Professional Documents
Culture Documents
Hematology. 1
Hematology. 1
Uploaded by
Krismas Eka SaputraOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hematology. 1
Hematology. 1
Uploaded by
Krismas Eka SaputraCopyright:
Available Formats
online April 13, 2007
originally published doi:10.1182/blood-2006-09-018655
2007110: 1411-1419
George L. Chen and Josef T. Prchal
X-linked clonality testing: interpretation and limitations
http://bloodjournal.hematologylibrary.org/content/110/5/1411.full.html
Updated information and services can be found at:
(58 articles) Reviews in Translational Hematology
(3208 articles) Hematopoiesis and Stem Cells
Articles on similar topics can be found in the following Blood collections
http://bloodjournal.hematologylibrary.org/site/misc/rights.xhtml#repub_requests
Information about reproducing this article in parts or in its entirety may be found online at:
http://bloodjournal.hematologylibrary.org/site/misc/rights.xhtml#reprints
Information about ordering reprints may be found online at:
http://bloodjournal.hematologylibrary.org/site/subscriptions/index.xhtml
Information about subscriptions and ASH membership may be found online at:
Copyright 2011 by The American Society of Hematology; all rights reserved.
of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036.
Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society
For personal use only. on April 2, 2014. by guest bloodjournal.hematologylibrary.org From For personal use only. on April 2, 2014. by guest bloodjournal.hematologylibrary.org From
Review in translational hematology
X-linked clonality testing: interpretation and limitations
George L. Chen
1
and Josef T. Prchal
2
1
Division of Blood and Marrow Transplant, Department of Medicine, Stanford University School of Medicine, Palo Alto, CA;
2
Division of Hematology,
Department of Medicine, University of Utah School of Medicine, Salt Lake City
Clonality often denes the diseased state
in hematology. Clonal cells are geneti-
cally homogenous and derived from the
same precursor; their detection is based
on genotype or phenotype. Genotypic
clonality relies on somatic mutations to
mark the clonal population. Phenotypic
clonality identies the clonal popula-
tion by the expression pattern of surro-
gate genes that track the clonal pro-
cess. The most commonly used
phenotypic clonality methods are based
on the X-chromosome inactivation prin-
ciple. Clonality detection based on X-
chromosome inactivation patterns (XCIP)
requires discrimination of the active from
the inactive X chromosome and differen-
tiation of each X chromosomes parental
origin. Detection methods are based on
detection of X-chromosome sequence
polymorphisms identied by protein iso-
forms, transcribed mRNA, and methyl-
ation status. Errors in interpreting clonal-
ity tests arise from stochastic, genetic,
and cell selection pressures on the
mechanismof X inactivation. Progressive
X-chromosome skewing has recently
been suggested by XCIP clonality studies
in aging hematopoietic cells. This has led
to new insights into the pathophysiology
of X-linked and autoimmune disorders.
Other research applications include com-
bining XCIP clonality testing with genetic
clonality testing to identify clonal popula-
tions with yet-to-be-discovered genetic
changes. (Blood. 2007;110:1411-1419)
2007 by The American Society of Hematology
Introduction
Clonality studies have played an instrumental role in medicine and
hematology. They have been used to establish the single origin of
tumors and to differentiate nonmalignant from malignant states.
1
Most importantly, they have been used to elucidate the hematopoi-
etic hierarchy.
2,3
Much confusion exists, however, regarding the
application and interpretation of clonality studies. We discuss
clonality testing in general, emphasizing X-chromosome inactiva-
tion pattern (XCIP)based assays and the pitfalls in their interpreta-
tion. We also discuss new research applications of clonality testing.
Denition of clonality
For cells to be clonal means that they are derived from a single
precursor that has undergone a somatic mutation. Clonality is a
description of lineage as well as homogeneity of the tested tissue.
These aspects of clonality can be seen in the acquisition of
cytogenetic abnormalities on leukemic transformation in myelo-
brosis with myeloid metaplasia.
4
Of 28 patients with serial
karyotype analysis performed at the time of myelobrosis with
myeloid metaplasia diagnosis and leukemic transformation, 26 dem-
onstrated clonal evolution. Eleven of 26 had evolution of an
existing clone with additional cytogenetic abnormalities, whereas
15 of 26 with a normal karyotype acquired one or more cytogenetic
abnormalities. Here, a single clonal population could be dened by
the rst cytogenetic change, whereas a second clonal population
could be dened by the additional cytogenetic changes in 11 of
26 patients. These later cells would still have the original clonality
marker shared with the original clone, but they would also
represent a genetically distinct second clonal population evolving
from the original chromosomal aberration (Figure 1).
Clonality detection
Clonality detection requires a way to mark cells that is retained
generation after generation, enabling lineage to be traced by
following the marker back to a single progenitor. Cells can be
marked by genotype or phenotype (Table 1). In genotypic clonality,
an aberrant genetic sequence marks the cell and its progeny. The
aberrant sequence is usually related to the disease either as its cause
or as a lineage marker of the original precursor that has undergone
the disease causing somatic mutation. Examples of genetic clonal-
ity markers include the 9q:22q-translocation/BCR-ABL fusion in
chronic myelogenous leukemia and immunoglobulin or T-cell
receptor gene rearrangements in lymphoid malignancies.
5,6
The
aberrant sequences used for marking are somatic mutations,
simplifying the methodology for detection and differentiation of
the disease clone from normal, nonmutated cells.
The multitude of lymphoma and leukemia markers using T-cell
receptor/immunoglobulin gene rearrangements and chromosomal
translocations illustrates the clinical use of genetic clonality
markers. However, clonal cell populations without the tested-for
genetic markers exist and will not be detected. For detection of
clonal populations that do not have known genetic markers,
detection of clonality by phenotypic assays is necessary. It is not
that genetic changes do not underlie these clonal processes, but
rather because the specic mutation is not known, clonality testing
will need to depend on those surrogate markers whose expressions
are incidentally altered by or track the clonal process.
In contrast to genotypic clonality, which identies cells using
somatic mutations, phenotypic clonality identies cells using
changes in the expression pattern of housekeeping genes. These
genes are not mutated from their germline sequences but are
differentially expressed. Phenotypic clonality can be assayed by
Submitted September 1, 2006; accepted March 21, 2007. Prepublished online as
Blood First Edition paper, April 13, 2007; DOI 10.1182/blood-2006-09-018655.
2007 by The American Society of Hematology
1411 BLOOD, 1 SEPTEMBER 2007
VOLUME 110, NUMBER 5
For personal use only. on April 2, 2014. by guest bloodjournal.hematologylibrary.org From
performing ow cytometry for abnormally expressed antigens or
by using XCIP-based techniques to detect the loss of heterozygous
allele expression. The application of ow cytometry to clonality
detection is discussed in the following paragraphs. XCIP-based
assays are discussed in X chromosome inactivation and the
subsections that follow.
In ow cytometry, clonal populations are identied by the
constellation of antigens expressed by the cell. These antigens can
demonstrate aberrant lineage, asynchronous expression, or overex-
pression. Aberrant light scattering properties can also be used to
identify clonal populations.
Flow cytometry has been applied to the detection of residual
clonal populations after treatment (minimal residual disease [MRD])
for acute myelogenous leukemia (AML) and acute lymphoblastic
leukemia (ALL). In AML, immunophenotyping can detect clonal
populations with a sensitivity as small as one leukemic cell diluted
10
4
to 10
5
times (similar to the sensitivity for polymerase chain
reaction [PCR]).
7
The presence of such populations has been linked
to clinically relevant relapses, although the actual cutoffs vary with
the clinical study.
7,8
Clonality markers, genotypic or phenotypic, are surrogates for
clonal processes and must be differentiated from the actual clonal
processes. The absence of a clonality marker does not equate to the
absence of a clonal population. Clonal evolution frequently occurs
in acute lymphoblastic leukemia with concomitant surface antigen
shifts.
9
In the process, previously detected immunophenotypes may
become undetectable, suggesting a loss of clonality when in fact a
clonal population still exists, either changed by another clonal
somatic event or arising from a previously existent but undetected
subclone resulting in a false-negative interpretation. A similar
situation arises when PCR-based genetic markers are used.
10
False-negative interpretations of MRD can be avoided by following
multiple clonality markers so that if one is lost, another can still
track the clonal population.
The context of minimal residual clonal population detection
affects the interpretation. Whether these small populations result in
clinically relevant outcomes depends on the disease. In promyelo-
cytic leukemia, detection of a small residual population by reverse
Figure 1. X-chromosome inactivation and clonal development with further
subclone evolution. (A) Clonal populations can acquire multiple genetic abnormali-
ties; each can be used to distinguish subpopulations which remain clonal. Round
white Xp, nonclonal cell with active paternal X chromosome; round gray Xp, clonal
cell with active paternal X chromosome; oval dark gray Xp
, clonal cell with active
paternal X chromosome and new somatic mutation. (B) X-chromosome inactivation.
Early in development, both X chromosomes are expressed. Before hematopoietic
lineage differentiation, either X chromosome is inactivated. This random choice of
inactivated X chromosome is retained through subsequent mitoses. Oval XpXm
indicates early embryonic cells expressing both maternal and paternal X chromo-
somes; round Xp or Xm, nonclonal cells expressing a single X chromosome.
