Professional Documents
Culture Documents
Successful Treatment of Schizophrenia Requires Optimal Daily Doses of Vitamin b3
Successful Treatment of Schizophrenia Requires Optimal Daily Doses of Vitamin b3
Uploaded by
Joop WezenbeekOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Successful Treatment of Schizophrenia Requires Optimal Daily Doses of Vitamin b3
Successful Treatment of Schizophrenia Requires Optimal Daily Doses of Vitamin b3
Uploaded by
Joop WezenbeekCopyright:
Available Formats
Alternative Medicine Review Volume 13, Number 4 2008
Guest
Editorial
Page 287
Successful Treatment of Schizophrenia Requires Optimal Daily
Doses of Vitamin B
3
For over 50 years Dr. Abram Hoer has been educating clinicians about the need to
correctly (optimally) dose schizophrenics with vitamin B
3
(niacin; niacinamide). For the
past 10 years I have, likewise, educated numerous naturopathic and medical doctors about
the very same thing. For some reason, both types of clinicians routinely treat schizophrenic
patients with plenty of vitamins, minerals, and other natural health products, but they
never provide enough vitamin B
3
. In these authors opinions, schizophrenic patients cannot
get well if not provided with optimal doses of vitamin B
3
. Tis prevents the real acceptance
of nutritional treatment since clinicians will not observe favorable results when inadequate
treatment is provided; their schizophrenic patients will continue to suer needlessly.
To understand the importance of vitamin B
3
treatment, some background information
is needed. Schizophrenia is characterized by a combination of perceptual changes (e.g.,
hallucinations) and thought disorders (e.g., delusions).
1
Tese aberrant mental states, which
can lead to psychotic behavior, cause a tremendous amount of emotional and psychological
suering. Te cause of schizophrenia, the subject of much debate, is considered a
biochemical imbalance, although certain genetic factors most certainly play a role.
Te majority of scientists and psychiatrists subscribe to the dopamine excess theory of
schizophrenia; i.e., that too much dopamine is largely responsible for the symptoms of
psychosis. However, since 1952, Hoer, the founding father of orthomolecular medicine,
has researched, published, and expanded on the adrenochrome theory of schizophrenia.
1,2
He and his colleagues, Drs. Osmond and Smythies, arrived at this theory by studying and
researching the eects of substances such as mescaline, lysergic acid diethylamide (LSD),
and amphetamines all of which can cause a clinical syndrome in normal individuals that
would be clinically indistinguishable from schizophrenia.
Osmond and Smythies noted that mescaline had a similar chemical structure to that of
adrenaline. Hoer, Osmond, and Smythies concluded that since both can be converted
to indoles in the body, the potential schizophrenic toxin might be an indole derivative
of adrenaline with similar neurochemical properties to that of mescaline or LSD. Tey
eventually deduced that the schizophrenic toxin was an oxidized derivative of adrenaline
known as adrenochrome. Since the early 1950s, the adrenochrome theory has been
validated by the following ndings:
Copyright 2008 Thorne Research, Inc. All Rights Reserved. No Reprint Without Written Permission.
Alternative Medicine Review Volume 13, Number 4 2008
Page 288
Guest Editorial
1. Adrenochrome and its close relatives dopaminochrome (from dopamine) and
noradrenochrome (from noradrenaline) are present in the human brain.
3-5
2. Tese compounds probably induce a combination of neurotoxic and mind-
mood-altering eects.
3-5
3. Reducing adrenochrome, dopaminochrome, and noradrenochrome is
therapeutic for the treatment of schizophrenia.
6
To reduce the production of adrenochrome, Hoer and his team decided on the methyl
acceptor vitamin B
3
. Tis vitamin, previously used to treat pellagra (a disease clinically
indistinguishable from schizophrenia) had relevant biochemical properties.
1,2
Hoer and
his team researched the metabolism of adrenaline. Tey knew that the reaction involving
noradrenaline to adrenaline required the addition of one methyl group. Because vitamin
B
3
was known to function as a methyl acceptor, Hoers team theorized that an optimum
dose of niacin might decrease the amount of noradrenaline that would be converted to
adrenaline. Since adrenochrome was thought to be an oxidized derivative of adrenaline,
vitamin B
3
could help reduce the quantity of adrenochrome by simply limiting the
production of adrenaline.
