Professional Documents
Culture Documents
100%(1)100% found this document useful (1 vote)
70 viewsPancreatic Hormones
Pancreatic Hormones
Uploaded by
Bodea DoruThis document summarizes pancreatic hormones and their role in glucose metabolism. It discusses how insulin and glucagon are secreted by the pancreas to regulate blood glucose levels. Insulin promotes glucose uptake and storage in liver and muscle, while inhibiting gluconeogenesis. It stimulates fat and protein synthesis. Glucagon has opposing effects, stimulating glycogenolysis and gluconeogenesis in the liver. The document also describes the causes, symptoms, and diagnosis of Type 1 and Type 2 diabetes, which result from insulin deficiency and insulin resistance, respectively.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- Rebirth of The Useless Bastard SonDocument32 pagesRebirth of The Useless Bastard Sonthe.untamed.annaNo ratings yet
- Fce 2015 Complete Tests 1 e 2 AnswersDocument4 pagesFce 2015 Complete Tests 1 e 2 AnswersMárcia Bonfim83% (23)
- Anti Diabetic DrugsDocument58 pagesAnti Diabetic DrugsDaniel Wang100% (1)
- Establish Kinder Garden School - Develope Project ManagerDocument25 pagesEstablish Kinder Garden School - Develope Project ManagerVõ Thúy Trân0% (1)
- Mathematics of InvestmentsDocument2 pagesMathematics of InvestmentsShiera Saletrero SimbajonNo ratings yet
- 9 Diabetes Mellitus PHYSIOLOGYDocument22 pages9 Diabetes Mellitus PHYSIOLOGYEman KhammasNo ratings yet
- 14 - Blood Glucose HomeostasisDocument34 pages14 - Blood Glucose HomeostasischeckmateNo ratings yet
- Blood GlucoseDocument8 pagesBlood Glucoseعبدالرحمن عابدNo ratings yet
- Pathophysiology of DiabetesDocument88 pagesPathophysiology of DiabetesCahya SetiyaNo ratings yet
- Classifications of Insulin2Document116 pagesClassifications of Insulin2loglesb1No ratings yet
- Insulin and The Oral HypoglycemicsDocument9 pagesInsulin and The Oral HypoglycemicsHasibNo ratings yet
- Anti-Diabetic Drugs: Siti Farah MD Tohid (PHD)Document39 pagesAnti-Diabetic Drugs: Siti Farah MD Tohid (PHD)Nurul Mursyidah ZakariaNo ratings yet
- Glucose Homeostasis Disorders: by Julyn Marie Elnas Abad-GallardoDocument53 pagesGlucose Homeostasis Disorders: by Julyn Marie Elnas Abad-GallardoMarielle J GarciaNo ratings yet
- AntidiabetesDocument51 pagesAntidiabetesPuri Ratna KartiniNo ratings yet
- Physiology of Diabetes: Dr. Solomon Sathishkumar. MDDocument36 pagesPhysiology of Diabetes: Dr. Solomon Sathishkumar. MDKhaled LajmiNo ratings yet
- What Are The Cellular and Molecular Actions of Insulin?Document13 pagesWhat Are The Cellular and Molecular Actions of Insulin?Elle ReyesNo ratings yet
- Diabetes Mellitus and Laboratory Tests of DiabetesDocument24 pagesDiabetes Mellitus and Laboratory Tests of DiabetesturkiNo ratings yet
- Diabetes and PregnancyDocument49 pagesDiabetes and PregnancyCHRISTIAN SIDAYANo ratings yet
- Common Endocrine Disorders: Iril I. Panes, RN, MANDocument63 pagesCommon Endocrine Disorders: Iril I. Panes, RN, MANJona Phie Domingo MonteroNo ratings yet
- Diabetes1Document150 pagesDiabetes1Phyan HyunNo ratings yet
- Anti-Diabetic Drugs Part A-2Document35 pagesAnti-Diabetic Drugs Part A-2rimsha waseemNo ratings yet
- Diabetes MellitusDocument150 pagesDiabetes MellitusIan Mizzel A. Dulfina100% (1)
- CP2 MidtermsDocument278 pagesCP2 MidtermsDiana WadwasinNo ratings yet
- Pancreatic Hormones and The Treatment of Diabetes MellitusDocument46 pagesPancreatic Hormones and The Treatment of Diabetes MellitusasmaNo ratings yet
- Carbohydrates HandoutDocument15 pagesCarbohydrates HandoutnullNo ratings yet
- Hand Out DM Medical Surgical Nursing 2Document11 pagesHand Out DM Medical Surgical Nursing 2Zarlou OtamiasNo ratings yet
- DiabetesDocument10 pagesDiabetesLyNo ratings yet
- نسخة Blood Glucose 9Document16 pagesنسخة Blood Glucose 9نوف الحربي.No ratings yet
- Diabetes AssignmentDocument8 pagesDiabetes AssignmentMildred Obeng AgyeiwaaNo ratings yet
