Professional Documents
Culture Documents
Management of Limb Injuries in Adults and Children Over 2 Years
Management of Limb Injuries in Adults and Children Over 2 Years
Uploaded by
justforuro0 ratings0% found this document useful (0 votes)
47 views17 pagesThis document provides guidance on the assessment, treatment, and management of limb injuries like fractures and soft tissue injuries in adults and children over 2 years old. It outlines symptoms to assess for, specific history to obtain, examinations to perform, guidelines on radiography requests, descriptions of common fractures, and recommendations for management and follow-up of various upper limb injuries. Specific guidance is given for fractures of fingers, the wrist, radius, ulna, and elbow. All significantly displaced or angulated fractures should be referred to the acute hospital for further assessment and management.
Original Description:
Original Title
O
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document provides guidance on the assessment, treatment, and management of limb injuries like fractures and soft tissue injuries in adults and children over 2 years old. It outlines symptoms to assess for, specific history to obtain, examinations to perform, guidelines on radiography requests, descriptions of common fractures, and recommendations for management and follow-up of various upper limb injuries. Specific guidance is given for fractures of fingers, the wrist, radius, ulna, and elbow. All significantly displaced or angulated fractures should be referred to the acute hospital for further assessment and management.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
47 views17 pagesManagement of Limb Injuries in Adults and Children Over 2 Years
Management of Limb Injuries in Adults and Children Over 2 Years
Uploaded by
justforuroThis document provides guidance on the assessment, treatment, and management of limb injuries like fractures and soft tissue injuries in adults and children over 2 years old. It outlines symptoms to assess for, specific history to obtain, examinations to perform, guidelines on radiography requests, descriptions of common fractures, and recommendations for management and follow-up of various upper limb injuries. Specific guidance is given for fractures of fingers, the wrist, radius, ulna, and elbow. All significantly displaced or angulated fractures should be referred to the acute hospital for further assessment and management.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 17
Management of limb injuries in adults and children over 2 years
Last Review Date: March 2010
Version: 1 Page 1 of 17
Clinical Protocol
Title: Management of limb simple fractures and soft tissue Injuries in adults and
Children over 2 years
Document Author: Carol Gilmour Date March 2010
Ratified by: Care and clinical Policies
Group
Date: 17
th
March 2010
Review date: March 2012
Links to policies: TCT History taking and clinical documentation protocol, TCT
Consent Policy , TCT Child protection policy, TCT Safeguarding adults for abuse
policy, TCT Entonox PGD and TCT entonox protocol
1. Purpose of this document
1.1. To ensure registered nurses employed by Torbay Care Trust within MIU have clear
guidance on the assessment, treatment and management of limb simple fractures
and soft tissue injuries in adults and children over 2 years.
NOTE FOR CHILDREN AGED 2-5 YEARS CAUSING ANY CONCERN REFER TO A+E
FOR FURTHER ASSESSMENT
2. Presenting Symptoms
2.1. All or some of the following symptoms may be present in a patient presenting to the
MIU:
Pain, swelling, bruising/redness, wounds, inability/difficulty to weight bear,
reduced/loss of function and heat.
3. Specific recordings:
3.1 Additional history taking requirements include:
Record the mechanism
When, where and how the injury occurred and any resulting disability
Immediate /graduation of swelling
First aid treatment received including e.g. analgesics, ice, relocation of injury.
Record the pain score
Record any previous injury to the limb and relevant medical history, allergies ,tetanus
status and current medication ,especially warfarin or other anticoagulants and steroid
treatment. REFER ALL PATIENTS ON ANTICOAGULANT THERAPY TO A+E
Look for medical or non accidental causes of injury
Dominant hand
Management of limb injuries in adults and children over 2 years
Last Review Date: March 2010
Version: 1 Page 2 of 17
3. Clinical examination:
LOOK
Compare the limb on either side
Briefly examine the entire limb to exclude other injuries
Inspect limb for swelling, bruising or deformity or wounds
FEEL
Palpate for bony tenderness ( which usually indicates x-ray is required)
When palpating note crepitus
MOVE
Range of movement i.e. flexion and extension, abduction and adduction, supination
and pronation, internal and external rotation, thumb opposition, able to form tight
grip.
