Professional Documents
Culture Documents
Chart Hepatitis
Chart Hepatitis
Uploaded by
shiner990 ratings0% found this document useful (0 votes)
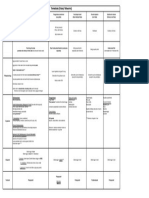
67 views2 pages1. The document describes several types of hepatitis viruses including Hepatitis A, B, C, D, E, and G.
2. It provides details on their structure, mode of transmission, incubation period, potential for chronic infection, treatment options, and methods of prevention.
3. Key differences between the viruses involve whether they have an envelope, their nucleic acid composition, and their potential to cause acute versus chronic infection.
Original Description:
Hepatitis chart
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document1. The document describes several types of hepatitis viruses including Hepatitis A, B, C, D, E, and G.
2. It provides details on their structure, mode of transmission, incubation period, potential for chronic infection, treatment options, and methods of prevention.
3. Key differences between the viruses involve whether they have an envelope, their nucleic acid composition, and their potential to cause acute versus chronic infection.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
67 views2 pagesChart Hepatitis
Chart Hepatitis
Uploaded by
shiner991. The document describes several types of hepatitis viruses including Hepatitis A, B, C, D, E, and G.
2. It provides details on their structure, mode of transmission, incubation period, potential for chronic infection, treatment options, and methods of prevention.
3. Key differences between the viruses involve whether they have an envelope, their nucleic acid composition, and their potential to cause acute versus chronic infection.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 2
Family Picornavirus Hepadnaviridae Flavivirus Deltavirus Calcivirus Flaviviridae
Hepatitis A Hepatitis B Hepatitis C Hepatitis D Hepatitis E Hepatitis G
Envelope Non-enveloped/ Naked Enveloped Enveloped
Enveloped
Defective virus (delta virus)
--> req. HBV for replication
--> forms ribozyme intermed. during replication
Noneveloped/ naked Enveloped
DNA/RNA (+) ssRNA
Partially circular dsDNA
Reverse transcribed & integrated into host chromosome
(+) ssRNA
circular ssRNA
HBV envelope
HDV core
(+) ssRNA (+) ssRNA
Source/
Transmission
Fecal/Oral*****
(shellfish/ polluted water)
[Parenteral spread]
High: blood, serum, wound exudates
Moderate: semen, vaginal fluid, saliva
Low: urine, feces, sweat, tears, breask milk
[Parenteral spread]
-Perinatal transmission
--> only if mom HCV-RNA (+) at delivery
--> 6% infection rate, higher if HIV+, role of viral titer unclear
--> no assoc. w/ delivery method or breastfeeding
--> infected infants do well
-Sexual transmission
--> MSM no higher risk vs. heterosexuals
--> Low prevalence amoung long-term partners
--> M to F transmission more efficient
--> Efficiency low (factors unknown)
--> Accounts for 15-20% of acute & chronic infections
[increased risk for infection]
--> Ever injected illegal drugs
--> Intranasal cocaine use
--> Received clotting factors made before '87
--> Received blood/organs before '92
--> Ever had chronic HD
--> Evidence of liver dz
[Parenteral spread]
Fecally contaminated water
Minimal person to person
Parenteral
Tattoos
Clinical
Manifestations
INCUBATION: Long (6 wk.- 6 month)
< 5 yoa
-Asymptomatic at first
-60% will be chronic*******
Adults:
Usually Symptomatic, LESS chronic (5%)
80% of infants born to infected mother get HBV*****
Mortality = 0.8% in acute illness
Hepatocellular carcinoma
