Professional Documents
Culture Documents
Congress Book
Congress Book
Uploaded by
Free Escort ServiceOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Congress Book
Congress Book
Uploaded by
Free Escort ServiceCopyright:
Available Formats
1
1
st
ISTANBUL - EURASIAN
REGIONAL CONGRESS OF BIOLOGICAL PSYCHIATRY
CONGRESS BOOK
May 27
th
- 31
st
, 2012
Istanbul, TURKEY
Editors
Prof. Dr. Bilgen Taneli
Assist. Prof. Dr. Yeim Taneli
2
Publisher
YAMUR TANITIM
Hacilyas Mah. 3. Din Sk. No:10-A
Osmangazi / BURSA / TURKEY
ISBN: 978 605 63112 0 - 8
3
Contents
Foreword ... 5
Committees ... 6
Scientific Program . 9
Lectures .. 21
Symposiums ... 37
Oral Presentations 127
Poster Presentations .... 147
4
5
Dear Colleagues,
We are delighted to welcome psychiatrists, other medical doctors, residents, scientists, researchers,
and health professionals to the 1st Istanbul-Eurasian Congress of Biological Psychiatry in Istanbul.
The field of Biological Psychiatry is rapidly evolving in different fronts such as scientific research and
clinical application; while ranging from early ages in childhood to later years in the adult lifespan. We
will have an opportunity to evaluate and discuss developments, as well as initiate new scientific
collaboration in Biological Psychiatry.
Preparations for the 1st Istanbul-Eurasian Congress of Biological Psychiatry were set in motion exactly
one year ago in Prague at the 10th World Congress of Biological Psychiatry, and concurred with the
WFSBP Executive Committee. International and National Scientific Committees have shaped the
Scientific Program through an intense effort. Suggestions for Symposia, as well as oral and poster
presentations have enriched the program with recent scientific work.
The congress is organized by the Turkish Society of Biological Psychiatry, and endorsed by the World
Federation of Societies of Biological Psychiatry. The congress is also co-sponsored by the World
Psychiatric Association (WPA), and Psychiatric Association of Turkey (TPD). We thank all involved for
their sincere support to the congress.
Since its founding in May 1993, TSBP has organized 8 congresses with international participation,
3 international symposia, and in 2000, co-organized a regional congress in Istanbul with WFSBP.
A majority of these scientific events have been organized by BURKON. We thank them for their
significant support to our congress.
Istanbul has a rich history that archeologists date back 7000 years based on recent excavations.
Bridging Europe and Asia, regarded as one of the most beautiful cities in the World by many travellers,
Istanbul offers not only a mesmerizing historical atmosphere, but also a beautiful landscape in May.
We welcome you in Istanbul to experience a stimulating scientific environment and the magical scene
of Istanbul.
We wish you a cheerful and productive congress participation and hope you will take home many
pleasant memories, as well as inspirations for your research and everyday clinical practice.
Thank you for uniting with us!
With our best regards,
Prof. Dr. Bilgen Taneli Prof. Florence Thibaut
TSBP President WFSBP President
Congress President
6
TSBP EXECUTIVE COMMITTEE WFSBP EXECUTIVE COMMITTEE HONORARY COMMITTEE
TSBP President
Bilgen Taneli
Vice President
Kemal Yazc
Secretary
Suna Taneli
Treasurer
Seluk Krl
Associate Treasurer
Arif Verimli
WFSBP President
Florence Thibaut, France
Vice Presidents
Robertas Bunevicius, Lithhuania
Constantin R Soldatos, Greece
Secretary - Treasurer
Norbert Mller, Germany
Associate Secretary - Treasurer
Yoshio Hirayasu, Japan
Jorge Tellez - Vargas, Colombia
Past President
Siegfried Kasper, Austria
Monte S. Buchsbaum, USA
Dargut Kemali, Italy
zcan Kknel, Turkey
Hans - Jurgen Mller, Germany
Orhan ztrk, Turkey
Refet Saygl, Turkey
Costas Stefanis, Greece
Cokun arman, Turkey
INTERNATIONAL SCIENTIFIC COMMITTEE
Chairs: Bilgen Taneli, Turkey - Florence Thibaut, France
Members:
Tun Alkn, Turkey
Kksal Alptekin, Turkey
Antoaneta Angelova, Bulgaria
Feyza Arcolu, Turkey
Cem Atbaolu, Turkey
Hamdullah Aydn, Turkey
Ayla Aysev, Turkey
brahim Balcplu, Turkey
Meltem Ballan, USA
In Baral Kulakszolu, Turkey
Sunar Birsz, Turkey
Monte S. Buchsbaum, USA
Charles Cartwright, USA
Mesut etin, Turkey
Fsun uhardarolu etin, Turkey
Jurgen Deckkert, Germany
Tamer Demiralp, Turkey
Nesrin Dilbaz, Turkey
Kerem Doksat, Turkey
Engin Eker, Turkey
Lutz Frlich, Germany
Ali Saffet Gnl, Turkey
Erbil Gzkrmz, Turkey
Sepideh Herizchi, Iran
Hasan Herken, Turkey
Yoshia Hirayasu, Japan
Ouz Karamustafalolu, Turkey
Siegfried Kasper, Austria
Seluk Krl, Turkey
Prerna Kukreti, India
Levent Key, Turkey
Mario Maj, Italy
Petar Marinov, Bulgaria
Olya Mikova, Bulgaria
M. Reza Mohammadi, Iran
Nahit Motavall Mukaddes, Turkey
Hans - Jurgen Mller, Germany
Norbert Mller, Germany
Timuin Oral, Turkey
Ayegl zerdem, Turkey
Tatiana Polyakovskaya, Russia
Ilya Reznik, Israel
Peter Riederer. Germany
Yacov Rofe, Israel
Gerda Saletu Zylharz, Austria
Bernd Saletu, Austria
Bengi Semerci, Turkey
Rinaldo Shishkov, Bulgaria
Constantin Soldatos, Greece
Haldun Soygr, Turkey
Mehmet Sungur, Turkey
Suna Taneli, Turkey
Nevzat Tarhan, Turkey
Jorge Tellez - Vargas, Columbia
Ertan Tezcan, Turkey
M. Thirunavukarasu, India
smail Tufan, Turkey
Ik Tulular, Turkey
Zeliha Tunca, Turkey
Rait Tkel, Turkey
smail Hakk Ulus, Turkey
Aylin Uluahin, Turkey
Tayfun Uzbay, Turkey
Simavi Vahip, Turkey
Arif Verimli, Turkey
Hakan Yaman, Turkey
Yank Yazgan, Turkey
Kemal Yazc, Turkey
Ayegl Yldz, Turkey
Joseph Zohar, Israel
7
NATIONAL SCIENTIFIC COMMITTEE
Chairs: Ercan Abay, Turkey - Hsn Erkmen, Turkey
Members:
Belma Aaolu
Fsun Akdeniz
Tamer Aker
Cengiz Akkaya
Zehra Arkan
Kemal Arkan
Rstem Akn
Murat Atmaca
mer Aydemir
Cahide Aydn
Nazan Aydn
Ahmet Ayer
Mustafa Batrk
Ayen Baykara
Erhan Bayraktar
Meral Berkem
Mansur Beyazyrek
Mustafa Bilici
Ali Bozkurt
Adnan Cansever
M. Emin Ceylan
Ayen Cokun
Blent Cokun
Hakan Cokunol
Okan alyurt
Ali aykyl
Serhat tak
Murat Demet
Orhan Doan
Hayriye Elbi Mete
Engin Eker
Murat Erdem
Turan Ertan
Ayen Esen Danac
Bahar Gkler
Ik Grker
Ahmet Turan Ik
Erdal Ik
lkin elli
Glst Kaptanolu
Fatih Karaaslan
Nesrin Karamustafalolu
Sacit Karamrsel
Kevser Kerimolu
Sultan Kl
smet Krpnar
Kaan Kora
Erturul Krolu
Erhan Kurt
Sava Kltr
Bekir Aydn Levent
Refik Mas
Sha Miral
Aslan Ouz
Gltekin gel
Sha zaknl
Esin zatalay
Haluk zbay
eref zer
Fuat zgen
Sedat zkan
Mine zmen
Ercan zmen
Nurgl zpoyraz
Asl Sarandl
Haluk Sava
Yusuf Sivriolu
Teoman Shmen
Vedat ar
ahnur ener
Lut Tamam
Ouz Tan
Tolga Taneli
Yeim Taneli
Sema Tanrver
Ertan Tezcan
Fevziye Toros
Musa Tosun
ener Tot Acar
smail Tufan
Cengiz Tulu
mit Tural
Tmer Trkbay
Hakan Trkapar
mran Tzn
Mfit Uur
Berna Ulu
Alp ok
Mehet nsal
Sheyla nal
M. Erdal Vardar
Hakan Yaman
Medaim Yank
Aylin Yazc
Olcay Yazc
Sinan Yetki
Mustafa Yldz
zgr Yorbik
Nevzat Yksel
ahika Yksel
8
9
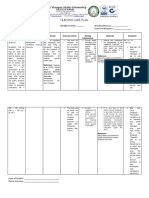
SCIENTIFIC PROGRAMME
27 May 2012, Sunday
09:00 - 10:30
Symposium: Neurobiology of Bipolar Disorder
Chair: Ali Bozkurt (Turkey)
Immunology of Bipolar Disorder
Sinan Glksz, Turkey
Genetics of Bipolar Disorder
Krat Altnba, Turkey
Cognitive Measures of Bipolar Disorder
Murat lhan Atagn, Turkey
Neuroimaging of Bipolar Disorder
Mehmet Alper nar, Turkey
10:30 - 11:00
Coffee Break
11:00 - 11:45
Lecture:
Chair: Manfred Gerlach, Germany - Timuin Oral, Turkey
Update on Treatment of Bipolar Disorder
Siegfried Kasper, Austria
11:45 - 12:00
Break
12:00 - 13:00
Dual Lecture:
Sleep Studies in Psychiatry
Chair: Bernd Saletu, Austria Fuat zgen, Turkey
Hamdullah Aydn, Turkey
Gerda Saletu-Zylharz, Austria
13:00 - 14:00
LUNCH & GUIDED POSTER TOURS
14:00 - 15:30
Symposium: Sleep Studies in Psychiatric Disorders.
Chair: Hamdullah Aydn, Turkey - Fuat zgen, Turkey
(Turkish With Simultaneous Translation)
Sleep Studies in Bipolar Disorder
Fuat zgen, Turkey
Sleep Studies in Posttraumatic Stress Disorder
Sinan Yetkin, Turkey
The Contribution of Arousal and Arousability Phenomenone to Clinical Conceptualization
in Psychiatry
Murat Erdem, Turkey
The Contribution of Sleep Studies as a Research Tool to Psychiatry Practice
Hamdullah Aydn, Turkey
15:30 - 16:00 Coffee Break
10
16:00 - 17:30
Symposium: Biological Aspects of Eating Disorders
Chair: Fulya Maner, Turkey
(Turkish With Simultaneous Translation)
Pharmacotherapy in Eating Disorders
Vesile Altnyazar, Turkey
Imaging in Eating Disorders
F. zlem Orhan, Turkey
Hormonal Changes in Eating Disorders
Bilge Burak Annagr, Turkey
Gene-Environment Interaction in Eating Disorders
Yasemin Grgl, Turkey
17:30 - 17:45 Break
17:45 - 18:45
Symposium: Schizophrenia With a Focus on GABA
Chair: Hseyin Gnay, Turkey
(Turkish With Simultaneous Translation)
The Effected of GABA on Schizophrenia From Pre-Clinical Stages
Hseyin Gnay, Turkey
Reflections of GABA in Schizophrenia
Recep Ttnc, Turkey
GABA in the Psychopharmacology of Schizophrenia
Hakan Balbey, Turkey
The Place of GABA in the Future of Schizophrenia
Murat Erdem, Turkey
28 May 2012, Monday
08:00 - 09:00
Oral Presentations 1
Hall A
Chair: Hseyin Gnay, Turkey George Awad, Canada
Oral Presentations 2
Hall B
Chair: Onur Noyan, Turkey
09:00 - 09:15 Break
09:15 - 09:45
OPENING CEREMONY
Welcome Addresses
Turkish Society of Biological Psychiatry President Prof. Dr. Bilgen Taneli
World Federation of Societies of Biological Psychiatry President - Prof. Dr. Florence Thibaut
World Psychiatry Association Secretary General Assoc. Prof. Dr. Levent Key
Past-President Psychiatric Association of Turkey Assoc. Prof. Dr. Doan Yeilbursa
09:45 - 10:30
OPENING LECTURE
Chair: Florence Thibaut, France
Neuropsychiatry: The Integrative Approach
Constantin Soldatos, Greece
10:30 - 11:00 Coffee Break
11
11:00 - 12:00
Lecture:
Chair: Jurgen Deckert, Germany Nevzat Tarhan, Turkey
Brain Imaging in Depression and Anxiety: Similarities and Differences
Siegfried Kasper, Austria
12:00 - 13:00
LUNCH & GUIDED POSTER TOURS
13:00 - 14:30
Symposium:
Modern Trends of Biological Psychiatry in Bulgaria
Chairs: Rinaldo Shishkov, Bulgaria - Olya Mikova, Bulgaria
Cyclone Gene Expression in the Peripheral Blood an Vrain of Patients With
Schizophrenia
Rinaldo Shishkov, Bulgaria
Screening for Depression and Anxiety in General Practice n Bulgaria
Antoaneta Angelova, Bulgaria
Suicidal Tendencies in Bulgarian Population
Petar Marinov, Bulgaria
HLA Subtypes in Affective Disorders in Bulgarian Population
Olya Mikova, Bulgaria
14:30 - 14:45 Break
14:45 - 16:15
Symposium:
Personalized Medicine in Psychiatry
Chair: Tuncel zden, Turkey
Therapeutic Drug Monitoring and Phenotyping in Psychiatry
Tuncel zden, Turkey
Pharmaco EEG
Bernd Saletu, Austria
Use of TDM in Psychiatry Practice
Nevzat Tarhan, Turkey
Psychiatric Pharmacogenomics
Serdar Nurmedov, Turkey
16:15 - 16:45 Coffee Break
16:45 - 18:15
Symposium: rTMS as a Treatment Strategy in Psychiatry
Chair: Hsn Erkmen, Turkey
Transcranial Magnetic Stimulation
Ouz Karamustafalolu, Turkey
Safety of High Frequency Repetitive Transcranial Magnetic Stimulation
Ouz Tan, Turkey
Efficacy of High Frequency rTMS in Treatment Resistant Depression: Overview of 600
Cases
Gkben Hzl Sayar, Turkey
19:00 - 21:00 WELCOME RECEPTION
12
29 May 2012, Tuesday
08:00 - 09:00
Oral Presentations - 3
Hall A
Chair: Kemal Yazc, Turkey
Oral Presentations 4
Hall B
Chair: Alper nar, Turkey
09:00 - 10:30
Symposium: Geriatry & Gerontology in Turkey
Chair: lkin elli, Turkey Hsn Erkmen, Turkey
(Turkish With Simultaneous Translation)
Multidisciplinary Approach to Alzheimers Disease
Bilgen Taneli, Turkey
Geriatric Assessment in Family Practice
Hakan Yaman, Turkey
Geriatric Psychiatry in Turkey
Engin Eker, Turkey
What should Turkey s Gerontology Agenda Include Through 2023
smail Tufan, Turkey
Falls and Other Accidents in the Household: The Nazilli Experiment
Sultan Kl, Turkey
10:30 - 11:00 Coffee Break
11:00 - 11:45
Lecture:
Chair: Rinaldo Shishkov, Bulgaria - brahim Balcolu, Turkey
Inflammation in Psychiatric Disorders: Pathogenetic and Therapeutic Aspects
Norbert Mller, Germany
11:45 - 12:00 Break
12:00 - 13:00
Lecture:
Chair: Peter Riederer, Austria - smail Hakk Ulus, Turkey
Biological Markers in Psychiatry
Florence Thibaut, France
13:00 - 14:00 LUNCH & GUIDED POSTER TOURS
14:00 - 15:30
Dual Lecture:
Chair: Florence Thibaut, France - Bilgen Taneli, Turkey
Biological Markers in Alzheimers disease and other Dementias
Peter Riederer, Germany
Contemporary Approach to Treating Alzheimers Disease and Future Prospects
smail Hakk Ulus, Turkey
15:30 - 16:00 Coffee Break
16:00 - 17:00
Lecture:
Chair: Engin Eker, Turkey
Late Depression or Vascular Dementia
Jorge Tellez-Vargas, Columbia
13
17:00 - 17:15 Break
17:15 - 18:15
Lecture:
Chair: Jorge Tellez-Vargas, Columbia Petar Marinov, Bulgaria
Current Challenges in Psychopathology: Clinical and Theoretical Implications of
Subtreshold States in Psychiatry
Levent Key, Turkey
18:15 - 18:30 Break
18:30 - 19:30
Dual Lecture:
Evolutionary Origins of Social Attachment and its Disorders
Chair: M. Kerem Doksat, Turkey Seluk Krl, Turkey
Evolutionary Basis of Social Attachment in Other Animal and Homo Sapiens, and
Mechanisms of Related Disorders
M. Kerem Doksat, Turkey
Evolutionary Aspects of Social Attachment in Children and Adolescents, and Mechanisms
of Related Disorders
Neslim G. Doksat, Turkey
30 May 2012, Wednesday
08:00 - 09:00
Oral Presentations 5
Hall A
Chair: Serdar Nurmedov, Turkey
09:00 - 10:30
Dual Lecture:
Chair: Mehmet Sungur, Turkey - Mesut etin, Turkey
The Mythos of Placebo With Known and Unknown Aspects, and Extending Remission in
Depression
Mehmet Sungur, Turkey
Update on Consequences of CBT on Imaging
Axel Wurz, Germany
10:30 - 11:00 Coffee Break
11:00 12:30
Dual Lecture:
Chair: Olya Mikova, Bulgaria - Suna Taneli, Turkey
Neurobiology of Anxiety Disorders: Relevance for Therapy
Jurgen Deckert, Germany
Neurobiology of ADHD
Manfred Gerlach, Germany
Neurobiology of PTSD: Relevance for Treatment
Ouz Karamustafalolu, Turkey
12:30 - 13:30 LUNCH & GUIDED POSTER TOURS
14
13:30 - 15:00
Symposium:
Chair: Jurgen Deckert, Germany smail Hakk Ulus, Turkey
Pharmacokinetic and Pharmacodynamic Aspects of Pediatric Psychopharmacotherapy
Yeim Taneli, Turkey
Pharmacogenetics in the Pervasive Development Disorders
Tolga Taneli, USA
Novel Therapeutics in Autism
Tolga Taneli, USA
15:00 - 15:15 Break
15:15 - 16:15
Lectures:
Chair: Kemal Yazc, Turkey Ouz Karamustafalolu, Turkey
Progressive Change and Effect of Aging on the Brain Volumes in Schizophrenia
Yoshio Hirayasu, Japan
Current Situation of Psychiatry Including Research After Disaster of Earthquake
/Tsunami on March 11,2 2011
Yoshio Hirayasu, Japan
16:15 - 17:00
Lecture:
Chair: smail Hakk Ulus, Turkey - Manfred Gerlach, Germany
Agmatine: A new Neurotransmitter in the Brain
Tayfun Uzbay, Turkey
17:00 - 17:15 Break
17:15 - 18:00
Lecture & Film Presentation:
Catatonia as a Subtype of Schizophrenia or as an Independent Syndrome
Bilgen Taneli & Suna Taneli, Turkey
18:30 - 19:30 CLOSING CEREMONY
15
ORAL PRESENTATION PROGRAMME
28 May 2012, Monday
08:00 - 09:00
Oral Presentations 1
Hall A
Chair: Hseyin Gnay, Turkey George Awad, Canada
OP-1
Low Striatal Dopamine and Comorbid Substance Abuse in Schizophrenia
George Awad
OP-2
Is It Time to Recognize Co-morbid Substance Abuse in Schizophrenia as New Dimension
and Indication for Antipsychotic Drug Development?
George Awad
OP-3
A Survey on Pain Assessment for Cancer patients in Shaheed Ghazi Hospital
Sepideh Herizchi
OP-4
Evaluation of Psychiatric Illness in Iranian Stoma Patients
Homa Mohammad Sadeghi
08:00 - 09:00
Oral Presentations 2
Hall B
Chair: Onur Noyan, Turkey
OP-5
Which Clinical Observations are Leading Further Psychiatric Evaluations?
Mehmet Alper nar
OP-6
Examination of Consultation Liaison Psychiatry Referrals at Rehabilitation Setting; 5
Months Experience
Mehmet Alper nar
OP-7
Trauma Symptomatology of the Trauma Survivors in the Rehabilitation Setting: 5 Moths
Experience
Mehmet Alper nar
OP-8
The Impact Of Work On Mothers Psychological Elements in Ardebil Province
Nasimifar Hojjar
29 May 2012, Tuesday
08:00 - 09:00
Oral Presentations - 3
Hall A
Chair: Kemal Yazc, Turkey
OP-9
Interleukin-6 Reflects Trait Impulsivity in Suicide Attempters
Jussi Jokinen
OP-10
Using Oxytocin to Modify Callous Unemotional Traits in Children Diagnosed With Conduct
Disorder, Subtype Significant Callous Unemotional Traits
Robin MacKenzie
OP-11
Rational-choice Theory of Neurosis: Development and Treatment
Yacov Rofe
08:00 - 09:00
Oral Presentations 4
Hall B
Chair: Alper nar, Turkey
OP-12
The Effect of Alexithymia on Treatment Response in Patients With Major Depressive
Disorder
Cemal Onur Noyan
16
OP-13
Event Related Potentials in Major Depressive Disorder: The Relationship Between P300 and
Treatment Response
Cemal Onur Noyan
OP-14
Oxcarbazepine for Compulsive Water Drinking
Cemal Onur Noyan
OP-15
Antisocial Personality Disorder: Theory Of Mind Disability
Cemal Onur Noyan
30 May 2012, Wednesday
08:00 - 09:00
Oral Presentations 5
Hall A
Chair: Serdar Nurmedov, Turkey
OP-16
Molecular Genetics of Autosomal Recessive Mental Disorders in Consanguineous
Pakistani Families
Shoaib Ur Rehman
OP-17
The Relationship Of Cognitive Impairment With Neurological and Psychiatric Variables
zden Arsoy
OP-18
QEEG-Neurometric Analysis Guided Neurofeedback (Nf) Treatment in Dementa: 23
Cases. How Neurometric Analysis is Important for the Treatment of Dementia As Well
As Diagnosis?
Tanju Srmeli
17
POSTER PRESENTATION PROGRAMME
28 May 2012, Monday
P-1
Life Satisfaction Among Iranian Elderly
Aazam Asadollahikordkandi
P-2
Does The Presence Of A Psychiatrist
Or A Psychiatric Outpatient Clinic Prevent The Attempted Suicide?
Abdullah Akpinar, Hseyin Yumrukcal
P-3
The Presence Or Absence Of A Psychiatry Clinic And A Psychiatrist In The District: Can It
Change The Number Of Diazepam Injections For To Psychiatric Symptoms In The
Emergency Department?
Abdullah Akpinar
P-4
Evaluation Of The Treatment Compliances For Illegal Drug Users Who Has Under The
Probations Treatment In Samsun-turkey
Abdullah Akpinar, Osman al, Umut Mert Aksoy
P-5
Is There Any Risk On Leukocyte With Combination Of Clozapine And Amilsulpride In The
Treatment For Schizophrenia
Abdullah Akpinar, Osman al
P-6
Rtms Augmentation In Treatment
Resistant Depression Patients (preliminary Report)
Ali Bozkurt, Sleyman zselek, Mehmet Ak, zlem Hekim Bozkurt
P-7
Tdo2 Gene Polymorphism In Turkish Children With Autism
zlem Hekim Bozkurt, Tezan Bildik, Afik Berdeli, Ali Bozkurt
P-8
An Epileptic Psychosis Case Seen In Childhood
zlem Hekim Bozkurt, Ali Bozkurt
P-9
Tbars And Lipid Profile In Tunisian Bipolar I Patients
Asma Ezzaher, Dhouha Haj Mouhamed, Anwar Mechri , Fadoua Neffat, Ilhem Hellara, Wahiba Douki,
Lotfi Gaha ,Mohamed Fadhel Najjar
P-10
The Impact Of Attention Deficit Hyperactivity Disorder On Sleep And Screen Exposure
Among School Children
Ayse Rodopman Arman , A. Bkmazer, B. Acar, F. Husrevoglu, A. Slocum, B. Turan, P. Ay
P-11
Association Of The Vamp2, Synapsin 3 And Syntaxin 1a Genes With Adult Attention
Deficit Hyperactivity Disorder
Aye Nur Inci Kenar, Hasan Herken, M. Emin Erdal, Tuba Gkdoan Edgnl
P-12
Is Maternal Depressive Symptomatology Effective On Exclusive Breastfeeding During
Postpartum 6 Weeks?