SPECIAL TESTS
Check for rotational deformity of fingers in finer/hand injuries
Always examine the neck in shoulder injuries and the pelvis in femur injuries
Examine for adequate skin perfusion, pulses, sensation and movement distal to the
injury
Check and record capillary refill
Examine for neurovascular compromise and transfer urgently to A+E if identified
For general approach to wounds see TCT wound management protocol
Management of limb injuries in adults and children over 2 years
Last Review Date: March 2010
Version: 1 Page 3 of 17
Radiography: Where nurses have undertaken specific training they can request x-
rays
Give a brief description of the trauma sustained and state where the suspected injury is
Request the correct views
With long bone shaft injuries always include views of the proximal and distal joints
Do not rely on poorly centred views of the suspected area, e.g. elbow in forearm views,
hip or knee in femur view
Always take views in at least two planes, at 90 where possible (not usually necessary
for the clavicle)
Where appropriately trained/experienced x-ray can be viewed and interpreted by MIU
nurse and/or advice sought from Torbay A+E medical practitioner .Clearly documenting
the name of clinician and advice given
Describing A Fracture
Closed or open
Name of the bone, left or right, and part of the bone fractured e.g. distal, midshaft,
proximal.
Type of fracture (transverse, oblique, spiral, compression, comminuted, impacted,
avulsion, greenstick)
Any intra-articular involvement
Describe any deformity in terms of displacement, tilt or rotation of the distal fragment
from the anatomical position, and state the direction of displacement (e.g. dorsal, volar,
radial, ulnar, lateral, medial, valgus, varus)
State the Grade or Classification of the fracture where common practice
Immediate Management of Any Limb Injury
Analgesia until pain score ideally below 4/10
Immobilise to minimise pain, blood loss and neurovascular damage
Elevate to minimise pain and swelling
Follow Up
Refer all fractures to the Fracture Clinic or orthopaedic team /A+E dependent on
presentation and finding as detailed below
Arrange follow-up of other injuries as appropriate by appropriate health care
professionals
GP or Practice Nurse
MIU
Physiotherapy
Management of limb injuries in adults and children over 2 years
Last Review Date: March 2010
Version: 1 Page 4 of 17
Management of Specific Fractures
Patients with specific upper limb fractures should be managed as below:
1
ST
MC
Significant angulation, dislocation and /or
fracture involving the joint
Refer to acute hospital
#not involving the joint Bennetts POP and check x-ray
Refer to #clinic
5
TH
MC
5th MC Neck-displaced/severely angulated,
any rotation ( lateral x-ray to measure)
Discuss x-ray with A+E team at SDHfT
Un- displaced or minor angulation DTG/crepe/neighbour strapping
Finger exercise
MIU follow up or #clinic
5
th
MC shaft-> 30 degrees angulation Discuss x-ray with A+E team at SDHfT
5
th
MC base Refer to orthopaedic team? plastics
involvement
Other MC
Displaced/multiple/angulated >30 Refer to A+E orthopaedic team? Plastics
input required
Base of MC Futura splint & refer to Plastics
Un-displaced or minor angulation
buddy strapping and refer to fracture clinic at
SDHfT
Finger exercise
Management of limb injuries in adults and children over 2 years
Last Review Date: March 2010
Version: 1 Page 5 of 17
All Phalanx # to Index, Middle, Ring, Little Digits
Check for rotation deformity and overlap
Angulated transverse fractures of the Proximal Phalanx may be very disabling,
if in doubt refer to A+E for medical practitioner assessment
Check base of little finger Proximal Phalanx carefully, may be difficult to see
angulation
Displaced/angulated,
comminuted (mulitfragmentary)
Refer to A+E orthopaedic team SDHfT
Un-displaced
Digit Phalanx -Buddy strapping
Thumb Phalanx Elastoplast thumb spica.
If laxity at 1st MCPJ - Refer to A+E
orthopaedic team at SDHfT
Finger exercise
MIU follow up
Mallet Finger
Always x-ray
Mallet splint and instructions. (Inform
patient splint
will be insitu for at least 6 weeks
Refer to SDHfT fracture clinic
Dislocations of Proximal and Distal Interpharangeal Joints
Check the history of injury fits with a dislocation
Check circulation of the digit, if in doubt refer to A+E for medical practitioner assessment
Check the nerves distal to the dislocation.
Uncomplicated dislocations
Buddy Strapping
Refer to A+E for medical practitioner
assessment
Signs of a fracture with dislocation
Refer to A+E orthopaedic team
Management of limb injuries in adults and children over 2 years
Last Review Date: March 2010
Version: 1 Page 6 of 17
Wrist
No bony injury Treat according to severity of pain or
swelling
Supportive bandage with or without sling
Un-displaced fracture P.O.P. backslab, sling,
Fracture clinic,
Instruction sheet regarding care of plaster
Displaced fracture Splint/sling, backslab.
Liaise with hospital re: transfer with
documentation
and
X-ray number documented clearly on notes,
nil by mouth
Scaphoid
Fracture may not show on first x-ray.
