Professional Documents
Culture Documents
Oral Lichen Planus: Clinical Presentation and Management: Paul C. Edwards, BSC, MSC, Dds Robert Kelsch, DMD
Oral Lichen Planus: Clinical Presentation and Management: Paul C. Edwards, BSC, MSC, Dds Robert Kelsch, DMD
Uploaded by
Pieter JohnyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Oral Lichen Planus: Clinical Presentation and Management: Paul C. Edwards, BSC, MSC, Dds Robert Kelsch, DMD
Oral Lichen Planus: Clinical Presentation and Management: Paul C. Edwards, BSC, MSC, Dds Robert Kelsch, DMD
Uploaded by
Pieter JohnyCopyright:
Available Formats
Journal of the Canadian Dental Association 494 September 2002, Vol. 68, No.
8
C L I N I C A L P R A C T I C E
L
ichen planus is a relatively common disorder, esti-
mated to affect 0.5% to 2.0% of the general popula-
tion.
1
It isa chronic, inammatory disease that affects
mucosal and cutaneous tissues. Oral lichen planus (OLP)
occursmore frequently than the cutaneousform and tendsto
be more persistent and more resistant to treatment.
2
In view of the prevalence of OLP and the potential of
this chronic disease to cause signicant discomfort, it is
important for clinicians to be aware of its clinical presenta-
tion and management.
Etiology and Pathogenesis
Lichen planus is believed to result from an abnormal
T-cell-mediated immune response in which basal epithelial
cells are recognized as foreign because of changes in the
antigenicity of their cell surface.
3
The cause of this
immune-mediated basal cell damage is unknown. Likewise,
it is unknown if lichen planus represents a single disease
process or several closely related entities with similar clini-
cal presentations. A recent immunologic comparison of
2 variants of OLP suggested that different immunopatho-
genic mechanisms might be involved.
4
Clinical Presentation
Lichen planus affects primarily middle-aged adults, and
the prevalence is greater among women.
5
Children are only
rarely affected.
6
The classic skin lesions of the cutaneous
form of lichen planus can be described as purplish, polygo-
nal, planar, pruritic papules and plaques.
7
These skin lesions
commonly involve the exor surfaces of the legs and arms,
especially the wrists (Fig. 1). The nail beds may also be
affected, with resultant ridging, thinning and subungual
hyperkeratosis.
7
Scalp involvement, if untreated, can lead to
scarring and permanent hair loss.
Since 30% to 50% of patients with oral lesions also
have cutaneous lesions, the presence of these characteristic
cutaneous lesions can aid in the diagnosis of OLP.
Several types of OLP have been described, the 2 main
types being reticular and erosive OLP.
2
It is not uncommon
for the same patient to present with multiple forms of OLP.
Reticular OLP
The reticular form is the most common type of OLP. It
presents as interlacing white keratotic lines (known as
Wickhams striae) with an erythematous border (Fig. 2).
The striae are typically located bilaterally on the buccal
Oral Lichen Planus:
Clinical Presentation and Management
Paul C. Edwards, BSc, MSc, DDS
Robert Kelsch, DMD
A b s t r a c t
Oral lichen planus (OLP) is a chronic mucosal condition commonly encountered in clinical dental practice. Lichen
planus is believed to represent an abnormal immune response in which epithelial cells are recognized as foreign,
secondary to changes in the antigenicity of the cell surface. It has various oral manifestations, the reticular form
being the most common. The erosive and atrophic forms of OLP are less common, yet are most likely to cause
symptoms. Topical corticosteroids constitute the mainstay of treatment for symptomatic lesions of OLP. Recalcitrant
lesions can be treated with systemic steroids or other systemic medications. However, there is only weak evidence
that these treatments are superior to placebo. Given reports of a slightly greater risk of squamous cell carcinoma
developing in areas of erosive OLP, it is important for clinicians to maintain a high index of suspicion for all
intraoral lichenoid lesions. Periodic follow-up of all patients with OLP is recommended.
MeSH Key Words: lichen planus, oral/diagnosis; lichen planus, oral/therapy; precancerous conditions/pathology
J Can Dent Assoc 2002; 68(8):494-9
This article has been peer reviewed.
September 2002, Vol. 68, No. 8 495 Journal of the Canadian Dental Association
Oral Lichen Planus: Clinical Presentation and Management
mucosa, mucobuccal fold, gingiva and, less commonly, the
tongue, palate and lips.
A variant of reticular OLP is the plaque-like form, which
clinically resembles leukoplakia but which has a multifocal
distribution. These plaque-like lesions can range in
presentation from smooth, at areas to irregular, elevated
areas. This variant is commonly found on the dorsum
of the tongue (Fig. 3) and on the buccal mucosa.
Both the reticular form and its plaque-like variant are
usually asymptomatic.
Erosive OLP
Erosive OLP is the second most common type. It
presents as a mix of erythematous and ulcerated areas
surrounded by nely radiating keratotic striae (Figs. 4 and
5). When erosive OLP involves the attached gingival tissue,
it is called desquamative gingivitis. The lesions of erosive
OLP migrate over time and tend to be multifocal. Patients
with this form of OLP often present with symptoms
ranging from episodic pain to severe discomfort that can
interfere with normal masticatory function.
