Professional Documents
Culture Documents
Nuclear Medicine
Nuclear Medicine
Uploaded by
Jose NicoliellyOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nuclear Medicine
Nuclear Medicine
Uploaded by
Jose NicoliellyCopyright:
Available Formats
Nuclear medicine
1
Nuclear medicine
Nuclear medicine
Intervention
ICD-10-PCS
C
[1]
ICD-9:
92
[2]
MeSH
D009683
[3]
OPS-301code:
3-70
[4]
-3-72
[5]
, 8-53
[6]
Nuclear medicine is a medical specialty involving the application of radioactive substances in the diagnosis and
treatment of disease.
In nuclear medicine procedures, radionuclides are combined with other elements to form chemical compounds, or
else combined with existing pharmaceutical compounds, to form radiopharmaceuticals. These radiopharmaceuticals,
once administered to the patient, can localize to specific organs or cellular receptors. This property of
radiopharmaceuticals allows nuclear medicine the ability to image the extent of a disease process in the body, based
on the cellular function and physiology, rather than relying on physical changes in the tissue anatomy. In some
diseases, nuclear medicine studies can identify medical problems at an earlier stage than other diagnostic tests.
Nuclear medicine, in a sense, is "radiology done inside out", or "endo-radiology", because it records radiation
emitting from within the body rather than radiation that is generated by external sources like X-rays.
Treatment of diseased tissue, based on metabolism or uptake or binding of a particular ligand, may also be
accomplished, similar to other areas of pharmacology. However, the treatment effects of radiopharmaceuticals rely
on the tissue-destructive power of short-range ionizing radiation.
In the future, nuclear medicine may provide added impetus to the field known as molecular medicine. As
understanding of biological processes in the cells of living organisms expands, specific probes can be developed to
allow visualization, characterization, and quantification of biologic processes at the cellular and subcellular levels.
[7]
Nuclear medicine is a possible specialty for adapting to the new discipline of molecular medicine because of its
emphasis on function and its utilization of imaging agents that are specific for a particular disease process.
Diagnostic medical imaging
Diagnostic
In nuclear medicine imaging, radiopharmaceuticals are taken internally, for example, intravenously or orally. Then,
external detectors (gamma cameras) capture and form images from the radiation emitted by the
radiopharmaceuticals. This process is unlike a diagnostic X-ray, where external radiation is passed through the body
to form an image.
There are several techniques of diagnostic nuclear medicine.
2D: Scintigraphy ("scint") is the use of internal radionuclides to create two-dimensional images.
[8]
Nuclear medicine
2
A nuclear medicine whole body
bone scan. The nuclear
medicine whole body bone
scan is generally used in
evaluations of various
bone-related pathology, such as
for bone pain, stress fracture,
nonmalignant bone lesions,
bone infections, or the spread
of cancer to the bone.
Nuclear medicine myocardial
perfusion scan with
thallium-201 for the rest images
(bottom rows) and Tc-Sestamibi
for the stress images (top rows).
The nuclear medicine
myocardial perfusion scan plays
a pivotal role in the noninvasive
evaluation of coronary artery
disease. The study not only
identifies patients with coronary
artery disease; it also provides
overall prognostic information
or overall risk of adverse
cardiac events for the patient.
A nuclear medicine parathyroid
scan demonstrates a parathyroid
adenoma adjacent to the left
inferior pole of the thyroid gland.
The above study was performed
with Technetium-Sestamibi (1st
column) and iodine-123 (2nd
column) simultaneous imaging
and the subtraction technique
(3rd column).
Normal hepatobiliary scan
(HIDA scan). The nuclear
medicine hepatobiliary scan is
clinically useful in the detection
of the gallbladder disease.
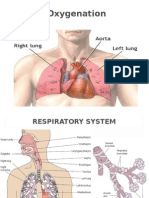
Normal pulmonary ventilation
and perfusion (V/Q) scan. The
nuclear medicine V/Q scan is
useful in the evaluation of
pulmonary embolism.
Thyroid scan with
iodine-123 for
evaluation of
hyperthyroidism.
3D: SPECT is a 3D tomographic technique that uses gamma camera data from many projections and can be
reconstructed in different planes. Positron emission tomography (PET) uses coincidence detection to image
functional processes.
Nuclear medicine
3
A nuclear medicine SPECT liver scan with technetium-99m labeled
autologous red blood cells. A focus of high uptake (arrow) in the liver
is consistent with a hemangioma.
Maximum intensity
projection (MIP) of a
whole-body positron
emission tomography (PET)
acquisition of a 79kg female
after intravenous injection of
371MBq of 18F-FDG (one
hour prior measurement).
Nuclear medicine tests differ from most other imaging modalities in that diagnostic tests primarily show the
physiological function of the system being investigated as opposed to traditional anatomical imaging such as CT or
MRI. Nuclear medicine imaging studies are generally more organ- or tissue-specific (e.g.: lungs scan, heart scan,
bone scan, brain scan, etc.) than those in conventional radiology imaging, which focus on a particular section of the
body (e.g.: chest X-ray, abdomen/pelvis CT scan, head CT scan, etc.). In addition, there are nuclear medicine studies
that allow imaging of the whole body based on certain cellular receptors or functions. Examples are whole body PET
scans or PET/CT scans, gallium scans, indium white blood cell scans, MIBG and octreotide scans.
Iodine-123 whole body scan for thyroid cancer
evaluation. The study above was performed after
the total thyroidectomy and TSH stimulation with
thyroid hormone medication withdrawal. The
study shows a small residual thyroid tissue in the
neck and a mediastinum lesion, consistent with
the thyroid cancer metastatic disease. The
observable uptakes in the stomach and bladder
are normal physiologic findings.
While the ability of nuclear metabolism to image disease processes
from differences in metabolism is unsurpassed, it is not unique. Certain
techniques such as fMRI image tissues (particularly cerebral tissues)
by blood flow and thus show metabolism. Also, contrast-enhancement
techniques in both CT and MRI show regions of tissue that are
handling pharmaceuticals differently, due to an inflammatory process.