History may be of a fall onto outstretched hand or a starting handle type injury.
If the mechanism of injury or the clinical signs suggest a possible fracture of the
Scaphoid ALWAYS treat as for a fractured Scaphoid.
Clinical signs include:
Specific tenderness and/or swelling in the anatomical snuffbox
Specific tenderness over the Scaphoid tubercle
Pain on telescoping the thumb
Very poor grip
Reduced wrist movement
Management:
Scaphoid P.O.P for confirmed fracture, sling 24 hours
Confirmed fracture to Fracture clinic,
Instruction sheet regarding care of plaster
Suspected fracture rather than proven futura splint, sling for 24 hours - refer to GP
Management of limb injuries in adults and children over 2 years
Last Review Date: March 2010
Version: 1 Page 7 of 17
Radius and Ulna
No bony injury
.
Supportive bandage, with or without sling
Follow up at GPs surgery if necessary
Un-displaced fracture
Appropriate P.O.P ,sling
Fracture clinic appointment,
Instructions regarding care of plaster.
NB. An isolated mid-shaft fracture of one of forearm bones (except transverse mid
shaft Ulna) (Defence fracture) with other intact suggests Radio-ulnar joint
dislocation. It is essential that x-rays include the joints above and below the injury.
MONTEGGIA- Dislocation radial head with fracture ulna
GALEAZZI- Fracture radius with dislocation inferior radio-ulnar joint
Radial Head/Neck
Un-displaced
Collar & cuff
Fracture clinic
Severe/dislocated Refer to SDHfT Orthopaedics
NB effusion /inflammation in elbow joint suggest possible fracture and should be referred to
General Practitioner. If patient unwell or pyrexial consider infective arthritis or bursitis and
refer to A+E for further investigation.
Supracondylar
Displaced or dislocated
Check radial pulse if absent, gentle traction
may restore
Refer to SDHfT A+E
Un-displaced
Above Elbow backslab POP
Collar & cuff
Refer to Fracture clinic
Beware of compartment syndrome especially in children
Management of limb injuries in adults and children over 2 years
Last Review Date: March 2010
Version: 1 Page 8 of 17
Olecranon
Displaced
Refer to SDHfT A+E
Un-displaced
Long arm pop & sling
Next Fracture clinic
All Elbow Injuries are Treated in Collar
& Cuff not a Broad Arm Sling
Humerus
Shaft Un-displaced
Test radial nerve
Collar and cuff
Refer next Fracture clinic
Shaft displaced
Refer to Orthopaedic team via A+E
Neck Un-displaced
Collar and Cuff
Fracture clinic
Neck displaced
Comminuted
Refer to SDHfT Orthopaedic team via A+E
Clavicle
No bony injury
Broad arm sling if necessary, early
mobilisation
Fracture
Broad arm sling
Fracture clinic
Displaced
Check pulse/nerve function. If normal broad
arm sling
and Fracture clinic, if absent refer to SDHfT
orthopaedic team via A+E
hospital
Management of limb injuries in adults and children over 2 years
Last Review Date: March 2010
Version: 1 Page 9 of 17
Shoulder Injuries
No bony injury
Broad arm sling for a short time if necessary
Analgesia in accordance with analgesia
protocol
Refer to GP within 3 days consider self
referral to physiotherapy
Suspected acute soft tissue
injury
Broad arm sling
Refer to A+E
Fracture
Refer to A+E
Dislocation
Analgesia in accordance with entonox
protocol
Refer to A+E by ambulance
Dislocation/Subluxation AC Joint Broad arm sling
Refer Fracture clinic
Complete Disfruption AC Joint Broad arm sling
Refer Fracture clinic
Patient with specific Lower limb fractures should be managed as below:
Fracture Neck of Femur
Requires Orthopaedic admission
Analgesia & transfer to acute hospital via
999
Cannulate if nurse has cannulation
skills and Sodium Chloride 0.9%
injection as per PGD.
Obtain ECG, if time permits
Management of limb injuries in adults and children over 2 years
Last Review Date: March 2010
Version: 1 Page 10 of 17
Fracture Shaft of Femur
Requires Orthopaedic admission
Analgesia & transfer to acute hospital via
999
Cannulate if nurse has cannulation
skills and Sodium Chloride 0.9%
injection as per PGD.
