Professional Documents
Culture Documents
100%(1)100% found this document useful (1 vote)
176 viewsPsy - Disord
Psy - Disord
Uploaded by
Shaz ChindhyThis document provides an overview of depression and schizophrenia. It discusses epidemiology, risk factors, pathophysiology, diagnostic criteria, treatment and course for each disorder. For depression, it notes the lifetime prevalence is 17%, females are affected twice as often as males, and risk factors include family history, childhood abuse, and medical illnesses. Treatment involves medication such as SSRIs, SNRIs, psychotherapy such as CBT, and lifestyle changes. For schizophrenia, it reports a lifetime prevalence of 0.5-1%, onset is typically in the late teens to mid-20s, and pathophysiology involves dysregulation of dopamine and glutamate neurotransmission in the prefrontal cortex and temporal lobes. Symptoms include positive symptoms such as
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- Reiki Manual LVL 2Document9 pagesReiki Manual LVL 2atosmdq79930% (1)
- Shadow Integration - The Complete Shadow Work Process in Four Steps - Words From The WindDocument15 pagesShadow Integration - The Complete Shadow Work Process in Four Steps - Words From The WindAR75% (4)
- Fundamentals Nursing Active Learning 1st Edition Yoost Crawford - Test BankDocument44 pagesFundamentals Nursing Active Learning 1st Edition Yoost Crawford - Test BankRaymondCenteno100% (3)
- Manual Handling Mini EbookDocument15 pagesManual Handling Mini EbookJohnPaulBascoNo ratings yet
- Second and Third Generation Antipsychotics: A Comprehensive HandbookFrom EverandSecond and Third Generation Antipsychotics: A Comprehensive HandbookRating: 5 out of 5 stars5/5 (1)
- Lac+Usc Internal Medicine Residency Survival Guide 2013-2014Document226 pagesLac+Usc Internal Medicine Residency Survival Guide 2013-2014Shaz ChindhyNo ratings yet
- Ancef Drug CardDocument1 pageAncef Drug CardSheri490No ratings yet
- Interpersonal Psychotherapy NewDocument119 pagesInterpersonal Psychotherapy Newdrkadiyala2100% (1)
- Prochaska & DiClemente (1982) Transtheoretical Therapy (Toward A More Integrative Model of Change) PDFDocument13 pagesProchaska & DiClemente (1982) Transtheoretical Therapy (Toward A More Integrative Model of Change) PDFSuryo HapsoroNo ratings yet
- Psychiatry Info - FinalDocument8 pagesPsychiatry Info - FinalH_QasimNo ratings yet
- Psych Ch. 7 Notes (Tutor)Document5 pagesPsych Ch. 7 Notes (Tutor)Haylle ThomasNo ratings yet
- Psych Ch. 5 NotesDocument7 pagesPsych Ch. 5 NotesHaylle ThomasNo ratings yet
- PSYCH 1.2A Mood DisordersDocument22 pagesPSYCH 1.2A Mood DisordersZaza100% (1)
- Kring Abnormal Psychology Chapter 5 Mood Disorders NotesDocument14 pagesKring Abnormal Psychology Chapter 5 Mood Disorders NotesAnn Ross FernandezNo ratings yet
- Pharmacology - (5) Psychotic DrugsDocument8 pagesPharmacology - (5) Psychotic DrugsSamantha DiegoNo ratings yet
- BEHS Disorders ChartDocument7 pagesBEHS Disorders ChartAndrew PatelNo ratings yet
- 10 Cognitive DisordersDocument16 pages10 Cognitive DisordersFarrah MaeNo ratings yet
- Just Getting The Main RX Names Down : Antidepressants Mood StabilizersDocument1 pageJust Getting The Main RX Names Down : Antidepressants Mood StabilizersCarlos Eduardo LinaresNo ratings yet
- Disorders of Thought & Speech (Psychopathology)Document21 pagesDisorders of Thought & Speech (Psychopathology)Upasana Baruah100% (2)
- 5 - Childhood Psychiatric Disorder (2017!06!02 23-15-39 UTC)Document60 pages5 - Childhood Psychiatric Disorder (2017!06!02 23-15-39 UTC)drillercz12zNo ratings yet
- Psych TemplateDocument1 pagePsych TemplateWilliam Yang100% (1)
- Sudden Onset (Within 2 Weeks) of at Least One of TheDocument2 pagesSudden Onset (Within 2 Weeks) of at Least One of TheNeicole BandalaNo ratings yet
- Psychopharmacology in PsychiatryDocument94 pagesPsychopharmacology in PsychiatryOslo Saputra100% (1)
- Neuroleptics & AnxiolyticsDocument65 pagesNeuroleptics & AnxiolyticsAntonPurpurov100% (1)
- Shortened REM Latency and Increased REM: Previous AttemptDocument19 pagesShortened REM Latency and Increased REM: Previous AttemptActeen MyoseenNo ratings yet
- Provisional: Borderline Personality Disorder Differential DXDocument6 pagesProvisional: Borderline Personality Disorder Differential DXhernandez2812No ratings yet
- AntipsychoticsDocument4 pagesAntipsychoticsRana MuhammadNo ratings yet
- Disorders Duration/Onset Symptoms/Manifestations Treatment: Childhood DDocument7 pagesDisorders Duration/Onset Symptoms/Manifestations Treatment: Childhood DActeen Myoseen100% (2)
- Psychiatric Nursing ReviewDocument44 pagesPsychiatric Nursing ReviewramemgarNo ratings yet
- Consultationliaison Psychiatry IcuDocument56 pagesConsultationliaison Psychiatry IcuChrisAlipioNo ratings yet
- Psychotropic Medication ReviewDocument7 pagesPsychotropic Medication ReviewAakash Shah100% (2)
- Epidemiological Data: Paper B Syllabic Content 7.xDocument5 pagesEpidemiological Data: Paper B Syllabic Content 7.xAnamika SinhaNo ratings yet
- Glossary of Psychiatric TermsDocument42 pagesGlossary of Psychiatric TermsÏtz ShãrîNo ratings yet
- Study Guide For The Psychiatry NBME Content Exam AKA The Psychiatry Shelf Exam!Document2 pagesStudy Guide For The Psychiatry NBME Content Exam AKA The Psychiatry Shelf Exam!DoriNo ratings yet
- Disorders of ThoughtDocument30 pagesDisorders of ThoughtRenault Jia Kai50% (2)
- Lecture No. 3 Semiology of Psychiatry Part 2Document26 pagesLecture No. 3 Semiology of Psychiatry Part 2ozgur.yonlukNo ratings yet
- Vascular DementiaDocument5 pagesVascular DementiaAna Ramos LopezNo ratings yet
- Antipsychotic Medication: Generic Name Trade Name Indications Contraindications Drug Interaction Side Effects Nursing ImplicationDocument6 pagesAntipsychotic Medication: Generic Name Trade Name Indications Contraindications Drug Interaction Side Effects Nursing ImplicationJaylord Verazon100% (1)
- Introduction To Psychiatric Nursing: Mercedes A Perez-Millan MSN, ARNPDocument33 pagesIntroduction To Psychiatric Nursing: Mercedes A Perez-Millan MSN, ARNPSachiko Yosores100% (1)
- Exam 1 2Document18 pagesExam 1 2api-444187370No ratings yet
- Mental Status Examination Rapid Record Form: CatatoniaDocument3 pagesMental Status Examination Rapid Record Form: CatatoniaNicole Tangco100% (1)
- DSM-IV Criteria MnemonicsDocument4 pagesDSM-IV Criteria Mnemonicsleonyap100% (2)
- Glossary of Psychiatric TerminologyDocument20 pagesGlossary of Psychiatric Terminologyphoebe_62002239No ratings yet
- AntipsychoticsDocument10 pagesAntipsychoticswawing16No ratings yet
- Psych Final BlueprintDocument10 pagesPsych Final BlueprintGrace LivingstonNo ratings yet
- Medication Conversion ChartDocument2 pagesMedication Conversion ChartIlinca mirnoviciNo ratings yet
- PSYCH 011 Clinical Diagnosis of Neurocognitive DisorderDocument7 pagesPSYCH 011 Clinical Diagnosis of Neurocognitive DisorderKaye NeeNo ratings yet
- DR - Usama.mahmoud Psychiatry - Notes MSDocument64 pagesDR - Usama.mahmoud Psychiatry - Notes MSMariam A. KarimNo ratings yet
- Child and Adolescent Psychiatry: A. Pervasive and Developmental DisordersDocument6 pagesChild and Adolescent Psychiatry: A. Pervasive and Developmental DisordersIsabel CastilloNo ratings yet
- Psychiatry Notes Psychiatry Notes: Medicine (Queen Mary University of London) Medicine (Queen Mary University of London)Document28 pagesPsychiatry Notes Psychiatry Notes: Medicine (Queen Mary University of London) Medicine (Queen Mary University of London)Noman ButtNo ratings yet
- Glossary of Frequently Used Mental Health TermsDocument6 pagesGlossary of Frequently Used Mental Health TermsWarren MillerNo ratings yet
- Study Guide Test 1Document11 pagesStudy Guide Test 1jwasylow13No ratings yet
- Initial Interview TemplateDocument4 pagesInitial Interview TemplateJoan ChoiNo ratings yet
- PMHNP Case Study - EditedDocument7 pagesPMHNP Case Study - EditedSoumyadeep BoseNo ratings yet
- Intro Child PsychiatryDocument122 pagesIntro Child PsychiatryayunisallehNo ratings yet
- DELIRIUM PresentationDocument26 pagesDELIRIUM PresentationAnkush Sharma100% (1)
- Substance Use DisordersDocument28 pagesSubstance Use DisordersAbdul NazarNo ratings yet
- Clozapine Care GuideDocument16 pagesClozapine Care GuideERWIN SUMARDINo ratings yet
- Pharmacotherapy in PschiatryDocument8 pagesPharmacotherapy in PschiatryygfhdgNo ratings yet
- Psycho-Pharmacotherapy: Major Tranquilizers, D2 - Receptor Blockers and Anti - Schizophrenic DrugsDocument29 pagesPsycho-Pharmacotherapy: Major Tranquilizers, D2 - Receptor Blockers and Anti - Schizophrenic DrugsPoonam RanaNo ratings yet
- Psychiatry MnemonicsDocument4 pagesPsychiatry MnemonicsHiruni Tharuka100% (2)
- 1 - Signs and Symptoms of Mental Illness-PartDocument49 pages1 - Signs and Symptoms of Mental Illness-PartAljoker FarragNo ratings yet
- Psychiatrypoisoning E.ODocument24 pagesPsychiatrypoisoning E.OZeenat JunaidNo ratings yet
- Anxiety/Depression: S AlprazolamDocument2 pagesAnxiety/Depression: S AlprazolamleesaNo ratings yet
- Psychiatric Diagnosis: Challenges and ProspectsFrom EverandPsychiatric Diagnosis: Challenges and ProspectsIhsan M. SalloumRating: 5 out of 5 stars5/5 (1)
- Pericardial Disease: Adel Hasanin Ahmed 1Document5 pagesPericardial Disease: Adel Hasanin Ahmed 1Shaz ChindhyNo ratings yet
- Cong HeartDocument7 pagesCong HeartShaz ChindhyNo ratings yet
- Me 1Document74 pagesMe 1Shaz ChindhyNo ratings yet
- ST NoDocument89 pagesST NoShaz Chindhy100% (1)
- I. Definition/General Considerations: Colon CancerDocument2 pagesI. Definition/General Considerations: Colon CancerShaz ChindhyNo ratings yet
- Endocrine Learning ObjDocument2 pagesEndocrine Learning ObjShaz ChindhyNo ratings yet
- Alcohol Dependednce Vs Abuse: Best TX Is Conseling + Drug. Combining Drugs Is NOT More EfficatiousDocument4 pagesAlcohol Dependednce Vs Abuse: Best TX Is Conseling + Drug. Combining Drugs Is NOT More EfficatiousShaz ChindhyNo ratings yet
- IMDocument128 pagesIMShaz ChindhyNo ratings yet
- I. Definition/General Consideration: Acute Asthma ExacerbationDocument2 pagesI. Definition/General Consideration: Acute Asthma ExacerbationShaz ChindhyNo ratings yet
- All of Medicine FlashcardsDocument142 pagesAll of Medicine FlashcardsShaz Chindhy100% (2)
- Cardio AnswersDocument26 pagesCardio AnswersShaz ChindhyNo ratings yet
- MKSAPDocument2 pagesMKSAPShaz ChindhyNo ratings yet
- Diabetes: Foot ExamDocument4 pagesDiabetes: Foot ExamShaz ChindhyNo ratings yet
- I. Definition/General Considerations: HypercalcemiaDocument2 pagesI. Definition/General Considerations: HypercalcemiaShaz ChindhyNo ratings yet
- Hiit On The GoDocument41 pagesHiit On The Godee138No ratings yet
- David A. Nicholls - The End of Physiotherapy (2017, Routledge) - Libgen - LiDocument378 pagesDavid A. Nicholls - The End of Physiotherapy (2017, Routledge) - Libgen - LiMina RizqinaNo ratings yet
- Dapsone 2Document2 pagesDapsone 2JeanMENo ratings yet
- Resume PDFDocument1 pageResume PDFapi-266278027No ratings yet