- Diabetes Millitus PDFDocument41 pagesDiabetes Millitus PDFAbdullah BhattiNo ratings yet
- Dr. Solomon Sathishkumar, MD Department of Physiology Christian Medical College Vellore, IndiaDocument48 pagesDr. Solomon Sathishkumar, MD Department of Physiology Christian Medical College Vellore, IndiaKrairat KomdeeNo ratings yet
- Presented by DR Ashish Sharma Guided by DR Meena PatelDocument74 pagesPresented by DR Ashish Sharma Guided by DR Meena PatelAndrew Surya Putra SccNo ratings yet
- Nursing Care of Patients With Diabetes MellitusDocument43 pagesNursing Care of Patients With Diabetes MellitusRashida RuwaNo ratings yet
- Pathophysiology Notes: Diabetes Mellitus Is A Group of Metabolic Disorders Characterized HyperglycemiaDocument14 pagesPathophysiology Notes: Diabetes Mellitus Is A Group of Metabolic Disorders Characterized HyperglycemiaHaifa ibrahimNo ratings yet
- Diabetes OutlineDocument7 pagesDiabetes OutlineJenny VargheseNo ratings yet
- Insulin Resistance.:) DocxDocument2 pagesInsulin Resistance.:) DocxHerbert Shirov Tendido SecurataNo ratings yet
- Hyperglycemic Crises: ReferralDocument51 pagesHyperglycemic Crises: ReferralKokohNo ratings yet
- GLUCOSE_HOMEOSTASIS[1]Document13 pagesGLUCOSE_HOMEOSTASIS[1]shreyamahajan010No ratings yet
- Pancreas: Cells and Secretions of The Pancreatic IsletsDocument8 pagesPancreas: Cells and Secretions of The Pancreatic IsletsansahNo ratings yet
- Group 3 Concepcion Contacto Cordero Cornejo Cornell Cortez CruzDocument62 pagesGroup 3 Concepcion Contacto Cordero Cornejo Cornell Cortez CruzConcepcion Kevin ChuckNo ratings yet
- Diabetes MellitusDocument13 pagesDiabetes MellitusGeoffreyNo ratings yet
- Diabetes Mellitus Final SibiDocument62 pagesDiabetes Mellitus Final SibiSibi JohnNo ratings yet
- DR - Mohammed Qasim 2017-2018 4 GradeDocument40 pagesDR - Mohammed Qasim 2017-2018 4 GradeFarah Bashar Al-RawachyNo ratings yet
- Blood Glucose (Homeostasis)Document17 pagesBlood Glucose (Homeostasis)areebaNo ratings yet
- Dilated Eye Exam: An Eye Care Professional Uses Eye Drops To Temporarily Widen, orDocument5 pagesDilated Eye Exam: An Eye Care Professional Uses Eye Drops To Temporarily Widen, orClare LsyNo ratings yet
- Appendix B Pathophysiology of DM Type 2Document20 pagesAppendix B Pathophysiology of DM Type 2Jennifer AlvarezNo ratings yet
- Risk Factors For Diabetes MellitusDocument16 pagesRisk Factors For Diabetes Mellitusavinash dhameriyaNo ratings yet
- Diabetes MellitusDocument31 pagesDiabetes MellitusElenaCondratscribdNo ratings yet
- Screening of Antidiabetic Drugs: Presented ByDocument35 pagesScreening of Antidiabetic Drugs: Presented BysharonNo ratings yet
- Anti-Diabetic Agents: DR - Jahid Head of Pharmacology Md-AucmsDocument65 pagesAnti-Diabetic Agents: DR - Jahid Head of Pharmacology Md-AucmsMuhamad HilmiNo ratings yet
- Pancreas 2021Document32 pagesPancreas 2021Dr. AliNo ratings yet
- DIABETISDocument52 pagesDIABETISNeeraja M SureshNo ratings yet
- Diabetes Mellitus Type 11Document44 pagesDiabetes Mellitus Type 11MARICRIS NEBIARNo ratings yet
- Diabetes Mellitus: - ClassificationDocument22 pagesDiabetes Mellitus: - ClassificationFernando Junior Parra UchasaraNo ratings yet
- Insulin and Oral Hypoglycemic AgentsDocument27 pagesInsulin and Oral Hypoglycemic Agentsapi-19916399100% (1)
- 01 - CLS 382 - 443 - DMDocument19 pages01 - CLS 382 - 443 - DMamalNo ratings yet
- Unit 5 Part 2 InsulinDocument68 pagesUnit 5 Part 2 InsulinKhairunnisa Loqman100% (1)
- Glucose, Part1Document33 pagesGlucose, Part1SarahNo ratings yet
- GI and Reproductive HormoneDocument74 pagesGI and Reproductive Hormonepranutan739No ratings yet
- Destruction of Alpha and Beta Cells of The PancreasDocument6 pagesDestruction of Alpha and Beta Cells of The PancreasMelodia Turqueza GandezaNo ratings yet
- Lecture16 Anti Diabetic DrugsDocument61 pagesLecture16 Anti Diabetic Drugsharis.18No ratings yet
