Professional Documents
Culture Documents
Toxina en Oetoartritis
Toxina en Oetoartritis
Uploaded by
Danaes CaballeroCopyright:
Available Formats
You might also like
- Pain Neuroscience EducationDocument26 pagesPain Neuroscience EducationGustavo Cabanas100% (1)
- Adhesive Capsulitis Presentation May 2009Document29 pagesAdhesive Capsulitis Presentation May 2009cm4100% (1)
- Alzheimer's Disease Research PaperDocument24 pagesAlzheimer's Disease Research Papershayne86% (22)
- Muscle-Brain Communication in Pain The Key Role of MyokinesDocument11 pagesMuscle-Brain Communication in Pain The Key Role of MyokinesGrossl Schorr FernandoNo ratings yet
- NCPs For ParotidectomyDocument12 pagesNCPs For ParotidectomyCarla Manaloto50% (2)
- Chapter 4. Determinants of LearningDocument36 pagesChapter 4. Determinants of LearningAlyssa Marie SociasNo ratings yet
- CVI and Sensory IntegrationDocument8 pagesCVI and Sensory IntegrationKriti ShuklaNo ratings yet
- Ejp 1773Document20 pagesEjp 1773xbeligNo ratings yet
- The Effectiveness of Pain Neuroscience Education Combined With Manual Therapy and Home Exercise For Chronic Low Back PainDocument12 pagesThe Effectiveness of Pain Neuroscience Education Combined With Manual Therapy and Home Exercise For Chronic Low Back PainBruno AssunçaoNo ratings yet
- Low Back PainDocument16 pagesLow Back PainartgpsNo ratings yet
- Ijerph 19 02559Document13 pagesIjerph 19 02559Luisa BarbeitoNo ratings yet
- Exercise For Chronic Musculoskeletal Pain: A Biopsychosocial ApproachDocument9 pagesExercise For Chronic Musculoskeletal Pain: A Biopsychosocial ApproachAndressa FerreiraNo ratings yet
- Axial Low Back Pain One Painful Area - Many Perceptions and Mechanisms - Förster Et Al '13Document8 pagesAxial Low Back Pain One Painful Area - Many Perceptions and Mechanisms - Förster Et Al '13Craig ChambersNo ratings yet
- Effective Treatment Options For Musculoskeletal Pain in Primary Care: A Systematic Overview of Current EvidenceDocument30 pagesEffective Treatment Options For Musculoskeletal Pain in Primary Care: A Systematic Overview of Current EvidenceAndrewL91No ratings yet
- Real Project EditedDocument27 pagesReal Project EditedAbdulrahman YakubuNo ratings yet
- PieberDocument10 pagesPieberPablo WoodwardNo ratings yet
- An Overview of The Management of Persistent Musculoskeletal PainDocument9 pagesAn Overview of The Management of Persistent Musculoskeletal PainFebyan FebyanNo ratings yet
- Naturally Occurring Glucosinolates and Isothiocyanates As A Weapon Against Chronic Pain: Potentials and LimitsDocument19 pagesNaturally Occurring Glucosinolates and Isothiocyanates As A Weapon Against Chronic Pain: Potentials and LimitsKEYLA VANESSA MORALES RODRIGUEZ ESTUDIANTENo ratings yet
- Tzenalis Study ProtocolDocument9 pagesTzenalis Study ProtocolCristoper PanjaitanNo ratings yet
- Heuts Fear OA Pain 2004Document8 pagesHeuts Fear OA Pain 2004damien333No ratings yet
- 105221-Article Text-284848-1-10-20140710Document6 pages105221-Article Text-284848-1-10-20140710hariNo ratings yet
- Botulinum Toxin Use in Post Traumatic Cervical Dystonia and Head TremorDocument14 pagesBotulinum Toxin Use in Post Traumatic Cervical Dystonia and Head TremorSynergy Taman ratuNo ratings yet
- Castrogiovanni 2016Document14 pagesCastrogiovanni 2016carlos corteNo ratings yet
- Relations Between Brain Alterations and Clinical Pain Measures in Chronic Musculoskeletal Pain: A Systematic ReviewDocument41 pagesRelations Between Brain Alterations and Clinical Pain Measures in Chronic Musculoskeletal Pain: A Systematic ReviewRodrigo GuzmánNo ratings yet
- Orofacial Musculoskeletal Pain. An Evidence-Based Bio-Psycho-Social Matrix ModelDocument27 pagesOrofacial Musculoskeletal Pain. An Evidence-Based Bio-Psycho-Social Matrix ModelAMBAR JOSEFA ALEJANDRA MORAGA VALENZUELANo ratings yet
- 10 1002@ejp 1666Document45 pages10 1002@ejp 1666Gabriel DelfinoNo ratings yet
- Ex. ProtocolDocument17 pagesEx. ProtocoladityaNo ratings yet
- 10 1016@j Ultrasmedbio 2020 02 004Document15 pages10 1016@j Ultrasmedbio 2020 02 004Humberto Salas VelizNo ratings yet
- Osteoarthritis in The Geriatric Population 1Document7 pagesOsteoarthritis in The Geriatric Population 1api-532703094No ratings yet
- 10 2519:jospt 2018 7476Document8 pages10 2519:jospt 2018 7476Evelyn MalaguttiNo ratings yet
- Best Practice & Research Clinical Rheumatology: Fiona M. Blyth, Naomi NoguchiDocument9 pagesBest Practice & Research Clinical Rheumatology: Fiona M. Blyth, Naomi NoguchiGufron MustofaNo ratings yet
- Evaluating Meridian-Sinew Release Therapy For The Treatment of Knee OsteoarthritisDocument10 pagesEvaluating Meridian-Sinew Release Therapy For The Treatment of Knee OsteoarthritisGuilherme PenicheNo ratings yet
- Dysfunctional Analgesia During ExerciseDocument10 pagesDysfunctional Analgesia During ExerciseEric MatsuzakiNo ratings yet
- Wells and T 2017Document9 pagesWells and T 2017Alejita TingoNo ratings yet
- Walet (5615275) ThesisDocument24 pagesWalet (5615275) ThesisAmna SandhuNo ratings yet
- Effects of Emg Biofeedback On Pain and Quality of Life in Cervical Dystonia 2329 6895.1000144Document6 pagesEffects of Emg Biofeedback On Pain and Quality of Life in Cervical Dystonia 2329 6895.1000144danishmujibNo ratings yet
- Anxiety July 2011Document8 pagesAnxiety July 2011aswadiibrahimNo ratings yet
- Use of Botulinum Toxin in Orofacial Clinical PracticeDocument16 pagesUse of Botulinum Toxin in Orofacial Clinical Practiceluis castroNo ratings yet
- Dekhne 2023 - Effectiveness of Botulinum Toxin in The Treatment of Neuropathic Pain A Literature ReviewDocument7 pagesDekhne 2023 - Effectiveness of Botulinum Toxin in The Treatment of Neuropathic Pain A Literature ReviewDwika AudiyanandaNo ratings yet
- A Multinational Cross-Sectional StudyDocument15 pagesA Multinational Cross-Sectional StudySadam AbbasiNo ratings yet
- BurstDr Visceral PainDocument11 pagesBurstDr Visceral Painnavid.amirabadiNo ratings yet
- EJHC Volume 14 Issue 3 Pages 593-604Document12 pagesEJHC Volume 14 Issue 3 Pages 593-604sutgaming375No ratings yet
- Cheung2020 PDFDocument15 pagesCheung2020 PDFSandra Milena Cortes SotoNo ratings yet
- Schwerla 2020Document8 pagesSchwerla 2020João Paulo Vila Nova GomesNo ratings yet
- Reduced Pressure PainDocument7 pagesReduced Pressure PaindanaNo ratings yet
- Lateral Epicondylalgia A Musculoskeletal Physiotherapy PerspectiveDocument14 pagesLateral Epicondylalgia A Musculoskeletal Physiotherapy PerspectiveyanikaiNo ratings yet
- Orita 2011Document8 pagesOrita 2011iosif iliaNo ratings yet
- Jmu 26 194Document6 pagesJmu 26 194Arkar SoeNo ratings yet
- 1 s2.0 S204908012101027X Main 1Document10 pages1 s2.0 S204908012101027X Main 1Amirah FaridahNo ratings yet
- Toxins: Central Effects of Botulinum Neurotoxin-Evidence From Human StudiesDocument11 pagesToxins: Central Effects of Botulinum Neurotoxin-Evidence From Human StudiesTameemNo ratings yet
- Fotobiomodulacion - FibromialgiaDocument15 pagesFotobiomodulacion - FibromialgiaGonzalo MoragaNo ratings yet
- Journal 7 PDFDocument9 pagesJournal 7 PDFfransAPNo ratings yet
- Draft Rol-1Document3 pagesDraft Rol-1rosemarytimiyaNo ratings yet
- New Synopsis PranjalDocument5 pagesNew Synopsis PranjalPranjalNo ratings yet
- 28 Autoantibodies and Neuropathic Pain: John M. Dawes David L. BennettDocument18 pages28 Autoantibodies and Neuropathic Pain: John M. Dawes David L. Bennett363331272No ratings yet
- Physical Therapy Protocols To Attenuate Skeletal Muscle Atrophy in Critically Ill Patients Narrative ReviewDocument11 pagesPhysical Therapy Protocols To Attenuate Skeletal Muscle Atrophy in Critically Ill Patients Narrative ReviewVladimir AlvarezNo ratings yet
- Etoricoxib For Arthritis and Pain ManagementDocument15 pagesEtoricoxib For Arthritis and Pain Managementbkvuvce8170No ratings yet
- Artigo Comparação Botox e DyportDocument5 pagesArtigo Comparação Botox e DyportGabriela IesNo ratings yet
- Mechanical Neckpain Article 1Document8 pagesMechanical Neckpain Article 1Zulaikatu MustaphaNo ratings yet
- 2014 The Pain of Tendinopathy - Physiological or PathophysiologicalDocument15 pages2014 The Pain of Tendinopathy - Physiological or PathophysiologicalDavid Alejandro Cavieres AcuñaNo ratings yet
- Autonomic Nervous System Dysregulation and Osteoarthritis PainDocument9 pagesAutonomic Nervous System Dysregulation and Osteoarthritis Paincursotplo2021No ratings yet
- Feasibility of High Dose Medical Exercise Therapy in Patients With Long Term Symptomatic Knee OsteoarthritisDocument10 pagesFeasibility of High Dose Medical Exercise Therapy in Patients With Long Term Symptomatic Knee OsteoarthritisKasmia MalikNo ratings yet
- Fibromyalgia SyndromeFrom EverandFibromyalgia SyndromeJacob N. AblinNo ratings yet
- Herbert 1997 Fortnightly Review Stress The BrainDocument6 pagesHerbert 1997 Fortnightly Review Stress The BrainIqhsan IbrNo ratings yet
- 7 Memory Attention and Mental WorkloadDocument30 pages7 Memory Attention and Mental WorkloadGretchen Laurente100% (4)
- 14 Disability Categories Under Idea PDFDocument3 pages14 Disability Categories Under Idea PDFvenicedmNo ratings yet
- Hydrocephalus: Common Names For DisorderDocument5 pagesHydrocephalus: Common Names For DisorderGita Herminda PutriNo ratings yet
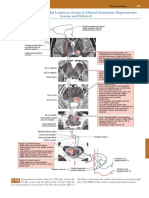
- Posterior Column-Medial Lemniscus System in Clinical Orientation: Representative Lesions and DeficitsDocument1 pagePosterior Column-Medial Lemniscus System in Clinical Orientation: Representative Lesions and DeficitsEduardo RodriguezNo ratings yet
- Directions: Each Item Below Contains A Question Followed by Suggested Responses. Select The One Best ResponseDocument7 pagesDirections: Each Item Below Contains A Question Followed by Suggested Responses. Select The One Best ResponseEsmareldah Henry SirueNo ratings yet
- Final Exam of g10 2019 - 2020Document2 pagesFinal Exam of g10 2019 - 2020Sfa Mabini BatangasNo ratings yet
- NCP LeptoDocument1 pageNCP LeptoFranz RolfNo ratings yet
- Learning Disabilities PDFDocument32 pagesLearning Disabilities PDFchester chesterNo ratings yet
- Epilepsy EpilepsyDocument8 pagesEpilepsy EpilepsyJobelle AcenaNo ratings yet
- Monro-Kellie 2.0: The Dynamic Vascular and Venous Pathophysiological Components of Intracranial PressureDocument13 pagesMonro-Kellie 2.0: The Dynamic Vascular and Venous Pathophysiological Components of Intracranial PressureLeandro NogueiraNo ratings yet
- Biom3003 Sample Exam::) Fuck Yess We Did It!!! Notes From Someone Who Took The Exam Last YearDocument18 pagesBiom3003 Sample Exam::) Fuck Yess We Did It!!! Notes From Someone Who Took The Exam Last Yearbrip selNo ratings yet
- Rajah Menunjukkan Carta Alir Sistem Saraf. Apakah P?: A KraniumDocument20 pagesRajah Menunjukkan Carta Alir Sistem Saraf. Apakah P?: A KraniumanabukitmertajamNo ratings yet
- APPETITE: Physiological and Neurobiological AspectsDocument8 pagesAPPETITE: Physiological and Neurobiological AspectsTamara Souza RossiNo ratings yet
- Carpal Tunnel SyndromeDocument2 pagesCarpal Tunnel SyndromeHejar A.No ratings yet
- EpilepsyDocument28 pagesEpilepsyRajeev RanjanNo ratings yet
- SpineInjury - Dr. PuntodewaDocument41 pagesSpineInjury - Dr. PuntodewaWindy MentariNo ratings yet
- Neurocritical CareDocument337 pagesNeurocritical Cares SNo ratings yet
- Applications On Neurological and Neuropsychiatric Diseases: MembersDocument14 pagesApplications On Neurological and Neuropsychiatric Diseases: MembersNiobe LilithNo ratings yet
- Reye SyndromeDocument15 pagesReye Syndromezeeky35No ratings yet
- Autism PDFDocument25 pagesAutism PDFTalal 197No ratings yet
- Fundamentals of Nervous System Conduction: B. Pathophysiology 1.) Anatomy and PhysiologyDocument27 pagesFundamentals of Nervous System Conduction: B. Pathophysiology 1.) Anatomy and PhysiologyJanine P. Dela CruzNo ratings yet
- 2017 A Neurobiologist's Attempt To Understand Persistent PainDocument8 pages2017 A Neurobiologist's Attempt To Understand Persistent PainCristian OyarzoNo ratings yet
- Brain WavesDocument7 pagesBrain WavesvamseenetsNo ratings yet
- The Pupillary Light Reflex PathwayDocument5 pagesThe Pupillary Light Reflex PathwayNauli PanjaitanNo ratings yet
- M2 Cia-Observation Skills - ManzanilloDocument2 pagesM2 Cia-Observation Skills - ManzanilloSheena Lhane ManzanilloNo ratings yet
Toxina en Oetoartritis
Toxina en Oetoartritis
Uploaded by
Danaes CaballeroOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Toxina en Oetoartritis
Toxina en Oetoartritis
Uploaded by
Danaes CaballeroCopyright:
Available Formats
Botulinum toxin therapy for osteoarticular
pain: an evidence-based review
Jasvinder A. Singh
Abstract: Botulinum (BoNT) toxin has been used for its muscle-paralyzing action in conditions
such as treatment of wrinkles, cervical dystonia and blephrospasm. There is preclinical and
emerging clinical evidence of another mechanism of action of BoNT, namely, an antinociceptive
action. In this review, we provide an evidence-based review of clinical studies of BoNT in
osteoarticular conditions, such as osteoarthritis, tennis elbow, low back pain, and hand pain.