Donway splint (Supplied by
Ambulance)
Significant Avulsion Fracture Tibial Spine
Requires Orthopaedic Admission
Refer to hospital
Analgesia in accordance with
analgesia protocol
Long Leg Backslab POP
Osteochondral Fractures
Requires Orthopaedic Admission if
severe
Discus with A+E
Analgesia in accordance with
analgesia protocol
Long Leg Backslab POP
Fracture of Tibial Plateau
Discuss with orthopaedic team at SDHfT for
advice
Analgesia in accordance with
analgesia protocol
Long Leg Backslab POP
Refer to fracture clinic
Management of limb injuries in adults and children over 2 years
Last Review Date: March 2010
Version: 1 Page 11 of 17
Isolated Fracture Upper Midshaft Fibula
Examine lateral popliteal nerve
Discuss with orthopaedic team at SDHfT
Analgesia in accordance with
analgesia protocol
Treat with tubigrip or POP if severe
pain if POP assess for
Thromboprophlaxis.
Refer to Fracture Clinic
Fractured Tibia and Fibula
Undisplaced
Long Leg POP
Adults Assess for
Thromboprophlaxis and refer to
Orthopaedics for advice
Children non-weight bearing on
crutches. Refer to fracture clinic
Displaced
Immobilise in backslab assess for
Thromboprophylaxis
Analgesia in accordance with
analgesia protocol
Refer to A+E Orthopaedics
Fractures with sever soft tissue injury
Orthopaedic referral via A+E
Epiphyseal Fracture Lower Tibia
Undisplaced
Discuss with orthopaedic team at SDHfT
Displaced
Refer to Orthopaedic team SDHfTvia A+E
Toddlers Fracture
A toddler who falls and who will not
weight bear must have the whole limb x-
rayed
unless clinical examination can
localise an injured area. Spiral fractures
of the tibia may not be visible on initial x-
rays.
Refer to SDHfT for assessment and
management
Management of limb injuries in adults and children over 2 years
Last Review Date: March 2010
Version: 1 Page 12 of 17
This clinical guideline provides guidance to MIU nurses .If any potential
bony injury attending the MIU is outside your scope of practice arrange
transfer of the patient to A+E for further assessment and investigations
The need to X-ray a knee injury should be assessed using the Ottawa knee rules as
below and the patient referred to A+E
Knee X-ray in acute injury are required only for patients with any of the following :
1. Age 55 years or older
2. Isolated tenderness of the patella (no bone tenderness of the knee other than the
patella)
3. Tenderness at the head of the fibula
4. Inability to flex the knee to 90 degrees
5. Inability to bear weight (four steps) both immediately and in the department (unable
to transfer weight twice onto each lower limb regardless of limping)
The need to X-ray an ankle injury should be assessed using the 'Ottawa ankle rules'
see below:
Ankle X-ray is required only if there is pain in the malleolar region and any of the
following:-
1. Tenderness upon palpation of distal 6cms of posterior edge and tip of lateral and/or
medial malleolus.
2. Inability to weight bear both immediately after injury and/or in the department
(4 steps)
3. Age over 55
Foot X-ray is required only if there is any pain in the midfoot area and any of the
following: -
1. Tenderness upon palpation at the base of 5th MT and/or medial aspect of navicular.
2. Inabilities to weight bear, both immediately after injury and in the department
(4 steps)
3. Age over 55
Management of limb injuries in adults and children over 2 years
Last Review Date: March 2010
Version: 1 Page 13 of 17
Knee Injuries
Suspected Cruciate or Meniscus injury:
Knee gives way or locks
Any instability on movements
Unable to walk or weight bear
Pop felt or heard clicking
Pain on rotational movements
Refer to A+E
Haemarthrosis/large effusion
Refer to A+E
Dislocate patella
Check pedal pulses and circulation refer to
A+E
Definite minor sprain without instability or
effusion
Double tubigrip
Crutches if applicable
Analgesia in accordance with protocol
Give advice about exercising joint
Follow up with GP within one week
Suggest self referral to physiotherapy
Diagnosis uncertain
Refer to A+E
Ankle Injuries
No bony injury
Double tubigrip or Crepe if required.
Advice RICE.
Follow up GP/Physio if required (unable to
weight bear
without crutches)
Un-displaced fracture
Below knee P.O.P,
Crutches (none weight bearing)
Fracture clinic
Advice Re: aftercare of P. O. P
Displaced fracture
Refer to Orthopaedic team via A+E
A Severely Displaced Fracture that Poses a Risk of Neurovascular Deficit or Skin
Damage Should Be transferred urgently via 999 ambulance
Management of limb injuries in adults and children over 2 years
Last Review Date: March 2010
Version: 1 Page 14 of 17
Achilles Tendon (Ruptured)
Very sudden pain in lower calf may occur
spontaneously,
and/or History of injury with sudden pain in
lower calf.