- Course Name: Pharmacology Ii Course Code:Shs.314 Credit Hours: 2Hrs Lectures: 20 INSTRUCTOR: Dr. KhurramDocument27 pagesCourse Name: Pharmacology Ii Course Code:Shs.314 Credit Hours: 2Hrs Lectures: 20 INSTRUCTOR: Dr. KhurramAmynah WasimNo ratings yet
- Hypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandHypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Tender Bids From March 2012 To April 2017Document62 pagesTender Bids From March 2012 To April 2017scribd_109097762No ratings yet
- Contemporary World: Colt Ian U. Del CastilloDocument34 pagesContemporary World: Colt Ian U. Del CastilloNORBERT JAY DECLARONo ratings yet
- Satellite CommunicationsDocument57 pagesSatellite Communicationsheritage336No ratings yet
- Ahad NaamahDocument2 pagesAhad NaamahedoolawNo ratings yet
- BBB October 2023 Super SpecialsDocument4 pagesBBB October 2023 Super Specialsactionrazor38No ratings yet
- SY BSC IT SEM IV CORE JAVA UNIT 1Document56 pagesSY BSC IT SEM IV CORE JAVA UNIT 1stellaNo ratings yet
- Collections and Recollections by Russell, George William Erskine, 1853-1919Document202 pagesCollections and Recollections by Russell, George William Erskine, 1853-1919Gutenberg.org100% (1)
- Transmission System Pressure TestDocument3 pagesTransmission System Pressure TestFerdinand FernandezNo ratings yet
- Learn Computer in Simple StepsDocument104 pagesLearn Computer in Simple StepsSparkle SocietyNo ratings yet
- ChalazionDocument5 pagesChalazionSzakál Timea-BlankaNo ratings yet
- FisheriesDocument31 pagesFisheriesGarima LoonaNo ratings yet
- Premier's Technology Council: A Vision For 21st Century Education - December 2010Document51 pagesPremier's Technology Council: A Vision For 21st Century Education - December 2010The Georgia StraightNo ratings yet
- The Wholly BibleDocument10 pagesThe Wholly BibleFred_Carpenter_12No ratings yet
- El Ensayo Del Gato NegroDocument4 pagesEl Ensayo Del Gato Negroafefhrxqv100% (1)
- Comparison of Starbucks With The Coffee BeanDocument16 pagesComparison of Starbucks With The Coffee BeanshaiNo ratings yet
- 11 Business Studies SP 1Document11 pages11 Business Studies SP 1Meldon17No ratings yet
- December 2023 1Document14 pagesDecember 2023 1febri.putra7280No ratings yet
- Karakteristik Material Baja St.37 Dengan Temperatur Dan Waktu Pada Uji Heat Treatment Menggunakan FurnaceDocument14 pagesKarakteristik Material Baja St.37 Dengan Temperatur Dan Waktu Pada Uji Heat Treatment Menggunakan FurnaceYudii NggiNo ratings yet
- World Red Cross DayDocument17 pagesWorld Red Cross DayAshwani K SharmaNo ratings yet
- Brgy - OrdinanceDocument4 pagesBrgy - OrdinanceJulie Faith Aquimba Bulan100% (1)
- E M II: Synchronous MachineDocument10 pagesE M II: Synchronous MachineAkashman ShakyaNo ratings yet
- FSA Enrollment Form - English PDFDocument1 pageFSA Enrollment Form - English PDFLupita MontalvanNo ratings yet
- Oracle Weblogic Server 12c Troubleshooting WorkshopDocument3 pagesOracle Weblogic Server 12c Troubleshooting WorkshopMarcelo BerriosNo ratings yet
- Print 2 PDFDocument6 pagesPrint 2 PDFChris ThomasNo ratings yet
- Project of WCM 19c0h008 Madhu MaamDocument41 pagesProject of WCM 19c0h008 Madhu MaamSourav TiwariNo ratings yet
- Fire-Surya ElectricalDocument6 pagesFire-Surya ElectricalSURAJ PratapNo ratings yet
Pancreatic Hormones
Pancreatic Hormones
Uploaded by
Bodea Doru100%(1)100% found this document useful (1 vote)
70 views41 pagesThis document summarizes pancreatic hormones and their role in glucose metabolism. It discusses how insulin and glucagon are secreted by the pancreas to regulate blood glucose levels. Insulin promotes glucose uptake and storage in liver and muscle, while inhibiting gluconeogenesis. It stimulates fat and protein synthesis. Glucagon has opposing effects, stimulating glycogenolysis and gluconeogenesis in the liver. The document also describes the causes, symptoms, and diagnosis of Type 1 and Type 2 diabetes, which result from insulin deficiency and insulin resistance, respectively.