Many randomized controlled trials (RCTs) found evidence of short-term efficacy of an injection
of BoNT in relief of pain, and in some cases, improvement of function and quality of life.
However, more clinical trials are needed to better define the clinical use of BoNT for treatment
of refractory osteoarticular pain.
Keywords: arthritis, Botulinum toxin, pain, therapy
Introduction
Recent population surveys have reported that
2228% of adults in the US reported
physician-diagnosed arthritis [Huijnen et al.
2006; Layeeque et al. 2004]. Arthritis and rheu-
matism are the leading causes of disability in
adults aged 18 years and over in the US
[Centers for Disease Control and Prevention,
2009]. In a European survey of prevalence of
pain in the general population, moderate to
severe pain lasting 6 months or longer was
reported by 19% of respondents, of whom 40%
(8% of all respondents) had joint pain due to
osteoarthritis and rheumatoid arthritis [Breivik
et al. 2006], the two most common types of
arthritic conditions in the population [Lawrence
et al. 1998]. Both osteoarthritis and rheumatoid
arthritis are associated with significant joint pain
and functional limitations [Hunter et al. 2009;
Bjork et al. 2007] and deficits in health-related
quality of life [Slatkowsky-Christensen et al.
2007; Salaffi et al. 2005; Kvien and Uhlig,
2005]. Thus, arthritis constitutes a significant
public health burden.
While significant therapeutic advances have been
made in targeting inflammation in patients with
rheumatoid arthritis [Feldmann and Maini,
2008; Siddiqui, 2007], few therapies are available
to treat refractory pain and functional limitation
in patients with osteoarthritis. Use of common
therapies such as nonsteroidal anti-inflammatory
drugs (NSAIDs), opioid medications and analge-
sics is associated with significant adverse events
in some patients [Zhang et al. 2008, 2007; Ge
et al. 2006]. Intra-articular corticosteroids,
intra-articular hyaluronic acid and topical pre-
parations have limited efficacy in patients with
osteoarthritis [Bellamy et al. 2006a, 2006b;
Van Der Windt et al. 2003; Green et al. 2003;
Rains and Bryson, 1995]. Physical therapy is
effective [Jamtvedt et al. 2008]; however, compli-
ance with therapy has not been assessed and
many patients are unable to pursue the therapy
due to personal preference, comorbidities and/or
distance from the therapy site. Thus, limited
effective and safe therapeutic options are avail-
able for the treatment of refractory joint pain in
patients with arthritis. There is a need therefore
for new therapeutic options for treatment of
refractory osteoarticular pain.
Botulinum toxin (BoNT) is one of the most
potent neurotoxins. It exists in seven serotypes,
A through G. It consists of a 50KDa light chain
and a 100KDa heavy chain linked with a disul-
fide bond. Most clinical applications of BoNTare
based on its ability to block neuromuscular trans-
mission by blocking the release of acetylcholine
[Arnon et al. 2001], which leads to reversible
muscle paralysis. However, in several clinical
studies, including those of treatment of painful
http://tab.sagepub.com 105
Therapeutic Advances in Musculoskeletal Disease Review
Ther Adv Musculoskel Dis
(2010) 2(2) 105118
DOI: 10.1177/
1759720X09357113
! The Author(s), 2010.
Reprints and permissions:
http://www.sagepub.co.uk/
journalsPermissions.nav
Correspondence to:
Jasvinder A. Singh,
MD, MPH
Minneapolis VA Medical
Center, Rheumatology
(111R), One Veterans
Drive, Minneapolis,
MN 55417, USA
Jasvinder.md@gmail.com
muscle contractions in patients with cervical dys-
tonia [Sycha et al. 2004; Jankovic and Schwartz,
1990] and migraine/tension headaches [Gobel
et al. 2001], an independent antinociceptive
action was noted [Freund and Schwartz, 2003;
Aoki, 2003]. The onset of muscle pain relief after
muscular injection of BoNT occurred sooner
than relief of muscle spasm; it outweighed and
often lasted longer than the relief of muscle
spasm, thereby suggesting a different antinoci-
ceptive action [Sycha et al. 2004; Freund and
Schwarz, 2003]. This led to investigation of
BoNT as a treatment for headaches, with many
randomized controlled trials (RCTs) underway.
In this evidence-based review, the evidence from
nonhuman studies and the clinical observations
from nonmusculoskeletal application in human
studies supporting an antinociceptive action of
BoNT are summarized. A systematic review of
published nonrandomized (prospective and ret-
rospective cohort studies and case series) and
randomized studies of BoNT for osteoarticular
pain was then undertaken by performing
Pubmed searches for various musculoskeletal
pain conditions and BoNT. Case reports were
not included in this review. Myofascial pain
syndromes were not included in this review,
since they have been the focus of previous
reviews [Ho and Tan, 2007; Cuevas-Trisan and
Cruz-Jimenez, 2006].
Role of neuropeptides in chronic joint pain and
effect of botulinum toxin on neuropeptides
Recent reviews summarize our current under-
standing of joint pain and various mechanisms
contributing to it [Schaible et al. 2009, 2006].
The joints are innervated with articular nerves
that contain A-delta, A-beta and C-fibers. All
joint structures except articular cartilage have
these nerve endings. In normal healthy indivi-
duals, these nociceptors have a high threshold
for excitation in response to mechanical and
thermal stimuli, such that normal activities of
walking, stair climbing, sports, and palpation of
the joint are not associated with pain/unpleasant
sensation. However, in the presence of joint
injury or inflammation, the excitation threshold
of many of these nerve fibers is decreased. This
leads to enhanced responses to both innocuous
and noxious mechanical, chemical and thermal
stimuli. This phenomenon is called peripheral
sensitization [Schaible et al. 2009]. Chronic
joint inflammation is also associated with
hyperexcitability of spinal nociceptive neurons,
ie central sensitization [Neugebauer et al. 1993;
Schaible et al. 1987]. A variety of mediators can
sensitize joint nerves and nociceptors to mechan-
ical stimuli including bradykinin, prostaglandin
E2, prostaglandin I2, serotonin, substance P
(SP) and neuropeptide Y [Schaible et al. 2006].
Another contributor to joint pain and inflamma-
tion is neurogenic inflammation. Articular nerves
stimulated due to inflammation in arthritis
release neuropeptides from nerve terminals as a
result of axon reflexes. Postganglionic sympa-
thetic nerves release neuropeptides due to sym-
pathetic reflexes, and local inflammatory cells
release neuropeptides due to cytokine or
neuropeptide-stimulation [Schaible et al. 2005].
It is likely that these processes underlie the clin-
ical observed signs and symptoms of pain and
mechanical hyperalgesia in inflamed joints.
Activation of glial cells, other immune cells, cyto-
kines and neuropeptides contributes to the gen-
eration of pain [Watkins et al. 2003; Watkins and
Maier, 2003, 2002; Woolf et al. 1997, 1994;
Woolf and Weisfeld-Hallin, 1986]. Pain path-
ways, pain receptors and various contributors to
both inflammatory and neuropathic pain have
been summarized in recent studies and reviews
[Woolf, 2004; Woolf and Mannion, 1999; Woolf
and Decosterd, 1999; Woolf and Costigan, 1999;
Willis and Westlund, 1997; Jones, 1991].
BoNT has been shown to interfere with expres-
sion of various neuropeptides such as SP and
calcitonin gene-related protein (CGRP), which
are key mediators of neurogenic inflammation
[Birklein and Schmelz, 2008]. In an animal
model of botulinum toxin A (BoNT/A), injec-
tions into rat paws reduced formalin-induced
paw edema, tissue glutamate release and spinal
cord electrical excitations [Cui et al. 2004].
BoNT/A inhibited stimulated SP release
[Lucioni et al. 2008; Purkiss et al. 2000] and
CGRP release [Lucioni et al. 2008; Rapp et al.
2006; Durham et al. 2004] in models of acute
and chronic inflammation. In vitro studies
showed that BoNT/A inhibited stimulated
CGRP release from rat trigeminal ganglia [Meng
et al. 2007] and capsaicin-stimulated SP release
from embryonic rat dorsal root ganglia neurons
[Purkiss et al. 2000]. In particular, BoNT have
been shown to inhibit cytokines, neuropeptides
and other inflammatory mediators that play an
important role in pathophysiology of both
rheumatoid arthritis and rat adjuvant arthritis
Therapeutic Advances in Musculoskeletal Disease 2 (2)
106 http://tab.sagepub.com
(animal model similar to human rheumatoid
arthritis) [Ahmed et al. 1995; Larsson et al.
1991; Kar et al. 1991; Devillier et al. 1986].
Thus, there is preclinical evidence suggesting an
antinociceptive mechanism of action of BoNT.
Clinical observations suggesting
antinociceptive action of botulinum toxin
Various clinical studies support the antinocicep-
tive action of BoNT [Yuan et al. 2009; Patti et al.
2008; Kramer et al. 2003], while some studies
found no such evidence [Sycha et al. 2006;
Voller et al. 2003; Blersch et al. 2002].
Kramer and colleagues studied the effect of intra-
dermal injection of 520 mouse units of BoNT/A
or placebo in a RCT in 15 healthy volunteers,
followed up for 14 days [Kramer et al. 2003].
Transcutaneous electrical stimulation was used
to produce pain, hyperalgesia and neurogenic
flare. BoNT/A caused an anhidrotic skin area in
all cases, and had a significantly smaller axon
reflex flare, lower pain rating, but similar
amount of hyperalgesia to pinprick and allodynia
after electrical stimulation, as compared to pla-
cebo. This study suggested that BoNT/A reduces
peripheral neuropeptide release, but the evidence
for a direct analgesic effect was limited.
Yuan and colleagues performed a double-blind
crossover trial of intradermal BoNT/A for dia-
betic neuropathic pain in 18 patients [Yuan
et al. 2009]. There was a significant reduction
in visual analog scale (VAS) pain by 0.83 at 1
week, 2.22 at 4 weeks, 2.33 at 8 weeks, and
2.53 at 12 weeks after injection in the BoNT/A
group, as compared to the respective changes of
0.39, 0.11, 0.42, and 0.53 for the placebo
group at the same time points (p <0.05).
Within the BoNT/A group, 44.4% of the
participants experienced a reduction in VAS
of 3 or more within 3 months of injection,
whereas there was no similar response in the
placebo group.
Patti and colleagues studied 30 patients with
thrombosed external hemorrhoids who did not
desire surgery [Patti et al. 2008]. Patients were
randomized to a single intrasphincteric injection
of 30 units of BoNT or saline. After 5 days of
treatment, the maximum resting pressure on
anal manometry fell more significantly in the
BoNT group (p 0.004). The reduction in pain
intensity with BoNT was noted within 1 day of
injection (p <0.001).
Ranoux and colleagues performed a RCT of
single intradermal injection of 20190 units of
BoNT/A into the painful area in 29 patients
with focal painful neuropathies and mechanical
allodynia [Ranoux et al. 2008]. Patients were fol-
lowed for 24 weeks. BoNT/A injections were
associated with persistent sustained effects on
spontaneous pain intensity, neuropathic symp-
toms, and general activity from 2 weeks after
the injection to 14 weeks, compared to placebo.
In a randomized, double-blind study, Sycha et al.
compared a single intracutaneous injection of
BoNT/A 100 units to placebo in six healthy
volunteers using a human acute inflammatory
skin model with ultraviolet B radiation induced
sunburn [Sycha et al. 2006]. No significant dif-
ferences were noted between the groups in heat
or cold pain perception threshold, skin blood
flow, mechanical pain threshold or mechanical
allodynia. BoNT/A produced changes in sudo-
motor function. The sample size in this study
was very small, leading to a possibility of type II
error, ie failure to notice a difference when one
truly exists. Blersch and colleagues compared the
heat and cold thresholds in 50 healthy volunteers
who were each injected with BoNT/A 100 units
or placebo in the two forearms in a double-blind
fashion [Blersch et al. 2002]. Using quantitative
sensory testing, no differences were found
between the groups with regards to heat and
cold pain thresholds at 4 and 8 weeks. In addi-
tion, no differences were found in electric stimu-
lation pain thresholds between the groups. This
study suggested that there was no evidence of
direct antinociceptive effect of BoNT/A in this
skin model of nociception, and that antinocicep-
tive action may be secondary to other effects
of BoNT/A such as chemodenervation or
anti-inflammatory effects.