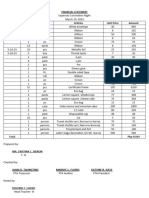
Table 1. Methods of clonality detection
Marker Detection method Clinical application Research application
Genotypic
Disease-associated somatic
mutation
PCR; cytogenetics Differentiation of clonal from reactive polyclonal
processes; diagnosis and subtyping of
leukemia and lymphoma; MRD monitoring in
acute leukemia
Demonstration of clonal processes,
lineage, clonal evolution
Immunoglobulin
rearrangement
PCR Differentiation of clonal from reactive polyclonal
processes; demonstration of clonality,
lineage, and differentiation of B-cell
lymphoma/leukemia; MRD monitoring in
B-cell lymphoma/leukemia
Demonstration of B-cell clonality,
lineage, differentiation
T-cellreceptor
rearrangement
PCR Demonstration of clonality, lineage, and
differentiation of T-cell lymphoma/leukemia;
MRD monitoring in T-cell lymphoma/
leukemia
Demonstration of T-cell clonality,
lineage, differentiation
Phenotypic
Immunophenotype Flow cytometry Diagnosis of malignancy; determination of
clonality, lineage; differentiation of leukemias/
lymphomas; MRD monitoring in acute
leukemias
Demonstration of clonality, lineage,
clonal evolution
X-chromosome inactivation
pattern
Protein isoform detection by electrophoretic
mobility*; methylation of X-chromosome
polymorphic region; transcription-based
assays
Differentiation of clonal from reactive polyclonal
processes
Demonstration of clonality, lineage;
elucidation of the hematopoietic
hierarchy; possible identication
of premalignant disease phases;
facilitation of demonstration of
subclonal development from
unrelated somatic processes
*Limited to females of African origin.
Majority of females informative but inuenced by environmental factors.
Several polymorphic loci need to be screened, better differentiation of active from inactive X chromosome.
1412 CHEN and PRCHAL BLOOD, 1 SEPTEMBER 2007
VOLUME 110, NUMBER 5
For personal use only. on April 2, 2014. by guest bloodjournal.hematologylibrary.org From
transcription PCR for the normalized quotient of promyelocytic
leukemiaretinoic acid receptor (PML-RAR) mRNA/glyceralde-
hyde-3-phosphate dehydrogenase (GAPDH) mRNA predicts a
7.6-fold increase in relative risk for disease recurrence if greater
than 10
6
and a 17.5-fold increase in relative risk if greater than
10
5
. At less than 10
6
, relative risk for relapse was 0.18.
11
In
contrast, small residual populations in t(8;21) AMLmay exist for as
long as 8 years without clinical relapse.
12
Similar observations have
been reported for acute lymphoblastic leukemia in which molecu-
larly detected residual leukemic clones in bone marrow did not
result in clinical relapse for as long as 9 years.
13
These instances of
clinically insignicant MRD may be attributable to eradication of
more aggressive subclones with persistence of premalignant
clones, differences in disease biology, or to control of the clones by
immunologic or other homeostatic mechanisms.
The timing of MRD also affects interpretation. In chronic
myelogenous leukemia, MRD detected by qualitative reverse
transcriptase-PCR of BCR-ABL less than 6 months after transplan-
tation is not predictive for relapse. If detected 6 to 12 months after
transplantation, PCR-positive MRD is associated with a 26-fold
increase in relative risk for relapse.
14
Progressive immune reconsti-
tution after transplantation may make early positive results less
signicant, and the use of qualitative 2-step nested PCR to amplify
BCR-ABL transcripts may introduce variance in the level detected.
Indeed, if a quantitative reverse transcriptase-PCRdetection method
is used, then an early positive result within 3 to 5 months of
transplantation coupled with increasing transcript numbers is
predictive of relapse.
15,16
In summary, interpretation of MRD must
consider the disease, timing, and detection method.
The remainder of this article deals with clonality assays based
on X-chromosome inactivation patterns. These assays can be
classied as phenotypic assays because the change in expression of
an X-linked gene is used as the marker of cell origin rather than
disease-causing or disease-related genetic changes. We also discuss
the methodologies and pitfalls in XCIP interpretation. The relation-
ship between genotypic detection of clonality, phenotypic detection
of clonality, and the discovery of disease-causing genes is dis-
cussed in Integrating genotypic and phenotypic clonality detection.
X-chromosome inactivation
During early female embryonic development, one of the X chromo-
somes (or more accurately, most of the genes on that X chromo-
some) is inactivated in each cell. The subsequent progeny of each
cell maintain the same inactivated X chromosome, resulting in an
organism that is a mosaic of cells expressing genes from one
X chromosome or the other (Figure 1).
Historical background
Modern clonality testing originated in the X-chromosome inactiva-
tion (XCI) hypothesis of Ernest Beutler.
17
This hypothesis postu-
lated that females inactivate one X chromosome to maintain dosage
parity with the single X chromosome in males (dosage compensa-
tion).
18
At approximately the same time, Mary Lyon separately
proposed XCI as a mechanism for X-linked coat color variation in
mice.
19
Seminal observations providing background for the XCI
hypothesis came from Ohno, Hauschka, and Makino who demon-
strated, rst in mice and then in humans, that Barr bodies did not
consist of portions of 2 X chromosomes in opposition to each other.
Rather, each Barr body was a single X chromosome.
20,21
This, with
the additional insight that differential chromosome use could result
in differential genetic function, led Beutler and Lyon to indepen-
dently dene the XCI phenomenon.
Mary Lyon proposed that the single Barr body X chromosome
came randomly from either parent rather than always the father and
that it was genetically inactivated. She based her hypothesis on
observations of X-linked coat color mutations in heterozygous
female mice. In these mice, the phenotype was always a mosaic
consisting of patches of normal or mutant color rather than a
homogenous blending, suggesting that early in development, the
pigmented cells inactivated one or the other X chromosome. Thus,
if the X chromosome carrying the mutant allele was inactivated, the
patch was of normal color, whereas if the X chromosome carrying
the normal allele was inactivated, the patch was of mutant color.
19
Beutler and colleagues formulated the XCI hypothesis using
studies of the human X chromosome gene glucose 6-phosphate
dehydrogenase (G6PD).
18
They found that, in females, G6PD
activity was not twice that of males and postulated a dosage
compensation mechanism. In females heterozygous for G6PD
deciency, dosage compensation results in G6PD expression at half
the rate of normal hemizygous males. This could be attributable to
either half-level activity in all cells or normal expression in some
cells and low expression in other cells, resulting in overall
half-level expression. Using a mixture of male cells with decient
G6PD activity and normal G6PD activity, Beutler and colleagues
measured G6PD activity (by glutathione stability) and compared it
with the response of female erythrocytes. They found that the
response curves of the 2 samples were similar in shape and
concluded that intermediate activity in females was probably
attributable to the same mechanism as in the mixture of male
normal and G6PD activity-decient erythrocytes. Synthesizing
these data on X-chromosome dosage compensation with Ohnos
cytogenetic data led to the concept of random XCI. Beutler and
colleagues later directly demonstrated that cells in an obligate
G6PD-decient heterozygous female were a mixture of erythro-
cytes with either normal or decient G6PD function.
Mechanism of X-chromosome inactivation
The exact molecular mechanisms behind XCI are still not fully
claried but involve several steps, including the determination of
the number of X chromosomes per cell, selection of either the
paternal or maternal X chromosome for subsequent inactivation,
and initiation of the actual inactivating process. It has been
demonstrated in mice that there are 3 noncoding loci located near
the X chromosome X center of inactivation (XCI) that play a
pivotal role in the mechanism of X-chromosome inactivation.
These loci are X (inactive)-specic transcript (Xist), its antisense
partner Tsix, and the intergenic locus Xite.
22-25
Xist is necessary for
cis inactivation of the X chromosome.
26,27
In cell culture systems,
autosomally translocated Xist silences the surrounding chromatin,
albeit incompletely.
28
Tsix and Xite work in parallel to Xist by
maintaining X-chromosome transcriptional competence.
23,24,29,30
Although the functions of these 3 loci have been deduced using
complementary cell lines, the actual physical interactions of these
components are less well known. Xist is proposed to achieve cis
inactivation of the X chromosome through close interactions
between its RNA transcript and the segment of X chromosome to
be inactivated.
31
The putative trans interactions based on the need
to determine one X to be exclusively activated and the other X to be
X-LINKED CLONALITYTESTING 1413 BLOOD, 1 SEPTEMBER 2007
VOLUME 110, NUMBER 5
For personal use only. on April 2, 2014. by guest bloodjournal.hematologylibrary.org From
exclusively inactivated remained problematic until recent experi-
ments demonstrated that the 2 X chromosomes undergo interchro-
mosomal pairing.
32,33
This is remarkable in that such interchromo-
somal pairings typically occur in germ cells undergoing meiosis
rather than somatic cells undergoing mitosis.
X-chromosome inactivation timing is crucial to the interpreta-
tion of XCIP-based clonality assays. It has been assumed that
preblastocyst embryos express both X chromosomes and that
inactivation did not occur until after implantation and the embry-
onic stem cells began to differentiate into separate cell lineages.
34
Recent experiments, however, demonstrate that XCI occurs as
early as the 4-cell stage of the embryo but is variable and leaky and
does not become xed until after implantation but before differen-
tiation of embryonic stem cells into the various cell lineages.
35,36
XCI before cell lineage differentiation is crucial for the interpreta-
tion of XCIP clonality studies. Hematopoietic cell lines derive not
from a single embryonic stem cell but from several progenitors,
allowing for the mosaic expression of genes from both
X chromosomes.