INCUBATION: Long (2 - 26 wks)
Acute infection (20%)- Mild anicteric (NO JAUNDICE)
Chronic (80%)
Of the Chronic cases- Cirrhosis in 20%
-Way more Cirrhosis than HBV
Rarely Fulminant Hepatitis
Infected infants do well (unlike HBV)
-Chronic/ severe hepatitis RARE in them
Other presentations:
Cryoglobulinemia (IgM precipitates in cold temps)
Porphyria cutanea tarda, Aplastic anemia (BM stops)
INCUBATION: Long (6 wks - 6 months)
Worsening of HBV
-Leads to Fulminant Cirrhosis (40%
Coinfection (both at same time)
Severe acute disease
Does NOT go chronic
Superinfection (one after the other)
Get Chronic HDV
High risk of Severe Chronic Liver Disease
Incubation: ~40 days (1.5 month)
No chronic disease
Similar to HAV
High mortality in pregnant****
-20% DIE
Similar to Hep C
Histopathology
Ground-glass cytoplasm of hepatocytes******
Hepatocellular necrosis
Fibrosis & Cirrhosis
Portal and lobular inflammation
Portal dense lymphocyte infiltrate w/ follicle forming
Lobular inflammation
Patchy lobar Steatosis
Kuppfer cell hyperplasia
Cholestasis- blocking of biliary tree --> jaundice
Fibrosis & Cirrhosis
Mnemonic: Hep D for Defective
!"#$%&%&' )&*+'"'
INCUBATION: 1 month (2-3 weeks)
-No carrier state or chronic dz
-Mortality 0.1%
-Immunity lifelong
Epidemiology
1.2 million carriers in U.S.
70% - 90% in Asia, Pacific islands, Middle east
Factors Promoting Chronic HCV
Increased alcohol intake- 7X likely******
Age >40 years when get infected
HIV co-infection
Male
Other infections (ex: HBV)
Note: not so much Occupational transmission
15 million cases in world. Italy, middle east, Africa. Endemic in developing countries
(India, Asia, Africa, Mexico)
Lab Diagnosis
Anti-HAV Ig = exposed
Anti-HAV IgM = recently vaccinated
Immunostaining of HBcAg or HBsAg AA
HBV surface antigen (HBsAg): (outer surface envelope)
-Infected/carrier
HBV core antigen (HBcAg): (core protein)
-NO DETECTION/ TEST, don't order
HBV e antigen (HBeAg): (DNA polymerase)
-Means highly infectious due to active viral replication
CHRONIC HBV: NEVER develop anti-HBs (ab to surface ag)
Anti-HCV enzyme immunoassay (EIA) or ELISA
-Screen for infected, chronic cases
Recombinant immunoblot assay (RIBA)
-Needed to confirm infection, chronic case
HCV RT-PCR
-For active infection to determine viral load
Anti-HDV IgM
Need to test Hep B also
Anti-HEV Ig = exposed
Anti-HEV IgM
-use for Acute Infection
Treatment
No treatment available/ needed
Interferon alpha 2B x 48 wks
Entecavir or Tenofovir if resistance
Tenofovir/Emtricitabine- if co-HIV
-Assess for biochemical evidence of CLD
-Assess for severity of dz & possible tx, according to current practice
guidelines
--> 30-40% sustained response to antiviral combo therapy
(IFN alpha, Ribavirin)
-6 Genotypes, 1 most common & hardest to treat
-Ribavirin & IFN alpha-2b & Telapravir or Bocepivir
(if Genotype I)
No treatment available
Can give HBV vaccine to help prevent
No treatment available/ needed
Post-exposure IgG prophylaxis??
Prevention
Routine childhood vaccine
Who needs vaccine:
Travelers, gay men, drug users, chronic liver dz
Immunization of infants required
(@ 0-, 1-, 6- mo)
-Also give to susceptible groups healthcare workers, sexual contacts
of HBV carriers
-Vaccinate vs. Hep A
-Limit or abstain from alcohol
NO immunization
Give HBV though
Ensure safe drinking water
Only eat pealable fruit
Don't eat uncooked shellfish
Notes:
Gotten from oysters and pools Only 1.8% transmitted after needle stick
-Test for anti-HCV on source
-If source positive: Test Anti-HCV & LFTs
-Get baseline of both tests
-Anti-HCV & LFTs @ 4- 6 mo., or PCR @ 4-6 wk.