Hoer and his team also discovered an additional biochemical property of vitamin B
3
that
would help to explain its therapeutic ecacy. Vitamin B
3
is a precursor to nicotinamide
adenine dinucleotide, which is present in both oxidized (NAD) and reduced (NADH)
forms in the body. In the brain, adrenaline loses one electron to become oxidized adrenaline.
If enough NAD and NADH are available then the oxidized adrenaline is reconverted to
adrenaline. Tese back and forth processes continue to occur in the presence of sucient
vitamin B
3
coenzymes. However, in the absence of sucient NAD and NADH, the
oxidized adrenaline loses an additional electron and becomes adrenochrome. Tis last
reaction is irreversible, and presumably occurs in much greater concentrations in the
schizophrenic brain.
Tat being said, where is the proof? Can vitamin B
3
help in the treatment of acute
and chronic schizophrenia? Te rst report on the therapeutic use of vitamin B
3
for
schizophrenia was presented in 1952 at the Saskatchewan Committee on Schizophrenia.
At this meeting, eight cases were presented, each demonstrating favorable eects from
giving 1-10 g vitamin B
3
, and, in the majority of cases, equal amounts of vitamin C.
1
After
a more involved pilot study demonstrated excellent therapeutic responses to vitamin B
3
,
1
the rst North American double-blind, placebo-controlled experiment was undertaken
to assess whether or not this vitamin was eective for schizophrenia. Te study, which
began in 1952 but was not published until 1957, involved 30 acute schizophrenic patients
who were each randomized to placebo, niacinamide, or niacin.
1,2
Tey were given 1 g three
times daily for 30 days, and then followed for one year. After one year, the patients given
vitamin B
3
with the standard treatments at that time had more than double the recovery
rate (80%) compared to patients in the placebo group (33%).
7
Copyright 2008 Thorne Research, Inc. All Rights Reserved. No Reprint Without Written Permission.
Alternative Medicine Review Volume 13, Number 4 2008
Guest Editorial
Page 289
In their second double-blind, placebo-controlled experiment, Hoer and his team used
only niacin and placebo.
1,8
Te study lasted 33 days and involved 82 patients (43 in the
placebo group and 39 in the niacin group). Vitamin B
3
once again contributed signicantly
to the recovery of acute schizophrenic patients. In the niacin group, 79.5 percent improved
compared to 41.9 percent in the placebo group. Other parameters evaluated by Hoer
and his team included the number of patients readmitted, the number of readmissions,
the number of well or much improved patients, and the number of patients who were
considered cured. Tis data involved the following groups of patients: (1) those who
only took vitamin B
3
in the hospital and not in the community; (2) patients who did
not take vitamin B
3
in the hospital but did take the vitamin when in the community; (3)
patients who took vitamin B
3
in the hospital and community; and (4) patients who never
took vitamin B
3
. Te results demonstrated that patients in the community who were
taking niacin (groups 2 and 3) had more community years that were free of readmissions
compared to patients not taking vitamin B
3
(groups 1 and 4) 91 percent versus 62
percent of the community years free of readmissions. Te entire niacin group (group 3)
was readmitted 38 times for 67 readmissions (average 64 days per patient); whereas, the
placebo/non-niacin group (group 4) was readmitted 36 times for 81 readmissions (average
147 days per patient). Once all the data was combined, the results revealed that the most
ve-year cures and best treatment responses were among the patients who took vitamin B
3
in the hospital and in the community.
Hoer followed patients from 1953 to 1960, publishing a total of six double-blind,
randomized controlled clinical trials. All trials conrmed the positive eects that vitamin
B
3
had on the recovery of acute schizophrenic patients, and that the use of this vitamin
substantially reduced patients reliance on the health care system.
2
In terms of treating chronic schizophrenic patients, Hoers early studies did not show a
favorable response among chronic schizophrenic patients who were ill longer than one year.
When Hoer reviewed this problem more thoroughly, however, he discovered that the
treatment duration was not long enough to have produced adequate results. Chronic patients
required vitamin B
3
treatment for ve or more years in order to derive observable benets.
1,9
In one study involving 32 chronic patients, no patient responded to vitamin B
3
after two
years of use.
