Professional Documents
Culture Documents
Cerny Fixed Retainer
Cerny Fixed Retainer
Uploaded by
chinchiayeh5699Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cerny Fixed Retainer
Cerny Fixed Retainer
Uploaded by
chinchiayeh5699Copyright:
Available Formats
Contents
Original articles
1 Comparison of surgical and non-surgical methods of treating palatally impacted canines.
I Periodontal and pulpal outcomes
Kwok K. Ling, Christopher T.C. Ho, Olena Kravchuk and Richard J. Olive
8 Comparison of surgical and non-surgical methods of treating palatally impacted canines.
II Aesthetic outcomes
Kwok K. Ling, Christopher T.C. Ho, Olena Kravchuk and Richard J. Olive
16 Changes in interdental papillae heights following alignment of anterior teeth
Sanjivan Kandasamy, Mithran Goonewardene and Marc Tennant
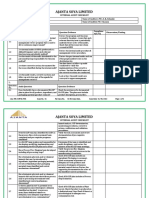
24 The reliability of bonded lingual retainers
Robert Cerny
30 Sella turcica bridges in orthodontic and orthognathic surgery patients. A retrospective cephalometric study
Hussam M. Abdel-Kader
36 Static frictional resistances of polycrystalline ceramic brackets with conventional slots, glazed slots and metal
slot inserts
Steven P. Jones and Gyaami Amoah
41 Lower intercanine width and gingival margin changes. A retrospective study
Luciane Closs, Karine Squeff, Dirceu Raveli and Cassiano Rsing
46 Effect of Topacal C-5 on enamel adjacent to orthodontic brackets. An in vitro study
Navid Karimi Nasab, Zahra Dalili Kajan and Azadeh Balalaie
50 The impact of orthodontic treatment on normative need. A case-control study in Peru
Eduardo Bernab, Socorro A. Borges-Yez and Carlos Flores-Mir
Review
55 Three-dimensional computed craniofacial tomography (3D-CT): potential uses and limitations
Hong Jin Chan, Michael Woods and Damien Stella
Case reports
65 Treatment of skeletal 2 malocclusion using bone-plate anchorage. A case report
Kallaya Kraikosol, Charunee Rattanayatikul, Keith Godfrey and T. Vattraraphoudet
72 Space closure using the Hycon device. A case report
Viral A. Kachiwala, Anmol S. Kalha and J. Vigneshwaran
Editorial
76 Forty years of publication
Michael Harkness
General
78 Book reviews
81 Recent publications
84 New Products
86 Calendar
Australian
Orthodontic Journal
Volume 23 Number 1, May 2007
Australian Orthodontic Journal Volume 23 No. 1 May 2007
Introduction
The preferred management of an ectopic or impacted
palatal canine is early diagnosis and interceptive
treatment, often involving extraction of the overlying
primary canine in the hope that the impaction will
resolve spontaneously.
18
The success of this form of
treatment appears to be related to the timing of treat-
ment and availability of space in the dental arch.
7,9,10
If diagnosis of an ectopic canine is delayed or if
extraction of the primary canine and creation of
excess space in the arch fails to correct an impaction,
the only reliable option appears to be surgical expo-
sure followed by orthodontic treatment to extrude
and position the impacted tooth in the arch.
Part of the reluctance for surgical treatment is the
likelihood of poor periodontal and pulpal out-
comes.
1116
However there is some dispute about
the clinical significance of undesirable periodontal
and pulpal changes following surgical exposure of
impacted canines.
13,15,17
The aims of this study were to compare the
periodontal and pulpal health of palatally
impacted maxillary canines following either surgical
exposure and assisted eruption or unassisted
eruption following extraction of the overlying
deciduous canine and orthodontic creation of space
in the arch.
Subjects and methods
Ethical clearance for this study was obtained from the
Medical Research Ethics Committee of the University
of Queensland. The subjects were selected from the
Australian Orthodontic Journal Volume 23 No. 1 May 2007 1
Comparison of surgical and non-surgical methods
of treating palatally impacted canines.
I - Periodontal and pulpal outcomes
Kwok K. Ling,
*
Christopher T. C. Ho,
*
Olena Kravchuk
and Richard J. Olive
School of Dentistry,
*
School of Land and Food Sciences,
University of Queensland and Specialist Practice,
Brisbane, Australia
Background: Inferior periodontal and pulpal outcomes may follow surgical exposure of palatally impacted maxillary canines.
Objectives: To compare the periodontal and pulpal health of palatally impacted maxillary canines following either surgical
exposure and assisted eruption (SE) or unassisted eruption following extraction of the overlying deciduous canine and
orthodontic creation of space in the arch (OT).
Methods: Twentyeight subjects (OT group: N = 14; SE group: N = 14) with unilateral palatally impacted canines were
examined at least six months after orthodontic treatment. The gingival index score, plaque index score, pocket depth,
attachment loss, tenderness to percussion, pulpal responses to stimuli and radiographic assessment of changes in the pulpal
cavities and peri-radicular areas were collected on the maxillary canines, lateral incisors and premolars. The contralateral teeth
were used as controls.
Results: There were no significant differences in the plaque index scores, the gingival index scores or the periodontal outcomes
between the impacted canines in the two groups (SE and OT). More impacted canines than control canines had lost some
periodontal attachment in the SE group (p = 0.004). Although more lateral incisors, canines and premolars on the impacted
side had partially obliterated pulps than the corresponding teeth on the control side, the teeth in both groups had similar pulpal
responses (p = 0.064).
Conclusions: Natural eruption and conservative surgical exposure with orthodontic alignment have minor effects on the
periodontium. Impacted canines treated surgically and non-surgically had a higher prevalence of pulpal changes than the control
canines. Ultimately, the choice of treatment may depend on the clinical indications, the patients and the orthodontists preferences.
(Aust Orthod J 2007; 23: 17)
Received for publication: July 2006
Accepted: February 2007
records of three orthodontic practices providing they
met the following criteria:
1. A unilateral palatally impacted canine was present.
2. A pretreatment panoramic radiograph was available.
3. There was no significant medical history.
4. Treatment had been completed for at least six
months.
5. In the surgical group, the subjects had undergone
conservative surgical exposure and the wound had
been dressed for 710 days before any orthodontic
attachments were bonded.
Of the 28 subjects who met these requirements and
were examined at least six months post-treatment, 14
subjects (5 males, 9 females) had been treated by
extraction of the overlying deciduous canine and
creation of excess space in the arch (OT group) and
14 subjects (2 males, 12 females) had been treated by
open surgical exposure followed by orthodontic
extrusion and alignment of the canine in the arch (SE
group). In the latter group the surgery was performed
by different oral and maxillofacial surgeons and the
wounds were dressed for between seven and 10 days.
One orthodontist treated the subjects in the OT
group and three orthodontists treated the subjects in
the SE group. At the time of the post-treatment
examination the subjects in the OT group were, on
average, 19.1 years of age and the subjects in the SE
group were 18.8 years of age (Table I).
The pretreatment panoramic radiographs were used
to classify the sector of impaction using Lindauer
et al.s
18
modification of Ericson and Kurols
classification.
6
Two subjects in the OT group were
treated with extraction of both maxillary second pre-
molars.
Post-treatment assessments of the maxillary
lateral incisors, canines and first premolars
Periodontal assessments
The assessor (KKL) was blinded as to the identity of
the side with the impacted canine. Oral hygiene was
assessed with the Plaque Index,
19
and gingival health
with the Gingival Index.
20
Pocket depths were meas-
ured at six sites (mesio-buccal, mid-buccal, disto-
buccal, mesio-palatal, mid-palatal and disto-palatal)
around each tooth using a University of Michigan O
probe with Williams markings. Pocket depths were
measured from the gingival margins to the bottom of
the clinical pockets. The distance from the gingival
margin to the cemento-enamel junction (CEJ) was
also measured, and loss of attachment was deter-
mined by subtracting this distance from the pocket
depth measurement.
12,16
When the level of the CEJ
could not be located, it was assumed to be situated at
the bottom of the clinical pocket.
16
All clinical meas-
urements were made to the nearest 0.25 mm and
were repeated 10 minutes after the initial recordings.
Percussion and vitality assessments
Percussion tests were performed by tapping the incisal
edges or occlusal surfaces of the teeth with the blunt
end of a dental mirror handle. The response to this
test was recorded as either positive or negative. For
the cold thermal test each tooth was isolated with
cotton rolls and dried thoroughly. A cotton pellet
soaked with carbon dioxide spray (Miracold spray,
LING ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 2
Table I. Description of the sample.
OT (N=14) SE (N=14) p
p
+
Mean (SD) Mean (SD)
Male : Female 5 : 9 2 : 12 0.190
Right : Left proportion 8 : 6 4 : 10 0.127
Sector of impaction II : III : IV 5 : 7 : 2 1 : 4 : 9 0.019
Age at start of treatment (years) 13.5 (1.3) 13.5 (1.6) 0.979
Age at recall (years) 19.1 (2.2) 18.8 (2.5) 0.749
Active treatment duration (months) 27.9 (9.3) 28.4 (7.5) 0.877
Recall period (years) 3.4 (3.0) 3.2 (2.4) 0.847
Chi-squared test, significant value in bold
+
Students t-test
Hager Werke, Germany) was then applied to the
middle of the tooth. A negative response was regis-
tered if no sensation was reported after 10 seconds.
The electrical pulp test was carried out with an
Analytic Technology vitality scanner (Analytic
Technology Corporation, Redmond, Washington,
USA). Each tooth was isolated with cotton rolls and
dried and the tip of the probe, coated with toothpaste
as conductant, placed on the incisal third midway
between the mesial and distal surfaces of each tooth.
21
If part of the clinical crown had been restored the
probe was placed on the enamel as close as possible
to the incisal third of the tooth. If sensation was
reported before the reading reached 80, a positive
response was recorded. A negative response was
recorded if no sensation was felt when the reading
reached 80.
To assess reliability, the percussion and vitality tests
were repeated 10 minutes after the initial recordings.
One subject in the SE group had a root-filled lateral
incisor on the impacted side. This tooth had been
traumatised and root-filled prior to orthodontic
treatment and was excluded from the percussion and
vitality tests.
Radiographic assessment
Periapical radiographs were taken of the lateral
incisors, canines and first premolars on both sides.
Radiographic changes in the pulpal cavities and peri-
radicular areas were evaluated using the criteria
described by Jacobsen and Kerekes.
22
Total obliter-
ation of the pulp chamber was noted if the pulp
chamber and root canal were not discernible and
partial obliteration was noted if the root canal was
markedly narrowed, but clearly visible. Previous
endodontic treatment was also recorded. The peri-
radicular area was registered as normal if the
periodontal space was of normal width and as patho-
logical if there was marked widening of the space or
there was an associated radiolucent area. All radio-
graphs were re-evaluated one week after the initial
assessment.
Statistical analysis
Statistical analysis was carried out with Minitab for
Windows (Release 14, Minitab Inc., USA) and the
significance level for all statistical procedures was set
at 5 per cent. Additionally, SPSS for Windows
(Version 12.0, SPSS Inc., Chicago, USA) was used to
perform the McNemar test. The Bonferroni correc-
tion was applied where appropriate. Chi-squared tests
were used to analyse the difference between the two
groups in terms of gender, side and sector of
impaction. Treatment-related variables, such as age at
commencement of treatment, age at recall, duration
of active treatment and recall period, were compared
with the unpaired t-test.
Plaque Index and Periodontal Index data were
analysed with the Mann-Whitney test. The pro-
portions of subjects with index scores greater than
zero were analysed with the binomial test for propor-
tions. The maximum score for each site was noted to
provide a clinical picture of severity.
To address reliability issues, periodontal measure-
ments taken 10 minutes apart were statistically
analysed using the paired t-test. Average values of the
measurements were used for subsequent analysis if no
significant differences were detected between two
time points. Differences between the groups for the
mean probing pocket depths were tested using
unpaired t-tests. Paired t-tests were used to test for
differences within the groups (e.g. between the
impacted canine and the contralateral control
canine).
Attachment loss was analysed by comparing the pro-
portions of teeth with attachment losses. The Mood
Median Test was used to compare the difference in
maximum attachment loss and to give a confidence
interval, which may indicate the potential attachment
loss to be expected in each group. Fishers Exact test
was used to test the differences in proportion between
groups for percussion tests, vitality responses and
radiographic findings.
Results
Subjects in both groups were similar in terms of the
gender distribution, the proportion of impacted
canines on either the right or the left side, age at com-
mencement of treatment, age at recall, the duration
of treatment and the post-treatment recall period.
The latter was the period that had elapsed from the
end of active treatment to the date of examination for
this study (Table I). The only significant difference
between the SE and OT groups was the distribution
of subjects in the sectors of impaction (p = 0.019).
There was a higher percentage of sector IV
impactions in the surgical group, which is not
SURGICAL AND NON- SURGICAL METHODS OF TREATING PALATALLY IMPACTED CANINES. I - PERIODONTAL AND PULPUL OUTCOMES
Australian Orthodontic Journal Volume 23 No. 1 May 2007 3
surprising as severe impaction is generally not
amenable to orthodontic treatment alone.
9
The Plaque Index and Gingival Index scores in the
two groups were similar (Table II). The proportions
of subjects in the OT group with a total Plaque Index
score above zero was greater on the impacted side in
comparison with the non-impacted side, but the
difference was not statistically significant (Table II).
The maximum Plaque and Gingival Index scores at
individual tooth sites did not exceed two.
There were no statistically significant differences
between the initial and second measurements of
pocket depth and the level of the cemento-enamel
junction.
The pocket depths ranged from 0.5 to 3 mm (Figures
1 to 3). When the pocket depths on the impacted side
were compared with the pocket depths on the contra-
lateral teeth, only the disto-palatal sites of the lateral
incisors on the impacted side in the OT group were
significantly deeper (Mean difference: 0.28 mm; SD:
0.33 mm; Paired t-test: p = 0.007) (Figure 1). The
periodontal pockets were significantly deeper mid-
buccally on the control lateral incisor in the SE group
when compared with the OT group (Mean differ-
ence: 0.20 mm; Pooled SD: 0.21 mm; Unpaired
t-test: p = 0.020) and mid-palatally on the control
canine (Mean difference: 0.25 mm; Pooled SD: 0.32
mm; Unpaired t-test: p = 0.048) (Figures 1 and 2).
One subject in the OT group had lost periodontal
attachment on the lateral incisors, canines and
premolars (Table III). In the SE group the number of
previously impacted canines with attachment loss was
LING ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 4
Table II. Comparison of the Plaque Index and Gingival Index scores
greater than zero.
Group Impacted side Control side p
Plaque Index
OT (N=14) 10 5 0.063
SE (N=14) 8 6 0.500
p
+
0.695 1
Gingival Index
OT (N=14) 7 3 0.219
SE (N=14) 10 6 0.219
p
+
0.440 0.420
McNemar test
+
Fishers Exact test Figure 1. Box plot of probing pocket depth for lateral incisors. Impacted
side (I); non-impacted side (N); mesio-buccal (MB); mid-buccal (MidB);
disto-buccal (DB); mesio-palatal (MP); mid-palatal (MidP); disto-palatal (DP).
Figure 2. Box plot of probing pocket depth for canines. Impacted side (I);
non-impacted side (N); mesio-buccal (MB); mid-buccal (MidB); disto-buccal
(DB); mesio-palatal (MP); mid-palatal (MidP); disto-palatal (DP).
Figure 3. Box plot of probing pocket depth for first premolars. Impacted
side (I); non-impacted side (N); mesio-buccal (MB); mid-buccal (MidB); disto-
buccal (DB); mesio-palatal (MP); mid-palatal (MidP); disto-palatal (DP).
P
o
c
k
e
t
d
e
p
t
h
(
m
m
)
P
o
c
k
e
t
d
e
p
t
h
(
m
m
)
P
o
c
k
e
t
d
e
p
t
h
(
m
m
)
Treatment
and sites
Treatment
and sites
Treatment
and sites
OT OT OT OT OT OT OT OT OT OT OT OT
SE SE SE SE SE SE SE SE SE SE SE SE
IMB NMB IMidB NmidB IDB NDB IMP NMP IMidP NMidP IDP NDP
OT OT OT OT OT OT OT OT OT OT OT OT
SE SE SE SE SE SE SE SE SE SE SE SE
IMB NMB IMidB NmidB IDB NDB IMP NMP IMidP NMidP IDP NDP
OT OT OT OT OT OT OT OT OT OT OT OT
SE SE SE SE SE SE SE SE SE SE SE SE
IMB NMB IMidB NmidB IDB NDB IMP NMP IMidP NMidP IDP NDP
Boxplot of pocket depth for first premolars, OT vs SE
Boxplot of pocket depth for lateral incisors, OT vs SE
Boxplot of pocket depth for canines, OT vs SE
3.0
2.5
2.0
1.5
1.0
0.5
3.0
2.5
2.0
1.5
1.0
3.0
2.5
2.0
1.5
1.0
0.5
0.0
significantly greater than the number of control
canines with loss of attachment (Table III). On the
impacted sides, attachment loss (in any site) was
found in five subjects (35.7 per cent) in the OT
group and in 10 subjects (71.4 per cent) in the SE
group. The proportion of subjects with attachment
loss on the impacted side in both groups was not
significantly different (Fishers Exact test; p = 0.128).
The maximum loss of attachment around any of the
six teeth tested was 1.75 mm. The maximum loss of
attachment in the SE group was greater than the loss
of attachment in the OT group at the 10 per cent
level of significance (Mood Median test: p = 0.058).
Ninety-five per cent confidence levels indicated that
SE treatment would result in a maximum attachment
loss of up to 1.01 mm greater than in the OT group.
All teeth tested responded normally to the percussion
test. More teeth failed to respond to the cold thermal
test (19 teeth) compared with the electrical pulp test
(2 teeth), but only two teeth did not respond to both
tests. One of these was a lateral incisor on the non-
impacted side in the OT group and the other was a
lateral incisor on the impacted side in the SE group.
The pulpal responses by the teeth in the SE and OT
groups were similar (p > 0.05).
None of the teeth (canines, lateral incisors, pre-
molars) showed periapical pathology on the radio-
graphs. Pulpal pathology was not detected in any
teeth on the control side in either group. The pulps
were partially obliterated in two premolars (14 per
cent) and one canine (7 per cent) on the impacted
side in the OT group, and in two lateral incisors (14
per cent) on the impacted side in the SE group. One
lateral incisor (7 per cent) on the impacted side from
the surgical group was endodontically treated prior to
orthodontic treatment due to trauma. Overall, four
out of 27 subjects (15 per cent) showed partial pulpal
obliteration or had root treatment on the impacted
side compared with the control side and this is sig-
nificant at the 10 per cent level of significance
(McNemar test, p = 0.064).
Discussion
Both methods of treatment for palatally impacted
maxillary canines had comparable periodontal and
pulpal outcomes. Both methods were accompanied
by minor periodontal changes, and a higher incidence
of pulpal changes occurred in the previously
impacted canines. The latter did not appear to be of
any clinical significance. The choice of treatment may
depend on the clinical situation, the patients and the
orthodontists preferences. Conservative surgical
exposure followed by assisted eruption was more
suited to severe impactions.
A potential problem with the present study is the
small sample size. Analysis of the required sample size
to detect a difference between the groups was not per-
formed as the magnitude of the difference between
the groups had not been previously tested. While
there was no indication that the small sample
affected our ability to draw conclusions regarding the
periodontal outcomes, a larger sample may have
improved our ability to detect a difference in the pul-
pal outcomes. The possibility of sampling bias cannot
be dismissed as any retrospective study may be prone
to selection bias, where patients unhappy with the
treatment outcome may be unwilling to participate in
the study, resulting in an underestimation of the com-
plications of the treatment. One of the strengths of
our study is our finding that the age of the subjects
and the duration of active treatment of the two
groups were similar.
Although we found more previously impacted
canines than control canines in the SE group had lost
SURGICAL AND NON- SURGICAL METHODS OF TREATING PALATALLY IMPACTED CANINES. I - PERIODONTAL AND PULPUL OUTCOMES
Australian Orthodontic Journal Volume 23 No. 1 May 2007 5
Table III. Loss of periodontal attachment in the OT and SE groups.
OT SE OT vs SE
Teeth (N=14) (N=14) Impacted side
Impacted side Control side p
Impacted side Control side p
p
+
Lateral incisors 3 1 0.500 4 0 0.125 0.661
Canines 5 1 0.125 7 0 0.004 0.440
Premolars 2 1 1.000 2 0 0.500 1.000
McNemar test, significant value in bold
+
Fishers Exact test
some periodontal attachment, the difference between
the impacted sides in the OT and SE groups was not
statistically significant. The proportion of subjects
with attachment loss at all sites suggests that impact-
ed canines fared less favourably than the control
canines in the SE group, which is in agreement with
previous studies.
11,16,23,24
Impacted canines treated
surgically may be more likely to suffer some loss of
attachment than impacted canines treated non-
surgically. Gingival recession with an exposed cemento-
enamel junction was not found in any of the
subjects. Attachment loss appeared to be confined
to particular subjects and was usually present in
multiple sites. Loss of periodontal attachment on the
control side was minimal and found in only one sub-
ject. This subject demonstrated poor oral hygiene at
the recall appointment and had generalised enamel
demineralisation indicative of inadequate plaque
control during orthodontic treatment, and loss of
periodontal attachment on both the impacted and
control sides. Attachment loss appears to be a rare
event in patients receiving treatment for impacted
canines.
14,16
Pulpal changes were similar in both groups. Five out
of 84 teeth (6 per cent) on the impacted side showed
partial pulpal obliteration or were treated endo-
dontically, which is significantly higher than the con-
trol side. Only teeth from the impacted side were
affected, but these effects were not limited to the
canines. They included two premolars in the OT
group and two lateral incisors in the SE group. In
agreement with Blair et al.
15
we found few teeth on
the impacted side had pulpal changes, and fewer teeth
than the number reported by Woloshyn et al.
13
The
subjects in Woloshyn et al.s study were four years
older and had a wider age range than our study,
which may account for this difference since pulpal
obliteration is age-related.
22
Changes in the pulpal
response and radiographic appearance reflect changes
within the dental pulp, but the long-term impact of
these changes on pulpal health cannot be determined.
A longer study will be required to address these
concerns.
In terms of the periodontal and pulpal outcomes,
extraction of the primary canine followed by ortho-
dontic space opening to encourage the eruption of
the impacted permanent canine appears to be a
satisfactory alternative to surgical exposure and
assisted eruption, providing clinical indications such
as age of the patient and degree of impaction are
taken into account.
Conclusions
Within the limitations of this study, the following
conclusions are reached:
1. Encouraged natural eruption and conservative
surgical exposure with orthodontic alignment have
minor effects on the periodontium.
2. Increased incidence of pulpal changes were
observed in previously impacted canines after both
methods of treatment.
3. As both methods of treatment resulted in similar
periodontal and pulpal outcomes the choice of treat-
ment may depend on clinical indications, the
patients and the orthodontists preferences.
Acknowledgments
This study was supported by a grant from the
Australian Society of Orthodontists Foundation for
Research and Education. The authors would like to
thank the orthodontists who were involved in this
study for their assistance with assembling the study
sample and data collection.
Corresponding author
Dr R. J. Olive
141 Queen Street
Brisbane, Qld 4000
Australia
Email: r.h.olive@uq.net.au
References
1. Ericson S, Kurol J. Radiographic examination of ectopically
erupting maxillary canines. Am J Orthod Dentofacial
Orthop 1987;91:48392.
2. Bishara SE. Impacted maxillary canines: a review. Am J
Orthod Dentofacial Orthop 1992;101:15971.
3. McSherry PF. The ectopic maxillary canine: a review. Br J
Orthod 1998;25:20916.
4. Lappin MM. Practical management of the impacted
maxillary cuspid. Am J Orthod 1951;37:76978.
5. Newcomb MR. Recognition and interception of aberrant
canine eruption. Angle Orthod 1959;29:1618.
6. Ericson S, Kurol J. Early treatment of palatally erupting
maxillary canines by extraction of the primary canines. Eur
J Orthod 1988;10:28395.
7. Power SM, Short MB. An investigation into the response of
palatally displaced canines to the removal of deciduous
canines and an assessment of factors contributing to
favourable eruption. Br J Orthod 1993;20:21523.
LING ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 6
8. Becker A. The Orthodontic Treatment of Impacted Teeth.
Martin Dunitz Ltd; 1998.
9. Olive RJ. Orthodontic treatment of palatally impacted
maxillary canines. Aust Orthod J 2002;18:6470.
10. Leonardi M, Armi P, Franchi L, Baccetti T. Two interceptive
approaches to palatally displaced canines: a prospective
longitudinal study. Angle Orthod 2004;74:5816.
11. Wisth PJ, Norderval K, Boe OE. Comparison of two sur-
gical methods in combined surgical-orthodontic correction
of impacted maxillary canines. Acta Odontol Scand 1976;
34:537.
12. Boyd RL. Clinical assessment of injuries in orthodontic
movement of impacted teeth. I. Methods of attachment. Am
J Orthod 1982;82:47886.
13. Woloshyn H, Artun J, Kennedy DB, Joondeph DR. Pulpal
and periodontal reactions to orthodontic alignment of
palatally impacted canines. Angle Orthod 1994;64:25764.
14. Becker A, Kohavi D, Zilberman Y. Periodontal status fol-
lowing the alignment of palatally impacted canine teeth. Am
J Orthod 1983;84:33236.
15. Blair GS, Hobson RS, Leggat TG. Posttreatment assessment
of surgically exposed and orthodontically aligned impacted
maxillary canines. Am J Orthod Dentofacial Orthop 1998;
113:32932.
16. Wisth PJ, Norderval K, Boe OE. Periodontal status of ortho-
dontically treated impacted maxillary canines. Angle Orthod
1976;46:6976.
17. Burden DJ, Mullally BH, Robinson SN. Palatally ectopic
canines: closed eruption versus open eruption. Am J Orthod
Dentofacial Orthop 1999;115:6404.
18. Lindauer SJ, Rubenstein LK, Hang WM, Andersen WC,
Isaacson RJ. Canine impaction identified early with
panoramic radiographs. J Am Dent Assoc 1992;123:912,
957.
19. Silness J, Loe H. Periodontal disease in pregnancy.
II. Correlation between oral hygiene and periodontal
condition. Acta Odontol Scand 1964;22:12135.
20. Loe H, Silness J. Periodontal disease in pregnancy.
I. Prevalence and severity. Acta Odontol Scand 1963;21:
53351.
21. Cave SG, Freer TJ, Podlich HM. Pulp-test responses in
orthodontic patients. Aust Orthod J 2002;18:2734.
22. Jacobsen I, Kerekes K. Long-term prognosis of traumatized
permanent anterior teeth showing calcifying processes in the
pulp cavity. Scand J Dent Res 1977;85:58898.
23. Hansson C, Linder-Aronson S. Gingival status after ortho-
dontic treatment of impacted upper canines. Trans Eur
Orthod Soc 1972:43341.
24. Kohavi D, Becker A, Zilberman Y. Surgical exposure, ortho-
dontic movement, and final tooth position as factors in
periodontal breakdown of treated palatally impacted
canines. Am J Orthod 1984;85:727.
SURGICAL AND NON- SURGICAL METHODS OF TREATING PALATALLY IMPACTED CANINES. I - PERIODONTAL AND PULPUL OUTCOMES
Australian Orthodontic Journal Volume 23 No. 1 May 2007 7
Introduction
Despite extensive interest in the aetiology and man-
agement options for ectopic canines, only a few stud-
ies have focussed on the position and colour of the
canines after treatment.
15
The maxillary canine is
situated in a strategic position between the anterior
and posterior segments and has important roles in an
attractive smile and a functional occlusion.
6,7
Early diagnosis and interceptive treatment with
extraction of the overlying primary canines have been
advocated for the management of impacted maxillary
canines.
8,9
In less severe and uncrowded cases this
simple procedure is relatively successful.
10
However, a
recent prospective study of palatally impacted canines
failed to find any difference between the success rates
of impacted maxillary canines treated with extraction
of the overlying primary canines and no treatment.
11
In patients with crowding in the canine region,
between 75 and 80 per cent of palatally impacted
canines will emerge without direct orthodontic assis-
tance if space is created in the upper arch.
11,12
If a
palatally impacted canine fails to erupt following
Australian Orthodontic Journal Volume 23 No. 1 May 2007 8
Comparison of surgical and non-surgical methods
of treating palatally impacted canines.
II - Aesthetic outcomes
Kwok K. Ling,
*
Christopher T. C. Ho,
*
Olena Kravchuk
and Richard J. Olive
School of Dentistry,
*
School of Land and Food Sciences,
University of Queensland and Specialist practice,
Brisbane, Australia
Background: Palatally impacted maxillary canines may appear unsightly after treatment because of changes in position and
colour.
Aim: To determine if palatally impacted canines treated either by surgical exposure and orthodontic repositioning or by creation
of space in the arch and unassisted eruption have different aesthetic outcomes.
Methods: Twenty eight subjects with unilateral palatally impacted canines who had completed orthodontic treatment at least
6 months previously were recruited from three specialist practices. In 14 subjects the canines had been treated by surgical
exposure, orthodontic extrusion and repositioning in the arch (SE group) and in the remainder the deciduous canines were
extracted and excess space created in the arch for the canines to erupt naturally (OT group). The contralateral canines were
used as controls. The mean pretreatment ages of the subjects in the SE and OT groups were 13.5 (SD: 1.6) years and 13.5
(SD: 1.3) years respectively. The position and colour of the canines were assessed on post-treatment study models and 35 mm
slides using the American Board of Orthodontics Objective Grading System (ABO OGS) and subjective appraisal by two
orthodontists. Each subject used a semantic scale to rate the aesthetic outcome of treatment.
Results: Sixty four per cent of the treated canines in the SE group were significantly more intruded than the treated canines
in the OT group (p = 0.004) and the control canines (p = 0.004). The ABO OGS grades of the canines in the SE and OT
groups were similar (p = 0.173). While the assessors detected a lack of labial root torque and gingival margin changes in
the canines in the SE group, the subjects in both groups were satisfied with the appearance of the canines post-treatment.
Conclusions: Palatally impacted canines treated by surgical exposure, extrusion and orthodontic treatment were more likely to
be displaced vertically (intruded) after treatment than palatally impacted canines treated by extraction of the overlying
deciduous canines and creation of excess space in the arch. Small occlusal and aesthetic changes detected by the
orthodontists, but not the ABO OGS, did not appear to detract from the satisfaction of the subjects with the results of
orthodontic treatment.
(Aust Orthod J 2007; 23: 815)
Received for publication: July 2006
Accepted: February 2007
extraction of the overlying primary canine and cre-
ation of excess space in the arch, the most reliable
treatment option is surgical exposure and ortho-
dontic repositioning of the impacted tooth in the
arch.
A reliable and objective method is required to evalu-
ate tooth position following treatment. Previous stud-
ies have relied on assessments by orthodontists, by
other dental professional groups, by the public, and
measuring instruments, such as the American Board
of Orthodontics Objective Grading System (ABO
OGS).
5,1316
The ABO OGS scores eight criteria,
which are considered to provide a reliable and objec-
tive appraisal of tooth position.
16
There have been no
previous reports of the use of the ABO OGS to deter-
mine the stability, or otherwise, of specific traits of
malocclusion. A trained and observant eye may detect
minor deviations in tooth position(s) that patients
may be either unaware of or are satisfied with.
17,18
Patient perception and satisfaction may be assessed
with instruments such as a semantic scale or a
questionnaire.
The principal aim of this retrospective study was to
determine if palatally impacted canines treated either
by surgical exposure and orthodontic repositioning or
by creation of space in the arch and unassisted erup-
tion have different aesthetic outcomes. Additional
aims were to determine if the ABO OGS could be
used to assess the positions of the canines after treat-
ment and to determine if the method of treatment
influenced patient satisfaction.
Material and methods
Ethical clearance for this study was granted by the
Medical Research Ethics Committee of the University
of Queensland. Twenty eight subjects with unilateral
palatally impacted canines who had completed ortho-
dontic treatment at least 6 months previously were
recruited from three specialist practices. In 14 sub-
jects the canines had been treated by surgical
exposure, orthodontic extrusion and repositioning in
the arch (SE group) and in the remainder, the decid-
uous canines were extracted and excess space created
in the arch for the canines to erupt naturally (OT
group). Subjects were selected if they met the
following criteria:
1. A unilateral palatally impacted canine was present.
2. A pretreatment panoramic radiograph was
available.
3. There was no significant medical history.
4. Treatment had been completed at least six months
previously.
5. In the surgical group, the subjects had undergone
conservative surgical exposure and the wound had
been dressed for 710 days before any orthodontic
attachments were bonded.
The 14 subjects (5 males, 9 females) in the OT group
had a mean age of 19.1 (SD: 2.2) years and the mean
post-treatment period was 3.4 (SD: 3.0) years. The
same orthodontist treated all subjects in the OT
group. The 14 subjects (2 males, 12 females) in the
SE group had a mean age of 18.8 (SD: 2.5) years and
the mean post-treatment period was 3.2 (SD: 2.4)
years (Table I). Three orthodontists treated the sub-
jects in the SE group. The pretreatment panoramic
radiographs were used to classify the sector of
impaction using Lindauer et al. modification
19
of
Ericson and Kurols classification.
9
No sector I
impacted canines were included in the study.
DIFFERENT METHODS OF TREATING PALATALLY IMPACTED CANINES. II - AESTHETIC OUTCOMES
Australian Orthodontic Journal Volume 23 No. 1 May 2007 9
Table I. Description of the sample.
OT (N=14) SE (N=14) p
p
+
Mean SD Mean SD
Male : Female 5 : 9 2 : 12 0.190
Right : Left proportion 8 : 6 4 : 10 0.127
Sector of impaction II : III : IV 5 : 7 : 2 1 : 4 : 9 0.019
Age at start of treatment (years) 13.5 1.3 13.5 1.6 0.979
Age at recall (years) 19.1 2.2 18.8 2.5 0.749
Active treatment duration (months) 27.9 9.3 28.4 7.5 0.877
Recall period (years) 3.4 3.0 3.2 2.4 0.847
Chi-squared test, significant value in bold
+ Students t - test
American Board of Orthodontics Objective
Grading System
All subjects had a wax occlusal record and alginate
impressions of both arches taken at the post-
treatment assessment. The resulting study models
were scored by a single examiner (KKL) with no prior
knowledge of the side of impaction or the method of
treatment. The alignment, marginal ridges, bucco-
lingual inclinations, interproximal contacts, overjet,
occlusal contacts and occlusal relationships of the
teeth were assessed with the ABO OGS and the
standardised measuring gauge. Root angulations were
not assessed because post-treatment panoramic radio-
graphs were not available. For each criterion, points
were assigned based on the degree to which a
relationship deviated from ideal. The individual com-
ponents were scored and summed to yield an overall
score. To assess intra-examiner reliability the ABO
OGS scoring was repeated one week later.
Canine position and dental midline
The positions of both maxillary canines in each sub-
ject in relation to the adjacent teeth and the upper
and lower dental midlines were analysed on the
dental casts by one examiner. Intrusions, rotations
and palatal translations were recorded as present or
absent. Canines were classified as intruded when
there was no inter-arch contact or the height differ-
ence between the canines and adjacent teeth was
greater than one millimetre. A rotation was recorded
if a tooth was rotated more than five degrees. A
canine was in palatal translation if the buccal overjet
was reduced by more than one millimetre, if the
tooth was in edge-to-edge relationship or in lingual
cross-bite. The upper and lower dental midlines were
measured with digital callipers.
Canine colour and side of impaction
Two independent orthodontists (Assessor A and
Assessor B) subjectively assessed the colour of the
maxillary canines on projected 35 mm Kodachrome
slides of the frontal smile, the anterior occlusal view
and the upper occlusal view. The slides were taken at
standardised settings with the same camera at the
post-treatment assessments. The assessors were
unaware of the side of impaction and method of
treatment. They were asked to assess the colour of
both canines and to identify the side of impaction
from the dental casts and colour slides.
