Professional Documents
Culture Documents
Retrograde Percutaneous Closure of A Ventricular Septal Defect
Retrograde Percutaneous Closure of A Ventricular Septal Defect
Uploaded by
Aída TreviñoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Retrograde Percutaneous Closure of A Ventricular Septal Defect
Retrograde Percutaneous Closure of A Ventricular Septal Defect
Uploaded by
Aída TreviñoCopyright:
Available Formats
2013 by the Texas Heart
Institute, Houston
Volume 40, Number 4, 2013 468 Retrograde Percutaneous VSD Closure
Retrograde Percutaneous
Closure of a Ventricular
Septal Defect
after Myectomy for Hypertrophic
Obstructive Cardiomyopathy
In patients with hypertrophic obstructive cardiomyopathy, hemodynamically significant
ventricular septal defect after septal myectomy is a rare sequela that warrants closure. Per-
cutaneous closure provides a safer alternative to repeated sternotomy, which is associated
with significant morbidity and mortality rates. We report a possibly unique case of suc-
cessful retrograde percutaneous closure, with an AMPLATZER Muscular VSD Occluder, of
an iatrogenic ventricular septal defect consequent to surgical therapy for hypertrophic ob-
structive cardiomyopathy. (Tex Heart Inst J 2013;40(4):468-71)
P
atients with hypertrophic obstructive cardiomyopathy (HOCM) are candi-
dates for surgical myectomy or ethanol ablation if, despite medical therapy,
they remain symptomatic with New York Heart Association functional class
III disease and severe left ventricular outflow tract (LVOT) gradients.
1
A rare sequela
of myectomy via the Morrow procedure is iatrogenic ventricular septal defect (VSD).
Although surgical closure remains the mainstay of treatment for most VSDs, treat-
ment of clinically significant postoperative residual VSDs remains a challenge. Per-
cutaneous closure provides a safer alternative to reoperation.
2,3
We report a possibly
unique case of successful retrograde percutaneous closure of an iatrogenic VSD, con-
sequent to surgical therapy for HOCM, by means of an AMPLATZER
Muscular VSD
Occluder (St. Jude Medical, Inc.; St. Paul, Minn).
Case Report
A 68-year-old woman presented at another medical center after experiencing a synco-
pal episode while walking. She had a history of hypertension, dyslipidemia, coronary
artery disease (including drug-eluting stent placement to the left circumflex coronary
artery), and medically managed HOCM. Evaluation revealed asymmetric left ventric-
ular (LV) hypertrophy with LVOT obstruction and moderate-to-severe mitral valve
regurgitation. The patient underwent a septal myectomy, bileaflet mechanical mitral
valve replacement, and tricuspid annuloplasty; however, soon after these procedures,
she developed progressively worsening dyspnea and bilateral leg edema. During the
next few weeks, she underwent multiple thoracenteses to relieve recurrent transuda-
tive pleural effusions. Two-dimensional (2D) echocardiograms, transesophageal echo-
cardiograms, and cardiac computed tomograms revealed a muscular VSD 0.7 cm in
size, associated with a significant left-to-right shunt. The patient was referred to our
facility for percutaneous closure of the VSD (Figs. 1 and 2A).
First Attempt
Using a Cook needle, we cannulated the left femoral vein and advanced a 10F intra-
cardiac echocardiographic catheter (SOUNDSTAR, Biosense-Webster Inc.; Dia-
mond Bar, Calif ) into the right atrium. We then cannulated the left femoral artery
and inserted a 7F sheath. Subsequently, we advanced a Judkins right 4 (JR4) diag-
nostic catheter into the LV. Using the guidance from the JR4 catheter, we advanced
a Wholey wire (Mallinckrodt Inc.; Hazelwood, Mo) from the LV to the right ventri-
cle (RV), through the VSD. Attempts to advance the wire through the tricuspid valve
into the right atrium were unsuccessful because of the presence of the annuloplasty
Case
Reports
Vikas Singh, MD
Apurva O. Badheka, MD
Syed S. Bokhari, MD
Eduard Ghersin, MD
Pedro Martinez Clark, MD
William W. ONeill, MD
Key words: Cardiac cath-
eterization/methods;
cardiomyopathy, hypertro-
phic/therapy; heart septal
defects, ventricular/ther-
apy; iatrogenic disease;
myectomy; postoperative
complications; prosthesis
implantation/methods;
septal occluder device;
ventricular septal defect
Drs. Singh and Badheka
contributed equally to this
manuscript.
