Professional Documents
Culture Documents
Movement Disorders
Movement Disorders
Uploaded by
Esty JimenezOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Movement Disorders
Movement Disorders
Uploaded by
Esty JimenezCopyright:
Available Formats
Review
Movement disorders and the osmotic demyelination syndrome
Aaron de Souza
*
Department of Neurology, Goa Medical College, Bambolim, Goa 403 202, India
a r t i c l e i n f o
Article history:
Received 9 February 2013
Received in revised form
11 April 2013
Accepted 13 April 2013
Keywords:
Parkinsonism
Osmotic demyelination
Central pontine myelinolysis
Extrapontine myelinolysis
Movement disorders
a b s t r a c t
With the advent of MRI, osmotic demyelination syndromes (ODS) are increasingly recognised to affect
varied sites in the brain in addition to the classical central pontine lesion. Striatal involvement is seen in a
large proportion of cases and results in a wide variety of movement disorders. Movement disorders and
cognitive problems resulting from ODS affecting the basal ganglia may occur early in the course of the
illness, or may present as delayed manifestations after the patient survives the acute phase. Such delayed
symptoms may evolve over time, and may even progress despite treatment. Improved survival of pa-
tients in the last few decades due to better intensive care has led to an increase in the incidence of such
delayed manifestations of ODS. While the outcome of ODS is not as dismal as hitherto believed e with
the acute akinetic-rigid syndrome associated with striatal myelinolysis often responding to dopami-
nergic therapy e the delayed symptoms often prove refractory to medical therapy. This article presents a
review of the epidemiology, pathophysiology, clinical features, imaging, and therapy of movement dis-
orders associated with involvement of the basal ganglia in ODS. A comprehensive review of 54 previously
published cases of movement disorders due to ODS, and a video recording depicting the spectrum of
delayed movement disorders seen after recovery from ODS are also presented.
2013 Elsevier Ltd. All rights reserved.
Since Adams and Victors original description of pontine myeli-
nolysis in alcoholic patients in 1959 [1], the disease subsequently
named osmotic demyelination syndrome (ODS) in recognition of
the importance of osmotic shifts in its pathogenesis has seen sig-
nicant changes indiagnosis, course, and outcomes over the past few
decades [2,3]. Increasingly common ante-mortemdiagnosis after the
advent of magnetic resonance imaging (MRI) has led to a revision of
long-held concepts about the clinical course and prognosis of this
disease. The recognition of osmotic demyelination in locations other
than the central pons provided a pathophysiologic basis for the
frequent association of movement disorders with ODS. These may be
present in the acute phase or manifest as delayed sequelae, after
recovery fromthe initial quadriparesis. With increasing survival from
acute ODS due to better intensive care, it is likely that more delayed
movement disorders will be seen as sequelae [4]. This review de-
scribes the epidemiology, clinical features and prognosis of move-
ment disorders due to ODS in the modern era.
1. Epidemiology and pathophysiology
Hitherto thought to be uncommon, ODS is increasingly reported
today, and has accounted for 0.4e0.56% of admissions to neurology
services at tertiary-care referral centres and 0.06% of all admissions
to the medical service of a general hospital [4e6]. Clinically rec-
ognised ODS may be on the rise possibly due to the inability of some
patients to tolerate rapid increase in sodium levels [2]. Magnetic
resonance imaging (MRI) has enabled ante-mortem diagnosis of
ODS, and has expanded its clinical spectrumwith detection of many
mild, atypical or asymptomatic cases [7e11]. Recent data suggest
that ODS is under-diagnosed: 0.3e1.1% of consecutive unselected
autopsies showed evidence of unsuspected CPMand the proportion
was as high as 9.8e29% in liver transplant recipients and 9.5% in
asymptomatic patients with chronic liver disease [12e17]. Autopsy
ndings and retrospective clinical correlation, as well as studies in
living patients using MRI suggest that many, if not most, cases of
ODS are clinically asymptomatic, possibly due to the small size of
the lesion [2,12,13,18,19]. Thus the true incidence of ODS is un-
known: it has been suggested that this rate may be most accurately
estimated by autopsy series [13]. The fact that ODS, despite the
striking pathological abnormalities seen, was not recognised before
the 1950s suggests that it is an iatrogenic disease: the consequence
of the widespread use of intravenous uid therapy at that time
following the introduction of plastic tubing [16,20].
Recent evidence suggests that the distinctive clinical, patholog-
ical, and radiological features of ODS may not be as characteristic as
once believed, and that the clinical syndrome of ODS may be
expanding to include a wider variety of patients [16]. Central pontine
myelinolysis (CPM) and extrapontine myelinolysis (EPM) are but two
* Tel.: 91 832 249 5085; fax: 91 832 245 8728.
E-mail address: adesouza1@gmail.com.
Contents lists available at SciVerse ScienceDirect
Parkinsonism and Related Disorders
j ournal homepage: www. el sevi er. com/ l ocat e/ parkrel di s
1353-8020/$ e see front matter 2013 Elsevier Ltd. All rights reserved.
http://dx.doi.org/10.1016/j.parkreldis.2013.04.005
Parkinsonism and Related Disorders 19 (2013) 709e716
aspects of the same disease. Initially considered a distinct entity from
CPM, EPM is now well-recognised as the manifestations of ODS
occurring in the brain in locations other than the pons. CPMand EPM
have the same pathology, associations and time course but show
differing clinical features [20]. Although the classic description of
ODS includes the central pontine myelinolytic lesion affecting the
transverse pontocerebellar bres and the long rostrocaudal tracts
[21], histological examination failed to show a pontine lesion e
hitherto the sine qua non of ODS e in 21% of cases of ODS. Extra-
pontine sites were involved in 53% of patients in the same autopsy
series [22]. These involve predominantly subcortical grey matter
nuclei, rather than white matter tracts, and include the cerebellum,
putamina, caudate nuclei, thalami, lateral geniculate bodies, and
fronto-temporal cortex or subcortical white matter. Other locations
include the cerebellar peduncles, fornix, hippocampi and external
capsules [2,5,7,21,23e25]. Initial reports found the cerebellum to be
most frequently involved (33e55%), followed by the thalami and
striatum (34% each) which characteristically spares the globus pal-
lidus although rare cases of presumed myelinolysis restricted to the
pallidum have been reported [2,7,22,23,26,27]. Recent papers have
highlighted the high incidence of striatal lesions in ODS (76e100%)
which may be more common than pontine involvement [5,6]. This
topographical localisation is responsible for the clinical syndrome in
the individual patient, and is useful to make a diagnosis. A variety of
movement disorders result from striatal involvement in ODS
[2,5,22e24] (Table 1).
Early reports stressed the rarity of EPM: in many series, as fewas
10% of patients with CPM had concomitant EPM [15,17,20,23,28].
However, in other published series, the proportion of EPM in ODS
detected on imaging or at autopsy varies from 22 to 80%
[2,5,7,12,19,22]. In specic situations, for example liver transplant
recipients, EPM probably occurs in a higher proportion of patients
than is currently recognised, but is not adequately investigated. It
may be responsible for many cases of acute encephalopathy
following liver transplantation, which are not adequately investi-
gated and no denite cause is found [7]. Similarly, presentation of
EPM as a diffuse encephalopathy may lead to confusion with
persistent hyponatraemic encephalopathy, and thus to its under-
diagnosis. Progression of CPM to involve extrapontine locations on
subsequent MRI or autopsy has also been demonstrated [29]. The
high incidence of EPMin recent studies has been attributed to better
qualityMRI, use of diffusion-weightedimaging, or tothefact that MRI
done later in the course of the illness would detect more lesions [5].
ODS occurs in the setting of signicant medical illness: hypo-
natraemia was associated with 21.5% of all ODS cases reported
between 1986 and 2002 with 39% were associated with alcohol use
[2,18]. Myelin destruction follows osmotic stress resulting from a
failure to compensate for rising plasma tonicity: oligodendrocytes
are most susceptible to physical damage and triggering of apoptosis
following shrinkage [7,20,22]. The end result is circumscribed
spheroidal areas of demyelination, loss of oligodendrogliocytes, and
astrocytic and microglial hyperplasia without inammation or
destruction of neuronal bodies or axons [2,7,9,10,17,19,23,29]. The
predilection for certain areas such as the central pons may be due to
the inexible grid-like arrangement of oligodendrocytes in these
regions, rendering them prone to osmotic damage during electro-
lyte correction [5,30]. ODS is also more common in sites where grey
and white matter interdigitate, and may be due to the chemical
effect of endothelial myelinotoxic factors entering the more
vascular grey matter from blood (particularly after correction of
dyselectrolytaemia as the bloodebrain barrier is often disrupted at
this time) [11,18,26,28,31] or the mechanical effects of vasogenic
oedema or rapid local shifts in osmolarity as ions diffuse across the
bloodebrain barrier [7,17,24,28,29]. Detailed discussions of factors
predisposing to ODS and pathogenesis are available [2,6,7].
