Professional Documents
Culture Documents
Atients Hospitalized After Initial Outpatient Treatment For Community-Acquired Pneumonia
Atients Hospitalized After Initial Outpatient Treatment For Community-Acquired Pneumonia
Uploaded by
MazKha BudCopyright:
Available Formats
You might also like
- Ineffective Airway Clearance Related To Retained Mucus Secretion As Evidenced by Unproductive CoughDocument1 pageIneffective Airway Clearance Related To Retained Mucus Secretion As Evidenced by Unproductive Coughdana93% (30)
- Assessment and Management of Preoperative Anxiety: London, United KingdomDocument6 pagesAssessment and Management of Preoperative Anxiety: London, United KingdomrsudabadiNo ratings yet
- Critical Care Goals and ObjectivesDocument28 pagesCritical Care Goals and ObjectivesjyothiNo ratings yet
- Gapuz Maternal Health NursingDocument80 pagesGapuz Maternal Health NursingHayes Clover100% (6)
- Articulo NeumoniaDocument7 pagesArticulo NeumoniaEd BarajasNo ratings yet
- Jurnal 1Document6 pagesJurnal 1Pratiwi AyuningtyasNo ratings yet
- Treatment Completion and Costs of A Randomized Trial of Rifampin For 4 Months Versus Isoniazid For 9 MonthsDocument5 pagesTreatment Completion and Costs of A Randomized Trial of Rifampin For 4 Months Versus Isoniazid For 9 MonthsSyairah Banu DjufriNo ratings yet
- The Pattern of Antimicrobial Use For Palliative Care In-Patients During The Last Week of LifeDocument4 pagesThe Pattern of Antimicrobial Use For Palliative Care In-Patients During The Last Week of Lifem1k0eNo ratings yet
- Long-Stay of PICU in SepsisDocument6 pagesLong-Stay of PICU in SepsisSanti IskandarNo ratings yet
- Coach 2023Document11 pagesCoach 2023Guilherme CarelliNo ratings yet
- Medicine American Journal of Hospice and PalliativeDocument6 pagesMedicine American Journal of Hospice and Palliativem1k0eNo ratings yet
- High-Dose Rifapentine With Moxifloxacin For Pulmonary TuberculosisDocument10 pagesHigh-Dose Rifapentine With Moxifloxacin For Pulmonary TuberculosisSoleh SundawaNo ratings yet
- Chan 2004Document8 pagesChan 2004clinica cuelloNo ratings yet
- Selected Topics: Prehospital CareDocument9 pagesSelected Topics: Prehospital CareYo MeNo ratings yet
- Two-Year Survival Comparing Web-Based Symptom Monitoring Vs Routine Surveillance Following Treatment For Lung CancerDocument6 pagesTwo-Year Survival Comparing Web-Based Symptom Monitoring Vs Routine Surveillance Following Treatment For Lung CancerValerie LascauxNo ratings yet
- Huang 2018Document14 pagesHuang 2018amazeyragNo ratings yet
- PROCESSDocument11 pagesPROCESSandrea vargasNo ratings yet
- Oral AbstractsDocument210 pagesOral AbstractspascutaNo ratings yet
- Procalcitonin PneumoniaDocument14 pagesProcalcitonin PneumoniaMr. LNo ratings yet
- Prediction Model For Shortterm Mortality After Palliative Therapy For Patients Having Advanced Cancer - A Cohort Study From Routine Electronic Medical DataDocument10 pagesPrediction Model For Shortterm Mortality After Palliative Therapy For Patients Having Advanced Cancer - A Cohort Study From Routine Electronic Medical DataHollis LukNo ratings yet
- Low Dose Prednisolone in Community Acquired PneumoniaDocument15 pagesLow Dose Prednisolone in Community Acquired PneumoniaIsaac SalazarNo ratings yet
- Appropriate Antibiotics For Peritonsillar Abscess - A 9 Month CohortDocument5 pagesAppropriate Antibiotics For Peritonsillar Abscess - A 9 Month CohortSiti Annisa NurfathiaNo ratings yet
- Valacyclovir For Episodic Treatment of Genital Herpes: A Shorter 3-Day Treatment Course Compared With 5-Day TreatmentDocument5 pagesValacyclovir For Episodic Treatment of Genital Herpes: A Shorter 3-Day Treatment Course Compared With 5-Day TreatmentEpi PanjaitanNo ratings yet
- Journal Presentation: Presented By-Vidisha Adarsh MPT (Neurosciences) Evaluator - Dr. Kritika Sharma (PT)Document51 pagesJournal Presentation: Presented By-Vidisha Adarsh MPT (Neurosciences) Evaluator - Dr. Kritika Sharma (PT)Urvashi SilalNo ratings yet
- Original Research: Intensive Care Unit Structure Variation and Implications For Early Mobilization PracticesDocument12 pagesOriginal Research: Intensive Care Unit Structure Variation and Implications For Early Mobilization Practicesandi kurniawanNo ratings yet
- Discharge Planning For Acute Coronary Syndrome Patients in A Tertiary Hospital: A Best Practice Implementation ProjectDocument17 pagesDischarge Planning For Acute Coronary Syndrome Patients in A Tertiary Hospital: A Best Practice Implementation ProjectMukhlis HasNo ratings yet
- Goal-Directed Resuscitation For Patients With Early Septic ShockDocument11 pagesGoal-Directed Resuscitation For Patients With Early Septic ShockmmsNo ratings yet
- P2.06-041 Telenursing: A Thoracic Surgery Nursing Initiative Aimed at Decreasing Hospital Readmissions and Increasing Patient SatisfactionDocument2 pagesP2.06-041 Telenursing: A Thoracic Surgery Nursing Initiative Aimed at Decreasing Hospital Readmissions and Increasing Patient Satisfactionervina wulandariNo ratings yet
- Effect of Intensive Health Education On Adherence To Treatment in Sputum Positive Pulmonary Tuberculosis PatientsDocument6 pagesEffect of Intensive Health Education On Adherence To Treatment in Sputum Positive Pulmonary Tuberculosis PatientspocutindahNo ratings yet
- Case Study #3Document26 pagesCase Study #3Reshma MohabeirNo ratings yet
- Medication-Related Problems in Critical Care Survivors - A Systematic ReviewDocument7 pagesMedication-Related Problems in Critical Care Survivors - A Systematic ReviewenesNo ratings yet
- Randomized Trial of An Education and Support Intervention To Prevent Readmission of Patients With Heart FailureDocument7 pagesRandomized Trial of An Education and Support Intervention To Prevent Readmission of Patients With Heart FailureThyka MayasariNo ratings yet
- Daily Interruption of Sedation in Patients Treated With Mechanical VentilationDocument4 pagesDaily Interruption of Sedation in Patients Treated With Mechanical VentilationMark_LiGx_8269No ratings yet