1
Nineteen patients discontinued the vitamin, while the remaining 13 patients
continued with the vitamin treatment. Data was obtained for the years, 1956-1964. Of the
patients not on niacin, the mean number of days spent in hospital was 691 compared to 79
in the niacin group. Te proportion of time spent in the hospital was substantially less for
the chronic patients who remained on the vitamin.
In a more recent analysis of 27 chronic schizophrenic patients who had been under
treatment for at least 10 years, consistent treatment with vitamin B
3
produced the
following results: 11 patients were able to work; two patients were able to marry and look
after their families and homes; two patients were single mothers able to care for their
children; and three patients were able to manage their own businesses.
9
Tese results are
remarkable when one considers the state of these patients prior to receiving optimal doses
Copyright 2008 Thorne Research, Inc. All Rights Reserved. No Reprint Without Written Permission.
Alternative Medicine Review Volume 13, Number 4 2008
Page 290
Guest Editorial
of vitamin B
3
. Te average age of these patients was 40, the majority of them were ill for
seven years before they sought treatment from Hoer, and all had been unresponsive to
previous treatments.
Te starting dose of niacin for adults is 1,000 mg three times daily. In our opinion, the
daily dose should be slowly increased to 4,500-18,000 mg to achieve the best possible
outcome. Patients must be educated about the ushing, heat, itchiness, pruritis, redness,
and tingling that they will transiently experience. Tese benign cutaneous reactions usually
begin 15 minutes after taking niacin for the rst time, and are rst noticed around the
forehead, then descend to the thorax, and sometimes to the feet. Tese reactions typically
abate 1-2 hours following the ingestion of niacin. Niacin causes such cutaneous reactions
by inducing the production of prostaglandin D
2
in the skin, leading to vasodilation and
a marked increase of its metabolite (9, 11-PGF
2
) in the plasma.
10
Niacin is its own
anti-ushing agent because taking it regularly depletes the skin of prostaglandin D
2
and
prevents subsequent cutaneous reactions. At 3,000 mg daily, the ush and other symptoms
will cease to be an issue following the rst 2-3 days of treatment, and will practically
disappear thereafter. If patients are not consistently taking these optimal doses throughout
the day, they will continually re-experience cutaneous reactions and possibly discontinue
treatment.
Te concern over liver toxicity is very minor if immediate-release niacin preparations are
used.
11,12
Timed-release preparations can cause liver toxicity and are not recommended
for schizophrenic patients unless under very close supervision.
13
In Prouskys
clinical experience, niacin is more eective and better tolerated than niacinamide for
schizophrenia. Some patients prefer niacinamide since it does not cause ushing or other
cutaneous reactions. Nausea and dry mouth are much more common with the use of
niacinamide than with niacin. Te daily dosages of niacinamide should not exceed 6,000
mg since the likelihood of nausea accompanied with vomiting is much greater.
14
Te prognosis for the majority of schizophrenic patients is bleak, especially if they only
receive contemporary medical treatments. About 90 percent will remain unwell and
nonfunctional for the rest of their lives despite receiving the most advanced drugs and
social services currently available.
15
Estimates of rst episode schizophrenics are a little
more optimistic and indicate that of ve recently diagnosed patients, one will recover
suciently to live an almost normal life without medication or with very low doses of
medication.
16
Te economic costs of schizophrenia to society are enormous, amounting
to approximately two million dollars for each schizophrenic patient over a 40-year course
of the illness.
17
In a recent publication examining the economic burden of schizophrenia
in Canada, the direct and indirect health care costs associated with this disease were
estimated to be 2.02 billion Canadian dollars in 2004.
18
In addition, when these gures
were added to the high unemployment rate with additional productivity, morbidity,
and mortality losses, the estimate reached 4.83 billion Canadian dollars, for a total cost
estimate of 6.85 billion Canadian dollars in 2004. Te authors of this report arrived
at the following conclusion: Despite signicant improvements in the past decade in
pharmacotherapy, programs, and services available for patients with schizophrenia, the
economic burden of schizophrenia in Canada remains high.
Copyright 2008 Thorne Research, Inc. All Rights Reserved. No Reprint Without Written Permission.
Alternative Medicine Review Volume 13, Number 4 2008
Guest Editorial
Page 291
As clinicians we need to oer restorative care to patients who suer with schizophrenia,
a severe and usually chronic mental illness. Te only reasonable conclusion to be made
from this data is that all schizophrenic patients, including both acute and chronic patients,
need to be treated with vitamin B
3
as quickly as possible and for the duration of their lives.
