Professional Documents
Culture Documents
PIV Blood Draws
PIV Blood Draws
Uploaded by
phidelt649Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PIV Blood Draws
PIV Blood Draws
Uploaded by
phidelt649Copyright:
Available Formats
HEMOLYSIS OF COAGULATION SPECIMENS:
A COMPARATIVE STUDY OF INTRAVENOUS
DRAW METHODS
Authors: Mary Stauss, RN, MSN, APN, CEN, Beth Sherman, RN, BSN, CEN, Lorene Pugh, RN, BSN CEN,
Dominic Parone, RN, BSN, CEN, Karen Looby-Rodriguez, LPN, Annette Bell, MS, MT (ASCP) SH, and
Carole-Rae Reed, RN, PhD, APRN-BC, Camden, NJ
Earn Up to 10 CE Hours. See page 109.
Introduction: Hemolysis of blood samples creates significant
delays in the treatment and disposition of patients in the
emergency department. The purpose of this study was to compare
the hemolysis rates of coagulation blood samples obtained during
insertion of an intravenous (IV) catheter without (group 1) or with
(group 2) extension tubing connected to the IV catheter hub. A
secondary purpose of this study was to determine whether the
investigators could predict whether a coagulation sample was
hemolyzed based on visual observation during the specimen
withdrawal process.
Methods: A prospective, 2-group randomized comparative design
was used to determine which method of blood collection for
coagulation specimens provided the lowest hemolysis rate. This
study was conducted in an urban level I emergency department
averaging 58,000 visits per year. The sample consisted of 121 adult
ED patients randomly assigned to 1 of the 2 groups. Data collectors
were trained in the 2 methods of coagulation sample collection and
followed a strict protocol. The clinical laboratory used a
standardized color-coded scale to determine hemolysis.
Results: Pearson
2
analysis was used to test for differences
between all nominal variables. The level of significance for all
tests was P < .05. There was no significant difference in
hemolysis rates between the groups by use of
2
analysis (P =
.84). Nurses were significantly more likely to predict that a
sample was hemolyzed when it was not and to think that it was
not hemolyzed when in fact it was (P < .001).
Discussion: High hemolysis rates occurred equally when
coagulation blood samples were drawn via a peripheral IV
catheter either at the hub or through extension tubing.
Emergency nurse investigators could not accurately predict by
visualization whether a coagulation sample was hemolyzed at
the time of blood withdrawal. Venipuncture as the preferred
method of blood draw is an industry recommendation. This
method has been shown in prior experimental studies to
reduce hemolysis rates to less than 4%. Therefore, if hemolysis
rates are a concern, one should consider obtaining blood
whenever possible through a venipuncture rather than through
an IV catheter. Replication studies are needed to determine
whether the findings of this study can be generalized to the
larger population.
Key words: Hemolysis; Emergency department; Coagulation
specimens
H
emolysis of blood samples creates significant
delays in the treatment and disposition of patients
in the emergency department. This has multiple
clinical implications. Hemolysis of red blood cells during
the coagulation specimen collection process leads to a fal-
sely low test result as the spillage of red blood cell contents
Mary Stauss, Member, Southern Jersey Chapter, Clinical Nurse Specialist,
Cooper Medical Center, Camden, NJ.
Beth Sherman, Member, Southern Jersey Chapter, is Staff Nurse, Emergency
Department, Cooper Medical Center, Camden, NJ.
Lorene Pugh, Member, Southern Jersey Chapter, Staff Nurse, Emergency
Department, Cooper Medical Center, Camden, NJ.
Dominic Parone, Member, Southern Jersey Chapter, Staff Nurse, Emergency
Department, Cooper Medical Center, Camden, NJ.
Karen Looby-Rodriguez, Member, Southern Jersey Chapter, Staff Nurse, Emer-
gency Department, Cooper Medical Center, Camden, NJ.
Annette Bell is Hematology Manager, Cooper Medical Center, Camden, NJ.
Carole-Rae Reed is Nursing Research Coordinator, Cooper Medical Center,
Camden, NJ.
For correspondence, write: Mary Stauss, RN, MSN, APN, CEN, Emergency
Department, Cooper Medical Center, 1 Cooper Plaza, Camden, NJ 08083;
E-mail: stauss-mary@cooperhealth.edu.
J Emerg Nurs 2012;38:15-21.
Available online 2 October 2010.
0099-1767/$36.00
Copyright 2012 Emergency Nurses Association. Published by Elsevier Inc.
All rights reserved.
doi: 10.1016/j.jen.2010.08.011
R E S E A R C H
January 2012 VOLUME 38 ISSUE 1 WWW.JENONLINE.ORG 15
activates the clotting mechanism. For example, a PTT may
actually be 41 seconds, but a hemolyzed sample may show
a normal result. In our emergency department, redrawing a
blood specimen extends our disposition time by 45 to 60
minutes on average. This leads to increased time to treat-
ment and disposition, patient and staff dissatisfaction,
higher facility costs, and extended waiting times for
patients yet to be seen.
Venipuncture is the recommended method of blood
draw to minimize hemolysis of blood samples.
1
However,
our emergency nurses rarely use this method. Typically,
our emergency nurses draw blood samples during the inser-
tion of an intravenous (IV) line either directly from the hub
of the IV catheter or from extension tubing connected to
the IV catheter. This is done to minimize patient discom-
fort from multiple insertions. In our emergency depart-
ment, coagulation samples were the specimens identified
by the nurses as those most frequently rejected because
of hemolysis by our clinical laboratory.
