Professional Documents
Culture Documents
1 s2.0 S1110569013000022 Main
1 s2.0 S1110569013000022 Main
Uploaded by
AripinSyarifudin0 ratings0% found this document useful (0 votes)
23 views5 pagesThis study evaluated the predictive value of follicular fluid antimüllerian hormone (AMH) levels for in vitro fertilization (IVF) outcomes in polycystic ovary syndrome (PCOS) patients. The study found that serum AMH levels were higher in PCOS patients and correlated with number of oocytes retrieved and mature oocytes. However, follicular fluid AMH levels did not correlate with number of oocytes, embryo quality, fertilization rate, or clinical pregnancy rate in PCOS patients. The study concludes that serum AMH can predict oocyte yield in PCOS patients undergoing IVF, but follicular fluid AMH is not a useful predictor of IVF outcomes in this group.
Original Description:
pcos
Original Title
1-s2.0-S1110569013000022-main
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis study evaluated the predictive value of follicular fluid antimüllerian hormone (AMH) levels for in vitro fertilization (IVF) outcomes in polycystic ovary syndrome (PCOS) patients. The study found that serum AMH levels were higher in PCOS patients and correlated with number of oocytes retrieved and mature oocytes. However, follicular fluid AMH levels did not correlate with number of oocytes, embryo quality, fertilization rate, or clinical pregnancy rate in PCOS patients. The study concludes that serum AMH can predict oocyte yield in PCOS patients undergoing IVF, but follicular fluid AMH is not a useful predictor of IVF outcomes in this group.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
23 views5 pages1 s2.0 S1110569013000022 Main
1 s2.0 S1110569013000022 Main
Uploaded by
AripinSyarifudinThis study evaluated the predictive value of follicular fluid antimüllerian hormone (AMH) levels for in vitro fertilization (IVF) outcomes in polycystic ovary syndrome (PCOS) patients. The study found that serum AMH levels were higher in PCOS patients and correlated with number of oocytes retrieved and mature oocytes. However, follicular fluid AMH levels did not correlate with number of oocytes, embryo quality, fertilization rate, or clinical pregnancy rate in PCOS patients. The study concludes that serum AMH can predict oocyte yield in PCOS patients undergoing IVF, but follicular fluid AMH is not a useful predictor of IVF outcomes in this group.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 5
ORIGINAL ARTICLE
Follicular uid antimullerian hormone (AMH) does
not predict IVF outcomes in polycystic ovary syndrome
patients
Bushra Abu-Fakher
a,
*
, Faizeh Al-Quobaili
b
, Marwan Alhalabi
c,d
a
Faculty of Pharmacy, Damascus University, Damascus, Syria
b
Department of Clinical Biochemistry and Microbiology, Faculty of Pharmacy, Damascus University, Syria
c
Department of Embryology and Reproductive Medicine, Faculty of Medicine, Damascus University, Syria
d
Assisted Reproduction Unit, Orient Hospital, Damascus, Syria
Received 28 October 2012; accepted 9 December 2012
Available online 4 February 2013
KEYWORDS
Follicular uid;
Antimullerian hormone;
AMH;
IVF;
PCOS
Abstract Introduction: AMH, is a member of the transforming growth factor (TGF-b) produced
by granulosa cells with the highest expression being in small antral follicles. Our objective is to eval-
uate the predictive value of follicular AMH levels as an indicator of IVF outcomes in PCOS
patients.
Material and methods: A total of 63 patients undergoing the IVF trail were recruited for this pro-
spective case-control study. The patients were classied into three groups: Group I: 43 patients with
Polycystic ovary syndrome (PCOS). Group II: 20 normo-ovulatory patients were recruited for the
IVF trail because of the male infertility factor (control group). Group III: consists of 33 patients
from group I recruited to determine the effect of controlled ovarian hyperstimulation (COH) on
serum AMH levels. Serum AMH levels were performed on day 3 of the menstrual cycle whereas
the follicular uid AMH level has been evaluated at the time of oocyte retrieval by enzyme linked
immune-sorbent assay (AMH Gen II ELISA kit, Beckman Coulter, Inc. USA). AMH concentra-
tions were adjusted to its protein content, to avoid possible bias due to FF volume variability.
The relationship between follicular uid AMH (FF AMH) levels and the number of oocytes
retrieved, number of mature oocytes, number of embryos, fertilization and clinical pregnancy rate
were assessed. The demographic data were similar between two groups as regards age and BMI.
Results: Both serum AMH levels and FF AMH levels were signicantly higher in PCOS patients
than in the controls, the values for serum levels were (5.07 3.39 ng/ml, 3.07 2.09 ng/ml) respec-
tively and for follicular uid levels were (67 50.7 ng/g
*
, 38.5 44.4 ng/g) respectively. Serum
*
Corresponding author. Tel.: +963 932749900.
E-mail address: ph.bushra@outlook.com (B. Abu-Fakher).
Peer review under responsibility of Middle East Fertility Society.