Bilge Burak Annagur, Ali Annagur, Akkz ahin, Rahmi rs, Fatih Kara
P-13
Role Of Mood And Impulsivity In Obese People With Binge Eating Disorder
Bilge Burcak Annagur, Fatma zlem Orhan, Ali zer, Nur Yaln Yetiir, Lut Tamam
P-14
Intoxication with an extreme overdose of extended-release quetiapine
Mehmet Inta, Cemal Onur Noyan*
P-15
Ego-dystonic Auditory And Visual Hallucinations During Isoretinonin Therapy
C. Onur Noyan*, Mehmet Inta
P-16
Restless Legs Syndrome Induced By Quetiapine
C. Onur Noyan, Gener Gen
P-17
Hyponatrema Durng Clozapne Treatment In Schzophrena: A Case Report
C. Onur Noyan, Levent Emirzeolu
P-18
The Importance Of Pseudocholinesterase Deficiency In Electroconvulsive Therapy (ect)
Cagatay Karsidag, GokselYuksel, Nihat Alpay
18
P-19
Neurobiology of Violence Behavior
Cagatay Karsidag, Armagan Ozdemir, Nihat Alpay, Nesrin B. Tomruk, Umut Mert Aksoy
P-20
Functional Connectivity Via Fmri In Response To High-Calorie Food Cues In Obese
Persons With Binge Eating Disorder
Deniz Atalayer,Spiro Pantazatos, Lauren Puma, Allan Geliebter
P-21
Nasu Hakola Disease : A Case Report Which Is Characterized By Presenil Dementia And
Bone Fractures
Derya Ipekiolu, Nesrin Karamustafalolu, Nazan Karagz Sakall, zlem etinkaya, Mehmet Cem
Ilnem
29 May 2012, Tuesday
P-22
Effect Of Cigarette Smoking On Insulin Resistance Risk
Haj Mouhamed D, Ezzaher A, Neffati F, Douki W, Gaha L, Najjar Mf
P-23
Music And Dementia Patients: The Effects On Agitated Behaviors: A Review Of The
Litareture
Elcin Babaoglu Akdeniz
P-24
Phenotype-genotype And Conventional Therapeutic Doze Monitoring (tdm) Relationship
: A Case Report.
Esra Saglam , Selma zilhan , Fadime Canbolat, Nevzat Tarhan
P-25
Phenotype Compare With Conventional Therapeutic Doze Monitoring (tdm) At
Psychiatric Patients
Esra Saglam , Selma zilhan , Fadime Canbolat, Nevzat Tarhan
P-26
Clinical Efficacy Of Hydroethanolic Extract Of Hypericum Perforatum In Patients With
Hypertension And Concomitant Depression
Fatemeh Ranjbar , Fatemeh Fathi Azad, Fariborz Akbarzadeh, Keivan Shirzadi, Amirhossein
Akbarzadeh, Fahimeh Kazemi Nava
P-27
Night Eating Syndrome Among Patients With Depression
Fatma zlem Orhan, Ufuk Gney zer, Ali zer, zlem Altunren, Mustafa elik, Mehmet Fatih
Karaaslan
P-28
Sociodemographic Variables And Depression In Turkish Women From Polygamous
Versus Monogamous Families
Ali zer, Fatma zlem Orhan, Hasan etin Ekerbier
P-29
Anxiety And Serum Vitamin B12, Folate, Tsh, And Ferritin Levels In Telogen Alopecia
Patients With Trichodynia
Perihan ztrk, Fatma zlem Orhan, Ali zer, Yasemin Akman
P-30
Assesment Of Temperament And Character Profile In Patients With Acne
Perihan Ozturk, Fatma Ozlem Orhan, Tugba karakas, Ali Nuri Oksuz, Nur Yalcin Yetisir
P-31
Dependence To Ketamine And Suicidal Behavior
Vsquez F., Paima R, Crdova R., Nicols Y. Falcon S. Vite V.
P-32
Transcranial Direct Current Stimulation In A Patient With Shizoaffective Disorder Manic
Episode
Gkben Hzl Sayar , Celal Salcini, Ali Bayram, Gaye Kagan, Nevzat Tarhan
P-33
Transcranial Magnetic Stimulation During Pregnancy
Gkben Hzl Sayar, Eylem Ozten, Emine Satmis, Gaye Kagan, Nevzat Tarhan
P-34
Inutero Psychiatric Drug Exposure Resulted As Brachydactyly
Gken Yksel, aatay Karda
P-35
Tbars And Non-enzymatic Antioxidants Markers In Schizophrenic Patients
Hajer Mabrouk, Ikram Houas, Haithem Mechria, Anouar Mechri, Wahiba Douki, Lotfi Gaha,
Mohamed Fadhel Najjar
19
P-36
Homocysteine In Epileptic Patients
Saadaoui Mohamed Hachem, Mabrouk Hajer, Chebel Saber, Hellara Ilhem, Neffati Fadoua, Douki
Wahiba, Frih-ayed Mahbouba, Najjar Mohamed Fadhel
P-37
Shared Obsessive Compulsive Disorder:a Case Report
Hakan Balibey, Recep Tutuncu, Huseyin Gunay
P-38
A Case Report Of Tardive Dyskinesia And Tremor Due To Use Of Aripiprazole
Hakan Balibey, Halit Yaar, Hseyin Gnay
P-39
An Obsessive Compulsive Patient With Increased Serum Prolactin Levels And
Galactorrhea Hakan Balibey, Hseyin Gnay, Recep Ttnc
P-40
The Relationship Of Incarceration, Past Suicide Attempts, Depression, Anxiety And
Attention Deficit Disorder/hyperactivity In Cases Of Anti-social Personality Disorder.
Hakan Balbey, Trker Trker, M. Boran Evren, Nalan Bayar.
P-41
Eye Movement Desensitization And Reprocessing (emdr) Treatment In A Patient With
Posttraumatic Stress Disorder: Case Report
Hakan Balibey, Adem Balikci
30 May 2012, Wednesday
P-42
A Case Series of Hwa-byung Patients Using Instrument of Pattern Identification for
Hwa-byung and Instrument of Oriental Medical Evaluation for Hwa-byung
Dae-myung Park, Sang-ryong Lee, In-chul Jung
P-43
Immunology And Alzheimer - State Of The Art
Joana Andrade, Horacio Firmino, Joo Relvas
P-44
Functional Mri And Obsessive-compulsive Disorder
Joana Andrade, Paula Banca, Susan Santo, Nuno Madeira, Flavia Polido, Fernando Pocinho,
Miguel Castelo-branco, Joo Relvas
P-45
Internet Addiction Among University Students
Eda Aslan karde, Aylin Yazc, Kemal Yazc
P-46
Outcomes Of A Smoking Cessation Outpatient Clinic
Hatice Kaya, M. Alper nar
P-47
Thyroxine Induced Mania In A Case With Thyroidectomy
Eda Aslan karde , M. Alper inar
P-48
Epidemiologic Features Of The Psychiatry Outpatient Clinic Admissions In A County
Hospital Eda Aslan karde, M. Alper inar
P-49
Epidemiologic Features Of Anxiety Disorders In A County Hospital
Eda Aslan karde, M. Alper inar
P-50
The Study Of Effectiveness Instruction And Counseling Premarital On Consolidation Of
Family Basis
Manouchehr Saadatkhah
P-51
Preliminary Study Title: Frontal Gamma Activities as a Biomarker of Family History
Meltem Ballan, John H. Gilmore, Jessica Beattie
P-52
Biosensors For Clinical Neuropsychopharmacology
Bragazzi Nicola Luigi
P-53
Three Different Specific Internet Addiction Cases From The Internet Addiction Clinic Of A
Tra n ng And Research Hospital
mer enormanc, Ramazan Konkan, Oya Gl, Gl z enormanci
P-54
To Cases Of General zed Internet Addiction From The Internet Addiction Clinic Of A
Training And Research Hospital
mer enormanc, Ramazan Konkan, Oya Gl, Gl z enormanci
20
P-55
Effect Of Treatment On Inflammation Biomarkers, Heart Rate Variability And Arterial
Stiffness In Depressed Patients
Angelos Halaris, Edwin Meresh, Ozden Arisoy, Jawed Fareed, Debra Hoppenstead, Steven Kimmons
P-56
Inflammation And Heart Rate Variability In Major Depression
Angelos Halaris, Edwin Meresh, Ozden Arisoy, Jawed Fareed, Debra Hoppenstead, Steven Kimmons
P-57
The Role Of Psychiatrist In Apalliative Care Mobile Team
Tomislav Peharda, Dragan Trivanovic, Krizo Katinic, Dragutin Breski
P-58
Personality Traits In Schizophrenia Patients At Remission Phase And Their First Degree
Relatives: A Dopaminergic And Glutamatergic Genes Polymorphism Study
Vesile Altinyazar, Azad Gnderici
P-59
Peripheral Edema Associated With Olanzapine- Valproate Combination: A Case Report
Leylya Bozatl, Yasemin Grgl, Rugl Kse nar, M. Blent Snmez,M. Erdal Vardar
P-60
Quality of life in adolescent epileptic patients with and without psychiatric comorbidity
Erdem Beyoglu, Yesim Taneli, zlem zdemir, Mehmet Sait Okan, Suna Taneli
P-61
Methylenetetrahydropholate Reductase (Mthfr) Gene Polymorphism In Pediatric
Attention Deficit And Hyperactivity Disorder
Algun Tfekci, Yesim Taneli, Emine Kirhan, Melahat Dirican
21
LECTURES
22
Sleep Studies in Psychiatry
Hamdullah Aydn, MD
Sleep studies (Polysomnography-PSG-) are based on electrophysiological recordings of the brains
and other systems activities. In fact, psychiatric disorders are closely related to CNS abnormalities
which have reflections on electrophysiological differences. It is accepted that electrophysiological
studies such as the PSG are reliable methods of scientific research. Sleep is a physiological state and
a part of life. Thus, research during sleep gives an opportunity to reach more reliable results.
Sleep studies on depression
It is well known that depression is characterized with short REM latency. This is also a marker for
severity of the disorder. Shorter REM latency indicates the severity of depression.
Two points attract attention in studying depression and related pathologies: the first one is continuity of
shortened REM latency until full recovery. In fact, it is also possible to observe short REM latency in
patients who have previously had depression. The second point is, when depression is seen with a
comorbid disorder, REM latency may also be shortened. These critical observations that indicate
depression should be considered when a sleep study is planned in psychiatric disorders.
The effects of antidepressant medicines on sleep
The first effect of antidepressant medicines on sleep pattern is increasing the REM latency. This effect
is also a marker of medicines effectiveness. Long-term use of antidepressants triggers fragmentation of
sleep by causing arousals and leg movements. MAOI cause more fragmentations during sleep. These
results are concordant with patients explanation of the effects of medicines. Most of the patients
explain these effects as my sleep was regulated at the beginning of treatment, but I started to be
frequently awakened during the two or three weeks of treatment.
The first study on depression in our sleep research center had been made in 1990. It was focused on
the effect of Imipramin in patients with depression. REM latency was found to be prolonged, which has
been a well known point. The study was designed to continue for six weeks to observe the treatment
response and changes in the sleep structure. More arousals and awakenings attracted our attention.
Data analysis revealed that Imipramine, which has a dual effect on autonomic nervous system as
monoaminergic and cholinergic activities, had more effects during REM sleep in terms of paradoxical
and also parallel (Aydn, zgen, 1992).
Our research group has been studying sleep in depression for many years. In general, we have
observed that most of the antidepressants caused sleep fragmentation in long term treatment, except
for dopamine agonist antidepressants.
Sleep studies on anxiety disorders
Our research group mainly studied sleep in general anxiety disorder, panic disorder and posttraumatic
stress disorder patients. Our main findings in anxiety disorder patients indicated that their sleep
structure is characterized with decreased total sleep time, long sleep latency, low sleep efficiency
index, more arousals, decreased delta sleep. Sleep studies on PTSD basically have revealed more
arousals during sleep. Detailed analysis indicated physiological changes accompanying arousals
during sleep. It was shown that heart rate is increased in delta sleep compared to normal controls
(Yetkin, et al., 2011). Sleep studies on anxiety disorder have demonstrated that subjects with comorbid
depression or a history of depression in the past should be excluded from the study. (Otherwise, sleep
data is contaminated)
Sleep studies on mania
Although bipolar disorders have a wide spectrum, depression and mania are well defined main clinical
pictures. Sleep in depression has been widely studied while sleep studies on mania are very limited.
Sleep study results in patients with mania show relatively less total sleep time. An interesting finding is,
although total sleep time reduced, amount of deep sleep and REM sleep are protected.
Sleep studies on schizophrenia
Main results can be summarized as decreased total sleep time, disturbed sleep maintenance, delta
sleep normal/decreased, total amount of delta waves decreased, severity of negative symptoms is
related to decreased delta waves, total REM sleep increased or decreased, weak REM rebound after
23
REM deprivation. Spectral analysis indicated that the patient with chronic schizophrenia and
deterioration has low delta wave amplitude (Yetkin, et al, 2011).
Sleep studies on PMS
Women with premenstrual syndrome (PMS) suffer from insomnia. Sleep study has indicated that there
is no difference in sleep structure compared to healthy controls, except that PMS group has more
arousals (unpublished data).
Sleep studies on insomnia
Insomnia is related with very complex dynamics in terms of biological and physiological phenomena.
Sleep studies in the standard model have yielded limited explanation for the pathologies. On the other
hand, spectral analysis has contributed to the description of intrinsic dynamics of insomnia. Specifically,
amplitude and frequency analysis have explored micro structure of sleep.
References:
1. Aydn H, zgen F: Effect of Imipramine on REM: paradoxical or parallel? European
Neuropsychopharmacology, 2(3):389-391, 1992.
2. Grr D, Halc U, Aydn H, Ongun G, zgen F, Leblebiciolu K: Sleep spindles detection using
short time Fourier transform and neural networks, Proc. IJCNN 2002, Hawai, USA, pp. 1631-1636,
2002.
3. Korkmazhan H, Yetkin S, Stcigil L, zgen F, Aydn H. Panik bozukluu hastalarnda
polisomnografi bulgular (Polysomnographic findings in patients with panic disorder). Glhane Tp
Dergisi (Gulhane Medical Journal) 52: 237-240, 2010.
4. Akpnar , Aydn H, Ktk Y: In restless legs syndrome, during changes in vigilance, the forced
EEG shifts from alpha activity to delta or high alpha may lead to the altered states of dopamine
receptor function and the symptoms. Medical Hypotheses, 69: 273-281, 2007.
5. Yetkin S, Aydn H, zgen F. Polysomnography in patients with posttraumatic stress disorder.
Psychiatry and Clinical Neuroscience, 64: 309-317, 2010.
6. Yetkin S, Aydn H, zgen F, Stigil L, Bozkurt A. izofreni hastalarnda uyku yaps (Sleep
architecture in schizophrenia patients). Trk Psikiyatri Dergisi (Turkish Journal of Psychiatry)
2011; 22(1): 1-9
7. Yetkin S, Doruk A, zgen F, Aydn H. Travma sonras stres bozukluu hastalarnda gece idrar
noradrenalin dzeyleri ve uyku yaps (Nocturnal levels of urinary noradrenaline and sleep structure
in patients with post-traumatic stress disorder). Glhane Tp Dergisi (Gulhane Medical Journal) 52:
252-256, 2010.
24
Biological Markers in Psychiatry
Prof. Florence Thibaut
Dept of Psychiatry and Addictive Disorders,
University Hospital/INSERM U 614, Rouen, France
A biological marker is an indicator of the pathogenic process of a disease, or of the pharmacological
response to a therapeutic intervention. Biological markers may be trait markers (persistent
abnormalities) or state-dependent markers (episodic markers).
Markers may be used as diagnostic tools, as markers of the disease progression, or to study the
pathophysiology of the disease (risk factors), or to monitor treatment efficacy or side effects
(pharmacogenetics). The sensitivity, specificity and ease-of-use of a biomarker (especially for
diagnosis) are the most important factors. Some examples of biomarkers which might be used in
psychiatry will be described.
25
Comtemporaray Approach to Treating Alzheimers Disease and
Future Prospects (*)
Prof. Dr. smail H. Ulus
Acibadem University, School of Medicine, Department of Pharmacology, Maltepe, Istanbul
Background information
Clinical overview: Alzheimers Disease (AD) is a progressive neurodegenerative disease associates
with an impairment of cognitive abilities that is gradual in onset but relentless in progression.
Impairment of short-term memory (i.e., misplaced items, forgotten details of daily life, missing
appointments, repeating questions etc) usually is the first clinical feature of AD. Retrieval of distant
memories is preserved relatively well into the course of the disease. As the condition progresses,
additional cognitive abilities are impaired, among them the ability to calculate, exercise visuospatial
skills, and use common objects and tools. The level of arousal or alertness of the patient is not affected
until the condition is very advanced, nor is there motor weakness, although muscular contractures are
an almost universal feature of advanced stages of the disease. Death, most often from a complication
of immobility such as pneumonia or pulmonary embolism, usually ensues within 6 to 12 years of onset.
Pathophysiology: AD is characterized by marked atrophy of the cerebral cortex and loss of cortical
and subcortical neurons. The pathological hallmarks of AD are senile plaques, which are extracellular
accumulations of the protein b-amyloid (Ab) accompanied by degenerating neuronal processes, and
intracellular neurofibrillary tangles, composed of the microtubule associated protein tau. Small
numbers of senile plaques and neurofibrillary tangles can be observed in intellectually normal
individuals, they are far more abundant in patients with AD. The abundance of tangles is roughly
proportional to the severity of cognitive impairment. The current consensus is that Ab accumulation is
an upstream event that triggers tau pathology, resulting in impaired neuronal function and cell loss.
Accumulation of Ab, and by implication AD, could be resulted either with its over production and/or its
impaired clearance. In advanced AD, senile plaques and neurofibrillary tangles are numerous and most
abundant in the hippocampus and associative regions of the cortex, whereas areas such as the visual
and motor cortices are relatively spared. The factors underlying the selective vulnerability of particular
cortical neurons to the pathological effects of AD are presently not known.
Neurochemistry: The neurochemical disturbances that arise in AD have been studied intensively.
Direct analysis of neurotransmitter content in the cerebral cortex shows a reduction of many transmitter
substances that parallels neuronal loss. The most striking neurochemical disturbance in AD is a
deficiency of acetylcholine. The anatomical basis of the cholinergic deficit is the atrophy and
degeneration of subcortical cholinergic neurons, particularly those in the basal forebrain (nucleus
basalis of Meynert), that provide cholinergic innervation to the whole cerebral cortex. The selective
deficiency of acetylcholine in AD has given rise to the "cholinergic hypothesis," which proposes that a
deficiency of acetylcholine is critical in the genesis of the symptoms of AD. it is important to note that
the deficit in AD is far more complex, involving multiple neurotransmitter systems, including serotonin,
glutamate, and neuropeptides, and that in AD there is destruction of not only cholinergic neurons but
also the cortical and hippocampal targets that receive cholinergic input.
Genetics: Mutations in three genes have been identified as causes of autosomal dominant, early-
onset AD. These are APP, which encodes amyloid-b-precursor protein (APP) and PREN1 and PSEN2,
endcoding proteins presenilin 1 and 2. These three genes are involving in the production of AB. Ab is
known to be generated by sequential proteolytic cleavage of APP by b-secretase and g-secretase. The
mutation in APP causes with over production of APP which result with accumulation of Ab. The
presenilins form the catalytic core of g-secretase. Some genes have also been identified as having
alleles that increase AD risk. The most important of these is APOE, which encodes the lipid carrier
protein apolipoprptein E (apoE). Individuals that are carrying e4 allele of APOE have a greater risk
(about 3-fold) for developing AD.
Treatment of AD
There are two main strategies for drug treatment of AD: 1) symptomatic drug treatment, and 2)
disease-modifying drug therapy. There are aggressive attempts to develop drugs targeting Ab, tau,
apoE and other molecules are known to involved in AD pathogenesis (see below). However, at the
present, no disease-modifying therapy is available. Current drug treatment in AD is aimed to alleviate
symptoms.
26
1. Treatment of Cognitive Symptoms in AD
Currently there two approaches for the drug treatment of cognitive symptoms in AD: 1) augmentation of
cholinergic neurotransmission and 2) suppressing NMDA-receptor mediated excitatory glutamatergic
neurotransmission.
1. 1. Augmentation of cholinergic neurotransmission. A major approach to the treatment of AD has
involved attempts to augment the cholinergic neurotransmission in the brain. An early approach was
the use of precursors of acetylcholine synthesis [i.e., choline chloride, and phosphatidyl choline
(lecithin)].
Although these precursors generally are well tolerated, randomized trials have failed to demonstrate
any clinically significant efficacy.
A somewhat more successful strategy has been the use of inhibitors of acetylcholinesterase (AChE),
the catabolic enzyme for acetylcholine. AChE inhibitors augment cholinergic neurotransmission at the
cholinergic synapsis by extending half-life of neurotransmitter acetylcholine at the synaptic cleft.
Physostigmine, a rapidly acting, reversible AChE inhibitor, produces improved responses in animal
models of learning, and some studies have demonstrated mild transitory improvement in memory
following physostigmine treatment in patients with AD. The use of physostigmine has been limited
because of its short half-life and tendency to produce symptoms of systemic cholinergic excess at
therapeutic doses.
Four inhibitors of AChE are approved for treatment of Alzheimer's disease: tacrine, donepezil,
rivastigmine, and galantamine . Tacrine is a potent centrally acting inhibitor of AChE. Studies of oral
tacrine in combination with lecithin have confirmed that there is indeed an effect of tacrine on some
measures of memory performance, but the magnitude of improvement observed with the combination
of lecithin and tacrine is modest at best. The side effects of tacrine often are significant and dose-
limiting; abdominal cramping, anorexia, nausea, vomiting, and diarrhea are observed in up to one-third
of patients receiving therapeutic doses, and elevations of serum transaminases are observed in up to
50% of those treated. Because of significant side effects, tacrine is not used widely clinically.
Currently, three AChE inhibitor drugs, donezepil, rivastigmine and galantamine, are widely used for
first-line therapy of cognitive symptoms in AD. These agents have a beneficial effect on cognition in
clinical AD. Donepezil is a selective inhibitor of AChE in the CNS with little effect on AChE in peripheral
tissues. It produces modest improvements in cognitive scores in Alzheimer's disease patients and has
a long half-life, allowing once-daily dosing. Rivastigmine and galantamine are dosed twice daily and
produce a similar degree of cognitive improvement. Adverse effects associated with donepezil,
rivastigmine, and galantamine are similar in character but generally less frequent and less severe than
those observed with tacrine; they include nausea, diarrhea, vomiting, and insomnia. Donepezil,
rivastigmine, and galantamine are not associated with the hepatotoxicity that limits the use of tacrine.
Combination of AChE inhibitors with neurotransmitter acetylcholine precursor choline could be
enhanced their beneficial effects in AD and could protects cholinergic neurons from autocannabilism.
1. 2. Suppressing NMDA-receptor mediated glutamatergic neurotransmission. Memantine is a
noncompetitive antagonist of the NMDA-type ionotrop glutamate receptors. Memantine interacts with
the Mg
++
binding site of the NMDA receptor channel and prevents excessive activation of NMDA
receptors, without altering normal function of the receptor. Memantine can be used as an adjunct or an
alternative to AChE inhibitors. In patients with moderate to severe AD, use of memantine is associated
with a reduced rate of clinical deterioration. Whether this is due to a true disease-modifying effect,
possibly reduced excitotoxicity, or is a symptomatic effect of the drug is unclear. Adverse effects of
memantine usually are mild and reversible and may include headache or dizziness.
2. Disease-modifying Drug Therapy in AD
Diseases modifying drug therapy in AD could be 1) non-specific and 2) specific approaches.
2.1. Non specific disease modifying drug therapy in AD.
Hormone replacement. Some studies suggest that estrogen therapy (supplementation) at the critical
periodmay reduce the risk of developing AD in later life.
Nonsteroidal anti-inflammatory drugs. Some, but not all, studies suggest that treatment with
nonsteroidal anti-inflammatory drugs has some beneficial effects on the risk of developing AD .
27
Vitamines and antioxidants. Some, but not all, studies suggest that treatment with vitamines and anti-
oxidants drugs has some beneficial effects on the risk of developing AD.
2.2. Specific disease modifying drug therapy in AD.
Antiamyloid therapy. Experimetal studies have shown that antibodies against Ab and some
secretase inhibitors have beneficial effect for restoring neuronal pathology and neurochemistry
abnormalities in the brain of animals. Number of clinical trials, at phase 3, with some secretase
inhibitors and nntibodies for Ab are currently performing. Next few years we will able see whether any
these drugs and or antibodies are approved for the treatment of AD as disease modifying drugs.
Stimulation of synaptogenesis. AD associated with a significant loss of synapses in the specific
brain areas. The magnitude of reduction in synaptic numbers is known to correlated to the severity of
cognitive dysfunctions. It has been shown that treatment with the combination of phosphatide
precursors (i.e., uridine monophosphate, choline and docosahexaenoic acid) enhances synaptogenesis
in experimental animals and improve significantly cognitive impairments in mild AD patients in tow
clinical trials.
3. Treatment of Behavioral Symptoms in AD
In addition to cognitive decline, AD is also associated with some behavioral and psychiatric symptoms,
including, irritability, agitation, paranoia, delusional thinking, sleep disorders, anxiety and depression.
ACHE inhibitors and memantine can reduce some of these symptoms but their effects are usually
modest. Antipsychotics, mood stabilizers and antidepressants (i.e., serotonergic antidepressants) can
be used to control these behavioral and psychiatric symptoms in AD.
(*) The text of this presentation is mainly prepared from the Goodman & Gilmans The
Pharmacological Basis of Therapeutics 11
th
and 12
th
editions.
