Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
98 viewsNeonatal Hiatal Hernia - A Rare Case Report
Neonatal Hiatal Hernia - A Rare Case Report
Uploaded by
Agus DarwiyantoThis document reports a case study of a rare case of neonatal hiatal hernia in a newborn female infant. The infant presented with severe respiratory distress at birth. Initial diagnosis was thought to be congenital diaphragmatic hernia based on clinical exam and chest x-ray findings. Surgical exploration was performed but the infant did not improve. A barium study later revealed a sliding hiatal hernia. Hiatal hernias are rarely seen in neonates and can be misdiagnosed as other conditions causing respiratory distress. The infant deteriorated over her 19 day hospital stay and ultimately expired. The case highlights that hiatal hernia should be considered as a differential diagnosis in neonates presenting with respiratory distress.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- The Amazing DayDocument1 pageThe Amazing DayLê Công HậuNo ratings yet
- Yeast Buster To The Rescue (Brochure)Document71 pagesYeast Buster To The Rescue (Brochure)Ема Иван100% (3)
- NCP EsrdDocument2 pagesNCP EsrdAziil LiizaNo ratings yet
- A Case Presentation of Diabetes Mellitus Type 2 Uncontrolled Non-Healing WoundDocument67 pagesA Case Presentation of Diabetes Mellitus Type 2 Uncontrolled Non-Healing Woundashamy acolNo ratings yet
- Caring and The Professional Practice of NursingDocument20 pagesCaring and The Professional Practice of NursingAnaleah MalayaoNo ratings yet
- NCP FdarDocument13 pagesNCP FdarJhaymee Pineda100% (1)
- Related To Limited Financial ResourcesDocument2 pagesRelated To Limited Financial ResourcesDan HizonNo ratings yet
- Acute PainDocument4 pagesAcute PainIvan Jules P. PALMARESNo ratings yet
- St. Paul University Philippines: Community Health Nursing Brgy. Diora-Zinungan, Sta - Ana, CagayanDocument3 pagesSt. Paul University Philippines: Community Health Nursing Brgy. Diora-Zinungan, Sta - Ana, CagayanimnasNo ratings yet
- Module 2 National Immunization Program (Npi) - MihpDocument15 pagesModule 2 National Immunization Program (Npi) - MihpNurhaifa Mocadema100% (1)
- PoliomyelitisDocument28 pagesPoliomyelitisshanel18No ratings yet
- Pathophysiology (Client Base) :: Predisposing Factors: Precipitating FactorsDocument1 pagePathophysiology (Client Base) :: Predisposing Factors: Precipitating Factorsleslie_macasaetNo ratings yet
- Patho DHFDocument2 pagesPatho DHFPhillip GoNo ratings yet
- NCP CaDocument3 pagesNCP CaAnn Benito RNNo ratings yet
- Amoebiasis Case StudyDocument13 pagesAmoebiasis Case StudymelvinpasionaNo ratings yet
- Gordon's Typology of 11 Functional Health PatternDocument12 pagesGordon's Typology of 11 Functional Health PatternJ. ishtelleNo ratings yet
- BSN 2B 2d CASE STUDY FinalDocument35 pagesBSN 2B 2d CASE STUDY Finalann camposNo ratings yet
- Chronic PyelonephritisDocument5 pagesChronic PyelonephritisIsak ShatikaNo ratings yet
- Assess The Knowledge and Attitude On Prevention of Dengue Among The Patients AttendantsDocument6 pagesAssess The Knowledge and Attitude On Prevention of Dengue Among The Patients AttendantsIJAR JOURNALNo ratings yet
- Ao2018 0025Document15 pagesAo2018 0025Klayte TayongNo ratings yet
- Problem IdentificationDocument3 pagesProblem IdentificationkgxviiNo ratings yet
- Burns ActvityDocument5 pagesBurns ActvityJoshua TercenoNo ratings yet
- Final Bsn2f 2c Pcap Case Pres 1Document54 pagesFinal Bsn2f 2c Pcap Case Pres 1Rod Reynon BorceNo ratings yet
- Family Nursing Care Plan TypologyDocument6 pagesFamily Nursing Care Plan TypologyLouwella RamosNo ratings yet
- Pathophysiology of PTBDocument4 pagesPathophysiology of PTBChelsea AquinoNo ratings yet
- Patho of CA & Breast CaDocument3 pagesPatho of CA & Breast CaAngeline EspinasNo ratings yet
- Pathophysiology (Book-Based) : CystitisDocument9 pagesPathophysiology (Book-Based) : CystitisIrish EspinosaNo ratings yet