Production and hosting by Elsevier
Middle East Fertility Society Journal (2013) 18, 110114
Middle East Fertility Society
Middle East Fertility Society Journal
www.mefsjournal.org
www.sciencedirect.com
1110-5690 2013 Middle East Fertility Society. Production and hosting by Elsevier B.V. All rights reserved.
http://dx.doi.org/10.1016/j.mefs.2012.12.005
AMH levels showed a positive correlation with oocytes retrieved and mature oocyte number, but
there was no signicant correlation with good quality embryo number, fertilization rate or clinical
pregnancy rate in PCOS patients. On the other hand FF AMH levels do not show correlation with
any of the IVF outcomes mentioned above in PCOS patients. Interestingly, the interval change in
serum AMH levels between baseline AMH levels and levels after COH had a signicant predictive
value of pregnancy.
Conclusions: Serum AMH levels can predict the number of the retrieved oocytes and mature
oocytes, whereas FF AMH may not be a valuable predictor for IVF outcomes in PCOS patients.
2013 Middle East Fertility Society. Production and hosting by Elsevier B.V. All rights reserved.
1. Introduction
Polycystic ovary syndrome is the most frequent cause of
anovulatory infertility and hyperandrogenism in young women
(1). It affects upto 10% of reproductive age women (2). PCOS
is characterized by a clustering of hyperandrogenism, hyperin-
sulinemia, hypersecretion of LH, menstrual dysfunction, hir-
sutism, infertility and pregnancy and neonatal complications
(3). Although PCOS patients are typically characterized by
producing an increased number of oocytes, they are often of
poor quality, leading to lower fertilization, cleavage and
implantation rates, and a higher miscarriage rate in PCOS pa-
tients undergoing IVF treatment (4).
AMH is a glycoprotein of the transforming growth factor-
beta (TGF-b) super family. AMH is produced by granulosa
cells from 36 weeks of gestation until menopause, with the
highest expression being in small antral follicles. AMH pro-
duction gradually declines as follicles grow, once follicles reach
a size at which they are dominant it has largely disappeared. Its
removal from these larger follicles appears to be an important
requirement for dominant follicle selection and progression to
ovulation as AMH has an inhibitory role in the ovary, reduc-
ing both primordial follicle initiation and follicle sensitivity to
FSH by the inhibition of aromatase. It is for this reason that
AMH is a focus of interest in polycystic ovary syndrome (5).
Women with PCOS have elevated serum and FF AMH lev-
els versus those of normal controls (6). Recent study suggests
that increased FF AMH in women with PCOS may have
harmful consequences on oocyte quality and maturation, via
an unclear molecular mechanism, but does not have an effect
on pregnancy rates (7), whereas other investigations reveal that
women with PCOS who have lower FF AMH levels have sim-
ilar rates of oocyte maturation, fertilization and embryonic
development compared with normo ovulatory women (8).
To determine whether AMH could play a role in the success
rate of IVF- embryo transfer, this study aims to conrm the
relationship between serum and intrafollicular AMH levels,
and to determine the relationship of intrafollicular AMH to
IVF outcomes in PCOS patients and normal ovulatory women.
2. Materials and methods
A prospective case control study was performed in a total of 43
infertile PCOS patients and 20 normo-ovulatory patients. The
diagnosis of PCOS was based on Rotterdam criteria 2003, the
association of at least two of the three following criteria:
1) Ovulatory disturbance, mainly oligomenorrhea or
amenorrhea.
2) Hyperandrogenism as dened either clinically by hirsut-
ism (modied Ferriman and Gallwey score > 6), or
severe acne/seborrhea, and/or biologically by a testoster-
one serum level greater than 0.7 ng/ml and/or D4-andro-
stenedione greater than 2.2 ng/ml.
3) More than 12 follicles in the 29 mm range in each ovary
with peripheral distribution at ultrasound and/or an
ovarian volume higher than 10 ml were found. Ultra
sound examination was performed with a 7.5-MHz
transvaginal transducer.
All the control population underwent the IVF trail because of
the male factor. Exclusion criteria for the controls were a his-
tory of menstrual disturbances, absence of one of the ovaries,
abnormal serum levels of prolactin or androgens (i.e. serum
testosterone above 0.7 ng/ml and/or D4-androstenedione
above 2.2 ng/ml) and any hormonal treatment during the
3 months before the study.
The patients followed a long protocol for controlled ovar-
ian hyperstimulation which was initiated with the oral contra-
ceptive pill (OCP) on day three or ve of the cycles and
continued with pituitary downregulation by a gonadotropin-
releasing hormone (GnRH) agonist consisting of 0.05 mg of
buserelin in the mid-luteal phase (day 21) of the cycle, given
daily until the day of human chorionic gonadotropin (hCG)
administration.
On day 23 of the new cycle, ovarian stimulation was
started with an injection of recombinant FSH or human men-
opausal gonadotropin (hMG). The gonadotropin dosage was
adjusted according to the follicular growth, which was moni-
tored by ultrasound. The patients were given 10 000 IU of
hCG when at least three follicles became more than 17
18 mm. The oocytes were retrieved 35 h after hCG administra-
tion and IVF/ICSI followed by embryo transfer was per-
formed 3 days after oocyte retrieval.