- Helfaer P. M. Positive Development For Persons With Trauma. USABPJ 9.2 2010Document14 pagesHelfaer P. M. Positive Development For Persons With Trauma. USABPJ 9.2 2010tonkoslavNo ratings yet
- Renal MedsurgDocument14 pagesRenal MedsurgCliff Lois ╭∩╮⎷⎛⎝⎲⏝⏝⎲⎠⎷⎛╭∩╮ Ouano100% (1)
- EphedraDocument9 pagesEphedraapi-367367047No ratings yet
- HDFC Life Critical Illness Plus Rider BrochureDocument8 pagesHDFC Life Critical Illness Plus Rider Brochurepinky_y2kNo ratings yet
- Farmacologia em Cães GeriátricosDocument12 pagesFarmacologia em Cães GeriátricosRafaela RodriguesNo ratings yet
- Neurosurgery 4 Mental DisordersDocument82 pagesNeurosurgery 4 Mental DisordersTomChristianNo ratings yet
- Guidance and Counselling.Document10 pagesGuidance and Counselling.Stacy SangmaNo ratings yet
- Resources#2 Severe Clutter LocalDocument1 pageResources#2 Severe Clutter LocalMargaret Pearson Pinkham100% (1)
- 10 Steps For Any Dilemma PDFDocument2 pages10 Steps For Any Dilemma PDFMitchell StroiczNo ratings yet
- tp53 Concept MapDocument1 pagetp53 Concept Mapapi-449993710No ratings yet
- The Bobath Concept (NDT) As Rehabilitation in Stroke Patients - Revisión SistemáticaDocument8 pagesThe Bobath Concept (NDT) As Rehabilitation in Stroke Patients - Revisión SistemáticaCristian Manuel Goicochea ChuqueNo ratings yet
- Sri LankDocument20 pagesSri LankVangeesa SumanasekaraNo ratings yet
- HIV and PregnancyDocument9 pagesHIV and PregnancyUm HamoOdNo ratings yet
- Principles of Hemodialysis: Module No: - 02 - Module TitleDocument10 pagesPrinciples of Hemodialysis: Module No: - 02 - Module TitleIan LelisNo ratings yet
- SBARDocument2 pagesSBARJason Kai Poth100% (1)
- Atraumatic Nursing Very FinalDocument50 pagesAtraumatic Nursing Very FinalLatha VenkatesanNo ratings yet
- Antiphospholipid SyndromeDocument6 pagesAntiphospholipid SyndromeOm Lakhani100% (1)
- Aversive ConditioningDocument4 pagesAversive Conditioningiulia9gavrisNo ratings yet
- Magnet Therapyncreasingly Gaining in Popularity The World OverDocument3 pagesMagnet Therapyncreasingly Gaining in Popularity The World OverPradeep PatilNo ratings yet
- Morse Fall ScaleDocument1 pageMorse Fall Scalecardiology serdangNo ratings yet
Psy - Disord
Psy - Disord
Uploaded by
Shaz Chindhy100%(1)100% found this document useful (1 vote)
176 views18 pagesThis document provides an overview of depression and schizophrenia. It discusses epidemiology, risk factors, pathophysiology, diagnostic criteria, treatment and course for each disorder. For depression, it notes the lifetime prevalence is 17%, females are affected twice as often as males, and risk factors include family history, childhood abuse, and medical illnesses. Treatment involves medication such as SSRIs, SNRIs, psychotherapy such as CBT, and lifestyle changes. For schizophrenia, it reports a lifetime prevalence of 0.5-1%, onset is typically in the late teens to mid-20s, and pathophysiology involves dysregulation of dopamine and glutamate neurotransmission in the prefrontal cortex and temporal lobes. Symptoms include positive symptoms such as
Original Description:
psy
Original Title
Psy- Disord
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document provides an overview of depression and schizophrenia. It discusses epidemiology, risk factors, pathophysiology, diagnostic criteria, treatment and course for each disorder. For depression, it notes the lifetime prevalence is 17%, females are affected twice as often as males, and risk factors include family history, childhood abuse, and medical illnesses. Treatment involves medication such as SSRIs, SNRIs, psychotherapy such as CBT, and lifestyle changes. For schizophrenia, it reports a lifetime prevalence of 0.5-1%, onset is typically in the late teens to mid-20s, and pathophysiology involves dysregulation of dopamine and glutamate neurotransmission in the prefrontal cortex and temporal lobes. Symptoms include positive symptoms such as
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
100%(1)100% found this document useful (1 vote)
176 views18 pagesPsy - Disord
Psy - Disord
Uploaded by
Shaz ChindhyThis document provides an overview of depression and schizophrenia. It discusses epidemiology, risk factors, pathophysiology, diagnostic criteria, treatment and course for each disorder. For depression, it notes the lifetime prevalence is 17%, females are affected twice as often as males, and risk factors include family history, childhood abuse, and medical illnesses. Treatment involves medication such as SSRIs, SNRIs, psychotherapy such as CBT, and lifestyle changes. For schizophrenia, it reports a lifetime prevalence of 0.5-1%, onset is typically in the late teens to mid-20s, and pathophysiology involves dysregulation of dopamine and glutamate neurotransmission in the prefrontal cortex and temporal lobes. Symptoms include positive symptoms such as
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 18
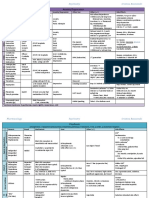
Psych disorders
Epidemiology Pathophysiology Risk factors Criteria Tx/Course Misc
Depression
MIXED
EPISODE =
DEPRESSI
VE
+MANIC
SYMPT
diathesis-
stress
framework-
more
vulnerable
Psychotic
depression=
delusions or
hallucinatio
ns with
depression
Seasonal D
RF: W,
young
adults, !
altitude
Life prev 17%
(does not vary
with SES or
ethnicity)
F:M 2:1
Med AoO 32
yrs
Males 3-4x
more likely to
complete
suicide
Women more
likely to attempt
suicide
Native Am and
Whites highest
rate of suicide
If committed
suicide - < 30
substance
abuse/personalit
y vs >30 mood
disorder
MDD = RF for
IHD
Learned helplessness- neg
cog. Style
Genetics- BDNF, COMT, 5-
HTTPR (short allele + child
maltreatment) diathesis-
stress
Neural circuitry/plasticity-
PFC, ant. cingulate,
amygdala, hippocampus. PFC
connections to inhibit
amygdala disrupted.
Monoamine H
0
-" 5-HT, NE,
& DA
Hormones- HPA axis:
stimulated by amygdala and
some PFC ! ! cortisol. Neg
FB impaired (on hippo, PFC,
hypothal, and pituitary). Low
test., thyroid, post-partum,
pre-menses
Psychosocial
For suicide:
" serotonin, tryptophan
hydroxylase. Mutation
For depression:
Gender (F),
MI/CAD, Fam hx,
Child abuse*,
Stressful events,
Neg. cog. style,
Previous dep.
episode, loss of
parent as child*,
substance use
disorders, anxiety
disorders, medical
conditions
For suicide: (sad
persons)
Gender (M with
gun/subs), Race
(W+NA), Marital
status for M, Age
(M 10-24, >65 and F
in 40s), Fam hx,
Mental illness
(bipolar/MDD),
Medical illness
(HIV, HD, CA, TBI,
Sz, spinal cord
injury), Recent loss,
Substance abuse,
Past attempt (MOST
imp)
Protective: religion,
social support,
marriage for men
Most people w/
multiple RF will
NOT complete
suicide
Episode= !5 for 2 wks (SIG
E CAPS)
Sad/suicidal
Interest (loss of)
Guilt
Energy
Concentration
Appetite/weight "
Psychomotor
agitation/redardation
Sleep
Disorder:
At least one episode, not d/t
other things...
Subtypes: psychotic
depression, seasonal affective
disorder, post-partum
Core symptoms of MDD:
dysphoric mood and
anhedonia
Vegetative Symp: change in
appetite/weight, sleep, loss of
energy, psychomotor
retardation
Atypical depression: !
appetite and sleep, can get
some pleasure from some
activities (Tx w/ SSRIs or
MAOIs)
40% remit after 1 yr
60% of pts will have another
episode and risk ! w/ more
episodes
Early episodes of relapse
assocd w/ stressors and older
episodes are not
Light therapy- seasonal
depression
Electroconvulsive (safe
pregnancy, cardiac/memory
compl)- Most effective for
severe or psychotic depression
Meds: SSRIs*, SNRIs*,
bupropion*, TCAs, MAO-Is,
atypical antipsychotics (+ BZD
for insomnia and anx, and
antipsychotics, T3, lithium, or
buspirone for augmentation)
Psychotherapy: CBT,
interpersonal (both for
mild/mod), psychodynamic (for
chronic or co-morbid)
Neuromodulation (ECT, vagal
nerve stimulation [VM PF],
rTMS)- enhancement of
neuroplasticity
Tx of comorbidities
Suicide prevention (lithium,
clozapine, dialectical behavior
therapy), support
" stigma
Exercise/diet (omega-3, SAM-
e)
Best tx: meds + therapy
Men- suicide risk ! sharply in
adolescence, plateaus, ! slightly
in mid-life, ! sharply in late life
Women- risk peaks in late 40s
Reserpine caused dep (blocked
VMAT which moved MOAs in
vesicles)
Test- 2 item pt health
questionnaire (PHQ-2)- asks
about sadness and anhedonia
(80 sens, 71 spec)
59% also have anxiety
disorder
24% also have substance use
As # of previous depressive
episodes goes up, risk of
stressor triggering another
episode goes ", just start for no
reason
Make sure you rule out
bipolar b/c treatments w/
antidepressants can lead to
mania in BP pts
Brain: PFC (stim HPA);
amygdal, hippocam & AC
(inhibit HPA)
GABA, glutamate- local
signaling
Post/Peripartum D= full MDD
1 mo of giving birth VS. post
partum blues
Adolescents w/o mental illness
have 13x suicide completion if
firearm present
Physical exercise heightens
plasticity
Dysthymic
disorder
Life prev 3% See depression, but less severe
and > 2 yrs
At least 2: CASE
Concentration, appetite, sleep,
energy. + low self-esteem and
feelings of hopelessness
Interpersonal therapy or
psychodynamic therapy
Double depression: pts w/
dysthymic disorder who
develop MDD
Schizophren
ia
Part of
psychotic/
thought
disorders
Deficit in
thought,
perception,
emotion
Anosognosi
a: not
recognizing
one has an
illness
Prev 0.5-1%
Onset 15-35,
Average in 20s
(M before F-27)
10-15% suicide
risk
0.7% have onset
40-59
70-90% smoke
tobacco
33% are
homeless
male=female;
blacks=whites
Schizophrenics:
low SES
Dx:
Low B12
DiGeorge
Temp lobe
epilepsy
Huntingtons
Wilson dz
Stimulants
Hallucinogens
Anticholinergics
Withdrawl from
EtOH/barbituate
s
PFC- Orbitofrontal/medial
area: affective/emotional
regulation. Dorsolateral:
allows executive function,
working memory, and
response shifting. " PFC
activity in these pts
Temporal lobe- regulates
thought/ perception. Active in
hallucinations. Abnl in
schizophrenic brains
DA system-
Mesocorticolimbic path: VTA
to PFC, accumbens, and temp
lobe (amyg and hippo).
Important for reward +
reinforcement. DA important
for thought/perception. DA
agonist ! psychosis. DA
antag ! antipsychotic.
Hypofrontality (" DA in
PFC) and ! DA in ventral
striatum
Glutamate- NMDA antags !
psychosis. ! glycine ! !
glutamate binding to NMDA
! improvement
Cognitive dysmetria H
0
:
disruption of neural net w/
PFC, ant. cingulate gyrus,
thalamus, temporal cortex,
and cerebellum
Imaging: enlarged ventricles
from atrophy, " PFC and/or
Genetics
Intrauterine injury
esp in 2
nd
tri (flu,
starvation)
Cannabis during
teens (debatable)
Low SES
(downward drift,
cause vs. effect)
Families w/ high
expressed emotion
Risk for poor
outcome: lower
premorbid IQ, male,
earlier AoO, neg sxs
and cog sxs, brain
abnormalities on
imaging, long
prodrome, no mood
sxs, obsessions,
compulsions, neuro
soft signs, fam hx
PATHOPHYS: the
inhibitory pathways
from PFC to limbic
areas and VTA !
disinhibition of VTA
! hyperactivity of
DA in
mesocorticolimbic
pathway /ventral
striatum!