Many of our emergency nurses were certain that they
knew whether a coagulation specimen was hemolyzed
before sending it for analysis. They were convinced that
hemolysis of coagulation specimens was related to the indi-
vidual laboratory technician analyzing the specimen. They
were also concerned that anticoagulant therapy might be
the cause of hemolysis. We were curious whether either
draw method led to less hemolysis of coagulation speci-
mens and whether the nurses perceptions were accurate.
Prior studies found that hemolysis rates in emergency
departments were between 10% and 20%.
2-9
Our coagula-
tion hemolysis rate was 15.2%for the month before the start
of this study. Multiple factors are associated with these high
hemolysis rates.
2-11
Drawing blood through IVcatheters was
identified as having a significantly higher hemolysis rate than
when blood was drawn directly through a needle inserted
into the vein.
2,3,6,9,10
Other research suggests that hemolysis
rates were affected by the size of the catheter,
2,5
number of
attempts at catheter placement,
2
type of collection system
used (syringe with transfer to a Vacutainer tube [Becton
Dickinson (BD), Franklin Lakes, NJ], directly into a Vacu-
tainer tube,
2-4
or via a butterfly needle
4,8,10
); site of the
blood draw,
2,3,5
and medical diagnosis of the patient.
2
These
studies indicate that hemolysis rates are higher in the follow-
ing circumstances: in specimens obtained fromsmaller-sized
catheters or needles; when sites other than the antecubital
vein are used; when blood is transferred by syringe to Vacu-
tainer tubes; when specimens are obtained through IVcathe-
ters; with multiple attempts at IV insertion; and in patients
with cardiovascular, respiratory, or reproductive disorders.
We found few experimental studies that determined
whether any of these factors can be altered to decrease hemo-
lysis rates. Our study was prompted by a difference of opi-
nion among our emergency nurses as to whether less
hemolysis occurs with coagulation specimens drawn directly
fromthe IVcatheter hub or through the catheter tubing. We
were also interested in ascertaining whether nurses could
indeed determine whether a specimen was hemolyzed.
The primary purpose of this study was to compare the hemo-
lysis rates of coagulation blood samples obtained during the
insertion of an IV catheter with or without extension tubing
connected to the IV catheter hub. A secondary purpose of
this study was to determine whether the nurse investigators
could predict sample hemolysis.
Methods
STUDY DESIGN
A prospective, 2-group randomized comparative design was
used to determine which method of blood collection for coa-
gulation specimens (directly fromthe catheter hub vs through
extension tubing) provided the lowest hemolysis rate.
SAMPLE AND SETTING
This study was conducted in an urban level I emergency
department averaging 58,000 visits per year. Before data col-
lection, approval for the study was obtained from the insti-
tutions investigational review board. All study investigators
completed our institutions investigational review board
education requirements. The emergency nurse investigators
explained the study to eligible patients, obtained verbal con-
sent, and obtained the specimens. Confidentiality of all
study participants data was maintained.
To test the primary hypothesis of a significant difference
in hemolysis rates by type of blood withdrawal, a minimum
sample size of 118 participants (59 per group) was needed to
achieve 80% power to detect differences with a significance
level of .05, assuming a medium effect size. We decided to
recruit 122 participants to allowfor incomplete data or other
unexpected events that could compromise data.
Inclusion criteria were patients aged 21 years or older
who required a coagulation study and insertion of a 20-
gauge IV catheter. Exclusion criteria were level I patients
as per the Emergency Severity Index criteria,
12
a body tem-
perature lower than 35.5C (96F), and/or a systolic blood
pressure lower than 90 mm Hg. Level I patients were
excluded because of the critical nature of their illness.
Potentially eligible participants were assigned a number
randomly generated by Microsoft Excel (Microsoft Office
2003; Microsoft, Redmond, WA) before enrollment. Con-
senting participants were randomly assigned to 1 of the study
groups when a physician ordered an IV line inserted and a
coagulation study. Emergency nurse investigators were
RESEARCH/Stauss et al
16 JOURNAL OF EMERGENCY NURSING VOLUME 38 ISSUE 1 January 2012
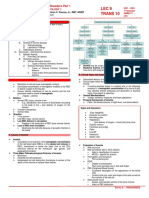
Procedure for Coagulation Blood Sampling
Group 1:
Blood sample directly from
catheter hub
Group 2:
Blood sample via extension
tubing connected to IV
catheter hub
Insert #20 g IV catheter
1.Screw a Vacutainer needle Leur Adapter onto the end of a
Vacutainer holder*
2. Using sterile technique insert the assembled Vacutainer
needle and holder into the hub of the # 20 g intravenous
catheter +
Screw the male end of the extension tubing ^ into the hub of the
20 g intravenous catheter using sterile technique.
Press on the end of the Vacutainer tube until the Vacutainer
needle Leur Adapter pierces the diaphragm.
Maintain pressure on the end of the Vacutainer tube until the tube is filled to the top of the Vacutainer label.
Remove the Vacutainer tube from the holder and discard the specimen.
Insert a 2.7mL plastic, coagulation sample Vacutainer tube with sodium citrate preservative & into the open
end of Vacutainer holder.
