Professional Documents
Culture Documents
Chapter 26. Alarm Devices
Chapter 26. Alarm Devices
Uploaded by
adham08Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 26. Alarm Devices
Chapter 26. Alarm Devices
Uploaded by
adham08Copyright:
Available Formats
Chapter 26
Alarm Devices
The purposes of an al arm are to transf er i nf ormati on, enhance vi gi l ance, and warn
of a potenti al or actual abnormal or unusual condi t i on (1,2, 3,4). I t i s essenti al that
t here be a means of al erti ng personnel to a change or potenti al change i n
equipment f uncti on or t he pat ient , for there wi l l al ways be occasi ons when operat or
vi gi lance wi l l be lowered or at tenti on reduced whi l e perf ormi ng ot her t asks.
The number of al arms i n anestheti zi ng areas has i ncreased great l y. To add f urther
confusi on, al arm sounds may come f rom sources other than f rom anesthesi a
apparatus, i ncl udi ng el ect rosurgi cal equi pment , l asers, heari ng ai ds, and beepers
(5,6,7). The Joi nt Commi ssi on on the Accredi tati on of Heal thcare Organizati ons has
made i t a goal to i mprove the eff ecti veness of al arm syst ems (8,9).
Standards
An i nternati onal st andard f or al arm systems was publ i shed i n 2003 (10).
Terminology (10)
Al arm Condi t i on Del ay: Time f rom the occurrence of a t ri ggeri ng event t o
when t he al arm system determi nes that an alarm condi ti on exi sts.
Al arm Si gnal Generat ion Delay: Ti me f rom the onset of an al arm condi ti on to
t he generat i on of i ts al arm si gnal s.
Al arm Li mi t : Threshol d used by an al arm system to determi ne an al arm
condi ti on.
Al arm Of f: St ate of i ndef i ni t e durat ion i n whi ch an al arm system or part of an
al arm system does not generat e al arm si gnals.
Al arm Paused: State of l i mi t ed durati on i n whi ch the alarm system or part of
t he al arm system does not generate al arm si gnal s.
Al arm Preset : Set of stored confi gurati on parameters, i ncluding sel ect ion of
al gori thms and i ni t ial val ues f or use.
Al arm Reset: Operator act ion t hat causes the cessati on of an al arm si gnal for
whi ch no associat ed al arm condi ti on currentl y exi sts.
Al arm Set ti ngs: Al arm system conf igurati on, i ncluding but not li mi ted t o alarm
l i mi ts, the characteristi cs of any al arm si gnal inact ivat ion states, and t he
values of vari abl es or parameters that determine the f unct i on of the al arm
system.
Al arm Si gnal : Si gnal generated by t he al arm system to i ndi cat e the presence
of an alarm condi t ion.
Al arm System: Part s of medical el ectrical equi pment t hat detect al arm
condi ti ons and, as appropriat e, generate alarm si gnal s.
Audi o Of f: St ate of i ndef i ni te durat ion i n whi ch t he alarm system or part of
t he al arm system does not generate an audi tory al arm si gnal .
Audi o Paused: State of l i mi ted durat ion i n whi ch the alarm system or part of
t he al arm system does not generate an audi tory al arm si gnal .
Defaul t Al arm Preset: Al arm preset t hat can be act ivated by the alarm syst em
wi thout operator act ion.
Fal se-negat ive Al arm Condi ti on: Absence of an alarm condi t i on when a val i d
t ri ggeri ng event has occurred.
P. 829
Fal se-posi ti ve Al arm Condi ti on: Presence of an alarm condi t i on when no
vali d triggeri ng event has occurred.
Hi gh Pri ori ty: Indicates that i mmedi ate operat or response i s requi red.
I nformat i on Si gnal : Any si gnal t hat i s not an alarm si gnal or a remi nder
si gnal . Exampl es i ncl ude t he tone of the pul se oximeter or
el ect rocardi ograph, the wavef orm of t he el ect rocardi ograph, and the heart
rate numeri c.
I ntel l i gent Alarm System: Al arm system t hat makes l ogi cal deci si ons based
on moni t ored i nf ormati on wi thout operator i nterventi on. I ntel l i gent al arm
system methodol ogi es i ncl ude anal ysi s of trends, l i mi t comparisons, data
redundancy, data fusi on, rul es, f uzzy logic cont rol l ers, and neural net works.
Latchi ng Al arm Si gnal : Alarm si gnal t hat cont i nues to be generated af ter i ts
t ri ggeri ng event no l onger exi sts unt i l stopped by del i berat e operat or acti on.
Low Pri ori ty: Indi cates that operator awareness i s requi red.
Medi um Pri ori ty: I ndicates t hat prompt operat or response i s requi red.
Remi nder Signal : Peri odi c si gnal that remi nds t he operator t hat t he al arm
system i s in an alarm signal i nacti vat i on state.
I nhi bi t, si l ence, and suspend have been used in past termi nol ogy f or alarms.
Unf ortunatel y, di ff erent meani ngs were att ri buted t o these terms. For t his reason,
t hese terms wi l l not be used.
Alarm Prioritization
Al l al arms are not equall y import ant . The i nf ormati on that an al arm conveys may
represent an emergency, t he potent i al f or an emergency, or j ust an unusual
condi ti on. Pri ori t ized al arms hel p to dif f erenti ate l i fe-t hreat eni ng si tuati ons f rom
t hose that are l ess urgent. Al arm condi ti ons pri ori t i es are shown i n Tabl e 26.1. It
may be possi bl e to i ncrease t he pri ori ty of an al arm, but the pri ori t y cannot be
decreased.
A hi gh-pri ori t y al arm i ndi cates a condi t i on that requi res i mmedi ate act ion. Exampl es
i ncl ude asyst ol e, vent ri cul ar f ibri l l at i on, cardi ac support devi ce (i nt ra-aort ic bal l oon
pump, cardi opul monary bypass machi ne) f ai l ure, high ai rway pressure, ext reme
hypoxemia, and sustai ned hi gh-energy radiati on beam.