Diagnostic tests in nuclear medicine exploit the way that the body
handles substances differently when there is disease or pathology
present. The radionuclide introduced into the body is often chemically
bound to a complex that acts characteristically within the body; this is
commonly known as a tracer. In the presence of disease, a tracer will
often be distributed around the body and/or processed differently. For
example, the ligand methylene-diphosphonate (MDP) can be
preferentially taken up by bone. By chemically attaching
technetium-99m to MDP, radioactivity can be transported and attached
to bone via the hydroxyapatite for imaging. Any increased
physiological function, such as due to a fracture in the bone, will
usually mean increased concentration of the tracer. This often results in
the appearance of a "hot spot", which is a focal increase in radio
Nuclear medicine
4
accumulation or a general increase in radio accumulation throughout the physiological system. Some disease
processes result in the exclusion of a tracer, resulting in the appearance of a "cold spot". Many tracer complexes have
been developed to image or treat many different organs, glands, and physiological processes.
Hybrid scanning techniques
In some centers, the nuclear medicine scans can be superimposed, using software or hybrid cameras, on images from
modalities such as CT or MRI to highlight the part of the body in which the radiopharmaceutical is concentrated.
This practice is often referred to as image fusion or co-registration, for example SPECT/CT and PET/CT. The fusion
imaging technique in nuclear medicine provides information about the anatomy and function, which would otherwise
be unavailable or would require a more invasive procedure or surgery.
Normal whole body PET/CT scan with FDG-18. The whole
body PET/CT scan is commonly used in the detection, staging
and follow-up of various cancers.
Abnormal whole body PET/CT scan with multiple metastases from a
cancer. The whole body PET/CT scan has become an important tool in
the evaluation of cancer.
Practical concerns in nuclear imaging
Although the risks of low-level radiation exposures are not well understood, a cautious approach has been
universally adopted that all human radiation exposures should be kept As Low As Reasonably Practicable,
"ALARP". (Originally, this was known as "As Low As Reasonably Achievable" (ALARA), but this has changed in
modern draftings of the legislation to add more emphasis on the "Reasonably" and less on the "Achievable".)
Working with the ALARP principle, before a patient is exposed for a nuclear medicine examination, the benefit of
the examination must be identified. This needs to take into account the particular circumstances of the patient in
question, where appropriate. For instance, if a patient is unlikely to be able to tolerate a sufficient amount of the
procedure to achieve a diagnosis, then it would be inappropriate to proceed with injecting the patient with the
radioactive tracer.
When the benefit does justify the procedure, then the radiation exposure (the amount of radiation given to the
patient) should also be kept as low as reasonably practicable. This means that the images produced in nuclear
medicine should never be better than required for confident diagnosis. Giving larger radiation exposures can reduce
the noise in an image and make it more photographically appealing, but if the clinical question can be answered
without this level of detail, then this is inappropriate.
As a result, the radiation dose from nuclear medicine imaging varies greatly depending on the type of study. The
effective radiation dose can be lower than or comparable to or can far exceed the general day-to-day environmental
Nuclear medicine
5
annual background radiation dose. Likewise, it can also be less than, in the range of, or higher than the radiation dose
from an abdomen/pelvis CT scan.
Some nuclear medicine procedures require special patient preparation before the study to obtain the most accurate
result. Pre-imaging preparations may include dietary preparation or the withholding of certain medications. Patients
are encouraged to consult with the nuclear medicine department prior to a scan.
Analysis
The end result of the nuclear medicine imaging process is a "dataset" comprising one or more images. In
multi-image datasets the array of images may represent a time sequence (i.e. cine or movie) often called a "dynamic"
dataset, a cardiac gated time sequence, or a spatial sequence where the gamma-camera is moved relative to the
patient. SPECT (single photon emission computed tomography) is the process by which images acquired from a
rotating gamma-camera are reconstructed to produce an image of a "slice" through the patient at a particular position.
A collection of parallel slices form a slice-stack, a three-dimensional representation of the distribution of
radionuclide in the patient.
The nuclear medicine computer may require millions of lines of source code to provide quantitative analysis
packages for each of the specific imaging techniques available in nuclear medicine.
[citation needed]
Time sequences can be further analysed using kinetic models such as multi-compartment models or a Patlak plot.
Interventional nuclear medicine
Radionuclide therapy can be used to treat conditions such as hyperthyroidism, thyroid cancer, and blood disorders.
In nuclear medicine therapy, the radiation treatment dose is administered internally (e.g. intravenous or oral routes)
rather from an external radiation source.
The radiopharmaceuticals used in nuclear medicine therapy emit ionizing radiation that travels only a short distance,
thereby minimizing unwanted side effects and damage to noninvolved organs or nearby structures. Most nuclear
medicine therapies can be performed as outpatient procedures since there are few side effects from the treatment and
the radiation exposure to the general public can be kept within a safe limit.
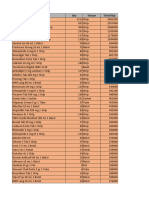
Common nuclear medicine (unsealed source) therapies
Substance Condition
Iodine-131-sodium iodide hyperthyroidism and thyroid cancer
Yttrium-90-ibritumomab tiuxetan (Zevalin) and Iodine-131-tositumomab (Bexxar) refractory lymphoma
131
I-MIBG (metaiodobenzylguanidine)
neuroendocrine tumors
Samarium-153 or Strontium-89 palliative bone pain treatment
In some centers the nuclear medicine department may also use implanted capsules of isotopes (brachytherapy) to
treat cancer.