Press on the end of the Vacutainer tube until the Vacutainer needle pierces the diaphragm of the tube.
Maintain pressure on the end of the Vacutainer tube until the tube is filled to the top of the Vacutainer label.
Remove the Vacutainer tube from the holder and gently invert several times.
Screw a Vacutainer needle Leur Adapter onto the female end of
the extension tubing using sterile technique.
* BD, Franklin Lakes, NJ (BD), Franklin Lakes, NJ)
+ Introcan Safety IV Catheters, Braun, Bethlehem, Pa)
^ Macro CLAVE seven inch extension tubing # B9095, ICU Medical Inc., San Clemente, Ca)
& Coagulation tube # 363083, BD, Franklin Lakes, NJ
FIGURE
Procedure for coagulation blood sampling. This figure is available in color and as a full-page document at www.jenonline.org.
Stauss et al/RESEARCH
January 2012 VOLUME 38 ISSUE 1 WWW.JENONLINE.ORG 17
trained in the study techniques for obtaining specimens and
obtained all specimens collected for this study.
STUDY PROCEDURES
A standard procedure for obtaining coagulation blood sam-
ples was followed. Coagulation samples were obtained
immediately after insertion of a 20-gauge by 1-inch IV
catheter. IV insertion sites varied. Order of the draw, as
recommended by BD for blood collection tubes, was
observed: (1) blood culture or non-additive discard tube,
(2) citrate (coagulation/blue top), (3) gel separator and
serum (gold and red top), (4) heparin (green top), (5) ethy-
lenediaminetetraacetic acid (EDTA) (purple and pink top),
and (6) fluoride (gray top).
13
The armtourniquet applied for
IV insertion was released once the sample was drawn. Inser-
tion sites were not specified in the blood draw protocol.
Once the coagulation sample was obtained, the nurse
investigator acquiring the sample rated the difficulty of
obtaining the blood (difficulty/no difficulty with needle
insertion), how well the blood flowed into the Vacutainer
specimen tube (easy flow or poor flow), and whether he or
she thought the specimen was hemolyzed (Figure). Speci-
mens were then sent to the clinical laboratory for analysis.
The number of insertion attempts was not recorded.
The coagulation specimen was received by the clinical
laboratory and sent to the laboratory technologist for ana-
lysis. The technologist checked the specimen for a clot by
rimming the tube with 2 wooden applicator sticks. Next,
the technologist examined the coagulation tube to ensure
the volume in the tube was sufficient. (Coagulation tube
volume must be within 10% of the fill line.) After this,
the specimen was centrifuged at approximately 2,800g for
5 to 7 minutes to separate the cells from the plasma. Once
the plasma was removed from the centrifuge, the techno-
logist examined it for presence of hemolysis.
Before this study, each laboratory technologist visually
determined the level of hemolysis present and then decided
whether to accept or reject the specimen; no established
reference guide was used by the laboratory to determine
hemolysis levels. Therefore, for the duration of this study,
we asked the clinical laboratory technologists to use a stan-
dardized, color visualization hemolysis scale that rated
hemolysis on a range from 0 mg/dL (clear, no hemolysis)
to 1,100 mg/dL (dark red, large amount of hemolysis).
14
Because this visual scale is not routinely used in our hospi-
tal, laboratory personnel were trained in its use before data
collection. The laboratory technologist compared the cen-
trifuged sample with 7 pictures on the scale. Each picture
had a designated value of 0, 35, 70, 140, 275, 550, or
1,100 mg/dL. On the basis of input from the Clinical
Laboratory Hematology Manager, coagulation samples
with readings of 0 (no hemolysis) to 70 mg/dL (slight
hemolysis) were considered nonhemolyzed for purposes
of this study, whereas those rated 140 mg/dL or greater
were considered hemolyzed.
DATA ANALYSIS PROCEDURES
Data were summarized by use of descriptive statistics. Pear-
son
2
analysis was used to test for differences in hemolysis
rates between the 2 groups. The level of significance for all
tests was P < .05. All statistical analyses were done with SPSS
software, version 15.1 (SPSS, Chicago, IL). To determine
whether nurses could predict sample hemolysis by visualiza-
tion, Pearson
2
was used. A 2-sided t test was used to deter-
mine differences in mean age between the study groups. To
determine whether the difficulty of insertion, ease of draw,
and blood flow resulted in significant differences in hemoly-
sis rates, the Mantel-Haenszel trend test was used. This test
was used because 1 cell had an expected count of less than 5;
the minimum expected count was 3.63.
Results
During the study period, a total of 122 participants were
recruited and their coagulation samples drawn. One sub-
ject was eliminated because of not meeting the minimum
age requirement of greater than 21 years. Study subjects
ranged in age from 26 to 96 years, with a mean of
60.49 years (standard deviation [SD], 16.67). We elimi-
nated 1 participants specimen from the study because of
an inadequate sample volume, resulting in a final sample
size of 120. Five subjects were missing age data. At the
time of the study, 19 subjects were receiving anticoagulant
therapy (12 in group 1 [hub draws] and 7 in group 2
[extension tubing draws]). Anticoagulant data were missing
for 2 subjects. There was no significant difference between
groups in relation to anticoagulant therapy (P = .23).