2. Movement disorders due to ODS
Clinical or radiologic evidence of neurologic damage due to ODS
begins 0.5e7 days after osmotic shifts occur, but may be delayed by
as long as 16 days [19,23,31,32]. Symptoms may be mild and a high
degree of suspicion is necessary to make the diagnosis [11]. Patients
generally e but not in all cases e exhibit a biphasic course in which
the rst set of symptoms are due to a nonlocalising encephalopathy
due to hyponatraemia, and a period of relative improvement (the
lucent interval) lasting one to seven days separates this from the
subsequent development of ODS [5,6,19,22,29,33]. The disease has
been characterised as a prominent neuro-behavioural disorder due
to white matter disease in the pons and elsewhere in the brain [2].
CPM is classically associated with severe tetraparesis, bulbar palsy,
coma or locked-in state, and less commonly dysarthria, dysphagia,
ophthalmoplegia, or facial paresis [7,8,10e12,17,23,26,34]. The
varied topographic localisation of lesions in EPM leads to many
different clinical symptoms: altered consciousness, confusion,
emotional lability, ataxia, tremor, myoclonus, akinetic mutism,
catatonia, dysautonomia, quadriparesis and others with later pro-
gression to dystonia, choreoathetosis or parkinsonism which is
often poorly responsive to levodopa (Table 2) [2,15,16,19,20,35e39].
Early reports stressed the rarity of extrapyramidal symptoms in
ODS, often thought to be masked by corticospinal or brainstem
dysfunction, but noted delayed development of tremor, rigidity,
bradykinesia, dystonia, choreoathetosis and released reexes
which manifested 10e150 days after ODS begins [20,23,39,40].
Such delayed clinical features are due to ineffective neuronal
reorganisation or repair, and may be progressive and refractory to
treatment [19,20,35,36,38,39]. These delayed movement disorders
may be analogous to delayed dystonia seen with static encepha-
lopathy, and are likely due to neuronal reorganisation with new
synaptic connections, delayed death of affected neurons, denerva-
tion supersensitivity, trans-synaptic degeneration of neural struc-
tures or ongoing myelinolysis [39]. Patients may evolve through a
variety of clinical features: from the initial spastic tetraparesis to
an akinetic-rigid state to choreoathetosis or dystonia (Video)
[7,20,39,41].
Supplementary data related to this article can be found online at
http://dx.doi.org/10.1016/j.parkreldis.2013.04.005.
However, extrapyramidal syndromes are now well recognised
as common early manifestations of ODS: 44e50% of patients with
ODS had parkinsonism at onset, and a further 16% developed
delayed symptoms e either parkinsonism, choreoathetosis or
dystonia [5,6]. Hypokinesia, cogwheel rigidity and tremor were
present with varying combinations and severity. Tremor has been
reported in 33% of all cases of ODS [11], and an anecdotal report of
cortico-basal syndrome is available. The latter patient presented
with asymmetric cogwheel rigidity and bradykinesia with ideo-
motor apraxia and pyramidal signs, but with only CPM on MRI. The
authors were unable to explain the presence of cortical signs or
continued progression with a single pontine lesion [38]. General-
ised dystonia due to striatal myelinolysis has been reported in pa-
tients with hypoadrenalism due to sellar tumours [42]. Akinesia,
catatonia, encephalopathy with altered consciousness, opsoclonus,
emotional lability, and gait disorders have also been attributed to
striatal involvement in other reports [2,15,16,19,20,37e39]. Due to
the combination of hypo- and hyper-kinetic movement disorders
seen in EPM it has been postulated that striatal lesions result in
variable disruption of both direct and indirect striato-pallidal
pathways. Both types of movement disorders can be seen due to
alterations in the rate or pattern of activity in thalamic, pallidal,
subthalamic or cortical neurons [20].
EPMis a rare cause of secondary parkinsonism, which is thought
to result from a relative dopamine deciency due to reduction of
A. de Souza / Parkinsonism and Related Disorders 19 (2013) 709e716 710
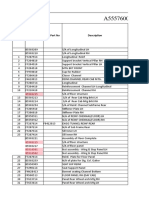
Table 1
Reported cases of movement disorders due to ODS.
Ref Ref Author Year Age Sex CPM EPM:
striatum
EPM: Other
sites
Imaging Autopsy/
Biopsy
HypoNa
Rapid
osmotic
shift
Timing
of MD*
Type
of MD**
Treatment
a
Efcacy
b
Video
[6,41] 6,41 de Souza 2012 50 M e MRI e A P LD, amantadine e
62 F e e MRI e A, D P, later D LD, amantadine
45 F e e MRI e A P,D LD, anticholinergic e
89 F e e MRI e A P LD e e
65 M e Thalamus MRI e A P LD e
[55] 55 Imam 2012 30 M e Thalamus MRI e A P LD e
[43] 43 Toft 2011 42 F e e Midbrain MRI e ? A, D P, later D LD, ropinirole e
[19] 19 Odier 2010 45 M e MRI e A P ? e
66 F e MRI e A P ? ? e
62 F e e MRI e e e A Dyskinesia ? ? e
50 M e MRI e A P, D, M ? e
[25] 25 Gujjar 2010 40 F e Thalamus MRI e e A P, T Pramipexole e
[29] 29 Pietrini 2009 61 F Thalamus MRI e A T e e e
[46] 46 Shin 2009 36 M e MRI e A P LD e
[22] 22 Post 2009 63 F e e MRI e A P ? e
[42] 42 Srimanee 2009 35 M e e MRI e A D ? e e
24 M e e MRI e e A D LD, anticholinergic e
[37] 37 Wu 2009 48 F e e MRI e D P LD
[4] 4 Bhoi 2007 44 M Thalamus MRI e e A D, P, T LD, anticholinergic,
clonazepam,
baclofen
e
62 M Periventricular MRI e e A P Anticholinergic e
36 M Thalamus,
midbrain
MRI e e A, D P, later
D, T
? e
53 F ? MRI e D P, D LD, Botulinum
toxin
e
55 M e e MRI e A P e e
[56] 56 Twardowschy 2007 53 F e MRI e A P e e
[57] 57 Gupta 2007 45 F Thalamus MRI e A P, D Anticholinergic e
[35] 35 Ho 2006 45 M e MRI e A P, T, M ? e
[38] 38 Shamim 2006 61 F e e MRI e D CBS, D ? e e
[23] 23 Sajith 2006 41 F e e MRI e A P LD, baclofen e
[58] 58 Okada 2005 37 F e e MRI e A P e e
[34] 59 Pangariya 2005 50 M Midbrain MRI e ? A P ? e
[59] 60 Tison 2004 e e MRI e A C, D ? ? e
[45] 45 Koussa 2003 59 F e Periventricular,
thalamus
MRI e A P, T,
catatonia
Bromocritpine e
[20] 20 Seah 2002 60 F e MRI e A,D T,M, later
P, D, C
LD, baclofen,
antichol
e
[44] 44 Kim 2002 61 F e MRI e A P LD e
[40] 40 Sullivan 2000 56 M e MRI e A P, T LD e
[28] 28 Nagamitsu 1999 11 F e Thalamus MRI e A P LD e
[36] 36 Seiser 1998 51 F Thalamus MRI e e A, D P,M,
later D
LD, tiapride,
perphenazine
e
[60] 61 Salvesen 1998 F e e MRI e A P ? e
[61] 62 Federlein 1998 39 F e e MRI e A C e e
[62] 63 Tomita 1997 53 M e e MRI e A P, D LD, amantadine,
pergolide,
bromocriptine
anticholinergic,
e e
[63] 64 Pradhan 1995 39 M e Thalamus MRI e e A P ? e
[64] 65 Sadeh 1993 52 F e e e D P LD e
[39] 39 Maraganore 1992 51 F e MRI e D D Anticholinergic,
baclofen
e
55 F MRI e D P ? ?
63 F e MRI e A P,D ? ?
[65] 66 Wu 1992 47 F e e MRI e D D Anticholinergic e
[66] 67 Hirano 1992 43 M e Midbrain,
thalamus
MRI e A P LD e
[67] 68 Salerno 1992 44 F e e MRI e A, D P, later D LD, haloperidol,
clonazepam
e e
[68] 69 Niwa 1991 39 M Subcortical MRI e A P ? ? e
[69] 70 Tinker 1990 66 F e e MRI e A P LD e
[70] 71 Thompson 1989 52 F e e MRI e D D ? ? e
[71] 72 Grafton 1988 57 M e e MRI e D D LD, anticholinergic e e
[72] 73 Dickoff 1988 50 M e MRI e A P ? ?