Commonly used radiation sources (radionuclides) for brachytherapy
[9]
Nuclear medicine
6
Radionuclide Type Half-life Energy
Caesium-137 (
137
Cs)
-ray 30.17 years 0.662 MeV
Cobalt-60 (
60
Co)
-ray 5.26 years 1.17, 1.33 MeV
Iridium-192 (
192
Ir)
-
-particles
73.8 days 0.38 MeV (mean)
Iodine-125 (
125
I)
-rays 59.6 days 27.4, 31.4 and 35.5 keV
Palladium-103 (
103
Pd)
-ray 17.0 days 21 keV (mean)
Ruthenium-106 (
106
Ru)
-
-particles
1.02 years 3.54 MeV
History
The history of nuclear medicine is rich with contributions from gifted scientists across different disciplines in
physics, chemistry, engineering, and medicine. The multidisciplinary nature of nuclear medicine makes it difficult
for medical historians to determine the birthdate of nuclear medicine. This can probably be best placed between the
discovery of artificial radioactivity in 1934 and the production of radionuclides by Oak Ridge National Laboratory
for medicine related use, in 1946.
[10]
The origins of this medical idea date back as far as the mid-1920s in Freiburg, Germany, when George de Hevesy
made experiments with radionuclides administered to rats, thus displaying metabolic pathways of these substances
and establishing the tracer principle. Possibly, the genesis of this medical field took place in 1936, when John
Lawrence, known as "the father of nuclear medicine", took a leave of absence from his faculty position at Yale
Medical School, to visit his brother Ernest Lawrence at his new radiation laboratory (now known as the Lawrence
Berkeley National Laboratory) in Berkeley, California. Later on, John Lawrence made the first application in
patients of an artificial radionuclide when he used phosphorus-32 to treat leukemia.
[11][12]
Many historians consider the discovery of artificially produced radionuclides by Frdric Joliot-Curie and Irne
Joliot-Curie in 1934 as the most significant milestone in nuclear medicine. In February 1934, they reported the first
artificial production of radioactive material in the journal Nature, after discovering radioactivity in aluminum foil
that was irradiated with a polonium preparation. Their work built upon earlier discoveries by Wilhelm Konrad
Roentgen for X-ray, Henri Becquerel for radioactive uranium salts, and Marie Curie (mother of Irne Curie) for
radioactive thorium, polonium and coining the term "radioactivity." Taro Takemi studied the application of nuclear
physics to medicine in the 1930s. The history of nuclear medicine will not be complete without mentioning these
early pioneers.
Nuclear medicine gained public recognition as a potential specialty on December 7, 1946 when an article was
published in the Journal of the American Medical Association by Sam Seidlin. The article described a successful
treatment of a patient with thyroid cancer metastases using radioiodine (I-131). This is considered by many
historians as the most important article ever published in nuclear medicine.
[13]
Although the earliest use of I-131 was
devoted to therapy of thyroid cancer, its use was later expanded to include imaging of the thyroid gland,
quantification of the thyroid function, and therapy for hyperthyroidism.
Widespread clinical use of nuclear medicine began in the early 1950s, as knowledge expanded about radionuclides,
detection of radioactivity, and using certain radionuclides to trace biochemical processes. Pioneering works by
Benedict Cassen in developing the first rectilinear scanner and Hal O. Anger's scintillation camera (Anger camera)
broadened the young discipline of nuclear medicine into a full-fledged medical imaging specialty.
In these years of nuclear medicine, the growth was phenomenal. The Society of Nuclear Medicine was formed in
1954 in Spokane, Washington, USA. In 1960, the Society began publication of the Journal of Nuclear Medicine, the
premier scientific journal for the discipline in America. There was a flurry of research and development of new
Nuclear medicine
7
radionuclides and radiopharmaceuticals for use with the imaging devices and for in-vitro studies5.
Among many radionuclides that were discovered for medical-use, none were as important as the discovery and
development of Technetium-99m. It was first discovered in 1937 by C. Perrier and E. Segre as an artificial element
to fill space number 43 in the Periodic Table. The development of a generator system to produce Technetium-99m in
the 1960s became a practical method for medical use. Today, Technetium-99m is the most utilized element in
nuclear medicine and is employed in a wide variety of nuclear medicine imaging studies.
By the 1970s most organs of the body could be visualized using nuclear medicine procedures. In 1971, American
Medical Association officially recognized nuclear medicine as a medical specialty.
[14]
In 1972, the American Board
of Nuclear Medicine was established, and in 1974, the American Osteopathic Board of Nuclear Medicine was
established, cementing nuclear medicine as a stand-alone medical specialty.
In the 1980s, radiopharmaceuticals were designed for use in diagnosis of heart disease. The development of single
photon emission computed tomography (SPECT), around the same time, led to three-dimensional reconstruction of
the heart and establishment of the field of nuclear cardiology.
More recent developments in nuclear medicine include the invention of the first positron emission tomography
scanner (PET). The concept of emission and transmission tomography, later developed into single photon emission
computed tomography (SPECT), was introduced by David E. Kuhl and Roy Edwards in the late 1950s
[citation needed]
.
Their work led to the design and construction of several tomographic instruments at the University of Pennsylvania.
Tomographic imaging techniques were further developed at the Washington University School of Medicine. These
innovations led to fusion imaging with SPECT and CT by Bruce Hasegawa from University of California San
Francisco (UCSF), and the first PET/CT prototype by D. W. Townsend from University of Pittsburgh in 1998
[citation
needed]
.
PET and PET/CT imaging experienced slower growth in its early years owing to the cost of the modality and the
requirement for an on-site or nearby cyclotron. However, an administrative decision to approve medical
reimbursement of limited PET and PET/CT applications in oncology has led to phenomenal growth and widespread
acceptance over the last few years, which also was facilitated by establishing 18F-labelled tracers for standard
procedures, allowing work at non-cyclotron-equipped sites. PET/CT imaging is now an integral part of oncology for
diagnosis, staging and treatment monitoring. A fully integrated MRI/PET scanner is on the market from early
2011.