!2 sxs for most of 1 mo but
disturbance persists for at
least 6 mo w/ prodromal or
residual sxs
Delusions, hallucinations,
disorganized speech,
disorganized behavior, neg
sxs
Cognitive sxs, positive sxs,
and negative sxs (affective
flattening, avolition, alogia)
Often see neuro soft signs:
poor coordination, R/L
confusion, gait impairment
different from extrapyramidal
Sx from drug tx
antipsychotics
Kurt Schneiders pos sxs: aud.
thoughts, voices arguing /
discussing / commenting,
somatic passivity experiences,
thought w/d / broadcasting,
delusional perception
Eugen Bleulers 4 As (neg
sxs): associational
disturbances, affective
disturbances, autism,
ambivalence
Nigrostriatal pathway is
involved in motor movement,
and dysfunction in this
pathway causes movement-
related neurological disorders
Prodrome (subtle sxs of
psychosis ie social withdrwl,
hygiene, anhedonia) months to
years before active phase.
Active phase develops over
weeks to months. Residual
phase is one option. 1/3 good
outcome, 1/3 moderate, 1/3 bad
Strongest predictors of poor
outcome include: lower pre-
morbid intelligence, male
gender, earlier age of onset, the
presence of negative and
cognitive symptoms, and the
presence of structural brain
abnormalities. Industrialized pt
have poorer outcomes
Meds: atypical antipsychotics*
(a/w EPS, NMS), try another if
1st doesnt work, typicals used
less commonly, clozapine for
tx-refractory cases.
Typicals- metabolic SE; atyp:
extrapyramidal SE
Psychotherapy: Psychosocial
rehab (teach living skills,
social networks, housing,
jobs, reintegration), assertive
community treatment program
(part of rehab), familial
psychoeducation, CBT
Tx of comorbidities- substance
use and mood disorders esp
20-40% attempt suicide, 10-15
complete
High rates of tobacco use
+ sym: Kurt Schneider:
delusions, hallucinations,
paranoia, perceptual
abnormalities
- sym: Eugen Bleuler: affective
flattening (emotional blunting),
anhedonia, avolition (difficulty
initiating or persisting goal
behavior), alogia (diminution
of thought and speech)
cognitive sym: disorganized
speech & behavior (hygiene),
dec cognitive function (IQ),
poor attention
Thought: integrating multiple
stimuli to make informed
decisions and execute goals
Perception: the process by
which the stimuli reach
conscious awareness; regulated
by temporal lobe which
includes lateral surface
neocortex, amygdala,
hippocampus, parahippocampal
gyrus
DA agonists (L-DOPA,
cocaine, amphetamines) cause
psychosis (thought disorder,
hallucinations)
Delusions,
hallucinations,
disorganized
speech
temp lobe gray matter,
cytoarchitectual abnormalities
in temp lobe and PFC area, "
frontal lobe metab.
GENETICS- neuregulin1,
dysbindin, COMT, BDNF
polymorphisms, complex
Other RFs: Injury during 2
nd
trimester,
Cannabis use in adolescents
hypoactivity of PFC
(hypofrontality) and
inc DA
(for example, Parkinsons
disease, and tardive
dyskinesia, which are side
effects of antipsychotics
cognitive dysmetria
hypothesis - symptoms of
schizophrenia arise from
disruption of neural network
in PFC, anterior cingulate
gyrus, thalamus, temporal
cortex, and the cerebellum
Antipsychotics- address + sym
Cog therapy- address psychosis
Psychosocial rehab- address
functional consequences of
psychosis
Family psychoeducation-
improve family support
Tx comorbid conditions-
substance abuse, mood
disorders
DA antagonists (especially D2)
are antipsychotic and normalize
schizophrenia
Schizophrenia has a premorbid
and prodromal phase prior to
diagnosis
Maternal influenza or
starvation in 2
nd
trimester !
schizophrenia
Schizoaffect
ive disorder
Pt meets schizophrenic criteria
+ has an episode of major
depression, mania, or mixed
for some time
Pt had delusions or
hallucinations w/o mood sxs
for 2 weeks
Mood problem present for
>30% of illness
Antipsychotic + antidepressant
(if dysphoric) or mood
stabilizer (if manic or mixed)
The course and prognosis of
schizoaffective disorder
appears to be better than
schizophrenia, but worse than
major depressive disorder and
bipolar disorder.
Hallucinations are sensory
perceptions in absence of
associated environmental
stimuli
Delusional
disorder
F>M Nonbizarre delusions for ! 1
mo
Never met schizophrenia
criteria
Functioning pretty good
If present, hallucinations are
NOT prominent and are related
to the content of the delusions.
Negative and cognitive
symptoms are not present
Delusions are fixed false beliefs
that cannot be explained on the
basis of the patients cultural or
spiritual background
Panic
disorder
Subtype of
anxiety
disorder
prevalence
of anxiety
disorders !
with " SES
SPONTAN
Lifetime prev
2-3% of F
0.5-1.5% of M
F>M
Av. Onset early
adulthood
Functional neuroanatomy-
PFC not inhibiting amygdala
like it shouldsds. 2 routes to
emotional response: low route
via amygdala, quick and dirty.
high route via cortex, slower,
more processing, then back to
amyg.
NTs and anxiety- need more
GABA and less glutamate, to
! inhibitory tone. NE and 5-
HT too elevated?
Stress and HPA- chronic
Race (W), SES
(lower), fam hx,
genetics >
environment
Recurrent panic attacks w/ 1
month of worrying about
further attacks (anticipatory
anxiety) or behavioral change
d/t attacks or concerned that
these panic attacks are not
medical
Attack: !4 sxs, sudden onset,
peak w/in 10 min
Palpitations, sweating,
trembling, SOB, choking, CP,
N, dizzy/light-headed,
Meds + psychotherapy
Meds: SSRIs*, SNRIs, TCAs,
MAO-Is, BZD for short term or
acute attacks
Psychotherapy: CBT, exposure
therapy
Higher rates of peptic ulcer dz,
HTN, death
Comorbid w/ depression and
etoh abuse
PANICS
Palpitations parathesia
abdominal distress
nausea
intense fear of dying, light
headedness
Chest pain, chills, choking
Sweating, shaking, shortness of
breath
EOUS
PANIC
ATTACKS
stress ! abnl activation of
HPA ! psych issues. See
adrenal hypertrophy,
atrophy in hippo.
Anxious temperament-
genetic, freezing w/ new
situations, predicts anxiety,
depression, and/or substance
abuse later on, a/w hippo and
amyg
Bio disturbances:
" catecholamines, abnormal
locus ceruleus , CO2
hypersensitivity (false
suffocation alarm), problem
w/ lactate metab, problem
w/ GABA system
Imaging: Abnl temporal lobe,
esp hypothalamus. PET shows
cerebral vasoconstriction.
Genetic certain alleles, amyg
fires up faster/stronger w/ fear
stimulus
derealization, fear of losing
control, fear of dying,
paresthesias, chills/hot flashes
Often develop agoraphobia:
intense anxiety about two or
more of these situations: using
public transportation
(including airplanes), being in
open spaces (e.g.,
marketplaces), being in
enclosed spaces (e.g., shops),
standing in line or being in a
crowd, or being outside of the
home alone.
Generalized
anxiety
disorder
Can have it
with panic
attacks
Lifetime prev
4-7% F>M
Av. Onset early
adulthood
See top paragraph of panic
disorder; see disturbances in
NE, 5HT, GABA in PFC &
amygdala
+
Genetics
Race (W), SES
(lower), fam hx,
environment >
genetics
Excessive anxiety and worry
for ! 6 mo
Plus ! 3 sxs of: sleep
disturbance, muscle tension,
easily fatigued, restlessness,
irritability, poor concentration.
STERIC
Meds + Psychotherapy
Meds: SSRIs*, SNRIs,
buspirone, BZD for short
term(SSRI+BZD;remove latter)
Psychotherapy: CBT, behavior
interventions- breathing,
relaxation, imagery
*first line*
! risk for depression and/or
substance abuse
lifelong prognosis
OCD
Subtype of
anxiety
disorder
Lifetime prev
2-3% F=M
prevalence but
onset earlier in
men
Av. Onset early
adulthood
See top paragraph of panic
disorder
+
NTs: too much 5-HT
Neuro findings: Abnl EEG,
abnl auditory evoked
potentials, growth delays, abnl
neuropsych test results
Race (W), SES
(lower), fam hx,
med conditions
(TBI, epilepsy, HD,
tourettes)
Poor prognosis risk
factors: yielding to
Ego-dystonic: pt feels
ashamed b/c disorder is
inconsistent w/ ideal self-
image
Must have either obsessions
of compulsions and know its
unreasonable or excessive
Meds + psychotherapy
Meds: SSRIs*, clomipramine
(TCA). SSRIs need to be
higher dose for longer time
period. Refractory cases- !
dose, add antipsychotic, surgery
(cingulotomy)
Comorbid w/ depression (80%)
or tics (involuntary
movements/vocalizations) and
Tourettes
Most common obsessions:
contamination, pathological
doubt, somatic, symmetry /
Whites>blacks
20-30% -
improvement in
their symptoms,
40-50%
moderate
improvement,
and
20-40% no
improvement or
worsening
Infection: PANDAS seen after
GA beta Strep infection, kids,
OCD w/ tics
Imaging: ! metab in caudate
and PFC. Think PFC for
planning and caudate for
motor programs
Genetics
See OCD with tics dubbed
PANDAS (Pediatric
Autoimmune
Neuropsychiatric Disorders
Associated after group A
Streptococcal Infections
Imaging: ! metab in caudate
of basal ganglia and PFC
Hyperactive ACC
compulsions,
childhood onset,
bizarre compulsion,
need for
hospitalization,
coexisting MDD or
PD.
Good prognosis:
good
social/occupational
adjustment,
precipitating event,
episodic course
Core symptoms of OCD are
obsessions (recurrent ideas)
and compulsions (recurrent
behaviors). Only 1 is reqd for
diagnosis
Obsessions create anxiety,
while compulsions attempt to
alleviate that anxiety.
Most common obsessions are
contamination and doubt
Psychotherapy: CBT, exposure
and response therapy , family
therapy
Clomipramine is gold std but
high SE
Non-serotonergic
antidepressants are not effective
for OCD.
20-30% have improvement
RULE of thirds
order, aggressive impulses,
sexual impulses
Most common compulsions:
checking, washing, counting,
need to ask/confess, symmetry
and precision, hoarding.
Poor prognostic variables for
OCD include: yielding,
compulsions; childhood
onset; bizarre compulsions; need
for hospitalization; coexisting
major depression or personality
disorder.
Favorable prognosis is
suggested by: good social and
occupational adjustment;
presence of a precipitating
event (such as pregnancy);
episodic symptom course.
Specific
phobias
/social
phobia/
social anx
disor
#1 mental
disorder in F, #2
in males
Social phobia a/w CRHR1
gene
Fear that causes avoidance,
anxious anticipation, or
distress when exposed to
trigger
Somatizatio
n disorder
0.2-2% life prev
5:1 F:M
Genetics
Somatization disorder can
occur with medical
illness like MS, SLE,
HIV , MG
hyperthyroidism.
Fam hx Somatic symptoms that cannot
be explained adequately on
basis of physical and lab exam
Fluctuations 6-9 mo of severe
sxs, 9-12 mo mild sxs
Periods of stress !
exacerbation
Dx hard b/c need to r/o med
conditions
Conversion disorder: related
disorder where pt has sudden
loss of sensory/motor function
w/o identifiable neuro cause
and pt appear unconcerned;
Psych factors seem contributory
PTSD Lifetime prev
~8%
2:1 F:M
Prev/PTSD
Traumatic
events: 50-60 /
Genetic predisposition +
stressor
Genetics: smaller hippo
HPA- low cortisol, d/t
enhanced neg FB
NTs: hyperactive
Type, proximity, and
severity of stressor
Fam hx, gender, hx
of prev trauma, lack
of soc support after
trauma, use of BZD
Sxs persist > 1 mo
Exposure (except TV)
Re-experiencing (flashbacks,
nightmares)
Avoidance sx
Hyperarousal (insomnia,
Meds: SSRIs* (esp sertraline
and paroxetine), $1-blockers
(prazosin- helps w/
nightmares), anti-convulsants,
atypical antipsychotics
AVOID BZDs! ! risk of PTSD
PTSD patients practice
avoidance
Comorbid with mood, anxiety,
13.6 %
Violence: 17 /
25 %
Sexual assault:
6 / 29%
War: high / 29%
Natural
disasters: 5 / 4
%
noradrenergic syst.