[73] [74] Stam 1984 e e CT e A P, T ? ? e
HypoNa
: hyponatraemia. *MD: movement disorder; A: acute onset; D: delayed onset. **P: parkinsonism; D: dystonia; T: tremor; M: myoclonus; C: choreoathetosis;
CBS: cortico-basal syndrome.
a
LD: levodopa.
b
e: no improvement; : minimal improvement; : better than minimal improvement; ?: not specied.
A. de Souza / Parkinsonism and Related Disorders 19 (2013) 709e716 711
the presynaptic striatal dopamine transporter and of dopamine
receptors on myelinated bres in the striatum. A symmetric
akinetic-rigid state with or without signicant tremor and/or
postural dysfunction is the commonest movement disorder in
many large series of patients with ODS [5]. Although the midbrain
has been identied as a key area for the development of parkin-
sonism, most reported cases show lesions involving the striatum:
only recently has a case of presumed myelinolysis involving the
substantia nigra been reported [43]. The pathogenesis of the
parkinsonian syndrome is not fully clear [22,44]. Structural imaging
with MRI is unable to delineate the severity of involvement of the
nigrostriatal dopaminergic pathway in individuals with EPM with
parkinsonism and does not correlate well with clinical features
[37]. Studies using single-photon emission computed tomography
(SPECT) have been used to study the functional status of the sub-
stantia nigra and its dopaminergic neurons in patients with
parkinsonismdue to ODS affecting the caudate and putamen. These
have shown a severe reduction in the density of the presynaptic
striatal dopamine transporter, suggesting osmotic damage to the
nigrostriatal pathway in addition to local striatal pathology in EPM
affecting the postsynaptic dopaminergic receptor. Involvement was
more severe in presynaptic neurons, and asymmetry of clinical
signs correlated well with asymmetric reduction in uptake of the
radiotracer ligand [37,43,44]. Increased levels of dopamine me-
tabolites like homovanillic acid in the cerebrospinal uid of a pa-
tient with acute parkinsonism due to EPM without CPM suggest
that the disease causes a reduction of dopamine receptors on
myelinated bres in the striatum. This leads to decreased function
of the striatonigral negative feedback loop and of inhibitory
autoreceptors thereby enhancing dopamine and serotonin secre-
tion, with a consequent rise in cerebrospinal uid levels of dopa-
mine metabolites. The relative dopamine deciency would likely
explain the akinetic-rigid syndrome seen in EPM. Such a model
would not necessarily implicate midbrain or pontine involvement
[28]. Dopaminergic therapy, principally levodopa but also prami-
pexole, leads to clinical improvement similar to that seen in idio-
pathic Parkinsons disease, by activating the remaining dopamine
receptors and ameliorating the relative dopaminergic decit due to
reduced presynaptic nigrostriatal outow [16,28,37,44]. The CSF
level of homovanillic acid should then fall to normal levels, as has
been demonstrated by Nagamitsu and co-workers [28].
Persistent encephalopathy seen in patients with only striatal
involvement may be due to disruption of frontal-subcortical
cognitive circuits or due to small myelinolytic lesions in or near
the cortex which were not detected by MRI. Even patients with
isolated CPM show cognitive dysfunction: this may be due to
concomitant EPM, missed by MRI, or to disruption of cortico-
subcortical circuits or the ascending reticular activating systemdue
to pontine dysfunction [2,19]. That striatal myelinolysis is often
associated with depression serves to reiterate the role that the deep
grey matter plays in the control of affect and emotion. Neuro-
behavioral and cognitive symptoms in EPM may also be due to
arcuate u-bre damage at the cortico-subcortical junction [2].
Catatonia has rarely been reported, either as a brief episode lasting
days before resolving and being replaced with parkinsonian fea-
tures, or two weeks after onset of ODS following the resolution of
spastic tetraparesis [7,45]. Delusions, depression, emotional lability,
disinhibition, paranoia, rage, disorientation, apathy, and mutism
are usually due to disruption of the frontal-subcortical circuits
running through the basal ganglia, and often improve signicantly
[2,16,20,31]. Recovery is often good in patients who survive the
initial illness, but may be incomplete, mimicking a subcortical de-
mentia (mild affection of intelligence, language relatively spared,
problems with executive function and with retrieving memories).
These behavioural symptoms may cause signicant disruption
during the acute illness and during the process of recovery [2].
Primitive reexes are often a prominent feature, even in the
absence of frontal cortical or subcortical white matter lesions, and
may be possibly due to damage to the frontal-subcortical cognitive
and motor circuits by the striatal lesions of EPM that produced
release of these reexes [6]. Most patients with ODS have
severely reduced speech output with hypokinetic dysarthria or
nonspecic slurring of speech even in the absence of pontine le-
sions. Decreased orobuccolingual movements, speech tremor and
poor speech output have all been attributed to striatal dysfunction
in EPM [23]. Mutism and dysphagia have been noted to occur in
32% of patients with ODS even in the absence of bulbar palsy or
quadriparesis [5,34].
3. Role of MRI
By 1972, only 2 of 100 reported cases of ODS had been diagnosed
ante-mortem [10]. The modern scenario is very different, thanks to
the advent of neuroimaging. MRI is decisive in making a diagnosis
of ODS, helping to uncover new cases, delineate the extent of and
trace evolution of the lesion, and correlate progression or regres-
sion with clinical features [8]. It is useful to detect asymptomatic or
mild ODS cases [2,10,16]. Although clinical features of ODS usually
precede MRI changes e indeed MRI may take weeks to become
abnormal e rarely a typical imaging picture can be seen up to a
week before onset of ODS [5,8,11,16,19,24,31,46]. Typically CPM
produces a trident-shaped lesion in the basis pontis from the
pontomedullary junction to the midbrain sparing peripheral tissue
including the corticospinal tracts and ventrolateral tegmentum
[10,23]. No correlation exists between clinical features and MRI
ndings in CPM [24,47]. The lesions of EPM are symmetric and
contemporaneous in age at various sites [7]. Striatal and thalamic
lesions are symmetric, T2- and FLAIR-hyperintense, and T1-
hypointense without contrast enhancement [5,16,37]. In one se-
ries lesions in the basal ganglia were seen in two-thirds of patients
with ODS, while in another, all patients showed striatal lesions [5,6]
(Fig. 1).
Since ODS is due to disturbed uid and osmotic balance, it is not
surprising that DWI abnormalities along with restriction seen on
ADC maps may be useful for early diagnosis. The disease may not be
visible on other sequences even as late as 12 days after onset
[7,15,21,37,46,48]. Low ADC values early on are due to cytotoxic
oedema and a rise in the volume of intracellular uid as compared
with extracellular volume, producing restriction of movement of
water molecules. This restriction may also help indifferentiating ODS
from multiple sclerosis, acute disseminated encephalomyelitis or
certain tumours [15,48,49]. Restriction may increase on subsequent
imaging studies but is not seen beyond three weeks after onset of
ODS: high signal on DWI without restriction may be due to a T2
shine-through effect or bloodebrain barrier breakdown [15,21].
Table 2
Clinical features due to ODS affecting the basal ganglia. See the text for references.