Vitamin B
3
treatment oers signicant hope of a reasonable quality of life among patients
who would otherwise remain incapacitated and in and out of hospitals for the remainder
of their lives. Some might improve so much that they achieve clinical remission. Since not
enough clinicians utilize optimal doses of vitamin B
3
with their schizophrenic patients,
we hope that the information presented here persuades other clinicians to adopt this very
eective and safe treatment.
Respectfully,
Abram Hoer, MD (retired), PhD
Jonathan Prousky, ND
Abram Hoffer, PhD, MD, FRCP(C), ROHP President, Orthomolecular Vitamins Information Centre; professor psychiatry, 1955-1967;
Director Psychiatric Research, Department Health, Saskatchewan, 1950-1967; President Emeritus, International Schizophrenia
Foundation; Editor, Journal Orthomolecular Medicine; 2007 winner of Dr Rogers Prize; pain in the neck to orthodox psychiatry.
Correspondence address: 2727 Quadra Street, Suite 3A, Victoria BC, V8T 4E5
Jonathan E. Prousky, BPHE, BSc, MSc, ND Chief Naturopathic Medical Ofcer and professor of clinical nutrition, Canadian College of
Naturopathic Medicine.
References
Hoer A. 1. Vitamin B-3 & Schizophrenia. Discovery, Recovery, Controversy. Kingston, ON: Quarry Press, Inc;
1998:28-76.
Hoer A. 2. Adventures in Psychiatry. Te Scientic Memoirs of Dr. Abram Hoer. Caledon, ON: KOS Publishing Inc;
2005:50-99.
Smythies J. Endogenous neurotoxins relevant to schizophrenia. 3. J R Soc Med 1996;89:679-680.
Smythies JR. Oxidative reactions and schizophrenia: a review-discussion. 4. Schizophr Res 1997;24:357-364.
Smythies J. Te adrenochrome hypothesis of schizophrenia revisited. 5. Neurotox Res 2002;4:147-150.
Hoer A. Te adrenochrome hypothesis and psychiatry. 6. J Orthomol Med 1999;14:49-62.
Hoer A, Osmond H, Callbeck MJ, Kahan I. Treatment of schizophrenia with nicotinic acid and nicotinamide. 7. J
Clin Exp Psychopathol 1957;18:131-158.
Hoer A. 8. Niacin Terapy In Psychiatry. Springeld, IL: Charles C. Tomas; 1962;35-71.
Hoer A. Chronic schizophrenic patients treated ten years or more. 9. J Orthomol Med 1994;9:7-37.
Morrow JD, Parsons WG 3rd, Roberts LJ 2nd. Release of markedly increased quantities of prostaglandin D 10.
2
in vivo
in humans following the administration of nicotinic acid. Prostaglandins 1989;38:263-274.
Hoer A. Vitamin B-3 and schizophrenia. 11. Townsend Lett Doctors Patients 2001;213:20-23.
Paterson ET. Vitamin B 12.
3
and liver toxicity. Townsend Lett Doctors Patients 2001;207:23.
Mullin GE, Greenson JK, Mitchell MC. Fulminant hepatic failure after ingestion of sustained-release nicotinic acid. 13.
Ann Intern Med 1989;111:253-255.
Hoer A. Vitamin B-3: niacin and its amide. 14. Townsend Lett Doctors Patients 1995;147:30-39.
Hoer A. 15. Healing Schizophrenia. Toronto, ON: CCNM Press Inc; 2004:7-21.
Horrobin D. 16. Te Madness of Adam and Eve. London, England: Corgi Books; 2001:149-151.
Hoer A. Treating chronic schizophrenic patients. 17. J Orthomol Med 2002;17:25-41.
Goeree R, Farahati F, Burke N, et al. Te economic burden of schizophrenia in Canada in 2004. 18. Curr Med Res Opin
2005;21:2017-2028.
Copyright 2008 Thorne Research, Inc. All Rights Reserved. No Reprint Without Written Permission.