Questionnaire
Subject satisfaction with the overall appearance of the
canines, colour of the canines, colour of the lateral
incisors and position of the canines were evaluated by
questionnaire. The subjects were asked to rate their
satisfaction with each of the four characteristics on a
5 point scale. The scale was anchored with the
descriptors, very satisfied and very dissatisfied.
Statistical analysis
Statistical analysis was carried out with Minitab for
Windows (Release 14, Minitab Inc., USA) and the
level of significance for all statistical procedures was
set at 5 per cent. Additionally, SPSS for Windows
(Version 12.0, SPSS Inc., Chicago, USA) was used to
perform the McNemar test. The Bonferroni correc-
tion was applied when appropriate. The age of the
subjects at commencement of active treatment, ages
at recall, the durations of treatment and the post-
treatment follow-up periods in the groups were
compared with Students t-tests. Chi-squared tests
were used to determine if there were different pro-
portions of subjects in the impaction sectors in the SE
and OT groups. The durations of treatment carried
out by the three orthodontists were examined with
the one-way analysis of variance. Post-hoc Tukey tests
were used to test the differences between pairs of
orthodontists.
Intra-observer duplication error for the ABO OGS
overall score was tested with the paired t-test. Overall
ABO OGS scores were analysed for the two treat-
ment groups. A one-way ANOVA was used to check
for a difference in ABO OGS scores between ortho-
dontists. Attribute agreement analysis (Cohens
Kappa) was used to examine the intra-examiner relia-
bility in determination of deviation from an ideal
canine position. As the results indicated a high degree
of reliability (Kappa: 0.65-1), either the initial or the
second set of measurements was chosen randomly to
be tested with Fishers Exact test for differences in the
proportions of canine intrusion, rotation and palatal
displacement in the groups. Comparison within each
group (palatally impacted canine versus the contra-
lateral canine) was tested with McNemar tests.
Differences in midline deviations between OT and
SE groups were tested with the Mann-Whitney U test.
Inter-examiner agreement for canine colour and iden-
tification of a previously palatally impacted maxillary
LING ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 10
canine from dental casts and colour slides were
analysed using attribute agreement analysis and
Cohens Kappa. The inter-examiner agreement was
low. Thus, results from each orthodontist assessor
were analysed separately with Fishers Exact test.
Ordinal data from the questionnaires assessing
patient satisfaction were analysed with the Mann-
Whitney U test.
Results
The results are given in Tables IVI and Figures 13.
There were significantly more sector IV canines in the
SE group and the durations of active treatment of the
three orthodontists were significantly different
(Tables I and II). The post-hoc Tukey test disclosed
that Orthodontist A took significantly longer than
Orthodontists B and C to complete treatment, but
there was no difference in the time taken by Ortho-
dontists B and C to complete treatment (Table II).
The scatter plot of the treatment duration versus age
at the commencement of treatment did not indicate
any relationship between the two variables (Figure 1).
Approximately 41 per cent of the variability in treat-
ment time of the subjects in the SE group was
accounted for by age at the commencement of treat-
ment and the orthodontist providing the treatment
(SE group: r-square, 40.68 per cent).
There was no statistically significant difference
between the two sets of ABO OGS overall scores
(p = 0.224). The first set of scores were used for
further analysis. When the distribution of the ABO
OGS overall scores was examined, nine subjects in
the OT group (64 per cent) and six subjects in the SE
group (43 per cent) had overall scores greater than 30
and failed to meet the treatment standards of the
DIFFERENT METHODS OF TREATING PALATALLY IMPACTED CANINES. II - AESTHETIC OUTCOMES
Australian Orthodontic Journal Volume 23 No. 1 May 2007 11
Table II. Duration of active treatment.
Treatment duration (Months) p
Mean SD Range
Orthodontist A
(N=3) 37.67 (4.16)
a
3341
Orthodontist B
N=8) 28.13 (5.08)
b
2136
Orthodontist C
(N=3) 20.00 (5.00)
b
1525
0.004
Different letters in the Mean (SD) column indicate a significant
difference
One-way ANOVA, significant value in bold
Figure 1. Treatment duration versus age at the commencement of active
treatment.
Table III. Frequency of intrusion, rotation and palatal translation of previously impacted canines (PIMC).
Intrusion Rotation Palatal translation
PIMC Control p
+
PIMC Control p
+
PIMC Control p
+
OT (N=14) 1 0 1.000 4 0 0.125 1 1 1.000
SE (N=14) 9 0 0.004 8 1 0.039 4 0 0.125
p
0.004 1.000 0.252 1.000 0.326 1.000
Significant values in bold
Fishers Exact test
+
McNemar test
Table IV. Discolouration of impacted canines reported by two
orthodontists.
OT (N=14) SE (N=14) p
Assessor A 2 5 0.190
Assessor B 1 1 1.000
Chi-squared test
Treatment commencement age (Years)
T
r
e
a
t
m
e
n
t
d
u
r
a
t
i
o
n
(
M
o
n
t
h
s
)
Ortho/Surgical
OT
SE
ABO. The ABO OGS scores for the OT (Mean:
39.9; SD:14.7) and SE (Mean: 32.6; SD:13.0)
groups were not significantly different (p = 0.173).
There were no significant differences between the
overall scores for the patients in the SE group treated
by each of the three orthodontists. The mean overall
ABO OGS scores for orthodontists A, B and C were
22.83, 36.88 and 30.83 respectively.
The number of previously impacted and control
(contralateral) canines that were intruded, rotated
and/or palatally placed in the OT and SE groups are
given in Table III. Nine out of 14 treated canines (64
per cent) in the SE group were intruded. Of the
treated canines more teeth were intruded in the SE
group compared with the OT group (p = 0.004) and
the control canines (p = 0.004). The latter finding
was statistically significant after the Bonferroni
correction had been applied. In the SE group more
treated canines were rotated at recall than control
canines (p = 0.039). There was no significant differ-
ence in midline deviations in the OT (Mean: 0.40
mm) and SE (Mean: 0.66 mm) groups. The
maximum midline deviations in the OT and SE
groups were 2.58 mm and 1.58 mm respectively
(Figure 2).
There were no significant inter-group differences in
the colour of the previously impacted teeth (Table
IV). Assessor A correctly identified 11 previously
impacted canines in the OT group and 12 teeth the
SE group (Table V). Assessor B was uncertain in eight
(57 per cent) cases in the OT group and two cases in
the SE group (14 per cent). Assessor B correctly iden-
tified five cases in the OT group and 12 cases in the
SE group. Both assessors used differences in inclina-
tion and the appearance of the labial and palatal
gingival contours to identify previously impacted
canines.
The subjects were generally satisfied or very satis-
fied with the colour and positions of the treated
canines. Only one subject in the OT group chose
very dissatisfied as the response to the question
about overall appearance. Similarly, the majority of
subjects were satisfied or very satisfied with the
colour of the lateral incisors and only one subject
from each group was dissatisfied. There were no sig-
nificant differences between the OT and SE groups to
the questions relating to overall satisfaction, colour of
the lateral incisors, colour and position of previously
impacted maxillary canines (Table VI). There was
also no significant difference between the OT and SE
LING ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 12
Figure 2. Individual post-treatment dental midline deviation. Figure 3. Overall ABO OGS score versus total satisfaction score.
A high score indicates a poor occlusal outcome and a low score greater
satisfaction.
Table V. Identification of previously impacted canines by two orthodontists.
OT (N=14) SE (N=14)
Incorrect Correct Uncertain Incorrect Correct Uncertain
Assessor A 3 11 0 2 12 0
Assessor B 1 5 8 0 12 2
Ortho/Surgical
Total satisfaction score
D
e
n
t
a
l
m
i
d
l
i
n
e
d
e
v
i
a
t
i
o
n
(
m
m
)
A
v
e
r
a
g
e
o
v
e
r
a
l
l
A
B
O
O
G
S
s
c
o
r
e
Ortho/Surgical
OT
SE
95% CI for the mean
groups when the scores of the four questions were
combined (p = 0.448). Finally, there was no signifi-
cant correlation between the combined satisfaction
scores and the ABO OGS scores (Figure 3).
Discussion
We set out to determine if palatally impacted canines
surgically exposed and repositioned in the arch had
better crown colour and position than canines per-
mitted to erupt naturally after excess space had been
created in the maxillary arch. Although the clinicians
were able to identify small variations in the positions
of the canines that the ABO OGS could not pick up,
the subjects were generally very satisfied with the out-
come.
The main limitation in this study is related to the
method of sampling. In this study, consecutively
treated patients fitting the inclusion criteria were
retrospectively identified and invited to participate.
The participation rate was only 58 per cent, which
resulted in a relatively small sample. Bias due to satis-
fied patients being more likely to participate in the
study cannot be eliminated. Another problem relat-
ing to the small sample size is the possibility of
having a Type II error, so that the null hypothesis is
wrongly accepted due the inability to detect a differ-
ence. The probability of a Type II error decreases as
the sample size increases. While the best strategy is to
obtain the largest possible sample, this was not pos-
sible because of the low participation rate.
20
A future
prospective study would be able to address some of
these concerns. There are also recognised objections
to the validity of findings from questionnaires, since
some respondents might have been inclined to select
the perceived right answer and selecting a suitable
answer format inevitably inhibits free expression.
21
Hence, the findings from the patient satisfaction
survey in this study may be optimistic.
Ideal alignment in the present study was 71 per cent
in the OT group and 14 per cent in the surgical
group. The result from the surgical group was much
lower than reported in the literature, which ranges
from 4048 per cent.
2,3,5
The differences between the
studies may be due to the differences in the criteria
for determining rotation, intrusion and palatal trans-
lation. Generally, it is accepted that some degree of
relapse is inevitable,
25
but the changes found in this
study were surprising. In the SE group, the previ-
ously impacted canines were intruded in nine subjects
(64 per cent) and rotated in eight subjects (57 per
cent). These are much higher proportions than in the
OT group or on the control sides in both groups.
Palatal displacement was a marginally less frequent
finding with four subjects (29 per cent) in the SE
group affected. Even though four subjects (29 per
cent) in the OT group presented with rotation of
previously impacted canines, palatal displacement
and intrusion rarely occurred in this group.
A concern with the technique of allowing an
impacted canine to erupt naturally is that a residual
DIFFERENT METHODS OF TREATING PALATALLY IMPACTED CANINES. II - AESTHETIC OUTCOMES
Australian Orthodontic Journal Volume 23 No. 1 May 2007 13
Table VI. Subject satisfaction post-treatment.
Very satisfied Satisfied Dont know Not satisfied Very dissatisfied p
Overall appearance OT 6 7 0 0 1
(Impacted canines) SE 6 8 0 0 0
0.872
Colour (PIMC) OT 5 8 0 1 0
(Impacted canines) SE 2 12 0 0 0
0.505
Colour - lateral OT 5 8 0 1 0
incisors SE 2 7 4 1 0
0.108
Position OT 5 7 1 1 0
(Impacted canines) SE 5 8 1 0 0
0.836
Mann-Whitney U test
dental midline deviation may persist post-treatment.
The technique involves the creation of excess space of
up to 10 mm and may require proclination and
displacement of the maxillary incisors across the mid-
line. Investigation of midline deviations yielded no
significant difference between the groups.
The ABO OGS found the scores for both groups
were similar, implying a similar standard of finishing
or amount of relapse. However, the scores did not
agree with the clinical assessment. The main reason
for the failure to detect a difference could be related
to the method of scoring the models. The full ABO
OGS sums the discrepancies in all criteria and it is
not sensitive enough to detect a small departure from
the ideal position, and it is not designed to assess the
positional deviation(s) of an impacted canine.
One of the factors that may influence the occlusal
outcome is the duration of active orthodontic treat-
ment.
22,23
In the present study there was no signifi-
cant difference between the groups in the duration of
treatment. The mean duration of treatment in the SE
group was 28 months and was comparable with other
studies where active eruption was used following
surgical exposure.
3,24
There was no colour difference between the canines
in the two groups. It was not possible to determine
the incidence of discolouration because of the poor
agreement between the assessors. Identification of
previously impacted canines by the two assessors also
showed poor agreement, although they were more
likely to correctly identify a previously impacted
canine in the SE group than in the OT group. The
lesser amount of relapse in the OT group may have
made identification of a previously impacted canine
difficult.
There was a high level of patient satisfaction follow-
ing both methods of treatment. Only one subject
from the OT group expressed dissatisfaction with
treatment, but this was not correlated with the
occlusal outcome, as demonstrated by the ABO OGS
score for this subject. Clustering of the satisfaction
scores in this study into a narrow range, irrespective
of the ABO OGS scores, indicates satisfaction was not
dependent on or correlated with occlusal outcome
(Figure 3). Overall, palatally impacted canines cor-
rected by extraction of the overlying primary canine and
orthodontic space opening showed better alignment
and less relapse than canines managed with surgical
exposure, extrusion and orthodontic alignment.
Conclusions
1. Palatally impacted canines treated by surgical
exposure, extrusion and orthodontic treatment were
more likely to relapse vertically than those treated by
extraction of the overlying deciduous canines and
creation of excess space in the arch.
2. The ABO OGS failed to detect small changes in
the positions of the canines in both groups.
3. There were no colour differences between the pre-
viously impacted canines in the two groups. The
assessors correctly identified high percentages of pre-
viously impacted canines in the surgical group, but
not the non-surgical group.
4. The subjects in both groups were satisfied with the
outcome of treatment.
Acknowledgments
This study was supported by a grant from the
Australian Society of Orthodontists Foundation for
Research and Education. The authors would like to
thank the orthodontists who were involved in this
study for their assistance with assembling the sample
and collecting the data.
Corresponding author
Dr R. J. Olive
141 Queen Street
Brisbane, Qld 4000
Australia
Email: r.h.olive@uq.net.au
References
1. Bennett JC, McLaughlin PP. Orthodontic management of
the dentition with the preadjusted appliance. Isis Medical
Media Ltd.; 1997.
2. Becker A, Kohavi D, Zilberman Y. Periodontal status fol-
lowing the alignment of palatally impacted canine teeth. Am
J Orthod 1983;84:3326.
3. Woloshyn H, Artun J, Kennedy DB, Joondeph DR. Pulpal
and periodontal reactions to orthodontic alignment of
palatally impacted canines. Angle Orthod 1994;64:25764.
4. Blair GS, Hobson RS, Leggat TG. Posttreatment assessment
of surgically exposed and orthodontically aligned impacted
maxillary canines. Am J Orthod Dentofacial Orthop 1998;
113:32932.
5. DAmico RM, Bjerklin K, Kurol J, Falahat B. Long-term
results of orthodontic treatment of impacted maxillary
canines. Angle Orthod 2003;73:2318.
6. Bishara SE. Clinical management of impacted maxillary
canines. Semin Orthod 1998;4:8798.
7. Karpagam S, Chacko RK. Guidelines for management of
impacted canines. Indian J Dent Res 2004;15:4853.
LING ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 14
DIFFERENT METHODS OF TREATING PALATALLY IMPACTED CANINES. II - AESTHETIC OUTCOMES
Australian Orthodontic Journal Volume 23 No. 1 May 2007 15
8. Ericson S, Kurol J. Radiographic examination of ectopically
erupting maxillary canines. Am J Orthod Dentofacial
Orthop 1987;91:48392.
9. Ericson S, Kurol J. Early treatment of palatally erupting
maxillary canines by extraction of the primary canines. Eur
J Orthod 1988;10:28395.
10. Power SM, Short MB. An investigation into the response of
palatally displaced canines to the removal of deciduous
canines and an assessment of factors contributing to
favourable eruption. Br J Orthod 1993;20:21523.
11. Leonardi M, Armi P, Franchi L, Baccetti T. Two interceptive
approaches to palatally displaced canines: a prospective lon-
gitudinal study. Angle Orthod 2004;74:5816.
12. Olive RJ. Orthodontic treatment of palatally impacted max-
illary canines. Aust Orthod J 2002;18:6470.
13. Scott SA, Freer TJ. Visual application of the American
Board of Orthodontics grading system. Aust Orthod J 2005;
21:5560.
14. Shaw WC, Richmond S, OBrien KD, Brook P, Stephens
CD. Quality control in orthodontics: indices of treatment
need and treatment standards. Br Dent J 1991;170:10712.
15. Tang EL, Wei SH. Recording and measuring malocclusion: a
review of the literature. Am J Orthod Dentofacial Orthop
1993;103:34451.
16. Casko JS, Vaden JL, Kokich VG, Damone J, James RD,
Cangialosi TJ et al. Objective grading system for dental casts
and panoramic radiographs. American Board of Ortho-
dontics. Am J Orthod Dentofacial Orthop 1998;114:
58999.
17. Miller CJ. The smile line as a guide to anterior esthetics.
Dent Clin North Am 1989;33:15764.
18. Kokich VO, Jr., Kiyak HA, Shapiro PA. Comparing the per-
ception of dentists and lay people to altered dental esthetics.
J Esthet Dent 1999;11:31124.
19. Lindauer SJ, Rubenstein LK, Hang WM, Andersen WC,
Isaacson RJ. Canine impaction identified early with
panoramic radiographs. J Am Dent Assoc 1992;123:912,
957.
20. Rinchuse DJ, Sweitzer EM, Rinchuse DJ, Rinchuse DL.
Understanding science and evidence-based decision making
in orthodontics. Am J Orthod Dentofacial Orthop 2005;
127:61824.
21. Shaw WC, Gbe MJ, Jones BM. The expectations of ortho-
dontic patients in South Wales and St Louis, Missouri. Br J
Orthod 1979;6:2035.
22. Lobb WK, Ismail AI, Andrews CL, Spracklin TE. Evaluation
of orthodontic treatment using the Dental Aesthetic Index.
Am J Orthod Dentofacial Orthop 1994;106:705.
23. Dyken RA, Sadowsky PL, Hurst D. Orthodontic outcomes
assessment using the peer assessment rating index. Angle
Orthod 2001;71:1649.
24. Iramaneerat S, Cunningham SJ, Horrocks EN. The effect of
two alternative methods of canine exposure upon subsequent
duration of orthodontic treatment. Int J Paediatr Dent
1998;8:1239.
Introduction
Orthodontic alignment of overlapped incisors can
reduce the apparent heights of the interdental papil-
lae leading to unsightly dark triangles or open
gingival embrasures.
13
It has been suggested that as
overlapped teeth are aligned the interdental papillae
stretch, their heights reduce and open gingival
embrasures develop.
13
Other factors, such as alveolar
bone levels, crown form, contact relationships, pre-
treatment crowding,
46
age,
7
and orthodontic effects
on the gingival fibres may also play a part in the
causation of open gingival embrasures or dark tri-
angles. Recently, Ko-Kimura et al.
8
and Ikeda et al.
9
reported that open gingival embrasures were associ-
ated with resorption of the alveolar crest, and were
more frequently found in patients over 20 years of
age.
Two factors believed to influence the form of the gin-
gival tissues post-treatment are the direction of tooth
movement and the faciolingual thickness of the sup-
porting bone and soft tissue.
10
For example, during
lingual or palatal tooth movement the gingival tissue
on the facial aspect of a tooth thickens and migrates
occlusally. The reverse may occur when teeth are
moved labially.
1113
Providing a tooth is moved with-
in the alveolar process the risk of gingival recession is
Australian Orthodontic Journal Volume 23 No. 1 May 2007 16
Changes in interdental papillae heights following
alignment of anterior teeth
Sanjivan Kandasamy,
*
Mithran Goonewardene
*
and Marc Tennant
Dental School, The University of Western Australia
*
and the Centre for Rural and Remote Oral Health, The University of Western Australia,
Perth, Australia
Background: Orthodontic alignment of overlapped incisors can reduce the apparent heights of the interdental papillae leading
to unsightly dark triangles or open gingival embrasures.
Aim: To determine if certain pretreatment contact point relationships between the maxillary anterior teeth were accompanied by
changes in the heights of the interdental papillae after orthodontic alignment.
Methods: Pre- and post-treatment intra-oral 35 mm slides, lateral cephalometric radiographs and study casts of 143 patients
(60 males, 83 females) between 13 and 16 years of age were used. The patients had diastamata closed, imbricated teeth
aligned and palatally or labially placed teeth repositioned. A sample of 25 patients (12 males, 13 females) between 13 and
16 years of age who had well-aligned anterior teeth at the start of treatment acted as a control group. All patients were
treated for approximately 18 months. The clinical crowns of the maxillary incisors and the heights of the interdental papilla
between the incisors were measured on projected images of the slides. The percentage increases or reductions in the heights of
the interdental papillae were compared.
Results: The heights of the interdental papillae increased following palatal movement of labially placed (p < 0.05) or
imbricated (p < 0.05) incisors and the intrusion of one incisor relative to an adjacent incisor (p < 0.01). The heights of the
interdental papillae reduced following labial movement of an imbricated (p < 0.05) or palatally placed (p < 0.05) incisor or
closure of a diastema (p < 0.01). Before treatment the midline papillae in the diastema subgroup were of similar length to the
midline papillae in the control group, but after treatment they were markedly shorter. The interdental papillae associated with
crowded or imbricated incisors were shorter than the interdental papillae in the control group before and after treatment.
Conclusions: Dark triangles are less likely to develop following palatal movement of labially placed or imbricated teeth and the
intrusion of one tooth relative to another. On the other hand, dark triangles are more likely to develop following labial move-
ment of imbricated or palatally placed incisors and closure of a diastema. Clinicians should be alert to the possibility of dark
triangles developing in the latter group, particularly in older patients.
(Aust Orthod J 2007; 23: 1623)
Received for publication: July 2006
Accepted: January 2007
minimal, irrespective of the dimensions or quality of
the gingival tissue.
14
The aim of this study was to determine if certain pre-
treatment contact point relationships between the
maxillary anterior teeth were accompanied by
changes in the heights of the interdental papillae after
orthodontic alignment.
Materials and methods
Ethical approval for this study was obtained from the
Human Research Ethics Committee of the University
of Western Australia. All assessments were carried out
in accordance with the guidelines of the National
Health and Medical Research Council of Australia.
All patients who commenced treatment in a private
orthodontic practice in 1996 and required alignment
of the upper anterior teeth were eligible for the study.
Patients with poor oral hygiene exhibiting swollen,
erythematous and/or hyperplastic gingivae, with
incomplete records and when two or more of the
contact relationships given in Table I were present,
were excluded. Patients with the latter condition were
excluded because the interdental papilla between the
teeth could be influenced differently by the different
tooth movements required to align the teeth. A total
of 143 patients (60 males, 83 females) between 13
and 16 years of age (Mean age: 14 years 7 months)
were available for the experimental group. A sample
of 25 patients (12 males, 13 females) who received
orthodontic treatment in the same practice, but
who had well aligned anterior teeth at the start of
treatment acted as a control group. These patients
were also between 13 and 16 years of age (Mean age:
14 years 4 months).
Pre- and post-treatment intra-oral 35 mm slides,
lateral cephalometric radiographs and study casts
were used. The intra-oral frontal photographs were
taken at the same magnification and standardised by
positioning the upper midline in the centre of the
view finder and sighting along the occlusal plane. All
patients were treated for approximately 18 months
and the post-treatment photographs were taken four
weeks after appliance removal. The pre- and post-
treatment lateral cephalometric radiographs were
used to assess qualitatively the overall direction of
maxillary incisor movement. The study models were
used to determine the arrangement of the anterior
teeth and allocation into the groups given in Table I.
The clinical crowns (incisal edge lowest point on
the gingival margin) of the central and lateral incisors
and the heights of the interdental papillae between
the incisors (tip of an interdental papilla to the line
joining the lowest points on the gingival margins of
adjacent incisors) were measured twice on standard-
ised images of the slides projected onto a white back-
ground (Figure 1). The maxillary incisors in both
experimental and control groups were measured.
Because it was not possible to measure the inter-
dental and crown heights precisely if adjacent teeth
were at different inclinations or displaced palatally/
labially, and pretreatment measurements of the
cemento-enamel junction gingival margin distances
CHANGES IN INTERDENTAL PAPILLAE HEIGHTS FOLLOWING ALIGNMENT OF ANTERIOR TEETH
Australian Orthodontic Journal Volume 23 No. 1 May 2007 17
Table I. Definitions.
Relationship Definition
Diastema The horizontal space between
adjacent incisors
Vertical discrepancy Adjacent incisors in different vertical
positions
Imbricated Incisors arranged in an overlapping
manner, one incisor may be palatally
or labially placed relative to the other
incisor
Labially or palatally Labially or palatally placed incisors.
placed incisors with Study models and lateral intraoral
no overlap photographs were used to determine
if an incisor was imbricated or
labially/palatally placed.
Figure 1. Crown height was measured from the incisal edge to the highest
point on the gingival margin. Interdental papilla height was measured from
the tip of an interdental papilla to the line joining the highest points on the
gingival margins of adjacent incisors.
were not available, the data were converted to per-
centages. The percentage loss or gain in the height of
an interdental papilla(e) were obtained by dividing
the mean height of the interdental papilla(e) by the
mean length of the clinical crowns of the incisors on
either side of the papilla(e) and converting the result
to a percentage. The mean pre- and post-treatment
percentage values were then used to obtain the
percentage increases or reductions.
The statistical analyses were performed using the
Intercooled Stata 8.0 statistical package (SPSS,
Chicago, Illinois, USA). Values of p less than 0.05
were considered significant. All measurements were
repeated by the same examiner two weeks later.
Results of the paired t-test showed there were no
significant differences at the 5 per cent level of signif-
icance between the first and second sets of measure-
ments. To improve the reliability of these measure-
ments the means of both sets of measurements were
used in all subsequent calculations.
Results
The results are given in Table II and Figures 27.
Control group
The mean pre- and post-treatment heights of the
interdental papillae in the control group were 45.6
and 47.1 per cent respectively. The difference
between the pre- and post-treatment heights was not
statistically significant.
Experimental group
Diastema
The diastemata were closed in 28 patients (Table II,
Figure 2). Following closure of diastemata the inter-
dental papillae between the central incisors were
significantly shorter at the end of treatment (Mean
difference: -10.5 per cent; p < 0.01). The post-
treatment heights of the interdental papillae in the
experimental sample were also significantly shorter
than the post-treatment heights of the interdental
papillae in the control group (Mean difference: -9.1
per cent; p < 0.01).
Vertical discrepancy
Before treatment the heights of the interdental papil-
lae in this group were significantly shorter than the
pretreatment heights of the interdental papillae in
the control group (Mean difference: -10.2 per cent;
p < 0.01). The control experimental difference after
treatment was not significant. Following correction of
a vertical discrepancy the interdental papillae
increased in height significantly (Mean difference: 8.1
per cent; p < 0.01). Pre- and post-treatment views of
a typical case are shown in Figure 3.
KANDASAMY ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 18
Table II. Pretreatment and post-treatment comparisons.
Group N Mean Pretreatment p Mean Intra-group p Post-treatment p
pretreatment difference post-treatment change difference
height E minus C height (Per cent) E minus C
(Per cent) (Per cent) (Per cent) (Per cent)
Control 25 56.6 (8.1) 47.1 (8.1) 1.5 NS
Diastema 28 48.5 (7.5) - 2.9 NS 38.0 (8.8) -10.5 0.01 -9.1 0.01
Vertical 31 35.4 (8.6) -10.2 0.01 43.5 (7.7) 8.1 0.01 -3.6 NS
discrepancy
Labially 11 34.6 (7.8) -11.0 0.01 45.1 (9.6) 10.5 0.01 -2.0 NS
overlapped
Palatally 25 43.3 (7.8) -2.3 NS 41.0 (6.1) -2.3 NS -6.1 0.01
overlapped
Labially 10 31.0 (8.3) -14.6 0.01 38.9 (8.6) 7.9 0.01 -8.2 0.05
placed
Palatally 28 42.8 (7.4) -2.8 NS 40.8 (6.5) -2.0 0.05 -6.3 0.01
E, experimental; C, control
NS, not significant
Standard deviations in brackets
Significant values in bold
Imbrication labially overlapped
There were 11 subjects with labially overlapped
teeth (Figure 4). The mean pre- and post-treatment
heights of the interdental papillae were 34.6 and
45.1 per cent respectively. The pretreatment heights
of the interdental papillae in the experimental
group were 11.0 per cent shorter than the pretreat-
ment papillae in the control group (p < 0.01). The
interdental papillae were significantly longer at the
end of treatment (Mean difference: 10.5 per cent;
p < 0.01)
Imbrication palatally overlapped
At the start of treatment the heights of the interden-
tal papillae in the 25 control and 25 experimental
patients were similar. The mean heights of the inter-
dental papillae pre- and post-treatment were also
similar. But after treatment the heights of the inter-
dental papillae in the experimental group were signif-
icantly shorter than the heights of the interdental
papillae in the control group (Mean difference: 6.1
per cent; p < 0.01). Pre- and post-treatment views of
a typical case are shown in Figure 5.
Labially placed
Before treatment the heights of the interdental papil-
lae in this group of 10 patients were significantly
shorter than the interdental papillae in the 25
patients in the control group (Mean difference: -14.6
per cent; p < 0.01). During treatment the papillae
increased in length significantly (Mean difference: 7.9
per cent; p < 0.01), but remained significantly short-
er than the post-treatment papillae in the control
group (Mean difference: -8.2 per cent; p < 0.05). Pre-
CHANGES IN INTERDENTAL PAPILLAE HEIGHTS FOLLOWING ALIGNMENT OF ANTERIOR TEETH
Australian Orthodontic Journal Volume 23 No. 1 May 2007 19
(2a)
(2b)
Figure 2. Closure of a diastema.Pretreatment (a) and post-treatment
(b) views.
(3a)
(3b)
Figure 3. Vertical discrepancy between the central and lateral incisors.
Pretreatment (a) and post-treatment (b) views.
and post-treatment views of a typical arrangement in
this group are shown in Figure 6.
Palatally placed
Before treatment the heights of the interdental papil-
lae in this group were similar to the heights of the
interdental papillae in the control subjects. The inter-
dental papillae were, however, significantly shorter
post-treatment (Mean difference: 2.0 per cent;
p < 0.05) and significantly shorter than the papillae in
the control group post-treatment (Mean difference:
-6.3 per cent; p < 0.01). A typical example is shown
in Figure 7.
Discussion
The present study confirms previous investigations
that palatal movement of labially displaced or imbric-
ated teeth and the intrusion of one tooth relative to
another tooth increases the height(s) of the inter-
dental papilla(e). It also confirms previous reports
that the height(s) of the interdental papilla(e) reduce
following labial movement of an imbricated or
palatally placed incisor. The finding that the inter-
dental papilla reduced substantially when a diastema
was closed is puzzling: it may be a normal age change
or it may have occurred because one or both central
incisors were extruded or moved labially during
closure of the diastema. Before treatment the papillae
connected to the labial frenum were of similar length
to the papillae in the control group, but after treat-
ment they were markedly shorter. At the outset the
papillae associated with labially overlapped incisors
were shorter than papillae in the control group, but
only the papillae associated with palatally overlapped
incisors were shorter after treatment.
KANDASAMY ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 20
(4a)
(4b)
Figure 4. Imbricated tooth, tooth 21 overlapped labially by tooth 11.
Pretreatment (a) and post-treatment (b) views.
(5a)
(5b)
Figure 5. Imbricated tooth, tooth 21 overlapped palatally by tooth 22.
Pretreatment (a) and post treatment (b) views.
In a study such as this there are some limitations that
should be considered. We used intra-oral photo-
graphs to measure the lengths of structures that were
not always viewed directly, the depth of the gingival
crevice was not probed and standardised periapical
radiographs were not available. Had the latter been
available we could have measured the distance
between the cemento-enamel junction and the gingi-
val margin and obtained information on the height of
the interproximal bone. A further limitation in our
study is that it only covers 18 months (the period
covered by treatment) and, as a result, the changes we
observed may not be maintained in a longer study.
Furthermore, gingival attachments change over time
and during adolescence marked changes can occur in
some individuals. Age changes in the interdental
papillae could have been masked or enhanced by the
type of tooth movement, particularly if the teeth on
either side of an interdental papilla were intruded or
extruded. This is a potential confounding variable
that was not assessed. It was mainly because of these
limitations that we used proportional changes.
Although our control group was made up of patients
that did not require alignment of the anterior teeth
some unintentional tooth movement may have
occurred. The possibility of this happening and pos-
sibility of confounding changes in the control group
also must be acknowledged.
The pretreatment heights of interdental papillae were
significantly shorter in groups with a vertical discrep-
ancy, labially overlapped and labially placed incisors.
The heights of the interdental papillae increased sig-
nificantly when a vertical discrepancy was corrected.
CHANGES IN INTERDENTAL PAPILLAE HEIGHTS FOLLOWING ALIGNMENT OF ANTERIOR TEETH
Australian Orthodontic Journal Volume 23 No. 1 May 2007 21
(6a)
(6b)
Figure 6. Labially placed tooth, tooth 12 is labially placed. Pretreatment (a)
and post-treatment (b) views.
(7a)
(7b)
Figure 7. Palatally placed tooth, tooth 22 is palatally placed. Pretreatment
(a) and post treatment (b) views.
During leveling one tooth may have been intruded
and the adjacent tooth extruded. This is a potential
confounding variable that was not assessed in this
study. Following extrusion the height of the alveolar
bone usually increases and there is a proportional
increase in the attachment of the supra-alveolar
connective tissues.
15
Whether the papilla between
overlapped teeth increased or reduced in height
during treatment was determined by the direction of
tooth movement: a papilla shortened if the over-
lapped tooth was moved labially, and increased
in height if the overlapped tooth was moved palat-
ally. Similar findings occurred when labially or
palatally placed teeth that were not overlapped were
repositioned.
Labial movement of palatally placed or imbricated
teeth may result in a number of unfavourable bone
and soft tissue changes considered to predispose gin-
gival recession following orthodontic treatment, such
as a reduced height and thickness of the free gingivae
and an increased clinical crown.
10,16
Gingival reces-
sion associated with labial tooth movement correlates
with our findings of interdental recession. In com-
parison with marginal gingival recession, interdental
recession can result in the characteristic open gingival
space or dark triangle, particularly between incisors.
Gingival recession is likely to be precipitated, firstly,
by inflammation induced by bacterial plaque and,
secondly, by trauma from tooth brushing.
9,16
Therefore, patients undergoing labial movement of
palatally placed teeth should be warned of the likeli-
hood of dark triangles and should use effective and
non-traumatic plaque control measures.
14,17
Palatal tooth movement, on the other hand, results
in an increased labio-palatal thickness of the tissue at
the labial aspect of the tooth. This often results in a
reduced clinical crown and coronal migration of the
soft tissue margin, which may require periodontal
treatment.
Open gingival embrasures frequently follow align-
ment of crowded maxillary incisors and, as we have
shown, closure of a diastema.
1
These findings disagree
with Kurth et al.
15
who could not demonstrate any
post-treatment difference in the form of the embra-
sures in patients with rotated or overlapped maxillary
central incisors before treatment. It has been reported
that following orthodontic treatment open gingival
embrasures are more likely to be found in patients
over 20 years of age than in younger patients.
7,8
In
the present study the patients were between 13 and
16 years of age so it would be reasonable to expect
greater changes in an older group of patients.
Periodontal assessment and warning of the likelihood
of dark triangles is a sensible precaution for patients
who present with diastemata, palatally overlapped and
palatally placed incisors in the permanent dentition.
Adult patients appear to be particularly prone to
develop dark triangles, but other factors such as the
form of the crowns, the position of the contact area and
the height of the interproximal bone may also influ-
ence the position of the interdental papilla.
7,8,12,13,18
It may be possible to minimise complications by
adopting procedures to locate the contact point
further apically, place bonded restorations inter-
proximally and/or by augmenting the gingival
tissues.
12,13
In the developing dentition, treatment strategies
should be aimed at establishing favourable contact
point relationships. Strategies such as early extraction
of deciduous canines, reducing the interproximal sur-
faces of deciduous teeth, and/or arch expansion may
allow early alignment of the permanent incisors and
prevent unfavourable contact point relationships
from developing later in life.