Classical conditioning - the
trauma (an unconditional
stimulus) is paired with
reminders of the trauma
(conditioned stimuli),
resulting in fear response even
in the absence of trauma.
or etoh, military
personnel, acute
stress disorder
irritability, hypervigilance)
The core components of
PTSD are exposure to trauma,
intrusive/ dissociative
symptoms, negative mood,
avoidance symptoms, and
hyperarousal
Pyschotherapy: cognitive
processing therapy type of
CBT w/ prolonged exposure
technique
Tx of comorbidities
50% of cases- remit w/in 3 mo
Many others- sxs last > 12 mo
substance use disorders
Acute stress
disorder
See PTSD, except sxs arise
immediately after trauma and
are " 1 month
+ !3 sxs during/after trauma:
sense of numbing/detachment,
" awareness, derealization,
depersonalization, dissociative
amnesia
Bipolar Lifetime prev:
4%
F:M 3:2,
F:M 1:1 in BPD
1
Med AoO = 25
yo
DIG FAST
Distractibility
Irresponsibility
seeks
pleasure without
regard to
consequences
(hedonistic)
Flight of
ideasracing
thoughts in
goal-directed
Activity in
goal-directed
/ psychomotor
Genetic 33-90% among twins
Imaging: enlarged ventricles,
impaired phospholipid
metabolism,! deep white
matter lesions (esp in frontal
lobes), " gray matter in parts
of limbic, ! metab in ant.
cingulate cortex, " metab in
PFC, " N-acetylaspartate in
various regions
HPA axis- ! cortisol d/t "
central glucocorticoid
signaling. ! IL-6, IL-8, TNF
Sleep deprivation d/t travel !
may trigger mania
Family history
Families w/ high
expressed emotion
! ! relapse rates
Life stressors
Hyperthyroidism,
stroke, HIV,
neoplastic tumors in
frontal lobe, MS are
medical conditions
associated with
mania
Most genetic
associated dz
Mania: ! 1 wk of ! 3 sxs- !
self-esteem or grandiosity, !
need for sleep (cardinal sx),
more talkative (pressured
speech), flight of ideas,
distractibility, ! goal-directed
activity or psychomotor
agitation, involvement in risky
activities
Mixed episode: meet criteria
for Manic episode and MDE
most of time !1 wk
Hypomania: does not impair
functioning, ! 4 days of
persistently elevated,
expansive (indiscriminate
enthusiasm), or irritable
mood (1 sx) ! 3 of the sxs
listed for mania.
BPD I: ! 1 manic or mixed
episode
BPD II: ! 1 MDE and !1
hypomanic episode but no
Acute manic/mixed: meds-
lithium*, valproic acid,
oxcarbamazepine, atypical
antipsychotics, BZD (as
adjunct). Psychotherapy
ineffective here.
Acute dep: Meds- lithium,
atypical antipsychotics,
lamotrigine. Psychotherapy,
ETC.
Maintenance: meds- lithium
(esp mania/mixed), lamotrigine
(esp dep), can combine ^,
valproic acid, atypical
antipsychotics.
Psychoeducation to !
adherence. " substance use.
Psychosocial: education, coping
mechs, interpersonal and
social rhythm therapy,
vocational rehab, credit
50% of pts attempt suicide, 10-
15% completion rate
Comorbid w/ substance use
(60%) and anxiety (50%)
Rapid cycling = pt w/ ! 4 mood
episodes per year, a/w younger
AoO, more MDE, suicide
attempts
Normal BPD: 4 mood episodes
per 10yr
Avoid anti-depressants unless
given w/ mood stabilizer:
triggers manic/mixed episode, !
cycling
Avoid ciprofloxacin, steroids,
psychostimulants such as
cocaine and amphetamines,
antidepressant medications,
glucocorticoids, and antibiotics.
Kindling- more frequent,
Agitation
" need for
Sleep
Talkativeness
or pressured
speech
manic or mixed episodes counseling severe, and refractory episodes
over time
Autism ~1/110 children
have an autism
spectrum
disorder
4-5:1 M:F
Av. Age of dx
3.1
Genes + environment
Prenatal insult (rubella,
CMV, thalidomide)
FMR1 gene in fragile X
TSC1 or TSC2 mutation in
Tuberous Sclerosis
PTEN gene ! macrocephaly
Advanced paternal
age
!6 w/ ! 2 from (1) and !1
from (2) and (3)
(1) social impairment.
Impairment in nonverb.
Behavior. Fail to devel. peer
r-ships. Lack of seeking to
share. Lack of
social/emotional reciprocity.
(2) impairment in
communication. Delay/lack in
spoken lang. Bad
starting/keeping convo.
Echolalia or pronoun reveral.
Lack of make believe play.
(3) repetitive and/or
stereotyped behaviors.
Preoccupation w/ stereotyped
pattern of interest and/or parts
of object. Routines. Repetitive
motor mvmnts.
Sxs noticed usually before 3
yo
Prog depends on level of social,
cog, and behavioral
impairments, but is usually
poor.
Tx: Speech, OT, classroom
interventions (high structure,
low student:teacher), social
skills training, parental
education/support.
ABA or Lovaas for social-
communication based therapy
Behavioral therapy to "
maladaptive behaviors and
reinforce good ones*.
Risperidone and aripiprazole
help w/ difficult behaviors.
Melatonin for sleep.
50-75% of kids have some
degrees of MR
50% of parents have concerns
before 12 mo of age
Regression seen in 25% of kids
Comorbid w/ seizures (25%),
pica (eating non food
materials), constipation,
feeding problems, psych
disorders, sleep disorders.
Delay = 2 SD below mean
Absolute indicators for eval:
*No single, meaningful words
by 16 months
*No communicative gestures
by 12 months
*No flexible 2 word phrases by
2 years
*ANY loss of ANY social or
language skill at any age.
Aspergers Nl except for significant
impairments in interpersonal
functioning or at school
Table 1 lists the most common mood disorders and the mood episodes associated with each.
Each mood episode will be described in detail below.
Table 1. Mood disorders and their associated mood episodes
Mood disorders
Mood episodes
major depressive
episode
manic episode hypomanic
episode
mixed features
major depressive
disorder
yes no no rarely
bipolar I disorder usually yes sometimes sometimes
bipolar II disorder yes no yes sometimes
Original table created by Dr. A. Walaszek
II. Epidemiology and Public Health Impact of Bipolar Disorder
The lifetime prevalence of bipolar disorder in the U.S. is 4%. It is estimated that only one-third
of patients are ever diagnosed and, of these, only one-third receive adequate treatment.
Women are more likely to have any bipolar disorder than men, with a ratio of 3:2, though bipolar
I disorder is equally common in men and women. The median age of onset is 25 years old, with
men having an earlier age of onset than women. The onset of bipolar disorder later in life (50
years or older) is rare and may be more likely to be due to medical conditions (mood disorder
due to general medical condition) or medications (substance-induced mood disorder). The
prevalence of bipolar disorder does not appear to vary by ethnicity.
Bipolar disorder is highly co-morbid with substance use disorders (60% of patients with bipolar
disorder) and anxiety disorders (50%). Most patients with bipolar disorder experience
depression and many have suicidal ideation. Completed suicide occurs in 10-15% of patients
with bipolar I disorder.
A World Health Organization survey of the global burden of disease found that bipolar disorder
was the 6
th
leading cause of disability due to non-infectious diseases. Episodes of bipolar
disorder can be associated with severe disruptions in interpersonal, social, and occupational
functioning, as described below.
III. Pathophysiology of Bipolar Disorder
The etiology of bipolar disorder is unclear, though it has been associated with a number of
biological and psychosocial factors.
Family studies, twin studies, adoption studies, and genome-wide scans indicate a clear genetic
component. First-degree relatives of patients with bipolar disorder are 7 times more likely to
develop bipolar disorder than control subjects. The concordance rate among monozygotic twins
is 33-90% and among dizygotic twins is 5-25%, depending on the study. Genome-wide
association studies have indicated heritability between 73% and 93%. No specific genetic
172
Childhood
disintegrativ
e disorder
Nl for first 2-10 yrs then loss
of skills ! severe devel.
disability. a/w rare metabolic
or epileptic syndrome. Poor
prog. lifelong care.
Retts
disorder
F>>M MECP2 gene mutation (X-
linked)
Mainly in females
Nl early development then
loss of developmental skills in
language, play, social, motor.
Deceleration of head growth
! postnatal microcephaly.
Sz common.
Pervasive
development
al disorder
NOS
NOS= not
otherwise
specified
4 of 12 characteristics listed in
autism dx
ADHD 8.6% prev in 8-
15 yo
M>F
Unknown, multifactorial
Genetic
Imaging- " brain vol, " gray
matter vol, " cortical
thickness in all lobes, ! white
matter vol
NT- a/w Epi, DA, NE
Psychosocial- stressful events,
emotional deprivation, family
disruptions
Pos corr w/ screen time
Fam Hx, dad w/
antisocial behavior,
mom w/ depression,
prenatal tobacco
exposure, young
maternal age at
birth, low BW,
premie
Persistence as adult
a/w fam hx of
ADHD, neg life
events, conduct
disorder, depression,
or anxiety
Must interfere w/ functioning
in ! 2 settings
Multiple informants
Sxs before age 7 for at least 6
mo
!6 Sxs of inattention OR
hyperactivity
Hyperactivity is first to show
up and first to remit (vs.
inattention)
Meds: psychostimulants
(methylphenidate,
dextroamphetamine) or
atomoxetine (nonstmulant)
Psych: " school distractions,
help w/ organizational and
study skills, social skills
training, train parents
*W/ stimulants, screen for heart
risk factors and perform routine
checks d/t rare chance of
sudden death when combined
w/ cardioactive meds
Often a/w anxiety, tics,
enuresis, conduct disorder,
depression, and later substance
abuse (if + conduct disorder)
Distinguish from mania where
sxs wax and wane, have
grandiosity or ! need for
sleep.
Usually remit between 12-20
but usually not before, 15%
persist into adulthood
Hyperactivity 1
st
sx to remit
while distractibility is last
Personality
disorders
Anti-social 1%
F and 3% M
Bipolar 2%
F>M
personality
disorder is an
enduring pattern
of maladaptive
traits that are
Genetics
Cloninger neurobio model-
temperament (novelty
seeking-DA, reward
dependence-NE, harm
avoidance-5-HT) + character
(persistence, self-directedness,
cooperativeness, self-
transcendence)
Five-factor model- openness,
Fam hx
Trauma/abuse
Change in
personality in mid-
life or late-life
unlikely to be d/t
PD, look for med
etiology
ASPD- since age 15 and now
> 18 yo. ! 3 sxs: failure to
conform to soc. norms,
deceitfulness, impulsivity,
irritability, reckless disregard
for safety of others/self,
consistent irresponsibility,
lack of remorse.
BPD- since early adulthood.
Difficult
BPD-
Meds: antidepressants for
dysphoria/anx, antipsychotics
for dissoc. / psychotic sxs,
anticonvulsants for mood
instability.
Psychotherapy: dialectical
behavioral therapy w/
validation, mindfulness,
Cluster A: Weird / odd
(paranoid, schizoid, &
schizotypal)
Cluster B: Wacky / emotional
(anti-social, BPD, histrionic,
narcissistic)
Cluster C: Worried / anxious
(avoidant, dependent, ob-comp)
ASPD- a/w substance use,
mood/anxiety disorders,
inflexible and
pervasive across
a broad range of
situations and
that cause
significant
distress or
impairment.
conscientiousness,
extraversion, agreeableness,
neuroticism (OCEAN)
Biologic factors-
trauma/abuse
Temp lobe and PFC big
influence on personality
!5 sxs: efforts to avoid
abandonment, unstable/intense
r-ships, identity disturbance,
impulsivity in 2 areas that can
be self-harming, recurrent SI
or mutilation, affective
instability, feeling empty,
anger issues, paranoid or
dissociative sxs
emotion regulation, distress
tolerance, and interpersonal
effectiveness skills
Avoid: BZD and tricyclics
ADHD, pathologic gambling,
suicide. Only 12% remit over
30 yrs.