Group 1 included 60 subjects ranging in age from 26 to
96 years (mean, 58.28 years; SD, 17.94). Group 2 included
60 subjects ranging in age from 33 to 88 years (mean, 62.71
years; SD, 15.14). There was no significant difference
between the groups in relation to age (P = .097) (Table 1).
Group 1 (hub group, n = 60) had 19 hemolyzed samples
(31.67%) and 41 nonhemolyzed samples (68.33%) when
the criterion for hemolysis was set at less than 140 mg/dL
on the colormetric scale. Group 2 (tubing group, n = 60)
had 18 hemolyzed samples (30%) and 42 nonhemolyzed
samples (70%) when the criterion for hemolysis was set at
less than 140 mg/dL on the colormetric scale. There was
no significant difference in hemolysis rates by use of Pearson
2
analysis (P = .84). Table 2 shows hub versus tubing
hemolysis rates.
RESEARCH/Stauss et al
18 JOURNAL OF EMERGENCY NURSING VOLUME 38 ISSUE 1 January 2012
Because no hemolysis, or 0 mg/dL, yields the best pos-
sible test result, we were interested in whether reanalyzing
the data using a criterion of 0 mg/dL to indicate no hemo-
lysis with any value greater than 0 mg/dL considered
hemolyzed would yield different results. When the data
were reanalyzed with that criterion, the rate of hemolysis
was the same for both groups (33.33% [n = 120]).
A secondary purpose of this study was to determine
whether the investigators could predict whether a coagula-
tion sample was hemolyzed. Nurses were significantly more
likely to predict that a sample was hemolyzed when it was
not and to think that it was not hemolyzed when in fact it
was (Pearson
2
, 18.18; P < .001, 2 sided).
The nurse investigators also reported difficulty of
insertion, ease of draw, and blood flow. Analysis showed
a significant difference in hemolysis rates (P = .00021,
Mantel-Haenszel trend test) with samples rated as no diffi-
culty and thus less likely to be hemolyzed than those rated
as either a difficult draw or difficult insertion.
Discussion
This is the first randomized clinical study to our knowledge
that evaluated hemolysis rates of coagulation specimens
drawn using extension tubing compared with those drawn
directly from an IV catheter hub. There were no statisti-
cally significant differences found in the hemolysis rates
between the 2 groups. Prior studies have evaluated blood
drawn from an IV catheter using a syringe compared with
blood drawn via a Vacutainer device, but none have com-
pared the 2 techniques used in this study.
2-5,10
During data collection, the nurse investigators indicated
whether they thought the coagulation specimen was hemo-
lyzed. At the time of this study, no literature was found that
addressed nurses ability to predict sample hemolysis. Some
of our staff nurses were convinced that they could tell
whether a sample was hemolyzed. Nurses in this study were
not able to predict hemolysis with any degree of certainty.
This misconception is most likely due to a lack of knowledge
regarding the clinical laboratory process for determining
hemolysis. Of interest was the finding that the nurses per-
ceptions regarding the difficulty of IV catheter insertion,
ease of blood draw via either method, and problems with
blood flow during specimen collection were associated with
hemolysis. In our sample these factors were associated with a
significantly higher hemolysis rate than samples rated as hav-
ing no difficulty. Any type of difficulty with the blood draw
was more likely to be associated with hemolysis than the
method of withdrawal. It seems that the difficulty of speci-
men collection may be an important factor associated with
hemolysis of coagulation specimens.
Although the cause of hemolysis in samples drawn
through IV catheters is unknown, other researchers have
hypothesized that the soft walls of the peripheral IV cathe-
ters used today may actually collapse and/or kink during
blood withdrawal, leading to excessive turbulence in blood
flow and hemolysis.
3,8
Finding methods for blood withdra-
wal that limit catheter wall collapse could lead to lower
hemolysis rates.
TABLE 1
Sample characteristics
Total sample
(N = 120)
Group 1: Hub
(n = 60)
Group 2: Tubing
(n = 60) P value
Age .15
*
Mean (SD) (y) 60.49 (16.67) 58.27 (17.93) 62.71 (15.14)
n 116 58 58
Anticoagulant use 19 12 7 .23
*
n (%) 119 (16%) 60 (20%) 59 (12%)
Hemolyzed at >0 mg/dL on colormetric scale, n (%) 40 (33%) 20 (33%) 20 (33%) >.99
*
Hemolyzed at 140 mg/dL on colormetric scale, n (%) 37 (31%) 19 (32%) 18 (30%) .84
*
*
There were no significant differences between groups for any variable.
TABLE 2
Hemolysis rates for blood coagulation samples
drawn from IV catheter hub versus extension tubing
Hemolyzed Hub group
*
Tubing group
*
Yes (139 mg/dL) 41 (68.3%) 42 (70%)
No (140 mg/dL) 19 (31.7%) 18 (30%)
Total 60 60
*
There was no significant difference between groups (P = .84).
Stauss et al/RESEARCH
January 2012 VOLUME 38 ISSUE 1 WWW.JENONLINE.ORG 19
Anatomic site of the blood draw may also affect hemo-
lysis rates. Several studies identified greater hemolysis rates
when sites other than the antecubital were used for blood
withdrawal.