19
If teeth are moved
beyond the biological limits of the alveolar bone it
may be advantageous to allow the interdental papillae
to reach their adult sizes before undertaking ortho-
dontic tooth movement likely to reduce the heights of
the interdental papillae.
Conclusions
The results of this study indicate that the interdental
papillae between the anterior teeth may lengthen
following palatal movement of labially displaced or
imbricated teeth and the intrusion of one tooth rela-
tive to another. In these cases dark triangles are less
likely to develop. On the other hand, the heights of
the interdental papillae are likely to reduce following
labial movement of imbricated or palatally placed
incisors and closure of a diastema and, as a result,
dark triangles may develop. Clinicians should be alert
to the possibility of dark triangles developing in the
latter group, particularly in older patients.
Acknowledgments
This research was supported by The University of
Western Australia Orthodontic Research Fund.
KANDASAMY ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 22
CHANGES IN INTERDENTAL PAPILLAE HEIGHTS FOLLOWING ALIGNMENT OF ANTERIOR TEETH
Australian Orthodontic Journal Volume 23 No. 1 May 2007 23
Corresponding author
Associate Professor Mithran Goonewardene
Program Director, Orthodontics
Dental School
The University of Western Australia
17 Monash Avenue
Nedlands WA 6009
Australia
Tel: (+61 8) 9346 7470
Fax: (+61 8) 9346 7666
Email: mithran.goonewardene@uwa.edu.au
References
1. Burke S, Burch JG, Tetz JA. Incidence and size of pretreat-
ment overlap and posttreatment gingival embrasure space
between maxillary central incisors. Am J Orthod Dentofacial
Orthop 1994;105:50611.
2. Atherton JD. The gingival response to orthodontic tooth
movement. Am J Orthod 1970;58:17986.
3. Atherton JD, Kerr NW. Effect of orthodontic tooth move-
ment upon the gingivae. An investigation. Brit Dent J 1968;
124:55560.
4. Diedrich PR. Orthodontic procedures improving perio-
dontal prognosis. Dent Clin North Am 1996;40:87587.
5. Waerhaug J. Eruption of teeth into crowded position, loss of
attachment, and downgrowth of subgingival plaque. Am J
Orthod 1980;78:4539.
6. El-Mangoury NH, Gaafar SM, Mostafa YA. Mandibular
anterior crowding and periodontal disease. Angle Orthod
1987;57:338.
7. Ainamo J, Paloheimo L, Norblad A, Murtomaa H. Gingival
recession in school children at 7, 12 and 17 years of age in
Espoo, Finland. Community Dent Oral Epidemiol 1986;14:
2836.
8. Ko-Kimura N, Kimura-Hayashi M, Yamaguchi M, Ikeda T,
Meguro D, Kanekawa M, Kasai K. Some factors associated
with open gingival embrasures following orthodontic treat-
ment. Aust Orthod J 2003;19:1924.
9. Ikeda T, Yamaguchi M, Meguro D, Kasai K. Prediction and
causes of open gingival embrasure spaces between the
mandibular central incisors following orthodontic treat-
ment. Aust Orthod J 2004;20:8792.
10. Wennstrom JL. Mucogingival considerations in orthodontic
treatment. Semin Orthod 1996;2:4654.
11. Andlin-Sobocki A, Bodin L. Dimensional alterations of the
gingiva related to changes of facial/lingual tooth position in
permanent anterior teeth of children. A 2-year longitudinal
study. J Clin Periodontol 1993;20:21924.
12. Zachrisson BU. Orthodontics and Periodontics. In: Lindhe
J, Karring T, Lang NP, editors. Clinical Periodontology and
Implant Dentistry. Copenhagen: Munksgaard, 1998:
74193.
13. Zachrisson BU. Interdental papilla reconstruction in adult
orthodontics. World J Orthod 2004;5:6773.
14. Wennstrom JL. The significance of the width and thickness
of the gingiva in orthodontic treatment. Dtsche Zahnarztl Z
1990;45:13641.
15. Maynard JG, Ochsenbein C. Mucogingival problems, preva-
lence and therapy in children. J Periodontol 1975;46:
54352.
16. Ericsson I, Lindhe J. Recession in sites with inadequate
width of the keratinized gingiva: an experimental study in
the dog. J Clin Periodontol 1984;11:95103.
17. Kurth JR, Kokich VG. Open gingival embrasures after
orthodontic treatment in adults: prevalence and etiology.
Am J Orthod Dentofacial Orthop 2001;120:11623.
18. Lindhe J. Textbook of Clinical Periodontology. 2nd ed.
Copenhagen: Munksgaard, 1997.
19. Rosa M, Cozzani M, Cozzani G. Sequential slicing of lower
deciduous teeth to resolve incisor crowding. J Clin Orthod
1994;28,5969.
Introduction
Two of the main objectives of orthodontic treatment
are the correction of irregularity and malocclusion of
the teeth. Following treatment, some conditions such
as imbricated, rotated, spaced and flared teeth show a
strong tendency to return to the original condition
following removal of the appliances. This process is
termed relapse or physiological recovery.
1
Preventing
relapse can be a long-term and difficult process
because many orthodontic results are potentially
unstable.
25
While the profession may acknowledge
that some relapse is inevitable, patients are under-
standably disappointed if some of the original condi-
tion returns after treatment.
2
The desire to retain the
results of treatment has lead to the development of
long-term or so-called permanent retainers, and pro-
cedures that appear to reduce the tendency of some
conditions to relapse.
67
Fixed retainers are preferable
to removable retainers because patients compliance
with wearing removable retainers is usually unreliable.
8
Long-term retention is more commonly employed in
the anterior region, and it is usually achieved by
bonding a fine wire to the lingual/palatal surfaces of
the anterior teeth. Bonded lingual or palatal retainers
were promoted as invisible retainers in the late
1970s.
9
They have steadily gained in popularity
because they are effective at preventing relapse of the
anterior teeth and patient involvement is minimal.
10
Because of the convenience of this form of retention,
they are preferred by many patients and parents.
However, there is little information on how reliable
these retainers are and how effective they are at pre-
venting relapse.
11
The aims of this retrospective study
were to investigate the reliability of fixed lingual
retainers made from looped round wires, and the
factors that may have contributed to their failure.
Australian Orthodontic Journal Volume 23 No. 1 May 2007 24
The reliability of bonded lingual retainers
Robert Cerny
Specialist practice, Newcastle, New South Wales, Australia
Background: Bonded lingual retainers have become increasingly popular, but there is little information on their long-term
reliability.
Objectives: The aims of this retrospective study were to investigate the reliability of bonded upper and lower lingual retainers
and the factors contributing to their failure.
Methods: The study group were 149 patients who returned between 2002 and 2005 with failed upper and/or lower fixed
lingual retainers. Approximately 230 patients were debonded each year and approximately 1150 patients were covered
annually by a 5-year guarantee of replacement or repair of failed retainers. The retainers were made from 0.018 inch round
stainless steel heat-treated orthodontic wire. The upper retainers had loops opposite the embrasures and the lower retainers had
loops between the lateral incisors and canines. The following details were recorded: teeth involved, patient gender, the likely
cause of any damage and the time taken for each repair.
Results: Between 35 and 40 patients required repair/replacement of their retainers each year. Multiple bond failures occurred
in approximately 9 per cent of these patients. Male patients had twice the fracture rate of female patients. Extra-oral trauma
was the most frequent cause of failure followed by intra-oral trauma, operator error and wire fracture. The central incisors in
both arches were the most frequent sites of failure. Single tooth repairs required approximately 12 minutes of the orthodontists
chair-side time.
Conclusions: Bonded lingual retainers are a reliable form of retention after orthodontic treatment.
(Aust Orthod J 2007; 23: 2429)
Received for publication: January 2006
Accepted: January 2007
Materials and methods
The subjects were 149 patients who returned with
failed upper and/or lower fixed retainers over a four
year period between 1 January 2002 and 31 December
2005. Of the 149 patients who returned for repairs
and/or replacement of a retainer(s), 76 were male
patients and 73 were female patients.
All patients were treated and reviewed by the same
orthodontist working in the same specialist practice.
At the conclusion of their active treatment with fixed
appliances, all patients were fitted with fixed looped
wire retainers bonded to the lingual surfaces of the
upper and lower anterior teeth. Actual figures for the
number of patients debonded were not available and
have been conservatively estimated from the approx-
imate number of patients debonded each working
week. This estimate was based on the orthodontist
working 46 weeks each year and debonding five
patients, that is, 10 dental arches each week. The
annual number of patients debonded was approx-
imately 230. Since 1990 each patient has been given
a written guarantee by the orthodontist that he would
undertake replacement or repair without cost to the
patient if a retainer was dislodged or fractured within
five years of the initial fitting of the retainers. Patients
also agreed to wear a mouthguard during contact
sports, not to use their teeth recklessly or inappro-
priately and to attend all orthodontic and dental
appointments. In each year of the study 1150 patients
were covered for repairs. Approximately twice as
many female to male patients were treated in this
practice. During the study no patient or parent
requested the removal of a fixed retainer.
The designs of the retainers used in this study are
shown in Figure 1. All retainers were made from
0.018 inch round single strand orthodontic wire
(Regular Plus, AJ Wilcock, Whittlesea, Victoria,
Australia) and bonded to the lingual or palatal sur-
faces of the anterior teeth with composite resin. A
direct bonding technique was used in all cases. The
same bonding primer (OrthoSolo universal bonding
primer, SDS Ormco, Glendora, Calif., USA) and
composite resin (Z100, 3M ESPE St. Paul, Minn.,
USA) were used on all patients. The upper retainers
had loops opposite the embrasures to provide stress
breaking and flexibility and to allow access to the
interproximal areas for brushing, flossing and place-
ment of dental restorations. All lower retainers had
loops between the lateral incisors and canines for the
same reasons. Loops were not placed between the lower
incisors because they are uncomfortable in these sites
and make tooth cleaning difficult. Wherever possible,
the wire was covered by at least one millimetre of
composite, as recommended by Bearn et al.
12
The following data were recorded for the patients
who attended for repairs/replacement of their retain-
ers: personal details, the retainer (upper/lower)
involved, teeth involved, nature of the damage (e.g.
fractured composite, delamination, wire fracture), the
gender of the patient, the likely cause of any damage,
and the time taken for each repair.
Results
The results are given in Tables IIII. In the first
year of the study 35 patients (21 male, 14 female)
attended for repairs or replacement and 13 of these
RELIABILITY OF BONDED LINGUAL RETAINERS
Australian Orthodontic Journal Volume 23 No. 1 May 2007 25
Figure 1. Lingual retainers bonded to the anterior teeth in the upper (left) and lower (right) arches.
patients (9 males, 4 females) attended more than once
for repair/replacement of a retainer. The total number
of bonds and/or wire breakages in 2002 was 52. The
figures in the following years were remarkably similar
with small fluctuations in the number of males and
females and number of patients with multiple break-
ages (Table I). On average, seven retainers each year
had fractured wires. As twice the number of females
to males were treated each year male patients
damaged/dislodged their fixed retainers twice as often
as female patients.
Over the four year period covered by the study the
fracture/dislodgments were attributed to extra-oral
trauma (43 per cent), intra-oral trauma (26 per cent),
operator error (18 per cent) and wire fracture (13 per
cent). A blow to the face playing sport, as a result of
fighting or an accident was considered extra-oral
trauma. Intra-oral trauma was loss or failure of a
retainer during biting or using the teeth for a task
other than eating or speaking (Table II). Bond failure
at the composite enamel interface was considered to
be due to contamination during bonding and has
been called operator error (Figure 2).
The most common sites of fracture were the lower
central incisors (29 per cent), upper central incisors
(26 per cent) and upper lateral incisors (21 per cent)
(Table III). Repairs to upper retainers were twice as
common as repairs to lower retainers. The average
clinical time taken to repair a single unit bond failure
was 12 minutes.
The retainers were effective at maintaining anterior
alignment providing they remained attached. When
breakages occurred, it was not uncommon to see dis-
placement of the tooth detached from the retainer
within a few days. Patients without exception
remarked that their retainers were comfortable with-
in one to two weeks of placement, and were rarely
CERNY
Australian Orthodontic Journal Volume 23 No. 1 May 2007 26
Table I. The number of patients experiencing breakages.
Year 2002 2003 2004 2005 Mean
Number Per cent Number Per cent Number Per cent Number Per cent Number Per cent
35 3.00 38 3.00 36 3.10 40 3.50 37 3.20
Repairs Male 21 1.80 16 1.40 17 1.47 22 1.90 19 1.60
Female 14 1.20 22 1.60 19 1.65 18 1.80 18 1.60
Total number of
unit bond and
wire breakages 52 0.38 50 0.36 56 0.40 53 0.38 53 0.38
Number of patients
with multiple bond
breakages 13 1.10 10 0.87 14 1.20 10 0.87 12 1.00
Multiple Male 9 0.78 3 0.26 6 0.50 4 0.35 6 0.50
repairs Female 4 0.35 7 0.00 8 0.70 6 0.52 6 0.50
Note. In each year 1150 patients were covered by the 5-year guarantee
Figure 2. Failure due to fracture at the enamel composite interface.
RELIABILITY OF BONDED LINGUAL RETAINERS
Australian Orthodontic Journal Volume 23 No. 1 May 2007 27
difficult to clean. Over the period covered by this
study there were no cases of caries or periodontal dis-
ease due to the presence of the retainers. In some
patients, there was a noticeable increase in supra-
gingival calculus around lower retainers.
Discussion
In this study, the reliability of fixed lingual retainers
made from looped round wires and the factors that
contributed to their failure were investigated. Out of
an annual total of approximately 1150 patients with
2300 upper and lower retainers covered by a guar-
antee, approximately 40 patients returned annually
for repairs or replacements to one or both retainers.
Of these patients 9 per cent returned for repairs on
more than one occasion each year. As twice the num-
ber of female patients to male patients were treated
male patients had twice the fracture rate of the female
patients. Extra-oral trauma was the most common
reason for failure, and failures most frequently
occurred at the central incisor regions in both dental
arches.
The number of patients who required repairs was
static each year and kept pace with the running sum
of retainers in place and under guarantee. In each year
of the study less than 4 per cent of the 1150 patients
covered by the guarantee returned for repair or
replacement of a retainer(s). This group of patients
had a combined total of 13800 unit bonds (1150
patients x 2 fixed retainers each x 6 unit bonds per
retainer) in place. The number of unit bonds that
needed to be repaired each year over the first 5 years
after their placement was 0.43 per cent of all unit
bonds involved.
This finding compares well with other dental treat-
ments involving restorative materials and appliances.
Hickel and Manhart
13
found dental restorations in
posterior teeth had an annual failure rate of up to 7
per cent for amalgams, 9 per cent for direct compos-
ites, 11.8 per cent for composite inlays and 5.9 per
Table II. The causes of failure and/or breakage.
Cause of fracture(s) 2002 2003 2004 2005 Mean
Number Per cent Number Per cent Number Per cent Number Per cent Number Per cent
a. Trauma extra-oral 33 63 20 40 14 25 23 43 23 43
b. Trauma intra-oral 9 17 18 37 18 32 11 20 14 26
c. Operator fitting 9 18 8 16 11 20 9 18 9 18
d. Wire fracture 1 2 4 7 13 23 10 20 7 13
Totals 52 100 50 100 56 100 53 100 53 100
Table III. The sites of failure and/or fracture.
2002 2003 2004 2005 Mean
Number Per cent Number Per cent Number Per cent Number Per cent Number Per cent
Maxillary anterior
teeth 1 7 13 18 36 13 23 12 23 14 26
2 15 28 9 18 15 26 8 14 11 21
3 6 12 7 14 10 18 6 12 8 14
Mandibular
anterior teeth 1 18 35 10 20 13 23 21 39 15 29
2 2 4 2 4 1 2 4 8 2 4
3 4 8 4 8 4 7 2 4 3 6
Note. In each year 1150 patients were covered by the 5-year guarantee
CERNY
Australian Orthodontic Journal Volume 23 No. 1 May 2007 28
cent for cast gold inlays and onlays. A 1990 study of
survival rates of implants by Adell et al. reported a
failure rate of approximately 5.5 per cent over 5 years
and 10.2 per cent over 10 years.
14
Bonded brackets
had a failure rate of around 5 per cent per annum
between 1986 and 2002.
15
The 0.018 inch round stainless steel Regular Plus
wire used in the retainers was adapted to the anterior
teeth and interproximal loops were used in the upper
arch in between the lower lateral incisors and canines.
Of the approximately 460 retainers placed each year
the wire frames in seven retainers fractured giving an
annual wire fracture rate of less than 2 per cent. Dahl
and Zachrisson who used five-strand 0.0215 inch
Twistiflex wire reported an annual failure rate of 1.1
per cent in their study of 2.5 years.
16
Rogers and
Andrews, who used round 0.025 inch stainless steel
wire bonded to the lower canines only, had an annu-
al bond fracture rate of 0.014 per cent per annum
over three years.
17
As more than 30 per cent of
the wire fractures and/or bond failures occurred in
the lower incisor region in the present study, the
reliability of the lower retainers would have been
improved markedly if the lower incisors had not been
bonded. However, if these teeth are not bonded any
relapse is visible and distressing to the patient. Rose et
al. who used polyethylene ribbon-reinforced resin
composite fixed retainers had a failure rate of 50 per
cent over 24 months.
18
The 3MZ100 Universal Composite paste was chosen
because it is claimed to have favourable strength, attri-
tion resistance, durable smoothness, ease of handling
and universal colour matching.
19
Wherever possible,
the wire was covered by at least one millimetre of
composite for optimum strength and patient comfort
as recommended by Bearn et al.
12
In the present study,
the fracture rate of this material was 0.26 per cent per
annum. The composite and bonding agent combine to
produce a fracture rate of 46 per annum from 13800
unit bonds which is 0.33 per cent per annum over the
first five years of fitting the fixed lingual retainers.
The fixed lingual retainers in the present study
were effective at maintaining the alignment of the
teeth they were attached to. When a wire fractured or a
bond failed the patients usually became aware of this
by movement of the teeth involved. Repairs of
fractures were generally straight-forward and
required, on average, 12 minutes per tooth bonded.
This amounted to 15 minutes each week of the
orthodontists clinical time.
Conclusions
1. Bonded lingual retainers are a reliable form of
retention after orthodontic treatment.
2. Male patients were more likely to have breakages
than female patients.
3. Measures to protect the teeth from trauma, both
extra-oral and intra-oral, may prevent some retainers
from becoming dislodged or fractured.
4. Fewer breakages may be experienced if the incisors
are not bonded, but it is not always possible to omit
the incisors from the retainer.
5. Repairs to fractured retainers required approxi-
mately 15 minutes of chairside time per week.
Corresponding author
Dr Robert Cerny
1st Floor
139 Scott Street
Newcastle NSW 2300
Australia
Tel: (+61 2) 4929 5885
Fax: (+61 2) 4926 4221
Email: rcerny@bigpond.net.au
References
1. Horowitz SL, Hixon EH. Physiologic recovery following
orthodontic treatment. Am J Orthod 1969;55:14.
2. Graber TM. Orthodontics Principles and practice. 3rd
edn. Philadelphia: Saunders, 1972:597608.
3. Angle EH. Treatment of Malocclusion of the teeth. Angles
system. 7th edn. Philadelphia: White, 1907:263304.
4. Little RM. Stability and relapse of mandibular anterior
alignment. University of Washington studies. Semin Orthod
1999;5:191204.
5. Sheridan JJ. The readers corner. J Clin Orthod 2001;35:
315.
6. Boese LR. Fiberotomy and reproximation without lower
retention, nine years in retrospect: Part I. Angle Orthod
1980;50:8897.
7. Boese LR. Fiberotomy and reproximation without lower
retention, nine years in retrospect: Part II. Angle Orthod
1980;50:16978.
8. Wong P, Freer TJ. Patients attitudes toward compliance
with retainer wear. Aust Orthod J 2005;21:4553.
9. Zachrisson BU. Clinical experience with direct-bonded
orthodontic retainers. Am J Orthod 1977;71:4408.
10. Wong PM, Freer TJ. A comprehensive survey of retention
procedures in Australia and New Zealand. Aust Orthod J
2004;20:99106.
RELIABILITY OF BONDED LINGUAL RETAINERS
Australian Orthodontic Journal Volume 23 No. 1 May 2007 29
11. Littlewood SJ, Millett DT, Doubleday B, Bearn DR,
Worthington HV. Retention procedures for stabilising tooth
position after treatment with orthodontic braces. Cochrane
Database Syst Rev. 2004;CD002283.
12. Bearn DR, McCabe JF, Gordon PH, Aird JC. Bonded ortho-
dontic retainers: The wire-composite interface. Am J Orthod
Dentofacial Orthop 1997;111:6774.
13. Hickel R, Manhart J. Longevity of restorations in posterior
teeth and reasons for failure. J Adhesive Dent 2001;3:
4564.
14. Adell R, Eriksson B, Lekholm U, Branemark PI, Jemt T.
Long-term follow-up study of osseointegrated implants in
the treatment of totally edentulous jaws. Int J Oral
Maxillofac Implants 1990;5:34759.
15. Keim RG, Gottlieb EL, Nelson AH, Vogels DS. 2002 JCO
study of orthodontic diagnosis and treatment procedures.
Part 1: Results and trends. J Clin Orthod 2002;36:55368.
16. Dahl EH, Zachrisson BU. Long-term experience with direct-
bonded lingual retainers. J Clin Orthod 1991;25:61930.
17. Rogers MB, Andrews LJ. Dependable technique for bonding
a 3x3 retainer. Am J Orthod Dentofacial Orthop 2004;126:
2313.
18. Rose E, Frucht S, Jonas IE. Clinical comparison of a multi-
stranded wire and a direct-bonded polyethylene ribbon-rein-
forced resin composite used for lingual retention.
Quintessence Int 2002;33:57983.
19. Neme A. 7-year clinical performance of 3M Z100
restorative. Dental Advisor 2000;17:12.
Introduction
Since the introduction of cephalometric radiography
by Broadbent in 1931 the centre of sella turcica has
been used in many cephalometric analyses.
1
This
point is relatively stable because the morphology of
sella turcica does not change significantly after 12
years of age.
2
On lateral radiographs the sella turcica
or pituitary fossa is the radiodense saddle-shaped
outline of the fossa extending between the anterior
and posterior clinoid processes. A sella turcica bridge
is the bony union that occasionally occurs between
the processes. In healthy individuals the surface area
of the sella turcica varies from 18 mm
2
to 115 mm
2
in females and from 22 mm
2
to 122 mm
2
in males.
3
The shape of sella turcica is usually oval, but round
and flat types can also occur.
4
Orthodontists should be familiar with variations in
the anatomical structures found on cephalometric
films so as to exclude any pathological changes.
The pituitary gland occupies the sella turcica and it is
considered to be a site for brain tumours.
57
Two
cases with Riegers syndrome were reported by
Koshino et al.,
8
the sellas in both cases were charac-
terised by prominent posterior clinoid processes:
the so-called J-shaped sella turcica.
9
Sellas of
unusual size, shape and/or with a poorly defined
outline may indicate pituitary problems and may
be associated with some types of craniofacial mal-
formation.
7,10
The prevalence of sella bridges determined by direct
inspection ranges from 1.54 per cent to 6 per
cent
11,12
and from 3.85 per cent to 18.6 per cent
when radiographs are used.
1315
The difference has
been attributed to superimposition of overlapping
clinoid processes. Sella bridges have been classified
radiographically into two types: Type A is a ribbon-
like extension linking the anterior and posterior
clinoid processes, and Type B is the bony extension(s)
Australian Orthodontic Journal Volume 23 No. 1 May 2007 30
Sella turcica bridges in orthodontic and
orthognathic surgery patients. A retrospective
cephalometric study
Hussam M. Abdel-Kader
Orthodontic Department, Faculty of Dental Medicine, Al-Azhar University, Cairo, Egypt
Objective: To investigate the prevalence of sella turcica bridges in patients accepted for conventional orthodontic treatment and
orthognathic surgery.
Methods: The pretreatment lateral cephalograms of 635 subjects scheduled for orthodontic treatment and 113 subjects
scheduled for orthognathic surgery were used. The number of subjects with complete sella bridges and the type of discrepancy
(Angle Class I, II, or III malocclusions, skeletal Class 2, 3 or bimaxillary protrusion) were recorded.
Results: Sella turcica bridges were found in 3.74 per cent of the total sample of 748 subjects. In the orthodontic group 3.21,
2.97 and 7.14 per cent of subjects in the Class I, II and III subgroups respectively had sella bridges. In the orthognathic
surgery group 2.86 and 10.71 per cent of the subjects in the Skeletal 2 and 3 subgroups respectively had sella bridges.
No subjects in the bimaxillary subgroup had sella bridges. In the orthodontic group 2.20 per cent of the female subjects and
1.10 per cent of the male subjects had sella bridges, while in the orthognathic surgery group 1.77 of the females and 4.42
per cent of the males had sella bridges.
Conclusions: Higher percentages of sella turcica bridges were found in subjects with Angle Class III and skeletal 3
discrepancies compared with subjects with Angle Class I, II, skeletal 2 or bimaxillary protrusion discrepancies.
(Aust Orthod J 2007; 23: 3035)
Received for publication: June 2006
Accepted: January 2007
SELLA TURCICA BRIDGES IN ORTHODONTIC AND ORTHOGNATHIC SURGERY PATIENTS
Australian Orthodontic Journal Volume 23 No. 1 May 2007 31
of the anterior and/or the posterior clinoid processes
bridging the pituitary fossa.
14
Higher prevalences of
sella bridges have been reported in patients with
severe craniofacial deformities and with increased
mandibular and maxillary overjets.
14
The prevalence of sella bridges in orthodontic
patients has been reported to be approximately half
that in orthognathic surgery patients.
15
The present study investigates the prevalence of sella
turcica bridges in subjects accepted for orthodontic
treatment and orthognathic surgery. The underlying
assumptions are that the former had malocclusions
that could be treated with conventional orthodontic
treatment, that the latter had severe skeletal mal-
occlusions necessitating orthognathic surgery, and
that the initial treatment recommendations were not
changed.
Materials and methods
The pretreatment lateral cephalograms of 748
patients entitled to receive orthognathic and/or
orthodontic treatment in the Orthodontic Clinic, Al-
Fanateer Hospital, Kingdom of Saudi Arabia between
2000 and 2004 were used. All patients were of Saudi
nationality with no history of systemic diseases, with
no craniofacial deformities such as cleft lip and
palate, or receiving long-term medical treatment. The
lateral cephalograms were taken by the same X-ray
technician and machine and processed in an auto-
matic developer using a standardised method. Only
good quality cephalograms with clear outlines of sella
turcica were selected. The cephalograms were
examined by the author in a darkroom, using an
X-ray viewer and magnifying lens, and the number of
cephalograms with complete sella turcica bridges
recorded.
Of the 748 pretreatment lateral cephalograms that
met the criteria, 635 were of patients scheduled for
orthodontic treatment of Angles Class I, II or III
dental malocclusions (Orthodontic group). There
were 445 females and 190 males in this group and
they were between 14 and 17 years of age. The
remainder comprised an older group of 113 patients
(42 females, 71 males) between 18 and 24 years
of age with severe maxillomandibular skeletal discrep-
ancies recommended for orthognathic surgery
(Orthognathic group). The latter malocclusions were
classified into skeletal Class 2, skeletal Class 3 and
skeletal bimaxillary protrusion.
Results
Details of the subjects are given in Table I. In the
orthodontic group, 405 subjects had Class I mal-
occlusions, 202 subjects had Class II malocclusions
and 28 subjects had Class III malocclusions. In the
orthognathic group, 35 subjects had skeletal Class
2 discrepancies, 56 subjects had skeletal Class 3 dis-
crepancies and 22 had skeletal bimaxillary protrusion.
Examples of the different types of sella turcica and
sella turcica bridges are shown in Figures 1 and 2. An
example of extreme variation in sella bridging and
sella turcica outline is shown in Figure 3. This 17
year-old male subject had an Angles Class II dental
malocclusion.
Sella bridges were found in 21 subjects in the ortho-
dontic group and in 7 subjects in the orthognathic
group (Table II). In the orthodontic group 14 female
subjects (2.20 per cent) and seven male subjects (1.10
per cent) had complete sella bridges. In the orthog-
nathic group two female subjects (1.77 per cent) and
five male subjects (4.42 per cent) had sella bridges.
Higher percentages of sella bridges were found in
the Angles Class III and skeletal Class 3 subgroups
than in the other malocclusion subgroups. No sella
bridges were found in the 22 subjects with skeletal
bimaxillary protrusion.
Discussion
The present study was designed to compare the num-
ber of complete sella turcica bridges in subjects sched-
uled for orthodontic treatment with the number of
complete sella bridges in subjects scheduled for
orthognathic surgery. Subjects in the orthodontic
group had Angle Class I, II and III malocclusions that
could be treated with conventional orthodontic
appliances while subjects in the orthognathic group
Table I. Number of subjects in the malocclusion subgroups.
Orthodontic group Orthognathic group
Class Class Class Class Class Bi-
I II III 2 3 maxillary
protrusion
Females 293 139 13 12 17 13
Males 112 63 15 23 39 9
Total 405 202 28 35 56 22
ABDEL- KADER
Australian Orthodontic Journal Volume 23 No. 1 May 2007 32
(a)
(b)
(d)
(e)
(c) (f )
Figure 1. Six examples of normal sella outlines found in the subjects.
had severe skeletal 2, 3 and bimaxillary malocclusions
requiring surgical correction. All subjects were in
good general health at the time of examination, had
no craniofacial malformations or previous systemic
illnesses. Previous studies have reported an increased
prevalence of sella bridges in subjects with severe
craniofacial disorders.
14,15
The subjects in both
groups fell within the range (14 to 24 years of age)
when the outline of sella turcica is considered to be
relatively stable.
2
The finding of 3.31 per cent sella bridging in the
orthodontic group is less than the 7.3 per cent
reported by Jones et al. in their orthodontic treatment
group.
15
We recorded the type of malocclusion and
found that a higher prevalence (7.14 per cent) of sella
bridges in the 28 Class III subjects than in the 607
Class I and II subjects. Jones et al. did not mention
malocclusions of their patients. The prevalence of
sella bridges in the orthognathic surgery group in the
present study (6.19 per cent) was also much less than
the 16.7 per cent reported by Jones and coworkers.
15
Some of this disagreement may be due to the com-
position of the samples: Jones et al. used patients
treated at a university clinic in Scotland while the
subjects in the present study were Saudi nationals.
The type of malocclusion appears to play an
important part in the prevalence of sella bridges. In
agreement with Becktor et al.
14
we found higher per-
centages of sella bridges in the Angle Class III and
skeletal Class 3 subgroups. The finding of sella
bridging in 9.52 per cent of the subjects in these sub-
groups is slightly less than the approximately 12 per
cent reported by Becktor et al. in their group with
mandibular overjet.
14
In a total sample of 177
orthognathic surgery patients Becktor et al found 21
subjects with Types A and B sella bridges. Smaller
SELLA TURCICA BRIDGES IN ORTHODONTIC AND ORTHOGNATHIC SURGERY PATIENTS
Australian Orthodontic Journal Volume 23 No. 1 May 2007 33
(a)
(b)
Figure 2. Four examples of sella bridges.
(c)
(d)
percentages of subjects with sella bridges were found
in the Angles Class I and II subgroups in the ortho-
subgroups in the orthognathic group.
The higher prevalence of sella bridging in radio-
graphic studies has been attributed to super-
processes. Autopsy studies have reported lower rates
of sella bridging (between 1.75 and 6 per cent) com-
pared with the higher rates found in radiographic
studies.
11,12
Although the differences have been
attributed to superimposition of the clinoid processes
other factors such as the composition of the samples
may account for some of the differences.
Conclusions
The pretreatment lateral cephalograms of 635 sub-
jects scheduled for orthodontic treatment and 113
subjects scheduled for orthognathic surgery were
examined for complete sella turcica bridges. The
types of dental/skeletal discrepancy in both groups
were recorded.
Higher percentages of sella turcica bridges were found
in the orthodontic subjects with Angle Class III mal-
occlusion compared with the subjects with Angle
Class I and II malocclusions, and in the orthog-
nathic surgery subjects with skeletal 3 discrepancy
compared with the subjects with skeletal 2 and
bimaxillary protrusion discrepancies.
Corresponding author
Prof. Hussam M. Abdel-Kader
5 Gamat AlDowal AlArbia Street
AlMohandessen 12411
Giza, Cairo
Egypt
Tel: (+20 2) 305 0468
Email: hmkader@hotmail.com
References
1. Broadbent BH. A new X-ray technique and its application to
orthodontia. Angle Orthod 1931;1:4566.
2. Melsen B. The cranial base. Acta Odontol Scand 1974;62:
112.
3. Abdel-Kader HM. Adolescent growth assessment (AGA):
Problems and approach. AlAzhar J Dent Sc 2000;3:93100.
4. Teal JS. Radiology of the adult sella turcica. Bull Los
Angeles Neurol Soc 1977;42:11174.
5. Abdel-Kader HM. Screening of cephalometric and panoram-
ic radiographs for significant pathological findings. AlAzhar
J Dent Sc 1998;1:1239.
6. El Gammal T, Allen MB. Further consideration of sella
changes associated with increased intracranial pressure. Br J
Radiol 1972;45:5619.
7. Weisberg LA. Asymptomatic enlargement of the sella tur-
cica. Arch Neurol 1975;32:4835.
ABDEL- KADER
Australian Orthodontic Journal Volume 23 No. 1 May 2007 34
Table II. Sella turcica bridges in orthodontic and orthognathic surgery patients.
Orthodontic group Orthognathic group
(N=635) (N=113)
Class I Class II Class III Total Class 2 Class 3 Bimaxillary Total
Females 293 139 13 445 12 17 13 42
Sella bridges 9 4 1 14 0 2 0 2
Male 112 63 15 190 23 39 9 71
Sella bridges 4 2 1 7 1 4 0 5
Total 405 202 28 635 35 56 22 113
Number with sella bridges
(Per cent) 13 (3.21) 6 (2.97) 2 (7.14) 21 (4.83) 1 (2.86) 6 (10.71) 0 (0) 7 (6.19)
Figure 3. Abnormal shape, size and sella outline found in 17 year-old male
subject with an Angles Class II malocclusion.
imposition of the anterior and posterior clinoid
dontic group and in the skeletal 2 and bimaxillary
SELLA TURCICA BRIDGES IN ORTHODONTIC AND ORTHOGNATHIC SURGERY PATIENTS
Australian Orthodontic Journal Volume 23 No. 1 May 2007 35
8. Koshino T, Konno T, Ohzeki T. Bone and joint manifesta-
tions in Riegers syndrome: a report of a family. J Pediatr
Orthop 1989;9:22430.
9. Kuhlberg AJ, Norton LA. Finding pathology on cephalo-
metric radiographs. In Athanasiou AE. Orthodontic ceph-
alometry. United Kingdom: Mosby-Wolfe, 1995. 17580.
10. Kjaer I, Fischer-Hansen B. Human fetal pituitary gland in
holoprosencephaly and anencephaly. J Craniofac Genet Dev
Biol 1995;15:2229.
11. Busch W. Die Morphologie der Sella Turcica und ihre
Bezeihung zur Hypophyse. [Morphology of sella turcica and
its relation to the pituitary gland]. Virchows Arch 1951;320:
43758.
12. Bergland RM, Ray BS, Torack RM. Anatomical variations in
the pituitary gland and adjacent structures in 225 human
autopsy cases. J Neurosurg 1968;28:939.
13. Muller F. Die Bedeutung der Sellabruecke fur das Auge.
[Sella turcica bridge and its importance for the eye]. Klin
Monatsbl Augenheilked 1952;120:298302.
