Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
1K viewsNo Balance Billing Policy
No Balance Billing Policy
Uploaded by
Rhyne Amante YpulongPhilHealth has established new case rates for selected medical cases and surgical procedures to improve member benefits and attain universal health coverage. The case rates will serve as standardized reimbursement amounts for medical interventions and include professional fees. A No Balance Billing policy has also been adopted to protect members from additional fees for cases covered under government facilities or outpatient packages. The policy aims to provide optimal financial risk protection and support efforts to reduce maternal and infant mortality rates.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- 2023 LGU HSC Indicators - Feb. 19Document76 pages2023 LGU HSC Indicators - Feb. 19Diane Joy EsquivelNo ratings yet
- Retirement ScriptDocument14 pagesRetirement ScriptBrian LindseyNo ratings yet
- Proposal For Retainer Agreement - SampleDocument2 pagesProposal For Retainer Agreement - SampleRhyne Amante Ypulong100% (2)
- BS 4254Document19 pagesBS 4254gugaruban100% (4)
- IEC 60950 Rev1Document3 pagesIEC 60950 Rev1Rip_BarNo ratings yet
- 4100XPB 4198 Grupo Mexico CananDocument758 pages4100XPB 4198 Grupo Mexico CananWalissonNo ratings yet
- The Constitution of Youth AssociationDocument9 pagesThe Constitution of Youth AssociationMeshack Lee Izu0% (1)
- Comparative Analysis-5 ILHZDocument59 pagesComparative Analysis-5 ILHZRegalado Aguhayon100% (3)
- Drug Consignment Agreement SampleDocument3 pagesDrug Consignment Agreement SampleremaxiloiloNo ratings yet
- Republic Act No. 9184Document67 pagesRepublic Act No. 9184Cire EtneilavNo ratings yet
- Commission On Audit: Republic of The PhilippinesDocument1 pageCommission On Audit: Republic of The Philippinesrocky CadizNo ratings yet
- 07-NEHEHRSV - How To Register UpdatedDocument49 pages07-NEHEHRSV - How To Register UpdatedClinton Lorbes100% (1)
- Civil Service Code of The Philippines - Senate Bill 1162Document45 pagesCivil Service Code of The Philippines - Senate Bill 1162tandangmark76% (17)
- Change of OwnershipDocument11 pagesChange of OwnershipGlenn JamesNo ratings yet
- Negros Occidental Consignment SystemDocument42 pagesNegros Occidental Consignment SystemThrees See100% (3)
- Proposed Billing System of STCDocument5 pagesProposed Billing System of STCjHUN aGANo ratings yet
- AO 2016-0032 QS of Medical PositionsDocument12 pagesAO 2016-0032 QS of Medical PositionsTotoDodongGus100% (10)
- Billing FormatDocument1 pageBilling FormatParag KhandelwalNo ratings yet
- Updated Research Assistant Confidentiality AgreementDocument2 pagesUpdated Research Assistant Confidentiality AgreementIlya ChNo ratings yet
- Billing System of Bacnotan District HospitalDocument29 pagesBilling System of Bacnotan District HospitalBlessie MercadoNo ratings yet
- Performance CommitmentDocument5 pagesPerformance CommitmentEmman Acosta DomingcilNo ratings yet
- Final LGU Scorecard Indicators 2012-2016 As of April 19Document22 pagesFinal LGU Scorecard Indicators 2012-2016 As of April 19Arianne A Zamora100% (19)
- DBM BudgetDocument85 pagesDBM BudgetGab Pogi100% (1)
- Sexual Assault in The Military 2018 DoD ReportDocument26 pagesSexual Assault in The Military 2018 DoD ReportAlanna JeanNo ratings yet
- Resolution TimbuktuDocument4 pagesResolution TimbuktuSummerRainNo ratings yet
- 2022 DOH Budget BrieferDocument34 pages2022 DOH Budget BrieferArabella CatindoyNo ratings yet
- UB-04 Billing Instructions Revision Table: Revision Date Sections Revised DescriptionDocument24 pagesUB-04 Billing Instructions Revision Table: Revision Date Sections Revised DescriptioncmabryNo ratings yet
- Afpces FinanceDocument5 pagesAfpces FinanceKathy Mercado100% (1)
- Tired of All The Guides and Never-Ending Instructions?: Try A Quicker WayDocument3 pagesTired of All The Guides and Never-Ending Instructions?: Try A Quicker WayJeremarkNo ratings yet
- Mandatory ROTCDocument2 pagesMandatory ROTCPrecious Ab0% (1)
- Pak Takaful Claim FormDocument2 pagesPak Takaful Claim FormRoger Eli Paul100% (1)
- Retirement Options Sample ComputationDocument11 pagesRetirement Options Sample Computationluna acosta0% (1)
- Wanted For The NTH Time: The Return of RotcDocument2 pagesWanted For The NTH Time: The Return of RotcAdor IsipNo ratings yet
- Doh Ihmop Filled UpDocument12 pagesDoh Ihmop Filled UpRex Quilla100% (1)
- Circ2020-0022 - Impleme Nting Guidelines For The PhiiHealth Konsultasyong Sulit at Tama PhiiHealth Konsulta PackageDocument8 pagesCirc2020-0022 - Impleme Nting Guidelines For The PhiiHealth Konsultasyong Sulit at Tama PhiiHealth Konsulta PackageJL CalvinNo ratings yet
- Entitlement To Hazard PayDocument16 pagesEntitlement To Hazard PayJanette SumagaysayNo ratings yet
- Sample Retirement LetterDocument1 pageSample Retirement LetterGilbert Javier100% (1)
- Medical Consent FormDocument2 pagesMedical Consent Formapi-235272235100% (1)