Blood samples were collected on day three of the menstrual
cycle. On the day of oocyte retrieval, the follicular uid was
aspirated from all follicles (1420) mm, and then it was centri-
fuged at 4000 rpm for 10 min and stored at 80C. All follic-
ular uid samples were examined on the same day to measure
AMH levels using enzyme linked immunosorbent assay (Beck-
man Coulter, Inc. USA). AMH concentrations were adjusted
to its protein content, to avoid possible bias due to FF volume
variability, by the Bradford assay. The assay was performed in
a 96 well plate using Bradfords reagent. Suitable dilutions of
bovine serum albumin (BSA) 1 lg/ml were used as standard
solutions. All FF samples were diluted 250 times, the absor-
bance of standard and unknown solutions were determined
using a spectrophotometer. The concentrations of AMH in fol-
Follicular uid antimullerian hormone (AMH) does not predict IVF outcomes in polycystic ovary syndrome patients 111
licular uid were presented as nanogram per gram (ng/g) of
protein.
3. Statistical analysis
The data were analyzed with MedCalc
v12.2.1. Data were ex-
pressed as mean standard deviation. Comparison of the
means was performed by the MannWhitney U test while
the degree of association between continuous variables was
calculated by the Spearmans correlation coefcient.
A p value <0.05 was considered statistically signicant.
4. Results
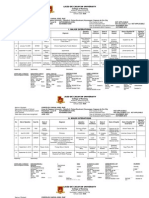
Demographic characteristics of each group (age, BMI, serum
AMH, FF AMH, retrieved oocyte number, mature oocyte
number, embryos number and fertilization rate are shown in
Table 1.
As expected PCOS patients had signicantly higher serum
AMH levels than controls (5.07 3.9 ng/ml, 3.07 2.09 ng/
ml) respectively (p < 0.01). On the other hand FF AMH levels
were signicantly higher in PCOS patients compared to the
controls (67 50.7 ng/g, 38.5 44.4 ng/g) respectively
(p < 0.05). Serum AMH levels were negatively correlated to
age in the control group (r =0.45, p = 0.04) but not in
PCOS patients. (r is Spearman correlation coefcient).
In PCOS patients, serum AMH levels were positively corre-
lated to the number of oocytes retrieved (r = 0.39, p = 0.01)
and the number of mature oocytes (r = 0.334, p = 0.03) (Fig-
ure 1) but not to the number of total embryos or the fertilization
rate, whereas follicular uid AMH levels were not signicantly
correlated to any of the IVF outcomes mentioned above.
Similar results were found in normo ovulatory women; ser-
um AMH levels were positively correlated to oocytes retrieved
(r = 0.513, p = 0.02) mature oocytes (r = 0.615, p = 0.002)
(Figure 1) and embryo number (r = 0.625, p = 0.002).
FF AMH levels were not signicantly correlated to any of
the IVF outcomes as well. Both serum and FF AMH levels
had not a signicant predictive value of pregnancy. But inter-
estingly the interval change between baseline serum AMH lev-
els and levels after controlled ovarian hyperstimulation (values
are shown in Table 2) had a signicant predictive value of
pregnancy.
The predictive potency of the AMH interval change was
tested by the Receiver operating characteristic (ROC) proce-
dure. The area under the curve was 0.697. Several cutoff values
of AMH interval change were analyzed in terms of specicity
and sensitivity from the ROC curve data (Figure 2).
Table 3. Showed that the best adjustment between specic-
ity (92%) and sensitivity (54%) was obtained with a cutoff va-
lue of 54.7%.
5. Discussion
The nding of increased AMH levels in both follicular uid
and the serum of PCOS patients compared with controls can
be explained with the fact that PCOS patients have increasing
number of small antral follicles which are the major sites of
producing AMH and further more by the nding of Pellat
et al. who demonstrated that AMH production was on average
75 times higher per granulosa cell from anovulatory polycystic
ovaries than from normal cells (9). Our nding is in agreement
with the study of Fallat et al. who reported that the level of
AMH in the follicular uid and serum of patients with PCOS
undergoing IVF was signicantly higher than that in patients
with endometriosis or pelvic adhesions (10). We found a neg-
ative correlation between age and serum AMH only in the con-
trol group whereas FF AMH levels remain unaffected by age,
this nding is in agreement with both Das M et al. (11) and
Pigny et al. (6).
We found that serum AMH levels in PCOS patients can
predict oocyte quantity and quality (positive correlation with
mature oocytes) and this nding is in accordance with both
Arabzadeh et al. (12) and Aleyasin et al. (13).
No correlation between FF AMH and any of IVF out-
comes mentioned before were found in the PCOS group, this
is partially in agreement with Desforges who suggests that in-
creased FF AMH in women with PCOS may have harmful
consequences on oocyte quality but does not have an effect
Figure 1 Relationship between serum AMH on day three and
the number of mature oocytes in both PCOS and control groups.
Table 1 Clinical and biological features of patients.
Controls
(n = 20)
PCOS patients
(n = 43)
p-value
Age (year) 29.2 6.2 29.2 5.2 NS
BMI (kg/m
2
) 25.5 3.9 26.3 6.2 NS
sAMH (ng/ml) 3.07 2.09 5.07 3.39 0.004
FF AMH (ng/g) 38.5 44.4 67 50.7 0.02
Retrieved oocyte no. 14.4 8.2 20.1 11.2 0.05
Mature oocyte no. 10.1 5.3 13.3 8.6 0.04
Total embryos no. 8 4.3 13.2 9.1 0.04
Fertilization rate 84.2 19.4 83.8 21.7 NS
*NS = non-signicant; Values are expressed as the mean SD.
