Professional Documents
Culture Documents
Comp Cogn Beh Therapy 2
Comp Cogn Beh Therapy 2
Uploaded by
inanna12Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Comp Cogn Beh Therapy 2
Comp Cogn Beh Therapy 2
Uploaded by
inanna12Copyright:
Available Formats
Journal of Psychiatric and Mental Health Nursing,
2004,
11
, 508513
508
2004 Blackwell Publishing Ltd
VAN DEN BERG S., SHAPIRO D. A., BICKERSTAFFE D. & CAVANAGH K. (2004)
Journal of Psychiatric and Mental Health Nursing
11
, 508513
Computerized cognitivebehaviour therapy for anxiety and depression: a practical
solution to the shortage of trained therapists
Computerized cognitivebehaviour therapy (CCBT) programmes have been developed to
help meet the enormous need for evidence-based psychological treatment of common men-
tal health problems in the context of a severe shortage of trained therapists to meet that
need. Randomized controlled trials have conrmed the efcacy of such programmes. We
present the experience of a community mental health team (CMHT) resource centre with
one such programme,
Beating the Blues
, together with outcome data on a small sample of
its clients. We conclude that experience and data, taken together, demonstrate the practical
benets of CCBT in routine practice.
Keywords
: anxiety, Beating the Blues, cognitive-behaviour therapy, computerized cognitive-
behaviour therapy, computerized therapy, depression
Accepted for publication
:
6 February 2004
Blackwell Science, LtdOxford, UKJPMJournal of Psychiatric and Mental Health Nursing1351-0126Blackwell Publishing Ltd, 2004
11508513
Original Article
Computerized cognitivebehaviour therapyS. van den Berg
et al.
Computerized cognitivebehaviour therapy for anxiety and
depression: a practical solution to the shortage of trained therapists
S . VAN DEN BERG
1
B S
c , D. A. SHAPI RO
2
B A
MS
c
P
h
D
F B P
s
S
CP
s y c hol ,
D. BI CKERSTAFFE
3
RMN
P G
r ad
D
i p
M
ana g e me nt & K. CAVANAGH
4
DP
hi l
CP
s y c hol
1
Psychologist,
4
Senior Psychologist, Ultrasis plc, London, UK,
2
Honorary Professor, University of Leeds, Leeds, UK
and University of Shefeld, Shefeld, UK, and
3
Locality Manager, Doncaster West Community Mental Health Team,
Stapleton Road Mental Health Resource Centre, Doncaster, UK
Correspondence:
S. van den Berg
19 Rosebery Street
Fisher
ACT, 2611
Australia
Introduction
Computerized cognitivebehaviour therapy (CCBT) is
attracting increasing attention in mental health care. Most
recently, the National Institute for Clinical Excellence
(NICE) (2002) has issued guidance indicating that this
may be of value in the management of anxiety and depres-
sive disorders. For mental health nurses and others consid-
ering the use of this technology, several questions may
arise:
Why should clinical services consider the use of
CCBT?
Is there sufcient evidence from randomized con-
trolled trials (RCTs) to warrant belief in the efcacy
of such treatment?
How effective, in terms of achieving clinical improve-
ment in everyday practice, is such treatment?
What is it like to offer such treatment, in terms of
practical and logistic arrangements, and client and
staff experiences?
In this paper, we address these questions in relation to
the experience of a secondary mental health care service
that has used the CCBT programme,
Beating the Blues
.
Why should clinical services consider the use
of CCBT?