- Billing Guidance For Pharmacists Professional and Patient Care Services White PaperDocument9 pagesBilling Guidance For Pharmacists Professional and Patient Care Services White Paperkrishna krNo ratings yet
- 3 - 2022 MOA - iClinicSys - TemplateDocument4 pages3 - 2022 MOA - iClinicSys - TemplateGladdy CabrezaNo ratings yet
- Bir Cda Joint Rules and RegulationsDocument12 pagesBir Cda Joint Rules and RegulationsCha Ancheta CabigasNo ratings yet
- Iclte Press Release 2018 BLGFDocument2 pagesIclte Press Release 2018 BLGFElla LagorraNo ratings yet
- 2020 NEQAS CC Registration Form and Order of PaymentDocument2 pages2020 NEQAS CC Registration Form and Order of PaymentNovie FeneciosNo ratings yet
- Pro Health Billing Setup GuideDocument22 pagesPro Health Billing Setup Guideapi-248512169100% (1)
- Introduction To Health FinancingDocument101 pagesIntroduction To Health FinancingArianne A ZamoraNo ratings yet
- Project Report - Outdoor Patient Doctor's Booking SystemDocument51 pagesProject Report - Outdoor Patient Doctor's Booking SystemSoumya Kanti Ghosh100% (1)
- Office Order No. 2011-20Document25 pagesOffice Order No. 2011-20ciryajamNo ratings yet
- Guidelines On Hiring and Re-Hiring of Job Order Personnel in The DPWH (D.O. 2013)Document4 pagesGuidelines On Hiring and Re-Hiring of Job Order Personnel in The DPWH (D.O. 2013)Diana Lyn Bello CastilloNo ratings yet
- East Delta University: MBA Program: Summer 2021Document25 pagesEast Delta University: MBA Program: Summer 2021Mohammed Imtiaz Shayek67% (3)
- Migrant Workers Act RA 10022 and 9422 Amending 8042Document49 pagesMigrant Workers Act RA 10022 and 9422 Amending 8042adrianmdelacruzNo ratings yet
- CP LTC Ley GB CGSC Cl68Document151 pagesCP LTC Ley GB CGSC Cl68Jun LlaveNo ratings yet
- Civil Service HandbookDocument169 pagesCivil Service HandbookIkechukwu Igboebisi100% (1)
- Reaction PaperDocument3 pagesReaction PaperCamilla Reyes100% (1)
- BclteDocument2 pagesBcltereiman0590No ratings yet
- Billing ArrangementDocument6 pagesBilling ArrangementJalynLopezNostratis0% (1)
- Parental Consent and Waiver FormDocument1 pageParental Consent and Waiver FormErEr Uno Rosil100% (1)
- RetirementDocument4 pagesRetirementRayvantaKumarNo ratings yet
- Military Based Resume Example: ObjectiveDocument6 pagesMilitary Based Resume Example: ObjectiveAman KalraNo ratings yet
- Government of Andhra Pradesh C.T.Department: Form of Way Bill Form X or Form 600Document3 pagesGovernment of Andhra Pradesh C.T.Department: Form of Way Bill Form X or Form 600Arjun B Menon100% (1)
- (UIS TOF) UHC and PhilHealth Slide Deck PDFDocument82 pages(UIS TOF) UHC and PhilHealth Slide Deck PDFlilacNo ratings yet
- Consultation Form: (To Be Accomplished If The Issue(s) or Concern(s) Was/were Not Solved at The Faculty-Student Level.)Document1 pageConsultation Form: (To Be Accomplished If The Issue(s) or Concern(s) Was/were Not Solved at The Faculty-Student Level.)MyMy MargalloNo ratings yet
- Philhealth Agency's Mandate and FunctionsDocument10 pagesPhilhealth Agency's Mandate and FunctionsjonaNo ratings yet
- All Case RateDocument91 pagesAll Case RateTimothy Dycalle ManosNo ratings yet
- ao2016-0033-PHIC Pooling DistDocument5 pagesao2016-0033-PHIC Pooling DistAccount AlugrivNo ratings yet
- Employment Contract - SAMPLEDocument7 pagesEmployment Contract - SAMPLERhyne Amante YpulongNo ratings yet
- Demand Letter To UELDocument1 pageDemand Letter To UELRhyne Amante Ypulong100% (1)
- Proposal To For TIEZADocument4 pagesProposal To For TIEZARhyne Amante YpulongNo ratings yet
- Letter To Mrs. CastilloDocument1 pageLetter To Mrs. CastilloRhyne Amante YpulongNo ratings yet
- Demand - Second NoticeDocument2 pagesDemand - Second NoticeRhyne Amante YpulongNo ratings yet
- Law On Sales, Agency and Bailments-OverviewDocument6 pagesLaw On Sales, Agency and Bailments-OverviewRhyne Amante Ypulong0% (2)
- Accounting of Proceeds of Sale of Portion of The Estate of Ricardo Domingo and ExpensesDocument3 pagesAccounting of Proceeds of Sale of Portion of The Estate of Ricardo Domingo and ExpensesRhyne Amante YpulongNo ratings yet
- Sapoe Cofee Vending Machine-Joel Chua QuoteDocument3 pagesSapoe Cofee Vending Machine-Joel Chua QuoteRhyne Amante YpulongNo ratings yet
- Frenkel's ExerciseDocument40 pagesFrenkel's ExerciseManiu EmeseNo ratings yet
- Altitude, Cloud Cover and LatitudeDocument64 pagesAltitude, Cloud Cover and LatitudeIsarra AmsaluNo ratings yet
- Iec Inverse Protection CurvesDocument1 pageIec Inverse Protection CurvesEng-Ahmad Abo-AledousNo ratings yet
- Capinew Account June13Document7 pagesCapinew Account June13ashwinNo ratings yet
- On Light: Science Holiday Homework Made By-Aish Mishra Class-8 Diamond Roll No.-6Document9 pagesOn Light: Science Holiday Homework Made By-Aish Mishra Class-8 Diamond Roll No.-6Ansh MishraNo ratings yet
- Whirlpool BIWDWG861484uk enDocument4 pagesWhirlpool BIWDWG861484uk ennadaljoachim77No ratings yet
- Compact Evaporators: New Buffalo Trident GaccDocument16 pagesCompact Evaporators: New Buffalo Trident GaccPreeti gulatiNo ratings yet
- PHAS0027 RevisionDocument21 pagesPHAS0027 Revisionunknown.unknown9901No ratings yet
