Professional Documents
Culture Documents
Turp
Turp
Uploaded by
Coleen Comelle Huerto0 ratings0% found this document useful (0 votes)
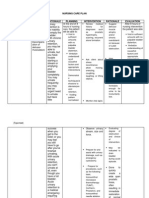
348 views23 pagesTransurethral Resection of the Prostate (TURP) is a common surgery to treat an enlarged prostate by removing prostate tissue blocking urine flow. During TURP, an instrument is inserted through the urethra to cut and remove prostate tissue using an electric cutting tool. The procedure usually takes an hour under general or spinal anesthesia, with most patients staying in the hospital 1-2 days to recover. TURP provides effective relief of urinary symptoms for 7-10 out of 10 men who have the surgery.
Original Description:
case
Original Title
turp
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentTransurethral Resection of the Prostate (TURP) is a common surgery to treat an enlarged prostate by removing prostate tissue blocking urine flow. During TURP, an instrument is inserted through the urethra to cut and remove prostate tissue using an electric cutting tool. The procedure usually takes an hour under general or spinal anesthesia, with most patients staying in the hospital 1-2 days to recover. TURP provides effective relief of urinary symptoms for 7-10 out of 10 men who have the surgery.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
348 views23 pagesTurp
Turp
Uploaded by
Coleen Comelle HuertoTransurethral Resection of the Prostate (TURP) is a common surgery to treat an enlarged prostate by removing prostate tissue blocking urine flow. During TURP, an instrument is inserted through the urethra to cut and remove prostate tissue using an electric cutting tool. The procedure usually takes an hour under general or spinal anesthesia, with most patients staying in the hospital 1-2 days to recover. TURP provides effective relief of urinary symptoms for 7-10 out of 10 men who have the surgery.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 23
Transurethral Resection of the Prostate (TURP) for Benign Prostatic Hyperplasia
During transurethral resection of the prostate (TURP), an instrument is inserted up
the urethra to remove the section of the prostate that is blocking urine flow.
TURP usually requires a stay in the hospital. It is done using a general or spinal
anesthetic.
What To Expect After Surgery
The hospital stay after TURP is commonly 1 to 2 days.
Following surgery, a catheter is used to remove urine and blood or blood clotsin
the bladder that may result from the procedure. When the urine is free of significant
bleeding or blood clots, the catheter can be removed and you can go home.
Strenuous activity, constipation, and sexual activity should be avoided for about 4 to 6
weeks. Symptoms such as frequent urination will continue for a while because of
irritation and inflammation caused by the surgery. But they should ease during the first 6
weeks.
Why It Is Done
Your doctor may recommend TURP if symptoms caused by benign prostatic
hyperplasia (BPH) have not improved in response to home treatment and medicines.
How Well It Works
For men who have moderate to severe symptoms of prostate enlargement, TURP is
more effective than watchful waiting in relieving urinary symptoms. Studies have found
that:
Men who had TURP had a lower symptom score compared with those who used
watchful waiting.
1
Symptoms get better for 7 to 10 out of 10 men who have the surgery.
2
Men experience about an 85% improvement in their American Urological Association
(AUA) symptom index scores.
2
For example, if you had a score of 25, after this surgery
it might be at about 4. Men who are very bothered by their symptoms are most likely to
notice great improvement in their symptoms after TURP. Men who are not very
bothered by their symptoms are less likely to notice a big change.
Risks
The risks of transurethral resection of the prostate (TURP) include problems with sexual
performance, incontinence, and problems from surgery.
Problems with sexual performance
Ejaculation into the bladder (retrograde ejaculation) is very common. It occurs in about
25 to 99 men out of 100.
2
This does not affect sexual function.
Men who have TURP appear to have no greater risk for erection problems than men
who do not have surgery.
3
For men who do have trouble getting an erection, medicine
can help.
Loss of ability to control urine flow (incontinence)
A small number of men (about 1 out of 100) say they are completely unable to hold
back their urine after the surgery.
2
But some experts say that men who have TURP
appear to have no greater risk for incontinence than men who do not have surgery.
3
Some men find that they can still hold in their urine after the surgery, but they tend to
leak or dribble.
Problems related to having surgery
About 5 out of 100 men have severe bleeding and need a blood transfusion.
4
Transurethral resection (TUR) syndrome occurs in about 2 out of 100 men who have
TURP.
2
This syndrome occurs when the body absorbs too much of the fluid used to
wash the area around the prostate while prostate tissue is being removed. The
symptoms of TUR syndrome include mental confusion, nausea, vomiting, high blood
pressure, slowed heartbeat, and visual disturbances. TUR syndrome is temporary
(usually lasting only the first 6 hours after surgery) and is treated with medicine that
removes excess water from the body (diuretic).
About 2 men out of 100 need to have another operation after 3 years. And about 8 men
out of 100 need to have another operation after 5 years.
2
Repeat surgery because of a complication of the surgery is needed less than 10% of
the time.
2
What To Think About
TUR syndrome doesn't happen when TURP is done using a bipolar tool (resectoscope)
compared to a monopolar resectoscope. You may want to ask your doctor which kind of
tool he or she uses.
Surgery usually is not required to treat BPH, although some men may choose it
because their symptoms bother them so much. Choosing surgery depends mostly on
your preferences and comfort with the idea of having surgery. Things to think about
include your expectation of the results of the surgery, the severity of your symptoms,
and the possibility of having complications from the surgery.
Men who have severe symptoms often have great improvement in quality of life
following surgery. Men whose symptoms are mild may find that surgery does not greatly
improve quality of life. Men with only mild symptoms may want to think carefully before
deciding to have surgery to treat BPH.
Transurethral resection of the prostate
Share on facebookShare on twitterBookmark & SharePrinter-friendly version
Transurethral resection of the prostate (TURP) is surgery to remove the inside part of
the prostate gland in order to treat an enlarged prostate.
Related topics include:
Benign prostatic hyperlasia
Prostate resection - minimally invasive
Simple prostatectomy
Description
The surgery takes about 1 hour.
You will be given medicine before surgery so you don't feel pain. You may get one of
the following:
General anesthesia: You are asleep and pain-free
Spinal anesthesia: You are awake, but relaxed and pain-free
The surgeon will insert a scope through the tube that carries urine from your bladder out
of the penis. This tube is called the urethra. A special cutting tool is placed through the
scope. It is used to remove the inside part of your prostate gland using electricity.
Why the Procedure is Performed
Your doctor may recommend this surgery if you have benign prostatic hyperplasia
(BPH). The prostate gland often grows larger as men get older. The larger prostate play
causes problems with urinating. Removing part of the prostate gland can often make
these symptoms better.
Prostate removal may be recommended if you have:
Difficulty emptying your bladder
Frequent urinary tract infections
Bleeding from the prostate
Bladder stones with prostate enlargement
Extremely slow urination
Damage to the kidneys
Before you have surgery, your doctor will suggest you make changes in how you eat or
drink. You may also be asked to try taking medicine. Your prostate may need to be
removed if these steps do not help. TURP is one of the most common type of prostate
surgery. Other procedures are also available.