Anxiety and depression are the most common mental
health problems, and the total burden they place on the
health of the community and on health care services out-
weighs that of more severe problems such as schizophre-
nia (Singleton
et al
. 2001). An estimated 20% of people
will suffer with anxiety and/or depression in any given
year, most of whom are treated within primary care. Cli-
2004 Blackwell Publishing Ltd,
Journal of Psychiatric and Mental Health Nursing
11
, 508513
509
Computerized cognitivebehaviour therapy
ents often refuse drug treatment or cease taking it. Client
demand and research data alike support the provision of
structured psychological treatments (Market & Opinion
Research International (MORI) poll for Defeat Depression
Campaign; Roth & Fonagy 1996). The National Service
Framework for Mental Health (Department of Health
1999) identies improved access to psychological treat-
ments as a key objective. Cognitivebehaviour therapy
(CBT) is the most thoroughly researched treatment of
depression and anxiety (Roth & Fonagy 1996, Watkins &
Williams 1998). However the availability of CBT falls far
short of the demand. It is labour-intensive and typically
requires 620 50-min sessions. There is a national short-
age of trained CBT therapists from all disciplines, whose
accessibility is further limited by their inequitable distribu-
tion across the country (Shapiro
et al.
2003).
Computer-delivered CBT offers a solution to this prob-
lem. It enables the principles and methods of CBT to be
made available to clients without requiring the presence of
a therapist. Growing evidence supports the efcacy of com-
puterized therapy (Kaltenthaler
et al
. 2002), and studies
have found equivalent efcacy of computer-delivered and
live or face-to-face CBT (Cavanagh
et al.
2003a,b). The
NICE guidance identies the potential of CCBT for anxiety
and depression and recommends its evaluation in the NHS
(NICE 2002). It considers the potential advantages of
CCBT to include accessibility, acceptability and increased
client choice, personalized treatment schedules, efciency,
availability of feedback, privacy, consistency of care and
ease of data collection.
Beating the Blues
is the most fully realized of the cur-
rently available CCBT programmes for anxiety and depres-
sion. It combines the principles and techniques of CBT with
interactive computer-based multimedia technology. In each
of its eight sessions, CBT principles and techniques are rst
explained, then illustrated by videos of ve patients using
them, and nally presented to the client for them to try
themselves.
Is there sufcient evidence from randomized
controlled trials to warrant belief in the
efcacy of such treatment?
The efcacy of
Beating the Blues
was established in a large
RCT, conducted in primary care (Proudfoot
et al
. 2003).
Clients who completed
Beating the Blues
showed signi-
cantly greater improvement in depression and anxiety, as
well as in work and social adjustment, compared to clients
receiving general practitioner (GP) treatment as usual
(TAU). These improvements were maintained up to
6 months follow up. The NICE guidance (NICE 2002, p.
10) acknowledges that the clinical efcacy of
Beating the
Blues
has been proven by RCT. As noted in the NICE guid-
ance, another programme,
Fearghter
, is also supported by
RCT evidence (Kaltenthaler
et al
. 2004). However, as its
name indicates, this programme specically targets anxiety
disorders and is therefore of less general applicability in
mental health care.
How effective, in terms of achieving clinical
improvement in everyday practice, is such
treatment? What is it like to offer such
treatment, in terms of practical and logistic
arrangements, and client and staff
experiences?
Despite recognizing that the clinical efcacy of
Beating the
Blues
is established, NICE also considered that its effec-
tiveness in routine practice was not established. There
exists a need for pragmatic implementation studies to
investigate the real-world value of
Beating the Blues
. The
present paper addresses this issue with reference to the
experiences of a community mental health team (CMHT)
resource centre. Here, we describe one services experience
with the programme, from acquisition to implementation
and the observed outcomes and impact of
Beating the Blues
on service provision.
Practicalities
Beating the Blues
is a stand-alone computer system which
is typically located within a general practice or mental
health centre. It is purchased as a complete system and the
price includes software, hardware, installation, training,
technical and clinical support. Clients with anxiety and/or
depression are assessed as suitable for the programme
based on a protocol agreed by the service. Those with
active suicidal plans, organic mental disorder, current diag-
nosis of psychosis or in the acute phase of drug or alcohol
dependence are not suitable for the programme.