Two additional presentations are the atrophic and
bullous forms, which are considered variants of the erosive
type. Atrophic OLP appears as diffuse, erythematous
patches surrounded by ne white striae. This form can
cause signicant discomfort. In the bullous form, intraoral
bullae are present on the buccal mucosa and the lateral
borders of the tongue; the bullae rupture soon after they
appear, which results in the classic appearance of erosive
OLP.
1
Differential Diagnosis
The diagnosis of OLP can be rendered more condently
when characteristic cutaneous lesions are present. Except
for the pathognomonic appearance of reticular OLP (white
striae occurring bilaterally on the buccal mucosa), in most
cases histopathologic evaluation of lesional tissue is
required to obtain a denitive diagnosis. Even classic cases
of lichen planus may be worthy of biopsy so as to establish
baseline histopathologic features.
The differential diagnosis of erosive OLP includes squa-
mous cell carcinoma, discoid lupus erythematosus, chronic
Figure 2: Reticular oral lichen planus involving the buccal mucosa.
Numerous interlacing white keratotic lines are evident.
Figure 3: Plaque-type variant of reticular oral lichen planus with
erosive areas involving the dorsum of the tongue.
Figure 4: Erosive oral lichen planus involving the buccal mucosa. The
condition is characterized by erythematous areas and interspersed
pseudomembranous areas.
Figure 1: Cutaneous lichen planus on the exor surface of the wrist.
The condition presents as purple, polygonal, plaque-like lesions.
Journal of the Canadian Dental Association 496 September 2002, Vol. 68, No. 8
Edwards, Kelsch
candidiasis, benign mucous membrane pemphigoid,
pemphigus vulgaris, chronic cheek chewing, lichenoid
reaction to dental amalgam or drugs, graft-versus-host
disease (GVHD), hypersensitivity mucositis and erythema
multiforme.
8
The plaque form of reticular OLP can resem-
ble oral leukoplakia.
Biopsy Procedures
The denitive diagnosis of OLP depends on histopatho-
logic examination of the affected tissue. However, perform-
ing a biopsy of lesional tissue, particularly if the OLP is of
the erosive form, can be challenging. It is important to
obtain an elliptical wedge of mucosa extending beyond the
affected area, to avoid stripping the supercial epithelial
layer from the underlying connective tissue.
Histopathologic Features
The classic histopathologic features of OLP include
liquefaction of the basal cell layer accompanied by apopto-
sis of the keratinocytes, a dense band-like lymphocytic inl-
trate at the interface between the epithelium and the
connective tissue, focal areas of hyperkeratinized epithelium
(which give rise to the clinically apparent Wickhams striae)
and occasional areas of atrophic epithelium where the rete
pegs may be shortened and pointed (a characteristic known
as sawtooth rete pegs) (Fig. 6).
8
Eosinophilic colloid
bodies (Civatte bodies), which represent degenerating
keratinocytes, are often visible in the lower half of the
surface epithelium.
Although the histopathologic features of OLP are
characteristic, other conditions, such as lichenoid reaction
to dental amalgam and drugs, may exhibit a similar histo-
logic pattern.
The histopathologic diagnosis of OLP can be compli-
cated by the presence of superimposed candidiasis; diagno-
sis can also be more difficult if the biopsy exhibits an
ulcerated surface. In these situations, the biopsy ndings are
sometimes interpreted as representing a nonspecic chronic
inammatory process.
9
On occasion, the histopathologic features are equivocal,
and the oral pathologist examining the submitted tissue
may recommend that a second biopsy be performed
to obtain fresh tissue for immunofluorescence.
10
Immunouorescent examination of OLP lesional tissue
usually demonstrates deposition of brinogen along the
basement membrane zone. Chronic ulcerative stomatitis
is a relatively recently described condition
11
that has light
microscopic features similar to OLP but possesses a charac-
teristic immunouorescent pattern. It is reportedly less
responsive to corticosteroid therapy than OLP.
If the biopsy report is equivocal, or does not agree with
the clinical picture, it may be prudent to perform another
biopsy, especially when dealing with isolated lesions occur-
ring in locations where the risk of development of squa-
mous cell carcinoma is higher, such as the lateral and ventral
surfaces of the tongue and the oor of the mouth.
Clinical Signicance of OLP
OLP is one of the most common mucosal conditions
affecting the oral cavity.
12
Therefore, dentists in clinical
practice will regularly encounter patientswith thiscondition.
Because patients with the atrophic and erosive forms of
OLP typically experience signicant discomfort, knowledge
of the treatment protocols available is important.
The similarity of OLP to several other vesiculo-
ulcerative conditions, some of which can lead to signicant
morbidity, makes accurate diagnosis essential. For example
OLP and GVHD can have similar histologic and clinical
presentations. GVHD is a serious condition that occurs in
bone marrow transplant patients when transplanted
marrow cells react against host tissues. The extent of oral
Figure 5: Erosive oral lichen planus involving the unattached gingiva. Figure 6: Histopathologic features of oral lichen planus, including
dense band-like lymphocytic inltrate at the interface between the
epithelium and the connective tissue, hyperkeratinized epithelium
and shortened rete pegs.