28
Current Challenges in Psychopathology: Clinical and Theoretical
Implications of Subtreshold States in Psychiatry
Levent Key
WPA Secretary General, Istanbul Bilgi University, Istanbul, Turkey
If one of the major current challenges in the classification and diagnosis of mental disorders is the issue
of multi-morbidities, a further one is the subtreshold states. These challenges could be partially
considered as the by-products of the prevailing current categorical approaches in our classification
systems.
The categorical approach needs and is based on vertical and horizontal boundaries to differentiate
different states of human behavior. While, at a horizontal level the boundaries between mental
disorders are elicited by strict diagnostic criteria, the issue of drawing a threshold at a vertical level
requests some dimensional approaches. These thresholds in the description of many mental disorders
in our current categorical approaches are defined by a combination of some dimensions; i.e., the
duration of the symptoms, the severity of the symptoms, and the effects of the symptoms on social
functioning and abilities.
Another problem in defining the thresholds for mental disorders is the consequence of the cross-
sectional approach. Since, the clinical pattern of many mental disorders change in time, the cross-
sectional approach does not reply to the requirements of a historical perspective from which the
variation of a mental disorder over and under a given cut-off line in due course could be understood. It
is a widely shared opinion that the necessity of defining thresholds for mental disorders is not only
taking the clinical, scientific and research motives into consideration, but also the forensic and
administrative grounds.
This presentation will mainly discuss the phenomenon of threshold and subtreshold states in the
context of psychopathology, clinical practice and classification systems.
29
Evolutionary Origins of Social Attachment and its Disorders
Mehmet Kerem Doksat, Neslim G. Doksat
Polimed Psychiatry Center
Child and Adolescent Psychiatrist The concept of attachment was first introduced by John Bowlby and
later it was adopted by evolutionary psychiatrists. Bowlby studied the effects of early experiences on
the development of self-concept and bond formation. He declared two types of bond formation. One is
stable attachment bond which is associated with emotional security and development of a worthy inner
model of the self. The other is unstable bond, resulting in emotional insecurity and anxious attachment.
Overall, consistent parental nurturing and protection provide a secure base which forms the sense of
basic trust called by Erik Erikson. Nurturing behavior of the mother is related with her mirroring
function, indicating her capacity of intuitions about the childs being hungry, soiled, frightened and etc. If
this mirroring function and secure bond formation do not work properly and persistently, it yields to
serious psychopathological consequences. Fear of loss of attachment bond can result in anger,
aggression and anxiety in babies, and further in life, adults. On the other hand, loss of an attachment
figure may be associated with grief, despair, depression and detachment. As a result, pathogenic
parenting leads to neurotic or psychotic symptoms such as phobias, anxiety, depression, and even
psychosis in children, adolescents, and adults. All the underlying mechanisms of this high level
cerebral and social attachment, ranking and hierarchy are under the control of an evolutionary
designed pre-program. This hardware in the brain requires installation of software epigenetically (etc.
learning to walk, talk and other more sophisticated abilities). If the software is not installed (taught) in
the right period, irreversible or distorted patterns of behaviors are the inevitable sequel. These
necessities for social adaptation last lifelong.
REFERENCES: Anthony Stevens, John Price (2000) Evolutionary Psychiatry: A New Beginning,
Second Edition. Routledge, London. Jean Decety, John T. Cacioppo (2011) The Oxford Handbook of
Social Neuroscience. Oxford University Press, New York.
30
Improving Remission in Treatment Resistant Depression via
Cognitive Behavioural Interventions and Understanding the
Placebo Response
Prof. Dr. Mehmet Sungur
President of Turkish Association for CBT
Department of Psychiatry, Universtiy of Marmara
Treatment resistant depression (TRD) is a reletive concept. Several definitions have been proposed
ranging from nonspecific to more operationally defined. There is no universally accepted evidence
based sequence for antidepressant intervention. However there is agreement that several strategies
such as optimization, switching, augmentation and combination should be considered. The advantages
and drawbacks of each strategy will be discussed. There is less known about the sequencial
integration of pharmacotherapy and psychotherapy in treatment of mood disorders. As residual
symptomatology is one of the strongest predictors of relapse and residual symptoms upon recovery
with antidepressant medication (ADM) are likely to become prodromal symptoms of future relapse,
research was conducted to see if integrating cognitive behavioural treatment (CBT) to medication in a
sequenced manner would stop that progression in to relapse. Result of these studies showed that CBT
was more effective then clinical management in preventing relapse. Studies are also conducted to
compare the efficiacy of CBT with that of ADM in sustained improvement after discontinuation of both
of the treatments. The results of these studies show that CBT have more enduring effects. This
presentation will discuss about possible reasons why CBT have more enduring effects. The costs of
both ADM and CBT in the longrun will also be discussed. New wave CBT approaches such as
mindfulness based cognitive therapy (MBCT) and their effect when compared to maintaining ADM for
relapse prevention will also be discussed. As the last but not the least the placebo effect will be
discussed. Understanding the placebo effect is crucial in order to understand psychological and
physiological mechanisms by which the placebo effects are produced. Placebo is not only a sugar pill.
Information will be given about the effects and ethics of placebo in clinical practice and comparison of
antidepressants with that of placebo how to maximize and minimize the placebo effect and how can
placebo effects be harnessed ethically in clinical practice.
31
Update on Consequences of CBT on Imaging
Axel Wrz
Marmara University, Istanbul
Cognitive Behaviour Therapy has become the most evidenced-based psychotherapy available. In
depression and anxiety disorders it has been shown as effective as pharmacological treatments in the
acute phase and with a substantially lower relapse rate. Also, in many other disorders such as bipolar
disorder, schizophrenia and substance abuse therapy models have been developed that can
successfully be used within an integrated treatment approach.
As a treatment cognitive therapy has always been driven by theory and research both in its cognitive
and its behavioural roots. Looking at the biological foundations of cognitive therapy it appears useful to
look at the changes after successful therapy that are detectable by functional brain imaging.
Furthermore, the results of research on attention, cognition, emotions and memory and learning can
integrated into cognitive models of psychological disorders and guide the use of various treatment
techniques.
Research using functional imaging techniques hint at the importance of the interplay between the limbic
system and the prefrontal cortex both in depression as well as in anxiety disorders and suggest that
cognitive therapy does influence this interplay. The presentation looks at the available studies, but also
highlights their limitations. Moreover, neuroimaging studies exploring processes that play a part in the
effectiveness of CBT such as reappraisal of and distancing oneself from situations have started to
emerge.
Despite methodological limitations neuroimaging and CBT have entered a mutually rewarding
relationship that can help to better understand brain function as well as to improve therapy.
32
Neurobiology of PTSD: Relevance for Treatment
Ouz Karamustafalolu
skdar University, Istanbul-Turkey
Post-traumatic stress disorder(PTSD) is a psychiatric condition that occur in anyone who has
experienced a life-threatening event of violent event. Studies across cultures, languages, and races
suggest that PTSD is a universal response to exposure to traumatic events. The brains's response to
trauma and stress termed as fight or flight response was first described in 1915 by Walter Cannon. The
chemicals unleased during a fight or flight response acts on spesific brain regions, in particular the
hippocamppus and amygdala, which are the parts of the limbic system related to emotion, memory and
cognition.
Serotonin, noradrenalin, acetylcholine, histamine, glutamate, GABA, hypocretin, cortizol,
glucocorticoids and endorphins play a role in the presentation of symptoms when patients develop
post-traumatic stress disorder. Serotonergic (SSRI2s and SNRI's) and noradrenergic (alfa-2
adrenoreceptor agonists and beta-adrenergic antagonists) drugs help to relieve PTSD symptoms.
Anticonvulsants and atypical antipsychotics are helpful in some conditions. Corticosteroids are used to
prevent development of PTSD in the acute term. Benzodiazepins worsens the clinical condition in
trauma patients.
33
Agmatine: A New Neurotransmitter in the Brain
Prof.Dr. Tayfun Uzbay, Ph.D.
Gulhane Military Medical Academy, Psychopharmacology Research Unit, Ankara Turkey
The term "agmatine" was expressed in 1910 by Albrecht Kossel, the German scientist who first
identified the substance in herring sperm almost a hundred years ago (Kossel, 1910). Agmatine is a
polyamine and ionic cation that is synthesized following decorboxylation of L-arginine by enzyme
arginine decarboxylase. Agmatine is produced in bacteria, plants and invertebrates and highly
conserved in nature. It is hydrolyzed to putressine, the precursor of spermine and spermidine, higher
polyamines, by enzyme agmatinase. Thus, agmatine is an intermediary in polyamine biosynthesis in a
pathway that parallels that in mammals. Thus, agmatine is an intermediary in polyamine biosynthesis in
a pathway that parallels that in mammals. This metabolic pathway is also related to synthesis of some
important neurotransmitters such as glutamate and GABA (Petroff, 2002). Arginine decarboxylase and
agmatinase have also been identified in mammalian brain and in many other organs.
The fact that the concentration of agmatine in brain was comparable to that of classic neurotransmitters
suggested that agmatine might be a neurotransmitter. It elicits biological actions within the central
nervous system (CNS) by interaction with some receptors (i.e. NMDA and alpha adrenergic receptors)
and neuronal pathways. It also inhibits enzyme nitric oxide synthase (NOS) in both vascular tissues
and brain (Auguet et al., 1995; Galea et al., 1996). Agmatine has been suggested that agmatine meets
many criteria as a novel neurotransmitter in agmatinergic synapses of CNS (Reis and Regunathan,
2000). From in the middle of 90s, many reports indicated that agmatine may be a key neurotransmitter
in several neurobiological events and implied that it could be an important role in etiopatogenezis of
several CNS diseases, have been published. In the past decade, accumulating evidence indicated that
central agmatinergic system may have a considerable potential to be a distinguished target for
understanding the mechanisms of several CNS disorders and in development of novel
pharmacotherapy strategies (Uzbay, 2012).
In experimental studies, agmatine exhibited anticonvulsant (Feng et al., 2005), antinociceptive
(Yesilyurt and Uzbay, 2001; Karadag et al., 2003), anxiolytic (Lavinsky et al., 2003) and antidepressant
(Zomkowsky et al., 2005) actions. Furthermore, it has some beneficial effects on cerebral ischemia
models in animals (Kuo et al., 2007). Agmatine interacts with the mechanisms of withdrawal syndromes
involved in several addictive agents such as morphine and ethanol (Aricoglu-Kartal and Uzbay, 1997;
Uzbay et al., 2000). Agmatine also blocked caffeine (Uzbay et al., 2010a) and ethanol (Ozden et al.,
2011)-induced locomotor hyperactivity in mice. It also modulates some processes involved in learning
and memory. Thus, agmatine seems to be a useful agent in treatment of behavioral and
neurodegenerative disorders. On the other hand, aberrant releasing and transmission of agmatine in
central nervous system (CNS) may be related to mechanisms of several CNS disorders such as
psychosis (Uzbay et al., 2010b). On the other hand, physiological concentrations of agmatine have
some beneficial effects on animal models of psychosis (Palsson et al., 2008; Kotagale et al., 2012).
In the light of the current data, central agmatinergic system seems to be a new and important target in
development of new drugs in treatment of CNS disorders (Uzbay, 2012; Molderings and Haenisc,
2012). However, the data are limited to animal studies and further clinical evidences are required
(Laube and Bernstein, 2012). In addition, we need more eligible studies that investigate alters in central
agmatinergic transmission (i.e., production rate, releasing, reuptake, turn-over) through CNS diseases.
Elucidation of pharmacokinetic features of agmatine is also required. Upcoming studies, especially
clinical trials, can provide more exciting results on the pharmacological and pharmacokinetic profile of
agmatine in CNS. At this time, we can say that the central agmatinergic system and polyamines seem
to be a key target for the treatment of several CNS disorders.
References
1. Aricioglu-Kartal F, Uzbay IT. Inhibitory effect of agmatine on naloxone-precipitated abstinence
syndrome in morphine dependent rats. Life Sci 1997; 61: 1775-1781.
2. Auguet M, Viossat I, Marin JG, Chabrier PE. 1995. Selective inhibition of inducible nitric oxide
synthase by agmatine. Jpn J Pharmacol 1995; 69: 285-287.
3. Feng Y, LeBlanc MH, Regunathan S. Agmatine reduces extracellular glutamate during
pentylenetetrazole-induced seizures in rat brain: a potential mechanism for the anticonvulsive
effects. Nerosci Lett 2005; 390: 129-133.
4. Galea E, Regunathan S, Eliopoulos V, Feinstein DL, Reis DJ. Inhibition of mammalian nitric oxide
synthases by agmatine, an endogenous polyamine formed by decarboxylation of arginine. Biochem
J 1996; 316(pt 1): 247-249.
34
5. Karadag HC, Ulugol A, Tamer M, Ipci Y, Dokmeci I. Systemic agmatine attenuates tactile allodynia
in two experimental neuropathic pain models in rats. Neurosci Lett 2003; 339: 88-90.
6. Kossel A. ber das Agmatin. Zeitschrift fr Physiologische Chemie 1910; 66: 257-261.
7. Kotagale NR, Taksande BG, Wadhwani PJ, Palhade MW, Mendhi SM, Gawande DY, Hadole PN,
Chopde CT. Psychopharmacological study of agmatine in behavioral tests of schizophrenia in
rodents. Pharmacol Biochem Behav 2012; 100: 398-403.
8. Kuo J-R, Lo C-J, Chio C-C, Chang C-P, Lin, M-T. Resuscitation from experimental traumatic brain
injury by agatine therapy. Resuscitation 2008; 75: 506-514.
9. Laube G, Bernstein HG. Agmatine in the brain: An emerging "human" perspective. Neurosci
Biobehav Rev 2012; 36: 872.
10. Lavinsky D, Sarmento N, Carlos A, Netto A. Agmatine induces anxiolysis in the elevated plus maze
task in adult rats. Behav Brain Res 2003; 141: 19-24.
11. Molderings GJ, Haenisch B. Agmatine (decarboxylated l-arginine): Physiological role and
therapeutic potential. Pharmacol Ther 2012; 133: 351-365.
12. Ozden O, Kayir H, Ozturk Y, Uzbay IT. Agmatine blocked ethanol-induced locomotor activity in
mice. Eur J Pharmacol 2011; 659: 26-29.
13. Palsson E, Fejgin K, Wass C, Klamer D. Agmatine attenuates the disruptive effects of phencyclidine
on prepulse inhibition. Eur J Pharmacol 2008; 590: 212-216.
14. Petroff OAC. GABA and glutamate in the human brain. Neuroscientist 2002; 8: 562573.
15. Reis DJ, Regunathan S. Is agmatine a novel neurotransmitter in brain? Trends Pharmacol Sci
2000; 21: 187-193.
16. Uzbay IT, Yesilyurt O, Celik T, Ergun H, Isimer A. Effects of agmatine on ethanol withdrawal
syndrome in rats. Behav Brain Res 2000; 107: 153-159.
17. Uzbay T, Kose A, Kayir H, Ulusoy G, Celik T. Sex-related effects of agmatine on caffeine-induced
locomotor activity in Swiss Webster mice. Eur J Pharmacol 2010a; 630: 69-73.
18. Uzbay IT, Kayir H, Goktalay G, Yildirim M. Agmatine disrupts prepulse inhibition of acoustic startle
reflex in rats. J Psychopharmacol 2010b; 24: 923-929.
19. Uzbay IT. Pharmacological importance of agmatine in brain. Neurosci Biobehav Rev 2012; 36: 502-
519.
20. Yesilyurt O, Uzbay IT. Agmatine potentiates the analgesic effect of morphine by an 2-
adrenoceptor-mediated mechanism in mice. Neuropsychopharmacology 2001; 25: 98-103.
21. Zomkowski ADE, Santos ADR, Rodrigues ALS. Evidence for the involvement of the opioid system
in the agmatine antidepressant-like effect in the forced swimming test. Neurosci Lett 2005; 381:
279-283.
35
Catatonia as a Subtype of Schizophrenia or as an Independent
Syndrome
Bilgen Taneli
Uluda University, Medical Faculty, Department of Psychiatry, Prof. Emeritus.
Turkish Society of Biological Psychiatry, President.
Suna Taneli
Uluda University, Medical Faculty, Department of Child and Adolescent Psychiatry, Prof. Emeritus.
Catatonia is a motor dysregulation syndrome described by German clinician Karl Ludwig Kahlbaum in
1874, who understood catatonia as a disease of its own.
Emil Kraepelin made it a fulcrum of his concept of dementia praecox. Eugen Bleuler sanctioned this
singular association. During the 20
th
century, catatonia has been considered a type of schizophrenia.
In the 1970s, American authors identified catatonia in patients with mania and depression, as a toxic
response, and in general medical and neurological illnesses.
Fink et al. argued that catatonia should be treated as an independent syndrome, and that Kraepelins
assessment was erroneous.
Catatonia is a brain disease with a cyclic, alternating course, in which the mental symptoms are,
successively, melancholy, mania, stupor, confusion, and eventually dementia.
Catatonia occurs as a consequence of various causes affecting the brain, and is found in more or less
10% of acute psychiatric disorders. It was only occasionally reported in patients with schizophrenia.
Diagnostic criteria for catatonia: motoric immobility, mutism, stupor, catalepsy, excessive motor activity
(not influenced by external stimuli), negativism, posturing, stereotypy, echolia, echopraxia.
Catatonic syndromes respond to Benzodiazepines (Lorazepam), or to ECT. Conversely, neuroleptics
used in schizophrenia, produce no response in catatonia patients, and may even worsen, increasing
the risk of malignant syndrome.
36
37
SYMPOSIUMS
38
Immunology of Bipolar Disorder
Sinan Glksz
Bipolar disorder (BD) is a disabling psychiatric illness with peaks of onset mostly occurring in early
adulthood. Although there are many studies focusing on the pathophysiology of bipolar disorder (BD),
the mechanism of this highly prevalent and severe illness remains unknown. The phasic nature of BD
(manic, depressive, and euthymic states) makes the investigation of BD pathophysiology more difficult
than the investigation of relatively more stable psychiatric disorders, such as schizophrenia and major
depression. Several studies in various fields of research interests have attempted to explain the
underlying factors related to BD. Inflammation theory in BD is one of the hypotheses that can contribute
to understanding the mechanism of BD and development of novel treatment options. The association
between the immune system and BD comes from either the evidence mounting sickness-like behavior
(i.e. somnolence, fatigue) as seen in mood disorders, which may also be associated with altered
immune function, or, from psychiatric symptomatology which is associated with numerous medical
disorders and treatments that regulate the immune function. Cytokines are generally known as
chemical messengers between immune cells, as they play a critical role in mediating inflammatory and
immune responses. Initial interest in cytokines in mood disorders did not only come from the theoretical
explanations but also from the observations of emerging depressive symptoms in patients who were
receiving purified or recombinant cytokines. Currently, it is well-known that cytokines play a regulatory
role in the central nervous system, similar to their role in the immune system. Yet, it is unclear if
cytokine elevations contribute to the provocation of the mood disorder. Although, there is still some
discrepancy in the findings of the manic patients with BD, overall they indicate that mania is a pro-
inflammatory state with higher levels of pro-inflammatory cytokines, such as interleukin-1 (IL-1), IL-6,
and tumor necrosis factor-alpha (TNF-) in patients with BD compared to healthy controls. Relatively
fewer studies investigating bipolar depression show that depressive episode of BD may also be
regarded as a pro-inflammatory state. Whereas, it seems that immune balance is restored in euthymia.
Recently, TNF- modulation has been proposed as a molecular target in pathophysiology of BD
regarding studies showing high levels of TNF- in acute episodes, high prevalence rates of medical
comorbidity related to inflammation (e.g. metabolic syndrome, cardiovascular diseases) and
association of TNF--308G/A promoter polymorphism with BD. Moreover, it has been suggested
biomarkers can be used as a tool for staging BD and higher levels of TNF- are related to advanced
stages of BD with severe impairment during the inter-episodic periods and reduced treatment
response. Current evidence also indicates that many of the psychotropics have immune-regulatory
effects, but lithium is specifically coming into prominence. The mere impact of lithium on cytokine
network related to mechanism of action has not been clarified due to the complex bi-directional
interaction between immune parameters, cellular signal transduction pathways and gene expression.
Overall, it is plausible to argue that lithium has a complex balancing effect on immune parameters
influencing both pro-inflammatory and anti-inflammatory cascades. When we combine this background
with our present findings showing inverse correlation between TNF- levels and longitudinal lithium
response, it is plausible to speculate that lithium may exert its long-term mood stabilizing effects via
down-regulating pro-inflammation, in addition to several other postulated mechanisms. However, we
should be very cautious while interpreting these results considering cytokines and soluble cytokine
receptors are very sensitive to various confounding factors like age, body mass index (BMI), gender,
smoking habits, other co-morbid medical illnesses (e.g. infectious or inflammatory diseases, obesity,
pulmonary, cardiac and endocrine diseases) and prior medication use. Thus, these findings require
further replication and cannot be taken to indicate that inflammatory markers represent a biomarker in
clinical practice, further studies are warranted that focus on immune alterations in patients with BD in
order to clarify the association between pathophysiology of BD and inflammation.
References
1. Guloksuz S, Cetin EA, Cetin T, Deniz G, Oral ET, Nutt DJ. Cytokine levels in euthymic bipolar
patients. J Affect Disord. 2010; 126:458-62.
2. Guloksuz S, Altinbas K, Aktas Cetin E, Kenis G, Gazioglu Bilgic S, Deniz G, Oral ET, van Os J.
Evidence for an association between tumor necrosis factor-alpha levels and lithium response. J
Affect Disord (in press)
3. Haack M, Hinze-Selch D, Fenzel T, Kraus T, Khn M, Schuld A, Pollmcher T. Plasma levels of
cytokines and soluble cytokine receptors in psychiatric patients upon hospital admission: effects of
confounding factors and diagnosis. J Psychiatr Res. 1999; 33:407-18.
39
4. Kapczinski F, Dias VV, Kauer-Sant'Anna M, Brietzke E, Vzquez GH, Vieta E, Berk M. The
potential use of biomarkers as an adjunctive tool for staging bipolar disorder. Prog
Neuropsychopharmacol Biol Psychiatry. 2009; 33:1366-71.
5. Soczynska JK, Kennedy SH, Goldstein BI, Lachowski A, Woldeyohannes HO, McIntyre RS. The
effect of tumor necrosis factor antagonists on mood and mental health-associated quality of life:
novel hypothesis-driven treatments for bipolar depression? Neurotoxicology. 2009; 30:497-521.
40
Genetics of Bipolar Disorder
Krat Altnba
Bipolar disorder (BPD) is a common and serious mental disorder characterized by severe mood
episodes, including mania/mixed, hypomania and depression. Although clinical course of bipolar
disorder is well-known, pathophysiology and etiology is still remain unclear. But, there have now been
many studies demonstrating that mood disorders are familial with a consistent pattern that if the index
case suffers from bipolar disorder, relatives are at increased risk of both bipolar disorder and also
unipolar depression. Additionally, estimates of heritability (variance in illness in the population due to
additive genetic causes) is between 60% and 80% for bipolar disorder and it is generally accepted that
the inheritance is complex which means that multiple genetic and environmental factors contribute to
the development of the disorder.
Twin studies have established that bipolar disorder is among the most heritable of medical disorders
and extensive efforts have been made over the past two decades to identify the susceptibility genes for
bipolar disorder on a molecular genetic level although the clinical heterogeneity and its phenotypic and
genetic overlap with other disorders (especially schizophrenia, schizoaffective disorder, and major
depressive disorder) have raised questions about the optimal phenotype denition for genetic studies.
In linkage and association studies, a series of chromosomal regions likely to contain susceptibility
genes have been idetified even the results are inconsistent and effect sizes are disappointing. It is now
widely accepted that the genetic liability to bipolar disorder reects the action of many genes of
individually small effect, a scenario for which linkage studies are poorly suited. Thus, association
studies, which are more powerful for the detection of modest effect loci, have become the focus of
gene-nding research in line with the rapid technological advances in psychiatry.
Recently, systematic genome-wide association and follow-up studies have reported genome-wide
significant association findings of common variants for schizophrenia and bipolar disorder. The risk
conferred by individual variants is small, and some variants confer a risk for both disorders. In addition,
recent studies have identified rare, large structural variants (copy number variants) that confer a
greater risk for schizophrenia. This review summarizes recent developments in genetic research into
schizophrenia and bipolar disorder, and discusses possible future directions in this field. Nevertheless,
genome-wide association analysis, which has successfully identied susceptibility genes for a variety of
complex disorders, has begun to implicate specic genes for bipolar disorder (DGKH, CACNA1C,
ANK3, NCAN, ODZ). The polygenicity of the disorder means that very large samples will be needed to
detect the modest effect loci that likely contribute to bipolar disorder. Detailed genetic dissection of the
disorder may provide novel targets. In this panel, genetics of bipolar disorder will be discussed under
the lights of current literature.
41
Cognitive Measures in Bipolar Disorder
Murat lhan Atagn, MD
During the last two decades, following the similar wave of researches in schizophrenia, cognitive
functions have been in the focus of intensive interest in bipolar disorder. This delay was probably
derived from the assumption that remitted patients would not have any disturbance in cognitive
functions. However, several findings including deficits in verbal memory, executive functions,
processing speed, working memory have been observed in researches. Heterogeneity of psychiatric
disorders was thought to be the barrier to identify pathogenesis and risk factors of psychiatric
disorders. That leaded attempts aiming to determine valid and reliable measures to form different
measures for psychiatric illnesses. Cognitive functions have been candidate measures to provide
another basement in search of biomarkers in a dimensional approach. In fact as cognitive functions do
exist in first-degree relatives, that may mean susceptibility mechanisms (genetic or environmental) may
underlie both the disorder and cognitive dysfunctions. Then it would be very appropriate to take
cognitive dysfunctions into account in researches. It is aimed to briefly review the cognitive
dysfunctions observed in patients and first-degree relatives in this talk.