Original Description:
Endo-Pancreatic
Original Title
pancreatic hormones
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document summarizes pancreatic hormones and their role in glucose metabolism. It discusses how insulin and glucagon are secreted by the pancreas to regulate blood glucose levels. Insulin promotes glucose uptake and storage in liver and muscle, while inhibiting gluconeogenesis. It stimulates fat and protein synthesis. Glucagon has opposing effects, stimulating glycogenolysis and gluconeogenesis in the liver. The document also describes the causes, symptoms, and diagnosis of Type 1 and Type 2 diabetes, which result from insulin deficiency and insulin resistance, respectively.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
100%(1)100% found this document useful (1 vote)
70 views41 pagesPancreatic Hormones
Pancreatic Hormones
Uploaded by
Bodea DoruThis document summarizes pancreatic hormones and their role in glucose metabolism. It discusses how insulin and glucagon are secreted by the pancreas to regulate blood glucose levels. Insulin promotes glucose uptake and storage in liver and muscle, while inhibiting gluconeogenesis. It stimulates fat and protein synthesis. Glucagon has opposing effects, stimulating glycogenolysis and gluconeogenesis in the liver. The document also describes the causes, symptoms, and diagnosis of Type 1 and Type 2 diabetes, which result from insulin deficiency and insulin resistance, respectively.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 41
Pancreatic hormones and
glucose metabolism
Dr. Isabel Hwang
Department of Physiology
Faculty of Medicine
University of Hong Kong
May 2007
(isabelss@hkucc.hku.hk)
Hormones important for glucose
metabolism
Blood glucose
Pancreas Insulin
Glucagon
Adrenal Cortisol
Epinephrine
Pituitary Growth hormone
Structure of the pancreas
2 major types of tissues
1. acini- secretes digestive juices into the
duodenum
2. The islets of Langerhans-secretes insulin
and glucagon into blood
The human pancreas bears 1 to 2 million islets of
Langerhands with 3 different types of cells
Alpha cells- 25% of total cells, secrete glucagon
Beta cells- 60% of total cells, secrete insulin and amylin
Delta cells- ~10% of total cells, secrete somatostatin
PP cells- secretes pancreatic polypeptide
Islets are richly
vascularised
Although islets comprise
only 1-2% of the mass of
the pancreas, they
receive about 10 to 15%
of the pancreatic blood
flow
They are innervated by
parasympathetic and
sympathetic neurons
In addition to blood
glucose changes,
nervous signals also
modulate secretion of
insulin and glucagon.
Structure of insulin
Small protein, with a
molecular weight (about
6000 Da)
2 chains (A- 21 a.a.; B-
30 a.a.)
Amino acid sequence is
highly conserved
among vertebrates,
many diabetic patients
are treated with insulin
extracted from pig and
cow pancreases.
Insulin and glucagon are critical participants
in glucose homeostasis and serve as acute
regulators of blood glucose concentration
Physiological effects
1. Carbohydrate Metabolism
- Insulin promotes muscle glucose uptake and
metabolism
- Normal resting muscle membrane is not highly
permeable to glucose, except when stimulated by
insulin
- Insulin stimulates glycogen storage in muscle
- Insulin facilitates glucose transport through the
muscle cell membrane
- Insulin promotes liver uptake, liver storage and use
of glucose
- Insulin promotes conversion of excess glucose into
fatty acids and inhibits gluconeogenesis in the liver
Mechanism of increased glucose
uptake and liver storage by insulin
1. Insulin inactivates liver phosphorylase, the enzyme
that converts glycogen to glucose
2. Insulin enhanced uptake of glucose from the blood
by increasing activity of an enzyme called
glucokinase (to phosphorylates glucose after it
diffuses into liver cells)
3. Insulin stimulates the activity of glycogen
synthase which promotes glycogen synthesis
Net effect: To increase amount of glycogen in liver
Insulin-independent effect
The brain cells normally use glucose for
energy
Therefore, the brain cells are permeable to
glucose and can utilize glucose
independently of the effect exerted by
insulin
2. Fat metabolism
- Insulin promotes fat synthesis and storage in
adipose tissue (fat-sparing effect)
- This is especially true when liver is saturated with
glycogen (5-6% of total liver mass), additional
glucose will be converted to fat
(glucosepyruvate acetyl coenzyme A
fatty acid)
- Insulin inhibits lipase activity which causes
hydrolysis of triglycerides
- Insulin also promotes glucose transport through
the cell membrane into fat cells to form glycerol
and small amount of fatty acid
3. Protein metabolism
- Insulin promotes protein synthesis and storage
- Insulin stimulates uptake of amino acid into cells
- Insulin activates translation of mRNA and
sometimes transcriptional rate and therefore
making new proteins
- Insulin inhibits the catabolism of proteins and thus
decreases the rate of amino acid releae into the
blood from cells, esp the muscle cells
- In liver, insulin inhibits the rate of
gluconeogenesis
Insulin lack causes
1. Increased plasma cholesterol and
phospholipids concentrations (due to excess
fatty acids)
2. Increased release of acetoacetic acid (ketone
bodies) from fatty acid oxidation and leads to
ketoacidosis
3. Increased protein breakdown (protein wasting)
and increased plasma amino acids and
therefore leads to enhanced urea excretion
Major
response of
target cells to
insulin
Stimulation of glucose transporter translocation by insulin in
muscle and adipocyte
Regulation of insulin secretion.
1. Negative feed-back by glucose.
(glucose stimulates)
2. Amino acids. (proteins).
3. Free fatty acids
3. Hormones.
GH, cortisol, adrenaline,
glucagon
GI hormones
4. Neural.
parasympathetic (stimulates)
sympathetic (inhibits)
Glucagon
- Linear peptide of 29 amino
acids
- Its primary sequence is
almost perfectly conserved
among vertebrates
- The major effect of glucagon
is to stimulate an increase in
blood concentration of glucose
Physiological effects of glucagon.