September 2002, Vol. 68, No. 8 497 Journal of the Canadian Dental Association
Oral Lichen Planus: Clinical Presentation and Management
involvement is highly predictive of the severity and
prognosis of GVHD.
13
Erosive OLP and lichenoid drug reactions can be
indistinguishable both histologically and clinically. Some of
the drugs commonly associated with lichenoid reactions
are nonsteroidal anti-inflammatory drugs, diuretics,
angiotensin-converting enzyme inhibitors, beta-blockers
and antimicrobials (Table 1).
14
It isalso necessary to distinguish isolated erosive or retic-
ular lesions from lichenoid reactions to dental amalgam.
15
Lichenoid reactionsto amalgam do not migrate, they occur
on mucosal tissue in direct contact with the restoration, and
they resolve once the amalgam restoration isremoved.
16
Some studies indicate an increased risk of squamous cell
carcinoma in patients with OLP lesions.
17-20
This increased
risk appears most common with the erosive and atrophic
forms and in cases of lesions of the lateral border of the
tongue. Other studies suggest that in some cases of
purported malignant transformation, the malignancy may
not have developed from true lesions of OLP but may
instead have arisen from areas of dysplastic leukoplakia
with a secondary lichenoid inammatory inltrate.
21,22
A review of previously published studies concluded that the
risk of developing squamous cell carcinoma in patients
with OLP is approximately 10 times higher than that in
the unaffected general population.
23
Other published reports have noted a possible associa-
tion between OLP and hepatitisC,
24
sclerosing cholangitis,
and primary biliary cirrhosis.
25
Treatment
There is currently no cure for OLP. Excellent oral
hygiene is believed to reduce the severity of the symptoms,
but it can be difficult for patients to achieve high levels of
hygiene during periods of active disease. Treatment is aimed
primarily at reducing the length and severity of sympto-
matic outbreaks. Asymptomatic reticular and plaque forms
of OLP do not require pharmacologic intervention.
Before initiating treatment, the diagnosis must be
conrmed histologically. It is also important to rule out
candidiasis, since many treatment modalities can aggravate
an existing candidal infection.
Corticosteroids
The most widely accepted treatment for lesions of OLP
involves topical or systemic corticosteroids to modulate the
patients immune response.
Topical corticosteroids are the mainstay in treating mild
to moderately symptomatic lesions. Options (presented in
terms of decreasing potency) include 0.05% clobetasol
propionate gel,
26
0.1% or 0.05% betamethasone valerate
gel,
6
0.05% uocinonide gel,
27
0.05% clobetasol butyrate
ointment or cream, and 0.1% triamcinolone acetonide
ointment.
28
Patients are instructed to apply a thin layer of the
prescribed topical corticosteroid up to 3 times a day, after
meals and at bedtime. The gel or ointment can be applied
directly or can be mixed with equal parts Orabase (a
gelatinpectinsodium carboxymethylcellulose-based oral
adhesive paste, ConvaTec, Division of Bristol-MyersSquibb,
Montreal, Que.) to facilitate adhesion to the gingival tissues.
The choice of delivery vehicle depends on clinician and
patient preference. In general, oral application is best
accomplished with a gel preparation if available.
In patients with widespread symptomatic lesions, in
whom direct mucosal application of topical medication
would be too uncomfortable, options include 1.0 mg/mL
aqueous triamcinolone acetonide or 0.1 mg/mL dexam-
ethasone elixir. These solutions can be prepared by a
compounding pharmacy. Patients should be instructed to
gargle with 5 mL of the solution for 2 minutes after meals
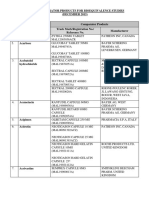
Table 1 Medications associated with mucosal
lichenoid reactions
14
Drug class
Antimalarials
Hydrochloroquine
Quinidine
Quinine
Nonsteroidal anti-inammatory drugs
Indomethacin
Naproxen
Phenylbutazone
Diuretics
Furosemide
Hydrochlorothiazide
Antihypertensives
Angiotensin-converting enzyme inhibitors
Captopril
Enalapril
Beta-blockers
Propranolol
Antibiotics
Penicillin
Sulfonamides
Tetracycline
Antifungals
Ketoconazole
Heavy metals
Bismuth
Chromium
Mercury
Nickel
Miscellaneous
Allopurinol
Carbamazepine
Lithium
Lorazepam
Methyldopa
Oral contraceptives
Journal of the Canadian Dental Association 498 September 2002, Vol. 68, No. 8
Edwards, Kelsch
and at night. After rinsing, the solution should be expecto-
rated, and nothing should be taken by mouth for one hour.
Alternative delivery methods include the use of cloth
strips
29
and custom trays
10
to serve as reservoirs for the
corticosteroid.
The advantage of topical steroid application is that side
effects are fewer than with systemic administration. Adverse
effects include candidiasis, thinning of the oral mucosa and
discomfort on application. Topical formulations of the
more potent corticosteroids can cause adrenal suppression
if used in large amounts for prolonged periods or with
occlusive dressings. The lowest-potency steroid that proves
effective should be used.