- Seed Extraction MethodsDocument3 pagesSeed Extraction MethodsPreetam NayakNo ratings yet
- DR Physique Lean Bulking Series II 2015Document121 pagesDR Physique Lean Bulking Series II 2015Vlad Alexandru50% (2)
- Soil Acidity and LimingDocument12 pagesSoil Acidity and LimingEloi Carlos GoveNo ratings yet
- Corn Growth StagesDocument33 pagesCorn Growth StagesIvan JovanovićNo ratings yet
- Inorganic Chemistry HomeworkDocument3 pagesInorganic Chemistry HomeworkAlpNo ratings yet
- GRES Integrated Energy Storage SystemDocument33 pagesGRES Integrated Energy Storage SystemVadim PopovichNo ratings yet
- 1 Case IDC PDFDocument7 pages1 Case IDC PDFPilar Dueñas Maldonado0% (1)
- Case Study On A Highway Project: Environmental Impact AssesmentDocument10 pagesCase Study On A Highway Project: Environmental Impact AssesmentSRUTHI FRANCIS M.Tech Environmental Engineering 2020-2022No ratings yet
- Emotional IntelligenceDocument43 pagesEmotional IntelligenceMelody ShekharNo ratings yet
- Case Study Booklet 2 PDFDocument43 pagesCase Study Booklet 2 PDFguddu yadavNo ratings yet
- The Development of A Heat Wave Vulnerability Index For London-2013Document10 pagesThe Development of A Heat Wave Vulnerability Index For London-2013gilberto777No ratings yet
- Safe Practices For Welding InspectorsDocument39 pagesSafe Practices For Welding InspectorsAlejandro RodríguezNo ratings yet
- NeuroVascular (NV) Holding PointsDocument2 pagesNeuroVascular (NV) Holding PointsHatem Farouk100% (2)
- Beyond FurosemideDocument13 pagesBeyond FurosemideHeath HensleyNo ratings yet
- Phason FHC1D User ManualDocument16 pagesPhason FHC1D User Manuale-ComfortUSANo ratings yet
- CAT MENTAL HEALTH FOR Community Health YEAR 4Document4 pagesCAT MENTAL HEALTH FOR Community Health YEAR 4Dennis ButtoNo ratings yet
- Microsoft Word - ETERSET 2960-2 - MSDSDocument5 pagesMicrosoft Word - ETERSET 2960-2 - MSDSWinsonLimHuiWahNo ratings yet
- XT Mobile Shear: Reference GuideDocument12 pagesXT Mobile Shear: Reference GuidePrudzNo ratings yet
- Surface Anatomy Lungs Group 2bDocument8 pagesSurface Anatomy Lungs Group 2bapi-323356666No ratings yet
No Balance Billing Policy
No Balance Billing Policy
Uploaded by
Rhyne Amante Ypulong0 ratings0% found this document useful (0 votes)
1K views6 pagesPhilHealth has established new case rates for selected medical cases and surgical procedures to improve member benefits and attain universal health coverage. The case rates will serve as standardized reimbursement amounts for medical interventions and include professional fees. A No Balance Billing policy has also been adopted to protect members from additional fees for cases covered under government facilities or outpatient packages. The policy aims to provide optimal financial risk protection and support efforts to reduce maternal and infant mortality rates.
Original Description:
No Balance Billing Policy - Philhealth
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentPhilHealth has established new case rates for selected medical cases and surgical procedures to improve member benefits and attain universal health coverage. The case rates will serve as standardized reimbursement amounts for medical interventions and include professional fees. A No Balance Billing policy has also been adopted to protect members from additional fees for cases covered under government facilities or outpatient packages. The policy aims to provide optimal financial risk protection and support efforts to reduce maternal and infant mortality rates.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
1K views6 pagesNo Balance Billing Policy
No Balance Billing Policy
Uploaded by
Rhyne Amante YpulongPhilHealth has established new case rates for selected medical cases and surgical procedures to improve member benefits and attain universal health coverage. The case rates will serve as standardized reimbursement amounts for medical interventions and include professional fees. A No Balance Billing policy has also been adopted to protect members from additional fees for cases covered under government facilities or outpatient packages. The policy aims to provide optimal financial risk protection and support efforts to reduce maternal and infant mortality rates.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 6
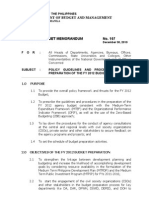
Republic of the Philippines
PHILIPPINE HEALTH INSURANCE CORPORATION
Citystate Centre, 709 Shaw Boulevard, Pasig City
Healthline 637-9999 www.philhealth.gov.ph
PHILHEAI.TH CIRCULAR
No. Oil- 2cD
To:All PhilHealth Stakeholders and All Concerned
Subject:New PhilHealth Case Rates for Selected Medical Cases
and Surgical Procedures and the No Balance Billing Policy
RATIONALE
In consonance with the Government's thrust to attain Universal Health Coverage
(UHC) in 3 years (by the end of CY2013), PhilHealth has embarked on continuous
improvement of member benefits to be consistently responsive to ever-changing
demands. This also serves to keep members within the PhilHealth system as well as
entice prospective members to join the social health insurance fund.