1. glycogenolysis (liver).
2. gluconeogenesis (liver).
3. lipolysis (adipose tissue,
minor)
Regulation of glucagon secretion.
1. Negative feed-back.
(glucose suppresses)
*2. Amino-acids (gluconeogenesis, e.g. after
protein rich meals)
(prevent hypoglycaemia)
3. Sympathetic nervous system stimulates.
4. Effect of insulin lack. (Insulin inhibits)
5. Exercise
*Since high blood levels of amino acids also stimulate
insulin release, this would be a situation in which both
insulin and glucagon are active.
Insulin Deficiency
Two principal forms
1. Type I or insulin-dependent diabetes
mellitus (IDDM), is caused by lack of insulin
secretion
2. Type II or non-insulin-dependent diabetes
mellitus, is caused by decreased sensitivity
of target tissues to the metabolic effect of
insulin (insulin resistance)
Type I or insulin-dependent diabetes
mellitus
Result of a deficiency of insulin.
Onset is typically in childhood (at about 14
years of age in US)
Due to destruction pancreatic B cells, most
likely the result of autoimmunity or viral
infections to one or more components of those
cells.
May have heredity tendency for beta cell
degeneration even in the absence of viral
infections or autoimmune disorders
Type I diabetes
Can develop abruptly in a period of few days
or weeks
1. blood glucose surge
2. Increased utilization of fats for energy
and formation of cholesterol by the liver
3. Increased protein breakdown
Consequences
1. High levels of blood glucose (100mg/dl up to
300-1200mg/dl)
2. Loss of glucose in urine
3. Dehydration
4. Tissue injury due to chronic high glucose level
(inadequate blood supply to the tissues leads to
increased risk of heart attack, stroke, kidney
disease, retinopathy and blindness, and
ischemia of the limbs)
5. Metabolic acidosis (pH 7.4 pH 6.9) due to
increased utilization of fat
6. Weight loss
7. Lack of energy
Physiological compensations for
metabolic acidosis
1. In lungs, hyperventilation helps to
remove excessive carbon dioxide (also
at expense of some bicarbonate as well)
2. In kidneys, excretion of bicarbonate will
be reduced together with increased
production of new bicarbonate to be
added back to the extracellular fluid
Type II or non-insulin-dependent diabetes
mellitus
Result of insulin resistance
Target tissues fail to respond appropriately to insulin.
The onset of this disease is in adulthood (after 30
years of age).
Accounts for ~90% of all diabetic cases
Is associated with increased plasma insulin
concentration (hyperinsulinemia) which is a
compensatory response by the pancreatic beta cells
for reduced sensitivity of target cells to insulin
The decrease in insulin sensitivity impairs
carbohydrate utilization and storage and raises blood
glucose level and therefore stimulating a
compensatory increase in insulin secretion
The culprit for Type II diabetes is obesity
and excess weight gain
Several studies have linked obesity with
decreased insulin receptors esp. in the
skeletal muscle, adipose tissue and liver
However, most of the insulin resistance
seems to be caused by abnormalities of
the signaling pathway mediated by insulin
Insulin resistance
Forms part of the cascade of metabolic
symptoms which have the following
features
1. Obesity
2. Insulin resistance
3. Fasting hyperglycaemia
4. Increased blood triglycerides and decreased
blood (high-density lipoprotein)cholesterol
5. Hypertension
Other factors that can cause insulin
resistance and Type II diabetes
1. Cushing syndrome/acromegaly/steroid
therapy have been suggested to
decrease the sensitivity of certain tissues
to the metabolic effects of insulin
2. Polycystic ovary syndrome (PCOS)
increases ovarian androgen production
and insulin resistance; insulin resistance
and hyperinsulinemia appears to be
found in ~80% of affected women
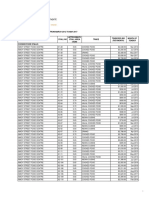
Clinical features of Type I and Type II diabetes
Feature Type I Type II
Age at onset <20 years >30 years
Body mass Low to normal Obese
Plasma insulin Low or absent Normal to high
Plasma glucagon High, High, resistant
can be suppressed to suppression
Plasma glucose Increased Increased
Insulin sensitivity Normal Reduced
Therapy Insulin Weight loss,
insulin
Diagnosis
1. Urinary glucose
2. Fasting blood glucose and insulin levels
- normal level is 90mg/dl, upper limit of normal is
110mg/dl, anything above indicates DM or
marked insulin resistance
- In type I diabetes, plasma insulin levels are
low or undetectable during fasting and
sometimes even after a meal
- in type II diabetes, plasma insulin may be
several fold higher in conc. than normal and
usually increases to greater extent after
ingestion of glucose
Diagnosis
3. Glucose tolerance test
- When a normal fasting person ingests 1g of glucose
(per kg body weight), the blood glucose level rises
from about 90mg/dl to 120mg/dl to 140mg/dl and
falls back to below normal in about 2 hours
- In persons with diabetes, the fasting blood glucose
conc. is always above 110mg/dl and often above
140mg/dl
- With ingestion of glucose, diabetic people show a
much greater increase in blood glucose level than
normal people and it usually takes longer for the
glucose level to fall back to normal (4-6 hours)
- Also, it fails to fall below the control level
Diagnosis
4. Acetone breath
- The presence of acetoacetic acid in the
blood is greatly elevated in severe
diabetes and they will be converted to
acetone
- Acetone is volatile and vaporized into the
expired air
- Ketoacids can also be determined in the
urine by common lab test
Treatment
In type I diabetes- insulin replacement
therapy
In type II diabetes- diet and exercise to
reduce weight and to reverse insulin
resistance; also exogenous insulin to
regulate blood glucose
Hyperinsulinemia (excessive insulin
secretion)
Result of an insulin-secreting tumor.