Intralesional injection of corticosteroid
28
for recalcitrant
or extensive lesions involves the subcutaneous injection of
0.20.4 mL of a 10 mg/mL solution of triamcinolone
acetonide by means of a 1.0-mL 23- or 25-gauge tuberculin
syringe.
Systemic steroid therapy should be reserved for patients
in whom OLP lesions are recalcitrant to topical steroid
management.
Because the dosage ranges for corticosteroids are wide
and patient responses variable, numerous dosing options
have been proposed.
1,14,30,31
Dosages should be individual-
ized according to the severity of the lesions and the patients
weight and should be modied on the basis of the patients
response to treatment. The oral dose of prednisone for a
70-kg adult ranges from 1020 mg/day for moderately
severe cases to as high as 35 mg/day (0.5 mg/kg daily)
for severe cases.
31
Prednisone should be taken as a single
morning dose to reduce the potential for insomnia
and should be taken with food to avoid nausea and peptic
ulceration.
Signicant response should be observed within one to
2 weeks.
When systemic corticosteroids are prescribed for periods
of longer than 2 weeks, the dosage of steroid must be
gradually tapered to avoid precipitating an adrenal crisis.
Tapering can be accomplished by decreasing the daily dose
of prednisone by 5 mg per week.
The potential side effects of short-term systemic steroid
therapy are numerous. They include insomnia, diarrhea,
disturbances of the central nervous system including
psychotic episodes, sodium and uid retention, muscle
weakness, decreased resistance to infection, hypertension,
hyperglycemia and adrenal suppression.
32
Steroid use is contraindicated in patients who are
breast-feeding. Steroids should be used with caution in
patients with herpetic infections, glaucoma, pregnancy,
HIV infection, tuberculosis, diabetes mellitus and
hypertension.
The prophylactic use of a 0.12% chlorhexidine
gluconate rinse may help reduce the incidence of fungal
infection during corticosteroid therapy.
33
An alcohol-free
rinse (available at most compounding pharmacies) should
be prescribed to avoid desiccation and irritation of the oral
tissues. If secondary growth of candidal organisms is
conrmed, antifungal agents should be prescribed.
Other Approaches
Twice-daily topical application of compounded 0.1%
tacrolimus ointment was recently reported to be effective in
controlling symptoms as well as clearing lesions of OLP.
34,35
Tacrolimus is a macrolide immunosuppressant with a
mechanism of action similar to that of cyclosporine, but is
10 to 100 times more potent and is better able to penetrate
the mucosal surface.
35
Other documented treatment modalities include
retinoids and vitamin A analogues, cyclosporine rinse,
the immunomodulating agent levamisole, PUVA treatment
(which consists of administration of 8-methoxypsoralen
and exposure to long-wave ultraviolet A light), dapsone,
griseofulvin, azathioprine and cryotherapy.
31
A recent systematic review by the Cochrane group
36
of
all published reports of randomized placebo-controlled
trials of palliative treatment for patients with symptomatic
OLP concluded that there was only weak evidence that the
evaluated treatments were superior to placebo. Specically,
9 qualifying studies examining the effect of topical steroids,
topical cyclosporine, and topical and systemic retinoids
were analyzed. The authors of the review concluded that
although most of the studies showed demonstrable treat-
ment effects, the results should be interpreted with caution
because of small sample sizes, lack of independent corrobo-
ration and difficulty in accurately measuring the results of
treatment.
Even though evidence of the efficacy of these treatment
approaches is not overwhelming, corticosteroid therapy
remains the most common approach for managing sympto-
matic lesions.
Because of the possibility of increased risk of malignant
transformation, periodic reassessment of all patients with
OLP is recommended.
Conclusion
Patients with OLP should be counselled as to the nature
of this chronic condition and the different approaches to
treatment. Patients should be informed that they may expe-
rience alternating periods of symptomatic remission and
exacerbation. Clinicians should maintain a high index of
suspicion for all intraoral areas that appear unusual, even in
patients with a histologically conrmed diagnosis of OLP.
This vigilance is especially important for isolated lesions
occurring in locations at higher risk for the development of
squamous cell carcinoma, such as the lateral and ventral
surfaces of the tongue and the oor of the mouth. C
September 2002, Vol. 68, No. 8 499 Journal of the Canadian Dental Association
Oral Lichen Planus: Clinical Presentation and Management
Acknowledgments: The authors would like to thank Dr. J ohn
Fantasia, head, division of oral and maxillofacial pathology, depart-
ment of dental medicine, Long I sland J ewish Medical Center,
New Hyde Park, New York, for his assistance in reviewing this
manuscript.
Dr. Edwardsisa resident, department of dental medicine, division of
oral pathology, LongI sland J ewish Medical Center, New HydePark,
New York.
Dr. Kelsch is an assistant attending, division of oral pathology,
department of dental medicine, LongI sland J ewish Medical Center,
New HydePark, New York.