Under Section 16, Article TV of Republic Act (RA) 7875 as amended by RA 9241,
PhilHealth has the power and function to formulate and promulgate policies for the
sound administration of the National Health Insurance Program. Further, under the
same Section, Philhealth can formulate and implement guidelines on contributions and
benefits; portability of benefits, cost containment and quality assurance; and health care
provider arrangements, payment methods, and referral systems. Meanwhile, Section 46,
Rule VIII of the Implementing Rules and Regulations of RA7875 as amended, provides
that, payment of a healthcare provider shall be made through such other mechanisms as
ma}' hereafter be determined by the Corporation.
Accordingly, case rates payment is an internationally accepted payment mechanism that
serves to package payment for health interventions. It is beneficial for members,
providers, and the Corporation as it is much simpler to administer, and it potentially is
more transparent in terms of prices for interventions. Through this mechanism,
members will be able to predict how much PhilHealth would be paying for each of the
services provided. Moreover, Case Rates improve turn-around time for claims processing
and payment to providers in order to achieve better cost-efficiency for PhilHealth and faster
reimbursements for accredited providers and members, when necessary.
The computation for fair rates were determined through a process where tariff rates,
contracting rates for public and private hospitals, and average value per claims for
preceding years were considered and percentage weights were given to each. The highest
computed rates were identified and used. The top conditions and procedures that make
up 49% of total claims from preceding years were prioritized to be packaged into case
rates.r@--@ -- /
!:@@;iC^H
@>/ I
Page 1 of 6
t
VI)
Corollary to case rate payments, and since it is the aspiration of UHC to provide optimal
financial risk protection tor all its members, especially to the most vulnerable groups
including the poorest of the poor, the Corporation, through PhilHealth Board Resolution
No. 1441, series of 2010, adopted a "No Balance Billing Policy" (NBB) for the most
common medical and surgical conditions experienced in the country. The "No Balance
Billing" policy and its conditions are defined under Section III of this Circular.
Of special note are the Maternity Care and Newborn Care packages. Consistent still with
the objectives of UHC and in support of the United Nation's Millennium Development
Goals (UN-MDGs) of reducing maternal and infant mortality rates through affordable
interventions, PhilHealth increased the existing Maternity Care package (MCP) and
Newborn Care Package (NCP) for non-hospital facilities. This is to promote facility-
based deliveries and ensure completeness of provision of quality newborn care,
("^@nirlplinps of the latfrr are included in this Circular.
II. CASE RATES AND PROFESSIONAL FEES
The new case rates shall be the new reimbursement rates for nil cases specified. These rates
shall be the amounts to be paid to the facilities and shall include the Professional lees.
Listed below are the approved cases and their corresponding rates:
,^'
! c;er-
.0 Page 2 of 6
\i
A.MedicalCases
1
2
3
4
5
DengueI(DengueFeverand
DHFGradesI&II)
DengueII
(DHFGradesIII&IV)
PneumoniaI(ModerateRisk)
PneumoniaII(HighRisk)
EssentialHypertension
Case
Rates
(Php)
8,000
16,000
15,000
32,000
9,000
MedicalCases
6
7
8
9
10
11
CerebralInfarction(CVAI)
Cerebro-vascularAccident
(hemorrhage)(CVAII)
AcuteGastroenteritis(AGE)
Asdima
TyphoidFever
NewbornCarePackagein
HospitalsandLyinginClinics
Case
Rates
(Php)
28,000
38,000
6,000
9,000
14,000
1,750
B.SurgicalCases
1
3
4
5
Hemodialysis
MaternityCarePackage
NSDPackageinLevel1
Hospitals
NSDPackageinLevels2to4
Hospitals
CaesareanSection
Appendectomy
Case
Rates
(Php)
3,000
4,000
8,000
8,000
6,500
19,000
24,000
SurgicalCases
6
7
8
9
10
11
12
Cholecystectomv
DilatationandCurettagc
Thyroidectomy
Hcrniorrhaphy
Mastectomy
Hysterectomy
CataractSurgery
Case
Rates
(Php)
31,000
11,000
31,000
21,000
22,000
30,000
16,000
The Professional Fees for the above medical cases shall be 30% of die reflected amounts
while that for surgical cases shall be 40%.
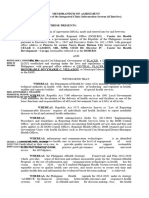
III. No Balance Billing (NBB) Policy
A.The No Balance Billing (NBB) Policy shall be applied to all PhilHcalth Sponsored
Program members and/or their dependents for the above specified cases and under any
of die following instances:
1.When admitted in government facilities/hospitals.
2.When claiming reimbursement for outpatient surgeries, he mo dialysis and
radiotherapy performed in accredited government hospitals and all non-
hospital facilities (ex. freestanding dialysis centers and ambulatory surgical
clinics (ASCs).
3.When availing of existing outpatient packages for TB-DOTS (Php 4,000),
Malaria (Php 600), and HIV-AIDS (Php 7,500 per quarter or Php 30,000 per
year). All other existing policies/guidelines covering these packages shall
remain in effect.
4.In support of the country commitment to reduce maternal and infant
mortality rates and improve maternal and newborn care enunciated in the
Millennium Development Goals (MDG), die NBB poLicy, in addition to
covering Sponsored members and dieix dependents, shall also apply to any
other member type in all accredited MCP (non-hospital) providers. This shall
cover cl-aims for MCP and Newborn Care Package (NCP) in these facilities.
B.For these purposes, the "No Balance Billing1' Policy shall mean that no other fees or
expenses shall be charged of paid for by the patient-member above and beyond the
packaged rates.
C.For drugs and medicines, supplies, or diagnostic procedures not available in the hospital,
said facility shall purchase necessary items/services in advance on behalf of the member.