BPD- ! suicide risk 70%
attempt, 10% complete, a/w
mood/anxiety disorders, PTSD,
eating disorders, substance use
disorders. Half persist > 10 yrs
Only disorder than includes
recurrent suicidal behavior in
definition
Cluster A Personality Disorders: hallmarks of eccentric or odd behavior with fear of
social relationships (they are Weird or Accusatory, Aloof, and Awkward)
No psychosis, but genetic association with schizophrenia
Paranoid:
- Suspicious, mistrustful, litigious
- Attributes responsibility for problems to others
- Projection is the main defense mechanism
Schizoid:
- Lifelong pattern of voluntary social withdrawal
- Limited emotional expression, content with social isolation
- Unlike avoidant personality disorder, schizoid is content with social isolation
Schizotypal:
- Peculiar appearance
- Odd thought patterns and magical thinking
- Interpersonal awkwardness
Cluster C Personality Disorders: hallmark of fearful or anxious behavior (they are
Worried or Cowardly, Compulsive, and Clingy)
Genetic association with anxiety disorders
Avoidant:
- Shy, sensitive to rejection, socially withdrawn
- Feelings of inadequacy, inferiority complex
- Desires relationship with others (vs. schizoid)
Obsessive-compulsive personality disorder:
- Orderly, stubborn, perfectionist
- Misnomer because there are no obsessions nor compulsions
- Preoccupation with control
- Ego-syntonic, unlike OCD patients that are ego-dystonic
Cluster B Personality Disorders: hallmark of emotional, dramatic or erratic behavior (they are
Wild or Bad to the Bone)
Genetic association with mood disorders and substance abuse
Histrionic:
- Dramatic
- Extroverted
- Emotional
- Sexually provocative and attention seeking behavior
- Overly concerned with appearance
- Inability to maintain intimate relationships
Narcissistic:
- Grandiosity
- Envy
- Sense of entitlement
- Lack of empathy
- May react to criticism with rage
- May demand "top" physician, best health care
Antisocial:
- Inability to conform to social norms
- Criminality
- Disregard for and violation of rights of others
- Considered conduct disorder if the patient is < 18 years old
Borderline:
- Unstable mood, behavior and interpersonal relationships
- Suicide attempts
- Boredom, emptiness, and loneliness
- Impulsiveness
- Splitting is the major defense mechanism used
Dependent:
- Lack of self-confidence
- Lets others assume responsibility
- Best treatment is dialectical behavior therapy (DBT)
Can get PD from neoplastic frontal lobe, temporal epilepsy, hyperthyroid, HIV, encephalitis
Substance
use
disorders
8.7% w/
substance abuse
or dependence
Etoh 5.9%
Illicit drugs
1.7%
DA- ! release in nucleus
accumbens and other limbic
regions, and PFC from VTA,
thought to underlie addiction
Genetics- 50% if dad is
alcoholic
5-HT- low in CSF !
impulsivity
Environmental- acceptance in
surroundings, parental
monitoring / discouragement
Defense mechs- denial,
rationalizing
Age- earlier use ! ! risk of
later dependence/abuse,
possibly d/t brain
vulnerability
Best predictor of
w/d severity is
previous w/d
severity. Severity !
as # of w/d !
Fam hx
Earlier use ! ! risk
of becoming
problem user
Substance abuse- 12 mo
period, at least one, failure to
fulfill duties, physically
hazardous situations w/ use,
legal problems, use despite
problems related to use. Never
met dependence criteria.
Substance dependence- 12 mo
period, 3 or more, tolerance,
w/d, taken longer or more than
intended, failed to cut down,
excessive time spent, other
activities reduced, continues
despite insight to problem
See table below for clinical
manifestation of intox and w/d
Etoh Intoxication: support
physiologically (check
breathing/airway, trauma) and
behaviorally. Psychotherapy
relapse prevention,
motivational enhancement and
12-step facilitation
W/D: etoh- BZD taper,
thiamine, Mg, anticonvulsants,
monitor BP. BZD- switch to
long acting and taper, use
anticonvulsants
Opioids- OD: Naloxone.
Longer term: buprenorphine
or methodone, clonidine/BZD
regimen, psychosocial support.
Stimulants- support, abstinence
Use/dependence: abstinence for
dependence, relapse prevention
CBT, motivational
Etoh intoxication depends on
gender, age, body weight, food
consumption
W/d from etoh or BZD can be
fatal, dangerous sxs = delirium,
psychosis and sz for etoh, just
sz for BZD.
First months- 1 yr most relapse
prone time, can be triggered by
stress, anger, exposure to drugs
or cues
Implications for HIV, hepatitis,
FAS, smoking related birth
defects
Dopamine- wanting, learning
reward (fires when something
happens that is good and
unexpected
Patients with personality disorders may pose a particular challenge in general medical settings,
where the symptoms of the disorders may interfere with the delivery of medical care and with the
patient-physician relationship. Table 4 lists interpersonal strategies that may be useful in such cases.
Table 4. Characteristics of personality disorders and recommended approaches
personality
disorder
common interpersonal style recommended interpersonal
approach
dependent clinging limit-setting, reassurance of
ongoing involvement
obsessive-
compulsive
insistence on rules and high
standards
logical suggestions, permission to
modify self-expectations
paranoid accusations and
(counter)attacks
non-defensive acknowledgement of
underlying fears, encouragement
narcissistic entitled, putting others down non-defensive collaboration
histrionic theatrical, charming (alternating
with despair)
consistent, stabilizing
responsiveness
antisocial exploitation of others limit-setting, with legal backup if
necessary
borderline alternating between idealizing
& devaluating
validating, but with appropriate
limit-setting
Adapted from Howell & Walaszek, Emotional and behavioral problems, in The Practice of
Geriatrics, 4e, eds. Duthie, Katz & Malone (2008)
230
enhancement, 12-step
facilitation. Meds for etoh
relapse: naltrexone (opioid-R
antag, helps w/ pos reinforce.),
acamprosate (block NMDA-R),
disulfiram (ADHase antag). For
opioid relapse: methadone,
buprenorphine
Opiods- liking, hedonism
Nucleus acumbens relay both
The predominant cell type in
the striatum is the medium-
spiny neuron
Tolerance: Progressively diminished physiological response to a drug with
repeated drug exposure, often defined operationally as a rightward shift in the
dose-effect function.
Sensitization: Progressively augmented physiological response to a drug with
repeated drug exposure, often defined operationally as a leftward shift in the
dose-effect function.
Dependence: A physiological state induced by repeated exposure to a drug, in
which presence of the drug is required for the system to function normally. In a
drug-dependent system, removal of the drug often precipitates a withdrawal
syndrome
Craving: A subjective state of intense desire for a particular goal, such as for a
drug of abuse. It is often operationalized as a state of increased motivation to
obtain a particular goal, or a narrowing of focus such that one goal is pursued at
the expense of others.
Addiction: a) loss of control over limiting drug intake, (b) drug-taking persists
despite negative consequences, (c) a narrowing of the motivational/emotional
repertoire such that alternatives to drug-seeking (work, relationships, leisure
activities) are no longer pursued, (d) the potential for relapse throughout the life-
span, regardless of successful treatment interventions or long periods of drug
abstinence.
Reinforcement: The process by which the outcome of a behavior increases the
likelihood that the behavior will be repeated. Examples: a hungry rat presses a
lever and gets a food pellet (positive reinforcement); a rat presses a lever to
avoid an electrical shock (negative reinforcement).
Reward: Often defined as the subjective emotional experience (pleasure,
euphoria, hedonia) that can accompany positive reinforcement.
Impulsive behavior: There are two features of impulsive behavior that are particularly
relevant to addiction: (1) the tendency to consistently choose immediate reinforcement
over delayed gratification, even when the immediate reinforcement is smaller or less
beneficial; (2) an impairment in the ability to inhibit a course of action once initiated.
This could occur in cases of excessive wanting of drugs or drug-related stimuli, such
that inhibitory control mechanisms are overwhelmed.
Compulsive behavior: Perseveration in a certain behavioral strategy even in the face of
unsuccessful or adverse outcomes.
Incentive-sensitization hypothesis: drug use leads to a long-lasting sensitization of
dopamines ability to produce drug wanting
Reward-error prediction hypothesis: enhanced dopamine release during drug taking
produces a condition in which ALL stimuli encountered during drug use are experienced as
being better than expected.
Compulsive behavior: In addiction, individuals often report wanting the drug more
even though they like it less. They also want the drug despite adverse outcomes (i.e.,
loss of jobs or relationships).
Impulsivity: thought to result from impaired function of PFC inhibitory control
Compulsivity: Thought to result from a shift from prefrontal-accumbens motor
circuits to an emphasis on dorsal striatal control. Dorsal striatum is thought to
mediate habits
addiction has the following stages:
binge/intoxication, in which the acute euphorigenic or rewarding
properties of the drug are critical, and during which drug-induced
dopamine release promotes cellular processes of learning and
memory; cocaine primarily causes elevations of NE, DA, and 5-
HT, while alcohol has primary effects on mu-opioids, DA,
GABA, and glutamate.
withdrawal/negative affect, in which drug-seeking
behavior is motivated by the attempt to alleviate
physical/emotional withdrawal symptoms;
anticipation/preoccupation, which can persist through
the lifespan, in which strongly overlearned drug cues can
promote relapse, because frontal deficits promote
impulsive and compulsive behavior patterns in response
to overlearned drug cues.
Naloxone reverse opiod intoxication
Withdrawal from alcohol or benzodiazepines can be life
threatening, while withdrawal from opioids and stimulants is
almost never life-threatening but is extremely
uncomfortable.
opiods- vomiting, muscle aches,
stim- overeating, craving, depressed
Eating
disorders
F ~ 14-24
anorexia 1%,
BN 4% . M rate
1/10 of F rate
Anorexia onsets
usually 14-18
BN usually 17-
27
Unclear
Genetic
Environment
Neurochemical disturbances-
! NE activity, " 5-HT
activity, activation of HPA
axis, suppression of thyroid
fx, opioid involvement
(blocking helps)
BN- binge eating with purge
AN- dangerously low body
weight, afraid of gaining,
distorted perception
between weight and body
image, may engage in binge
eating and purging.
Subdivided into restriction
Fam hx
Predictors of poor
outcomes: longer
duration of illness,
older age at onset,
prior psych
hospitalizations,
poor pre-morbid
adjustment, +
personality disorder
AN- 85% of expected weight,
fear of gaining weight,
disturbed perception, self-
eval, denial, amenorrhea
BN- ! 2x/week for 3 mo:
eating w/in 2 hr period more
than nl person and sense of
lack of control, compensatory
behavior, self-eval tied to
body
Effects of starvation: lose
weight, cold, no energy, HR
and BP ", constipation,
obsessed w/ food, " libido,
depression, mood swings,
attention problems
Restore nutritional state
(slowly, dont want re-feeding
syndrome), modify eating
behaviors, change beliefs
CBT, interpersonal
psychotherapy (for BN),
Maudsley method (for AN <
18 yo living at home),
Fluoxetine (AN BN), atypical
antipsychotics (AN BN),
naltrexone (BN; opiod antag),
ondansetron (BN; antiemetic
5HT3 antag)
Treat co-morbid dep, anx, etc
Contraindications: tricyclics
(AN-arrhythmias), bupropion
(AN BN- szs)
Co-morbid w/ depression,
social phobia, OCD
AN: Severe consequences-
dehydration, hypothermia,
bradycardia, hypotension,
electrolyte disturbance also low
testosterone, hypogonadism,
cog impairment
BN: consequences- " Ca or K,
met alk, EKG change, fatty
degen of liver, malnutrition,
parotid gland enlargement,
Russells sign, dental caries,
esophageal tears
AN subtypes- restricting and
binging/purging type
BN subtypes- purging and non-
purging
Use of anticonvulsants treats this unopposed opponent process state by modulating glutamate
function. See Table 3 for other treatments.
Table 3. Treatment of Selected Withdrawal Syndromes
Substance Treatment
Alcohol Most common treatment is benzodiazepine taper (plus thiamine,
magnesium, as needed, and support) using CIWA scale for
repeated assessment of symptoms; some now use
anticonvulsants (e.g., gabapentin)
Benzodiazepines Most common is switch to long acting benzodiazepine and
taper; some now using anticonvulsants.
Opioids Can use buprenorphine or methadone with special license; can
use clonidine/benzodiazepine regimen; intense psychosocial
support
Stimulants (cocaine/
methamphetamine)
Support; get into treatment for abstinence as soon as possible
VI. Clinical Presentation and Treatment of Substance Use Disorders
A. Diagnosis of Substance Use Disorder
While many users of substances remain in control of their drug use without significant
dependence, a significant number develop either a substance use disorder. Because there is such
a large difference between use and dependence rates (especially in the case of alcohol), doctors
need to screen not for use of alcohol but for the hazardous use of alcohol. NIAAA has set 14
drinks/week and no more than 4 drinks on any one occasion as the upper limit of relatively safe
drinking for healthy men under 65 and 7 drinks/week and no more than 3 drinks on any one
occasion as the upper limit of relatively safe drinking for healthy women under 65. Commonly
used screenings tools for alcohol use disorders including the CAGE and the AUDIT. The
diagnostic criteria for alcohol use disorder are in Table 4.
B. General Principles of Treatment
Both acute and long-term treatment are critical because substance use disorders can be chronic
and relapsing. For substance dependence, abstinence is the most risk-free approach to take with
drinking in terms of maximizing chances at a long and happy life. Unfortunately, relapse to use
of the substance on which one is dependent is frequent, frustrating, and expectable. Therefore
the goal of most treatment is to prevent relapse but a relapse should always be regarded as an
opportunity to learn how to improve ones next effort at abstinence.
The first months to year is the most relapse-prone time for most substances, though some relapse
risk probably lasts permanently (since some brain changes induced by drugs are probably
permanent.) This state is much like that described in studies of relapsing addicts in which stress
and anger, as well as exposure to drugs or drug cues, led to relapse. So, the period early in
abstinence/recovery is marked by negative moods, craving, less pleasure in life, and more
negative response to stress.