Early manifestations Late manifestations
Symmetric akinetic-rigid state
Dystonia
Tremor
Myoclonus
Corticobasal syndrome
Catatonia
Opsoclonus
Gait disorders
Apathy, akinetic mutism
Primitive reexes
Dysarthria, mutism, dysphagia
Dystonia
Parkinsonism
Chorea, choreoathetosis
Gait disorders
Subcortical dementia
Depression, emotional lability,
paranoia, disinhibition
A. de Souza / Parkinsonism and Related Disorders 19 (2013) 709e716 712
Even though it is very sensitive in detecting lesions of ODS, MRI
may miss small lesions found later at autopsy [19,31]. Repeated
imaging may detect involvement not seen earlier, and therefore
should be done at around two weeks interval in all patients with
suspected ODS [5,19,46,47]. Functional imaging has infrequently
been employed in studying ODS: 18-uorodeoxyglucose positron
emission tomography showed bilateral caudate and putaminal le-
sions [50] with evidence of early hypermetabolism and late hypo-
metablism within the demyelinating lesions [51]. The authors
speculated that active microglia and reactive astrocytes were the
main cause of the increased glucose metabolism.
4. Diagnosis
ODS is easily suspected in the typical clinical setting where a
patient with recent or ongoing electrolyte disturbance, malnutrition,
alcohol abuse, recent liver transplant, severe systemic illness or a
combination of these develops acute quadriparesis, parkinsonism or
coma. However the protean manifestations listed above as well as
the extensive list of conditions known to predispose to ODS neces-
sitate a high index of suspicion, particularly when an individual fails
to recover as expected or develops newpsychiatric symptoms after
a severe illness [7]. Although hyponatraemia is the commonest
factor precipitating ODS, it is by no means always present. The
clinical picture is often confounded by critical illness, neuromuscular
blockade or sedative administration [15]. The acute onset of a sym-
metric akinetic-rigid state with minimal tremor and moderate to
marked axial rigidity; dystonia; seizures; worsening of conscious-
ness in the appropriate clinical setting should prompt consideration
of EPM. Diagnosis in the pre-MRI era was nearly always post-
mortem [10], and even today arriving at a diagnosis of ODS
without the assistance of MRI remains difcult. However a normal
MRI does not rule out ODS: as mentioned above, clinical symptoms
and signs precede MRI changes - often by weeks - and a repeat
imaging study should be obtained after about 15 days if the rst does
not conrm the clinical impression of ODS. The MRI protocol should
include DWI, T2-weighted and FLAIR images. Contrast administra-
tion is unhelpful. Cerebrospinal uid examination is warranted only
to rule out other possible diagnoses. Brainstem auditory evoked
responses were used for diagnosis of CPM before CT scan became
available as they may show a prolonged interpeak latency between
waves I and V, but this is neither sensitive nor specic [18].
As the clinical manifestations of ODS vary according to the
topography of the myelinolytic lesions, a wide differential diagnosis
needs to be considered. Vertebrobasilar stroke, encephalitis or
postencephalitic sequelae, multiple sclerosis, acute disseminated
encephalomyelitis, drug or toxin exposure, prion disorders,
neurodegenerative disorders, or pontine tumours all produce
similar clinical and/or imaging ndings. Symmetric involvement of
the deep nuclei on MRI can be seen in toxic, hypoxic-ischaemic or
other metabolic encephalopathies [23].
5. Management and prognosis
Prevention of ODS is of paramount importance. CPM has been
associated with low, high or normal sodium levels [29] but
hyperosmolarity or rapid osmotic shifts are more important in the
pathogenesis of myelinolysis than the absolute sodium level.
Concomitant malnutrition, alcohol or drug abuse, Addisons dis-
ease, hypoxia, immunosuppression, hypoglycaemia, hypokalaemia
or azotaemia all increase the likelihood of developing ODS after
rapid sodium correction [22,23,52]. Patients with very low serum
Fig. 1. (A) MRI of the brain on 1.5 T system of a patient with symmetric parkinsonism and subcortical dementia due to combined pontine and extrapontine myelinolysis. The axial
T2-weighted (T2W) and FLAIR images show hyperintense lesions in the central pons, putamina and both caudate nuclei. The DWI (b 1000) and ADC images show restricted
diffusion in the striatal lesions. (B) MRI of the brain on 0.2 T system of a patient with symmetric parkinsonism and dystonia with later depression due to extrapontine myelinolysis.
The axial FLAIR images and coronal T2W images show hyperintense lesions in the thalami, putamina and both caudate nuclei. Pons was normal (not shown).
A. de Souza / Parkinsonism and Related Disorders 19 (2013) 709e716 713
sodium levels (<105 mmol/L) [47] and those with sodium levels
<120 mmol/L for >48 h treated with hypertonic saline infusions to
achieve rapid or over-correction are at greatest risk [10,17]. It is well
established that rapid correction following early aggressive treat-
ment is linked to ODS, and to persistent brain dysfunction after
sodium levels return to normal [13,47]. The optimal rate of
correction of sodium is still a matter of controversy: correction is
affected by the severity of hyponatraemia and its symptoms, and it
is not easy to maintain an optimal rate of correction throughout.
Although acute hyponatraemia mandates aggressive and rapid
treatment and rarely causes ODS [17], in case of any doubt it is
safest to assume that the electrolyte disturbance has been present
for more than 48 h, and to proceed with due caution particularly in
malnourished patients [7,32]. Early studies showed that a rise in
sodium levels by >12 mmol/L day or >25 mmol/L in 48 h was a risk
factor for ODS [26,28,29]. The recommended maximum rate of
correction was subsequently lowered to 10 mmol/L day [19,33,37]
but even this rate may be too high [26,29]. Current data indicate
that the risk of ODS increases if sodium levels rise >8 mmol/L day
[7,52] but ODS occurs even with optimal rates of correction
[14,29,52]. This may be due to comorbid conditions, or may be due
to the role played by the absolute sodium level rather in addition to
the rate of correction [28,52]. To prevent this, some authors
recommend even slower correction (<12 mmol/L rise in 48 h or
<0.5 mmol/L rise per hour [18,29]), and avoidance of correction to
normal or elevated sodium levels within 48 h (i.e. maintenance of
mild hyponatraemia) [7,31,47]. Hypokalaemia was the only elec-
trolyte disturbance noted in the original paper describing CPM [1],
and is often noted in patients who eventually develop ODS [29]. It is
not often appreciated that normalisation of potassium levels before
sodium correction commences may minimise the risk of ODS [10]:
a recent series showed that adequate correction of hypokalaemia
was not carried out until after symptoms of ODS began [6].
No specic therapy exists for ODS [10]. Thyrotropin releasing
hormone, plasma exchange, methylprednisolone, and intravenous
immunoglobulin have all been anecdotally effective but no rand-
omised trial has ever been carried out, and the mechanism of
benet is not known. Only supportive care may be justied in the
absence of conrmed efcacy of the above treatment [11]. Steroids
are recommended on the basis of rat experiments in which dexa-
methasone prevented the development of ODS [33]. They prevent
microglial activation stabilising the bloodebrain barrier and sup-
pressing cytokine secretion. Therefore it has been proposed that
steroids be given just before sodium correction in severely hypo-
natraemic patients [2]. Although outcomes from ODS are reported
to improve with steroid therapy, particularly in EPM, the absence of
orid inammation on histological examination casts into doubt
the utility of immunomodulatory treatment [29,53]. ODS may be
prevented by reinduction of mild hyponatraemia if initial symp-
toms appear, and patients at risk of ODS after aggressive osmolar
correction may be rescued with appropriate uid management
before brain injury has occurred [7,16,33].
The movement disorders of EPM represent a treatable mani-
festation of the osmotic demyelination syndrome in that a
rewarding symptomatic improvement can occur with dopami-
nergic treatment in those with parkinsonian features [7]. Although
delayed movement disorders respond poorly to drug treatment
[20], in general parkinsonism resulting from acute ODS shows a
good response to levodopa [7,28]. Levodopa is thought to alleviate
symptoms by activating the remaining dopamine receptors in the
striatum. Dopamine agonists like pramipexole are also reported to
benet patients with EPMwho had a striatal presynaptic dopamine
transporter defect [25]. The presynaptic dopaminergic defect in
EPM resembles that in Parkinsons disease e often with similar
patterns of asymmetry in clinical and imaging data e and explains
the good response to levodopa seen in both conditions [37,44,45].
Clinical improvement has been shown to correspond to normal-
isation of radiotracer ligand uptake on serial SPECT studies after
initial SPECT showed severely reduced presynaptic uptake [37].
