Professional Documents
Culture Documents
In Vivo Animal Models in Preclinical Evaluation of Anti-Inflammatory Activity-A Review
In Vivo Animal Models in Preclinical Evaluation of Anti-Inflammatory Activity-A Review
Uploaded by
Nur Jannah Khairunnisa0 ratings0% found this document useful (0 votes)
394 views5 pagesThis document summarizes in vivo animal models used in preclinical evaluation of anti-inflammatory activity. It describes several common models, including UV-erythema in guinea pigs which measures delay of UV-induced erythema, vascular permeability tests in rats which measure inhibition of increased permeability induced by irritants, and oxazolone-induced ear edema in mice which quantifies anti-inflammatory effects by measuring edema reduction. These models are used to screen new substances by inducing inflammation through various agents and measuring the anti-inflammatory effects by the degree of reduction in inflammatory responses.
Original Description:
jurnal anti inflamasi
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document summarizes in vivo animal models used in preclinical evaluation of anti-inflammatory activity. It describes several common models, including UV-erythema in guinea pigs which measures delay of UV-induced erythema, vascular permeability tests in rats which measure inhibition of increased permeability induced by irritants, and oxazolone-induced ear edema in mice which quantifies anti-inflammatory effects by measuring edema reduction. These models are used to screen new substances by inducing inflammation through various agents and measuring the anti-inflammatory effects by the degree of reduction in inflammatory responses.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
394 views5 pagesIn Vivo Animal Models in Preclinical Evaluation of Anti-Inflammatory Activity-A Review
In Vivo Animal Models in Preclinical Evaluation of Anti-Inflammatory Activity-A Review
Uploaded by
Nur Jannah KhairunnisaThis document summarizes in vivo animal models used in preclinical evaluation of anti-inflammatory activity. It describes several common models, including UV-erythema in guinea pigs which measures delay of UV-induced erythema, vascular permeability tests in rats which measure inhibition of increased permeability induced by irritants, and oxazolone-induced ear edema in mice which quantifies anti-inflammatory effects by measuring edema reduction. These models are used to screen new substances by inducing inflammation through various agents and measuring the anti-inflammatory effects by the degree of reduction in inflammatory responses.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 5
Review Article ISSN 2277-3657
Available online at www.ijpras.com
Volume 1, issue2 (2012), 01-05
International Journal of
Pharmaceutical Research &
Allied Sciences
1
In Vivo Animal Models in Preclinical Evaluation of Anti-
Inflammatory Activity- A Review
Mitul Patel, Murugananthan, Shivalinge Gowda K,P.*
PES College of Pharmacy, Hanumanthanagagar, Bangalore-560050, India
*Corresponding author: shivalinge65@gmail.com
Abstract:
Inflammation is defined as the local response of living mammalian tissues to injury due to any agent.
Inflammation involves 2 basic processes early inflammatory response later followed by healing. There are two
types of inflammation, Acute and Chronic. Acute inflammation is of short duration and represents the early
body reaction, resolves quickly and is usually followed by healing. Chronic inflammation is defined as
prolonged process in which tissue destruction and inflammation occur at same time. The anti-inflammatory
activity of new substances can be evaluated by using various pre clinical screening method. Here by use of
various phlogestic agent like carragenan, brewer's yeast, dextran, egg albumin, kaolin, aerosil, croton oil, cotton
wool inflammation is induced and the amount of decrease in its inducing characteristics is measured.
Key words: Inflammation, brewers yeast, egg albumin, dextran
Introduction:
Inflammation is defined as the local response of
living mammalian tissues to injury due to any
agent. It is a body defence reaction to prevent the
spread of injurious agent and to remove the
necrosed cells and tissues. Inflammation may be
caused by like bacteria, viruses, fungi, parasites,
antigen-antibody reaction. Mechanical trauma,
organic and inorganic poisons and foreign bodies.
Inflammation involves 2 basic processes early
inflammatory response later followed by healing.
Signs of inflammation includes redness, swelling,
heat, pain, loss of function. There are two types of
inflammation, Acute and Chronic. Acute
inflammation is of short duration and represents the
early body reaction, resolves quickly and is usually
followed by healing. Chronic inflammation is
defined as prolonged process in which tissue
destruction and inflammation occur at same time.
[1]
In vivo animal models:
[2]
the inflammatory
response is accompanied by clinical signs of
erythema, edema, hyperalgesia and pain.
Inflammatory responses occur in three different
phases, each apparently mediated by different
mechanisms:
1. An acute transient phase characterised by local
vasodilation and increased capillary
permeability.
2. A subacute phase, characterised by
infilteration of leukocytes and phagocytic
cells.
3. A chronic proliferative phase, in which tissue
degeneration and fibrosis occurs.