- University of Cordilleras College of Nursing NCP: Mycobacterium TuberculosisDocument3 pagesUniversity of Cordilleras College of Nursing NCP: Mycobacterium TuberculosisLyn MhoreNo ratings yet
- Unit 1 5ADocument7 pagesUnit 1 5AArvin O-CaféNo ratings yet
- Pa Tho Irritable Bowel SyndromeDocument1 pagePa Tho Irritable Bowel Syndromekaye0403No ratings yet
- MoblityDocument2 pagesMoblityReyes MikkoNo ratings yet
- Journal For MEdical WardDocument8 pagesJournal For MEdical WardValcrist BalderNo ratings yet
- Pathophysiology of PneumoniaDocument2 pagesPathophysiology of PneumoniaJuneNo ratings yet
- Patho DengueDocument3 pagesPatho DengueLindy Shane BoncalesNo ratings yet
- Pathophysiology Cushing S SyndromeDocument4 pagesPathophysiology Cushing S SyndromeMaria Luisa VillalunaNo ratings yet
- NCM 101 GuideDocument78 pagesNCM 101 GuideTimi BCNo ratings yet
- BIOMOLECULES HandoutsDocument4 pagesBIOMOLECULES HandoutsJemuel Bucud LagartoNo ratings yet
- Gestational Conditions 1Document19 pagesGestational Conditions 1MrLarry Dolor100% (1)
- Manuscript-research-Impact With CorrectionsDocument88 pagesManuscript-research-Impact With CorrectionsJay VillasotoNo ratings yet
- NCP Risk For Infection Related To Postop IncisionDocument1 pageNCP Risk For Infection Related To Postop IncisionCharry de VeraNo ratings yet
- TextOfBioethics PDFDocument228 pagesTextOfBioethics PDFNgoc HoangNo ratings yet
- Case 6Document7 pagesCase 6Angel MayNo ratings yet
- Anatomy and Physiology For PudDocument6 pagesAnatomy and Physiology For PudBj Renquijo100% (1)
- Anatomy and Physiology - GallbladderDocument2 pagesAnatomy and Physiology - GallbladderCHi NAiNo ratings yet
- Pathophysiology Dengue Hemorrhagic FeverDocument1 pagePathophysiology Dengue Hemorrhagic FeverShiella Heart Malana100% (1)
- Metoclopramide Drug StudyDocument2 pagesMetoclopramide Drug StudyRem remNo ratings yet
- Pa Tho PhysiologyDocument3 pagesPa Tho Physiologyaprilkow07No ratings yet
- NCP AgnDocument2 pagesNCP AgnMichael Vincent DuroNo ratings yet
- CiprobayDocument2 pagesCiprobayianecunar100% (1)
- Pathophysiology Plueral Effusion Secondary To Pneumonia: GreenDocument7 pagesPathophysiology Plueral Effusion Secondary To Pneumonia: Greenkuro hanabusaNo ratings yet
- A Multidisciplinary Care Map For A Woman in Preterm Labor LazaletaDocument3 pagesA Multidisciplinary Care Map For A Woman in Preterm Labor Lazaletablythe RiveroNo ratings yet
- Annotated Group 2 Impetigo Concept Mapping 1Document30 pagesAnnotated Group 2 Impetigo Concept Mapping 1DHANE ANN CAMPOSANONo ratings yet
- Group 33 Module 7 ManuscriptDocument56 pagesGroup 33 Module 7 ManuscriptMARIA KHIM ROSE BALCITANo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationMary Hope BacutaNo ratings yet
- Icu CPDocument5 pagesIcu CPJezner GamosNo ratings yet
- Nsg. Research Chap. 1 - 3Document38 pagesNsg. Research Chap. 1 - 3John Harvey PerezNo ratings yet
- CeferoximeDocument1 pageCeferoximeGwen Stefanie Lagrimas ValloyasNo ratings yet
- Pathophysiology of Acute AppendicitisDocument1 pagePathophysiology of Acute AppendicitissiarahNo ratings yet
- A. Case Study Thesis-Front Page (Revised)Document10 pagesA. Case Study Thesis-Front Page (Revised)Lopirts NiganiNo ratings yet
- Pre TEST CD Set 1Document5 pagesPre TEST CD Set 1Princess Mae MagadanNo ratings yet
- Pediatric Clinics of North America IIDocument54 pagesPediatric Clinics of North America IIkarenNo ratings yet
- Patient Scenario, Chapter 45, Nursing Care of A Family When A Child Has A Gastrointestinal DisorderDocument93 pagesPatient Scenario, Chapter 45, Nursing Care of A Family When A Child Has A Gastrointestinal DisorderDay MedsNo ratings yet
- Gastric Perforation in Neonates: Analysis of Five Cases: Case ReportDocument3 pagesGastric Perforation in Neonates: Analysis of Five Cases: Case ReportwineniNo ratings yet
- PE Day 2Document3 pagesPE Day 2Joi Joi JoiNo ratings yet
- 30 Mins.Document3 pages30 Mins.Jude NapireNo ratings yet