42
Neuroimaging in Bipolar Disorder, Neurobiology of
Bipolar Disorder
Mehmet Alper INAR, M.D.
Bipolar disorder is a common psychiatric disorder with a 1.5 % incidence rate and high disabling
disorder affecting up to 3% percent of the population. While bipolar disorder is one of the most common
psychiatric disorder, prognosis is not promising. Presentation of the illness frequently leads late
diagnosis or misdiagnosis. Neurobiological research findings will help to improve diagnostic accuracy
as well as treatment outcome and vulnerability factors. Structural and functional neuroimaging studies
provide evidence of neurobiological underpinnings of the disease.
Structural imaging studies in bipolar disease define particular neuroanatomical abnormalities. However,
anatomic abnormalities could not be translated as a functional abnormality, but these findings guide
functional studies. Magnetic resonance imaging (MRI) and computed x-ray tomography (CT) provide
morphometric findings which reported bipolar disorder is associated with smaller gray matter while no
evidence of different prefrontal cortex volumes. Striatum and thalamic size reported as increased in
bipolar patients inconsistently. Both amygdala and hippocampus are also region of interest. Normal
hippocampus and increased amygdala sizes reported in bipolar disorder different than patients with
schizophrenia.
In vivo brain chemistry can be studied by magnetic resonance spectroscopy (MRS). By detecting
structural and functional neurochemicals may help to clarify pathogenesis of bipolar disorder.
Functional imaging modalities as positron emission tomography (PET), single-photon emission
computed tomography (SPECT) and functional magnetic resonance imaging (fMRI) provide functional
anatomic information. Brain functions can be detected during rest or particular cognitive tasks.
Activation abnormalities reported in subgenual cortex and orbitofrontal cortex in different stages of the
disease.
Both nature of the bipolar disease and the medication effects interfere with the imaging findings.
Further studies focusing particular relationships within the anterior limbic network will provide deeper
understanding of the neurobiology of the bipolar disorder.
43
Sleep Studies in Bipolar Disorder
Prof.Dr. Fuat zgen
Mood disorders, including major depressive disorder (MDD), dysthymia, and bipolar disorders, are
among the most prevalent psychiatric illnesses, with an estimated lifetime prevalence of 1020%. The
greatest age of risk is in young to middle adulthood and women are at about twice the risk of men for
developing mood disorders, particularly for MDD. The increased risk in females is believed to be
primarily during the reproductive years, from adolescence through menopause. Mood disorders have a
slightly lower prevalence in children, estimated to occur in 815% of the population. However, there is
evidence of a secular trend in depression with an increasingly younger age of onset.
Sleep abnormalities are key features of depression and are included in most diagnostic and symptom-
severity classification instruments. Sleep complaints are pervasive in those diagnosed with depression
with subjective sleep complaints in more than 70% of adults and children with MDD. Sleep
disturbances that persist beyond clinical remission of depressive symptoms increase the risk of suicide
and the risk of relapse and recurrence of depression. Moreover, insomnia of at least 2 weeks duration
increases the lifetime risk of developing depression.
Difficulty falling asleep, intermittent awakenings, and early morning awakenings are the classic
insomnia-type sleep problems in MDD, usually accompanied by complaints of feeling unrested upon
awakening. Note, however, that it is estimated that more than 30% of patients with MDD experience
hypersomnia. Those with bipolar illness report even more extreme insomnia during manic episodes
and often repot sleeping 1214 hours a night during the depressed phase of the illness. These
subjective sleep complaints are often mirrored in the findings of laboratory sleep studies.
Early sleep studies indicated that MDD in adults was associated with prolonged sleep latency, and an
increase in both stage 1 sleep and wakefulness after sleep onset. Those with MDD also showed less
slow-wave sleep (stages 3 and 4), an early onset of REM sleep (<65 minutes compared to the 80120
minutes in healthy adults), a prolonged first REM period duration, and an overall increase in the total
amount of REM sleep. Increased phasic REM activity has also been reported in MDD. Laboratory
findings in childhood and adolescent depression have been much more equivocal, with short REM
latency in about only half of published studies and largely restricted to inpatients. Prolonged sleep
latency tends to be the most stable sleep finding in young depressed patients.
Research also suggested that the REM sleep abnormalities persisted into clinical remission and that
REM latency was also short (<65 minutes) in the family members of depressed patients. However,
most of the recent studies have failed to confirm that any one sleep architectural variable reliably
differentiates patients from healthy controls, including several from our own group. Moreover, a
metaanalysis of studies published before 1990 indicated that single sleep architectural measure
differentiated patients with MDD from those with other psychiatric disorders, bringing into question the
specificity of REM sleep abnormalities to depression. Studies that have included quantitative sleep
EEG measures such as spectral and period amplitude analyses have been more likely to differentiate
patients from controls with some exceptions. Collectively, these studies have shown decreased slow-
wave activity (delta in NREM sleep) and increased alpha or beta activity in patients with MDD, although
several studies have pointed to a greater prevalence of slow-wave abnormalities in men than in women
with MDD. Some research groups have also shown greater hemispheric asymmetries during sleep in
MDD and a reduction in the degree of synchronization of interhemispheric EEG activity and in the
relationship between fast and slow frequency EEG throughout sleep both in adults and in children and
adolescents. Perhaps most compelling, the quantitative sleep EEG abnormalities also appear to
prospectively identify those at greatest risk for developing future depression. Nevertheless,
disagreement among studies remains.
Assuming that unipolar and bipolar depression might represent different biological sub- types of
depressive disorders, it was hypothesized that these patient groups differ with regard to
polysomnographic features. Studies comparing unipolar depressed and bipolar depressed patients,
however, failed to detect any significant differences in nocturnal sleep patterns.
Several studies polysomnographically investigated sleep during manic episodes (Hudson et al., 1988,
1992; Knowles et al., 1979). The same abnormalities of sleep, also of REM sleep, were described in
manic patients. Our own study of a patient with rapid-cycling, displaying day to day changes of mood
from depression to hypomania, showed sleep-onset REM periods (SOREMPs, REM latency_25 min)
44
after depressed days, whereas after hypomanic days REM latency was slightly prolonged but still short
(_50 min, Gann et al., 1993).
Several polysomnographic studies have been also performed in patients with Seasonal Affective
Disorder (Anderson et al., 1994; Brunner et al., 1993, 1996; Partonen et al., 1993; Rosenthal et al.,
1989). In none of these investigations were the typical sleep patterns of major depression found.
In summary, polysomnographically measured abnormalities of sleep are not specific for subtypes of
depression and therefore support the concept of Major Depression. As already mentioned, a meta-
analysis of sleep laboratory studies in depressed patients and patients with other psychiatric disorders
(Benca et al., 1992) also demonstrated the occurrence of sleep disturbances and REM sleep
disinhibiton in other psychopathological conditions.
As can be seen, the combination of severe sleep continuity disturbances, SWS reduction and REM
sleep disinhibition is encountered most frequently, but is not highly specific to affective disorders
compared to all other psychopathological conditions investigated.
45
Sleep Studies in Post-traumatic Stress Disorder
Dr. Sinan Yetkin
Sleep disturbances are common among patients with posttraumatic stress disorder, and plays a
prominent role in the onset and maintenance of their symptoms. Unlike several of the other anxiety
disorders, PTSD is characterized by sleep-specific complaints. The DSM-IV-TR diagnostic criteria
include such complaints as difficulty falling or staying asleep as well as nightmares of the precipitating
traumatic event.
Although such complaints are not mandatory for assigning a PTSD diagnosis, survey studies have
demonstrated that insomnia complaints and reports of distressing, sleep-disruptive nightmares are
present in the majority of those with this condition. Furthermore, other sleep disturbances such as
sleep avoidance, sleep terrors, nocturnal anxiety attacks, simple and complex motor behaviors and
vocalizations, acting out dreams, sleep apnea, and periodic leg movement disorders are also frequently
reported and observed by PTSD patients.
Growing evidence shows that sleep disturbances seem to be a core feature of PTSD, and sleep
disruption following a traumatic event may constitute a specific mechanism involved in the
pathophysiology of chronic PTSD.
Sleep disturbances in the period immediately following trauma may also have prognostic significance
for the development of PTSD. Klein et al. , using the Mini Sleep Questionnaire, assessed 102 traffic
accident survivors and 19 matched controls admitted to an orthopedic unit for elective surgery. At 1
week there were no significant differences between the two groups, but using logistic regression, the
authors found that those patients with sleep disturbances 1 month posttrauma were significantly more
likely to develop PTSD by 12 months post trauma.
Additionally, sleep disturbances independently exacerbate daytime symptoms, and contribute to poor
clinical outcomes in PTSD, such increased severity of depression, suicidality, and general psychiatric
distress, poorer quality of life and functioning, and poorer perceived physical health, and increased
alcohol and drug use. Although subjective reports of sleep complaints are common, results of
polysomnographic studies are inconsistent. Several possible explanations for these inconsistent
findings have been posited, including differences between studies in time since traumatic events,
comorbidities examined, medications allowed, hospitalization status of participants, and sample size.
An investigation of sleep in a homogeneous patient sample controlling for additional confounding
factors would be of value. PTSD, however, is often associated with another psychiatric morbidity and
becomes chronic. Hence, it is difficult to separate the effects of PTSD from other concomitant
psychiatric disorders (particularly depression). In the literature there are only a few studies that have
attempted to discriminate between the direct effect of PTSD and that of comorbidity. Therefore, we
studied sleep structure of 24 non-medicated male PTSD patients with or without any psychiatric
comorbitiy on polysomnography an two consecutive nights.
Seventeen of the patients had combat-related PTSD (70.8%), five had traffic accident-related PTSD
(20.8%), and two had earthquake-related PTSD (8.3%). Thirteen patients who had combat-related
PTSD had been exposed to more than two traumatic events. Six of the patients had no other major
psychiatric disorder (25%). Fifteen had a current history of major depressive disorder (MDD; 62.5%),
eight had current alcohol abuse (33.3%), three had current generalized anxiety disorder (12.5%), and
two had current and lifetime social phobia (8.3%).
At first, all the PTSD patients were compared with normal controls. Table presents the means and
standard deviations of sleep variables for the second night in 24 PTSD patients and controls. On the
sleep continuity indexes, PTSD patients had a significantly longer sleep onset latency, a lower sleep
efficiency , and a decreased TST when compared with controls. With regard to sleep architecture, the
patients had less SWS compared with controls. Eight of the 24 patients had no score-worthy stage 4
sleep. The REM sleep latency in the patients was found to be shorter than that in the normal controls.
And then, the patients were divided into two groups: PTSD-only patients, and patients with comorbid
MDD. Both PTSD groups were compared to normal controls. Three PTSD patients who had other
comorbid anxiety disorders were not included in the study in the second step of the comparison. There
were no statistically significant differences between these two groups in the sleep variables, duration of
46
the disease, or the number of traumatic events. Total CAPS score in the PTSD patients with MDD was
significantly higher compared with PTSD-only patients. On CAPS subscale scores, the score of the
avoidance symptom cluster in the PTSD patients with MDD was significantly higher compared with
PTSD-only patients.
When both PTSD groups were compared with normal controls, PTSD patients with MDD had more
significant differences compared with normal controls on sleep variables than PTSD-only patients. On
the sleep continuity indexes, TST, SPT, and sleep efficiency were all found to be significantly
decreased, and sleep latency was significantly increased. And, with regard to sleep architecture,
PTSD-MDD patients had significantly less SWS. In addition, they had more abundant REM sleep
latency. The PTSD-only group had significantly reduced sleep efficiency, and increased sleep latency
on sleep continuity indexes when compared to the normal controls. The percentage of SWS and the
percentage of stage 4 sleep in the PTSD-only patients were significantly reduced, as found in patients
with MDD. But there was no significant difference in the REM latency between the PTSD-only group
and the normal control group.
In this study, we observed a higher degree of disturbed sleep continuity (reduced TST, increased sleep
latency, and reduced sleep efficiency) in PTSD patients with comorbid MDD than in PTSD-only
patients. As a group, all patients had profound difficulties falling and staying asleep, reduced SWS, and
reduced REM latency. When PTSD-only patients and PTSD patients with MDD were compared with
the normal controls, sleep disturbances were found to be more abundant in PTSD/MDD. But we did not
observe any significant differences in sleep structure between PTSD-only patients and PTSD patients
with MDD.
These findings in sleep continuity are also frequently found in various other psychiatric disorders;
hence, they are not specific to any one disorder. As proposed by some authors, the disruption in sleep
continuity may be related to psychological distress and its physiological correlations, inducing a non-
disengagement of the waking process. Therefore, in the present study, PTSD patients with comorbid
MDD, having high scores in the clinical scales, had more prominent sleep disturbances in sleep
continuity. Contrary to these findings, some sleep studies in PTSD, particularly those undertaken
recently, could not demonstrate a significant disturbance in sleep continuity, or in sleep architecture.
This inconsistency may be associated with the acuity of the trauma. In the present study the time
passed since the traumatic event was relatively shorter than that in recent studies.
As indicated in some studies, biological adaptive mechanisms may contribute to the normalization in
sleep structure by the time elapsed since the trauma.
In sleep studies performed on PTSD patients, the latency of REM sleep is controversial because of the
coexisting depression among PTSD patients. In the present study we found significant differences only
in REM latency between PTSD patients with comorbid MDD and normal controls. PTSD-only patients,
however, showed no significant difference in REM latency when compared with normal controls. In
PTSD patients with comorbid MDD, two of the 15 patients exhibited sleep onset REM (SOREM), and
had REM latencies <15 min. None of six PTSD-only patients displayed SOREM. In the present study
the impact of comorbid depression on sleep in PTSD was observed in PTSD patients with comorbid
MDD and reduced REM latency.
With regard to correlations between some symptoms scores and primary sleep variables. The startle
response score in CAPS was negatively correlated with the TST, and REM latency. In addition, the
startle response score also positively correlated with the number of traumatic events, CAPS total score,
and the HRSD total score. The severity of psychogenic amnesia was negatively correlated with the
percentage of SWS and sleeps efficiency, and positively correlated with sleep latency. We did not find
any significant correlation between primary sleep variables and the other symptoms of interest
(flashback, nightmare, irritability, and difficulty of concentration). None of the sleep variables was
correlated with the duration of the disease.
Taking all sleep studies together, the severity of sleep disturbances paralleled the severity of the
clinical picture of patients with PTSD. Coexisting depression is more likely to cause the sleep
disturbances than the PTSD itself. Therefore it seems reasonable that the extreme variability in sleep
architecture findings in these patients might arise from different comorbid condition.
Recently, some authors concluded that polysomnographicaly recorded sleep was notably better than
expected in the presence of clinically significant PTSD including typical histories of disrupted sleep. In a
large study (by Breslau et al., 2004), no polysomnographic sleep differences were noted between
subjects with and without PTSD, other than increased REM-related arousals in the PTSD group.
47
Interestingly, Hurwitz and colleagues found that their subjects consistently underestimated their total
sleep time and overestimated their sleep latency in their study. So, the authors suggested that PTSD
patients may have a form of sleep state misperception, leading them to over-report their sleep
difficulties.
However, the most consistent polysomnography findings In PTSD patients are difficulty in sleep
initiation and maintenance, including poor sleep efficiency, decreased total sleep time (TST), increased
sleep latency, and increased number of awakenings.
Several studies also reported an increased incidence of body/leg movement and apneas during sleep
in PTSD patients. Some studies also reported that increased REM density and increased REM sleep
phasic leg activity. Interestingly, Mellman and his collegues also reported that PTSD patients had both
the highest and the lowest values for REM latency compared to those with MD.
There are several suggested mechanisms to explain the findings seen in the sleep of PTSD patients.
The most common one is the hyperarousal theory, which is supported both by laboratory data and by
clinical correlates. Some laboratory evidence in support of the hyperaroused state in PTSD is given by
the findings of the nondiminished noradrenergic production in these patients during the night. In this
theory, as increased sensitivity and sensitization of the noradrenergic system may leave the individual
in a hyperaroused, sleep-deprived state that worsens over time. This hyperarousal state can explain
the clinical correlate of these patients in terms of fragmented sleep and tendency toward insomnia.
Second theory is sleep deepening. Three independent studies investigating the objectively
determined awakening threshold of these patients found that they actually have elevated awakening
thresholds, both in REM and NREM sleep. This might lead to the conclusion that in spite of their
general complaints concerning disturbed sleep, chronic PTSD patients in fact are more difficult to
awaken from sleep than normals. This might be a unique specific finding in PTSD and the
pathogenesis of this elevated awakening threshold has been postulated to be related to active blocking
mechanisms invoked to suppress trauma-related anxiety-provoking materials during sleep. As both the
hyperarousal theory and the sleep-deepening mechanism are supported by clinical and laboratory
findings, it may be possible that they exist simultaneously. Conceivably, the increased tone of the
brains catecholamines sets a sleep threshold higher, and thus PTSD patients tend to be insomniac,
but once they fall asleep, their sleep is deeper, with an elevated awakening threshold. It has also been
speculated that chronic hyperarousal leads to insomnia and partial sleep deprivation that gives way to
heightened arousal thresholds during recovery sleep (Pillar et al., 2006).
Another theory is the REM dysfunction theory. Some researchers have focused on the aberrations of
REM sleep and the presence of recurrent, repetitive nightmares in PTSD and have postulated that an
abnormal REM mechanism is central to this disorder (Fisk et al., 1994). In this theory, anxiety-related
dreams, increased REM phasic activity, and increased startle response may all be a result of an as yet
unknown mechanism in PTSD patients.
Ross et al. suggested that the flashbacks reported in PTSD patients during the daytime might parallel
the curve of REM sleep propensity, as measured by multiple naps. In addition, they found that tonic
and phasic REM sleep measures in PTSD subjects were significantly elevated, which is further
evidence for dysregulation of the REM sleep control system (particularly phasic event generation) in
PTSD.
As some of these may be explained by increased catecholaminic concentration in the brain, it might be
the same mechanism responsible for the REM dysfunction and the hyperarousal state.
While normally REM sleep is associated with spinal postsynaptic inhibition of motor neurons (e.g., REM
atonia), PTSD patients exhibit bursts of motor unit action potentials. In addition, the finding that these
patients show exaggerated abnormal startle response even while awake, might further link PTSD to
REM sleep dysfunction. PTSD occurring in the aftermath of an overwhelming psychological
stressorcould reflect plasticity in brainstem systems controlling REM sleep phasic activity. Lesions of
these brain regions in animals (pedunculopontine tegmental nucleus) have been shown to result in
dysinhibition of acoustic startle, as well as activation of REM sleep mediated by cholinergic neurons.
Thus the CNS processes generating REM sleep may participate in the control of the classical startle
response, which may be akin to the startle behavior commonly described in PTSD patients. Therefore it
seems possible that anxiety dreams, increased REM phasic activity, and increased startle response
are results of an as yet undefined abnormally activated mechanism in PTSD patients.
48
Actually, there is no clinically significant sleep disorder or typical sleep pattern by PSG in PTSD.
Collectively considered, anxiety dreams, increased REM phasic activity, increased arousals from REM
sleep, increased startle response, and possibly elevated awakening thresholds from sleep may
characterize PTSD. Other changes sometimes observed in PTSD, namely, changes in REM latency,
REM time, and REM density, seem related to frequent comorbidities rather than to a direct effect of the
trauma.
49
Arousal Phenomenon
Murat Erdem
The concept of arousal means transient mixing of wakefulness into sleep or sudden and temporarily
increasing of the arousal level spontaneously or at least due to a stimulus. Arousal causes the division
of sleep as well as it contributes to the daytime sleepiness and emergence of cognitive and
psychomotor dysfunction. American Sleep Disorders Association (ASDA), described arousal concept
as rapid change in the form of EEG frequency which may include alpha or theta rhythm and/or EEG
frequency being over 16 Hz without any emerging sleep spindles. Brain structures related to formation
of arousal form are located in the brain stem, thalamus, hypothalamus and basal forebrain.
1) Delta burst: Delta wave activity which can be detected in at least three EEG derivations, exceeding
at least 1/3 or over than the amplitude of background activity and lasted for at least 2 sec.
2) K-burst: It is characterized by sudden onset of two or more K complexes without alpha activity
which could be detected at least three EEG derivations.
3) Microarousal (MA): According to ASDA definition (1992) it is defined as alpha, theta or fast-
frequency EEG activity that significantly diverge from the background EEG activity. It lasts in 1.5-3
seconds. MA criteria for the period of REM includes change of EEG activity as well as the increase of
submental EMG amplitude.
4) PAT: It is defined as increased EMG activity with acceleration of the heart rate, as a result of a
decrease in the amplitude of background EEG activitiy the emergence of alpha or beta activity,
temporarily disappearing of the rapid eye movements during REM. PAT duration may be 3-30 sc.
5) Cyclic Alternating Pattern (CAP): It is defined as regular intervals of arousal for 20-40 seconds
during NREM sleep. A CAP cycle consists of two phases. Phase A, represents the period of phasic
activation and corresponds to simultaneous events. Phase B is the deactivation phase which includes
the actual sleep period. During this period, giving a sensory stimulus may cause re-emergence of
phase A. The period between two A phases is about 1 min. The average duration of phase A is 10-12
sec, and the B phase is 20-30 secs.
RELATIONSHIP of AROUSAL and INSOMNIA
The severity of the arousal activity as well as the individual susceptibility to formation of arousal activity
(arousability) is thought to play a role in the emergence of insomnia. A variety of activities related to
arousal have been reported to be increased in patients with insomnia (such as, somatic arousal which
can be measured by an increase in metabolic rate and heart rate variability, cortical arousal as
measured by EEG beta activity, nocturnal sympathetic arousal which can be demonstrated by
increased norepinephrine levels, cognitive arousal determined by relationship between intrusive
thoughts with sleep complaints). These findings support the hypothesis of excessive arousal in
insomnia. According to this hypothesis; increased somatic, cortical and / or cognitive arousal lies under
primary insomnia symptoms and this prevents patients from sleeping at an adequate level. Cortical
EEG beta activity which is taken as an indicator of arousal has been found to be increased in patients
with initial insomnia.
REFERENCES:
1. Terzano MG, Parrino L, Spaggiari MC ve ark. CAP variables and arousals as sleep
electroencephalogram markers for primary insomnia. Clinical Neurophysiology 2003; 114: 1715
1723.
2. Sforza E, Chapotot F, Pigeau R ve ark. Time of night and first night effects on arousal response in
healthy adults. Clinical Neurophysiology 2008; 119: 15901599.
3. Reinscheid RK, Xu YL, Civelli O. Neuropeptide S: A New Player in the Modulation
of Arousal and Anxiety. Molecular Interventions 2005, Vol 5: 42-46.
50
Pharmacotherapy in Eating Disorders
Vesile Altnyazar, MD.
Adnan Menderes University, Medical Faculty, Department of Psychiatry / Aydn-Turkey.
Eating disorders (EDs) are widespread, disabling, complex and often chronic psychiatric disorders.
Lifetime prevalence rates have been estimated for anorexia nervosa (AN) 0.60.9%, for bulimia
nervosa (BN) 12%, for binge-eating disorder (BED) 3.5%, and up to 10% for eating disorders not
otherwise specified (EDNOS) in young women (Hudson et al. 2007). In males, lifetime prevalence rates
are 0.3% for AN, for BN 0.5%, and for BED 2.0% (Hoek, 2006; Hudson et al. 2007). Comorbid
psychiatric features such as anxiety or mood disturbance, obsessionality and impulsivity are frequent.
The mortality among women with ED is almost 20% (Nielsen, 2001).
Anorexia nervosa:
No strong evidence support to drug treatment in the acute or maintenance phases of the AN (Claudino
et al. 2006; Crow t al.2009). A Cochrane review found no evidence from placebo-controlled trials of
antidepressants in AN for improved weight gain, eating disorder or associated psychopathology
(Claudino et al. 2006). Neurochemical abnormalities seconder to starvation may partially explain this
non-response, however nutritional supplementation (including tryptophan) with fluoxetine has not been
shown to increase efficacy (Barbarich et al.2004; Bailer ve ark. 2007). Mirtazapine is a noradrenergic
and specific serotonergic antidepressant (NaSSA) antidepressant which increases appetite and
induces weight gain. One open trial reported weight gain on mirtazapine in five AN inpatients (Schu le
et al. 2006). But also antidepressants are often used to treat co-morbid disorders such as depression
and obsessive compulsive disorder.
Antipsychotics are used to reduce extreme beliefs regarding body image and weight could be viewed
as delusional, intense ruminations about food, pseudo-hallucinations, agitation when people are
confronted with weight gain, however they may not consistently promote weight gain (Hay and
Claudino 2012). Traditional antipsychotics is no longer recommended because their short- and long-
term side-effects and weight gain tends and changes in attitudes towards eating and body shape not to
persist.