Once a client has been referred to
Beating the Blues
,
they are given information sheets on the programme and
watch a 15-min introductory video, following which their
rst treatment session is booked. At each of the eight ses-
sions of about 1 h, a clinical helper, typically a receptionist,
greets the client and settles them on the computer. The
helpers location is made clear so that the client can nd
them should they require any assistance during the session.
Approximately 5 min of a clinical helpers time is needed
for each 1-h session of
Beating the Blues
. A dedicated room
is also important, so a client can be left to work on their
own without any interruption. At every session the client
completes simple self-ratings, on a 08 scale, of anxiety,
depression, and suicidal ideas. These are printed out for the
S. van den Berg
et al.
510
2004 Blackwell Publishing Ltd,
Journal of Psychiatric and Mental Health Nursing
11
, 508513
referring doctor or for whoever has clinical responsibility
for the client within the service.
Measures
Consecutive patients were screened for inclusion into the
trial using the General Health Questionnaire-12 (Goldberg
1972) and demographic information was collected. Before
commencing the programme, all patients were given infor-
mation on the evaluation of the programme and signed a
consent form in order to take part. No patients refused to
take part in the study.
The CCBT programme routinely collects weekly single-
item measures of anxiety and depression (from 0 not at all
anxious/depressed to 8 extremely anxious/depressed).
Clinical Outcomes in Routine Evaluation Outcome
Measure
(
CORE-OM,
CORE system group, 1998)
.
Con-
sisting of 34 items, the CORE is a self-report questionnaire
with subdomains for subjective well-being, problem/symp-
tom severity, life functioning and risk to self and others.
Treatment
Beating the Blues
, consists of nine treatment sessions, com-
prising a 15-min introductory video, viewed on the com-
puter, followed by eight interactive therapy sessions each
normally taken once a week completed in the routine care
setting. Each weekly session lasts about 50 min, with
homework projects between the sessions. Weekly progress
reports, including whether the patient has expressed any
suicidal intent, are generated and delivered to the GP or
therapist at the end of each session. A clinical helper (gen-
erally receptionist or secretary) greets the patient and
ensures that they are settled at the computer before leaving
the patient to work through the programme unattended.
The clinical helpers location is made clear should the
patient require assistance at any time during the session.
The interactive nature of the computer programme permits
customization to the patients specic needs, with each ses-
sion building on the one before.
The Doncaster experience
A nurse behavioural therapist who had seen
Beating the
Blues
demonstrated at a national conference suggested a
meeting to show the programme to the management of a
mental health resource centre. This demonstration per-
suaded one of us (D.B.), the service manager, of the feasi-
bility of implementing
Beating the Blues
and that its cost
compared very favourably with face-to-face therapy. The
attraction of
Beating the Blues
was that it could reduce
waiting times (which were then around 18 months and
lengthening) by offering an immediately accessible, proven
alternative to face-to-face therapy. D.B. welcomed the
prospect of a proven new technology and wanted to
encourage clients and staff to consider the widest possible
range of treatment options. Further meetings resulted in the
approval of a proposal to set up a six-site pilot project
across Doncaster, involving ve primary care practices and
D.B.s CMHT. In what follows, we focus on the experience
of the CMHT with
Beating the Blues
provided at its
resource centre
A key issue in the implementation of CCBT is the nature
and extent of support required by clients attending for ses-
sions with the programme. In the resource centre, support
has been provided by secretarial staff, after training on the
package. They spend 1015 min at the rst treatment ses-
sion explaining how the programme works, including the
use of passwords, printer, homework assignments, arrange-
ments for making further appointments, trouble shooting,
etc. This is considered a purely administrative support role,
with the friendly customer skills of the teams administra-
tive staff being the most appropriate for this, and clinical
input not being needed at this stage. Administrative staff
are also well-placed to promote a self-help, non-profession-
alized atmosphere around the clients use of the pro-
gramme. Subsequent sessions usually entail no more than a
23-min reminder of the practicalities around use of the
programme. Administrative staff were prepared for their
role by viewing the introductory videotape seen by clients,
followed by a 2-h training session provided by the supplier.