~10-15% of these adenoma are malignant
This condition is much less common than diabetes
mellitus.
Causes a precipitious drop in blood glucose
The brain becomes starved for energy, leading to the
syndrome of insulin shock, which is acutely life-
threatening.
Usually, ~1000g glucose has to be administered
every 24 hours to prevent hypoglycemia in some
patients
Glucagon deficiency or excess
Diseases associated with hypo- or hypersecretion
of glucagon are rare.
Cancers of alpha cells (glucagonomas) are one
condition known to cause excessive glucagon
secretion.
These tumors typically lead to a wasting syndrome
and, interestingly, rash and other skin lesions.
Many diabetic patients with hyperglycemia also
have elevated blood concentrations of glucagon,
but glucagon secretion is normally suppressed by
elevated levels of blood glucose.
You might also like
- Rebirth of The Useless Bastard SonDocument32 pagesRebirth of The Useless Bastard Sonthe.untamed.annaNo ratings yet
- Fce 2015 Complete Tests 1 e 2 AnswersDocument4 pagesFce 2015 Complete Tests 1 e 2 AnswersMárcia Bonfim83% (23)
- Anti Diabetic DrugsDocument58 pagesAnti Diabetic DrugsDaniel Wang100% (1)
- Establish Kinder Garden School - Develope Project ManagerDocument25 pagesEstablish Kinder Garden School - Develope Project ManagerVõ Thúy Trân0% (1)
- Mathematics of InvestmentsDocument2 pagesMathematics of InvestmentsShiera Saletrero SimbajonNo ratings yet
- 9 Diabetes Mellitus PHYSIOLOGYDocument22 pages9 Diabetes Mellitus PHYSIOLOGYEman KhammasNo ratings yet
- 14 - Blood Glucose HomeostasisDocument34 pages14 - Blood Glucose HomeostasischeckmateNo ratings yet
- Blood GlucoseDocument8 pagesBlood Glucoseعبدالرحمن عابدNo ratings yet
- Pathophysiology of DiabetesDocument88 pagesPathophysiology of DiabetesCahya SetiyaNo ratings yet
- Classifications of Insulin2Document116 pagesClassifications of Insulin2loglesb1No ratings yet
- Insulin and The Oral HypoglycemicsDocument9 pagesInsulin and The Oral HypoglycemicsHasibNo ratings yet
- Anti-Diabetic Drugs: Siti Farah MD Tohid (PHD)Document39 pagesAnti-Diabetic Drugs: Siti Farah MD Tohid (PHD)Nurul Mursyidah ZakariaNo ratings yet
- Glucose Homeostasis Disorders: by Julyn Marie Elnas Abad-GallardoDocument53 pagesGlucose Homeostasis Disorders: by Julyn Marie Elnas Abad-GallardoMarielle J GarciaNo ratings yet
- AntidiabetesDocument51 pagesAntidiabetesPuri Ratna KartiniNo ratings yet
- Physiology of Diabetes: Dr. Solomon Sathishkumar. MDDocument36 pagesPhysiology of Diabetes: Dr. Solomon Sathishkumar. MDKhaled LajmiNo ratings yet
- What Are The Cellular and Molecular Actions of Insulin?Document13 pagesWhat Are The Cellular and Molecular Actions of Insulin?Elle ReyesNo ratings yet
- Diabetes Mellitus and Laboratory Tests of DiabetesDocument24 pagesDiabetes Mellitus and Laboratory Tests of DiabetesturkiNo ratings yet
- Diabetes and PregnancyDocument49 pagesDiabetes and PregnancyCHRISTIAN SIDAYANo ratings yet
- Common Endocrine Disorders: Iril I. Panes, RN, MANDocument63 pagesCommon Endocrine Disorders: Iril I. Panes, RN, MANJona Phie Domingo MonteroNo ratings yet
- Diabetes1Document150 pagesDiabetes1Phyan HyunNo ratings yet
- Anti-Diabetic Drugs Part A-2Document35 pagesAnti-Diabetic Drugs Part A-2rimsha waseemNo ratings yet
- Diabetes MellitusDocument150 pagesDiabetes MellitusIan Mizzel A. Dulfina100% (1)
- CP2 MidtermsDocument278 pagesCP2 MidtermsDiana WadwasinNo ratings yet
- Pancreatic Hormones and The Treatment of Diabetes MellitusDocument46 pagesPancreatic Hormones and The Treatment of Diabetes MellitusasmaNo ratings yet
- Carbohydrates HandoutDocument15 pagesCarbohydrates HandoutnullNo ratings yet
- Hand Out DM Medical Surgical Nursing 2Document11 pagesHand Out DM Medical Surgical Nursing 2Zarlou OtamiasNo ratings yet