14. Becktor JP, Einersen S, Kjaer I. A sella turcica bridge in sub-
jects with severe craniofacial deviations. Eur J Orthod
2000;22: 6974.
15. Jones RM, Faqir A, Millett DT, Moos KF, McHugh S.
Bridging and dimensions of sella turcica in subjects treated
by surgical-orthodontic means or orthodontics only. Angle
Orthod 2005;75:7148.
Introduction
Fixed appliance therapy using the pre-adjusted ortho-
dontic bracket system requires brackets to slide in
relation to the archwire. When sliding mechanics are
used, frictional resistance occurs at the bracket-wire
interface such that some of the applied force is dissi-
pated in overcoming friction and the remainder is
transferred to the tooth and its supporting structures
to mediate movement.
13
Frictional resistance is the result of a combination of
true friction, bracket binding and archwire notching.
Bracket binding occurs as a bracket tips in relation to
the archwire such that opposing corners of the brack-
et come into contact with the wire. The amount that
a bracket can tip before binding begins to occur is
termed the critical angle and varies according to
bracket slot and archwire dimensions.
4,5
As tipping
begins to exceed the critical angle, the edges of the
slot can cause notching of the wire, which further
increases resistance to sliding.
6
Tooth movement is dependent upon not just the
force system, but also biological factors, including
cellular turnover, vascularity and bone density. This
produces cyclical waves of remodelling events rather
than linear phenomena.
7
Intra-orally, bracket binding
can be influenced by factors such as masticatory
forces which flex the wire and in turn may disrupt the
binding effect.
8
Although laboratory testing is unable
to reproduce these biological and masticatory effects,
it is considered valuable because of its more con-
trolled environment and ability to limit variables.
Australian Orthodontic Journal Volume 23 No. 1 May 2007 36
Static frictional resistances of polycrystalline
ceramic brackets with conventional slots,
glazed slots and metal slot inserts
Steven P. Jones
*
and K. Gyaami Amoah
UCL Eastman Dental Institute for Oral Health Care Sciences, London, England
*
and University of Ghana Dental School, Accra, Ghana
Aims: To compare the static frictional resistance of ceramic brackets with a conventional slot (Allure), a glazed slot (Mystique)
and a metal slot insert (Clarity).
Method: Twenty five brackets of each type, with slot size 0.022 x 0.028 inch and Roth prescription were tested by sliding
against straight lengths of 0.019 x 0.025 inch rectangular stainless steel wire. During the tests the brackets and wire were
lubricated with artificial saliva. Static frictional forces at three different simulated binding angulations (0, 5 and 10 degrees)
were measured for each type of bracket.
Results: At each of the angulations tested, the Clarity brackets produced the lowest static frictional resistance. At 0 degree
angulation (below the critical angle for binding) the Allure brackets produced the greatest friction. The difference in friction
between the Clarity and Mystique brackets was not statistically significant. As the angulations were increased to 5 degrees
the Allure brackets again produced the greatest frictional resistance, although this was not significantly higher than the Mystique
brackets. The Mystique brackets produced the greatest frictional resistance at 10 degrees, but again there was no statistical
difference from the Allure brackets.
Conclusions: A glazed slot ceramic bracket demonstrates low frictional resistance at non-binding angulations and compares
favourably with a metal slot ceramic bracket. Increasing angulations through 5 to 10 degrees of simulated binding results in
high levels of static frictional resistance such that the bracket behaves more like a conventional polycrystalline ceramic bracket.
(Aust Orthod J 2007; 23: 3640)
Received for publication: October 2006
Accepted: February 2007
Such data can suggest clinical trends, but cannot
always be considered a good predictor of clinical
efficiency.
8
Several studies have shown that because of their hard
and rough slot bases, ceramic brackets tend to pro-
duce greater frictional resistance during sliding than
conventional stainless steel brackets.
914
Attempts at
reducing the frictional resistance have resulted in the
incorporation of metal slot linings, which have been
highly successful.
1517
Other developments seeking
to maximise aesthetics, but with improved frictional
behaviour, have included polycrystalline ceramic
brackets with either a silica insert
18
or a smooth,
glazed ceramic slot base. This study compared the
static frictional resistance between a glazed slot
ceramic bracket, a metal lined ceramic bracket and a
conventional ceramic bracket.
Materials and method
Three different polycrystalline ceramic brackets were
tested:
Allure (GAC International, Bohemia, New York,
USA): a conventional polycrystalline ceramic bracket.
Mystique (GAC International, Bohemia, New York,
USA): a polycrystalline ceramic bracket with a
smooth, glazed ceramic slot base.
Clarity (3M-Unitek, Monrovia, CA, USA): a polycrys-
talline ceramic bracket with a stainless steel slot insert.
All brackets used were upper left central incisor
brackets with Roth prescription and 0.022 x 0.028
inch slots. Incisor brackets were chosen due to their
flatter profile base which facilitated mounting in the
testing jig. The brackets were from the same batch
code for each bracket type. A sample size calculation
determined that at a statistical power of 90 per cent,
and a significance level of p 0.05, 25 brackets of
each type would be required.
Straight lengths of 0.019 x 0.025 inch rectangular
stainless steel wire Nubryte Gold (GAC
International, Bohemia, New York, USA) were used.
The wires were from the same batch code to ensure
consistency of manufacture.
Saliva Orthana (Nycomed Ltd., Birmingham, UK),
an artificial saliva spray which contains pig mucin,
xylitol, and mineral salts, was used for lubrication.
The three different types of brackets were tested
against the 0.019 x 0.025 inch archwire at 0, 5 and
10 degree bracket to archwire angulations to simulate
increasing levels of bracket binding. A specially con-
structed jig was used to hold the bracket and archwire
in place, with a predetermined archwire tension of
1 kg, bracket angulations of 0, 5 or 10 degrees and a
simulated ligation force of 200 grams.
12
Full details of
the jig have been published in a previous study.
17
Each group of 25 brackets was placed in a solution of
acetone for 10 minutes for degreasing and allowed to
air dry for an equivalent length of time. The brackets
were then transferred to a container containing 5 ml
of artificial saliva and left standing for 24 hours to
permit surface adsorption. The archwire was cut to
lengths of 10 cm and cleaned with an alcohol wipe
immediately before each test. The archwire and
bracket were mounted in the jig and liberally coated
with artificial saliva immediately before testing.
A universal load testing machine (Instron, High
Wycombe, UK) was used to hold the jig in place and
produce a steady movement of the archwire through
the bracket slot. The speed of movement was set at
0.5 mm/min and the test was run over 2.5 mm. All
results were recorded on a microprocessor connected
to the Instron machine. Units of measurement from
the Instron were kN (kiloNewtons) and data were of
the order of 10
3
to 10
4
kN. For data storage in the
computer this was recorded as E03 or E04 kN and
the tabulated data are in this format.
Initial examination of the data revealed that it fol-
lowed a normal distribution, and an analysis of vari-
ance (ANOVA) was carried out to determine statisti-
cally significant differences between groups. The
static frictional resistance of the three different
brackets at 0, 5 and 10 degrees angulations were com-
pared. Where the ANOVA identified significant dif-
ferences between the three brackets, a Bonferroni post
hoc correction was used to localise the differences.
Results
Table I presents the mean static frictional resistances
of each of the three ceramic brackets under test, at 0,
5 and 10 degrees of angulation, together with the 95
per cent confidence interval (95 per cent CI) and
standard error (SE) to report the precision of the
means. Figure 1 illustrates the data graphically.
Table II presents the results of the inter-bracket
Bonferroni post hoc corrections for static friction.
This is intended to identify statistically significant
STATIC FRICTIONAL RESISTANCES OF CERAMIC BRACKETS WITH DIFFERENT SLOT LINING
Australian Orthodontic Journal Volume 23 No. 1 May 2007 37
differences in static frictional resistance between the
three different brackets by comparing them at each of
the three fixed simulated binding angulations.
Discussion
This comparative laboratory study investigated the
static frictional resistance of three different types of
ceramic brackets under increasing levels of bracket
binding. Although the findings from this laboratory
study cannot be extrapolated directly to the clinical
state because of the lack of biological resistance effects
and occlusal forces on the system, the study has stan-
dardised the majority of variables to enable the effects
of bracket design and bracket/archwire angulation to
be compared. From this, trends may be applied to the
clinical state with caution and may form the basis for
future clinical studies.
8
At 0 degree angulation the Allure bracket produced
frictional forces that were significantly higher than
the other two brackets. (Allure mean: 8.03E-04 kN;
Mystique mean: 5.45E-04 kN; Clarity mean: 5.27E-
04 kN; p < 0.001). The Clarity bracket produced the
lowest resistance to sliding. These results agree with a
number of previous studies which showed that
ceramic brackets with metal slots exhibit lower fric-
tional resistance than conventional ceramic brackets
when sliding against stainless steel wires,
6,10,14,15,19
but is in contrast with a more recent study which
found that at 0 degree angulation a conventional
ceramic bracket demonstrated lower friction than
brackets with metal inserts.
17
However, the conven-
tional ceramic bracket tested was from a different
manufacturer than the Allure bracket used in the
present study and so this may reflect differences in
surface finish.
JONES AND AMOAH
Australian Orthodontic Journal Volume 23 No. 1 May 2007 38
Table I. Static frictional resistances of the brackets.
Bracket Angle Mean (kN) 95% CI SE
Mystique 0 5.45E-04 4.73E-04 3.47E-05
6.16E-04
Mystique 5 1.91E-03 1.77E-03 1.02E-04
2.09E-03
Mystique 10 6.47E-03 5.88E-03 2.85E-04
7.05E-03
Allure 0 8.03E-04 6.85E-04 5.74E-05
9.22E-04
Allure 5 2.05E-03 1.88E-03 8.67E-05
2.23E-03
Allure 10 5.97E-03 5.11E-03 4.18E-04
6.83E-03
Clarity 0 5.27E-04 4.46E-04 3.91E-05
6.083E-04
Clarity 5 1.59E-03 1.37E-03 1.03E-04
1.79E-03
Clarity 10 5.01E-03 4.59E-03 2.03E-04
5.42E-03
Figure 1. Graph of static frictional resistance against bracket type at 0, 5
and 10 degrees bracket/archwire angulations.
Table II. Inter-bracket multiple comparisons for static friction.
Angle Bracket Bracket Mean SE p
(Degrees) (I) (J) difference
(I minus J)
(kN)
0 Allure Mystique 2.58E-04 6.34E-05 < 0.001
Clarity 2.76E-04 6.34E-05 < 0.001
0 Mystique Clarity 1.80E-05 6.34E-05 > 0.99
5 Allure Mystique 1.40E-04 1.26E-04 > 0.99
Clarity 4.60E-04 1.26E-04 0.001
5 Mystique Clarity 3.20E-04 1.26E-04 0.02
10 Allure Mystique -5.00E-04 4.45E-04 0.815
Clarity 9.60E-04 4.45E-04 0.101
10 Mystique Clarity 1.46E-03 4.45E-04 0.005
Significant values are in bold
S
t
a
t
i
c
f
r
i
c
t
i
o
n
(
E
-
0
3
k
N
)
0 degree 5 degrees 10 degrees
Bracket/archwire angulation
7
6
5
4
3
2
1
0
Clarity Mystique Allure
Although the Clarity bracket produced lower fric-
tional values than the Mystique bracket, this was not
statistically significant (p > 0.99). This contrasts with
a previous study which investigated a polycrystalline
ceramic bracket with a silica insert and found lower
friction than with a bracket with a steel slot insert.
18
The statistically significant differences between the
Allure bracket and both the Mystique and Clarity
brackets may be considered clinically significant
when translated to orthodontic forces. The differ-
ences equated to friction levels of approximately
2628 g force.
At 5 degrees angulations, the Allure bracket again
produced the highest levels of friction (Mean: 2.05E-
03 kN), followed by Mystique (Mean: 1.91E-03 kN).
The Clarity bracket produced the least friction
(Mean: 1.59E-03 kN). The differences between the
Allure and Clarity brackets and the Mystique and
Clarity brackets were statistically significant (p = 0.001;
p = 0.02). The Allure bracket produced higher fric-
tional values than the Mystique bracket, but this was
not statistically significant (p > 0.99). Previous work
has suggested that as angulation increases, the resist-
ance to sliding produced is a combination of classic
friction, binding and notching.
46,20
The results of
this study suggest that more binding and notching
may have occurred with the Allure bracket at 5
degrees. The statistically significant differences
between the Clarity brackets and both the Mystique
and Allure brackets can be considered clinically sig-
nificant, and translates to frictional differences of
approximately 32 g force and 46 g force respectively.
At 10 degrees angulations, the Mystique bracket
produced the highest friction (Mean: 6.47E-03 kN),
followed by the Allure brackets (Mean: 5.97E-03 kN)
and the Clarity bracket (Mean: 5.01E-03 kN). The
difference in friction between the Mystique and
Clarity brackets was statistically significant (p = 0.005).
The differences in friction between the Mystique and
Allure brackets, and the Allure and Clarity brackets at
10 degrees were not statistically significant (p = 0.815;
p = 0.101). The greater frictional resistance in the
Mystique bracket at 10 degrees implies that binding
and notching in the Mystique bracket was worse, and
this may reflect a smooth glazed slot base, but rough
slot ends. The difference between the Mystique
bracket and Clarity bracket may be considered highly
clinically significant, with the difference equating to
approximately 146 g force.
Conclusions
1. At 0 degree angulation there was no statistically
significant difference in static friction between the
Mystique and the Clarity brackets. The Allure
bracket produced statistically significantly higher
values for static friction than the other two brackets.
This indicates that at non-binding angulations the
glazed surface of the Mystique may be effective in
reducing the roughness which is often associated with
ceramic brackets.
2. At 5 degrees angulations the Clarity brackets pro-
duced the lowest static frictional resistance and this
was statistically significant when compared to the
other two brackets. There was no significant differ-
ence in frictional resistance between the Mystique
and Allure brackets. This suggests that once the
critical angle for binding is exceeded, when the notch-
ing and binding components of friction are brought
into play, the harder and rougher edges of the
Mystique and Allure bracket slots may have resulted
in higher frictional values.
3. At 10 degrees angulations, the Clarity brackets
once again produced the least friction. The Mystique
bracket produced the highest friction. The only
statistically significant difference in friction was
between the Mystique and Clarity brackets.
4. These findings appear to partially confirm the
manufacturers claim that the frictional resistance of
Mystique brackets is comparable to sliding on metal
surfaces, but this seems only to be true when the
bracket to archwire angulation is below the critical
angle for binding. Once this critical angle is exceeded
the Mystique bracket begins to behave more like a
conventional ceramic bracket. Hence it is recom-
mended when using the Mystique or Allure brackets
in particular, the slots are properly aligned before
commencing sliding mechanics.
Acknowledgments
The authors would like to thank Mr Graham Palmer,
Department of Biomaterials Science, UCL Eastman
Dental Institute, London for technical assistance and
Dr David Moles, Department of Biostatistics, UCL
Eastman Dental Institute, London for statistical
advice. We would also like to thank 3M-Unitek (UK)
for generously donating their brackets for testing and
Nycomed Ltd. (UK) for kindly providing the Saliva
Orthana.
STATIC FRICTIONAL RESISTANCES OF CERAMIC BRACKETS WITH DIFFERENT SLOT LINING
Australian Orthodontic Journal Volume 23 No. 1 May 2007 39
JONES AND AMOAH
Australian Orthodontic Journal Volume 23 No. 1 May 2007 40
Corresponding author
Dr S.P. Jones
Unit of Orthodontics
UCL Eastman Dental Institute for Oral Health Care
Sciences
256 Grays Inn Road
London, WC1X 8LD
United Kingdom
Tel: (+44 0) 20 7915 1068
Fax: (+44 0) 20 7915 1238
Email: s.jones@eastman.ucl.ac.uk
References
1. Drescher D, Bourauel C, Schumacher H-A. Frictional forces
between bracket and arch wire. Am J Orthod Dentofacial
Orthop 1989;96:397404.
2. Kusy RP, Whitley JQ. Friction between different wire-
bracket configurations and materials. Semin Orthod 1997;3:
16677.
3. Articolo LC, Kusy RP. Influence of angulation on the resist-
ance to sliding in fixed appliances. Am J Orthod Dentofacial
Orthop 1999;115:3951.
4. Kusy RP, Whitley JQ. Assessment of second-order clearances
between orthodontic archwires and bracket slots via the
critical angle for binding. Angle Orthod 1999;69:7180.
5. Kusy RP, Whitley JQ. Influence of archwire and bracket
dimensions on sliding mechanics: derivations and deter-
minations of the critical contact angles for binding. Eur J
Orthod 1999;21:199208.
6. Articolo LC, Kusy K, Saunders CR, Kusy RP. Influence of
ceramic and stainless steel brackets on the notching of arch-
wires during clinical treatment. Eur J Orthod 2000;22:
40925.
7. Kuhlberg AJ, Priebe D. Testing force systems and bio-
mechanics measured tooth movements from differential
moment closing loops. Angle Orthod 2003;73:27080.
8. Kula K, Phillips C, Gibilaro A, Proffit WR. Effect of ion
implantation of TMA archwires on the rate of orthodontic
sliding space closure. Am J Orthod Dentofacial Orthop
1998;114:57780.
9. Angolkar PV, Kapila S, Duncanson MG Jr, Nanda RS.
Evaluation of friction between ceramic brackets and ortho-
dontic wires of four alloys. Am J Orthod Dentofacial
Orthop 1990;98:499506.
10. Kusy RP, Whitley JQ. Coefficients of friction for arch wires
in stainless steel and polycrystalline alumina bracket slots. 1.
The dry state. Am J Orthod Dentofacial Orthop 1990;98:
30012.
11. Pratten DH, Popli K, Germane N, Gunsolley JC. Frictional
resistance of ceramic and stainless steel orthodontic brackets.
Am J Orthod Dentofacial Orthop 1990;98:398403.
12. Keith O, Jones SP, Davies EH. The influence of bracket
material, ligation force and wear on frictional resistance of
orthodontic brackets. Br J Orthod 1993;20:10915.
13. Loftus BP, rtun, J, Nicholls JI, Alonzo TA, Stoner JA.
Evaluation of friction during sliding tooth movement in
various bracket-arch wire combinations. Am J Orthod
Dentofacial Orthop 1999;116:33645.
14. Nishio C, da Motta AF, Elias CN, Mucha JN. In vitro eval-
uation of frictional forces between archwires and ceramic
brackets. Am J Orthod Dentofacial Orthop 2004;125:
5664.
15. Dickson J, Jones S. Frictional characteristics of a modified
ceramic bracket. J Clin Orthod 1996;30:51618.
16. Thorstenson GA, Kusy RP. Influence of stainless steel inserts
on the resistance to sliding of esthetic brackets with second-
order angulation in the dry and wet states. Angle Orthod
2003;73:16775.
17. Rajakulendran J, Jones S. Static frictional resistances of
polycrystalline ceramic brackets with metal slot inserts. Aust
Orthod J 2006;22:14752.
18. Cha J-Y, Kim K-S, Hwang C-J. Friction of conventional
and silica-insert ceramic brackets in various bracket-wire
combinations. Angle Orthod 2007;77:1007.
19. Ireland AJ, Sheriff M, McDonald F. Effect of bracket and
wire composition on frictional forces. Eur J Orthod 1991;
13:3228.
20. Thorstenson GA, Kusy RP. Resistance to sliding of self-lig-
ating brackets versus conventional stainless steel twin brack-
ets with second-order angulation in the dry and wet (saliva)
states. Am J Orthod Dentofacial Orthop 2001;120:36170.
Introduction
Several studies have investigated the development of
gingival recession following orthodontic tooth move-
ment.
13
Some authors claim that sagittal expansion
of the lower arch moves the lower incisors labially and
causes the labial gingival attachment to break-
down.
47
This claim is supported by the finding of
alveolar bone dehiscences following labial movement
of the mandibular incisors in animals.
810
However,
other authors have reported there was no association
between labial movement of the lower incisors and
clinical crown length, gingival recession or loss of
attachment in patients.
1113
Transverse expansion may move the teeth beyond the
limits of their bony support and result in gingival
recession. Some studies have reported gingival reces-
sion following expansion of the upper arch and high-
lighted the potential risks of bone fenestration, but
the extent to which the mucogingival tissues can
adapt to transverse expansion is uncertain.
1416
There
is little information on the mucogingival changes in
the lower arch following transverse expansion. The
aim of this study was to determine if changes in the
lower intercanine widths during orthodontic treat-
ment with fixed appliances result in gingival margin
changes around the lower canines and incisors.
Material and methods
Subjects
The subjects of this investigation were 178 Caucasian
adolescents (101 females, 77 males) selected from a
pool of 209 patients treated by two orthodontists in a
private clinic. Subjects were included if they had
either an Angle Class I or a Class II malocclusion
either with or without a transverse and/or vertical
discrepancy, were treated without extractions, had
less than 4 mm spacing or crowding, the lower
permanent incisors were fully erupted, had good perio-
Australian Orthodontic Journal Volume 23 No. 1 May 2007 41
Lower intercanine width and gingival margin
changes. A retrospective study
Luciane Closs,
*
Karine Squeff,
Dirceu Raveli
*
and Cassiano Rsing
+
Araraquara School of Dentistry, Sao Paulo State University, Araraquara,
*
Specialist practice, Porto Alegre,
and Federal University of Rio Grande
do Sul, Porto Alegre,
+
Brazil
Objective: To determine if changes in the lower intercanine widths during orthodontic treatment with fixed appliances result in
gingival margin changes around the lower canines and incisors.
Method: Pre- and post-treatment intra-oral photographs and orthodontic study models of 178 Caucasian adolescents (101
female, 77 male) were used. All subjects were treated with fixed appliances. The subjects had mean ages of 11.41 (SD:
1.83) years and 14.91 (SD: 1.78) years on their initial and final records respectively. The latter were taken 28 days or more
after the appliances had been removed. The inclusion criteria were: Angle Class I or Class II malocclusion (with or without
transverse and/or vertical discrepancies); nonextraction treatment; less than 4 mm crowding or spacing; fully erupted lower
incisors and good periodontal health. The intercanine widths and the positions of the gingival margins relative to the maximum
curvatures of the labial surfaces of the lower canines and incisors were measured with digital calipers.
Results: A significant association was found between unaltered intercanine widths and coronal migration of the gingival margins
(p = 0.045). There were no significant associations between either increased or reduced intercanine widths and changes in
the gingival margins.
Conclusions: Following orthodontic treatment coronal migration of the gingival margins around the lower incisors and canines is
more likely to be associated with an unaltered intercanine width.
(Aust Orthod J 2007; 23: 4145)
Received for publication: April 2006
Accepted: February 2007
dontal health, and the final records (study
models, intra-oral photographs) were taken 28 days
or more after removal of the appliances. Patients were
excluded if they had a pre-existing systemic con-
dition, were taking medication with associated
gingival changes, if the pre- or the post-treatment
records could not be measured. Of the original 209
subjects 31 subjects were excluded because their
photographs or models could not be measured.
The subjects had mean ages of 11.41 years (SD: 1.83
years) and 14.91 years (SD: 1.78 years) on the initial
and final records respectively. All patients were
treated with either standard edgewise or Roth pre-
scription straight-wire appliances (0.022 inch slot).
The average duration of active treatment in the lower
arch was 1.99 years (SD: 0.89 years). All patients
received oral hygiene instructions immediately fol-
lowing placement of the fixed appliances and
throughout orthodontic treatment. Periodontal
maintenance was performed according to each
patients needs.
Assessment of gingival margin position
The positions of the gingival margins relative to the
maximum curvature of the labial surfaces of the lower
canines and incisors were measured with digital
calipers (Digimatic, Mitutoyo, Japan) on the pre- and
post-treatment 3.54 inch x 5.12 inch intra-oral photo-
graphs (anterior and lateral views) and study models.
Measurements were made from the maximum curva-
ture of the labial surfaces of the lower canines and
incisors to the deepest points on the curvature of the
gingival margins of each tooth or to the cemento-
enamel junction when visible. All gingival margin
measurements were made to the nearest 0.5 mm.
Depending on the direction of change the positions
of the gingival margins of the lower canines and inci-
sors on the post-treatment photographs were classi-
fied as: unaltered, migrated coronally, migrated
apically. Gingival recession was recorded when the
cemento-enamel junction was visible either on the
models or the photographs or if a labial gingival
margin was markedly below the gingival margins of
the adjacent teeth. The data were corrected by deriv-
ing a magnification factor for each photograph from
the width of the upper right central incisor on the
photograph and the corresponding study cast.
17
To determine the errors in the method, photographs
of 20 randomly selected patients with similar mal-
occlusions were measured on two occasions. Kappa
statistics were used to evaluate the intra-examiner
agreement, and a Kappa value of 1.0 was obtained.
Intercanine width measurements
The intercanine widths on the pre- and post-
treatment study models were measured with the
digital calipers from the most cervical points in the
middle of the buccal surfaces of the lower canines.
The cemento-enamel junction was used to define the
most inferior limit of this measurement in the
subjects with gingival recession. The intercanine
widths were then classified as: unaltered, increased
intercanine width, decreased intercanine width. All
intercanine measurements were made to the nearest
0.5 mm.
Error of the method
To determine the errors in the method the gingival
margin measurements were taken on two occasions
and compared with the paired t-test.
17
There was no
statistically significant difference between the two sets
of measurements (p = 0.505). The errors in the inter-
canine width measurements were assessed with
Pearsons product-moment correlation coefficient
and the paired t-test. The difference between the
duplicate measurements of intercanine width was not
statistically significant (r = 0.983, p = 0.662). The dif-
ference in paired intercanine width measurements
never exceeded 0.3 mm.
Statistical analysis
The data were analysed with the statistical package
for social sciences (SPSS 10.0, SPSS, Inc., Chicago,
Illinois, USA). The distributions of the subjects in the
intercanine width and the gingival margin subgroups
were compared using Chi-squared tests and comple-
mented by analysis of the adjusted residual. Quartiles
were calculated for the intercanine widths and the
Kruskal-Wallis test used to evaluate the differences in
the intercanine widths (Final minus Initial) in each
gingival margin subgroup (Unaltered, Coronal
migration, Apical migration). The significance of
the results was set at the 0.05 level of confidence.
Results
The results are given in Tables I and II. The distribu-
tions of the gingival margin changes in the three
intercanine subgroups are given in Table I. Of the
CLOSS ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 42
178 subjects, the intercanine width decreased in 27
subjects, was unaltered in 33 subjects and increased in
118 subjects. The gingival margins migrated coron-
ally in 9 subjects, were unaltered in 112 subjects and
migrated apically in 57 subjects. In the later subgroup
the lower canines were involved in 90.2 per cent of
the subjects, followed by the lower central incisors
(7.3 per cent) and lateral incisors (2.5 per cent). Of
the nine subjects in the coronal migration subgroup
the intercanine width was unaltered in five subjects
(55.6 per cent) and increased in three subjects.
Chi squared analysis, complemented by analysis of
the adjusted residual, demonstrated that there was a
significant association between unaltered intercanine
widths and coronal migration of the gingival margins
(Chi-squared, p = 0.045). The other variables, increased
intercanine width and decreased intercanine width,
did not show any statistically significant associations
with changes in the gingival margins.
Table II gives the associations between the variation
in the intercanine widths (quartiles) and changes in
the gingival margins at the end of treatment.
Statistically significant differences were observed
between subjects that had clear coronal migration of
the gingival margins and subjects who developed gin-
gival recession. However, subjects with an unaltered
gingival position remained in the intermediate cate-
gory, not displaying statistically significant differences
in relation to the two other categories (Kruskal-
Wallis test, complemented by multiple comparison
test, p = 0.028).
Discussion
The aims of this study were to determine if changes
in lower intercanine widths during orthodontic treat-
ment lead to gingival margin changes around the
lower incisors and canines. While recent studies have
reported that labial movement of the lower anterior
teeth does not necessarily lead to gingival recession,
the effects of expansion or constriction of the inter-
canine widths on the gingival margins have not been
reported.
12,13,18
We found the difference in inter-
canine widths in subjects with coronal migration of
the gingival margins was 0.57 mm at the upper quar-
tile point, but in the subjects with apical migration of
the gingival margins the difference was 2.58 mm at
the upper quartile point.
There are some limitations in the study we should
consider. As untreated controls were not available for
examination the possibility that apical migration of
LOWER INTERCANINE WIDTH AND GINGIVAL MARGIN CHANGES
Australian Orthodontic Journal Volume 23 No. 1 May 2007 43
Table I. Changes in intercanine width and gingival margin location.
Lower intercanine width Gingival migration Total
Coronal Unaltered Apical
n Per cent n Per cent n Per cent N Per cent
Decreased 1 11.1 17 15.2 9 15.8 27 15.2
Unaltered 5 55.6 21 18.8 7 12.3 33 18.5
Increased 3 33.3 74 66.1 41 71.9 118 66.3
Total 9 100.0 112 100.0 57 100.0 178 100.0
2
= 9.72; p = 0.045
Analysis of adjusted residual, p < 0.05, significant association in bold
Table II. Distribution of the Final Initial differences in the intercanine
width and gingival margins.
Differences in intercanine width
(Final minus Initial)
Gingival 1st 2nd 3rd Median
migration Quartile Quartile Quartile rank*
Coronal 0.00 0.01 0.57 50.56
A
Unaltered 0.14 0.90 1.85 87.88
AB
Apical 0.21 1.04 2.58 98.82
B
*Median ranks followed by different letters in the column represent
statistically significant differences between intercanine width in relation
to gingival position (Kruskal Wallis non parametric test: p = 0.028)
the gingival margins in some subjects may be a nor-
mal age change should be borne in mind. Our study
group was relatively young so one could argue that
age-related gingival changes were unlikely to occur.
On the other hand, a longitudinal study of dental
arch widths reported that the lower intercanine
widths were stable up to 6 years of age, increased
gradually with the emergence of the permanent
incisors, decreased up to 15 years of age, and then
remained more-or-less unchanged.
19
Thus, changes
in the intercanine widths in some subjects may have
been an age change, particularly if lower arch treat-
ment was started some time after the initial records
were taken. The final records were taken at least 28
days after removal of the appliances to allow any
inflammation, due to poor plaque control, to resolve.
20
We had a larger sample than other similar studies.
17,18,21
We selected subjects independently of any require-
ment for a change in lower intercanine width. Had
we used a prospective design we would have had bet-
ter control of the variables such as oral hygiene and
avoidance of traumatic tooth brushing. Previous
studies have reported that oral hygiene may be an
important factor. For example, Allais and Melsen
attributed the favourable response of the gingival tis-
sues following controlled proclination of the lower
incisors to maintenance of good oral hygiene.
12
The
same may be true in our study group. However, a
prospective study with a similar number of subjects
would be difficult and expensive to carry out. Our
results may better reflect the effect of orthodontic
treatment on the gingival margins without the
Hawthorne effect when oral hygiene measures are
closely monitored.
In previous studies the intercanine widths were meas-
ured between the cusp tips or the widest points on the
buccal surfaces of the lower canines.
22,23
We meas-
ured from the most cervical points in the middle of
the buccal surfaces of the lower canines with the
objective of measuring changes as close as possible to
the level of the alveolar bone. We have assumed that
the gingival changes around the lower canines and
incisors were associated with changes in intercanine
widths, when changes around the incisors may be due
to proclination. In the present study gingival changes
were based on intra-oral photographs complemented
by study models. This method has been used in pre-
vious studies and it is considered to be more accurate
than measurements carried out on study casts
alone.
12,13,18,21
The developmental position of the teeth is also con-
sidered to be an important predisposing factor to
local gingival recession.
24
Long supracrestal connec-
tive tissue attachments on the buccal surfaces of teeth
in patients undergoing orthodontic expansion are
considered to be at risk of developing gingival reces-
sion over time. Such speculation is reinforced by the
high frequency of gingival recession observed on the
labial/buccal aspects of prominent teeth in individ-
uals who have not received orthodontic treatment.
25,26
Since the maximum crowding in our sample was 4
mm, severely displaced teeth were not seen.
According to Bernimoulin and Curilovie,
27
gingival
recession is always accompanied by a bone dehis-
cence. Whether an underlying bone dehiscence
develops before or parallel with gingival recession has
not been determined. There is a suspicion that an
exaggerated labial tooth position leads to a thin
cortical plate, which is more susceptible to resorp-
tion.
4,28
A bone dehiscence may be an anatomical
variation or due to expansion of teeth through the
cortical plate.
In the present study the intercanine width increased
in the majority of the subjects (66.3 per cent), was
maintained in 18.5 per cent and decreased in 15.2
per cent of the subjects. There was a high percentage
of gingival recession in the subjects with increased
intercanine widths (71.9 per cent), although this per-
centage was not statistically significant. On the other
hand, there was a significant finding in the small
group that had unaltered intercanine widths and
coronal migration of the gingival margins. One
should question the clinical significance of this result
since there were only nine subjects in the group with
coronal gingival migration.
In conclusion, despite the finding that gingival mar-
gin changes tended to occur independently of
changes in intercanine widths, the gingival margins
around the lower incisors and canines are more likely
to migrate coronally when the intercanine width is
unchanged.
Acknowledgments
We thank Dr Susana Rizzatto for her help with the
sample for this study.
CLOSS ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 44
Corresponding author
Dr Luciane Q. Closs
Rua G.Couto de Magalhes 1070 apto. 801
Porto Alegre RS CEP: 90540-130
Brazil
Tel: (+55 51) 3337 3379
Fax: (+55 51) 3342 7284
Email: lucloss@uol.com.br
References
1. Geiger AM. Mucogingival problems and the movement of
mandibular incisors: a clinical review. Am J Orthod 1980;
78:51127.
2. Wennstrm JL.The significance of the width and thickness
of the gingiva in orthodontic treatment. Dtsch Zahnarztl Z
1990;45:13641.
3. Moriarty JD. Mucogingival considerations for the ortho-
dontic patient. Curr Opin Periodontol 1996;3:97102.
4. Hollender L, Rnnerman A, Thilander B. Root resorption,
marginal bone support and clinical crown length in ortho-
dontically treated patients. Eur J Orthod 1980;2:197205.
5. Coatoam GW, Behrents RG, Bissada NF. The width of kera-
tinized gingiva during orthodontic treatment: its signifi-
cance and impact on periodontal status. J Periodontol 1981;
52:30713.
6. De Loor P, De Smit AA, Adriaens PA. Periodontal changes
induced by orthodontically changed incisor inclination. Eur
J Orthod 1995;17:434.
7. rtun J, Krogstad O. Periodontal status of mandibular
incisors following excessive proclination: a study in adults
with surgically treated mandibular prognathism. Am J
Orthod Dentofacial Orthop 1987;91:22532.
8. Steiner GG, Pearson JK, Ainamo J. Changes of the mar-
ginal periodontium as a result of labial tooth movement in
monkeys. J Periodontol 1981; 52:31420.
9. Karring T, Nyman S, Thilander B, Magnusson I. Bone
regeneration in orthodontically produced alveolar bone
dehiscences. J Periodontal Res 1982;17:30915.
10. Thilander B, Nyman, S, Karring T, Magnusson I. Bone
regeneration in alveolar bone dehiscences related to ortho-
dontic tooth movements. Eur J Orthod 1983;5:10514.
11. Busschop JL, Van Vlierberghe M, De Boever J, Dermaut L.
The width of the attached gingiva during orthodontic treat-
ment: a clinical study in human patients. Am J Orthod
1985;87:2249.
12. Allais D, Melsen B. Does labial movement of lower incisors
influence the level of the gingival margin? A case-control
study of adult orthodontic patients. Eur J Orthod 2003;25:
34352.
13. Melsen B, Allais D. Factors of importance for the develop-
ment of dehiscences during labial movement of mandibular
incisors: a retrospective study of adult orthodontic patients.
Am J Orthod Dentofacial Orthop 2005;127:55261.
14. Carmen M, Marcella P, Giuseppe C, Roberto A. Periodontal
evaluation in patients undergoing maxillary expansion. J
Craniofac Surg 2000;11:4914.