37,38
X-chromosome inactivationbased
clonality studies
In normal human females, the hematopoietic organ is a mosaic of
2 populations. Each population expresses alleles from one of the
active X chromosomes and the choice of which X chromosome to
use is retained mitosis after mitosis. Cell lineage can be traced and
subpopulation clonality can be determined by following the
activated X chromosome. X chromosome protein products, tran-
scribed mRNA, and DNAmethylation status are used to determine
which X chromosome is active. Protein isoforms and DNA
sequence polymorphisms are used to identify the X chromosomes.
These markers must be heterozygous to differentiate between the
maternal or paternal origin of the X chromosome. Thus, XCIP
clonality assays are limited to females with informative markers.
The rst clonality studies using X-chromosome inactivation
were based on G6PD isoenzymes (Figure 2).
17
In the African
population, there are 3 main G6PD isoenzymes: G6PD A
and A
polymorphic variants with faster electrophoretic mobility than
wild-type G6PD B. Approximately 35% of black women are
heterozygous for the electrophoretically distinguishable isoen-
zymes. The use of G6PD as a marker of X-chromosome inactiva-
tion is limited to females who are heterozygous for these G6PD
alleles. Informative females have the A
or A
allele on one
chromosome and the wild B allele on the other.
A natural progression from using protein isoforms to identify
the active X chromosome and its parental origin is to directly assay
the transcribed mRNA products of the active X chromosome
(Figure 2). The parental origin of the activated X chromosome is
identied by DNAsequence polymorphisms. This method was rst
described by Ernest Beutlers laboratory and independently with a
modied methodology in our laboratory.
39,40
The exonic polymor-
phisms used to identify the Xchromosome are typically nonsynony-
mous mutations. A variety of genes are used to determine clonal
status, including G6PD
40
(using a polymorphism different from
that used in protein-based clonality assays), iduronate-2-sulfa-
tase,
41,42
MPP1 (also known as p55),
43
Bruton tyrosine kinase, and
FHL-1 (4.5 LIM domain 1).
44
In aggregate, approximately 95% of
females will be informative for transcriptionally based X-
chromosome inactivation clonality assays using these genes.
44
A widely used method for determining clonality using the X-
chromosome inactivation principle uses a different approach based
on DNA methylation and CAG tandem repeats at the human
androgen receptor assay (HUMARA) locus (Figure 3). The number
of tandem CAG repeats differentiates the maternal and paternal
X chromosomes, and methylation status distinguishes the inactive
and active X chromosome. At the HUMARA locus, the inactive
X chromosome is methylated, whereas the active X chromosome is
unmethylated.
45
The HUMARA method is more widely applicable
than protein isoform and transcription-based methods because the
variable number of CAG nucleotide repeats allows most patients to
be informative for the assay.
46
Using a variant of the HUMARA
method, the clonal origins of AML, leiomyoma, and Wilm tumor
have been demonstrated.
47
Pitfalls in the interpretation of clonality
assays based on X-chromosome inactivation
Interpretation of clonality studies can be confounded by technical
and methodologic errors as well as errors intrinsic to the mecha-
nism of X-chromosome inactivation.
Technical and methodologic errors
X-chromosome inactivation clonality assays are often performed as
in-house research tools. Technical errors can occur during the assay
such as incomplete digestion by methylation sensitive enzymes or
nonquantitative PCR when allelic fragments of different sizes
amplify with variable efcacy.
The methylation status of the HUMARAlocus is well character-
ized and has been reliably used to determine clonality. Ready
extension of this method to other X-chromosome loci is con-
founded by the effect of mitosis, drugs, nutrition, and the in vivo
manipulation of cells during diagnostic testing, which can alter
methylation patterns. Furthermore, the methylation of inactive
Figure 2. Clonality detection by mRNA (exonic polymorphisms) and protein
polymorphisms. (A) X-chromosome inactivation occurs early in embryonic develop-
ment. (B) mRNAtranscription occurs only from the active X chromosome (with some
exceptions). (C) Analysis of peripheral blood mRNA of a female with polycythemia
vera. The amplied products can be differentiated by sequence-specic polymerase
chain reaction of cDNA followed by ligase reaction detection. bp indicates base pair
standards; pos c., positive control; neg c., negative control (no mRNA added to
reaction mixture); R, reticulocytes; P, platelets; M, monocytes; Mo, cultured
macrophages; B, B lymphocytes; T, T lymphocytes; NK, natural killer cells.
(D) G6PDA and B isoforms can be differentiated by electrophoretic mobility.
1414 CHEN and PRCHAL BLOOD, 1 SEPTEMBER 2007
VOLUME 110, NUMBER 5
For personal use only. on April 2, 2014. by guest bloodjournal.hematologylibrary.org From
genes is not uniform throughout the inactive X-chromosome
regions because although many inactivated genes are methylated,
some are hypomethylated, and some show no difference in
methylation as seen in a region of conserved G6PD polymorphism
(G to T at nucleotide 1311) used in XCIP-based assays.
40,48
One theoretical concern in X-chromosome inactivation clonal-
ity testing is incomplete inactivation of X-chromosome genes.
Carrel and Willard have recently shown that 15% of X chromo-
some genes escape inactivation and 10% of X-chromosome genes
are incompletely inactivated and differentially expressed from each
chromosome.
49
These genes could not be used to determine
clonality because they would not accurately reect the true
proportions of clonal versus nonclonal cells. All new X-
chromosome polymorphic loci proposed as candidates for determin-
ing clonality must be shown to be subject to complete X-
chromosome inactivation before they can be used as a valid marker
for assessing clonality.
43,50
Misinterpretation errors intrinsic to
X-chromosome inactivation
These errors do not occur because the assay was incorrectly performed
or unable to accurately measure clonality. Rather, the accurate but
extreme results are misinterpreted. These errors are false-negatives
and false-positives and can occur at 3 steps in the X-chromosome
inactivation process: at the time of XCI as a result of (1) genetic
and (2) stochastic skewing of the choice of X chromosome, and
(3) after XCI when cellular selection pressures for or against one of
the X-chromosome allelic gene products alters the apparent ratio of
other X-chromosome gene products used as clonality markers.
Stochastic skewing
XCI is a stochastic process and whether a germ cell and its progeny
ultimately express one or the other X allele is dependent on chance.
Whereas a 50/50 ratio of one allele to the other is ideal and
probable in large populations, in the small population of primordial
germ cells that undergo X-chromosome inactivation, it is possible
to achieve greater representation of one allele than the other (Figure
4). This frequently leads to a normal skewing of the X-chromosome
allelic use ratio in terminally differentiated cell populations that are
subject to analysis. Using G6PD synonymous alleles that differ
from each other by a single nucleotide change of C to T, it has been
demonstrated that normal females have variable G6PD allele use
ratios as great as 1:7.
38
Thus, large proportions of apparently
normal women have constitutional skewing of X inactivation.
Based on the degree of skewing, it has been calculated that
approximately 8 cells contribute to the embryonic pool of cells that
go on to form the denitive hematopoietic system.
37,38
Genetic skewing defects in the X-chromosome
inactivation process
Baseline skewing of X-chromosome inactivation can also be
attributable to genetic defects in the X-inactivation process (Figure
4). Among the candidates for genetic mutations is the Xist gene.
46
One family has been identied with a mutation in the Xist promoter
region and associated nonrandom X-chromosome inactivation.
51
Selection in females heterozygous for certain X-linked
genetic diseases
Baseline skewing can also be attributable to selection for or
against a particular X-chromosome germ line inherited mutation
(Figure 5). This has practical application in the interpretation of
clonality studies in females heterozygous for certain X-linked
genetic diseases. Wiskott-Aldrich syndrome is characterized by
eczema, thrombocytopenia with small platelets, and immune
decits apparent since infancy. Because it is X-linked, males are
often aficted but females generally are not. In females, the cells
with the X chromosome bearing the mutant gene are selected
against, whereas the cells with the X chromosome bearing the
normal gene preferentially survive.
52
The majority of heterozygous
female carriers of Wiskott-Aldrich syndrome have normal platelet
number and size and select against those hematopoietic progenitors
that express the Wiskott-Aldrich allele on their active X chromo-
some.
53
However, heterozygous females with Wiskott-Aldrich
Figure 3. Clonality detection by the HUMARA assay. (A) Methylation of the
inactive X chromosome at the HUMARA locus occurs early in embryonic develop-
ment. Shaded, inactivated X chromosome. (B) Schematic of HUMARA locus.
Crossbar indicates methylation sensitive endonuclease site; M, methylated methyl-
ation sensitive endonuclease site; CAG-p, paternal CAG tandem repeat sequence;
CAG-m, maternal CAG tandem repeat sequence. (C) After digestion by methylation
sensitive endonucleases, only inactive (methylated) DNA remains intact. (D) Only
intact DNA can be amplied by polymerase chain reaction with anking primers.
Products can be differentiated from each other by the number of tandem CAG
repeats in CAG-p and CAG-m and their resultant different electrophoretic mobility.
Figure 4. Stochastic/genetic skewing of X chromosome inactivation. (A) Both
X chromosomes are active in early embryonic stem cells. Crosshatching represents
the active X chromosomes of maternal (black) and paternal (white) origin.
(B) X chromosome inactivation choice is stochastic resulting in (C) variance of the
maternal/paternal inactivated X chromosome ratio from the theoretical 1:1. (D) Ge-
netic factors can also affect the choice of X chromosome inactivated, resulting in
skewed maternal/paternal inactivated X chromosome ratios. These skewed popula-
tions can result in a false determination of clonality.
