Professional Documents
Culture Documents
04061
04061
Uploaded by
Evelyn Hermida Lama0 ratings0% found this document useful (0 votes)
23 views10 pagesAnemia is associated with an increased risk of mortality in both systolic and diastolic CHF. Of the 153,180 CHF patients, 37.2% were anemic. Lower baseline hemoglobin values were associated with increased crude mortality rates.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentAnemia is associated with an increased risk of mortality in both systolic and diastolic CHF. Of the 153,180 CHF patients, 37.2% were anemic. Lower baseline hemoglobin values were associated with increased crude mortality rates.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
23 views10 pages04061
04061
Uploaded by
Evelyn Hermida LamaAnemia is associated with an increased risk of mortality in both systolic and diastolic CHF. Of the 153,180 CHF patients, 37.2% were anemic. Lower baseline hemoglobin values were associated with increased crude mortality rates.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 10
Heart Failure
Anemia and Mortality in Heart Failure Patients
A Systematic Review and Meta-Analysis
Hessel F. Groenveld, MD,* James L. Januzzi, MD, FACC, Kevin Damman, MD,*
Jan van Wijngaarden, MD, PHD, Hans L. Hillege, MD, PHD,*
Dirk J. van Veldhuisen, MD, PHD, FACC,* Peter van der Meer, MD, PHD
Groningen and Deventer, the Netherlands; and Boston, Massachusetts
Objectives The aim of this study was to assess the effect of anemia on mortality in chronic heart failure (CHF).
Background Anemia is frequently observed in patients with CHF, and evidence suggests that anemia might be associated
with an increased mortality.
Methods A systematic literature search in MEDLINE (through November 2007) for English language articles was per-
formed. In addition, a manual search was performed. We included cohort studies and retrospective secondary
analyses of randomized controlled trials whose primary objective was to analyze the association between ane-
mia and mortality in CHF. Of a total of 1,327 initial studies, we included 34 studies, comprising 153,180 pa-
tients. Information on study design, patient characteristics, outcome, and potential confounders were extracted.
Results Anemia was dened by criteria used in the original articles. Of the 153,180 CHF patients, 37.2% were anemic.
After a minimal follow-up of 6 months, 46.8% of anemic patients died compared with 29.5% of nonanemic pa-
tients. Crude mortality risk of anemia was odds ratio 1.96 (95% condence interval: 1.74 to 2.21, p 0.001).
Lower baseline hemoglobin values were associated with increased crude mortality rates (r 0.396, p
0.025). Adjusted hazard ratios showed an increased adjusted risk for anemia (hazard ratio 1.46 [95% con-
dence interval: 1.26 to 1.69, p 0.001]). Subgroup analysis showed no signicant difference between mortality
risk of anemia in diastolic or systolic CHF.
Conclusions Anemia is associated with an increased risk of mortality in both systolic and diastolic CHF. Anemia should,
therefore, be considered as a useful prognosticator, and therapeutic strategies aimed to increase hemoglobin
levels in CHF should be investigated. (J Am Coll Cardiol 2008;52:81827) 2008 by the American College of
Cardiology Foundation
Anemia is frequently observed in patients with chronic heart
failure (CHF) (15). Prevalence of anemia depends both on
the severity of CHF and diagnostic criteria used to dene it,
but may be as high as 50% in selected patient cohorts (3,6). Of
note, anemia is not only prevalent in the CHF population, but
several studies in different patient populations found an asso-
ciation with anemia, impaired cardiac function, more health
care utilization, and morbidity (1,711). In addition, numerous
studies have assessed associations between anemia and mortal-
ity in CHF. Although most studies have documented higher
mortality rates in anemic CHF patients (1,3,1217), some
studies report the absence of an adverse effect of anemia on
mortality in CHF (4,1820). Therefore, better understanding
of the risk associated with the presence of anemia is necessary.
Elucidating the contribution of anemia to mortality may lead
to a more accurate risk proling in CHF patients, especially
since several treatment options for anemia exist including
erythropoietin (EPO) and iron therapy (21,22). Ultimately,
this may lead to more effective therapeutic strategies from a
risk-benet perspective in heart failure patients.
We, therefore, performed a rigorous systematic review
and meta-analysis of published literature to more compre-
hensively assess the effect of anemia on mortality in CHF.
In addition, we explored whether subgroups of anemic
patients were at particularly high mortality risk.
Methods
Search strategy. We adhered to the MOOSE (Meta-
analysis Of Observational Studies in Epidemiology) study
guidelines as previously published (23). To identify all relevant
From the *Department of Cardiology, University Medical Center Groningen,
Groningen, the Netherlands; Division of Cardiology, Department of Medicine,
Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts;
and the Department of Cardiology, Deventer Hospital, Deventer, the Netherlands.
Dr. Damman is supported by the Netherlands Heart Foundation (grant 2006B157).
Dr. van Veldhuisen is a Clinical Established Investigator of the Netherlands Heart
Foundation (D97-017). Dr. van der Meer is supported by the Dutch Scientic
Organization (Rubicon grant: 825-07-011).
Manuscript received February 19, 2008; revised manuscript received April 23,
2008, accepted April 28, 2008.
Journal of the American College of Cardiology Vol. 52, No. 10, 2008
2008 by the American College of Cardiology Foundation ISSN 0735-1097/08/$34.00
Published by Elsevier Inc. doi:10.1016/j.jacc.2008.04.061
Downloaded From: http://content.onlinejacc.org/ on 05/07/2014
studies, we performed a literature search in MEDLINE
accessed by PubMed (1966 throughNovember 2007). Two of the
authors (H.G. and P.v.d.M.) developed a search strategy. To
identify heart failure patients and anemia, we used both the
Medical Subject Heading term (MeSH) and text word search
(Table 1). In addition, we identied potentially relevant
studies using a manual search of references lists from all
eligible studies and review articles. We consulted experts in
the eld and searched the Institute for Scientic Informa-
tion Web of Sciences for publications that cited key
publications.
Study selection. We included cohort studies and retro-
spective secondary analyses of randomized controlled trials
whose primary objective was to analyze the association
between anemia and mortality in CHF. Titles and abstracts
of all articles were evaluated and rejected on initial screen if
they: 1) included subjects other than CHF patients; 2) had
no evaluation of hemoglobin (Hb) or hematocrit (Ht) levels;
3) did not include all-cause mortality as outcome; 4) were
published only in abstract form; 5) included patients 18
years old; 6) had follow-up of 6 months; or 7) were
published in another language than English.
After obtaining full reports of candidate studies, the same
reviewers independently assessed eligibility. Differences in
data between the 2 reviewers were solved by rereviewing
corresponding articles, and the nal set was agreed on by
consensus. For studies in which not all data were published,
or data was insufcient, authors were addressed and asked
for additional information (3,4,12,19,2426).