[citation needed]
Source of radionuclides, with notes on a few radiopharmaceuticals
About a third of the world's supply, and most of North America's supply, of medical isotopes are produced at the
Chalk River Laboratories in Chalk River, Ontario, Canada. (Another third of the world's supply, and most of
Europe's supply, are produced at the Petten nuclear reactor in the Netherlands.) The Canadian Nuclear Safety
Commission ordered the NRU reactor to be shut down on November 18, 2007 for regularly scheduled maintenance
and an upgrade of the safety systems to modern standards. The upgrade took longer than expected and in December
2007, a critical shortage of medical isotopes occurred. The Canadian government unanimously passed emergency
legislation, allowing the reactor to restart on 16 December 2007, and production of medical isotopes to continue.
The Chalk River reactor is used to irradiate materials with neutrons which are produced in great quantity during the
fission of U-235. These neutrons change the nucleus of the irradiated material by adding a neutron, or by splitting it
in the process of nuclear fission. In a reactor, one of the fission products of uranium is molybdenum-99 which is
extracted and shipped to radiopharmaceutical houses all over North America. The Mo-99 radioactively beta decays
with a half-life of 2.7 days, turning initially into Tc-99m, which is then extracted (milked) from a "moly cow" (see
technetium-99m generator). The Tc-99m then further decays, while inside a patient, releasing a gamma photon
which is detected by the gamma camera. It decays to its ground state of Tc-99, which is relatively non-radioactive
compared to Tc-99m.
Nuclear medicine
8
The most commonly used radioisotope in PET F-18, is not produced in any nuclear reactor, but rather in a circular
accelerator called a cyclotron. The cyclotron is used to accelerate protons to bombard the stable heavy isotope of
oxygen O-18. The O-18 constitutes about 0.20% of ordinary oxygen (mostly O-16), from which it is extracted. The
F-18 is then typically used to make FDG (see this link for more information on this process).
Common isotopes used in nuclear medicine
isotope symbol Z T
1/2
decay gamma (keV) positron (keV)
Imaging:
fluorine-18 18
F
9 109.77 m
+ 511 (193%)
249.8 (97%)
[15]
gallium-67 67
Ga
31 3.26 d ec 93 (39%),
185 (21%),
300 (17%)
-
krypton-81m 81m
Kr
36 13.1 s IT 190 (68%) -
rubidium-82 82
Rb
37 1.27 m
+ 511 (191%) 3.379 (95%)
nitrogen-13 13
N
7 9.97 m
+ 511 (200%)
1190 (100%)
[16]
technetium-99m 99m
Tc
43 6.01 h IT 140 (89%) -
indium-111 111
In
49 2.80 d ec 171 (90%),
245 (94%)
-
iodine-123 123
I
53 13.3 h ec 159 (83%) -
xenon-133 133
Xe
54 5.24 d
- 81 (31%) 0.364 (99%)
thallium-201 201
Tl
81 3.04 d ec
6983
*
(94%),
167 (10%)
-
Therapy:
yttrium-90 90
Y
39 2.67 d
- - 2.280 (100%)
iodine-131 131
I
53 8.02 d
- 364 (81%) 0.807 (100%)
Z = atomic number, the number of protons; T
1/2
= half-life; decay = mode of decay
photons = principle photon energies in kilo-electron volts, keV, (abundance/decay)
= beta maximum energy in mega-electron volts, MeV, (abundance/decay)
+
=
+
decay;
-
=
-
decay; IT = isomeric transition; ec = electron capture
* X-rays from progeny, mercury, Hg
A typical nuclear medicine study involves administration of a radionuclide into the body by intravenous injection in
liquid or aggregate form, ingestion while combined with food, inhalation as a gas or aerosol, or rarely, injection of a
radionuclide that has undergone micro-encapsulation. Some studies require the labeling of a patient's own blood cells
with a radionuclide (leukocyte scintigraphy and red blood cell scintigraphy). Most diagnostic radionuclides emit
gamma rays, while the cell-damaging properties of beta particles are used in therapeutic applications. Refined
radionuclides for use in nuclear medicine are derived from fission or fusion processes in nuclear reactors, which
produce radionuclides with longer half-lives, or cyclotrons, which produce radionuclides with shorter half-lives, or
take advantage of natural decay processes in dedicated generators, i.e. molybdenum/technetium or
strontium/rubidium.
The most commonly used intravenous radionuclides are:
Technetium-99m (technetium-99m)
Nuclear medicine
9
Iodine-123 and 131
Thallium-201
Gallium-67
Fluorine-18 Fluorodeoxyglucose
Indium-111 Labeled Leukocytes
The most commonly used gaseous/aerosol radionuclides are:
Xenon-133
Krypton-81m
Technetium-99m Technegas
[17]
Wikipedia:Link rot a radioaerosol invented in Australia by Dr Bill Burch and Dr
Richard Fawdry
Technetium-99m DTPA
Radiation dose
A patient undergoing a nuclear medicine procedure will receive a radiation dose. Under present international
guidelines it is assumed that any radiation dose, however small, presents a risk. The radiation doses delivered to a
patient in a nuclear medicine investigation, though unproven, is generally accepted to present a very small risk of
inducing cancer. In this respect it is similar to the risk from X-ray investigations except that the dose is delivered
internally rather than from an external source such as an X-ray machine, and dosage amounts are typically
significantly higher than those of X-rays.
The radiation dose from a nuclear medicine investigation is expressed as an effective dose with units of sieverts
(usually given in millisieverts, mSv). The effective dose resulting from an investigation is influenced by the amount
of radioactivity administered in megabecquerels (MBq), the physical properties of the radiopharmaceutical used, its
distribution in the body and its rate of clearance from the body.
Effective doses can range from 6 Sv (0.006 mSv) for a 3 MBq chromium-51 EDTA measurement of glomerular
filtration rate to 37 mSv (37,000 Sv) for a 150 MBq thallium-201 non-specific tumour imaging procedure. The
common bone scan with 600 MBq of technetium-99m-MDP has an effective dose of approximately 3.5 mSv (3,500
Sv) (1).