Voller and colleagues studied 16 healthy volun-
teers after injection of either 30 units of BoNT/A
or placebo intracutaneously and responses
were studied up to 28 days after the injection
and after capsaicin application at 28 days
[Voller et al. 2003]. The groups did not differ
significantly in any of the following outcomes at
day 28: heat pain perception and tolerance
thresholds; electric pain perception and tolerance
thresholds; area of secondary hyperalgesia
JA Singh
http://tab.sagepub.com 107
after capsaicin application; and for the capsaicin-
induced flare.
Open-label studies of botulinum toxin
in osteoarticular pain
Refractory joint pain
In a retrospective study, we reported the results
of intra-articular injection of 25100 units of
BoNT/A in 15 refractory painful shoulder and
lower extremity joints in 11 patients [Mahowald
et al. 2006]. There were nine women and two
men with age ranging from 42 to 82 years. A
clinically and statistically significant decrease in
pain severity and improvement in function was
noted from baseline: lower extremity and shoul-
der pain decreased from 7 to 2.7 and 8.2 to 2.4,
respectively; shoulder flexion and abduction
improved from 68 to 113 degrees and 50 to 74
degrees, respectively; and timed stands test (time
to stand up 10 times from a sitting position)
improved from 36 to 23 seconds. The duration
of relief/improvement lasted 310 months, and
relief began by 2 weeks in most patients. None
of the patients experienced any adverse event.
In long-term follow-up of these 15 joints in 11
patients, 10 joints were reinjected with 30150
units of BoNT/A intra-articularly (Botox,
Allergan, Irvine, California, USA) [Singh et al.
2009a]. Nine of the 10 reinjections were asso-
ciated with pain reduction, as seen with the first
injection. Reduction in pain severity from 6.6
(SD, 1.2) to 3.3 (SD, 2.7) lasting 317 months
was noted, which was statistically significant
(p 0.003). None of the patients experienced
any systemic adverse event related to BoNT.
One patient had increased joint swelling with
no increase in joint pain 3 weeks after BoNT
injection. Another patient had continued increase
in joint pain after BoNT injection, which was
relieved with a subsequent BoNT injection.
In another case series, 11 adults with refractory
pain underwent injection of BoNT type A
(25100 units; Botox, Allergan) or type B
(5000 units; Myobloc, Solstice Neurosciences,
San Francisco, California, USA) into sacroiliac,
cervical/lumbar facet or sternoclavicular joint
joints and C-2 roots and lumbar disc [Dykstra
et al. 2007]. There were nine women and two
men with mean age of 48 years (SD, 10 years;
range, 3268 years). Median pain scores
decreased significantly after botulinum toxin
injections, with median decrease of 3 on 010
pain scale (range, 05; p 0.008). Pain decrease
began within 35 days for patients who
responded. Three patients had no change in
pain severity after BoNT injections, while eight
had a decrease. Five patients received repeat
injections with no evidence of decreasing efficacy
of pain relief with BoNT injections; in fact, the
duration of pain relief increased with each suc-
cessive treatment for four of the five patients
having multiple treatments. Median duration of
pain relief with BoNT injections was 1.6 months
longer than that seen with corticosteroid injec-
tions. No adverse events were reported by the
patients.
Tennis elbow
In an open-label case series of 14 patients with
treatment-resistant tennis elbow, 2040 units of
BoNT/A were injected into the extensor digi-
torum communis, Moore and colleagues found
>50% pain relief in nine of 14 patients, and com-
plete pain relief in four of 14 patients during the
68 month follow-up [Morre et al. 1997]. Pain
relief began by 2 weeks in 10 patients, 3 weeks in
one and after 1 month in two patients.
Temporomandibular joint pain
In an open-label study of 41 patients with painful
hyperactivity of the masticatory muscles, 200
units of BoNT/A (Dysport, Ipsen, Slough, UK)
was injected on either side under electromyo-
graphic guidance and patients observed for up
to 12 months [Von Lindern, 2001]. 80% patients
had improvement in pain; pain severity decreased
from a mean of 6.4 to 3.5 and 13 patients had a
major improvement as evident by disappearance
of pain. Relief lasted 312 months during the
observation period for most; only seven patients
requested reinjection. One patient had temporary
speech impairment and swallowing difficulty
postinjection. In an open-label study, 46 patients
with TMD for a median duration of 96 months
were injected with 150 units of BoNT A in both
massager and temporal is muscles and followed
up to 8 weeks [Freund et al. 2000]. A significant
improvement was noted in pain VAS, functional
index, tenderness to palpation and interincisal
oral opening.
Anterior knee pain
Singer and colleagues injected 300500 units of
BoNT/A (Dysport) into vastus lateralis muscles
followed by a 12 week home exercise program to
strengthen vastus medialis in eight female
patients with chronic anterior knee pain of
Therapeutic Advances in Musculoskeletal Disease 2 (2)
108 http://tab.sagepub.com
T
a
b
l
e
1
.
S
u
m
m
a
r
y
o
f
s
t
u
d
i
e
s
o
f
b
o
t
u
l
i
n
u
m
t
o
x
i
n
i
n
o
s
t
e
o
a
r
t
i
c
u
l
a
r
p
a
i
n
-
e
f
f
i
c
a
c
y
o
u
t
c
o
m
e
s
.
S
t
u
d
y
:
a
u
t
h
o
r
;
n
u
m
b
e
r
o
f
p
a
t
i
e
n
t
s
R
C
T
v
e
r
s
u
s
o
p
e
n
-
l
a
b
e
l
I
n
t
e
r
v
e
n
t
i
o
n
a
n
d
c
o
m
p
a
r
i
s
o
n
M
e
a
n
a
g
e
i
n
y
e
a
r
s
(
S
D
)
/
m
a
l
e
/
f
e
m
a
l
e
M
e
a
n
p
a
i
n
d
u
r
a
t
i
o
n
i
n
m
o
n
t
h
s
(
S
D
)
P
r
i
m
a
r
y
o
u
t
c
o
m
e
M
a
i
n
r
e
s
u
l
t
e
f
f
i
c
a
c
y
T
e
n
n
i
s
e
l
b
o
w
W
o
n
g
e
t
a
l
.
2
0
0
5
6
0
p
a
t
i
e
n
t
s
R
C
T
,
d
o
u
b
l
e
-
b
l
i
n
d
,
3
m
o
n
t
h
s
S
i
n
g
l
e
i
n
j
e
c
t
i
o
n
o
f
6
0
u
n
i
t
s
o
f
B
o
N
T
/
A
(
D
y
s
p
o
r
t
)
v
e
r
s
u
s
s
a
l
i
n
e
p
l
a
c
e
b
o
i
n
S
Q
t
i
s
s
u
e
a
n
d
m
u
s
c
l
e
B
o
N
T
:
4
6
(
9
)
P
L
:
4
4
(
6
)
/
4
9
M
/
1
1
F
B
o
N
T
:
1
2
(
9
)
P
L
:
1
9
(
2
1
)
P
a
i
n
o
n
V
A
S
0
1
0
0
m
m
a
t
4
a
n
d
1
2
w
e
e
k
s
B
o
N
T
:
2
5
.
3
m
m
a
t
4
w
e
e
k
s
;
2
3
.
5
m
m
a
t
1
2
w
e
e
k
s
P
L
:
5
0
.
5
m
m
a
t
4
w
e
e
k
s
;
4
3
.
5
m
m
a
t
1
2
w
e
e
k
s
D
i
f
f
e
r
e
n
c
e
s
s
i
g
n
i
f
i
c
a
n
t
a
t
b
o
t
h
4
(
p
<
0
.
0
0
0
1
)
a
n
d
1
2
w
e
e
k
s
(
p
0
.
0
0
0
6
)
K
e
i
z
e
r
e
t
a
l
.
2
0
0
2
4
0
p
a
t
i
e
n
t
s
R
a
n
d
o
m
i
z
e
d
,
n
o
t
b
l
i
n
d
e
d
,
2
4
m
o
n
t
h
s
S
u
r
g
i
c
a
l
r
e
l
e
a
s
e
v
e
r
s
u
s
o
n
e
o
r
t
w
o
i
n
j
e
c
t
i
o
n
s
o
f
3
0
4
0
u
n
i
t
s
B
o
N
T
A
l
l
p
t
s
:
4
3
y
e
a
r
s
(
r
a
n
g
e
,
2
5
7
2
y
e
a
r
s
)
1
9
M
/
2
1
F
A
l
l
p
t
s
:
1
1
(
r
a
n
g
e
,
6
4
8
m
o
n
t
h
s
)
P
a
i
n
o
n
V
A
S
,
r
a
n
g
e
o
f
m
o
t
i
o
n
,
s
i
c
k
l
e
a
v
e
,
m
o
d
i
f
i
e
d
s
c
o
r
i
n
g
s
y
s
t
e
m
o
f
p
a
i
n
,
f
u
n
c
t
i
o
n
,
t
e
n
d
e
r
n
e
s
s
,
a
n
d
s
a
t
i
s
f
a
c
t
i
o
n
N
o
d
i
f
f
e
r
e
n
c
e
i
n
p
a
i
n
b
e
t
w
e
e
n
g
r
o
u
p
s
R
a
n
g
e
o
f
m
o
t
i
o
n
s
i
g
n
i
f
i
c
a
n
t
l
y
b
e
t
t
e
r
i
n
B
o
N
T
c
o
m
p
a
r
e
d
t
o
s
u
r
g
e
r
y
g
r
o
u
p
a
t
3
a
n
d
6
m
o
n
t
h
s
;
n
o
d
i
f
f
e
r
e
n
c
e
a
t
1
2
o
r
2
4
m
o
n
t
h
s
S
i
c
k
l
e
a
v
e
l
o
w
e
r
i
n
s
u
r
g
e
r
y
g
r
o
u
p
v
e
r
s
u
s
B
o
N
T
g
r
o
u
p
a
t
3
m
o
n
t
h
s
(
p
0
.
0
1
)
,
b
u
t
n
o
d
i
f
f
e
r
e
n
c
e
a
t
6
,
1
2
a
n
d
2
4
m
o
n
t
h
s
O
v
e
r
a
l
l
s
c
o
r
e
w
a
s
s
i
m
i
l
a
r
i
n
t
h
e
t
w
o
g
r
o
u
p
s
a
t
3
,
6
,
1
2
a
n
d
2
4
m
o
n
t
h
s
H
a
y
t
o
n
e
t
a
l
.
2
0
0
5
4
0
p
a
t
i
e
n
t
s
R
C
T
,
d
o
u
b
l
e
-
b
l
i
n
d
,
3
m
o
n
t
h
s
S
i
n
g
l
e
i
n
j
e
c
t
i
o
n
o
f
5
0
u
n
i
t
s
o
f
B
o
N
T
/
A
v
e
r
s
u
s
s
a
l
i
n
e
p
l
a
c
e
b
o
i
n
t
r
a
m
u
s
c
u
l
a
r
5
c
m
d
i
s
t
a
l
t
o
a
r
e
a
o
f
m
a
x
i
m
u
m
t
e
n
d
e
r
n
e
s
s
A
l
l
p
t
s
:
4
7
y
e
a
r
s
(
r
a
n
g
e
,
3
5
7
1
y
e
a
r
s
)
2
1
M
/
1
9
F
A
l
l
p
t
s
:
1
1
(
r
a
n
g
e
,
6
4
8
m
o
n
t
h
s
)
P
a
i
n
o
n
V
A
S
,
g
r
i
p
s
t
r
e
n
g
t
h
,
S
h
o
r
t
F
o
r
m
1
2
D
i
f
f
e
r
e
n
c
e
s
i
n
p
a
i
n
s
c
o
r
e
s
w
e
r
e
n
o
t
s
i
g
n
i
f
i
c
a
n
t
a
t
3
m
o
n
t
h
s
N
o
s
i
g
n
i
f
i
c
a
n
t
d
i
f
f
e
r
e
n
c
e
s
i
n
g
r
i
p
s
t
r
e
n
g
t
h
o
r
S
F
-
1
2
s
c
o
r
e
s
b
e
t
w
e
e
n
g
r
o
u
p
s
a
t
3
m
o
n
t
h
s
F
a
c
i
a
l
p
a
i
n
a
n
d
t
e
m
p
o
r
o
m
a
n
d
i
b
u
l
a
r
d
i
s
o
r
d
e
r
V
o
n
L
i
n
d
e
r
n
,
2
0
0
1
9
0
p
a
t
i
e
n
t
s
R
C
T
,
d
o
u
b
l
e
-
b
l
i
n
d
,
1
3
m
o
n
t
h
s
B
o
N
T
/
A
3
5
M
U
(
M
U
-
m
o
u
s
e
u
n
i
t
s
)
v
e
r
s
u
s
p
l
a
c
e
b
o
i
n
j
e
c
t
e
d
o
n
e
a
c
h
s
i
d
e
o
f
m
a
s
t
i
c
a
t
o
r
y
m
u
s
c
l
e
N
o
i
n
f
o
r
m
a
t
i
o
n
p
r
o
v
i
d
e
d
F
a
i
l
e
d
c
o
n
s
e
r
v
a
t
i
v
e
t
r
e
a
t
m
e
n
t
f
o
r
3
3
4
m
o
n
t
h
s
P
a
i
n
o
n
V
A
S
R
e
d
u
c
t
i
o
n
i
n
V
A
S
p
a
i
n
a
t
1
3
m
o
n
t
h
s
p
o
s
t
i
n
j
e
c
t
i
o
n
s
i
g
n
i
f
i
c
a
n
t
l
y
m
o
r
e
i
n
B
o
N
T
v
e
r
s
u
s
p
l
a
c
e
b
o
(
p
<
0
.