Methods for testing acute and sub acute
inflammation are:
UV-erythema in guinea pigs
Vascular permeability
Oxazolone-induced ear edema in mice
Croton-oil ear edema in rats and mice
Paw edema in rats (various modifications and
various irritants)
Pleurisy tests
Granuloma pouch technique (various
modifications and various irritants)
The proliferative phase is measured by methods for
testing granuloma formation, such as:
Cotton wool granuloma
Glass rod granuloma
Methods for testing acute and sub acute
inflammation:
Available online at www.ijpras.com
2
1. UV-erythema in guinea pigs:
Prostaglandin E (PGE) levels in the skin have been
shown to be elevated during the 24 h period
following exposure of guinea pig skin to ultraviolet
radiation from 280-320 nm. The development of
increased PGE levels paralleled the development of
the delayed phase of erythema. Delay the
development of ultraviolet erythema on albino
guinea pig skin by systemic pretreatment with
clinically equivalent doses of phenylbutazone and
other nonsteroidal anti-inflammatory agents.
Erythema (redness) is the earliest sign of
inflammation, not yet accompanied by plasma
exudation and edema. This model depicts the delay
in development of UV erythema on albino guinea
pig skin by systemic pretreatment with clinically
equivalent doses of phenylbutazone and other
NSAIDs.
Procedure: Albino guinea pigs of both sexes with
an average weight of 350g are used. Four animals
are used each for treatment and control group.18 hr
prior testing, the animals are shaved on both the
flanks and on the back. Then they are chemically
depilated by a commercial depilation product or by
a suspension of barium sulphide. 20 min later, the
depilation paste and the fur are rinsed off in
running warm water. On the next day the test
compound is dissolved in the vehicle and half of
the test compound is administered by gavage (at 10
ml/kg) 30 min before UV exposure. Control animas
are treated with the vehicle alone. The guinea pigs
are placed in a leather cuff with a hole of 1.52.5
cm size punched in it, allowing the UV radiation to
reach only this area. Then animals are exposed to
UV radiation. After 2 min of expose the remaining
half of the test compound is administered. The
erythema is scored 2 and 4 hr after exposure.
Evaluation: The degree of erythema is evaluated
visually by 2 different investigators in a double-
blinded manner. The followings scores are given:
0 = no erythema,
1 = weak erythema,
2 = strong erythema,
4 = very strong erythema.
Animals with a score of 0 or 1 are considered to be
protected. The scoring after 2 and after 4 h gives
some indication of the duration of the effect. ED50
values can be calculated.
[3][2]
2. Vascular permeability: During inflammation,
vascular permeability increases to allow plasma
constituents such as antibodies and complement to
access injured or infected tissues. The test is used
to evaluate the inhibitory activity of drugs against
increased vascular permeability which is induced
by phlogistic substances. Mediators of
inflammation, such as histamine, prostaglandins
and leucotrienes are released following stimulation
e.g. of mast cells. This leads to a dilation of
arterioles and venules and to an increased vascular
permeability. As a consequence, fluid and plasma
proteins are extravasated and edemas are formed.
The increase of permeability can be recognized by
the infiltration of the injected sites of the skin with
the vital dye Evans blue.
Procedure: Albino Wistar are used each group
containing 4 rats. Control group will receive
distilled water 1%w/v 1ml/100g by oral route and
other group will receive test compound by oral
route and standard group will receive diclofenac
10ml/kg by intraperitoneal route. After 1h of these
administration rats are injected with 0.25ml of
0.6% v/v solution of acetic acid intraperitoneally.
Immediately, 10 ml/kg of 10%w/v Evans blue is
injected intravenously via tail vain. After 30 min ,
the animals are anesthetized with ether anaesthesia
and sacrificed. The abdomen is cut open and
exposed viscera. The animals are held by a flap of
abdominal wall over a Petri dish. The peritoneal
fluid (exudates) collected, filtered and made up the
volume to 10 ml using normal saline solution and
centrifuged at 3000 rpm for 15 min. The
absorbance (A) of the supernatant is measured at
590 nm using spectrophotometer.
Evaluation: Decreased concentration of dye with
respected to absorbance indicates reduction in
permeability. The result of test is compared with
that of standard. ED
50
values can also be
calculated.
[4][2]
3. Oxazolone-induced ear edema in mice: The
oxazolone-induced ear edema model in mice is a
model of delayed contact hypersensitivity that
permits the quantitative evaluation of the topical
and systemic anti-inflammatory activity of a
compound following topical administration. The
oxazolone-repeated challenge increased the level of
Th2 cytokines and decreased that of a Th1 cytokine
in the lesioned skin. The Th2 cytokines, especially
IL-4, play major roles in the development of
dermatitis in the present mouse model.
Procedure: Using 12mice in each group, the same
skin site of the right ear was sensitized by a single
application of 10 l (each 5 l for inner and outer
of ear) of 0.5% oxazolone in acetone 7 days before
the first challenge (day 0), and 10 l of 0.5%
oxazolone in acetone was repeatedly applied to the
sensitized right ear 3 times per week. In the non-
sensitized animals, acetone alone was applied to
the right ear. The mice are challenged 8 days later
again under anesthesia by applying 0.01 ml 2%
oxazolone solution to the inside of the right ear
(control) or 0.01 ml of oxazolone solution, in
which the test compound or the standard is solved.