Medi um priori ty i mpl i es a potenti al l y dangerous si tuati on that requi res a prompt
response. Exampl es i ncl ude many cardiac arrhyt hmi as, high or low bl ood pressure,
apnea (unl ess prol onged or associ ated wi t h ext reme hypoxia), mi ld hypoxemia, and
hi gh or l ow parti al pressure of carbon dioxide (pCO
2
).
A low pri ori t y alarm indicates that onl y operat or awareness i s requi red. Examples
i ncl ude f ai lure of an i nf usi on pump f or mai nt enance intravenous f luids and f ai l ure of
an enteral f eeding pump.
The object of pri ori t i zat ion i s to mi ni mi ze dist racti on f rom l ess i mportant al arms
duri ng an emergency. I t has been suggest ed t hat only t he al arm sound
correspondi ng to t he most urgent of the prevail i ng al arm condi t i ons shoul d be
annunciat ed; al l ot her sounds shoul d be temporari l y audi o paused (2). Once the
most urgent al arm condi t ion i s resol ved, the sound correspondi ng to t he
P. 830
next hi ghest priori ty condi ti on would t hen be i ni ti at ed. This pri ori t y i nterlock should
be l imi ted to audible annunci ati on; l ower pri ori t y vi sual si gnal s need not be
suppressed because they are rel ativel y unobt rusi ve.
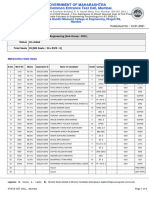
TABLE 26.1 Alarm Condition Priorities
Onset of Potential Harma Potential Result of
Failure to
Response to the
Cause of Alarm
Condition
Immediateb Promptc Delayedd
Death or
irreversible
injury
HIGH
PRIORITY
HIGH
PRIORITY
MEDIUM
PRIORITY
Reversible injury HIGH
PRIORITY
MEDIUM
PRIORITY
LOW PRIORITY
Minor injury or
discomfort
MEDIUM
PRIORITY
LOW
PRIORITY
LOW PRIORITY
or no alarm signal
An information signal may be used to indicate the potential for delayed minor injury
or discomfort
a
Onset of potential harm refers to when an injury occurs and not to when it is
manifested.
b
Having the potential for the event to developed within a period of time not usually
sufficient for manual corrective action.
c
Having the potential for the event to develop within a period of time that is usually
sufficient for manual corrective action.
d
Having the potential for the event to develop within an unspecified time that is greater
than that given under prompt.
From International Standards Organization. Medical electrical equipment-Part 18:
general requirements for safety. Collateral standard: general requirements, tests and
guidelines for alarm systems in medical electrical equipment and in medical electrical
systems (ISO-IEC 60601-1-8). Geneva, Switzerland: Author, 2003.
Audible Signals
The pri mary purpose of audi tory al arm si gnals i s to get the operator' s attenti on. In
addi ti on, t hey shoul d hel p the operator to i denti f y t he onset of al arm condi t ions, the
urgency of the requi red operator response and the l ocati on of the devi ce generat i ng
al arm si gnals.
An audible si gnal wi l l att ract at tenti on f aster and more reli ably t han one t hat i s
vi sual (11). Ideal l y, i t shoul d do t his i n a ti mel y, non-startl i ng, and non-i rri t at ing
f ashi on (12). Unf ort unatel y, the qual i ti es that cause sounds to at t ract at tenti on al so
t end to make them i nt rusive or start l i ng. Some are so unpl easant that the response
may be t o i nappropriatel y di sabl e or deact i vat e the al arm syst em.
There are a number of avail abl e opt ions i n alarm sound t echnol ogy, i ncl udi ng
vari ati ons in pat tern, pi tch, tone, f requency, and loudness. The int ernat ional al arm
standard speci f ies the characteri st ics of audi tory alarm signal s (10).
One probl em associ ated wi t h al arm sounds i s that cl inicians may not hear t hem.
Background noise and other al arms can i nterf ere wi t h heari ng an audi bl e alarm
si gnal (13). If an audi bl e si gnal i s al l owed to conti nue t o sound, other audi bl e
si gnals may not be noti ced (14,15). An anesthesi a provi der wi th a heari ng def i ci t
may have di f f icul ty determining t he source of a sound. One study f ound t hat many
anesthesi ol ogi sts have an abnormal audi ogram and that 7% had one or more al arm
i ntensi ti es bel ow t he detectabi l i t y threshol d (16). Audi bl e alarms should be adj usted
so t hat t he si gnal wi l l be percei ved despi te background noi se.
Once an audi bl e signal has been percei ved, t he next st ep i s to i dent if y i ts origin.
Thi s i s i mport ant because many moni tors are not i n the cli ni ci an' s i mmedi ate f ield
of view, and the operat or cannot al ways turn around t o vi ew them. Many anest hesi a
provi ders have t roubl e identif yi ng audibl e al arms (13, 17,18,19). I nabil i t y to i denti f y
an al arm may delay or prevent the appropri ate remedi al acti on (15,20).
Af ter an audi bl e si gnal has succeeded i n capt uring at tenti on, audio pausi ng
(muti ng, si l enci ng) wi l l provi de ti me to correct the si tuati on. The conti nuous
presence of an audi bl e si gnal can degrade task perf ormance and i mpai r detecti on
of new al arm condi t i ons and the abi l i t y to di st ingui sh bet ween exi sti ng and new
al arm condi ti ons. The visual component of the al arm i ndi cator and associ ated
f uncti ons shoul d stay act ivated unti l the condi ti on that t ri ggered the al arm i s
correct ed. If another al arm condi ti on occurs whi l e an al arm i s audi o paused, t he
addi ti onal alarm should have bot h audi bl e and vi sual i ndi cat i ons.