0
1
)
G
r
e
a
t
e
r
p
r
o
p
o
r
t
i
o
n
w
i
t
h
2
-
p
o
i
n
t
r
e
d
u
c
t
i
o
n
i
n
V
A
S
p
a
i
n
i
n
B
o
N
T
/
A
v
e
r
s
u
s
p
l
a
c
e
b
o
:
7
6
%
v
e
r
s
u
s
1
0
%
(
n
o
s
t
a
t
i
s
t
i
c
a
l
c
o
m
p
a
r
i
s
o
n
s
)
L
o
w
b
a
c
k
p
a
i
n
F
o
s
t
e
r
,
2
0
0
1
[
F
o
s
t
e
r
e
t
a
l
.
2
0
0
1
]
3
1
p
a
t
i
e
n
t
s
R
C
T
,
d
o
u
b
l
e
-
b
l
i
n
d
,
2
m
o
n
t
h
s
2
0
0
u
n
i
t
s
B
o
N
T
/
A
v
e
r
s
u
s
p
l
a
c
e
b
o
i
n
j
e
c
t
e
d
i
n
t
o
f
i
v
e
l
u
m
b
a
r
o
r
l
u
m
b
o
s
a
c
r
a
l
s
i
t
e
s
o
n
m
o
r
e
p
a
i
n
f
u
l
s
i
d
e
B
o
N
T
:
4
7
y
e
a
r
s
(
r
a
n
g
e
,
2
0
7
3
)
P
L
:
4
6
y
e
a
r
s
(
r
a
n
g
e
,
2
1
6
5
)
/
1
5
M
/
1
6
F
B
o
N
T
:
7
2
(
r
a
n
g
e
,
6
1
2
0
)
P
L
:
9
6
(
r
a
n
g
e
,
1
2
3
6
0
)
P
a
i
n
o
n
V
A
S
;
O
s
w
e
s
t
r
y
B
a
c
k
P
a
i
n
I
n
v
e
n
t
o
r
y
7
3
%
(
1
1
/
1
5
)
p
a
t
i
e
n
t
s
i
n
B
o
N
T
/
A
g
r
o
u
p
h
a
d
5
0
%
r
e
d
u
c
t
i
o
n
i
n
V
A
S
p
a
i
n
c
o
m
p
a
r
e
d
t
o
2
5
%
(
4
/
1
6
)
i
n
p
l
a
c
e
b
o
g
r
o
u
p
a
t
3
w
e
e
k
s
(
p
0
.
0
1
2
)
6
0
%
i
n
B
o
N
T
v
e
r
s
u
s
1
3
%
i
n
p
l
a
c
e
b
o
h
a
d
5
0
%
r
e
d
u
c
t
i
o
n
i
n
V
A
S
p
a
i
n
a
t
8
-
w
e
e
k
s
(
p
0
.
0
0
9
)
I
m
p
r
o
v
e
m
e
n
t
i
n
O
s
w
e
s
t
r
y
s
c
o
r
e
s
w
e
r
e
s
e
e
n
i
n
6
7
%
o
f
B
o
N
T
a
n
d
1
9
%
o
f
p
l
a
c
e
b
o
-
t
r
e
a
t
e
d
p
a
t
i
e
n
t
s
a
t
8
w
e
e
k
s
(
p
0
.
0
1
1
)
(
c
o
n
t
i
n
u
e
d
)
JA Singh
http://tab.sagepub.com 109
T
a
b
l
e
1
.
C
o
n
t
i
n
u
e
d
.
S
t
u
d
y
:
a
u
t
h
o
r
;
n
u
m
b
e
r
o
f
p
a
t
i
e
n
t
s
R
C
T
v
e
r
s
u
s
o
p
e
n
-
l
a
b
e
l
I
n
t
e
r
v
e
n
t
i
o
n
a
n
d
c
o
m
p
a
r
i
s
o
n
M
e
a
n
a
g
e
i
n
y
e
a
r
s
(
S
D
)
/
m
a
l
e
/
f
e
m
a
l
e
M
e
a
n
p
a
i
n
d
u
r
a
t
i
o
n
i
n
m
o
n
t
h
s
(
S
D
)
P
r
i
m
a
r
y
o
u
t
c
o
m
e
M
a
i
n
r
e
s
u
l
t
e
f
f
i
c
a
c
y
S
h
o
u
l
d
e
r
j
o
i
n
t
p
a
i
n
S
i
n
g
h
e
t
a
l
.
2
0
0
9
b
3
6
p
a
t
i
e
n
t
s
;
4
3
s
h
o
u
l
d
e
r
s
R
C
T
,
d
o
u
b
l
e
-
b
l
i
n
d
,
1
m
o
n
t
h
1
0
0
u
n
i
t
s
o
f
B
o
N
T
/
A
v
e
r
s
u
s
p
l
a
c
e
b
o
i
n
t
o
g
l
e
n
o
h
u
m
e
r
a
l
j
o
i
n
t
B
o
N
T
:
7
2
(
S
E
,
2
)
P
L
:
7
0
(
S
E
,
3
)
/
3
5
M
/
1
F
B
o
N
T
:
8
(
S
E
,
2
)
P
L
:
1
1
(
S
E
,
3
)
P
a
i
n
o
n
V
A
S
;
d
r
o
p
-
o
u
t
d
u
e
t
o
t
r
e
a
t
m
e
n
t
f
a
i
l
u
r
e
;
s
h
o
u
l
d
e
r
p
a
i
n
a
n
d
d
i
s
a
b
i
l
i
t
y
i
n
d
e
x
(
S
P
A
D
I
)
S
h
o
r
t
F
o
r
m
3
6
S
h
o
r
t
f
o
r
m
M
c
G
i
l
l
P
a
i
n
S
i
g
n
i
f
i
c
a
n
t
l
y
g
r
e
a
t
e
r
r
e
d
u
c
t
i
o
n
i
n
V
A
S
p
a
i
n
i
n
B
o
N
T
/
A
(
2
.
4
)
v
e
r
s
u
s
p
l
a
c
e
b
o
(
0
.
8
)
g
r
o
u
p
(
p
0
.
0
2
)
H
i
g
h
e
r
p
r
o
p
o
r
t
i
o
n
d
r
o
p
p
e
d
o
u
t
a
t
1
m
o
n
t
h
f
r
o
m
p
l
a
c
e
b
o
(
4
5
%
)
t
h
a
n
B
o
N
T
/
A
(
1
9
%
)
(
p
0
.
1
3
)
S
F
-
3
6
s
c
o
r
e
s
i
m
p
r
o
v
e
d
s
i
g
n
i
f
i
c
a
n
t
l
y
m
o
r
e
i
n
B
o
N
T
/
A
v
e
r
s
u
s
p
l
a
c
e
b
o
i
n
5
/
8
s
u
b
s
c
a
l
e
s
(
p
r
a
n
g
i
n
g
0
.
0
4
0
.
0
0
1
)
M
c
G
i
l
l
a
f
f
e
c
t
i
v
e
d
i
m
e
n
s
i
o
n
s
c
o
r
e
s
w
e
r
e
s
i
g
n
i
f
i
c
a
n
t
l
y
g
r
e
a
t
e
r
i
n
B
o
N
T
/
A
v
e
r
s
u
s
p
l
a
-
c
e
b
o
g
r
o
u
p
(
p
0
.
0
4
7
)
T
r
e
n
d
t
o
w
a
r
d
s
s
i
g
n
i
f
i
c
a
n
c
e
i
n
S
P
A
D
I
d
i
s
a
b
i
l
i
t
y
s
c
o
r
e
s
(
p
0
.
0
8
3
)
N
o
s
i
g
n
i
f
i
c
a
n
t
d
i
f
f
e
r
e
n
c
e
s
i
n
a
c
t
i
v
e
f
l
e
x
i
o
n
,
a
c
t
i
v
e
a
b
d
u
c
t
i
o
n
,
S
P
A
D
I
p
a
i
n
a
n
d
t
o
t
a
l
a
n
d
M
c
G
i
l
l
s
e
n
s
o
r
y
a
n
d
t
o
t
a
l
s
c
o
r
e
s
H
a
n
d
p
a
i
n
a
n
d
c
a
r
p
a
l
t
u
n
n
e
l
s
y
n
d
r
o
m
e
B
r
e
u
e
r
e
t
a
l
.
2
0
0
6
2
0
p
a
t
i
e
n
t
s
R
C
T
,
d
o
u
b
l
e
-
b
l
i
n
d
,
3
m
o
n
t
h
s
2
5
0
0
u
n
i
t
s
B
o
N
T
/
B
v
e
r
s
u
s
p
l
a
c
e
b
o
i
n
j
e
c
t
e
d
i
n
t
o
t
h
r
e
e
h
y
p
o
t
h
e
n
a
r
m
u
s
c
l
e
s
i
n
c
a
r
p
a
l
t
u
n
n
e
l
N
o
i
n
f
o
r
m
a
t
i
o
n
p
r
o
v
i
d
e
d
N
o
i
n
f
o
r
m
a
t
i
o
n
p
r
o
v
i
d
e
d
P
a
i
n
o
n
N
u
m
e
r
i
c
R
a
t
i
n
g
S
c
a
l
e
(
N
R
S
)
W
e
s
t
H
a
v
e
n
-
Y
a
l
e
M
u
l
t
i
d
i
m
e
n
s
i
o
n
a
l
P
a
i
n
I
n
v
e
n
t
o
r
y
(
W
H
Y
M
P
I
)
P
a
i
n
s
c
o
r
e
s
,
p
a
i
n
-
r
e
l
a
t
e
d
s
l
e
e
p
d
i
s
t
u
r
b
a
n
c
e
s
,
W
H
Y
M
P
I
s
c
o
r
e
s
i
m
p
r
o
v
e
d
i
n
b
o
t
h
g
r
o
u
p
s
a
t
f
o
l
l
o
w
-
u
p
,
b
u
t
d
i
d
n
t
s
i
g
n
i
f
i
c
a
n
t
l
y
d
i
f
f
e
r
b
e
t
w
e
e
n
g
r
o
u
p
s
A
t
6
w
e
e
k
s
,
8
/
1
0
(
8
0
%
)
B
o
N
T
p
a
t
i
e
n
t
s
v
e
r
s
u
s
6
/
9
(
6
7
%
)
h
a
d
c
l
i
n
i
c
a
l
l
y
m
e
a
n
i
n
g
f
u
l
r
e
d
u
c
t
i
o
n
o
f
p
a
i
n
V
A
S
(
3
0
%
o
r
2
p
o
i
n
t
r
e
d
u
c
t
i
o
n
)
.
S
i
m
i
l
a
r
r
e
d
u
c
t
i
o
n
s
a
t
1
3
w
e
e
k
s
w
e
r
e
2
/
7
(
2
9
%
)
B
o
N
T
v
e
r
s
u
s
4
/
9
(
4
4
%
)
o
f
p
l
a
c
e
b
o
.
P
l
a
n
t
a
r
f
a
s
c
i
i
t
i
s
B
a
b
c
o
c
k
e
t
a
l
.
2
0
0
5
2
7
p
a
t
i
e
n
t
s
;
4
3
f
e
e
t
R
C
T
,
d
o
u
b
l
e
-
b
l
i
n
d
,
2
m
o
n
t
h
s
7
0
u
n
i
t
s
B
o
N
T
/
A
(
4
0
u
n
i
t
s
o
n
m
e
d
i
a
l
a
s
p
e
c
t
o
f
t
h
e
h
e
e
l
a
n
d
3
0
u
n
i
t
s
i
n
t
h
e
f
o
o
t
a
r
c
h
)
v
e
r
s
u
s
p
l
a
c
e
b
o
A
l
l
:
m
e
d
i
a
n
a
g
e
,
4
4
(
r
a
n
g
e
,
2
1
6
5
)
9
M
/
1
8
F
N
o
i
n
f
o
r
m
a
t
i
o
n
p
r
o
v
i
d
e
d
P
a
i
n
V
A
S
,
0
1
0
c
m
P
r
e
s
s
u
r
e
a
l
g
o
m
e
t
r
y
r
e
s
p
o
n
s
e
M
a
r
y
l
a
n
d
F
o
o
t
S
c
o
r
e
(
0
1
0
0
p
o
i
n
t
s
)
P
a
i
n
r
e
l
i
e
f
V
A
S
,
0
1
0
c
m
A
t
3
w
e
e
k
s
,
i
m
p
r
o
v
e
m
e
n
t
s
w
e
r
e
s
i
g
n
i
f
i
c
a
n
t
l
y
h
i
g
h
e
r
f
o
r
B
o
N
T
v
e
r
s
u
s
p
l
a
c
e
b
o
:
P
a
i
n
V
A
S
,
2
.
7
(
3
9
%
d
e
c
r
e
a
s
e
)
v
e
r
s
u
s
4
.
7
(
p
<
0
.
0
0
4
)
;
M
a
r
y
l
a
n
d
F
o
o
t
s
c
o
r
e
,
7
2
(
3
4
%
)
v
e
r
s
u
s
4
9
(
p
0
.
0
0
1
)
;
p
r
e
s
s
u
r
e
a
l
g
o
m
e
t
r
y
,
2
.
7
(
4
0
%
i
n
c
r
e
a
s
e
)
v
e
r
s
u
s
1
.
8
(
p
0
.
0
0
3
)
;
a
n
d
p
a
i
n
i
m
p
r
o
v
e
m
e
n
t
s
c
a
l
e
,
4
.
8
v
e
r
s
u
s
0
.
6
(
p
<
0
.
0
0
5
)
A
t
8
w
e
e
k
s
,
i
m
p
r
o
v
e
m
e
n
t
s
w
e
r
e
s
i
g
n
i
f
i
c
a
n
t
l
y
h
i
g
h
e
r
f
o
r
B
o
N
T
v
e
r
s
u
s
p
l
a
c
e
b
o
:
P
a
i
n
V
A
S
,
1
.