Quality assessment and data abstraction. Each study was
evaluated on quality according to the guidelines provided by
the United States Preventive Task Force (27) and published
recommendations (28). The following characteristics were
assessed: 1) duration of follow-up 12 months; 2) reporting
loss of follow-up; 3) adjustment of possible confounders in
multivariate analysis; 4) denition of anemia; 5) full speci-
cation of outcome; 6) study sample representative for
mentioned population; 7) full specication of clinical and
demographic variables; 8) explanation of sample selection;
9) temporality (Hb measured at baseline, not at time of
outcomes assessment); and 10) clear inclusion and exclusion
criteria. Studies were graded as poor quality if they met 5
criterion, fair if they met 5 to 7
criteria, and good if they met 8
criteria.
Statistical analysis. Random
effects meta-analysis was con-
ducted to estimate the magni-
tude of risk associated with ane-
mia and all-cause mortality, as
measured by crude mortality
risks and unadjusted odds ratios
(ORs). Where available, adjusted
hazard ratios (HRs) were ex-
tracted from Cox regression
analysis. Adjusted risk estimates
included those components as
published in nal multivariate
models for each study including confounding sociodemo-
graphic and clinical covariates. We performed tests of
heterogeneity between studies using a standard chi-square
test and I
2
statistic. When heterogeneity was found to be
signicant, pooled estimates based on random effects mod-
els were reported. To examine sources of heterogeneity, we
conducted meta-regression analysis. Bias in published stud-
ies was assessed using a funnel plot of study results against
study precision. We tested symmetry of the funnel plot by
the Eggers test. Subgroup analysis was pre-dened for
systolic versus diastolic CHF. Statistical signicance was set
at p 0.05, and all statistical analyses were performed using
Stata 9.0 (Stata Corp., College Station, Texas).
Results
Description of included studies. The electronic search
retrieved 1,327 eligible studies. Nonelectrical search identi-
ed 4 additional studies. On initial screening, 1,142 were
rejected, based on title. Of the 185 screened abstracts, 56
studies were retrieved for detailed evaluation. Eventually 34
studies were included in this meta-analysis (Fig. 1). Sec-
ondary analysis of the Val-HeFT (Valsartan Heart Failure
Trial) study was described in 2 separate manuscripts: Anand
et al. (29) and Maggioni et al. (5). Crude mortality data
were not published by Anand et al. (29), and for this reason
this study was excluded and the data of Maggioni et al. (5)
was used. In addition, 1 article described the effect of
anemia from 2 different studies (5). Both studies in this
published report were analyzed separately for the meta-
analysis. The 34 included studies described a total of
153,180 patients (1,320,2426,3041). Characteristics of
the included studies are listed in Table 2, characteristics of
study populations are listed in Online Tables 1 and 2. Ten
different denitions of anemia were used in the included
studies. The World Health Organization (WHO) deni-
tion (Hb 13.0 g/dl for males and Hb 12.0 g/dl for
females) was used in the majority of the studies. Table 3
displays the different denitions of anemia in the included
studies. Anemia, as dened in the original articles, was
Terms Used in the Search Query
Table 1 Terms Used in the Search Query
Text words
Congestive heart failure, CHF, anemia, anaemia, hemoglobin, haemoglobin,
Hb, Hgb, hematocrit, haematocrit, Ht, Hct
MeSH terms
Heart failure, congestive; anemia; hemoglobin; hematocrit
Title and abstract search
Hemoglobins
Limits
English language
CHF congestive heart failure; MeSH Medical Subject Heading.
Abbreviations
and Acronyms
CHF chronic heart failure
CI condence interval
EPO erythropoietin
ESP erythropoiesis-
stimulating protein
Hb hemoglobin
HR hazard ratio
Ht hematocrit
OR odds ratio
WHO World Health
Organization
819 JACC Vol. 52, No. 10, 2008 Groenveld et al.
September 2, 2008:81827 Anemia and Mortality in Heart Failure
Downloaded From: http://content.onlinejacc.org/ on 05/07/2014
present in 37.2% of the CHF patients. Mean Hb from the
studies ranged from 12.2 to 14.0 g/dl. Mean Ht values
ranged from 36.6% to 42.7%.
Meta-analysis ndings. Among the 34 studies, mean
follow-up ranged from a minimum of 6 months to a
maximum of 5 years. Crude mortality data were available in
33 studies. In one study, only the adjusted HR was available,
whereas the unpublished crude mortality data were lost after
hurricane Katrina (25). Analysis of the crude mortality
revealed that 26,687 (46.8%) anemic patients died com-
pared with 28,274 (29.5%) nonanemic patients. This trans-
lated into an unadjusted mortality risk of OR 1.96 (95%
condence interval [CI]: 1.74 to 2.21, p 0.001) in anemic
CHF patients compared with that in nonanemic CHF
patients (Fig. 2). When the 2 largest studies (Go et al. [3]
and Kosiborod et al. [4]) were excluded, the mortality risk of
anemia was identical (OR: 1.95, 95% CI: 1.78 to 2.14, p
0.001). There was no evidence for publication bias. The
funnel plot did not show asymmetry (Fig. 3), which was
conrmed by the Eggers test (p 0.93). We found a
signicant heterogeneity between included studies (I
2
92.4%, p 0.001). Meta-regression analysis was performed
using sociodemographic variables, medical history, drug use,
and laboratory data as parameters. In this sensitivity analy-
sis, excluding studies not adhering to the WHO denition
of anemia, no heterogeneity was observed (I
2
36.5%, p
NS), yet the mortality risk remained (OR: 2.22, 95% CI:
2.04 to 2.42, p 0.001). In addition, we found an inverse
interstudy relationship between serum creatinine levels and
the effect of anemia on mortality. The effect of anemia on
mortality declined with higher serum creatinine levels.
When assessing the gradual effect of baseline Hb values on
mortality, we found a linear trend between baseline Hb
measurements and mortality rates. Lower baseline Hb
values were associated with increased annual mortality rates
(r 0.396, p 0.025) (Fig. 4).
Confouding factors. In 127,437 patients (83.1% of the
total included patients), reported mortality risks were ad-
justed for several sociodemographic and clinical covariates.
Potential confounders that were adjusted for in the original
reports are shown in Table 4. In all but one study, age and
renal function were considered as potential confounders
(this study included 178 patients) (33). When mortality risk,
estimated by adjusted HR, was combined, anemia remained
an independent predictor of mortality HR 1.46 (95% CI:
1.26 to 1.69, p 0.001).