197
Table 1. Clinical Manifestations of Intoxication with Selected Substances
Substance Low level Intoxication Severe Intoxication
Alcohol Pleasant (sometimes
euphoric) state, diminished
coordination, impaired
judgment
Aggression, poor judgment,
somnolence, severe decrease in
coordination, slurring of words,
loss of gag reflex, apnea
Opioids Euphoria followed by
somnolence, miosis
Somnolence, apnea, death
Cocaine and other
psychostimulants
Euphoria, inaomnia, intense
concentration, loss of
appetite
Anxiety, psychosis, agitation,
seizures, cardiac/cerebral
ischemia
Hallucinogens Intense change in perceptual
state leading to unusual
visual, auditory, and other
sensory experiences
Intense, more hallucinatory state
bordering on psychosis with
impulsive acts related to
perceptions
Different people will achieve these levels with different amounts of alcohol, with the amount
required varying based on gender, age, body weight, and recent food consumption with females,
older, and smaller people who havent eaten recently requiring much less alcohol consumption to
achieve the same blood level.
B. Treatment of Alcohol Intoxication
Treatment of alcohol intoxication is primarily supportive physiologically (i.e., making sure
breathing is not compromised, assessing for trauma a common, often unreported event in
intoxicated people and other medical problems and treating as needed) and psychologically (as
intoxicated people are often belligerent and impulsive, i.e., they may become violent or decide
suddenly to leave the emergency room to drive home).
There is no pharmacologic mechanism to reverse alcohol intoxication. The treatment of
intoxication with stimulants, opioids, and hallucinogens is also primarily supportive with the
length of time for support varying widely depending on half-life of the drug ingested. For
example, cocaine has a half-life of a couple of hours compared to methamphetamine, which is
several times that, and heroin has a similarly brief half-life compared to methadone. It should be
noted that one can use naloxone to reverse opioid intoxication. Finally, one should test for other
substances in the blood or urine of anyone who comes in intoxicated reportedly on one drug no
matter what history is given by the intoxicated party.
Alcohol is metabolized in most people at the rate of one standard drink per hour, meaning that if
one drinks no more than a one standard drink (1.5 ounces of liquor, 5 ounces of wine, 12 ounces
of beer) per hour, one will probably never be significantly impaired and that, if one has drunk
rapidly to achieve ones favorite alcohol level, it will take one drink per hour to maintain that
level. This metabolic rate translates to 20 to 30 mg/dL per hour for all blood levels > 100
mg/dL. This means that if someone comes in with a blood alcohol level of 300 mg/dL it will
take between 6.7 and 10 hours to get down to 100 mg/dL. This is important to realize as one
works with an intoxicated person who needs medical care or as one plans for support during the
intoxicated period.
195
V. Clinical Presentation and Treatment of Withdrawal
A. Withdrawal Syndromes
Cessation of the use of a substance, in particular one on which a patient has become
physiologically dependent, results in withdrawal. The nature, duration and severity of
withdrawal depend on the substance (Table 2). Withdrawal from alcohol or benzodiazepines can
be life threatening, while withdrawal from opioids and stimulants is almost never life-threatening
but is extremely uncomfortable. Severity of alcohol or benzodiazepine withdrawal must be
accurately assessed using standard scales and treated appropriately with supportive care as well
as pharmacologic intervention. The duration of withdrawal from substances will vary
dramatically according to the half-life of the abused substance.
It should be noted, however, that patients have a wide range of severity of withdrawal responses.
Some have severe withdrawal symptoms after relatively brief careers of alcohol use, while
other with more severe illness can have few symptoms. The best predictor of withdrawal
severity in alcohol withdrawal is previous withdrawal severity; severity of alcohol withdrawal
increases as the number of withdrawals in ones life increases.
Table 2. Common Withdrawal Syndromes
Substance Common Symptoms/Signs Dangerous
Symptoms
Timeline
Alcohol Anxiety, nausea, tremors,
sleeplessness, restlessness,
sweating, headaches, rapid
pulse and high blood pressure
Psychosis,
delirium,
seizures
Common symptoms
usually subside in 72-96
hrs; DTs can last 10+
days
Benzo-
diazepines
Anxiety, nausea, tremors,
sleeplessness, restlessness,
sweating, headaches, rapid
pulse, and high blood pressure
Seizures Entirely dependent on
half-life of drug and its
metabolites (varies from
days to weeks)
Opioids Nausea, vomiting, craving,
rhinorrhea, diarrhea, tearing,
muscle aches and cramps,
gooseflesh, dilated pupils
Dehydration
from diarrhea
and vomiting;
leaving care to
get more drug
Entirely dependent on
half-life of drug and its
metabolites (varies from
days (heroin/morphine)
to weeks (methadone)
Stimulants
(cocaine/-
metham-
phetamine)
Tired, prolonged sleeping,
amotivational, depressed,
overeating, craving
Will leave to
get more drug
Cocaine is shorter than
methamphetamine, which
has longer half-life
B. Treatment of Withdrawal
The aim of the treatment of alcohol withdrawal is to make patients comfortable and to avoid
seizures, severe hypertension, and delirium. Use of benzodiazepines is aimed at offsetting the
unopposed, opponent process of decreased GABA and increased glutamate function (as
benzodiazepines increase GABA function) and then the benzodiazepine can be tapered slowly.
196
type and bing type
Refeeding syndrome: resp
failure, cardiac failure,
hypotension, irreg. heartbeats,
sz, coma, sudden death. Avoid
by initiation of lower calorie
intake that is slowly advanced
and includes lytes and vits as
need
ED NOS- dx when pt doesnt
fit BN or AN exactly
Dementia /
Alzheimers
Amnesia
Agnosia
Apraxia
(unable to
do known
motor funct-
tying shoes)
Executive
function
aphasia
AD in 6% of ppl
> 65 yo, 20% >
85 yo, 45% > 95
yo
AD accounts for
50% of
dementia cases
Unknown.
Loss of neurons and synapses.
Loss of neurons ! ! ACh
and somatostatin.
Genetic (AD, prescenilin1 and
2 on chrom 14 and 1).
Imaging shows- cerebral
atrophy most prom. at frontal
and temp lobes, widened
sulci, atrophic narrowed gyri.,
hydrocephalus ex vacuo.
Histo- Amyloid plaques-
senile plaques, amyloid
deposited in vessel walls-
amyloid angiopathy, sig " in
hippocampus. Neurofibrillary
tangles. Microglial activation
Low-grade inflam
Amyloid H
0
: AB amyloid
builds up, cell death, lose
cholinergic systems first !
memory impairment
Risk " w/ age,
genetics (apoE-e4
allele), fam hx, TBI,
late-life depression,
CV risk factors,
excessive etoh
Protective: ApoE-e2
allele, NSAIDs,
statins, 1 drink etoh
per day, omega 3
FAs, exercise,
cognitive
stimulation
Gradual onset and continuing
cognitive decline
Memory impairment +/-
aphasia, apraxia, agnosia,
executive dysfunction
Age is the single most
powerful predictor of
alzheimers. Once hit 95 then
you are good.
-Less common causes of
dementia include
Huntingtons disease,
Creutzfeldt-Jakob disease
(prion disease),
neurosyphilis, Wernicke-
Korsakoff syndrome (i.e.,
dementia due to severe
alcohol use), repeated head
trauma (e.g. chronic traumatic
encephalopathy found in
professional football players),
CNS tumors, and HIV/AID
Cog enhancing drugs:
donepezil, galantamine,
rivastigmine, memantine
For behavioral and psych sxs,
behavioral interventions then
SSRIs or atypical
antipsychotics if no relief.
Treat caregivers (33% have
depression)
Plan for future while pt can
make decisions
6-12 yrs btwn dx and death.
Meds delay progression 6-12
mo.
Be weary of psuedodementia
person actually has
depression rather than
dementia
First get mild cognitive
impairment 2-3 yrs prior to
onset of dementia.
Caution w/ atypical
antipsychoitcs b/c risk " mort
in dementia pts
STM- occurs independent of
medial temporal lobe but if
need to retrieve STM then need
medial temporal lobe
STM is span of awareness in
the moment
HM has a pure global amnesia
(med temp lesion; not a
neurodegenerative dz) because
his nondeclarativ memory is
intact
Hippo- critical for time-limited
period of consolidation of
information into LTM
Episodic vs semantic (facts)
Vascular
dementia
~Age 65-75
(younger than
AD)
Cardiac risk factors
(HTN, high chol)
d/t cerebrovascular dz.
Manifestations depend on
location/extent of dz. Strokes.
Step-wise course, each
change thought to be d/t CVA.
Donepezil, galantamine,
rivastigmine, memantine may
help
Treat vascular risk factors
(statins, ACE-I, etc)
Asian japan have equal rate of
vascular an reg alzeimers
Dementia w/
lewy bodies
Characteristics: Fluctuating.
Visual hallucinations. Cog.
impairment. Less severe
parkinsonian sxs.
Lewy bodies found in cerebral
cortex
DLB often coexists w/ AD.
Donepezil, galantamine,
rivastigmine, memantine may
help
Parkinsons dz dementia also
gets dementia later, Lewy body
development in subcortical
regions
Frontotempo
ral dementia
AoO ~50-65 yo
Fam hx of early-
onset dementia
Characteristics: Tau inclusion
bodies, lobar degen. of frontal
and/or temp. lobe, behavioral
disturbances and/or aphasia.
Sxs: apathy, amotivation,
anergia, disinhibition,
impulsivity, irritability
More rapid course, death
usually w/in 5 yrs of dx.
No meds/treatment
Collection of diseases
(including Picks dz)
Other causes
of dementia
Mixed dementia (combo of
above causes), HD, CJD,
neurosyphilis, Wernicke-
Korsakoff, repeated head
trauma, CNS tumors,
HIV/AIDS
Reversible causes: depression
(pseudodementia),
hypothyroidism, VitB12
deficiency, NPH, subdural
hematoma
Delirium
also called
Major
neuro-
cognitive
disorder
0.8% in
community.
60% of nursing
home residents
> 75
Toxic: sed-hyps, anti-ACh
meds, opiates, steroids, abx
(quinolones), etoh w/d, sed-
hyp w/d
Metabolic: hypo/hyper
Na/Ca/sugar. Hypoxemia,
hypercapnia. Renal failure
(uremia), hepatic failure (hep.
encephalopathy)
Infectious: UTI, pneumonia,
meningitis, encephalitis,
sepsis, CNS abscess.
Other: TBI, CVA, epilepsy,
cardiac ischemia/arrhythmia,
pain, constipation,
dehydration, nutrition, sensory
deprivation (like from hearing
Age,
cerebrovascular dz,
neruodegen. dz,
chronic medical
conditions, recent
surgery, being in
unfamiliar
environment, taking
psychotropic meds,
malnutrition
Sudden onset, reversible
Acute alteration of mental
status
Waxing and waning sxs
Impairment of attention
Altered level of consciousness
Assoc. sxs: disorientation,
probs w/ sleep-wake cycle,
perceptual disturbances,
paranoia, memory loss,
emotional probs.
15% of pts die w/in 1 mo
25% of pts die w/in 6 mo
Tx of underlying condition,
discontinue suspect meds
Can give atypical antipsychs
for agitated pts
Avoid BZD except w/ etoh w/d
DELERIUM- duration hours to
days, abrupt onset, sxs wax and
wane, common causes- toxic,
metabolic, infectious.
Reversible
DEMENTIA- duration months
to yrs, insidious onset, sxs
slowly progress, common
Assessment: Mini-Mental
status exam, SLUMS, Animal
naming, Clock Drawing, Mini
Cog
Complications: pneumonia,
decubiti (skin breakdown) !
infection
Confusion assessment method:
94% sens, 90% spec to dx
delirium. PPV 91%.
Delerium is reversible
Table 1. Types of Long-Term Memory (LTM)
Key Feature Declarative LTM Nondeclarative LTM
Kind oI inIormation
remembered
Facts and events Skills, habits, and stimulus-
response associations
Rate oI acquisition Rapid (and oIten on just one
trial)
Slow (and oIten requires
repeated exposure)
Entails awareness oI the
inIormation being
remembered
yes no
Is amenable to volitional
retrieval
yes no
Typically impaired in
anterograde amnesia
yes no
Within the domain oI declarative long-term memory (LTM), there are several important
distinctions. For some inIormation, we remember the who, where, and when associated
with it. (For example, think oI what you ate Ior dinner last night you not only remember
the actual Iood that went into your mouth, you also remember who else was at dinner
with you, where you ate, and roughly what time it was.) This is reIerred to as episodic
memory, because together with the Iact in question (e.g., what you ate) you also
remember the episode in which this eating took place (i.e., the who, where, and when).
This additional inIormation is oIten reIerred to as the context or the source oI the
memory.
For other kinds oI memory, however, retrieval is not accompanied by the related episodic
inIormation. For example, the word 'memory. You know its deIinition, and the Iact that
you didn`t have this knowledge at birth means you must have learned it at some point in
your liIe; thereIore it is a memory. However, it is highly unlikely that anyone reading this
can remember who taught them the deIinition oI 'memory, where they were when this
inIormation was acquired, or when the learning took place. This is reIerred to as a
semantic memory, because it contains Iactual inIormation but is not associated with a
speciIic episode Irom the past.