Initially there was a lot of both interest in and opposi-
tion to the programme. Most health professionals could see
the benets of the programme but there were a few who
remained explicitly sceptical. Client views on the pro-
gramme varied widely, from I need more than a computer
to Ill give it a try or even, I like not having to talk to
another person about these problems.
In contrast to the primary care settings of Proudfoot
et al.
s (2003) RCT, experience in Doncaster demonstrates
the value of
Beating the Blues
to a secondary care service
accepting referrals from GPs across a geographical area. As
is well known, GPs nd it hard to differentiate common
mental health problems that can be managed in primary
care from those requiring specialist input. In Doncaster, the
availability of
Beating the Blues
has enhanced the CMHTs
role as a single point of access to mental health care. The
CMHT can offer, equitably across its catchment area, an
evidence-based intervention to clients who would otherwise
have been sent back to the GP as insufciently severe or
complex cases to be offered secondary care, given the
unmanageably high demand for all psychological treatment
services. Resource centre clinical staff have been able to
choose, on the basis of individual client needs, between
2004 Blackwell Publishing Ltd,
Journal of Psychiatric and Mental Health Nursing
11
, 508513
511
Computerized cognitivebehaviour therapy
Beating the Blues
and other options including nurse behav-
iour therapists and primary care counsellors. Clinical staff
estimate that 6070% of referrals would benet from
Beat-
ing the Blues
, and in practice about half of these commence
using it. This clinical screening has also minimized the occa-
sions on which high client scores on the
Beating the Blues
weekly rating scales have required therapist intervention.
The immediate advantages for the service soon became
apparent in that reduced numbers were entering the CBT
waiting list, and
Beating the Blues
enabled the service to
offer immediate help to clients referred with mild to mod-
erate anxiety and/or depression. Service providers also wel-
comed the fact that
Beating the Blues
encouraged the client
to develop ways of helping themselves rather than to
become dependent upon a therapist.
In practical terms, once the service began to feel con-
dent about the programme, it became routine to offer it as
a rst line of treatment to the majority of individuals
referred with mild to moderate anxiety or depression. As a
way of addressing the ever-increasing waiting list for CBT,
letters were also sent out to all patients on the waiting list
offering
Beating the Blues
as an interim treatment. Several
GPs in the surrounding area referred directly to the pro-
gramme. Alongside the data collected for a multisite, for-
mal evaluation to be reported in a future paper, informal
client feedback was generally very positive, with particular
mention being made of the speed and ease of access to the
programme and how easy it was to use.
Few clients have commented unfavourably on their
experience of using the programme, with only a single
individual citing its being too difcult as a reason for
discontinuing its use. One difculty of implementing
Beating the Blues
at the Doncaster resource centre has
been that 52 of 115 patients (45%) starting the pro-
gramme have not completed it. This is a slightly higher
discontinuation rate than for other treatments. Staff have
considered this matter carefully. Their view is that to
consider discontinuance a failure of the programme
reects an inappropriately provider-centred rather than
client-centred perspective.
Beating the Blues
is not a
course of antibiotics that must be completed to be effec-
tive. Clients may choose to stop using the programme
because they have gained sufcient from it rather than
because it is not for them. On this analysis, the appropri-
ate metric for evaluating the clinical effectiveness of
Beat-
ing the Blues
would not be the proportion of clients
helped by being offered the full programme, but the
extent of client benet experienced per
Beating the Blues
session undertaken. Does the same metric apply to face-
to-face counselling? Or is this a completely unusual con-
cept? Patients who dropped out were not followed up at
the CMHT so reasons for discontinuation were not col-
lected, however, in the RCT various reasons were given
for discontinuation ranging from positive reasons (e.g.
they felt better), through neutral reasons (e.g. moved out
of the area) to negative reasons (e.g. they didnt feel the
programme was right for them).