Atypical antipsychotic drugs (olanzapine, quetiapine, aripiprazole, amilsulpride) are often used and give
some benefits in decreases in obsessive symptoms and an increased rate of weight gain in some
studies and case reports but not all (Bissada ve ark. 2008; Bosanac et al. 2007; Trunko ve ark. 2010;
Ruggiero ve ark.2001). However they are not usually recommended for support the weight gain by
NICE guidelines (NICE Guideline 2004).
Lithium to induce weight gain and anti-epileptic medications with mood-stabilizing properties has been
used for AN patients, however, the use of lithium is not recommended in AN, because sodium and fluid
depletion may lead to reduced lithium clearance, and about anti-epileptic medications available data
are mixed (Flament et al.2012)
The opioid peptide system is role in modulating appetite, feeding behaviours, regulation of energy
intake and utilization through reward-mediated behavior (Baranowska et al. 1984). There were reported
in role of hedonic balance and emotional response in food choice and intake and disturbance in the
opioid function has been shown in patients with AN (Morley and Blundell 1988; Yeomans and Gray
2002). Some studies reported that administering naloxone to AN and BN resulted in weight gain, and/or
reduced binge/purge frequency (Marrazzi et al. 1995; Hubner 1993).
Zinc and cyproheptadine have been investigated in some trials of varying quality and success (Su et
al.; Halmi et al.1986). Ghrelin is circulating orexigenic hormone, and increases food intake by
interacting with hypothalamic and brainstem circuits involved in energy balance, as well as reward-
related brain areas. In acute phase of AN, ghrelin levels are elevated and return to normal levels after
weight restoration (Cano et al.2012). To date, only a few studies have analyzed the effect of ghrelin
treatment on patients with AN and finding are contradictory (Broglio et al.2004; Miljic et al.2006; Hotta
et al.2009) However, ghrelin agonists may be beneficial in increasing food intake in especially
restrictive type AN and larger clinical trials are needed.
Pharmacotherapy provides little benefit in the treatment of AN and need to biological markers of AN for
appropriate treatment (Crow et al.2009;Hatch, et al.2010)
51
Bulimia Nervosa and Binge Eating Disorder
Evidence from pharmacological treatment in bulimia nervosa is strong, however mainly efficacy
findings coming from in the acute stage after short-term treatment (Treasure et al.2010). Several
randomized controlled trials (RCTs) have been conducted by tricyclic antidepressants treatments
studies for treatment of BN and mostly indicated that reduction in frequency of binge eating (4791%)
significantly superior than placebo (Flament et al.2012). However, TCAs have the potential to be fatal
in overdose, because not considered as a first-line pharmacological treatment.
Serotonin reuptake inhibitors (SSRIs) are the drugs of first choice in treatment of BN (Taylor et al.
2009). Fluoxetine is the most tested drug in trials and recommended doses (60 mg per day) is higher
than is usually necessary to treat depression (2040 mg per day) (Shapiro et al.2007). There were
reported for improvement carbohydrate binges, and eating attitudes and also comorbid depression by
fluoxetine treatment at 60 mg dose. Several evidences are collecting of efficacy for other SSRIs
(citalopram, sertraline, fluvoxamine), monoamine oxidase inhibitors (MAOIs), reboxetine, milnacipran,
bupropion, and trazodone (Hay & Claudino, 2010; Bacaltchuk & Hay, 2003; Noma et al. 2008; Horne et
al. 1988; Fassino et al. 2004;). However, long term effect of antidepressant treatment for relapse
prevention is unknown, because mostly treatment trials around 8 weeks and when drugs are given
alone acceptability and stay in treatment of antidepressant are low (around 40% dropout rates)
(Bacaltchuk and Hay 2003).
Topiramate has been considered to be possibly useful in eating disorders for their anti-impulsivity and
weight-losing effects, and case series and several RCTs has supported the efficacy of topiramate on
reduced binge/purge frequency, weight and improved health related quality of life for bulimia nervosa
patients (McElroy et al. 2007; Nickel et al. 2005).
Some eating-disorder behaviours (specially binge eating) are considered addictive-like behaviours
and naltrexone has been conducted some studies in BN and bing eating disorder but results of clinical
trials are conflicting (Hay & Claudino, 2011).
REFERENCES
1. Bacaltchuk J, Hay P. Antidepressants vs. placebo for people with bulimia nervosa. Cochrane
Database of Systematic Reviews. 2003;Issue 1, Art. No. CD003391.
2. Bailer U, Frank G, Henry S, et al. Serotonin transporter binding after recovery from eating disorders.
Psychopharmacology (Berlin) 2007;195, 315324.
3. Barbarich NC et al. Use of nutritional supplements to increase the efficacy of fluoxetine in the
treatment of anorexia nervosa. Int J Eat Disord 2004;35:1015.
4. Baranowska B, Rozbicka G, Jeske W, et al. The role of endogenous opiates in the mechanism of
inhibited luteinizing hormone (LH) secretion in women with anorexia nervosa: the effect of
endorphin secretion. Journal of Clinical Endocrinology & Metabolism 1984;59,412416.
5. Bissada H, Tasca GA, Barber AM, et al. Olanzapine in the treatment of low body weight and
obsessive thinking in women with anorexia nervosa: a randomized, double-blind, placebo-controlled
trial. American Journal of Psychiatry 2008;165, 12271228.
6. Bosanac P, Norman T, Burrows G, et al. Serotonergic and dopaminergic systems in anorexia
nervosa: a role for atypical antipsychotics? Australian and New Zealand Journal of Psychiatry
2005;39, 146153.
7. Broglio F, Gianotti L, Destefanis S, et al. The endocrine response to acute ghrelin administration is
blunted in patients with anorexia nervosa, a ghrelin hypersecretory state. Clin Endocrinol (Oxf)
2004; 60 (5): 592-9
8. Cardona Cano S, Merkestein M, Skibicka KP, et al. Role of ghrelin in the pathophysiology of eating
disorders: implications for pharmacotherapy. CNS Drugs. 2012 Apr 1;26(4):281-96. doi:
10.2165/11599890-000000000-00000.
9. Claudino AM, Hay P, Lima MS, Bacaltchuk J, Schmidt U, Treasure J. Antidepressants for anorexia
nervosa. Cochrane Database Syst Rev 2006; 1: CD004365.
10. Crow SJ, Mitchell JE, Roerig JD, Steff en K. What potential role is there for medication treatment in
anorexia nervosa? Int J Eat Disord 2009; 42: 18.
11. Fassino F, Daga GA, Boggio S, et al. Use of reboxetine in bulimia nervosa: a pilot study. Journal of
Psychopharmacology 2004;18, 423428.
12. Flament MF, Bissada H, Spettigue W. Evidence-based pharmacotherapy of eating disorders. Int J
Neuropsychopharmacol. 2012 Mar;15(2):189-207.
13. Hatch A, Madden S, Kohn MR, Clarke S, et al. Emotion brain alterations in anorexia nervosa: a
candidate biological marker and implications for treatment.J Psychiatry Neurosci. 2010
Jul;35(4):267-74.
52
14. Halmi KA et al. Anorexia nervosa. Treatment efficacy of cyproheptadine and amitriptyline. Arch Gen
Psychiatry 1986; 43:177181.
15. Hay PJ, Claudino AC. Bulimia nervosa. Clinical Evidence Review Update 2010;7, 1009.
16. Hay PJ, Claudino AM. Clinical psychopharmacology of eating disorders: a research update. Int J
Neuropsychopharmacol. 2012 Mar;15(2):209-22.
17. Hoek HW. Incidence, prevalence and mortality of anorexia nervosa and other eating disorders.
Current Opinion in Psychiatry 2006;19, 389394.
18. Hotta M, Ohwada R, Akamizu T, et al. Ghrelin increases hunger and food intake in patients with
restricting-type anorexia nervosa: apilot study. Endocr J 2009; 56 (9): 1119-28
19. Horne RL, Ferguson JM, Pope Jr. HG, Hudson JI, et al. Treatment of bulimia with bupropion: a
multicenter controlled trial. Journal of Clinical Psychiatry 1988; 49, 262266.
20. Hubner HF. Endorphins, eating disorders, and other addictive behaviours. New York, USA: WW
Norton & Company; 1993.
21. Hudson JI, Hiripi E, Pope HG, et al. The prevalence and correlates of eating disorders in the
national comorbidity survey replication. Biological Psychiatry 2007;61, 348358.
22. Marrazzi MA, Bacon JP, Kinzie J. Naltrexone use in the treatment of anorexia nervosa and bulimia
nervosa. International Journal of Clinical Psychopharmacology 1995;10,163172.
23. Miljic D, Pekic S, Djurovic M, et al. Ghrelin has partial or no effect on appetite, growth hormone,
prolactin, and cortisol release in patients with anorexia nervosa. J Clin Endocrinol Metab 2006; 91
(4): 1491-5
24. McElroy SL, Hudson JI, Capece JA, et al. Topiramate for the treatment of binge eating disorder
associated with obesity : a placebo-controlled study. Biological Psychiatry 2007;61, 10391048.
25. Morley JE, Blundell JE. The neurobiological basis of eating disorders: some formulations. Biol
Psychiatry. 1988; 23: 5378.
26. National Institute for Clinical Excellence. Eating disorders: Core interventions in the treatment and
management of anorexia nervosa, bulimia nervosa and related eating disorders. Clinical Guidance
9. 2004; http://www.nice.org.uk.
27. Nickel C, Tritt K, Muehlbacher M, et al. Topiramate treatment in bulimia nervosa patients : a
randomized, double-blind placebo-controlled trial. International Journal of Eating Disorders 2005;
38, 295300
28. Nielsen S. Epidemiology and mortality of eating disorders. Psychiatric Clinics of North America
2001;24, 201214.
29. Noma S, Uwatoko T, Yamamoto H, et al. Effects of milnacipran on binge eating a pilot study.
Neuropsychiatric Disease and Treatment 2008;4, 295300.
30. Ruggiero GM, Laini V, Mauri MC, et al. A single blind comparison of amisulpride, fluoxetine and
clomipramine in the treatment of restricting anorectics. Progress in Neuro-Psychopharmacology
&Biological Psychiatry 2001;25, 10491059.
31. Schu le C, Sighart C, Hennig J, et al. Mirtazapine inhibits salivary cortisol concentrations in
anorexia nervosa. Progress in Neuro-Psychopharmacology &Biological Psychiatry 2006;30, 1015
1019.
32. Shapiro JR, Berkman ND, Brownley KA, et al. Bulimia nervosa treatment: a systematic review of
randomized controlled trials. Int J Eat Disord 2007; 40: 32136.
33. Su JC et al. Zinc supplementation in the treatment of anorexia nervosa. Eat Weight Disord 2002;
7:2022.
34. Taylor D, Paton C, Kapur S. The Maudsley Prescribing Guidelines, 10th Edition, The South London
and Maudsley NHS Foundation Trust, 2009; www.informahealthcare.com
35. Treasure J, Claudino AM, Zucker N. Eating disorders. Lancet. 2010 Feb 13;375(9714):583-93.
Review.
36. Trunko ME, Schwartz TA, Duvvuri V, et al. Aripiprazole in anorexia nervosa and low-weight bulimia
nervosa: case reports. International Journal of Eating Disorders 2010; 44, 269275.
37. Yeomans MR, Gray RW. Opioid peptides and the control of human ingestive behaviour. Neurosci
Biobehav Rev. 2002; 26: 71328.
53
Imaging in Eating Disorders
Fatma zlem Orhan
Neuroimaging techniques have been widely used in a range of psychiatric disorders, providing new
insights into neural brain circuits and neuroreceptor functions in vivo. This allows researchers to study
not only the configuration of brain structures but also aspects of normal and anomalous human
behavior more accurately. Neuroimaging techniques have been also useful tools for accurate
investigation of brain structure and function in eating disorders (1). The first studies of structural
neuroimaging, focused on the brain anatomy in patients with anorexia nervosa (AN) and consistently
showed sulcal widening and ventricular enlargement that usually decreased with refeeding (2,3). Other
specific findings have been a reduction in total gray and white matter volumes compared with healthy
controls or the persistence of the gray matter volume changes when weight is restored (4,5).
There is some debate about the abnormalities of cerebral blood flow in anorexia nervosa as to whether
these abnormalities are secondary to starvation or indicative of a primary abnormality predating the
illness, representing an underlying biological substrate. The main affected cerebral area was the medial
temporal region, the data suggesting that rCBF does not return to normal following weight restoration
(6).
Despite some differences, it seems that gray matter and white matter increase significantly following
weight restoration. With respect to possible differences between adolescents and adults, it has been
stated that gray matter is more affected than white matter in adolescents (7). Abnormalities in ill BN
individuals are less pronounced, although they also have decreased cortical mass (8,9,10). Functional
imaging methods have been utilized to obtain insight to the serotonin receptor binding, regional
cerebral blood flow or glucose consumption. With fMRI, differences have been found in cerebral
processing in patients with eating disorders in response to the presentation of different paradigms, the
majority consisting of showing images of body figures, given the importance of the alteration of body
perception in these disorders (11). fMRI studies using visual stimuli of food or body image in AN
suggested involvement of prefrontal, ACC, and parietal cortex (12). There is less conclusive evidence
for abnormal blood flow in BN patients in the ill state (13). Delvenne and colleagues (14) found reduced
cortical metabolism although this was not supported in other reports.
Images of food had been frequently used in fMRI studies. A study of this type demonstrated the
existence of activation of the anterior cingulate and prefrontal medial cortex in response to images of
food in patients diagnosed of eating disorders but not in controls (11). Additionally diminished activation
of the inferior parietal lobe and occipital cortex in response to visual food stimuli in both AN and BN had
been reported (15).
Abnormalities in the perception and evaluation of body shape are a hallmark of eating disorders and
often persist and pose a risk for relapse even after weight recovery. Therefore, there has been interest
in examining this aspect of the psychopathology. A variety of different experimental paradigms have
been used. The areas of interest for this aspect of psychopathology include both the left parietal lobe
and its connections to the thalamus, which are important for body schema representation (16) and also
the emotional limbic network.
Using line drawings of underweight, normal weight, and overweight female bodies, Uher and
colleagues (17) found a highly consistent pattern of brain activity related to body shape processing in
healthy women and in women with eating disorders. Compared with a control condition (line drawings
of houses), the body images activated in all groups the lateral prefrontal cortex, lateral fusiform gyrus,
and inferior parietal cortex. However, responses in the occipitotemporal and parietal cortices were less
strong in patients with eating disorders.
In accordance with the findings in the Uher and colleagues (17) study, Sachdev and colleagues (18)
found that processing of nonself-images generated a response in similar brain areas in eating
disorder patients (AN) and control subjects. This consisted of an activation of the inferior and middle
frontal gyri (somewhat higher in AN), superior and inferior parietal lobules, posterior lobe of the
cerebellum, and the thalamus (19).
54
In PET studies with 5-HT1A receptors, anorectic patients showed a marked increase (30%70%) in
[11C] WAY-100635BP, a selective ligand in the prefrontal and lateral orbital frontal regions, mesial and
lateral temporal lobes, parietal cortex, and dorsal raphe nuclei (20). Additionally PET studies with 5-
HT2A receptors, it has been found that anorectic patients had normal values of the [18F] altanserin
radioligand (20). Using SPECT and 123I-5-I-R91150, a significantly reduced 5-HT2A binding index
was shown in the left frontal cortex, left and right parietal cortex, and left and right occipital cortex in
patients with anorexia nervosa compared with healthy volunteers. A significant left-right asymmetry
was noted in the frontal cortex (left less than right)(21).
Frank and colleagues (22) demonstrated higher dopamine D2/D3 receptor binding in recovered AN
subjects in the anteroventral striatum, suggesting either decreased intrasynaptic dopamine
concentration or increased D2/D3 receptor density or affinity to be present in AN.
It must be noted that neuroimaging studies in eating disorders have varied widely in terms of sample
size, imaging technology used, age of participants, brain regions assessed, and duration of illness.
Sample sizes have usually been small, which potentially affects the statistical power of these studies
(1). Functional imaging findings with disease-specific cues in patient groups should be interpreted with
caution. These may be merely correlates of the disorder rather than biomarkers that may relate
etiology.
In this presentation, it was aimed to review the newly developed neuroimaging methods that have
gained importance in the field of research conducted on the etiology of eating disorders.
REFERENCES
1. Juregui-Lobera I. Neuroimaging in eating disorders. Neuropsychiatr Dis Treat.2011;7:577-84.
Epub 2011 Sep 29.
2. Palazidou E, Robinson P, Lishman WA. Neuroradiological and neuropsychological assessment in
anorexia nervosa. Psychol Med. 1990; 20(3):521527.
3. Katzmann DK, Zipursky RB, Lambe EK, Mikulis D. A longitudinal magnetic resonance imaging
study of brain changes in adolescents with anorexia nervosa. Arch Pediatr Adolesc Med.
1997;151(8):793797.
4. Artmann H, Grau H, Adelmann T, Schleiffer R. Reversible and nonreversible enlargement of
cerebrospinal fluid space in anorexia nervosa. Neuroradiology. 1985;27(4):304312.
5. Krieg JC, Pirke KM, Lauer C, Backmund H. Endocrine, metabolic, and cranial computed
tomographic findings in anorexia nervosa. Biol Psychiatry. 1988;23(4):377387.
6. Frampton I, Watkins B, Gordon I, Lask B. Do abnormalities in regional cerebral blood flow in
anorexia nervosa resolve after weight restoration? Eur Eat Disord Rev. 2011;19(1):5558.
7. Castro-Fornieles J, Cald X, Andrs-Perpi S, et al. A cross-sectional and follow-up functional
MRI study with a working memory task in adolescent anorexia nervosa. Neuropsychologia.
2010;48(14): 41114116.
8. Hoffman GW, Ellinwood EH Jr, Rockwell WJ, et al. Cerebral atrophy in bulimia. Biol Psychiatry
1989;25(7):894902.
9. Husain MM, Black KJ, Doraiswamy PM, et al. Subcortical brain anatomy in anorexia and bulimia.
Biol Psychiatry 1992;31(7):7358.
10. Laessle RG, Krieg JC, Fichter MM, et al. Cerebral atrophy and vigilance performance in patients
with anorexia nervosa and bulimia nervosa. Neuropsychobiology 1989;21(4):18791.
11. Tejado Lde A, Ruiz RM, Trebbau H, Diaz-Mars M, Perera JL. Functional magnetic resonance
studies in eating behavior disorders. Actas Esp Psiquiatr. 2010May-Jun;38(3):183-8.
12. Frank GK, Bailer UF, Henry S, Wagner A, Kaye WH. Neuroimaging studies in eating disorders.
CNS Spectr. 2004 Jul;9(7):539-48.
13. Delvenne V, Goldman S, Simon Y, et al. Brain hypometabolism of glucose in bulimia nervosa. Int J
Eat Disord 1997;21(4):31320.
14. Delvenne V, Goldman S, De MV, et al. Brain glucose metabolism in eating disorders assessed by
positron emission tomography. Int J Eat Disord 1999; 25(1):2937.
15. Uher R, Murphy T, Brammer MJ, Dalgleish T, Phillips ML, Ng VW, Andrew CM, Williams S,
Campbell IC, Treasure J. Medial prefrontal cortex activity associated with symptom provocation in
eating disorders. Am J Psychiatry 2004;161:1238-46.
16. McGlynn SM, Schacter DL. Unawareness of deficits in neuropsychological syndromes. J Clin Exp
Neuropsychol 1989;11(2):143205.
17. Uher R, Murphy T, Friederich HC, et al. Functional neuroanatomy of body shape perception in
healthy and eating-disordered women. Biol Psychiatry 2005; 58(12):9907.
18. Sachdev P, Mondraty N, Wen W, et al. Brains of anorexia nervosa patients process self-images
differently from non-self-images: an fMRI study. Neuropsychologia 2008;46(8):21618.
55
19. Van den Eynde F, Treasure J. Neuroimaging in eating disorders and obesity: implications for
research. Child Adolesc Psychiatr Clin N Am. 2009 Jan;18(1):95-115.
20. Bailer UF, Frank GK, Henry SE, et al. Exaggerated 5-HT1A but normal 5-HT2 A receptor activity in
individuals ill with anorexia nervosa. BiolPsychiatry. 2007;61(9):10901099.
21. Audenaert K, Van Laere K, Dumont F, et al. Decreased 5-HT2A receptor binding in patients with
anorexia nervosa. J Nucl Med. 2003;44(2):163169.
22. Frank GK, Bailer UF, Henry SE, et al. Increased dopamine D2/D3 receptor binding after recovery
from anorexia nervosa measured by positron emission tomography and [11c] raclopride. Biol
Psychiatry 2005;58(11):90812.
56
Hormonal Changes in Eating Disorders
Dr. Bilge Burak Annagr
Seluk University, Faculty of Medicine, Department of Psychiatry, Konya-Turkey
Patients with eating disorders are at risk of a wide range of physical complications. In anorexia nervosa
(AN), almost any physiological system may be affected, whereas in bulimia nervosa (BN) the potential
problems are more restricted. Although some complications are relatively benign, others are potentially
life-threatening; cardiac and biochemical abnormalities are particularly dangerous. Some complications
are secondary to malnutrition, while others are the result of purging. Re-feeding can lead to serious
physiological and biochemical disturbances.
The endocrine alterations reported in patients with anorexia nervosa appear to be secondary to
disturbed hypothalamic function. This is particularly so with regard to the gonadotropin disturbance
which reflects the amenorrhea. Basal luteinizing hormone (LH) levels are significantly lower in anorexic
patients when compared to nonanorexic dieters and to a normal control group. In addition, an
immaturity of the circadian pattern of plasma LH has been described in anorexic patients. Adequate
nutrition is essential for normal reproductive function in woman. Menarche occurs at a critical level of
'fatness' and it appears that the hypothalamic events leading to pubertal development and the
achievement of reproductive competence may be triggered by metabolic/endocrinological changes due
to an increase in fat. Amenorrhoea in anorexia nervosa is due to hypogonadotrophic hypogonadism
and the primary disturbance appears to be at the hypothalamic level. Levels of the weight regulatory
hormone leptin are low, and rising levels are thought to be important in triggering the resumption of
menstruation. Amenorrhoea is a sensitive indicator of weight loss and usually returns to normal on
weight restoration. However, the resumption of menstruation may be delayed by several months and
some patients need to attain a higher weight than that at menarche. Persistent amenorrhoea or
oligomenorrhoea at normal weight may indicate continuing disordered eating.
Pituitary GH secretion is increased at the expense of decreased IGF-1 production, suggesting tissue
resistance to GH. Although cause and effect relationship is not clear, previous studies indicated altered
concentrations of serum adipocytokines and/or loss of associations with body fat mass in AN patients.
Significant loss of bone mineral density occurs in up to 40% of patients and the risk of pathological
fractures is substantially increased. There are a number of possible aetiological mechanisms involved.
Oestrogen deficiency is a major risk factor but hypercortisolism, deficiency of specific nutrients and low
levels of insulin-like growth factor-I may also be relevant. Biochemically, there is evidence of increased
bone resorption and reduced bone formation. Women whose eating disorder begins early in life may
fail to attain their expected peak bone mass, and this has implications for osteoporosis and its
complications after the menopause.
In patients with AN, extremely low serum levels of T3 are though to be the result of impaired peripheral
conversion of thyroxin (T4) to T3, associated with chronic starvation. The secretion of cortisol has
previously been described in anorexia nervosa. Insulin sensitivity, and insulin resistance have been
documented. Moreover, AN-R patients have been found to have increased circulating ghrelin levels.
57
Gene-Environment Interaction in Eating Disorders
Dr. Yasemin Grgl
Trakya University, Faculty of Medicine, Department of Psychiatry, Edirne-Turkey
Eating disorders have complex aetiologies involving numerous and interacting environmental and
genetic risk factors. Disorders or traits that are not inherited in a Mendelian fashion are known as
complex or multifactorial diseases, which result from a complex interplay between multiple
environmental and genetic risk factors. The genetic component may be oligogenic, involving a small
number of gene variants or polygenic, involving the simultaneous action of many gene variants each of
individually small effect. The genetic variants that contribute to complex diseases are common in the
population, whereas Mendelian diseases are caused by relatively rare deleterious variants (mutations)
in single genes (monogenic disorder). The genetic variants of genes involved in the predisposition to a
complex disease are called susceptibility alleles and are neither necessary nor sufficient to cause
disease.
Polygenic traits will be continuously distributed in the population, they are quantitative traits. However,
many complex diseases are qualitative (dichotomous) disorders, where you either have or do not have
the disease, but are also polygenic. A liability-threshold model has been proposed for polygenic
dichotomous diseases. In this model the underlying polygenic liability is continuously distributed in the
population and there is a threshold of liability (1). A disease will only develop when the number of
susceptibility alleles exceeds the liability threshold. Genegene interactions (epistasis), in which a gene
variant will only confer susceptibility in the presence of another gene variant, and geneenvironment
interactions, in which susceptibility alleles will have their deleterious effects only in the presence of a
particular environmental factor, are likely to be involved in the predisposition to complex diseases.
Environmental factors are important and complex diseases will develop in those carrying the greatest
genetic and environmental loading.
Family, twin and adoption studies are used to determine the relative contribution of genetic and
environmental risk factors in the aetiology of complex diseases, such as eating disorders. In family
studies the frequency of a disease in the relatives of an affected individual is compared with the
frequency in the general population. A higher disease frequency in relatives compared to the general
population provides evidence for a genetic susceptibility to a disease. However, familial aggregation of
a disease could also be explained by shared family environment. Twin and adoption studies are
powerful methods of disentangling genetic from environmental sources of family resemblance (1).