6
(
5
6
%
d
e
c
r
e
a
s
e
)
v
e
r
s
u
s
4
.
4
(
p
<
0
.
0
0
5
)
;
M
a
r
y
l
a
n
d
F
o
o
t
s
c
o
r
e
,
8
1
(
4
7
%
)
v
e
r
s
u
s
5
4
(
p
0
.
0
0
1
)
;
p
r
e
s
s
u
r
e
a
l
g
o
m
e
t
r
y
,
2
.
8
(
5
6
%
i
n
c
r
e
a
s
e
)
v
e
r
s
u
s
1
.
8
(
p
0
.
0
0
3
)
;
a
n
d
p
a
i
n
i
m
p
r
o
v
e
m
e
n
t
s
c
a
l
e
,
5
.
0
v
e
r
s
u
s
1
.
2
(
p
<
0
.
0
0
5
)
B
o
N
T
,
b
o
t
u
l
i
n
u
m
t
o
x
i
n
;
B
o
N
T
/
A
,
B
o
t
u
l
i
n
u
m
t
o
x
i
n
t
y
p
e
A
;
B
o
N
T
/
B
,
B
o
t
u
l
i
n
u
m
t
o
x
i
n
t
y
p
e
B
;
N
R
S
,
N
u
m
e
r
i
c
R
a
t
i
n
g
S
c
a
l
e
;
P
L
,
p
l
a
c
e
b
o
;
p
t
s
,
p
a
t
i
e
n
t
s
;
R
C
T
,
r
a
n
d
o
m
i
z
e
d
c
o
n
t
r
o
l
l
e
d
t
r
i
a
l
;
S
E
,
s
t
a
n
d
a
r
d
e
r
r
o
r
;
S
F
-
1
2
,
S
h
o
r
t
F
o
r
m
1
2
;
S
P
A
D
I
,
s
h
o
u
l
d
e
r
p
a
i
n
a
n
d
d
i
s
a
b
i
l
i
t
y
i
n
d
e
x
;
S
Q
,
s
u
b
c
u
t
a
n
e
o
u
s
;
V
A
S
,
V
i
s
u
a
l
A
n
a
l
o
g
S
c
a
l
e
;
W
H
Y
M
P
I
,
W
e
s
t
H
a
v
e
n
-
Y
a
l
e
M
u
l
t
i
d
i
m
e
n
s
i
o
n
a
l
P
a
i
n
I
n
v
e
n
t
o
r
y
.
Therapeutic Advances in Musculoskeletal Disease 2 (2)
110 http://tab.sagepub.com
T
a
b
l
e
2
.
S
a
f
e
t
y
o
u
t
c
o
m
e
s
f
r
o
m
r
a
n
d
o
m
i
z
e
d
s
t
u
d
i
e
s
o
f
b
o
t
u
l
i
n
u
m
t
o
x
i
n
u
s
e
i
n
o
s
t
e
o
a
r
t
i
c
u
l
a
r
p
a
i
n
.
S
t
u
d
y
:
R
e
f
e
r
e
n
c
e
,
n
u
m
b
e
r
o
f
p
a
t
i
e
n
t
s
R
C
T
v
e
r
s
u
s
o
p
e
n
l
a
b
e
l
I
n
t
e
r
v
e
n
t
i
o
n
a
n
d
c
o
m
p
a
r
i
s
o
n
A
l
l
a
d
v
e
r
s
e
e
v
e
n
t
s
S
e
r
i
o
u
s
a
d
v
e
r
s
e
e
v
e
n
t
s
W
e
a
k
n
e
s
s
S
y
s
t
e
m
a
t
i
c
a
d
v
e
r
s
e
e
v
e
n
t
s
O
t
h
e
r
s
:
p
a
i
n
,
r
e
d
n
e
s
s
e
t
c
.
T
e
n
n
i
s
E
l
b
o
w
W
o
n
g
e
t
a
l
.
2
0
0
5
6
0
p
a
t
i
e
n
t
s
R
C
T
,
d
o
u
b
l
e
-
b
l
i
n
d
6
0
u
n
i
t
s
o
f
B
o
N
T
/
A
v
e
r
s
u
s
s
a
l
i
n
e
p
l
a
c
e
b
o
i
n
S
Q
t
i
s
s
u
e
a
n
d
m
u
s
c
l
e
B
o
N
T
:
1
9
/
3
0
P
L
:
9
/
3
0
W
e
a
k
n
e
s
s
i
n
f
i
n
g
e
r
e
x
t
e
n
s
i
o
n
:
B
o
N
T
1
0
/
3
0
,
P
L
6
/
3
0
a
t
4
w
e
e
k
s
;
B
o
N
T
2
/
3
0
,
P
L
1
/
3
0
a
t
1
2
w
e
e
k
s
P
a
r
e
s
i
s
o
f
d
i
g
i
t
s
:
B
o
N
T
4
/
3
0
,
P
L
0
/
3
0
a
t
4
w
e
e
k
s
;
B
o
N
T
1
/
3
0
,
P
L
0
/
3
0
a
t
1
2
w
e
e
k
s
N
a
u
s
e
a
:
B
o
N
T
0
/
3
0
,
P
L
1
/
3
0
P
a
i
n
:
B
o
N
T
2
/
3
0
,
P
L
1
/
3
0
K
e
i
z
e
r
e
t
a
l
.
2
0
0
2
4
0
p
a
t
i
e
n
t
s
R
a
n
d
o
m
i
z
e
d
,
n
o
t
b
l
i
n
d
e
d
S
u
r
g
e
r
y
v
e
r
s
u
s
s
i
n
g
l
e
i
n
j
e
c
t
i
o
n
o
f
B
o
N
T
/
A
N
o
d
a
t
a
p
r
o
v
i
d
e
d
o
n
a
d
v
e
r
s
e
e
v
e
n
t
s
H
a
y
t
o
n
e
t
a
l
.
2
0
0
5
4
0
p
a
t
i
e
n
t
s
R
C
T
,
d
o
u
b
l
e
-
b
l
i
n
d
5
0
u
n
i
t
s
o
f
B
o
N
T
/
A
v
e
r
s
u
s
s
a
l
i
n
e
p
l
a
c
e
b
o
i
n
t
r
a
m
u
s
c
u
l
a
r
E
x
t
e
n
s
o
r
l
a
g
o
f
l
o
n
g
f
i
n
g
e
r
B
o
N
T
:
1
2
/
1
8
P
L
:
0
/
1
9
F
a
c
i
a
l
p
a
i
n
a
n
d
t
e
m
p
o
r
o
m
a
n
d
i
b
u
l
a
r
d
i
s
o
r
d
e
r
V
o
n
L
i
n
d
e
r
n
,
2
0
0
1
9
0
p
a
t
i
e
n
t
s
R
C
T
,
s
i
n
g
l
e
-
b
l
i
n
d
7
0
u
n
i
t
s
o
f
B
o
N
T
/
A
v
e
r
s
u
s
s
a
l
i
n
e
p
l
a
c
e
b
o
i
n
t
r
a
m
u
s
c
u
l
a
r
S
w
a
l
l
o
w
i
n
g
d
i
f
f
i
c
u
l
t
y
o
r
t
e
m
p
o
r
a
r
y
p
a
r
a
l
y
s
i
s
o
f
f
a
c
i
a
l
e
x
p
r
e
s
s
i
o
n
m
u
s
c
l
e
:
B
o
N
T
:
1
/
6
0
P
L
:
0
/
/
3
0
(
c
o
n
t
i
n
u
e
d
)
JA Singh
http://tab.sagepub.com 111
T
a
b
l
e
2
.
C
o
n
t
i
n
u
e
d
.
S
t
u
d
y
:
R
e
f
e
r
e
n
c
e
,
n
u
m
b
e
r
o
f
p
a
t
i
e
n
t
s
R
C
T
v
e
r
s
u
s
o
p
e
n
l
a
b
e
l
I
n
t
e
r
v
e
n
t
i
o
n
a
n
d
c
o
m
p
a
r
i
s
o
n
A
l
l
a
d
v
e
r
s
e
e
v
e
n
t
s
S
e
r
i
o
u
s
a
d
v
e
r
s
e
e
v
e
n
t
s
W
e
a
k
n
e
s
s
S
y
s
t
e
m
a
t
i
c
a
d
v
e
r
s
e
e
v
e
n
t
s
O
t
h
e
r
s
:
p
a
i
n
,
r
e
d
n
e
s
s
e
t
c
.
L
o
w
b
a
c
k
p
a
i
n
F
o
s
t
e
r
e
t
a
l
.
2
0
0
1
3
1
p
a
t
i
e
n
t
s
R
C
T
,
d
o
u
b
l
e
-
b
l
i
n
d
2
0
0
u
n
i
t
s
B
o
N
T
/
A
v
e
r
s
u
s
p
l
a
c
e
b
o
i
n
j
e
c
t
e
d
i
n
t
o
f
i
v
e
l
u
m
b
a
r
o
r
l
u
m
b
o
s
a
c
r
a
l
s
i
t
e
s
o
n
m
o
r
e
p
a
i
n
f
u
l
s
i
d
e
W
o
r
s
e
n
i
n
g
o
f
p
a
i
n
:
B
o
N
T
:
0
/
1
5
P
L
:
2
/
1
6
S
h
o
u
l
d
e
r
j
o
i
n
t
p
a
i
n
S
i
n
g
h
e
t
a
l
.
2
0
0
9
b
3
6
p
a
t
i
e
n
t
s
;
4
3
s
h
o
u
l
d
e
r
s
R
C
T
,
d
o
u
b
l
e
-
b
l
i
n
d
,
1
m
o
n
t
h
1
0
0
u
n
i
t
s
o
f
B
o
N
T
/
A
v
e
r
s
u
s
p
l
a
c
e
b
o
i
n
t
o
g
l
e
n
o
h
u
m
e
r
a
l
j
o
i
n
t
B
o
N
T
:
5
0
A
E
s
P
L
:
4
6
A
E
s
B
o
N
T
:
3
S
A
E
s
P
L
:
9
S
A
E
s
B
o
N
T
:
1
P
L
:
1
D
r
y
m
o
u
t
h
B
o
N
T
:
5
P
L
:
3
C
o
u
g
h
B
o
N
T
:
4
P
L
:
3
D
i
z
z
i
n
e
s
s
B
o
N
T
:
3
P
L
:
4
P
a
i
n
i
n
s
t
u
d
y
j
o
i
n
t
B
o
N
T
:
1
P
L
:
2
H
a
n
d
p
a
i
n
a
n
d
c
a
r
p
a
l
t
u
n
n
e
l
s
y
n
d
r
o
m
e
B
r
e
u
e
r
e
t
a
l
.
2
0
0
6
2
0
p
a
t
i
e
n
t
s
R
C
T
,
d
o
u
b
l
e
-
b
l
i
n
d
,
3
m
o
n
t
h
s
2
5
0
0
u
n
i
t
s
B
o
N
T
/
B
v
e
r
s
u
s
p
l
a
c
e
b
o
i
n
j
e
c
t
e
d
i
n
t
o
t
h
r
e
e
h
y
p
o
t
h
e
n
a
r
m
u
s
c
l
e
s
i
n
c
a
r
p
a
l
t
u
n
n
e
l
F
i
r
s
t
t
w
o
p
a
t
i
e
n
t
s
w
i
t
h
w
e
a
k
n
e
s
s
o
f
f
i
n
g
e
r
m
u
s
c
l
e
s
P
l
a
n
t
a
r
f
a
s
c
i
i
t
i
s
B
a
b
c
o
c
k
e
t
a
l
.
2
0
0
5
[
2
7
p
a
t
i
e
n
t
s
;
4
3
f
e
e
t
R
C
T
,
d
o
u
b
l
e
-
b
l
i
n
d
,
2
m
o
n
t
h
s
7
0
u
n
i
t
s
B
o
N
T
/
A
v
e
r
s
u
s
p
l
a
c
e
b
o
(
4
0
u
n
i
t
s
o
n
m
e
d
i
a
l
a
s
p
e
c
t
o
f
t
h
e
h
e
e
l
a
n
d
3
0
u
n
i
t
s
i
n
t
h
e
f
o
o
t
a
r
c
h
N
o
c
o
m
p
l
i
c
a
t
i
o
n
s
i
n
p
a
t
i
e
n
t
s
w
h
o
f
o
l
l
o
w
e
d
u
p
B
o
N
T
,
b
o
t
u
l
i
n
u
m
t
o
x
i
n
;
B
o
N
T
/
A
,
b
o
t
u
l
i
n
u
m
t
o
x
i
n
t
y
p
e
A
;
P
L
,
p
l
a
c
e
b
o
;
p
t
s
,
p
a
t
i
e
n
t
s
;
R
C
T
,
r
a
n
d
o
m
i
z
e
d
c
o
n
t
r
o
l
l
e
d
t
r
i
a
l
;
A
E
s
,
a
d
v
e
r
s
e
e
v
e
n
t
s
;
S
A
E
s
,
s
e
r
i
o
u
s
a
d
v
e
r
s
e
e
v
e
n
t
s
;
S
Q
,
s
u
b
c
u
t
a
n
e
o
u
s
.
Therapeutic Advances in Musculoskeletal Disease 2 (2)
112 http://tab.sagepub.com
longer than 6 months that had failed conservative
management [Singer et al. 2006]. Patients
reported decreased knee pain, increased function
and had an improvement in the time taken to
ascend and descend a flight of 11 stairs from 12
to 10 seconds; improvements that were main-
tained at 24 weeks.
Low back pain
Ney and colleagues reported the results of
injection of 200500 units of BoNT/A intra-
muscularly from L2 to S1 in 60 patients with
chronic low back pain of 9-year mean disease
duration in an open-label prospective study
[Ney et al. 2006]. Response as defined by the
occurrence of two of three of the following crite-
ria: 50% improvement in pain VAS, 2 grade
improvement in pain and functional subsets of
Oswestry Low Back Pain Questionnaire, and
30% improvement in number of pain days
from baseline. At 2 months 58% patients
responded, with 17% still showed improvement
at 4 months of follow-up.