- G-4 Presentation DoneDocument24 pagesG-4 Presentation DoneAbdulrhman 123No ratings yet
- Search BMJ GroupDocument23 pagesSearch BMJ GroupCharles BrooksNo ratings yet
- Chlo Ramp He NicolDocument6 pagesChlo Ramp He NicolDivika ShilvanaNo ratings yet
- Breast-Cancer Adjuvant Therapy With Zoledronic Acid: Methods Study PatientsDocument11 pagesBreast-Cancer Adjuvant Therapy With Zoledronic Acid: Methods Study PatientsAn'umillah Arini ZidnaNo ratings yet
- Get Homework/Assignment DoneDocument6 pagesGet Homework/Assignment Donehomeworkping1No ratings yet
- THR RehabilitationDocument5 pagesTHR RehabilitationWei-Ting WuNo ratings yet
- Cisplatin-Based Adjuvant Chemotherapy in Patients With Completely Resected Non-Small-Cell Lung CancerDocument10 pagesCisplatin-Based Adjuvant Chemotherapy in Patients With Completely Resected Non-Small-Cell Lung CancerSouvik SahaNo ratings yet
- The Quality of Discharge Care Planning in Acute Stroke Care: Influencing Factors and Association With Postdischarge OutcomesDocument8 pagesThe Quality of Discharge Care Planning in Acute Stroke Care: Influencing Factors and Association With Postdischarge OutcomesnindyaNo ratings yet
- CRA 2010-Poster-PresentationsDocument236 pagesCRA 2010-Poster-PresentationsJoe GassNo ratings yet
- 2009hetrase CCMDocument12 pages2009hetrase CCMgiseladelarosa2006No ratings yet
- Out Come StudyDocument12 pagesOut Come StudyjaraNo ratings yet
- MeduloblastomaDocument7 pagesMeduloblastomasilvia erfanNo ratings yet
- Cannabis 10Document7 pagesCannabis 10CARLOS HERNAN FERNANDEZ CORDOBESNo ratings yet
- CMA AntibioticsDocument11 pagesCMA AntibioticsNovita Oktavianti DehiNo ratings yet
- Effect of A Centralized Clinical Pharmacy Anticoagulation Service On The Outcomes of Anticoagulation TherapyDocument8 pagesEffect of A Centralized Clinical Pharmacy Anticoagulation Service On The Outcomes of Anticoagulation TherapyDyla FaradhylaNo ratings yet
- ,adherence, 2008Document8 pages,adherence, 2008Abdurhman SeidNo ratings yet
- Journal Reading Etika MarcoDocument26 pagesJournal Reading Etika MarcoMarco GunawanNo ratings yet
- Pirfenidone and Nintedanib Compliance and Persistence in A Real World SettingDocument2 pagesPirfenidone and Nintedanib Compliance and Persistence in A Real World SettingmaleticjNo ratings yet
- Review 20 - 03 - 20 - 001Document18 pagesReview 20 - 03 - 20 - 001Ulices QuintanaNo ratings yet
- AddgfhgkklDocument10 pagesAddgfhgkklEza YusraNo ratings yet
- Farach 2014Document5 pagesFarach 2014mia widiastutiNo ratings yet
- IOI140094supp1 ProdDocument10 pagesIOI140094supp1 ProdArrizqi Ramadhani MuchtarNo ratings yet
- Which Patients Will Benefit From Psychosocial Intervention After Cystectomy For Bladder Cancer?Document8 pagesWhich Patients Will Benefit From Psychosocial Intervention After Cystectomy For Bladder Cancer?jedan185No ratings yet
- Pzad 183Document11 pagesPzad 183anvesh.jallapally.68No ratings yet
- Antibiotics For Abdominal Sepsis: Richard P. Wenzel, M.D., and Michael B. Edmond, M.D., M.P.HDocument2 pagesAntibiotics For Abdominal Sepsis: Richard P. Wenzel, M.D., and Michael B. Edmond, M.D., M.P.Hchebonk13No ratings yet
- Embedded Palliative Care For Patients With Metastatic Colorectal Cancer: A Mixed-Methods Pilot StudyDocument17 pagesEmbedded Palliative Care For Patients With Metastatic Colorectal Cancer: A Mixed-Methods Pilot StudyAnatha ChrisciliaNo ratings yet
- Early Intensive Care Unit Mobility Therapy in The Treatment of Acute Respiratory FailureDocument6 pagesEarly Intensive Care Unit Mobility Therapy in The Treatment of Acute Respiratory FailureTakashi NakamuraNo ratings yet
- Review of Acute Cancer Beds 1Document2 pagesReview of Acute Cancer Beds 1Cepi Ridwan FerdiansyahNo ratings yet
- Top Trials in Gastroenterology & HepatologyFrom EverandTop Trials in Gastroenterology & HepatologyRating: 4.5 out of 5 stars4.5/5 (7)
- Hirschprung's Disease, Celiac Disease, Hydrocephalus, Poisoning, Child Abuse, Anemia, Respiratory DisordersDocument139 pagesHirschprung's Disease, Celiac Disease, Hydrocephalus, Poisoning, Child Abuse, Anemia, Respiratory DisordersJhoms Poja FeriaNo ratings yet
- Medical Bacteriology (460 MIC) : Bacterial - Host RelationshipsDocument11 pagesMedical Bacteriology (460 MIC) : Bacterial - Host RelationshipsMuna Moh'dNo ratings yet
- Human ORFeome Gateway Entry Vector PENTR223Document6 pagesHuman ORFeome Gateway Entry Vector PENTR223Dave RapaconNo ratings yet
- Puttur DetailDocument12 pagesPuttur DetailakileshNo ratings yet
- SAI's vs. STD'S: - Syphilis - Chlamydia - Vaginitis - Herpes - GonnorheaDocument25 pagesSAI's vs. STD'S: - Syphilis - Chlamydia - Vaginitis - Herpes - GonnorheaMark CheneyNo ratings yet
- New Jersey Health Department Report RE: Dr. John VecchioneDocument11 pagesNew Jersey Health Department Report RE: Dr. John VecchioneNews12NJWebNo ratings yet
- SORL DEP Workout Phase 1Document17 pagesSORL DEP Workout Phase 1Anonymous pOggsIhOMNo ratings yet
- Joint Commision RegulationsDocument12 pagesJoint Commision Regulationsapi-223525467No ratings yet
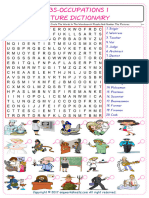
- Jobs-Occupations Find and Circle The Words in The Wordsearch Puzzle and Number The Pictures 7531Document2 pagesJobs-Occupations Find and Circle The Words in The Wordsearch Puzzle and Number The Pictures 7531Raquel NoeliaNo ratings yet
- Chemical Constituents From The Stems Of: Celastrus OrbiculatusDocument5 pagesChemical Constituents From The Stems Of: Celastrus OrbiculatusTuan PhamquocNo ratings yet
- Slender Quest DetailsDocument1 pageSlender Quest Detailsparents021No ratings yet
- Model AnalysisDocument7 pagesModel Analysissrishti jainNo ratings yet
- Aspartame Side EffectsDocument3 pagesAspartame Side Effectsnettie95No ratings yet
- Imogen Edwards-Jones, The Woman Behind Hotel Babylon, Is Training Her Sights On The Unlikeliest of Targets: The NHSDocument3 pagesImogen Edwards-Jones, The Woman Behind Hotel Babylon, Is Training Her Sights On The Unlikeliest of Targets: The NHSinfo7462100% (1)
- MDocument86 pagesMeheidariNo ratings yet
- PathologyDocument4 pagesPathologyVISHAKHANo ratings yet