-Confirm all anti-HCV with RIBA
Defective (needs HBV for replication)
Envelope= Hep B
RNA= Hep D
-Can only infect in someone already infected by
Hep B.
Clinical signs of hepatitis: cirrhosis, jaundice, ascites, splenomegaly, elevated liver enzymes (transaminases), anemia, leukopenia, thrombocytopenia, liver damage, portal hypertension
You might also like
- Prometric Exam Sample QuestionsDocument9 pagesPrometric Exam Sample QuestionsDe Dios JV100% (6)
- Eukaryotes: Base of Questions of Krok-1 Exam Medical BiologyDocument54 pagesEukaryotes: Base of Questions of Krok-1 Exam Medical BiologyKarla IngaNo ratings yet
- Surgical Wound ClassificationDocument1 pageSurgical Wound Classificationgeclear323No ratings yet
- Discharge-Summary-Template JogiDocument1 pageDischarge-Summary-Template JogiJoginderNo ratings yet
- Mahi Diagnostics: Mri: Both Hip JointDocument1 pageMahi Diagnostics: Mri: Both Hip JointManish KumarNo ratings yet
- Hepatitis FinalDocument73 pagesHepatitis FinalAkhil MuraliNo ratings yet
- Hepatitis A-EDocument34 pagesHepatitis A-EVer Garcera TalosigNo ratings yet
- HIV&HepatitisDocument46 pagesHIV&HepatitisRaja RuzannaNo ratings yet
- 2018 Hepatitis Viral InfectionDocument51 pages2018 Hepatitis Viral Infectionkomang nickoNo ratings yet
- Viral HepatitisDocument49 pagesViral HepatitisAster WidodoNo ratings yet
- Hepatitis A-E Viruses: Ini PPT DR - Catur Dari InternetDocument48 pagesHepatitis A-E Viruses: Ini PPT DR - Catur Dari InternetNurhidayahNo ratings yet
- Part 2 of Medical VirologyDocument113 pagesPart 2 of Medical Virologygatete samNo ratings yet
- Hepatitis A-E Viruses: An OverviewDocument48 pagesHepatitis A-E Viruses: An OverviewPrajakta TawdeNo ratings yet
- Jaundice and Hepatitis in Children: Dr. MwendwaDocument46 pagesJaundice and Hepatitis in Children: Dr. MwendwaAlvin OmondiNo ratings yet
- Hepatitis: Dr. Amany A. GhazyDocument44 pagesHepatitis: Dr. Amany A. GhazyJosé Luis García GarcíaNo ratings yet
- Hepatitis A-E Viruses: Ni Putu Galuh Wibhutisari (10-169)Document49 pagesHepatitis A-E Viruses: Ni Putu Galuh Wibhutisari (10-169)Echa Anskariani Jon PutriNo ratings yet
- HepatitisDocument39 pagesHepatitisRahmiati LaoNo ratings yet
- Hepatitis A, B and C VirusDocument46 pagesHepatitis A, B and C VirusChyzhi SylviaNo ratings yet
- CCE090 Liver and Biliary TractDocument21 pagesCCE090 Liver and Biliary TractBharathi ManiyanNo ratings yet
- Hepatitis C VirusDocument16 pagesHepatitis C Virusمصطفى رسول هاديNo ratings yet
- Viral Hepatitis: Nining Sri Wuryaningsih Bagian Patologi Klinik FK UNSDocument36 pagesViral Hepatitis: Nining Sri Wuryaningsih Bagian Patologi Klinik FK UNSdayanr02No ratings yet
- HepatitisDocument55 pagesHepatitisAbdirashidNo ratings yet
- HepatitisDocument19 pagesHepatitisDayana PrasanthNo ratings yet
- Chromosomal Structure Transmission - Epidemiology Pathogenesis - Symptoms Lab Id - Immunity Prevention and TreatmentDocument5 pagesChromosomal Structure Transmission - Epidemiology Pathogenesis - Symptoms Lab Id - Immunity Prevention and Treatmentsunnyorange88No ratings yet