Overall, the centres experience of
Beating the Blues
has
been a positive one; the programme is considered to have
made a real difference both to a large majority of clients
that have utilized it, and to the treatment options the ser-
vice can offer. Its ease of use, speed of access and proven
efcacy make it an important element of the repertoire of
therapy options available to the seemingly ever-growing
number of individuals with common mental health prob-
lems. The impact on waiting times has been to prevent any
increase beyond the pre-existing average of 1 year from ini-
tial assessment to treatment, despite an ever-increasing rate
of referrals for CBT.
Three case histories
Two individual clients illustrate favourable outcomes of
both uncompleted and completed
Beating the Blues
cases
observed at the Doncaster resource centre. A third client
however, felt that the programme did not meet their needs
at this time. Client 1 was a 66-year-old lady referred with
a 4-year history of mixed anxiety and depression who had
recently been prescribed antidepressant medication. She
dropped out at session 3 because she felt better able to deal
with her problems, reporting a drop over 4 weeks in anx-
iety and depression levels from 5 and 4, respectively, to 1
and 1. When it was suggested that she might benet from
completing the whole programme, she responded that the
initial explanation to the root causes of her anxiety and
depression, and the fact that these feelings were relatively
common in the rest of the population, had provided her
with answers that she had been looking for. She said that
these had spurred her on to manage her situation in a dif-
ferent way. Without the quick access to the programme this
lady would have been waiting a signicant period of time
to see a therapist and not have had the input she clearly
required.
Client 2 was a 53-year-old man with a 4-month history
of mixed anxiety and depression, who completed all eight
sessions of the programme. His anxiety and depression lev-
els dropped from a high in session 3 of 8 and 7, respec-
tively, to 2 and 1 by the end of the programme. When asked
to evaluate the programme he stated that after the initial
phase of getting to grips with some of the techniques
explained in the programme, he found himself looking at
things in a much more rational and logical way. Before this
he had a tendency to dramatize things and make mountains
out of molehills, which he recognized hadnt totally disap-
S. van den Berg
et al.
512
2004 Blackwell Publishing Ltd,
Journal of Psychiatric and Mental Health Nursing
11
, 508513
peared, but felt he could manage his thoughts, and
responses to his thoughts, more calmly, without letting
small things get him down. He was particularly impressed
with how easy the programme was to follow and claimed
that the weekly homework had helped him stay motivated
and interested in the programme thus making him turn up
every week.
Client 3 was a 34-year-old married woman who was
originally referred with generalized anxiety. She completed
three sessions of
Beating the Blues
after which she decided
to discontinue with the therapy. When asked why she
wanted to stop the sessions she felt she had found some of
the information useful and managed to understand a little
about why she became anxious and have some control over
some of her symptoms (e.g. panic attacks) but didnt think
she wanted to complete all eight sessions as she didnt
really see the point of interacting with a computer that
couldnt take part in a conversation. It was agreed that she
could restart the programme if she wanted to at a later
date, also if she felt that her symptoms were causing her
problems again that she could be referred to a face-to-face
therapist in the team. The client was happy with the out-
come.
Outcome data
This experience of the usability and practical benets of
Beating the Blues
at the resource centre is supported by
effectiveness data on a subset of the clients who have used
the programme. We present data from 13 clients as they
were the only ones to return completed CORE outcome
measures (Barkham
et al
. 2001) before and after treatment.
Repeated measures
t
-tests were applied to each CORE
subscale outcome measure. As shown in Table 1, despite
the small sample, statistically signicant improvements
were found in Well-being [
t
(12) = 7.675, P < 0.001], Prob-
lems [t(12) = 6.339, P < 0.001] and Functioning
[t(12) = 4.502, P < 0.05]; improvements in Risk were not
signicant. Risk scores were expected to be too low initially
to demonstrate signicant change as clients at high risk
were intentionally screened out. For all scales except Risk,
effect sizes were substantial, at over 1 standard deviation.