4,10,11
These studies used multiple devices for
blood sampling, so it is unclear what the best approach
is. One of the limitations of our study was that we did
not control for anatomic site for blood withdrawal. A com-
parison of the various methods using the antecubital site
may yield further clarity on this issue. In particular, butter-
fly devices, another method of blood withdrawal in emer-
gency departments, may warrant future investigation.
Another technique that might result in lower hemolysis
rates would be release of the tourniquet after successful
IV catheter insertion and reapplication of it to draw blood
specimens. Our study controlled for investigator differences
in tourniquet use by leaving the tourniquet in place until
after the blood sample was drawn.
The rate of hemolysis found in our study is higher
than the rates observed in prior research.
2-11
Although
most studies were non-experimental, none of the studies
had hemolysis rates greater than 21%, with the exception
of the study by Fang et al
11
(33.7%). We do not know why
our rate of hemolysis is so high. In the month before the
start of this study, our coagulation hemolysis rate was
15.2%. The higher hemolysis rate may be because of the
implementation of the color visualization scale chart. Our
study used methods for blood withdrawal that were very
similar to prior studies, including use of a Vacutainer
assembly device, emphasis on slow withdrawal of blood
from the catheter, and use of a larger-gauge IV catheter.
In addition, we used smaller-volume tubes (2.7 mL). A
prior experimental study showed decreased hemolysis rates
with lower-volume tubes (5 mL) compared with 10 mL.
7
Use of soft-draw coagulation tubes may also decrease
hemolysis.
7
However, soft-draw tubes for coagulation spe-
cimens are not available.
A likely cause of the hemolysis rate differences may be
the methods used for determining hemolysis in each of the
studies. This study used a standardized, visual inspection
method where individual specimens are compared with a
color chart depicting the color of samples with different
levels of hemolysis.
14
Although some of the studies did
not adequately describe the method used for determining
hemolysis, none of those studies appeared to have used the
particular hemolysis chart used in this study. In comparing
the hemolysis visualization chart used in this study with the
2 studies that did publish a figure of a hemolysis chart,
2,6
we
found that although the colors on the visual scale indica-
tors were similar, the designated level for a hemolyzed spe-
cimen in the studies was different. This study had a lower
threshold for hemolysis, rejecting specimens with a value of
140 mg/dL or greater. In 2005 Dugan et al
2
identified speci-
mens as hemolyzed at 200 mg/dL or greater on the color-
metric scale used in their study. If we used a higher
hemolysis cutoff level similar to that of Dugan et al, our hemo-
lysis rates would still be higher than in prior studies. This indi-
cates the need for further studies using similar criteria.
Temperature regulation of the blood sample tubes dur-
ing storage is another factor that could have accounted for
the high hemolysis rates observed in our study. The man-
ufacturer recommends that Vacutainer blood sample tubes
with sodium citrate are stored at room temperature.
15
Var-
iances in temperature affect the vacuum of the tube, which
may affect hemolysis rates. It is possible that the Vacutainer
tubes used in this study were not properly stored after man-
ufacture, leading to higher hemolysis rates.
Limitations
The results of this study cannot be generalized to other emer-
gency departments because of the small sample size. We
attempted to limit variations in technique between the emer-
gency nurse investigators by training all data collectors
before study enrollment. However, this study did not con-
trol for user differences in draw technique, anatomic site of
draw, or number of IV insertion attempts. Another limita-
tion was the use of a visual color scale to determine hemoly-
sis. Our clinical laboratory does not routinely use this scale
but instead relies on the individual technicians visual
inspection and judgment of level of hemolysis.
Implications for Emergency Nurses
In this study emergency nurse investigators could not accu-
rately predict by visualization whether a coagulation sample
was hemolyzed at the time of blood withdrawal. Second,
high hemolysis rates occurred equally when coagulation
blood samples were drawn via a peripheral IV catheter
either at the hub or through extension tubing. Replication
studies are needed to determine whether the findings of
this study can be generalized to the larger population. In
the interim, if hemolysis rates are a concern, one should
consider obtaining blood whenever possible through a
venipuncture rather than through an IV catheter. Veni-
puncture as the preferred method of blood draw is also
an industry recommendation.
1
Furthermore, this method
has been shown in prior experimental studies to reduce
hemolysis rates to less than 4%.
5,6
Conclusions
We found that neither method made a difference in hemo-
lysis rates in this study. Difficulty of IV catheter insertion,
RESEARCH/Stauss et al
20 JOURNAL OF EMERGENCY NURSING VOLUME 38 ISSUE 1 January 2012
ease of blood draw, and problems with blood flow during
specimen collection were associated with a significantly
higher hemolysis rate than samples rated as having no diffi-
culty. It seems that the difficulty of specimen collection may
be an important factor associated with hemolysis of coagula-
tion specimens. Additional research is needed to identify
whether this and/or other factors increase or reduce hemoly-
sis rates in coagulation samples obtained in ED patients.
Acknowledgment
We thank Barry Milcarek, PhD, Krystal Hunter, MBA, and Marianne Chulay,
RN, PhD, FAAN, for their mentorship and support of this research project.
REFERENCES
1. Bush V, Mangan L. The hemolyzed specimen: causes, effects, and reduc-
tion. BD Vacutainer Systems, Preanalytical Solutions. LabNotes. 2003;13
(1):1-5.
2. Dugan L, Leech L, Speroni KG, Corriher J. Factors affecting hemolysis
rates in blood samples drawn from newly placed IV sites in the emer-
gency department. J Emerg Nurs. 2005;31(4):338-45.