Groups of 10 to 15 animals are treated with the
irritant alone or with the solution of the test
compound. The left ear remains untreated. The
maximum of inflammation occurs 24 h later. At
Available online at www.ijpras.com
3
this time the animals are sacrificed under
anesthesia and a disc of 8 mm diameter is punched
from both sides. The discs are immediately
weighed on a balance. The weight difference is an
indicator of the inflammatory edema.
Evaluation: Average values of the increase of
weight are calculated for each treated group and
compared statistically with the control group.
[5][2]
4. Croton-oil ear edema in rats and mice: Croton
oil contains 12-o-tetracanoilphorbol-13-acetate
(TPA) and other phorbol esters as main irritant
agents. TPA is able to activate protein kinase C
(PKC), which activates other enzymatic cascades in
turn, such as mitogen activated protein kinases
(MAPK), and phospholipase A2 (PLA2), leading to
release of platelet activation factor (PAF) and AA.
This cascade of events stimulates vascular
permeability, vasodilation, polymorphonuclear
leukocytes migration, release of histamine and
serotonin and moderate synthesis of inflammatory
eicosanoids by cyclooxygenase (COX) and 5-
lipoxygenase (5-LOX) enzymes. COX and 5-LOX
inhibitors, leukotriene B4 (LTB4) antagonists and
corticosteroids show topical anti-inflammatory
action in animal models of Croton oil or TPA-
induced skin inflammation.
Procedure: A total of 15l of an acetonic solution
containing 75g of croton oil is applied to the inner
surface of right ear of each mouse. Left ear remains
untreated. Control animals receives only the irritant
while indomethacin (100g/ear) serves as
reference. Varying dose levels of test drug are
applied to the inner surface of right ear of each
mouse by dissolving them in inflammation
inducing solution. Animals are sacrificed by
cervical dislocation 6 hr later and a plug (6 mm in
diameter)is removed from both the treated and
untreated ear. The difference in weight between the
two plugs is taken as measure of edematous
response. Since tetradecanoyl porbol acetate (TPA)
is the chief ingredient of croton oil, purified TPA
has also been used to induce ear edema in mice.
Evaluation: The antiphlogistic effect can be
determined by expressing the increase in weight of
the treated ear as percentage of the weight of the
contralateral control ear. The difference
between both ears or excised discs is calculated as
the average values for treated and control groups
and the effect is evaluated by statistical
methods.
[6][7][2]
5. Paw edema in rats: The ability of anti-
inflammatory drugs to inhibit the edema produced
in the hind paw of the rat after injection of a
phlogistic agent. Many phlogistic agents (irritants)
have been used, such as brewers yeast,
formaldehyde, dextran, egg albumin, kaolin,
Aerosil, sulfated polysaccharides like carrageenan
or naphthoylheparamine. The volume of the
injected paw is measured before and after
application of the irritant and the paw volume of
the treated animals is compared to the controls.[
Plethysmograph]. Carrageenan-induced rat paw
edema is associated with three distinct phases. The
first phase is early mediated by mast cell
degranulation and histamine and serotonin release
(1 h), the second phase (60 to 150 min) is
characterized by bradykinin release and pain, and
further eicosanoid production in the late phase (3-4
h). So here the anti-inflammatory effect of the test
compound is due to inhibition of which mediator
can also be known.
Procedure: Male or female Sprague-Dawley rats
with a body weight between 100 and 150 g are
used. The animals are starved overnight. To insure
uniform hydration, the rats receive 5 ml of water by
stomach tube (controls) or the test drug dissolved
or suspended in the same
volume. Thirty minutes later, the rats are
challenged by a subcutaneous injection of 0.05 ml
of 1% solution of carrageenan into the plantar side
of the left hindpaw. The paw is marked with ink at
the level of the lateral malleolus and immersed in
mercury up to this mark. The paw volume is
measured plethysmographically immediately after
injection, again 3 and 6 h, and eventually 24 h after
challenge. Various devices have been developed
for plethysmography of the paw, like mercury for
immersion of the paw, more sophisticated
apparatusbased on the principle of transforming the
volume being increased by immersion of the paw
into a proportional voltage using a pressure
transducer, sensitive method of measuring mouse
paw volume by interfacing a Mettler Delta Range
top-loading balance with a microcomputer,
commercially available plethysmometer.
Evaluation: The increase of paw volume after 3 or
6 h is calculated as percentage compared with the
volume measured immediately after injection of the
irritant for each animal. Effectively treated animals
show much less edema. The difference of average
values between treated animals and control groups
is calculated for each time interval and statistically
evaluated. The difference at the various time
intervals gives some hints for the duration of the
anti-inflammatory effect. A dose- response curve is
run for active drugs and ED50 values can be
determined.