- HRDDocument16 pagesHRDSuhani jainNo ratings yet
- Final Report of The UNDAF MTR ReportDocument171 pagesFinal Report of The UNDAF MTR ReportSheilaNo ratings yet
- A Nurse AdministratorDocument2 pagesA Nurse AdministratorBethChay LacsonNo ratings yet
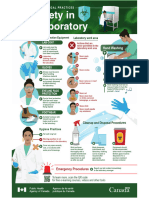
- Biosafety in The LaboratoryDocument1 pageBiosafety in The LaboratoryALFARO CHAT CARMINA ROSARIONo ratings yet
- WFHT Test Your Stress Iq Quiz Answer Key FinalDocument4 pagesWFHT Test Your Stress Iq Quiz Answer Key FinalHailey MallerieNo ratings yet
- Emergency Evacuation PlanDocument4 pagesEmergency Evacuation PlanSujan AugustinNo ratings yet
- Pob East Masterlist 2023Document35 pagesPob East Masterlist 2023Sylvia N. CantoriaNo ratings yet
- Neonatal NotesDocument34 pagesNeonatal Notesgridchan100% (2)
- Tatalaksana Awal Koreksi Cairan Pada Kasus Syok - Dr. Rudy K, SP - PDDocument60 pagesTatalaksana Awal Koreksi Cairan Pada Kasus Syok - Dr. Rudy K, SP - PDmuhammad benyNo ratings yet
- PollutionDocument3 pagesPollutionMARIANA YSABEL SANTILLAN DAVILANo ratings yet
- The Assessment of Malingering Within Forensic Populations PDFDocument71 pagesThe Assessment of Malingering Within Forensic Populations PDFJ. M. Solis100% (1)
- Young Star - One Pager - Version 1.4 - September 2021Document1 pageYoung Star - One Pager - Version 1.4 - September 2021ShihbNo ratings yet
- What Is Bisexual - Google SearchDocument1 pageWhat Is Bisexual - Google SearchYe etNo ratings yet
- Unit 5 English For Nursing IDocument17 pagesUnit 5 English For Nursing IWazif dan AmjadNo ratings yet
- PCL-R II Advanced PCL-R TrainingDocument113 pagesPCL-R II Advanced PCL-R TrainingDr. Anna C. Salter100% (1)
- Hema Complex, Sector - 3, Channi Himmat, Jammu/ Zamzam Complex Rambagh SrinagarDocument2 pagesHema Complex, Sector - 3, Channi Himmat, Jammu/ Zamzam Complex Rambagh SrinagarBaljeet KourNo ratings yet
- Chapter 5 ENGLISHDocument24 pagesChapter 5 ENGLISHvenda novi riantaNo ratings yet
- Nursing Services Manual, Aiims New Delhi - 25!2!21Document91 pagesNursing Services Manual, Aiims New Delhi - 25!2!21praveenjenaNo ratings yet
- Cognitive RoboticsDocument17 pagesCognitive RoboticsJoao Biffe JuniorNo ratings yet
- Physical Education FrameworkDocument342 pagesPhysical Education Frameworkapi-233188563No ratings yet
- Dr. Ysr University of Health Sciences, Ap, Vijayawada - 08 College Wise Allotment List of MSC Nursing Courses, (Phase I), 2022-23Document6 pagesDr. Ysr University of Health Sciences, Ap, Vijayawada - 08 College Wise Allotment List of MSC Nursing Courses, (Phase I), 2022-23Pattem StellaNo ratings yet
- Corn Description and BenefitsDocument4 pagesCorn Description and BenefitsErwin SesioNo ratings yet
- Cerebrovascular Accident - CaseDocument18 pagesCerebrovascular Accident - CaseHazel AsperaNo ratings yet
- KELAS 4 - SMT 2 - Good HabitsDocument23 pagesKELAS 4 - SMT 2 - Good HabitsLefi AdibaNo ratings yet
- Nodir - E - CV - 06 12 2023 - V2Document2 pagesNodir - E - CV - 06 12 2023 - V2shohkingghostNo ratings yet
Neonatal Hiatal Hernia - A Rare Case Report
Neonatal Hiatal Hernia - A Rare Case Report
Uploaded by
Agus Darwiyanto0 ratings0% found this document useful (0 votes)
98 views4 pagesThis document reports a case study of a rare case of neonatal hiatal hernia in a newborn female infant. The infant presented with severe respiratory distress at birth. Initial diagnosis was thought to be congenital diaphragmatic hernia based on clinical exam and chest x-ray findings. Surgical exploration was performed but the infant did not improve. A barium study later revealed a sliding hiatal hernia. Hiatal hernias are rarely seen in neonates and can be misdiagnosed as other conditions causing respiratory distress. The infant deteriorated over her 19 day hospital stay and ultimately expired. The case highlights that hiatal hernia should be considered as a differential diagnosis in neonates presenting with respiratory distress.