Most manuf act urers provide a means of audi o pausi ng. The ti me vari es wi t h the
i nst rument and can somet i mes be vari ed. Some moni tors i ndicate el apsed ti me. The
al arm st andard requi res that there be a visual i ndi cati on that any alarm si gnal has
been inact ivated (10).
Some al arms can be t urned to AUDI O OFF (def eat ed, disabl ed) f or an unl imi ted
t i me. The vol ume of some al arms can be decreased to a poi nt where t he audi bl e
si gnal cannot be heard (21). Usi ng AUDI O OFF or low volume i s dangerous, as
ei ther can l ead t o a f al se-negat ive alarm.
Visual Signals
Vi sual si gnal s hel p the operator l ocat e the equi pment where response or awareness
i s needed and i dent if y the speci f i c alarm condi t ion. Thei r pri nci pal drawback i s that
t hey can go unrecognized for a much longer t i me than audi bl e signal s (22). I n a
si tuat ion where the indi vi dual responsibl e for react ing t o an al arm i s requi red to use
hi s or her vi si on for other tasks, a vi sual message may go unnoti ced. It may not be
possi bl e f or t he i ndi vi dual to turn and l ook at the source of the al arm (e.g., duri ng
l aryngoscopy). Graphical symbol s f or alarm systems f rom the internat i onal standard
are shown i n Fi gure 26.1 (10).
Table 26.2 shows the col or and f lashi ng requi rements f or alarm i ndicator l i ghts or
graphical si mul ati on of indicator l i ghts i n t he i nt ernati onal st andard (10). The al arm
standard al so requi res that the presence of an al arm condi ti on and i ts pri ori t y be
correct l y perceived f rom a distance of 4 m and be l egi bl e f rom at l east 1 m f rom t he
operator' s posi ti on.
Alarm Organization
Al arm messages somet imes arrive i n an unorgani zed pat t ern. The si ngl e, i ntegrated
di spl ay i s designed to ai d al arm i denti f i cat ion. Thus, anesthesia personnel need t o
l ook i n onl y one pl ace to i denti f y problems.
P. 831
P. 832
A di sadvantage of t hi s is t hat a crowded di spl ay may be di f fi cul t t o read duri ng a
crisis. It may not be possi bl e to i ntegrate al l moni tors i nto a si ngl e displ ay.
TABLE 26.2 Characteristics of Alarm Indicator Lights
Alarm Category I ndicator Color Flashing Frequency
HIGH PRIORITY Red 1.4 Hz to 2.8 Hz
MEDIUM PRIORITY Yellow 0.4 Hz to 0.8 Hz
LOW PRIORITY Cyan or yellow Constant
View Figure
Figure 26.1 Graphic symbols for alarm systems. (From
ISO IEC 60601-1-8, Medical electrical equipmentPart
1-8: general requirements for safetycollateral
standard general requirements, tests and guidelines for
alarm systems in medical electrical equipment and in
medical electrical systems, 2003
).
Alarm Limits
An al arm l i mi t (set point, t hreshol d value, t hreshol d, setti ng) may be non-
adj ustable, operator-adjustable, or an al gori thmi cal l y det ermi ned cri t eri on (12). The
al arm st andard requi res that i f an operat or-adj ustabl e alarm l i mi t i s provi ded, the
l i mi t shall be indicat ed cont i nuousl y or by operat or acti on so t hat i t can be
determined if t he set val ues are appropri at e f or t he pati ent and procedure (10)
(Fi gs. 26.2, 26.3).
Def aul t al arm l i mi ts can be set by the manuf act urer, t he heal th care faci l i ty, or t he
operator. Those set by the manufact urer may be def aul t values or may be bracket ed
around the val ue of a moni tored vari abl e at a poi nt i n ti me, recent val ues of a
moni tored variable, or a current control setti ng (10). Most moni tors al l ow the
operator t o al ter the defaul t set ti ngs.
Reali st ic al arm l i mi ts need to be set . Wide l i mi ts resul t i n f ewer f al se al arms but
i ncrease t he ri sk of missi ng a t rue alarm (good specif i ci ty but poor sensi t ivi t y) (12).
Wi th pressure and vol ume alarms duri ng art i fi ci al venti l at ion, a low sett i ng may
resul t i n a part i al di sconnecti on or smal l leak bei ng mi ssed. Constricti ons i n the
breat hi ng system t hat i ncrease resistance can cause t he ai rway pressure t o remain
above a low al arm set point al t hough a total disconnecti on woul d probabl y not be
mi ssed (23).
Ensuri ng t hat an alarm is acti vated bef ore a dangerous condi t ion has occurred
wi thout creat i ng f requent spuri ous alarms requi res i nt el l i gence on t he part of both
t he al arm system and t he operator. Some operat ors set l i mi ts to extremes unl i kel y
t o be encount ered cli ni cal l y. The f arther threshol ds are f rom normal val ues, the
great er t he probabi l i t y that a dangerous condi ti on wi l l occur wi t hout acti vating the
al arm. Others si mpl y use the l i mi ts set by the l ast person who used t he devi ce.
Ot hers keep the threshol ds cl ose t o the manufacturer-preset l i mi ts.
I t i s good pract ice t o record al arm l i mi ts on t he anesthesi a record. Thi s provi des
evidence that the al arms were acti vated. I t may al so i ncrease the operator' s
awareness of the al arms and/or make i t more l i kel y t hat appropri ate val ues wi l l be
used. I t i s possibl e that the set alarm l i mi ts may be recorded i n the el ectroni c
record.
False Alarms
Actual al arm mal functi ons are rare (24,25). The anesthesi a provi der can reduce t he
number of f al se-posi t i ve and f alse-negat i ve al arms by caref ul l y preparing t he
pati ent i nt erface, securel y attaching probes, select ing moni t ors wi t h art i fact
rej ecti on capabil i t i es, usi ng wi der l i mi ts, i ncreasi ng the alarm si gnal generat i on
del ay, and t ai l ori ng the al arms to the pat ient or operati on (25, 26,27,28, 29).