Refer these
patients to
Orthopaedic team via A+E
May be missed because of pain and swelling
at the time of
injury and foot can be plantar flexed by the
long toe flexors
Refer these
patients to
Orthopaedic team via A+E
Signs of rupture include
Palpable gap in Tendon or
Inability to stand on tiptoe on the affected
foot or
Positive squeeze Test (Simmonds Test)
Refer these
patients to
Orthopaedic team via A+E
Bilateral fractures Requires Orthopaedic admission refer to hospital
Calcaneum
# Calcaneum
Wool & crepe
Crutches
Advice/elevation
Discuss with A+E orthopaedic team at
SDHfT (May also require
admission for elevation)
Fracture clinic
If involves subtalar
joint/depressed fracture
Requires Orthopaedic admission-refer via
A+E
Fracture Base 5
th
Metatarsal
Symptomatic treatment, usually crepe/DTG
but if severe pain Below Knee POP &
crutches
Refer fracture clinic
Management of limb injuries in adults and children over 2 years
Last Review Date: March 2010
Version: 1 Page 15 of 17
Other Fractured Metatarsals
Displaced/multiple
Refer via A+E to orthopaedic team
Un-displaced
Symptomatic treatment as above
Discuss with fracture clinic or A+E
Fracture Talus/Subtalar/Midtarsal Refer A+E
All Phalanges # to Great, 2
nd
, 3
rd
, 4
th
and 5
th
Toes
No bony injury
Two toe strapping if required Advise
supportive
sensible footwear
Un-displaced fracture
Two toe strapping
Advise supportive sensible footwear
Refer GP
Displaced fracture
Liaise with A+E orthopaedic team
Dislocations to Proximal or Distal Interpharagel Joints-Toes
Check the history of injury fits with a dislocation
Check circulation of the digit, if in doubt refer to a doctor for assessment
Check the nerves distal to the dislocation.
Uncomplicated dislocations
X-ray to confirm diagnosis
Buddy Strapping
Check X-ray
Refer to A+E
Signs of a fracture with dislocation
Refer to A+E
Management of limb injuries in adults and children over 2 years
Last Review Date: March 2010
Version: 1 Page 16 of 17
3. References:
Adapted from Plymouth teaching Primary Care Trust Minor Injury Unit Handbook of
clinical Protocols (V2:1)
Amendment History
Issue Status Date Reason for Change Authorised
Management of limb injuries in adults and children over 2 years
Last Review Date: March 2010
Version: 1 Page 17 of 17
CLINICAL PROTOCOL FOR THE MANAGEMENT OF SOFT TISSUE AND BONY
INJURIES ATTENDING MIU
The registered health professionals named below, being employees of Torbay Care
Trust and based at . Have received training and are
competent to operate under this clinical guideline
NAME
( Please print)
PROFESSIONAL
TITLE
SIGNATURE AUTHORISING
MANAGER
( Please print)
DATE
You might also like
- Verstegen 04 Movement Prep CH 5Document22 pagesVerstegen 04 Movement Prep CH 5trtraining100% (2)
- Iontophoresis GOLFERS ELBOW (Medial Epicondylitis)Document2 pagesIontophoresis GOLFERS ELBOW (Medial Epicondylitis)Ikre19100% (1)
- SOG 101 - FreeWorkout - EbookSnippetDocument4 pagesSOG 101 - FreeWorkout - EbookSnippetChris VisNo ratings yet
- Shinden Fudo Ryu: JutaijutsuDocument14 pagesShinden Fudo Ryu: Jutaijutsutopolevich100% (2)
- Bovine Anatomy An Illustrated Text 2nd EditionDocument185 pagesBovine Anatomy An Illustrated Text 2nd Editionluis feo100% (4)
- Sample Test Questions V 3Document43 pagesSample Test Questions V 3Jignasha VadiNo ratings yet
- General Examination..Document6 pagesGeneral Examination..zaid100% (2)
- Tools For Diagnosis of Knee InjuriesDocument10 pagesTools For Diagnosis of Knee Injuriesmanjukumard2007No ratings yet
- Common Orthopedic Emergency Conditions and Their ManagementDocument6 pagesCommon Orthopedic Emergency Conditions and Their ManagementDhruva PatelNo ratings yet