Formerly, units of measurement were the curie (Ci), being 3.7E10 Bq, and also 1.0 grams of Radium (Ra-226); the
rad (radiation absorbed dose), now replaced by the gray; and the rem (Rntgen equivalent man), now replaced with
the sievert. The rad and rem are essentially equivalent for almost all nuclear medicine procedures, and only alpha
radiation will produce a higher Rem or Sv value, due to its much higher Relative Biological Effectiveness (RBE).
Alpha emitters are nowadays rarely used in nuclear medicine, but were used extensively before the advent of nuclear
reactor and accelerator produced radionuclides. The concepts involved in radiation exposure to humans are covered
by the field of Health Physics.
References
Notes
[1] http:/ / www. icd10data. com/ ICD10PCS/ Codes/ C
[2] http:/ / icd9cm. chrisendres.com/ index.php?srchtype=procs& srchtext=92& Submit=Search& action=search
[3] http:/ / www. nlm. nih.gov/ cgi/ mesh/ 2011/ MB_cgi?field=uid& term=D009683
[4] http:/ / ops. icd-code. de/ ops/ code/ 3-70.html
[5] http:/ / ops. icd-code. de/ ops/ code/ 3-72.html
[6] http:/ / ops. icd-code. de/ ops/ code/ 8-53.html
[7] http:/ / www. molecularimagingcenter. org, Gambhir S. Just what is molecular medicine.
[8] thefreedictionary.com > scintigraphy (http:/ / medical-dictionary. thefreedictionary. com/ scintigraphy) Citing: Dorland's Medical Dictionary
for Health Consumers, 2007 by Saunders; Saunders Comprehensive Veterinary Dictionary, 3 ed. 2007; McGraw-Hill Concise Dictionary of
Modern Medicine, 2002 by The McGraw-Hill Companies
Nuclear medicine
10
[9] Nuclear Wallet Cards (http:/ / www. nndc.bnl. gov/ wallet/ wc7. html)
[10] Edwards Cl: Tumor localizing radionuclides in retrospect and prospect. Semin Nucl Med 3:186189, 1979.
[11] Donner Laboratory: The Birthplace of. Nuclear Medicine (http:/ / jnm. snmjournals. org/ content/ 40/ 1/ 16N. full. pdf)
[12] Important Moments in the History of Nuclear Medicine (http:/ / interactive. snm. org/ index. cfm?PageID=1107)
[13] [13] Henkin R. et al: Nuclear Medicine. First edition 1996. ISBN 978-0-8016-7701-4.
[14] http:/ / interactive.snm.org/ docs/ whatisnucmed. pdf from the Society of Nuclear Medicine.
[15] Sodium Fluoride F 18 Injection Drug Label (http:/ / dailymed. nlm. nih. gov/ dailymed/ archives/ fdaDrugInfo. cfm?archiveid=43688)
[16] N-13 Ammonia prescribing information (Drugs.com) (http:/ / www. drugs. com/ pro/ ammonia-n-13. html)
[17] http:/ / jcsmr. anu. edu. au/ technegas/ home. html
Further reading
Mas JC: A Patient's Guide to Nuclear Medicine Procedures: English-Spanish. Society of Nuclear Medicine, 2008.
ISBN 978-0-9726478-9-2
Taylor A, Schuster DM, Naomi Alazraki N: A Clinicians' Guide to Nuclear Medicine, 2nd edition. Society of
Nuclear Medicine, 2000. ISBN 978-0-932004-72-7
Mark J. Shumate MJ, Kooby DA, Alazraki NP: A Clinician's Guide to Nuclear Oncology: Practical Molecular
Imaging and Radionuclide Therapies. Society of Nuclear Medicine, January 2007. ISBN 978-0-9726478-8-5
Ell P, Gambhir S: Nuclear Medicine in Clinical Diagnosis and Treatment. Churchill Livingstone, 2004. (1950
pages) ISBN 978-0-443-07312-0
External links
Nuclear medicine (http:/ / www. dmoz. org/ Health/ Medicine/ Medical_Specialties/ Nuclear_Medicine/ / ) on the
Open Directory Project
The Nuclear Medicine and Molecular Medicine Podcast (http:/ / molcast. com)
Keyword Search on Nuclear Medicine at the United States Department of Labor (US DOL) Occupational
Information Network (O*NET) database (http:/ / www. onetonline. org/ find/ quick?s=Nuclear+ Medicine) -
Shows several occupational categories where people may use nuclear medicine technologies in their work. Linked
occupation summaries include information about work and worker characteristics, updated using aggregate level
input from people who have performed this work.