D.In instances when out-of-pocket spending is incurred for health facility costs (Ex.^when
PhilHcalth members/dependents are made to purchase necessary items and sendees
during confinement, whether from die health facility itself and/or providers outside the
health facility), the health facility is required to attach the official receipt/* (OR/s)
detailing the purchases in the claim application fot the said confinement. The member
shall be reimbursed allowable expenses detailed in die attached OR/s with the said
payment to the member deducted front die case payment diat would be paid to die
health facility.
E.la instances when out-of-pocket spending is incurred for professional fees (such as when
PhiiHealth members/dependents are made to pay professional fees (PF) over and above
die case payment), the health facility is required to attach the official receipt/s (OR/s)
detailing die PF payment in the claim application for die said confinement. The member
shall be reimbiiised allowable PF payment expenses detailed in die attached OH/s with
die said payment to the member deducted from the case payment paid to die health
tacilitv. The healdi facility shall dicn make die necessary adjustments and application of
sanctions to die health professional/s.
F.In instances wherein the case rate was already paid in full to die facility but die official
receipts for necessary items and services bought during confinement or payment tor
professional fees were not attached to the claim application, die member may request for
re-adjustment within six (6) months from die date of discharge. This shall be evaluated
a ad paid accordingly to the member once-rccjuesthas been.jiia.de and the necessary
i'^-@:-r;^-.- =,7.--.^! page3of6 t4
evidences of payment have been submitted to PhilHealth. This shall be charged to
future claims of the health facility with corresponding sanctions or penalties the
Corporation may charge.
IV. General Rules
A.Reimbursement for the abovemendoncd case rates shall be made directly to the facility.
Hospitals shall act as the withholding tax agent for Professional Fees.
B.Abovementioned case rates arc inclusive of payment to all accredited doctors who
attended or managed a specific case. Cases attended by non accredited professionals shall
be denied. Government hospitals shall facilitate die payment of the PF share to health
personnel with the payment of PF subject to die existing rules on pooling as stated in
Section 35 of RA7875 as amended and its Implementing Rules and Regulations and
PhUHealth Circular No. 27, s-2009.
C.For Claims of PhUHealth members not covered by Section III (NBB Policy) of this
circular, the benefit shall be deducted from die total actual charges, with the remaining
amount to be charged to the member as out-of-pocket payment. For example: Acute
Gastroenteritis=Php6,000
D.For purposes of efficient processing of claims, all accredited facilities ate required to
provide correct RVS and/or ICD-10 codes in Claim Form 2.
E.Reimbursement for these packages shall be based on die main condition as stated in
PhiJ Health Circular No. 04, s-2002.
F.The total number of confinement days shall be deducted from the 45-day limit per
calendar year as stated in PhilHealth Circular 14 s. 2010 re: Order of Discharge. For
hemodialysis and radiotherapy, one (1) day shall be deducted from the 45-day allowance
per year for each availment. For the outpatient packages for Malaria and HIV"-AIDS,
existing rules on the 45-day limit will apply. TB DOTS is excluded from the 45 day limit.
G.The case rates shall follow the rule on single period of confinement except for
hemodialysis and radiotherapy packages, where availment is on a per session basis.
H. Upon evaluation and monitoring, all inconsistencies regarding reimbursement policies
shall be charged to future claims of the facilities.
V. Rules on Filing Claims
A.All claims shall be filed within sixty (60) days from the date of discharge.
B.All existing documents and information shall still be required. Please be reminded on the
proper accomplishment of the claim form 2 and to indicate correct RVS/ICD10 code
appropriate for the package being claimed.
C.For NCP claims, under die column of drugs and medicines specify Hepatitis B and BCG
vaccination if given. Essential Newborn Care, NBS and Newborn Hearing Screening
Test should be written under laboratories, supplies and others.
D.Claims with incomplete documentary requirements shall be returned to die tacility for
completion and shall be re-filed within 60 days from receipt of notice; otherwise it shall
be denied.
E.The hospitals shall segregate the claims with separate transmittal as follows:
1.Case Payment claimsi C\.v^.-.."..-.'"'/.
2.Fee for service claims! ; -, __ ^$$1 -- _ _ l.
CEKTii-i.-:,'.
@;
r:@ -
Pat>e 4 of 6
tf
TotalActualCharges
Php9,000
PhilHealthBenefit
Php6,000
Co-paymentofmember
Php3,000
VI. Specific Rules Per Package
A. Maternity Care Package (MCP)
1. The payment for this enhanced package shall be Eight Thousand Pesos (Php 8,000)
in accredited non-hospital facilities (e.g., lying-in clinics, maternity clinics, birthing
homes and RHUs) and divided as follows:
2.The NBB Policy shall only be applied to all claims as described in Section III above. -
3.Reimbursement shall be made to the facility except for components direcdy payable
to the member (prenatal care fee).
4.For normal deliveries completed in accredited MCP providers requiring emergency
obstetric services and subsequent referral to a higher facility, die MCP provider shall
be reimbursed fully and trie referral facility shall also be reimbursed depending on the
services rendered.
5.For instances where no deliveries were completed in the MCP facility due to
complications, die MCP facility shall also be reimbursed die total amount equivalent
to ten percent (10%) of the facility fee (amounting to Php 650) for the services
provided.
B. Normal Spontaneous Delivery (NSD) Package
1. The payment for normal spontaneous delivery (NSD) package in accredited
government and private hospitals shall be as follows:
2.The NBB Policy shall be applied to claims as described in Section III.
3.Reimbursement shall be made directly to die facility including payment of
professional fees for medically necessary services except for components directly
payable to the member.