Family Studies of Eating Disorders
Two controlled family studies have found an average 3% lifetime risk of Anorexia Nervosa (AN) in first-
degree relatives of patients, being equivalent to an approximate relative risk of at least 10 (2). AN was
found to be infrequent in 1,831 relatives of 504 patients with eating disorders, whereas full and partial
syndromes of these eating disorders aggregated in female relatives of both anorexic and bulimic
probands. Relative risks were 11.3 and 12.3 for the full syndrome of AN in first-degree female relatives
of patients with AN or ulimia Nervosa (BN), respectively (3), suggesting that specific genes can
predispose to both eating disorders. The relative risks for BN were 4.2 and 4.4 for first-degree female
relatives of patients with AN or BN, respectively.
The majority of family studies have shown that eating disorders are familial. One of the largest case-
control family study, the risk for AN in female relatives of anorexic probands was 11.4 times higher than
the risk in the relatives of control subjects, and the risk for BN in female relatives of bulimic probands
was 3.7 times higher (4). Some family studies have also reported familial aggregation of milder,
broader (subthreshold) phenotypes of AN and BN among female relatives of AN and BN probands
respectively (5). The prevalence of full and subthreshold BN has been shown to be greater in female
relatives of AN probands than in the relatives of control subjects, and the converse for relatives of BN
probands. Based on the above observations it has been proposed that the full and subthreshold forms
of eating disorders form a spectrum of clinical severity in which there is a continuum of familial liability
(4).
The familial aggregation of full and subclinical eating disorders suggests that genetic factors are likely
to be involved in causation. The relative contribution of genetic and environmental factors in the
aetiology of eating disorders has been determined in twin studies.
58
Twin Studies of AN and BN
Evidence from family and twin studies suggests a substantial genetic contribution to the etiology of both
AN and BN. Different estimates of heritability have been obtained from twin studies of AN. Holland et
al. showed proband-wise concordance rates for AN of 0.71 for monozygotic twins and 0.1 for dizygotic
twins (6). Heritability estimates based on these rates ranged from 0.86 to 0.98 for AN (7). Higher
concordance rates for monozygotic twins than for dizygotic twins have been shown in most twin
studies. The heritability of AN was estimated to be 76% in another population-based twin sample and
58% in a bivariate analysis of AN and major depression. The magnitude of the genetic contribution to
AN remains unresolved. Large-scale twin studies are needed to define the extent and nature of the
genetic and environmental contributions to the aetiology of AN.
Three clinically ascertained twin pair studies of BN and two population-based twin studies of BN have
been conducted and have consistently demonstrated significant genetic contributions in the liability to
BN. Reanalysis of the data from the twin studies of BN produced estimates of heritabilty ranging from
31% to 83%. In general non-shared environmental effects were shown to account for the remaining
variance in liability to BN. The magnitude of the contribution of shared environmental effects is unclear
but in the majority of the twin studies it appears to be less important than additive genetic effects and
non-shared environmental effects (8).
Several of the symptoms, behaviours and attitudes associated with disordered eating have been shown
to be heritable in different populations of twins. These continuous traits are assessed using
psychometric questionnaires. Heritabilities of 46% and 70% have been reported for binge eating and
self-induced vomiting respectively. There is evidence of age-related differences in genetic and
environmental influences on these traits. Marked differences in heritabilities for Eating Disorder
Inventory (EDI) subscales have been reported for a preadolescent (aged 11 years) and an adolescent
(aged 17 years) twin sample from the same population. The contribution of additive genetic effects for
the EDI subscales was greater in the adolescent twin sample than in the preadolescent group. Based
on this finding it has been proposed that puberty may activate the heritability of eating disorders (9).
Several family and twin studies have investigated the causes of comorbidity between eating disorders
and personality traits and other psychiatric disorders. Family studies investigating the relationship
between personality traits and eating disorders have shown that some personality traits are significantly
elevated in the unaffected relatives of probands with an eating disorder compared to the relatives of the
control group. For example perfectionism, ineffectiveness, and interpersonal distrust has been found to
be significantly elevated in the unaffected relatives of BN probands compared to the relatives of the
control group. There is evidence to suggest that the familial cotransmission of eating pathology and
some personality traits results from the sharing of common genetic risk factors. Results from twin
studies suggest that the comorbidity between AN and major depression and between BN and major
depression is most likely due to genetic factors that influence both disorders. It is evident from these
studies that there are also unique genetic effects influencing eating disorders that are independent of
those contributing to the personality traits and psychiatric disorders.
Candidate gene studies
Basically, two approaches are involved in the molecular genetic analysis of a complex phenotype: (1)
association studies (casecontrol studies), including genome-wide association studies (GWAS) and (2)
family-based linkage studies. Both approaches have in general been used for molecular genetic
studies of eating disorders, although GWAS are still lacking. The candidate gene approach relies on
genetic, physiological, biochemical or pharmacological evidence to determine the involvement of a
specific gene in the analyzed phenotype.
Neurotransmitter systems implicated in eating disorders
Serotonergic system
Several lines of evidence implicate the serotonergic system in body weight regulation and more
specifically in eating behaviorand eating disorders. The 5-HT2A receptor gene might tentatively be
considered as a candidate gene for AN. The promoter region of the serotonin transporter (5-HTTLPR)
harbors a functional insertion/deletion polymorphism with two frequent alleles that were designated as
short (S) and long (L) alleles. The frequency of the 5-HTTLPR S allele has been assessed in AN and
BN, with conflicting results. A meta-analysis for AN indicates that the S allele could represent a risk
factor for AN (10).
59
Norepinephrine
In long-term weight-restored patients with AN, lower serum norepinephrine levels than in controls were
measured. Following up on previous studies on single genes, Urwin et al. investigated epistasis
between the 5-HTT and NET in AN. However, epistasis between the 5-HTTLPR and the polymorphism
within the NET promoter polymorphic region (NETpPR) was not observed (11).
Dopaminergic system
The dopaminergic system has been implicated in the pathophysiology of AN and BN. For example,
major symptoms related to AN like repulsion to food, weight loss, hyperactivity, distortion of body
image, and obsessivecompulsive behavior have all been related to dopamine activity. Association
studies on the role of polymorphisms in the dopamine D4 receptor gene (DRD4), mainly the 7-repeat
allele of the DRD4 exon 3 repeat, in AN have yielded positive as well as negative results (12). The
catechol-O-methyltransferase gene (COMT) catabolizes brain catecholamine neurotransmitters such
as dopamine and norepinephrine. An initial study suggested an influence of the Val158Met
polymorphism on susceptibility to AN. Data were confirmed in some but not all studies. As most of the
reported studies on the genetic influence of the dopaminergic system on the etiology of AN and BN did
not have sufficient statistical power, these findings require replication in large independent samples or
at least in a meta-analytical approach.
Body weight regulation: leptinergicmelanocortinergic system
Hypoleptinemia is a cardinal feature of acute AN, and in most studies the low leptin levels are typically
below those of healthy gender- and age-matched controls and reflect the low fat mass, thus signaling
energy depletion to the brain. A mutation analysis of the coding region and part of the promoter region
of the leptin gene in patients with AN, followed by casecontrol studies of the detected polymorphisms,
yielded negative results. Leptin receptor gene SNPs also do not appear to be associated with
regulation of body weight or with AN (13). Agouti related peptide (AGRP) is an important orexigenic
peptide that regulates energy balance downstream of leptin. AGRP is an endogenous inverse agonist
at melanocortinergic receptors and therefore involved in body weight regulation. Loss-of-function
mutations in AGRP could result in an inadequate starvation signaling in the brain. In patients with AN
three polymorphisms were detected in AGRP.
Melanocortin-4 receptor
A dominant form of obesity is conferred by mutations in MC4R that lead to a reduced receptor function.
BDNF
Several studies investigated the role of the BDNF non-synonymous polymorphism Val66Met in the
etiology of EDs. The 66Met variant was found to be associated with AN restricting type in a Spanish
sample.
Genome-wide linkage studies
AN
Several regions of suggestive linkage were found: one close to genome-wide significance on
chromosome 1, chromosome 2 and on chromosome 13. By comparing these results with those
implemented using more standard linkage methods, covariates that convey substantial information for
the linkage analysis were found. Initial candidate gene analyses pertaining to the linkage region on
chromosome 1p36.334.3 (14). Linkage analysis of polymorphisms in the serotonin 1D receptor gene
(5-HT1DR) and the opioid delta receptor gene (OPRD1) together with 33 microsatellite markers in
families including relative pairs concordantly affected with restricting AN substantially increased the
evidence for linkage of this region to restricting AN.
BN
A gene on chromosome 10p might well be involved in both obesity and BN. Another region on 14q met
the criterion for genome-wide suggestive linkage for BN at 62 cM from p-ter (15). The underlying genes
for BN have not been described yet.
Epigenetics
Epigenetic factors are thought to mediate, at least in part, the relationship between the genome and the
environment. Research on epigenetic factors underlying eating disorders is at the very beginning. A
first study revealed global DNA hypomethylation, but at the same time DNA hypermethylation of the
alpha synuclein gene promoter in females with AN. Two further studies investigated whether the mRNA
expression of dopaminergic genes or of genes for the peptide hormones vasopressin and atrial
natriuretic peptide (ANP) are altered in blood of patients suffering from eating disorders. It was also
analyzed if these alterations can be explained by changes in the promoter specific DNA methylation of
60
these genes (16). The primary results in a very small sample pointed to a disturbed expression of the
dopaminergic genes and ANP.
Eating disorders endophenotypes
The definition of endophenotypes and their use for genetic association studies to reduce the
heterogeneity in samples based on a clinical diagnostic category has been widely discussed. Defined
endophenotypes as measurable neurophysiological, biochemical, endocrinological, neuroanatomical,
cognitive, or neuropsychological components see also (17). Additionally, they are heritable,
cosegregate with a psychiatric clinical phenotype in the general population, are state independent, and
are found in non-affected family members at a higher rate than in the general population (18). Specific
susceptibility gene variants may underly endophenotypes, which in turn may predispose individuals to
develop eating disorders and related conditions.
Gene and environment interactions
Both genetic and environmental factors contribute to the development of complex diseases like eating
disorders. If a genetic factor requires the presence of an environmental factor to result in increased
risk, a situation of gene and environment interactions (G&E) is given. Interacting genetic and
environmental factors are distinguished by small to moderate effects. A number of genetic variants
might affect several genes influencing vulnerability to eating disorders. As an example, an individual
with genetic vulnerability to AN might become ill by exposure to high-risk environments like figure
skating or fashion shows. While both the current knowledge on genetic risk factors and on
environmental risk factors has been excellently reviewed previously the knowledge on G & E is limited.
No studies have yet reported distinct findings on G & E interactions in eating disorders. In part this may
be due to design challenges of G & E studies reviewed in (19). Following Dempfle et al., the
investigation of G & E interactions may be more rewarding for the detailed characterization of identified
disease genes (i.e., at advanced stages of genetic research) as strong G & E interactions may have
also contributed to the detection of the gene itself (20). Variations in the 5-HT2A receptor gene as well
as in the BDNF gene represent the most consistently supported genetic findings for eating disorders.
As their genetic impact on the etiology of eating disorders was solidly shown, they are presumably the
best candidates to investigate interactions with environmental factors. Ideally, genetic research will help
to improve the understanding of environmental risk factors for eating disorders.
References
1. Plomin, R., Defries, J.C., McClearn, G.E. & McGuffin, P. (2001) Behavioural Genetics (4th edition).
Worth Publishers and W.H. Freeman & Company.
2. Kaye WH, Klump KL, Frank GK, Strober M. Anorexia and bulimia nervosa. Annu Rev Med.
2000;51:299313.
3. Strober M, Freeman R, Lampert C, Diamond J, Kaye W. Controlled family study of anorexia
nervosa and bulimia nervosa: evidence of shared liability and transmission of partial syndromes.
Am J Psychiatry. 2000;157:393401.
4. Strober, M., Freeman, R., Lampert, C., Diamond, J. & Kaye, W. (2000) Controlled family studyof
anorexia nervosa and bulimia nervosa: Evidence of shared liability and transmision of partial
syndromes. Am. J. Psychiat., 157, 393401.
5. Stein, D., Lilenfeld, L.R., Plotnicov, K., Pollice, C., Rao, R., Strober, M. & Kaye,W. (1998) Familial
aggregation of eating disorders: Results from a controlled family study of bulimia nervosa. Int. J.Eat.
Disord., 26, 211215.
6. Holland AJ, Hall A, Murray R, Russell GF, Crisp AH. Anorexia nervosa: a study of 34 twin pairs and
one set of triplets. Br J Psychiatry. 1984;145:414419.
7. Holland AJ, Sicotte N, Treasure J. Anorexia nervosa: evidence for a genetic basis. J Psychosom
Res. 1988;32:561571.
8. Bulik, C.M., Sullivan, P.F., Wade, T.D. & Kendler, K.S. (2000) Twin sudies of eating disorders: A
review. Int. J. Eat. Disord., 27, 120.
9. Klump, K.L., McGue, M. & Iacono, W.G. (2000) Age differences in genetic and environmental
influences on eating attitudes and behaviours in preadolescent and adolescent twins. J. Abnorm.
Psychol., 109, 239251.
10. Gorwood P. Eating disorders, serotonin transporter polymorphisms and potential treatment
response. Am J Pharmacogenomics. 2004;4:917.
11. Urwin RE, Bennetts BH, Wilcken B, Beumont PJ, Russell JD, Nunn KP. Investigation of epistasis
between the serotonin transporter and norepinephrine transporter genes in anorexia nervosa.
Neuropsychopharmacology. 2003;28:13511355.
12. Hinney A, Schneider J, Ziegler A, Lehmkuhl G, Poustka F, Schmidt MH et al. No evidence for
involvement of polymorphisms of the dopamine D4 receptor gene in anorexia nervosa, underweight,
and obesity. Am J Med Genet. 1999;88:594597.
61
13. Quinton ND, Meechan DW, Brown K, Eastwood H, Blakemore AI. Single nucleotide polymorphisms
in the leptin receptor gene: studies in anorexia nervosa. Psychiatr Genet. 2004;14:191194.
14. Bergen AW, Bree MB, Yeager M, Welch R, Ganjei JK, Haque K, et.al. Candidate genes for
anorexia nervosa in the 1p3336 linkage region: serotonin 1D and delta opioid receptor loci exhibit
significant association to anorexia nervosa. Mol Psychiatry. 2003;8:397406.
15. Bulik CM, Devlin B, Bacanu SA, Thornton L, Klump KL, Fichter MM, et al. Significant linkage on
chromosome 10p in families with bulimia nervosa. Am J Hum Genet. 2003;72:200207.
16. Frieling H, Bleich S, Otten J, Rmer KD, Kornhuber J, Zwaan M, et al. Epigenetic downregulation of
atrial natriuretic peptide but not vasopressin mRNA expression in females with eating disorders is
related to impulsivity. Neuropsychopharmacology. 2008;33:26052609.
17. Gottesman I, Gould T. The endophenotype concept in psychiatry: etymology and strategic
intentions. Am J Psychiatry. 2003;160:636645
18. Hasler G, Drevets W, Gould T, Gottesman I, Manji H. Toward constructing an endophenotype
strategy for bipolar disorders. Biol Psychiatry. 2006;60:93105.
19. Moore JH, Williams SM. Epistasis and its implications for personal genetics. Am J Hum Genet.
2009;85:309320.
20. Dempfle A, Scherag A, Hein R, Beckmann L, Chang-Claude J, Schfer H. Gene-environment
interactions for complex traits: definitions, methodological requirements and challenges. Eur J Hum
Genet. 2008;16:11641172.
62
GABA and Schizophrenia in Preclinical Relationship Reflections
Hseyin Gnay
Which is an inhibitory neurotransmitter in the pathophysiology of schizophrenia aminoaist amino
butyric acid (GABA) are also mentioned. GABA, glutamic acid decarboxylase (GAD) produces by way
of. Directly under the control of GABA ergic neurons in the production of dopaminergic neurons
dopmin. Low density of GAD, and ultimately lower levels of dopamine leads to increase of GABA.
Pyridoxal 5-phosphate (vitamin B6), the basic cofactor in the synthesis of GABA.
Geneticabnormalities in the metabolism of pyridoxine or pyridoxine antagonist (eg, isoniazid) taken,
and schizophrenia is associated with a decrease in GAD activity by disrupting the synthesis of GABA
leads to the emergence of symptoms of confusion and irritability.
GABA receptors in the GABA A and GABA B receptors are divided into two main groups. GABA A
receptors was found to be associated with schizophrenia. The activity of GABA by increasing GABA A
receptor agonists such as clonazepam, some lead toattenuating symptoms of schizophrenia (1).
Divided into 19 different subtype of GABA A receptors:
Composition of the different subtypes, anatomical, physiological and pharmacologicalcharacteristics.
Tonic and phasic GABA A receptor subunit in two separate acts according to their form.Extra-synaptic
localization of subunit containing receptors showing regulate tonicGABAergic inhibition.
Chloride gradient is provided by the inhibitory actions of GABA as a basis. In this, the primary K / Cl
cotransporteri KCC2 plays a role in adult brain. The surface expression ofKCC2 and KCC2 activity is
regulated by residue Ser940.
Immature neurons, Na, K, Cl, the depolarising effect of GABA cotransporter result inexpression of
mature neurons, GABA the depolarization, the inhibitory effect throughinhibition of hippocampal
neurons shunting. KCC2 in the deficit, resulting crop ofGABAergic inhibition and ischemia, neuropathic
pain, trauma, can cause many diseasessuch as epilepsy (2).
GABAergic markers were decreased in schizophrenia in postmortem tissue samples.GAD67 mRNA
primary GABA-synthesizing enzyme and this enzyme s neocorticalregions decreased in patients with
schizophrenia. (3). Perisomatik GABAergicinterneurons and pyramidal cells responsible for the axon-
aksonik awakenings, and calcium-binding protein and parvalbumin (PV) contain. Schizophrenia is a
reduction inexpression of parvalbuminin neocortical regions. (4). Regulated activity in the cerebral
cortex are intenronlar PV oscillator. (5). Neurocognitive deficits in schizophrenia on the basis of
many corruption lies in the dynamics of cortical oscillator (6).
Animal test models, NMDA receptor antagonists are shown to decrease expression ofadministration of
PV. (7). Acute administration of NMDA receptor antagonists (PCP, ketamine, MK-801), attempted to
establish findings and behavioral symptoms ofschizophrenia. Romo et al made a study, 4 and 24
hours after administration of MK-801and PV GAD67 mRNA expression in brain regions, and look at 4
hours afteradministration of MK801 Frequence dentate gyrus and hippocampus mRNA decreaseof
PV, PV mRNA expression 24 hours after the reduction of medial prefrontal,orbitofrontal and entorhinal
cortex, hippocampus, and amygdala, the basolateral nucleusis shown spread. PV mRNAs decreased
in these brain regions, the postmortem brains of schizophrenia decreased GABAergic markers
detected findings are in line with the departments. (8)
The most widely used model of acute or chronic NMDA antagonism in schizophrenia. Excitatory
pyramidal neurons and GABAergic interneurons in the PFC with the prenatal and postnatal periods is
responsible for the development of executive functions. A developmental damage, may be responsible
for dysfunction in adult age. In a study, 7th postnatal day NMDA antagonist, was given. This adult
hippocampal neuronal loss inthe thalamic regions and damage. GABAergic cortical interneurons about
50% of superficial layers have recently been shown to cause a loss. (9).
As a result, GABA association with schizophrenia and should be reconsidered with the developments
in the field of neuroscience. In addition, the former hypothesis appears to be abandoned again to
review the conviction will benefit from growing stronger.
63
REFERENCES:
1. Uzun .,izofreni Farmakolojik Tedavi Klavuzu, 2008, s:21
2. Sarkar J, Wakefield S, MacKenzie G, Stephen J, Maguire M, Neurosteroidogenesis Is Required for
the Physiological Response to Stress: Role of Neurosteroid-Sensitive GABAA Receptors, 2011,
The Journal of Neuroscience, December 14, 2011 31(50):18198 18210)
3. Akbarian S, Huang HS (2006) Molecular and cellular mechanisms of altered GAD1/GAD67
expression in schizophrenia and related disorders. Brain Res Brain Res Rev 52:293 304
4. Lewis DA, Hashimoto T, Volk DW (2005) Cortical inhibitory neurons and schizophrenia. Nat Rev
Neurosci 6:312 324
5. Sohal VS, Zhang F, Yizhar O, Deisseroth K (2009) Parvalbumin neurons and gamma rhythms
enhance cortical circuit perfor-mance. Nature 459:698 702
6. Lewis DA, Gonzlez-Burgos G (2008) Neuroplasticity of neocortical circuits in schizophrenia.
Neuropsychopharmacology 33:141 165
7. Morrow BA, Elsworth JD, Roth RH (2007) Repeated phencyclidine in monkeys results in loss of
parvalbumin-containing axo-axonic projections in the prefrontal cortex. Psychopharmacology
Berl192:283 290
8. Romon T, Mengod G, Adell A, (2011) Expression of parvalbumin a nd glutamic acid
decarboxylase-67 after acute administration of MK-801. I mplications for the NMDA hypofunction
model o f schizophrenia, Psychopharmacology DOI 10.1007/s00213-011-2268-6
9. Leon G, Coleman L, Jarskog F, Sheryl S, Fulton M, (2009)Decits in adult prefrontal cortex
neurons and behavior following early postnatal NMDA antagonist treatment Pharmacology,
Biochemi stry and Behavior 93 322 330
64
Schizophrenia and GABA Reflections
Recep Ttnc
Gamma amino butyric acid (GABA) is the most common neurotransmitter in central nervous system. It
has pre and post synaptic effects. It inhibits presynaptic excitator neurotransmitter release and
stimulates postsynaptic GABA-A receptors. GABAergic neurons are mostly inhibitory interneurons.
They may be as principle efferents in striatum.
There are findings of GABA and schizophrenia in 1970s. It is known that GABA and dopamin act
reciprocally. In 1972, Robert et.al. found GABA decline in schizophrenia and suggested an etiological
model. But postmortem studies did not support this suggestion. In 1978, Bird et. al. stated that GABA
decline is related to agony during death and it is not due to neurochemical abnormalities.
In the last decade, GABA deficit hypothesis again became important. It was showed that parvalbumin
expressing GABA interneurons were reduced in cortex and hippocampus. This is also supported by
molecular evidence, indicating reduced mRNA and protein for the GABA synthesizing enzyme, GAD67,
in cortex and hippocampus. Another product of GABA secreting neurons during adulthood, reelin is
reduced 30 to 50 percent in schizophrenia and bipolar disorder with psychotic symptoms. This
decrease does not appear disease specific but it is consistent with interneuron deficiency. Such a
deficiency, leading to diminished GABA signaling, may underlie a potential compensatory increase in
GABA-A receptor binding and benzodiazepine binding remains unchanged. Generally, specific
changes in a subpopulation of GABA interneurons may underlie in schizophrenia etiology.
Different subpopulations of GABA internerons originate from distinct precursors. In addition, the timing
and sequence of GABA interneuron generation may depend on a regulatory genetic network which are
gene candidates to examine in schizophrenia. The abnormal regulation of these factors may lead to
GABA interneuron formation and cause genetic vulnerability.
As a result, the deficit of GABAergic system that is shown in schizophrenia, is a new etiolgical
possibility with the other factors.
65
GABA in the Psychopharmacology of Schizophrenia
Hakan Balbey
The dopamine neurotransmission is the most intensively studied brain system in schizophrenia.
Several technical approaches have been used to test the hypothesis that dopaminergic transmission
hyperactivity is associated with this psychiatric disorder. Thus, in postmortem brain studies, an
increased density of striatal D2 dopamine (D2) receptors is the most common finding. The dopamine
hypothesis of schizophrenia has guided schizophrenia research for several decades and has clearly
proven its heuristic value. However, despite emerging direct evidence supporting a dopaminergic
dysfunction in schizophrenia, this hypothesis is now yielding to a multifactorial view, in which the other
monoamines as well as glutamate and GABA are joining up. Research in this area tends to focus on
neurotransmitter interactions in complex neurocircuits. The primary lesion(s) in schizophrenia may not
even involve any of these neurotransmitters directly but could deal, for example, with a more general
defect in connectivity, perhaps of developmental origin. Nevertheless, the identification of
neurotransmitter aberrations in schizophrenia, now underway, is likely to bring clues for understanding
the fundamental nature of the disease as well as for the development of new treatment and prevention
strategies.
GABA, the principal inhibitory neurotransmitter in the brain. Gamma-amino butyric acid (GABA) is
thought to play a role in the pathophysiology of schizophrenia. Impairments in cognitive control, such
as those involved in working memory, are associated with dysfunction of the dorsolateral prefrontal
cortex (DLPFC) in individuals with schizophrenia. This dysfunction appears to result, at least in part,
from abnormalities in GABA-mediated neurotransmission. Synchronization of neuronal activity in the
neocortex may underlie the coordination of neural representations and thus is critical for optimal
cognitive function. Because cognitive deficits are the major determinant of functional outcome in
schizophrenia, identifying their neural basis is important for the development of new therapeutic
interventions.