- Case Study - Galeazzi FractureDocument14 pagesCase Study - Galeazzi FractureRio Cornell Golo50% (2)
- Open Fracture Raju3Document72 pagesOpen Fracture Raju3Chowdhury Iqbal MahmudNo ratings yet
- Fracture Nursing Care Management: Study GuideDocument5 pagesFracture Nursing Care Management: Study Guidezahwa ayundaNo ratings yet
- Case Report Juli 2013Document21 pagesCase Report Juli 2013NahdiaNo ratings yet
- Trauma - Intertrochanteric Fracture - RustiniDocument7 pagesTrauma - Intertrochanteric Fracture - Rustinidedyalkarni08No ratings yet
- FRACTURES AND ITS MANAGEMENT - by Prof M Ayoub Laghari 24-4-2013Document40 pagesFRACTURES AND ITS MANAGEMENT - by Prof M Ayoub Laghari 24-4-2013SeyfNo ratings yet
- Open Reduction Internal FixationDocument7 pagesOpen Reduction Internal FixationalcojonicNo ratings yet
- Bagian Ilmu Bedah Laporan KasusDocument20 pagesBagian Ilmu Bedah Laporan KasusrendyNo ratings yet
- Fracture PresentationDocument53 pagesFracture Presentationrahul yadav100% (8)
- Nursing Service Training Section Clinical Case AnalysisDocument5 pagesNursing Service Training Section Clinical Case AnalysisBernadeth LabradorNo ratings yet
- Trauma Case Reports: Jugert Bango, Evan Zhang, Daniel L. Aaron, Amna DiwanDocument4 pagesTrauma Case Reports: Jugert Bango, Evan Zhang, Daniel L. Aaron, Amna DiwanCristhian Jover CastroNo ratings yet
- Tuberculosis of The HipDocument33 pagesTuberculosis of The Hipmuhammad bayu wicaksonoNo ratings yet
- Dis HandDocument11 pagesDis HandSteven OwensNo ratings yet
- AAOS Foot Ankle 2018abDocument54 pagesAAOS Foot Ankle 2018abFasa Roshada100% (3)
- Bone Healing ModuleDocument7 pagesBone Healing ModuleIceKing233No ratings yet
- 1 Ulnar Radial FX CWU Deirdre%27sDocument7 pages1 Ulnar Radial FX CWU Deirdre%27sAyeshaNo ratings yet
- The Problem Knee 3rd Ed. Hodder ArnoldDocument253 pagesThe Problem Knee 3rd Ed. Hodder Arnoldvasili11175% (4)
- Atraumatic Cuff TearsDocument7 pagesAtraumatic Cuff Tearschandan noelNo ratings yet
- Bennett FractureDocument5 pagesBennett FractureeviherdiantiNo ratings yet
- Justin Ubay BSN212 Group 48A FracturesDocument5 pagesJustin Ubay BSN212 Group 48A FracturesubaycentralNo ratings yet
- Surgical Treatment of Chronic Elbow Dislocation Allowing For Early Range of Motion: Operative Technique and Clinical ResultsDocument8 pagesSurgical Treatment of Chronic Elbow Dislocation Allowing For Early Range of Motion: Operative Technique and Clinical ResultsLuis Carlos HernandezNo ratings yet
- Tibia Fractures Overview - StatPearls - NCBI BookshelfDocument6 pagesTibia Fractures Overview - StatPearls - NCBI BookshelfVivi DeviyanaNo ratings yet
- Orthopaedic Surgery Study Guide FOR Medical Students, R1S and R2SDocument17 pagesOrthopaedic Surgery Study Guide FOR Medical Students, R1S and R2SlanghalilafaNo ratings yet
- Fractures: Mary Grace B. Gutierrez Resti Mariano Ma. Cindy O. BautistaDocument50 pagesFractures: Mary Grace B. Gutierrez Resti Mariano Ma. Cindy O. BautistaJustin Ahorro-DionisioNo ratings yet
- Case Report (Ola)Document44 pagesCase Report (Ola)amel015No ratings yet
- Neglected Bilateral Triphalangeal of The Thumb 2024 International Journal ofDocument4 pagesNeglected Bilateral Triphalangeal of The Thumb 2024 International Journal ofRonald QuezadaNo ratings yet
- Extensor Tendon Injuries 2010 The Journal of Hand SurgeryDocument8 pagesExtensor Tendon Injuries 2010 The Journal of Hand SurgeryProfesseur Christian DumontierNo ratings yet
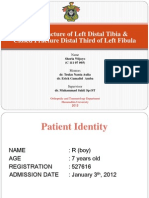
- "Emergency Orthopedics": Suci Purnamaza M. AimanDocument38 pages"Emergency Orthopedics": Suci Purnamaza M. AimanWhite WheelNo ratings yet
- Orthopaedic PocketDocument22 pagesOrthopaedic PocketAbdullah AzmyNo ratings yet