Six month follow up data from nine patients revealed sig-
nicant improvements in Well-being (P < 0.05). Although
improvements were evident in Problems, Functioning and
Risk following the programme, these were found not to be
signicant. Table 2 shows that on all indices except Risk,
11 of 13 clients were above the clinical cut-off dened by
Barkham et al. (2001) before undertaking Beating the
Blues; afterwards, this proportion was reduced to about
one half (either 5, 6 or 7 out of 13 on each index).
Analysis of self-reported anxiety and depression ratings
from 46 patients who completed the programme revealed
statistically signicant improvements from session 1 to ses-
sion 8 [anxiety: t(48) = 4.141, P < 0.001; depression:
t(48) = 3.972, P < 0.001]. Mean anxiety and depression
ratings at the rst session were 5.24 and 4.76, respectively,
compared with 4.15 and 3.65 at session 8.
Conclusion
Beating the Blues is a new and innovative way of delivering
CBT to the large number of clients with anxiety and/or
depression. The present report complements the demon-
stration of its efcacy in the RCT by Proudfoot et al. (in
press) by showing its practical value. This is apparent from
a services positive experience of Beating the Blues within its
mental health resource centre, together with illustrative
case histories and outcome data. This account has also pro-
vided insight into the obstacles and advantages associated
with implementing Beating the Blues in a real-world setting.
Even clients who discontinue use of the programme appear
to derive benet. As the boundaries between primary and
secondary mental health care are redrawn over the coming
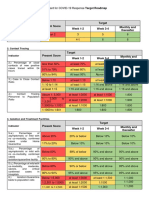
Table 1
CORE-outcome measure scores before and after Beating the Blues (n = 13)
CORE-OM scale Before Beating the Blues After Beating the Blues Effect size Signicance
CORE mean 1.85 1.28 1.10 P < 0.001
All non-risk items 2.30 1.52 1.42 P < 0.001
Well-being 2.54 1.50 1.44 P < 0.001
Problems 2.44 1.65 1.15 P < 0.001
Functioning 2.07 1.39 1.24 P < 0.005
Risk 0.36 0.19 0.34 NS
Table 2
Clients above CORE-outcome measure clinical cut-offs before and
after Beating the Blues (n = 13)
CORE-OM index
Before Beating
the Blues
After Beating
the Blues
Well-being 11 7
Problems 11 6
Functioning 11 6
Risk 4 3
All non-risk items 11 5
Mean item score 11 5
2004 Blackwell Publishing Ltd, Journal of Psychiatric and Mental Health Nursing 11, 508513 513
Computerized cognitivebehaviour therapy
years, CCBT has a signicant role to play at the interface,
however, this comes to be dened in a given locality.
References
Barkham M., Margison F., Leach C., Lucock M., Mellor-Clark J.,
Evans C., Benson L., Connell J. & Audin K. (2001) Service
proling and outcomes benchmarking using the CORE-OM:
toward practice-based evidence in the psychological therapies.
Journal of Consulting and Clinical Psychology 69, 184196.
Cavanagh K., Zack J. & Shapiro D.A. (2003a) Empirically sup-
ported computerised psychotherapy. In: Tele-psychiatry and E-
mental Health (eds Wootton, R., Yellowless, P. & McLaren, P.),
pp. 273290. Royal Society of Medicine Press, London.
Cavanagh K., Wright J.H., Zack J. & Shapiro D.A. (2003b)
Computer programmes for psychotherapy. In: Technology in
Counselling and Psychotherapy (eds Goss, S. & Amnthony, K.),
Palgrave, London.
Department of Health (1999) National Service Framework for
Mental Health. Department of Health, London.
Goldberg D.P. (1972) The detection of psychiatric illness by ques-
tionnaire (Maudsley Monograph No. 21). Oxford University
Press, Oxford.
Kaltenthaler E., Parry G. & Beverley C. (2004) Computerized
cognitive behaviour therapy: A systematic review. Behav-
ioural and Cognitive Psychotherapy 32, 3155.