- Critical Care EnvironmentDocument16 pagesCritical Care EnvironmentJeffrey KauvaNo ratings yet
- Lewis: Medical-Surgical Nursing, 10 Edition: Professional Nursing Practice Key Points Professional Nursing PracticeDocument3 pagesLewis: Medical-Surgical Nursing, 10 Edition: Professional Nursing Practice Key Points Professional Nursing PracticePrincess AgarwalNo ratings yet
- Stephen's Story: A 19 Year Old'S Life Lessons OnDocument16 pagesStephen's Story: A 19 Year Old'S Life Lessons OnSylvia DobsonNo ratings yet
- Your Electro Vibratory Body 13MB Re OCRedDocument305 pagesYour Electro Vibratory Body 13MB Re OCRedDanilo TorresNo ratings yet
- Nursing TheoryDocument15 pagesNursing TheoryTherese CanapiNo ratings yet
- SimuDocument13 pagesSimuPrince Rener Velasco PeraNo ratings yet
- Laporan Home Visit (Revin)Document24 pagesLaporan Home Visit (Revin)marinNo ratings yet
- Discontinuing An Intravenous InfusionDocument2 pagesDiscontinuing An Intravenous InfusionAgustin TrinaNo ratings yet
- Levetiracetam in Refractory Pediatric EpilepsyDocument11 pagesLevetiracetam in Refractory Pediatric EpilepsyAdlinaNo ratings yet
- Closed Fracture of Middle ClaviculaDocument12 pagesClosed Fracture of Middle ClaviculachiciNo ratings yet
- Cystic Lung Disease2Document26 pagesCystic Lung Disease2Shoban RajNo ratings yet
- DR Prathap C ReddyDocument4 pagesDR Prathap C ReddyShakin ShaNo ratings yet
Atients Hospitalized After Initial Outpatient Treatment For Community-Acquired Pneumonia
Atients Hospitalized After Initial Outpatient Treatment For Community-Acquired Pneumonia
Uploaded by
MazKha BudOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Atients Hospitalized After Initial Outpatient Treatment For Community-Acquired Pneumonia
Atients Hospitalized After Initial Outpatient Treatment For Community-Acquired Pneumonia
Uploaded by
MazKha BudCopyright:
Available Formats
INFECTIOUS DISEASE/BRIEF REPORT
376 A N N A LS OF EM ERGEN CY M ED I CI N E 3 1 : 3 MARCH 1998
P ati en ts H osp i tali zed After I n i ti al O u tp ati en t
Treatm en t for C om m u n i ty-Acqu i red P n eu m on i a
Michael FMinogue, MD, MS
*
Christopher M Coley, MD
*
Michael J Fine, MD, MSc
Thomas J Marrie, MD
Wishwa N Kapoor, MD, MPH
Daniel E Singer, MD
*
Study objective:To det ermi ne t he i nci dence, causes, and out -
comes of pat i ent s hospi t al i zed wi t hi n 30 days of i ni t i at i ng out -
pat i ent t reat ment f or communi t y-acqui red pneumoni a (CAP).
Design:Patients were enrolled in the Pneumonia Patient Out comes
Research Teams mul t i cent er, prospect i ve cohort st udy of CAP. Al l
hospi t al i zat i ons wi t hi n 30 days of st udy enrol l ment of pat i ent s
i ni t i al l y t reat ed as out pat i ent s f or CAP were recorded. Two physi -
ci ans used a set of predet ermi ned def i ni t i ons t o i ndependent l y
cat egori ze t he reasons f or t hese subsequent hospi t al i zat i ons.
Thi rt y-day mort al i t y rat e and measures of resol ut i on of pneumo-
ni a were assessed. The set t i ng i ncl uded t hree uni versi t y t eachi ng
hospi t al s, a communi t y t eachi ng hospi t al , and a st af f model medi -
cal pract i ce wi t hi n a heal t h mai nt enance organi zat i on.
Results:Of t he 944 enrol l ees wi t h CAP i ni t i al l y t reat ed i n t he
out pat i ent set t i ng, 71 (7.5%) w ere subsequent l y hospi t al i zed
wi t hi n 30 days. The reason f or subsequent hospi t al i zat i on was
CAP rel at ed i n 40 pat i ent s and comorbi di t y rel at ed i n 26 pat i ent s;
5 ref used an i ni t i al of f er of hospi t al i zat i on. Ni net y percent of
pneumoni a-rel at ed hospi t al i zat i ons occurred wi t hi n 10 days of
i ni t i al present at i on. Pat i ent s who were subsequent l y hospi t al i zed
requi red a medi an of 14 days t o ret urn t o usual act i vi t i es compared
wit h 6 days f or t hose who were not hospit alized (P<.0001). Pat i ent s
wi t h a subsequent hospi t al i zat i on had a hi gher 30-day mort al i t y
rat e, 4.2% compared wi t h .3% (P<.01).
Conclusion:A smal l proport i on of pat i ent s wi t h CAP i ni t i al l y
t reat ed i n t he out pat i ent set t i ng are subsequent l y hospi t al i zed.
Such pat i ent s f ace a hi gher ri sk of del ayed recovery or deat h.
However, t he vast maj ori t y of out pat i ent s, whet her subsequent l y
hospi t al i zed or not , had a successf ul resol ut i on of t hei r i l l ness.
Subsequent hospi t al i zat i on by 10 days af t er i ni t i al out pat i ent t reat -
ment seems a reasonabl e screeni ng t ool f or pot ent i al l y unsat i s-
f act ory qual i t y of care f or pat i ent s wi t h CAP.
[Mi nogue MF, Col ey CM, Fi ne MJ, Marri e TJ, Kapoor WN, Si nger
DE: Pat i ent s hospi t al i zed af t er i ni t i al out pat i ent t reat ment f or
communi t y-acqui red pneumoni a. Ann Emerg Med March 1998;31:
376-380.]
FromtheGeneral MedicineDivision,
Department of Medicine,
Massachusetts General Hospital and
Harvard Medical School, Boston,
MA
*
; theDivision of General Internal
Medicine, Department of Medicine,
University of Pittsburgh, Pittsburgh,
PA
; and theDepartments of
Medicineand Microbiology, Victoria
General Hospital and Dalhousie
University, Halifax, Nova Scotia,
Canada.
Received for publication
December 2, 1996. Revisions received
June5, 1997, August 15, 1997, and
November 5, 1997. Accepted for
publication November 18, 1997.
Presented at theSociety of General
Internal Medicines national meeting,
Washington DC, May 3, 1996.
Supported in part by theAgency for
Health CarePolicy and Research
(grant No. R01 HS06468) as part of
thePneumonia Patient Outcomes
Research Team(PORT) Project.
Dr Minoguewassupported by National
Research ServiceAward Training
Grant, No. PE 110001-06. Dr Fineis
supported by theRobert Wood Johnson
Foundation as a Generalist Physician
Faculty Scholar.
Copyright 1998 by theAmerican
Collegeof Emergency Physicians.
I N T R O D U C T I O N
Four million cases of community-acquired pneumonia (CAP)
occur annually in the United States with an estimated total
cost of $23 billion.