112 B. Abu-Fakher et al.
on pregnancy rates (7). Mashiach found that women with
PCOS who have lower FFAMH levels have similar rates of oo-
cyte maturation, fertilization, and embryonic development
compared with ovulating women (14). On the other hand, con-
icting results were obtained from Pabuccu 2009 who demon-
strated better fertilization, implantation and clinical pregnancy
rates in the PCOS group with highest FFAMH concentration
compared with any other group with a lower concentration (8).
In normo-ovulatory women, we found that serum AMH
levels could be a good predictor for oocyte quantity and qual-
ity (positive correlation with maturation rate) and furthermore
for embryo number, and this is in agreement with Vanrooij
et al. 2002 who demonstrated that serum AMH levels are a
good predictor of retrieved oocytes (15) and with Arabzadah
2010 who found that serum AMH levels can predict both the
quantity and quality of oocytes (12). FF AMH levels do not
relate to any of the IVF outcomes in PCOS patients and this
is in agreement with Yilmaz 2012 who showed that there is
no signicant correlation between FF AMH and IVF out-
comes in patients underwent IVF for male infertility or unex-
plained infertility(16). Fanchin et al. suggest that FF AMH
concentrations are only strongly and positively associated with
oocyte quality and implantation rates, but not with fertiliza-
tion rate, and embryo morphology in normal ovulation (17)
and this conict can be explained by the differences in the pa-
tients groups since Fanchin et al. studied non PCOS infertile
patients who underwent the IVF trial.
There are conicting results about the relation between
AMH levels and pregnancy, the most recent studies demon-
strate that Clinical pregnancy rates were lower in the high
AMH group than that of the low and average groups but this
difference was only close to statistical signicance Xi et al.
2012 (18), whereas Yilmaz 2012 found that FF AMH levels
can predict the recovery of oocytes but not oocyte quality, em-
bryo quality or pregnancy in non-obese non-hyperandrogene-
mic PCOS patients (16). Desforges 2009 demonstrated that the
AMH levels were signicantly lower in patients who began a
pregnancy (7).
So, we concluded that AMH may not be a valuable predic-
tor for outcomes success in PCOS patients and normo-ovula-
tory women undergoing IVF. Other randomized control
studies are needed.
6. Conict of interest
None.
References
(1) Franks S. Polycystic ovary syndrome. N Engl J Med
1995;333:85361.
(2) Norman R, Dewailly D, Legro R, Hickey T. Polycystic ovary
syndrome. Lancet 2007;370:68597.
(3) Moran L, Teede H. Metabolic features of the reproductive
phenotypes of polycystic ovary syndrome. Hum Reprod Update
2009;15:47788.
(4) Boomsma CM, Fauser BCJM, Macklon NS. Pregnancy compli-
cations in women with Polycystic ovary syndrome. Semin Reprod
Med 2008;26:7284.
(5) Pellatt L, Rice S, Mason H. Anti-Mullerian Hormone and
polycystic ovary syndrome: a mountain too high. Reproduction
2010;139:82533.
(6) Pigny P, Merlen E, Robert Y, Cortet-Rudelli C, Decanter C,
Jonard S, Dewailly D. Elevated serum level of Anti-Mu llerian
hormone (AMH) in polycystic ovarysyndrome: relationship to the
ovarian follicle excess and to the follicular arrest. J Clin
Endocrinol Metab 2003;88:595762.
(7) Desforges-Bullet V, Gallo C, Lefebvre C, Pigny P, Dewailly D,
Jonard CJ. Increased anti mullerian hormone and decreased FSH
levels in follicular uid obtained in women with polycystic ovaries
at the time of follicle puncture for in vitro fertilization. Fertil
Steril 2010;94:198204.
Table 2 Serum AMH interval change.
Baseline serum AMH levels
(ng/ml)
Serum AMH after COH
(ng/ml)
Interval change
(%)
PCOS patients
a
(n = 33) 5.4 3.4 1.9 1.3 60.8 20.9
Controls
a
(n = 20) 3.07 2.09 1.04 1.06 68.7 16.6
a
mean SD.
Figure 2 ROC curve for AMH interval change.
Table 3 ROC curve data.
AMH interval change (%) Specicity (%) Sensitivity (%)
36.8 20.8 100
47.1 37.5 96
54.7 54.1 92
68.4 58.3 48
80.4 91.6 28
Follicular uid antimullerian hormone (AMH) does not predict IVF outcomes in polycystic ovary syndrome patients 113
(8) Pabuccu R, Kaya C, Caglar GS, Oztas E, Satiroglu H. Follicular-
uid anti-Mullerian hormone concentrations are predictive of
assisted reproduction outcome in PCOS patients. Reprod Biomed
Online 2009;19:6317.
(9) Pellatt L, Hanna L, Brincat M, Galea R, Brain H, Whitehead S,
Mason H. Granulosa cell production of anti-Mullerian hormone
is increased in polycystic ovaries. J Clin Endocrinol Metab
2007;92:2405.
(10) Fallat ME, Siow Y, Marra M, Cook C, Carrillo A. Mullerian-
inhibiting substance in follicular uid and serum: a comparison of
patients with tubal factor infertility, polycystic ovary syndrome,
and endometriosis. Fertil Steril 1997;67:9625.
(11) Das M, Gillot D, Saridogan E, Djahanbakhch O. Anti-Mullerian
hormone is increased in follicular uid from unstimulated ovaries in
womenwithpolycysticovarysyndrome. HumReprod2008;23:21226.