Subgroup analysis. In the subgroup analysis, we assessed
the difference between mortality risk of anemia in patients
with systolic or diastolic CHF. Table 5 displays the deni-
tions of systolic and diastolic CHF used in the original
articles. Studies or substudies in patients with only diastolic
CHF included 20,924 patients of which 5,957 (28.5%)
patients died. In studies or substudies including only pa-
tients with systolic CHF, 40,025 patients were included, of
which 12,423 (31.0%) died. The mortality risk associated
with the presence of anemia was not signicantly different
between patients with systolic CHF (OR: 1.96, 95% CI:
1.70 to 2.25, p 0.001) and diastolic CHF (OR: 2.09, 95%
CI: 1.53 to 2.86, p 0.001).
Discussion
This is the rst meta-analysis to address the relationship
between anemia and mortality in patients with CHF. In our
analysis, which examined more than 150,000 subjects,
anemia was frequently observed, found in over one-third of
CHF patients. Presence of anemia in CHF patients is
associated with an increased mortality risk in patients with
systolic as well as diastolic heart failure. The adverse effect
we found is substantial and signicant. When assessing the
mortality risk by using multivariate analyses, anemia re-
mains an independent risk factor for mortality in CHF
patients.
Prevalence. In prior studies, it is observed that CHF is
often accompanied by anemia. A wide range of anemia
prevalence in CHF has been reported, ranging from 7% to
Figure 1 Flow Chart for Study Selection
CHF chronic heart failure; Hb hemoglobin.
820 Groenveld et al. JACC Vol. 52, No. 10, 2008
Anemia and Mortality in Heart Failure September 2, 2008:81827
Downloaded From: http://content.onlinejacc.org/ on 05/07/2014
Study Characteristics
Table 2 Study Characteristics
Author (Ref. #), Year Follow-Up n Patients End Points Major Exclusion Criteria Study Design Study
Al-Ahmad et al. (12), 2001 33.4 months 6,360 CHF, LVEF 35%,
age 21 to 81 yrs
Mortality Recent MI, unstable angina,
sCR 2.5 mg/dl
Secondary analysis of
clinical trial
(SOLVD)
Good
Horwich et al. (9), 2002 5 yrs 1,061 Referred for heart
transplantation
evaluation
Mortality LVEF 40%, NYHA class
III, no initial Hb, dry
weight, or adequate
follow-up
Retrospective,
observational,
single-center
cohort study
Good
McClellan et al. (38), 2002 2 yrs 633 Discharge diagnosis
of HF (ICD-9-CM)
Mortality Dialysis, death during
index hospitalization,
missing records
Retrospective,
observational,
multicenter cohort
study
Good
Tanner et al. (32), 2002 6 months 193 Outpatient HF clinic at
university hospital
Mortality, heart
transplantation
Secondary anemia,
hemodialysis,
coronary intervention
last 3 months
Retrospective,
observational,
single-center
cohort study
Good
Kalra et al. (26), 2003 3 yrs 531 HF Mortality Prospective
observational,
single-center
cohort study
Fair
Kosiborod et al. (39), 2003 1 yr 2,281 Principal discharge
diagnosis of HF
(ICD-9-CM),
age 65 yrs
Mortality,
hospitalization
Severe AoS or MiS, HF due
to acute illness, missing
Htc values, in-hospital
mortality
Retrospective,
observational,
multicenter chart
review
Good
Mozaffarian et al. (37), 2003 15 months 1,130 LVEF 30% and
NYHA class IIIB or
IV HF symptoms
Mortality MI; unstable angina; stroke
or revascularization;
severe pulmonary,
renal, or hepatic disease,
sCR 3.0 mg/dl
Secondary analysis of
multicenter clinical
trial (PRAISE)
Good
Kerzner et al. (40), 2003 25 months 367 Primary discharge
diagnosis of HF
Mortality Retrospective,
observational,
single-center chart
review
Fair
Szachniewicz et al. (33), 2003 529 days 176 Admitted for HF Mortality Anemia due to known
secondary cause
Prospective,
observational,
single-center,
cohort study
Good
Sharma et al. (34), 2004 551 days 3,044 NYHA II to IV,
LVEF 40%,
age 60 yrs
Mortality Severe valvular disease,
recent PTCA, CABG,
MI, or unstable angina,
sCR 220 mol/l
Secondary analysis of
multicenter clinical
trial (ELITE II)
Good
Anand et al. (1), 2004 12.7 months 912 NYHA II to IV,
LVEF 30%,
age 18 to 55 yrs
Mortality,
hospitalization
Surgically correctable
causes of HF, other
serious illness, recent or
planned revascularization
Secondary analysis of
clinical trial
(RENAISSANCE)
Good
van der Meer et al. (30), 2004 1,100 days 74 Mild-to-severe CHF Mortality MI, CVA, severe renal
failure, valvular disease,
isolated systolic
dysfunction
Retrospective,
observational,
single-center
cohort study
Good
Ezekowitz et al. (24), 2005 962 days 791 Referred for
assessment and
management
of CHF
Mortality Missing Hb values Prospective
observational,
single-center
cohort study
Good
Maggioni et al. (5), Val-HeFT
2005
23 months 5,010 Symptomatic HF
(NYHA II),
clinically stable
Mortality, time to
death, rst
morbid event
Rapidly deteriorating HF,
acute MI, CAD likely to
require intervention,
unstable angina, recent
CVA, sCR 2.5 mg/dl
Secondary analysis of
a randomized
clinical trial
(Val-HeFT)