Solving the Medical Isotope Crisis (http:/ / purl. fdlp. gov/ GPO/ gpo28578) Hearing before the Subcommittee on
Energy and Environment of the Committee on Energy and Commerce, House of Representatives, One Hundred
Eleventh Congress, First Session, September 9, 2009
Library resources about
Nuclear medicine
Resources in your library (http:/ / tools. wmflabs. org/ ftl/ cgi-bin/ ftl?st=wp& su=Nuclear+ medicine)
Article Sources and Contributors
11
Article Sources and Contributors
Nuclear medicine Source: http://en.wikipedia.org/w/index.php?oldid=591836570 Contributors: ABF, APH, Acdx, Acrabb, Acroterion, AdamJ-TRX, AdjustShift, AjAldous, Alansohn,
Alex.tan, Alistair1978, Altenmann, AndreasJS, Andrel, Anypodetos, Arcadian, ArcadianOnUnsecuredLoc, Arostron, Art LaPella, Ashleyleia, Axeman89, Barlow, Bazzel, Beavertank,
Benjaminevans82, Beyond My Ken, Blai40, Blanchardb, Bobblewik, Bogey97, Boing! said Zebedee, BrightStarSky, Brimcmike, Brookie, Btyner, Bumm13, BusterNutBag, CWenger, Calvin
1998, Camonaghan, CanadianLinuxUser, Captain Zyrain, Centrx, ChillyMD, Chowbok, CiaPan, Clicketyclack, Cnort59, Colonies Chris, Csblackburn, Csutric, Ctande, Cyfal, DV8 2XL, Damato,
DanMS, Daveswagon, DavidLeighEllis, Davidruben, Deagle AP, Delaroyas, Dgw, Diberri, Dirac66, Discospinster, Disenraged, Download, Dozenne, DrFO.Jr.Tn, Drbreznjev, Drilnoth,
Dspradau, Dwayne Reed, ESkog, Edward, Eiland, Elassint, Elockid, Enderwiki, Epbr123, EpicDream86, Eth4n, Evil Monkey, Fizzy, Fnielsen, Formol, Frickeg, Galoubet, GangofOne, Gilliam,
Good Olfactory, GraemeL, HowardJWilk, II MusLiM HyBRiD II, IOPhysics, Igoldste, Iorsh, J.delanoy, Jagged 85, Jamesofur, Jennifergr, Jerry, Jfdwolff, Jjkusaf, Jmjanzen, Jncraton, Joel7687,
Josve05a, Jrtayloriv, JustAGal, Keereann, Khatriaditya, Kirachinmoku, Kubanczyk, Kyng, LMB, Laurens-af, Lb.at.wiki, Lcolson, Leafyplant, Leszek Jaczuk, Levent, Li4kata, Librsh, Limnalid,
LittleWink, Luckyz, Luna Santin, Lyoel, MER-C, MacsBug, Madhero88, Mallyest, Mco44, Meelar, Mefanch, Mercurous, Mikael Hggstrm, Mikespedia, Mild Bill Hiccup, Mion, Muv4zqlvc3,
Myasuda, Mygerardromance, Myohan, Nen, NickW557, Nihiltres, Nukemedsb, Oldnoah, OohBunnies!, Orhan94, Ottawakismet, Paulc206, PeteVerdon, Peter Horn, PloniAlmoni, Possum,
Profplum27, Quinlan Vos, Ratman90, Raven in Orbit, RazorICE, Rl, Robcw, Robertvan1, Rod57, Ronhjones, RoyBoy, Rsabbatini, SBaker43, SKvalen, SWAdair, Saimhe, Salvadorjo, Saric,
Sbharris, Sceptre, SchreiberBike, Semperf, Sfan00 IMG, Shadowjams, Sherool, Shmeeninja, Simesa, Simonbayly, Social Climber, Some jerk on the Internet, SpecMode, SriMesh, Stephenb,
Stepped, Suffusion of Yellow, Tcb0667, Tekks, Th4n3r, Thatguyflint, Thomasneilp, Thumperward, Tide rolls, Tmarlow, Tommy2010, Tony46, Torres Carlos M, Treaclecustard, Treuss,
TylerDurden8823, Ultimus, Uncle Dick, Vchorozopoulos, Venu62, Wasbeer, Wasted Sapience, Wavelength, Woohookitty, Wouterstomp, Xrayburst1, YUL89YYZ, Yoderj, Zereshk, ,
431 anonymous edits
Image Sources, Licenses and Contributors
File:Nl bone scan2.jpg Source: http://en.wikipedia.org/w/index.php?title=File:Nl_bone_scan2.jpg License: Creative Commons Attribution 3.0 Contributors: Hellerhoff
File:nl mpi2.jpg Source: http://en.wikipedia.org/w/index.php?title=File:Nl_mpi2.jpg License: Creative Commons Attribution 3.0 Contributors: Myohan
File:parathyroid subtraction.jpg Source: http://en.wikipedia.org/w/index.php?title=File:Parathyroid_subtraction.jpg License: Creative Commons Attribution 3.0 Contributors: -
File:HIDA.jpg Source: http://en.wikipedia.org/w/index.php?title=File:HIDA.jpg License: Creative Commons Attribution 3.0 Contributors: Hellerhoff, Magog the Ogre, Senator2029
File:ventperf.jpg Source: http://en.wikipedia.org/w/index.php?title=File:Ventperf.jpg License: Creative Commons Attribution 3.0 Contributors: Hellerhoff, Senator2029
File:thyroid scan.jpg Source: http://en.wikipedia.org/w/index.php?title=File:Thyroid_scan.jpg License: Creative Commons Attribution 3.0 Contributors: Hellerhoff
File:hemangioma scan.jpg Source: http://en.wikipedia.org/w/index.php?title=File:Hemangioma_scan.jpg License: Creative Commons Attribution 3.0 Contributors: Myohan
File:PET-MIPS-anim.gif Source: http://en.wikipedia.org/w/index.php?title=File:PET-MIPS-anim.gif License: Public Domain Contributors: Jens Langner (http://www.jens-langner.de/)
File:Iodine wb scan.jpg Source: http://en.wikipedia.org/w/index.php?title=File:Iodine_wb_scan.jpg License: Creative Commons Attribution 3.0 Contributors: Myohan
File:nl petct.jpg Source: http://en.wikipedia.org/w/index.php?title=File:Nl_petct.jpg License: Creative Commons Attribution 3.0 Contributors: Verne Equinox
File:abnl petct.jpg Source: http://en.wikipedia.org/w/index.php?title=File:Abnl_petct.jpg License: Creative Commons Attribution 3.0 Contributors: User:Myohan
License
Creative Commons Attribution-Share Alike 3.0
//creativecommons.org/licenses/by-sa/3.0/
You might also like
- Original - The Anger Disorders ScaleDocument3 pagesOriginal - The Anger Disorders ScaleCláudia Oliveira75% (4)