You might also like
- Mckinsey - Style Practice Case #8: Ronald ChocolatesDocument12 pagesMckinsey - Style Practice Case #8: Ronald ChocolatesHiếu LươngNo ratings yet
- IOSA ManualDocument702 pagesIOSA ManualManisha YuukiNo ratings yet
- In Their Own Words: Symptoms of Morgellons and Neuro-Cutaneous Syndrome (NCS)Document8 pagesIn Their Own Words: Symptoms of Morgellons and Neuro-Cutaneous Syndrome (NCS)domasjeffersonNo ratings yet
- Tdap Waiver 2011 CDPH 8261 ColorDocument1 pageTdap Waiver 2011 CDPH 8261 Colorrhawk301No ratings yet
- Halent Chart PDFDocument1 pageHalent Chart PDFmarianNo ratings yet
- Criminal Law Essay FinalDocument15 pagesCriminal Law Essay FinalAlexander PletschNo ratings yet
- Between Helping Hand and Reality (MOM's TJS) by Yi enDocument23 pagesBetween Helping Hand and Reality (MOM's TJS) by Yi encyeianNo ratings yet
- A New Theory and Case Report - David B. Miller D.D.S PDFDocument11 pagesA New Theory and Case Report - David B. Miller D.D.S PDFdrgayen60420% (1)
- Antipurinergic Therapy For Autism-An In-Depth Review.Document15 pagesAntipurinergic Therapy For Autism-An In-Depth Review.Miguel Romero100% (1)
- Autism and Autism Spectrum Disorder Medical Hypothesis For Parasites Influencing AutismDocument3 pagesAutism and Autism Spectrum Disorder Medical Hypothesis For Parasites Influencing AutismCATHYNo ratings yet
- Pneumonia: Past and Present: Dr. Pushpa Raj Sharma Professor of Child Health Institute of MedicineDocument41 pagesPneumonia: Past and Present: Dr. Pushpa Raj Sharma Professor of Child Health Institute of MedicineKartika RezkyNo ratings yet
- Ciprofloxacin Induced Chondrotoxicity and Tendinopathy PDFDocument7 pagesCiprofloxacin Induced Chondrotoxicity and Tendinopathy PDFAvelox FloxNo ratings yet
- Vitamin C Cures PneumoniaDocument3 pagesVitamin C Cures PneumoniafluckiluckNo ratings yet
- Childhood Schizophrenia A Case of Treatment With Nicotinamide and NiacinDocument11 pagesChildhood Schizophrenia A Case of Treatment With Nicotinamide and NiacinJim BennyNo ratings yet
- Abraham HofferDocument6 pagesAbraham Hofferb0409c6d66No ratings yet
- Bio Toxin PathwayDocument1 pageBio Toxin PathwayJackie De Vries100% (1)
- Steps To Peace With GodDocument3 pagesSteps To Peace With GodsudarilNo ratings yet
- The Unitarian or Trophoblastic Thesis of CancerDocument32 pagesThe Unitarian or Trophoblastic Thesis of Canceruge9No ratings yet
- DR Rebecca Carley Is One of Our Greatest Anti-Vaccination CampaignersDocument1 pageDR Rebecca Carley Is One of Our Greatest Anti-Vaccination Campaignersvicaltan100% (1)
- A Novel Therapeutic Strategy To Address: CancerDocument34 pagesA Novel Therapeutic Strategy To Address: CancerAethlon MedicalNo ratings yet
- Disease Reprieve: Living into the Golden YearsFrom EverandDisease Reprieve: Living into the Golden YearsRating: 5 out of 5 stars5/5 (1)
- Speaking TongesDocument3 pagesSpeaking TongesEliezerlunaNo ratings yet
- Nad Therapy Too Good To Be True Theo Verwey Abram Hoffer Ebook PDFDocument150 pagesNad Therapy Too Good To Be True Theo Verwey Abram Hoffer Ebook PDFpdf ebook free download100% (1)
- Multidisciplinary Approach To ProstatitisDocument22 pagesMultidisciplinary Approach To ProstatitisGabrielAbarcaNo ratings yet
- EndoNasal Cranial CorrectionDocument2 pagesEndoNasal Cranial CorrectionYour Charleston HealthNo ratings yet