C. Newborn Care Package (NCP)
1. The package shall be increased to One Thousand Seven Hundred and Fifty Pesos
(Php 1,750) which shall include die following services, immediate drying of the
newborn, early skin-to-skin contact, cord clamping, non-separadon of mother/baby
for early breastfeeding initiation, eye prophylaxis, Vitamin K administration, weighing
of die newborn, BCG vaccination, ^e^tie6"-B-uMKuiaiza-Eio-n.{-lst dose), Newborn
Page 5 of 6
rf
a.Facilityfee(Includingprofessionalfee)
b.Member'sprenatalcarefee
TOTAL
6,500
1,500
8,000
LevelofFacility
Level1Hospitals
Levels2to4
Hospitals
PrenatalCare FacilityincludingPF
Php8,000
1,500
6,500
Php6,500
1,500
5,000
Screening Test (NBS), Newborn Hearing Screening Test, and Professional fee (that
includes breastfeeding advice and physical examination of the baby, among others).
2.In instances when die enumerated sendees for NCP above were not provided
completely or patient-members were asked to purchase/access sendees outside the
facility -and an Official receipt is attached to the claim, die member shall be reimbursed
all eligible expenses detailed in the attached OR/s with the said payment to the member
deducted from the case payment that would be pud to the health facility.
3.In instances where, upon post-audit, services were not rendered or were not
complete as shown above, dien diese shall be charged to future claims of the healdi
facility with corresponding sanctions or penalties the Corporation may chat.i>e
4.All NCP claims arc covered by the. NBB Policy as described in Section III.
VII.Compliance Monitoring
Compliance to the above shall be monitored and evaluated periodically in accordance with
implementing guidelines to be issued.
VIII.Penalties And Sanctions
Accredited providers diat violate any provision of this Circular shall be meted the
appropriate sanctions and penalties available to die Corporation. Furthermore, these shall be
included in die Provider Assessment Monitoring System (PAMS) and shall be subjected to
warranties of accreditation and other such instruments that the Corporation may utilize.
Finally, dicse may be repotted to the Department of Healdi (DOH) and/or Professional
Regulation Commission for appropriate action, when necessary.
IX.Periodic Review, Evaluation, And Adjustments
This Circular, including die case rates, processes, and the no balance billing policy, shall be
subject to regular evaluation and adjustments as necessary. Such review and evaluation shall
be done 6 months after effectivity of this Circular and yearly thereafter unless revoked,
modified, amended or repealed.
X.Repealing Clause
All provisions of previous issuances that are inconsistent with any provisions of this Circular
are hereby amended/modified/or repealed accordrngly.
XI.Effectivity
This Circular shall take effect for all claims with admission date of September 1, 2011.
Further, this Circular shall be published in any newspaper of general circulation and shall be
deposited thereafter with die National Administrative Register at the University of die
Philippines-!^w Center.
'XuP"
DR. REYB! AQUINO
President arnd CEO ,
Date signed: (K(' I/@-
'lUL.
m
PhilHealth
OP-S11-43026
Page 6 of 6
*@
yI
You might also like
- 2023 LGU HSC Indicators - Feb. 19Document76 pages2023 LGU HSC Indicators - Feb. 19Diane Joy EsquivelNo ratings yet
- Retirement ScriptDocument14 pagesRetirement ScriptBrian LindseyNo ratings yet
- Proposal For Retainer Agreement - SampleDocument2 pagesProposal For Retainer Agreement - SampleRhyne Amante Ypulong100% (2)
- BS 4254Document19 pagesBS 4254gugaruban100% (4)
- IEC 60950 Rev1Document3 pagesIEC 60950 Rev1Rip_BarNo ratings yet
- 4100XPB 4198 Grupo Mexico CananDocument758 pages4100XPB 4198 Grupo Mexico CananWalissonNo ratings yet
- The Constitution of Youth AssociationDocument9 pagesThe Constitution of Youth AssociationMeshack Lee Izu0% (1)
- Comparative Analysis-5 ILHZDocument59 pagesComparative Analysis-5 ILHZRegalado Aguhayon100% (3)
- Drug Consignment Agreement SampleDocument3 pagesDrug Consignment Agreement SampleremaxiloiloNo ratings yet
- Republic Act No. 9184Document67 pagesRepublic Act No. 9184Cire EtneilavNo ratings yet
- Commission On Audit: Republic of The PhilippinesDocument1 pageCommission On Audit: Republic of The Philippinesrocky CadizNo ratings yet
- 07-NEHEHRSV - How To Register UpdatedDocument49 pages07-NEHEHRSV - How To Register UpdatedClinton Lorbes100% (1)
- Civil Service Code of The Philippines - Senate Bill 1162Document45 pagesCivil Service Code of The Philippines - Senate Bill 1162tandangmark76% (17)
- Change of OwnershipDocument11 pagesChange of OwnershipGlenn JamesNo ratings yet
- Negros Occidental Consignment SystemDocument42 pagesNegros Occidental Consignment SystemThrees See100% (3)
- Proposed Billing System of STCDocument5 pagesProposed Billing System of STCjHUN aGANo ratings yet