- 3.0HEPATIT Lecture 5Document48 pages3.0HEPATIT Lecture 5Jiya MuhammadNo ratings yet
- HEPATITIS Compilation (From Various Sources)Document44 pagesHEPATITIS Compilation (From Various Sources)Cathy TajaoNo ratings yet
- Hepatitis BDocument23 pagesHepatitis BMarty Asis100% (1)
- HepatitisDocument55 pagesHepatitisdebdeepbhattacharya411No ratings yet
- Hepatitis: DR Putra Hendra SPPD UnibaDocument87 pagesHepatitis: DR Putra Hendra SPPD Unibayoga yogafenkanoNo ratings yet
- Hepatitis A-E Viruses: An OverviewDocument55 pagesHepatitis A-E Viruses: An OverviewRitu TripathiNo ratings yet
- HepatitisDocument55 pagesHepatitisSUTHAN100% (1)
- Hep B VirusDocument20 pagesHep B VirusBhupesh ChandNo ratings yet
- Infeksi Virus Pada Sistem Pencernaan Bawah: Hepatitis: Ety AprilianaDocument27 pagesInfeksi Virus Pada Sistem Pencernaan Bawah: Hepatitis: Ety AprilianaAsmorowatiNo ratings yet
- Hepatitis Viral - Dr. José Gonzáles BenavidesDocument64 pagesHepatitis Viral - Dr. José Gonzáles BenavidesEfrain Brian SilvaNo ratings yet
- Presented By:-Himanshu Dev DMLT VI TH Sem. VMMC & SJHDocument55 pagesPresented By:-Himanshu Dev DMLT VI TH Sem. VMMC & SJHKailash Nagar100% (1)
- Viral Hepatitis: DR - Abiy F. Nov 2019 Arsi UniversityDocument67 pagesViral Hepatitis: DR - Abiy F. Nov 2019 Arsi UniversityWakjira NigusuNo ratings yet
- HCVDocument33 pagesHCVsherif555No ratings yet
- Hepatitis A-E Viruses: Farida Purnamasari.,SKM 2012Document51 pagesHepatitis A-E Viruses: Farida Purnamasari.,SKM 2012siapaa01No ratings yet
- Hepatitis Virus A Sampai eDocument48 pagesHepatitis Virus A Sampai eaulia rahmahNo ratings yet
- Hepatitis Viruses: Dr. Muna. M. A. Yousif M.D Clinical MicrobiologyDocument45 pagesHepatitis Viruses: Dr. Muna. M. A. Yousif M.D Clinical MicrobiologyMAxeneNo ratings yet
- Acute Viral Hepatitis: Acute Inflamation of The Liver Caused by Primarly Hepatotropic Viruses (A, B, C, D, E)Document35 pagesAcute Viral Hepatitis: Acute Inflamation of The Liver Caused by Primarly Hepatotropic Viruses (A, B, C, D, E)Tarik PlojovicNo ratings yet
- 1010 M Balm - Viral HepatitisDocument17 pages1010 M Balm - Viral HepatitisSaad KhanNo ratings yet
- Viral HepatitisDocument30 pagesViral HepatitisAliya DawoodNo ratings yet
- Hepatitis: Hepatitis A Hepatitis B Hepatitis C Sirrosis HepatisDocument48 pagesHepatitis: Hepatitis A Hepatitis B Hepatitis C Sirrosis Hepatisfarah maulida martaNo ratings yet
- Hepatitis A VirusDocument27 pagesHepatitis A VirusAna KarlaNo ratings yet
- Microbiology and Parasitology 100: Trinity University of Asia St. Luke's College of NursingDocument11 pagesMicrobiology and Parasitology 100: Trinity University of Asia St. Luke's College of NursingFereli Joy SupanNo ratings yet
- 2 Hepatitis VirusDocument31 pages2 Hepatitis VirusDr. Md. Abdullah YusufNo ratings yet