From: Cardiovascular Divi-
sion, University of Miami
Hospital, Miller School of
Medicine, Miami, Florida
33136
Dr. ONeill is now at the
Center for Structural Heart
Disease, Henry Ford Hospi-
tal, Detroit, Michigan.
Address for reprints:
Vikas Singh, MD,
University of Miami
Hospital, 1400 NW 12th
Ave., Suite 1179,
Miami, FL 33136
E-mail:
vsingh@med.miami.edu
Texas Heart Institute Journal Retrograde Percutaneous VSD Closure 469
ring. The procedure was then aborted, and all guide-
wires and catheters were removed.
Second Attempt
After 48 hours, the patient was taken to the cardiac cath-
eterization laboratory again with the intent of closing
the VSD in a retrograde fashion, after the failed ante-
grade attempt. We obtained right radial artery access by
using an argon needle and advanced a 6F pigtail cath-
eter into the LV to perform a left ventriculogram. We
cannulated the right femoral artery and inserted a 7F
sheath. The JR4 catheter and the Wholey wire were
subsequently advanced into the LV and then through
the VSD to the RV. Simultaneous measurement of RV
and LV pressures showed the LV pressure to be 118
mmHg, with an end-diastolic pressure of 16 mmHg,
and the RV pressure to be 44 mmHg, with an end-dia-
stolic pressure of 16 mmHg. We then exchanged the 7F
arterial sheath for an 8F delivery sheath, which we ad-
vanced across the aortic valve into the LV, then through
the VSD into the RV. A 12-mm AMPLATZER VSD clo-
sure device was advanced and deployed under real-time
fluoroscopy and transthoracic echocardiography. Two-
dimensional echocardiography and repeat left ventric-
ulography confirmed that there was no residual VSD
(Figs. 2B and 3). We removed the sheath and achieved
Fig. 1 Electrocardiographic-gated multidetector computed
tomograms (4-chamber views) of the heart show a 0.7-cm ven-
tricular septal defect (VSD) (arrows) at the membranous sep-
tum during A) end-diastole and B) peak systole. A jet of dense
intravenous contrast medium (arrowheads), from the relatively
hyperdense left ventricular lumen through the VSD toward the
relatively hypodense right ventricular lumen, indicates a left-to-
right shunt.
Fig. 2 Two-dimensional color-flow Doppler echocardiograms
(4-chamber views) show A) a ventricular septal defect with large
left-to-right flow (arrow), and B) no flow between the left and
right ventricles after closure of the defect.
A
A
B
B
Volume 40, Number 4, 2013 470 Retrograde Percutaneous VSD Closure
hemostasis at the arteriotomy site with an 8F Angio-
Seal closure device (St. Jude Medical). A transradial
band was applied to the right radial site.
Discussion
Ventricular septal defect, a rare sequela of septal my-
ectomy, is reported in 1% of HOCM patients who
undergo this procedure.
4
The presence of a hemody-
namically significant VSD with left-to-right shunting
can result in LV volume overload with signs and symp-
toms of heart failure.
5
Closure of the VSD is needed
to prevent sequelae such as LV dysfunction, arrhyth-
mias, aortic regurgitation, recurrent endocarditis, and
pulmonary hypertension. Surgical closure of VSDs,
first performed in 1954, has long been considered the
gold-standard treatment. However, surgical closure that
involves cardiopulmonary bypass and sternotomy is as-
sociated with significant morbidity and mortality rates,
especially in adults who have undergone prior sternoto-
my.
6,7
Percutaneous device closure of congenital or iat-
rogenic VSDs has been performed since the late 1980s
with reasonable success in both pediatric and adult pop-
ulations.
3,8,9
The procedure is technically challenging
and can cause rhythm disturbances or damage the tri-
cuspid valve. Moreover, conduction tissue can run near
the edges of the VSD and be damaged by manipula-
tion of the device. This risk is of greater magnitude if
the VSD is located near the aortic or tricuspid valve, in
which case device placement can result in temporary or
permanent atrioventricular block.
2,3
Transcatheter clo-
sure of postoperative VSDs has been described chiefly
in patients who have had residual VSDs after primary
VSD closure. These cases are substantially distinct from
those involving VSD after myectomy for HOCM, in
which instances the defect is surrounded by relatively
thick myocardiumdepending on the amount of myo-
cardial tissue excised during surgery.