- AO 2016-0032 QS of Medical PositionsDocument12 pagesAO 2016-0032 QS of Medical PositionsTotoDodongGus100% (10)
- Billing FormatDocument1 pageBilling FormatParag KhandelwalNo ratings yet
- Updated Research Assistant Confidentiality AgreementDocument2 pagesUpdated Research Assistant Confidentiality AgreementIlya ChNo ratings yet
- Billing System of Bacnotan District HospitalDocument29 pagesBilling System of Bacnotan District HospitalBlessie MercadoNo ratings yet
- Performance CommitmentDocument5 pagesPerformance CommitmentEmman Acosta DomingcilNo ratings yet
- Final LGU Scorecard Indicators 2012-2016 As of April 19Document22 pagesFinal LGU Scorecard Indicators 2012-2016 As of April 19Arianne A Zamora100% (19)
- DBM BudgetDocument85 pagesDBM BudgetGab Pogi100% (1)
- Sexual Assault in The Military 2018 DoD ReportDocument26 pagesSexual Assault in The Military 2018 DoD ReportAlanna JeanNo ratings yet
- Resolution TimbuktuDocument4 pagesResolution TimbuktuSummerRainNo ratings yet
- 2022 DOH Budget BrieferDocument34 pages2022 DOH Budget BrieferArabella CatindoyNo ratings yet
- UB-04 Billing Instructions Revision Table: Revision Date Sections Revised DescriptionDocument24 pagesUB-04 Billing Instructions Revision Table: Revision Date Sections Revised DescriptioncmabryNo ratings yet
- Afpces FinanceDocument5 pagesAfpces FinanceKathy Mercado100% (1)
- Tired of All The Guides and Never-Ending Instructions?: Try A Quicker WayDocument3 pagesTired of All The Guides and Never-Ending Instructions?: Try A Quicker WayJeremarkNo ratings yet
- Mandatory ROTCDocument2 pagesMandatory ROTCPrecious Ab0% (1)
- Pak Takaful Claim FormDocument2 pagesPak Takaful Claim FormRoger Eli Paul100% (1)
- Retirement Options Sample ComputationDocument11 pagesRetirement Options Sample Computationluna acosta0% (1)
- Wanted For The NTH Time: The Return of RotcDocument2 pagesWanted For The NTH Time: The Return of RotcAdor IsipNo ratings yet
- Doh Ihmop Filled UpDocument12 pagesDoh Ihmop Filled UpRex Quilla100% (1)
- Circ2020-0022 - Impleme Nting Guidelines For The PhiiHealth Konsultasyong Sulit at Tama PhiiHealth Konsulta PackageDocument8 pagesCirc2020-0022 - Impleme Nting Guidelines For The PhiiHealth Konsultasyong Sulit at Tama PhiiHealth Konsulta PackageJL CalvinNo ratings yet
- Entitlement To Hazard PayDocument16 pagesEntitlement To Hazard PayJanette SumagaysayNo ratings yet
- Sample Retirement LetterDocument1 pageSample Retirement LetterGilbert Javier100% (1)
- Medical Consent FormDocument2 pagesMedical Consent Formapi-235272235100% (1)
- Billing Guidance For Pharmacists Professional and Patient Care Services White PaperDocument9 pagesBilling Guidance For Pharmacists Professional and Patient Care Services White Paperkrishna krNo ratings yet
- 3 - 2022 MOA - iClinicSys - TemplateDocument4 pages3 - 2022 MOA - iClinicSys - TemplateGladdy CabrezaNo ratings yet
- Bir Cda Joint Rules and RegulationsDocument12 pagesBir Cda Joint Rules and RegulationsCha Ancheta CabigasNo ratings yet
- Iclte Press Release 2018 BLGFDocument2 pagesIclte Press Release 2018 BLGFElla LagorraNo ratings yet
- 2020 NEQAS CC Registration Form and Order of PaymentDocument2 pages2020 NEQAS CC Registration Form and Order of PaymentNovie FeneciosNo ratings yet
- Pro Health Billing Setup GuideDocument22 pagesPro Health Billing Setup Guideapi-248512169100% (1)
- Introduction To Health FinancingDocument101 pagesIntroduction To Health FinancingArianne A ZamoraNo ratings yet
- Project Report - Outdoor Patient Doctor's Booking SystemDocument51 pagesProject Report - Outdoor Patient Doctor's Booking SystemSoumya Kanti Ghosh100% (1)
- Office Order No. 2011-20Document25 pagesOffice Order No. 2011-20ciryajamNo ratings yet
- Guidelines On Hiring and Re-Hiring of Job Order Personnel in The DPWH (D.O. 2013)Document4 pagesGuidelines On Hiring and Re-Hiring of Job Order Personnel in The DPWH (D.O. 2013)Diana Lyn Bello CastilloNo ratings yet
- East Delta University: MBA Program: Summer 2021Document25 pagesEast Delta University: MBA Program: Summer 2021Mohammed Imtiaz Shayek67% (3)
- Migrant Workers Act RA 10022 and 9422 Amending 8042Document49 pagesMigrant Workers Act RA 10022 and 9422 Amending 8042adrianmdelacruzNo ratings yet
- CP LTC Ley GB CGSC Cl68Document151 pagesCP LTC Ley GB CGSC Cl68Jun LlaveNo ratings yet
- Civil Service HandbookDocument169 pagesCivil Service HandbookIkechukwu Igboebisi100% (1)
- Reaction PaperDocument3 pagesReaction PaperCamilla Reyes100% (1)
- BclteDocument2 pagesBcltereiman0590No ratings yet
- Billing ArrangementDocument6 pagesBilling ArrangementJalynLopezNostratis0% (1)
- Parental Consent and Waiver FormDocument1 pageParental Consent and Waiver FormErEr Uno Rosil100% (1)
- RetirementDocument4 pagesRetirementRayvantaKumarNo ratings yet
- Military Based Resume Example: ObjectiveDocument6 pagesMilitary Based Resume Example: ObjectiveAman KalraNo ratings yet