[8][7][2]
6. Pleurisy tests: In experimental animals pleurisy
can be induced by several irritants, such as
histamine, bradykinin, prostaglandins, mast cell
degranulators, dextran, enzymes, antigens,
microbes, and nonspecific irritants, like turpentine
and carrageenan. Carrageenan-induced pleurisy in
rats is considered to be an excellent acute
inflammatory model in which fluid extravasation,
leukocyte migration and the various biochemical
parameters involved in the inflammatory response
can be measured easily in the exudate.
Procedure: The mouse pleurisy was induced by a
single intrapleural injection of 0.1 ml of
Available online at www.ijpras.com
4
carrageenan (1%). After 4 h the animals were killed
with an overdose of ether, the thorax was opened
and the pleural cavity was washed with 1.0 ml of
sterile PBS, containing heparin (20 IU per ml).
Samples of the pleural lavage were collected for
determination ofexudation, myeloperoxidase ,
adenosine-deaminase activities, and nitric oxide
levels, as well as for determination of total and
differential leukocyte counts . Total leukocyte
counts were performed in a Neubauer chamber.
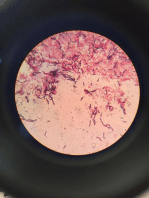
The cytospin preparations of pleural wash were
stained with MayGrunwald Giemsa for the
differential count which was performed under an
oil immersion objective. The serum level of the C-
reactive protein was also analysed. In another set of
experiment animals were treated 30 min before
carrageenan with a solution of Evans blue dye (25
mg/kg, i.v.) in order to evaluate the degree of
exudation in the pleural space. A sample (500 l)
of the fluid leakage collected from the pleural
cavity was stored in a freezer (20 C) to further
determine the concentration of Evans blue dye. To
this end, on the day of the experiments, a batch of
samples was thawed at room temperature. and the
amount of dye was estimated by colorimetry using
an Elisa plate reader at 600 nm, by interpolation
from a standard curve of Evans blue dye in the
range of 0.01 to 50 g/ml.
Evaluation: One ml (the added Hanks solution) is
subtracted from the measured volume. The values
of each experimental group are averaged and
compared with the control group. ED50 values can
be calculated using various doses.
[9][2]
7. Granuloma pouch technique: With the
introduction of an irritant substance into an s.c. air
pocket, granulation tissue begins to proliferate and
soon covers the whole inside of the pouch. This
tissue consists of fibroblasts, endothelial cells and
an infiltrate of macrophages and
polymorphonuclear leukocytes. In the GPA this
rapidly growing tissue can be exposed to
carcinogenic and mutagenic sub-stances. One of
the major advantages of the system is the
possibility of bringing the test compounds into
direct contact with the target cells, by injecting
them into the air pocket. It is also possible to
administer the material by the oral and parenteral
routes. It does not provide quantitative information
on cytotoxicity of the test compounds in vivo.
Procedure: Male or female Sprague-Dawley rats
with a body weight between 150 and 200 g are
used. Ten animals are taken for controls and for
test groups. The back of the animals is shaved and
disinfected. With a very thin needle a
pneumoderma is made in the middle of the dorsal
skin by injection of 20 ml of air under ether
anesthesia. Into the resulting oval airpouch 0.5 ml
of a 1% solution of Croton oil in sesame oil is
injected avoiding any leakage of air. Forty-eight
hours later the air is withdrawn from the pouch and
72 h later any resulting adhesions are broken.
Instead of croton oil 1 ml of a 20% suspension of
carrageenan in sesame oil can be used as irritant.
Starting with the formation of the pouch, the
animals are treated every day either orally or
subcutaneously with the test compound or the
standard. For testing local activity, the test
compound is injected directly into the air sac at the
same time as the irritant. On the 4th or the 5th day
the animals are sacrificed under anesthesia. The
pouch is opened and the exudate is collected in
glass cylinders. The pouches are washed with 1 ml
of saline, exudates are immediately cooled on ice
and the volume is recorded. Total no. of leukocytes
migrated into the pouch are evaluated after staining
with Erythrosine B and remaining exudates is
centrifuged at 3000 rpm for 10 min at 4 degrees
and supernatant stored at -20 degrees until use.
Evaluation: The average value of the exudate of
the controls and the test groups is calculated.
Comparison is made by statistical means.
[10][11][2]
Methods to evaluate proliferative phase of
inflammation:
1. Cotton wool granuloma: The foreign body
granulomas were provoked in rats by subcutaneous
implantation of pellets of compressed cotton. After
several days, histologically giant cells and
undifferentiated connective tissue can be observed
besides the fluid infiltration. The amount of newly
formed connective tissue can be measured by
weighing the dried pellets after removal. More
intensive granuloma formation has been observed
if the cotton pellets have been impregnated with
carrageenin.