1
Inpatient treatment for CAP adds great
expense to the costs of patient care for CAP. Studies demon-
strating markedly different rates of hospitalization for CAP
in nearby geographic areas suggest that substituting out-
patient for inpatient therapy may be a reasonable strategy
for a large number of patients with CAP.
2
We anticipate
increasing use of such a strategy under the growing influ-
ence of managed care, especially where capitation contracts
place physicians at financial risk for the cost of patient care.
To ensure the safety of such a strategy, improved methods
of monitoring outcomes of patients treated for CAP in the
outpatient setting are needed. Subsequent CAP-related
hospitalization after initial outpatient therapy is a clinically
relevant outcome measure to assess in these quality improve-
ment efforts.
We studied patients from a large cohort of outpatients
treated for CAP who were hospitalized within 30 days after
beginning outpatient treatment. The goals of this study
were as follows: (1) to determine the incidence of subsequent
hospitalization with this illness, (2) to assess the reasons for
subsequent hospitalizations, and (3) to describe the out-
comes of outpatients who were subsequently hospitalized.
M E T H O D S
This study was conducted as part of the Patient Outcomes
Research Team (PORT) multicenter, prospective, cohort
study of patients with CAP. This article reports the analysis
of the subset of enrollees who were initially treated in the
outpatient setting. The bioethics institutional review board
at each study site approved this study.
Study sites
The pneumonia PORT cohort study was conducted be-
tween October 1991 and March 1994 at five medical insti-
tutions in three geographic locations: University of Pittsburgh
Medical Center, a 942-bed university teaching hospital, and
St. Francis Medical Center, a 427-bed community teaching
hospital, in Pittsburgh, PA; Massachusetts General Hospital,
an 889-bed university teaching hospital, and Harvard
Community Health Plan-Kenmore Center, a 44,931-mem-
ber staff model health care center within a large health main-
tenance organization, in Boston, MA; and Victoria General
Hospital, a 637-bed university teaching hospital, in Halifax,
Nova Scotia, Canada, with a large number of affiliated com-
munity practitioners in the greater Halifax region.
Study population
Potential study subjects were identified by screening
patients presenting to emergency departments, medical
walk-in clinics, and practitioner offices. Eligible patients
were identified by clinical research assistants through daily
review of emergency, admitting, and radiology department
records as well as patient logs kept in these areas. Study
inclusion criteria were as follows: (1) age 18 years or older,
(2) acute onset of one or more clinical symptoms suggestive
of pneumonia, (3) an acute radiographic infiltrate within
24 hours of presentation, and (4) provision of informed con-
sent by the patient or proxy. Patients were ineligible for the
study if they were discharged from the hospital within 10
days preceding presentation, were known to be HIV-posi-
tive, or were previously enrolled in the cohort study. Approxi-
mately 40% of the patients recruited from the Massachusetts
General Hospital and the University of Pittsburgh were
enrolled from an ED.
Baseline characteristics and medical outcomes
Trained research staff collected baseline data on patient
sociodemographic characteristics, comorbid illnesses, physi-
cal examination findings, and laboratory findings. The
presence of five CAP-related symptoms (cough, sputum
production, dyspnea, pleuritic chest pain, and fatigue) was
assessed at baseline and at 30 days. Severity of illness at
presentation with CAP was classified into five ordered classes
with an increasing risk of 30-day mortality on the basis of
a validated prediction rule that incorporates patient demo-
graphics, comorbidity, vital signs, and laboratory informa-
tion.
3
The cumulative mortality rates for these classes are
as follows: Class I .1%, class II .6%, class III .9%, class IV
9.3%, and class V 27%. Class I patients were young (median
age, 35 to 37 years) without pertinent coexisting illnesses
or abnormalities on physical examination. Class II patients
were typically middle-aged (median age, 58 to 59 years),
and assigned to this class solely on the basis of their age.
Class III patients were older (median age, 72 years), and
most had at least one pertinent coexisting illness, physical
examination abnormality, or laboratory or radiographic
abnormality. Class IV and V patients were typically elderly
(median age 75) and never assigned to these classes because
of age alone; the majority had abnormalities in two (class
IV) or all three (class V) of the pertinent risk factor cate-
gories.
3
Outcomes, such as time to return to usual activity
and mortality rate at 30 days after study enrollment, were
determined by follow-up interviews and medical record
reviews. For all patients who died, clinical synopses were
prepared using patients medical records and interviews of
families and caregivers of the deceased. Underlying and
immediate causes of death were assigned independently
COMMUNITY-ACQUIRED PNEUMONIA
Minogueet al
MARCH 1998 3 1 : 3 A N N A LS OF EM ERGEN CY M ED I CI N E 377
by two investigators according to World Health Organiza-
tion definitions.
Reasons for subsequent hospitalization
Two physicians (MFM, CMC) applied a predetermined
set of categories to assign independently reasons for sub-
sequent hospitalizations that occurred within 30 days of
presentation with CAP. The 30-day period was chosen be-
cause it is a sufficiently long interval to capture most medical
care relevant to a given episode of CAP.
The categories considered were (1) patient refusal of an
initial offer of hospitalization, (2) adverse reaction to therapy
for CAP, (3) worsening symptoms or signs of CAP, and (4)
management of a condition other than CAP. We defined
CAP-related hospitalizations as those related to either
worsening symptoms or signs of CAP or adverse reactions
to therapy for CAP (hospitalization reasons 2 or 3). We de-
fined comorbidity-related hospitalizations as those related
to a condition other than CAP (hospitalization reason 4).
We limited the comorbidity-related category to those where
the comorbid condition was the dominant cause for the
hospitalization. Disagreements between the two investiga-
tors were resolved by reviewing the individual cases with
a third investigator.
A representative example of a hospitalization related to
an adverse reaction to therapy for CAP is a 48-year-old
woman for whom erythromycin was prescribed. She re-
turned to the ED 1 day later with nausea and vomiting and
was hospitalized. A representative case of a hospitalization
related to worsening symptoms or signs of CAP is a 52-
year-old man initially treated as an outpatient who returned
5 days later with increased shortness of breath and pleurisy
and was hospitalized. A representative case of a hospitaliza-
tion related to a comorbid condition is a 37-year-old woman
who was hospitalized for the management of a ureteral
calculus 23 days after a diagnosis of CAP. We assessed the
reliability of assignment of reasons for subsequent hospitaliza-
tion using the statistic.
Statistical analysis
The outpatients who were not hospitalized were com-
pared with those who had a subsequent hospitalization using
the
2
statistic or Fishers exact test for categorical variables
and Students ttest or Wilcoxon rank sum test for continuous
variables. Time to return to usual activities was analyzed
according to the Kaplan-Meier technique with statistical
significance assessed by the log-rank test.
R E S U L T S
Of the 4,002 patients who met study eligibility criteria,
2,287 (57.1%) were enrolled. One thousand three hundred
thirty-seven of the enrollees were admitted to a hospital at
presentation. The remaining 944 patients were initially
treated in an outpatient setting and constitute the study
population. The dominant reason for nonenrollment was
physician or patient refusal. Enrolled outpatients were
younger (mean age 44.6 versus 50.0 years, P=.001), more
likely to be white (84% versus 64%, P=.001), and less
severely ill at presentation (risk class I, 62.2% versus 50.6%,
P=.001), than the eligible patients who were not enrolled.