- Semiconstrained Total Elbow Arthroplasty-1Document6 pagesSemiconstrained Total Elbow Arthroplasty-1Ευαγγελια ΚιμπαρηNo ratings yet
- Surgical Treatment of Neglected Malunion of Shaft Femur: Case ReportDocument13 pagesSurgical Treatment of Neglected Malunion of Shaft Femur: Case ReportNando OktariNo ratings yet
- Classification of FracturesDocument26 pagesClassification of FracturesHoney May Rollan VicenteNo ratings yet
- Principles of Treatment of FracturesDocument27 pagesPrinciples of Treatment of FracturesBanna Kiran KumarNo ratings yet
- FracturesDocument26 pagesFracturesMelinda MelinNo ratings yet
- Menckhoff - Orthopedic Pearls and Pitfalls Handout 3-25-13Document34 pagesMenckhoff - Orthopedic Pearls and Pitfalls Handout 3-25-13Sasi KumarNo ratings yet
- Functional Outcome After The Conservative Management of A Fracture of The Distal HumerusDocument7 pagesFunctional Outcome After The Conservative Management of A Fracture of The Distal HumerusnireguiNo ratings yet
- Hip and Pelvic Injections PDFDocument12 pagesHip and Pelvic Injections PDFVijay Kumar100% (1)
- Temporomandibular Joint Disorder ThesisDocument5 pagesTemporomandibular Joint Disorder Thesisheatherdionnemanchester100% (2)
- Thetrigeminalnerve Injury: Arshad Kaleem,, Paul Amailuk,, Hisham Hatoum,, Ramzey TursunDocument13 pagesThetrigeminalnerve Injury: Arshad Kaleem,, Paul Amailuk,, Hisham Hatoum,, Ramzey TursunPriyanka SinhaNo ratings yet
- Complications and Outcomes of The Transfibular Approach For Posterolateral Fractures of The Tibial Plateau PDFDocument19 pagesComplications and Outcomes of The Transfibular Approach For Posterolateral Fractures of The Tibial Plateau PDFSergio Tomas Cortés MoralesNo ratings yet
- Intertan Nail Vs PFN ADocument7 pagesIntertan Nail Vs PFN AzubayetarkoNo ratings yet
- 9 Suppl - 1 S58Document7 pages9 Suppl - 1 S58ChristopherLawrenceNo ratings yet
- Management of Patellofemoral Chondral InjuriesDocument24 pagesManagement of Patellofemoral Chondral InjuriesBenalNo ratings yet
- Fractures of The Distal Radius Wrist FracturesDocument10 pagesFractures of The Distal Radius Wrist Fracturescharlyn206No ratings yet
- Tennis Elbow - StatPearls - NCBI BookshelfDocument9 pagesTennis Elbow - StatPearls - NCBI BookshelfADITYA ARI HERLAMBANGNo ratings yet
- (POLI TRAUMA) Decision Making in Trauma SurgeryDocument15 pages(POLI TRAUMA) Decision Making in Trauma SurgeryEdward Ojeda100% (1)
- PIP Joint InjuryDocument4 pagesPIP Joint InjurySAYEM AHAMMEDNo ratings yet
- Ankle FractureDocument7 pagesAnkle FractureAbdallah AqrooqNo ratings yet
- Amputation AssignmentDocument19 pagesAmputation Assignmentmushimiyimana jacquelineNo ratings yet
- Cas RepotDocument8 pagesCas RepotKrishna CaitanyaNo ratings yet
- Fractures: A. Pusey-Murray (MRS) RN, Cert Psych Nursing & Nursing Admin, BSC (Hons), MPH, Dip. Ed. PHD (C)Document68 pagesFractures: A. Pusey-Murray (MRS) RN, Cert Psych Nursing & Nursing Admin, BSC (Hons), MPH, Dip. Ed. PHD (C)okacia100% (1)
- Is Extracorporeal Shockwave Therapy Effective Even in The Treatment of Partial Rotator Cuff TearDocument6 pagesIs Extracorporeal Shockwave Therapy Effective Even in The Treatment of Partial Rotator Cuff TearmitchelNo ratings yet
- A Fracture Is A BreakDocument7 pagesA Fracture Is A BreakStepyn SalvadorNo ratings yet
- Current Concepts in Open-Wedge High Tibial Osteotomy: Review ArticleDocument11 pagesCurrent Concepts in Open-Wedge High Tibial Osteotomy: Review ArticleAhmed SalmanNo ratings yet
- Ntroduction: (1) (2) (3) Go ToDocument8 pagesNtroduction: (1) (2) (3) Go ToCoass Pediatri FKUHONo ratings yet
- Clavicle FractureDocument6 pagesClavicle FractureYbis LizarzaburuNo ratings yet
- Orthopedic Trauma Office Management of MDocument28 pagesOrthopedic Trauma Office Management of MVladislav KotovNo ratings yet