Procedure: Male rats weighing 180200 g were
used. Test drugs were administered orally on a
once daily dosage regimen for 7 days, and the
control group received vehicle. Two sterilized
pellets of cotton wool were implanted
subcutaneously, one on each side of abdomen of
the animal, under the light ether anesthesia and
sterile technique. The rats were sacrificed on the
eighth day. The implanted pellets were dissected
out and recorded for wet weight. Thymuses were
also dissected out. Both pellet and thymus were
dried at60 C for 18 h and the dry weight was
recorded.
Evaluation: The weight of the transudate and the
granuloma as well as the percent granuloma
inhibition of the test drugs were calculated. The
body weight gain was also recorded.
[12][13][2][7]
2. Glass rod granuloma: These reflects the
chronic proliferative inflammation. Of the newly
formed connective tissue not only wet and dry
weight, but also chemical composition
andvmechanical properties can be measured.
Procedure: Glass rods with a diameter of 6 mm are
cut to a length of 40 mm and the ends rounded off
by flame melting. Male Sprague-Dawley rats with
an initial weight of 130 g are anaesthetized with
Available online at www.ijpras.com
5
ether, the back skin shaved and disinfected. From
an incision in the caudal region a subcutaneous
tunnel is formed in cranial direction with a closed
blunted forceps. One glass rod isintroduced into
this tunnel finally lying on the back of the animal.
The incision wound is closed by sutures. The
animals are kept in separate cages. The rods remain
in situ for 20 or 40 days. Treatment with drugs is
either during the whole period or only during the
last 10 or 2 days. At the end the animals are
sacrificed under CO
2
anesthesia. The glass rods are
prepared together with the surrounding connective
tissue which forms a tube around the glass rod. By
incision at one end the glass rod is extracted and
the granuloma sac inverted forming a plain piece of
pure connective tissue. Wet weight of the
granuloma tissue is recorded. Finally, the
granuloma tissue is dried and the dry weight is
recorded. In addition, biochemical analyses, such
as determination of collagen and
glycosaminoglycans can be performed.
Evaluation:Several parameters can be determined
by this method. Granuloma weight was reduced by
test compound is compared with that of standard.
[2]
Cite this article
Bibliography:
1. Harsh M. Text book of Pathophysiology. 5
th
ed.
New Delhi: Jaypee publication. 2005. p. 126-
34.
2. Gerhard vogel H, Wolfganga HV, Bernward
AS, Jurgen S, Gunter M, Wolfganga FV. Drug
discovery and evaluation pharmacological
assays.2
nd
ed , Berlin, Germany : Spinger
;2002. p. 725-71.
3. Snyder. DS. Effect of topical indomethacin on
uvr-induced redness and prostaglandin e levels
in sunburned guinea pig skin. Prostaglandins.
1976;11(4):631-43.
4. Yashraj.Y, Mohanty.P.K, Kasture.S.B. Anti-
inflammatory activity of hydroalcoholic
extract of Quisqualis indica Linn. flower in
rats. International Journal of Pharmacy & Life
sciences. 2011;2(8):977-81.
5. Tadafumi.T, Toru.A, Kenji.O, Haruhiko.M.
The effects of olopatadine hydrochloride on
the number of scratching induced by repeated
application of oxazolone in mice. Eur J
Pharmacol. 2005;524:149-54.
6. Rogerio.A.S, Mariana.K.A.Araruna,
Romagna.C.Oliveira, Kleber.D.P.Menezes,
Gerlania.O.Leite, Marta.R.Kerntopf, et al.
Topical anti-inflammatory effect of Caryocar
coriaceum Wittm. (Caryocaraceae) fruit pulp
fixed oil on mice ear edema induced by
different irritant agents. J Ethnopharmacol.
2011;136:504- 10.
7. Gupta.SK. Drug screening methods. 2 ed. New
Delhi: Jaypee; 2009.
8. Penna.S.C, Medeiros.M.V, Aimbire.F.S.C,
Faria-Neto.H.C.C, Sertie.J.A.A, Lopes-
Martins.R.A.B. Anti-inflammatory effect of
the hydralcoholic extract of Zingiber officinale
rhizomes on rat paw and skin edema.
Phytomedicine. 2003;10:3815.
9. Vargas.A.J, Geremias.D.S, Provensi.G,
Fornari.P.E, Reginatto.F.H, Gosmann.G, et al.
Passiflora alata and Passiflora edulis spray-
dried aqueous extracts inhibit inflammation in
mouse model of pleurisy. Fitoterapia.
2007;78:112-9.
10. Maier.P, Manser.P, Zbinden.G. Granuloma
pouch assay i. induction of ouabain resistance
in vivo. Mutation Research. 1978;54:159--65.
11. Martin.S.W, Stevens.A.J, Brennan.B.S,
Davies.D, Rowland.M, Houston.J.B. The six-
day-old rat air pouch model of Inflammation:
Characterization of the inflammatory response
to carrageenan. JPM. 1994;32(3):139-47.
12. Intahphuak.S, Panthong.A, Kanjanapothi.D,
Taesotikul.T, Krachangchaeng.C, Reutrakul.V.
Anti-inflammatory and analgesic activities of
Mallotus spodocarpus Airy Shaw. J
Ethnopharmacol. 2004;90:69-72.