Correspondence to: Dr. Paul C. Edwards, Department of Dental
Medicine, LongI sland J ewish Medical Center, 270-05 76th Avenue,
New Hyde Park, New York, 11040, USA. E-mail: dental919@
hotmail.com.
The authors have no declared nancial interests in any company
manufacturingthetypesof productsmentioned in thisarticle.
References
1. McCreary CE, McCartan BE. Clinical management of lichen planus.
Brit J Oral Maxillofacial Surg1999; 37(5):338-43.
2. Mollaoglu N. Oral lichen planus: a review. Brit J Oral Maxillofacial
Surg2000; 38(4):370-7.
3. Sapp JP, Eversole LR, Wysocki GP. Contemporary oral and maxillofa-
cial pathology. St. Louis(MI): Mosby; 1997.
4. Rodriguez-Nunez I, Blanco-Carrion A, Garcia AG, Rey JG. Peripheral
T-cell subsets in patients with reticular and atrophic-erosive oral lichen
planus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;
91(2):180-8.
5. Brown RS, Bottomley WK, Puente E, Lavigne GL. A retrospective
evaluation of 193 patients with oral lichen planus. J Oral Pathol Med
1993; 22(5):69-72.
6. Jungell P. Oral lichen planus: a review. Int J Oral MaxillofacSurg1991;
20(3):129-35.
7. Katta R. Lichen planus. AmFamPhysician2000; 61(11):3319-28.
8. Regezzi JA, Sciubba JJ. Oral pathology: clinical pathologic correla-
tions. 3rd ed. Philadelphia: WB Saunders; 1999.
9. BurgessKL, McComb RJ. The gingivae in dermatoses. Ont Dent1997;
74(5):25-9.
10. Murrah VA, Perez LM. Oral lichen planus: parameters affecting
accurate diagnosis and effective management. Pract PeriodonticsAesthet
Dent 1997; 9(6):613-20.
11. LewisJE, Beutner EH, Rostami R, Chorzelski TP. Chronic ulcerative
stomatitis with stratied epithelium-specic antinuclear antibodies.
Int J Dermatol 1996; 35(4):272-5.
12. Pynn BR, BurgessKL, Wade PS, McComb RJ. A retrospective survey
of 2021 patients referred to the Toronto Hospital Mouth Clinic. Ont
Dent 1995; 72(1):21-4.
13. Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillo-
facial pathology. 2nd ed. Philadelphia: WB Saunders; 2002.
14. Bernstein ML. The diagnosisand management of chronic nonspecic
mucosal lesions. J Calif Dent Assoc1999; 27(4):290-9.
15. Ostman PO, Anneroth G, Skoglund A. Oral lichen planuslesionsin
contact with amalgam llings: a clinical, histologic, and immunohisto-
chemical study. Scand J Dent Res1994; 102(3):172-9.
16. Damm DD, Fantasia JE. Radiating white lesion of the ventral surface
of the tongue. Gen Dent 1993; 41(1):26
17. Silverman SJr, Bahl S. Oral lichen planusupdate: clinical character-
istics, treatment responses, and malignant transformation. AmJ Dent
1997; 10(6):259-63.
18. Barnard NA, Scully C, Eveson JW, Cunningham S, Porter SR. Oral
cancer development in patientswith oral lichen planus. J Oral Pathol Med
1993; 22 (9):421-4.
19. Holmstrup P. The controversy of a premalignant potential of oral
lichen planusisover. Oral SurgOral Med Oral Pathol 1992; 73(6):704-6.
20. Silverman S. Oral lichen planus: a potentially premalignant lesion.
J Oral Maxillofacial Surg2000; 58(11):1286-8.
21. Eisenberg E, Krutchkoff DJ. Lichenoid lesions of oral mucosa.
Diagnostic criteria and their importance in the alleged relationship to oral
cancer. Oral SurgOral Med Oral Pathol 1992; 73(6):699-703.
22. Eisenberg E. Oral lichen planus: a benign lesion. J Oral Maxillofacial
Surg2000; 58(11):1278-85.
23. Drangsholt M, Truelove EL, Morton TH Jr, Epstein JB. A man with
a thirty-year history of oral lesions. J Evid Base Dent Pract 2001;
1(2):123-35.
24. Bellman B, Reddy RK, Falanga V. Lichen planus associated with
hepatitisC. Lancet 1995; 346(8984):1234.
25. Fantasia JE. Diagnosisand treatment of common oral lesionsfound
in the elderly. Dent Clin North Am1997; 41(4):877-90.
26. Muzio LL, della Valle A, Mignogna MD, Pannone G, Bucci P, Bucci
E, and other. The treatment of oral aphthousulceration or erosive lichen
planuswith topical clobetasol propionate in three preparations: a clinical
and pilot study on 54 patients. J Oral Pathol Med2001; 30(10):611-7.
27. Voute AB, Schulten EA, Langendijk PN, Kostense PJ, van der Waal
I. Fluocinonide in an adhesive base for treatment of oral lichen planus: a
double-blind, placebo-controlled clinical study. Oral SurgOral Med Oral
Pathol 1993; 75(2):181-5.
28. Vincent SD. Diagnosing and managing oral lichen planus.
JADA1991; 122(6):93-6.