X-LINKED CLONALITYTESTING 1415 BLOOD, 1 SEPTEMBER 2007
VOLUME 110, NUMBER 5
For personal use only. on April 2, 2014. by guest bloodjournal.hematologylibrary.org From
phenotype, who presumably inactivate the normal allele in the
early embryogenesis, exist.
54
Pseudoclonality attributable to cell
selection has also been reported in females heterozygous for other
X-linked disorders such as Lowe Oculo-cerebro-renal syndrome,
55
X-linked agammaglobulinemia,
56
and G6PDdeciency variants.
57,58
Aging and X-chromosome inactivation
Skewed lyonization may occur as part of the aging process,
although the mechanism is less clear. In a study of peripheral
granulocytes using the methylation-based HUMARA assay, skew-
ing was reported to be progressive with age: 1.9% in neonates,
4.5% in women 28 to 32 years old, and 22.7% in women older than
60. Essentially only neutrophils showed skewing with age and
T lymphocytes showed less evidence of unbalanced X inactivation.
The hematopoietic cells (including the erythroid, granulocytic,
monocytic, and megakaryocytic lineages) of 30% to 40% of elderly
women were reported to have more than 90% expression of one
parental X chromosome.
59
Although suggestive of an effect of age
on X-chromosome inactivation, this study was limited because it
compared the average skew of an older versus younger population
instead of the skew in a person after aging. Another study
addressed this concern by examining X-chromosome skewing
using HUMARA methylation in paired samples taken an average
of 16.5 years apart in 178 patients ranging in age from 0 to 74.
These investigators found more progression of X-inactivation
skewing in women older than 60 when they entered the study. In
women younger than 60, no consistent trend toward increased
skewing was found. Based on their ndings, these investigators
proposed that age-related X-chromosome skewing may occur in a
discontinuous/catastrophic manner rather than one of gradual
accretion.
60
Increased X-chromosome inactivation pattern skewing
after age 50 has also been found by other investigators.
61
The apparent development of clonality related to age has been
challenged by investigators using methylation-based clonality
assays as well as X-chromosome transcriptionbased clonality
assays.
62
When age-related clonality is reported, it is generally
correlated with a skewed allelic ratio rather than the exclusive
expression of a single X-chromosome allele. Dening clonality
more stringently as expression of only a single X-chromosome
transcript in the studied tissue, our laboratory has not observed any
clonal XCIP in studies of 200 samples of apparently nonclonal
tissue taken from heterozygous females, suggesting the rarity of
this phenomenon in the general population.
38
However, we have not yet
systematically studied large numbers of females older than 70 years.
Experimental evidence exists supporting clonal expansion and
XCIP skewing with age in cats.
63
Abkowitz and colleagues
performed serial determinations of XCIP skewing using G6PD
isoforms in a feline hematopoiesis model. The cats were derived
from 2 different feline strains with divergent X-chromosome
polymorphisms. They found that over a period of several years,
progenitor cell populations shifted toward the same allelic pheno-
type secondary to hemizygous selection. Thus, age-related skewing
of XCIP occurs in felines and may be related to genetic factors.
A similar phenomenon may exist in humans.
64
Recent studies
comparing the magnitude and direction of presumed acquired
skewing in granulocytes compared with T cells in monozygotic
versus dizygotic twins suggest a genetic contribution to the
observed variance in skewing. The calculated estimate of heritabil-
ity was 68%, although the condence interval ranged from 0% to
100%.
65
Age-related X-chromosomeinactivation skewing can manifest
clinically as late-onset X-linked disorders. An 81-year-old woman
who was heterozygous for the erythroid-specic 5-aminolevulnate
synthase gene and unaffected in her youth later developed micro-
cytic sideroblastic anemia. She was initially thought to have
myelodysplastic syndrome but on true diagnosis was treated to
resolution with pyridoxine.
66
Whether this was related to acquired
clonality associated with myelodysplastic syndrome is not clear.
Recently, age-related X-chromosomeinactivation skewing has
been implicated in the pathogenesis of scleroderma, autoimmune
thyroid disease (AITD, including Graves disease and Hashimoto
thyroiditis), and primary biliary cirrhosis.
67-69
All 3 of these
diseases are more common in females later rather than earlier in
life, providing an epidemiologic basis for further investigation. The
increased autoimmune susceptibility in 45 XO Turner syndrome
also suggests a role for loss of X-chromosome material through
skewing or monosomy in the pathogenesis of autoimmune disor-
ders.
70
Using the HUMARAassay to determine XCIP, it was found
that 64% of patients with scleroderma versus 8% of control
subjects showed X-chromosome skewing less than 80% (P
.001). When XCIP were studied with the HUMARAin AITD, 34%
of concordant twins compared with 11% of normal control subjects
had X-chromosome skewing less than 80% (P .003). A similar
ratio was found when discordant twin pairs were studied.
68
Fluorescent in situ hybridization analysis was used to study the
prevalence of monosomy X in primary biliary cirrhosis versus
hepatitis C and normal controls. The investigators found that in
peripheral blood cells, the age-adjusted frequency of monosomy X
was 0.05 in primary biliary cirrhosis, 0.032 in hepatitis C, and
0.028 in normal controls (P .001).
67
These investigators applied
the same uorescent in situ hybridization analysis to determine
monosomy X rates in systemic sclerosis and autoimmune thyroid
disease. They found a frequency of 6.2% in systemic sclerosis,
4.3% in AITD, and 2.9% in normal female controls (P .001).
71
Several mechanisms have been proposed linking X-chromosome
skewing and monosomy with autoimmune disease, including the
loss of X-chromosome genes crucial to maintaining sex hormone
levels as well as those mediating immune tolerance.
72
Linkage
studies of autoimmune disorders have identied several non-MHC
loci on the X chromosome that may be involved in immune
Figure 5. Somatic selection after X-chromosome inactivation. (A) Early embry-
onic cells express both X chromosomes and undergo X-chromosome inactivation.
(B) After inactivation, embryonic cells express one or the other X chromosome.
Thus, in a disease like Wiskott-Aldrich syndrome, a heterozygous female can
express both the normal and mutant alleles, albeit in different cells. (C) The
embryonic cells undergo proliferation. (D) Cellular selection against the cells
bearing the active X chromosome with the mutant allele results in elimination of
that population of cells, resulting in (E) an apparently clonal (pseudoclonal)
population.
1416 CHEN and PRCHAL BLOOD, 1 SEPTEMBER 2007
VOLUME 110, NUMBER 5
For personal use only. on April 2, 2014. by guest bloodjournal.hematologylibrary.org From
regulation.
73,74
Other proposed mechanisms include loss of anti-
gens expressed from the inactivated X chromosome followed by
loss of T-cell tolerance and autoimmunity. This mechanism seems
less likely given the disparateness of affected organ and tissue
types. In contrast to a deciency of X-chromosome function, a
competing theory of pathogenesis is residual microchimerism from
previous pregnancies. Although not eliminating microchimerism as
a cause of autoimmune disease, experimental evidence obtained by
uorescent in situ hybridization analysis showing the absence of
Y-chromosome material in scleroderma and AITD peripheral blood
cells that are monosomal for the X chromosome suggests this is
less likely.
71
Although no studies have formally linked age-related
XCIP skewing with the development of autoimmune disease, the
available evidence suggests a connection may exist and deserves
further research.
Integrating genotypic and phenotypic
clonality detection
Genotypic and XCIP clonality represent different ways of looking
at the same process. Use of either method to detect a dominant
clonal population has been discussed. Use of genotypic clonality to
detect a small clonal population in the context of a larger nonclonal
population was discussed as minimal residual disease detection.
Use of XCIP analysis to detect a small clonal population in the
context of a larger nonclonal population is more difcult because
the presence of a small clonal population would be indicated by an
increase in XCIP skewing above a theoretical baseline. The
theoretical baseline is often assumed to be 50%, but recent studies
have demonstrated unequal expression of certain X-chromosome
genes.
49
Both the theoretical baseline and degree of XCIP skew
would be subject to statistical variation, which could overshadow
the true difference. XCIP clonal population size estimates in
essential thrombocytosis have been shown to have wide 95%
condence intervals, more so in older patients, with systemic
biases toward overestimating the true population size.
75
The large
variability in XCIP clonality testing limits its use to dominant
clonal populations rather than small clonal populations.
XCIP analysis and concurrent JAK2 617VF testing of large
clonal populations has resulted in new insights into the pathophysi-
ology of myeloproliferative disorders. Not all cases of suspected
myeloproliferative disease proven to be clonal by XCIP clonality
testing have JAK2 617VF mutations.
76-79
The XCIP markers
iduronate-2-sulfatase and MPP1 and the genetic marker JAK2
617VF were used to characterize the granulocytes of patients
with MPD. All the granulocytes were clonal by XCIP, but not all
the granulocytes in the same patient had the JAK2 617VF
mutation, suggesting the presence of a JAK2 617VF-negative
population.
80
In addition to the concerns about XCIP analysis
variability raised by Campbell et al,
75
age-related and constitutive
XCIP skewing can confound the nding of discordant clonal
population sizes. These concerns were refuted by demonstrating
the presence of del20q, an independent clonality marker, in all cells
and by demonstrating polyclonal T cells, which would not be
present if constitutive skewing were present.