- DiabetesDocument10 pagesDiabetesLyNo ratings yet
- نسخة Blood Glucose 9Document16 pagesنسخة Blood Glucose 9نوف الحربي.No ratings yet
- Diabetes AssignmentDocument8 pagesDiabetes AssignmentMildred Obeng AgyeiwaaNo ratings yet
- Diabetes Millitus PDFDocument41 pagesDiabetes Millitus PDFAbdullah BhattiNo ratings yet
- Dr. Solomon Sathishkumar, MD Department of Physiology Christian Medical College Vellore, IndiaDocument48 pagesDr. Solomon Sathishkumar, MD Department of Physiology Christian Medical College Vellore, IndiaKrairat KomdeeNo ratings yet
- Presented by DR Ashish Sharma Guided by DR Meena PatelDocument74 pagesPresented by DR Ashish Sharma Guided by DR Meena PatelAndrew Surya Putra SccNo ratings yet
- Nursing Care of Patients With Diabetes MellitusDocument43 pagesNursing Care of Patients With Diabetes MellitusRashida RuwaNo ratings yet
- Pathophysiology Notes: Diabetes Mellitus Is A Group of Metabolic Disorders Characterized HyperglycemiaDocument14 pagesPathophysiology Notes: Diabetes Mellitus Is A Group of Metabolic Disorders Characterized HyperglycemiaHaifa ibrahimNo ratings yet
- Diabetes OutlineDocument7 pagesDiabetes OutlineJenny VargheseNo ratings yet
- Insulin Resistance.:) DocxDocument2 pagesInsulin Resistance.:) DocxHerbert Shirov Tendido SecurataNo ratings yet
- Hyperglycemic Crises: ReferralDocument51 pagesHyperglycemic Crises: ReferralKokohNo ratings yet
- GLUCOSE_HOMEOSTASIS[1]Document13 pagesGLUCOSE_HOMEOSTASIS[1]shreyamahajan010No ratings yet
- Pancreas: Cells and Secretions of The Pancreatic IsletsDocument8 pagesPancreas: Cells and Secretions of The Pancreatic IsletsansahNo ratings yet
- Group 3 Concepcion Contacto Cordero Cornejo Cornell Cortez CruzDocument62 pagesGroup 3 Concepcion Contacto Cordero Cornejo Cornell Cortez CruzConcepcion Kevin ChuckNo ratings yet
- Diabetes MellitusDocument13 pagesDiabetes MellitusGeoffreyNo ratings yet
- Diabetes Mellitus Final SibiDocument62 pagesDiabetes Mellitus Final SibiSibi JohnNo ratings yet
- DR - Mohammed Qasim 2017-2018 4 GradeDocument40 pagesDR - Mohammed Qasim 2017-2018 4 GradeFarah Bashar Al-RawachyNo ratings yet
- Blood Glucose (Homeostasis)Document17 pagesBlood Glucose (Homeostasis)areebaNo ratings yet
- Dilated Eye Exam: An Eye Care Professional Uses Eye Drops To Temporarily Widen, orDocument5 pagesDilated Eye Exam: An Eye Care Professional Uses Eye Drops To Temporarily Widen, orClare LsyNo ratings yet
- Appendix B Pathophysiology of DM Type 2Document20 pagesAppendix B Pathophysiology of DM Type 2Jennifer AlvarezNo ratings yet
- Risk Factors For Diabetes MellitusDocument16 pagesRisk Factors For Diabetes Mellitusavinash dhameriyaNo ratings yet
- Diabetes MellitusDocument31 pagesDiabetes MellitusElenaCondratscribdNo ratings yet
- Screening of Antidiabetic Drugs: Presented ByDocument35 pagesScreening of Antidiabetic Drugs: Presented BysharonNo ratings yet
- Anti-Diabetic Agents: DR - Jahid Head of Pharmacology Md-AucmsDocument65 pagesAnti-Diabetic Agents: DR - Jahid Head of Pharmacology Md-AucmsMuhamad HilmiNo ratings yet
- Pancreas 2021Document32 pagesPancreas 2021Dr. AliNo ratings yet
- DIABETISDocument52 pagesDIABETISNeeraja M SureshNo ratings yet
- Diabetes Mellitus Type 11Document44 pagesDiabetes Mellitus Type 11MARICRIS NEBIARNo ratings yet
- Diabetes Mellitus: - ClassificationDocument22 pagesDiabetes Mellitus: - ClassificationFernando Junior Parra UchasaraNo ratings yet
- Insulin and Oral Hypoglycemic AgentsDocument27 pagesInsulin and Oral Hypoglycemic Agentsapi-19916399100% (1)
- 01 - CLS 382 - 443 - DMDocument19 pages01 - CLS 382 - 443 - DMamalNo ratings yet
- Unit 5 Part 2 InsulinDocument68 pagesUnit 5 Part 2 InsulinKhairunnisa Loqman100% (1)
- Glucose, Part1Document33 pagesGlucose, Part1SarahNo ratings yet