29. Aleinikov A, Jordan RC, Main JH. Topical steroid therapy in
oral lichen planus: review of a novel delivery method in 24 patients.
J Can Dent Assoc1996; 62(4):324-7.
30. Sinz DE, Kaugars GE. Corticosteroid therapy in general dental
practice. Gen Dent 1992; 40(4):298-9.
31. Carrozzo M, Gandolfo S. The management of oral lichen planus.
Oral Dis1999; 5(3):196-205.
32. Mackay S, Eisendrath S. Adverse reaction to dental corticosteroids.
Gen Dent 1992; 40(2):136-8.
33. Ellepola AN, Samaranayake LP. Adjunctive use of chlorhexidine in
oral candidoses: a review. Oral Dis2001; 7(1):11-7.
34. Rozycki TW, RogersRS3rd, Pittelkow MR, McEvoy MT, el-Azhary
RA, Bruce AJ, and others. Topical tacrolimus in the treatment of
symptomatic oral lichen planus: a seriesof 13 cases. J AmAcad Dermatol
2002; 46(1):27-34.
35. Kaliakatsou F, Hodgson TA, Lewsey JD, Hegarty AM, Murphy AG,
Porter SR. Management of recalcitrant ulcerative oral lichen planuswith
topical tacrolimus. J AmAcad Dermatol 2002; 46(1):35-41.
36. Chan ES, Thornhill M, Zakrzewska J. Interventionsfor treating oral
lichen planus. CochraneDatabaseSyst Rev2000; 18(2):CD 001168.
You might also like
- APC CAOP Practice Paper Answer Sheet v1.2014 PDFDocument4 pagesAPC CAOP Practice Paper Answer Sheet v1.2014 PDFhappyscottlee3438100% (1)
- Anesthetic Formulation of Tumescent SolutionsDocument9 pagesAnesthetic Formulation of Tumescent SolutionsJorgeNo ratings yet
- Premalignant Lesions and Conditions: Submitted by-BALJEET KAUR B.D.S.-3 Year Roll No.15Document60 pagesPremalignant Lesions and Conditions: Submitted by-BALJEET KAUR B.D.S.-3 Year Roll No.15Rajat NangiaNo ratings yet
- Rough DraftDocument3 pagesRough Draftapi-285224563No ratings yet
- Cannabis ReportDocument7 pagesCannabis ReportKlaudija LutovskaNo ratings yet
- Symbicort LeafletDocument10 pagesSymbicort Leafletsheeno2607No ratings yet
- Ophthalmic Drugs PDFDocument21 pagesOphthalmic Drugs PDFHussain Syed100% (2)
- 494 PDFDocument6 pages494 PDFranz ibonkNo ratings yet
- Oral Lichen PlanusDocument10 pagesOral Lichen PlanusChander KantaNo ratings yet
- Australian Dental Journal - 2010 - Schifter - Oral Mucosal Diseases The Inflammatory DermatosesDocument16 pagesAustralian Dental Journal - 2010 - Schifter - Oral Mucosal Diseases The Inflammatory Dermatosesneetika guptaNo ratings yet
- Painfulorallesions: Istvan A. HargitaiDocument13 pagesPainfulorallesions: Istvan A. HargitaiAlejandro Ln CNo ratings yet
- OLPandupdate Carrozzo ThorpeDocument13 pagesOLPandupdate Carrozzo ThorpeAstrid Dwi SattiNo ratings yet
- Oral Leukoplakia and ErythroplakiaDocument8 pagesOral Leukoplakia and ErythroplakiadeepaNo ratings yet
- 4 PDFDocument5 pages4 PDFLisda PraditaNo ratings yet
- KP Lesi Pre Kanker Kanker Dan Efek Terapi Kanker Rongga MulutDocument58 pagesKP Lesi Pre Kanker Kanker Dan Efek Terapi Kanker Rongga MulutAditya ZulfikarNo ratings yet
- Lichen Planus and Lichenoid Reactions of The Oral Mucosa: Bethanee J. SchlosserDocument17 pagesLichen Planus and Lichenoid Reactions of The Oral Mucosa: Bethanee J. SchlosserYeni PuspitasariNo ratings yet
- Keratoses IIDocument83 pagesKeratoses IIGomogi SouqNo ratings yet
- Arduino 2017Document8 pagesArduino 2017neetika guptaNo ratings yet
- Leukoplakia 170519204224Document27 pagesLeukoplakia 170519204224Mihai SemeniucNo ratings yet
- White Lesions of The Oral MucosaDocument213 pagesWhite Lesions of The Oral MucosaJunaid Ramzan100% (1)
- Keratoses and Related Disorders of Oral Mucosa II (Slide 4 + 5 + 6)Document83 pagesKeratoses and Related Disorders of Oral Mucosa II (Slide 4 + 5 + 6)JustDen09No ratings yet
- Oral Lichenoid Lesions Distinguishing The Benign From The Deadly Modern PathologyDocument1 pageOral Lichenoid Lesions Distinguishing The Benign From The Deadly Modern PathologyPreda MihaelaNo ratings yet
- DR Meenakshi MDS Oral PathologyDocument29 pagesDR Meenakshi MDS Oral PathologyDr. Meenakshi SinghalNo ratings yet