- COVID-19 Protocol by EVMSDocument13 pagesCOVID-19 Protocol by EVMSKrishnamurthi CG100% (1)
- The Borax Conspiracy: How The Arthritis Cure Has Been StoppedDocument14 pagesThe Borax Conspiracy: How The Arthritis Cure Has Been StoppedMaria & Ioan Mun100% (1)
- BeljanskiDocument2 pagesBeljanskirbtakemotoNo ratings yet
- Mcs Under SiegeDocument16 pagesMcs Under Siegeapi-269724919No ratings yet
- Fake Cancer CuresDocument4 pagesFake Cancer Curesmarianne2009No ratings yet
- No Long-Term or Real-World Safety Studies: Vaccine ChoicesDocument8 pagesNo Long-Term or Real-World Safety Studies: Vaccine Choicesapi-127658921No ratings yet
- Genetic Engineering: Report By: Jess PaloDocument19 pagesGenetic Engineering: Report By: Jess PalorajyavardhanNo ratings yet
- Degeneracion CerebralDocument13 pagesDegeneracion CerebralcarlosNo ratings yet
- Open Universal AntidoteDocument80 pagesOpen Universal AntidoteJusst PainNow100% (1)
- LDN Information PackDocument17 pagesLDN Information PackkindheartedNo ratings yet
- Immunology Final Slide #6 - Stress and The Immune SystemDocument19 pagesImmunology Final Slide #6 - Stress and The Immune SystemMED4HOPENo ratings yet
- Dental Health and Overall Health4Document3 pagesDental Health and Overall Health4Adinda Vashia OktegiandaNo ratings yet
- The Challenges of Lupus - Henrietta Aladjem (Orthomolecular Medicine)Document262 pagesThe Challenges of Lupus - Henrietta Aladjem (Orthomolecular Medicine)Anonymous gwFqQcnaXNo ratings yet
- Dismantling The Virus TheoryDocument11 pagesDismantling The Virus TheoryMilan KosticNo ratings yet
- Ospolot 200 MG, Film-Coated Tablets: Summary of Product Characteristics (SPC)Document7 pagesOspolot 200 MG, Film-Coated Tablets: Summary of Product Characteristics (SPC)ddandan_2No ratings yet
- Colostrum BenefitsDocument8 pagesColostrum BenefitsjcenizalNo ratings yet
- TD DMPS 1Document8 pagesTD DMPS 1api-3714923No ratings yet
- The Truth Behind The Vaccine Cover-Up, Russell Blaylock Neurosurgeon 2004Document28 pagesThe Truth Behind The Vaccine Cover-Up, Russell Blaylock Neurosurgeon 2004karatekla100% (1)
- AO Conference Guide 2014Document60 pagesAO Conference Guide 2014autismoneNo ratings yet
- DMSO + MSM Patent Na Leczenie AutyzmuDocument15 pagesDMSO + MSM Patent Na Leczenie Autyzmumarmar6382No ratings yet
- Zoonotic Parasitic InfectionsDocument1 pageZoonotic Parasitic InfectionsNanda FinisaNo ratings yet
- Telomere PDFDocument2 pagesTelomere PDFsoumita100% (1)
- Brain-Spleen ConnectionDocument2 pagesBrain-Spleen Connectiondupuytren100% (1)
- The Link Between Vitamin B12 and Methylmercury - A ReviewDocument5 pagesThe Link Between Vitamin B12 and Methylmercury - A ReviewOstensibleNo ratings yet
- Gall Bladder & Pancreas 2010Document61 pagesGall Bladder & Pancreas 2010Ali_Hussain_Bo_3755No ratings yet
- Review of Orthomolecular Medicine For Everyonerthomolecular Medicine For EveryoneDocument2 pagesReview of Orthomolecular Medicine For Everyonerthomolecular Medicine For EveryoneJoop Wezenbeek100% (1)
- Metformin Patient HandoutDocument3 pagesMetformin Patient HandoutsilvanaanggraeniNo ratings yet
- 2014 Detox RecipeDocument2 pages2014 Detox RecipefiiansiNo ratings yet
- Dr. Jay Davidson: Let'S "Talk" WithDocument32 pagesDr. Jay Davidson: Let'S "Talk" WithDorian GrayNo ratings yet
- Read The Book Titled Virus ManiaDocument2 pagesRead The Book Titled Virus Maniatesla20080% (1)