Plantar fasciitis
Placzek and colleagues reported 1 year follow-up
of a case series of nine patients with chronic plan-
tar fasciitis, who were injected with 200 units of
BoNT/A (Dysport). Statistically significant pain
relief began 2 weeks after the injection (pain
scale, 010, 4.21.9, p 0.012) and persisted
until 52 weeks (pain scale, 010, 4.20.4,
p 0.043) [Placzek et al. 2005].
Randomized controlled trials of botulinum
toxin in osteoarticular pain
Tennis elbow
In a study by Hayton and colleagues 40 patients
with refractory painful tennis elbow with pain
lasting more than 6 months, who had failed treat-
ment with one or more corticosteroid injections
and a full course of physiotherapy were rando-
mized to 50 units of BoNT/A (Allergan) or
normal saline placebo (2 ml) 5 cm distal to the
area of maximal tenderness at the lateral epicon-
dyle (Tables 1 and 2) [Hayton et al. 2005]. There
were no statistically significant differences
between BoNT and placebo groups at 3 months
after the injection in pain, grip strength or quality
of life measured by Short-Form 12 physical and
mental component summary scores.
In another study by Wong and colleagues (Tables 1
and 2), 60 patients with painful tennis elbow
for 3 months or longer were randomized to
either a single injection of 60 units of BoNT/A
(Dysport; Ipsen) or placebo and followed for 12
weeks in a double-blinded multicenter study
[Wong et al. 2005]. Patients were treatment-
na ve with no prior local acupuncture therapy
for their tennis elbow. Pain on a VAS
(0100 mm) scale decreased significantly more
in the active treatment group (65.5 at baseline
to 25.3 at week 4 and 23.5 at week 12) than pla-
cebo (66.2 at baseline to 50.5 at week 4 and 43.5
at week 12). The differences between groups
were statistically significant at both week 4
(p <0.001) and week 12 (p 0.006). Although
four patients in the botulinum group had paresis
of the fingers at 4 weeks (in one patient it
persisted to week 12) compared to none in the
placebo group, the grip strength was similar in
both groups at the two time points. A small
sample and short follow-up period are the limita-
tions of the study. These two studies differed in
patient population (all patients versus those with
refractory disease), duration of disease (>3
months versus >6 months), site of injection
(1 cm versus 5cm from the lateral epicondyle)
and the preparation used [60 units of Dysport
(Ipsen Pharmaceuticals) versus 50 units of
Botox (Allergan Pharmaceuticals)].
Another randomized study (Tables 1 and 2) com-
pared one or two injections of 3040 units of
BoNT/A (Allergan) with the surgical release of
the extensor origin of the extensor carpi radialis
brevis tendon in 40 patients with refractory
chronic painful tennis elbow (average duration
of symptoms 10 months) [Keizer et al. 2002].
They found no differences between the groups
with regards to pain and grip strength up to
2 years of follow-up, while minor differences
were noted at shorter follow-up periods. A limi-
tation of the study was lack of description of out-
comes, no a priori designation of outcomes as
primary versus secondary and use of nonvalidated
outcomes.
Facial pain and temporomandibular disorder
Temporomandibular disorder is a group of
pathologic conditions affecting the temporoman-
dibular joint, its associated structures and its
functions. In a single-blinded, randomized
study of 90 patients with chronic facial pain
caused by hyperactivity of masticatory muscles,
who had failed conservative treatment, received
JA Singh
http://tab.sagepub.com 113
intramuscular injections of 35 mouse units of
BoNT/A (Allergan; n 60) or placebo (n 30)
on each side of the masticatory muscle
(Tables 1 and 2) [Von Lindern et al. 2003].
A significantly greater reduction of 010 VAS
pain was noted in the botulinum toxin (3.2
units) versus placebo group (0.4 units) (p <0.01;
at follow-up between 1 and 3 months). A greater
proportion of patients in BoNT/A compared to
the placebo group had 2-point improvement in
VAS pain during the follow-up (Table 1). This
study has many limitations: blinding was not
described (patient or physician blinded single-
blind), the outcome measurement time-point
was not described, and the study had a very
short follow-up duration.
Low back pain
Foster and colleagues compared 200 units of
BoNT/A (Allergan) injected intramuscular para-
vertebrally from L1-5/L2-S1 (n 15) to placebo
(n 16) in 31 patients with chronic back pain of
6 month duration (Table 1) [Foster et al. 2001].
Pain relief exceeding 50% on VAS was signifi-
cantly higher in Botox versus placebo group,
respectively: 73% versus 25% at 3 weeks, and
60% versus 13% at 8 weeks (Table 1). The
Oswestry Low Back Pain Questionnaire score
improved in significantly more patients in Botox
versus placebo group. A small sample size is a
limitation of this study.
Refractory shoulder joint pain
Singh and colleagues injected 100 units of
BoNT/A (Allergan Pharmaceuticals) into gleno-
humeral (shoulder) joints of patients with
osteoarthritis or rheumatoid arthritis related
refractory, chronic shoulder joint pain due to
osteoarthritis or rheumatoid arthritis, who had
all failed conservative management with intra-
articular corticosteroids and oral medications
(Tables 1 and 2) [Singh et al. 2009b].
Hand pain and carpal tunnel syndrome
Breuer and colleagues randomized 20 patients
with carpal tunnel syndrome with hand pain to
receive electromyographically-guided placebo or
botulinum toxin type B injections in three
hypothenar muscles anatomically attached to
the carpal tunnel (Tables 1 and 2) [Breuer et al.
2006]. During the 13-week trial, significant
decrease in pain outcomes and improvement in
function were noted in both placebo and the
BoNT/A groups compared to the baseline, but
there were no significant differences between
the two groups. A small sample size, unblinding
of the first two patients and variation in the
BoNT/A dose during the trial were the limita-
tions of this study.
Heel pain and plantar fasciitis
Babcock and colleagues compared 70 units of
BoNT/A injected into plantar fascia compared
to a placebo injection in 27 patients (43 feet)
with chronic refractory plantar fasciitis for 6
months, that had failed all conservative strategies
except surgery or extracorporeal shock therapy
(Tables 1 and 2) [Babcock et al. 2005].
Compared to the placebo group, botulinum
group improved significantly more pain relief on
a VAS (4.75 versus 0.6 at 3 weeks and 4.95 versus
1.2 at 8 weeks, p <0.005 for both; 010 cm
scale), significantly lower VAS pain, and signifi-
cantly better foot function as assessed by the
Maryland Foot Score and less muscle tenderness
at plantar fascia insertion as assessed by pressure
algometry response at both 3 and 8 weeks
follow-up.
Summary and conclusions
In this paper, studies of use of BoNT for osteoar-
ticular pain are reviewed. Preclinical laboratory
evidence and clinical evidence emerging from
use of BoNT for other applications suggests an
independent antinociceptive mechanism of
action. While there are several osteoarticular con-
ditions for which BoNT had been studied in an
RCT compared to placebo, for most conditions
there was a single RCT. These studies had several
limitations. Most studies were single center, had
a small sample size, short follow-up and in some
cases, nonstandardized injection techniques.
Observation of larger effect size in uncontrolled
studies (retrospective and prospective) as com-
pared to controlled trials indicates bias and
placebo effect, as reported previously for other
conditions. The evidence for an antinociceptive
action of BoNT in osteoarticular pain is
growing. Larger multicenter studies of longer
duration that test various doses, regimens and
routes of administration of BoNT are needed
to better define its role in management of
osteoarticular pain.
Conflict of interest statement
Grant Support: Supported by NIH CTSA Award
1 KL2 RR024151-01 (Mayo Clinic Center for
Clinical and Translational Research).
Therapeutic Advances in Musculoskeletal Disease 2 (2)
114 http://tab.sagepub.com
References
Ahmed, M., Bjurholm, A., Schultzberg, M.,
Theodorsson, E. and Kreicbergs, A. (1995) Increased
levels of substance P and calcitonin gene-related
peptide in rat adjuvant arthritis. A combined
immunohistochemical and radioimmunoassay
analysis. Arthritis Rheum 38: 699709.
Aoki, K.R. (2003) Evidence for antinociceptive activity
of botulinum toxin type A in pain management.
Headache 43(Suppl 1): S915.
Arnon, S.S., Schechter, R., Inglesby, T.V., Henderson,
D.A., Bartlett, J.G., Ascher, M.S. et al. (2001)
Botulinum toxin as a biological weapon: medical and
public health management. JAMA 285: 10591070.
Babcock, M.S., Foster, L., Pasquina, P. and Jabbari, B.
(2005) Treatment of pain attributed to plantar fasciitis
with botulinum toxin A: a short-term, randomized,
placebo-controlled, double-blind study. Am J Phys
Med Rehabil 84: 649654.
Bellamy, N., Campbell, J., Robinson, V., Gee, T.,
Bourne, R. and Wells, G. (2006a) Intraarticular
corticosteroid for treatment of osteoarthritis of the
knee. Cochrane Database Syst Rev CD005328.
Bellamy, N., Campbell, J., Robinson, V., Gee, T.,
Bourne, R. and Wells, G. (2006b) Viscosupplementation
for the treatment of osteoarthritis of the knee. Cochrane
Database Syst Rev CD005321.
Birklein, F. and Schmelz, M. (2008) Neuropeptides,
Neurogenic inflammation and complex regional pain
syndrome (CRPS). Neurosci Lett 437: 199202.
Bjork, M.A., Thyberg, I.S., Skogh, T. and Gerdle,
B.U. (2007) Hand function and activity limitation
according to health assessment questionnaire in
patients with rheumatoid arthritis and healthy refer-
ents: 5-year followup of predictors of activity limitation
(the Swedish Tira Project). J Rheumatol 34: 296302.
Blersch, W., Schulte-Mattler, W.J., Przywara, S., May,
A., Bigalke, H. and Wohlfarth, K. (2002) Botulinum
toxin A and the cutaneous nociception in humans: a
prospective, double-blind, placebo-controlled, rando-
mized study. J Neurol Sci 205: 5963.
Breivik, H., Collett, B., Ventafridda, V., Cohen, R. and
Gallacher, D. (2006) Survey of chronic pain in europe:
prevalence, impact on daily life, and treatment. Eur J
Pain 10: 287333.
Breuer, B., Sperber, K., Wallenstein, S., Kiprovski, K.,
Calapa, A., Snow, B. et al. (2006) Clinically significant
placebo analgesic response in a pilot trial of botulinum
B in patients with hand pain and carpal tunnel syn-
drome. Pain Med 7: 1624.
Centers for Disease Control and Prevention (CDC)
(2009) Prevalence and most common causes of
disability among adultsUnited States, 2005.
MMWR Morb Mortal Wkly Rep 58: 421426.
Cuevas-Trisan, R.L. and Cruz-Jimenez, M. (2006)
The use of botulinum toxin in physical medicine and
rehabilitation. Bol Asoc Med P R 98: 4255.
Cui, M., Khanijou, S., Rubino, J. and Aoki, K.R.
(2004) Subcutaneous administration of botulinum
toxin A reduces formalin-induced pain. Pain
107: 125133.
Devillier, P., Weill, B., Renoux, M., Menkes, C. and
Pradelles, P. (1986) Elevated levels of tachykinin-like
immunoreactivity in joint fluids from patients with
rheumatic inflammatory diseases. N Engl J Med
314: 1323.
Durham, P.L., Cady, R. and Cady, R. (2004)
Regulation of calcitonin gene-related peptide secretion
from trigeminal nerve cells by botulinum toxin type A:
implications for migraine therapy. Headache
44: 3542, discussion 4233.
Dykstra, D., Stuckey, M.W., Schimpff, S.N., Singh,
J.A. and Mahowald, M.L. (2007) The effects of
intra-articular botulinum toxin on sacroiliac, cervical/
lumbar facet and sterno-calvicular joint pain and C-2
root and lumbar disc pain: a case series of 11 patients.
The Pain Clinic 19: 2732.
Feldmann, M. and Maini, S.R. (2008) Role of
cytokines in rheumatoid arthritis: an education in
pathophysiology and therapeutics. Immunol Rev
223: 719.
Foster, L., Clapp, L., Erickson, M. and Jabbari, B.
(2001) Botulinum toxin A and chronic low back pain:
a randomized, double-blind study. Neurology
56: 12901293.
Freund, B. and Schwartz, M. (2003) Temporal
relationship of muscle weakness and pain reduction
in subjects treated with botulinum toxin A. J Pain
4: 159165.
Freund, B., Schwartz, M. and Symington, J.M. (2000)
Botulinum toxin: new treatment for temporomandib-
ular disorders. Br J Oral Maxillofac Surg 38: 466471.
Ge, Z., Hu, Y., Heng, B.C., Yang, Z., Ouyang, H.,
Lee, E.H. et al. (2006) Osteoarthritis and therapy.
Arthritis Rheum 55: 493500.
Gobel, H., Heinze, A., Heinze-Kuhn, K. and Jost, W.
(2001) Evidence based medicine: botulinum toxin A in
migraine and tension type headache. J Neurol
248(Suppl): 3438.
Green, S., Buchbinder, R., Glazier, R. and Forbes, A.
(2003) Interventions for shoulder pain. Cochrane
Database Syst Rev.
Hayton, M.J., Santini, A.J., Hughes, P.J., Frostick,
S.P., Trail, I.A. and Stanley, J.K. (2005) Botulinum
toxin injection in the treatment of tennis elbow. A
double-blind, randomized, controlled, pilot study.
J Bone Joint Surg Am 87: 503507.
Ho, K.Y. and Tan, K.H. (2007) Botulinum toxin A
for myofascial trigger point injection: a qualitative
systematic review. Eur J Pain 11: 519527.
Huijnen, B., Van Der Horst, F., Van Amelsvoort, L.,
Wesseling, G., Lansbergen, M., Aarts, P. et al. (2006)
Dyspnea in elderly family practice patients.