(12) Arabzadeh S, Hossein G, Rashidi B, Hosseini M, Zeraati H.
Comparing serum basal and follicular uid levels of anti-
Mu llerian hormone as a predictor of in vitro fertilization
outcomes in patients with and without polycystic ovary syn-
drome. Ann Saudi Med 2010;30:4427.
(13) Aleyasin A, Aghahoseini M, Mokhtar S, Fallahi P. Anti-
mullerian hormone as a predictive factor in assisted reproductive
technique of polycystic ovary syndrome patients. Acta Med Iran
2011;49(11):71520.
(14) Mashiach R, Amit A, Hasson J, Amzalzg S, Almog B, Ben-Yosef
D, et al. Follicular uid levels of anti-Mullerian hormone as a
predictor of oocyte maturation, fertilization rate, and embryonic
development in patients with polycystic ovary syndrome. Fertil
Steril 2010;93:2299302.
(15) Van Rooij IA, Broekmans FJ, Te Velde ER, Fauser BC, Bancsi
LF, Jong FH, Themmen AP. Serum AMH levels: a novel measure
of ovarian reserve. Hum Reprod 2002;17:306571.
(16) Yilmaz N, Uygur D, Dogan M, Ozgu E, Salman B, Mollamahm-
utoglu L. The effect of follicular antimullerian hormone levels of
non-obese, non-hyperandrogenemic polycystic ovary syndrome
patients on assisted reproduction outcome. Gynecol Endocrinol
2012;28(3):1625.
(17) Fanchin R, Mendez Lozano DH, Frydman N, Gougeon A, di
Clemente N, Frydman R, Taieb J. Anti-Mullerian hormone
concentrations in the follicular uid of the preovulatory follicle
are predictive of the implantation potential the ensuing embryo
obtained by in vitro fertilization. J Clin Endocrinol Metab
2007;92:1796802.
(18) Xi W, Gong F, Lu G. Correlation of serumAnti-Mu llerian hormone
concentrations on day 3 of the in vitro fertilization stimulation cycle
with assisted reproduction outcome in polycystic ovary syndrome
patients. J Assist Reprod Genet 2012;29(5):397402.
114 B. Abu-Fakher et al.
You might also like
- The Use of Hormonal Contraceptives in Fertility Treatments - A Committee OpinionDocument7 pagesThe Use of Hormonal Contraceptives in Fertility Treatments - A Committee Opinionjorge nnNo ratings yet
- Gynaecological Ultrasound in Clinical PracticeDocument247 pagesGynaecological Ultrasound in Clinical Practiceyulb_1100% (5)
- Lesson Plan Ectopic PregnancyDocument3 pagesLesson Plan Ectopic PregnancyRimaNo ratings yet
- AMC Obstetrics TopicsDocument29 pagesAMC Obstetrics TopicsMoe Zaw Lin100% (1)
- Palast1 +223052021 2Document784 pagesPalast1 +223052021 2school adressNo ratings yet
- Pelvic TuberculosisDocument11 pagesPelvic TuberculosisAmalia Zulfa AmandaNo ratings yet
- Low Antimullerian Hormone Levels Improve Fertility Outcome in Patients With Polycystic Ovary Syndrome 1665Document5 pagesLow Antimullerian Hormone Levels Improve Fertility Outcome in Patients With Polycystic Ovary Syndrome 1665GayathriMaranNo ratings yet
- Lin 2013Document7 pagesLin 2013Siti NurfauzianaNo ratings yet
- Lukaszuk Et Al. - 2014 - Anti-Müllerian Hormone (AMH) Is A Strong Predictor of Live Birth in Women Undergoing Assisted Reproductive TDocument6 pagesLukaszuk Et Al. - 2014 - Anti-Müllerian Hormone (AMH) Is A Strong Predictor of Live Birth in Women Undergoing Assisted Reproductive TKrzysztof ŁukaszukNo ratings yet
- 3e03436a-b0ee-47c0-810d-24373fbc6adaDocument29 pages3e03436a-b0ee-47c0-810d-24373fbc6adaCẩm VânNo ratings yet
- Out PDFDocument7 pagesOut PDFYuli HdyNo ratings yet
- Associations Between Free Fatty Acids, Cumulus Oocyte Complex Morphology and Ovarian Function During in Vitro FertilizationDocument5 pagesAssociations Between Free Fatty Acids, Cumulus Oocyte Complex Morphology and Ovarian Function During in Vitro FertilizationAdeodata LilyNo ratings yet
- Metformin Monotherapy in Lean Women With Polycystic Ovary SyndromeDocument5 pagesMetformin Monotherapy in Lean Women With Polycystic Ovary SyndromeQuratul AyunNo ratings yet
- Laparoscopic ClomipenDocument5 pagesLaparoscopic ClomipenHar YudhaNo ratings yet
- Medip, IJRCOG-3288 ODocument5 pagesMedip, IJRCOG-3288 Ozulva azizaNo ratings yet