Your doctor will consider the following when deciding on the type of surgery:
Size of your prostate gland
Your health
What type of surgery you may want
Risks
Risks for any surgery are:
Blood clots in the legs that may travel to the lungs
Breathing problems
Infection, including in the surgical wound, lungs (pneumonia), or bladder or
kidney
Blood loss
Heart attack or stroke during surgery
Reactions to medications
Additional risks are:
Problems with urine control
Loss of sperm fertility
Erection problems
Passing the semen into the bladder instead of out through the urethra (retrograde
ejaculation)
Urethral stricture (tightening of the urinary outlet from scar tissue)
Transurethral resection (TUR) syndrome (water buildup during surgery)
Damage to internal organs and structures
Before the Procedure
You will have many visits with your doctor and tests before your surgery. Your visit will
include:
Complete physical exam
Treating and controlling diabetes, high blood pressure, heart or lung problems,
and other conditions
If you are a smoker, you should stop several weeks before the surgery. Your doctor or
nurse can give you tips on how to do this.
Always tell your doctor or nurse what drugs, vitamins, and other supplements you are
taking, even ones you bought without a prescription.
During the weeks before your surgery:
You may be asked to stop taking medicines that can thin your blood, such as
aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), vitamin E,
clopidogrel (Plavix), warfarin (Coumadin), and others.
Ask your doctor which drugs you should still take on the day of your surgery.
On the day of your surgery:
Do not eat or drink anything after midnight the night before your surgery.
Take the drugs your doctor told you to take with a small sip of water.
Your doctor or nurse will tell you when to arrive at the hospital.
After the Procedure
You will stay in the hospital for 1 to 3 days.
After surgery, you will have a small tube, called a Foley catheter, in your bladder to
remove urine. The urine will look bloody at first. The blood goes away within a few days
in most cases. Blood can also seep around the catheter. A special solution may be used
to flush out the catheter and keep it from getting clogged with blood. The catheter will be
removed within 1 to 3 days for most people
You will be able to go back to eating a normal diet right away.
You will need to stay in bed until the next morning. You will be asked to move around as
much as possible after that point.
Your health care team will:
Help you change positions in bed
Teach you exercises to keep blood flowing
Teach you how to perform coughing and deep breathing techniques. You should
do these every 3 to 4 hours.
Tell you how to care for yourself after your procedure.
You may need to wear tight stockings and use a breathing device to keep your lungs
clear.
You may be given medication to relieve bladder spasms.
Outlook (Prognosis)
TURP relieves symptoms of an enlarged prostate most of the time. You may have
burning with urination, blood in your urine, urinate often, and need to urgently urinate.
Background
For most of the 20th century, from 1909 until the late 1990s, the premier treatment for
symptomatic benign prostatic hypertrophy (BPH) was transurethral resection of the
prostate (TURP). TURP was the first successful, minimally invasive surgical procedure
of the modern era. To this day, it remains the criterion standard therapy for obstructive
prostatic hypertrophy and is both the surgical treatment of choice and the standard of
care when other methods fail.
Since the advent of medical therapy for symptomatic prostatic hypertrophy with 5-alpha
reductase inhibitors and alpha-adrenergic blockers, the need for immediate surgical
intervention in symptomatic prostatic obstruction has been reduced substantially.
However, alpha-blockers do not modify prostate growth, and even the use of prostatic
growth inhibitors such as finasteride or dutasteride often fails to prevent recurrent
urinary symptoms of BPH and retention. In the past, these patients would almost
certainly have undergone TURP years earlier.
The criteria for performing TURP surgery are now more stringent than before. In
general, TURP surgery is reserved for patients with symptomatic BPH who have acute,
recurrent, or chronic urinary retention; in whom medical management and less-invasive
prostatic surgical procedures failed; who have prostates of an unusual size or shape
(eg, a markedly enlarged median lobe, significant intravesical prostatic encroachment);
who have azotemia or renal insufficiency due to prostatic obstruction; or who have the
most severe symptoms of prostatism.
Less common uses of TURP include intractable prostatitis or for tissue sampling when
standard biopsy techniques cannot be used.
The relative frequency of TURP compared to open prostatectomy in surgical patients
varies from country to country. In 1990, the relative frequency rate of TURPs in surgical
patients with BPH in the United States was 97%, with similar rates in Denmark and
Sweden. The lowest rates of TURP were noted in Japan (70%) and France (69%).
The average age of patients currently undergoing TURP is approximately 69 years, and
the average amount of prostate tissue resected is 22 g. Risk factors associated with
increased morbidity include prostate glands larger than 45 g, operative time longer than
90 minutes, and acute urinary retention as the presenting symptom. The 5-year risk rate
for a reoperation following TURP is approximately 5%. Overall mortality rates following
TURP by a skilled surgeon are virtually 0%.
African Americans more typically present for TURP surgery with urinary retention or
urinary infections and have a higher incidence of preexisting medical problems
compared to the general population. According to Kang et al (2004), reports from the
Prostate, Lung, Colorectal, and Ovarian (PLCO) cancer screening trial indicate that
Asian and Asian American men have the lowest overall risk of clinical BPH and eventual
TURP.
[1]
Go to Prostate Cancer, Prostate-Specific Antigen, and Benign Prostatic Hypertrophy for
complete information on these topics.
Indications
According to the Agency for Health Care Policy and Research guidelines for the
diagnosis and treatment of BPH and the recommendations of the Second International
Consultation on Benign Prostatic Hypertrophy, the absolute indications for primary
surgical management of BPH are as follows:
[2]
Refractory urinary retention
Recurrent urinary tract infections due to prostatic hypertrophy
Recurrent gross hematuria
Renal insufficiency secondary to bladder outlet obstruction
Bladder calculi
Permanently damaged or weakened bladders
Large bladder diverticula that do not empty well secondary to an enlarged prostate
Most men who present for surgical correction of their urinary outlet obstruction are those
in whom medical therapy or alternative procedures have failed or are inappropriate for
some reason. In general, patients with moderate-to-severe lower urinary tract
obstructive symptoms (American Urological Association [AUA] symptom index >8) who
have not responded to alpha-adrenergic blockers and/or 5-alpha reductase inhibitors
are also candidates for surgical intervention.
A study by Blanchard et al showed that patients in whom alpha-blocker therapy is
ineffective or those in whom it has failed tend to have poorer outcomes after TURP than
men who proceed directly to a transurethral resection.
[3]
This is presumably from
preoperative bladder damage and other risk factors that affect voiding rather than the
size of the prostate. Operating time and weight of resected tissue have been
documented as the same between the 2 groups; therefore, prostatic size alone does not
account for the difference in outcomes.
Although persistent, progressive, or bothersome symptoms of urinary obstruction due to
prostatic hypertrophy that are refractory to medical therapy constitute the most common
indication for TURP, 70% of men undergoing the procedure have multiple indications.
Patients with prostates larger than 45 g, who present with acute urinary retention, or
who require operating times in excess of 90 minutes, are at increased risk for
postoperative complications.
Surgical treatment of BPH is also indicated in cases of renal failure or insufficiency
secondary to prostatic obstruction. Catheter drainage is usually recommended in such
cases until the renal failure resolves. As many as 10% of men with BPH present with
some degree of renal insufficiency.
Contraindications
The only absolute indication for an open prostatectomy over a TURP is the need for an
additional open procedure on the bladder that must be performed at the same time as
the prostatectomy. Such indications include open surgical resection of a large bladder
diverticulum or removal of a bladder stone that cannot be easily fragmented by
intracorporeal lithotripsy.