GABA neurons may play a role in the synchronization of rhythms across brain regions. For example,
they could be targets of long distance projections between different cortical areas or may be the targets
of a common input that provides a synchronization signal across cortical regions. Thus, alterations in
GABA neurotransmission might also contribute to the reported deficits in synchronization of oscillation
phase, or phase locking, in schizophrenia.
Postmortem studies suggest that markers of reduced GABA neurotransmission in schizophrenia may
be selective for, or at least particularly prominent in, the subclass of GABA neurons, chandelier cells,
that provide inhibitory input to the axon initial segment of populations of pyramidal neurons. Given the
critical role that chandelier cells play in synchronizing the activity of pyramidal neurons, the
pharmacological amelioration of this deficit may be particularly effective in normalizing the neural
network activity required for working memory function. Because GABA
A
receptors containing the a
2
subunit are selectively localized to the axon initial segment of pyramidal cells, and appear to be
markedly up-regulated in schizophrenia, treatment with novel benzodiazepine-like agents with
selective activity at GABA
A
receptors containing the a
2
subunit may be effective adjuvant agents for
improving working memory function in schizophrenia.
The past couple of decades witnessed the emergence of novel ideas regarding schizophrenia
pathophysiology that originated from both human and animal studies. The findings that glutamate and
gamma-aminobutyric acid transmission are affected in the disease led to the hypothesis of altered
inhibitory neurotransmission as critical for cognitive deficits and to an exploration of novel therapeutic
approaches aimed at restoring excitation-inhibition balance. Much is to be done yet to elucidate the
ultimate mechanisms by which excitation and inhibition are affected in schizophrenia. Understanding
the interactions between, and the pathophysiological consequences of, these alterations in markers of
GABA neurotransmission may lead to the identification of new drug targets for improving the cognitive
deficits of schizophrenia. Usually betwen GABA and Dopamine (DA) assumed to be an inverse
relationship. Benzodiazepines can be used as an effective treatment of schizophrenia clarified certain
points. But at some point have had no reply yet. There are questions waiting to be researched.
Developed in the last few years some partial benzodiazepine agonists used in the clinic.
GABA for future treatment of schizophrenia has an increasing importance in which must be studied
carefully on the neurotransmitter. Drugs will have an effect on GABA can provide significant benefits in
the treatment of psychosis. In this presentation in light of the current literature GABA in the
psychopharmacology of schizophrenia will be discussed.
66
The Future of Schizophrenia and GABA
Murat Erdem
Early findings indicated that GABA has a profound influence on dopamine activity. This hypofunctional
GABA hypothesis is now gaining wide acceptance as genetic, molecular, and circuit-based studies
clarify the contribution of GABA signaling abnormalities to the disease. Cognitive deficits are
considered to be core features of schizophrenia and there is strong evidence that disturbances in
GABA signaling may contribute to these deficits. The ionotropic GABA type A receptors (GABAARs)
mediate the majority of fast synaptic inhibition in the mammalian brain. GABAARs are sensitive to a
considerable number of pharmacological agents (benzodiazepines, barbiturates, neurosteroids and
ethanol) and different GABAAR subtypes have been shown to exhibit unique pharmacological profiles.
GABAAR subunits are expressed at varying levels in different cell types throughout the brain suggests
that distinct GABAAR subtypes are regionally distributed in a manner that is specific for the neural
circuits in which they participate. Since the pathological entity of schizophrenia and related disorders in
the adult brain is ultimately characterized by deficits in neural circuitry, GABAARs are ideal therapeutic
targets because of their putative role in circuit dysfunction combined with circuit-specific expression of
subtypes exhibiting unique pharmacological properties. Given that cognitive deficits are considered to
be core features of schizophrenia and given the strong evidence implicating disturbances in GABA
signaling as contributing to these deficits, it is not surprising that the effects of GABA-modulating drugs
on clinical measures related to schizophrenia, including cognitive and positive symptoms, have been
investigated. One early study investigated bretazenil (Ro 16-6028), a short-acting partial
benzodiazepine agonist, on clinical outcome measures predictive of antipsychotic efficacy in
schizophrenic patients. Other studies have demonstrated the efficacy of diazepam and lorazepam
exacerbated working memory deficits in schizophrenic patients, while flumazenil, a GABAAR partial
inverse agonist, ameliorated working memory deficits in these patients. MK-0777, improved subject
performance in three tasks for working memory and/or cognitive control, as well as increased gamma
band power during one of these tasks. In addition to benzodiazepines, GABAARs are also sites for
endogenous neuroactive steroids such as allopregnanolone, which potentiate the response to GABA
with greater potency than benzodiazepine binding. According to a small sample size study; Sodium
Oxybate (SXB) may improve objective sleep architecture and moreover, improvement in sleep may
lead to downstream improvement in symptoms in schizophrenic patients.
REFERENCES
1. Lewis DA, Hashimoto T, Morris HM. Cell and Receptor Type-Specific Alterations in Markers of
GABA Neurotransmission in the Prefrontal Cortex of Subjects with Schizophrenia. Neurotoxicity
Research 2008; 14: 237-248.
2. Charych E, Liu F, Moss SJ, Brandon NJ. GABAA receptors and their associated proteins:
Implications in the etiology and treatment of schizophrenia and related disorders.
Neuropharmacology 2009; 57: 481495.
67
Cyclon Gene Expression in Peripheral Blood and Brain of
Patients with Schizophrenia
Rinaldo Shishkov*, T Chervenkov, A Tonchev
*University Hospital St. Marina, 1 Hr. Smirnenski Str., 9010 Varna, Bulgaria
Results of several studies in schizophrenia show link between the IL-3 coding gene and the IL-3
receptor subunits coding genes. In the context of the study on IL-3 gene activity induced by IL-3 cell
line in pro-B-cell line Akemi Hoshino and Hodaka Fujii 2008 identify directly induced by IL-3 gene
ccdc86 (coiled-coil domain containing 86) with unknown by that time function, called by them Cyclon
(cytokine induced protein with coiled-coil domain), (1). Saint Fleur t l. 2009 find that Cyclon is a
regulator of expression of CD95/Fas receptor in T-lymphocytes in vivo during activation of T-cell
receptor and by that means it participates in the phenomenon activation induced cell death (2).
Considering that signal IL-3 pathway and functional changes in immune system are connected with the
disease and the fact that until now there are no studies on Cyclon gene expression in schizophrenic
patients, we decided to investigate Cyclon gene expression in peripheral blood and brain. Contingent
and methods Cyclon in blood Cyclon mRNA expression in peripheral blood was studied by qRT-PCR in
21patients with schizophrenia. All of them are tested during relapse and a sub sample of
12 of them were retested during remission. As a control group 7 healthy people were included, who
were matched by gender and age. Cyclon in the brain Using immune-fluorescence method we tested
expression of protein product of gene Cyclon in the brain of 5 adult primates (Macaca fuscata) and post
mortem in a brain of schizophrenic patient. Results Our results show statistically significant higher
expression of gene Cyclon in peripheral blood of schizophrenic patients during relapse, compared to
remission. Expression in remission is not different than that in control group. Important finding from
brain study is that gene expression is higher in zones of neurogenesis, which is related to the
pathogenesis of schizophrenia.
References:
1. Hoshino A, Fujii H. Redundant promoter elements mediate IL-3-induced expression of a novel
cytokine-inducible gene, cyclon. FEBS Lett. 2007 Mar 6;581(5):975-80.
2. Saint Fleur S, Hoshino A, Kondo K, Egawa T, Fujii H. Regulation of Fas-mediated immune
homeostasis by an activation-induced protein, Cyclon. Blood. 2009 Aug 13;114(7):1355-65.
68
Screening for Depression and Anxiety in General Practice
in Bulgaria
Antoaneta Angelova, Md *
* Foundation Biological Psychiatry; Medical Center "st. Sofia", R.a. Lulin, Bl. 775, Sofia, Bulgaria
Depressive and anxiety disorders are more common in general practice than in general population (1).
They are widely under-diagnosed and under-treated. In Bulgaria epidemiological EPIBUL study found
that lifetime prevalence for depression is 5.6 % of general population (2). Life-time prevalence of
anxiety disorders is 11.4 (2). Prevalence of depressive and anxiety disorders is higher in general
practice than in community (3). The aim of present study is to apply PHQ2 as a quick screening tool for
depression in general practice in Bulgaria. There are lots of studies on this approach, confirming its
usefulness in general medical practice (3). Methods: We investigated 216 patients in 19 GPs practices
all over Bulgaria. 184 of them agreed to fill questionnaires. We used a general demographic
questionnaire and PHQ. The translation of PHQ was based on World Health Organisation guidelines. It
consisted of the following phases:
Initial translation by a specialist health interpreter
Modification by a panel of bilingual mental health professionals assisted by the project coordinator
Field trial by bilingual general practitioners
Further modification by bilingual panel based on comments by general practitioners
Final check and proofreading by second translator
Throughout this process it was emphasised that the language used should be simple so that it would
be comprehensible to the maximum number of people. Medical terms and less-familiar words were
avoided. We used two sets of screening questions. First PHQ2 consisted of 2 questions for lowered
mood and anhedonia respectively. Second consisted of 2 questions for panic attacks and generalized
anxiety respectively. Results: We found that almost a half of patients have depressive symptoms,
which are distributed from sub-syndrome to severe depression. We investigated people, who answered
with Yes to at least one of the two screening questions. Questions for lowered mood and anhedonia
appeared to be useful for the screening for depression in general practice (sensitivity: 0.89). As to other
two questions for panic attacks and generalized anxiety we found also high sensitivity as measured by
AUC (0.86 and 0.85 respectively). Discussion: The PHQ2 is a useful as a screening tool for depression
and anxiety disorders in general practice.
References:
1. Katon W, Schulberg H. Epidemiology of depression in primary care. Gen Hosp Psychiatry. 1992
Jul;14(4):237-47.
2. Okoliyski M, et al. 2010 (in Bulgarian)
69
Suiciadal Tendances in General Practice in Bulgaria
Petar Marinov, Md, Phd
Associated Professor, Medical University "prof. P. Stoyanov" Varna, Varna, Bulgaria
Using PHQ we found that a significant proportion of patients in general medical practice have suicidal
thoughts. As much as 16 % of the cohort (n=184) have various levels of suicidal ideation (n=29). It was
positively correlated with severity of depression, insomnia and panic attacks. About 5 % of the cohort
have moderate to severe suicidal ideation. This area of psychiatry in general practice is very important
for the assessment, treatment and prevention of suicidal behaviour.
70
HLA Subtypes in Affective Disorders in Bulgarian Population
Olya Mikova* , Milena Ivanova **, Tzvetelin Lukanov**, Antoaneta Angelova*, Petar
Marinov *, Anastassia Mihaylova **, Elissaveta Naumova **
*Foundation Biological Psychiatry, Sofia, Bulgaria
**University Hospital Alexandrovska, Sofia, Bulgaria
Genetic, endocrine, immunologic and environmental factors are involved in the pathogenesis of
psychiatric diseases. In this context, innate and adaptive immunity genes are possible biomarkers,
despite the lack of consistency in some of the results reported to date. The aim of the present study
was to investigate genetic causes underlying predisposition to bipolar and unipolar affective disorders,
focusing on HLA class I and class II antigens. Objectives: In order to investigate a possible genetic
cause underlying the clinical association between several autoimmune and inflammatory diseases
(autoimmune thyroiditis, MS, etc.) and affective disorders, we have studied HLA class I and II antigens
in patients with bipolar and unipolar affective disorders, compared with healthy controls. Results: The
following patients: 39 with major depressive disorder (MDD) and 25 with bipolar disorder (BPD) were
compared to 40 healthy age and sex matched controls from the Bulgarian population. HLA-A, -B, -
DRB1, -DQB1 typing was performed by PCR-SSP and PCR-SBT methods. For MBL2 genotyping
including 6 functionally relevant SNPs, a novel Luminex-based assay that we developed was applied.
HLA-A*33 (p=0.04) and B*07 (p=0.021) alleles were significantly increased among MDD patients, while
DRB1*14:01 (p=0.01) and DQB1*05:03 (p=0.002) were increased in BPD patients compared to healthy
controls. Comparison between both groups with affective disorders showed statistically significant
prevalence of DRB1*07:01 (p=0.031) and DQB1*0503 (p=0.031) alleles among BPD group. Despite of
the relatively small groups, the analysis of haplotypes also suggested disease predisposing patterns. In
conclusion, our preliminary data suggests predisposing association of HLA class I alleles with MDD,
while BPD is associated mainly with DRB1 and DQB1 alleles. Haplotype analysis would contribute to
clarify further the role of adaptive and innate immunity genes in the pathogenesis of affective disorders.
This study was supported by EU Grant - FP7-Health-2007 Project 222963, MOODINFLAME
71
Therapeutic Drug Monitoring and Phenotyping in Psychiatry
Tuncel zden
72
73
74
75
76
77
78
79
80
81
82
83
84
85
86
87
88
89
90
91
92
93
94
95
96
97
98
99
100
101
102
103
104
105
106
107
108
109
110
The Use of TDM and Phenotyping in Psychiatric Illnesses
Prof. Dr. Nevzat Tarhan, MD Y. Do Dr. Gkben Hzl
USKDAR University NPISTANBUL Hospital, stanbul
The response of individual patients to the same drug given in the same dose varies considerably. Many
patients will experience the desired drug effect, others may experience no effects, yet others may
suffer from well-known adverse drug reactions, and very rarely individual patients will die from severe
side effects.
TDM is based on the principle that for some drugs there is a close relationship between the plasma
level of the drug and its clinical effect. If such a relationship does not exit TDM is of little value. Like any
diagnostic test, the measurement of plasma level is justified only when the information provided is of
potential therapeutic benefit. The clinical value of plasma level monitoring depends on how precisely
the treatment outcome can be defined.
TDM will be useful if the following criteria are met:
1. the drug in question has a narrow therapeutic range,
2. a direct relationship exists between the drug or drug metabolite levels in plasma and the
pharmacological or toxic effects,
3. the therapeutic effect can not be readily assessed by the clinical observation,
4. large individual variability in steady state plasma concentration exits at any given dose and
5. appropriate analytic techniques are available to determine the drug and metabolite levels.
TDM is unnecessary when
1. Clinical outcome is unrelated either to dose or to plasma concentration
2. dosage need not be individualized
3. the pharmacological effects can be clinically quantified
4. when concentration effect relationship remains unestablished,
5. drugs with wide therapeutic range such as beta blockers and calcium channel blockers
TDM is a method used to provide optimal pharmaceutical therapy. Knowing the plasma concentration
of psychoactive medication helps monitor the side effects of the medication in order to prevent toxicity
and increase the responsivenes of the medication. In therapeutic drug monitoring, psychoactive drugs
are divided into 4 groups:
1. The most recommended group consists of: lithium and carbamazepine. Monitoring the levels
of valproic acid is important in order to prevent toxicity from occuring.
2. Clozapine and similar medications are considered one group of medication whose side effects
shoule be monitored.
3. On the other hand, medications that should be closely observed but have an elapsed response
rate are included into the group monitored for response-time.
4. This group of medication is often monitored in order to place a pre-diagnosis for treatment-
resistant patients who may have genetic polymorphism and choose the correct medication.
A genetic profile (DNA tests) can be considered as a reflection of the human genome project into
psychiatry. In this project, 30,000 genes have been identified and 3 times that many proteins are being
identified. The cytochrome gene and the isoform proteins make-up the basic pharmacokinetic
foundation of psychiatric medications. In order to predict the possibility for the patient to experience
toxicity, monitoring when the medication effect increases and decreases is very imperative. In order to
produce important clinical results, it is important to know about gene polymorphisms. With the
combination of the analysis of DNA series for psychiatry and therapeutic drug montoring, clinical
pharmacogenetics has started a new period in which patients are provided with a personalized
pharmaceutical treatment.
Phenotyping
The rapid advances in pharmacogenetic knowledge and genotyping methodology however provide a
basis and challenge for clinical studies on the role and usefulness of pharmacogenetic testing in clinical
psychiatry. Using modern DNA amplification techniques, genotyping allows characterization of many
significant CYP genes with only a single venous blood sample. However, genotyping is only clinically
relevant to the degree with which it predicts phenotype. Consequently, the optimal method of
111
describing real-time enzyme activity is phenotyping, where metabolism of a carefully selected probe
compound is used to estimate the activity of one or more of the enzymes involved in its metabolism.
Although it is often more cumbersome than genotyping, phenotyping provides the most clinically
relevant information because it is a reflection of the combined effects of genetic, environmental, and
endogenous factors on CYP activity. Several potential phenotyping probes have been proposed for
most CYP enzymes, each with unique advantages and disadvantages.
The pharmacogenetic tools available are phenotyping, i.e. measurement of a specific enzyme activity
by use of a probe drug, and genotyping, analysis of functionally important mutations in the gene coding
for the specific enzyme.
Numerous CYP enzymes involved in the metabolic processing of psychotropic medications have
genetic variants or polymorphisms. These polymorphisms result in a wide range of metabolic capacity
across patients, and can substantially alter the metabolism of specific drugs in certain patients. A
genetically poor metabolizer who was not exposed to a CYP inhibitor would have the same phenotype
for metabolism as that of a regular metabolizer who was taking a CYP inhibitor. Interestingly, in a poor
metabolizer, the effects of a CYP inhibitor would be less important as the enzyme is already deficient.
Clinical studies have shown that in patients with CYP 2D6 polymorphism, treatment with the atypical
antipsychotic risperidone is associated with an 3-fold risk of adverse effects because of the inability to
metabolize the drug adequately in poor metabolizers.
Alternatively, a genetically super metabolizer (due to gene amplification) who was not exposed to a
CYP inducer would exhibit the same phenotype as a regular metabolizer administered a CYP inducer;
thus, administration of a CYP inducer to a genetically extensive metabolizer would result in particularly
rapid removal of substrate drugs from the system. For many of the phenotypes (eg, poor, intermediate,
wild-type-extensive, and super metabolizer), there is a wide range of capacities due to heterozygous
alleles. For some there are commercial tests available to determine genotype.
CYP2D6 phenotyping
CYP2D6 plays a pivot role in metabolism of xenobiotics, especially psychotropic drugs. Predicting its
metabolic activity in patients may help to personalize pharmacotherapy.Eight-hour urinary ratio of
dextromethorphan/dextrorphan molar concentrations serves as a measure of CYP2D6 activity with 0.3
as a cut-off value separating poor and extensive metabolizers . Unfortunately, collecting of urine for 8
hours may be difficult in psychiatric patients. The assessment of dextromethorphan/dextrorphan molar
concentrations in serum is less used since correlation with urine dextromethorphan/dextrorphan molar
concentrations and cut-off value in serum is not well established
Previous studies showed that metoprolol can be used as the CYP2D6 probe for determining the
polymorphism of CYP2D6.
Debrisoquine hydroxylation polymorphism is by far the most thoroughly studied genetic polymorphism
of the CYP2D6 drug-metabolizing enzyme. Debrisoquine hydroxylation phenotype has been the most
used test in humans to evaluate CYP2D6 activity. Two debrisoquine hydroxylation phenotypes have
been described: poor and extensive metabolizers. A group with a very low debrisoquine metabolic ratio
within the extensive metabolizers, named ultrarapid metabolizers, has also been distinguished. This
CYP2D6 variability can be for a large part alternatively determined by genotyping, which appears to be
of clinical importance given CYP2D6 involvement in the metabolism of a large number of commonly
prescribed drugs. CYP2D6 pharmacogenetics may then become a useful tool to predict drug-related
side effects, interactions or therapeutic failures.
CYP1A2 phenotyping
Caffeine (1,3,7-trimethylxanthine [137X]) is one of the most commonly ingested compounds throughout
the world. The metabolic pathways of caffeine are complex but involve the formation of three principal
metabolites: theobromine (3,7-dimethyl xanthine [37X]), theophylline (1,3-dimethylxanthine [13X]), and
paraxanthine (1,7-dimethylxanthine [17X]). Each of these metabolites are primarily formed by
cytochrome CYP 1A2. Caffeine has become popular as a metabolic probe for CYP1A2 activity in
humans. It is one of the major P450 cytochromes in the liver and accounts for 15% of the total P450
content.
If a CYP1A2 phenotyping needed, subjects were asked to comply with a diet free of caffeine, ethanol,
and grapefruit juice/products for 48 h, and come to the hospital for an overnight stay of approximately
12 h prior to the initiation of the sample taking. After eating a standardized breakfast, subjects received
200 mg of caffeine. Immediately after caffeine administration, subjects began to collect their urine and
continued to do so over the next 8 h.
112
CYP2C9 phenotyping
Despite the few reports to the contrary, significant evidence supports the use of tolbutamide as a
selective in-vivo CYP2C9 probe. Isolated reports also support the use of the 6 h DPH/HPPH ratio, but
more clinical data are required before recommending its widespread use. Concerns over the extremely
narrow therapeutic index and possible need for steady-state sampling will have to be addressed prior
to more widely applied use of warfarin as a CYP2C9 probe. Alternately, the use of warfarin as a probe
may be limited to those requiring warfarin therapy for a medical indication. The metabolic pathways of
losartan and its metabolite need to be further elucidated prior to its use for CYP2C9 phenotyping.
CYP3A4 phenotyping
Several methods of phenotyping CYP3A activity have been proposed, and identification of the ideal
probe has been difficult. The most widely accepted and tested CYP3A probes are erythromycin and
midazolam. However, in their current form, neither phenotyping procedure is ideal.
Coctail approach
Marker or probe drugs have been widely used for phenotyping various individual cytochrome P450
(CYP) activities, and this approach has been widely used in many clinical investigations in the field of
drug metabolism and pharmacogenetics. A practical limitation of such phenotyping has been the
inability to test the activity of several enzymes simultaneously, because a separate probe drug is
generally required for each enzyme. As a result, attempts have been made to permit concurrent
administration of probes so that multiple enzymes can be tested at once. Thus the cocktail approach
was developed, involving the administration of multiple probe drugs simultaneously and the mea
surement of plasma kinetics and/or urinary excretion of unchanged parent compound and metabolites.
Genetic polymorphisms have been described for most drug-metabolizing enzymes, including CYP2C19
and CYP2D6, that give rise to distinct subgroups in the population that differ in their ability to perform
certain drug biotransformation reactions. The functional importance of genomic variability in CYP1A2,
CYP2E1, and CYP3A remains unclear, but it was found that genetic polymorphisms of CYP1A2 were
related to the inducibility of CYP1A2 in vivo.7 CYP3A accounts for up to 25% of the total CYP present
in adult human liver and is the major CYP present in the human intestine. The importance of the
CYP3A enzymes is most established with respect to the metabolism of xenobiotics and medications.
CYP2E1 has received much attention because of its ability to bioactivate a number of potentially
harmful compounds, including some toxins and carcinogens. Therefore phenotyping individuals with
respect to CYP3A, CYP1A2, CYP2C19, CYP2E1, and CYP2D6 activities is of clinical relevance.
Because the complications that should be avoided in a cocktail approach are mutual interactions
between the probe drugs, low doses need to be used. Another consideration is that several drugs and
metabolites must be analyzed in the same biologic sample, which requires an appropriate degree of
selectivity and sensitivity of the analytic methods.
113
Transcranial Magnetic Stimulation
Ouz Karamustafalolu
Professor of Psychiatry
skdar University Istanbul Turkey
Repetitive transcranial magnetic stimulation (rTMS) is an accepted treatment modality for the treatment
of depression.
During the last decade numerous studies including meta-analyses indicated the efficacy of rTMS in the
acute treatment of major depressive disorder.
After the positive results seen in depression other psychiatric disorders like OCD, schizophrenia,
PTSD, addiction, memory disorders and bipolar disorder are studied using rTMS for treatment.
Although the results dont seem to be as clear as in majr depression there is a place further
evaluations.
The current status of rTMS seems to be rewarding for future studies. Deep TMS, long term efficacy,
target area of application and the role of concurrent medication are the main questions needed be
answered.
114
Safety of High-Frequency Transcranial Magnetic Stimulation
Ouz Tan, M.D.
Psychiatrist
skdar University
Repetitive transcranial magnetic stimulation (rTMS) is emerging as a new therapeutic tool in psychiatry.
Its efficacy especially in depressive disorder has been demonstrated by clinical studies. rTMS sessions
have been conducted in thousands of healthy subjects or patients with various neurological or
psychiatric diseases, allowing a reliable assessment of risks associated with this technique. Adverse
events attributed to rTMS are generally mild and occurred in a small proportion of subjects, the most
common one being headache. The most serious complication is the occurrence of seizures that have
been extremely rare and usually observed in patients under treatment with medications which
potentially lower the seizure threshold. In most reported seizures, the stimulation parameters have not
followed the previously published recommendations. rTMS is generally a well-tolerated and safe
method of treatment.
115
Efficacy of High Frequency (25 Hz) Repetitive Transcranial
Magnetic Stimulation in Treatment-Resistant Depression:
Overview of 419 Cases
F. Gkben Hzl Sayar
Department of Psychiatry, NPISTANBUL Neuropsychiatry Hospital, Uskudar University, Istanbul,
Turkey
The clinical applications of rTMS have rapidly expanded over the last few years. This technique was
initially proposed and has been most thoroughly studied for the treatment of depression. In 2008, the
US Food and Drug Administration approved TMS as an alternative form of treatment for depression
resistant to other treatments. While TMS has its own limitations, it can be quite effective for those of
you who don't tolerate treatment with medications and aren't willing to consider electroconvulsive
therapy.