3. Grant MS. The effect of blood drawing techniques and equipment on
the hemolysis of ED laboratory blood samples. J Emerg Nurs. 2003;29
(2):116-21.
4. Pretlow L, Gandy T, Leibach EK, Russell B, Kraj B. A quality improve-
ment cycle: hemolyzed specimens in the emergency department. Clin
Lab Sci. 2008;21(4):219-24.
5. Kennedy C, Angermuller S, King R, Noviello S, Walker J, Warden J,
et al. A comparison of hemolysis rates using intravenous catheters ver-
sus venipuncture tubes for obtaining blood samples. J Emerg Nurs.
1996;22(6):566-9.
6. Lowe G, Strike R, Pollack M, Bosley J, OBrien P, Hake A, et al. Nur-
sing blood specimen collection techniques and hemolysis rates in the
emergency department: analysis of veniinsertion versus catheter collec-
tion techniques. J Emerg Nurs. 2008;34(1):26-32.
7. Cox SR, Dages JH, Jarjoura D, Hazelett S. Blood samples drawn from
IV catheters have less hemolysis when 5-mL (vs. 10-mL) collection tubes
are used. J Emerg Nurs. 2004;30(6):529-33.
8. Lippi G, Salvagno GL, Brocco G, Guidi GC. Preanalytical variability in
laboratory testing: influence of the blood drawing technique. Clin Chem
Lab Med. 2005;43(3):319-25.
9. Seemann S, Reinhardt A. Blood sample collection from a peripheral
catheter system compared with phlebotomy. J Intraven Nurs. 2000;
23(5):290-7.
10. Tanabe P, Kyriacou D, Garland F. Factors affecting the risk of blood
bank specimen hemolysis. Acad Emerg Med. 2003;10(8):897-900.
11. Fang L, Fang S-H, Chung Y-H, Chien S-T. Collecting factors related
to the haemolysis of blood specimens. J Clin Nurs. 2008;17(17):
2343-51.
12. Gilboy N, Tanabe P, Travers DA, Rosenau AM, Eitel DR. Emergency
severity index, version 4: implementation handbook. AHRQ Publica-
tion No. 05-0046-2. Rockville, MD: Agency for Healthcare Research
and Quality; 2005. www.ahrq.gov/research/esi/esi2.htm. Accessed Sep-
tember 22, 2010.
13. Smith B. Preanalytical errors in the emergency department. LabNotes. 2007;
17(1):1-5. http://www.bd.com/vacutainer/labnotes/Volume17Number1/.
Accessed September 22, 2010.
14. BD Global Technical Services. Relative hemolysis scale. 2005. BD Diag-
nostics Preanalytical Systems. www.bd.com/Vacutainer2005. Accessed
March 19, 2007.
15. Becton, Dickinson and Company. BD Vacutainer CPT cell prepara-
tion tube with sodium citrate http://www.bd.com/Vacutainer/pro-
ducts/molecular/citrate/procedure.asp. Accessed August 9, 2008.
Stauss et al/RESEARCH
January 2012 VOLUME 38 ISSUE 1 WWW.JENONLINE.ORG 21
You might also like
- ASCP Review Course: Review Questions: Blood Banking and Transfusion MedicineDocument18 pagesASCP Review Course: Review Questions: Blood Banking and Transfusion MedicineMarl Estrada100% (1)
- The Teaching-Coaching FunctionDocument14 pagesThe Teaching-Coaching Functionapi-419091662100% (1)
- Difficult IV Access C PGDocument42 pagesDifficult IV Access C PGFitrii WulanDari FitriNo ratings yet
- Ali, P. 2008. Professional Development and The Role of Mentorship. Nursing StandardDocument5 pagesAli, P. 2008. Professional Development and The Role of Mentorship. Nursing Standardsiti akbariNo ratings yet
- Describing - Nurse - Manager - Role - Preparation - and CompetencyDocument7 pagesDescribing - Nurse - Manager - Role - Preparation - and CompetencyAnita FaúndezNo ratings yet
- Nursing Students Perceptions of Desirable Leadership Qualities in NurseDocument15 pagesNursing Students Perceptions of Desirable Leadership Qualities in NurseRereNo ratings yet
- Educator Portfolio TemplateDocument5 pagesEducator Portfolio Templateapi-257029163No ratings yet
- CapitalNurse Preceptorship FrameworkDocument23 pagesCapitalNurse Preceptorship FrameworkRijantono Franciscus Maria100% (1)
- Introduction For Nurse Leader InterviewDocument4 pagesIntroduction For Nurse Leader Interviewapi-312833369No ratings yet
- 50 IV Therapy Tips and TricksDocument10 pages50 IV Therapy Tips and TricksAmar Freebiker Abaza0% (1)
- The Ward Leader's Handbook: October 2018Document49 pagesThe Ward Leader's Handbook: October 2018MaggieNo ratings yet
- Competences of Advanced NursingDocument8 pagesCompetences of Advanced NursingNatukunda DianahNo ratings yet
- The Transition From Staff Nurse To Ward Leader PDFDocument4 pagesThe Transition From Staff Nurse To Ward Leader PDFStephany ZamorasNo ratings yet