A relative indication for the selection of an open prostate surgery over a TURP is
generally based on prostatic volume and the ability of the surgeon to complete the
TURP in less than 90 minutes of actual operating time (although < 60 min is considered
optimal).
In general, open prostatectomy can be justified in a patient with a prostate of 45 g or
larger, but this is totally dependent on the skill and experience of the endoscopic
urological surgeon. Most experienced urologists use a prostatic volume of 60-100 g as
the upper limit amenable to endoscopic removal, but some highly skilled resectionists
are capable of safely treating a 200-g prostate with TURP in less than 90 minutes.
Declining Frequency of TURP
The new availability of reasonable alternative medical and surgical treatment options
means that TURP, once one of the most commonly practiced urological procedures, is
now performed much less frequently. In 1962, TURP operations accounted for more
than 50% of all major surgical procedures performed by urologists in the United States.
By 1986, this had declined to 38%.
The 1985 Veterans Administration Normative Aging Study estimated the lifetime
probability of surgical intervention for prostatic enlargement at 29%, and the 1986
National Health Survey estimated that 350,000 patients in the Medicare age group had
a TURP that year, compared to fewer than 200,000 in that same age group by 1998.
These numbers should be considered within the context that the median age of the
typical patient is rising (the number of older men with BPH-related symptoms in the
United States is expected to increase from 5 million to 9 million persons by 2025), the
size of the average resected prostate gland is increasing, and the typical patient has
more comorbidities and is generally less healthy than surgical patients of the past.
A comprehensive review of transurethral prostatectomy in the Medicare beneficiaries by
Wasson et al compared a national sample from 1991-1997 to a similar group for the
period 1984-1990 found that the more recent group demonstrated a substantial decline
in the number of TURP surgeries: 50% for white men and 40% for black
men.
[4]
Compared to the peak period of TURP use in the 1980s, a higher proportion of
the men undergoing the procedure were older in the more recent period, with 53% aged
75 years or older.
Another factor that must be considered when evaluating the general decline in the
number of TURP procedures performed is the significant reduction in financial
reimbursement to urologists for TURP surgeries in the United States.
Physician reimbursement from Medicare for a TURP has dropped from a high of $2000-
$3000 in the past to approximately $650 today, with a 90-day global period that covers
all postoperative care by the surgeon for 3 months. In many instances, performing a
TURP is simply not profitable for the urologist when office overhead, billing and
malpractice costs are considered, especially when complications occur.
Alternative surgical procedures, such as microwave therapy and prostatic laser surgery,
are reimbursed at much higher levels, even though they may not be as durable or
effective. This creates a strong financial disincentive for urologists to perform TURP
procedures, except when no reasonable alternatives exist. A 2002 article by Donnell
examined the history of Medicare policies and the effect of changes in Medicare
reimbursement on TURP.
[5]
In a large Canadian series reported by Borth et al, the number of TURP procedures
dropped by 60% between 1988 and 1998, presumably because of medical therapy,
despite an increase of 16% in the male population older than 50 years.
[6]
While the
number of patients presenting with urinary retention was significantly higher in the 1998
group than in the 1988 cohort (55% vs 23%), no significant difference was noted in their
average age, medical comorbidities, operative parameters, average size of prostate
tissue resected, or complication rates.
Anatomic Considerations
The prostate is divided into 3 zones: peripheral, central, and transition. The peripheral
zone is the largest of the zones, encompassing approximately 75% of the total prostate
glandular tissue in men without BPH. Most prostate cancers originate in the peripheral
zone. It is located posteriorly and extends laterally on either side of the urethra.
The central zone is smaller and extends primarily around the ejaculatory ducts. It differs
from the peripheral zone primarily in cytologic details and architecture.
The transition zone is usually the smallest of the 3: it occupies only 5% of the prostate
volume in men younger than 30 years. This is the zone thought to be the origin of BPH.
The transition zone consists of two separate lobes on either side of the urethra and
usually involves a small grouping of ductal tissue near the central portion of the prostatic
urethra near the internal sphincter.
As the transition zone expands, it can comprise up to 95% of the prostate volume,
compressing the other zones. Intraoperatively, the 2 enlarged lobes of the transition
zone can be seen obstructing the prostatic urethra on either side. Thus, the term lateral
lobes is often used intraoperatively for this tissue to distinguish it from any hyperplastic
periurethral gland tissue.
The periurethral glands are less commonly involved with BPH, but when they do
become enlarged, they can form what is termed a median lobe, which appears as a
teardrop-shaped midline structure at the posterior bladder neck. This can ball-valve into
the urethra, creating severe obstructive voiding symptoms. Any significant intravesical
extension of prostatic tissue can act as a valve when the detrusor pressure increases
and presses this tissue against the bladder neck or across the outlet to the urethra,
creating a functional obstruction (see the image below).
Benign prostatic hypertrophy of the lateral and median lobes. Various
configurations.
In some earlier jargon, the transition zone and periurethral region were called the
central gland or inner gland, and the peripheral and central zones were called the outer
gland. This terminology should be avoided both because it is vague and because it
creates confusion with the now-standard anatomical label of the central zone.
Prostatic calculi are formed from calcification of the corpora amylacea and precipitation
of prostatic secretions. They occur between the transition zone and the compressed
peripheral zone; in fact, they can be used as a marker for this border. Prostatic calculi
are generally composed of calcium phosphate and are not considered clinically
significant. Chemical analysis is unnecessary.
Although prostatic calculi may arise spontaneously, they also may be formed in
response to an inflammatory reaction or as a consequence of another pathological
process that produces acinar obstruction. Some practitioners believe that calcifications
that form in response to bacterial prostatitis may harbor bacteria that periodically
flourish, causing recurrent prostatitis. Proponents of this theory advocate TURP to
liberalize these calcifications as a treatment for recurrent prostatitis.
If a channel is opened during surgery that allows these calculi to be expressed, they
often flow out by themselves if the opening is large enough. They can be milked out by
using the end of the cutting loop without current to gently press around the opening
where the prostatic stones are seen and can be pushed into the opened prostatic fossa.
They can be rinsed into the bladder and evacuated with the rest of the resected
prostatic chips.
The prostate is thinnest and most narrow anteriorly (the 12-oclock position when
viewed through a cystoscope). Care should be taken when operating in this area to
avoid perforating the prostatic capsule, especially if this portion of the prostate is
resected early in the operation. Abundant venous blood vessels are located in the area
just anterior to the prostatic capsule, which can cause significant bleeding that cannot
be easily controlled if the vessels are damaged during resection.
The external sphincter muscle tends to be slightly tilted, with the most proximal portion
located anteriorly, opposite the verumontanum. The external sphincter can be identified
cystoscopically by its wrinkling and constricting action as the resectoscope is withdrawn.
Upon reinsertion, the superficial mucosa in front of the telescope tends to bunch up.
This is because the external sphincter muscle is imbedded within the urogenital
diaphragm, which is relatively fixed in position, while the prostate has some limited
mobility.
The verumontanum is the single most important anatomical landmark in TURP (see the
image below). It is a midline structure located on the floor of the distal prostatic urethra
just proximal to the external sphincter muscle. It appears as a small, rounded hump that
is best seen when withdrawing the telescope through the prostate while visualizing the
prostatic floor at the 6-oclock position.