Good
Maggioni et al. (5), IN-CHF
2005
1 yr 2,411 Diagnosis of HF
according to
European Society
of Cardiology
Mortality Retrospective,
observational,
multicenter cohort
study
Good
Gardner et al. (19), 2005 554 days 182 Advance HF, referred
for cardiac Tx
assessment
Mortality Age 16 yrs, pregnancy,
known malignancy
Prospective,
observational,
single-center cohort
study
Fair
Continued on next page
821 JACC Vol. 52, No. 10, 2008 Groenveld et al.
September 2, 2008:81827 Anemia and Mortality in Heart Failure
Downloaded From: http://content.onlinejacc.org/ on 05/07/2014
Continued
Table 2 Continued
Author (Ref. #), Year Follow-Up n Patients End Points Major Exclusion Criteria Study Design Study
Rosolova et al. (35), 2005 4 yrs 508 Suspected HF Mortality Retrospective,
observational,
multicenter cohort
study
Fair
Grigorian et al. (14), 2006 1.5 yrs 205 Admitted to tertiary
center for CHF
Mortality LVEF 50% Retrospective,
observational,
Single-center
cohort study
Good
Kosiborod et al. (4), 2005 1 yr 50,405 Discharge diagnosis
of HF
Mortality,
hospitalization
for HF
Patients without documented
HF on admission, age
65 yrs, hemodialysis,
severe Aos, MiS,
Retrospective,
observational,
multicenter cohort
study
Good
Ralli et al. (16), 2005 1 yr 264 Referred to a
university hospital
for HF
management or
heart Tx
Mortality ACS or myocarditis,
LVEF 40%
Retrospective,
observational,
single-center
cohort study
Good
OMeara et al. (36), 2006 37.7 months 2,653 Symptomatic (NYHA II
to IV) HF, for at
least 4 weeks,
age 18 yrs
Mortality sCR 265 mol/l,
symptomatic HT, MI, CVA
Secondary analysis of
clinical trial
(CHARM)
Good
Felker et al. (13), 2006 3.6 yrs 4,951 Symptomatic HF
(NYHA II) patients
undergoing cardiac
catheterization
Mortality Primary valvular heart
disease or congenital
heart disease
Retrospective,
observational,
single-center
cohort study
Fair
Terrovitis et al. (31), 2006 2 yrs 160 Symptomatic HF
(NYHA II to IV),
LVEF 35%
Mortality Recent MI or CABG,
unstable angina,
anticipated cardiac
surgery, sCR 3 mg/dl
Secondary analysis of
multicenter,
prospective clinical
trial
Good
Hebert et al. (25), 2006 436 days 410 LVEF 40%, enrolled
in chronic HF
disease
managemant
program
Mortality Missing baseline values
of Hb, sCR
Retrospective,
observational,
single-center
cohort study
Fair
Formiga et al. (18), 2006 1 yr 103 Admitted for
symptomatic,
previously
unknown HF
Mortality,
hospitalization
for HF
Chronic advanced disease,
COPD, advanced renal
failure hemodialysis,
in-hospital mortality
Prospective,
observational,
single-center
cohort study
Good
Newton and Squire (15), 2006 1,257 days 528 Discharge diagnosis of
HF, without previous
hospitalization for
HF
Mortality Insufcient evidence of new
diagnosis of CHF
Retrospective,
observational,
single-center chart
review
Good
Komajda et al. (10), 2006 58 months 2,996 NYHA class II to IV
and LVEF 35%
Mortality,
hospitalization
Recent change of
treatment, requirement
of IV medication
Secondary analysis of
clinical trial
(COMET)
Good
Go et al. (3), 2006 2 yrs 59,772 Diagnosed with CHF Mortality,
hospitalization
Retrospective
observational,
longitudinal cohort
study
Good
Berry et al. (7), 2006 814 days 519 Diagnosed with CHF
or a treatment
for CHF
Mortality,
hospitalization,
HF
hospitalization
Primary or secondary
diagnosis of acute MI
Retrospective,
observational,
single-center chart
review
Fair
de Silva et al. (42), 2006 531 days 955 LVEF 45%, CHF
enrolled in a
community-based
program
Mortality Pregnancy, dialysis,
disorders resulting in
anemia
Prospective,
observational,
single-center
cohort study
Fair
Maraldi et al. (11), 2006 12 months 567 Diagnosed with HF,
age 65 yrs
Mortality,
physical
disability
Physical disability at
hospital discharge,
dementia, or severe
cognitive impairment
Secondary analysis of
longitudinal
observational study
Fair
Elabbassi et al. (8), 2006 1.3 yrs 437 Systolic or diastolic
CHF
Mortality,
hospitalization,
ED visit
No complete follow-up Prospective
observational,
single-center
cohort study
Good
Continued on next page
822 Groenveld et al. JACC Vol. 52, No. 10, 2008
Anemia and Mortality in Heart Failure September 2, 2008:81827
Downloaded From: http://content.onlinejacc.org/ on 05/07/2014
over 50% (14,10,17,32,35). This range can be attributed to
multiple factors, including the use of multiple denitions of
anemia. The WHO criteria was used in the majority of
studies. In addition, administrational codes or arbitrary
boundary values to dene anemia were also used. Studies
dening anemia with administrative codes (such as Inter-
national Classication of Diseases, 9th Revision, codes)
have clear limitations. The use of this coding system solely
relies on physicians to consider anemia as a possible
diagnosis leading to an underestimation of the preva-
lence. Therefore, we excluded in this meta-analysis stud-
ies without measurements of actual Hb or Ht values. This
resulted in the exclusion of only one study (2). Results of
the current meta-analysis clearly indicate the need for
standardized denitions of anemia in CHF patients. The
denition of anemia appeared to be a major source of
heterogeneity. However, despite different denitions of
anemia in the present meta-analysis, the association with
mortality was robust, using different analysis strategies.
Pathophysiology. It is tempting to speculate about the
mechanisms behind the increased mortality risk observed in
anemic CHF patients. Anemia may lead to an increased
work load, resulting from an increased heart rate and stroke
volume (32,42,43). In response to the increased workload,
the heart undergoes remodeling, marked by left ventricu-
lar hypertrophy and dilation. This eventually may lead to
CHF with an increased mortality risk. Also, renal failure, as
a common comorbidity in CHF, might be implicated in the
pathophysiology. CHF and renal failure are 2 entities that
are often seen together with prevalences ranging from 20%
to 40% (2,38,4446). With meta-regression analysis, we
found an inverse interstudy relationship between serum
creatinine levels and the effect of anemia on mortality.
However, this result does not suggest that the mortality risk
declines with higher creatinine levels. It merely illustrates a
statistical decreasing effect of anemia on mortality with
increasing creatinine levels; the decline of the effect of
anemia on mortality can be the result of an increased
Denitions of Anemia Used in the Original Articles
Table 3 Denitions of Anemia Used in the Original Articles
Denition of Anemia Author (Ref. #)
WHO Elabbassi et al. (8), Maraldi et al. (11), De Silva et al. (42), Go et al. (3), Komajda
et al. (10), Formiga et al. (18), Hebert et al. (25), OMeara et al. (36), Felker et
al. (13), Ralli et al. (16), Grigorian Shamagian et al. (14), Rosolova et al. (35),
Gardner et al. (19), Ezekowitz et al. (24), van der Meer et al. (30), Kerzner et
al. (40), Mozaffarian et al. (37), Schou et al. (17)
Hb 11.5 g/dl Kalra et al. (26)
Hb 12.0 g/dl Varadarajan et al. (6), Anand et al. (1), Szachniewicz et al. (33), Tanner et al. (32)
Hb 12.3 g/dl Horwich et al. (9)
Hb 13.0 g/dl Sharma et al. (34)
Hb 11.0 g/dl in women Maggioni et al. (Val-HeFT) (5), Maggioni et al. (IN-CHF) (5)
and Hb 12.0 g/dl in men
Hb 11.5 g/dl in women Berry et al. (7), Newton and Squire (15)
and 13.0 g/dl in men
Ht 35% Al-Ahmad et al. (12)
Ht 37% Kosiborod et al. 2003 (39), McClellan et al. (38)
Ht 37% Terrovitis et al. (31)
Ht 37% in women and
40% in men
Kosiborod et al. 2005 (4)
Ht hematocrit; WHO World Health Organization denition of anemia, Hb 12.0 g/dl in women, 13.0 in men; other abbreviations as in Table 2.