- Disorders of the Patellofemoral Joint: Diagnosis and ManagementFrom EverandDisorders of the Patellofemoral Joint: Diagnosis and ManagementNo ratings yet
- Presentation Title: My Name Contact Information or Project DescriptionDocument2 pagesPresentation Title: My Name Contact Information or Project DescriptionjustforuroNo ratings yet
- Presentation Title: My Name My Position, Contact Information or Project DescriptionDocument2 pagesPresentation Title: My Name My Position, Contact Information or Project DescriptionjustforuroNo ratings yet
- Bisa 1Document8 pagesBisa 1justforuroNo ratings yet
- Comparison of Radical Cystectomy With Conservative Treatment in Geriatric ( 80) Patients With Muscle-Invasive Bladder CancerDocument9 pagesComparison of Radical Cystectomy With Conservative Treatment in Geriatric ( 80) Patients With Muscle-Invasive Bladder CancerjustforuroNo ratings yet
- BDocument86 pagesBjustforuroNo ratings yet
- Natalie Jill Home Workout Book V1.2Document46 pagesNatalie Jill Home Workout Book V1.2Holly Sheríf-Alsammani100% (1)
- Spanimax Full-Body Dumbbell WorkoutDocument12 pagesSpanimax Full-Body Dumbbell Workoutmihaib2007100% (1)
- Self Massage TechniquesDocument24 pagesSelf Massage TechniquesI.S.100% (4)
- Plantar Fasciitis and The Windlass MechanismDocument6 pagesPlantar Fasciitis and The Windlass MechanismEric Urbina SantibañezNo ratings yet
- Traction in ORTHOPAEDICSDocument16 pagesTraction in ORTHOPAEDICSJuswa ViasonNo ratings yet
- Splinting Guide For Ems/Hospital Providers: Introduction (Louis Spina M.D., 9/2016)Document10 pagesSplinting Guide For Ems/Hospital Providers: Introduction (Louis Spina M.D., 9/2016)cscott805No ratings yet
- TBWDocument45 pagesTBWveedee cikalNo ratings yet
- Ergo ExerciseDocument1 pageErgo ExercisecrestdavidNo ratings yet
- Yoga For Runners - Runner's WorldDocument12 pagesYoga For Runners - Runner's WorldNitish_Katal_9874No ratings yet
- 36 Knee Conditions: EMQ Answers 87Document10 pages36 Knee Conditions: EMQ Answers 87Eunice LimNo ratings yet
- 12 Trigger Finger ExerciseDocument6 pages12 Trigger Finger ExerciseAr AryaNo ratings yet
- Module 3-Anatomy and Physiology (Abegail Relunia - Bsed3-C Science) )Document3 pagesModule 3-Anatomy and Physiology (Abegail Relunia - Bsed3-C Science) )Abegail ReluniaNo ratings yet
- Clavicle Orif Rehabilitation ProtocolDocument1 pageClavicle Orif Rehabilitation ProtocolAndreas Arie WidiadiaksaNo ratings yet
- Trigger Points Release Through Scalp AcupunctureDocument112 pagesTrigger Points Release Through Scalp AcupunctureTri Dewi Larasati80% (5)
- Hip Knee Ankle Foot OrthosisDocument44 pagesHip Knee Ankle Foot OrthosisGulzar Ahmad100% (1)
- Modification of QF ExerciseDocument7 pagesModification of QF ExerciseTomBramboNo ratings yet
- Intramedullary Nail Fixation of Tibial Shaft FracturesDocument2 pagesIntramedullary Nail Fixation of Tibial Shaft FracturesNanda PerdanaNo ratings yet
- Specific Sports Related InjuriesDocument528 pagesSpecific Sports Related Injuriesorthofitness2017No ratings yet
- Arthroscopic Ramp Repair No-Implant, Pass, Park, and Tie Technique Using Knee Scorpion, GustaDocument8 pagesArthroscopic Ramp Repair No-Implant, Pass, Park, and Tie Technique Using Knee Scorpion, GustaAlhoi lesley davidsonNo ratings yet
- Foot Ability ProgramDocument4 pagesFoot Ability ProgramZakary KharouneNo ratings yet
- Erb'S Palsy: Definition/DescriptionDocument10 pagesErb'S Palsy: Definition/DescriptionGuhan SubramaniamNo ratings yet
- Anterior Knee Pain ExercisesDocument6 pagesAnterior Knee Pain ExercisesJobin VargheseNo ratings yet
- Handout 1 - Body RegionsDocument3 pagesHandout 1 - Body RegionsminionofcthulhuNo ratings yet