National Institute for Clinical Excellence (NICE) (2002) Guid-
ance on the use of computerised cognitive-behaviour therapy
for anxiety and depression. Technology Appraisal
Guidance No. 51. Available at: http://www.nice.org.uk/pdf/
51_CCBT_Full_guidance.pdf
Proudfoot J., Goldberg D., Mann A., Everitt B., Marks I. & Gray
J. (2003) Computerized, interactive, multimedia cognitive-
behavioural therapy programme for anxiety and depression in
general practice. Psychological Medicine 33, 217227.
Roth A. & Fonagy P. (1996) What Works for Whom: a Critical
Review of Psychotherapy Research. Guilford Press, New York.
Shapiro D.A., Cavanagh K. & Lomas H. (2003) Geographic
inequity in the availability of cognitive behavioural therapy
in England and Wales. Behavioural and Cognitive Psycho-
therapy 31, 185192.
Singleton N., Bumpstead R., OBrien M., Lee A. & Meltzer H.
(2001) Psychiatric Morbidity Among Adults Living in Private
Households, 2000. The Stationery Ofce, London.
Watkins E. & Williams R. (1998) The efcacy of cognitive-
behavioural therapy. In: The Management of Depression (ed
Checkley, S), pp. 165187. Blackwell Science Ltd., Oxford.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Romantic AgonyDocument521 pagesThe Romantic Agonyinanna12100% (3)
- PlayingByTheRules Apexart PDFDocument178 pagesPlayingByTheRules Apexart PDFinanna12No ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Latin American Art of The 20th Century by Edward Lucie-SmithDocument220 pagesLatin American Art of The 20th Century by Edward Lucie-Smithinanna12100% (1)
- Twopri00weis PDFDocument876 pagesTwopri00weis PDFinanna1250% (2)
- The Pillow BookDocument284 pagesThe Pillow Bookinanna12100% (2)
- Animal Myth and Magic: Images From Pre-Columbian TextilesDocument168 pagesAnimal Myth and Magic: Images From Pre-Columbian Textilesinanna12100% (1)
- Brand Henrik Ibsen (Ebooksread - Com) PDFDocument248 pagesBrand Henrik Ibsen (Ebooksread - Com) PDFinanna120% (1)
- Iracmahoneylip00alenuoft PDFDocument268 pagesIracmahoneylip00alenuoft PDFinanna12No ratings yet
- Guided Self Help AnxietyDocument9 pagesGuided Self Help Anxietyinanna12No ratings yet
- Social Science Computer Review: Internet Abuse: Addiction? Disorder? Symptom? Alternative Explanations?Document11 pagesSocial Science Computer Review: Internet Abuse: Addiction? Disorder? Symptom? Alternative Explanations?inanna12100% (1)
- Digital Education ElearningDocument5 pagesDigital Education Elearninginanna12No ratings yet
- MODULE4Document38 pagesMODULE4Caryl SequitinNo ratings yet
- DCMSTIS-Senior Citizen Action Plan FY2022Document2 pagesDCMSTIS-Senior Citizen Action Plan FY2022Zoe GALLARDO33% (3)
- Wins Action PlanDocument3 pagesWins Action PlanCHRISTINE GASPACHO100% (1)
- Malariafinalthesis PDFDocument67 pagesMalariafinalthesis PDFVitalis MbuyaNo ratings yet
- Bell's Palsy - Symptoms and Causes - Mayo ClinicDocument6 pagesBell's Palsy - Symptoms and Causes - Mayo ClinicRoxan PacsayNo ratings yet
- 01f2 - ICD vs. DSM - APA PDFDocument1 page01f2 - ICD vs. DSM - APA PDFfuturistzgNo ratings yet
- A Review of Classification of Disease in AyurvedaDocument11 pagesA Review of Classification of Disease in AyurvedaEditor_IAIMNo ratings yet