13. Smita.S, Shwetha.K, Prabhu.K, Maradi.R,
Bairy.KL, Shanbhag.T. Evaluation of
antiinflammatory activity of Tephrosia
purpurea in rats. Asian Pac J Trop Med.
2010:193-5.
Mitul Patel, Murugananthan, Shivalinge Gowda
K,P In Vivo Animal Models in Preclinical
Evaluation of Anti-Inflammatory Activity-A
Review Int. J. of Pharm. Res. & All. Sci 2012;
Volume 1, Issue 2, 01-05
You might also like
- Ebook Campbell Essential Biology 5Th Edition Simon Test Bank Full Chapter PDFDocument36 pagesEbook Campbell Essential Biology 5Th Edition Simon Test Bank Full Chapter PDFtristandoyledtnpkozbgj100% (17)
- Notes About BiologyDocument81 pagesNotes About BiologyRichard Coffey100% (1)
- Histology of The EAR Histology of The EARDocument21 pagesHistology of The EAR Histology of The EARhendri67% (3)
- CSEC Biology - EcologyDocument74 pagesCSEC Biology - EcologyRic Flamboyant FraserNo ratings yet
- Anatomia VenelorDocument4 pagesAnatomia Venelorflorentyna78No ratings yet
- In - Vivo - Animal - Models - in - Preclinical - Evaluation - of - Anti-Inflammatory - Activity-A Review PDFDocument5 pagesIn - Vivo - Animal - Models - in - Preclinical - Evaluation - of - Anti-Inflammatory - Activity-A Review PDFnoorivanamandaNo ratings yet
- Various Animal Models For Preclinical Testing of Anti-Inflammatory AgentsDocument8 pagesVarious Animal Models For Preclinical Testing of Anti-Inflammatory AgentsDrShailesh Madhukar KewatkarNo ratings yet
- Inflamationppt 180928164511Document37 pagesInflamationppt 180928164511misdduaaNo ratings yet
- ANTI INFLAMMATORY Screening MethodsDocument7 pagesANTI INFLAMMATORY Screening MethodsBrajesh Thankamony67% (3)
- Anti InflammatoryDocument20 pagesAnti InflammatoryKrupasagar Pn PalegarNo ratings yet
- Experimental Pharmacology Unit 2 (Part 3)Document23 pagesExperimental Pharmacology Unit 2 (Part 3)Tannu SharmaNo ratings yet
- Study of Anti-Inflammatory Activity of Drugs Using Carrageenan Induced Paw Edema ModelDocument10 pagesStudy of Anti-Inflammatory Activity of Drugs Using Carrageenan Induced Paw Edema ModelLithin LekkalaNo ratings yet
- AllergyDocument35 pagesAllergyAhmed ImranNo ratings yet
- Allergy: Pharm .D, M. Phil Lecturer (Pharmacognosy)Document35 pagesAllergy: Pharm .D, M. Phil Lecturer (Pharmacognosy)Ahmed Imran0% (1)
- BP 507 Pexp 14&15 FormatDocument10 pagesBP 507 Pexp 14&15 FormatLithin LekkalaNo ratings yet
- Interantiinflamasi PDFDocument4 pagesInterantiinflamasi PDFJumardinNo ratings yet
- Vijayalaxmi ADocument7 pagesVijayalaxmi AShaikh AyyubNo ratings yet
- VENENODETARANTULADocument38 pagesVENENODETARANTULARicardo Pacheco RiosNo ratings yet
- S.A. Raja Pharmacy College: Pharmacology - IiiDocument25 pagesS.A. Raja Pharmacy College: Pharmacology - IiialiangomalianNo ratings yet
- Allergy Skin TestsDocument6 pagesAllergy Skin TestsAnindya Putri KusumajatiNo ratings yet
- Pcol Lab FinalsDocument8 pagesPcol Lab Finalslingadanne1103No ratings yet
- Practical Lab Manual: Pharmacology - Iii B. PharmDocument16 pagesPractical Lab Manual: Pharmacology - Iii B. PharmPrincipal, Spectrum Hi Pharmacy College, SultanpurNo ratings yet
- Anti Allergics 1Document30 pagesAnti Allergics 1beulahNo ratings yet
- B - 06 - English JournalDocument3 pagesB - 06 - English JournalTazkia AuditaNo ratings yet
- Jurnal 2Document3 pagesJurnal 2MargaretaNo ratings yet
- Pharmacology IIIDocument23 pagesPharmacology IIIAkshay ShindeNo ratings yet
- 90-Article Text With Names and Affiliation-154-1!10!20190919Document4 pages90-Article Text With Names and Affiliation-154-1!10!20190919Agharid Ali HusseinNo ratings yet
- Pain PDFDocument4 pagesPain PDFSetyo RahmanNo ratings yet
- Skin Irritation & Skin SesnsitizationDocument47 pagesSkin Irritation & Skin SesnsitizationRaunakkumar ChaurasiyaNo ratings yet
- Anti-Inflammatory Assay: Dr. Khajista JabeenDocument10 pagesAnti-Inflammatory Assay: Dr. Khajista JabeenRabiya RamzanNo ratings yet