Continued
Table 2 Continued
Author (Ref. #), Year Follow-Up n Patients End Points Major Exclusion Criteria Study Design Study
Varadarajan et al. (6), 2006 5 yrs 2,246 Primary discharge of
diagnosis of CHF
Mortality,
hospitalization,
ED visit
CHF excluded with
Framingham criteria,
no ECG
Retrospective,
observational,
single-center,
chart review
Good
Schou et al. (17), 2007 30 months 345 Systolic HF
(LVEF 45%)
Mortality Prospective,
observational,
single-center
cohort study
Good
ACS acute coronary syndromes; AoS aortic valve stenosis; CABG coronary arterial bypass graft surgery; CAD coronary artery disease; CHARM Candesartan in Heart Failure trial; CHF chronic
heart failure; COMET Carvedilol Or Metoprolol European Trial; COPD chronic obstructive pulmonary disease; CVA cerebral vascular accident; ECG electrocardiogram; ED emergency department;
ELITE II Losartan Heart Failure Survival Study; F/U follow-up; Hb hemoglobin; HF heart failure; HT hypertension; Htc hematocrit; ICD-9-CM International Classication of Diseases, 9th
Revision, Clinical Modication; IN-CHF Italian NetworkCongestive Heart Failure trial; IV intravenous; LVEF left ventricular ejection fraction; MI myocardial infarction; MiS mitral valve stenosis;
NYHA New York Heart Association functional class; PRAISE Prospective Randomized Amlopidine Survival Evaluation trial; PTCA percutaneous transluminal coronary angioplasty; RENAISSANCE
Randomized Etanercept North American Strategy to Study Antagonism of Cytokines; sCR serum creatinine; Tx heart transplantation; Val-HeFT Valsartan Heart Failure Trial.
823 JACC Vol. 52, No. 10, 2008 Groenveld et al.
September 2, 2008:81827 Anemia and Mortality in Heart Failure
Downloaded From: http://content.onlinejacc.org/ on 05/07/2014
mortality risk caused by renal failure (47). From a patho-
physiological standpoint, CHF can also cause renal failure
due to a decreased cardiac output reducing renal perfusion
(i.e., forward failure); subsequent renal failure may lead to
decreased endogenous EPO levels and may ultimately
induce anemia, leading to an increased cardiac workload
completing the vicious circle. Recently this has been called
the cardio-renal-anemia syndrome (48).
Findings from intervention studies. Considering the in-
creased mortality risk caused by anemia, in heart failure as
well as renal failure, trials have been designed in which
patients receive erythropoiesis-stimulating proteins (ESPs)
to increase Hb levels. The rst intervention study to address
the efcacy of EPO in CHF patients was performed by
Silverberg et al. (49) in 32 patients. Correction of anemia
with EPO and intravenous iron led to a signicant increase
in left ventricular ejection fraction and decrease in New
York Heart Association functional class, which was re-
ected by almost 90% reduction in the number of hospital-
Figure 2 Risk of All-Cause Mortality of Anemic Versus Nonanemic CHF Patients
CHF chronic heart failure. CI condence interval.
Figure 3 Funnel Plot for Publication Bias
OR odds ratio.
824 Groenveld et al. JACC Vol. 52, No. 10, 2008
Anemia and Mortality in Heart Failure September 2, 2008:81827
Downloaded From: http://content.onlinejacc.org/ on 05/07/2014
izations. A similar study showed that EPO treatment
signicantly increased peak oxygen consumption and exer-
cise duration in patients with moderate-to-severe CHF
(50). Recently, 2 substantially larger multicenter phase II
studies evaluated the effects of darbepoetin (a long-acting
ESP) on surrogate cardiovascular end points (51,52). Treat-
ment with darbepoetin was safe and effectively raised Hb.
Moreover, it signicantly improved clinical status; however,
no signicant improvement in exercise tolerance could be
observed.
However, recently several studies showed a potentially
harmful effect of ESP treatment in patients with kidney
disease and malignancies. A meta-analysis in patients with
cancer-associated anemia showed an increased risk in ve-
nous thromboembolism and mortality associated with re-
combinant EPO and darbepoetin administration (53). Fur-
thermore, concerns about the cardiovascular safety of ESP
in patients with kidney disease have been raised. Two
separate studies showed that patients targeted to a higher
Hb level had an increased incidence of cardiovascular events
(54,55). However, in these studies, no placebo groups were
included. These studies were all performed in patients with
severe renal failure, and only a minority of patients suffered
from heart failure. Consequently, the results of the studies
mentioned in the preceding text cannot be extrapolated to
the CHF population.
Larger randomized studies are clearly needed to deter-
mine the impact on morbidity and mortality in CHF.
Currently, a large phase III morbidity and mortality trial,
the RED-HF (Reduction of Events with Darbepoetin
alfa in Heart Failure) trial (56), is being conducted to
answer the question whether the use of ESPs in anemic
heart failure patients is benecial. Besides ESP, intrave-
nous iron treatment is another intervention modality in
anemic CHF patients. Recently, 2 trials appeared show-
Figure 4
Relationship Between Baseline
Hemoglobin and Annual Mortality
The area of each circle is proportional to the sample size in each cohort. The cen-
ter line shows the estimated mortality risk per year of lower baseline Hb values on
a continuous scale. The dotted lines represent the 95% condence intervals.
Potential Confounders of Included Studies
Table 4 Potential Confounders of Included Studies
Author (Ref. #) Number of Patients Age Gender Renal Function
Severity of
Heart Failure Medical History Medication
Elabbassi et al. (8) 437
Maraldi et al. (11) 567
Berry et al. (7) 519
Newton and Squire (15) 528
Hebert et al. (25) 410
Felker et al. (13) 4,951
Kosiborod et al. (4) 50,405
Maggioni-V et al. (5) 5,010
Maggioni-I et al. (5) 2,411
van der Meer et al. (30) 74
Szachniewicz et al. (33) 176
Mozaffarian et al. (37) 1,130
Go et al. (3) 59,772
Kalra et al. (26) 531
Schou et al. (17) 345
Denitions of Systolic and Diastolic HF Used in the Original Articles
Table 5
Denitions of Systolic and
Diastolic HF Used in the Original Articles
LVEF (%)
Systolic CHF
Mozaffarian et al. (37), Anand et al. (1) 30
Komajda et al. (10), Terrovitis et al. (31) 35
Sharma et al. (34), Ralli et al. (16), Maggioni et al. (5),
Kerzner et al. (40), Kosiborod et al. (4), OMeara et al. (36),
Felker et al. (13)
40
Schou et al. (17) 45
Diastolic CHF
Kerzner et al. (40), Kosiborod et al. (4), OMeara et al. (36),
Felker et al. (13)
40
Grigorian Shamagian et al. (14) 50
Abbreviations as in Table 2.