- General Signs/Symptoms Labs/Diagnosis Prevention Treatment: Hepatitis ADocument2 pagesGeneral Signs/Symptoms Labs/Diagnosis Prevention Treatment: Hepatitis A85robertNo ratings yet
- Vaksinasi Hep BDocument28 pagesVaksinasi Hep BMahasti AndrariniNo ratings yet
- Hepatitis B Dan C Dalam KehamilanDocument15 pagesHepatitis B Dan C Dalam Kehamilanzrombie7No ratings yet
- Hepatitis B Dalam KehamilanDocument15 pagesHepatitis B Dalam KehamilanjenniNo ratings yet
- Hepatitis: Dr. Leonardo B Dairi SPPD KgehDocument114 pagesHepatitis: Dr. Leonardo B Dairi SPPD KgehIlham riandaNo ratings yet
- Class 3: Hepatitis Outline I. Hepatitis A Transmission RiskDocument5 pagesClass 3: Hepatitis Outline I. Hepatitis A Transmission RiskTonyNo ratings yet
- Presented By:-Himanshu Dev DMLT VI TH Sem. VMMC & SJHDocument55 pagesPresented By:-Himanshu Dev DMLT VI TH Sem. VMMC & SJHwira guna pratiwiNo ratings yet
- Hepatitis ADocument16 pagesHepatitis AIngrid Masson PintoNo ratings yet
- 1 HepatitisDocument62 pages1 HepatitisKamal AhmedNo ratings yet
- HepatitisDocument46 pagesHepatitisGusti Tirtha Drag JrNo ratings yet
- Infectious Gastrointestinal Diseases: MicrobiologyDocument37 pagesInfectious Gastrointestinal Diseases: MicrobiologyRakesh KumarNo ratings yet
- Hepatitis ViralDocument17 pagesHepatitis ViralKristine Joyce RabanoNo ratings yet
- Hepatologi 1 (CMP)Document61 pagesHepatologi 1 (CMP)Yun ZhaNo ratings yet
- GUASA MT 38 ACTIVITY 8 Hepatitis UPDATEDDocument46 pagesGUASA MT 38 ACTIVITY 8 Hepatitis UPDATEDAllyssa May Callao BongcawilNo ratings yet
- Hepatitis Virus: Bagian Mikrobiologi FK UnissulaDocument36 pagesHepatitis Virus: Bagian Mikrobiologi FK UnissulaKarina Mega WNo ratings yet
- Feature HAV HBV HCV HDV HEV: HepatitisDocument9 pagesFeature HAV HBV HCV HDV HEV: HepatitisPulseWangminNo ratings yet
- Urinechemistries: Walter P. Mutter,, Cynthia A. KorzeliusDocument15 pagesUrinechemistries: Walter P. Mutter,, Cynthia A. Korzeliusshiner99No ratings yet
- Chart TrematodsDocument1 pageChart Trematodsshiner99No ratings yet
- Parasitology SummaryDocument7 pagesParasitology Summaryshiner99100% (1)
- Chart ArbovirusesDocument1 pageChart Arbovirusesshiner99No ratings yet
- Chart RhabdovirusDocument2 pagesChart Rhabdovirusshiner99No ratings yet
- Treponema Pallidum Pallidum Borrelia Recurrentis & Hermsii Borellia Burgdorferi Leptospira InterrogansDocument2 pagesTreponema Pallidum Pallidum Borrelia Recurrentis & Hermsii Borellia Burgdorferi Leptospira Interrogansshiner99No ratings yet
- Chart Pox VirusesDocument1 pageChart Pox Virusesshiner99No ratings yet
- Intestinal Protozoa: Entamoeba Histolytica Giardia Lamblia Cryptosporidium ParvumDocument12 pagesIntestinal Protozoa: Entamoeba Histolytica Giardia Lamblia Cryptosporidium Parvumshiner99No ratings yet
- Lecture 2 (Prostatitis)Document43 pagesLecture 2 (Prostatitis)Rian Permana PNo ratings yet
- Asma Dan DBDDocument18 pagesAsma Dan DBDReynaldo SutantoNo ratings yet