Of the 944 study patients initially treated as outpatients
(Figure), 71 (7.5%) were hospitalized within 30 days of
presentation with CAP. Five of these subsequently hospital-
ized patients refused an initial recommendation for hospital-
ization; it is not known how many of the not hospitalized
outpatients (n=873) had refused hospitalization. Forty
COMMUNITY-ACQUIRED PNEUMONIA
Minogueet al
378 A N N A LS OF EM ERGEN CY M ED I CI N E 3 1 : 3 MARCH 1998
Figure.
Carepath of patients initially treated in an outpatient setting
for CAP by 30 days fromenrollment. A total of 944 patients
enrolled in thePORT multicenter, prospectivecohort study of
CAP initially received outpatient therapy. Of these, 873 were
not hospitalized within 30 days of presentingwith CAP. The
other 71 outpatients weresubsequently hospitalized within
30 days of presentation with CAP. Of these71 patients, 5
refused an initial recommendation of hospitalization, 40 had
a CAP-related reason for hospitalization, and theother 26
werehospitalized for a comorbidity-related reason. Of the40
CAP-related hospitalizations, 33 wererelated to worsening
symptoms or signs of CAP and 7 becauseof an adverse
reaction to therapy for CAP.
944
Out pat i ent s
71 (7.5%)
Subsequent hospi t al i zat i ons
873 (92.5%)
Not hospi t al i zed
26 Comorbi di t y-rel at ed
hospi t al i zat i ons
5 Ref used
i ni t i al hospi t al i zat i on
40 CAP-rel at ed
hospi t al i zat i ons
33 had worseni ng sympt oms or si gns of CAP.
7 had an adverse react i on t o t herapy f or CAP.
patients had a CAP-related reason for subsequent hospital-
ization33 because of worsening symptoms or signs of
CAP and 7 because of an adverse reaction to an antibiotic
prescribed for CAP. The statistic was .81, indicating excel-
lent reliability between the physicians assigning reasons
for hospitalization.
4
Outpatients who were subsequently hospitalized were
older than those who were not (Table 1). Although patients
who were subsequently hospitalized had higher levels of
illness severity at presentation than those who were not sub-
sequently hospitalized, both groups of patients were pre-
dominantly in the lower risk classes (class I, II, or III). No
significant differences in vital signs were detected between
these two groups. However, because many patients were
seen in clinic settings, vital sign data, such as respiratory rate,
were frequently not recorded. A higher percentage of the
subsequently hospitalized group had comorbid cardiac dis-
ease or chronic obstructive pulmonary disease. No signifi-
cant differences were found in sex, race, or living location.
Reasons for subsequent hospitalization according to time from
presentation
Among the patients who were hospitalized within 30
days of presentation with CAP, those with a CAP-related
reason were hospitalized a mean of 4.9 days from presenta-
tion, compared with 13.6 days for those with a comorbid-
ity-related reason (P<.001). Table 2 shows the time from
enrollment to hospitalization for these two categories of
hospitalization. By day 10, 36 (90%) of 40 CAP-related and
9 (35%) of 26 comorbidity-related hospitalizations had
occurred. The majority of hospitalizations that occurred
more than 10 days after enrollment, 17 of 21 (81%), were
comorbidity related.
Outcomes
The subsequent hospitalization group had a higher 30-
day mortality rate, 4.2% (n=3) compared with .3% (n=3)
for the not hospitalized group (P<.01). The three deaths
in the not hospitalized group included a 90-year-old nurs-
ing home resident whose family requested that only limited
medical interventions be made, an 84-year-old who was
found dead at home by family members, and a 31-year-old
patient with type I diabetes who had a sudden cardiac death
27 days after presenting with CAP. Of the three deaths among
patients in the subsequent hospitalization group, only one
had a CAP-related reason for hospitalization, a 98-year-old
whose underlying cause of death was listed as renal failure.
The other two deaths in this group were in elderly patients
as well80 and 84 years of age. Their underlying causes
of death were end-stage renal disease and pancreatic cancer,
respectively. None of these three patients had a do not
resuscitate order listed in their medical record.
Patients in the subsequent hospitalization group (n=71)
took a median of 14 days (range 0 to 35 days) to return to
COMMUNITY-ACQUIRED PNEUMONIA
Minogueet al
MARCH 1998 3 1 : 3 A N N A LS OF EM ERGEN CY M ED I CI N E 379
Table 1.
Outpatients with CAP: Comparison of thosehospitalized within
30 days with thosenot hospitalized.
Hospitalized Not Hospitalized
Patient Characteristics (n=71) (n=873) P Value
Age (mean, yearsSD) 52.020.4 44.117.9 <.001
Baseline risk class (%)
*
.001
I 44 64
II 28 26
III 17 7
IV and V 11 3
Vital signs at presentation (%)
Temperat ure >38.4 C (101 F) 21 19 .72
Syst ol i c bl ood pressure <90 mm Hg 2 .5 .28
Respi rat i ons >30/ mi nut e 2 1 .52
Pul se >100 beat s/ mi nut e 40 29 .11
Sex (%male) 52 46 .34
Race (%white) 80 84 .44
Living location 86 82 .52
(%at home)
Selected comorbid
conditions
(%)
Ci garet t e smoki ng hi st ory 35 28 .18
Coronary art ery di sease 14 5 .01
Neopl ast i c di sease 10 6 .18
Chroni c obst ruct i ve pul monary 15 5 <.001
di sease
Di abet es mel l i t us 6 4 <.35
Congest i ve heart f ai l ure 11 2 <.0001
*
30-Day mort al i t y rat e by ri sk cl ass: I=.1%, II=.6%, III=.9%, IV=9.3%, and V=27%.
Val ues f or t emperat ure, syst ol i c bl ood pressure, respi rat i on rat e, and pul se were mi ssi ng i n
27%, 27%, 49%, and 33% of pat i ent s, respect i vel y.
Sel ect ed comorbi d condi t i ons are not mut ual l y excl usi ve.
Table 2.
Patients hospitalized within 30 days of initial outpatient treat-
ment of CAP: Timeto hospitalization by hospitalization category.
Pneumonia-Related Comorbidity-Related
Hospitalizations (n=40) Hospitalizations (n=26)
Time from
Enrollment to
Hospitalization Cumulative Cumulative
(Range in Days) No. No. (%) No. No. (%)
02 21 21 (53) 5 5 (19)
37 12 33 (83) 2 7 (27)
810 3 36 (90) 2 9 (35)
1120 2 38 (95) 11 20 (77)
2129 2 40 (100) 6 26 (100)
usual activities compared with 6 days (range 0 to 86 days)
for those in the not hospitalized group (n=873, P<.0001).
However, 88% of the subsequent hospitalization and 93%
of the not hospitalized patients had returned to usual activi-
ties by 30 days from study enrollment. By 30 days there
were no significant differences in CAP-related symptoms
(eg, cough, sputum production, dyspnea, pleuritic chest
pain, and fatigue).