825 JACC Vol. 52, No. 10, 2008 Groenveld et al.
September 2, 2008:81827 Anemia and Mortality in Heart Failure
Downloaded From: http://content.onlinejacc.org/ on 05/07/2014
ing that intravenous iron without ESPs increased Hb
levels in patients with CHF. Moreover, they showed an
improved exercise capacity and decreased NT-proBNP
levels (57,58). Further research is needed to study the
effect of intravenous iron on morbidity and mortality in
anemic CHF patients.
Study limitations. Limitations of meta-analyses include
differences in designs and populations used in included
trials, quality of studies, and heterogeneity (59). However,
the quality of all studies was graded according to published
guidelines and all met at least 7 of 12 criteria.
Evaluation of anemia was only at baseline in all
included studies. Tang et al. (60) recently reported a
study with serial hemoglobin measurements and showed
that persistent anemia has a larger effect on mortality
than transient anemia. No evaluation of Hb was per-
formed during the studies; thus, it remains unknown
whether anemia in the included studies was persistent or
transient. Furthermore, heterogeneity in our study is
substantial and can be attributed to differences in dura-
tion of follow-up, type of patients included, study design,
and denition of anemia. Denition of anemia was a
major cause of heterogeneity. When mortality risk was
assessed using studies that dened anemia by WHO
criteria, heterogeneity was no longer signicant, while
the increased mortality risk caused by anemia remained.
Furthermore, our meta-analysis could not exclude resid-
ual confounding from studies in the adjusted analyses,
although most studies adjusted for many known major
confounders. However, this limitation emphasizes the
inability of our analysis to prove causality.
Previously, it has been argued that a larger meta-analysis
(e.g., 1,000 events) is clinically more meaningful (59); our
study, which includes over 50,000 events, is therefore of
particular note. Besides the overall size, the individual
studies in the present analysis were of considerable size, with
14 including more than 1,000 patients. These strengths
make our ndings all the more rm.
Conclusions
Anemia is present in one-third of the CHF population
and is an independent risk prognosticator for mortality in
subjects so affected, irrespective of a systolic versus
diastolic etiology of CHF. Further research is needed to
assess the effect of correcting anemia in CHF patients.
Reprint requests and correspondence: Dr. Peter van der Meer,
Cardiovascular Research Center, Massachusetts General Hospital,
Charles River Plaza, 185 Cambridge Street, Boston, Massachu-
setts 02114. E-mail: pvandermeer@partners.org.
REFERENCES
1. Anand I, McMurray JJ, Whitmore J, et al. Anemia and its relationship
to clinical outcome in heart failure. Circulation 2004;110:14954.
2. Ezekowitz JA, McAlister FA, Armstrong PW. Anemia is common in
heart failure and is associated with poor outcomes: insights from a
cohort of 12 065 patients with new-onset heart failure. Circulation
2003;107:2235.
3. Go AS, Yang J, Ackerson LM, et al. Hemoglobin level, chronic kidney
disease, and the risks of death and hospitalization in adults with
chronic heart failure: the Anemia in Chronic Heart Failure: Outcomes
and Resource Utilization (ANCHOR) study. Circulation 2006;113:
271323.
4. Kosiborod M, Curtis JP, Wang Y, et al. Anemia and outcomes in
patients with heart failure: a study from the National Heart Care
Project. Arch Intern Med 2005;165:223744.
5. Maggioni AP, Opasich C, Anand I, et al. Anemia in patients with
heart failure: prevalence and prognostic role in a controlled trial and in
clinical practice. J Card Fail 2005;11:918.
6. Varadarajan P, Gandhi S, Sharma S, Umakanthan B, Pai RG.
Prognostic signicance of hemoglobin level in patients with congestive
heart failure and normal ejection fraction. Clin Cardiol 2006;29:
4449.
7. Berry C, Norrie J, Hogg K, Brett M, Stevenson K, McMurray JJ. The
prevalence, nature, and importance of hematologic abnormalities in
heart failure. Am Heart J 2006;151:131321.
8. Elabbassi W, Fraser M, Williams K, Cassan D, Haddad H. Prevalence
and clinical implications of anemia in congestive heart failure patients
followed at a specialized heart function clinic. Congest Heart Fail
2006;12:25864.
9. Horwich TB, Fonarow GC, Hamilton MA, MacLellan WR, Boren-
stein J. Anemia is associated with worse symptoms, greater impairment
in functional capacity and a signicant increase in mortality in patients
with advanced heart failure. J Am Coll Cardiol 2002;39:17806.
10. Komajda M, Anker SD, Charlesworth A, et al. The impact of new
onset anaemia on morbidity and mortality in chronic heart failure:
results from COMET. Eur Heart J 2006;27:14406.
11. Maraldi C, Volpato S, Cesari M, et al. Anemia, physical disability, and
survival in older patients with heart failure. J Card Fail 2006;12:5339.
12. Al-Ahmad A, Rand WM, Manjunath G, et al. Reduced kidney
function and anemia as risk factors for mortality in patients with left
ventricular dysfunction. J Am Coll Cardiol 2001;38:95562.
13. Felker GM, Shaw LK, Stough WG, OConnor CM. Anemia in
patients with heart failure and preserved systolic function. Am Heart J
2006;151:45762.
14. Grigorian Shamagian L, Varela RA, Garcia-Acuna JM, Mazon RP,
Virgos LA, Gonzalez-Juanatey JR. Anaemia is associated with higher
mortality among patients with heart failure with preserved systolic
function. Heart 2006;92:7804.
15. Newton JD, Squire IB. Glucose and haemoglobin in the assessment of
prognosis after rst hospitalisation for heart failure. Heart 2006;92:
14416.
16. Ralli S, Horwich TB, Fonarow GC. Relationship between anemia,
cardiac troponin I, and B-type natriuretic peptide levels and mortality
in patients with advanced heart failure. Am Heart J 2005;150:12207.
17. Schou M, Gustafsson F, Kistorp CN, Corell P, Kjaer A, Hildebrandt
PR. Prognostic usefulness of anemia and N-terminal pro-brain natri-
uretic peptide in outpatients with systolic heart failure. Am J Cardiol
2007;100:15716.
18. Formiga F, Chivite D, Castaner O, Manito N, Ramon JM, Pujol R.
Anemia in new-onset congestive heart failure inpatients admitted for
acute decompensation. Eur J Intern Med 2006;17:17984.
19. Gardner RS, Chong KS, Morton JJ, McDonagh TA. N-terminal
brain natriuretic peptide, but not anemia, is a powerful predictor of
mortality in advanced heart failure. J Card Fail 2005;11:S4753.
20. Silva RP, Barbosa PH, Kimura OS, et al. Prevalance of anemia and its
association with cardio-renal syndrome. Int J Cardiol 2007;120:2326.