- Endodontic EmmergenciesDocument27 pagesEndodontic EmmergenciesJitender Reddy100% (2)
- ABMM Sample QuestionsDocument7 pagesABMM Sample QuestionsRanjit Kumar ShahNo ratings yet
- Cephalosporins Quick ReviewDocument19 pagesCephalosporins Quick ReviewErinson Custodio PlasenciaNo ratings yet
- Non-Traditional Security Threats in Southeast Asia: Emerging Infectious DiseasesDocument103 pagesNon-Traditional Security Threats in Southeast Asia: Emerging Infectious DiseasesSophal Ear100% (1)
- 001 230277754 CC2 117 1Document1 page001 230277754 CC2 117 1irshad72No ratings yet
- Typhoid FeverDocument24 pagesTyphoid FeverHazielle BondocNo ratings yet
- Influenza: Flu "Influenza" Definition, Symptoms, Causes, Treatment, PreventionDocument3 pagesInfluenza: Flu "Influenza" Definition, Symptoms, Causes, Treatment, PreventionYusuf Rony LosongNo ratings yet
- Endodontic Microbiology: Dr. Ammar Abu MostafaDocument12 pagesEndodontic Microbiology: Dr. Ammar Abu MostafapattasonNo ratings yet
- VPD Surveillance Guidelines - PunjabDocument91 pagesVPD Surveillance Guidelines - PunjabjamshaidjiNo ratings yet
- Appendix-Vii Planned Video Teaching On Control and Prevention of Dengue FeverDocument11 pagesAppendix-Vii Planned Video Teaching On Control and Prevention of Dengue Feverkuruvagadda sagarNo ratings yet
- Pathology Mcqs 2Document6 pagesPathology Mcqs 2Numan Rox100% (5)
- An Introduction To Probiotics: Key PointsDocument6 pagesAn Introduction To Probiotics: Key PointsDinesh PuppalaNo ratings yet
- Hand Hygiene in Dental Health-Care SettingsDocument55 pagesHand Hygiene in Dental Health-Care SettingsManu DewanNo ratings yet
- Plac Pathology - Drucilla RobertsDocument11 pagesPlac Pathology - Drucilla RobertsconstantinilieNo ratings yet
- Abdominal AbscessDocument3 pagesAbdominal AbscessIchalAzNo ratings yet
- "Bloody Scours": Swine DysenteryDocument29 pages"Bloody Scours": Swine DysenteryleaNo ratings yet
- Tumour Immunology: Von Ryan F. Lingcallo, RMTDocument20 pagesTumour Immunology: Von Ryan F. Lingcallo, RMTJuan SalenNo ratings yet
- Biodata March 19Document81 pagesBiodata March 19ULAGANATHAN MNo ratings yet
- B.SC in Nursing Syllabus 2018 For Web PDFDocument100 pagesB.SC in Nursing Syllabus 2018 For Web PDFYolanda Nadya0% (1)
- Red Eye The Role of Primary CareDocument16 pagesRed Eye The Role of Primary CareNatukunda DianahNo ratings yet
- Liver Nursing NotesDocument7 pagesLiver Nursing NotesHeather ShantaeNo ratings yet
- Retrospective Study of Feline and Canine Cryptococcosis in Australia From 1981 To 2001: 195 CasesDocument12 pagesRetrospective Study of Feline and Canine Cryptococcosis in Australia From 1981 To 2001: 195 CasesKlaus Ramirez SuarezNo ratings yet
- Thesis DoneDocument24 pagesThesis DoneAmira SaidinNo ratings yet
- Approach To Neurologic Infections.4 PDFDocument18 pagesApproach To Neurologic Infections.4 PDFosmarfalboreshotmail.comNo ratings yet
- tmpC061 TMPDocument34 pagestmpC061 TMPFrontiersNo ratings yet