- Nurses Knowledge and Competence in Wound Management PDFDocument9 pagesNurses Knowledge and Competence in Wound Management PDFWawan Febri RamdaniNo ratings yet
- Literature Review On Nursing MentorshipDocument5 pagesLiterature Review On Nursing Mentorshipc5nj94qn100% (1)
- Nursing AuditDocument26 pagesNursing AuditpkvNo ratings yet
- Leardership Challeges Encountered by NurseDocument96 pagesLeardership Challeges Encountered by NurseyowiskieNo ratings yet
- Improving Documentation Using A Nursing ModelDocument10 pagesImproving Documentation Using A Nursing ModelLaraBindeNo ratings yet
- English 1 - Nursing Activity (Leader and Manager)Document5 pagesEnglish 1 - Nursing Activity (Leader and Manager)agannn573No ratings yet
- Epidural Analgesia - A Self-Directed Learning Module 3rdDocument41 pagesEpidural Analgesia - A Self-Directed Learning Module 3rdAnnisa Chaerani BurhanuddinNo ratings yet
- ChesttubesDocument30 pagesChesttubesapi-2692977900% (1)
- Nur 862 Clinical Competencies PortfolioDocument11 pagesNur 862 Clinical Competencies Portfolioapi-457407182No ratings yet
- Safe IV CannulationDocument32 pagesSafe IV Cannulationanon_281166672No ratings yet
- 128 Professional StandardsDocument40 pages128 Professional StandardsPaul BensonNo ratings yet
- Concept Map BlankDocument16 pagesConcept Map BlankEric MillsNo ratings yet
- Venous UlcersDocument11 pagesVenous UlcersAndrea Gómez SchulzNo ratings yet
- Ana Self AssessmentDocument7 pagesAna Self Assessmentapi-301349934No ratings yet
- Nursing Interview - PrepDocument4 pagesNursing Interview - PrepDev Ebenezer JohnsonNo ratings yet
- Career PlanningDocument27 pagesCareer PlanningGelah DacanayNo ratings yet
- Lesson Plan On Wound Care - With CommentsDocument7 pagesLesson Plan On Wound Care - With CommentsJoyJoy Tabada CalunsagNo ratings yet
- Portfolio Nursing ToolsDocument10 pagesPortfolio Nursing ToolsNining Komala SariNo ratings yet
- Practice Development Workbook for Nursing, Health and Social Care TeamsFrom EverandPractice Development Workbook for Nursing, Health and Social Care TeamsNo ratings yet
- Career Development Guide: Engineers AustraliaDocument37 pagesCareer Development Guide: Engineers AustraliaRico PadillaNo ratings yet
- Charge Nurse, Reading, Kardex, AnecdotalDocument10 pagesCharge Nurse, Reading, Kardex, AnecdotalAubrey Unique EvangelistaNo ratings yet
- Wound Case Study AssessmentDocument7 pagesWound Case Study Assessmentcass1526100% (2)
- Resources For EportfoliosDocument3 pagesResources For EportfoliosHazel Owen100% (2)
- Advanced Wound Care Therapies UlcerDocument182 pagesAdvanced Wound Care Therapies UlcerJuan Jose Leon100% (1)
- Role of The Nurse To Nurse Handover in Patient CareDocument5 pagesRole of The Nurse To Nurse Handover in Patient CarefarahdlcNo ratings yet
- Leadership Skills For Nurses PDFDocument34 pagesLeadership Skills For Nurses PDFshrikantgakhareNo ratings yet
- Peripheral IVs For BeginnersDocument19 pagesPeripheral IVs For BeginnersMark Hammerschmidt86% (7)
- Critical Care Nursing ClinicsDocument133 pagesCritical Care Nursing ClinicsJune DumdumayaNo ratings yet
- Effective Communication in NursingDocument19 pagesEffective Communication in Nursingyanuar anazdiNo ratings yet
- Clinical Nurse Leader Portfolio 1Document7 pagesClinical Nurse Leader Portfolio 1api-247952145No ratings yet
- Dialysis Nurse ResumeDocument7 pagesDialysis Nurse Resumeaflkotkax100% (1)
- Registered Professional Nurse: Passbooks Study GuideFrom EverandRegistered Professional Nurse: Passbooks Study GuideNo ratings yet
- Nursing LeadershipDocument15 pagesNursing LeadershipRolando PinchettiNo ratings yet
- A Review of The Cardiovascular System and ECG Performance, Troubleshooting, and InterpretationDocument47 pagesA Review of The Cardiovascular System and ECG Performance, Troubleshooting, and InterpretationRetroPilotNo ratings yet
- A Strategic Guide to Continuing Professional Development for Health and Care Professionals: The TRAMm ModelFrom EverandA Strategic Guide to Continuing Professional Development for Health and Care Professionals: The TRAMm ModelNo ratings yet
- Clinical LeadershipDocument18 pagesClinical Leadershipsamz Khaizer001100% (1)
- Career Clarity for Nurses: Navigating Nursing Through Challenging TimesFrom EverandCareer Clarity for Nurses: Navigating Nursing Through Challenging TimesRating: 1 out of 5 stars1/5 (1)