- Relationship Between Anti-Müllerian Hormone, Antral Follicle Count, Thyroid Hormone, Age and BMI in Patients With Polycystic Ovary SyndromeDocument7 pagesRelationship Between Anti-Müllerian Hormone, Antral Follicle Count, Thyroid Hormone, Age and BMI in Patients With Polycystic Ovary SyndromeInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Age-Related Normograms of Antimullerian Hormone Level in Healthy Repoductive Woman A Single Center StudyDocument12 pagesAge-Related Normograms of Antimullerian Hormone Level in Healthy Repoductive Woman A Single Center StudyRosdi AbdullahNo ratings yet
- Jurnal Ketokonazol Ade 2 PDFDocument5 pagesJurnal Ketokonazol Ade 2 PDFSyaifulBahriNo ratings yet
- Role of Anti-Müllerian Hormone in The Pathogenesis of Polycystic Ovary SyndromeDocument9 pagesRole of Anti-Müllerian Hormone in The Pathogenesis of Polycystic Ovary SyndromeHAVIZ YUADNo ratings yet
- Med Term JounralDocument6 pagesMed Term JounralKaroline FarleyNo ratings yet
- Early Follicular Phase LH Concentration PDFDocument7 pagesEarly Follicular Phase LH Concentration PDFgeorgianaNo ratings yet
- TestosteronDocument8 pagesTestosteronAndrea VargaNo ratings yet
- Effects of Anti M Llerian Hormone and Follicle Sti - 2014 - Taiwanese Journal ofDocument4 pagesEffects of Anti M Llerian Hormone and Follicle Sti - 2014 - Taiwanese Journal ofSami KahtaniNo ratings yet
- Jbra1117 PDFDocument4 pagesJbra1117 PDFAgusNo ratings yet
- ijrb-16-299Document6 pagesijrb-16-299ttriayatiNo ratings yet
- JurnalDocument6 pagesJurnalWidya Rachmania PutriNo ratings yet
- S0015028213X00202 S0015028213023716 Main PDFDocument1 pageS0015028213X00202 S0015028213023716 Main PDFAnton ArifinNo ratings yet
- Mono-Ovulation in Women With Polycystic Ovary Syndrome: A Clinical Review On Ovulation InductionDocument21 pagesMono-Ovulation in Women With Polycystic Ovary Syndrome: A Clinical Review On Ovulation InductionnandaNo ratings yet
- Humanities-Low Dose Gonadotropin Protocol For Ovulation Induction in Low Resource Centre-Dr A. I. IsawumiDocument8 pagesHumanities-Low Dose Gonadotropin Protocol For Ovulation Induction in Low Resource Centre-Dr A. I. IsawumiBESTJournalsNo ratings yet
- Fertility & Sterility: A A B B C A ADocument1 pageFertility & Sterility: A A B B C A ASri HariNo ratings yet
- Relationship Between The Duration of Sexual Abstinence and Semen Quality: Analysis of 9,489 Semen SamplesDocument7 pagesRelationship Between The Duration of Sexual Abstinence and Semen Quality: Analysis of 9,489 Semen SamplesReski AdeliaNo ratings yet
- Dengan Keberhasilan Stimulasi OvariumDocument7 pagesDengan Keberhasilan Stimulasi OvariumSri IriantiNo ratings yet
- ARTDocument36 pagesARTTtyyfff Fyyu89-No ratings yet
- GENETIC COUNSELLING (FARHEEN KHAN MSC 1st Year)Document8 pagesGENETIC COUNSELLING (FARHEEN KHAN MSC 1st Year)Farheen khanNo ratings yet
- Anti-Mu Llerian Hormone: Ovarian Reserve Testing and Its Potential Clinical ImplicationsDocument14 pagesAnti-Mu Llerian Hormone: Ovarian Reserve Testing and Its Potential Clinical ImplicationsSri IriantiNo ratings yet
- Impact of Endometrial Preparation Protocols For Frozen Embryo Transfer On Live Birth RatesDocument8 pagesImpact of Endometrial Preparation Protocols For Frozen Embryo Transfer On Live Birth RatesSri HariNo ratings yet
- Mioma FertilidadDocument6 pagesMioma FertilidadJorge A. VasquezNo ratings yet
- EG0800339 Hyperhomocysteinemia in Recurrent Miscarriage: Kh. R. Gaber, M. K. Farag, S. ET. Soliman, M. A. Abd Al-KaderDocument6 pagesEG0800339 Hyperhomocysteinemia in Recurrent Miscarriage: Kh. R. Gaber, M. K. Farag, S. ET. Soliman, M. A. Abd Al-KaderElena VisterniceanNo ratings yet
- Evaluation of Ultrasonographic and Anti M Llerian Hormone Amh Changes As Predictors For Ovarian Reserve After Laparoscopic Ovarian Drilling For Women With Polycystic Ovarian SyndromeDocument10 pagesEvaluation of Ultrasonographic and Anti M Llerian Hormone Amh Changes As Predictors For Ovarian Reserve After Laparoscopic Ovarian Drilling For Women With Polycystic Ovarian SyndromeJacob HaleNo ratings yet
- O@g Maternal and Fetal Mesures ContentDocument22 pagesO@g Maternal and Fetal Mesures Contentjeya maniNo ratings yet
- The Clinical Significance of Anti-M Llerian Hormone Evaluation in Gynecological EndocrinologyDocument9 pagesThe Clinical Significance of Anti-M Llerian Hormone Evaluation in Gynecological EndocrinologyDrAstha GuptaNo ratings yet