15. Bassarelli T, Dalstra M, Melsen B. Changes in clinical crown
height as a result of transverse expansion of the maxilla in
adults. Eur J Orthod 2005;27:1218.
16. Greenbaum KR, Zachrisson BU. The effect of palatal expan-
sion therapy on the periodontal supporting tissues. Am J
Orthod 1982;81:1221.
17. Djeu G, Hayes C, Zawaideh S. Correlation between
mandibular central incisor proclination and gingival reces-
sion during fixed appliance therapy. Angle Orthod 2002;72:
23845.
18. Ruf S, Hansen K, Pancherz H. Does orthodontic proclina-
tion of lower incisors in children and adolescents cause gin-
gival recession? Am J Orthod Dentofacial Orthop 1998;114:
1006.
19. Tsujino K, Machida Y. A longitudinal study of the growth
and development of the dental arch width from childhood to
adolescence in Japanese. Bull Tokyo Dent Coll 1998;39:
7589.
20. Sallum EJ, Nouer DF, Klein MI, Gonalves RB, Machion L,
Wilson Sallum A, Sallum EA. Clinical and microbiologic
changes after removal of orthodontic appliances. Am J
Orthod Dentofacial Orthop 2004;126:3636.
21. rtun J, Grobty D. Periodontal status of mandibular inci-
sors after pronounced orthodontic advancement during ado-
lescence: a follow-up evaluation. Am J Orthod Dentofacial
Orthop 2001;119:210.
22. Kahl-Nieke B, Fischbach H, Schwarze C. Treatment and
postretention changes in dental arch width dimensions a
long-term evaluation of influencing cofactors. Am J Orthod
Dentofacial Orthop 1996;109:36878.
23. Richardson ME. Late lower arch crowding: the role of the
transverse dimension. Am J Orthod Dentofacial Orthop
1995;107:6137.
24. Parfitt GJ, Mjr IA. A clinical evaluation of local gingival
recession in children. J Dent Child 1964;31:25762.
25. Gorman WJ. Prevalence and etiology of gingival recession. J
Periodontol 1967;38:31622.
26. Maynard JG, Ochsenbein C. Mucogingival problems, preva-
lence and therapy in children. J Periodontol 1975;46:
54352.
27. Bernimoulin JP, Curilovie Z. Gingival recession and tooth
mobility. J Clin Periodontol 1977;4:10714.
28. Fuhrmann R. Three-dimensional interpretation of periodon-
tal lesions and remodeling during orthodontic treatment.
Part III. J Orofac Orthop 1996;57:22437.
LOWER INTERCANINE WIDTH AND GINGIVAL MARGIN CHANGES
Australian Orthodontic Journal Volume 23 No. 1 May 2007 45
Introduction
The prevalence of white spots in patients treated with
fixed orthodontic appliances varies between 12 and
26 per cent.
13
The ability of fluoride compounds to
prevent enamel demineralisation is well known.
48
For example, Basdera et al. reported that fluoride
released from orthodontic bonding agents partially
protected the enamel surface from demineralisation.
8
Topacal C-5, a milk protein-based formulation super-
saturated with calcium and phosphate, has been
shown to remineralise enamel lesions in humans.
9
An
in vitro study also demonstrated that casein phos-
phopeptide stabilised calcium phosphate solution
(CPP-ACP) will remineralise subsurface lesions in
human enamel,
10
and incorporation of CPP-ACP in
a self-cure glassionomer cement will protect the
dentine against acid attack.
11
Since no quantitative
information has been reported on the effect of
CPP-ACP on the enamel surrounding orthodontic
brackets this study was designed to determine if
Topacal C-5 inhibits enamel demineralisation
adjacent to orthodontic brackets in vitro.
Materials and methods
Twenty four paired right and left non-carious human
premolars with no visible enamel defects were used in
this study. The teeth (N = 48) were extracted from 24
orthodontic patients living in a low fluoride area (0.4
ppm). The patients were between 10 and 14 years of
age at the time of the extractions. Any soft tissue, cal-
culus and/or bone remaining on the teeth following
extraction were removed with a dental scaler and the
teeth stored in deionised water until required.
One premolar in each pair was randomly assigned to
the control group and the contralateral premolar was
assigned to the experimental group. The buccal sur-
faces of the crowns were polished with a mixture of
non-fluoridated pumice and water and masked with
Australian Orthodontic Journal Volume 23 No. 1 May 2007 46
Effect of Topacal C-5 on enamel adjacent to
orthodontic brackets. An in vitro study
Navid Karimi Nasab, Zahra Dalili Kajan and Azadeh Balalaie
Dental School, Guilan University of Medical Sciences, Rasht, Iran
Background: Enamel demineralisation leading to white spots can occur during orthodontic treatment. Casein phosphopeptides
may reduce demineralisation during orthodontic treatment.
Aims: To determine if a casein phosphopeptide preparation, Topacal C-5 (Enamel Improving Cream, NSI Dental Pty Ltd,
Leighton, Hornsby, Australia), will inhibit demineralisation of enamel adjacent to orthodontic brackets.
Methods: Twenty-four pairs of human premolars from 24 subjects were used. One premolar in each pair was randomly
assigned to the control group and the contralateral premolar was assigned to the experimental group. A stainless steel
orthodontic bracket was bonded to the buccal surface of each tooth and a window of enamel (4 mm x 1 mm) left open to
acid attack. The teeth were cycled alternately through an artificial saliva medium (11 hours) and an acid medium (1 hour) for
31 days. Topacal C-5 was applied to the exposed enamel windows in the experimental group after immersion in the acid
medium. After 31 days the teeth were sectioned longitudinally and the depths of the enamel lesions measured by polarised
light microscopy.
Results: Significantly deeper demineralisation occurred in the control teeth not protected by Topacal C-5 and at sites close to the
brackets in both groups.
Conclusions: In this in vitro system, Topacal C-5 partially reduced the depth of enamel demineralisation compared with teeth
not covered with Topacal C-5. Topacal C-5 may reduce enamel demineralisation in patients with fixed orthodontic appliances.
(Aust Orthod J 2007; 23: 4649)
Received for publication: July 2006
Accepted: March 2007
EFFECT OF TOPACAL C- 5 ON ENAMEL ADJACENT TO ORTHODONTIC BRACKETS
Australian Orthodontic Journal Volume 23 No. 1 May 2007 47
tape. A small window was left in the tape to accom-
modate a premolar bracket with 1 mm clearance on
all sides of the base. A premolar stainless steel
bracket (3M Unitek, Monrovia, California, USA) was
bonded to the buccal surface of each tooth with a
fluoride-free composite resin (Prime-dent, Dent
World, Chicago, USA). The masking tape was
removed and any residue of the tape wiped away with
ethanol. Acid resistant nail varnish (Nivea,
Beiersdorf, Hamburg, Germany) was then painted on
the enamel surface leaving a rectangular window (4
mm x 1 mm) extending occlusally from each bracket.
The teeth in each group were immersed separately in
an artificial saliva solution for 11 hours and an acid
solution for 1 hour. Both solutions were agitated con-
stantly and maintained at room temperature. The
artificial saliva solution had a neutral pH and con-
tained 20 mmol/L KHCO
3
, 3 mmol/L KH2PO4
and 1 mmol/L CaCl
2
. After 11 hours the teeth were
removed and immersed in the acid solution for 1
hour. The acid solution contained 2.2 mmol/L Ca
2
+,
2.2 mmol/L PO
4
- and 50 mmol/L acetic acid at 4.4
pH. After each acid challenge, the surface layers in
the exposed enamel windows in both groups were
removed by brushing for 5 seconds with a soft tooth-
brush (Oral-B Laboratories, Belmont, California,
USA). Topacal C-5 was applied to the exposed
enamel in the experimental group before immersion
in the saliva solution. The teeth were immersed alter-
nately in the saliva and acid solutions for 31 days.
The solutions were changed twice a week and the pH
of each solution was monitored.
After 31 days the brackets were removed and the
teeth mounted in polyester resin. The teeth were
sectioned longitudinally through the buccal windows
with a hard tissue microtome (Figure 1). Two sections,
each approximately 0.5 mm thick, were obtained
from each specimen. The sections were thinned and
polished with increasing finer grades of aluminum
oxide powder (Buehler, Evanston, Illinois, USA).
The sections were mounted in water and photo-
graphed with a polarised light microscope (Zeiss,
Oberkochen, Germany) at 4x magnification (Figure
2). To facilitate measurement of the photographs a
straight line was drawn between the intact enamel
areas on the buccal surface of each specimen. The
depths of demineralised enamel (m) in each section
were measured at three sites: near the gingival margin
and close to the bracket, d1; in the middle of the
demineralised area, d2; and near the occlusal margin,
d3. The observer was blinded to the identity of the
sections (i.e. experimental or control). The means and
standard deviations of the depths at the three sites
(d1, d2, d3) were calculated.
The t-test for unpaired data was used to compare the
depths of the lesions in the control and the experi-
mental groups and the paired t-test was used to com-
pare the depths of the lesions at d1 and d3 in the
same specimens. Statistical significance was set at the
5 per cent level.
Results
The results are given in Table I and Figure 3.
Significantly deeper demineralisation occurred in the
Figure 1. Longitudinal section of tooth embedded in polyester. The lesion is
indicated by the arrow.
Figure 2. Enamel lesion in the control group viewed by polarised light
microscopy. A, demineralised lesion; B, residual enamel; C, amelo-dentinal
junction (4x magnification).
control teeth compared with the experimental teeth
and at sites (d1) close to the brackets in both groups.
In the experimental group the enamel was demin-
eralised to a depth of 5.17 m close to the bracket
(d1), 2.79 m in the centre of the demineralised
area (d2) and only 1.58 m at d3, where it was fur-
thest from the base of the bracket. In the experi-
mental group the difference between d1 and d3 was
statistically significant.
Deeper demineralisation occurred in all sites in the
control group compared with the experimental
group. In this group demineralisation extended 11.25
m into the enamel close to the bracket (d1), 8.37
m in the mid-zone (d2) and 6.92 m at d3.
Furthermore, deeper demineralisation occurred at d3
in the control group than at d1 in the experimental
group. In the control group the difference between d1
and d3 was also statistically significant.
Discussion
The results confirmed that regular applications of
Topacal C-5 to teeth subjected to acid attack in vitro
had less enamel demineralisation compared with
teeth not treated with Topacal C-5. The deepest dem-
ineralisation occurred close to the bracket bases in
both the Topacal C-5 treated teeth and untreated
teeth. Casein phosphopeptide preparations, such as
Topacal C-5, inhibit enamel demineralistion and
enhance remineralisation of subsurface enamel
lesions in vivo by creating a supersaturated zone of
calcium and phosphate ions in dental plaque.
810
Although Topacal C-5 conferred partial protection
against acid attack in our in vitro model, it still needs
to be tested clinically.
Our finding that the deepest demineralisation in
both groups occurred close to the bracket bases and
the shallowest demineralisation occurred towards the
occlusal surface may be due to morphological differ-
ences in the enamel, or it may be due to the different
environmental conditions in our in vitro model. It
could be postulated that fluid movement and/or the
chemical conditions in our model reduced either the
amount or the effectiveness of the Topacal C-5 close
to the brackets. The former could be due to agitation
and the latter to components in the artificial saliva,
the bracket and/or the bonding agent. These factors
require further investigation.
Regular applications of Topacal C-5 to sites at risk
may prove to be an effective method of reducing the
effects of demineralisation in susceptible patients,
such as those with poor oral hygiene or salivary gland
dysfunction.
4
However, Topacal C-5 is a milk
product and should not be used on patients allergic to
milk protein. The effectiveness of Topacal C-5 in
preventing white spot lesions may be further
enhanced if it is combined with fluoride-releasing
cements, bonding materials and varnishes.
6
It has
been postulated that fluoride-releasing materials may
inhibit enamel demineralisation adjacent to ortho-
dontic brackets by forming a protective deposit
of calcium fluoride-like particles on the enamel
surface.
8
Although these materials may not prevent
NASAB ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 48
Table I. Comparison of enamel demineralisation (m) in the experimental
and control groups.
Site Experimental Control p
d1 N 24 24 0.000
Mean 5.17 11.25
SD 3.77 3.10
d2 N 24 24 0.000
Mean 2.79 8.37
SD 1.82 3.16
d3 N 24 24 0.000
Mean 1.58 6.92
SD 1.21 3.68
Significant values in bold
Experimental group, d1 versus d3, p < 0.000
Control group, d1 versus d3, p < 0.019
Figure 3. Mean depths of the enamel lesions in the control and experimental
groups.
Control group Experimental group
11.2
5.1
8.3
2.7
6.9
1.5
12
10
8
6
4
2
0
D
e
p
t
h
(
m
)
d1 d2 d3
EFFECT OF TOPACAL C- 5 ON ENAMEL ADJACENT TO ORTHODONTIC BRACKETS
Australian Orthodontic Journal Volume 23 No. 1 May 2007 49
demineralisation they may reduce the formation of
enamel lesions and remineralise subsurface enamel
lesions.
Previous studies have reported white spot lesions in
patients treated with fixed orthodontic appliances.
13
These lesions can occur rapidly in susceptible patients
with fixed appliances. They invariably occur in areas
on the tooth surface that are difficult to clean, and
often on the labial surfaces of the incisors and canines.
Materials such as Topacal C-5
9,10
and fluoride
varnishes
6,7
that promote remineralisation of existing
lesions or prevent small lesions from becoming larger,
should be used if possible. In comparison with the
effect of fluoride varnish on demineralised enamel
adjacent to orthodontic brackets,
7
the casein
phosphopeptide preparation we used also reduced
demineralisation by more than 50 per cent.
Conclusions
In this in vitro study Topacal C-5 reduced the demin-
eralisation of enamel adjacent to orthodontic brackets
compared with teeth not covered with Topacal C-5.
Topacal C-5 may reduce enamel demineralisation in
patients with poor oral hygiene or patients suscept-
ible to enamel demineralisation, but it may not be
appropriate in patients allergic to milk products.
Corresponding author
Professor Zahra Dalili
Department of Maxillofacial Radiology
Dental School
Opp. Pardis Hotel
P.C. 41887-94755, Rasht
Iran
Tel: +98(0) 131 772 5968
Fax: +98(0) 131 772 5968 or 323 0776
Email: dalili@gums.ac.ir
References:
1. Mizrahi E. Enamel demineralization following orthodontic
treatment. Am J Orthod 1982;82:627.
2. Ogaard B. Prevalence of white spot lesions in 19year-olds:
a study on untreated and orthodontically treated persons
5 years after treatment. Am J Orthod Dentofacial Orthop
1989;96:4237.
3. Gorelick L, Geiger AM, Gwinnett AJ. Incidence of white
spot formation after bonding and banding. Am J Orthod
1982;81:938.
4. Ogaard B, Rolla G, Arends J, Ten Cate JM. Orthodontic
appliances and enamel demineralization: Part I. Am J
Orthod Dentofacial Orthop 1988;94:6873.
5. Van der Linden RP, Dermaut LR. White spot formation
under orthodontic bands cemented with glass ionomer with
or without Fluor Protector. Eur J Orthod 1998;20:21924.
6. Todd MA, Staley RN, Kanellis M, Donly KJ, Wefel JS.
Effect of a fluoride varnish on demineralization adjacent to
orthodontic brackets. Am J Orthod Dentofacial Orthop
1999;116:15967.
7. Schmit JL, Staley RN, Wefel JS, Kanellis M, Jakobsen JR,
Keenan PJ. Effect of fluoride varnish on demineralization
adjacent to brackets bonded with RMGI cement. Am J
Orthod Dentofacial Orthop 2002;122:12534.
8. Basdra EK, Huber H, Komposh G. Fluoride released from
orthodontic bonding agents alters the enamel surface and
inhibits enamel demineralization in vitro. Am J Orthod
Dentofacial Orthop 1996;109:46672.
9. Reynolds EC. Remineralization of enamel subsurface lesions
by casein phosphopeptide-stabilized calcium phosphate
solutions. J Dent Res 1997;76:158795.
10. Mazzaoui SA, Burrow MF, Tyas MJ, Dashper SG, Eakins D,
Reynolds EC. Incorporation of casein phosphopeptide-
amorphous calcium phosphate into a glass-ionomer cement.
J Dent Res 2003;82:91418.
11. Ogaard B. Effects of fluoride on caries development and
progression in vivo. J Dent Res 1990;69:8139.
Introduction
Interest in orthodontic treatment as well as provision
of orthodontic care has increased considerably over
the past decades.
15
The evaluation of orthodontic
care is necessary to determine if treatment was under-
taken appropriately.
3,4
Several studies have shown
that even after orthodontic treatment significant
levels of malocclusion remain, and children have
reported unfavourable impacts on their quality of life
related to their teeth.
57
With increasing emphasis on evidence-based health
services, the need to document the impact of pro-
vided care is a challenge to the orthodontic profes-
sion.
8
Hence, in communities with public-funded
orthodontic care and where the selection of patients
for treatment is based on severity of the malocclusion,
the impact of orthodontic care is usually assessed by
selecting cases with a clear-cut treatment need from
the population.
3,4,9
Whereas in communities where
the patient pays for treatment, concern for and a
desire to improve dentofacial appearance is a signifi-
cant motive to seek orthodontic treatment,
10,11
but is
still strongly dependent on the ability to pay. In such
cases, treatment is often influenced more by demand
than by need.
6,12,13
Obviously the impact of provided orthodontic treat-
ment should be evaluated, irrespective of the payment
system. Assessment of the impact of the orthodontic
care systems, either in individual patients or in the
population at large, does permit a better allocation of
the available resources and manpower, improvement
in the laws and regulations governing the provision
of orthodontic care, and the planning of different
alternatives in order to solve the populations needs.
In Peru, where there are few orthodontists and treat-
ment is too expensive for most people, two recent
studies reported that approximately a third of a
sample of young adults had a definite orthodontic
Australian Orthodontic Journal Volume 23 No. 1 May 2007 50
The impact of orthodontic treatment on normative
need. A case-control study in Peru
Eduardo Bernab,
*
Socorro A. Borges-Yez
and Carlos Flores-Mir
+
Departamento de Odontologa Social, Facultad de Estomatologa, Universidad Peruana Cayetano Heredia, Lima, Per,
*
Divisin de Estudios de
Postgrado e Investigacin, Facultad de Odontologa, Universidad Nacional Autnoma de Mxico, Mxico D.F., Mxico,
and Department of
Dentistry, University of Alberta, Edmonton, Canada
+
Objective: To assess the impact of previously provided orthodontic treatment on the normative need in a sample of young adult
Peruvians.
Methods: Six hundred and thirty five freshmen, representative of all first year students registering in 2002 at a private university
in Lima, were randomly screened to obtain 63 cases and 126 controls. A case was defined as having a definite orthodontic
treatment need determined by the DAI and IOTN indices simultaneously. A control was defined as having no need of orthodon-
tic treatment based on both indices. Students were also asked if they had previously undergone any orthodontic treatment.
Binary logistic regression was used for the statistical analysis.
Results: Sex, age and socioeconomic status of the students were not statistically associated with normative orthodontic treatment
need (p = 0.258, 0.556 and 0.272 respectively). The percentage of students with a previous history of orthodontic treat-
ment was similar between the cases and the controls (14.3 per cent and 11.9 per cent respectively). There were no statistically
significant associations between the variables.
Conclusions: The impact of previously provided orthodontic treatment on the current normative need of young adults was limit-
ed. Properly designed studies are required to assess the reasons for these findings.
(Aust Orthod J 2007; 23: 5054)
Received for publication: September 2006
Accepted: April 2007
IMPACT OF ORTHODONTIC TREATMENT ON NORMATIVE NEED
Australian Orthodontic Journal Volume 23 No. 1 May 2007 51
treatment need based on clinical normative need.
14,15
In such circumstances, before planning ortho-
dontic services, it is important to evaluate whether
treatments currently being done are effective.
Therefore, the objective of this study was to assess the
impact of previously provided orthodontic treatment
on the normative treatment need in a sample of
young adult Peruvians. It was hypothesised that the
percentage of individuals with a previous history of
orthodontic treatment would be higher in the group
without normative orthodontic treatment need than
in the group with normative orthodontic treatment
need. Since previous studies have reported that the
desire for orthodontic treatment and orthodontic
treatment need are influenced by age, sex and socio-
economic status,
10,1618
we controlled for these
sociodemographic characteristics.
Materials and methods
Study design
For this case-control study, 635 freshmen, representa-
tive of all first year students admitted in 2002 to a
private university in Lima, Peru were randomly
screened. A final sample of 63 cases and 126 controls
was selected for this case-control study. The sample
size was calculated to find a statistically significant
association between previous history of orthodontic
treatment and normative orthodontic treatment
need (Odds ratio = 0.25), with an 80 per cent power
( = 0.20) and at the 5 per cent level ( = 0.05).
A case was defined as a young adult with an ortho-
dontic treatment need based on two needs indices: a
mandatory to highly desirable need (31 points or
more) according to Dental Aesthetic Index (DAI) and
very great to great need (categories 4 or 5) accord-
ing to Dental Health Component of the Index for
Orthodontic Treatment Need (DHC-IOTN).
11,19
A
control was a young adult with no or slight need (25
points or less) according to DAI and little to no
need (categories 1 or 2) according to DHC-IOTN.
The indices were selected because of their wide inter-
national use. The DAI has been adopted by the
WHO as a cross-cultural index,
20
and the IOTN is
commonly used in European countries.
9,12
Previous
authors have reported differences in the diagnostic
results attained with both indices individually,
2123
therefore both the DAI and IOTN indices were used
to ensure rigorous criteria of need. Although all
indices have their limitations,
9,12
simultaneous use of
more than one index could partially overcome the
limitations of a single index. It was considered that
the information collected by one index would com-
plement the information collected by the other index
and vice versa.
All assessed students signed a voluntary consent form
and none were receiving active orthodontic treat-
ment. The International Research Board at the
Universidad Peruana Cayetano Heredia gave ethical
approval for the study.
Data collection
Data were collected by a clinical examination and a
structured interview. Clinical examinations were
carried out at the University Dental Clinic by one
calibrated examiner using the DAI and the DHC-
IOTN. Intra-examiner reliability was assessed by
repeated assessments on 10 students on different days
(0.85 and 0.89 respectively, weighted Kappa).
For the DAI, 10 occlusal traits were assessed accord-
ing to three components: dentition, spacing-
crowding and occlusion.
19
Scores for each trait were
weighted and added to a constant to obtain a final
DAI score for each student. Based on this score,
students were classified as having no or slight ( 25
points), elective (2630 points), highly desirable
(3135 points) or mandatory ( 36 points)
orthodontic treatment need.
19,20
For the DHC-IOTN, 10 traits of malocclusion were
assessed: overjet, reverse overjet, overbite, openbite,
crossbite, crowding, impeded eruption, defects of
cleft lip and palate as well as any craniofacial anom-
aly, Class II and Class III buccal occlusions, and
hypodontia. Only the highest scoring trait was used
for assessing the treatment need.
9,11
Each student
was then classified as having no (1), slight (2),
moderate (3), great (4) or very great (5) treatment
need.
11
During interviews, students were asked to give per-
sonal data as well as their university tuition fee scale
as an indirect measure of their socioeconomic status
(SES). At this private university, students pay differ-
ent tuition fees based upon family income as well as
their parents and/or their own main occupation.
With this information, an ordinal scale of three cate-
gories was created: low, medium and high SES.
15,24
Finally, students were asked if they had previously
had orthodontic treatment, irrespective of whether
removable or fixed appliances were used.
Statistical analysis
The effect of each covariable (sex, age and SES) on
normative orthodontic treatment need was assessed
by univariate binary logistic regression analyses.
Then, the impact of the previous history of ortho-
dontic treatment on normative need was also assessed
through a univariate binary logistic regression.
Finally, a multivariate binary logistic regression was
carried out to assess possible interactions between a
previous history of orthodontic treatment and the
covariables on normative need. Odds Ratios (OR)
were also calculated as a measure of effect.
Results
Sixty three young adult cases with normative ortho-
dontic treatment need (Mean age: 18.03 years;
Females: 41.3 per cent) and 126 young adult controls
without normative orthodontic treatment need
(Mean age: 17.90 years; Females: 50.0 per cent) were
clinically assessed using the two indices.
The distribution of cases and controls according to
covariables is shown in Table I. There were no statis-
tically significant associations between students
normative orthodontic treatment need and their sex
(p = 0.258), age (p = 0.556) and SES (p 0.272).
A higher percentage of students with normative
orthodontic treatment need, based on the DAI and
DHC-IOTN, reported a previous history of ortho-
dontic treatment than those without normative
orthodontic treatment need (14.3 per cent versus
11.9 per cent): the difference was not statistically sig-
nificant (p = 0.556). When the association between
previous history of orthodontic treatment and nor-
mative need was assessed by multivariate analysis,
controlling for sex, age and SES of the students as
well as including possible two-term and three-term
interactions in the model, no statistically significant
association or interaction was found (p > 0.05 for all
cases).
Discussion
In our study, contrary to what we expected, the per-
centage of previously treated young adults was similar
among those with and without normative ortho-
dontic treatment need. Almost 15 per cent of subjects
with a definite level of normative treatment need had
previously received orthodontic treatment. That sug-
gests that the orthodontic treatment provided to
these individuals was ineffective.
The results of orthodontic treatment are not always
ideal or even satisfactory.
1,2
A point to consider is that
it is likely that individuals who have been ortho-
dontically treated had more severe orthodontic
problems than those who have not been treated.
1
BERNAB
E ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 52
Table I. Associations between the covariables, past history of orthodontic treatment and normative orthodontic treatment need in young adult Peruvians.
Factors Need No need
N Per cent N Per cent Odds ratio 95% CI p*
Sex
Female 26 41.3 63 50.0 1.00
Male 37 58.7 63 50.0 1.42 0.77; 2.62 0.258
Age in years
Mean (SD) 18.03 (1.50) 17.90 (1.35) 1.07 0.86; 1.32 0.556
Socioeconomic status (SES)
Low SES 37 58.7 64 50.8 1.00
Medium SES 23 36.5 51 40.5 0.78 0.41; 1.48 0.445
High SES 3 4.8 11 8.7 0.47 0.12; 1.80 0.272
Previous history of orthodontic treatment
Without 54 85.7 111 88.1 1.00
With 9 14.3 15 11.9 1.23 0.51; 2.99 0.643
* Binary logistic regression
IMPACT OF ORTHODONTIC TREATMENT ON NORMATIVE NEED
Australian Orthodontic Journal Volume 23 No. 1 May 2007 53
Therefore, the amount and complexity of ortho-
dontic treatment required could have been higher
and optimal results more difficult to obtain.
An evaluation of the occlusal characteristics of the
nine unsuccessfully treated individuals in this study
showed that four of them had an increased overjet
greater than 6 mm, four had dental crowding greater
than 4 mm, and one had extensive hypodontia
with restorative implications. Therefore, reasons for
the results reported here might be an unfavourable
skeletal growth pattern during and/or after treatment,
relapse after treatment or insufficient compliance
resulting in incomplete treatment or compromised
treatment goals.
2,24
No information about the
completion of previous orthodontic treatment was
collected.
Other significant factors not evaluated were: if the
previous orthodontic treatment was provided by
general dentists or by orthodontic specialists, and the
type of appliances used. It is not uncommon for
general practitioners to treat individuals with minor
malocclusions.
25,26
Although the merits of ortho-
dontic care by general dentists will continue to be
debated, it would be useful to determine the amount
and types of orthodontic care that general dentists
perform and compare them to the cases specialists
treat.
27,28
Even though the finding from this study may be sur-
prising, some previous cross-sectional studies have
reported similar normative treatment need levels in
orthodontically treated and untreated groups.
1,2,8,29
Conversely, when longitudinal designs were used,
based mainly on pre- and post-treatment records, the
provision of orthodontic treatment was shown to be
effective, and cost-effective.
4,28,3032
Although almost 12 per cent of the young adults
without normative need had received previous ortho-
dontic treatment it was not possible to measure the
magnitude of change because the study design did
not allow us to determine the initial occlusal condi-
tion. No longitudinal data on pre- and post-ortho-
dontic treatment was available. This limitation has
been previously reported.
28,33
It has been recommended that the impact of ortho-
dontic services should be assessed by longitudinal
studies with initial and final clinical examinations.
3,4
However, the quality of the case records varies widely
among dental professionals in Peru, especially among
general dentists, making this information difficult to
obtain. In such situations, alternative study designs
are required and observational studies might provide
some useful information.
To date, there has been no published work on the
impact of orthodontic treatment provided in Peru.
Therefore, the present results will serve as a starting
point to set standards for the provision of ortho-
dontic care in Peru by orthodontists and general prac-
titioners, using evidence-based outcomes to assign
scarce public resources to those with the most need.
Although this study was only designed to assess the
impact of treatment on normative orthodontic treat-
ment need, it has to be understood that the profes-
sional perspective is only one of the components to be
evaluated. If the objective for orthodontic treatment
is only related to clinically measurable physical defor-
mities, the broader concepts of health are not taken
into account.
29,34
Especially in orthodontics, broader
concepts of health should be considered. They
include the psychological and social well-being of the
individual since orthodontic treatment may alter the
individuals facial appearance, thereby affecting self-
image.
1,24,34
Further studies should be done which
involve not only the effect of the orthodontic treat-
ment from a professional perspective, but also the
psychosocial impact of treatment on individuals and
their satisfaction with their teeth and mouth.
It must be noted that the population of young
adults attending the selected university may not
represent typical young adult Peruvians as this uni-
versity was selected for its convenience. For that
reason generalisation of the results has to be made
with caution.
Since the hypothesis that a higher percentage of
orthodontic treatment would be found in individuals
without normative need than in those with need
could not be confirmed, it is concluded that the
impact of the orthodontic treatment provided in this
sample of young adults was limited. As the design of
the present study did not allow us to determine the
factors responsible for the present results, further
studies are required to answer this question.
Acknowledgments
The authors would like to thank Professor Aubrey
Sheiham for his comments on the final version of this
article.
BERNAB
E ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 54
Corresponding author
Dr Eduardo Bernab
Departamento de Odontologa Social
Facultad de Estomatologa
Avenida Honorio Delgado 430
Universidad Peruana Cayetano Heredia,
Lima 31, Peru
Tel: (+51 1) 319 0059
Fax: (+51 1) 381 0607
Email: 06032@upch.edu.pe
References
1. Tuominen ML, Nystrom M, Tuominen RJ. Subjective and
objective orthodontic treatment need among orthodontic-
ally treated and untreated Finnish adolescents. Community
Dent Oral Epidemiol 1995;23:28690.
2. Kerosuo H, Kerosuo E, Niemi M, Simola H. The need for
treatment and satisfaction with dental appearance among
young Finnish adults with and without a history of ortho-
dontic treatment. J Orofac Orthop 2000;61:33040.
3. Richmond S, Phillips CJ, Dunstan F, Daniels C, Durning P,
Leahy F. Evaluating the cost-effectiveness of orthodontic
provision. Dent Update 2004;31:14652.
4. Richmond S, Dunstan F, Phillips C, Daniels C, Durning P,
Leahy F. Measuring the cost, effectiveness, and cost-effec-
tiveness of orthodontic care. World J Orthod 2005;6:
16170.
5. Zhang M, McGrath C, Hagg U. The impact of malocclusion
and its treatment on quality of life: a literature review. Int J
Paediatr Dent 2006;16:3817.
6. de Oliveira CM, Sheiham A. Orthodontic treatment and its
impact on oral health-related quality of life in Brazilian
adolescents. J Orthod 2004;31:207; discussion 15.
7. Klages U, Bruckner A, Zentner A. Dental aesthetics, self-
awareness, and oral health-related quality of life in young
adults. Eur J Orthod 2004;26:50714.
8. Lagerstrom L, Stenvik A, Espeland L, Hallgren A. Outcome
of a scheme for orthodontic care: a comparison of untreated
and treated 19-year-olds. Swed Dent J 2000;24:4957.
9. Shaw WC, Richmond S, OBrien KD. The use of occlusal
indices: a European perspective. Am J Orthod Dentofacial
Orthop 1995;107:110.
10. Reichmuth M, Greene KA, Orsini MG, Cisneros GJ, King
GJ, Kiyak HA. Occlusal perceptions of children seeking
orthodontic treatment: impact of ethnicity and socio-
economic status. Am J Orthod Dentofacial Orthop 2005;
128:57582.
11. Brook PH, Shaw WC. The development of an index of
orthodontic treatment priority. Eur J Orthod 1989;11:30920.
12. Jarvinen S. Indexes for orthodontic treatment need. Am J
Orthod Dentofacial Orthop 2001;120:2379.
13. Hamdan AM. The relationship between patient, parent and
clinician perceived need and normative orthodontic treatment
need. Eur J Orthod 2004;26:26571.
14. Bernab E, Flores-Mir C. Normative and self-perceived
orthodontic treatment need of a Peruvian university
population. Head Face Med 2006;2:22.
15. Bernab E, Flores-Mir C. Orthodontic treatment need in
Peruvian young adults evaluated through Dental Aesthetic
Index. Angle Orthod 2006;76:41721.
16. Stenvik A, Espeland L, Berset GP, Eriksen HM. Attitudes to
malocclusion among 18- and 35-year-old Norwegians.
Community Dent Oral Epidemiol 1996;24:3903.
17. Tickle M, Kay EJ, Bearn D. Socio-economic status and
orthodontic treatment need. Community Dent Oral
Epidemiol 1999;27:41318.
18. Bos A, Hoogstraten J, Prahl-Andersen B. Attitudes towards
orthodontic treatment: a comparison of treated and untreated
subjects. Eur J Orthod 2005;27:14854.
19. Cons NC, Jenny J, Kohout FJ. DAI: the dental aesthetic
index. Iowa City: College of Dentistry, University of Iowa;
1986.
20. WHO. Oral Health Surveys: basic methods. Geneva: World
Health Organization; 1997.
21. Jenny J, Cons NC. Comparing and contrasting two ortho-
dontic indices, the Index of Orthodontic Treatment need
and the Dental Aesthetic Index. Am J Orthod Dentofacial
Orthop 1996;110:41016.
22. Beglin FM, Firestone AR, Vig KW, Beck FM, Kuthy RA,
Wade D. A comparison of the reliability and validity of 3
occlusal indexes of orthodontic treatment need. Am J
Orthod Dentofacial Orthop 2001;120:2406.
23. Johnson M, Harkness M, Crowther P, Herbison P. A com-
parison of two methods of assessing orthodontic treatment
need in the mixed dentition: DAI and IOTN. Aust Orthod
J 2000;16:827.
24. Tuominen ML, Tuominen RJ, Nystrom ME. Subjective
orthodontic treatment need and perceived dental appearance
among young Finnish adults with and without previous
orthodontic treatment. Community Dent Health 1994;11:
2933.
25. Huang GJ, Marston BE, del Aguila MA. Orthodontic care in
an insured population in Washington: demographic factors.
Am J Orthod Dentofacial Orthop 2004;125:7416.
26. Mirabelli JT, Huang GJ, Siu CH, King GJ, Omnell L. The
effectiveness of phase I orthodontic treatment in a Medicaid
population. Am J Orthod Dentofacial Orthop 2005;127:
5928.
27. Huang GJ, del Aguila MA. Distribution of orthodontic
services and fees in an insured population in Washington.
Am J Orthod Dentofacial Orthop 2003;124:36672.
28. Radnzic D. Effectiveness of community-based salaried
orthodontic services provided in England and Wales. J
Orthod 2002;29:11923.
29. Pietila T, Pietila I. Dental appearance and orthodontic ser-
vices assessed by 15-16-year-old adolescents in eastern
Finland. Community Dent Health 1996;13:13944.
30. OBrien KD, Shaw WC, Roberts CT. The use of occlusal
indices in assessing the provision of orthodontic treatment
by the hospital orthodontic service of England and Wales. Br
J Orthod 1993;20:2535.