80
Our laboratory has
also reported similar discrepancies in clonal population size. XCIP
analysis demonstrated granulocyte clonality in 10 female patients
with polycythemia vera (PV), but the JAK2 617VF mutation
frequency was less than 50% (27.5% 11%) in 3 patients and
more than 50% (75% 10.5%) in 7 patients. Because of potential
confounding from constitutive or age-related skewing, we con-
rmed clonality analysis with erythropoietin growth-independent
colonies from the same patients. Individual colonies represent
clonal processes because they are derived from single progenitors.
Of 69 individual colonies, JAK2 was wild type in 10, mutated
heterozygous in 6, and mutated homozygous in 23, indicating the
presence of a clonal JAK2 617VFnegative population.
81
Other
investigators have also reported discordant clonal populations in
the essential thrombocythemia and myelobrosis with myeloid
metaplasia when analyzed with the HUMARA assay or XCIP in
combination with JAK2 gene analysis.
82-84
In aggregate, these
studies document the existence of clonal JAK2 617VFnegative
populations in the development of myeloproliferative diseases.
Because clonal processes are thought to be initiated by underlying
somatic mutations, the clonal JAK2 617VFnegative populations
may harbor as-yet-undiscovered mutations contributing to the
pathogenesis of myeloproliferative disease. The majority of JAK2
617VFpositive patients with polycythemia vera who transform
to acute leukemia have leukemic blasts that are JAK2 617VF
negative. However, it remains to be determined if they originate
from the preJAK2 617VF clone.
85
Summary
Clonality testing has played an important role in medicine and
hematology. Detection of clonality can be based on genotype and
phenotype. The most frequently used phenotypic clonality tech-
nique is based on the X-chromosome inactivation principle. Proper
interpretation of these results can be confounded by technical errors
and methodological errors. Methodological errors can occur as a
result of stochastic skewing, genetically determined skewing,
environmentally induced methylation changes, and somatic selec-
tion after X-chromosome inactivation. The primary limitation of
XCI clonality studies is the need for informative female patients.
XCIP clonality testing has been applied to demonstrate progres-
sive X-chromosome skewing in aging hematopoietic cells. This has
led to new insights into the pathophysiology of X-linked and
autoimmune disorders. Other research applications include combin-
ing XCIP clonality testing with genotypic clonality testing to
identify clonal populations with unknown underlying genetic mutations,
allowing the identication of novel disease-associated mutations.
Acknowledgments
This work was supported by 1P01CA108671-O1A2, 1R01HL50077
12, and a VAMerit ReviewAward (J.T.P., primary investigator).
Authorship
Contribution: G.L.C. wrote and extensively revised the rst draft;
J.T.P. contributed key portions to the rst draft and critically
reviewed and revised the manuscript.
Conict-of-interest disclosure: The authors declare no compet-
ing nancial interests.
Correspondence: Josef Prchal, Division of Hematology, Depart-
ment of Medicine, University of Utah School of Medicine Room
5C402 SOM, 30 North 1900 East, Salt Lake City, UT 84132;
e-mail: josef.prchal@hsc.utah.edu.
X-LINKED CLONALITYTESTING 1417 BLOOD, 1 SEPTEMBER 2007
VOLUME 110, NUMBER 5
For personal use only. on April 2, 2014. by guest bloodjournal.hematologylibrary.org From
References
1. Adolphson CC, Prchal JT, Carroll AJ. Colonic vil-
lous adenoma: monoclonal origin. JAMA. 1982;
247:829-830.
2. Adamson JW, Fialkow PJ, Murphy S, Prchal JF,
Steinmann L. Polycythemia vera: stem-cell and
probable clonal origin of the disease. N Engl
J Med. 1976;295:913-916.
3. Prchal JT, Throckmorton DW, Carroll AJ III, Fuson
EW, Gams RA, Prchal JF. Acommon progenitor
for human myeloid and lymphoid cells. Nature.
1978;274:590-591.
4. Mesa RA, Li CY, Ketterling RP, Schroeder GS,
Knudson RA, Tefferi A. Leukemic transformation
in myelobrosis with myeloid metaplasia: a
single-institution experience with 91 cases.
Blood. 2005;105:973-977.
5. Rowley JD. Anew consistent chromosomal ab-
normality in chronic myelogenous leukaemia
identied by quinacrine uorescence and Giemsa
staining [Letter]. Nature. 1973;243:290-293.
6. Bahloul M, Asna V, Macintyre E. Clinical impact
of molecular diagnostics in low-grade lymphoma.
Best Pract Res Clin Haematol. 2005;18:97-111.
7. Venditti A, Buccisano F, Del Poeta G, et al. Level
of minimal residual disease after consolidation
therapy predicts outcome in acute myeloid leuke-
mia. Blood. 2000;96:3948-3952.
8. San Miguel JF, Vidriales MB, Lopez-Berges C, et
al. Early immunophenotypical evaluation of mini-
mal residual disease in acute myeloid leukemia
identies different patient risk groups and may
contribute to postinduction treatment stratica-
tion. Blood. 2001;98:1746-1751.
9. Langebrake C, Brinkmann I, Teigler-Schlegel A,
et al. Immunophenotypic differences between
diagnosis and relapse in childhood AML: Implica-
tions for MRD monitoring. Cytometry B Clin Cy-
tom. 2005;63:1-9.
10. Li A, Zhou J, Zuckerman D, et al. Sequence anal-
ysis of clonal immunoglobulin and T-cell receptor
gene rearrangements in children with acute lym-
phoblastic leukemia at diagnosis and at relapse:
implications for pathogenesis and for the clinical
utility of PCR-based methods of minimal residual
disease detection. Blood. 2003;102:4520-4526.
11. Gallagher RE, Yeap BY, Bi W, et al. Quantitative
real-time RT-PCR analysis of PML-RAR alpha
mRNAin acute promyelocytic leukemia: assess-
ment of prognostic signicance in adult patients
from intergroup protocol 0129. Blood. 2003;101:
2521-2528.
12. Nucifora G, Larson RA, Rowley JD. Persistence
of the 8;21 translocation in patients with acute
myeloid leukemia type M2 in long-term remission.
Blood. 1993;82:712-715.
13. Potter MN, Steward CG, Oakhill A. The signi-
cance of detection of minimal residual disease in
childhood acute lymphoblastic leukaemia. Br J
Haematol. 1993;83:412-418.
14. Radich JP, Gehly G, Gooley T, et al. Polymerase
chain reaction detection of the BCR-ABL fusion
transcript after allogeneic marrow transplantation
for chronic myeloid leukemia: results and implica-
tions in 346 patients. Blood. 1995;85:2632-2638.
15. Lin F, van Rhee F, Goldman JM, Cross NC. Kinet-
ics of increasing BCR-ABL transcript numbers in
chronic myeloid leukemia patients who relapse
after bone marrow transplantation. Blood. 1996;
87:4473-4478.
16. Olavarria E, Kanfer E, Szydlo R, et al. Early de-
tection of BCR-ABL transcripts by quantitative
reverse transcriptase-polymerase chain reaction
predicts outcome after allogeneic stem cell trans-
plantation for chronic myeloid leukemia. Blood.
2001;97:1560-1565.
17. Beutler E, Collins Z, Irwin LE. Value of genetic
variants of glucose-6-phosphate dehydrogenase
in tracing the origin of malignant tumors. N Engl
J Med. 1967;276:389-391.
18. Beutler E, Yeh M, Fairbanks VF. The normal hu-
man female as a mosaic of X-chromosome activ-
ity: studies using the gene for C-6-PD-deciency
as a marker. Proc Natl Acad Sci U SA. 1962;48:
9-16.
19. Lyon MF. Gene action in the X-chromosome of
the mouse (Mus musculus L.). Nature. 1961;190:
372-373.
20. Ohno S, Makino S. The single-X nature of sex
chromatin in man. Lancet. 1961;1:78-79.
21. Ohno S, Hauschka TS. Allocycly of the X-chromo-
some in tumors and normal tissues. Cancer Res.
1960;20:541-545.
22. Brown CJ, Hendrich BD, Rupert JL, et al. The hu-
man XIST gene: analysis of a 17 kb inactive X-
specic RNAthat contains conserved repeats
and is highly localized within the nucleus. Cell.
1992;71:527-542.
23. Lee JT, Davidow LS, Warshawsky D. Tsix, a gene
antisense to Xist at the X-inactivation centre. Nat
Genet. 1999;21:400-404.
24. Ogawa Y, Lee JT. Xite, X-inactivation intergenic
transcription elements that regulate the probabil-
ity of choice. Mol Cell. 2003;11:731-743.
25. Brockdorff N, Ashworth A, Kay GF, et al. The
product of the mouse Xist gene is a 15 kb inactive
X-specic transcript containing no conserved
ORF and located in the nucleus. Cell. 1992;71:
515-526.
26. Clemson CM, McNeil JA, Willard HF, Lawrence
JB. XIST RNApaints the inactive X chromosome
at interphase: evidence for a novel RNAinvolved
in nuclear/chromosome structure. J Cell Biol.
1996;132:259-275.
27. Penny GD, Kay GF, Sheardown SA, Rastan S,
Brockdorff N. Requirement for Xist in X chromo-
some inactivation. Nature. 1996;379:131-137.
28. Popova BC, Tada T, Takagi N, Brockdorff N, Nest-
erova TB. Attenuated spread of X-inactivation in
an X-autosome translocation. Proc Natl Acad Sci
U SA. 2006;103:7706-7711.