- Bio Physics AssignmentDocument8 pagesBio Physics AssignmentAli InamNo ratings yet
- Respiratory FailureDocument7 pagesRespiratory FailuremuhammadridhwanNo ratings yet
- Nuclear MedicineDocument25 pagesNuclear MedicineRafalNo ratings yet
- Nuclear Medicine: Definition of The Specialty and Scope of Nuclear MedicineDocument23 pagesNuclear Medicine: Definition of The Specialty and Scope of Nuclear MedicinePriya SalunkeNo ratings yet
- What Is Molecular Imaging?Document10 pagesWhat Is Molecular Imaging?Akshat SinghNo ratings yet
- Medical ImagingDocument93 pagesMedical ImagingpraveenNo ratings yet
- A Compilation of Procedural Manual - Reflective Journal and Learning Journal Presented To The FacultyDocument56 pagesA Compilation of Procedural Manual - Reflective Journal and Learning Journal Presented To The Facultymark jay jamboyNo ratings yet
- Nuclear MedicineDocument5 pagesNuclear MedicineEmmanuelNo ratings yet
- Medical Imaging Is The Technique and Process Used To CreateDocument11 pagesMedical Imaging Is The Technique and Process Used To Creates.reeganNo ratings yet
- Medical Imaging Is The Technique and Process Used To Create: o o o o o o o o o o o o o oDocument10 pagesMedical Imaging Is The Technique and Process Used To Create: o o o o o o o o o o o o o osukudec17No ratings yet
- Nuclear Medicine - Imaging, Diagnosis, and TreatmentDocument3 pagesNuclear Medicine - Imaging, Diagnosis, and TreatmentkenyorumosesNo ratings yet
- Nuclear Medicine ResearchDocument4 pagesNuclear Medicine ResearchRagor TUNo ratings yet
- Medical ImagingDocument16 pagesMedical ImagingBoobalan RNo ratings yet
- The Application of Nuclear Physics in Biology and Medicine 1Document7 pagesThe Application of Nuclear Physics in Biology and Medicine 1essaidNo ratings yet
- Physics: Mission Statement of Medical PhysicistsDocument18 pagesPhysics: Mission Statement of Medical PhysicistspiyaNo ratings yet
- Radioisotopes in MedicineDocument19 pagesRadioisotopes in MedicineAllen PetrovicNo ratings yet
- Title of The Paper: Student's Name University Course Professor DateDocument5 pagesTitle of The Paper: Student's Name University Course Professor DatebrianNo ratings yet
- A Paragraph About CancerDocument17 pagesA Paragraph About Cancersalmanaltaf890No ratings yet
- Whatisnucmed2 Nuclear MedicineDocument8 pagesWhatisnucmed2 Nuclear Medicinevb.dipeshNo ratings yet
- THJKDocument19 pagesTHJKMamdooh AlqathamiNo ratings yet
- Diagnostic Medical ImagingDocument8 pagesDiagnostic Medical ImagingSusan FNo ratings yet
- Radiology - Examination Methods 2Document78 pagesRadiology - Examination Methods 2Abishek DhinakaranNo ratings yet
- Overview of Nuclear Medical Imaging Instrumentation and TechniquesDocument12 pagesOverview of Nuclear Medical Imaging Instrumentation and Techniquesknno87No ratings yet
- On The Brain PDFDocument6 pagesOn The Brain PDFNezrin BaxisliNo ratings yet
- Radioisotopes in MedicineDocument5 pagesRadioisotopes in MedicineEnya BautistaNo ratings yet
- Magnetic Resonance Imaging: Main ArticleDocument4 pagesMagnetic Resonance Imaging: Main ArticleDana TimushNo ratings yet
- Class NotesDocument4 pagesClass NotesSamrat banerjeeNo ratings yet
- Patient Exposure NMRDocument5 pagesPatient Exposure NMRFayzan AhmedNo ratings yet
- General Nuclear Medicine: RadioactiveDocument21 pagesGeneral Nuclear Medicine: RadioactiveRana SayedNo ratings yet
- Project in MAPEHDocument14 pagesProject in MAPEHRamel Yen CerantesNo ratings yet
- Exercise NM 4 Nuclear MedicineDocument15 pagesExercise NM 4 Nuclear MedicineMadhumala KumariNo ratings yet
- Radiology - Nuclear MedicineDocument5 pagesRadiology - Nuclear MedicineKirstinNo ratings yet
- 6257155572d49 Nuclear Medicine - EditedDocument4 pages6257155572d49 Nuclear Medicine - EditedBandah Mwiti JosephNo ratings yet
- X Rays Benefit RiskDocument16 pagesX Rays Benefit RiskGianne KuizonNo ratings yet
- BME-417L - PET ScanDocument5 pagesBME-417L - PET Scansarmadmukhtar21No ratings yet
- Medical Imaging Write UpDocument25 pagesMedical Imaging Write Upelfaruk37No ratings yet
- Radiation and Nuclear MedicineDocument29 pagesRadiation and Nuclear MedicineGoran MaliNo ratings yet
- Radionuclides in Medicine Student Worksheet 19-06-2020 Numbers DeletedDocument14 pagesRadionuclides in Medicine Student Worksheet 19-06-2020 Numbers DeletedРуслан ГрибNo ratings yet
- Non Invasive Tests Appreciation of Diagnostic Procedures For Cardiovascular ProblemsDocument9 pagesNon Invasive Tests Appreciation of Diagnostic Procedures For Cardiovascular ProblemsMark Nel NuñezNo ratings yet
- Radiologists: Chronicle Guidance Publications Brief 462Document4 pagesRadiologists: Chronicle Guidance Publications Brief 462Madison DahseNo ratings yet
- Nuclear MedicineDocument2 pagesNuclear MedicineTomáš KřenekNo ratings yet
- Retina Full DocumentDocument34 pagesRetina Full DocumentThe MindNo ratings yet
- What Is Medical Equipment and Types of Medical EquipmentDocument5 pagesWhat Is Medical Equipment and Types of Medical EquipmentNor Hassan AmbaNo ratings yet