31. Bergstrom K, Halling A. Orthodontic treatment outcome in
three Swedish counties with different orthodontic resources.
Swed Dent J 1996;20:5160.
32. Richmond S, Ikonomou C, Williams B, Ramel S, Rolfe B,
Kurol J. Orthodontic treatment standards in a public group
practice in Sweden. Swed Dent J 2001;25:13744.
33. Shaw WC, Addy M, Dummer PM, Ray C, Frude N. Dental
and social effects of malocclusion and effectiveness of ortho-
dontic treatment: a strategy for investigation. Community
Dent Oral Epidemiol 1986;14:604.
34. WHO. Oral health for the 21st century. Geneva: World
Health Organization; 1994.
Introduction
Broadbent
1
first introduced the use of cephalometry
in dentistry approximately 36 years after the dis-
covery of X-rays by Roentgen in 1895.
2
Despite
accepted limitations, lateral and posteroanterior
cephalometry is still considered to be a practical,
affordable and low radiation dose imaging technique.
To the trained eye, the information gained from these
cephalograms is often adequate for use in clinical
orthodontics. Despite the availability of perhaps
more sophisticated imaging techniques, the replace-
ment of cephalometry in orthodontic practice would
require a real analysis of the cost:benefit ratio for
individual orthodontic patients.
In 1917, Radon demonstrated that an infinite set of
two-dimensional (2D) projections could be used to
create a representative image of a three-dimensional
(3D) structure. Hounsfield later developed the
computerised axial transverse scanning technique and
the first commercially available computed tom-
ography (CT) scanner was later marketed in 1972.
3
By the early 1980s, both researchers and clinicians
were investigating the potential for 3D imaging of
craniofacial structures and deformities. Continued
development of CT scanners since then, has involved
changes in the geometry of the radiation beam, the
number of detector rows, the image resolution and
the speed and efficiency of image acquisition.
3D reconstructed images may enhance the clinicians
three-dimensional perception of anatomical and
morphological features of individual patients, in turn,
facilitating the development of a more appropriate
individualised treatment plan than might have been
possible with the use of conventional 2D imaging
techniques. With all this in mind, this review article
addresses the basic principles behind the use of CT
imaging, the potential clinical applications of 3D-CT
images in orthodontic practice and the possible
limitations of the technique.
What is computed tomography?
The basic component of a helical CT scanner is the
gantry that continuously rotates during volume data
acquisition, as the patient is transported through the
machine.
The gantry is comprised of numerous rows of
detector arrays, an X-ray source and the patient
Australian Orthodontic Journal Volume 23 No. 1 May 2007 55
Three-dimensional computed craniofacial
tomography (3D-CT): potential uses and
limitations
Hong Jin Chan,
*
Michael Woods
and Damien Stella
+
Private practice, Melbourne,
*
School of Dental Science, The University of Melbourne
and Department of Radiology,
Royal Melbourne Hospital,
+
Melbourne, Australia
Aims: To determine the potential uses and limitations of 3D-CT craniofacial imaging in contemporary clinical practice.
Methods: The relevant historical and contemporary literature was reviewed.
Results: There would seem to be many potential uses for 3D-CT craniofacial imaging in clinical practice. Significant
limitations may, however, relate to the availability and cost of such imaging and the delivered radiation dose.
Conclusions: With continued research and development, the use of such 3D-CT craniofacial imaging techniques may become
appropriate for future orthodontic and clinical diagnostic applications.
(Aust Orthod J 2007; 23: 5564)
Received for publication: November 2006
Accepted: March 2007
support couch.
4
The desired collimation of X-ray
photons is directed at the patient and subsequently
received by the detector array rows. The volume
coverage performance of a CT scanner is limited by
its maximum pitch. Pitch is defined as the rate of
table travel per gantry rotation, divided by the beam
collimation or slice thickness.
4,5
An increase in table
travel speed, pitch or collimation in turn increases
volume coverage speed. The image resolution is, how-
ever, inversely affected by an increasing table travel
speed or collimation.
4,5
The more current multidetector row CT (MDCT)
scanners permit acquisition of volume data up to 64
contiguous slices with each gantry rotation. While
the reconstructed slice thickness cannot be smaller
than the effective detector row thickness,
3,6
64-slice
CT results in significant improvement in diagnostic
accuracy as a result of increased spatial and temporal
resolution
7,8
compared with the earlier 4- or 16-slice
MDCT systems.
Three-dimensional reconstruction from
computed tomography images
3D imaging is not new. It has, however, evolved
rapidly over the past 20 years and has found applica-
tions in both medicine and dentistry. Uses for 3D
imaging in orthodontics and oral and maxillofacial
surgery may include pre- and post-orthodontic assess-
ment of dentoskeletal relationships and facial aesthet-
ics, evaluation of orthodontic outcomes with regard
to the effects on both hard and soft tissues, 3D treat-
ment planning and simulation, 3D fabrication of cus-
tomised orthodontic archwires and computerised
archiving of 3D records.
9
The greater understanding of mathematical algo-
rithms has underpinned the rapid development of
3D-CT rendering techniques. The degree of resol-
ution and the accuracy of 3D-CT images are both
continually improving, with the use of smaller axial
CT slice thickness and slice overlapping scans.
Cavalcanti et al.
10
found a high level of precision and
accuracy in their study of anthropometric measure-
ments of both soft and hard tissues using 3D-CT
images. Similar studies by Matteson et al.
11
and
Hildebolt et al.
12
on measurements of the skull using
3D-CT images have also shown favourable results.
The typical image matrix for most CT scanners is 512
x 512 pixels. Pixels are 2D entities and therefore,
voxels provide a better representation of the tissue
volume. Voxels can be thought of as tiny cubes
arranged adjacent to each other. Each voxel can be
calculated by multiplying pixel dimensions by the
slice width,
3
thereby representing the density of
the particular anatomical structure.
13
Based on the
original series of CT data, new 2D or 3D axial or
correspondent multiplanar reconstructed (MPR)
images can then be created and further manipulated
for improved visualisation. These MPR images can
be used to display CT slices in any direction
14
and
have been validated for quantitative and qualitative
analyses.
10
Different types of tissues are characterised by a
specific range of voxel values, often defined in
Hounsfield units (HU). In order to visualise separate
anatomical structures, such as bone, teeth, muscles or
skin, a relationship between voxel value and voxel
opacity value must first be established. This is referred
to as the transfer function.
13
This transfer function
can also match voxel values to colours. The combined
use of colours, threshold HU and opacity values
preselected for a range of voxel values, helps to
differentiate the volumetric data and hence the
selective display of the anatomical structures of
interest (Figure 1).
1315
Contemporary volume
rendering 3D images can therefore demonstrate
specific internal features of a 3D structure based on
this concept.
CHAN ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 56
Figure 1. An example of a volume-rendering 3D lateral profile image
with selective illustration of the superficial masseter, temporalis and neck
muscles. Computed analyses also help to highlight the individual under-
lying vertical facial pattern.
Other applications of 3D-CT imaging techniques
may include shaded surface display (SSD), maximum
intensity projection (MIP), model production and
virtual reality. Shaded surface display assesses the sur-
face details of specific structures e.g. bone, teeth or
skin, in three-dimensions.
14
Projection, hidden-part
removal and shading are all applied in this viewing
mode, to impart a sense of 3D perspective to the
created image.
16
MIP, on the other hand, is used
more often in medicine to enhance angiographic
images.
Potential uses of 3D-CT images in clinical
orthodontics
With the development of helical MDCT scanners
and sophisticated 3D rendering software, 3D-CT
images can now be more readily generated and poten-
tially used for both diagnostic imaging and biomedical
research in dentistry.
14
Previous researchers have actu-
ally assessed the practicality of utilising such 3D-CT
scans in the clinical evaluation of the masseter muscle
morphology and the anthropometric measurements
of the craniofacial region.
10,1719
Katsumata et al.
19
and Ariji et al.,
17
for instance, evaluated the surface
topography of the masseter muscle, and its cross-
sectional area and orientation to the Frankfort hori-
zontal plane in adults presenting with mandibular
prognathism. Similarly, Kitai et al.,
18
investigated the
morphological association of craniofacial form within
a similar sample group with the cross-sectional areas
and volumes of the temporal and masseter muscles,
respectively.
Following these investigations, a recent 3D-CT study
was undertaken to assess the cross-sectional area, the
volume and the spatial orientation of the masseter,
medial pterygoid and lateral pterygoid muscles in
young orthodontic patients presenting with different
THREE- DIMENSIONAL COMPUTED CRANIOFACIAL TOMOGRAPHY
Australian Orthodontic Journal Volume 23 No. 1 May 2007 57
MPR-CT images corresponding to the darker reference plane
Figure 2. Analysis of the cross-sectional areas of the masseter, medial pterygoid and lateral pterygoid muscles. Transfer functions and a predetermined
range of window level and width were applied to selectively block out unwanted overlying fatty and skin structures.
Bisecting reference planes
Masseter Medial pterygoid muscle Lateral pterygoid muscle
underlying vertical facial patterns (Figures 2 and 3).
20
Based on the results of that study, craniofacial form,
and the cross-sectional area and volume of these mus-
cles could be accurately measured using 3D-CT
images with a high level of reproducibility. The sur-
face topography of the superficial masseter could also
be identified and measured (Figure 1).
3D-CT images are capable of providing an accurate
representation of the osseous structures of the cranio-
facial region. The ability to regenerate and man-
ipulate these images enhances the accuracy of the
analytical measurements typically used with traditional
2D cephalograms. The inherent errors associated
with plain radiograph cephalometry can therefore be
eliminated. Such errors would include those of radio-
graphic magnification and poor head posturing dur-
ing exposure, as well as examiner-biased assumptions
in locating anatomical landmarks for structures that
are either displaced or not clearly seen. 3D-CT
cephalometry is a potentially powerful craniofacial
measurement tool and has proven to be highly
accurate and reliable.
21
Also, with the application of transfer functions
during 3D-CT volume rendering techniques, an
accurate perception of the 3D positions and angul-
ations of the teeth is possible. This may include the
3D assessment of stages of the tooth development
and eruption process, the relationship of underlying
supernumerary teeth and impacted teeth to adjacent
dental structures, the relationships between the tooth
roots and the surrounding alveolar bone, and the
location of the mandibular canal (Figure 4). Macchi
et al.
22
described the combined use of CT tech-
nology and laser scanning of dental casts in the cre-
ation of an interactive 3D digital replica of the dental
anatomy of an individual. From this, the 3D anatom-
ical relationships between the teeth and with the sur-
rounding bone can be viewed and altered according
CHAN ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 58
Frontal view
Figure 3. Calculations of muscular volumes based on composites of all muscular outlines which had been digitally traced from the sequential axial
CT images.
Superior view
Masseter Medial pterygoid muscle Lateral pterygoid muscle
to the effects of certain treatment goals prior to active
treatment (e.g. for extractions, root torque changes).
The benefits of 3D simulated surgical planning with
CT data have also been assessed.
2325
The 3D visual-
isation of the facial skeleton, landmark identification,
quantitative analysis of craniofacial structures, simu-
lation of CT model osteotomies and surgical reposi-
tioning of bones, detection of skeletal interferences
and superimposition of scans are among some of the
reported benefits.
23,26,27
These features provide the
opportunity for accurate evaluation and prediction of
the outcomes of proposed craniomaxillofacial surgery
in three-dimensions. This might not have been poss-
ible with the use of standard 2D diagnostic tools.
23
A similar degree of accuracy and reliability in 3D-CT
imaging for dental implant planning and placement
has also been reported.
28,29
Following the precise
planning of implant positions using interactive
3D-CT based software, customised guide splints and
final dental prostheses are fabricated for delivery at
the time of implant placement, ensuring high preci-
sion transfer of the planned positions to the operative
field and an immediate rigid splinting of the installed
implants.
30,31
3D-CT technology can also be used to assess patients
with congenital facial anomalies, asymmetries
26,32
and facial injuries.
15,33
The morphology and position
of the temporomandibular joint (TMJ)
34
and the
patency of the airway
35,36
can be similarly assessed
(Figure 5). Kawamata et al.
35
and Fairburn et al.
36
have both described morphological changes in the
airway of adult patients following orthognathic
surgery. With regard to the TMJ region, MDCT
images can provide an accurate assessment of con-
dylar displacement and superior delineation of
TMJ osseous changes and morphology.
37
However,
magnetic resonance imaging (MRI) may still be a
better alternative in the evaluation of the soft tissue
changes and the internal derangement of the
joint.
3739
Nevertheless, considerable diagnostic
possibilities exist with the use of multiplanar recon-
structions of 3D-CT images from a single set of CT
volume data. This may in the future be of great
benefit for those managing complicated orthodontic
cases.
40
THREE- DIMENSIONAL COMPUTED CRANIOFACIAL TOMOGRAPHY
Australian Orthodontic Journal Volume 23 No. 1 May 2007 59
Figure 4. Assessment of tooth position, angulations and relationships (including supernumerary and unerupted teeth) under the radiographic
viewing mode.
Lateral view Frontal view Oblique view
Figure 5. Semi-transparent 3D-CT image showing the outlines of the
pharyngeal airway from the lateral view. The 1:1 ratio with the actual
size can allow for volumetric measurement of the pharyngeal airway.
Limitations of the 3D-CT imaging
technique
Radiation dose
Considerations that are unique to the paediatric pop-
ulation over their lifetime with repeated CT examin-
ations may include increased radiosensitivity of cer-
tain tissues, a longer lifetime for radiation-related
cancer to manifest, and a cumulative cancer risk for
certain organs. However, great debate still exists with
regard to whether low-level radiation from CT scan-
ning does significantly increase the risk of developing
fatal cancer.
41
Two main factors that may influence the radiation
exposure to the patient would be the X-ray beam
energy (determined by tube potential, measured in
kilovoltage peak, kVp) and photon fluence (affected
by the product of tube current, measured in mil-
liamperes, mA, and time).
5
In contrast to conven-
tional radiography, radiation dose used in CT does
not reduce as the incident beam penetrates the body
from the periphery to the core. Rather, the radiation
dose from a cranial CT examination is more uni-
formly distributed across the scanning plane with the
patient equally irradiated from all directions. Also,
other factors such as scattered radiation, the diver-
gence of the radiation beam and limitations in the
efficiency of beam collimation may further con-
tribute to additional radiation absorption beyond the
boundaries of the scan volume.
5
Image noise is an important determinant of the CT
image quality. Given that it is also inversely affected
by X-ray beam energy, strategies for managing radia-
tion risks have been directed toward radiation dose
optimisation rather than dose reduction per se. The
challenge has therefore been for clinicians to identify
acceptable thresholds of image quality to minimise
radiation doses and for manufacturers to improve the
dose efficiency of their CT systems.
5
The ALARA (as
low as reasonably achievable) principle has been sug-
gested for radiation dose minimisation.
41
Appropriate
strategies may involve limiting the number of CT
examinations, the region of coverage, and customis-
ing CT settings based on the indication, the cross-
sectional dimensions of the region to be examined
and the weight and size of the patient.
5,41,42
Scanning
parameters that affect CT radiation dose include the
scanner geometry, tube current and voltage, scanning
modes, length and collimations, table speed and
pitch, gantry rotation time, and shielding.
5,41,43
Most
of these parameters can be modulated to obtain the
desired image quality.
Other innovations that have served to address the
issue of radiation optimisation have included pre-
patient tracking or the control of beam collimation
and tube focal spot motion; automatic tube current
modulation (ATCM); efficient detector configur-
ation; the use of improved filters to reduce soft
X-rays and image noise or to increase the filtration of
signal dependent noise; and the improvement in
image processing algorithms.
5
ATCM is a recent
technical innovation that can substantially reduce
radiation dose. With automatic adjustments of the
tube current to reflect the changing anatomy of
the patient, the quantum noise in projections can also
be adjusted to maintain a desired noise level on the
image and to improve dose efficiency.
5,43
The annual effective dose limit for continuous or
repeated exposures, as established by National
Council on Radiation Protection Measurements
(NCRP) in the United States, is recommended to be
around 1 mSv.
44
For perspective, the average person
receives approximately 13 mSv of natural back-
ground radiation annually.
41,44
The range of radiation
exposure values previously reported for cranial CT
examination is from 0.152.30 mSv.
4547
Due to the
issue of high cost, the size of the equipment and rela-
tively high radiation exposure, cone beam computed
tomography (CBCT) has recently been introduced as
a 3D dental imaging alternative. The effective radia-
tion dose previously reported for CBCT is from
0.051.19 mSv.
45,4749
It is perhaps generally accepted
that the exposure levels from CBCT are typically
lower than MDCT.
45,4850
The image quality of
CBCT, however, does not generally correspond to
the usual quality of CT.
51,52
CBCT is designed to
scan high contrasting structures, typical of osseous
structures,
47,50
and is incapable of discriminating soft
tissue because of its low contrast resolution.
50,53,54
Initially, the typical field of view with CBCT image is
small and similar to the size of a periapical radio-
graph.
55
Larger image sizes of 13 to 19 cm in height
have now been reported, but they may come at the
expense of image resolution.
51
In time, further
improvement in the CBCT technology should
address these issues.
While the effective dose contribution from a
panoramic examination (0.010.03 mSv
46,49,53,56
) or
CHAN ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 60
a full-mouth examination (0.030.10 mSv
45,46
) is
still substantially smaller than either system, exposure
levels from low-dose regular dental CT can be signif-
icantly reduced to levels comparable with CBCT
systems and without the loss of diagnostic image
quality.
53,54
Calculations of the actual radiation dose
levels found in a 3D-CT study investigated by the
present authors showed that the mean radiation dose
level for each Melbourne facial morphology scan was
0.37 mSv ( 0.04 mSv).
20
This dose would be within
the lower range of radiation dose values reported for
CT examinations, still allowing for the accurate
assessment of the morphology of the cranial soft
tissues and dentoskeletal form. While such a dose
may still be higher than that to be expected for
routine lateral cephalograms and panoramic radio-
graphs, or perhaps with localised CBCT imaging,
dose-reduced MDCT scanning does not necessarily
result in excessive radiation exposure, especially
when taking into account the multiple diagnostic
possibilities associated with a single CT examination.
Measurement of rendered images from
3D-CT
A high precision level and accuracy in the measure-
ment of hard
1012
and soft tissues
10
using 3D-CT
imaging technique is generally accepted. However, a
number of factors may affect such accuracy. These
include the presence of artefacts, the choice of slice
plane, slice thickness and degree of slice overlapping,
the window level and width, the matrix size and the
chosen rendering technique.
10,19
It is important to
note that while 3D-CT images simulate the mor-
phology of the original subject, they are still often
viewed in a 2D format on a monitor screen or film;
hence providing a perception of the object in three
dimensions. Measurements are often considered more
reliable if they are made on the rendered images of
objects that are oriented in planes whose axes are per-
pendicular to the perspective of the viewer. Oblique
orientations may potentially affect measurement
accuracy because of elongation or foreshortening of
the image or parallax problems.
57
Identification and delineation of all soft
tissue types
Similar tissue types (e.g. muscles) are defined by a
similar range of density values. Therefore, the precise
delineation of closely approximated muscle groups is
often difficult. Superficial muscles, such as the mas-
seter, are identifiable, but the assessment of deeper
components or muscles may be affected (Figure 1).
Even with effective transfer functions, visualisation of
the internal structures may still be difficult.
13
Such
limitations can be minimised by using alternative
viewing planes and assessing the CT data in smaller
cut-out sections (Figure 6). With the appropriate
window level and width settings to selectively filter
THREE- DIMENSIONAL COMPUTED CRANIOFACIAL TOMOGRAPHY
Australian Orthodontic Journal Volume 23 No. 1 May 2007 61
Skeletal view Muscular view
Figure 6. Use of clip planes to display a section or a determined slice thickness of volume data at any given time.
out unwanted overlying fatty and skin structures, the
delineation of the topography of the mandibular
muscles from the transverse or superior plane is pos-
sible (Figures 2 and 3). Therefore, not only are the
dentoskeletal structures identifiable and measurable
with 3D-CT images, but similar accuracy can also be
achieved during the assessment of the cross-sectional
size and volume of mandibular muscles. While MRI
is currently accepted to produce superior soft tissue
contrast compared with CT scans, limited literature
exists to directly compare the effectiveness of both
imaging techniques using the more recent models
in the delineation and identification of closely
approximated facial muscles.
Logistics and commercial availability of
MDCT scanners
MDCT scanners are often limited to specialist imag-
ing practices or hospitals that may perform a large
range of CT-related imaging applications, in order to
cover the cost of equipment installation. The manipu-
lation of 3D rendering images is also often done with
the use of appropriate software developed by the
manufacturers and is hence licensed for use only with
the purchase of a MDCT scanner. While the process-
ing capacity of a CT workstation is often no different
from a typical personal computer, such software is
rarely available within an orthodontic practice or
clinic. However, it may in the future be possible to
purchase extra software licences. Alternatively, other
software companies may develop programs which
could read the archived CT data format. Auxiliary
personnel within an orthodontic practice could also
be appropriately trained to analyse the cranial muscu-
loskeletal form.
Conclusions
Despite the limitations outlined above, three-dimen-
sional computed tomography (3D-CT) may, in the
future, become a practical technique for the assess-
ment of craniofacial soft and hard tissues in selected
dental and surgical cases. 3D-CT provides a more
detailed appreciation of the interaction and relation-
ships between the dentoskeletal structures and the
overlying soft tissue environment. While progressive
advances in this technology would inevitably fur-
ther improve scanning efficiency while decreasing
radiation risk, further research is still be required to
determine appropriate scanning protocols for deliver-
ing minimal radiation exposure, before the technique
can be recommended for routine clinical use.
Consideration should also be given to the use of
3D-CT cephalometric analyses including the assess-
ment of the masticatory muscles, since these muscles
are now widely accepted to be closely involved in the
facial growth and development process, and to influ-
ence the predictability and long-term outcomes of
clinical treatment.
Acknowledgments
The authors would like to thank Mrs Shona
Robertson and Mr Paul Einsiedel from the
Department of Radiology at the Royal Melbourne
Hospital for their assistance in the application of the
3D-CT technique. This study was supported in part
by a grant from the Australian Society of
Orthodontists Foundation for Research and
Education.
Corresponding author
Professor Michael Woods
School of Dental Science
The University of Melbourne
720 Swanston Street
Melbourne, Victoria 3010
Australia
Tel: (+61 3) 9341 1497
Fax: (+61 3) 9341 1593
Email: mgwoods@unimelb.edu.au
References
1. Broadbent B. A new X-ray technique and its application to
orthodontia. Angle Orthod 1931;1:4566.
2. Quintero J, Trosien A, Hatcher D, Kapila S. Craniofacial
imaging in orthodontics: historical prespective, current
status, and future developments. Angle Orthod 1999;69:
491506.
3. Parks E. Computed tomography applications for dentistry.
Dent Clin North Am 2000;44:37194.
4. Dawn S, Gotway M, Webb W. Multidetector-row spiral
computed tomography in the diagnosis of thoracic diseases.
Respir Care 2001;46:91221.
5. Kalra M, Maher M, Toth T, Hamberg L, Blake M, Shepard J
et al. Strategies for CT radiation dose optimization.
Radiology 2004;230:61928.
6. Saini S. Multi-detector row CT: principles and practice for
abdominal applications. Radiology 2004;233:3237.
7. Hausleiter J, Meyer T, Hadamitzky M, Huber E, Zankl M,
Martinoff S et al. Radiation dose estimates from cardiac
multislice computed tomography in daily practice: impact of
different scanning protocols on effective dose estimates.
Circulation 2006;113:130510.
CHAN ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 62
8. Sun Z, Jiang W. Diagnostic value of multislice computed
tomography angiography in coronary artery disease: a meta-
analysis. Eur J Radiol 2006;60:27986.
9. Hajeer M, Millett D, Ayoub A, Siebert J. Applications of 3D
imaging in orthodontics: Part I. J Orthod 2004;31:6270.
10. Cavalcanti M, Rocha S, Vannier M. Craniofacial measure-
ments based on 3D-CT volume rendering: implications for
clinical applications. Dentomaxillofac Radiol 2004;33:
1706.
11. Matteson S, Bechtold W, Phillips C, Staab E. A method for
three-dimensional image reformation for quantitative
cephalometric analysis. J Oral Maxillofac Surg 1989;47:
105361.
12. Hildebolt C, Vannier M, Knapp R. Validation study of skull
three-dimensional computerized tomography measurements.
Am J Phys Anthropol 1990;82:28394.
13. Halazonetis D. From 2-dimensional cephalograms to 3-
dimensional computed tomography scans. Am J Orthod
Dentofacial Orthop 2005;127:62737.
14. Kawamata A, Ariji Y, Langlais R. Three-dimensional com-
puted tomography imaging in dentistry. Dent Clin North
Am 2000;44:395410.
15. Luka B, Brechtelsbauer D, Gellrich N-C, Knig M. 2D and
3D CT reconstructions of the facial skeleton: an unneces-
sary option or a diagnostic pearl? Int J Oral Maxillofac Surg
1995;24:7683.
16. Udupa J. Three-dimensional visualization and analysis
methodologies: a current prespective. Radiographics 1999;
19:783806.
17. Ariji Y, Kawamata A, Yoshida K, Sakuma S, Nawa H,
Fujishita M et al. Three-dimensional morphology of the
masseter muscle in patients with mandibular prognathism.
Dentomaxillofac Radiol 2000;29:1138.
18. Kitai N, Fujii Y, Murakami S, Furukawa S, Kreiborg S,
Takada K. Human masticatory muscle volume and
zygomatico-mandibular form in adults with mandibular
prognathism. J Dent Res 2002;81:7526.
19. Katsumata A, Fujishita M, Ariji Y, Ariji E, Langlais R. 3D
CT evaluation of masseter muscle morphology after setback
osteotomy for mandibular prognathism. Oral Surg Oral Med
Oral Pathol Oral Radiol Endod 2004;98:46170.
20. Chan HJ, Woods M, Stella D. Mandibular muscle morphol-
ogy in growing children with different vertical facial
patterns: a 3D-CT study. Am J Orthod Dentofacial Orthop
2007 (in press).
21. Swennen G, Schutyser F. Three-dimensional cephalometry:
spiral multi-slice vs cone-beam computed tomography. Am J
Orthod Dentofacial Orthop 2006;130:4106.
22. Macchi A, Carrafiello G, Cacciafesta V, Norcini A. Three-
dimensional digital modeling and setup. Am J Orthod
Dentofacial Orthop 2006;129:60510.
23. Troulis M, Everett P, Seldin E, Kikinis R, Kaban L.
Development of a three-dimensional treatment planning
system based on computed tomographic data. Int J Oral
Maxillofac Surg 2002;31:34957.
24. Girod S, Keeve E, Girod B. Advances in interactive cranio-
facial surgery planning by 3D simulation and visualization.
Int J Oral Maxillofac Surg 1995;24:1205.
25. Xia J, Wang D, Samman N, Yeung R, Tideman H.
Computer-assisted three-dimensional surgical planning and
simulation: 3D color facial model generation. Int J Oral
Maxillofac Surg 2000;29:210.
26. Katsumata A, Fujishita M, Maeda M, Ariji Y, Ariji E,
Langlais R. 3D-CT evaluation of facial asymmetry. Oral
Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:
21220.
27. Papadopoulos M, Christou P, Athanasiou A, Boettcher P,
Zeilhofer H, Sader R et al. Three-dimensional craniofacial
reconstruction imaging. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod 2002;93:38293.
28. Jacobs R, Adriansens A, Verstreken K, Suetens P, van
Steenberghe D. Predictability of a three-dimensional plan-
ning system for oral implant surgery. Dentomaxillofac
Radiol 1999;28:10511.
29. Cavalcanti M, Ruprecht A, Vannier M. 3D volume ren-
dering using multislice CT for dental implants. Dento-
maxillofac Radiol 2002;31:21823.
30. Holst S, Blatz M, Eitner S. Precision for computer-guided
implant placement: using 3D planning software and fixed
intraoral reference points. J Oral Maxillofac Surg 2007;65:
3939.
31. van Steenberghe D, Glauser R, Blomback U, Andersson M,
Schutyser F, Pettersson A et al. A computed tomographic
scan-derived customized surgical template and fixed pros-
thesis for flapless surgery and immediate loading of implants
in fully dentulous maxillae: a prospective multicenter study.
Clin Implant Dent Relat Res 2005;7 Suppl 1:S11120.
32. Ono I, Ohura T, Narumi E, Kawashima K, Matsuno I,
Nakamura S et al. Three-dimensional analysis of craniofacial
bones using three-dimensional computer tomography. J
CranioMaxillofac Surg 1992;20:4960.
33. Salvolini U. Traumatic injuries: imaging of facial injuries.
Eur Radiol 2002;12:125361.
34. Kawamata A, Fujishita M, Nagahara K, Kanematu N, Niwa
K, Langlais R. Three-dimensional computed tomography
evaluation of postsurgical condylar displacement after
mandibular osteotomy. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod 1998;85:3716.
35. Kawamata A, Fujishita M, Ariji Y, Ariji E. Three-dimen-
sional computed tomographic evaluation of morphologic
airway changes after mandibular setback osteotomy for
prognathism. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod 2000;89:27887.
36. Fairburn S, Waite P, Vilos G, Harding S, Bernreuter W, Cure
J et al. Three-dimensional changes in upper airways of
patients with obstructive sleep apnea following maxilloman-
dibular advancement. J Oral Maxillofac Surg 2007;65: 612.
37. Katsumata A, Nojiri M, Fujishita M, Ariji Y, Ariji E,
Langlais R. Condylar head remodeling following mandibular
setback osteotomy for prognathism: a comparative study of
different imaging modalities. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod 2006;101:50514.
38. Gerhard S, Ennemoser T, Rudisch A, Emshoff R. Condylar
injury: magnetic resonance imaging findings of temporo-
mandibular joint soft tissue changes. Int J Oral Maxillofac
Surg 2007;36:2148.
39. S,ener S, Akganl F. MRI characteristics of anterior disc dis-
placement with and without reduction. Dentomaxillofac
Radiol 2004;33:24552.
40. Hatcher D, Aboudara C. Diagnosis goes digital. Am J
Orthod Dentofacial Orthop 2004;125:5125.
41. Frush D, Donnelly L, Rosen N. Computed tomography and
radiation risks: what pediatric health care providers should
know. Pediatrics 2003;112:9517.
42. Wilting J, Zwartkruis A, van Leeuwen M, Timmer J, Kam-
phuis A, Feldberg M. A rational approach to dose reduction
in CT: individualized scan protocols. Eur Radiol 2001;11:
262732.
THREE- DIMENSIONAL COMPUTED CRANIOFACIAL TOMOGRAPHY
Australian Orthodontic Journal Volume 23 No. 1 May 2007 63
43. Kalra M, Maher M, Toth T, Schmidt B, Westerman B,
Morgan H et al. Techniques and applications of automatic
tube current modulation for CT. Radiology 2004;233:
64957.
44. Mupparapu M. Radiation protection guidelines for the prac-
ticing orthodontist. Am J Orthod Dentofacial Orthop 2005;
128:16872.
45. Mah J, Danforth R, Bumann A, Hatcher D. Radiation
absorbed in maxillofacial imaging with a new dental com-
puted tomography device. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod 2003;96:50813.
46. Ngan D, Kharbanda O, Geenty J, Darendeliler M.
Comparison of radiation levels from computed tomography
and conventional dental radiographs. Aust Orthod J 2003;
19:6775.
47. Wrtche R, Hassfeld S, Lux C, Mssig E, Hensley F,
Krempien R et al. Clinical application of cone beam digital
volume tomography in children with cleft lip and palate.
Dentomaxillofac Radiol 2006;35:8894.
48. Hashimoto K, Arai Y, Iwai K, Araki M, Kawashima S,
Terakado M. A comparison of a new limited cone beam
computed tomography machine for dental use with a multi-
detector row helical CT machine. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod 2003;95:3717.
49. Ludlow J, Davies-Ludlow L, Brooks S. Dosimetry of two
extraoral direct digital imaging devices: NewTom cone beam
CT and Orthophos Plus DS panoramic unit. Dento-
maxillofac Radiol 2003;32:22934.
50. Schulze D, Heiland M, Thurmann H, Adam G. Radiation
exposure during midfacial imaging using 4- and 16-slice
computed tomography, cone beam computed tomography
systems and conventional radiography. Dentomaxillofac
Radiol 2004;33:836.
51. Araki K, Maki K, Seki K, Sakamaki K, Harata Y, Sakaino R
et al. Characteristics of a new developed dentomaxillofacial
x-ray cone beam CT scanner (CB MercuRayTM): system
configuration and physical properties. Dentomaxillofac
Radiol 2004;33:519.
52. Holberg C, Steinhuser S, Geis P, Rudzki-Janson I. Cone-
beam computed tomography in orthodontics: benefits and
limitations. J Orofac Orthop 2005;66:43444.
53. Cohnen M, Kemper J, Mbes O, Pawelzik J, Mdder U.
Radiation dose in dental radiology. Eur Radiol 2002;12:
6347.
54. Rustemeyer P, Streubhr U, Suttmoeller J. Low-dose dental
computed tomography: significant dose reduction without
loss of image quality. Acta Radiol 2004;45:84753.
55. Arai Y, Tammisalo E, Iwai K, Hashimoto K, Shinoda K.
Development of a compact computed tomographic appara-
tus for dental use. Dentomaxillofac Radiol 1999;28:2458.
56. Gijbels F, Jacobs R, Bogaerts R, Debaveye D, Verlinden S,
Sanderink G. Dosimetry of digital panoramic imaging. Part
I: patient exposure. Dentomaxillofac Radiol 2005;34:1459.
57. Covino SW, Mitnick RJ, Shprintzen RJ, Cisneros GJ. The
accuracy of measurements of three-dimensional computed
tomography reconstructions. J Oral Maxillofac Surg 1996;
54:98290. Discussion 9901.
CHAN ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 64
Introduction
It is generally accepted that a skeletal 2 malocclusion
is associated with a large maxilla, a deficient mandible
or a combination of these factors. On the other hand,
a dental Class II division 1 malocclusion is due to
dentoalveolar variation and may result from pro-
clined maxillary anterior teeth. The treatment
approaches for a skeletal 2 malocclusion include
growth modification, camouflage treatment or
combined orthodontic treatment and orthognathic
surgery. The choice of treatment will depend on
factors such as: the cause(s) of the malocclusion, the
site and severity of the discrepancy, the age or growth
potential of the patient, the facial aesthetics, psycho-
logical factors and financial concerns.
1
Growth modification of a skeletal 2 malocclusion in
a growing patient may be achieved with either extra-
oral or functional appliances.
2,3
The treatment pos-
sibilities for skeletal 2 malocclusions in non-growing
patients may be either by orthodontic tooth move-
ment to camouflage the underlying jaw discrepancy
or by surgical repositioning of the jaws.
1
Compared
with the surgical method, camouflage treatment is a
simpler procedure, has fewer risks and complications,
costs less and often results in an improved occlusion
with a small change in the facial profile.
4,5
Camouflage treatment of a Class II division 1 mal-
occlusion with a large overjet is considered to be one
of the most difficult forms of orthodontic treatment
because of the difficulty in preventing anchorage loss.
The difficulties arise because methods of intra-oral
anchorage, such as transpalatal bars or Nance appli-
ances, are not completely stable and, in some cir-
cumstances, cannot support the forces used to move
the teeth.
6
Additional extra-oral anchorage in the
form of headgear can provide stable anchorage, but
this form of anchorage depends on the patients
compliance.
79
To provide stationary anchorage that will allow
orthodontic treatment to proceed rapidly with a pre-
dictable result, osseous implants of various materials
and designs have been developed.
1013
An osseointe-
grated implant placed in the palate is an effective
form of intra-oral orthodontic anchorage for Class II
division 1 treatment.
14
A number of other designs of
orthodontic implants can be used to provide station-
ary anchorage for Class II treatment such as: mini-
screws,
12,13,15
miniplates with tube,
16
the zygomatic
anchorage system,
17
and microscrews.