21. van der Meer P, Voors AA, Lipsic E, van Gilst WH, van Veldhuisen
DJ. Erythropoietin in cardiovascular diseases. Eur Heart J 2004;25:
28591.
22. van Veldhuisen DJ, McMurray JJ. Are erythropoietin stimulating
proteins safe and efcacious in heart failure? Why we need an
adequately powered randomised outcome trial. Eur J Heart Fail
2007;9:1102.
23. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observa-
tional studies in epidemiology: a proposal for reporting. Meta-analysis
Of Observational Studies in Epidemiology (MOOSE) group. JAMA
2000;283:200812.
826 Groenveld et al. JACC Vol. 52, No. 10, 2008
Anemia and Mortality in Heart Failure September 2, 2008:81827
Downloaded From: http://content.onlinejacc.org/ on 05/07/2014
24. Ezekowitz JA, McAlister FA, Armstrong PW. The interaction among
sex, hemoglobin and outcomes in a specialty heart failure clinic. Can
J Cardiol 2005;21:16571.
25. Hebert K, Horswell R, Arcement L, Hare J, Stevenson L. The effect
of anemia on mortality in indigent patients with mild-to-moderate
chronic heart failure. Congest Heart Fail 2006;12:759.
26. Kalra PR, Collier T, Cowie MR, et al. Haemoglobin concentration
and prognosis in new cases of heart failure. Lancet 2003;362:2112.
27. Harris RP, Helfand M, Woolf SH, et al. Current methods of the US
Preventive Services Task Force: a review of the process. Am J Prev
Med 2001;20:2135.
28. Altman DG. Systematic reviews of evaluations of prognostic variables.
BMJ 2001;323:2248.
29. Anand IS, Kuskowski MA, Rector TS, et al. Anemia and change in
hemoglobin over time related to mortality and morbidity in patients
with chronic heart failure: results from Val-HeFT. Circulation 2005;
112:11217.
30. van der Meer P, Voors AA, Lipsic E, Smilde TD, van Gilst WH, van
Veldhuisen DJ. Prognostic value of plasma erythropoietin on mortality
in patients with chronic heart failure. J Am Coll Cardiol 2004;44:
637.
31. Terrovitis JV, Anastasiou-Nana MI, Alexopoulos GP, et al. Preva-
lence and prognostic signicance of anemia in patients with congestive
heart failure treated with standard vs high doses of enalapril. J Heart
Lung Transplant 2006;25:3338.
32. Tanner H, Moschovitis G, Kuster GM, et al. The prevalence of
anemia in chronic heart failure. Int J Cardiol 2002;86:11521.
33. Szachniewicz J, Petruk-Kowalczyk J, Majda J, et al. Anaemia is an
independent predictor of poor outcome in patients with chronic heart
failure. Int J Cardiol 2003;90:3038.
34. Sharma R, Francis DP, Pitt B, Poole-Wilson PA, Coats AJ, Anker
SD. Haemoglobin predicts survival in patients with chronic heart
failure: a substudy of the ELITE II trial. Eur Heart J 2004;25:10218.
35. Rosolova H, Cech J, Simon J, et al. Short to long term mortality of
patients hospitalised with heart failure in the Czech Republica
report from the EuroHeart Failure Survey. Eur J Heart Fail 2005;7:
7803.
36. OMeara E, Clayton T, McEntegart MB, et al. Clinical correlates and
consequences of anemia in a broad spectrum of patients with heart
failure: results of the Candesartan in Heart Failure: Assessment of
Reduction in Mortality and Morbidity (CHARM) program. Circula-
tion 2006;113:98694.
37. Mozaffarian D, Nye R, Levy WC. Anemia predicts mortality in severe
heart failure: the prospective randomized amlodipine survival evalua-
tion (PRAISE). J Am Coll Cardiol 2003;41:19339.
38. McClellan WM, Flanders WD, Langston RD, Jurkovitz C, Presley
R. Anemia and renal insufciency are independent risk factors for
death among patients with congestive heart failure admitted to
community hospitals: a population-based study. J Am Soc Nephrol
2002;13:192836.
39. Kosiborod M, Smith GL, Radford MJ, Foody JM, Krumholz HM.
The prognostic importance of anemia in patients with heart failure.
Am J Med 2003;114:1129.
40. Kerzner R, Gage BF, Freedland KE, Rich MW. Predictors of
mortality in younger and older patients with heart failure and preserved
or reduced left ventricular ejection fraction. Am Heart J 2003;146:
28690.
41. de Silva R, Rigby AS, Witte KK, et al. Anemia, renal dysfunction, and
their interaction in patients with chronic heart failure. Am J Cardiol
2006;98:3918.
42. Akhter MW, Aronson D, Bitar F, et al. Effect of elevated admission
serum creatinine and its worsening on outcome in hospitalized patients
with decompensated heart failure. Am J Cardiol 2004;94:95760.
43. Varat MA, Adolph RJ, Fowler NO. Cardiovascular effects of anemia.
Am Heart J 1972;83:41526.
44. Dries DL, Exner DV, Domanski MJ, Greenberg B, Stevenson LW.
The prognostic implications of renal insufciency in asymptomatic and
symptomatic patients with left ventricular systolic dysfunction. J Am
Coll Cardiol 2000;35:6819.
45. Foley RN. Myocardial disease, anemia, and erythrocyte-stimulating
proteins in chronic kidney disease. Rev Cardiovasc Med 2005;6 Suppl
3:S2734.
46. Ruilope LM, van Veldhuisen DJ, Ritz E, Luscher TF. Renal function:
the Cinderella of cardiovascular risk prole. J Am Coll Cardiol
2001;38:17827.
47. Smith GL, Lichtman JH, Bracken MB, et al. Renal impairment and
outcomes in heart failure: systematic review and meta-analysis. J Am
Coll Cardiol 2006;47:198796.
48. Silverberg DS, Wexler D, Iaina A. The importance of anemia and its
correction in the management of severe congestive heart failure. Eur
J Heart Fail 2002;4:6816.
49. Silverberg DS, Wexler D, Sheps D, et al. The effect of correction of
mild anemia in severe, resistant congestive heart failure using subcu-
taneous erythropoietin and intravenous iron: a randomized controlled
study. J Am Coll Cardiol 2001;37:177580.
50. Palazzuoli A, Silverberg D, Iovine F, et al. Erythropoietin improves
anemia exercise tolerance and renal function and reduces B-type
natriuretic peptide and hospitalization in patients with heart failure
and anemia. Am Heart J 2006;152:1096115.
51. van Veldhuisen DJ, Dickstein K, Cohen-Solal A, et al. Randomized,
double-blind, placebo-controlled study to evaluate the effect of two
dosing regimens of darbepoetin alfa in patients with heart failure and
anaemia. Eur Heart J 2007;28:220816.