- Accepted Manuscript: Oral Surgery, Oral Medicine, Oral Pathology and Oral RadiologyDocument33 pagesAccepted Manuscript: Oral Surgery, Oral Medicine, Oral Pathology and Oral RadiologyJihan AttamimiNo ratings yet
- Oral Pathology: Hyperplasia of Oral MucosaDocument7 pagesOral Pathology: Hyperplasia of Oral Mucosaعلي صادق جعفرNo ratings yet
- Oral Lichen PlanusDocument12 pagesOral Lichen PlanusMeuthia AzzahraNo ratings yet
- Lec. 13 &14 Epithelial DisordersDocument10 pagesLec. 13 &14 Epithelial DisordersZainab Alshamary0% (1)
- Scientific Dental Journal: Pigmented Oral Lichen Planus: A Case ReportDocument6 pagesScientific Dental Journal: Pigmented Oral Lichen Planus: A Case ReportSasa AprilaNo ratings yet
- Pre Malignant Conditions of Oral CavityDocument20 pagesPre Malignant Conditions of Oral CavityAsma sultanaNo ratings yet
- Transformasi Ganas Lichen Planus F, Rosif Mukosamulut: IJD 2006 Edisi Khusus KppkgxiyDocument3 pagesTransformasi Ganas Lichen Planus F, Rosif Mukosamulut: IJD 2006 Edisi Khusus KppkgxiyMuhammadNaufalNo ratings yet
- KalmarDocument8 pagesKalmarKING COMICNo ratings yet
- Oral Leukoerythroplakia A Case ReportDocument6 pagesOral Leukoerythroplakia A Case ReportArdelvie YoandaNo ratings yet
- Unilateral LeUkoedema - Case ReportDocument2 pagesUnilateral LeUkoedema - Case ReportBramita Beta ArnandaNo ratings yet
- LeukoplakiaDocument60 pagesLeukoplakiadimasahadiantoNo ratings yet
- Vesicubullous Diseases & Mucocutaneous DisordersDocument23 pagesVesicubullous Diseases & Mucocutaneous Disordersshahlaraib001No ratings yet
- A Clinical Approach White LesionDocument5 pagesA Clinical Approach White LesionTirta KusumaNo ratings yet
- Desquamative Gingivitis: A Sign of Mucocutaneous Disorders - A ReviewDocument6 pagesDesquamative Gingivitis: A Sign of Mucocutaneous Disorders - A Reviewsidra malikNo ratings yet
- Speckled Leukoplakia-Case Report and Review of LiteratureDocument3 pagesSpeckled Leukoplakia-Case Report and Review of LiteratureAlya Hana NatasyaNo ratings yet
- White & Red Lesion 33333 Lecture (1)Document16 pagesWhite & Red Lesion 33333 Lecture (1)ربيد احمد مثنى يحيى كلية طب الاسنان - جامعة عدنNo ratings yet
- Premalignant LesionsDocument76 pagesPremalignant LesionsGowri RaguNo ratings yet
- LP 160610182350Document25 pagesLP 160610182350Karthik TNo ratings yet
- Report OncoDocument23 pagesReport Oncoabdallahtarek2000No ratings yet
- Chronic Oral LesionsDocument16 pagesChronic Oral LesionsJAVIERA HIDALGONo ratings yet
- Proceedings 35 00001 v3Document3 pagesProceedings 35 00001 v3Georgi GugicevNo ratings yet
- Premalignant Oral LesionsDocument94 pagesPremalignant Oral LesionssdinyantiNo ratings yet
- Jurnalku OsccDocument4 pagesJurnalku OsccAndiOctafiantoNo ratings yet
- Out 7Document8 pagesOut 7Musthafa Afif WardhanaNo ratings yet
- DBST Dlja INO Studentov (PDF - Io)Document6 pagesDBST Dlja INO Studentov (PDF - Io)eidNo ratings yet
- Oral Leukoplakia: Well-Demarcated, White Plaques Are Visible On The Lateral Aspects of The TongueDocument3 pagesOral Leukoplakia: Well-Demarcated, White Plaques Are Visible On The Lateral Aspects of The TonguePhúc Hồ Văn TâmNo ratings yet
- Management of Oral Lichen Plannus: A Clinical Study: Jayachandran S, Koijamsashikumar SDocument4 pagesManagement of Oral Lichen Plannus: A Clinical Study: Jayachandran S, Koijamsashikumar Sranz ibonkNo ratings yet
- Vulvar Lichen Planus - Goldstein MetzDocument6 pagesVulvar Lichen Planus - Goldstein MetzMahmud Abdullah RrahmanosmaniNo ratings yet
- Leukoplakia and HomoeopathyDocument8 pagesLeukoplakia and HomoeopathyDr. Rajneesh Kumar Sharma MD Hom100% (1)
- Pathology of The Oral Cavity and Salivary GlandsDocument10 pagesPathology of The Oral Cavity and Salivary GlandsAbdul hadiNo ratings yet
- Salinan Terjemahan Jamur Fitzpatricks Dermatology in General Medicine 8ed - 1Document4 pagesSalinan Terjemahan Jamur Fitzpatricks Dermatology in General Medicine 8ed - 1RubiahSheBiachNo ratings yet
