes Mellitus Type 2 On Glycated Hemoglobin and Insulin SensitivityDocument5 pagesEffect of Increasing Duration of Diabetes Mellitus Type 2 On Glycated Hemoglobin and Insulin SensitivityAlifLaelaNo ratings yet
- 881 Full PDFDocument5 pages881 Full PDFRizki GiofaniNo ratings yet
- Jurnal TerbaruDocument5 pagesJurnal TerbaruSuci Ramadhani PutriNo ratings yet
- 64 Ej16-0546Document8 pages64 Ej16-0546jzhongg91No ratings yet
- Mean Platelet Volume in Type 2 Diabetic Patients.: J Diabetes ComplicationsDocument1 pageMean Platelet Volume in Type 2 Diabetic Patients.: J Diabetes ComplicationsummibarchiaNo ratings yet
- Introduction: Diabetes Mellitus (DM) Is The Most Common Endocrine ProblemDocument6 pagesIntroduction: Diabetes Mellitus (DM) Is The Most Common Endocrine ProblemHeribertus Andi WidagdoNo ratings yet
- Assessment and Treatment of Hyperglycemia in Critically IllDocument6 pagesAssessment and Treatment of Hyperglycemia in Critically IllYousif ElmasryNo ratings yet
- An Evaluation of The Accuracy of A Flash Glucose Monitoring System in Children With Diabetes in Comparison With Venous Blood GlucoseDocument8 pagesAn Evaluation of The Accuracy of A Flash Glucose Monitoring System in Children With Diabetes in Comparison With Venous Blood GlucosesovalaxNo ratings yet
- Wang 2020Document10 pagesWang 2020DR VENKATARAMANA MurthyNo ratings yet
- Obsgyn Referat FullDocument3 pagesObsgyn Referat FullasdaadNo ratings yet
- 2021 Journal of Personalized Medicine. 11 (8) 799Document14 pages2021 Journal of Personalized Medicine. 11 (8) 799Sofa ChaNo ratings yet
- Jurnal Proposal7Document14 pagesJurnal Proposal7ArjunaPamungkasNo ratings yet
- Nutrients: Dietary Salt Restriction in Chronic Kidney Disease: A Meta-Analysis of Randomized Clinical TrialsDocument15 pagesNutrients: Dietary Salt Restriction in Chronic Kidney Disease: A Meta-Analysis of Randomized Clinical TrialsMutiara Putri UtamiNo ratings yet
- Gornik 2007Document6 pagesGornik 2007Sintya RadhayantiNo ratings yet
- Implications of The United Kingdom Prospective Diabetes StudyDocument5 pagesImplications of The United Kingdom Prospective Diabetes StudyAgustin MendezNo ratings yet
- Articulo Chingon E.FDocument4 pagesArticulo Chingon E.FRuggery LeonNo ratings yet
- 1 s2.0 S0168822703002201 MainDocument7 pages1 s2.0 S0168822703002201 MainaasdaNo ratings yet
- tmpFF74 TMPDocument2 pagestmpFF74 TMPFrontiersNo ratings yet
- Insulin Detemir and Basal Insulin TherapyDocument7 pagesInsulin Detemir and Basal Insulin Therapymayrapp16No ratings yet
- Research ArticleDocument8 pagesResearch ArticlebegumbahceciNo ratings yet
- The Effects of High Haematocrit Levels On Glucose Metabolism DisordersDocument5 pagesThe Effects of High Haematocrit Levels On Glucose Metabolism DisordersTsegay AsefawNo ratings yet
- 881 Full PDFDocument5 pages881 Full PDFrizki giofaniNo ratings yet
- DSPN ResearchFormDocument5 pagesDSPN ResearchFormThanisha SanthoshNo ratings yet
- The Efficacy and Safety of Triple Vs Dual Combination of ARB, CCB, and DiureticsDocument9 pagesThe Efficacy and Safety of Triple Vs Dual Combination of ARB, CCB, and DiureticsLucky PratamaNo ratings yet
- Continuous Glucose MonitoringFrom EverandContinuous Glucose MonitoringWeiping JiaNo ratings yet
- Pediatric Notes: Nutrition and Metabolic DiseaseDocument33 pagesPediatric Notes: Nutrition and Metabolic DiseasefraditayyunusNo ratings yet
- Igd ManDocument1 pageIgd ManfraditayyunusNo ratings yet
- AanDocument1 pageAanfraditayyunusNo ratings yet
- Poed APN: Jadwal Jaga Kepaniteraan Klinik Rsud Labuang Baji Periode 7 - 14 Desember 2014Document2 pagesPoed APN: Jadwal Jaga Kepaniteraan Klinik Rsud Labuang Baji Periode 7 - 14 Desember 2014fraditayyunusNo ratings yet
- Victoria Secret Body (A Month On December !) : Step 1 60 Dumbell Side LungesDocument5 pagesVictoria Secret Body (A Month On December !) : Step 1 60 Dumbell Side LungesfraditayyunusNo ratings yet
- Morning Report: Emergency Room Wahidin Sudirohusodo General Hospital Makassar July 9th, 2014Document20 pagesMorning Report: Emergency Room Wahidin Sudirohusodo General Hospital Makassar July 9th, 2014fraditayyunusNo ratings yet