18,19
Sukawara introduced a skeletal anchorage system
(SAS) using bone-plates and screws as orthodontic
anchorage.
20
Bone-plates fixed with screws can be
Australian Orthodontic Journal Volume 23 No. 1 May 2007 65
Treatment of skeletal 2 malocclusion using
bone-plate anchorage. A case report
Kallaya Kraikosol,
*
Charunee Rattanayatikul,
*
Keith Godfrey,
*
Departments of Orthodontics
*
and Oral Surgery,
Faculty of Dentistry, Khon Kaen University, Khon Kaen, 40002 Thailand
Objective: To report the treatment of a severe Class II division 1 malocclusion using bone-plate anchorage.
Methods: A 12 year-old Thai girl presented with a skeletal 2, Class II division 1 malocclusion. Following extraction of the
maxillary first premolars and mandibular second premolars, the maxillary anterior teeth were retracted and the mandibular
posterior teeth moved mesially. A miniplate with screws, placed in each zygomatic buttress, was used as absolute anchorage
for coil springs to retract the maxillary anterior six teeth.
Results: After treatment, the patient presented with a normal overjet and overbite, a dental Class I relationship bilaterally and an
improved facial profile.
(Aust Orthod J 2007; 23: 6571)
Received for publication: February 2006
Accepted: February 2007
and Theparith Vattraphudej
placed at a safe distance from the roots of teeth, in
areas such as the midpalate or zygomatic buttress,
where they are easily placed and removed. This type
of implant is considered to provide absolute skeletal
anchorage for tooth movement.
2123
This report will
describe the treatment of a severe Class II division 1
malocclusion using bone-plate anchorage.
Case report
A 12 year-old Thai girl with a Class II division 1 mal-
occlusion on a skeletal 2 base and a convex profile was
accepted for treatment in the orthodontic depart-
ment, Khon Kaen University. When she first
presented the patient complained of proclined upper
anterior teeth. It was felt that the malocclusion and
KRAIKOSOL ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 66
Figure 1. Initial study models.
Table I. The summary of the changes between the pretreatment and post-treatment conditions.
Area consideration Pretreatment Post-treatment
Skeleton Antero-posterior Skeletal 2 Skeletal 2
Vertical Skeletal hyperdivergence Skeletal hyperdivergence
Dental arch Alignment Malaligned, mild crowding, large overjet Well-aligned, no crowding, normal overjet
Arch form Tapered maxillary and mandible arch Parabolic maxillary and mandible arch
Dental Canine relation Class II on both sides Class I on both sides
Molar relation Class II on right side Class I on both sides
Class I on left side
Overjet 6.5 mm 1.5 mm
Overbite 3.0 mm 1.5 mm
Maxillary incisor Proclined and protruded Retroclined and retruded
Mandibular incisor Proclined and protruded Normal inclination and position
Midline Mandibular dental midline Maxillary and mandibular dental midlines
shifted to right 2 mm. are at the centre line.
Tooth number Remained primary maxillary second molars. Balanced
Soft tissue Upper lip Protrusion (moderate) Protrusion (mild)
Lower lip Protrusion (moderate) Normal position
Face Frontal Symmetry Symmetry
Profile Convex Normal
her facial appearance had contributed to her lack of
self-confidence. She had good general health and was
a sporadic attendee for dental check-ups.
The patients facial profile was convex, with slightly
long lower anterior facial height relative to the upper
anterior facial height. She had an acute nasolabial
angle and her lips were incompetent at rest and pro-
trusive with slightly everted upper lip. The smile line
was normal and 100 per cent of upper incisors were
displayed. Her chin lacked prominence and the chin
button was on the facial midline.
The patients main problem was maxillary incisor
proclination. She had a late mixed dentition with
maxillary second primary molars about to exfoliate.
There was a Class II end-on molar occlusion on the
right side, Class I molar on the left, and Class II
canine relationships on both sides, and an overjet
of 6.5 mm. The mandibular incisors were also
proclined. She had 3.0 mm of positive overbite.
The upper dental midline coincided with the
midsagittal plane, while the lower dental midline
deviated 2.0 mm to the right. In a functional
evaluation, there were no CR CO discrepancies and
no signs or symptoms of temporomandibular
dysfunction.
There was 3 mm crowding in the maxillary anterior
segment and 2 mm crowding in the mandibular ante-
rior segment. Boltons ratios indicated that there was
no tooth-size discrepancy. The initial study models
are shown in Figure 1.
Radiographic and cephalometric findings
The pretreatment radiographs are shown in Figure 2.
The panoramic radiograph showed the late mixed
dentition with all teeth present including developing
third molars. No significant abnormalities were
detected. The cephalometric analysis indicated a
skeletal 2 relationship. The maxillary and mandibular
TREATMENT OF SKELETAL 2 MALOCCLUSION WITH BONE- PLATE AND SCREW ANCHORAGE
Australian Orthodontic Journal Volume 23 No. 1 May 2007 67
Figure 2. Initial panoramic radiograph and lateral cephalometric radiograph with tracing.
KRAIKOSOL ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 68
Figure 3. Panoramic radiograph and lateral cephalometric radiograph show implanting bone-plates with
screws and orthodontic forces application by NiTi coil springs after anterior retraction for one month.
incisors were proclined and protruded. The upper
and lower lips were protrusive. Pretreatment cephalo-
metric findings are summarised in Table I.
Diagnosis
The diagnosis for this case was Class II division I on
a skeletal 2 base with a convex profile. The clinical
problems were: a skeletal 2 pattern with slightly prog-
nathic maxilla and orthognathic mandible; Class II
molar and canine relationships; a convex profile with
protrusive lips; severely proclined and protruded
maxillary and mandibular incisors; an overjet of 6.5
mm; the lower dental midline was 2 mm to the right;
there was 3 mm crowding in upper arch and 2 mm
crowding in lower arch.
Treatment plan
The objectives in treating the malocclusion were to
retract the maxillary anterior teeth, to achieve a
normal overjet and overbite, to obtain a Class I
canine relationship, and to move the mandibular
posterior teeth forwards into Class I occlusion and
to improve the facial and lip profiles. The initial
treatment plan involved extraction of both maxillary
first premolars and both mandibular second premo-
lars and use of a transpalatal bar and headgear for
control of anchorage.
Treatment
Both arches were banded and bonded with 0.022 x
0.028 inch preadjusted fixed appliances for initial
leveling and aligning on 0.014 inch, 0.016 inch, and
0.018 inch stainless steel arch wires successively. To
relieve the anterior protrusion the upper canines were
retracted on a 0.016 x 0.022 inch stainless steel arch-
wire by power chain between the canines and first
molars. During treatment it became apparent that the
transpalatal bar and headgear were not going to pro-
vide sufficient anchorage to complete treatment.
After re-evaluation, the decision was taken to use
bone-plates with screws as absolute anchorage to
Figure 4. Facial photograph show slightly improvement in facial profile after
anterior retraction for one month.
support coil springs to retract the maxillary anterior
teeth.
Bone-plates and screws were placed at the inferior
borders of the zygomatico-maxillary buttresses. A
0.019 x 0.025 inch stainless steel arch wire was
inserted and nickel titanium (NiTi) closed coil
springs with a force of 200 g were applied between
the maxillary implants and the hooks on the canine
brackets (Figure 3). Slight improvement in facial
profile after one month is shown in Figure 4.
Some inflammation and infection occurred around
the implants because they were placed too high in the
vestibule. The infection was relieved by systemic
antibiotic medication and oral hygiene instruction.
Most profile change occurred during the first 10
months of treatment using the bone-plate anchorage.
The results after two years and two months treatment
are shown in Figure 5. There was a marked improve-
ment in the patients profile and the occlusion.Wrap-
around retainers were used in both arches for retention.
The pre- and post-treatment cephalometric superim-
positions on the S-N plane are shown in Figure 6.
During treatment the maxilla moved forward and the
mandible moved downward. In addition, upper and
lower lips moved backward and soft tissue chin
downward, all leading to a significantly improved
facial profile. Superimposition on the best fit of max-
illa and on stable structures of the mandible revealed
that the maxillary anterior teeth had tipped palatally,
the mandibular anterior teeth had tipped lingually
and the mandibular molars moved 3 mm mesially
into a Class I molar relationship. The pre- and post-
treatment cephalometric changes are summarised in
Table I.
Discussion
A Class II division 1 malocclusion on a skeletal 2
base is of special interest in orthodontics. There are
several different ways of correcting this malocclusion
and each depends on a number of factors. As a start-
ing point, the envelope of discrepancy should be
TREATMENT OF SKELETAL 2 MALOCCLUSION WITH BONE- PLATE AND SCREW ANCHORAGE
Australian Orthodontic Journal Volume 23 No. 1 May 2007 69
Figure 5. Final facial photograph, lateral cephalometric radiograph with tracing, and intra-oral photographs show improvement in facial profile and dental
relationship.
considered to decide if the deformity can be treated
by orthodontics alone or by combined orthodontics
and orthognathic surgery.
1
For a patient whose dis-
crepancy falls at the edge of the envelope, factors to
be considered are: the aesthetic impact of treatment,
the patients preferences, the cost of treatment, likely
complications, the length of treatment time and the
mechanics that can be used.
In the majority of cases it may be possible to achieve
acceptable results by orthodontic treatment alone,
but this patient had a severe maxillary protrusion and
anchorage loss that required skeletal anchorage to
complete treatment. It was not a case of converting
to surgical correction. Apart from providing station-
ary anchorage, implants may simplify the treatment
mechanics, enable entire quadrants rather than indi-
vidual teeth to be moved, and reduce the duration of
treatment.
24
In this case, the skeletal anchorage
system (SAS) using surgical miniplates was chosen
because the plates can be placed in safe sites. While
the surgical procedure to place the SAS is more exten-
sive than that used to insert microscrew implants, the
SAS can support higher forces than those employed
with microscrews.
1922
A NiTi coil spring was selected for force application
because it offered a continuous, controlled force. The
most outstanding results were the large retraction of
maxillary anterior teeth without mesial movement
of maxillary posterior teeth, which are the anchor
units in conventional orthodontic treatment.
However, it must be noted that the improvement in
the overjet was due to retroclination of the maxillary
incisors. In retrospect, more attention could have
been paid to bodily retraction of the incisors. The fact
that this did not happen is attributed to the sig-
nificant play between the 0.022 inch pre-adjusted
bracket slots and the 0.019 x 0.025 inch finishing
arches. Maintaining the position of the maxillary
incisors will depend not only on the wraparound
retainer, but also on an altered lower lip posture.
The mild mucosal inflammation around the screw
was traced to irritation from the ligature wire between
the implants and NiTi springs. To prevent any
inflammation in this area the patient should be
instructed to keep the area around the implants clean
with meticulous oral hygiene.
16
In the present case,
systemic antibiotics were used to deal with the local
infection that occurred around the implants and not
continued as a prophylactic measure.
Conclusion
The skeletal anchorage system provides stationary
anchorage that, under normal circumstances, will
allow the anterior teeth to be retracted bodily. In this
case, conventional intra-oral anchorage provided by a
transpalatal bar and extra-oral traction proved
unreliable, with the result that anchorage was lost and
the treatment could not be completed without
KRAIKOSOL ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 70
Figure 6. Cephalometric superimposition pretreatment (solid line) and post-treatment (dotted line).
further extractions or surgery. However, maximum
retraction of maxillary anterior teeth and improve-
ment in the facial profile were achieved without
further loss of anchorage with the bone-plates and
screws as anchorage.
Corresponding author
Dr Kallaya Kraikosol
Faculty of Dentistry
Khon Kaen University
Khon Kaen 40002, Thailand
Email: puffypui@yahoo.com
References
1. Proffit WR. Malocclusion and dentofacial deformity in con-
temporary society. In: Proffit WR, Fields HW, 3rd ed.
Contemporary orthodontics. St. Louis: C.V. Mosby
Company; 2000:122.
2. Norton LA, Melsen B. Functional appliances. In: Melsen B,
ed. Current controversies in orthodontics. Chicago:
Quintessence Publishing Co.;1991:10330.
3. Teuscher U. A growth-related concept for skeletal Class II
treatment. Am J Orthod 1978;74:25875.
4. Mihalik CA, Proffit WR, Phillips C. Long-term follow-up of
Class II adults treated with orthodontic camouflage: a com-
parison with orthognathic surgery outcomes. Am J Orthod
Dentofac Orthop 2003;123:26678.
5. Proffit WR, Phillips C, Douvartzidis N. A comparison of
outcomes of orthodontic and surgical-orthodontic treatment
of Class II malocclusion in adults. Am J Orthod Dentofacial
Orthop 1992;101:55665.
6. Melsen B, Bosch C. Different approaches to anchorage:
a survey and evaluation. Angle Orthod 1997;67:2330.
7. American Association of Orthodontists. Special bulletin on
extra-oral appliance care. Am J Orthod 1975;68: 457.
8. Hubbard GW, Nanda RS, Currier GF. A cephalometric eval-
uation of nonextraction cervical headgear treatment in Class
II malocclusions. Angle Orthod 1994;64:35970.
9. Kuhn RJ. Control of anterior vertical dimension and proper
selection of extra-oral anchorage. Angle Orthod 1968;38:
34050.
10. Creekmore TD, Eklund MK. The possibility of skeletal
anchorage. J Clin Orthod 1983;17:2669.
11. Block MS, Hoffman DR. A new device for absolute anchor-
age for orthodontics. Am J Orthod Dentofacial Orthop
1995;107:2518.
12. Kanomi R. Mini-implant for orthodontic anchorage. J Clin
Orthod 1997;31:7637.
13. Costa A, Raffini M, Melsen B. Miniscrews as orthodontic
anchorage: A preliminary report. Int J Adult Orthodon
Orthognath Surg 1998;13:2019.
14. Nojima K, Komatsu K, Isshiki Y, Ikumoto H, Hanai J, Saito
C. The use of an osseointegrated implant for orthodontic
anchorage to a Class II Div 1 malocclusion. Bull Tokyo Dent
Coll 2001;42:17783.
15. Paik CH, Woo YJ, Boyd RL. Treatment of an adult patient
with vertical maxillary excess using miniscrew fixation. J
Clin Orthod 2003;37:4238.
16. Chung KR, Kim YS, Linton JL, Lee YJ. The miniplate with
tube for skeletal anchorage. J Clin Orthod 2002;36:40712.
17. De Clerck H, Geerinckx V, Siciliano S. The zygoma anchor-
age system. J Clin Orthod 2002;36:4559.
18. Park HS. The skeletal cortical anchorage using titanium
microscrew implants. Korean J Ortho 1999;29:699705.
19. Bae SM, Park HS, Kyung HM, Kwon OW, Sung JH. Clinical
application of micro-implant anchorage. J Clin Orthod
2002;36:298302.
20. Sugawara J. Interviews Dr Junji Sugawara on the skeletal
anchorage system. J Clin Orthod 2001; 35:68996.
21. Umemori M, Sugawara J, Mitani H, Nagasaka H, Kawamura
H. Skeletal anchorage system for open-bite correction. Am J
Orthod Dentofacial Orthop 1999;115:16674.
22. Sugawara J, Baik UB, Umemori M. Treatment and post-
treatment dentoalveloar changes following intrusion of
mandibular molars with application of a skeletal anchorage
system (SAS) for open bite correction. Int J Adult Orthodon
Orthognath Surg 2002;17:24353.
23. Sugawara J, Daimaruya T, Umemori M, Nagasaka H,
Takahashi I, Kawamura H, Mitani H. Distal movement of
mandibular molars in adult patients with the skeletal
anchorage system. Am J Orthod Dentofac Orthop 2004;
125:1308.
24. Park HS, Bae SM, Kyung HM, Sung JH. Simultaneous inci-
sor retraction and distal molar movement with microimplant
anchorage. World J Orthod 2004;5:16471.
TREATMENT OF SKELETAL 2 MALOCCLUSION WITH BONE- PLATE AND SCREW ANCHORAGE
Australian Orthodontic Journal Volume 23 No. 1 May 2007 71
Introduction
Some orthodontists prefer to use sliding mechanics
for space closure because the retraction force can be
quantified. Sliding mechanics do, however, have to
overcome the friction between the archwire and
brackets, which may slow the rate of space closure
and contribute to loss of anchorage. In spite of these
disadvantages, sliding mechanics are an important
part of several treatment methods.
1,2
While the char-
acter of tooth movement (i.e. tipping versus bodily
movement) and the magnitude of a force are usually
mentioned, the frequency of activation is rarely
considered. The latter is an important point because
fewer visits may be required if the patient can activate
the appliance. Also there is convincing evidence that
intermittent forces are more effective than continuous
forces in promoting orthodontic tooth movement.
35
Recently, Schuetz introduced a screw for space
closure called the Hycon device (Adenta, Ivyland, Pa,
USA) for space closure. It was specifically introduced
for cases where space closure is problematic because
of increased friction, increased bone density or
narrowing of the alveolar process in an extraction
site.
1,6
The device consists of a bolt and nut assembly.
The nut is soldered to a 0.021 inch x 0.025 archwire
inserted into the first molar tubes, and the softened
ends of the archwire are turned down distally. The
neck of the bolt is then tied to the anterior tooth seg-
ment with a stainless steel wire ligature. The patient
is instructed to turn the bolt one full turn twice a
week.
6
The activated bolt, which delivers a
relatively high force over a short distance (0.35 mm),
results in rapid space closure and, it is claimed, a
favourable remodeling response.
6
Friction between
the wire and bracket/tube is thought to be high. A
0.021 inch x 0.025 inch archwire is used to prevent
deflection of archwire under load.
Case report
A 16 year-old woman presented with Class I skeletal
relationship and proclined upper and lower anterior
teeth. She was mesofacial with a convex profile, had
incompetent and protrusive lips, a short upper lip
and an acute nasolabial angle. She had a full comple-
ment of teeth, except the third molars. She had Class
I molar and canine relationships. There was 2 mm
crowding in the upper arch and 4 mm crowding in
the lower arch (Table I).
Australian Orthodontic Journal Volume 23 No. 1 May 2007 72
Space closure using the Hycon device.
A case report
Viral A. Kachiwala, Anmol S. Kalha and J. Vigneshwaran
College of Dental Sciences, Davangere, Karnataka, India
Background: Space closure can be a difficult and uncomfortable procedure. Appliances able to be activated by the patient
may reduce the number of visits for adjustment.
Objective: To describe the closure of spaces with the Hycon device, an intra-oral screw that can be activated by the patient.
Method: Sliding mechanics were used to retract the upper and lower anterior teeth following extraction of the first premolars in
a patient with bimaxillary protrusion. The active force for retraction was derived from the Hycon device
activated twice a week by the patient.
Results: The rate of space closure achieved was of the order of 1.9 mm/month. The extraction spaces were closed by distal
movement of the anterior teeth and mesial movement of the posterior teeth.
Conclusion: The Hycon device proved to be an effective means of retracting the anterior teeth and protracting the posterior
teeth. Because the device can be activated by the patient fewer visits for adjustment may be required.
(Aust Orthod J 2007; 23: 7275)
Received for publication: June 2006
Accepted: April 2007
SPACE CLOSURE USING HYCON DEVICE
Australian Orthodontic Journal Volume 23 No. 1 May 2007 73
The treatment objectives for the patient included
retroclination of the upper and lower anterior teeth,
resolution of the crowding in lower arch, mainte-
nance of the Class I canine and molar relationships
and a pleasing smile. The upper and lower first bicus-
pids were extracted and 0.022 inch slot MBT brack-
ets bonded in both arches. Leveling and alignment
was carried out with 0.016 inch heat activated NiTi
archwires followed by 0.019 inch x 0.025 inch heat
activated NiTi archwires. When the arches had been
leveled and aligned 0.021 inch x 0.025 inch stainless
steel archwires with passive tie backs were used for
four weeks. The upper and lower anterior teeth were
retracted en masse with a Hycon screw activated by
the patient twice a week (Figure 1). After space clo-
sure, the brackets were repositioned to parallel the
roots of the teeth. Upper and lower Hawley retainers
were fitted at the completion of treatment.
Table I. Cephalometric findings.
Measurements Mean (SD) Pretreatment Post-treatment
Skeletal
1 SNA () 82 83 82
2 SNB () 80 79 79
3 ANB () 2 4 3
4 N perpendicular-B (mm) 0 (2.0) -2 -1
5 N perpendicular-Pog (mm) 0 to -4 -3 -6
6 GoGn/SN () 32 31 32
7 Inclination () 85 85 86
8 LAFH (mm) 66.1 (4.1) 67 69
9 Maxillary length (mm) 92.7 (2.3) 90 89
10 Mandibular length (mm) 120 (3.4) 111 113
11 Y axis () 66 67 67
12 Facial axis angle () 0 0 0
13 Sum of posterior angles () 396 (6.0) 392 394
Dental
14 U1/NA angle () 22 30 28
15 U1-NA (mm) 4 8 6
16 U1/SN angle () 102 113 110
17 L1/NB angle () 25 35 30
18 L1-NB (mm) 4 10 7
19 IMPA () 90 104 97
20 Interincisal angle () 130 114 124
Soft tissue
21 S line-U lip (mm) -2- 0 -1
22 S line-L lip (mm) 0 -3 -2
23 Nasolabial angle () 90-110 69 98
Figure 1. Intra-oral view of the Hycon device.
KACHIWALA ET AL
Australian Orthodontic Journal Volume 23 No. 1 May 2007 74
Discussion
The concept of using a light continuous force in
orthodontic tooth movement has been challenged by
recent developments in the fields of cell biology and
physiology. Interrupted forces, as provided by the
Hycon device, that do not exceed the biologic width
of the periodontal ligament are thought to maintain
the vascularity of the ligament, resulting in improved
bone turnover and more efficient tooth movement.
46
Maintenance of adequate vascularity of the perio-
dontal ligament has been reported to be a rate-limiting
step in orthodontic tooth movement.
7
The Hycon
screw was used in the present case because it delivered
an interrupted force over a distance that did not
exceed the estimated width of a normal periodontal
ligament. The patient experienced minimal discom-
fort after each activation.
6
After leveling and alignment the 4 mm of space in the
upper arch and 3 mm of space in the lower arch were
closed by en masse retraction of the upper and lower
anterior teeth using the Hycon device. As recom-
mended by the manufacturer we advised the patient
to turn the screw two full turns every week. Space clo-
sure was completed in nine weeks at a mean rate of
1.9 mm/month, which is faster than conventional
methods of space closure.
8
The treatment changes are
shown in Figures 24.
Retracting the teeth on a 0.021 inch x 0.025 inch
stainless steel archwire controlled the torque and
avoided deepening the bite. Friction was of little con-
cern as the activated screw applied about 410 g of
force.
6
Typically, the teeth bordering the extraction
spaces move towards each other. The width of a
healthy periodontal ligament is 0.25 mm
9
and as one
full turn of the screw produces 0.35 mm of activa-
tion, the activation for each tooth is about 0.175 mm,
which is less than the estimated periodontal space.
The relatively short distance of activation is thought
to stimulate the tissue response and ensure a con-
tinuous blood supply to the periodontal ligament
and the surrounding structures.
6
Forces that are cyclic
Figure 2. Superimposed cephalometric tracings. Figure 3. Superimposition of maxilla at ANS. Figure 4. Superimposition of mandible on internal
structures.
Table II. Pre- and post-treatment PAR findings.
Region Pretreatment Post-treatment
Upper right segment 3 3
Upper anterior segment 10 0
Upper left segment 1 0
Lower right segment 2 0
Lower anterior segment 10 0
Lower left segment 2 1
Right buccal 0 0
Left buccal 0 0
Overjet and crossbite 3 0
Overbite and openbite 1 1
Centreline 0 0
Total 32 5
SPACE CLOSURE USING HYCON DEVICE
Australian Orthodontic Journal Volume 23 No. 1 May 2007 75
in nature are considered to evoke a better cellular
response that lead to an upregulation of various
cellular markers necessary for bone remodeling.
35
All the objectives of treatment were met at the end of
treatment and to audit the results achieved, a PAR
assessment was used (Table II).
10
The treated case fell
into the greatly improved category (84.3 per cent
improvement).
There were no accidental breakages during treatment
and the Hycon device remained firmly attached to
the archwire throughout treatment. Significant health
concerns can be excessive mobility of the teeth being
moved, loss of periodontal support, ulceration of the
buccal mucosa and accidental swallowing of the screw
by the patient. Of the 25 cases we have treated with
this device we have not encountered any of these
complications.
Conclusions
1. The Hycon device is an intra-oral closing screw
that can be activated by either the orthodontist or the
patient.
2. Space closure occurs by movement of teeth on
either side of the extraction site towards each other.
3. The appliance is indicated when spaces are
resistant to traditional methods of closure.
4. Further research on this appliance is required
to investigate its efficiency in different clinical
situations.
Corresponding author
Dr Viral A. Kachiwala
46/4, Devchaya Apartments, Haji Ali
Mumbai 400034, Maharashtra
India
Email: viral.kachiwala@gmail.com
Tel: +91 9819567816
References
1. McLaughlin RP, Bennett JC, Trevisi HJ. Systemized ortho-
dontic treatment mechanics. Mosby, Edinburgh, 2001.
2. Bennett JC, Mc Laughlin RP. Orthodontic treatment mech-
anics and the preadjusted appliance. Mosby, London, 1993.
3. Mao JJ, Nah HD. Growth and development: Hereditary and
mechanical modulations. Am J Orthod Dentofacial Orthop
2004;125:67689.
4. Lee KJ, Park YC, Yu HS, Choi SH, Yoo YJ. Effects of con-
tinuous and interrupted force on interleukin-1b and
prostaglandin E2 production in gingival crevicular fluid. Am
J Orthod Dentofacial Orthop 2004;125:16877.
5. Carano A, Siciliani G. Effects of continuous and intermit-
tent forces on human fibroblasts in vitro. Eur J Orthod
1996;18:1926.
6. McLaughlin RP, Kalha AS, Scheutz W. An alternative
method of space closure: the Hycon Device. J Clinical
Orthod 2005;39:47484.
7. Krishnan V, Davidovitch Z. Cellular, molecular, and tissue-
level reactions to orthodontic force. Am J Orthod
Dentofacial Orthop 2006;129:469.e132.
8. Dixon V, Read MJF, OBrien D, Worthington HV, Mandall
NA. A randomized controlled trial to compare three meth-
ods of orthodontic space closure. J Orthod 2002;29:316.
9. Lindhe J. Clinical periodontology and implant dentistry.
Munksgaard, Copenhagen, Denmark, 1998, 27.
10. Richmond S, Shaw WC, OBrien K, Buchanan IB, Jones R,
Stephens CD et al. The development of PAR Index: reliabil-
ity and validity. Eur J Orthod 1992,14:12539.
Australian Orthodontic Journal Volume 23 No. 1 May 2007 76
Editorial
The Australian Orthodontic Journal is proud to cele-
brate forty years of publication. In June 1967 the first
issue of the Journal was published with John Moffatt
as editor. Before the Journal appeared, members
activities and interests had been recorded in a series of
bulletins circulated to members, thus the actual
period of service to the profession is much longer than
40 years. Over the years there has been a shift in the
type of contribution: early issues of the Journal were
mainly reviews of clinical topics, occasional reprints of
articles from other orthodontic journals and a few
scientific studies whereas today most contributions are
scientific articles with occasional reviews and case
reports. Other changes have been to widen the scope
of the Letters section, introduce a Comment section
and electronic submission. The latter has speeded and
eased our handling of contributions.
We are greatly indebted to the Australian Society of
Orthodontists for its leadership, to previous editors
of the Journal and the many peer reviewers who vol-
unteered their services, for its success over the years.
The peer review process, used by many journals and
funding organisations, is an essential means of evalu-
ating information in a healthcare profession. By
donating their time our reviewers have enhanced the
quality of the Journal and contributed to improve-
ments in the care of our patients. I would also like to
thank my predecessors: John Moffatt, Terry Freer,
Darryle Bowden, Barry Mollenhauer and Brian Lee,
who set the high standards that have guided me.
In this issue of the Journal we have two articles by
Ling, Ho, Kravchuk and Olive comparing the
periodontal, pulpal and aesthetic outcomes of surgical
and non-surgical treatment of palatally impacted
canines. According to this team, impacted canines
treated by both methods had a higher prevalence of
pulpal changes compared with control canines, and
both methods of treatment were followed by minor
periodontal changes.
The article by Kandasamy, Goonewardene and
Tennant investigates changes in the heights of the
interdental papillae following orthodontic alignment.
They suggest dark triangles, which can mar otherwise
excellent results, are likely to develop following certain
types of tooth movement, particularly in older
patients.
Bonded lingual retainers, in one form or another, are
used by many orthodontists. According to Cerny they
are a reliable form of retention and take up little chair-
side time if repairs are necessary. He incorporates
small loops opposite the embrasures in the upper
retainers, which aid flossing and access for restorative
procedures. Somewhat predictably, they were more
likely to fail in males and fracture behind the central
incisors.
Higher percentages of sella turcica bridges were found
in Class III dental and Class 3 skeletal malocclusions
by Abdel-Kader. Because sellas of unusual size or
shape may be associated with some types of cranio-
facial malformation we should pay more attention to
the morphology of sella on our radiographs.
In another paper from their laboratory, Jones and
Amoah compare the static frictional resistances of
three ceramic brackets with different slot finishes. The
authors report that glazed slot brackets have some
advantages at angulations below the critical angle for
binding, and have an important recommendation
when using ceramic brackets with conventional and
glazed slots.
Also on the subject of gingival changes Closs, Squeff,
Raveli and Rosing describe the gingival margin
changes accompanying changes in lower intercanine
widths. A higher percentage of subjects had gingival
recession in the group with increased intercanine
widths, but it was not statistically significant. It appears
gingival margin changes are more-or-less independent
of changes in the lower intercanine width.
Topacal C-5, a milk protein product developed in
Australia, will protect teeth from demineralisation in
vitro, and according to Nasab, Kajan and Balalaie,
may reduce enamel demineralisation in patients with
poor oral hygiene. But it should not be used by
patients allergic to milk products.
In their investigation of the impact of orthodontic
treatment on normative need Bernab, Borges-Yez
Forty years of publication
Australian Orthodontic Journal Volume 23 No. 1 May 2007
EDITORIAL
77
and Flores-Mir report that similar levels of treatment
need were found in treated and untreated groups.
This article provides thoughtful reading for ortho-
dontists concerned about the long-term impact of
orthodontic treatment.
A timely review of three-dimensional computed cranio-
facial tomography is provided by Chan, Woods and
Stella. This is a rapidly developing, and important,
field for orthodontists and this review gives an excel-
lent overview of the potential uses and limitations of
3D-CT.
We are also fortunate to have two case reports in this
issue. The first by Kraikosol, Rattanayatikul, Godfrey
and Vattraraphoudet is a detailed report of a patient
with a severe Class II division 1 malocclusion treated
with the aid of bone-plate anchorage. In this case
bone plate anchorage provided the anchorage to com-
plete treatment after other methods had failed. The
second case by Kachiwala, Kalha and Vigneshwaran
uses an intra-oral screw activated by the patient to
retract the anterior teeth and protract the posterior
teeth. According to the authors fewer visits for adjust-
ment may be required because the device can be
activated by the patient.
Finally, we seek your comments and contributions so
that we can continue to provide the best information
to the profession. I ask that you contact us with your
suggestions for further enhancing and improving the
quality of your journal.
Michael Harkness
Australian Orthodontic Journal Volume 23 No. 1 May 2007 78
Risk Management in Orthodontics:
Experts Guide to Malpractice
Thomas M. Graber,
Theodore Eliades and
Athanasios E. Athanasiou
Publisher: Quintessence
Price: UK78 (A$185.40)
ISBN: 0867154314
This readable, practical textbook is a high quality
production relevant to the clinical practice of ortho-
dontics. The text comprises 238 pages spread over 15
chapters, and is divided into two sections. Written by
a team of 21 specialists drawn from different countries
and representing different professional, academic and
research interests, it is tightly edited to produce a con-
sistent writing style. The first aim of this book is to
explore the pathology of various conditions that may
emanate from orthodontic treatment. The second aim
is to define the risk factors associated with ortho-
dontic treatment, so that they can be eliminated from
clinical practice.
The material in each chapter is presented concisely.
An adequate background of relevant scientific prin-
ciples, biology and research results support the view-
points presented. Clearly labelled diagrams, summary
tables, graphs and clinical photographs are of
uniformly high quality and are appropriate to the
accompanying text. All chapters are comprehensively
referenced with a reference summary at the end of
each chapter.
Chapter 1, written by the editors, outlines the wide
variety of risk factors relating to orthodontic treat-
ment. It also gives a framework for the following
chapters. Section 1 follows and consists of 10
chapters, all discussing topics related to iatrogenic
responses to orthodontic treatment. Enamel colour
alterations associated with orthodontics are briefly
discussed in Chapter 2. We are provided with an inter-
esting summary of colour science. Potential problems
related to the whitening of orthodontically treated
teeth due to residual adhesive on the tooth surface are
also covered. This information leads logically to the
next chapter which details the effects fixed ortho-
dontic treatment can have on enamel. The principles
of enamel bonding are revisited in some depth. Recent
literature comparing different bonding methods is
well summarised, as are different debonding tech-
niques, all accompanied by clear photographs and
diagrams. Potential bracket bonding and debonding
problems and other preventive methods aimed at
reducing enamel decalcification during treatment are
thoroughly outlined.
Chapter 4 is carefully crafted, and presents a con-
densed review of the literature on root resorption. It
also develops an argument supporting the hypothesis
of a biological predisposition to root resorption,
demonstrating occurrence of root resorption in indi-
viduals who have not received orthodontic treatment.
Mechanisms of root resorption, hormonal influences
and other factors influencing root resorption are
covered.
Chapter 5 summarises factors to consider in minimis-
ing orthodontically induced root resorption. Some of
the recommendations suggested here are not always
necessarily practical. For example, hereditary factors
can be difficult if not impossible to ascertain.
Additionally, the recommendation to routinely take
standard full mouth periapical radiographs pretreat-
ment and then six months into treatment is not
standard orthodontic clinical practice in Australia.
Nevertheless, arguments for such procedures are
made.
The effects of damage to the supporting tissues during
orthodontic treatment are comprehensively outlined
in Chapter 6. This is a particularly useful and readable
chapter, with excellent accompanying illustrations and
clinical photographs. It includes reproductions of
interesting histological sections. Results of long-term
clinical studies are shown and the chapter concludes
with a useful, if brief, discussion concerning the
potential problems with dental implants in adolescent
Book
Reviews
patients. Chapter 7 is a concise review of the release
of wear and corrosion products from orthodontic
alloys. Problems of research in this particular field are
discussed. Many orthodontists will find this review
strikes a thoughtful balance between recent dental
materials science and its practical application in
orthodontics. Chapter 8 questions if the clinical uses
of polymers are a danger. The use of polymers in
orthodontics is outlined, and the subjects of the
toxicity of polymers and other additives to ortho-
dontic products are described. The results shown
were sometimes inconclusive, but the information
challenges our daily use of materials with regard to
their potential toxicity to the patient.
More familiar territory is covered in the following
chapter, which has pain and patient discomfort in
orthodontics as its main theme. Pain control theories
are reviewed, as is pain resulting from orthodontic
treatment, and practical pain management methods
presented. Contradictory study results in this field are
discussed. The information presented in Chapter 10
includes a literature review and epidemiological
summary of temporomandibular joint disorders
(TMD). Diagnosis and management of these dis-
orders are discussed. Examination protocols are
outlined, as are current treatment guidelines.
Orthodontic treatment for the medically compro-
mised patient is the subject of the final chapter in this
first section. Examples of genetic and acquired con-
ditions are examined to illustrate overall management
principles. No one chapter can cover this extensive
subject thoroughly, however, this is a useful revision.