Basic anatomy of the prostate, sagittal section.
The orifices to the ejaculatory ducts emerge in the verumontanum (see the first image
below). Its importance lies in its position immediately proximal to the external sphincter
muscle (see the second image below), which allows it to be used as the distal landmark
for prostate resection. The precise distance between the verumontanum and the
external sphincter demonstrates some slight individual variation and should be verified
visually before starting the resection and periodically during the surgery.
Anatomy of the prostate and bladder, posterior view. Anatomy of the prostate
and urethra.
The proximity of the ureteral orifices to the cephalad margin of the hypertrophied
prostate varies, particularly in patients with an enlarged median lobe. This distance
should be frequently assessed throughout surgery.
The vascular anatomy of the prostate was accurately described in detail by Rubin
Flocks in 1937.
[7]
The blood supply of the prostate comes primarily from branches of the
inferior vesical artery, which is a branch of the internal iliac artery (see the image
below).
Blood supply to the prostate.
When the inferior vesical artery reaches the prostate just at the vesicoprostatic border, it
branches into 2 groups of arteries (see the image below). One penetrating group
passes directly into the prostate toward the interior of the bladder neck. Upon reaching
the prostatic interior near the urethra, most of these branches turn distally and parallel
the prostatic urethra, while others supply the median lobe.
Blood supply to the prostate. Note the two main branches: urethral and capsular.
Vessels that parallel the prostatic urethra supply most of the blood to the hypertrophied
lateral lobes. The second large group of arteries follows the exterior of the prostatic
capsule posterolaterally, periodically giving rise to perforating vessels, and supplies the
area around the verumontanum.
See Prostate Anatomy and Male Urethra Anatomy for more information.
Development of Benign Prostatic Hyperplasia
Mechanisms of disease
The prostate has been described as the organ of the body most likely to be involved
with disease of some sort in men older than 60 years. This statement characterizes any
histological evidence of BPH as a disease, which is certainly debatable, but there is no
argument that BPH is an extremely common clinical entity.
As the hyperplastic process increases the volume of the prostate, the urethral lumen is
compressed, causing outlet obstruction. An enlarged median lobe may cause relatively
more severe symptoms than lateral lobe hyperplasia of similar magnitude because it
can act as a valve at which increased bladder pressure may actually cause further
obstruction. Intravesical extension of the lateral lobes may act in a similar fashion.
It has been known for many years, however, that prostate size alone is not a reliable or
accurate predictor of the presence or degree of urinary outlet obstruction. The failure of
several purely obstructive therapies, such as prostatic balloon dilatation, and the
obvious success of alpha-adrenergic blockers eventually led to the description of BPH
as having both a dynamic (neurogenic) and a mechanical (obstructive) component.
Thus, at the same time as the occurrence of mechanical obstruction, a dynamic
component involving the stromal prostatic tissue and bladder is present, which is often
more significant in causing urinary symptoms than simple mechanical obstruction from
an enlarged prostate. The precise interaction of these two mechanisms, mechanical and
dynamic, is not well understood.
When a bladder is trying to empty through a blocked outlet from an obstructing prostate
gland, the intravesical pressure required to open the bladder neck is increased. The
bladder is initially able to produce a higher transitory voiding pressure when required,
but loses muscle tone over time.
Isolated muscle bundles hypertrophy in response to the need for a higher intravesical
pressure to overcome the increased resistance to voiding, and bladder trabeculation
often follows. The spaces between these hypertrophied bundles tend to become
thinner, with less functional muscle. Eventually, this can progress to the point at which
the bladder becomes almost nonfunctional.
Bladder trabeculation is usually graded on a scale of I-IV. When seen on cystoscopy
images, it is a relative indicator of the degree and duration of any bladder outlet
obstruction (eg, BPH), although any detrusor hyperactivity problem can possibly
produce bladder trabeculations, even without an identifiable obstruction. Initial
symptomatic changes include increased bladder instability and irritability, which can
eventually progress to muscular decompensation with permanent loss of detrusor
contractile ability.
Evidence indicates that obstruction causes partial denervation of bladder smooth
muscle, which results in further bladder irritability and involuntary detrusor contractions.
Fortunately, most of these hyperactive symptoms resolve over time with removal of the
prostatic obstruction or with a response to appropriate medications. The detrusor
becomes less able to maintain a constant voiding pressure over time, which leads to
early termination of voiding, intermittency of the urinary stream, and higher residual
urine volume, accompanied by loss of bladder compliance.
Overall bladder mass increases because of detrusor muscle hypertrophy, but collagen
deposition is also increased, which eventually contributes to decompensation, urinary
retention, and permanent loss of detrusor contractile ability.
Proposed causes
BPH is thought to be caused by aging and by long-term testosterone and
dihydrotestosterone (DHT) production, although their precise roles are not completely
clear.
Histopathologic evidence of BPH is present in approximately 8% of men in their fourth
decade and in 90% of men by their ninth decade. Loss of testosterone early in life
prevents the development of BPH. The similarities in presentation, pathological
examination findings, and symptoms of BPH among identical twins suggest a hereditary
influence.
Once BPH has developed, it tends to progress. Cross-sectional studies based on
cadaver autopsies or consecutive patients seen in urology clinics suggest that the
growth rate decreases with age. In patients aged 31-50 years, the prostate doubling
time averages 4.5 years. In men aged 51-70 years, the prostatic doubling time is
approximately 10 years, while in men older than 70 years, the doubling time increases
to more than 100 years. Note that these findings may only reflect a selection bias in the
sample group.
A 5-year longitudinal study by Rhodes and colleagues of 631 community men aged 40-
79 years from Olmsted County, Minnesota demonstrated an average annual prostate
growth rate of 1.6%. This remained essentially constant regardless of age, although
men with larger prostates tended to have higher growth rates.
The average prostate weighs approximately 20 g by the third decade and remains
relatively constant in size and weight unless BPH develops. The typical patient with
BPH has a prostate that averages 33 g. Only 4% of the male population ever develops
prostates of 100 g or larger. (The largest recorded prostatectomy specimen weighed
820 g. This prostate was removed by open suprapubic prostatectomy. Unfortunately,
the patient ultimately died of hemorrhage.)
Symptoms of BPH tend to progress slowly over time in most individuals, with an
average annual increase of 0.14-0.44 points per year in the AUA symptom index for
men aged 60 years and older. Once BPH has begun, the prostate grows an average of
0.6 mL in volume annually, with a mean decrease in average urinary peak flow rate of
0.2 mL per second each year. Men older than 70 years and those with a baseline peak
flow rate less than 10 mL/s tend to have a more rapid and dramatic decline in their peak
flow rates over time.
DHT has an affinity for prostate cell androgen receptors that is 5 times greater than that
of testosterone. The levels of 5-alpha reductase are increased in the stromal tissue of
men with BPH compared to controls. This and other data indicate that DHT is much
more important in the development of prostatic hypertrophy than testosterone is.
The success of 5-alpha reductase blockers, such as finasteride and dutasteride, in
reducing prostatic size and relieving symptoms seems to confirm this, although it does
not explain the relative lack of symptom relief in those with smaller prostate glands
treated with these agents.
Clinical manifestations and medical treatment
Classic symptoms of BPH include a slow, intermittent, or weak urinary stream; the
sensation of incomplete bladder emptying; double voiding (the need to void within a few
seconds or minutes of urinating); postvoid dribbling; urinary frequency; and nocturia.