Hitherto commonly believed to have a very poor prognosis
[8,52], ODS is more benign than previously thought [15]. The
outcome is not inevitably poor and the disease is no longer as
devastating as it was 50 years ago [16,52]. This is due to early
recognition using MRI, better knowledge of the pathophysiology of
electrolyte disorders, more precise uid management, and better
intensive care techniques [16]. Most patients survive if secondary
complications due to debility like aspiration, sepsis or pulmonary
thromboembolismcan be avoided [2]. From 90 to 100% mortality at
three months in earlier series [10,11,54], with modern intensive
care almost half the patients have a good outcome with 28e39%
recovering completely, and a further 16e34% becoming indepen-
dent for ADL [5,11,19,54]. In paediatric series, 94% of cases prior to
1990 and only 7% of cases from 1990 onward resulted in patient
mortality [3]. Recovery is usually seen early but may be delayed by
as much as four years [22,23]. Hospital stay averaged 28e32 days
[5,6]. Prompt improvement may be due to selective myelin damage
with relative sparing of axons [23] or reversal of neurotransmitter
block in the pons after resolution of vasogenic oedema, while
delayed recovery has been attributed to synaptic plasticity [34].
Good nursing care and aggressive rehabilitative measures are
therefore essential, given the prospect of a good recovery despite an
initially severe decit [10,19].
As the disorder is of diverse aetiologies and often associated
with severe medical illness, outcomes vary [19]. Attempts to
describe prognostic factors in patients with ODS have been largely
unsuccessful: outcome is not correlated with clinical features or the
size of the lesion on MRI [5,7,8,16,42,54]. The size of the lesion on
MRI is not proportional to severity or outcome [8,42]. The abnormal
signal intensity changes usually persist, although normalisation of
the MRI over a period of up to four years has been reported
[16,22,31]. Although some authors have suggested that patients
with normal ADC maps at an early stage have better recovery [46],
this was not conrmed in other series [5,6]. However, some authors
have suggested that the presence of altered consciousness or sei-
zures had a detrimental effect on the outcome [6] and were
indicative of potential mortality, in contrast to other presentations
like ataxia which had a better prognosis [19]. ODS arising as a
complication of severe systemic illness, associated liver dysfunc-
tion, lowsodium and potassium levels at admission, absent lucent
interval, and severe disability at admission and discharge were
predictive of poor outcome [5,6,16]. In keeping with the recent
trends towards improved survival in ODS, a retrospective series of
76 paediatric cases of ODS over 50 years identied the decade in
which the case was reported as the strongest predictor of outcome,
followed by sodium dysregulation and dehydration [3]. Even in
patients who survive the initial illness, neuropsychological abnor-
malities suggesting frontal-subcortical dysfunction persist in most
and may be the only signicant residuumof neurological damage in
as many as a third of survivors, precluding a return to a normal life
[19]. The commonest neurological sequelae in survivors of EPM are
global cognitive defects, extrapyramidal or cortico-bulbar disorders
[45]. Patients with delayed progression of extrapyramidal symp-
toms have a poor prognosis due to ineffective or haphazard reor-
ganisation and repair of neural structures [20].
6. Conclusion
The widespread use of MRI has resulted in increasing recogni-
tion of the association of ODS e in particular EPM e with move-
ment disorders. Parkinsonism and less commonly dystonia are
A. de Souza / Parkinsonism and Related Disorders 19 (2013) 709e716 714
often noted in the initial evaluation of patients with EPM, while
those surviving the acute illness may manifest delayed dystonia,
parkinsonism, choreoathetosis and other movement disorders.
Such delayed movement disorders are likely to become more
common as improvements in intensive care techniques lead to
increased survival of acutely ill patients with ODS. Parkinsonism
often shows a salutary response to dopaminergic therapy, while
delayed manifestations may be refractory to treatment and may
progress despite the physicians best efforts.
Ethical approval
The patient depicted in the video provided written informed
consent to being lmed and for the recording to be used for
teaching and research. The hospital ethics committee of Goa
Medical College approved the article.
Funding
None.
Conict of interest
None.
References
[1] Adams RD, Victor M, Mancall EL. Central pontine myelinolysis. Arch Neurol
Psychiatry 1959;81:154e72.
[2] Kleinschmidt-DeMasters BK, Rojiani AM, Filley CM. Central and extrapontine
myelinolysis. then and now. J Neuropathol Exp Neurol 2006;65:1e11.
[3] Ranger AM, Chaudhary N, Avery M, Fraser D. Central pontine and extrapontine
myelinolysis in children: a review of 76 patients. J Child Neurol 2012;27:
1027e37.
[4] Bhoi KK, Pandit A, Guha G, Barma P, Misra AK, Garai PK, et al. Reversible
parkinsonism in central pontine and extrapontine myelinolysis: a report of
ve cases from India and review of the literature. Neurol Asia 2007;12:101e9.
[5] Kallakatta RN, Radhakrishnan A, Fayaz RK, Unnikrishnan JP, Kesavadas C,
Sarma SP. Clinical and functional outcome and factors predicting prognosis in
osmotic demyelination syndrome(central pontine and/or extrapontine mye-
linolysis) in 25 patients. J Neurol Neurosurg Psychiatry 2011;82:326e31.
[6] de Souza A, Desai PK. More often striatal myelinolysis than pontine? A
consecutive series of patients with osmotic demyelination syndrome. Neurol
Res 2012;34:262e71.
[7] Martin RJ. Central pontine and extrapontine myelinolysis: the osmotic
demyelination syndromes. J Neurol Neurosurg Psychiatry 2004;75:iii22e8.
[8] Laubenberger J, Schneider B, Ansorge O, Gtz F, Hussinger D, Volk B, et al.
Central pontine myelinolysis: clinical presentation and radiologic ndings. Eur
Radiol 1996;6(2):177e83.
[9] Hadeld MG, Kubal WS. Extrapontine myelinolysis of the basal ganglia
without central pontine myelinolysis. Clin Neuropathol 1996;15:96e100.
[10] Kiley MA, King M, Burns RJ. Central pontine myelinolysis. J Clin Neurosci
1999;6:152e7.
[11] Musana AK, Yale SH. Central pontine myelinolysis: case series and review. Wis
Med J 2005;104:56e60.
[12] Razvi SSM, Leach JP. Asymptomatic pontine myelinolysis. Eur J Neurol
2006;13:1261e3.
[13] Newell KL, Kleinschmidt-DeMasters BK. Central pontine myelinolysis at autopsy;
a twelve year retrospective analysis. J Neurol Sci 1996;142:134e9.
[14] Huq S, Wong M, Chan H, Crimmins D. Osmotic demyelination syndromes:
central and extrapontine myelinolysis. J Clin Neurosci 2007;14:684e8.
[15] Kumar S, Fowler M, Gonzalez-Toledo E, Jaffe SL. Central pontine myelinolysis,
an update. Neurol Res 2006;28:360e6.
[16] Brown WD. Osmotic demyelination disorders: central pontine and extrap-
ontine myelinolysis. Curr Opin Neurol 2000;13:691e7.
[17] Luzzio C. Central pontine myelinolysis. Online, http://emedicine.medscape.
com/article/1174329-overview; August 26, 2009 [accessed 14.07.10].
[18] Lampl C, Yazdi K. Central pontine myelinolysis. Eur Neurol 2002;47:3e10.
[19] Odier C, Nguyen DK, Panisset M. Central pontine and extrapontine myeli-
nolysis: from epileptic and other manifestations to cognitive prognosis.
J Neurol 2010;257:1176e80.
[20] Seah ABH, Chan LL, Wong MC, Tan EK. Evolving spectrum of movement dis-
orders in extrapontine and central pontine myelinolysis. Parkinsonism Relat
Disord 2002;9:117e9.
[21] Ruzek KA, Campeau NG, Miller GM. Early diagnosis of central pontine mye-
linolysis with difusion-weighted imaging. Am J Neuroradiol 2004;25:210e3.
[22] Post B, van Gool WA, Tijssen MAJ. Transient parkinsonism in isolated
extrapontine myelinolysis. Neurol Sci 2009;30:325e8.
[23] Sajith J, Ditcheld A, Kati HA. Extrapontine myelinolysis presenting as acute
parkinsonism. BMC Neurol 2006;6:33e5.
[24] Brown WD, Caruso JM. Extrapontine myelinolysis with involvement of the
hippocampus in three children with severe hyperatremia. J Child Neurol
1999;14:428e33.
[25] Gujjar A, Al-Mamari A, Jacob PC, Jain R, Balkhair A, Al-Asmi A. Extrapontine
myelinolysis as presenting manifestation of adrenal failure: a case report.
J Neurol Sci 2010;290:169e71.