D I S C U S S I O N
This study provides insights for clinicians who now man-
age resource utilization and administrators who monitor
quality of medical care. We found that 71 (7.5%) of 944
outpatients with CAP, derived from a variety of outpatient
settings, were subsequently hospitalized within 30 days of
beginning outpatient treatment. Forty of these 71 hospital-
izations were CAP related. We found that 90% of all CAP-
related hospitalizations occurred within 10 days of initial
presentation, whereas hospitalizations beyond 10 days were
predominantly related to comorbid illnesses. Outpatients
who had a subsequent hospitalization tended to be older,
were more severely ill at presentation, and more frequently
had significant comorbid illnesses than those who were not
hospitalized. Although these differences were statistically
significant, there was considerable overlap in the distribu-
tions of these features in the two groups. The subsequently
hospitalized group also had worse outcomes measured in
terms of delayed return to usual activities and higher 30-day
mortality rate. Overall, though, the majority of patients who
initially received outpatient treatment for CAP, even those
who had a subsequent hospitalization, had a successful
resolution of their illness.
The generalizability of our findings may be limited by the
way our patient cohort was assembled. In particular, the
proportion hospitalized will likely vary somewhat in differ-
ent outpatient settings, with patient populations present-
ing a different spectrum of disease severity or psychosocial
problems.One can anticipate higher rates of subsequent
hospitalization among patients initially seen in an emergency
department than office or clinic settings.
For any given patient, neither subsequent hospitalization
nor poor outcome necessarily demonstrates poor quality care.
Some small percentage of patients at low risk of a complicated
course of CAP who appear likely to improve with outpatient
treatment will require subsequent hospitalization.
5
However,
as the percentage requiring subsequent hospitalization in-
creases, the appropriateness of the initial site of care decision
will be called into question, particularly if clinically meaning-
ful complications develop in such patients. Improved pro-
cesses of care may be achieved by studying such putative
failures of therapy in the same manner as studying hospital
readmissions after initial inpatient care.
6
Because of the growing influence of managed care orga-
nizations on health care delivery, it is likely that a greater
proportion of treatment of CAP will be performed in the
outpatient setting. Evidenced-based triage rules may help
to optimize this increased emphasis on outpatient treat-
ment.
7
Patient outcomes must be monitored closely. An
overzealous use of outpatient treatment of CAP may worsen
outcomes.
8
Our results suggest that the incidence of hos-
pitalization within 10 days of beginning outpatient treat-
ment for CAP is a reasonable screening tool for unsatisfactory
quality of care in this illness. With the growing sophistica-
tion of billing and clinical information systems, health
delivery organizations may be able to readily identify these
cases. Further detailed review of such subsequent hospital-
izations can confirm poor quality of care and lead to strate-
gies to improve treatment of CAP.
R E F E R E N C E S
1. Bart l et t JG, M undy LM : Communi t y-acqui red pneumoni a. N Engl J M ed 1995;333:1618-1624.
2. Wennberg JE, M cpherson K, Caper P: Wi l l payment based on di agnosi s-rel at ed groups cont rol
hospi t al cost s? N Engl J M ed 1984;311:295-300.
3. Fi ne M J, Aubl e TE, Yearl y DM , et al : Improvi ng t he appropri at eness of hospi t al care i n commu-
ni t y-acqui red pneumoni a: A predi ct i on rul e t o i dent i f y pat i ent s at l ow ri sk f or mort al i t y and ot her
adverse out comes. N Engl J M ed 1997;336:243-250.
4. Sacket t DL, Haynes RB, Guyat t GH, et al : Cl i ni cal Epi demi ol ogy A Basi c Sci ence f or Cl i ni cal
M edi ci ne, ed 2. Bost on: Li t t l e Brown, 1991:30-31.
5. M assanari RM : Qual i t y i mprovement : Cont rol l i ng t he ri sks of adverse event s, i n Wenzel RP
(ed): Assessi ng Qual i t y Heal t h Care. New York: Wi l l i ams & Wi l ki ns, 1992:201.
6. Frankl SE, Breel i ng JL, Gol dman L: Prevent abi l i t y of emergent hospi t al readmi ssi on. Am J M ed
1991;90:667-674.
7. Wasson JH, Sox HC: Cl i ni cal Predi ct i on rul es, have t hey come of age? JAMA 1996;275:641-642.
8. Denman SJ, Et t i nger WH, Zarki n BA, et al : Short -t erm out comes of el derl y pat i ent s di scharged
f rom an emergency depart ment . J Am Geri at r Soc 1989;37:937-943.
We grat ef ul l y acknowl edge t he assi st ance of El mer Hol zi nger, M D, f or coordi nat i ng
st udy act i vi t i es at St Franci s Medi cal Cent er; Karen Lahi ve, MD, f or coordi nat i ng st udy
act i vi t i es at t he Harvard Communi t y Heal t h Pl an; Li nda Hough, M PH, as proj ect coor-
di nat or, Terry Sef ci k, M S, f or dat a management , D Scot t Obrosky, M S, f or st at i st i cal
assi st ance; and t he f ol l owi ng cl i ni cal research assi st ant s f or cohort st udy pat i ent enrol l -
ment and dat a col l ect i on: Mary Wal sh, RN, Lei l a Haddad, AB, and Mari an Hendershot ,
RN, i n Bost on; Rhonda Grandy, RN, Jacki e Cunni ng, RN, Dawn Menon, RN, Li nda Kraf t ,
RN, and M axi ne Young, RN, i n Hal i f ax.