- Tutorial 3.1 Ke-1 (Biduran)Document2 pagesTutorial 3.1 Ke-1 (Biduran)DaivaNo ratings yet
- Pengaruh Ekstrak Daun Codorata Terhadap 734bd139Document7 pagesPengaruh Ekstrak Daun Codorata Terhadap 734bd139lalu reza rezki muanggaraNo ratings yet
- Induksi AlergiDocument5 pagesInduksi AlergiBilly Shan LastKagerooboroNo ratings yet
- Membrane Stabilization As A Mechanism of TheDocument7 pagesMembrane Stabilization As A Mechanism of TheAlexandru SavaNo ratings yet
- 1688 3737 1 PB PDFDocument4 pages1688 3737 1 PB PDFputri firda erlinaNo ratings yet
- Patch Testing of Experimentally Sensitized Beagle Dogs - Development of A Model For Skin Lesions of Atopic Dermatitis (Pages 95-102)Document8 pagesPatch Testing of Experimentally Sensitized Beagle Dogs - Development of A Model For Skin Lesions of Atopic Dermatitis (Pages 95-102)jenNo ratings yet
- Aggarwal 2011Document8 pagesAggarwal 2011rani nareza ulfaNo ratings yet
- Evaluation of Wound Healing Effect of Jasminum Grandiflorum in Albino Rats by Histopathological StudiesDocument4 pagesEvaluation of Wound Healing Effect of Jasminum Grandiflorum in Albino Rats by Histopathological StudiesAgung Tri LaksonoNo ratings yet
- Averrhoa Carambola: Original ArticleDocument8 pagesAverrhoa Carambola: Original ArticleelvinaNo ratings yet
- Evaluation of Wound Healing Activity of Leaves of Crinum AsiaticumDocument5 pagesEvaluation of Wound Healing Activity of Leaves of Crinum AsiaticumxiuhtlaltzinNo ratings yet
- Giansanti Rabbit and Cell Culture 2010Document8 pagesGiansanti Rabbit and Cell Culture 2010Igor VainerNo ratings yet
- Full Thickness Wound Healing in Induced Diabetic Mice Using Low Level Laser in Comparison With UltrasoundDocument9 pagesFull Thickness Wound Healing in Induced Diabetic Mice Using Low Level Laser in Comparison With UltrasoundAnonymous UXBSV13cNo ratings yet
- Allergic Rhinitis and It's TreatmentDocument4 pagesAllergic Rhinitis and It's TreatmentCentral Asian StudiesNo ratings yet
- Delayed: and Hypersensitivity TheDocument12 pagesDelayed: and Hypersensitivity TheMina BekNo ratings yet
- 106 GuptaDocument5 pages106 GuptaDyah Putri Ayu DinastyarNo ratings yet
- WINTER - Carragenin - Induced Edema in PawDocument5 pagesWINTER - Carragenin - Induced Edema in PawCecy ToaquizaNo ratings yet
- 3rd ReportDocument3 pages3rd ReportYazeed AsrawiNo ratings yet
- Elixir Food Science PublishedDocument5 pagesElixir Food Science PublishedRajaram KrishnasamyNo ratings yet
- Inprocess Quality Control Tests For Biological ProductsDocument34 pagesInprocess Quality Control Tests For Biological ProductsnishathfathimaNo ratings yet
- Draft Jurnal Ppikid Dina Cek LEF 230417Document8 pagesDraft Jurnal Ppikid Dina Cek LEF 230417Regina SinagaNo ratings yet
- Antinociceptive and Anti-Inflammatory Activity of Alkaloid Fraction of Trichopus Zeylanicus Gaertn PDFDocument4 pagesAntinociceptive and Anti-Inflammatory Activity of Alkaloid Fraction of Trichopus Zeylanicus Gaertn PDFbravohr98No ratings yet
- Chronic Toxicity of Chenopodium Ambrosioides in Rats: Biomedical Research 2005 16 (2) : 111-113Document3 pagesChronic Toxicity of Chenopodium Ambrosioides in Rats: Biomedical Research 2005 16 (2) : 111-113Entang The'FirsterNo ratings yet
- Research ArticleDocument6 pagesResearch Articletri sutrianiNo ratings yet
- Chronic Generalized Dermatophilosis in A BuffaloDocument3 pagesChronic Generalized Dermatophilosis in A BuffaloHendroNo ratings yet
- Session 7Document15 pagesSession 7madcalNo ratings yet
- Moringa Anti Asthma Activity PDFDocument8 pagesMoringa Anti Asthma Activity PDFCisco SilvaNo ratings yet
- Calendula 8Document7 pagesCalendula 8Zeila OmarNo ratings yet
- International Journal of Pharmaceutical Research Analysis: Screening of Wound Healing Activity of Bark ofDocument5 pagesInternational Journal of Pharmaceutical Research Analysis: Screening of Wound Healing Activity of Bark ofElisaDwiRestianaNo ratings yet