[26] Pirzada NA, Ali II. Central pontine myelinolysis. Mayo Clin Proc 2001;76(5):
559e62.
[27] Hsieh CY, Huang CW. Extrapontine myelinolysis in a patient following
correction of hyponatremia. Acta Neurol Taiwanica 2007;16:188e9.
[28] Nagamitsu S, Matsuishi T, Yamashita Y, Yamada S, Kato H. Extrapontine
myelinolysis with parkinsonism after rapid correction of hyponatremia: high
cerebrospinal uid levels of homovanillic acid and successful dopaminergic
treatment. J Neurol Transm 1999;106:949e53.
[29] Pietrini V, Mozzani F, Crafa P, Sivelli R, Cademartiri F, Crisi G. Central pontine
and extrapontine myelinolysis despite careful correction of hyponatremia:
clinical and neuropathological ndings of a case. Neurol Sci 2010;31:227e30.
[30] Riggs JE, Schochet Jr SS. Osmotic stress, osmotic myelinolysis and oligoden-
drocyte topography. Arch Pathol Lab Med 1989;113:1386e8.
[31] McGraw P, Edwards-Brown MK. Reversal of MR ndings of central pontine
myelinolysis. J Comp Assist Tomogr 1998;22:989e91.
[32] Omari A, Kormas N, Field M. Delayed onset of central pontine myelinolysis
despite appropriate correction of hyponatremia. Int Med J 2002;33:273e4.
[33] Lin CM, Po HL. Extrapontine myelinolysis after correction of hyponatremia
presenting as generalised tonic seizures. Am J Emerg Med 2008;26. 632.e5e
636.e5.
[34] Panagariya A, Sureka RK, Udainiya DK. Parkinsonism and recovery in central
and extrapontine myelinolysis. Neurol India 2005;53(2):219e20.
[35] Ho B, Apetauerova D, Thomas C, Arle J, Russell JA. Reversible extrapontine and
central pontine myelinolysis presenting with extrapyramidal features. Mov
Disord 2006;21:585e6.
[36] Seiser A, Schwarz S, Aichinger-Steiner MM, Funk G, Schnider P, Brainin M.
Parkinsonism and dystonia in central pontine and extrapontine myelinolysis.
J Neurol Neurosurg Psychiatry 1998;65:119e21.
[37] Wu YC, Peng GS, Cheng CA, Lin CC, Huang WS, Hsueh CJ, et al. 99m-Tc-
TRODAT-1 and123I-IBZM SPECT studies in a patient with extrapontine mye-
linolysis with parkinsonian features. Ann Nucl Med 2009;23:409e12.
[38] Shamim A, Siddiqui BK, Josephs KA. The corticobasal syndrome triggered by
central pontine myelinolysis. Eur J Neurol 2006;13:82e4.
[39] Maraganore DM, Folger WN, Swanson JW, Ahlskog JE. Movement disorders as
sequelae of central pontine myelinolysis: report of three cases. Mov Disord
1992;7(2):142e8.
[40] Sullivan AA, Chervin RD, Albin RL. Parkinsonism after correction of hypona-
traemia with radiological central pontine myelinolysis and changes in the
basal ganglia. J Clin Neurosci 2000;7(3):256e9.
[41] de Souza A, Desai PK. Delayed chorea after recovery from a symmetric
parkinsonian syndrome due to striatal myelinolysis. J Clin Neurosci 2012;19:
1165e7.
[42] Srimanee D, Bhidayasiri R, Phanthumchinda K. Extrapontine myelinolysis in
preoperative sellar region tumor: report of two cases. J Med Assoc Thai
2009;92:1548e53.
[43] Toft M, Dietrichs E. Levodopa-responsive parkinsonism in probable extrap-
ontine myelinolysis of the mesencephalon. Mov Disord 2011;26:2180e1.
[44] Kim JS, Lee KS, Han SR, Chung YA. Decreased striatal dopamine transporter
binding in a patient with extrapontine myelinolysis. Mov Disord 2003;18:
342e5.
[45] Koussa S, Nasnas R. Catatonia and parkinsonism due to extrapontine myeli-
nolysis following rapid correction of hyponatremia. J Neurol 2003;250:103e5.
[46] Shin HW, Song D, Sohn YH. Normal diffusion-weighted MR imaging predicts a
good prognosis in extrapontine myelinolysis-induced parkinsonism. Mov
Disord 2009;24:1701e3.
[47] Brunner JE, Redmond JM, Haggar AM, Kruger DF, Elias SB. Central pontine
myelinolysis and pontine lesions after rapid correction of hyponatremia: a
prospective magnetic resonance imaging study. Ann Neurol 1990;27:61e6.
[48] Cramer SC, Stegbauer KC, Schneider A, Mukai J, Maravilla KR. Decreased
diffusion in central pontine myelinolysis. Am J Neuroradiol 2001;22:1476e9.
[49] Chu K, Kang DW, Ko SB, Kim M. Diffusion-weighted MR ndings of central
pontine and extrapontine myelinolysis. Acta Neurol Scand 2001;104:385e8.
[50] Tosaka M, Kohga H. Extrapontine myelinolysis and behavioral change after
transsphenoidal pituitary surgery: case report. Neurosurgery 1998;43:933e6.
[51] Roh JK, Nam H, Lee MC. A case of central pontine and extrapontine myeli-
nolysis with early hypermetabolism on 18FDGPET scan. J Korean Med Sci
1998;13:99e102.
[52] Georgy V, Mullhi D, Jones AF. Central pontine myelinolysis following optimal
rate of correction of hyponatraemia with a good clinical outcome. Ann Clin
Biochem 2007;44(Pt 5):488e90.
[53] Naik KR, Saroja AO. Seasonal postpartum hypernatremic encephalopathy with
osmotic extrapontine myelinolysis and rhabdomyolysis. J Neurol Sci
2010;291:5e11.
[54] Menger H, Jorg J. Outcome of central pontine and extrapontine myelinolysis
(n 44). J Neurol 1999;246:700e5.
A. de Souza / Parkinsonism and Related Disorders 19 (2013) 709e716 715
[55] Imam YZ, Saqqur M, Alhail H, Deleu D. Extrapontine myelinolysis-induced
parkinsonism in a patient with adrenal crisis. Case Rep Neurol Med 2012..
http://dx.doi.org/10.1155/2012/327058.
[56] Twardowschy CA, Bertolucci CB, de Macedo Gracia C. Pontine and extrap-
ontine osmotic myelinolysis after the syndrome of inappropriate secretion of
antidiuretic hormone (SIADH) associated with uoxetine. Arq Neuropsiquiatr
2007;65(3-B):858e64.
[57] Gupta R, Goel D, Sangal A, Kukreti R, Singhal A. Extrapontine myelinolysis
without striatal involvement presenting as pathological crying, reversible
parkinsonism and dystonia. Delhi Psy J 2007;10(2):150e3.
[58] Okada K, Nomura M, Furusyo N, Otaguro S, Nabeshima S, Hayashi J. Amelio-
ration of extrapontine myelinolysis and reversible parkinsonism in a patient
with asymptomatic hypopituitarism. Intern Med 2005;44(7):739e42.
[59] Tison FX, Ferrer X, Julien J. Delayed onset movement disorders as a compli-
cation of central pontine myelinolysis. Move Disord 1991;6:171e3.
[60] Salvesen R. Extrapontine myelinolysis after surgical removal of a pituitary
tumour. Acta Neurol Scand 1998;98(3):213e5.
[61] Federlein J, Postert T, Przuntek H, Muller T. Central pontine myelinolysis
causes bilateral loss of deep sensitivity and pseudochoreoathetosis. J Neurol
Neurosurg Psychiatry 1998;65:607e9.
[62] Tomita I, Satoh H, Satoh A, Seto M, Tsujihata M, Yoshimura T. Extra pontine
myelinolysis presenting with parkinsonism as a sequel of rapid correction of
hyponatremia. J Neurol Neurosurg Psychiatry 1997;62:422e3.
[63] Pradhan S, Jha R, Singh MN, Gupta S, Phadke RV, Kher V. Central pontine
myelinolysis following slow correction of hyponatremia. Clin Neurol Neu-
rosurg 1995;97:340e3.
[64] Sadeh M, Goldhammer J. Extrapyramidal syndrome responsive to dopami-
nergic treatment following recovery from central pontine myelinolysis. Eur
Neurol 1993;33:48e50.