- Megan Fish: 2781 Holman Drive Erie, PA 16509 (814) 460-9473Document2 pagesMegan Fish: 2781 Holman Drive Erie, PA 16509 (814) 460-9473MeganNo ratings yet
- Spinal Cord Injury Rehabilitation Webinar 2020 PDFDocument2 pagesSpinal Cord Injury Rehabilitation Webinar 2020 PDFGirijashankar KhuntiaNo ratings yet
- The in Uence of Impaction To The Third Molar Mineralization in Northwestern Chinese PopulationDocument8 pagesThe in Uence of Impaction To The Third Molar Mineralization in Northwestern Chinese PopulationIvan GalicNo ratings yet
- Modern and Classic Wound Dressing Comparison in WoDocument6 pagesModern and Classic Wound Dressing Comparison in WoJuan LuckyNo ratings yet
- Anesthesia Guide VASG 12-4-04Document164 pagesAnesthesia Guide VASG 12-4-04Radu TudorNo ratings yet
- Covid-19 and The Former Spanish Flu: PrevalenceDocument9 pagesCovid-19 and The Former Spanish Flu: PrevalenceAailaa SagharNo ratings yet
- A Model To Predict Short-Term Death or Readmission After Intensive Care Unit DischargeDocument10 pagesA Model To Predict Short-Term Death or Readmission After Intensive Care Unit DischargeInnani Wildania HusnaNo ratings yet
- Cot Demo Health 6-Guro21 - 3q - March 16 2023Document5 pagesCot Demo Health 6-Guro21 - 3q - March 16 2023Diego MapulaNo ratings yet
- OB NotesDocument2 pagesOB NotesJudy Ann CristeNo ratings yet
- Faris Akbar Ashari 30101407181Document25 pagesFaris Akbar Ashari 30101407181Fariseilaa PurakbarNo ratings yet
- Musculoskeletal Ultrasound Imaging Training, Use, and KnowledgeDocument10 pagesMusculoskeletal Ultrasound Imaging Training, Use, and KnowledgeChristian F. VegaNo ratings yet
- The Importance of Good PostureDocument1 pageThe Importance of Good Postureerica thapaNo ratings yet
- LipCancer BrachyDocument10 pagesLipCancer Brachyarungoel2No ratings yet
- AmputationDocument51 pagesAmputationStar CruiseNo ratings yet
- Skills Checklist Blood AdminDocument3 pagesSkills Checklist Blood AdmingtsantosNo ratings yet
- CHN Week 1 Day 2 and 3 Activity Initial Data BaseDocument6 pagesCHN Week 1 Day 2 and 3 Activity Initial Data BaseGailNo ratings yet
- Diabetic Foot Care Before and During The COVID-19 Epidemic: What Really Matters?Document2 pagesDiabetic Foot Care Before and During The COVID-19 Epidemic: What Really Matters?SitiNo ratings yet
- Medical Safety Clinical Reviewer in Chicago IL Resume Rachel DohrDocument3 pagesMedical Safety Clinical Reviewer in Chicago IL Resume Rachel DohrRachelDohr2No ratings yet
- Present Score Target Week 1-2 Week 3-4 Monthly and ThereafterDocument2 pagesPresent Score Target Week 1-2 Week 3-4 Monthly and ThereafterFret Ramirez Coronia RNNo ratings yet
- Reviewer Grade 12 Physical EducationDocument3 pagesReviewer Grade 12 Physical EducationKervin PlatonNo ratings yet
- Epirubicin: The Following Side Effects Are Common (Occurring in Greater Than 30%) For Patients Taking EpirubicinDocument5 pagesEpirubicin: The Following Side Effects Are Common (Occurring in Greater Than 30%) For Patients Taking EpirubicinSteffi EllaNo ratings yet
- DMMMSU-RETC-F013-Application For Ethics Review of A New ProtocolDocument4 pagesDMMMSU-RETC-F013-Application For Ethics Review of A New ProtocoluzamarknielconNo ratings yet
- Jospt 2009 2857Document11 pagesJospt 2009 2857Novy DitaNo ratings yet