Posi t i oni ng the pulse oxi met er probe away f rom el ectrosurgery
P. 833
wi res may also hel p, as may l ocati ng the electrosurgery groundi ng pad far away
f rom the pul se oxi met er probe and electrocardi ogram el ect rodes (30).
View Figure
Figure 26.2 Alarms limits are displayed continuously to the
right of the values for the parameters. (Picture courtesy of
Draeger Medical, Inc.)
View Figure
Figure 26.3 The complete set of alarm values is displayed.
To display the alarm limits menu, the alarm limits soft key
(1) is pressed. The menu (2) lists the parameters, their
current measured values (larger numbers), and the current
low and high alarm limits. The alarm limits also appear on
the curves as dashed lines (3). (Picture courtesy of Draeger
Medical, Inc.)
False-positive Alarms
Many alarms are spurious. Onl y a smal l number i ndi cate act ual ri sk
(31,32,33, 34, 35,36,37, 38,39,40).
An al arm acti vated wi thout proper cause requi res t ime and eff ort to check the
actual condi ti ons. Thi s wi l l resul t i n less at tenti on to other tasks and may l ead t o an
i nappropri at e act ion. Fal se-posi t i ve al arms are a source of i rri tat i on and di st racti on
and are a threat to pati ent care, because t he anesthesi a provi der becomes
i ncreasi ngly l ikel y to i gnore the signal s, l ower t he al arm volume, turn OFF the
enti re al arm system, use t he AUDI O OFF or AUDIO PAUSE wi thout l ooking f or t he
cause, or set the al arm l i mi ts at such ext remes that the al arm system is eff ect ivel y
di sabled (12,41, 42,43,44,45). False-posi ti ve al arms may f ri ghten pat ients and
rel atives.
Fal se-posi ti ve al arms are a fact of l i f e. Whi l e there are st rategi es f or mi ni mi zi ng
t hem, t hey cannot be ent i rel y eli mi nated.
Fal se-posi ti ve al arms may be caused by al arm mal f unct ion, arti facts, extraneous
sounds being mi staken f or alarm si gnal s, and i nappropriate set poi nts.
The start-up sequence on equi pment can prevent f al se-posi tive alarms. Medi cal
equipment that automati cal l y enables the al arm system when a pat ient i s connect ed
t o t he equipment when a val id physi ol ogi c si gnal is f i rst detected, or t hrough an
admi t new pat i ent f unct ion acti vated by t he operator wi l l decrease the number of
such al arms.
Fal se al arms may be reduced by changing al arm li mi ts at cert ai n ti mes, since
cl i nical ranges vary during di f ferent phases of anest hesi a (46). For exampl e, t he
hi gh heart rat e alarm li mi t mi ght be set hi gher duri ng i ntubat ion than duri ng
mai ntenance.
The ALARM PAUSED state can be used t o avoi d nui sance al arm si gnal s bef ore
perf ormi ng an acti on that i s l i kel y to cause an alarm condi t ion (10,38). Exampl es of
such acti ons are i ntenti onal breathi ng system disconnect i on to perf orm ai rway
sucti oning, opening a t ransducer t o ai r f or zero cal ibrat ion, i nt ubat i on, and t rying to
restore spontaneous breat hi ng at the end of a case.
Moni tors wi t h art i f act rej ect i on such as pul se oxi meters wi t h moti on-resi stant
al gori thms can decrease the
P. 834
number of f al se-posi t i ve al arms (47,48, 49,50). Fi l teri ng i n the algori thm that is
moni tori ng f or an al arm condi ti on of ten causes al arm condi ti on del ay (10). For
i nstance, a heart rate moni tor can average the R-R i nt erval f or several heart beats.
An abrupt change i n R-R i nterval s wi l l not immediatel y cause an al arm condi ti on,
because i t wi l l take several consecutive heart beats f or the cal cul at ed heart rate to
exceed the al arm l i mi t. Some elect rocardiogram moni tors have aut omat i c l ead
swi t chi ng so that moni t oring can conti nue even if one or t wo el ectrodes come OFF.
Thi s can decrease f al se-posi tive alarms.
Fal se al arms can be reduced by integrat i ng moni tors (38,51). An exampl e i s
synchroni zi ng the pul se oximeter and noni nvasive bl ood pressure moni t or. If the
oximet er probe i s on t he same arm as the bl ood pressure cuff , no al arm wi l l sound
i f no pul se i s det ected when the cuf f i s i nfl at ed. Another exampl e i s the pul se
oximet er and el ect rocardiogram (ECG). SpO
2
val ues are rej ected unl ess t he pul se
rate measured on the oxi meter matches that on the ECG.
False-negative Alarms
I f an al arm system f ai ls t o generate a si gnal when i t should (f al se negat ive), the
pati ent 's safety may be t hreatened. An al arm condi ti on may be rejected or missed
because of spuri ous i nf ormati on produced by the pati ent, the pat i ent -equi pment
i nterf ace, other equipment , or t he equipment i tself .
Another cause is t he al arm bei ng t urned OFF. Subsequent users may not be aware
t hat i t has been turned OFF. Aut omati c enabl i ng is present on many newer
moni tors. Once a moni t ored parameter is sensed, the al arm becomes acti ve. This
el i mi nates the probl em of forgett i ng to t urn an al arm ON or not bei ng aware that an
al arm has been turned OFF by a previ ous user. Appropri at e appl i cat ion of reminder
si gnals shoul d reduce t he chance that the al arm system i s uni ntent ional l y l ef t in an
al arm si gnal i nacti vation state (10).
Speaker fai l ure, set ti ng t he audi bl e vol ume t oo l ow, and sett ing t he al arm l imi ts too
wi del y may al so cause false-negative alarms (52).