- Government of Andhra Pradesh C.T.Department: Form of Way Bill Form X or Form 600Document3 pagesGovernment of Andhra Pradesh C.T.Department: Form of Way Bill Form X or Form 600Arjun B Menon100% (1)
- (UIS TOF) UHC and PhilHealth Slide Deck PDFDocument82 pages(UIS TOF) UHC and PhilHealth Slide Deck PDFlilacNo ratings yet
- Consultation Form: (To Be Accomplished If The Issue(s) or Concern(s) Was/were Not Solved at The Faculty-Student Level.)Document1 pageConsultation Form: (To Be Accomplished If The Issue(s) or Concern(s) Was/were Not Solved at The Faculty-Student Level.)MyMy MargalloNo ratings yet
- Philhealth Agency's Mandate and FunctionsDocument10 pagesPhilhealth Agency's Mandate and FunctionsjonaNo ratings yet
- All Case RateDocument91 pagesAll Case RateTimothy Dycalle ManosNo ratings yet
- ao2016-0033-PHIC Pooling DistDocument5 pagesao2016-0033-PHIC Pooling DistAccount AlugrivNo ratings yet
- Employment Contract - SAMPLEDocument7 pagesEmployment Contract - SAMPLERhyne Amante YpulongNo ratings yet
- Demand Letter To UELDocument1 pageDemand Letter To UELRhyne Amante Ypulong100% (1)
- Proposal To For TIEZADocument4 pagesProposal To For TIEZARhyne Amante YpulongNo ratings yet
- Letter To Mrs. CastilloDocument1 pageLetter To Mrs. CastilloRhyne Amante YpulongNo ratings yet
- Demand - Second NoticeDocument2 pagesDemand - Second NoticeRhyne Amante YpulongNo ratings yet
- Law On Sales, Agency and Bailments-OverviewDocument6 pagesLaw On Sales, Agency and Bailments-OverviewRhyne Amante Ypulong0% (2)
- Accounting of Proceeds of Sale of Portion of The Estate of Ricardo Domingo and ExpensesDocument3 pagesAccounting of Proceeds of Sale of Portion of The Estate of Ricardo Domingo and ExpensesRhyne Amante YpulongNo ratings yet
- Sapoe Cofee Vending Machine-Joel Chua QuoteDocument3 pagesSapoe Cofee Vending Machine-Joel Chua QuoteRhyne Amante YpulongNo ratings yet
- Frenkel's ExerciseDocument40 pagesFrenkel's ExerciseManiu EmeseNo ratings yet
- Altitude, Cloud Cover and LatitudeDocument64 pagesAltitude, Cloud Cover and LatitudeIsarra AmsaluNo ratings yet
- Iec Inverse Protection CurvesDocument1 pageIec Inverse Protection CurvesEng-Ahmad Abo-AledousNo ratings yet
- Capinew Account June13Document7 pagesCapinew Account June13ashwinNo ratings yet
- On Light: Science Holiday Homework Made By-Aish Mishra Class-8 Diamond Roll No.-6Document9 pagesOn Light: Science Holiday Homework Made By-Aish Mishra Class-8 Diamond Roll No.-6Ansh MishraNo ratings yet
- Whirlpool BIWDWG861484uk enDocument4 pagesWhirlpool BIWDWG861484uk ennadaljoachim77No ratings yet
- Compact Evaporators: New Buffalo Trident GaccDocument16 pagesCompact Evaporators: New Buffalo Trident GaccPreeti gulatiNo ratings yet
- PHAS0027 RevisionDocument21 pagesPHAS0027 Revisionunknown.unknown9901No ratings yet
- Seed Extraction MethodsDocument3 pagesSeed Extraction MethodsPreetam NayakNo ratings yet
- DR Physique Lean Bulking Series II 2015Document121 pagesDR Physique Lean Bulking Series II 2015Vlad Alexandru50% (2)
- Soil Acidity and LimingDocument12 pagesSoil Acidity and LimingEloi Carlos GoveNo ratings yet
- Corn Growth StagesDocument33 pagesCorn Growth StagesIvan JovanovićNo ratings yet
- Inorganic Chemistry HomeworkDocument3 pagesInorganic Chemistry HomeworkAlpNo ratings yet
- GRES Integrated Energy Storage SystemDocument33 pagesGRES Integrated Energy Storage SystemVadim PopovichNo ratings yet
- 1 Case IDC PDFDocument7 pages1 Case IDC PDFPilar Dueñas Maldonado0% (1)
- Case Study On A Highway Project: Environmental Impact AssesmentDocument10 pagesCase Study On A Highway Project: Environmental Impact AssesmentSRUTHI FRANCIS M.Tech Environmental Engineering 2020-2022No ratings yet
- Emotional IntelligenceDocument43 pagesEmotional IntelligenceMelody ShekharNo ratings yet
- Case Study Booklet 2 PDFDocument43 pagesCase Study Booklet 2 PDFguddu yadavNo ratings yet
- The Development of A Heat Wave Vulnerability Index For London-2013Document10 pagesThe Development of A Heat Wave Vulnerability Index For London-2013gilberto777No ratings yet
- Safe Practices For Welding InspectorsDocument39 pagesSafe Practices For Welding InspectorsAlejandro RodríguezNo ratings yet
- NeuroVascular (NV) Holding PointsDocument2 pagesNeuroVascular (NV) Holding PointsHatem Farouk100% (2)
- Beyond FurosemideDocument13 pagesBeyond FurosemideHeath HensleyNo ratings yet
- Phason FHC1D User ManualDocument16 pagesPhason FHC1D User Manuale-ComfortUSANo ratings yet
- CAT MENTAL HEALTH FOR Community Health YEAR 4Document4 pagesCAT MENTAL HEALTH FOR Community Health YEAR 4Dennis ButtoNo ratings yet
- Microsoft Word - ETERSET 2960-2 - MSDSDocument5 pagesMicrosoft Word - ETERSET 2960-2 - MSDSWinsonLimHuiWahNo ratings yet
- XT Mobile Shear: Reference GuideDocument12 pagesXT Mobile Shear: Reference GuidePrudzNo ratings yet
- Surface Anatomy Lungs Group 2bDocument8 pagesSurface Anatomy Lungs Group 2bapi-323356666No ratings yet