29. Lee JT. Disruption of imprinted X inactivation by
parent-of-origin effects at Tsix. Cell. 2000;103:17-
27.
30. Sado T, Wang Z, Sasaki H, Li E. Regulation of
imprinted X-chromosome inactivation in mice by
Tsix. Development. 2001;128:1275-1286.
31. Heard E. Recent advances in X-chromosome in-
activation. Curr Opin Cell Biol. 2004;16:247-255.
32. Xu N, Tsai CL, Lee JT. Transient homologous
chromosome pairing marks the onset of X inacti-
vation. Science. 2006;311:1149-1152.
33. Bacher CP, Guggiari M, Brors B, et al. Transient
colocalization of X-inactivation centres accompa-
nies the initiation of X inactivation. Nat Cell Biol.
2006;8:293-299.
34. Gartler SM, Riggs AD. Mammalian X-chromo-
some inactivation. Annu Rev Genet. 1983;17:
155-190.
35. Huynh KD, Lee JT. Inheritance of a pre-inacti-
vated paternal X chromosome in early mouse
embryos. Nature. 2003;426:857-862.
36. Okamoto I, Otte AP, Allis CD, Reinberg D, Heard
E. Epigenetic dynamics of imprinted X inactiva-
tion during early mouse development. Science.
2004;303:644-649.
37. Puck JM, Stewart CC, Nussbaum RL. Maximum-
likelihood analysis of human T-cell X chromo-
some inactivation patterns: normal women versus
carriers of X-linked severe combined immunode-
ciency. Am J Hum Genet. 1992;50:742-748.
38. Prchal JT, Prchal JF, Belickova M, et al. Clonal
stability of blood cell lineages indicated by
X-chromosomal transcriptional polymorphism. J
Exp Med. 1996;183:561-567.
39. Curnutte JT, Hopkins PJ, Kuhl W, Beutler E.
Studying X inactivation. Lancet. 1992;339:749.
40. Prchal JT, Guan YL. Anovel clonality assay
based on transcriptional analysis of the active X
chromosome. Stem Cells. 1993;11(Suppl 1):62-
65.
41. Gregg XT, Kralovics R, Prchal JT. Apolymor-
phism of the X-linked gene IDS increases the
number of females informative for transcriptional
clonality assays. Am J Hematol. 2000;63:184-
191.
42. el-Kassar N, Hetet G, Briere J, Grandchamp B.
Clonality analysis of hematopoiesis in essential
thrombocythemia: advantages of studying T lym-
phocytes and platelets. Blood. 1997;89:128-134.
43. Luhovy M, Liu Y, Belickova M, Prchal JF, Prchal
JT. Anovel clonality assay based on transcrip-
tional polymorphism of X chromosome gene p55.
Biol Blood Marrow Transplant. 1995;1:81-87.
44. Liu E, Jelinek J, Pastore YD, Guan Y, Prchal JF,
Prchal JT. Discrimination of polycythemias and
thrombocytoses by novel, simple, accurate
clonality assays and comparison with PRV-1 ex-
pression and BFU-E response to erythropoietin.
Blood. 2003;101:3294-3301.
45. Allen RC, Zoghbi HY, Moseley AB, Rosenblatt
HM, Belmont JW. Methylation of HpaII and HhaI
sites near the polymorphic CAG repeat in the hu-
man androgen-receptor gene correlates with X
chromosome inactivation. Am J Hum Genet.
1992;51:1229-1239.
46. Belmont JW. Genetic control of X inactivation and
processes leading to X-inactivation skewing.
Am J Hum Genet. 1996;58:1101-1108.
47. Vogelstein B, Fearon ER, Hamilton SR, Feinberg
AP. Use of restriction fragment length polymor-
phisms to determine the clonal origin of human
tumors. Science. 1985;227:642-645.
48. Gale RE, Wheadon H, Linch DC. X-chromosome
inactivation patterns using HPRT and PGK poly-
morphisms in haematologically normal and post-
chemotherapy females. Br J Haematol. 1991;79:
193-197.
49. Carrel L, Willard HF. X-inactivation prole reveals
extensive variability in X-linked gene expression
in females. Nature. 2005;434:400-404.
50. Liu Y, Phelan J, Go RC, Prchal JF, Prchal JT.
Rapid determination of clonality by detection of
two closely-linked X chromosome exonic poly-
morphisms using allele-specic PCR. J Clin In-
vest. 1997;99:1984-1990.
51. Plenge RM, Hendrich BD, Schwartz C, et al. A
promoter mutation in the XIST gene in two unre-
lated families with skewed X-chromosome inacti-
vation. Nat Genet. 1997;17:353-356.
52. Carroll AJ, Prchal JT, Crist WM, Prchal JF. Cellu-
lar expression of Wiskott-Aldrich allele. Lancet.
1980;1:601-602.
53. Prchal JT, Carroll AJ, Prchal JF, et al. Wiskott-
Aldrich syndrome: cellular impairments and their
implication for carrier detection. Blood. 1980;56:
1048-1054.
54. Parolini O, Ressmann G, Haas OA, et al. X-linked
Wiskott-Aldrich syndrome in a girl. N Engl J Med.
1998;338:291-295.
55. Hittner HM, Carroll AJ, Prchal JT. Linkage studies
in carriers of Lowe oculo-cerebro-renal syn-
drome. Am J Hum Genet. 1982;34:966-971.
56. Haire RN, Ohta Y, Strong SJ, et al. Unusual pat-
terns of exon skipping in Bruton tyrosine kinase
are associated with mutations involving the intron
17 3 splice site. Am J Hum Genet. 1997;60:798-
807.
57. Luzzatto L, Usanga EA, Bienzle U, Esan GF,
Fusuan FA. Imbalance in X-chromosome expres-
sion: evidence for a human X-linked gene affect-
ing growth of hemopoietic cells. Science. 1979;
205:1418-1420.
58. Filosa S, Giacometti N, Wangwei C, et al. So-
matic-cell selection is a major determinant of the
1418 CHEN and PRCHAL BLOOD, 1 SEPTEMBER 2007
VOLUME 110, NUMBER 5
For personal use only. on April 2, 2014. by guest bloodjournal.hematologylibrary.org From
blood-cell phenotype in heterozygotes for glu-
cose-6-phosphate dehydrogenase mutations
causing severe enzyme deciency. Am J Hum
Genet. 1996;59:887-895.
59. Busque L, Mio R, Mattioli J, et al. Nonrandom X-
inactivation patterns in normal females: lyoniza-
tion ratios vary with age. Blood. 1996;88:59-65.
60. Sandovici I, Naumova AK, Leppert M, Linares Y,
Sapienza C. Alongitudinal study of X-inactivation
ratio in human females. Hum Genet. 2004;115:
387-392.
61. Kristiansen M, Knudsen GP, Bathum L, et al. Twin
study of genetic and aging effects on X chromo-
some inactivation. Eur J Hum Genet. 2005;13:
599-606.
62. Racchi O, Mangerini R, Rapezzi D, Rolfo M,
Gaetani GF, Ferraris AM. X chromosome inacti-
vation patterns in normal females. Blood Cells
Mol Dis. 1998;24:439-447.
63. Abkowitz JL, Taboada M, Shelton GH, Catlin SN,
Guttorp P, Kiklevich JV. An X chromosome gene
regulates hematopoietic stem cell kinetics. Proc
Natl Acad Sci U SA. 1998;95:3862-3866.
64. Christensen K, Kristiansen M, Hagen-Larsen H,
et al. X-linked genetic factors regulate hematopoi-
etic stem-cell kinetics in females. Blood. 2000;95:
2449-2451.
65. Vickers MA, McLeod E, Spector TD, Wilson IJ.
Assessment of mechanism of acquired skewed X
inactivation by analysis of twins. Blood. 2001;97:
1274-1281.
66. Cotter PD, May A, Fitzsimons EJ, et al. Late-on-
set X-linked sideroblastic anemia. Missense mu-
tations in the erythroid delta-aminolevulinate syn-
thase (ALAS2) gene in two pyridoxine-responsive
patients initially diagnosed with acquired refrac-
tory anemia and ringed sideroblasts. J Clin In-
vest. 1995;96:2090-2096.
67. Invernizzi P, Miozzo M, Battezzati PM, et al. Fre-
quency of monosomy X in women with primary
biliary cirrhosis. Lancet. 2004;363:533-535.
68. Brix TH, Knudsen GP, Kristiansen M, Kyvik KO,
Orstavik KH, Hegedus L. High frequency of
skewed X-chromosome inactivation in females
with autoimmune thyroid disease: a possible ex-
planation for the female predisposition to thyroid
autoimmunity. J Clin Endocrinol Metab. 2005;90:
5949-5953.
69. Ozbalkan Z, Bagislar S, Kiraz S, et al. Skewed X
chromosome inactivation in blood cells of women
with scleroderma. Arthritis Rheum. 2005;52:1564-
1570.
70. Ranke MB, Saenger P. Turners syndrome. Lan-
cet. 2001;358:309-314.
71. Invernizzi P, Miozzo M, Selmi C, et al. X chromo-
some monosomy: a common mechanism for au-
toimmune diseases. J Immunol. 2005;175:575-
578.
72. Gartler SM, Goldman MA. Biology of the X chro-
mosome. Curr Opin Pediatr. 2001;13:340-345.
73. Imrie H, Vaidya B, Perros P, et al. Evidence for a
Graves disease susceptibility locus at chromo-
some Xp11 in a United Kingdom population.