Fal se-negat ive al arms may be reduced by not set ti ng the l i mi ts too wi del y, usi ng
t he AUDIO PAUSE rather t han the AUDIO OFF st ate, and checking al arm systems
at regular int erval s to detect probl ems such as a faul t y loudspeaker or l ow audi bl e
volume that can resul t in an audi bl e si gnal not bei ng heard.
Intelligent Alarm Systems
An i ntell i gent (smart, expert ) al arm system may do one or more of the f ol l owi ng
wi thout operator i nterventi on: determi ne an al arm condi ti on on the basi s of t i me,
wei ght i ngs, mul t i ple vari abl es, or other advanced processi ng; generat e al arm
si gnals f or t wo or more alarm condi t ions of equal pri ori t y; change t he previ ousl y
assi gned pri ori ty or rel ative pri ori t i zat i on of a parti cul ar alarm condi ti on; change t he
al arm si gnal generati on delay or al arm condi t i on del ay; change the characteri st i cs
of t he generated alarm signal s (e. g. , to i ndicate a change i n urgency); provide the
operator wi t h a l i st of condi t ions that coul d have triggered the alarm(s); and present
i nformati on that is hel pful in deal ing wi t h t he condi ti on t hat t ri ggered t he al arm
(36,46,53, 54, 55,56,57, 58,59,60).
Smart al arms can reduce the number of f al se al arms by discri minat ing between
arti f acts and trul y threateni ng condi t ions. Human response t i mes are l onger and
have greater variabi l i ty wi t h conventi onal al arms than i nt el l i gent al arms (61).
Alarm Condition Logging
Many modern moni tors and l i f e-support ing equi pment are equi pped wi th al arm
condi ti on l oggi ng. Logging can be used t o det ermi ne the cause of a transient al arm
condi ti on, for qual i t y assurance purposes, to st udy cri ti cal i nci dents, and to
determine when an al arm condi ti on occurred. The l og should i ncl ude t he val ue of
t he variabl e that caused the al arm condi t ion, t he alarm l i mi ts, and the alarm status
(ON, Audi o Paused, Paused, Audi o Off , etc). Thi s i nformat ion can then be made
avai l able i f a probl em occurs.
References
1. Beneken JEW, van der Aa JJ. Al arms and t hei r l imi ts i n moni tori ng. J Cl i n Moni t
1989; 5:205210.
[CrossRef ]
[Medli ne Li nk]
2. Schrei ber PJ, Schrei ber J. Structured al arm systems f or t he operat i ng room. J
Cl in Moni t 1989; 5:201204.
[CrossRef ]
[Medli ne Li nk]
3. Qui nn ML. Semi practi cal al arms. A parabl e. J Cl in Moni t 1989; 5:196200.
[CrossRef ]
[Medli ne Li nk]
4. Wei nger MB, Smi th NT. Vigi l ance, al arms, and i nt egrated moni tori ng systems. In:
Ehrenwert h J, Ei senkraf t JB, eds. Anesthesi a equi pment, pri nci pl es and
appli cati ons. St. Loui s: CV Mosby, 1993:350384.
5. El l iott B, Chestnut J. Dangers of al arms. Anaesthesia 1996;51: 799800.
[Full text Li nk]
[CrossRef ]
[Medli ne Li nk]
6. Zmysl owski WP, Ravi VS, Chua M, et al . Spuri ous anesthesi a al arm i n an
anesthet i zed pat ient. Anesthesi ology 1993;79:11501151.
[CrossRef ]
[Medli ne Li nk]
7. Tayl or S, Wandl ess J, Harrup K. A f alse alarm wi t h the oxygen f ai l ure warni ng
device. Anaest hesi a 1995;40:210.
8. Wi l l i ams JS. Meeti ng the chal l enge: how hospi tal s compl i ed wi th t he new cl inical
al arms requi rement . Bi omed I nst rum Technol 2003;37:319328.
[Medli ne Li nk]
9. Anonymous. Joi nt Commi ssi on announces f ive new goal s i n i ts 2005 nat i onal
pati ent saf ety goal s. Heal th Devi ces Al erts 2004; 28:14.
10. Int ernati onal Standards Organi zat ion. Medi cal el ect ri cal equi pmentPart 18:
general requi rements f or safety. Col lateral standard: general requi rements, tests
and guidel ines for alarm systems i n medi cal electri cal equi pment and in medical
el ect rical systems (ISO-I EC 60601-1-8). Geneva, Swi t zerl and: Author, 2003.
11. Morri s RW, Montang SR. Response t i mes to vi sual and audi tory al arms duri ng
anaesthesia. Anaesth Int ens Care 1996;24:682684.
[Medli ne Li nk]
12. Block FE, Nuuti nen L, Bal last B. Opti mizati on of alarms: a study on al arm li mi ts,
al arm sounds, and f al se al arms, i ntended t o reduce annoyance. J Cl i n Moni t
Comput 1999;15:7583.
[CrossRef ]
[Medli ne Li nk]
13. Momtahan K, Het u R, Tansl ey B. Audi bi l i t y and i denti f i cati on of audi tory al arms
i n the operati ng room and i ntensi ve care uni t. Ergonomi cs 1993;36:11591176.
[CrossRef ]
[Medli ne Li nk]
14. Chui PT, Gi n T. Fal se al arms and i ntegrat ed al arm system: report of a pot ent i al
hazard. Anesth Anal g 1994;68: 193199.
15. Jones D, Lawson A, Hol l and R. Case reports. I ntegrated alarms and al arm
overl oad . Anaesth Intens Care 1991;19: 101102.
[Medli ne Li nk]
16. Wal l ace MS, Ashman MN, Mat j asko MJ. Heari ng acui ty of anesthesi ol ogi sts and
al arm detecti on. Anesthesi ol ogy 1994;81:1328.