JA Singh
http://tab.sagepub.com 115
Occurrence, severity, quality of life and mortality
over an 8-year period. Fam Pract 23: 3439.
Hunter, D.J., McDougall, J.J. and Keefe, F.J. (2009)
The symptoms of osteoarthritis and the genesis of
pain. Med Clin North Am 93: 83100, xi.
Jamtvedt, G., Dahm, K.T., Christie, A., Moe, R.H.,
Haavardsholm, E., Holm, I. et al. (2008) Physical
therapy interventions for patients with osteoarthritis
of the knee: an overview of systematic reviews.
Phys Ther 88: 123136.
Jankovic, J. and Schwartz, K. (1990) Botulinum
toxin injections for cervical dystonia. Neurology
40: 277280.
Jones, S.L. (1991) Descending noradrenergic
influences on pain. Prog Brain Res 88: 381394.
Kar, S., Gibson, S.J., Rees, R.G., Jura, W.G.,
Brewerton, D.A. and Polak, J.M. (1991) Increased
calcitonin gene-related peptide (CGRP), substance P,
and enkephalin immunoreactivities in dorsal spinal
cord and loss of CGRP-immunoreactive motoneurons
in arthritic rats depend on intact peripheral nerve
supply. J Mol Neurosci 3: 718.
Keizer, S.B., Rutten, H.P., Pilot, P., Morre, H.H., V
Os, J.J. and Verburg, A.D. (2002) Botulinum toxin
injection versus surgical treatment for tennis elbow: a
randomized pilot study. Clin Orthop Relat Res
125131.
Kramer, H.H., Angerer, C., Erbguth, F., Schmelz, M.
and Birklein, F. (2003) Botulinum toxin A reduces
neurogenic flare but has almost no effect on pain
and hyperalgesia in human skin. J Neurol
250: 188193.
Kvien, T.K. and Uhlig, T. (2005) Quality of life
in rheumatoid arthritis. Scand J Rheumatol
34: 333341.
Larsson, J., Ekblom, A., Henriksson, K., Lundeberg,
T. and Theodorsson, E. (1991) Concentration of
substance P, neurokinin A, calcitonin gene-related
peptide, neuropeptide Yand vasoactive intestinal
polypeptide in synovial fluid from knee joints in
patients suffering from rheumatoid arthritis. Scand J
Rheumatol 20: 326335.
Lawrence, R.C., Helmick, C.G., Arnett, F.C., Deyo,
R.A., Felson, D.T., Giannini, E.H. et al. (1998)
Estimates of the prevalence of arthritis and selected
musculoskeletal disorders in the United States.
Arthritis Rheum 41: 778799.
Layeeque, R., Hochberg, J., Siegel, E., Kunkel, K.,
Kepple, J., Henry-Tillman, R.S. et al. (2004)
Botulinum toxin infiltration for pain control after
mastectomy and expander reconstruction. Ann Surg
240: 608613, discussion 613614.
Lucioni, A., Bales, G.T., Lotan, T.L., McGehee, D.S.,
Cook, S.P. and Rapp, D.E. (2008) Botulinum toxin
type A inhibits sensory neuropeptide release in rat
bladder models of acute injury and chronic
inflammation. BJU Int 101: 366370.
Mahowald, M.L., Singh, J.A. and Dykstra, D. (2006)
Long term effects of intra-articular botulinum toxin A
for refractory joint pain. Neurotox Res 9: 179188.
Meng, J., Wang, J., Lawrence, G. and Dolly, J.O.
(2007) Synaptobrevin I mediates exocytosis of CGRP
from sensory neurons and inhibition by botulinum
toxins reflects their anti-nociceptive potential. J Cell Sci
120: 28642874.
Morre, H.H., Keizer, S.B. and Van Os, J.J. (1997)
Treatment of chronic tennis elbow with botulinum
toxin. Lancet 349: 1746.
Neugebauer, V., Lucke, T. and Schaible, H.G. (1993)
N-methyl-D-aspartate (NMDA) and non-NMDA
receptor antagonists block the hyperexcitability of
dorsal horn neurons during development of acute
arthritis in rats knee joint. J Neurophysiol
70: 13651377.
Ney, J.P., Difazio, M., Sichani, A., Monacci, W.,
Foster, L. and Jabbari, B. (2006) Treatment of chronic
low back pain with successive injections of botulinum
toxin A over 6 months: a prospective trial of 60
patients. Clin J Pain 22: 363369.
Patti, R., Arcara, M., Bonventre, S., Sammartano, S.,
Sparacello, M., Vitello, G. et al. (2008) Randomized
clinical trial of botulinum toxin injection for pain relief
in patients with thrombosed external haemorrhoids.
Br J Surg 95: 13391343.
Placzek, R., Deuretzbacher, G., Buttgereit, F. and
Meiss, A.L. (2005) Treatment of chronic plantar
fasciitis with botulinum toxin A: an open case series
with a 1 year follow up. Ann Rheum Dis
64: 16591661.
Purkiss, J., Welch, M., Doward, S. and Foster, K.
(2000) Capsaicin-stimulated release of substance P
from cultured dorsal root ganglion neurons: involve-
ment of two distinct mechanisms. Biochem Pharmacol
59: 14031406.
Rains, C. and Bryson, H.M. (1995) Topical capsaicin.
A review of its pharmacological properties and
therapeutic potential in post-herpetic neuralgia,
diabetic neuropathy and osteoarthritis. Drugs Aging
7: 317328.
Ranoux, D., Attal, N., Morain, F. and Bouhassira, D.
(2008) Botulinum toxin type A induces direct
analgesic effects in chronic neuropathic pain.
Ann Neurol 64: 274283.
Rapp, D.E., Turk, K.W., Bales, G.T. and Cook, S.P.
(2006) Botulinum toxin type A inhibits calcitonin
gene-related peptide release from isolated rat bladder.
J Urol 175: 11381142.
Salaffi, F., Carotti, M., Stancati, A. and Grassi, W.
(2005) Health-related quality of life in older adults
with symptomatic hip and knee osteoarthritis: a
comparison with matched healthy controls. Aging Clin
Exp Res 17: 255263.
Schaible, H.G., Schmidt, R.F. and Willis, W.D. (1987)
Enhancement of the responses of ascending tract cells
Therapeutic Advances in Musculoskeletal Disease 2 (2)
116 http://tab.sagepub.com
in the cat spinal cord by acute inflammation of the
knee joint. Exp Brain Res 66: 489499.
Schaible, H.G., Del Rosso, A. and Matucci-Cerinic,
M. (2005) Neurogenic aspects of inflammation.
Rheum Dis Clin North Am 31: 77101, ix.
Schaible, H.G., Schmelz, M. and Tegeder, I. (2006)
Pathophysiology and treatment of pain in joint disease.
Adv Drug Deliv Rev 58: 323342.
Schaible, H.G., Richter, F., Ebersberger, A., Boettger,
M.K., Vanegas, H., Natura, G. et al. (2009) Joint pain.
Exp Brain Res 196: 153162.
Siddiqui, M.A. (2007) The efficacy and tolerability of
newer biologics in rheumatoid arthritis: best current
evidence. Curr Opin Rheumatol 19: 308313.
Singer, B.J., Silbert, P.L., Dunne, J.W., Song, S. and
Singer, K.P. (2006) An open label pilot investigation of
the efficacy of botulinum toxin type A [Dysport]
injection in the rehabilitation of chronic anterior knee
pain. Disabil Rehabil 28: 707713.
Singh, J.A., Mahowald, M.L., Kushnaryov, A., Goelz,
E. and Dykstra, D. (2009) Repeat Injections of
intra-articular botulinum toxin A for the treatment of
chronic arthritis joint pain. J Clin Rheumatol
15: 3538.
Singh, J.A., Mahowald, M.L. and Noorbaloochi, S.
(2009) Intra-articular botulinum toxin A for refractory
shoulder pain: a randomized, double-blinded,
placebo-controlled trial. Transl Res 153: 205216.
Slatkowsky-Christensen, B., Mowinckel, P., Loge, J.H.
and Kvien, T.K. (2007) Health-related quality of life
in women with symptomatic hand osteoarthritis: a
comparison with rheumatoid arthritis patients, healthy
controls, and normative data. Arthritis Rheum
57: 14041409.
Sycha, T., Kranz, G., Auff, E. and Schnider, P. (2004)
Botulinum toxin in the treatment of rare head and
neck pain syndromes: a systematic review of the
literature. J Neurol 251(Suppl 1): I1930.
Sycha, T., Samal, D., Chizh, B., Lehr, S., Gustorff, B.,
Schnider, P. et al. (2006) A lack of antinociceptive or
antiinflammatory effect of botulinum toxin A in an
inflammatory human pain model. Anesth Analg
102: 509516.
Van Der Windt, D.A. and Bouter, L.M. (2003)
Physiotherapy or corticosteroid injection for shoulder
pain? Ann Rheum Dis 62: 385387.
Voller, B., Sycha, T., Gustorff, B., Schmetterer, L.,
Lehr, S., Eichler, H.G. et al. (2003) A randomized,
double-blind, placebo controlled study on analgesic
effects of botulinum toxin A. Neurology 61: 940944.
Von Lindern, J.J. (2001) Type A botulinum toxin in
the treatment of chronic facial pain associated with
temporo-mandibular dysfunction. Acta Neurol Belg
101: 3941.
Von Lindern, J.J., Niederhagen, B., Berge, S. and
Appel, T. (2003) Type A botulinum toxin in the
treatment of chronic facial pain associated with
masticatory hyperactivity. J Oral Maxillofac Surg
61: 774778.
Watkins, L.R. and Maier, S.F. (2002) Beyond
neurons: evidence that immune and glial cells
contribute to pathological pain states. Physiol Rev
82: 9811011.
Watkins, L.R. and Maier, S.F. (2003) Glia: a novel
drug discovery target for clinical pain. Nat Rev Drug
Discov 2: 973985.
Watkins, L.R., Milligan, E.D. and Maier, S.F. (2003)
Glial proinflammatory cytokines mediate exaggerated
pain states: implications for clinical pain. Adv Exp Med
Biol 521: 121.
Willis, W.D. and Westlund, K.N. (1997)
Neuroanatomy of the pain system and of the
pathways that modulate pain. J Clin Neurophysiol
14: 231.
Wong, S.M., Hui, A.C., Tong, P.Y., Poon, D.W., Yu,
E. and Wong, L.K. (2005) Treatment of lateral
epicondylitis with botulinum toxin: a randomized,
double-blind, placebo-controlled trial. Ann Intern Med
143: 793797.
Woolf, C.J. (2004) Pain: moving from symptom
control toward mechanism-specific pharmacologic
management. Ann Intern Med 140: 441451.
Woolf, C.J. and Costigan, M. (1999) Transcriptional
and posttranslational plasticity and the generation of
inflammatory pain. Proc Natl Acad Sci U S A
96: 77237730.
Woolf, C.J. and Decosterd, I. (1999) Implications
of recent advances in the understanding of pain
pathophysiology for the assessment of pain in patients.
Pain Suppl 6: S141147.
Woolf, C.J. and Mannion, R.J. (1999) Neuropathic
pain: aetiology, symptoms, mechanisms, and
management. Lancet 353: 19591964.
Woolf, C. and Wiesenfeld-Hallin, Z. (1986)
Substance P and calcitonin gene-related peptide
synergistically modulate the gain of the nociceptive
flexor withdrawal reflex in the rat. Neurosci Lett
66: 226230.
Woolf, C.J., Safieh-Garabedian, B., Ma, Q.P., Crilly, P.
and Winter, J. (1994) Nerve growth factor
contributes to the generation of inflammatory sen-
sory hypersensitivity. Neuroscience
62: 327331.
Woolf, C.J., Allchorne, A., Safieh-Garabedian, B. and
Poole, S. (1997) Cytokines, nerve growth factor and
inflammatory hyperalgesia: the contribution of
tumour necrosis factor alpha. Br J Pharmacol
121: 417424.
Yuan, R.Y., Sheu, J.J., Yu, J.M., Chen, W.T.,
Tseng, I.J., Chang, H.H. et al. (2009) Botulinum
toxin for diabetic neuropathic pain: a randomized
double-blind crossover trial. Neurology
72: 14731478.
JA Singh
http://tab.sagepub.com 117
Zhang, W., Moskowitz, R.W., Nuki, G., Abramson, S.,
Altman, R.D., Arden, N. et al. (2007) Oarsi recom-
mendations for the management of hip and knee
osteoarthritis, part I: critical appraisal of existing
treatment guidelines and systematic review of current
research evidence. Osteoarthritis Cartilage 15: 9811000.
Zhang, W., Moskowitz, R.W., Nuki, G., Abramson, S.,
Altman, R.D., Arden, N. et al. (2008) Oarsi recom-
mendations for the management of hip and knee
osteoarthritis, part II: oarsi evidence-based, expert
consensus guidelines. Osteoarthritis Cartilage
16: 137162.