J Clin Endocrinol Metab. 2001;86:626-630.
74. Barbesino G, Tomer Y, Concepcion ES, Davies
TF, Greenberg DA. Linkage analysis of candidate
genes in autoimmune thyroid disease. II. Se-
lected gender-related genes and the X-chromo-
some. International Consortium for the Genetics
of Autoimmune Thyroid Disease. J Clin Endocri-
nol Metab. 1998;83:3290-3295.
75. Campbell PJ, Baxter EJ, Beer PA, et al. Mutation
of JAK2 in the myeloproliferative disorders: tim-
ing, clonality studies, cytogenetic associations,
and role in leukemic transformation. Blood. 2006;
108:3548-3555.
76. James C, Ugo V, Le Couedic JP, et al. Aunique
clonal JAK2 mutation leading to constitutive sig-
nalling causes polycythaemia vera. Nature. 2005;
434:1144-1148.
77. Kralovics R, Passamonti F, Buser AS, et al. A
gain-of-function mutation of JAK2 in myeloprolif-
erative disorders. N Engl J Med. 2005;352:1779-
1790.
78. Zhao R, Xing S, Li Z, et al. Identication of an ac-
quired JAK2 mutation in polycythemia vera. J Biol
Chem. 2005;280:22788-22792.
79. Baxter EJ, Scott LM, Campbell PJ, et al. Acquired
mutation of the tyrosine kinase JAK2 in human
myeloproliferative disorders. Lancet. 2005;365:
1054-1061.
80. Kralovics R, Teo SS, Li S, et al. Acquisition of the
V617F mutation of JAK2 is a late genetic event in
a subset of patients with myeloproliferative disor-
ders. Blood. 2006;108:1377-1380.
81. Nussenzveig RH, Swierczek SI, Jelinek J, et al.
Polycythemia vera is not initiated by JAK2V617F
mutation. Exp Hematol. 2007;35:32-38.
82. Levine RL, Belisle C, Wadleigh M, et al. X-inacti-
vation-based clonality analysis and quantitative
JAK2V617F assessment reveal a strong asso-
ciation between clonality and JAK2V617F in PV
but not ET/MMM, and identies a subset of
JAK2V617F-negative ET and MMM patients
with clonal hematopoiesis. Blood. 2006;107:
4139-4141.
83. Kiladjian JJ, Elkassar N, Cassinat B, et al. Essen-
tial thrombocythemias without V617F JAK2 muta-
tion are clonal hematopoietic stem cell disorders.
Leukemia. 2006;20:1181-1183.
84. Antonioli E, Guglielmelli P, Pancrazzi A, et al.
Clinical implications of the JAK2 V617F mutation
in essential thrombocythemia. Leukemia. 2005;
19:1847-1849.
85. Jelinek J, Oki Y, Gharibyan V, et al. JAK2 muta-
tion 1849G T is rare in acute leukemias but can
be found in CMML, Philadelphia-chromosome
negative CML and megakaryocytic leukemia.
Blood. 2005;106:3370-3373.
Erratum
In the commentary by Spivak entitled Thrombocytosis, pregnancy, and
regression toward mean, which appeared in the July 15, 2007, issue of
Blood (Volume 110:472-473), a word was omitted from the title. The title
should have read Thrombocytosis, pregnancy, and regression toward the
mean.
X-LINKED CLONALITYTESTING 1419 BLOOD, 1 SEPTEMBER 2007
VOLUME 110, NUMBER 5
For personal use only. on April 2, 2014. by guest bloodjournal.hematologylibrary.org From
You might also like
- Very Advanced Maternal Age, TOG-2021Document10 pagesVery Advanced Maternal Age, TOG-2021saeed hasan saeedNo ratings yet
- Case StudyDocument21 pagesCase StudyLuige AvilaNo ratings yet
- Religion and Belief Systems in Australia Post 1945Document6 pagesReligion and Belief Systems in Australia Post 1945Jananee SundarakumarNo ratings yet
- Chronic Lymphocytic Leukemia: A Clinical and Molecular Heterogenous DiseaseDocument14 pagesChronic Lymphocytic Leukemia: A Clinical and Molecular Heterogenous DiseaseCallisthenisLeventisNo ratings yet
- ClonalDocument11 pagesClonalprateek bhatiaNo ratings yet
- CancerDocument20 pagesCancerManisha DasNo ratings yet
- Cytogenetic Analysis in The Diagnosis of Acute Leukemia: Sverre Heim, FelixDocument9 pagesCytogenetic Analysis in The Diagnosis of Acute Leukemia: Sverre Heim, FelixEnas KharbotlyNo ratings yet
- 3941 FullDocument28 pages3941 FullMunawwar AweNo ratings yet
- Flow Cytometry Immunophenotyping For Hematologic NeoplasmsDocument28 pagesFlow Cytometry Immunophenotyping For Hematologic NeoplasmsAti Rahmi PurwandariNo ratings yet
- Flowcytometryin Diagnosis, Prognostication, Andmonitoringofmultiple MyelomaandrelateddisordersDocument13 pagesFlowcytometryin Diagnosis, Prognostication, Andmonitoringofmultiple MyelomaandrelateddisordersmatanhibNo ratings yet
- Paper Seminario Jose EpulefDocument11 pagesPaper Seminario Jose EpulefJL EulefiNo ratings yet
- 2016 Article 70Document8 pages2016 Article 70sawantleena62No ratings yet
- Cancer Res 1990 Wainscoat 1355 60Document7 pagesCancer Res 1990 Wainscoat 1355 60Shahab Ud DinNo ratings yet
- Dinosaurs Before DarkDocument9 pagesDinosaurs Before DarkIna SimacheNo ratings yet
- New England Journal Medicine: The ofDocument16 pagesNew England Journal Medicine: The ofMauricio FemeníaNo ratings yet
- Article 2Document5 pagesArticle 2Mahadev HaraniNo ratings yet
- CLL Complete 041013Document2 pagesCLL Complete 041013CGIdocsNo ratings yet
- Minimal Residual Disease in Acute Lymphoblastic Leukemia: Dario CampanaDocument6 pagesMinimal Residual Disease in Acute Lymphoblastic Leukemia: Dario CampanaJAIR_valencia3395No ratings yet
- Flow CytometryDocument7 pagesFlow CytometryMayHnin KhaingNo ratings yet
- Malignant or Benign Leukocytosis: Tracy I. GeorgeDocument10 pagesMalignant or Benign Leukocytosis: Tracy I. GeorgeirdinamarchsyaNo ratings yet
- Autophagy Limits Proliferation and Glycolytic Metabolism in Acute Myeloid LeukemiaDocument10 pagesAutophagy Limits Proliferation and Glycolytic Metabolism in Acute Myeloid LeukemiaFadlan AbduhrahmanNo ratings yet
- Abnormalities of RUNX1, CBFB, CEBPA, and NPM1 Genes in Acute Myeloid LeukemiaDocument10 pagesAbnormalities of RUNX1, CBFB, CEBPA, and NPM1 Genes in Acute Myeloid LeukemiaAndikhaNo ratings yet
- Flow Cytometry CD45 Gating For Immunophenotyping of Acute Myeloid LeukemiaDocument9 pagesFlow Cytometry CD45 Gating For Immunophenotyping of Acute Myeloid LeukemiaKATHERINE ALEXANDRA ESCARRAGA CORREALNo ratings yet
- Describe The Molecular Basis Underlying Haematological MalignancyDocument3 pagesDescribe The Molecular Basis Underlying Haematological MalignancyAlison HinesNo ratings yet
- Molecular Analysis To Demonstrate That Odontogenic Keratocysts Are NeoplasticDocument5 pagesMolecular Analysis To Demonstrate That Odontogenic Keratocysts Are NeoplasticSamar KhanNo ratings yet
- Myeloid LeukemiaDocument36 pagesMyeloid LeukemiaLia pramitaNo ratings yet
- Reviews: Chronic Lymphocytic Leukaemia: From Genetics To TreatmentDocument18 pagesReviews: Chronic Lymphocytic Leukaemia: From Genetics To Treatmentlengers poworNo ratings yet
- Bosch2019 PDFDocument18 pagesBosch2019 PDFlengers poworNo ratings yet
- Plasma Cell Myeloma Literature Review and Case StudyDocument6 pagesPlasma Cell Myeloma Literature Review and Case StudyafdtygyhkNo ratings yet
- 976 FullDocument7 pages976 FullFirda PotterNo ratings yet
- Ijlh 1251Document6 pagesIjlh 1251Ramadhan OlongNo ratings yet
- SF3B1 and Other Novel Cancer Genes: in Chronic Lymphocytic LeukemiaDocument10 pagesSF3B1 and Other Novel Cancer Genes: in Chronic Lymphocytic LeukemiaRafael ColinaNo ratings yet
- Citometria 2005Document8 pagesCitometria 2005Leslie AraujoNo ratings yet
- Morfologi PlateletDocument24 pagesMorfologi PlateletEllya Latifah IlyasNo ratings yet
- Acute Myeloid Leukemia: Advances in Diagnosis and Classi CationDocument9 pagesAcute Myeloid Leukemia: Advances in Diagnosis and Classi CationTay SalinasNo ratings yet
- Pages 4 7Document4 pagesPages 4 7andreas_251650No ratings yet