[Full text Li nk]
[CrossRef ]
[Medli ne Li nk]
P. 835
17. Finley GA, Cohen AJ. Percei ved urgency and the anaesthet i st: responses to
common operat ing room moni tor al arms. Can J Anaesth 1991;38: 958964.
[Medli ne Li nk]
18. Gri ff i th RL, Raci ot BM. A survey of pract i ci ng anesthesiologists on audi tory
al arms i n the operati ng room. In: Hedl ey-Whyte J, ed. Operati ng room and intensi ve
care al arms and informati on t ransf er (STP 1152). Phil adelphia: Ameri can Soci et y
f or Testi ng and Materi als, 1992:1018.
19. Loeb RG, Jones BR, Leonard RA, et al . Recogni ti on accuracy of current
operati ng room al arms. Anesth Anal g 1992;75:499505.
[Full text Li nk]
[CrossRef ]
[Medli ne Li nk]
20. Andrzej owski J, Freeman R. Oxygen f ai l ure alarms on modern anaest het i c
machi nes. Anaesthesi a 2002;57: 931932.
[Full text Li nk]
[Medli ne Li nk]
21. Anonymous. Cri ti cal al arms: pat i ents as ri sk. Technol Anest h 1996;16(10): 1
6.
22. Morri s RW, Montano SR. Response t i mes to vi sual and audi tory al arms duri ng
anaesthesia. Anaesth Int ens Care 1996;24:682684.
[Medli ne Li nk]
23. Anonymous. Mini -set vent il ator al arms can be l ethal . Technol Anesth
1999; 20:12.
24. Anonymous. Why alarm-rel ated probl ems reall y happen. Technol Anest h
2002; 23:18.
25. Watson MO, Sanderson PM, Russel l WJ. Tai l oring reveals i nf ormati on
requi rements: the case of anaesthesi a al arms. Interact Comput 2004;16:271293.
[CrossRef ]
26. Anonymous. Del ay ci rcui t may reduce pul se oximetry f al se al arms. Bi omed Saf e
St and 1992; 22:162163.
27. Anonymous. Noi se pol l uti on i n t he operati ng room f rom moni t or al arms. Technol
Anesth 1993; 13(10):3.
28. Ahl born V, Bohnhorst B, Peter CS, et al . False alarms i n t he neonat al i ntensi ve
care uni t : compari son between 3 modul ar moni t ori ng systems. Acta Paedi atr
2000; 89:571576.
[CrossRef ]
[Medli ne Li nk]
29. Seagull FJ, Sanderson PM. Anesthesia al arms in context : an observati onal
study. Hum Factors 2001;43:6678.
[CrossRef ]
[Medli ne Li nk]
30. Block FE, Detko GJ. Minimi zi ng interf erence and f al se al arms f rom
el ect rocautery in t he Nel lcor N-100 pul se oxi meter. J Cl i n Moni t 1986;2: 203205.
[CrossRef ]
[Medli ne Li nk]
31. Koski EMJ, Makivi rta A, Sukuvaara T, et al . Frequency and rel i abi l i t y of al arms
i n the moni tori ng of cardi ac postoperat i ve pat i ents. Int J Cl i n Moni t Comput 1990;7:
129133.
[CrossRef ]
[Medli ne Li nk]
32. Schaaf C, Bl ock FE. Eval uati on of al arm sounds in the operati ng room. J Cl i n
Moni t 1989;5: 300301.
33. O' Carrol l TM. Survey of al arms i n an intensi ve therapy uni t. Anaesthesi a
1986; 41:742744.
[CrossRef ]
[Medli ne Li nk]
34. Kest i n I G, Mi l l er BR, Lockhart CH. Audi tory alarms duri ng anesthesi a
moni tori ng. Anesthesi ology 1988;69:106109.
[Full text Li nk]
[CrossRef ]
[Medli ne Li nk]
35. Lawl ess ST. Cryi ng wol f : false alarms i n a pedi atri c i ntensive care uni t . Cri t
Care Med 1994;22:981985.
[CrossRef ]
[Medli ne Li nk]
36. Tsi en CL, Fackl er JC. Poor prognosi s f or exi st i ng moni tors i n t he i ntensi ve care
uni t . Cri t Care Med 1997;25:614619.
[Full text Li nk]
[CrossRef ]
[Medli ne Li nk]
37. Chambri n M-C, Ravaux P, Cal velo-Aros D, et al . Mul t icent ri c study of
moni tori ng al arms in the adul t i ntensi ve care uni t (ICU): a descript i ve anal ysis.
I ntensive Care Med 1999;25:13601366.
[CrossRef ]
[Medli ne Li nk]
38. Block FE, Schaaf C. Audi tory al arms duri ng anesthesia moni tori ng wi t h an
i ntegrated moni tori ng system. I nt J Cl in Moni t Comput 1996; 13:8184.
[Medli ne Li nk]
39. Wi kl ung LM, Hok B, St ahl K, et al . Post anesthesi a moni tori ng revi si ted:
f requency of true and f al se al arms f rom di f ferent moni tori ng devi ces. J Cl in Anesth
1994; 6: 182188.
40. Yasumoto M, Sakuragi T, Maruta S, et al . Act ivati on of apnea al arm by a
surgi cal theat er l ight duri ng ophthal mol ogi cal surgery. Anesth Anal g 1997;85:1414
1415.
[Full text Li nk]
[CrossRef ]
[Medli ne Li nk]
41. McIntyre JWR. Ergonomics. Anaesthet i sts' use of audi tory alarms in the
operati ng room. Int J Cli n Moni t Comput 1985;2:4755.
[Medli ne Li nk]
42. Anonymous. Cri ti cal al arms: pat i ents at ri sk. Technol Anesth 1987;7(10): 16.
43. Geddes LA. Some exampl es of hazards i n the operati ng room. J Cl i n Eng
1999; 24:175186.