[65] Wu CL, Lu CS. Delayed-onset dystonia following recovery from central pontine
myelinolysis. J Formos Med Assoc 1992;91:1013e6.
[66] Hirano F, Makino I, Kimura K, Narita S. A case of parkinsonism due to pontine
and extrapontine myelinolysis. Rinsho Shinkeigaku Clin Neurol 1992;32:
1006e12.
[67] Salerno SM, Kurlan R, Joy SE, Shoulson I. Dystonia in central pontine myeli-
nolysis without evidence of extrapontine myelinolysis. J Neurol Neurosurg
Psychiatry 1993;56:1221e3.
[68] Niwa K, Matsushima K, Yamamoto M, Shinohara Y. Morels laminar necrosis
like ndings on MRI in a case of extra-pontine myelinolysis. Rinsho Shinkei-
gaku 1991;31(3):327e30.
[69] Tinker T, Anderson MG, Anand P, Kermode A, Harding AE. Pontine myeli-
nolysis presenting with acute parkinsonism as a sequel of corrected hypo-
natremia. J Neurol Neurosurg Psychiatry 1990;53:87e8.
[70] Thompson PD, Miller D, Gledhill RF, Rossor MN. Magnetic resonance im-
aging in central pontine myelinolysis. J Neurol Neurosurg Psychiatry
1989;52:675e7.
[71] Grafton ST, Bahls FH, Bell KR. Acquired focal dystonia following recovery from
central pontine myelinolysis. J Neurol Neurosurg Psychiatry 1988;51:1354e5.
[72] Dickoff DJ, Raps M, Yahr M. Striatal syndrome following hyponatremia and its
rapid correction. Arch Neurol 1988;45:112e4.
[73] Stam J, van Oves MHJ, Verbeeten B. Recovery after central pontine myeli-
nolysis. J Neurol 1984;231:52e3.
A. de Souza / Parkinsonism and Related Disorders 19 (2013) 709e716 716
You might also like
- ESPECIFICACIONES D12C Motor VolvoDocument44 pagesESPECIFICACIONES D12C Motor VolvoErika Salinas100% (4)
- Manicure and PedicureDocument38 pagesManicure and PedicureDesiree Clarisse B. DelaCruz100% (4)
- Calcific Tendinitis of The Rotator Cuff State of The Art in Diagnosis PDFDocument8 pagesCalcific Tendinitis of The Rotator Cuff State of The Art in Diagnosis PDFItai IzhakNo ratings yet
- A Brief History of The Vikings - Jonathan ClementsDocument1,459 pagesA Brief History of The Vikings - Jonathan ClementsRodrigo Hky100% (2)
- Metatonin & Pineal GlandDocument107 pagesMetatonin & Pineal GlandSoman100% (2)
- Central Pontine and Extrapontine Myelinolysis. A Systematic ReviewDocument8 pagesCentral Pontine and Extrapontine Myelinolysis. A Systematic ReviewFernando Vazquez SSNo ratings yet
- Conversion of Optic Neuritis To Relapsing Remitting Multiple Sclerosis: A Retrospective Comorbidity Cohort StudyDocument6 pagesConversion of Optic Neuritis To Relapsing Remitting Multiple Sclerosis: A Retrospective Comorbidity Cohort StudymesrurekoseogluNo ratings yet
- Complicated Pyelonephritis Associated With Chronic Renal Stone DiseaseDocument12 pagesComplicated Pyelonephritis Associated With Chronic Renal Stone Diseasecrisvbarros8865No ratings yet
- InternalMedicine Revazut 1Document40 pagesInternalMedicine Revazut 1Roxana Alexandra BogosNo ratings yet
- Internal MedicineDocument36 pagesInternal MedicineRoxana Alexandra BogosNo ratings yet
- Journal Reading 3 - NODocument6 pagesJournal Reading 3 - NOezradamanikNo ratings yet
- Visualizing Cerebral Small Vessel Degeneration During Aging and Diseases Using2Document15 pagesVisualizing Cerebral Small Vessel Degeneration During Aging and Diseases Using2Sofía ValdésNo ratings yet
- 2023, 13 Sept-Dr. I Gede Yasa - Effect of Residual Kidney Function and Dialysis Adequacy On Chronic Pruritus in Dialysis PatientsDocument11 pages2023, 13 Sept-Dr. I Gede Yasa - Effect of Residual Kidney Function and Dialysis Adequacy On Chronic Pruritus in Dialysis PatientsYuyun RasulongNo ratings yet
- Internal MedicineDocument38 pagesInternal MedicineRoxana Alexandra BogosNo ratings yet
- Heart Kidney InteractionDocument11 pagesHeart Kidney InteractionMichael HostiadiNo ratings yet
- Fisiopatologia Paper Haibo 2016Document14 pagesFisiopatologia Paper Haibo 2016Daniela Vargas ZuñigaNo ratings yet
- CSR 2018 s40942-018-0137-8Document5 pagesCSR 2018 s40942-018-0137-8Felix Valerian HalimNo ratings yet
- Frey's Syndrome A Review of Aetiology and TreatmentDocument10 pagesFrey's Syndrome A Review of Aetiology and TreatmentscribdarnabNo ratings yet
- Diagnostics: Uremic Pruritus: From Diagnosis To TreatmentDocument14 pagesDiagnostics: Uremic Pruritus: From Diagnosis To TreatmentsteviaNo ratings yet
- Https:emedicine Medscape Com:article:1227025-PrintDocument18 pagesHttps:emedicine Medscape Com:article:1227025-PrintSalsa BillaNo ratings yet
- TB Tulang 3 PDFDocument6 pagesTB Tulang 3 PDFkeysmeraudjeNo ratings yet
- Complication CSOMDocument8 pagesComplication CSOMOliviastNo ratings yet
- Uveitis Associated With Multiple Sclerosis: Complications and Visual PrognosisDocument4 pagesUveitis Associated With Multiple Sclerosis: Complications and Visual PrognosisnovywardanaNo ratings yet
- Complications of Radiotherapy and Radiosurgery inDocument7 pagesComplications of Radiotherapy and Radiosurgery inzn69h45hn4No ratings yet
- Otogenic Complications of Otitis Media Experience at Tertiary Care HospitalDocument5 pagesOtogenic Complications of Otitis Media Experience at Tertiary Care HospitalAjeng Ratna HaryantiNo ratings yet
- CSCR MedscapeDocument13 pagesCSCR MedscapeFelix Valerian HalimNo ratings yet
- Cardiac Involvement in Systemic SclerosisDocument7 pagesCardiac Involvement in Systemic SclerosisWisnu MataramNo ratings yet
- Omsk KomplikasiDocument10 pagesOmsk KomplikasiYudwari Adhicha Nuredis HarahapNo ratings yet
- CE Update: Wegener's Granulomatosis: A Review of The Clinical Implications, Diagnosis, and TreatmentDocument3 pagesCE Update: Wegener's Granulomatosis: A Review of The Clinical Implications, Diagnosis, and TreatmentAfif FaiziNo ratings yet
- Research: The Profile of Patients With Obstructive Uropathy in Cameroon: Case of The Douala General HospitalDocument6 pagesResearch: The Profile of Patients With Obstructive Uropathy in Cameroon: Case of The Douala General HospitalSidan EmozieNo ratings yet
- Spondt (Spondylodiscitis Diagnosis and Treatment) : Spondylodiscitis Scoring SystemDocument8 pagesSpondt (Spondylodiscitis Diagnosis and Treatment) : Spondylodiscitis Scoring SystemZak harNo ratings yet
- JCM 10 01302Document13 pagesJCM 10 01302Anum ArifNo ratings yet
- Diagnostic Challenge of Tuberculosis in Systemic Lupus ErythematosusDocument9 pagesDiagnostic Challenge of Tuberculosis in Systemic Lupus ErythematosusBelinda Putri agustiaNo ratings yet
- Multiple Organ Syndrome: Clinic BdepartmewtDocument10 pagesMultiple Organ Syndrome: Clinic BdepartmewttommyakasiaNo ratings yet
- COPD and Pulmonary Thromboembolism (For Galley Proof)Document6 pagesCOPD and Pulmonary Thromboembolism (For Galley Proof)Ram AdhikariNo ratings yet