- Subject: Assertion of Religious Exemption To VaccinationDocument2 pagesSubject: Assertion of Religious Exemption To VaccinationRosshondra IrvingNo ratings yet
- b3 ArthritisDocument9 pagesb3 ArthritisdaveNo ratings yet
- Cancer - The Terrain and The Living Power PDFDocument3 pagesCancer - The Terrain and The Living Power PDFpaulxe100% (1)
- TEST - Cancer-ParasiteDocument41 pagesTEST - Cancer-ParasiteRazvan Andrei Valcu100% (2)
- (Cáncer - Comparativa) - 6. Ellagic AcidDocument7 pages(Cáncer - Comparativa) - 6. Ellagic Acidpedpix100% (1)
- An Unfortunate Coincidence: A Mother's Life inside the Autism ControversyFrom EverandAn Unfortunate Coincidence: A Mother's Life inside the Autism ControversyNo ratings yet
- Compact Ct-Based Explosives Detection: Technical InformationDocument2 pagesCompact Ct-Based Explosives Detection: Technical InformationraviNo ratings yet
- Graduate Programs and CoursesDocument75 pagesGraduate Programs and CoursesDarwin Aldas BasquialNo ratings yet
- Causes of MeanderingDocument1 pageCauses of MeanderingBalagopal V50% (2)
- Action Plan CommDocument3 pagesAction Plan CommEwan Mary Rose GalagalaNo ratings yet
- 68406-Ch 02Document28 pages68406-Ch 02Kirat Kamboz100% (1)
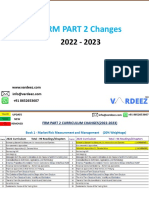
- Macro Curriculum Changes 2023 Part 2Document6 pagesMacro Curriculum Changes 2023 Part 2Al VelNo ratings yet
- Foremans Topic V2 78F Classes of FireDocument2 pagesForemans Topic V2 78F Classes of FireAnonymous 5PsGXCNo ratings yet
- Mining Iii To Viii PDFDocument77 pagesMining Iii To Viii PDFRaja Prabhu0% (1)
- Hazard Assessment Report Legaspi AlbayDocument7 pagesHazard Assessment Report Legaspi AlbayJosh 施志勇 HarderNo ratings yet
- A9810029 enDocument3 pagesA9810029 enAnonymous nIcSGEwNo ratings yet
- Nuvance Health Strategic PlanDocument7 pagesNuvance Health Strategic Planfranjo bacicNo ratings yet
- Find RoommateDocument2 pagesFind RoommateAyaz QaiserNo ratings yet
- Meaning of LeverageDocument5 pagesMeaning of LeverageAdeem AshrafiNo ratings yet
- Desain Pengembangan Karir FTDocument39 pagesDesain Pengembangan Karir FTasma hayatiNo ratings yet
- Boiler Thermal CalculationDocument83 pagesBoiler Thermal Calculation9913489806100% (1)
- Reconciling The Past and The PresentDocument8 pagesReconciling The Past and The PresentJeurdecel Laborada Castro - MartizanoNo ratings yet
- Godly MarriageDocument159 pagesGodly MarriageNonielyn SabornidoNo ratings yet
- Christina H. Parks: Magna Cum Laude, Chemistry HonorsDocument2 pagesChristina H. Parks: Magna Cum Laude, Chemistry HonorsTim BrownNo ratings yet
- Discrimination (Different Type)Document2 pagesDiscrimination (Different Type)Jep DVNo ratings yet
- 2.tfs Spring Source DDocument2 pages2.tfs Spring Source DErica DouglasNo ratings yet
- SeqdumpDocument2 pagesSeqdump20-2020 Rahita purbaNo ratings yet
- Module 4Document5 pagesModule 4Engelbert RespuestoNo ratings yet
- PCPNDT AssignmentDocument5 pagesPCPNDT Assignmentricha ayengia100% (2)
- Structural Chemistry Organic Chemistry Summary: Alkynes: Structure, Conformations, PropertiesDocument20 pagesStructural Chemistry Organic Chemistry Summary: Alkynes: Structure, Conformations, PropertiesMohanraj ShanmugamNo ratings yet
- Yasnac J300 Connecting Manual (Type B)Document186 pagesYasnac J300 Connecting Manual (Type B)sunhuynh100% (1)
- Synthesis of AcetaminophenDocument8 pagesSynthesis of Acetaminophenapi-383568092No ratings yet