B. Retrieval of Memory
Episodic memory can be retrieved via one oI two broad classes oI retrieval: recall or
recognition. A test oI recall would be 'What did you have Ior dinner last night? A test oI
recognition would be 'Here are pictures oI a pizza, a salad, and a bag oI chips; which oI
these did you eat Ior dinner? (This would be a 3-alternative Iorced-choice recognition
test. A yes/no recognition test, in contrast, might be 'Did you eat pizza Ior dinner last
night?) We perIorm both kinds oI memory retrieval hundreds oI times each day. Tests oI
recognition are easier than tests oI recall because recognition necessarily provides cues
('hints) that can aid in retrieval.
235
impairment), changes in
environment. Multifactorial.
causes- neurodegen. disorders,
cerebrovascular dz. Rarely
reversible
Insomnia 10-15% of ppl
report insomnia
sxs
Autonomic NS: ! activation
HPA axis abnormalities
EEG: shows ! % and #
activity (hyperarousal)
PET: ! brain glucose metab
overall
Genetics: a/w short allele of
5-HTTPR
Psych: these pts more reactive
to stress and more prone to
worry, vicious cycle, negative
associations toward sleep,
maladaptive behaviors
Age (older), gender
(F), personality traits
(anx), past hx of
insomnia, fam hx of
insomnia,
psychiatric disorders
(anx, dep), medical
problems, stress
One or more: difficulty falling
asleep, maintaining sleep,
waking up too early,
nonrestorative sleep
At least one daytime symptom
Treat any underlying causes or
comorbid conditions. Promote
good sleep habits via education.
CBT.
Meds: BZDs, zolpidem,
eszopiclone, melatonin R
agonists, sedating
antidepressants trazadone and
mirtazapine, atypical antipsychs
quetiapine and olanzapine,
OTCs like diphenhydramine.
Avoid substances causing
insomnia: stimulants, SSRIs,
bupropion, theophylline,
caffeine, decongestants,
diuretics, corticosteroids,
antihypertensives, alcohol, w/d
from sedative-hypnotics
Prog: 70% of pts w/ insomnia
at baseline have insomnia 1 yr
later. 50% 3 yrs later.
W/ CBT: 70-80% response.
40% remit.
Chronic insomnia ! risk of dep,
anx, substance use, HTN, and
in older adults-mortality.
CBT: sleep restriction (limit
time in bed except sleep).
Stimulus control (! assoc. btwn
bed and sleep). Relaxation
training (muscles). Cognitive
therapy (change
misconceptions bout sleep,
insomnia, daytime). Education
about sleep hygiene
Parasomnia 20% of kids
have >1
episodes of
sleep-walk. 4%
adults.
REM behavior
disorder: 0.5%
Occur as a result of sleep state
instability (incomplete
transitions between stages of
sleep and waking)
REM behavior
disorder: age>50,
Male, PD
Undesirable behaviors or
experiences during sleep
period including
sleepwalking, aggression,
eating, sex
Night terrors
REM behavior disorder:
muscle atonia not maintained
during REM, act dreams
Sleep hygiene
Avoid sleep deprivation &
substance use
Ensure safety of bedroom
BZD
Melatonin
Circadian
rhythm
disorder
0.13-1.3%
Delayed sleep
disorder
common in
Delayed sleep disorder: pts
have difficulty falling asleep
until several hrs after desired
bedtime. Difficulty waking
Delayed sleep disorder: bright
light exp in morning, avoid
bright light from late afternoon
onward, melatonin in early
Sleep hygiene! For all disorders
Exercise daily (preferably in
AM)
Use bed for sleep and sex only
young adults.
Advanced sleep
disorder
common in
elderly
up for school/work.
Advanced sleep phase
disorder: difficulty staying up
until desired bedtime, then
have early awakening
Shift work disorder: difficulty
sleeping at scheduled time and
sleepiness at work
evening
Advanced sleep disorder: bright
light exp in evening, avoid
bright light in the morning,
melatonin in early morning
Shift work: bright light exp
during first half of work shift,
minimize light exposure on the
way home and during sleep
periods, nap before scheduled
shift; caffeine to improve
alertness during work shift
Keep bedroom dark, quiet, and
at comfortable temp
Go to bed only when sleep, get
up if unable to sleep
Avoid naps
Avoid stimulants several hrs b4
bed
Avoid etoh at bedtime
Narcolepsy 0.05% Cataplexy- loss of hypocretin-
producing cells in lateral
thalamus (a/w HLA marker)
Excessive daytime sleepiness
(! tendency to fall asleep
and/or need to exert effort to
stay awake in low-stimulus
situations). Chronic and
persistent level of sleepiness
w/ strong urges to sleep
various times in day.
Cataplexy. Sleep paralysis.
Hypnagogic hallucinations.
stimulants- modafinil,
methylphenidate,
amphetamines
Restless leg
syndrome
3% Urge to move legs, often
accompanied by
uncomfortable sensation. Sxs
worsen at rest and at night.
Relieved by movement or
stretching.
Sleep hygiene
Avoid sleep deprivation,
caffeine, etoh
Iron replacement (if low
ferritin)
Anticonvulsants (gabapentin)
Dopaminergic agents
(levodopa, ropinirole,
pramipexole)
familiarity vs recollection based recognition
CLINICAL MANIFESTATIONS OF INTOXICATION w/ SELECT SUBSTANCES
Substance Low level intoxication High level intoxication
Etoh Pleasant, sometimes euphoric state w/ "
coordination and relaxed judgment
Violence and poor judgment, sedation to
somnolence w/ severe " in coordination, slurring of
words, etc, and possible loss of gag reflex and
apnea
Opioids Euphoria followed by somnolence; miosis Euphoria followed by somnolence w/ potential
apnea and death; miosis
Cocaine/other stimulants Euphoric, excited state w/ lack of sleep, intense
concentration, lack of appetite
Anxiety, psychosis, agitation, sz, cardiac/cerebral
ischemia
Hallucinogens Intense change in perceptual state leading to
unusual visual, auditory, and other sensory
experiences
Intense, more hallucinatory state bordering on
psychosis w/ impulsive acts related to perceptions
COMMON W/D SXS
Substance Common sxs/signs Dangerous sxs Timeline
Table 1. Types of Long-Term Memory (LTM)
Key Feature Declarative LTM Nondeclarative LTM
Kind oI inIormation
remembered
Facts and events Skills, habits, and stimulus-
response associations
Rate oI acquisition Rapid (and oIten on just one
trial)
Slow (and oIten requires
repeated exposure)
Entails awareness oI the
inIormation being
remembered
yes no
Is amenable to volitional
retrieval
yes no
Typically impaired in
anterograde amnesia
yes no
Within the domain oI declarative long-term memory (LTM), there are several important
distinctions. For some inIormation, we remember the who, where, and when associated
with it. (For example, think oI what you ate Ior dinner last night you not only remember
the actual Iood that went into your mouth, you also remember who else was at dinner
with you, where you ate, and roughly what time it was.) This is reIerred to as episodic
memory, because together with the Iact in question (e.g., what you ate) you also
remember the episode in which this eating took place (i.e., the who, where, and when).
This additional inIormation is oIten reIerred to as the context or the source oI the
memory.
For other kinds oI memory, however, retrieval is not accompanied by the related episodic
inIormation. For example, the word 'memory. You know its deIinition, and the Iact that
you didn`t have this knowledge at birth means you must have learned it at some point in
your liIe; thereIore it is a memory. However, it is highly unlikely that anyone reading this
can remember who taught them the deIinition oI 'memory, where they were when this
inIormation was acquired, or when the learning took place. This is reIerred to as a
semantic memory, because it contains Iactual inIormation but is not associated with a
speciIic episode Irom the past.
B. Retrieval of Memory
Episodic memory can be retrieved via one oI two broad classes oI retrieval: recall or
recognition. A test oI recall would be 'What did you have Ior dinner last night? A test oI
recognition would be 'Here are pictures oI a pizza, a salad, and a bag oI chips; which oI
these did you eat Ior dinner? (This would be a 3-alternative Iorced-choice recognition
test. A yes/no recognition test, in contrast, might be 'Did you eat pizza Ior dinner last
night?) We perIorm both kinds oI memory retrieval hundreds oI times each day. Tests oI
recognition are easier than tests oI recall because recognition necessarily provides cues
('hints) that can aid in retrieval.
235
Distinguishing delirium from dementia is critical because of the distinct etiologies and treatments
(Table 1).
Table 1. Delirium versus dementia
Delirium Dementia
Duration hours-to-days months-to-years
Onset of symptoms abrupt insidious
Course of symptoms waxing and waning very slowly progressive
Most common causes toxic, metabolic, infectious neurodegenerative disorders,
cerebrovascular disease
Reversible? yes rarely
II. Clinical Manifestations and Management of Delirium
A. Epidemiology and Public Health Impact
The prevalence of delirium varies dramatically, depending on the setting:
0.8% among community-dwelling older adults;
25% among patients hospitalized with cancer;
60% among nursing home residents older than 75 years old;
80% among the terminally ill.
Risk factors include age, cerebrovascular disease, neurodegenerative disease (typically
Alzheimers disease or Parkinsons disease), chronic medical conditions, recent surgery, being in
an unfamiliar environment, taking psychotropic medications (especially sedative-hypnotics or
medications with anticholinergic properties), and malnutrition.
Delirium has a high mortality rate. Up to 15% of elderly patients with delirium die within 1
month, and up to 25% die within 6 months. This is due to the fact that delirium may be a marker
of severe underlying illness and may also be due to complications of delirium such as pneumonia
and decubiti (skin breakdown, which may in turn result in infection). Delirium is associated with
worse post-surgical outcome, including increased complications of surgery and increased
disability. Individuals with delirium may lose their independence, at least transiently; delirium is
associated with a longer length of stay in the hospital and with a higher risk of nursing home
placement. It is being increasingly recognized that many patients with delirium do not return to
their premorbid cognitive and functional level even after resolution of the underlying cause(s).