- Sympathetic Ophthalmia: Ocular Immunology and InflammationDocument4 pagesSympathetic Ophthalmia: Ocular Immunology and InflammationOskar MartinezNo ratings yet
- 8584-Article Text-31293-1-10-20110913Document5 pages8584-Article Text-31293-1-10-20110913Maksudur Rahman ShawonNo ratings yet
- Angiosacroma PDFDocument9 pagesAngiosacroma PDFeltouffuNo ratings yet
- Paraneoplastic Syndromes in Small Cell Lung CancerDocument11 pagesParaneoplastic Syndromes in Small Cell Lung CancerFebri Dwi HaryonoNo ratings yet
- SJAMS 66 2563 2566 C PDFDocument4 pagesSJAMS 66 2563 2566 C PDFVitta Kusma WijayaNo ratings yet
- Ref 31 Meningeal LeukemiaDocument9 pagesRef 31 Meningeal LeukemiamuarifNo ratings yet
- CKD PDFDocument7 pagesCKD PDFniaNo ratings yet
- Kelainan PonsDocument5 pagesKelainan PonsDiaz Aulia YunindaNo ratings yet
- Review: Lancet Diabetes Endocrinol 2016Document14 pagesReview: Lancet Diabetes Endocrinol 2016Putri Atthariq IlmiNo ratings yet
- 1Document16 pages1Luis Rafael Suárez U.No ratings yet
- Fcell 09 653138Document30 pagesFcell 09 653138BCR ABLNo ratings yet
- Nusantara Medical Science JournalDocument5 pagesNusantara Medical Science JournalfebifebriantyNo ratings yet
- Medicina 55 00365Document21 pagesMedicina 55 00365Sundas EjazNo ratings yet
- Mitochondrial Myopathies - Clinical Features and Diagnosis - UpToDateDocument37 pagesMitochondrial Myopathies - Clinical Features and Diagnosis - UpToDateNana ShkodinaNo ratings yet
- MoyamoyaDocument11 pagesMoyamoyaSubashssNo ratings yet
- Cardiac Arrest After Small Doses Ropivacaine: Local Anesthetic Systemic Toxicity in The Course of Continuous Femoral Nerve BlockadeDocument5 pagesCardiac Arrest After Small Doses Ropivacaine: Local Anesthetic Systemic Toxicity in The Course of Continuous Femoral Nerve BlockadeAmbot NimoNo ratings yet
- AbstractDocument9 pagesAbstractari wiramaNo ratings yet
- Myelodysplastic Syndromes: Diagnosis, Prognosis, and TreatmentDocument11 pagesMyelodysplastic Syndromes: Diagnosis, Prognosis, and TreatmentTataNo ratings yet
- Spinal Epidural Abscess A Review With Special Emph PDFDocument7 pagesSpinal Epidural Abscess A Review With Special Emph PDFadeNo ratings yet
- Complications of Brain Tumors and Their TreatmentDocument18 pagesComplications of Brain Tumors and Their TreatmentBenedictus Yudha BaskaraNo ratings yet
- Euro J of Neurology - 2023 - Abou Mrad - Central Vein Sign and Paramagnetic Rim Sign From Radiologically Isolated SyndromeDocument7 pagesEuro J of Neurology - 2023 - Abou Mrad - Central Vein Sign and Paramagnetic Rim Sign From Radiologically Isolated SyndromeRenju KuriakoseNo ratings yet
- Progress in Retinal and Eye Research: Contents Lists Available atDocument40 pagesProgress in Retinal and Eye Research: Contents Lists Available atSalsa BillaNo ratings yet
- Link Between Neurodegeneration and Trabecular Meshwork Injury in Glaucomatous PatientsDocument7 pagesLink Between Neurodegeneration and Trabecular Meshwork Injury in Glaucomatous Patientsfaruq azmiNo ratings yet
- Risk of Perforation Using Rigid Oesophagoscopy in The Distal Part of OesophagusDocument4 pagesRisk of Perforation Using Rigid Oesophagoscopy in The Distal Part of OesophagusAgus KarsetiyonoNo ratings yet
- Urolithiasis (Definisi)Document7 pagesUrolithiasis (Definisi)Putri AndiraNo ratings yet
- J Neurosci Rural PractDocument22 pagesJ Neurosci Rural PractSyarifah NurhayatiNo ratings yet
- HSDCDocument5 pagesHSDCCelebre MualabaNo ratings yet
- Denniston Crabb BJO 2017Document7 pagesDenniston Crabb BJO 2017Nindhya PutriNo ratings yet
- A5557600PH79Document31 pagesA5557600PH79Sridharan VenkatNo ratings yet
- Advanced LWRsDocument4 pagesAdvanced LWRsyaprak dönerNo ratings yet
- An0002 Efm32 Hardware Design ConsiderationsDocument16 pagesAn0002 Efm32 Hardware Design ConsiderationsRam SakthiNo ratings yet
- ECE Workshop Practicals Exp No.2Document6 pagesECE Workshop Practicals Exp No.2msdineshpaiNo ratings yet
- Applications of DEsDocument37 pagesApplications of DEsjomgir09No ratings yet
- "Nausicaa" Compression SutureDocument14 pages"Nausicaa" Compression SutureAyu Dyah PrimaningrumNo ratings yet
- DNV-CG-0037 2021-11Document74 pagesDNV-CG-0037 2021-11wfxNo ratings yet
- BLOBITECTUREDocument23 pagesBLOBITECTURESonal TarkasbandNo ratings yet
- Parts Catalog ARDFDocument30 pagesParts Catalog ARDFUlmanu ValentinNo ratings yet
- Kezelesi Utmutato Q3 RF 2010 AngolDocument12 pagesKezelesi Utmutato Q3 RF 2010 AngolClaudiu AdamNo ratings yet
- Construction Terms - English-FilipinoDocument1 pageConstruction Terms - English-FilipinoRhomayne Triz LapuzNo ratings yet
- 2021 - 1 - Alternative Sampling Arrangement For Chemical Composition Tests For General Acceptance (GA) ApplicationDocument5 pages2021 - 1 - Alternative Sampling Arrangement For Chemical Composition Tests For General Acceptance (GA) Applicationkumshing88cwNo ratings yet
- GSB PDFDocument4 pagesGSB PDFsachin sNo ratings yet
- Transformer MaintenanceDocument22 pagesTransformer MaintenanceAugustine Owo UkpongNo ratings yet
- PVC Pressure Pipes and Fittings Catalogue (Pannon Pipe)Document8 pagesPVC Pressure Pipes and Fittings Catalogue (Pannon Pipe)vuthy prakNo ratings yet
- Quantitative Interpretation of The Response of Surface Plasmon Resonance Sensors To Adsorbed FilmsDocument13 pagesQuantitative Interpretation of The Response of Surface Plasmon Resonance Sensors To Adsorbed FilmsKaren Régules MedelNo ratings yet
- Outsmart Your Anxious Brain - Worksheet Diagnosis Guide ExercisesDocument6 pagesOutsmart Your Anxious Brain - Worksheet Diagnosis Guide Exercisesdoppler_100% (1)
- Railway Ballast PerformanceDocument27 pagesRailway Ballast PerformanceSamuel Carlos Sanjuán TorresNo ratings yet
- Motion Information and MediaDocument39 pagesMotion Information and Mediajadeshades12No ratings yet
- RAS AQ DIYproteinskimmer ManualDocument8 pagesRAS AQ DIYproteinskimmer ManualBishri LatiffNo ratings yet
- Sonia Thakker 184 Jignesh Bhatt 105 Rekha Wachkawde 188 Shailendra Singh 178 Pravin Nayak 147 Jibu James 128Document44 pagesSonia Thakker 184 Jignesh Bhatt 105 Rekha Wachkawde 188 Shailendra Singh 178 Pravin Nayak 147 Jibu James 128treakoNo ratings yet
- Methods?: Condoms Internal Condoms Sexually Transmissible Infections (Stis)Document25 pagesMethods?: Condoms Internal Condoms Sexually Transmissible Infections (Stis)Alecia R. CastilloNo ratings yet
- Boundary Wall Design Calculations With PileDocument32 pagesBoundary Wall Design Calculations With PileWahid wrbel100% (1)
- Vol 3 2451-2468 PedreschiDocument18 pagesVol 3 2451-2468 PedreschiAveksaNo ratings yet
- DIAGRAMA - 2007 - NEW YarisDocument1 pageDIAGRAMA - 2007 - NEW YarisLuis M. Valenzuela Arias50% (2)
- Open Web Floor Trusses - MiTek IncDocument7 pagesOpen Web Floor Trusses - MiTek IncinfoNo ratings yet