An extensive literature review revealed only 4 re-
ported cases of iatrogenic VSD after septal myectomy,
which were treated with a transcatheter technique.
3,9-11
However, in all these cases the occluder device was de-
livered antegrade via the femoral vein or internal jug-
ular vein. To our knowledge, ours is the first reported
case of a successful percutaneous VSD closure after
surgical therapy for HOCM wherein the AMPLATZER
occluder device was delivered retrograde through the
femoral artery. The presence of the annuloplasty ring
in the tricuspid valve made it diff icult to achieve an
arteriovenous loop or to advance the catheter in an an-
tegrade fashion. This report adds to the increasing ev-
idence of the AMPLATZER Muscular VSD Occluders
suitability for treatment of a postsurgical VSD after
septal myectomy in patients with HOCM. Salient fea-
tures of this case include a failed antegrade attempt at
closure of a septal myectomy VSD, use of radial access
for left ventriculography, and retrograde closure of the
defect.
References
1. Maron BJ, McKenna WJ, Danielson GK, Kappenberger LJ,
Kuhn HJ, Seidman CE, et al. American College of Cardiolo-
gy/European Society of Cardiology clinical expert consensus
document on hypertrophic cardiomyopathy. A report of the
American College of Cardiology Foundation Task Force on
Clinical Expert Consensus Documents and the European So-
ciety of Cardiology Committee for Practice Guidelines. J Am
Coll Cardiol 2003;42(9):1687-713.
2. Okubo M, Benson LN, Nykanen D, Azakie A, Van Arsdell
G, Coles J, Williams WG. Outcomes of intraoperative device
closure of muscular ventricular septal defects. Ann Thorac
Surg 2001;72(2):416-23.
3. Chessa M, Carminati M, Cao QL, Butera G, Giusti S, Bini
RM, Hijazi ZM. Transcatheter closure of congenital and ac-
quired muscular ventricular septal defects using the Am-
platzer device. J Invasive Cardiol 2002;14(6):322-7.
4. Schonbeck MH, Brunner-La Rocca HP, Vogt PR, Lachat
ML, Jenni R, Hess OM, Turina MI. Long-term follow-up in
hypertrophic obstructive cardiomyopathy after septal myecto-
my. Ann Thorac Surg 1998;65(5):1207-14.
5. Carminati M, Butera G, Chessa M, De Giovanni J, Fisher
G, Gewillig M, et al. Transcatheter closure of congenital ven-
tricular septal defects: results of the European Registry. Eur
Heart J 2007;28(19):2361-8.
6. Holzer R, Balzer D, Cao QL, Lock K, Hijazi ZM; Amplatzer
Muscular Ventricular Septal Defect Investigators. Device
closure of muscular ventricular septal defects using the Am-
platzer muscular ventricular septal defect occluder: immedi-
ate and mid-term results of a U.S. registry. J Am Coll Cardiol
2004;43(7):1257-63.
7. Rose EA. Off-pump coronary-artery bypass surgery. N Engl J
Med 2003;348(5):379-80.
8. Knauth AL, Lock JE, Perry SB, McElhinney DB, Gauvreau
K, Landzberg MJ, et al. Transcatheter device closure of con-
genital and postoperative residual ventricular septal defects.
Circulation 2004;110(5):501-7.
Fig. 3 Repeat left ventriculogram shows resolution of the ven-
tricular septal defect.
Texas Heart Institute Journal Retrograde Percutaneous VSD Closure 471
9. Al-Kashkari W, Balan P, Kavinsky CJ, Cao QL, Hijazi ZM.
Percutaneous device closure of congenital and iatrogenic ven-
tricular septal defects in adult patients. Catheter Cardiovasc
Interv 2011;77(2):260-7.
10. De Wolf D, Taeymans Y, Suys B, Matthys D, Van Nooten G.
Percutaneous closure of a ventricular septal defect after surgi-
cal treatment of hypertrophic cardiomyopathy. J Thorac Car-
diovasc Surg 2006;132(1):173-4.