Original Description:
Neonatal Hiatal Hernia-
Original Title
Neonatal Hiatal Hernia- A Rare Case Report
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document reports a case study of a rare case of neonatal hiatal hernia in a newborn female infant. The infant presented with severe respiratory distress at birth. Initial diagnosis was thought to be congenital diaphragmatic hernia based on clinical exam and chest x-ray findings. Surgical exploration was performed but the infant did not improve. A barium study later revealed a sliding hiatal hernia. Hiatal hernias are rarely seen in neonates and can be misdiagnosed as other conditions causing respiratory distress. The infant deteriorated over her 19 day hospital stay and ultimately expired. The case highlights that hiatal hernia should be considered as a differential diagnosis in neonates presenting with respiratory distress.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
98 views4 pagesNeonatal Hiatal Hernia - A Rare Case Report
Neonatal Hiatal Hernia - A Rare Case Report
Uploaded by
Agus DarwiyantoThis document reports a case study of a rare case of neonatal hiatal hernia in a newborn female infant. The infant presented with severe respiratory distress at birth. Initial diagnosis was thought to be congenital diaphragmatic hernia based on clinical exam and chest x-ray findings. Surgical exploration was performed but the infant did not improve. A barium study later revealed a sliding hiatal hernia. Hiatal hernias are rarely seen in neonates and can be misdiagnosed as other conditions causing respiratory distress. The infant deteriorated over her 19 day hospital stay and ultimately expired. The case highlights that hiatal hernia should be considered as a differential diagnosis in neonates presenting with respiratory distress.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 4
Curr Pediatr Res Volume 15 Issue 1 51
Curr Pediatr Res 2011; 15 (1): 55-57
Neonatal Hiatal Hernia- A rare case report
Sriram P, Femitha P, Nivedita Mondal, Prakash V, Bharathi B, Vishnu Bhat B
Department of pediatrics, J IPMER, Puducherry, India
Abstract
Hiatal Hernia is rarely seen in a neonate. The mode of presentation in the neonatal period
can be confused with the possibility of a congenital diaphragmatic hernia and other chest
pathologies. The upper gastrointestinal tract contrast study is diagnostic in this disease, but
careful viewing of the plain X-ray of the chest can also suggest the diagnosis.
Key Words: Hiatal hernia, congenital diaphragmatic hernia
Accepted August 2010
Introduction
Hiatal hernia is the herniation of abdominal viscera into
the thoracic cavity through the esophageal hiatus due to
the disorder of gastroesophageal junction and is rarely
seen in neonatal period [1,2]. This entity may result in
misdiagnosis such as congenital diaphragmatic hernia,
eventration of diaphragm, lobar emphysema, pneumato-
coele, pneumothorax, pleural effusion and esophageal
atresia [3, 4]. Rapid diagnosis and treatment is essential.
It avoids lethal complications such as gastric dilatation,
gangrene and perforation, which in turn may lead to car-
diopulmonary arrest. We report a case of hiatal hernia in a
neonate clinically similar to the presentation of a congeni-
tal diaphragmatic hernia.
Case report:
A 25year primi gravida presented in active labour at 37
weeks of gestation to our hospital. There was no apparent
medical illness and there was no history of consanguinity
among parents. There was evidence of fetal distress and a
lower segment caesarean section was conducted. A fe-
male baby was delivered weighing 2.71 Kg, with Apgar
score of 5 at 5 minutes. The baby was stained with thick
meconium and was non vigorous. There was evidence of
severe respiratory distress and peripheral cyanosis. The
airway was cleared and tracheal suctioning was done and
was intubated and shifted to neonatal intensive care unit
where it was immediately ventilated. On examining the
child further, there was evidence severe respiratory dis-
tress and there was shifting of mediastinum to the right
side. The breath sounds on the left side were diminished,
while bowel sounds were heard on the left side of the
chest. The chest was hyperinflated and abdomen was
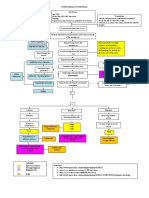
mildly scaphoid. Chest radiography showed abdominal
viscera protruding into the left hemithorax with nasogas-
tric tube in the stomach (Fig 1) and a congenital dia-
phragmatic hernia was suspected. Child was ventilated for
96hours and was then taken for surgery. Exploratory lapa-
rotomy through left subcostal incision was done and the
hernia repair was done. After 48hrs, there was rapid dete-
riation of the condition with reduced air entry on the left
side and Chest x ray was repeated. It showed bowel loops
in the left hemithorax with evidence of fluid collection in
the pleural space on the left side. A repeat Chest X ray on
day 9 of life showed bilateral homogenous opacity with
mediastinum still shifted to the right side and bowel loops
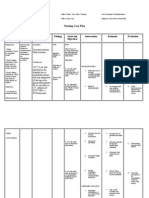
in the left hemithorax. Based on the above findings Bar-
ium study was planned. Barium contrast study revealed
evidence of sliding hiatus hernia protruding into the left
hemi thorax (Fig 2).