Section 2 of this text has just four chapters which col-
lectively deal with risk management and malpractice
relating to orthodontic statement. As the legal system
discussed is that of the USA, not all of this section is
relevant to Australian practice. In Chapter 12
Thomas Graber discusses risk management issues,
using actual cases in the USA as examples. Patient
consent issues are discussed, as are standards of
clinical records. Robert Vanarsdall in Chapter 13
writes on malpractice aspects relating to periodontal
disease. The subjects of plaque and other iatrogenic
factors are clearly outlined. Treatment regimes, diag-
nostic hints and management protocols make valu-
able reading. The final two chapters, based on actual
malpractice cases, are written with the United States
legal system in mind, but still contain practical infor-
mation. They summarise the important information
presented in the preceding chapters. The 10 page
appendix then presents useful draft medical and
dental history forms, as well as a draft patient consent
form, courtesy of the American Association of
Orthodontists.
This textbook is so broad in its scope it precludes full
discussion on every topic covered, but it does collate
relevant clinical and theoretical information in a
concise and reader friendly format. It can be con-
fidently recommended as a valuable addition to any
orthodontic library.
Peter Synnott
Color Atlas of Dental Hygiene
Periodontology
Herbert F. Wolf and
Thomas M. Hassell
Publisher: Thieme
Price: Soft cover US$69.95
(A$84.80)
ISBN: 9781588904409 /
7983131417619
This new book on periodontology targets dental
hygienists, academics in dental hygiene education
and dental hygiene students. The authors main
intention in writing the book is to provide current
up-to-date scientific and clinical information and to
integrate this information into clinical practice. The
book delivers on its promise as a colour atlas. It is
packed with excellent photographs and illustrations,
which support the well-written and easy-to-read text.
Fundamental concepts as well as current concepts are
presented, which provide the reader with a broad per-
spective on the current issues in periodontology. The
chapter headings include etiology, pathogenesis, oral
pathological changes in the gingiva and perio-
dontium, oral manifestations of HIV disease and
treatment, gingival recession, new diagnostic tests,
phase 1 therapy (motivation, oral hygiene, closed
non-surgical periodontal treatment, full mouth
therapy), pharmacologic strategies for periodontitis,
Australian Orthodontic Journal Volume 23 No. 1 May 2007
BOOK REVIEWS
79
phase 2 therapy (summary of surgical treatment),
phase III therapy (periodontal maintenance), perio-
dontal wound healing and periodontal diseases in the
elderly. The chapters are easy to understand and are
sufficiently comprehensive for dental hygienists and
clinicians other than periodontists who would like a
pictorial update on periodontology.
There are a number of chapters that may be of inter-
est to clinicians providing orthodontic treatment.
The chapter on oral pathological alterations describes
the diseases likely to be encountered during ortho-
dontic treatment, such as phenytoin-induced gingival
overgrowth, puberty gingivitis, medicament-elicited
hyperplasia and diabetes, to name just a few. A con-
cise summary of the disease followed by recommen-
dations for therapy are presented. The phases of
periodontal therapy are well-described. Of impor-
tance to orthodontic patients with periodontal dis-
ease is phase 3 therapy. This phase, which covers
periodontal maintenance therapy, determines the
long-term success of periodontal treatment, which
can impact upon the successful completion of ortho-
dontic treatment. Practical guidelines and continuous
risk assessment are discussed by the authors.
The chapter on dental implants questions the appro-
priateness of natural teeth or dental implants for the
treated periodontitis patient, and provides an
overview of some of the issues involved in the
decision-making process. Augmentation techniques
are also described in this chapter. The chapter on
geriatric periodontology provides a basic overview of
the age-related changes in the periodontium and its
influence on treatment planning. Within this age
group, modified concepts of treatment are presented.
As advances in periodontology have accelerated in
the last decade, the book can be recommended to
practicing orthodontists who wish to update their
scientific and clinical knowledge in periodontology. It
is, however, not sufficiently detailed to be used on its
own if in-depth knowledge of the topic is required.
The book provides an informative reference source
for practices that employ dental hygienists.
Christopher T.C. Ho
BOOK REVIEWS
Australian Orthodontic Journal Volume 23 No. 1 May 2007 80
Australian Orthodontic Journal Volume 23 No. 1 May 2007 81
TMD and occlusion Part 1. Damned if we do?
Occlusion: the interface between dentistry
and orthodontics
F. Luther
This is the first of two online articles that reviews the
relationship between dental occlusion and TMD.
The author scoured the electronic databases of
Medline and the Cochrane Database of Systematic
Reviews, to produce the first article which reviews
how occlusion, facial growth, TM disc position, mal-
occlusion and orthodontic treatment may relate to
TMD. It was found that the literature contains articles
supporting and also denying the contribution of all
examined factors in TMD due to the flawed nature of
the reported research. This was disconcerting and the
author was at pains to point out that, to alleviate
the problem, studies should be prospective, be under-
taken by clinicians using a reproducible and validated
index, be undertaken by clinicians blind to the groups
to which the subjects belong, have patients randomly
assigned to test and control groups, be appropriately
powered and include patients of similar backgrounds
with similar malocclusions with comparison of appro-
priate controls. The article concluded that there was
no meaningful data and insight as to whether the
researched factors played a role in TMD. The debate
and argument over TMD will continue!
British Dental Journal
online resource
2007; 200: E2
TMD and Occlusion Part II. Damned if we
dont! Functional occlusal problems:
TMD epidemiology in a wider context
F. Luther
The second of two articles on factors related to
TMD explores whether functional occlusal problems
have an effect. Electronic databases were searched for
references to occlusal interference and bruxism in the
possible causation of TMD.
The author found no meaningful evidence to suggest
that functional occlusal factors were involved in TMD
and, in fact, that studies involving the assumption that
orthodontic treatment causes TMD have restricted
more useful studies assessing aetiology. The review
revealed that multiple TMD treatment interventions
have the same or similar outcomes to no treatment
intervention indicating that clinicians should use a
low tech approach.
British Dental Journal
online resource
2007; 202: E3
Bacteraemia following debanding and gold
chain adjustment
V.S. Lucas, A. Kyriazidou, M. Gelbier and G.J. Roberts
At a time when antibiotic prophylaxis is being
reviewed in relation to infective endocarditis, Lucas et
al. have re-examined the likelihood and extent of a
bacteraemia following debanding and gold chain
adjustment. Ethics approval was granted for the sam-
pling of blood from patients under 16 years of age
who were to undergo either of the above procedures.
Forty-nine patients of which 25 were males and 24
were females were included in the study. A cannula
was inserted into an antecubital fossa and 6 ml of
blood withdrawn before and 30 sec after an upper
deband or a gold chain adjustment.
Lysis filtration was used to determine the prevalence
of the bacteraemia, its intensity and the identity of
the organisms involved. Statistical tests were applied
to validate results. Results indicated that there was
no significant difference in the prevalence and inten-
sity of positive organism cultures before or after
debanding and gold chain adjustment.
The identity of the bacteria remained unremarkable
but consistent. The conclusion of the paper suggested
Recent
publications
Abstracts of recently published papers reviewed by the Assistant Editor, Craig Dreyer
RECENT PUBLICATIONS
Australian Orthodontic Journal Volume 23 No. 1 May 2007 82
that there was no difference in the prevalence and
intensity of bacteraemia between baseline levels and
following orthodontic procedures but it remains to be
seen as to how medical and legal guidelines might
consider these findings.
European Journal of Orthodontics
Advance Access Online Article
February 2007
Orthodontic root resorption of
endodontically treated teeth
T. Esteves, A.L. Ramos, C.M. Pereira and M.M. Hidalgo
Should orthodontists be concerned about a higher
possibility of root resorption involving teeth that have
been treated endodontically prior to orthodontic
therapy? Esteves et al. examined this question radio-
graphically in a group of patients who had an upper
central incisor previously root-filled. Of 2500 treat-
ment records examined, only 16 patients were
selected who fitted the category of having one
affected central incisor with the other incisor un-
affected (presumably) and therefore serving as a
control.
Standardised periapical radiographs were taken before
and after orthodontic treatment and, after being
scanned and enlarged, both incisors greatest length
was measured. Measurements were repeated one week
later, the means determined and Students t-test for
paired values applied at the 5 per cent probability
level. The results indicated that there was no statisti-
cal difference between apical root resorption in
untreated teeth and endodontically-treated teeth,
although the vital teeth showed a slightly greater
mean apical resorption. If the radiography and the
measurements are accepted, the results provide com-
fort for the orthodontic management of root-filled
teeth. However, a higher experimental number would
have provided greater confidence.
Journal of Endodontics
2007; 33: 119-22
The acceptability of variations in smile arc
and buccal corridor space
S. Parekh, H.W. Fields, F.M. Beck and S.M. Rosenstiel
The orthodontic world has considered that the dark
spaces in the buccal corridors of patients with less
than full smiles do not have the highest aesthetic
appeal. While there are reasons why the dark buccal
corridors might exist, the authors of the current
article sought to determine and evaluate an aesthetic
acceptability range. This they did by the comput-
erised generation of variations in buccal corridor
dimension (none, ideal, excessive) along with varia-
tions in smile arc (flat, ideal, excessive) from a single
frontal intra-oral image. A male image was created by
the addition of moustache hair and the 9 male and 9
female image combinations were posted on the inter-
net for layperson and orthodontist assessment. One
hundred and fifteen lay and 131 orthodontist replies
were received via an on-screen interactive sliding bar
similar to a Likert scale. The results indicated that
laypersons and orthodontists showed good reliability
when repeated images were assessed, but that there
was a broad range of acceptability. No significant dif-
ferences were detected in the assessment of the two
variables as laypersons and orthodontists considered
that patients with excessive buccal corridors were less
appealing than those with ideal or no buccal corri-
dors. However, patients with flat smile arcs were even
less acceptable and the combination of an excessive
buccal corridor coupled with a flat smile arc was the
least acceptable combination of all.
The study concluded that laypersons and ortho-
dontists had similar aesthetic preferences in relation
to buccal corridors and smile arcs. Flat smile arcs were
more detrimental to smile aesthetics compared with
increased buccal corridors. The study overlooked the
influences of facial type, arch form and malocclusion
on the parameters being assessed, but indicated that,
although attractiveness might be diminished by
variations in buccal corridors and smile arcs, the
result might be acceptable to the majority of people.
Orthodontics and Craniofacial Research
2007; 10: 1521
Oral appliances for treatment of sleep-
disordered breathing
V. Hoffstein
What is the best oral appliance to manage the
problems of sleep apnoea and/or snoring? This ques-
tion was examined by the author of this article by way
of a literature review. Eighty-nine publications exam-
ining sleep-disordered breathing were identified
between the years of 1982 and 2006. This seems a
small number as a PubMed search reveals consider-
ably more, which suggest that other criteria were used
in the authors search. The criteria for inclusion
Australian Orthodontic Journal Volume 23 No. 1 May 2007
RECENT PUBLICATIONS
83
was literature whose topics focussed on sleep apnoea,
the ability of oral appliances to reduce snoring, the
effect of oral appliances on daytime function, the
comparisons of oral appliances with other treatments,
appliance side effects, dental changes and long-term
compliance. The author encountered a lack of
standardisation between the articles which was not
unexpected, but nevertheless some consistent effects
were identified.
The article provided a brief historical outline and
described a range of oral appliances that had previ-
ously been used. By far the most common current
appliance was the mandibular advancement splint
whose mechanism of action was to clear the retro-
glossal and retropalatal areas in the pharynx which
indicates that diagnosis and case selection are
important features of sleep management.
The author reported that the success rate, defined as
the ability of the oral appliance to reduce
apnoea/hyponoea to an index less than 10 was 54 per
cent. The response rate, defined as a 50 per cent
decrease in the apnoea/hypopnoea index, was 21 per
cent. Snoring was reduced, but not entirely elimin-
ated in 45 per cent of wearers. A comparison with
other modes of treatment indicated that CPAP
offered by far the best outcome, but sufferers pre-
ferred to use an oral appliance. Daytime function was
improved and the Epworth Sleepiness Scale reduced
while the side effects of excessive salivation and tooth
discomfort were minor, but frequent. The article con-
cluded that an oral appliance of the mandibular
advancement type was valuable and beneficial in the
management of sleep-disordered breathing, but not as
beneficial as CPAP.
Sleep Breath
2007; 11: 122
Australian Orthodontic Journal Volume 23 No. 1 May 2007 84
Lo-Rider
The TP Orthodontics Lo-Rider
molar tube has a translucent
base, which according to the
manufacturer, allows for a
faster, full light cure and
a stronger bond than tradi-
tional metal-base molar
tubes. Other design features
to aid bonding include an
anatomical base that
conforms to the buccal sur-
face, large flats for secure holding and placement, and a
diamond-shaped indentation for precise positioning.
For further information contact TP Orthodontics
Website: www.tportho.com
NV hybrid bracket
The NV hybrid bracket from TP
Orthodontics has a clear con-
toured polymer mesh base to
allow light to fully penetrate and
a low profile for aesthetic
appeal and patient comfort.
Made from cobalt chromium
(CoCr), it is essentially nickel-
free and biocompatible for sen-
sitive patients, according to the
manufacturer.
For further information contact TP Orthodontics
Website: www.tportho.com
Equipment for sale
Medfin is offering a new free
service to healthcare practition-
ers to buy or sell secondhand
dental or medical equipment.
For further information contact
Medfin
Tel: Sonya Mears
(+61 2) 9462 2255
Website: www.medfin.com.au
Aquarium
Created for interactive patient
education and case presen-
tation, Aquarium is a communi-
cation tool utilising high-quality
3D graphics. According to the
manufacturer, it is designed to
demonstrate topics such as
diagnostic findings, corrective
procedures and appliance use.
For further information contact Dolphin Imaging &
Management Solutions
Tel: (+61 2) 4228 8530 Fax: (+61 2) 4229 7745
Website: www.dolphinimaging.com
Email: australia@dolphinimaging.com
InOvationC self-ligating ceramic
bracket system
The InOvationC self-ligating
ceramic bracket system com-
bines the aesthetics of a ceramic
bracket and the efficiency of a
self-ligating bracket, according
to the manufacturer. Fully com-
patible with the InOvationR
metal bracket system, it features
a polycrystalline ceramic bracket body with a rhodium coat-
ed Co-Cr clip and a mechanical lock base for bonding and
debonding. It is available in 0.018 inch and 0.022 inch slot
sizes.
For further information contact GAC Australia Pty Ltd
Tel: 1800 422 287
Email: info@gacaustralia.com.au
Distal bender
The distal bender is made from stainless steel and has an
angled tube on one end. The tube is used to bend the end of
the archwire distal to the buccal tube.
For further information contact Ortho Organisers
Tel: 1800 645 813 NZ 0800 440 883
Website: www.orthoorganizers.com.au
New
Products
CNA palatal arch
This new version of the
palatal bar is made
from CNA wire and is
shaped to the contours
of the palate. According
to the manufacturer, it
has more comfortable
low profile inserts that fit
easily into standard horizontal 0.036 inch lingual sheaths. It
is available in 2 mm increments from 28 to 42 mm.
For further information contact Ortho Organisers
Tel: 1800 645 813 NZ 0800 440 883
Website: www.orthoorganizers.com.au
Tomas screw
According to Dentaurum, the
Tomas concept creates an
effective, temporary anchor-
age point for the movement of
teeth. It is comfortable for the
patient to wear and easy for
the orthodontist to use.
For further information contact Dentaurum Australia
Tel: 1800 808 695
Mini-Mold bite opening kit
The Mini-Mold bite opening kit allows
the user to fill the mould, place on the
desired tooth and cure. According to
the manufacturer, a precise light-cured
resin appliance is cast in seconds. The
kit includes 5 bite ramp bonders, 5
molar pad bonders and 2 handles.
For further information contact
Ortho Organisers
Tel: 1800 645 813
NZ 0800 440 883
Website: www.orthoorganizers.com.au
NEW PRODUCTS
85 Australian Orthodontic Journal Volume 23 No. 1 May 2007
New products are presented as a service to our
readers, and in no way imply endorsement by the
Australian Orthodontic Journal
Australian Orthodontic Journal Volume 23 No. 1 2007 86
2007
June 1317
21st Congress of International Association of Paediatric Dentistry
IAPD, Hong Kong Convention and Exhibition Centre, Hong
Kong, China.
Website: www.iapd2007.com
June 1517
Bulgarian Orthodontic Society and Balkan Orthodontic
Symposium, Sofia, Bulgaria.
Email: cic@cic-pco.com
June 2024
83rd European Orthodontic Society Congress and Centenary
of the European Orthodontic Society, Philharmonic Hall, Berlin,
Germany. President: Professor Rainer-Reginald Miethke.
Website: www.eos2007.de
June 2525
4th World Edgewise Orthodontic Congress, Seoul, Korea.
Website: www.weoc2007.org
July 1217
2nd World Society of Lingual Orthodontics Meeting, Seoul, Korea.
Website: www.wslo2nd.info
August 1718
New Zealand Association of Orthodontists Symposium,
Queenstown, New Zealand.
Email: kierano@oneillortho.co.nz
September 2326
British Orthodontic Society Conference, Harrogate,
United Kingdom.
Website: www.new.bos.org.uk
September 2629
59th Annual Scientific Meeting of the Canadian Association of
Orthodontists, St Johns, Newfoundland, Canada.
Website: www.cao-aco.org
October 1213
University of Sydney Orthodontic Alumni Meeting, Swiss Grande
Resort, Bondi Beach, NSW, Australia. Keynote speaker: Professor
Birte Melsen. For further information contact Dr Kerry Lester.
Tel: (+61 2) 9389 0980
Email: drlester@o-3.com.au
October 2427
FDI Annual World Dental Congress, Dubai, United Arab Emirates.
Website: www.fdiworldental.org
November 1619
2nd International Conference on Evidence-based Advanced
Dentistry and Silver Jubilee Celebrations of the Faculty
of Dentistry, Hong Kong Academy of Medicine, Hong
Kong, China.
Website: dent25.khu.hk/congress
December 1416
Taiwan Association of Orthodontists 20th Annual Meeting and
6th Asian Implant Orthodontic Conference, Nan Shan Education
and Training Centre, Taichung, Taiwan.
Website: www.6thaioc.org.tw
2008
March 15
21st Australian Society of Orthodontists Congress, Gold Coast
Convention and Exhibition Centre, Queensland, Australia.
Email: info@aso08.com.au
Website: www.aso08.com.au
March 2830
6th Asian-Pacific Orthodontic Conference of the Asian-Pacific
Orthodontic Society, Shangri-la Hotel, Bangkok, Thailand.
Email: apoc2008@yahoo.com
Website: www.apoc2008.com
May 1620
American Association of Orthodontists Convention and 108th
AAO Annual Session, Denver, Colorado, USA.
June 1014
84th Congress of the European Orthodontic Society, Lisbon,
Portugal.
Website: www.eos2008.com
September 1113
Canadian Association of Orthodontists 60th Annual Scientific
Meeting, Winnipeg, Manitoba, Canada.
Website: www.cao-aco.org
September 2427
FDI Annual World Dental Congress, Stockholm, Sweden.
www.fdiworldental.org
Orthodontic
Calendar
2009
May 26
American Association of Orthodontists' Convention, Boston,
Massachusetts, USA.
June 1014
European Orthodontic Society Congress, Helsinki, Finland.
September 25
FDI Annual World Dental Congress, Singapore.
September 1012
Canadian Association of Orthodontists 61st Annual Scientific
Meeting, Kelowna, British Columbia, Canada.
2010
February 69
7th International Orthodontic Congress and the 4th Meeting of
the World Federation of Orthodontists, Sydney, Australia.
Website: www.wfosydney.com
CALENDAR
Australian Orthodontic Journal Volume 23 No.1 May 2007 87
Please direct all meeting queries and requests for inclusion in the calendar to Dr Tony Collett.
Tel: (+61 3) 9756 0519.
Email: tonycol@netspace.net.au
Swiss Grande Resort, Bondi Beach, NSW, Australia
12 13 October 2007
Keynote speaker Professor Birte Melsen
Adult orthodontics: interdisciplinary management and the compromised patient
Development of skeletal anchorage: current status
Periodontal considerations during orthodontic treatment
Current research at Aarhus.
Dr Birte Melsen is Professor and Head of the Department of Orthodontics, Royal Dental College, The
University of Aarhus, Denmark. She is an internationally recognised educator who has authored over 200
publications and is also involved in private practice.
Attendees wishing to stay at the venue are advised to contact the hotel directly as accommodation is limited
(call Cathy Soriano 02 9365 9722)
For further information contact:
Dr Kerry Lester, Secretary
University of Sydney Orthodontic Alumni
Tel: (+61 2) 9389 0980
Email: drlester@o-3.com.au
The University of Sydney
UNI VERSI T Y OF SYDNEY ORT HODONT I C AL UMNI
You might also like
- Ganapati UpanishadDocument4 pagesGanapati UpanishadNeha SharmaNo ratings yet
- 1.2 Points, Lines, PlanesDocument24 pages1.2 Points, Lines, PlanesDeo Di Lyn100% (1)
- Schmidt ArticleDocument7 pagesSchmidt ArticleJa MishicaNo ratings yet
- 10.2478 - Aoj 2007 0002Document8 pages10.2478 - Aoj 2007 0002H SabriNo ratings yet
- Periodontal Status of Buccally and Palatally Impacted PDFDocument5 pagesPeriodontal Status of Buccally and Palatally Impacted PDFDiana ElíasNo ratings yet
- Artigo BomDocument6 pagesArtigo BomCiro GassibeNo ratings yet
- Deguchi, 2011Document9 pagesDeguchi, 2011Laiana LarussaNo ratings yet
- Caninos RetenidosDocument9 pagesCaninos RetenidosNayely MiguelNo ratings yet
- A One Year Pilot Prospective Multicenter StudyDocument10 pagesA One Year Pilot Prospective Multicenter StudyEly Valentina Contreras ArceoNo ratings yet
- Newer Orthodontic Archwires Imparting EfDocument244 pagesNewer Orthodontic Archwires Imparting EfSelvaArockiamNo ratings yet
- Root Cementum Part 27Document11 pagesRoot Cementum Part 27Sumedha MalshetwarNo ratings yet
- Mandibular Incisor Alignment in Untreated Subjects Compared With Long-Term Changes After OrthodonticDocument9 pagesMandibular Incisor Alignment in Untreated Subjects Compared With Long-Term Changes After OrthodonticPAOLA IVETTE MARTINEZ RODRIGUEZNo ratings yet
- Long Term Vertical ChangesDocument5 pagesLong Term Vertical ChangesthganooNo ratings yet
- Daring Occlusal Adjusment (Oa)Document9 pagesDaring Occlusal Adjusment (Oa)Arlanda Diane MahendraNo ratings yet
- Long-Term Effectiveness of Canine-To-Canine Bonded Exible Spiral Wire Lingual RetainersDocument8 pagesLong-Term Effectiveness of Canine-To-Canine Bonded Exible Spiral Wire Lingual RetainersVinit SinghNo ratings yet
- Terapia MiofuncionalDocument10 pagesTerapia MiofuncionalvivianaNo ratings yet
- Fixed Versus Removable Orthodontic Appliances To Correct Anterior Crossbite in The Mixed Dentition-A Randomized Controlled Trial PDFDocument6 pagesFixed Versus Removable Orthodontic Appliances To Correct Anterior Crossbite in The Mixed Dentition-A Randomized Controlled Trial PDFJejeNo ratings yet
- Long-Term Evaluation of Periodontal Therapy: I. Response To 4 Therapeutic ModalitiesDocument11 pagesLong-Term Evaluation of Periodontal Therapy: I. Response To 4 Therapeutic ModalitiesdhillaNo ratings yet
- Analysis of The Treatment of Impacted Canines During A Twenty-Year PeriodDocument4 pagesAnalysis of The Treatment of Impacted Canines During A Twenty-Year PeriodgekdiahNo ratings yet
- Gorucu Coskuner2017Document8 pagesGorucu Coskuner2017MairenNo ratings yet
- 10 1067@mpr 2000 107113Document7 pages10 1067@mpr 2000 107113gbaez.88No ratings yet
- Body PostureDocument7 pagesBody Posturepopat78No ratings yet
- Eross 2015Document9 pagesEross 2015serahNo ratings yet
- Twenty-Yearfollow-Up of Patients With Permanentlybondedmandibular Canine-To-canine Retainers-2008Document7 pagesTwenty-Yearfollow-Up of Patients With Permanentlybondedmandibular Canine-To-canine Retainers-2008chinchiayeh5699No ratings yet
- Ajodo 1Document7 pagesAjodo 1ayis100% (1)
- Morphology of Plans MCQDDocument8 pagesMorphology of Plans MCQDAneesa TafheemNo ratings yet
- Maxillary Dentoalveolar Assessment Following Retraction of Maxillary Incisors: A Preliminary StudyDocument8 pagesMaxillary Dentoalveolar Assessment Following Retraction of Maxillary Incisors: A Preliminary StudyAndrea TokumotoNo ratings yet
- Magnetic BBDocument7 pagesMagnetic BBVicente ContrerasNo ratings yet
- Changes in Maxillary Incisor Inclination and Position After Traction of Unilateral Vs Bilateral Maxillary Impacted Canines in Nonextraction Treatment: A Cone-Beam Computed Tomography StudyDocument12 pagesChanges in Maxillary Incisor Inclination and Position After Traction of Unilateral Vs Bilateral Maxillary Impacted Canines in Nonextraction Treatment: A Cone-Beam Computed Tomography StudyALONDRA GARCIANo ratings yet
- Lip BumperDocument7 pagesLip BumperMiguel JaènNo ratings yet
- Effects of Glass Ionomer Temporary Restorations On Pulpal Diagnosis and TreatmentDocument7 pagesEffects of Glass Ionomer Temporary Restorations On Pulpal Diagnosis and TreatmentKamila BencosmeNo ratings yet
- CJN 079Document199 pagesCJN 079SelvaArockiamNo ratings yet
- Orthodontic Treatment Acceleration With Corticotomy-Assisted Exposure of Palatally Impacted CaninesDocument4 pagesOrthodontic Treatment Acceleration With Corticotomy-Assisted Exposure of Palatally Impacted CaninesLoredana IvanovNo ratings yet
- Recovery of Pulp Sensibility After The Surgical Management of A Large Radicular CystDocument5 pagesRecovery of Pulp Sensibility After The Surgical Management of A Large Radicular CystmeryemeNo ratings yet
- 1 s2.0 S088954060901155X MainDocument8 pages1 s2.0 S088954060901155X Mainbruno mañonNo ratings yet
- Postoperative Pain After Root Canal Treatment A Prospective Cohort StudyDocument8 pagesPostoperative Pain After Root Canal Treatment A Prospective Cohort Studyibrahim bataNo ratings yet
- Outcome of Single Immediate Implants Placed inDocument8 pagesOutcome of Single Immediate Implants Placed injuanita enriquezNo ratings yet
- Mermigos 11 01Document4 pagesMermigos 11 01Sankurnia HariwijayadiNo ratings yet
- Implant-Supported Removable Partial Dentures in The Mandible A 3-16 Year Retrospective StudyDocument8 pagesImplant-Supported Removable Partial Dentures in The Mandible A 3-16 Year Retrospective StudyMohammad Fadyl YunizarNo ratings yet
- Preservation and Augmentation of Molar Extraction Sites Affected by Severe Bone Defect Due To Advanced Periodontitis A Prospective Clinical TrialDocument12 pagesPreservation and Augmentation of Molar Extraction Sites Affected by Severe Bone Defect Due To Advanced Periodontitis A Prospective Clinical TrialBagis Emre GulNo ratings yet
- Evaluation of Alveolar Process Resorption After Tooth Extraction Using The Socket Shield Technique Without Immediate Installation of Implants: A Randomised Controlled Clinical TrialDocument6 pagesEvaluation of Alveolar Process Resorption After Tooth Extraction Using The Socket Shield Technique Without Immediate Installation of Implants: A Randomised Controlled Clinical TrialPedro PachecoNo ratings yet
- Cekic Nagas2016 PDFDocument8 pagesCekic Nagas2016 PDFAkanksha MahajanNo ratings yet
- Clinical Evaluation of Failures in Removable Partial DenturesDocument6 pagesClinical Evaluation of Failures in Removable Partial Denturesruli nurul amanNo ratings yet
- 8 - Clinical Outcome in Periradicular Surgery Effect of Patient - and Tooth-Related Factors - A Multicenter StudyDocument8 pages8 - Clinical Outcome in Periradicular Surgery Effect of Patient - and Tooth-Related Factors - A Multicenter StudykochikaghochiNo ratings yet
- Stalpers Am JOrthod Dentofac Orthop 2007132316323Document8 pagesStalpers Am JOrthod Dentofac Orthop 2007132316323thomas QuilangNo ratings yet
- Abnormal Ridge TypeDocument3 pagesAbnormal Ridge TyperekabiNo ratings yet
- Apical Root Resorption of Incisors After Orthodontic Treatment of Impacted Maxillary Canines, Radiographic StudyDocument9 pagesApical Root Resorption of Incisors After Orthodontic Treatment of Impacted Maxillary Canines, Radiographic StudyJose CollazosNo ratings yet
- Cju 005Document5 pagesCju 005gifar ihsanNo ratings yet
- Long-Term Space Changes After Premature Loss of A Primary Maxillary First MolarDocument5 pagesLong-Term Space Changes After Premature Loss of A Primary Maxillary First MolarFernanda OchoaNo ratings yet
- EDJ - Volume 63 - Issue Issue 4 - October (Orthodontics, Pediatric & Preventive Dentistry) - Pages 2939-2947Document9 pagesEDJ - Volume 63 - Issue Issue 4 - October (Orthodontics, Pediatric & Preventive Dentistry) - Pages 2939-2947Shady AshrafNo ratings yet
- Long-Term Stability of Anterior Open-Bite Treatment by Intrusion of Maxillary Posterior TeethDocument9 pagesLong-Term Stability of Anterior Open-Bite Treatment by Intrusion of Maxillary Posterior TeethNg Chun HownNo ratings yet
- Skeletal Anchorage Augmentation in Extraction/Nonextraction Orthodontic Treatment: A Randomized Clinical StudyDocument13 pagesSkeletal Anchorage Augmentation in Extraction/Nonextraction Orthodontic Treatment: A Randomized Clinical Studyaleja.b7815No ratings yet
- ScriptDocument3 pagesScriptNurhayani AkhiriyahNo ratings yet
- Roots Cybercommunity - Summit VDocument92 pagesRoots Cybercommunity - Summit VCorneliaBroatecNo ratings yet
- The Premature Loss of Primary First Molars: Space Loss To Molar Occlusal Relationships and Facial PatternsDocument6 pagesThe Premature Loss of Primary First Molars: Space Loss To Molar Occlusal Relationships and Facial PatternsSuci Sylvana HrpNo ratings yet
- Practice-Based Clinical Evaluation of Zirconia PDFDocument12 pagesPractice-Based Clinical Evaluation of Zirconia PDFDiego Alejandro Cortés LinaresNo ratings yet
- Hines 1979Document19 pagesHines 1979Devin Chun Yue KwanNo ratings yet
- Long-Term Spontaneous Changes Following Removal of All First Premolars in Class I Cases With CrowdingDocument12 pagesLong-Term Spontaneous Changes Following Removal of All First Premolars in Class I Cases With CrowdingElizabeth MesaNo ratings yet
- PerioDocument6 pagesPeriohusenahNo ratings yet
- 1999 115 1 29 38 ChangDocument10 pages1999 115 1 29 38 ChangAlla MushkeyNo ratings yet
- The Single-Tooth Implant:: A Minimally Invasive Approach for Anterior and Posterior Extraction SocketsFrom EverandThe Single-Tooth Implant:: A Minimally Invasive Approach for Anterior and Posterior Extraction SocketsNo ratings yet
- Implant Therapy: Clinical Approaches and Evidence of Success, Second EditionFrom EverandImplant Therapy: Clinical Approaches and Evidence of Success, Second EditionNo ratings yet
- VaughanDocument16 pagesVaughanMalik RizwanNo ratings yet
- Cradles of Early ScienceDocument6 pagesCradles of Early ScienceMelody Balingasa NapireNo ratings yet
- D0128506a Model 116 170 and pc850 Service ManualDocument15 pagesD0128506a Model 116 170 and pc850 Service ManualcontactNo ratings yet
- AAS TroubleshootDocument30 pagesAAS TroubleshootKimi RinaNo ratings yet
- Machine Design Final Coaching ProblemsDocument63 pagesMachine Design Final Coaching ProblemsasapamoreNo ratings yet
- Star Delta Transformations: 1. Calculate The Total Resistance, R, of The Circuit BelowDocument11 pagesStar Delta Transformations: 1. Calculate The Total Resistance, R, of The Circuit BelowTina EllisonNo ratings yet
- Lab Manual Toad DissectionDocument5 pagesLab Manual Toad DissectionDegorio, Jay Anthony G. 11 - QuartzNo ratings yet
- Kingdom Plantae Phylum Anthophyta: Systematics LaboratoryDocument6 pagesKingdom Plantae Phylum Anthophyta: Systematics LaboratorySIlverNo ratings yet
- Autoclaved Aerated ConcreteDocument4 pagesAutoclaved Aerated ConcreteArunima DineshNo ratings yet
- Location Recce - Horror SceneDocument2 pagesLocation Recce - Horror Sceneapi-634642526No ratings yet
- Christian SongsDocument12 pagesChristian Songsmarie crisNo ratings yet
- Lateral ThinkingDocument3 pagesLateral Thinkingapi-258279026No ratings yet
- Updated Term Paper (5310) PDFDocument21 pagesUpdated Term Paper (5310) PDFSourae MridhaNo ratings yet
- Protocol Document 1.1.4Document114 pagesProtocol Document 1.1.4Jose Daniel Zaraza Marcano100% (2)
- Basic Grammar Unit6 Without AnswersDocument1 pageBasic Grammar Unit6 Without AnswerstitnNo ratings yet
- Internal Audit Checklist Food Safety-MRDocument5 pagesInternal Audit Checklist Food Safety-MRRavi BaghelNo ratings yet
- MB Manual Ga-C807n eDocument40 pagesMB Manual Ga-C807n eJairo maldonadoNo ratings yet
- Basketball-2 0Document46 pagesBasketball-2 0Catherine EscartinNo ratings yet
- Comparison of Greenhouse Gas AnalyzersDocument7 pagesComparison of Greenhouse Gas AnalyzersSabeeqa MalikNo ratings yet
- Homeopathy in Reflexive PerspectiveDocument398 pagesHomeopathy in Reflexive Perspectivealex100% (1)
- Win LandDocument20 pagesWin LandaowsNo ratings yet
- CMC Development Project Management in Boston MA Resume Gary LavineDocument4 pagesCMC Development Project Management in Boston MA Resume Gary LavineGaryLavine2No ratings yet
- Oluwarotimi Ademola OmotolaDocument5 pagesOluwarotimi Ademola OmotolaOluwarotimi Ademola OMOTOLANo ratings yet
- Foreign Part A: Fire Suppression System S/N Description Unit Foam Proportioning Unit Vertical Bladder Type Ul ListedDocument6 pagesForeign Part A: Fire Suppression System S/N Description Unit Foam Proportioning Unit Vertical Bladder Type Ul ListedNakoraNo ratings yet
- Timber Code Check Theory Enu PDFDocument34 pagesTimber Code Check Theory Enu PDFjcvalenciaNo ratings yet
- Eon 2019 Sustainability ReportDocument122 pagesEon 2019 Sustainability ReportDarryl Farhan WidyawanNo ratings yet
- Application Areas of Intelligent Transport System: READ MORE: GIS in TransportationDocument2 pagesApplication Areas of Intelligent Transport System: READ MORE: GIS in TransportationIonut CarstovNo ratings yet
- CDU BIOCHEMISTRY Structure of Triacylglycerols WorksheetDocument2 pagesCDU BIOCHEMISTRY Structure of Triacylglycerols WorksheetKrisha Mae VillanuevaNo ratings yet