- CV Building ExercisesDocument15 pagesCV Building ExercisesSid KrishNo ratings yet
- A Daybook For Nurse Educators - K. Parkieser-Reed (STI Int'l., 2011) WWDocument191 pagesA Daybook For Nurse Educators - K. Parkieser-Reed (STI Int'l., 2011) WWRadu Șopu100% (1)
- Hemodialysis Thesis - Analytical EssayDocument4 pagesHemodialysis Thesis - Analytical EssayDianne LopezNo ratings yet
- Sample Assignment of Nursing LeadershipDocument5 pagesSample Assignment of Nursing LeadershipPrasiddha Parajuli100% (1)
- Observation Summary 2Document5 pagesObservation Summary 2api-493028287No ratings yet
- Sun-6000 User's ManualDocument44 pagesSun-6000 User's Manualfrancisco mendezNo ratings yet
- University of Saint Louis Tuguegarao City, Philippines: Maternal and Child Health NursingDocument70 pagesUniversity of Saint Louis Tuguegarao City, Philippines: Maternal and Child Health NursingSam PothNo ratings yet
- Clinical Pathology MCQDocument14 pagesClinical Pathology MCQhshshhsjsjsbxxhNo ratings yet
- F1841 1479757-1Document5 pagesF1841 1479757-1Thaweekarn Changthong100% (1)
- G6PD, GalactosemiaDocument32 pagesG6PD, GalactosemiaEricka B. BanaszczukNo ratings yet
- Transfusion Reaction and Coombs Test: Moderator:-Dr Sanjay Agrwal Presenter: - DR Pratima Singh PG Jr-1Document33 pagesTransfusion Reaction and Coombs Test: Moderator:-Dr Sanjay Agrwal Presenter: - DR Pratima Singh PG Jr-1UmikaguptaNo ratings yet
- RBC Count: Why The Test Is PerformedDocument3 pagesRBC Count: Why The Test Is PerformedFahmi SaputraNo ratings yet
- Methyldopa Drug StudyDocument2 pagesMethyldopa Drug Studymilkv100% (14)
- PDF Anemia in The Young and Old Diagnosis and Management Robert T Means JR Editor Ebook Full ChapterDocument51 pagesPDF Anemia in The Young and Old Diagnosis and Management Robert T Means JR Editor Ebook Full Chapterelaine.ruiz756100% (5)
- Prolong Storage of Blood in EDTADocument5 pagesProlong Storage of Blood in EDTAGriffin MulofwaNo ratings yet
- Blood Transfusion ChecklistDocument2 pagesBlood Transfusion ChecklistMary Grace GestiadaNo ratings yet
- Haematology Dissertation TopicsDocument6 pagesHaematology Dissertation TopicsCollegePapersWritingServiceCanada100% (1)
- TESTS DISEASES OF BLOOD AND ENDOCRINE SYSTEM Methodical Manual For The 5 Year PDFDocument152 pagesTESTS DISEASES OF BLOOD AND ENDOCRINE SYSTEM Methodical Manual For The 5 Year PDFMayur WakchaureNo ratings yet
- Tanzania - CBC Lecture-2-17-14Document61 pagesTanzania - CBC Lecture-2-17-14Jonathan Jas100% (2)
- Dr. Mohammed H Saiemaldahr Blood Bank Med Tech Dep @kaauDocument20 pagesDr. Mohammed H Saiemaldahr Blood Bank Med Tech Dep @kaauKristiann lourine ProvidoNo ratings yet
- Blood Physio MCQSDocument6 pagesBlood Physio MCQSHammad Tariq0% (1)
- Answers, Rationales, and Test Taking Strategies: Managing Care Quality and SafetyDocument16 pagesAnswers, Rationales, and Test Taking Strategies: Managing Care Quality and SafetyNursyNurseNo ratings yet
- HemoCue Plasma Low HB Overview 131123Document22 pagesHemoCue Plasma Low HB Overview 131123Trung LeNo ratings yet
- Chapter Four: Chemical Analysis of UrineDocument211 pagesChapter Four: Chemical Analysis of UrineErenjaeger TitanNo ratings yet
- Pancreas and SpleenDocument106 pagesPancreas and SpleenJorge De Vera100% (1)
- Hematology Trans 10Document6 pagesHematology Trans 10Claire GonoNo ratings yet
- Microcytic AnemiaDocument6 pagesMicrocytic AnemiaharideepNo ratings yet
- Pengaruh Hemolisis Terhadap Nilai Trombosit Dengan Menggunakan Metode Direct CountingDocument6 pagesPengaruh Hemolisis Terhadap Nilai Trombosit Dengan Menggunakan Metode Direct CountingyudhaNo ratings yet
- Pre Analitica X 3 Libros Variabilidad BiologicaDocument20 pagesPre Analitica X 3 Libros Variabilidad BiologicaUlises Saldias RoaNo ratings yet
- CC 1 - Specimen CollectionDocument6 pagesCC 1 - Specimen CollectionRoy Anthony CenizaNo ratings yet
- ISE y Las InterferenciasDocument9 pagesISE y Las InterferenciasUlises Saldías RoaNo ratings yet
- Resealed ErythrocyteDocument50 pagesResealed ErythrocytebritorajNo ratings yet
- Understanding Transfusion Reactions in Oncology by NurseDocument6 pagesUnderstanding Transfusion Reactions in Oncology by NursefitriNo ratings yet
- Normocytic Normochromic AnemiaDocument18 pagesNormocytic Normochromic AnemiaElaizha PagulayanNo ratings yet