- Mechanism of Trauma Lauge-Hansen Classification: Acute Fractures and Dislocations in Netter's and Sport MedicineDocument4 pagesMechanism of Trauma Lauge-Hansen Classification: Acute Fractures and Dislocations in Netter's and Sport MedicinefraditayyunusNo ratings yet
- P ('t':'3', 'I':'3054456811') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Document4 pagesP ('t':'3', 'I':'3054456811') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)fraditayyunusNo ratings yet
- Guidelines For Mini Research Projects/ Programmes: BackgroundDocument4 pagesGuidelines For Mini Research Projects/ Programmes: BackgroundSurya Singh TiwariNo ratings yet
- NanotechnologyDocument32 pagesNanotechnologyAshwin KumarNo ratings yet
- Chapter 1: Exploring Data: Section 1.2Document16 pagesChapter 1: Exploring Data: Section 1.2张书No ratings yet
- Electrical Machines and EquipmentDocument76 pagesElectrical Machines and EquipmentsirageldeenNo ratings yet
- Class 7 Integers Word Problems: C C C CDocument1 pageClass 7 Integers Word Problems: C C C CAnjali SainiNo ratings yet
- Nalanda Modern Public School: Unit Test-1 (July) DATE SHEET (2022-23) Timing - 40 Minutes (1 Period)Document1 pageNalanda Modern Public School: Unit Test-1 (July) DATE SHEET (2022-23) Timing - 40 Minutes (1 Period)Vansh GoelNo ratings yet
- Ef3e Int Filetest 07bDocument5 pagesEf3e Int Filetest 07bCarlos Daniel Lupaca ChipanaNo ratings yet
- List of Computer Sindh Board of Technical EducationDocument17 pagesList of Computer Sindh Board of Technical Educationmuhamedshuaibbhai50% (2)
- Quantum Compatibility RulesDocument4 pagesQuantum Compatibility RulesAbel AndradaNo ratings yet
- Lec 3 - AssumptionsDocument13 pagesLec 3 - AssumptionsPriyadharshan BobbyNo ratings yet
- Bourdieu, Pierre & Angela Zanott-Karp. 1968. Structuralism & Theory of Sociological KnowledgeDocument27 pagesBourdieu, Pierre & Angela Zanott-Karp. 1968. Structuralism & Theory of Sociological KnowledgeDrew HopkinsNo ratings yet
- DR Giron 1 K To 12 Enhanced Edited PATEF 2 August 22 2013 1 PDFDocument80 pagesDR Giron 1 K To 12 Enhanced Edited PATEF 2 August 22 2013 1 PDFJaquelyn Dela Victoria100% (3)
- Uel Secondary Standards Tracker 2012Document13 pagesUel Secondary Standards Tracker 2012api-229636179No ratings yet
- DLP in Science 3 Day 1Document6 pagesDLP in Science 3 Day 1Wilmar MondidoNo ratings yet
- Activity Guide For JuniorsDocument2 pagesActivity Guide For JuniorsMELISSA PANAGANo ratings yet
- Magazine CoverDocument2 pagesMagazine Coverapi-330469878No ratings yet
- Momentum TransferDocument40 pagesMomentum TransferDecien Dee Ferraren-De CagalitanNo ratings yet
- ROD REYES LAC Form-4 Module 1Document3 pagesROD REYES LAC Form-4 Module 1Rodrigo Reyes88% (8)
- SWDD TemplateDocument6 pagesSWDD TemplateSulthonul MubarokNo ratings yet
- Producing Clinical Laboratory Shift Tables From Adam Data: Rao Bingi, Octagon Research Solutions, Wayne, PADocument12 pagesProducing Clinical Laboratory Shift Tables From Adam Data: Rao Bingi, Octagon Research Solutions, Wayne, PAlenithNo ratings yet
- Data Domain DD OS 5.4 Hardware Installation: Student GuideDocument83 pagesData Domain DD OS 5.4 Hardware Installation: Student GuideLouis Thierry Ekwa Bekok0% (1)
- Daily Lesson Log School Grade Level Teacher Learning Area MATHEMATICS Dates and Time November 15, 2022 QuarterDocument7 pagesDaily Lesson Log School Grade Level Teacher Learning Area MATHEMATICS Dates and Time November 15, 2022 QuarterRydan MinorNo ratings yet
- 2Nd Generation Cpted: An Antidote To The Social Y2K Virus of Urban DesignDocument19 pages2Nd Generation Cpted: An Antidote To The Social Y2K Virus of Urban DesignFábio SalvadorNo ratings yet
- QMM Assignment 2Document2 pagesQMM Assignment 2Ambika Sharma0% (1)
- Link L6 U1 Writing ProjectDocument1 pageLink L6 U1 Writing ProjectAlexNo ratings yet
- Binary To DecimalDocument13 pagesBinary To DecimalCyrus R. FloresNo ratings yet
- Policy Review: Myanmar Migrants To Thailand and Implications ToDocument9 pagesPolicy Review: Myanmar Migrants To Thailand and Implications ToKo NgeNo ratings yet
- IKOS Ability Test June 2009Document6 pagesIKOS Ability Test June 2009cocoNo ratings yet
- Core Java PDFDocument177 pagesCore Java PDFpratikshaNo ratings yet