11. Spies C, Ujivari F, Schraeder R. Transcatheter closure of a
ventricular septal defect following myectomy for hypertrophic
obstructive cardiomyopathy. Cardiology 2009;112(1):31-4.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5822)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- CVS ExaminationDocument10 pagesCVS ExaminationAhmedNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- ECG Clinical TeachingDocument21 pagesECG Clinical TeachingSumi SajiNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Defibrillation - E-Learning Quiz 1. Identify The RhythmDocument3 pagesDefibrillation - E-Learning Quiz 1. Identify The RhythmBalaji Chinnasami100% (1)
- Congenital Heart DiseaseDocument13 pagesCongenital Heart DiseaseRaja67% (9)
- Easy ECG GuideDocument17 pagesEasy ECG GuideDr.Chinmay Kulkarni83% (12)
- OS 213 B07 Auscultation and Demonstration of Heart Sounds PDFDocument4 pagesOS 213 B07 Auscultation and Demonstration of Heart Sounds PDFMigs Medina100% (1)
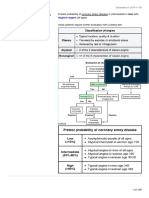
- Coronary Artery Disease:: Pathology & TreatmentDocument17 pagesCoronary Artery Disease:: Pathology & TreatmentJohn FisherNo ratings yet
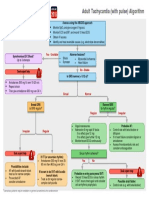
- G2015 Adult Tachycardia PDFDocument1 pageG2015 Adult Tachycardia PDFibbs91No ratings yet
- Introduction To ECG For NursingDocument75 pagesIntroduction To ECG For NursingRashid AlHamdan100% (1)
- A Guide To: Noob'SDocument103 pagesA Guide To: Noob'STeodorescu Claudia GabrielaNo ratings yet
- Atrioventricular Septal Defect: From Fetus To Adult: Congenital Heart DiseaseDocument7 pagesAtrioventricular Septal Defect: From Fetus To Adult: Congenital Heart Diseaseratna ardianaNo ratings yet
- ECG NotesDocument8 pagesECG NotesPeer TutorNo ratings yet
- Informe DEMO Del Holter de Arritmia Contec TLC9803Document14 pagesInforme DEMO Del Holter de Arritmia Contec TLC9803Edward MoralesNo ratings yet
- Zanki Step 2 - Cardiovascular SystemDocument129 pagesZanki Step 2 - Cardiovascular SystemChunlei WangNo ratings yet
- Susunan Acara Seminar ANGINA 2019Document2 pagesSusunan Acara Seminar ANGINA 2019Mellia Wida MasitaNo ratings yet
- (:875 (: "M FlyerDocument1 page(:875 (: "M FlyerFsNo ratings yet
- MEGACODEDocument6 pagesMEGACODESafety JNo ratings yet
- MCQ CardioDocument12 pagesMCQ CardioAhmed MahanaNo ratings yet
- Dopamine Drug StudyDocument3 pagesDopamine Drug StudyKwin Saludares100% (1)
- Cardiology STEMIDocument1 pageCardiology STEMIAishwarya WadikarNo ratings yet
- Lippincotts Antiarrhythmics 5Document1 pageLippincotts Antiarrhythmics 5Wijdan HatemNo ratings yet
- Vivi FrailDocument28 pagesVivi FrailCătălina Mihaela DascăluNo ratings yet
- High Quality CPR, DR Ali Haedar PDFDocument45 pagesHigh Quality CPR, DR Ali Haedar PDFTaufik SuhendarNo ratings yet
- Arrhythmia 6 YrDocument72 pagesArrhythmia 6 YrPiyush MalikNo ratings yet
- A Student'S Guide To The Interpretation of Ecgs: by Richard MckearneyDocument12 pagesA Student'S Guide To The Interpretation of Ecgs: by Richard MckearneyEba'a GamilNo ratings yet
- D S2 - Diastolic Murmur - S1 Ms - Mitral Stenosis Ts - Tricuspid Stenosis Ar - Aortic RegurgitationDocument7 pagesD S2 - Diastolic Murmur - S1 Ms - Mitral Stenosis Ts - Tricuspid Stenosis Ar - Aortic RegurgitationMiguel Cuevas DolotNo ratings yet
- Heart RhythmDocument68 pagesHeart RhythmMwanja MosesNo ratings yet
- Nursing Journal EcgDocument2 pagesNursing Journal EcgCharlene Jacobe CornistaNo ratings yet
- ECG Interpretation For Beginners Deel 1Document39 pagesECG Interpretation For Beginners Deel 1coffeerelatedthoughts 28No ratings yet
- Management of Perioperative Arrhythmias: PathogenesisDocument15 pagesManagement of Perioperative Arrhythmias: PathogenesisSudar Pecinta ParawaliNo ratings yet