Patients may also present with acute or chronic urinary retention, urinary tract
infections, gross hematuria, renal insufficiency, bladder pain, a palpable abdominal
mass, or overflow incontinence.
Upon physical examination, the bladder may be palpable during the abdominal
examination and the prostate may be enlarged during the digital rectal examination.
Symptoms are not necessarily proportional to the size of the prostate on digital rectal
examination or transrectal ultrasound findings.
Alpha-adrenergic receptors are present and functional in the stromal smooth muscle of
the prostate and especially at the bladder neck. Many studies have documented the
success of various alpha-adrenergic blockers in relieving symptoms of BPH. Evidence
from the Medical Therapy of Prostate Symptoms Trial indicates that combination
therapy with both an alpha-blocker and a 5-alpha reductase inhibitor can delay the
progression of symptoms and is more effective over time than either medication alone
for reducing symptom scores and improving peak urinary flow rates.
Preparing for your procedure
Your surgeon will explain how to prepare for your procedure. For example, if you smoke
you will be asked to stop, as smoking increases your risk of getting a chest and wound
infection, which can slow your recovery.
If you have been prescribed anticoagulant medicines, such as clopidogrel, which can
stop your blood from clotting, you may be advised to stop taking these before your
procedure. This is because you may bleed more after your procedure if youre taking
these.
Your surgeon will discuss with you what will happen before, during and after your
procedure, and any pain you might have. This is your opportunity to understand what
will happen, and you can help yourself by preparing questions to ask about the risks,
benefits and any alternatives to the procedure. This will help you to be informed, so you
can give your consent for the procedure to go ahead, which you may be asked to do by
signing a consent form.
The procedure is usually carried out under general anaesthesia. This means you will be
asleep during the procedure. Alternatively, you may have the procedure under spinal or
epidural anaesthesia. This completely blocks feeling from your waist down and you will
stay awake during the procedure. You may be offered a sedative with a spinal
anaesthetic this relieves anxiety and helps you to relax.
Your surgeon or anaesthetist will advise which type of anaesthesia is most suitable for
you.
If youre having a general anaesthetic, you will be asked to follow fasting instructions.
This means not eating or drinking, typically for about six hours beforehand. However,
its important to follow your anaesthetists or surgeons advice.
You may be asked to wear compression stockings to help prevent blood clots forming in
the veins in your legs. You may need to have an injection of an anticlotting medicine
called heparin as well as, or instead of, wearing compression stockings.
What happens during TURP
The procedure will take up to an hour.
Your surgeon will insert a narrow, rigid, metallic, tube-like telescopic camera called an
endoscope into your urethra (the tube that carries urine from your bladder and out
through your penis). He or she will then insert a specially adapted surgical instrument
called a resectoscope. This is an electrically heated wire loop that is used to cut out and
remove the middle of your enlarged prostate. Your surgeon will insert a catheter (a thin
flexible tube) into your urethra to drain urine from your bladder into a bag. This is
because you may not be able to urinate normally immediately after the procedure as
you may have some swelling.
What to expect afterwards
You will need to rest until the effects of the anaesthetic have passed. You may not be
able to feel or move your legs for several hours after a spinal or epidural anaesthetic.
You may need pain relief to help with any discomfort as the anaesthetic wears off.
You will have a catheter to drain urine from your bladder into a bag. The catheter will
also be used to wash out your bladder with a sterile solution, which helps to flush out
any blood clots in your bladder. The catheter will be removed when your urine begins to
run clear. This is usually within 24 to 48 hours. Occasionally, you may need to keep the
catheter in for a short period after you go home. If so, your nurse will show you how to
look after it.
You may have a drip in your arm to prevent you getting dehydrated. This will be
removed once youre drinking enough fluids. You will be encouraged to get out of bed
and move around as this helps prevent chest infections and blood clots developing in
your legs.
You will usually be able to go home after about two days. You will need to arrange for
someone to drive you home. General anaesthesia temporarily affects your co-ordination
and reasoning skills, so you must not drive, drink alcohol, operate machinery or sign
legal documents for 24 hours afterwards. If youre in any doubt about driving, contact
your motor insurer so that youre aware of their recommendations, and always follow
your surgeons advice.
Recovering from TURP
If you need pain relief, you can take over-the-counter painkillers, such as paracetamol
or ibuprofen. Always read the patient information that comes with your medicine and if
you have any questions, ask your pharmacist for advice.
You may be advised to increase your fluid intake to flush out your bladder and help you
to recover. You may find that you have some blood clots in your urine around 10 to 14
days after your procedure. These are scabs from your prostate healing and coming
away. If increasing your fluid intake doesnt clear this up, see your GP.
A small number of men get a urinary infection after the TURP procedure. If you have
any stinging when you urinate, see your GP so that your urine can be tested for an
infection. Your GP will prescribe you antibiotics if you need them.
It can take up to four weeks to recover fully from TURP. After two to three weeks you
can resume your normal activities. To help your recovery, your surgeon may
recommend that you do pelvic floor exercises. Your doctor or nurse at the hospital will
explain how to do these and how often. Please see our frequently asked questions for
more information about pelvic floor exercises.
Dont do any strenuous activity for about four weeks after your procedure. You can have
sex as soon as youre comfortable this will probably be at least three to four weeks
after your procedure.
What are the risks?
As with every procedure, there are some risks associated with TURP. We have not
included the chance of these happening as they are specific to you and differ for every
person. Ask your surgeon to explain how these risks apply to you.
Side-effects
Side-effects are the unwanted but mostly temporary effects you may get after having
the procedure, for example, feeling sick from the effects of the anaesthetic.
Some specific side-effects of TURP include the following.
Blood in your urine. This is usually an expected side-effect of the procedure and isnt
normally a cause for concern. If it continues for longer than two weeks, see your GP.
An urgent need to pass urine. This is sometimes accompanied by a burning sensation
when you pass urine.
Incontinence (urine leakage). Talk to your GP if this happens, but it usually improves
with time.
Erectile dysfunction (impotence). This doesnt usually happen and youre unlikely to be
affected if you had normal erections before your procedure.
Complications
Complications are when problems occur during or after your procedure. The possible
complications of any procedure includes an unexpected reaction to the anaesthetic,
excessive bleeding or developing a blood clot, usually in a vein in your leg (deep vein
thrombosis, DVT). Specific complications of TURP include the following.
Retrograde ejaculation. This is where semen passes into your bladder during an
orgasm instead of out of your penis. You will then pass the semen mixed with urine the
next time you urinate. Retrograde ejaculation is permanent and can affect your fertility,
so talk to your doctor if youre concerned.
Infection. You may be given antibiotics before your procedure to prevent infection.
TURP syndrome. This is a condition that can develop if the fluid used to flush your
bladder during your procedure is absorbed into your body. This can cause changes in
your blood pressure and you may feel sick or vomit. However, this is becoming less
common as a different type of fluid is often used to flush your bladder, which is less
likely to cause TURP syndrome. Please see our frequently asked questions for more
information about TURP syndrome.
Urethral stricture. This is scarring of the inside of your urethra, which causes it to
become narrower. Symptoms include problems when urinating, such as urinary
retention (being unable to pass urine at all) or incontinence (urine leakage). You may
be advised to have a further procedure to widen the inside of your urethra again.