248
Etoh Anx, N, tremors, sleeplessness,
restlessness, sweating, HA, ! HR and
BP
Psychosis, delirium, sz Commons sxs subside ~72-96 hrs
Delerium tremens can last 10+ days
BZDs Anx, N, tremors, sleeplessness,
restlessness, sweating, HA, ! HR and
BP
Sz Depends on drugs half-life
Varies from days to weeks
Opioids N/V, craving, rhinorrhea, diarrhea,
tearing, muscle aches/cramps,
gooseflesh, dilated pupils
Dehydration from diarrhea and
vomiting
Leaving care to get more drug
Depends on drugs half life
Days- morphine/heroin
Weeks- methadone
Stimulants Tired, prolonged sleeping,
amotivational, depressed, overeating,
craving
Will leave to get more drug Cocaine shorter than meth, which has
longer half life
You might also like
- Reiki Manual LVL 2Document9 pagesReiki Manual LVL 2atosmdq79930% (1)
- Shadow Integration - The Complete Shadow Work Process in Four Steps - Words From The WindDocument15 pagesShadow Integration - The Complete Shadow Work Process in Four Steps - Words From The WindAR75% (4)
- Fundamentals Nursing Active Learning 1st Edition Yoost Crawford - Test BankDocument44 pagesFundamentals Nursing Active Learning 1st Edition Yoost Crawford - Test BankRaymondCenteno100% (3)
- Manual Handling Mini EbookDocument15 pagesManual Handling Mini EbookJohnPaulBascoNo ratings yet
- Second and Third Generation Antipsychotics: A Comprehensive HandbookFrom EverandSecond and Third Generation Antipsychotics: A Comprehensive HandbookRating: 5 out of 5 stars5/5 (1)
- Lac+Usc Internal Medicine Residency Survival Guide 2013-2014Document226 pagesLac+Usc Internal Medicine Residency Survival Guide 2013-2014Shaz ChindhyNo ratings yet
- Ancef Drug CardDocument1 pageAncef Drug CardSheri490No ratings yet
- Interpersonal Psychotherapy NewDocument119 pagesInterpersonal Psychotherapy Newdrkadiyala2100% (1)
- Prochaska & DiClemente (1982) Transtheoretical Therapy (Toward A More Integrative Model of Change) PDFDocument13 pagesProchaska & DiClemente (1982) Transtheoretical Therapy (Toward A More Integrative Model of Change) PDFSuryo HapsoroNo ratings yet
- Psychiatry Info - FinalDocument8 pagesPsychiatry Info - FinalH_QasimNo ratings yet
- Psych Ch. 7 Notes (Tutor)Document5 pagesPsych Ch. 7 Notes (Tutor)Haylle ThomasNo ratings yet
- Psych Ch. 5 NotesDocument7 pagesPsych Ch. 5 NotesHaylle ThomasNo ratings yet
- PSYCH 1.2A Mood DisordersDocument22 pagesPSYCH 1.2A Mood DisordersZaza100% (1)
- Kring Abnormal Psychology Chapter 5 Mood Disorders NotesDocument14 pagesKring Abnormal Psychology Chapter 5 Mood Disorders NotesAnn Ross FernandezNo ratings yet
- Pharmacology - (5) Psychotic DrugsDocument8 pagesPharmacology - (5) Psychotic DrugsSamantha DiegoNo ratings yet
- BEHS Disorders ChartDocument7 pagesBEHS Disorders ChartAndrew PatelNo ratings yet
- 10 Cognitive DisordersDocument16 pages10 Cognitive DisordersFarrah MaeNo ratings yet
- Just Getting The Main RX Names Down : Antidepressants Mood StabilizersDocument1 pageJust Getting The Main RX Names Down : Antidepressants Mood StabilizersCarlos Eduardo LinaresNo ratings yet
- Disorders of Thought & Speech (Psychopathology)Document21 pagesDisorders of Thought & Speech (Psychopathology)Upasana Baruah100% (2)
- 5 - Childhood Psychiatric Disorder (2017!06!02 23-15-39 UTC)Document60 pages5 - Childhood Psychiatric Disorder (2017!06!02 23-15-39 UTC)drillercz12zNo ratings yet
- Psych TemplateDocument1 pagePsych TemplateWilliam Yang100% (1)
- Sudden Onset (Within 2 Weeks) of at Least One of TheDocument2 pagesSudden Onset (Within 2 Weeks) of at Least One of TheNeicole BandalaNo ratings yet
- Psychopharmacology in PsychiatryDocument94 pagesPsychopharmacology in PsychiatryOslo Saputra100% (1)
- Neuroleptics & AnxiolyticsDocument65 pagesNeuroleptics & AnxiolyticsAntonPurpurov100% (1)
- Shortened REM Latency and Increased REM: Previous AttemptDocument19 pagesShortened REM Latency and Increased REM: Previous AttemptActeen MyoseenNo ratings yet
- Provisional: Borderline Personality Disorder Differential DXDocument6 pagesProvisional: Borderline Personality Disorder Differential DXhernandez2812No ratings yet
- AntipsychoticsDocument4 pagesAntipsychoticsRana MuhammadNo ratings yet
- Disorders Duration/Onset Symptoms/Manifestations Treatment: Childhood DDocument7 pagesDisorders Duration/Onset Symptoms/Manifestations Treatment: Childhood DActeen Myoseen100% (2)
- Psychiatric Nursing ReviewDocument44 pagesPsychiatric Nursing ReviewramemgarNo ratings yet
- Consultationliaison Psychiatry IcuDocument56 pagesConsultationliaison Psychiatry IcuChrisAlipioNo ratings yet
- Psychotropic Medication ReviewDocument7 pagesPsychotropic Medication ReviewAakash Shah100% (2)
- Epidemiological Data: Paper B Syllabic Content 7.xDocument5 pagesEpidemiological Data: Paper B Syllabic Content 7.xAnamika SinhaNo ratings yet
- Glossary of Psychiatric TermsDocument42 pagesGlossary of Psychiatric TermsÏtz ShãrîNo ratings yet
- Study Guide For The Psychiatry NBME Content Exam AKA The Psychiatry Shelf Exam!Document2 pagesStudy Guide For The Psychiatry NBME Content Exam AKA The Psychiatry Shelf Exam!DoriNo ratings yet
- Disorders of ThoughtDocument30 pagesDisorders of ThoughtRenault Jia Kai50% (2)
- Lecture No. 3 Semiology of Psychiatry Part 2Document26 pagesLecture No. 3 Semiology of Psychiatry Part 2ozgur.yonlukNo ratings yet
- Vascular DementiaDocument5 pagesVascular DementiaAna Ramos LopezNo ratings yet
- Antipsychotic Medication: Generic Name Trade Name Indications Contraindications Drug Interaction Side Effects Nursing ImplicationDocument6 pagesAntipsychotic Medication: Generic Name Trade Name Indications Contraindications Drug Interaction Side Effects Nursing ImplicationJaylord Verazon100% (1)
- Introduction To Psychiatric Nursing: Mercedes A Perez-Millan MSN, ARNPDocument33 pagesIntroduction To Psychiatric Nursing: Mercedes A Perez-Millan MSN, ARNPSachiko Yosores100% (1)
- Exam 1 2Document18 pagesExam 1 2api-444187370No ratings yet
- Mental Status Examination Rapid Record Form: CatatoniaDocument3 pagesMental Status Examination Rapid Record Form: CatatoniaNicole Tangco100% (1)
- DSM-IV Criteria MnemonicsDocument4 pagesDSM-IV Criteria Mnemonicsleonyap100% (2)
- Glossary of Psychiatric TerminologyDocument20 pagesGlossary of Psychiatric Terminologyphoebe_62002239No ratings yet
- AntipsychoticsDocument10 pagesAntipsychoticswawing16No ratings yet
- Psych Final BlueprintDocument10 pagesPsych Final BlueprintGrace LivingstonNo ratings yet
- Medication Conversion ChartDocument2 pagesMedication Conversion ChartIlinca mirnoviciNo ratings yet
- PSYCH 011 Clinical Diagnosis of Neurocognitive DisorderDocument7 pagesPSYCH 011 Clinical Diagnosis of Neurocognitive DisorderKaye NeeNo ratings yet
- DR - Usama.mahmoud Psychiatry - Notes MSDocument64 pagesDR - Usama.mahmoud Psychiatry - Notes MSMariam A. KarimNo ratings yet
- Child and Adolescent Psychiatry: A. Pervasive and Developmental DisordersDocument6 pagesChild and Adolescent Psychiatry: A. Pervasive and Developmental DisordersIsabel CastilloNo ratings yet
- Psychiatry Notes Psychiatry Notes: Medicine (Queen Mary University of London) Medicine (Queen Mary University of London)Document28 pagesPsychiatry Notes Psychiatry Notes: Medicine (Queen Mary University of London) Medicine (Queen Mary University of London)Noman ButtNo ratings yet
- Glossary of Frequently Used Mental Health TermsDocument6 pagesGlossary of Frequently Used Mental Health TermsWarren MillerNo ratings yet
- Study Guide Test 1Document11 pagesStudy Guide Test 1jwasylow13No ratings yet
- Initial Interview TemplateDocument4 pagesInitial Interview TemplateJoan ChoiNo ratings yet
- PMHNP Case Study - EditedDocument7 pagesPMHNP Case Study - EditedSoumyadeep BoseNo ratings yet
- Intro Child PsychiatryDocument122 pagesIntro Child PsychiatryayunisallehNo ratings yet
- DELIRIUM PresentationDocument26 pagesDELIRIUM PresentationAnkush Sharma100% (1)
- Substance Use DisordersDocument28 pagesSubstance Use DisordersAbdul NazarNo ratings yet
- Clozapine Care GuideDocument16 pagesClozapine Care GuideERWIN SUMARDINo ratings yet
- Pharmacotherapy in PschiatryDocument8 pagesPharmacotherapy in PschiatryygfhdgNo ratings yet
- Psycho-Pharmacotherapy: Major Tranquilizers, D2 - Receptor Blockers and Anti - Schizophrenic DrugsDocument29 pagesPsycho-Pharmacotherapy: Major Tranquilizers, D2 - Receptor Blockers and Anti - Schizophrenic DrugsPoonam RanaNo ratings yet
- Psychiatry MnemonicsDocument4 pagesPsychiatry MnemonicsHiruni Tharuka100% (2)
- 1 - Signs and Symptoms of Mental Illness-PartDocument49 pages1 - Signs and Symptoms of Mental Illness-PartAljoker FarragNo ratings yet
- Psychiatrypoisoning E.ODocument24 pagesPsychiatrypoisoning E.OZeenat JunaidNo ratings yet
- Anxiety/Depression: S AlprazolamDocument2 pagesAnxiety/Depression: S AlprazolamleesaNo ratings yet
- Psychiatric Diagnosis: Challenges and ProspectsFrom EverandPsychiatric Diagnosis: Challenges and ProspectsIhsan M. SalloumRating: 5 out of 5 stars5/5 (1)
- Pericardial Disease: Adel Hasanin Ahmed 1Document5 pagesPericardial Disease: Adel Hasanin Ahmed 1Shaz ChindhyNo ratings yet
- Cong HeartDocument7 pagesCong HeartShaz ChindhyNo ratings yet
- Me 1Document74 pagesMe 1Shaz ChindhyNo ratings yet
- ST NoDocument89 pagesST NoShaz Chindhy100% (1)
- I. Definition/General Considerations: Colon CancerDocument2 pagesI. Definition/General Considerations: Colon CancerShaz ChindhyNo ratings yet
- Endocrine Learning ObjDocument2 pagesEndocrine Learning ObjShaz ChindhyNo ratings yet
- Alcohol Dependednce Vs Abuse: Best TX Is Conseling + Drug. Combining Drugs Is NOT More EfficatiousDocument4 pagesAlcohol Dependednce Vs Abuse: Best TX Is Conseling + Drug. Combining Drugs Is NOT More EfficatiousShaz ChindhyNo ratings yet
- IMDocument128 pagesIMShaz ChindhyNo ratings yet
- I. Definition/General Consideration: Acute Asthma ExacerbationDocument2 pagesI. Definition/General Consideration: Acute Asthma ExacerbationShaz ChindhyNo ratings yet
- All of Medicine FlashcardsDocument142 pagesAll of Medicine FlashcardsShaz Chindhy100% (2)
- Cardio AnswersDocument26 pagesCardio AnswersShaz ChindhyNo ratings yet
- MKSAPDocument2 pagesMKSAPShaz ChindhyNo ratings yet
- Diabetes: Foot ExamDocument4 pagesDiabetes: Foot ExamShaz ChindhyNo ratings yet
- I. Definition/General Considerations: HypercalcemiaDocument2 pagesI. Definition/General Considerations: HypercalcemiaShaz ChindhyNo ratings yet
- Hiit On The GoDocument41 pagesHiit On The Godee138No ratings yet
- David A. Nicholls - The End of Physiotherapy (2017, Routledge) - Libgen - LiDocument378 pagesDavid A. Nicholls - The End of Physiotherapy (2017, Routledge) - Libgen - LiMina RizqinaNo ratings yet
- Dapsone 2Document2 pagesDapsone 2JeanMENo ratings yet
- Resume PDFDocument1 pageResume PDFapi-266278027No ratings yet
- Helfaer P. M. Positive Development For Persons With Trauma. USABPJ 9.2 2010Document14 pagesHelfaer P. M. Positive Development For Persons With Trauma. USABPJ 9.2 2010tonkoslavNo ratings yet
- Renal MedsurgDocument14 pagesRenal MedsurgCliff Lois ╭∩╮⎷⎛⎝⎲⏝⏝⎲⎠⎷⎛╭∩╮ Ouano100% (1)
- EphedraDocument9 pagesEphedraapi-367367047No ratings yet
- HDFC Life Critical Illness Plus Rider BrochureDocument8 pagesHDFC Life Critical Illness Plus Rider Brochurepinky_y2kNo ratings yet
- Farmacologia em Cães GeriátricosDocument12 pagesFarmacologia em Cães GeriátricosRafaela RodriguesNo ratings yet
- Neurosurgery 4 Mental DisordersDocument82 pagesNeurosurgery 4 Mental DisordersTomChristianNo ratings yet
- Guidance and Counselling.Document10 pagesGuidance and Counselling.Stacy SangmaNo ratings yet
- Resources#2 Severe Clutter LocalDocument1 pageResources#2 Severe Clutter LocalMargaret Pearson Pinkham100% (1)
- 10 Steps For Any Dilemma PDFDocument2 pages10 Steps For Any Dilemma PDFMitchell StroiczNo ratings yet
- tp53 Concept MapDocument1 pagetp53 Concept Mapapi-449993710No ratings yet
- The Bobath Concept (NDT) As Rehabilitation in Stroke Patients - Revisión SistemáticaDocument8 pagesThe Bobath Concept (NDT) As Rehabilitation in Stroke Patients - Revisión SistemáticaCristian Manuel Goicochea ChuqueNo ratings yet
- Sri LankDocument20 pagesSri LankVangeesa SumanasekaraNo ratings yet
- HIV and PregnancyDocument9 pagesHIV and PregnancyUm HamoOdNo ratings yet
- Principles of Hemodialysis: Module No: - 02 - Module TitleDocument10 pagesPrinciples of Hemodialysis: Module No: - 02 - Module TitleIan LelisNo ratings yet
- SBARDocument2 pagesSBARJason Kai Poth100% (1)
- Atraumatic Nursing Very FinalDocument50 pagesAtraumatic Nursing Very FinalLatha VenkatesanNo ratings yet
- Antiphospholipid SyndromeDocument6 pagesAntiphospholipid SyndromeOm Lakhani100% (1)
- Aversive ConditioningDocument4 pagesAversive Conditioningiulia9gavrisNo ratings yet
- Magnet Therapyncreasingly Gaining in Popularity The World OverDocument3 pagesMagnet Therapyncreasingly Gaining in Popularity The World OverPradeep PatilNo ratings yet
- Morse Fall ScaleDocument1 pageMorse Fall Scalecardiology serdangNo ratings yet