Reprint no. 47/1/88395
Address for reprints:
M i chael F M i nogue, M D, M S380
Harvard Af f i l i at ed Emergency M edi ci ne Resi dency
Bri gham and Women s Hospi t al M assachuset t s General Hospi t al
75 Franci s St reet 32 Frui t St reet
Bost on, M A 02114 Bost on, M A 02115
COMMUNITY-ACQUIRED PNEUMONIA
Minogueet al
380 A N N A LS OF EM ERGEN CY M ED I CI N E 3 1 : 3 MARCH 1998
You might also like
- Ineffective Airway Clearance Related To Retained Mucus Secretion As Evidenced by Unproductive CoughDocument1 pageIneffective Airway Clearance Related To Retained Mucus Secretion As Evidenced by Unproductive Coughdana93% (30)
- Assessment and Management of Preoperative Anxiety: London, United KingdomDocument6 pagesAssessment and Management of Preoperative Anxiety: London, United KingdomrsudabadiNo ratings yet
- Critical Care Goals and ObjectivesDocument28 pagesCritical Care Goals and ObjectivesjyothiNo ratings yet
- Gapuz Maternal Health NursingDocument80 pagesGapuz Maternal Health NursingHayes Clover100% (6)
- Articulo NeumoniaDocument7 pagesArticulo NeumoniaEd BarajasNo ratings yet
- Jurnal 1Document6 pagesJurnal 1Pratiwi AyuningtyasNo ratings yet
- Treatment Completion and Costs of A Randomized Trial of Rifampin For 4 Months Versus Isoniazid For 9 MonthsDocument5 pagesTreatment Completion and Costs of A Randomized Trial of Rifampin For 4 Months Versus Isoniazid For 9 MonthsSyairah Banu DjufriNo ratings yet
- The Pattern of Antimicrobial Use For Palliative Care In-Patients During The Last Week of LifeDocument4 pagesThe Pattern of Antimicrobial Use For Palliative Care In-Patients During The Last Week of Lifem1k0eNo ratings yet
- Long-Stay of PICU in SepsisDocument6 pagesLong-Stay of PICU in SepsisSanti IskandarNo ratings yet
- Coach 2023Document11 pagesCoach 2023Guilherme CarelliNo ratings yet
- Medicine American Journal of Hospice and PalliativeDocument6 pagesMedicine American Journal of Hospice and Palliativem1k0eNo ratings yet
- High-Dose Rifapentine With Moxifloxacin For Pulmonary TuberculosisDocument10 pagesHigh-Dose Rifapentine With Moxifloxacin For Pulmonary TuberculosisSoleh SundawaNo ratings yet
- Chan 2004Document8 pagesChan 2004clinica cuelloNo ratings yet
- Selected Topics: Prehospital CareDocument9 pagesSelected Topics: Prehospital CareYo MeNo ratings yet
- Two-Year Survival Comparing Web-Based Symptom Monitoring Vs Routine Surveillance Following Treatment For Lung CancerDocument6 pagesTwo-Year Survival Comparing Web-Based Symptom Monitoring Vs Routine Surveillance Following Treatment For Lung CancerValerie LascauxNo ratings yet
- Huang 2018Document14 pagesHuang 2018amazeyragNo ratings yet
- PROCESSDocument11 pagesPROCESSandrea vargasNo ratings yet
- Oral AbstractsDocument210 pagesOral AbstractspascutaNo ratings yet
- Procalcitonin PneumoniaDocument14 pagesProcalcitonin PneumoniaMr. LNo ratings yet
- Prediction Model For Shortterm Mortality After Palliative Therapy For Patients Having Advanced Cancer - A Cohort Study From Routine Electronic Medical DataDocument10 pagesPrediction Model For Shortterm Mortality After Palliative Therapy For Patients Having Advanced Cancer - A Cohort Study From Routine Electronic Medical DataHollis LukNo ratings yet
- Low Dose Prednisolone in Community Acquired PneumoniaDocument15 pagesLow Dose Prednisolone in Community Acquired PneumoniaIsaac SalazarNo ratings yet
- Appropriate Antibiotics For Peritonsillar Abscess - A 9 Month CohortDocument5 pagesAppropriate Antibiotics For Peritonsillar Abscess - A 9 Month CohortSiti Annisa NurfathiaNo ratings yet
- Valacyclovir For Episodic Treatment of Genital Herpes: A Shorter 3-Day Treatment Course Compared With 5-Day TreatmentDocument5 pagesValacyclovir For Episodic Treatment of Genital Herpes: A Shorter 3-Day Treatment Course Compared With 5-Day TreatmentEpi PanjaitanNo ratings yet
- Journal Presentation: Presented By-Vidisha Adarsh MPT (Neurosciences) Evaluator - Dr. Kritika Sharma (PT)Document51 pagesJournal Presentation: Presented By-Vidisha Adarsh MPT (Neurosciences) Evaluator - Dr. Kritika Sharma (PT)Urvashi SilalNo ratings yet
- Original Research: Intensive Care Unit Structure Variation and Implications For Early Mobilization PracticesDocument12 pagesOriginal Research: Intensive Care Unit Structure Variation and Implications For Early Mobilization Practicesandi kurniawanNo ratings yet
- Discharge Planning For Acute Coronary Syndrome Patients in A Tertiary Hospital: A Best Practice Implementation ProjectDocument17 pagesDischarge Planning For Acute Coronary Syndrome Patients in A Tertiary Hospital: A Best Practice Implementation ProjectMukhlis HasNo ratings yet
- Goal-Directed Resuscitation For Patients With Early Septic ShockDocument11 pagesGoal-Directed Resuscitation For Patients With Early Septic ShockmmsNo ratings yet
- P2.06-041 Telenursing: A Thoracic Surgery Nursing Initiative Aimed at Decreasing Hospital Readmissions and Increasing Patient SatisfactionDocument2 pagesP2.06-041 Telenursing: A Thoracic Surgery Nursing Initiative Aimed at Decreasing Hospital Readmissions and Increasing Patient Satisfactionervina wulandariNo ratings yet
- Effect of Intensive Health Education On Adherence To Treatment in Sputum Positive Pulmonary Tuberculosis PatientsDocument6 pagesEffect of Intensive Health Education On Adherence To Treatment in Sputum Positive Pulmonary Tuberculosis PatientspocutindahNo ratings yet
- Case Study #3Document26 pagesCase Study #3Reshma MohabeirNo ratings yet
- Medication-Related Problems in Critical Care Survivors - A Systematic ReviewDocument7 pagesMedication-Related Problems in Critical Care Survivors - A Systematic ReviewenesNo ratings yet
- Randomized Trial of An Education and Support Intervention To Prevent Readmission of Patients With Heart FailureDocument7 pagesRandomized Trial of An Education and Support Intervention To Prevent Readmission of Patients With Heart FailureThyka MayasariNo ratings yet
- Daily Interruption of Sedation in Patients Treated With Mechanical VentilationDocument4 pagesDaily Interruption of Sedation in Patients Treated With Mechanical VentilationMark_LiGx_8269No ratings yet
- G-4 Presentation DoneDocument24 pagesG-4 Presentation DoneAbdulrhman 123No ratings yet
- Search BMJ GroupDocument23 pagesSearch BMJ GroupCharles BrooksNo ratings yet
- Chlo Ramp He NicolDocument6 pagesChlo Ramp He NicolDivika ShilvanaNo ratings yet
- Breast-Cancer Adjuvant Therapy With Zoledronic Acid: Methods Study PatientsDocument11 pagesBreast-Cancer Adjuvant Therapy With Zoledronic Acid: Methods Study PatientsAn'umillah Arini ZidnaNo ratings yet
- Get Homework/Assignment DoneDocument6 pagesGet Homework/Assignment Donehomeworkping1No ratings yet
- THR RehabilitationDocument5 pagesTHR RehabilitationWei-Ting WuNo ratings yet