- Tes HCG Kehamilan & Korelasi Kadar Serum Basal AMH Dengan Respons Ovarium Terhadap Stimulasi Ovulasi Putu Mahalika, Satyanegara, Ahmad Dori TiamungDocument7 pagesTes HCG Kehamilan & Korelasi Kadar Serum Basal AMH Dengan Respons Ovarium Terhadap Stimulasi Ovulasi Putu Mahalika, Satyanegara, Ahmad Dori TiamungFiona Febriyanti CiamanNo ratings yet
- A Review Article EndocrineDocument14 pagesA Review Article EndocrineJohn DoeNo ratings yet
- Predictive value of maternal s erum β-hCG concentration in the ruptured tubal ectopic pregnancyDocument7 pagesPredictive value of maternal s erum β-hCG concentration in the ruptured tubal ectopic pregnancyyayayaNo ratings yet
- Ready 0915Document5 pagesReady 0915elfiqiNo ratings yet
- The Use of Antimullerian Hormone in Women Not Seeking Fertility CareDocument5 pagesThe Use of Antimullerian Hormone in Women Not Seeking Fertility CareLaura RojasNo ratings yet
- Acta Obstet Gynecol Scand - 2015 - Abu Hashim - Combined Metformin Clomiphene in Clomiphene Resistant Polycystic OvaryDocument10 pagesActa Obstet Gynecol Scand - 2015 - Abu Hashim - Combined Metformin Clomiphene in Clomiphene Resistant Polycystic Ovarymed2dianavNo ratings yet
- J of Obstet and Gynaecol - 2021 - Oride - Reproductive Prognosis of Patients With Hypogonadotropic HypogonadismDocument8 pagesJ of Obstet and Gynaecol - 2021 - Oride - Reproductive Prognosis of Patients With Hypogonadotropic Hypogonadismaarthisjayraj91No ratings yet
- Aub PDFDocument3 pagesAub PDFNinikNo ratings yet
- 10.1007@s00404 018 4680 1Document12 pages10.1007@s00404 018 4680 1Eva OretlaNo ratings yet
- 1 s2.0 S2666335X22000581 MainDocument9 pages1 s2.0 S2666335X22000581 Mainvantrung_liNo ratings yet
- Amh Serum Dan CairanDocument2 pagesAmh Serum Dan CairanAnton ArifinNo ratings yet
- 2012 Article 61Document5 pages2012 Article 61Al MubartaNo ratings yet
- Ovarian Reserve Testing: A User's Guide: Expert ReviewsDocument12 pagesOvarian Reserve Testing: A User's Guide: Expert ReviewsYosep SutandarNo ratings yet
- Fetal Inflamatory Response SyndromeDocument9 pagesFetal Inflamatory Response SyndromeAnonymous mvNUtwidNo ratings yet
- s12884 018 1908 9 PDFDocument10 pagess12884 018 1908 9 PDFdhea handyaraNo ratings yet
- Best Practice & Research Clinical Obstetrics and GynaecologyDocument12 pagesBest Practice & Research Clinical Obstetrics and GynaecologyGrit WingsNo ratings yet
- 2015 Ovulation-InductionDocument11 pages2015 Ovulation-InductionMARIAPAULACASTILLO1No ratings yet
- Karimzadeh 2010Document5 pagesKarimzadeh 2010Derevie Hendryan MoulinaNo ratings yet
- Can Serum Progesterone Concentration Direct A FresDocument8 pagesCan Serum Progesterone Concentration Direct A FresashrafmogyNo ratings yet
- 1genetic Testing (L1)Document50 pages1genetic Testing (L1)d.djumanalieva.97No ratings yet
- Hinz 2010Document6 pagesHinz 2010djsuraz0No ratings yet
- Bushaqer-2018-Follicular Aspiration Versus CoaDocument6 pagesBushaqer-2018-Follicular Aspiration Versus Coanathalieleclef125No ratings yet
- Complementary and Alternative Medical Lab Testing Part 9: GynecologyFrom EverandComplementary and Alternative Medical Lab Testing Part 9: GynecologyNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 10: ObstetricsFrom EverandComplementary and Alternative Medical Lab Testing Part 10: ObstetricsNo ratings yet
- Committee Opinion: Dual Therapy For Gonococcal InfectionsDocument5 pagesCommittee Opinion: Dual Therapy For Gonococcal InfectionsAripinSyarifudinNo ratings yet
- Female PelvisDocument9 pagesFemale PelvisAripinSyarifudinNo ratings yet
- The WH and Un Pages: Who Director-General Briefs Executive Board On Zika SituationDocument4 pagesThe WH and Un Pages: Who Director-General Briefs Executive Board On Zika SituationAripinSyarifudinNo ratings yet
- Jms 50 061 Chandrashekar OutcomeDocument6 pagesJms 50 061 Chandrashekar OutcomeAripinSyarifudinNo ratings yet
- Mussap 2007 03 J Pediatr SurgDocument7 pagesMussap 2007 03 J Pediatr SurgAripinSyarifudinNo ratings yet
- T - P D U I R E: Hree Dimensional and Ower Oppler Ltrasonography in Nfertility and Eproductive NdocrinologyDocument6 pagesT - P D U I R E: Hree Dimensional and Ower Oppler Ltrasonography in Nfertility and Eproductive NdocrinologyAripinSyarifudinNo ratings yet