- GI and Reproductive HormoneDocument74 pagesGI and Reproductive Hormonepranutan739No ratings yet
- Destruction of Alpha and Beta Cells of The PancreasDocument6 pagesDestruction of Alpha and Beta Cells of The PancreasMelodia Turqueza GandezaNo ratings yet
- Lecture16 Anti Diabetic DrugsDocument61 pagesLecture16 Anti Diabetic Drugsharis.18No ratings yet
- Course Name: Pharmacology Ii Course Code:Shs.314 Credit Hours: 2Hrs Lectures: 20 INSTRUCTOR: Dr. KhurramDocument27 pagesCourse Name: Pharmacology Ii Course Code:Shs.314 Credit Hours: 2Hrs Lectures: 20 INSTRUCTOR: Dr. KhurramAmynah WasimNo ratings yet
- Hypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandHypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Tender Bids From March 2012 To April 2017Document62 pagesTender Bids From March 2012 To April 2017scribd_109097762No ratings yet
- Contemporary World: Colt Ian U. Del CastilloDocument34 pagesContemporary World: Colt Ian U. Del CastilloNORBERT JAY DECLARONo ratings yet
- Satellite CommunicationsDocument57 pagesSatellite Communicationsheritage336No ratings yet
- Ahad NaamahDocument2 pagesAhad NaamahedoolawNo ratings yet
- BBB October 2023 Super SpecialsDocument4 pagesBBB October 2023 Super Specialsactionrazor38No ratings yet
- SY BSC IT SEM IV CORE JAVA UNIT 1Document56 pagesSY BSC IT SEM IV CORE JAVA UNIT 1stellaNo ratings yet
- Collections and Recollections by Russell, George William Erskine, 1853-1919Document202 pagesCollections and Recollections by Russell, George William Erskine, 1853-1919Gutenberg.org100% (1)
- Transmission System Pressure TestDocument3 pagesTransmission System Pressure TestFerdinand FernandezNo ratings yet
- Learn Computer in Simple StepsDocument104 pagesLearn Computer in Simple StepsSparkle SocietyNo ratings yet
- ChalazionDocument5 pagesChalazionSzakál Timea-BlankaNo ratings yet
- FisheriesDocument31 pagesFisheriesGarima LoonaNo ratings yet
- Premier's Technology Council: A Vision For 21st Century Education - December 2010Document51 pagesPremier's Technology Council: A Vision For 21st Century Education - December 2010The Georgia StraightNo ratings yet
- The Wholly BibleDocument10 pagesThe Wholly BibleFred_Carpenter_12No ratings yet
- El Ensayo Del Gato NegroDocument4 pagesEl Ensayo Del Gato Negroafefhrxqv100% (1)
- Comparison of Starbucks With The Coffee BeanDocument16 pagesComparison of Starbucks With The Coffee BeanshaiNo ratings yet
- 11 Business Studies SP 1Document11 pages11 Business Studies SP 1Meldon17No ratings yet
- December 2023 1Document14 pagesDecember 2023 1febri.putra7280No ratings yet
- Karakteristik Material Baja St.37 Dengan Temperatur Dan Waktu Pada Uji Heat Treatment Menggunakan FurnaceDocument14 pagesKarakteristik Material Baja St.37 Dengan Temperatur Dan Waktu Pada Uji Heat Treatment Menggunakan FurnaceYudii NggiNo ratings yet
- World Red Cross DayDocument17 pagesWorld Red Cross DayAshwani K SharmaNo ratings yet
- Brgy - OrdinanceDocument4 pagesBrgy - OrdinanceJulie Faith Aquimba Bulan100% (1)
- E M II: Synchronous MachineDocument10 pagesE M II: Synchronous MachineAkashman ShakyaNo ratings yet
- FSA Enrollment Form - English PDFDocument1 pageFSA Enrollment Form - English PDFLupita MontalvanNo ratings yet
- Oracle Weblogic Server 12c Troubleshooting WorkshopDocument3 pagesOracle Weblogic Server 12c Troubleshooting WorkshopMarcelo BerriosNo ratings yet
- Print 2 PDFDocument6 pagesPrint 2 PDFChris ThomasNo ratings yet
- Project of WCM 19c0h008 Madhu MaamDocument41 pagesProject of WCM 19c0h008 Madhu MaamSourav TiwariNo ratings yet
- Fire-Surya ElectricalDocument6 pagesFire-Surya ElectricalSURAJ PratapNo ratings yet





































![GLUCOSE_HOMEOSTASIS[1]](https://imgv2-1-f.scribdassets.com/img/document/747352994/149x198/94f3bf247e/1719941429?v=1)