- Cisplatin-Based Adjuvant Chemotherapy in Patients With Completely Resected Non-Small-Cell Lung CancerDocument10 pagesCisplatin-Based Adjuvant Chemotherapy in Patients With Completely Resected Non-Small-Cell Lung CancerSouvik SahaNo ratings yet
- The Quality of Discharge Care Planning in Acute Stroke Care: Influencing Factors and Association With Postdischarge OutcomesDocument8 pagesThe Quality of Discharge Care Planning in Acute Stroke Care: Influencing Factors and Association With Postdischarge OutcomesnindyaNo ratings yet
- CRA 2010-Poster-PresentationsDocument236 pagesCRA 2010-Poster-PresentationsJoe GassNo ratings yet
- 2009hetrase CCMDocument12 pages2009hetrase CCMgiseladelarosa2006No ratings yet
- Out Come StudyDocument12 pagesOut Come StudyjaraNo ratings yet
- MeduloblastomaDocument7 pagesMeduloblastomasilvia erfanNo ratings yet
- Cannabis 10Document7 pagesCannabis 10CARLOS HERNAN FERNANDEZ CORDOBESNo ratings yet
- CMA AntibioticsDocument11 pagesCMA AntibioticsNovita Oktavianti DehiNo ratings yet
- Effect of A Centralized Clinical Pharmacy Anticoagulation Service On The Outcomes of Anticoagulation TherapyDocument8 pagesEffect of A Centralized Clinical Pharmacy Anticoagulation Service On The Outcomes of Anticoagulation TherapyDyla FaradhylaNo ratings yet
- ,adherence, 2008Document8 pages,adherence, 2008Abdurhman SeidNo ratings yet
- Journal Reading Etika MarcoDocument26 pagesJournal Reading Etika MarcoMarco GunawanNo ratings yet
- Pirfenidone and Nintedanib Compliance and Persistence in A Real World SettingDocument2 pagesPirfenidone and Nintedanib Compliance and Persistence in A Real World SettingmaleticjNo ratings yet
- Review 20 - 03 - 20 - 001Document18 pagesReview 20 - 03 - 20 - 001Ulices QuintanaNo ratings yet
- AddgfhgkklDocument10 pagesAddgfhgkklEza YusraNo ratings yet
- Farach 2014Document5 pagesFarach 2014mia widiastutiNo ratings yet
- IOI140094supp1 ProdDocument10 pagesIOI140094supp1 ProdArrizqi Ramadhani MuchtarNo ratings yet
- Which Patients Will Benefit From Psychosocial Intervention After Cystectomy For Bladder Cancer?Document8 pagesWhich Patients Will Benefit From Psychosocial Intervention After Cystectomy For Bladder Cancer?jedan185No ratings yet
- Pzad 183Document11 pagesPzad 183anvesh.jallapally.68No ratings yet
- Antibiotics For Abdominal Sepsis: Richard P. Wenzel, M.D., and Michael B. Edmond, M.D., M.P.HDocument2 pagesAntibiotics For Abdominal Sepsis: Richard P. Wenzel, M.D., and Michael B. Edmond, M.D., M.P.Hchebonk13No ratings yet
- Embedded Palliative Care For Patients With Metastatic Colorectal Cancer: A Mixed-Methods Pilot StudyDocument17 pagesEmbedded Palliative Care For Patients With Metastatic Colorectal Cancer: A Mixed-Methods Pilot StudyAnatha ChrisciliaNo ratings yet
- Early Intensive Care Unit Mobility Therapy in The Treatment of Acute Respiratory FailureDocument6 pagesEarly Intensive Care Unit Mobility Therapy in The Treatment of Acute Respiratory FailureTakashi NakamuraNo ratings yet
- Review of Acute Cancer Beds 1Document2 pagesReview of Acute Cancer Beds 1Cepi Ridwan FerdiansyahNo ratings yet
- Top Trials in Gastroenterology & HepatologyFrom EverandTop Trials in Gastroenterology & HepatologyRating: 4.5 out of 5 stars4.5/5 (7)
- Hirschprung's Disease, Celiac Disease, Hydrocephalus, Poisoning, Child Abuse, Anemia, Respiratory DisordersDocument139 pagesHirschprung's Disease, Celiac Disease, Hydrocephalus, Poisoning, Child Abuse, Anemia, Respiratory DisordersJhoms Poja FeriaNo ratings yet
- Medical Bacteriology (460 MIC) : Bacterial - Host RelationshipsDocument11 pagesMedical Bacteriology (460 MIC) : Bacterial - Host RelationshipsMuna Moh'dNo ratings yet
- Human ORFeome Gateway Entry Vector PENTR223Document6 pagesHuman ORFeome Gateway Entry Vector PENTR223Dave RapaconNo ratings yet
- Puttur DetailDocument12 pagesPuttur DetailakileshNo ratings yet
- SAI's vs. STD'S: - Syphilis - Chlamydia - Vaginitis - Herpes - GonnorheaDocument25 pagesSAI's vs. STD'S: - Syphilis - Chlamydia - Vaginitis - Herpes - GonnorheaMark CheneyNo ratings yet
- New Jersey Health Department Report RE: Dr. John VecchioneDocument11 pagesNew Jersey Health Department Report RE: Dr. John VecchioneNews12NJWebNo ratings yet
- SORL DEP Workout Phase 1Document17 pagesSORL DEP Workout Phase 1Anonymous pOggsIhOMNo ratings yet
- Joint Commision RegulationsDocument12 pagesJoint Commision Regulationsapi-223525467No ratings yet
- Jobs-Occupations Find and Circle The Words in The Wordsearch Puzzle and Number The Pictures 7531Document2 pagesJobs-Occupations Find and Circle The Words in The Wordsearch Puzzle and Number The Pictures 7531Raquel NoeliaNo ratings yet
- Chemical Constituents From The Stems Of: Celastrus OrbiculatusDocument5 pagesChemical Constituents From The Stems Of: Celastrus OrbiculatusTuan PhamquocNo ratings yet
- Slender Quest DetailsDocument1 pageSlender Quest Detailsparents021No ratings yet
- Model AnalysisDocument7 pagesModel Analysissrishti jainNo ratings yet
- Aspartame Side EffectsDocument3 pagesAspartame Side Effectsnettie95No ratings yet
- Imogen Edwards-Jones, The Woman Behind Hotel Babylon, Is Training Her Sights On The Unlikeliest of Targets: The NHSDocument3 pagesImogen Edwards-Jones, The Woman Behind Hotel Babylon, Is Training Her Sights On The Unlikeliest of Targets: The NHSinfo7462100% (1)
- MDocument86 pagesMeheidariNo ratings yet
- PathologyDocument4 pagesPathologyVISHAKHANo ratings yet
- Critical Care EnvironmentDocument16 pagesCritical Care EnvironmentJeffrey KauvaNo ratings yet
- Lewis: Medical-Surgical Nursing, 10 Edition: Professional Nursing Practice Key Points Professional Nursing PracticeDocument3 pagesLewis: Medical-Surgical Nursing, 10 Edition: Professional Nursing Practice Key Points Professional Nursing PracticePrincess AgarwalNo ratings yet
- Stephen's Story: A 19 Year Old'S Life Lessons OnDocument16 pagesStephen's Story: A 19 Year Old'S Life Lessons OnSylvia DobsonNo ratings yet
- Your Electro Vibratory Body 13MB Re OCRedDocument305 pagesYour Electro Vibratory Body 13MB Re OCRedDanilo TorresNo ratings yet
- Nursing TheoryDocument15 pagesNursing TheoryTherese CanapiNo ratings yet
- SimuDocument13 pagesSimuPrince Rener Velasco PeraNo ratings yet
- Laporan Home Visit (Revin)Document24 pagesLaporan Home Visit (Revin)marinNo ratings yet
- Discontinuing An Intravenous InfusionDocument2 pagesDiscontinuing An Intravenous InfusionAgustin TrinaNo ratings yet
- Levetiracetam in Refractory Pediatric EpilepsyDocument11 pagesLevetiracetam in Refractory Pediatric EpilepsyAdlinaNo ratings yet
- Closed Fracture of Middle ClaviculaDocument12 pagesClosed Fracture of Middle ClaviculachiciNo ratings yet
- Cystic Lung Disease2Document26 pagesCystic Lung Disease2Shoban RajNo ratings yet
- DR Prathap C ReddyDocument4 pagesDR Prathap C ReddyShakin ShaNo ratings yet