Other investigations revealed Haemoglobin of 14.7gm%,
total leukocyte count 8,800 with differential count
showed N60L38E0 M2, Platelet count 2 47,000 and pe-
ripheral smear showed normocytic, normochromic picture
with mild anisocytosis. Sepsis screen was negative and
blood culture was sterile. Blood sugar was 74mg/dl, Urea
18mg/dl, calcium 8.8mg/dl, sodium 138mEq/l, potassium
4.8 mEq/l. The total serum protein was 3.3 g/dl, with al-
bumin 2.5gm/dl, SGOT 23U/L, SGPT 14U/L, and Alka-
line phosphatase of 445U/L. The mothers blood group
was O+ve and babys blood was A1positive. ECHO study
showed situs solitus with small ASD ostium secundum of
3.7mm with left to right shunt without evidence of pul-
monary arterial hypertension.
A Barium study showed evidence of sliding hiatal hernia
with stomach protruding into the left hemithorax. A re-
peat sepsis screen on day 10 life was positive and blood
culture grew candida non albicantes species. Urine culture
also showed evidence of candida glabrata infection sensi-
tive to Amphotericin B.Tracheal aspirate grew kleibsiella
and acinetobacter with resistance to most of the antibiot-
ics. A diagnosis of neonatal hiatal hernia with persistent
pneumonia was made. A second surgical intervention was
Sriram/ Femitha/ Mondal/ Prakash/ Bharathi/ Bhat
Curr Pediatr Res Volume 15 Issue 1 52
planned for repair of the defect of hiatal hernia once the
general condition of the child improves. However the
child worsened and expired after nineteen days of hospital
stay.
Figure 1. Chest x ray showing herniation of abdominal
viscera into left hemithorax
Figure 2. Barium study showing sliding hernia into the
left hemithorax
Discussion
Hiatal hernias have been classified into 4 types as Type 1-
sliding hernia, Type 2- rolling or paraesophageal hernia,
Type 3-a combination of these two types and Type 4- all
or part of the stomach herniates into the thorax, usually
with organoaxial rotation of the stomach [5]. There is an
anatomical defect in the hiatus without any derangement
of the gastroesophageal sphincter mechanism. The most
common of these is a sliding-type hernia accounting for
more than 90% of all the cases of hiatal hernia. Although
a paraesophageal hernia is a rare entity it is more prone to
incarceration, strangulation, complete gastric herniation
with organoaxial volvulus (upside down stomach), and a
perforation of herniated viscera [6,7].
A hiatal hernia is considered as massive if more than one
third of the stomach is located above the diaphragm [8]. It
has been reported that massive hiatal hernias may occur
due to progression of a paraesophageal hiatus hernia [9].
However massive hiatal hernia may also occur due to
sliding hiatal hernia. However, massive hiatus hernia has
been rarely reported in children [10, 11].The main pre-
senting features are respiratory distress, failure to thrive
and poor feeding. Parida and Hall reported higher inci-
dence of congenital anomalies in such children [12]. They
can also be misdiagnosed as lobar pneumonia, pneumato-
coele, pneumothorax, pleural effusion or congenital dia-
phragmatic hernia.
Barium swallow examination, upper gastro-intestinal en-
doscopy and computed tomography are routinely used to
confirm the diagnosis of Hiatus hernia. Manometry, 24
hour pH monitoring and gastric scintigraphy are done to
rule out the presence of gastroesophageal reflux. Chest
radiographs may show opacity in the posterior mediasti-
num with or without an air-fluid level. Barium swallow
will show three or more gastric folds above the diaphragm
hiatus and a pouch of stomach more than two cm above
the hiatus. On CT scan, the diaphragmatic crura are seen
separated by more than 15mm and the protrusion of her-
nia above the diaphragm hiatus. Medical management
include use of antacids, H
2
-receptor antagonist and proton
pump inhibitors and Nissen fundoplication is done in re-
fractory cases.
In our case the neonate presented with severe respiratory
distress at birth and an initial diagnosis of congenital dia-
phragmatic hernia was thought and surgical exploration
was done. But there was no improvement in the child. A
barium study was done which showed sliding hiatal her-
nia. A hiatal hernia repair with fundoplication and gas-
tropexy was planned once the childs condition improves.
However the childs condition worsened after nineteen
days of hospital stay.
Hiatal hernia although rare, should be considered in dif-
ferential diagnosis of severe respiratory distress in a neo-
nate as early intervention will be life saving.
References
1. Anderson KD. Congenital diaphragmatic hernia. In:
Welch KJ , Randolph JG, Ravitch Mm, Rome MC, edi-
tors. Paediatric Surgery 4
th
ed. Chicago: Year Book
medical publishers; 1986. P-599.
2. Senocak ME, Buyukpamukcu N, Hisconmez A. Mas-
sive hiatal hernia containing colon and stomach with
organo-axial volvulus in a child. Turk J Pedaitr 1990;
32:53-58.
3. Al-Arfaj AL, Khwaja MS, Upadhyaya P. Hiatal hernia
in children. Eur J Surg 1991; 157:465-468.