Visit SAGE journals online
http://tab.sagepub.com
Therapeutic Advances in Musculoskeletal Disease 2 (2)
118 http://tab.sagepub.com
You might also like
- Pain Neuroscience EducationDocument26 pagesPain Neuroscience EducationGustavo Cabanas100% (1)
- Adhesive Capsulitis Presentation May 2009Document29 pagesAdhesive Capsulitis Presentation May 2009cm4100% (1)
- Alzheimer's Disease Research PaperDocument24 pagesAlzheimer's Disease Research Papershayne86% (22)
- Muscle-Brain Communication in Pain The Key Role of MyokinesDocument11 pagesMuscle-Brain Communication in Pain The Key Role of MyokinesGrossl Schorr FernandoNo ratings yet
- NCPs For ParotidectomyDocument12 pagesNCPs For ParotidectomyCarla Manaloto50% (2)
- Chapter 4. Determinants of LearningDocument36 pagesChapter 4. Determinants of LearningAlyssa Marie SociasNo ratings yet
- CVI and Sensory IntegrationDocument8 pagesCVI and Sensory IntegrationKriti ShuklaNo ratings yet
- Ejp 1773Document20 pagesEjp 1773xbeligNo ratings yet
- The Effectiveness of Pain Neuroscience Education Combined With Manual Therapy and Home Exercise For Chronic Low Back PainDocument12 pagesThe Effectiveness of Pain Neuroscience Education Combined With Manual Therapy and Home Exercise For Chronic Low Back PainBruno AssunçaoNo ratings yet
- Low Back PainDocument16 pagesLow Back PainartgpsNo ratings yet
- Ijerph 19 02559Document13 pagesIjerph 19 02559Luisa BarbeitoNo ratings yet
- Exercise For Chronic Musculoskeletal Pain: A Biopsychosocial ApproachDocument9 pagesExercise For Chronic Musculoskeletal Pain: A Biopsychosocial ApproachAndressa FerreiraNo ratings yet
- Axial Low Back Pain One Painful Area - Many Perceptions and Mechanisms - Förster Et Al '13Document8 pagesAxial Low Back Pain One Painful Area - Many Perceptions and Mechanisms - Förster Et Al '13Craig ChambersNo ratings yet
- Effective Treatment Options For Musculoskeletal Pain in Primary Care: A Systematic Overview of Current EvidenceDocument30 pagesEffective Treatment Options For Musculoskeletal Pain in Primary Care: A Systematic Overview of Current EvidenceAndrewL91No ratings yet
- Real Project EditedDocument27 pagesReal Project EditedAbdulrahman YakubuNo ratings yet
- PieberDocument10 pagesPieberPablo WoodwardNo ratings yet
- An Overview of The Management of Persistent Musculoskeletal PainDocument9 pagesAn Overview of The Management of Persistent Musculoskeletal PainFebyan FebyanNo ratings yet
- Naturally Occurring Glucosinolates and Isothiocyanates As A Weapon Against Chronic Pain: Potentials and LimitsDocument19 pagesNaturally Occurring Glucosinolates and Isothiocyanates As A Weapon Against Chronic Pain: Potentials and LimitsKEYLA VANESSA MORALES RODRIGUEZ ESTUDIANTENo ratings yet
- Tzenalis Study ProtocolDocument9 pagesTzenalis Study ProtocolCristoper PanjaitanNo ratings yet
- Heuts Fear OA Pain 2004Document8 pagesHeuts Fear OA Pain 2004damien333No ratings yet
- 105221-Article Text-284848-1-10-20140710Document6 pages105221-Article Text-284848-1-10-20140710hariNo ratings yet
- Botulinum Toxin Use in Post Traumatic Cervical Dystonia and Head TremorDocument14 pagesBotulinum Toxin Use in Post Traumatic Cervical Dystonia and Head TremorSynergy Taman ratuNo ratings yet
- Castrogiovanni 2016Document14 pagesCastrogiovanni 2016carlos corteNo ratings yet
- Relations Between Brain Alterations and Clinical Pain Measures in Chronic Musculoskeletal Pain: A Systematic ReviewDocument41 pagesRelations Between Brain Alterations and Clinical Pain Measures in Chronic Musculoskeletal Pain: A Systematic ReviewRodrigo GuzmánNo ratings yet
- Orofacial Musculoskeletal Pain. An Evidence-Based Bio-Psycho-Social Matrix ModelDocument27 pagesOrofacial Musculoskeletal Pain. An Evidence-Based Bio-Psycho-Social Matrix ModelAMBAR JOSEFA ALEJANDRA MORAGA VALENZUELANo ratings yet
- 10 1002@ejp 1666Document45 pages10 1002@ejp 1666Gabriel DelfinoNo ratings yet
- Ex. ProtocolDocument17 pagesEx. ProtocoladityaNo ratings yet
- 10 1016@j Ultrasmedbio 2020 02 004Document15 pages10 1016@j Ultrasmedbio 2020 02 004Humberto Salas VelizNo ratings yet
- Osteoarthritis in The Geriatric Population 1Document7 pagesOsteoarthritis in The Geriatric Population 1api-532703094No ratings yet
- 10 2519:jospt 2018 7476Document8 pages10 2519:jospt 2018 7476Evelyn MalaguttiNo ratings yet
- Best Practice & Research Clinical Rheumatology: Fiona M. Blyth, Naomi NoguchiDocument9 pagesBest Practice & Research Clinical Rheumatology: Fiona M. Blyth, Naomi NoguchiGufron MustofaNo ratings yet
- Evaluating Meridian-Sinew Release Therapy For The Treatment of Knee OsteoarthritisDocument10 pagesEvaluating Meridian-Sinew Release Therapy For The Treatment of Knee OsteoarthritisGuilherme PenicheNo ratings yet
- Dysfunctional Analgesia During ExerciseDocument10 pagesDysfunctional Analgesia During ExerciseEric MatsuzakiNo ratings yet
- Wells and T 2017Document9 pagesWells and T 2017Alejita TingoNo ratings yet
- Walet (5615275) ThesisDocument24 pagesWalet (5615275) ThesisAmna SandhuNo ratings yet
- Effects of Emg Biofeedback On Pain and Quality of Life in Cervical Dystonia 2329 6895.1000144Document6 pagesEffects of Emg Biofeedback On Pain and Quality of Life in Cervical Dystonia 2329 6895.1000144danishmujibNo ratings yet
- Anxiety July 2011Document8 pagesAnxiety July 2011aswadiibrahimNo ratings yet
- Use of Botulinum Toxin in Orofacial Clinical PracticeDocument16 pagesUse of Botulinum Toxin in Orofacial Clinical Practiceluis castroNo ratings yet
- Dekhne 2023 - Effectiveness of Botulinum Toxin in The Treatment of Neuropathic Pain A Literature ReviewDocument7 pagesDekhne 2023 - Effectiveness of Botulinum Toxin in The Treatment of Neuropathic Pain A Literature ReviewDwika AudiyanandaNo ratings yet
- A Multinational Cross-Sectional StudyDocument15 pagesA Multinational Cross-Sectional StudySadam AbbasiNo ratings yet
- BurstDr Visceral PainDocument11 pagesBurstDr Visceral Painnavid.amirabadiNo ratings yet
- EJHC Volume 14 Issue 3 Pages 593-604Document12 pagesEJHC Volume 14 Issue 3 Pages 593-604sutgaming375No ratings yet
- Cheung2020 PDFDocument15 pagesCheung2020 PDFSandra Milena Cortes SotoNo ratings yet
- Schwerla 2020Document8 pagesSchwerla 2020João Paulo Vila Nova GomesNo ratings yet
- Reduced Pressure PainDocument7 pagesReduced Pressure PaindanaNo ratings yet
- Lateral Epicondylalgia A Musculoskeletal Physiotherapy PerspectiveDocument14 pagesLateral Epicondylalgia A Musculoskeletal Physiotherapy PerspectiveyanikaiNo ratings yet
- Orita 2011Document8 pagesOrita 2011iosif iliaNo ratings yet
- Jmu 26 194Document6 pagesJmu 26 194Arkar SoeNo ratings yet
- 1 s2.0 S204908012101027X Main 1Document10 pages1 s2.0 S204908012101027X Main 1Amirah FaridahNo ratings yet
- Toxins: Central Effects of Botulinum Neurotoxin-Evidence From Human StudiesDocument11 pagesToxins: Central Effects of Botulinum Neurotoxin-Evidence From Human StudiesTameemNo ratings yet
- Fotobiomodulacion - FibromialgiaDocument15 pagesFotobiomodulacion - FibromialgiaGonzalo MoragaNo ratings yet
- Journal 7 PDFDocument9 pagesJournal 7 PDFfransAPNo ratings yet
- Draft Rol-1Document3 pagesDraft Rol-1rosemarytimiyaNo ratings yet
- New Synopsis PranjalDocument5 pagesNew Synopsis PranjalPranjalNo ratings yet
- 28 Autoantibodies and Neuropathic Pain: John M. Dawes David L. BennettDocument18 pages28 Autoantibodies and Neuropathic Pain: John M. Dawes David L. Bennett363331272No ratings yet
- Physical Therapy Protocols To Attenuate Skeletal Muscle Atrophy in Critically Ill Patients Narrative ReviewDocument11 pagesPhysical Therapy Protocols To Attenuate Skeletal Muscle Atrophy in Critically Ill Patients Narrative ReviewVladimir AlvarezNo ratings yet
- Etoricoxib For Arthritis and Pain ManagementDocument15 pagesEtoricoxib For Arthritis and Pain Managementbkvuvce8170No ratings yet
- Artigo Comparação Botox e DyportDocument5 pagesArtigo Comparação Botox e DyportGabriela IesNo ratings yet
- Mechanical Neckpain Article 1Document8 pagesMechanical Neckpain Article 1Zulaikatu MustaphaNo ratings yet
- 2014 The Pain of Tendinopathy - Physiological or PathophysiologicalDocument15 pages2014 The Pain of Tendinopathy - Physiological or PathophysiologicalDavid Alejandro Cavieres AcuñaNo ratings yet
- Autonomic Nervous System Dysregulation and Osteoarthritis PainDocument9 pagesAutonomic Nervous System Dysregulation and Osteoarthritis Paincursotplo2021No ratings yet
- Feasibility of High Dose Medical Exercise Therapy in Patients With Long Term Symptomatic Knee OsteoarthritisDocument10 pagesFeasibility of High Dose Medical Exercise Therapy in Patients With Long Term Symptomatic Knee OsteoarthritisKasmia MalikNo ratings yet
- Fibromyalgia SyndromeFrom EverandFibromyalgia SyndromeJacob N. AblinNo ratings yet
- Herbert 1997 Fortnightly Review Stress The BrainDocument6 pagesHerbert 1997 Fortnightly Review Stress The BrainIqhsan IbrNo ratings yet
- 7 Memory Attention and Mental WorkloadDocument30 pages7 Memory Attention and Mental WorkloadGretchen Laurente100% (4)
- 14 Disability Categories Under Idea PDFDocument3 pages14 Disability Categories Under Idea PDFvenicedmNo ratings yet
- Hydrocephalus: Common Names For DisorderDocument5 pagesHydrocephalus: Common Names For DisorderGita Herminda PutriNo ratings yet
- Posterior Column-Medial Lemniscus System in Clinical Orientation: Representative Lesions and DeficitsDocument1 pagePosterior Column-Medial Lemniscus System in Clinical Orientation: Representative Lesions and DeficitsEduardo RodriguezNo ratings yet
- Directions: Each Item Below Contains A Question Followed by Suggested Responses. Select The One Best ResponseDocument7 pagesDirections: Each Item Below Contains A Question Followed by Suggested Responses. Select The One Best ResponseEsmareldah Henry SirueNo ratings yet
- Final Exam of g10 2019 - 2020Document2 pagesFinal Exam of g10 2019 - 2020Sfa Mabini BatangasNo ratings yet
- NCP LeptoDocument1 pageNCP LeptoFranz RolfNo ratings yet
- Learning Disabilities PDFDocument32 pagesLearning Disabilities PDFchester chesterNo ratings yet
- Epilepsy EpilepsyDocument8 pagesEpilepsy EpilepsyJobelle AcenaNo ratings yet
- Monro-Kellie 2.0: The Dynamic Vascular and Venous Pathophysiological Components of Intracranial PressureDocument13 pagesMonro-Kellie 2.0: The Dynamic Vascular and Venous Pathophysiological Components of Intracranial PressureLeandro NogueiraNo ratings yet
- Biom3003 Sample Exam::) Fuck Yess We Did It!!! Notes From Someone Who Took The Exam Last YearDocument18 pagesBiom3003 Sample Exam::) Fuck Yess We Did It!!! Notes From Someone Who Took The Exam Last Yearbrip selNo ratings yet
- Rajah Menunjukkan Carta Alir Sistem Saraf. Apakah P?: A KraniumDocument20 pagesRajah Menunjukkan Carta Alir Sistem Saraf. Apakah P?: A KraniumanabukitmertajamNo ratings yet
- APPETITE: Physiological and Neurobiological AspectsDocument8 pagesAPPETITE: Physiological and Neurobiological AspectsTamara Souza RossiNo ratings yet
- Carpal Tunnel SyndromeDocument2 pagesCarpal Tunnel SyndromeHejar A.No ratings yet
- EpilepsyDocument28 pagesEpilepsyRajeev RanjanNo ratings yet
- SpineInjury - Dr. PuntodewaDocument41 pagesSpineInjury - Dr. PuntodewaWindy MentariNo ratings yet
- Neurocritical CareDocument337 pagesNeurocritical Cares SNo ratings yet
- Applications On Neurological and Neuropsychiatric Diseases: MembersDocument14 pagesApplications On Neurological and Neuropsychiatric Diseases: MembersNiobe LilithNo ratings yet
- Reye SyndromeDocument15 pagesReye Syndromezeeky35No ratings yet
- Autism PDFDocument25 pagesAutism PDFTalal 197No ratings yet
- Fundamentals of Nervous System Conduction: B. Pathophysiology 1.) Anatomy and PhysiologyDocument27 pagesFundamentals of Nervous System Conduction: B. Pathophysiology 1.) Anatomy and PhysiologyJanine P. Dela CruzNo ratings yet
- 2017 A Neurobiologist's Attempt To Understand Persistent PainDocument8 pages2017 A Neurobiologist's Attempt To Understand Persistent PainCristian OyarzoNo ratings yet
- Brain WavesDocument7 pagesBrain WavesvamseenetsNo ratings yet
- The Pupillary Light Reflex PathwayDocument5 pagesThe Pupillary Light Reflex PathwayNauli PanjaitanNo ratings yet
- M2 Cia-Observation Skills - ManzanilloDocument2 pagesM2 Cia-Observation Skills - ManzanilloSheena Lhane ManzanilloNo ratings yet