52. Ghali JK, Anand IS, Abraham WT, et al. Randomized double-blind
trial of darbepoetin alfa in patients with symptomatic heart failure and
anemia. Circulation 2008;117:52635.
53. Bennett CL, Silver SM, Djulbegovic B, et al. Venous thromboembo-
lism and mortality associated with recombinant erythropoietin and
darbepoetin administration for the treatment of cancer-associated
anemia. JAMA 2008;299:91424.
54. Drueke TB, Locatelli F, Clyne N, et al. Normalization of hemoglobin
level in patients with chronic kidney disease and anemia. N Engl
J Med 2006;355:207184.
55. Singh AK, Szczech L, Tang KL, et al. Correction of anemia with
epoetin alfa in chronic kidney disease. N Engl J Med 2006;355:
208598.
56. Young JB, Anand IS, Diaz R, et al. Reduction of events with
darbepoetin alfa in Heart Failure (RED-HF) trial (abstr). J Card Fail
2006;12 Suppl 1:S77.
57. Okonko DO, Grzeslo A, Witkowski T, et al. Effect of intravenous
iron sucrose on exercise tolerance in anemic and nonanemic patients
with symptomatic chronic heart failure and iron deciency FERRIC-
HF: a randomized, controlled, observer-blinded trial. J Am Coll
Cardiol 2008;51:10312.
58. Toblli JE, Lombrana A, Duarte P, Di GF. Intravenous iron reduces
NT-pro-brain natriuretic peptide in anemic patients with chronic
heart failure and renal insufciency. J Am Coll Cardiol 2007;50:
165765.
59. Flather MD, Farkouh ME, Pogue JM, Yusuf S. Strengths and
limitations of meta-analysis: larger studies may be more reliable.
Control Clin Trials 1997;18:56879.
60. Tang WH, Tong W, Jain A, Francis GS, Harris CM, Young JB.
Evaluation and long-term prognosis of new-onset, transient, and
persistent anemia in ambulatory patients with chronic heart failure.
J Am Coll Cardiol 2008;51:56976.
Key Words: heart failure y anemia y prognosis.
APPENDIX
For the Acknowledgments and supplementary Tables 1 and 2, please see
the online version of this article.
827 JACC Vol. 52, No. 10, 2008 Groenveld et al.
September 2, 2008:81827 Anemia and Mortality in Heart Failure
Downloaded From: http://content.onlinejacc.org/ on 05/07/2014
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Blank MoaDocument3 pagesBlank MoaGary Arlene Yalung0% (1)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Lesson Plan On Placenta PraeviaDocument14 pagesLesson Plan On Placenta PraeviaSanthu Su67% (6)
- 1490823659-Ch. 4 GA Story BibleDocument19 pages1490823659-Ch. 4 GA Story BibleKorry ShepardNo ratings yet
- ThedaCare Medical Center-Shawano Grand OpeningDocument44 pagesThedaCare Medical Center-Shawano Grand OpeningWolfRiverMediaNo ratings yet
- Physiology Summary Chapter 20Document9 pagesPhysiology Summary Chapter 20gail01850% (2)
- Beyond The Breech Trial. Maggie BanksDocument4 pagesBeyond The Breech Trial. Maggie Bankspurpleanvil100% (2)
- Teerthanker Mahaveer College of Nursing: SubjectDocument9 pagesTeerthanker Mahaveer College of Nursing: SubjectPrasann RoyNo ratings yet
- Republic of The PhilippinesDocument3 pagesRepublic of The Philippinesnhoj eca yabujNo ratings yet
- Chronic Pain Assessment QuestionnaireDocument2 pagesChronic Pain Assessment QuestionnaireHosam Mahmoud100% (1)
- Fabrication of Occlusal RimsDocument4 pagesFabrication of Occlusal RimsHarsha Reddy100% (1)
- Tatz Pa ToolDocument23 pagesTatz Pa Toolian_mendoza_3No ratings yet
- OBN Approver Website 02-2013Document2 pagesOBN Approver Website 02-2013James LindonNo ratings yet
- Cross-Sectional Tomography: Oral and Maxillofacial RadiologyDocument7 pagesCross-Sectional Tomography: Oral and Maxillofacial RadiologyPhanQuangHuyNo ratings yet
- PLANNINGDocument4 pagesPLANNINGAnonymous hYMWbANo ratings yet
- Syllabus DraftDocument7 pagesSyllabus Draftapi-440514424No ratings yet
- Carrie Fisher-Bipolar 1-PaperDocument5 pagesCarrie Fisher-Bipolar 1-Paperapi-487208181No ratings yet
- Examination of The Shoulder The Complete Guide PDFDocument2 pagesExamination of The Shoulder The Complete Guide PDFJasmine0% (2)
- 31-10-19, Mrs. SY, 33 Y.O. Fraktur Blow Out+Fraktur Maxilla Le Fort I+Fr. Nasal. Dr. Saktrio D Subarno, Sp. BP-REDocument28 pages31-10-19, Mrs. SY, 33 Y.O. Fraktur Blow Out+Fraktur Maxilla Le Fort I+Fr. Nasal. Dr. Saktrio D Subarno, Sp. BP-REanon_893244902No ratings yet
- Schiller At-102 - Service HandbookDocument140 pagesSchiller At-102 - Service HandbookpabloNo ratings yet
- Inflammatory Bowel Disease: What Is IBD?Document6 pagesInflammatory Bowel Disease: What Is IBD?Raluca ChisuNo ratings yet
- Ob Rapid Response Team Plan1Document20 pagesOb Rapid Response Team Plan1api-255697457100% (1)
- Fitness Choices and First Aid Study NotesDocument11 pagesFitness Choices and First Aid Study NotesAlan VanNo ratings yet
- CEBM Levels of EvidenceDocument2 pagesCEBM Levels of Evidence2012100% (2)
- 032 Orm or Scrub Major Case FormDocument1 page032 Orm or Scrub Major Case FormDana Marie LeanoNo ratings yet
- Chronic Periodontitis: DR Jebin, Mds.,D.IcoiDocument34 pagesChronic Periodontitis: DR Jebin, Mds.,D.IcoiAndra PorimeNo ratings yet
- Barium MealDocument12 pagesBarium Mealbagasaditya480No ratings yet
- Medical Requirement: Director General DirectivesDocument33 pagesMedical Requirement: Director General DirectivesChiu ChernNo ratings yet
- Neonatal SepsisDocument18 pagesNeonatal SepsisMoe KebabNo ratings yet
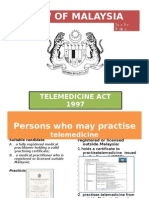
- Law of Malaysia TelemedicineDocument18 pagesLaw of Malaysia TelemedicineDefoe2008No ratings yet
- JainamDocument20 pagesJainamSpandan KadamNo ratings yet