- Leukemia Stem Cells: Eike C. Buss and Anthony D. HoDocument9 pagesLeukemia Stem Cells: Eike C. Buss and Anthony D. HoPedro AzevedoNo ratings yet
- PUIMay 1604 Finalto PuiDocument120 pagesPUIMay 1604 Finalto Puijsbart330No ratings yet
- Emma - 2019 - Aging and HematopoiesisDocument9 pagesEmma - 2019 - Aging and Hematopoiesispratista adi krisnaNo ratings yet
- Author 'S Accepted Manuscript: WWW - Elsevier.de/endendDocument31 pagesAuthor 'S Accepted Manuscript: WWW - Elsevier.de/endendJose Angel AbadíaNo ratings yet
- Blood 2008 Craig 3941 67Document28 pagesBlood 2008 Craig 3941 67czumoffenNo ratings yet
- Hematopoiesis: Makio Ogawa, MD, PHDDocument6 pagesHematopoiesis: Makio Ogawa, MD, PHDVredy LesnarNo ratings yet
- Blood-2014 - JAK2 Et CalreticulineDocument16 pagesBlood-2014 - JAK2 Et Calreticulineamara.ablaNo ratings yet
- Chromosome AbnormalitiesDocument27 pagesChromosome AbnormalitiesNatasa BajalovicNo ratings yet
- New AML Fusion in AML NK, Wen Hongxiue, 2012Document10 pagesNew AML Fusion in AML NK, Wen Hongxiue, 2012mrkhprojectNo ratings yet
- IPT For Plasma Cell DisordersDocument23 pagesIPT For Plasma Cell DisordersDAWOODNo ratings yet
- Aberrant DNA Methylation Is A Dominant Mechanism in MDS Progression To AMLDocument11 pagesAberrant DNA Methylation Is A Dominant Mechanism in MDS Progression To AMLJuan GomezNo ratings yet
- 5446.full 2Document12 pages5446.full 2malik003No ratings yet
- Rodrguez Vicente 2013Document14 pagesRodrguez Vicente 2013Jose AbadiaNo ratings yet
- Synne - Torkildsen - 2015 - Novel ZEB2-BCL11B Fusion Gene Identified by RNA-Sq in AML With T (2 14) (q22 q32)Document12 pagesSynne - Torkildsen - 2015 - Novel ZEB2-BCL11B Fusion Gene Identified by RNA-Sq in AML With T (2 14) (q22 q32)mrkhprojectNo ratings yet
- Vicki A. Morrison and Grzegorz S. NowakowskiDocument19 pagesVicki A. Morrison and Grzegorz S. NowakowskiCristian Villarroel SNo ratings yet
- Cytogenetics: Alkitab University - Collage of Medical Techniques Department of Medical Analysis 3 Rd. Stage - A4Document4 pagesCytogenetics: Alkitab University - Collage of Medical Techniques Department of Medical Analysis 3 Rd. Stage - A4Mohammed R.HusseinNo ratings yet
- Principles of Clinical CytogeneticsDocument34 pagesPrinciples of Clinical CytogeneticsZainab Jamal SiddiquiNo ratings yet
- Answers - Haematological Malignancies Digital Images QuizDocument4 pagesAnswers - Haematological Malignancies Digital Images Quizcande casanasNo ratings yet
- FPDMM3Document10 pagesFPDMM3sccNo ratings yet
- Identification of Recurring Tumor Specific Somatic Mutations in AML by Transcriptome Seq Greif2011Document7 pagesIdentification of Recurring Tumor Specific Somatic Mutations in AML by Transcriptome Seq Greif2011mrkhprojectNo ratings yet
- The Detection of Mutations in The APC Gene of Romanian Patients With Colorectal Cancer Through Two Independent TechniquesDocument9 pagesThe Detection of Mutations in The APC Gene of Romanian Patients With Colorectal Cancer Through Two Independent TechniquesiuventasNo ratings yet
- Short-And Long-Term Effects of Chromosome Mis-Segregation and AneuploidyDocument37 pagesShort-And Long-Term Effects of Chromosome Mis-Segregation and AneuploidyMuh. Taqwin 1015No ratings yet
- Citom NeoplasiasHemat Rev2008Document28 pagesCitom NeoplasiasHemat Rev2008liliana_solari_1No ratings yet
- Quinn Et Al-2016-British Journal of HaematologyDocument9 pagesQuinn Et Al-2016-British Journal of HaematologyRagul BiotechNo ratings yet
- 364 FullDocument12 pages364 FullDesi HutapeaNo ratings yet
- Diagnosis of Blood and Bone Marrow DisordersFrom EverandDiagnosis of Blood and Bone Marrow DisordersSa A. WangNo ratings yet
- Angela SolikovaDocument10 pagesAngela SolikovaGirisha PathakNo ratings yet
- Aire - 1 ReinigenDocument25 pagesAire - 1 Reinigengino aldo palomino ludeñaNo ratings yet
- CH 2 Climate of PakistanDocument29 pagesCH 2 Climate of PakistanZeeshan HassanNo ratings yet
- CFP Registration Process (Final) - 3Document39 pagesCFP Registration Process (Final) - 3nishiNo ratings yet
- Igc Code Implemented in DNV RulesDocument123 pagesIgc Code Implemented in DNV Ruleslearsipi061No ratings yet
- Aluda Move (Rayan Nadr J Zahra Ozair)Document2 pagesAluda Move (Rayan Nadr J Zahra Ozair)varaxoshnaw36No ratings yet
- Asuhan Keperawatan Pada Klien Dengan Pasca Operasi Hernia Inguinalis Di Lt.6 Darmawan Rs Kepresidenan Rspad Gatot Soebroto Jakarta Tahun 2019Document7 pagesAsuhan Keperawatan Pada Klien Dengan Pasca Operasi Hernia Inguinalis Di Lt.6 Darmawan Rs Kepresidenan Rspad Gatot Soebroto Jakarta Tahun 2019Ggp Kristus Raja SuliNo ratings yet
- UIL Calculator Applications Study ListDocument7 pagesUIL Calculator Applications Study ListRocket FireNo ratings yet
- Financial Statement Coronation NightDocument8 pagesFinancial Statement Coronation NightRuel Gapuz ManzanoNo ratings yet
- Monitoring Times 1998 03Document116 pagesMonitoring Times 1998 03Benjamin DoverNo ratings yet
- Earth and Lice Science Quarter 2 BrochureDocument2 pagesEarth and Lice Science Quarter 2 BrochureCamille NavorNo ratings yet
- Enfermedades Emergentes y Embarazo - EID - November 2006 - Volume CompletoDocument187 pagesEnfermedades Emergentes y Embarazo - EID - November 2006 - Volume CompletoRuth Vargas GonzalesNo ratings yet
- Steamshovel Press Issue 04Document60 pagesSteamshovel Press Issue 04liondog1No ratings yet
- μου κάνειDocument43 pagesμου κάνειΚατερίνα ΠαπαδάκηNo ratings yet
- Jersey Documentation 1.0.3 User GuideDocument35 pagesJersey Documentation 1.0.3 User Guidenaresh921No ratings yet
- Annex B - Intake Sheet FinalDocument2 pagesAnnex B - Intake Sheet FinalCherry May Logdat-NgNo ratings yet
- Omm Tank, Combat, Full Tracked 105-MM Gun, M60a3 and TTS TurretDocument663 pagesOmm Tank, Combat, Full Tracked 105-MM Gun, M60a3 and TTS TurretSTGN100% (1)
- Time Clauses - That Vs Which-Relative ClausesDocument8 pagesTime Clauses - That Vs Which-Relative ClausesZuza AlexandrinaNo ratings yet
- Effect of Oral Cryotherapy in Preventing Chemotherapy Induced Oral Stomatitis Among Childhood Acute Lymphoblastic LeukemiaDocument10 pagesEffect of Oral Cryotherapy in Preventing Chemotherapy Induced Oral Stomatitis Among Childhood Acute Lymphoblastic LeukemiaIjahss JournalNo ratings yet
- 1chea Expt4 PPTDocument37 pages1chea Expt4 PPTJimin No JamsNo ratings yet
- English For Nursing Topic 12 Reinforcing A Dietary ProgramDocument6 pagesEnglish For Nursing Topic 12 Reinforcing A Dietary ProgramEha Huwaida HayatiNo ratings yet
- MPTH Reviewer Part 1Document27 pagesMPTH Reviewer Part 1Hani VitalesNo ratings yet
- Novello's Catalogue of Orchestral MusicDocument212 pagesNovello's Catalogue of Orchestral MusicAnte B.K.No ratings yet
- BIZHUB 240f SM PDFDocument355 pagesBIZHUB 240f SM PDFBranga CorneliuNo ratings yet
- Dance Like A ManDocument4 pagesDance Like A ManShubhadip aichNo ratings yet
- Solution Manual For Transportation: A Global Supply Chain Perspective, 8th Edition, John J. Coyle, Robert A. Novack, Brian Gibson, Edward J. BardiDocument34 pagesSolution Manual For Transportation: A Global Supply Chain Perspective, 8th Edition, John J. Coyle, Robert A. Novack, Brian Gibson, Edward J. Bardielizabethsantosfawmpbnzjt100% (21)
- Light Sport Aircraft: Standard Terminology ForDocument6 pagesLight Sport Aircraft: Standard Terminology ForAhmad Zubair RasulyNo ratings yet
- Graded Lab Lab - 7 Introduction To Computing: Topics: If - Else Conditions, While LoopDocument5 pagesGraded Lab Lab - 7 Introduction To Computing: Topics: If - Else Conditions, While LoopqwertyNo ratings yet