- Anti InflamasiDocument27 pagesAnti InflamasiAuLia DamayantiNo ratings yet
- The Effects of Epidermal Growth Factor On Early Burn-Wound Progression in RatsDocument7 pagesThe Effects of Epidermal Growth Factor On Early Burn-Wound Progression in RatsNatalindah Jokiem Woecandra T. D.No ratings yet
- Allium Cepa Wound Healing PDFDocument9 pagesAllium Cepa Wound Healing PDFUiSNo ratings yet
- Q Mix™ - in Vivo Study PDFDocument7 pagesQ Mix™ - in Vivo Study PDFAdriana Sorina SegărceanuNo ratings yet
- Nursing Care of Clients With Allergic DisordersDocument12 pagesNursing Care of Clients With Allergic Disordersbwee bweeNo ratings yet
- Errores de FlebotomiaDocument5 pagesErrores de FlebotomiaSandra Amayrane Alcántara Balderas100% (1)
- Appositive Relative Clauses in EnglishDocument248 pagesAppositive Relative Clauses in EnglishAnonymous wJFC79YlUlNo ratings yet
- RENUMF90Document10 pagesRENUMF90hehirukanake0% (1)
- Cnidarians OverviewDocument46 pagesCnidarians OverviewTiff VoNo ratings yet
- Cardio Tonic DrugDocument25 pagesCardio Tonic DrugNistha MudgilNo ratings yet
- Chapter 3 - Herbarium Methods and ExchangesDocument28 pagesChapter 3 - Herbarium Methods and ExchangesHenrique ScreminNo ratings yet
- Chapter 4: Chemical Composition in A CellDocument14 pagesChapter 4: Chemical Composition in A CellEma Fatimah100% (1)
- Bhadauria V (Ed.) - Next-Generation Sequencing and Bioinformatics For Plant Science-Caister (2017)Document204 pagesBhadauria V (Ed.) - Next-Generation Sequencing and Bioinformatics For Plant Science-Caister (2017)张振No ratings yet
- Science 10 Self Learning Module 8Document7 pagesScience 10 Self Learning Module 8Princess Jane DimpasNo ratings yet
- MicrobiologyDocument40 pagesMicrobiologyRasty Baku100% (1)
- Research BioplasticDocument27 pagesResearch BioplasticDezalene CierteNo ratings yet
- HPV Genotypes 14 Real-TM Quant: HandbookDocument19 pagesHPV Genotypes 14 Real-TM Quant: HandbookHarun GanićNo ratings yet
- Storm StressDocument35 pagesStorm Stressmoo2elynNo ratings yet
- Genetic Algebras: Proceedings of The Royal Society of Edinburgh 59 (1939) 242-258Document22 pagesGenetic Algebras: Proceedings of The Royal Society of Edinburgh 59 (1939) 242-258shiksha torooNo ratings yet
- Practice Recitation Delete LaterDocument3 pagesPractice Recitation Delete LaterCyrus YahyaviNo ratings yet
- The Fat Compartments of The Face: Anatomy and Clinical Implications For Cosmetic SurgeryDocument9 pagesThe Fat Compartments of The Face: Anatomy and Clinical Implications For Cosmetic SurgeryBruno BallestraNo ratings yet
- Full Chapter Respiratory Delivery of Biologics Nucleic Acids and Vaccines 2Nd Edition Harry Perlstadt PDFDocument53 pagesFull Chapter Respiratory Delivery of Biologics Nucleic Acids and Vaccines 2Nd Edition Harry Perlstadt PDFkelly.bressette297100% (5)
- Long Test 3 Ready To PrintDocument3 pagesLong Test 3 Ready To Printjayrald cruzadaNo ratings yet
- Tesis CrossfitDocument155 pagesTesis CrossfitMiguel Lampre EzquerraNo ratings yet
- Bhopal As Global Environment CityDocument20 pagesBhopal As Global Environment CityarchimosheNo ratings yet
- Human Genetics Unit Test Study Guide - 09-10Document5 pagesHuman Genetics Unit Test Study Guide - 09-10Tina HowitsonNo ratings yet
- DYS091 EletrophoresisCelluloseAcetateDocument4 pagesDYS091 EletrophoresisCelluloseAcetateeviprimaNo ratings yet
- Arun Sudhagar S (Resume)Document4 pagesArun Sudhagar S (Resume)Arun SudhagarNo ratings yet
- Overview of Standards Test Conditions Pass Criteria EnglishDocument15 pagesOverview of Standards Test Conditions Pass Criteria EnglishDavide GrioniNo ratings yet
- Gender Is The Range of Characteristics Pertaining To, and DifferentiatingDocument38 pagesGender Is The Range of Characteristics Pertaining To, and DifferentiatingNaeem JanNo ratings yet