44. Lof sky AS. TURN YOUR ALARMS ON! APSF Newsl et t 20042005; 19(4): 43.
45. Nort on RN. Si l enced alarm resul ts i n near-miss. APSF Newsl et t 2005;20:42.
46. Myl rea KC, Orr JA, Westenskow DR. Integrat i on of moni tori ng f or i ntel l i gent
al arms i n anesthesi a: neural networkscan they hel p? J Cli n Moni t 1993;9:3137.
47. Mi yasaka K. Pul se oxi met ry i n the management of chi ldren i n t he PI CU. Anesth
Anal g 2002;94:S44S46.
[Medli ne Li nk]
48. Ahl born V, Bohnhorst B, Peter CS, et al . False alarms i n t he neonat al i ntensi ve
care uni t : compari son between 3 modul ar moni t ori ng systems. Acta Paedi atr
2000; 89:571576.
[CrossRef ]
[Medli ne Li nk]
49. Hay WW, Rodden DJ, Col l i ns SM, et al . Rel iabi l i ty of convent ional and new
pulse oxi metry in neonatal pati ents. J Peri nat ol 2002;22: 360366.
[CrossRef ]
[Medli ne Li nk]
50. Malviya S, Reynol ds PI, Voepel -Lewi s T, et al . Fal se al arms and sensi t ivi t y of
conventi onal pul se oxi met ry versus the Maxi mo SET t echnol ogy i n the pedi atri c
postanest hesi a care uni t . Anesth Anal g 2000; 90:13361340.
[Full text Li nk]
[CrossRef ]
[Medli ne Li nk]
51. Navabi MJ, Wat t RC, Hameroff SR, et al . I ntegrated moni toring can detect
cri t i cal events and i mprove al arm accuracy. J Cl i n Eng 1991;16:295306.
[Medli ne Li nk]
52. Anonymous. Nel lcor-Vari ous pul se oxi met ers: audio alarm f ai l ure. Heal th
Devices Alert s 2004;28:56.
53. Anonymous. Al arms i n the operati ng room. Can J Anaesth 1991; 38:951.
[Medli ne Li nk]
54. Fukui Y, Masuzawa T. Knowl ege-based approach to i ntel l i gent al arms. J Cli n
Moni t 1989;5: 211216.
[CrossRef ]
[Medli ne Li nk]
55. Pan PH. False al arms di st ri but ion i n i ntraoperati ve pul se oxi metry.
Anesthesi ol ogy 1992; 77:A494.
[Full text Li nk]
[CrossRef ]
56. Farrel l RM, Orr JA, Kuck K, et al . Di f ferenti al f eat ures f or a neut ral net work
based anesthesi a al arm system. Biomed Sci ences 1992;28:99104.
57. Orr JA, Westenskow DR. A breathing ci rcui t al arm system based on neural
net works. J Cl i n Moni t 1994;10:101109.
[Medli ne Li nk]
58. Watt RC, Masl ana ES, Myl rea KC. Al arms and anesthesi a chal l enges in t he
design of i ntel l i gent syst ems f or pati ent moni tori ng. IEEE Eng Med Biol Mag
1993; (Dec):3441.
[CrossRef ]
59. Oberl i C, Urzua J, Saez C, et al . An expert system f or moni tor al arm
i ntegrati on. J Cl i n Moni t 1999;15:2935.
60. Imhoff M, Kuhl s S. Al arm al gori t hms i n cri ti cal care moni tori ng. Anest h Anal g
2006; 102: 15251537.
[Full text Li nk]
[CrossRef ]
[Medli ne Li nk]
61. West enskow DR, Orr JA, Si mon FH, et al . I ntel l i gent al arms reduce
anesthesi ol ogi st ' s response t i me t o cri t ical f aul ts. Anesthesi ol ogy 1992;77: 1074
1079.
[Medli ne Li nk]
P. 836
Questions
For the f ol lowing quest ions, answer
i f A, B, and C are correct
i f A and C are correct
i f B and D are correct
i s D i s correct
i f A, B, C, and D are correct .
1. Purposes of an al arm include
A. Warni ng of a potenti al or actual abnormal or unusual condi ti on
B. Get t ing att ent ion
C. Transferri ng i nf ormati on
D. Transferri ng l egal responsi bi l i ty f rom t he manuf acturer t o the user
Vi ew Answer2. Probl ems associated wi th determini ng the source of an
al arm include
A. The hearing of the anesthesi a provider
B. Di f fi cul ty i n recognizing tone patt erns
C. Noise l evels i n the operati ng room
D. Audible si gnals t hat do not sound conti nuousl y
Vi ew Answer3. Visual si gnals
A. Gi ve l ess speci f i c i nformat i on than audi bl e signal s
B. May go unrecogni zed for a l onger peri od of t i me than audible si gnals
C. Use cont inuous l i ghts f or more cruci al i nf ormati on
D. Requi re the anesthesi a provider t o be l ooking at the moni tor instead of the
pati ent
Vi ew Answer4. Causes of fal se-posi tive alarms i nclude
A. Acti vat i on by an i nappropri ate devi ce
B. Extraneous sounds t hat sound l ike an alarm si gnal
C. Al arm mal f unct i on
D. Wi del y set l i mi ts
Vi ew Answer5. Means to reduce the incidence of the false-positive alarms
i ncl ude
A. Al t eri ng al arm l imi ts duri ng the procedure
B. Synchroni zi ng moni t ors
C. Del aying the t i me bet ween detect ion of an al arm condi ti on and al arm activati on
D. Decreasi ng the averagi ng t i me
Vi ew Answer6. Concerni ng alarm pri ori tizati on, whi ch of the fol lowing
are true?