- College News Spring 2016Document32 pagesCollege News Spring 2016AripinSyarifudinNo ratings yet
- Brmedj03895 0013Document2 pagesBrmedj03895 0013AripinSyarifudinNo ratings yet
- Management of The Critically Ill Obstetric Patient: ReviewDocument9 pagesManagement of The Critically Ill Obstetric Patient: ReviewAripinSyarifudinNo ratings yet
- Efficacy, Acceptability and Side Effects of The Levonorgestrel Intrauterine System For MenorrhagiaDocument5 pagesEfficacy, Acceptability and Side Effects of The Levonorgestrel Intrauterine System For MenorrhagiaAripinSyarifudinNo ratings yet
- MainDocument4 pagesMainAripinSyarifudinNo ratings yet
- Parenteral Nutrition Patients: ObstetricDocument14 pagesParenteral Nutrition Patients: ObstetricAripinSyarifudinNo ratings yet
- MainDocument2 pagesMainAripinSyarifudinNo ratings yet
- Proof: Abstracts / Gynecologic Oncology 137 (2015) 591 - 599 598Document1 pageProof: Abstracts / Gynecologic Oncology 137 (2015) 591 - 599 598AripinSyarifudinNo ratings yet
- Perbandingan Perubahan Profil Biofisik Janin Akibat Paparan Lagu Mozart K265 Pada Siang Dan Malam HariDocument1 pagePerbandingan Perubahan Profil Biofisik Janin Akibat Paparan Lagu Mozart K265 Pada Siang Dan Malam HariAripinSyarifudinNo ratings yet
- Vaginal Foreign Body - Mohamad Radhi Bin Mohd Ariffin C 111 12 810Document19 pagesVaginal Foreign Body - Mohamad Radhi Bin Mohd Ariffin C 111 12 810aliffikri52No ratings yet
- Antepartal Care: Prepared By: Shalini Santiago-Barroso, RN MANDocument11 pagesAntepartal Care: Prepared By: Shalini Santiago-Barroso, RN MANJabelle Mae DoteNo ratings yet
- Perioperative Preparation and Management: Pre-OperativeDocument14 pagesPerioperative Preparation and Management: Pre-OperativeRed StohlNo ratings yet
- MRCPI O&G Regs 2023Document17 pagesMRCPI O&G Regs 2023Qamarshahzad Joia0% (1)
- List of Infertlity Training Centers: Dr. Jaideepmalhotra / Dr. Narendramalhotra Dr. Asha Anil BaxiDocument8 pagesList of Infertlity Training Centers: Dr. Jaideepmalhotra / Dr. Narendramalhotra Dr. Asha Anil BaxiDSSNo ratings yet
- English Pil KBDocument4 pagesEnglish Pil KBNINING ARIESTINo ratings yet
- Vulvovaginal Health & HygieneDocument131 pagesVulvovaginal Health & HygieneJasmine SardanaNo ratings yet
- True / False QuestionsDocument23 pagesTrue / False QuestionsShawnetz CoppNo ratings yet
- Untitled DocumentDocument2 pagesUntitled DocumentCristina OribelloNo ratings yet
- Oral Contra Ceptive S Pills: Famlily PlanningDocument6 pagesOral Contra Ceptive S Pills: Famlily PlanningnutriNo ratings yet
- Folkesundhedsprojekt KopiDocument108 pagesFolkesundhedsprojekt KopiOlga zivanovicNo ratings yet
- Clinical Case 47 - InfertilityDocument5 pagesClinical Case 47 - Infertilityselina kalenderNo ratings yet
- Benign Tumors of UterusDocument44 pagesBenign Tumors of UterusZunaira ZahraNo ratings yet
- Eejay TemplatesDocument5 pagesEejay TemplatesanmaGirl8611No ratings yet
- Provider Directory Find Care UPMC Health Plan 2Document1 pageProvider Directory Find Care UPMC Health Plan 2Gonzalez Ruscalleda Marie NatashaNo ratings yet
- Syndromic Management of STDsDocument13 pagesSyndromic Management of STDsMeenachi S100% (1)
- Cervical Cancer ScreeningDocument13 pagesCervical Cancer ScreeningshivNo ratings yet
- Chapter 1.1 No Period For 3 Months, Why?Document1 pageChapter 1.1 No Period For 3 Months, Why?TriLightNo ratings yet
- A Textbook of Postpartum HemorrhageDocument496 pagesA Textbook of Postpartum Hemorrhagevalitim89% (9)
- List of Hospitals Jaipur - 2Document17 pagesList of Hospitals Jaipur - 2Global Health Alliance FoundationNo ratings yet
- Adnexal Torsion: Clinical, Radiological and Pathological Characteristics in A Tertiary Care Centre in Southern IndiaDocument6 pagesAdnexal Torsion: Clinical, Radiological and Pathological Characteristics in A Tertiary Care Centre in Southern IndiaKriti KumariNo ratings yet
- Devar Ka LundDocument7 pagesDevar Ka LundAdnan SharifNo ratings yet
- Pelvic ExamDocument5 pagesPelvic ExamKate RamosNo ratings yet
- Final Niki (Perbaikan)Document71 pagesFinal Niki (Perbaikan)Niki Siwi UtamiNo ratings yet
- Reading Part A (Text) Endometriosis V2Document3 pagesReading Part A (Text) Endometriosis V2shinojNo ratings yet