Your prostate may grow again. If this happens, you may need to have another
procedure if too little was removed during the first procedure.
What is a transurethral resection of the prostate or TURP?
A transurethral resection of the prostate (TURP) is a surgical procedure that removes
portions of the prostate gland through the penis. A TURP requires no external incision.
The surgeon reaches the prostate by inserting an instrument through the urethra (the
narrow channel through which urine passes from the bladder out of the body). This
instrument, called a resectoscope, is about 12 inches long and one-half inch in
diameter. It contains a light, valves that control irrigating fluid, and an electrical loop that
cuts tissue and seals blood vessels. It's inserted through the penis and the wire loop is
guided by the surgeon so it can remove the obstructing tissue one piece at a time. The
pieces of tissue are carried by fluid into the bladder and flushed out at the end of the
procedure.
What is the prostate gland?
Click Image to Enlarge
The prostate gland is about the size of a walnut and surrounds the neck of a man's
bladder and urethrathe tube that carries urine from the bladder. It's partly muscular
and partly glandular, with ducts opening into the prostatic portion of the urethra. It's
made up of three lobes, a center lobe with one lobe on each side.
As part of the male reproductive system, the prostate gland's primary function is to
secrete a slightly alkaline fluid that forms part of the seminal fluid (semen), a fluid that
carries sperm. During male climax (orgasm), the muscular glands of the prostate help to
propel the prostate fluid, in addition to sperm that was produced in the testicles, into the
urethra. The semen then travels through the tip of the penis during ejaculation.
Researchers don't know all the functions of the prostate gland. However, the prostate
gland plays an important role in both sexual and urinary function. It's common for the
prostate gland to become enlarged as a man ages, and it's also likely for a man to
encounter some type of prostate problem in his lifetime.
Many common problems are associated with the prostate gland. These problems may
occur in men of all ages and include:
Benign prostatic hyperplasia (BPH). An age-related enlargement of the prostate
that isn't malignant. BPH is the most common noncancerous prostate problem,
occurring in most men by the time they reach their 60s. Symptoms are slow,
interrupted, or weak urinary stream; urgency with leaking or dribbling; and frequent
urination, especially at night. Although it isn't cancer, BPH symptoms are often
similar to those of prostate cancer.
Prostatism. This involves decreased urinary force due to obstruction of flow through
the prostate gland. The most common cause of prostatism is BPH.
Prostatitis. Prostatitis is inflammation or infection of the prostate gland
characterized by discomfort, pain, frequent or infrequent urination, and sometimes
fever.
Prostatalgia. This involves pain in the prostate gland, also called prostatodynia. It's
frequently a symptom of prostatitis.
Cancer of the prostate is a common and serious health concern. According to the
American Cancer Society, prostate cancer is the most common form of cancer in men
older than age 50, and the third leading cause of death from cancer.
There are different ways to achieve the goal of removing the prostate gland. Methods of
performing prostatectomy include:
Surgical removal includes a radical prostatectomy (RP), with either a retropubic or
perineal approach. This is used to treat cancer. Radical prostatectomy is the
removal of the entire prostate gland. Nerve-sparing surgical removal is important to
preserve as much function as possible.
Transurethral resection of the prostate, or TURP, which also involves removal of part
of the prostate gland, is an approach performed through the penis with an
endoscope (small, flexible tube with a light and a lens on the end).
Cryosurgery is a less invasive procedure than surgical removal of the prostate gland.
Treatment is administered using probe-like needles that are inserted in the skin
between the scrotum and anus. The urologist can also use microwaves.
Laparoscopic surgery, done manually or by robot, is another method of removal of
the prostate gland.
Reasons for the procedure
TURP is generally done to relieve symptoms due to prostate enlargement, often due to
BPH. When the prostate gland is enlarged, the gland can press against the urethra and
interfere with or obstruct the passage of urine out of the body. BPH is a condition in
which the prostate gland may become quite enlarged and cause problems with
urination. Symptoms may include:
Problems with getting a urine stream started
Having to urinate more frequently at night
Having an urgent need to urinate
Dribbling after you finish urinating
These symptoms can create problems such as retaining urine in the bladder, which can
contribute to bladder infections or formation of stones in the bladder.
BPH can also raise prostate-specific antigen (PSA) levels two to three times higher than
the normal level. An increased PSA level doesn't always indicate cancer, but the higher
the PSA level, the higher the chance for having cancer. A TURP may be done in men
who can't tolerate a radical prostatectomy due to their age or overall health status.
Specific treatment for BPH will be determined by your doctor based on:
Your age, overall health, and medical history
Extent of the disease
Your tolerance for specific medications, procedures, or therapies
Expectations for the course of the disease
Your opinion or preference
Eventually, BPH symptoms usually require some kind of treatment. When the gland is
just mildly enlarged, treatment may not be needed, as research has shown that some of
the symptoms of BPH can clear up without treatment in some mild cases. This decision
can only be made by your doctor after careful evaluation of your individual condition.
Regular checkups are important, however, to watch for developing problems.
Sometimes a TURP is done to treat symptoms only, not to cure the disease. For
example, if you're unable to urinate because of cancer, but radical prostatectomy isn't
an option for you, you may need a TURP.
There may be other reasons for your doctor to recommend a TURP.
Risks of the procedure
As with any surgical procedure, certain complications can occur. Some possible
complications may include:
Blood in the urine after surgery
Painful or difficult urination
Possibility of infection
Retrograde ejaculation (when ejaculation occurs in the bladder and not the penis)
Bleeding
Infection
There may be other risks depending on your specific medical condition. Be sure to
discuss any concerns with your doctor prior to the procedure.
Before the procedure
Some things you can expect before the procedure include:
Your doctor will explain the procedure to you and offer you the opportunity to ask
any questions that you might have about the procedure.
You'll be asked to sign a consent form that gives permission to do the procedure.
Read the form carefully and ask questions if something isn't clear.
In addition to a complete medical history, your doctor may perform a physical
examination to ensure you're in good health before you undergo the procedure. You
may also undergo blood tests and other diagnostic tests.
You'll be asked to fast for eight hours before the procedure, generally after midnight.
Notify your doctor if you're sensitive to or are allergic to any medications, latex,
iodine, tape, contrast dyes, and anesthetic agents (local or general.)
Notify your doctor of all medications (prescribed and over the counter) and herbal
supplements that you're taking.
Notify your doctor if you have a history of bleeding disorders or if you're taking any
anticoagulant (blood-thinning) medications, aspirin, or any other medications that
affect blood clotting. It may be necessary for you to stop these medications prior to
the procedure.
If you smoke, you should stop smoking as soon as possible prior to the procedure, in
order to improve your chances for a successful recovery from surgery and to
improve your overall health status.
You may receive a sedative prior to the procedure to help you relax.
Based on your medical condition, your doctor may request other specific preparation.
During the procedure
Click Image to Enlarge
Transurethral resection of the prostate requires a stay in the hospital. Procedures may
vary depending on your condition and your doctor's practices.
Generally, a TURP follows this process:
You'll be asked to remove any jewelry or other objects that may interfere with the
procedure.
You'll be asked to remove your clothing and will be given a gown to wear.
You'll be asked to empty your bladder prior to the procedure.
An intravenous (IV) line will be started in your arm or hand.