A. Low-pri ori t y visual si gnal s need not be suppressed
B. Wi th mul ti pl e al arm condi ti ons, al l al arms wi l l be annunci ated
C. Al l al arms are not equal l y i mportant
D. Al arm pri ori t ies may be i ncreased or decreased.
Vi ew Answer7. The purpose(s) of alarm signals i ncl ude(s)
A. Gai ni ng at tent ion
B. Noti f ying t he operator of the alarm urgency
C. I dent i fying the onset of an alarm condi t i on
D. I dent i fying the device that provi des the al arm
Vi ew Answer8. The characteri stics of a fal se-negati ve alarm include
A. Automati c enabl i ng
B. The alarm may be turned OFF
C. Narrow al arm l i mi t range
D. Fai l ure t o generate a si gnal when t here i s a threat to pati ent saf ety
Vi ew Answer9. Which are some of the functi ons that a smart alarm may
perform?
A. Determining the al arm condi ti on on t he basis of mul ti pl e vari abl es
B. Changi ng t he al arm si gnal generati on del ay
C. Presenti ng a l ist of condi ti ons that may have generat ed the al arm
D. Changi ng the alarm pri ori t y
Vi ew Answer10. Alarm condi ti on logging
A. Shoul d include the val ue of the variable that caused the al arm condi t ion
B. Can hel p t o det ermi ne the cause of t ransi ent al arm condi t ions
C. I s usef ul f or qual i t y assurance
D. Can determi ne when an al arm condi t ion occurred
Vi ew Answer
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5834)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (350)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- CVC Reading PassagesDocument8 pagesCVC Reading PassagesChase Smythe100% (1)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Ultra Dense NetworkDocument27 pagesUltra Dense NetworkYounesNo ratings yet
- Topic 4-Bv2Document77 pagesTopic 4-Bv2hooranghooraeNo ratings yet
- Let's Celebrate Diversity! : English: Level A2+Document10 pagesLet's Celebrate Diversity! : English: Level A2+JAIR DIEGO VIDAURRE QUISPENo ratings yet
- Solution of Assignment 5Document5 pagesSolution of Assignment 5Reza Borah100% (1)
- Bank Management System Source CodeDocument5 pagesBank Management System Source CodetheblueartboxNo ratings yet
- InfoDocument2 pagesInfofukinbobNo ratings yet
- Half-Cell Potential Test From The Upper-Side and The Lower-Side of Reinforced Concrete Slabs: A Comparative StudyDocument6 pagesHalf-Cell Potential Test From The Upper-Side and The Lower-Side of Reinforced Concrete Slabs: A Comparative StudyANNADURAINo ratings yet
- Rollarc 400Document48 pagesRollarc 400m khNo ratings yet
- StaircasesDocument11 pagesStaircasesatiNo ratings yet
- Measurement GER NER GPI - Version 1.0Document8 pagesMeasurement GER NER GPI - Version 1.0Wouter RijneveldNo ratings yet
- Shortest Route ProblemDocument7 pagesShortest Route ProblemkaushalmightyNo ratings yet
- Emerging Horizons in HRM FinalDocument72 pagesEmerging Horizons in HRM Finalprernanew100% (5)
- Lab ReportpdfDocument7 pagesLab ReportpdfStefano FochesattoNo ratings yet
- 937 Soldering Station: Setting The TemperatureDocument1 page937 Soldering Station: Setting The TemperatureSuriawati NordinNo ratings yet
- Demography Is The: Statistical Study Human PopulationDocument17 pagesDemography Is The: Statistical Study Human PopulationYash SejpalNo ratings yet
- 1st Quarter ToolkitDocument6 pages1st Quarter ToolkitDimple BolotaoloNo ratings yet
- 2127 - Mahatma Gandhi Missions College of Engineering, Hingoli RD, NandedDocument8 pages2127 - Mahatma Gandhi Missions College of Engineering, Hingoli RD, NandedAjit DeshmukhNo ratings yet
- Oilfield Products - Valves & Wellheads: YyycwuvtcnkcprkrgnkpgxcnxgeqocwDocument48 pagesOilfield Products - Valves & Wellheads: Yyycwuvtcnkcprkrgnkpgxcnxgeqocwjhonny barrantesNo ratings yet
- 1001076002-HT8911 Datasheet - V1.1Document13 pages1001076002-HT8911 Datasheet - V1.1Zhang EthanNo ratings yet
- Unit 1 Nissim Ezekiel and Eunice de Souza: 1.0 ObjectivesDocument14 pagesUnit 1 Nissim Ezekiel and Eunice de Souza: 1.0 ObjectivesJasmineNo ratings yet
- DMA Actuator Drives For - Motorised Butterfly Valve DMK - Motorised Throttle DMLDocument8 pagesDMA Actuator Drives For - Motorised Butterfly Valve DMK - Motorised Throttle DMLemil_88No ratings yet
- IntroductionDocument15 pagesIntroductionMc Keteqman0% (2)
- Office of The President: Bicol UniversityDocument1 pageOffice of The President: Bicol UniversityElmer BelgaNo ratings yet
- R Reference Manual Volume 1Document736 pagesR Reference Manual Volume 1PH1628No ratings yet
- Contoh Skrip Rakaman AudioDocument2 pagesContoh Skrip Rakaman AudioconankoayNo ratings yet
- Fun With Magnets PDFDocument4 pagesFun With Magnets PDFMohamed SoudhNo ratings yet
- Transducer Engineering Lab ManualDocument44 pagesTransducer Engineering Lab Manualspgmaniarunagiri100% (2)
- Modeling and Simulation of Fluid Catalytic Cracking Unit: Reviews in Chemical Engineering January 2005Document38 pagesModeling and Simulation of Fluid Catalytic Cracking Unit: Reviews in Chemical Engineering January 2005Diyar AliNo ratings yet
- Deflocculation of Concentrated Aqueous Clay Suspensions With SodDocument5 pagesDeflocculation of Concentrated Aqueous Clay Suspensions With SodkhosrosaneNo ratings yet