Neonatal Hiatal Hernia- A rare case report
Curr Pediatr Res Volume 15 Issue 1 53
4. Yadav K, Myers NA. Paraesophageal hernia in the
neonatal period-another differential diagnosis of eso-
phageal atresia. Pediatr Surg International 1997; 12:
420-421.
5. Lister J . Hiatal hernia in children. Postgrad Med J
1972; 48: 501-506.
6. Stiefel D, Willi UV, Sacher P, Schwobel MG, Stauffer
UG. Pitfalls in therapy of upside-down stomach. Eur J
Pediatr Surg 2000; 10: 162-166.
7. Maruyama T, Fukue M, Imamura F, Nozue M. Incar-
cerated paraesophageal hernia associated with perfora-
tion of the fundus of the stomach: report of a case. Surg
Today 2001; 31: 454-457.
8. Pearson FG, Cooper JD, Ilves R, Todd TR, J amieson
WR. Massive hiatal hernia with incarceration: a report
of 53 cases. Ann Thorac Surg 1983; 35: 45-51.
9. Geha AS, Massad MG, Snow NJ , Bau AE. A 32-year
experience in 100 patients with giant paraesophageal
hernia: the case for abdominal approach and selective
and antireflux repair. Surgery 2000; 128: 623-630.
10. Arima T, Igarashi M, Shiraishi M, Nakamura T. Hiatal
herniation of colon in an infant. Int Surg 1988; 73: 196-
197.
11. Maziak DE, Todd TR, Pearson FG. Massive hiatal her-
nia: evaluation and surgical management. J Thorac
Cardiac vasc Surg 1998; 115: 53-62.
12. Parida SK, Kriss VM, Hall BD. Hiatal hernia in neona-
tal Marfan syndrome. Am J Med Genet 1997; 72: 156-
158.
Corespondence to:
Vishnu Bhat B.
Department of Pediatrics,
J IPMER, Puducherry 6
India
E-mail: drvishnubhat@yahoo.com
Al Fawaz/ Ahmad
54
You might also like
- The Amazing DayDocument1 pageThe Amazing DayLê Công HậuNo ratings yet
- Yeast Buster To The Rescue (Brochure)Document71 pagesYeast Buster To The Rescue (Brochure)Ема Иван100% (3)
- NCP EsrdDocument2 pagesNCP EsrdAziil LiizaNo ratings yet
- A Case Presentation of Diabetes Mellitus Type 2 Uncontrolled Non-Healing WoundDocument67 pagesA Case Presentation of Diabetes Mellitus Type 2 Uncontrolled Non-Healing Woundashamy acolNo ratings yet
- Caring and The Professional Practice of NursingDocument20 pagesCaring and The Professional Practice of NursingAnaleah MalayaoNo ratings yet
- NCP FdarDocument13 pagesNCP FdarJhaymee Pineda100% (1)
- Related To Limited Financial ResourcesDocument2 pagesRelated To Limited Financial ResourcesDan HizonNo ratings yet
- Acute PainDocument4 pagesAcute PainIvan Jules P. PALMARESNo ratings yet
- St. Paul University Philippines: Community Health Nursing Brgy. Diora-Zinungan, Sta - Ana, CagayanDocument3 pagesSt. Paul University Philippines: Community Health Nursing Brgy. Diora-Zinungan, Sta - Ana, CagayanimnasNo ratings yet
- Module 2 National Immunization Program (Npi) - MihpDocument15 pagesModule 2 National Immunization Program (Npi) - MihpNurhaifa Mocadema100% (1)
- PoliomyelitisDocument28 pagesPoliomyelitisshanel18No ratings yet
- Pathophysiology (Client Base) :: Predisposing Factors: Precipitating FactorsDocument1 pagePathophysiology (Client Base) :: Predisposing Factors: Precipitating Factorsleslie_macasaetNo ratings yet
- Patho DHFDocument2 pagesPatho DHFPhillip GoNo ratings yet
- NCP CaDocument3 pagesNCP CaAnn Benito RNNo ratings yet
- Amoebiasis Case StudyDocument13 pagesAmoebiasis Case StudymelvinpasionaNo ratings yet
- Gordon's Typology of 11 Functional Health PatternDocument12 pagesGordon's Typology of 11 Functional Health PatternJ. ishtelleNo ratings yet
- BSN 2B 2d CASE STUDY FinalDocument35 pagesBSN 2B 2d CASE STUDY Finalann camposNo ratings yet
- Chronic PyelonephritisDocument5 pagesChronic PyelonephritisIsak ShatikaNo ratings yet
- Assess The Knowledge and Attitude On Prevention of Dengue Among The Patients AttendantsDocument6 pagesAssess The Knowledge and Attitude On Prevention of Dengue Among The Patients AttendantsIJAR JOURNALNo ratings yet
- Ao2018 0025Document15 pagesAo2018 0025Klayte TayongNo ratings yet