You'll be positioned on the operating table, lying on your back.
The anesthesiologist will continuously monitor your heart rate, blood pressure,
breathing, and blood oxygen level during the surgery. Once you're sedated, a
breathing tube will be inserted through your throat into your windpipe and you'll be
connected to a ventilator, which will breathe for you during the surgery.
The surgeon will inspect the urethra and bladder with an endoscope. This is done by
passing the scope through the tip of the penis, then into the urethra and bladder. This
allows the doctor to examine these areas for any tumors or stones in the bladder.
Next, the resectoscope (electrical loop) is passed into the urethra. It cuts out pieces
of tissue from the prostate that are bulging or blocking the urethra. Electricity will be
applied through the resectoscope to stop any potential bleeding.
The doctor will insert a catheter into the bladder to empty urine.
You'll be transferred from the operating table to a bed then taken to the recovery
room.
After the procedure
In the hospital
After the procedure, you may be taken to the recovery room to be closely monitored.
You'll be connected to monitors that will constantly display your electrocardiogram (ECG
or EKG) tracing, blood pressure, other pressure readings, breathing rate, and your
oxygen level.
Once your blood pressure, pulse, and breathing are stable and you're alert, you'll be
taken to your hospital room.
You may receive pain medication as needed, either by a nurse, or by administering it
yourself through a device connected to your intravenous line.
Once you're awake and your condition has stabilized, you may start liquids to drink.
Your diet may be gradually advanced to more solid foods as you are able to tolerate
them.
The urine catheter will stay in place for one to three days to help urine drain while your
prostate gland heals. You'll probably have blood in your urine after surgery.
Also, a liquid solution may be attached to the catheter to flush the blood and potential
clots out of the catheter. The bleeding will gradually decrease, and then the catheter will
be removed.
Arrangements will be made for a follow-up visit with your doctor.
Your doctor may give you additional or alternate instructions after the procedure,
depending on your particular situation.
At home
Once you're home, it'll be important to drink lots of fluid. This aids in flushing out any
remaining blood or clots from your bladder.
You'll be advised to not do any heavy lifting for several weeks after the TURP. This is to
prevent any recurrence of bleeding.
You may be tender or sore for several days after a TURP. Take a pain reliever for
soreness as recommended by your doctor.
You shouldn't drive until your doctor tells you to. Other activity restrictions may apply.
Notify your doctor to report any of the following:
Fever and/or chills
Redness, swelling, or bleeding or other drainage from the incision site
Increase in pain around the incision site
Trouble urinating
Your doctor may give you additional or alternate instructions after the procedure,
depending on your particular situation.
You might also like
- NCP For Urinary RetentionDocument5 pagesNCP For Urinary RetentionColeen Comelle Huerto60% (5)
- Acute Renal FailureDocument33 pagesAcute Renal FailureAqsa Akbar AliNo ratings yet
- Case Study CLD 1Document12 pagesCase Study CLD 1MoonNo ratings yet
- LeptospirosisDocument9 pagesLeptospirosisDeepu VijayaBhanuNo ratings yet
- DSMTS 0005 3 AlODocument4 pagesDSMTS 0005 3 AlOSimanchal KarNo ratings yet
- Yarn ManufacturerersDocument31 pagesYarn ManufacturerersMarufNo ratings yet
- A Simple Guide to Parathyroid Adenoma, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Parathyroid Adenoma, Diagnosis, Treatment and Related ConditionsNo ratings yet
- StomachGastricCancerDocument12 pagesStomachGastricCancerBhawna JoshiNo ratings yet
- Brain TumorDocument50 pagesBrain TumorbudiNo ratings yet
- Drug StudyDocument8 pagesDrug StudyJheryck SabadaoNo ratings yet
- Cholelithiasis GallstoneDocument22 pagesCholelithiasis GallstoneBheru LalNo ratings yet
- NeuroblastomaDocument4 pagesNeuroblastomaGeleine Curutan - OniaNo ratings yet
- Abdominal Trauma Is An Injury To The Abdomen. Signs and Symptoms Include AbdominalDocument5 pagesAbdominal Trauma Is An Injury To The Abdomen. Signs and Symptoms Include AbdominalVictoria DolințăNo ratings yet
- Case Pre Ovarian CystDocument56 pagesCase Pre Ovarian Cystthesa1201No ratings yet
- Devices Used in ICU: Critical Care NursingDocument95 pagesDevices Used in ICU: Critical Care NursinghendranatjNo ratings yet
- MI LABS ExplainedDocument3 pagesMI LABS Explainedjrubin83669No ratings yet
- Chronic Kidney DiseaseDocument7 pagesChronic Kidney DiseaseLardel Balbiran LafortezaNo ratings yet
- CellulitisDocument15 pagesCellulitisSujatha J JayabalNo ratings yet
- STI College of Nursing Sta. Cruz, Laguna College of Nursing: Submitted To: Mrs. Aurea Celino, RN Clinical InstructorDocument41 pagesSTI College of Nursing Sta. Cruz, Laguna College of Nursing: Submitted To: Mrs. Aurea Celino, RN Clinical InstructorPong's Teodoro SalvadorNo ratings yet
- Case Study PresentationDocument44 pagesCase Study Presentationapi-31876231450% (2)
- CholelitiasisDocument42 pagesCholelitiasisEdwin YosuaNo ratings yet
- Case Study About: Cardiac Failure and Pulmonary EdemaDocument32 pagesCase Study About: Cardiac Failure and Pulmonary EdemaIan Simon DorojaNo ratings yet
- A Drug Study On: EpinephrineDocument16 pagesA Drug Study On: EpinephrineJay Jay JayyiNo ratings yet
- Pulmonary AngiographyDocument3 pagesPulmonary AngiographyBiway RegalaNo ratings yet
- Pyloric StenosisDocument2 pagesPyloric Stenosisreshmivunni0% (1)
- 10 Golden Rules of IV TherapyDocument8 pages10 Golden Rules of IV Therapybbasya eihynaNo ratings yet
- Throid StormDocument19 pagesThroid StormDurgesh PushkarNo ratings yet
- Case Study JatDocument45 pagesCase Study JatHSEINNo ratings yet
- Abnormal LabourDocument7 pagesAbnormal LabourSaman SarKo0% (1)
- Miconium Aspiration SyndromeDocument19 pagesMiconium Aspiration SyndromeEnna PaulaNo ratings yet
- Cholecystectomy (: Laparoscopic GallstonesDocument4 pagesCholecystectomy (: Laparoscopic GallstonesAlexia BatungbacalNo ratings yet
- Men in NursingDocument2 pagesMen in NursingMark JosephNo ratings yet
- LYMPHOMADocument12 pagesLYMPHOMAश्रीकृष्ण हेङ्गजूNo ratings yet