- Oral Oncology: Isaäc Van Der WaalDocument3 pagesOral Oncology: Isaäc Van Der WaalFrancisco VargasNo ratings yet
- Lichen Planus: DR Hira BashirDocument37 pagesLichen Planus: DR Hira BashirSaroash SadruddinNo ratings yet
- Keratosis PatologiaDocument9 pagesKeratosis PatologiakaryNo ratings yet
- Oral UlcerationDocument10 pagesOral Ulcerationمحمد حسنNo ratings yet
- Mollaoglu 2000Document8 pagesMollaoglu 2000MilenaNo ratings yet
- Oral Patho Lecture Shlav BDocument65 pagesOral Patho Lecture Shlav Bشبيبةالروم الملكيين الكاثوليكNo ratings yet
- Erosive Lichen Planus: A Case ReportDocument4 pagesErosive Lichen Planus: A Case ReportNuningK93No ratings yet
- Hairy LeukoplakiaDocument2 pagesHairy LeukoplakiaEka Septariana PuspaNo ratings yet
- Leukoplakia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandLeukoplakia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Complications in UveitisFrom EverandComplications in UveitisFrancesco PichiNo ratings yet
- 2012 Resistant HypertensionDocument9 pages2012 Resistant HypertensionBarry Tumpal Wouter NapitupuluNo ratings yet
- Malaysia-NPRA List of Comparator Products For Bioequivalence Studies December 2015Document47 pagesMalaysia-NPRA List of Comparator Products For Bioequivalence Studies December 2015Noples RozaliaNo ratings yet
- Case-A-Thon Group 2Document9 pagesCase-A-Thon Group 2MatthiasNo ratings yet
- SteroidsDocument13 pagesSteroidsPrajakta DhumaleNo ratings yet
- Primaxin (Imipenem - Cilistatin)Document2 pagesPrimaxin (Imipenem - Cilistatin)ENo ratings yet
- GST Price List - Dt. 14.12.18 - Updated MRPDocument11 pagesGST Price List - Dt. 14.12.18 - Updated MRPSuryaji TelavekarNo ratings yet
- VIVIX COLLECTION PART IIedit PDFDocument4 pagesVIVIX COLLECTION PART IIedit PDFFelicia MgNo ratings yet
- Glyphosate Poisoning: Presenter: Prabu Medical Officer: Dr. NG KL Specialist: DR KauthmanDocument39 pagesGlyphosate Poisoning: Presenter: Prabu Medical Officer: Dr. NG KL Specialist: DR KauthmanPrabu PonuduraiNo ratings yet
- Jurnal Alveolar Osteitis PDFDocument6 pagesJurnal Alveolar Osteitis PDFkrwulanNo ratings yet
- Learning Book: Name: HQ: DivisionDocument39 pagesLearning Book: Name: HQ: DivisionkurutalaNo ratings yet
- Dream Job AssignmentDocument3 pagesDream Job Assignmentapi-354947009No ratings yet
- Infusion Pump & Syringe Pump RevisedDocument18 pagesInfusion Pump & Syringe Pump Revisedfrances182871% (7)
- NyeriDocument1 pageNyeriIlmiyatul MuhimmahNo ratings yet
- Potential of Piperine As A Bioavailability Enhancer: Vasika LeavesDocument10 pagesPotential of Piperine As A Bioavailability Enhancer: Vasika LeavesSushilkumar ShindeNo ratings yet
- SOP in OPTHAMOLOGYDocument6 pagesSOP in OPTHAMOLOGYKynachasya' RiverNo ratings yet
- Prescription Drug Abuse Crisis in NYS - Comprehensive ApproachDocument26 pagesPrescription Drug Abuse Crisis in NYS - Comprehensive ApproachNew York SenateNo ratings yet
- Albizzia The Tree of HappinessDocument4 pagesAlbizzia The Tree of HappinessslowhaNo ratings yet
- Paxil Withdrawal Guide 2005Document102 pagesPaxil Withdrawal Guide 2005Sunit P MehtaNo ratings yet
- Starting A PharmacyDocument8 pagesStarting A PharmacyLloyd Fyl O. RazoNo ratings yet
- Pneumococcus ExpertRules V3.2 20190613Document3 pagesPneumococcus ExpertRules V3.2 20190613Julyadharma Wangsa DharmaNo ratings yet
- Beyond Use DateDocument56 pagesBeyond Use DateDa Chan100% (1)
- Public Assessment Report Decentralised ProcedureDocument22 pagesPublic Assessment Report Decentralised ProcedureHemang M. GajjarNo ratings yet
- Antidepressant Medication - Physiologic Processes and ExerciseDocument1 pageAntidepressant Medication - Physiologic Processes and ExerciseGuille monsterNo ratings yet
- Misuse of Drugs Regulations (Document57 pagesMisuse of Drugs Regulations (Terrence LiNo ratings yet