- Problem IdentificationDocument3 pagesProblem IdentificationkgxviiNo ratings yet
- Burns ActvityDocument5 pagesBurns ActvityJoshua TercenoNo ratings yet
- Final Bsn2f 2c Pcap Case Pres 1Document54 pagesFinal Bsn2f 2c Pcap Case Pres 1Rod Reynon BorceNo ratings yet
- Family Nursing Care Plan TypologyDocument6 pagesFamily Nursing Care Plan TypologyLouwella RamosNo ratings yet
- Pathophysiology of PTBDocument4 pagesPathophysiology of PTBChelsea AquinoNo ratings yet
- Patho of CA & Breast CaDocument3 pagesPatho of CA & Breast CaAngeline EspinasNo ratings yet
- Pathophysiology (Book-Based) : CystitisDocument9 pagesPathophysiology (Book-Based) : CystitisIrish EspinosaNo ratings yet
- University of Cordilleras College of Nursing NCP: Mycobacterium TuberculosisDocument3 pagesUniversity of Cordilleras College of Nursing NCP: Mycobacterium TuberculosisLyn MhoreNo ratings yet
- Unit 1 5ADocument7 pagesUnit 1 5AArvin O-CaféNo ratings yet
- Pa Tho Irritable Bowel SyndromeDocument1 pagePa Tho Irritable Bowel Syndromekaye0403No ratings yet
- MoblityDocument2 pagesMoblityReyes MikkoNo ratings yet
- Journal For MEdical WardDocument8 pagesJournal For MEdical WardValcrist BalderNo ratings yet
- Pathophysiology of PneumoniaDocument2 pagesPathophysiology of PneumoniaJuneNo ratings yet
- Patho DengueDocument3 pagesPatho DengueLindy Shane BoncalesNo ratings yet
- Pathophysiology Cushing S SyndromeDocument4 pagesPathophysiology Cushing S SyndromeMaria Luisa VillalunaNo ratings yet
- NCM 101 GuideDocument78 pagesNCM 101 GuideTimi BCNo ratings yet
- BIOMOLECULES HandoutsDocument4 pagesBIOMOLECULES HandoutsJemuel Bucud LagartoNo ratings yet
- Gestational Conditions 1Document19 pagesGestational Conditions 1MrLarry Dolor100% (1)
- Manuscript-research-Impact With CorrectionsDocument88 pagesManuscript-research-Impact With CorrectionsJay VillasotoNo ratings yet
- NCP Risk For Infection Related To Postop IncisionDocument1 pageNCP Risk For Infection Related To Postop IncisionCharry de VeraNo ratings yet
- TextOfBioethics PDFDocument228 pagesTextOfBioethics PDFNgoc HoangNo ratings yet
- Case 6Document7 pagesCase 6Angel MayNo ratings yet
- Anatomy and Physiology For PudDocument6 pagesAnatomy and Physiology For PudBj Renquijo100% (1)
- Anatomy and Physiology - GallbladderDocument2 pagesAnatomy and Physiology - GallbladderCHi NAiNo ratings yet
- Pathophysiology Dengue Hemorrhagic FeverDocument1 pagePathophysiology Dengue Hemorrhagic FeverShiella Heart Malana100% (1)
- Metoclopramide Drug StudyDocument2 pagesMetoclopramide Drug StudyRem remNo ratings yet
- Pa Tho PhysiologyDocument3 pagesPa Tho Physiologyaprilkow07No ratings yet
- NCP AgnDocument2 pagesNCP AgnMichael Vincent DuroNo ratings yet
- CiprobayDocument2 pagesCiprobayianecunar100% (1)
- Pathophysiology Plueral Effusion Secondary To Pneumonia: GreenDocument7 pagesPathophysiology Plueral Effusion Secondary To Pneumonia: Greenkuro hanabusaNo ratings yet
- A Multidisciplinary Care Map For A Woman in Preterm Labor LazaletaDocument3 pagesA Multidisciplinary Care Map For A Woman in Preterm Labor Lazaletablythe RiveroNo ratings yet
- Annotated Group 2 Impetigo Concept Mapping 1Document30 pagesAnnotated Group 2 Impetigo Concept Mapping 1DHANE ANN CAMPOSANONo ratings yet
- Group 33 Module 7 ManuscriptDocument56 pagesGroup 33 Module 7 ManuscriptMARIA KHIM ROSE BALCITANo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationMary Hope BacutaNo ratings yet
- Icu CPDocument5 pagesIcu CPJezner GamosNo ratings yet
- Nsg. Research Chap. 1 - 3Document38 pagesNsg. Research Chap. 1 - 3John Harvey PerezNo ratings yet
- CeferoximeDocument1 pageCeferoximeGwen Stefanie Lagrimas ValloyasNo ratings yet
- Pathophysiology of Acute AppendicitisDocument1 pagePathophysiology of Acute AppendicitissiarahNo ratings yet