- Product Information Avil Product NamesDocument4 pagesProduct Information Avil Product Namesindyanexpress100% (1)
- Thrombolytic TherapyDocument16 pagesThrombolytic TherapyAnonymous nrZXFwNo ratings yet
- 130300-Standards For Acute and Critical Care NursingDocument12 pages130300-Standards For Acute and Critical Care Nursingapi-315277523No ratings yet
- Myocardial Infarction: Signs and SymptomsDocument5 pagesMyocardial Infarction: Signs and SymptomsKelly OstolNo ratings yet
- Cushings SyndromeDocument51 pagesCushings SyndromeTina TalmadgeNo ratings yet
- Dr. H. Achmad Fuadi, SPB-KBD, MkesDocument47 pagesDr. H. Achmad Fuadi, SPB-KBD, MkesytreiiaaNo ratings yet
- Asking Your Question (PICO) - NursingDocument5 pagesAsking Your Question (PICO) - NursingBentaigaNo ratings yet
- Oro & Nasopharyngeal SuctioningDocument16 pagesOro & Nasopharyngeal SuctioningHERLIN HOBAYANNo ratings yet
- Acute GlomerulonephritisDocument7 pagesAcute GlomerulonephritisSel CuaNo ratings yet
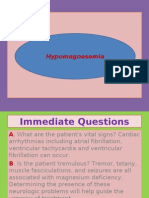
- HypomagnesemiaDocument7 pagesHypomagnesemiaNader SmadiNo ratings yet
- Surgical Treatment For BREAST CANCERDocument5 pagesSurgical Treatment For BREAST CANCERJericho James TopacioNo ratings yet
- 6 Managing Complications of IVTDocument42 pages6 Managing Complications of IVT4LetterLie31No ratings yet
- SmallpoxDocument3 pagesSmallpoxKailash NagarNo ratings yet
- Tracheostomy Care: PhysiologyDocument2 pagesTracheostomy Care: PhysiologyrajirajeshNo ratings yet
- DEFINITION: Abortion Is The Expulsion or Extraction From Its MotherDocument10 pagesDEFINITION: Abortion Is The Expulsion or Extraction From Its MothermOHAN.SNo ratings yet
- Case StudyDocument23 pagesCase StudyFarah Jelimae BagniNo ratings yet
- Hypertension Health EducationDocument5 pagesHypertension Health EducationOrlino PeterNo ratings yet
- Treatments and Drugs: by Mayo Clinic StaffDocument23 pagesTreatments and Drugs: by Mayo Clinic StaffJr D BayzNo ratings yet
- RBS and FBSDocument5 pagesRBS and FBSAllenne Rose Labja Vale100% (1)
- Pulmonary Function TestsDocument2 pagesPulmonary Function TestsSafuan Sudin100% (1)
- MSN CASE STUDY FORMATnew-1Document26 pagesMSN CASE STUDY FORMATnew-1Dinesh BanerjeeNo ratings yet
- Chronic Renal FailureDocument7 pagesChronic Renal FailureMary Jane Tiangson100% (1)
- Cerebral Aneurysm Case Analysis and Concept MapDocument5 pagesCerebral Aneurysm Case Analysis and Concept Mapate NarsNo ratings yet
- Wound AssessmentDocument19 pagesWound Assessmentdrsonuchawla100% (1)
- Burn RehabilitationDocument4 pagesBurn RehabilitationSuneel Kumar PrajapatiNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- The Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeFrom EverandThe Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeRating: 4.5 out of 5 stars4.5/5 (2)
- Ebstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandEbstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- CefuroximeDocument4 pagesCefuroximeColeen Comelle HuertoNo ratings yet
- Terminal Care What Is Terminal Care?Document6 pagesTerminal Care What Is Terminal Care?Coleen Comelle HuertoNo ratings yet
- FLUID and ElectrolytesDocument18 pagesFLUID and ElectrolytesColeen Comelle HuertoNo ratings yet
- Claudine Huerto MrsDocument4 pagesClaudine Huerto MrsColeen Comelle HuertoNo ratings yet
- Report PaperDocument1 pageReport PaperColeen Comelle HuertoNo ratings yet
- AldazideDocument1 pageAldazideColeen Comelle HuertoNo ratings yet
- Introduction of Africa and AsiaDocument9 pagesIntroduction of Africa and AsiaEllen Jane SilaNo ratings yet
- Eon 2019 Sustainability ReportDocument122 pagesEon 2019 Sustainability ReportDarryl Farhan WidyawanNo ratings yet
- Wild Magic Extended ListDocument6 pagesWild Magic Extended ListbeepboopbotNo ratings yet
- DJ X11Document113 pagesDJ X11AbrahamNo ratings yet
- Barbering M1 2nd SemDocument10 pagesBarbering M1 2nd Semjaymarnel1996No ratings yet
- Basketball-2 0Document46 pagesBasketball-2 0Catherine EscartinNo ratings yet
- Chapter 12Document58 pagesChapter 12reymark ramiterreNo ratings yet
- Protocol Document 1.1.4Document114 pagesProtocol Document 1.1.4Jose Daniel Zaraza Marcano100% (2)
- Mod 2Document150 pagesMod 2Prem SivamNo ratings yet
- WDM OTN Raman Feature Guide 05Document218 pagesWDM OTN Raman Feature Guide 05Ghallab Alsadeh100% (1)
- Gothra PattikaDocument172 pagesGothra PattikaParimi VeeraVenkata Krishna SarveswarraoNo ratings yet
- Autoclaved Aerated ConcreteDocument4 pagesAutoclaved Aerated ConcreteArunima DineshNo ratings yet
- Essay On All The Light We Cannot SeeDocument2 pagesEssay On All The Light We Cannot SeeJosh StephanNo ratings yet
- Different DietsDocument7 pagesDifferent DietsAntonyNo ratings yet
- Epidemiology and Public Health: Burton's Microbiology For The Health SciencesDocument33 pagesEpidemiology and Public Health: Burton's Microbiology For The Health SciencesMarlop Casicas100% (1)
- Official Ncm0200 Baird Parker Agar Base Technical Specifications en UsDocument3 pagesOfficial Ncm0200 Baird Parker Agar Base Technical Specifications en UsBty SaGNo ratings yet
- SIemens Air Damper ActuatorDocument40 pagesSIemens Air Damper ActuatorHENRYNo ratings yet
- Transport Management PlanDocument13 pagesTransport Management Planprmrao100% (3)
- Report Global Hemodialysis and Peritoneal Dialysis Market Size Estimates & Forecasts Through 2027Document235 pagesReport Global Hemodialysis and Peritoneal Dialysis Market Size Estimates & Forecasts Through 2027FaisalNo ratings yet
- IAAC Final Round 2020Document9 pagesIAAC Final Round 2020Dennil JobyNo ratings yet
- Updated Term Paper (5310) PDFDocument21 pagesUpdated Term Paper (5310) PDFSourae MridhaNo ratings yet
- Trends 11 Syllabus 5&6Document8 pagesTrends 11 Syllabus 5&6Victor John DagalaNo ratings yet
- Review Paper: There Are 5 Branches That We Choose To TasteDocument3 pagesReview Paper: There Are 5 Branches That We Choose To TasteAllysa BatoliñoNo ratings yet
- My Happy Marriage Volume 03 LNDocument252 pagesMy Happy Marriage Volume 03 LNnailsnailsgoodinbed100% (2)
- Equine Facilitated TherapyDocument100 pagesEquine Facilitated TherapyBasil Donovan Fletcher100% (1)
- LEAP Brochure 2013Document15 pagesLEAP Brochure 2013Reparto100% (1)
- NCR 7403 Uzivatelska PriruckaDocument149 pagesNCR 7403 Uzivatelska Priruckadukindonutz123No ratings yet
- Lasers in Oral MedicineDocument35 pagesLasers in Oral MedicineShreya singh0% (1)