- Exam Topics NMDocument80 pagesExam Topics NMAsaf Citrin100% (1)
- Neuclear MedicineDocument4 pagesNeuclear MedicineAyan SarderNo ratings yet
- Medical Exposures Fact Sheet PDFDocument4 pagesMedical Exposures Fact Sheet PDFSrinivas VenkataramanNo ratings yet
- Nuclear MedicineDocument10 pagesNuclear Medicinehomam Salim KhalafNo ratings yet
- NUCLEARDocument2 pagesNUCLEARasus predatorNo ratings yet
- Nuclear Medicine: Answering Your QuestionsDocument12 pagesNuclear Medicine: Answering Your Questionshoneyjoy76No ratings yet
- Nuclear MedicineDocument17 pagesNuclear MedicineMuhammad asif samiNo ratings yet
- Nuclear Medicine: Physics Education October 2001Document9 pagesNuclear Medicine: Physics Education October 2001Rizka Ramadhani AbrarNo ratings yet
- Applications of Image ProcessingDocument20 pagesApplications of Image ProcessingTinny SinghNo ratings yet
- Document My Assignment TherapyDocument5 pagesDocument My Assignment TherapynanaaishamahmudgazaraNo ratings yet
- Cuadernillo Bioimágenes 1 y 2 2020Document9 pagesCuadernillo Bioimágenes 1 y 2 2020Bárbara PeraltaNo ratings yet
- PET - CT ScanningDocument8 pagesPET - CT ScanningBMTNo ratings yet
- 4 IntroductionDocument70 pages4 IntroductionDebangshu RoyNo ratings yet
- Omni-Tomography / Multi-TomographyDocument43 pagesOmni-Tomography / Multi-Tomographyantonio ScacchiNo ratings yet
- Eanm Guideline Radioiodine Therapy Benign Thyroid DiseaseDocument25 pagesEanm Guideline Radioiodine Therapy Benign Thyroid Diseasechrisgiang552No ratings yet
- Nuclear MedicineDocument3 pagesNuclear Medicinekawayiie_o25No ratings yet
- Prabhsharn cl21m012Document12 pagesPrabhsharn cl21m012prabhsharn SinghNo ratings yet
- Nuclear Medicine Therapy: Principles and Clinical ApplicationsFrom EverandNuclear Medicine Therapy: Principles and Clinical ApplicationsNo ratings yet
- Abu Dhabi DRGDocument62 pagesAbu Dhabi DRGDolly creationsNo ratings yet
- Pharmacology Bullets (Nursing)Document2 pagesPharmacology Bullets (Nursing)Mariz Quidlat100% (2)
- Postlab #7-Water FiltrationDocument4 pagesPostlab #7-Water FiltrationBenny AzarconNo ratings yet
- Caso Practico Control de InventariosDocument24 pagesCaso Practico Control de InventariosAristides OchoaNo ratings yet
- Mr. Shoaib Hakeem How To Manage Recalls and Withdrawls of PharmaceuticalsDocument25 pagesMr. Shoaib Hakeem How To Manage Recalls and Withdrawls of PharmaceuticalsSally PujaNo ratings yet
- Presentation Fispas SusuDocument13 pagesPresentation Fispas SusuAdela Veneta KistiNo ratings yet
- Tender Loving CareDocument7 pagesTender Loving Careapi-253096399No ratings yet
- TB DrugsDocument14 pagesTB DrugsLexy CadigalNo ratings yet
- Tugas Pareto - Elsa Irnandari - 188114130Document17 pagesTugas Pareto - Elsa Irnandari - 188114130elsaairnandari13No ratings yet
- Treatment of Hyperprolactinemia A.7Document4 pagesTreatment of Hyperprolactinemia A.7Leyni fanny guerrero limaNo ratings yet
- LIFE SKETCH OF DR Christian Friedrich Samuel Hahnemann PDFDocument3 pagesLIFE SKETCH OF DR Christian Friedrich Samuel Hahnemann PDFkrsnaprakash8346100% (1)
- SL 7 Digital Rectal ExaminationDocument3 pagesSL 7 Digital Rectal ExaminationNjunn AriniNo ratings yet
- Surgical Antibiotic Prophylaxis Neurosurgery Adult and Paediatric PatientsDocument6 pagesSurgical Antibiotic Prophylaxis Neurosurgery Adult and Paediatric PatientsPraveen PadalaNo ratings yet
- Budwig Cancer GuideDocument101 pagesBudwig Cancer Guidedora.oreiro9920No ratings yet
- Chronic Total OcclusionsDocument37 pagesChronic Total OcclusionsValentin CHIONCELNo ratings yet
- KPC Biofilter Wastewater Treatment System For Single Dwellings PDFDocument14 pagesKPC Biofilter Wastewater Treatment System For Single Dwellings PDFqbich37No ratings yet
- Group ProcessesDocument46 pagesGroup ProcessesGenNo ratings yet
- Laryngeal Carcinoma - PPT Fix PDFDocument140 pagesLaryngeal Carcinoma - PPT Fix PDFInes Camilla PutriNo ratings yet
- Asian Music Research - J.C GarciaDocument5 pagesAsian Music Research - J.C GarciaJomel GarciaNo ratings yet
- Standards of Care For Breeders of Companion Animals ActDocument9 pagesStandards of Care For Breeders of Companion Animals ActBCLiberalCaucusNo ratings yet
- OXYGENATIONDocument69 pagesOXYGENATIONTina Talmadge100% (4)
- 2018-Bugada-Update On Selective Regional Analgesia For Hip Surgery PatientsDocument13 pages2018-Bugada-Update On Selective Regional Analgesia For Hip Surgery PatientsDr LAUMONERIENo ratings yet
- Me Tot Rex AteDocument1 pageMe Tot Rex AtekryslerbNo ratings yet
- Limitations of The StudyDocument3 pagesLimitations of The StudyCharlesGoNo ratings yet
- Richmond CrownDocument5 pagesRichmond Crownndra16No ratings yet
- PLAB Blueprint - PDF 25396434Document23 pagesPLAB Blueprint - PDF 25396434dostoviskyNo ratings yet
- Discharge Planning ProjectDocument5 pagesDischarge Planning Projectapi-259394980No ratings yet
- Lesson 15 - OB GYN, Neurology, Surgery BackupDocument28 pagesLesson 15 - OB GYN, Neurology, Surgery BackupAlejandro GuerreroNo ratings yet