- A. Case Study Thesis-Front Page (Revised)Document10 pagesA. Case Study Thesis-Front Page (Revised)Lopirts NiganiNo ratings yet
- Pre TEST CD Set 1Document5 pagesPre TEST CD Set 1Princess Mae MagadanNo ratings yet
- Pediatric Clinics of North America IIDocument54 pagesPediatric Clinics of North America IIkarenNo ratings yet
- Patient Scenario, Chapter 45, Nursing Care of A Family When A Child Has A Gastrointestinal DisorderDocument93 pagesPatient Scenario, Chapter 45, Nursing Care of A Family When A Child Has A Gastrointestinal DisorderDay MedsNo ratings yet
- Gastric Perforation in Neonates: Analysis of Five Cases: Case ReportDocument3 pagesGastric Perforation in Neonates: Analysis of Five Cases: Case ReportwineniNo ratings yet
- PE Day 2Document3 pagesPE Day 2Joi Joi JoiNo ratings yet
- 30 Mins.Document3 pages30 Mins.Jude NapireNo ratings yet
- HRDDocument16 pagesHRDSuhani jainNo ratings yet
- Final Report of The UNDAF MTR ReportDocument171 pagesFinal Report of The UNDAF MTR ReportSheilaNo ratings yet
- A Nurse AdministratorDocument2 pagesA Nurse AdministratorBethChay LacsonNo ratings yet
- Biosafety in The LaboratoryDocument1 pageBiosafety in The LaboratoryALFARO CHAT CARMINA ROSARIONo ratings yet
- WFHT Test Your Stress Iq Quiz Answer Key FinalDocument4 pagesWFHT Test Your Stress Iq Quiz Answer Key FinalHailey MallerieNo ratings yet
- Emergency Evacuation PlanDocument4 pagesEmergency Evacuation PlanSujan AugustinNo ratings yet
- Pob East Masterlist 2023Document35 pagesPob East Masterlist 2023Sylvia N. CantoriaNo ratings yet
- Neonatal NotesDocument34 pagesNeonatal Notesgridchan100% (2)
- Tatalaksana Awal Koreksi Cairan Pada Kasus Syok - Dr. Rudy K, SP - PDDocument60 pagesTatalaksana Awal Koreksi Cairan Pada Kasus Syok - Dr. Rudy K, SP - PDmuhammad benyNo ratings yet
- PollutionDocument3 pagesPollutionMARIANA YSABEL SANTILLAN DAVILANo ratings yet
- The Assessment of Malingering Within Forensic Populations PDFDocument71 pagesThe Assessment of Malingering Within Forensic Populations PDFJ. M. Solis100% (1)
- Young Star - One Pager - Version 1.4 - September 2021Document1 pageYoung Star - One Pager - Version 1.4 - September 2021ShihbNo ratings yet
- What Is Bisexual - Google SearchDocument1 pageWhat Is Bisexual - Google SearchYe etNo ratings yet
- Unit 5 English For Nursing IDocument17 pagesUnit 5 English For Nursing IWazif dan AmjadNo ratings yet
- PCL-R II Advanced PCL-R TrainingDocument113 pagesPCL-R II Advanced PCL-R TrainingDr. Anna C. Salter100% (1)
- Hema Complex, Sector - 3, Channi Himmat, Jammu/ Zamzam Complex Rambagh SrinagarDocument2 pagesHema Complex, Sector - 3, Channi Himmat, Jammu/ Zamzam Complex Rambagh SrinagarBaljeet KourNo ratings yet
- Chapter 5 ENGLISHDocument24 pagesChapter 5 ENGLISHvenda novi riantaNo ratings yet
- Nursing Services Manual, Aiims New Delhi - 25!2!21Document91 pagesNursing Services Manual, Aiims New Delhi - 25!2!21praveenjenaNo ratings yet
- Cognitive RoboticsDocument17 pagesCognitive RoboticsJoao Biffe JuniorNo ratings yet
- Physical Education FrameworkDocument342 pagesPhysical Education Frameworkapi-233188563No ratings yet
- Dr. Ysr University of Health Sciences, Ap, Vijayawada - 08 College Wise Allotment List of MSC Nursing Courses, (Phase I), 2022-23Document6 pagesDr. Ysr University of Health Sciences, Ap, Vijayawada - 08 College Wise Allotment List of MSC Nursing Courses, (Phase I), 2022-23Pattem StellaNo ratings yet
- Corn Description and BenefitsDocument4 pagesCorn Description and BenefitsErwin SesioNo ratings yet
- Cerebrovascular Accident - CaseDocument18 pagesCerebrovascular Accident - CaseHazel AsperaNo ratings yet
- KELAS 4 - SMT 2 - Good HabitsDocument23 pagesKELAS 4 - SMT 2 - Good HabitsLefi AdibaNo ratings yet
- Nodir - E - CV - 06 12 2023 - V2Document2 pagesNodir - E - CV - 06 12 2023 - V2shohkingghostNo ratings yet