I will summarize the data of a total of 419 patients who underwent rTMS treatment with a diagnosis of
treatment resistant depression to examine the effectiveness and safety issues of rTMS tratment. A total
of 636 depressed patients underwent rTMS treatment during a 3-year period. Of these 636 patients,
430 signed an informed consent to be enrolled in the study and received the first rTMS session,
constituting the intention-to-treat population. Of these 430 patients, 11 withdrew from the study.
Reasons for withdrawal were reconsideration of the risks and benefits of the study and/or unwillingness
to come to the hospital repeatedly on a daily basis.
Study Design
Patients who met the Structured Clinical Interview for DSM-IV criteria for depression were eligible for
the study. Treatment-resistant depression was described as a failure to respond adequately to two
successive courses of monotherapy with pharmacologically different antidepressants given in adequate
doses for 4-6 weeks. Subjects with minor neurological abnormalities (eg, essential tremor, chronic
headaches, gait ataxia, prior head injury) underwent neuroimaging unless they had prior neuroimaging
at the onset of the neurological dysfunction that showed no gross abnormality. Subjects were also
screened with a complete blood count, thyroid function tests, and electrolytes within 3 months of the
treatments. Concomitant medication for depression was authorized, provided the dose administered
had been stable for at least 1 month before enrollment and remained stable throughout the study.
Exclusion criteria included evidence of dementia on neuropsychological testing, or meeting the
Structured Clinical Interview for DSM-IV criteria for organic brain syndrome, organic mood disorder,
substance dependence within the last 6 months, a diagnosis of a significant central neurological
disorders including brain mass, epileptic seizures, stroke, transient ischemic attack within 2 years,
cerebral aneurysm, dementia, Parkinsons disease, Huntingtons chorea, multiple sclerosis, or other
major central nervous system dysfunction. Additional exclusion criteria included the presence of
cardiac pacemakers, cochlear implants, or other intracranial implants with the exception of dental
fillings, and the presence of psychiatric symptoms of significant severity (e.g. refusal of food and
medication or the presence of psychosis) that would prevent a 3-week trial of rTMS being tolerated.
Subjects with acute, unstable medical conditions that required stabilization (e.g. uncontrolled
hypertension) prior to treatment were also excluded. Pregnancy was not accepted as exclusion criteria
in our study group.
Stimulation
TMS was applied using the Magstim Super Rapid stimulator (Magstim Company, Whitland, UK) with
figure-of-eight shaped coil in all patients in an open label manner. The rTMS intensity was set at 100%
of the motor threshold which was determined by visual inspection. Stimulations were given to the left
prefrontal cortex, deemed to be located 5 cm forward from the cortical motor area of the abductor
pollicis brevis of which the motor threshold was determined. The treatment schedule was six days in a
week, from Monday to Saturday for three weeks. 25 Hz stimulation with the duration of 2 seconds was
delivered 20 times with 30-second intervals. A full course comprised 1000 magnetic pulses.
Outcome Measures
Depressive symptom changes were measured by validated Hamilton Depression Rating Scale. The
HAMD-17 scores were obtained at baseline and 1-week after completing the course of rTMS.
Secondary outcome parameters included response and remission rates. Response was defined as a
116
decrease in the HAMD-17 total score of at least 50%. Patients with HAMD-17 scores of less than 8
were considered to be in remission. Efficacy parameters were assessed by an independent rater who
was blind to the patient treatment status.
RESULTS
Prospectively planned data collection of 419 patients who completed the rTMS protocol was
retrospectively evaluated. The study population consisted of 271 females and 148 males, with an
average of 38.1 13,5 years (range, 15-83 years).
The mean HAMD score for the study group decreased from 22.65.9 to 10.55.8 (p<0.001). After a 18-
day treatment period, 268 out of our 419 patients (64%) demonstrated significant mood improvements,
as indexed by a reduction of more than 50% on the HAMD score. Besides, 140 patients (33.4%)
attained remission (HAMD score <8); and 11 patients achieved a partial response.
In our study group, 7 out of our 419 patients were pregnant. Of these 7 patients, 5 demonstrated
significant mood improvements and were classified as responders while 2 patients reached remission
status, with HAMD-17 scores less than 8, after rTMS. The newborns revealed no abnormalities.
Complete physical and neurologic examination, screening tests for phenylketonuria and
hypothyroidism, and hearing assessment was normal. None had congenital hip dysplasia, congenital
cardiac disease, cleft lip, or cleft palate. There were no gastrointestinal, pulmonary, or muscular
abnormalities.
The magnetic stimulation was generally well tolerated. Patients had previously been informed about
contractions of facial muscles. One patient presented tonic-clonic epileptic seizure lasting for 2
minutes developed immediately after the 4
th
session receiving 1000 pulses. Seizure was observed
immediately at the end of the rTMS session. It was a generalized tonic clonic seizure, lasted
approximately 30 seconds. After a tonic phase with contraction of limbs and loss of consciousness for
about 10 seconds, clonic contractions observed. She did not report an aura. No sphinchter
incontinence was observed. Afterwards she complained of headache and feeling tired. Her confusional
state subsided slowly after 30 minutes of the event. Regarding the differential diagnosis of seizures and
convulsive syncope, the case we observed was obviously a seizure not a convulsive syncope, since
the patient 1) was not upright at the onset of the attack, 2) did not report dizziness, light-headedness,
nausea, palpitation, weakness, visual impairment or feeling cold, 3) did not show prodromal
diaphoresis nor pallor (cyanosis was observed quite the contrary), 4) was aware of the sensation
experienced prior to loss of consciousness (if there is no preceding subjective sensation, the episode is
unlikely to be a syncopal event). Furthermore, in convulsive syncope patients experience myoclonic
jerks that are usually multifocal and nonrhythmic or multifocal and superimposed on generalized
myoclonus following loss of tonus (a relaxed phase), unlike generalized tonic clonic seizures during
which standart progression of tonic to clonic activity is observed which was the case in our patient.
Convulsive syncope usually lasts shorter than 30 seconds, whereas generalized tonic clonic seizures
last 30 seconds to 2 minutes in most cases just as in the present patient. Finally, our patient had no
history of cardiovascular disorder, syncope or substance use. Other side effects such as cognitive
difficulties, headache, tinnitus, dizziness or nausea which observed during rTMS studies in the
literature were not examined in our study group.
The main outcome of the study is that a significant reduction of baseline depression scores was
observed, indicating improvement of depressive symptoms. No significant adverse effects were
monitored in patients receiving treatment. The results of this study are in agreement with the findings of
previous studies suggesting that daily high frequency rTMS is well tolerated and effective in patients
with treatment-resistant depression.
In our study group, 268 out of our 419 patients (64%) demonstrated significant mood improvements
and classified as responders while 140 patients reached remission status. The response rates obtained
by other studies in the literature vary in great degree. Response rate of 30% was reported by Isenberg
et al. who gave 4 weeks of high frequency rTMS; and Avery et al. found a 32% response rate when
rTMS was administered for 15 sessions. It is not clear why the response rate in this trial was
significantly greater than in previous studies of rTMS, but combining the two treatment types
(pharmacologic and TMS) could potentially enhance the response. Furthermore, the greater benefits
seen with rTMS in this study may be due to the high frequency stimulation of 25 Hz. These issues will
only be resolved with a large double-blind randomized placebo controlled trial.
Clinical trials have confirmed rTMS to be without significant adverse effects in the treatment of
depression. In most cases these have been pain or discomfort during stimulation (owing to stimulation
of scalp nerves and muscles) and headache, often after rTMS. Mosimann et al. found rTMS to be a
117
safe treatment with none of the patients withdrawing from the study or reporting serious adverse
effects.
28
This is similar to the study by Su et al. where 3 out of 30 patients dropped out of the treatment
because of pain or worsening of clinical symptoms.
29
The magnetic stimulation was generally well
tolerated in our study group. Cognitive difficulties, headache, tinnitus, dizziness or nausea were not
reported in the study population. The most serious side effect of high-frequency rTMS is the induction
of a seizure.
A 38-year old female patient presented tonic-clonic epileptic seizure lasting for 2 minutes developed
immediately after the 4
th
session receiving 1000 pulses. rTMS treatment was stopped immediately.
Electroencephalogram assessed before treatment had showed no abnormality for this patient.
Induction of seizures is the most severe acute adverse effect for rTMS. Several cases of accidental
seizures induced by rTMS have been reported to date, most in the early days prior to the definition of
safety limits. Figiel et al. reported a case of a patient with major depression who developed left focal
motor seizures that followed at least 6 h after the end of stimulation (100% of MT, 10 Hz, and train
duration of 5 s).
36
Nowak et al. reported a case of a generalized tonic clonic seizure in a patient with
tinnitus receiving rTMS with parameters of 90% of MT, 1 Hz and 580 pulses.
37
Tharayil et al. reported
a generalized tonic clonic seizure in a patient with bipolar depression using single-pulse TMS during
motor threshold (MT) assessment.
38
Rosa et al. reported a generalized tonic clonic seizure in a patient
with chronic pain using parameters of 100% of MT, 10 Hz and train duration of 10 s.
39
Prikryl and
Kucerova reported a case of generalized tonic clonic seizure during rTMS treatment for major
depression.
40
The parameters of stimulation were 110% of MT using 15 Hz and train duration of 10s.
Considering the large number of subjects and patients who have undergone rTMS studies since and
the small number of seizures, we can assert that the risk of rTMS to induce seizures is certainly very
low. Spread of excitation with increasing stimulation frequency and intensity presumably indicates
increased cortical excitability and has been observed preceding TMS-induced seizures. The pattern of
muscle activation which follows their somatotopic representation and the delay in MEP latencies of
proximal muscles compared to when stimulated over their optimal position has been argued to point to
intra-cortical propagation. The precise mechanism is unknown.
The proper treatment of mood disorders occurring during pregnancy is a major therapeutic problem
since no antidepressant medications have been established as safe for the developing fetus. Apart
from antidepressants, the most commonly used biological therapeutic method is ECT
(electroconvulsive therapy). We believe that similar efficacy can be achieved using rTMS as a safer
option with substantially less side effects. In our study group, the magnetic stimulation was well
tolerated, no seizure or other significant side effect occurred. All the pregnant participants gave birth to
healthy babies and the newborns revealed no abnormalities. Up to now, we have not found that rTMS
can be harmful to fetuses or babies. The rTMS may be a good choice for treating pregnant women and
breast-feeding mothers with depression.
Compared to previous TMS studies, the present study population is larger. Furthermore, the instrument
(Hamilton Depression Rating Scale) used for outcome measure is specific for depression. Higher
responsiveness of specific rather than generic instruments should render the results of this study
usable for comparison with studies of other treatment modalities for treatment-resistant depression.
The main limitation of this study is the non-controlled design which likely restricted the statistical power.
Since the study lacks a control group we cannot exclude the possibility of a placebo effect. Further
studies are required to define the optimal parameters of stimulation (site, intensity, frequency, etc.), to
clarify which patient and treatment characteristics might lead to greater antidepressant effects with
rTMS, and to identify potential mechanisms by which rTMS produces antidepressant effects.
As the last words, high frequency (25Hz) repetitive transcranial magnetic stimulation was well tolerated
and found to be statistically and clinically effective in patients with treatment-resistant depression.
118
Multidisciplinary Approach to Alzheimers Disease
Bilgen Taneli
Uluda University, Medical Faculty, Department of Psychiatry, Prof. Emeritus.
Turkish Society of Biological Psychiatry, President.
Alzheimers Disease (AD) is a worldwide, increasingly prevalent, slowly progressive, irreversible,
neurodegenerative disease of the brain. AD asymptomatically progresses for decades, and is a
complex genetic disorder of non-Mendelian nature. It is generally observed in populations over 65
years of age, and becomes increasingly prevalent with age. AD is a multi-faceted, biopsychosocial
phenomenon, with dire consequences to the patient, patients family, and caregivers. Therefore, a
multidisciplinary team must manage treatment and caregiving in AD.
The AD treatment and caregiving team includes a multitude of professional and non-professional
individuals. These are, primary-care physicians (generalists or family doctors); psychiatrists (geriatric
psychiatrists), neurologists (geriatric neurologists), internists (specialist in geriatrics), or other
specialists as needed experienced with geriatric populations; as well as clinical pharmacologists,
clinical psychologists, neuropsychologists, geriatric clinical nurses, gerontologists, healthcare aides,
nutritionists, social workers, occupational therapists, physical therapists, architects specialized in
environment and behavior, and other professionals as suited (for instance lawyers). Additionally, pre-
clinical physicians, and the laboratory team must be mentioned as part of the AD Team.
The team may restructure as the patients needs vary with the stage of the disease. An effective
rapport is desired to best assist the patient.
119
Geriatric Assessment in Family Practice
Prof. Dr. Hakan Yaman
Akdeniz University, Faculty of Medicine, Department of Family Medcine, Antalya, Trkiye
In most countries the demographic change is resulting in the increase of the elderly population. This
change effect our societal life and also influences the health care system. Besides health problems, the
steady increase of non-communicable disease and the compression of morbidity results in steady
occupation of the health sytem. The presence of comorbidity and polypharmacy is an other problem
area. Functional decline, the geriatric gigants (i.e. urinary incontinence, falls, dementia, depression) are
other conditions to consider.
Health care service and elderly care service is provided by different institutions. The coordination and
integration these institutions is needed and a case manager be involved. Gerontologists might be the
best service provider. Geriatric assessment in family practice has an important role in the evaluation of
the present condition and status of the elderly person. This kind of assesment could performed by a
family doctor and his/ her team or by a multi-discplinary team in a geriatric center/hospital. We
recommend the WHO Elderly-Friendly Primary Health Care Toolkit for the evaluation of health care
needs of elderly people in the community; for patients who lack either empowerment to visit the family
health center or for people who have a disability and are not able to leave their home.
This toolkit has been developed by a panel of experts in geriatrics and elderly care and endorsed by
WHO. It covers to main areas: 1. Health promotion, 2. Screening. The health promotion part is an
important prevantatif medical service, which should be provided in primary health care setting. The
second part is more a periodic health examination of elderly patients concerning certain frequently
encountered health problems and medical conditions. It covers four geriatric giants (i.e. dementia,
depression, falls and urinary incontinence) and two chronic disease (i.e. diabetes mellitus and
hypertension). In a step by step way the patients goes through all parts of the assessment. After
receiving a consent from the patient and personal information have been recorded, the first step will
cover a ten minute screening for certain conditions (i.e. memory, mood, mobility, falls, urinary
incontinence, nutrition, hearing, vision). The second would be to evaluate positive findings of the first
step. Further scales are recommended and an approach with an algorithma could followed to conclude
the management of certain conditions.
The proposed comprehensive geriatric assessment toolkit by WHO is an easy applicable tool in
primary health care. With this instrument the continuity of care of other non-communicable could be
easily applied. This instrument itself could create an interface between primary care and secondary
care.
The WHO Elderly-Friendly Primary Health Care Toolkit should be implemented in turkish primary
health care system. With this concenpt the care of other chronic cnditions could be continued. To
support this project interprofessional oriented models of the care chronic diseases needs to be
developed. A further step would be the integration of health and eldelry care institutions. This
implementation should be fostered by positive motivation and incentives.
120
Geriatric Psychiatry in Turkey
Engin Eker, MD,
Emeratus Professor in Istanbul University,
Cerrahpasa Medical School, Department of Geriatric Psychiatry
It was thought that in Turkey a young population dominated untill recently. Researchers held point out
that Turkey is making a transition to a new demographic structure. It is foreseen that in near future the
total fertility rate which is currently 2.23 will drop to replacement level,and as a result, the number of
children and the young population will decrease over time and the share of the elderly population within
the overall population will increase However, 7 percent of the population was older than 65 in 2009,
approximately 4,5 million people. The percentage of the elderly is expected to double by 2020. Often
more visible in developed countries, ageing is an issue that needs to be appraised with much
significance also in developing countries just like Turkey Along with this expectation, geriatric
psychiatry is a rapidly developing area in Turkey perspectively.
In fact there is growing interest to the psychiatric problems of the elderly in the medical education and
the society in Turkey.But the stigma concerning the elderly population is continuing. On the other
hand,the effort is continuing on geriatric psychiatry to become a subspeciality in our country.In this
presention , the importance of geriatric psychiatry in Turkey as a developing country will be mentioned.
121
What Should Turkeys Gerontology Agenda Include
Through 2023
Dr. smail Tufan, Ph.D., Gerontology Department Head,
School of Human Sciences, Akdeniz University
What should Turkeys Gerontology Agenda include through 2023 in view of the results of the 12-year
all-encompassing research on the Turkish Gerontology Atlas conducted to explore the situation of the
aging population?
The increase in human life span will lead to significant changes for the Turkish population in the future.
These changes will in turn trigger a marked transformation in many aspects of the daily lives of
individuals. Sociodemographic changes to result from an increased life span will change the Turkish
communitys expectations from the elderly. There is a requirement for an early initiative to improve the
circumstances affecting the elderly with a view to preclude any misconception interpreting the old age
group of the population as an economic and moral burden on society. Turkeys Gerontology Agenda
attempts to focus expert knowledge and experience on the gerontologic platform to provide viable
answers to challenges associated with demographic developments affecting the outlook of the Turkish
population, thereby recommending common feasible solutions for problems and opportunities created
by and liable to emanate from the aging of the population.
In all dimensions of the living conditions model, 6 individuals in 10 perceive the elderly positively in
assessing their self-sufficiency in their daily lives. This indicates that the perception of aged adults is
positive among experts. However, findings based on empirical data indicate that a highly favourable
assessment of the elderly is not logical. This points at the acute requirement in Turkey for gerontologic
data to be transferred to experts.
122
Falls and Other Accidents in the Household:
The Nazilli Experiment
Sultan Kl, M.A., Gerontologist
This study will attempt to draw results from the falls of older adults in the Nazilli households. The
increase in the number of the elderly due to an increasing life span will obviously result in a growing
number of individuals with a higher risk of involvement in an accident, namely a fall. Measures should
be taken against both the individual and the societal adverse consequences of these accidents. Falls
result in injuries, loss of confidence and decreasing self-control. Fear of fall restrains bodily activity and
thus adversely affects quality of life. The growing number of individuals likely to experience a fall in
Turkey where 30 aged individuals in 100 are physically handicapped, coupled with an increase in the
number of particularly the elderly over 80, create a highly difficult situation when viewed within the
context of accidents involving falls. In this study, the role of age in accidents involving falls has been
reviewed from the viewpoints of bodily characteristics, walking difficulties, body balance problems,
impact of the residential environment, high blood pressure, influence of medication, role of the eyesight
and hearing abilities, fear of fall, movement constraints, isolation, impact on life satisfaction. When fear
of fall which is assessed to be higher among the elderly is evaluated within the context of demographic
changes, the eventual existence of a growing group of inactive aged people which may be forced to
secluded lives in their homes is a challenge deserving expert consideration.
123
Pharmacokinetic and Pharmacodynamic Aspects of Pediatric
Psychopharmacology
Yeim Taneli
Uludag University School of Medicine, Dept. of Child and Adolescent Psychiatry, Bursa, Turkey
As a childs physiology rapidly changes with ongoing development, pharmacokinetic and
pharmacodynamic changes follow. These changes will have to be taken into account during (psycho-)
pharmacotherapy. A child may encounter pharmacotherapeutics during pregnancy when the child or
the mother is the target of therapy; later via lactation during the mothers pharmacotherapy or
afterwards when the child itself is the subject of treatment.
The relationship between the applied dose of a drug and its observed effect depends on
pharmacokinetic (dose-concentration) and pharmacodynamic (concentration-effect) mechanisms. With
onset of puberty, boys and girls start to differ in pharmacokinetic properties due to different body fat
composition, muscle mass and hormonal cycles. Children also differ from adults in terms of
pharmacodynamic properties, due to ongoing development of neurotransmitter systems and
synaptogenesis. Pharmacokinetic factors are what the body does with the drug and can be
summarized as the absorption, distribution, metabolism and elimination (ADME) of a drug. The
properties of all four steps are subject to change with intrinsic or extrinsic influence. Bioavailability,
elimination halftime, steady state are further concepts of pharmacokinetics. Pharmacodynamic factors,
what the drug does to the body, may show higher individual variation than pharmacokinetics. The
dose needed for a certain effect varies from patient to patient; on the other hand patients with similar
serum concentration of a drug may differ in terms of pharmacological effect. In addition, a person may
differ in response rate during different stages of therapy. Drugs have desired and unwanted effects,
which both have to be followed during the individual course of pharmacotherapy. But there are also
placebo effects and drug interactions to be considered in certain situations. Therapeutic drug
monitoring, via drug concentration in body fluids, may assist in therapeutic decisions.
In pediatric pharmacotherapy, however, the real dose depends on the pharmaceutic formula and how
the drug is applied to the child by its parents. For better compliance, and as a basic right, the pediatric
patient should in an age and developmentally appropriate way always be informed about therapeutic
plans and be given the possibility to join in therapeutic decisions. For example the child could choose
between tablets and solutions, could offer which arm to apply an i.v. medication or ask for a specific
pen color to mark on his/her arm the date and time of i.v. infusion start. Informing patients and parents
about desired drug effects and side effects should always comprise main toxicological aspects, as
children and adolescents may intentionally overdose with suicidal aim. In addition, the pediatric patient
or his/her siblings may as well accidentally overdose
The success of any pediatric pharmacotherapy is limited (in addition to the dose prescriped, the dose
applied) by the dose kept inside (not vomited, spitted, nasogastric / i.v. line not torn out, etc.) by the
child, and therefore largely depends on good patient-doctor rapport.
124
Pharmacogenetics in the Pervasive Developmental Disorders
Tolga Taneli, M.D.
UMDNJ-New Jersey Medical School, Department of Psychiatry,
Division of Child & Adolescent Psychiatry
Pharmacogenetics in psychiatry is a nascent science that has yet to influence broad psychiatric
practice, despite growing evidence and reduced cost of study. An unlikely source of inspiration for a
conceptual framework is the expert update on HIV-1 drug resistance mutations, (1) a comprehensive
document of known HIV-1 gene mutations associated with clinical drug resistance published by the
International Antiviral Society-USA (www.iasusa.org.) In brief, four genes significant to drug resistance
in HIV have been fully decoded: Reverse transcriptase, protease, the envelope gene and integrase.
The IAS-USA list identifies the gene positions and amino acid substitutions (compared with wild type)
that confer resistance to specific drugs. For example, if wild type lysine at codon position 65 of the
reverse transcriptase gene is substituted for arginine (i.e. K65R), this confers resistance to the reverse
transcriptase inhibitor tenofovir.
McGough and colleagues illustrate the possibilities of pharmacogenetics in ADHD with their 2006
report (2) on determinants of phenotype, response, and side effects associated with methylphenidate
treatment. For example the 4-repeat variant of the dopamine receptor (DRD4) predicted both picking
and dose-dependent withdrawal.
Synaptosomal-associated protein 25 (SNAP25) is a neuron-specific protein implicated in exocytotic
catecholamine release. There is a small but significant increased ADHD risk associated with two
SNAP25 single nucleotide polymorphisms (SNPs; T1069C and T1065G) (3). Patients homozygous for
the T allele at codon 1065 have improved dose responses compared with the less common G allele,
whereas patients with the T allele of T1069C do worse with methylphenidate. Furthermore, the G allele
at T1065G carries two to three times the risk of irritability and sleep problems than the more common T
variant. Likewise, patients with the C allele at 1069 are two to four times more likely to develop tics and
other abnormal movements.
Compared with ADHD, autism is at a disadvantage for scrutiny, mostly due to a more heterogenous
phenotype that includes mental retardation, seizures, and in some instances dyspmorphism. As many
as 35% of boys with Fragile X Syndrome (FXS) will also meet criteria for autism, however, a phenotype
analysis reveals substantial differences from autism, for example via the Social Communication
Questionnaire (SCQ) (4).
Defining the broader phenotype for autism will be essential in order to take advantage of opportunities
to better match treatment agents to patients. A rate-limiting step is the tendency of diagnostic
classification systems, including the Diagnostic and Statistical Manual of Mental Disorders (DSM), to
seek the least common denominator. Progress in pharmacogenetics would only be possible through
highly nuanced descriptions of phenomenology that are captured in clinical classification systems.
Bibliography
1. Johnson VA, Calvez V, Gunthard HF, Paredes R, Pillay D, Shafer R, et al. 2011 update of the drug
resistance mutations in HIV-1. Topics in antiviral medicine. 2011;19(4):156-64.
2. McGough J, McCracken J, Swanson J, Riddle M, Kollins S, Greenhill L, et al. Pharmacogenetics of
methylphenidate response in preschoolers with ADHD. Journal of the American Academy of Child
and Adolescent Psychiatry. 2006;45(11):1314-22.
3. Faraone SV, Perlis RH, Doyle AE, Smoller JW, Goralnick JJ, Holmgren MA, et al. Molecular
genetics of attention-deficit/hyperactivity disorder. Biological psychiatry. 2005;57(11):1313-23.
4. Hall SS, Lightbody AA, Hirt M, Rezvani A, Reiss AL. Autism in fragile X syndrome: a category
mistake? Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(9):921-33.
125
Novel Therapeutics in Autism
Tolga Taneli, M.D.
UMDNJ-New Jersey Medical School, Department of Psychiatry, Division of Child & Adolescent
Psychiatry (tanelito@umdnj.edu)
While the role of SSRIs is well established in obsessive-compulsive disorder, their efficacy in Autism
has come into question, particularly in children (1). The atypical antipsychotic medicines risperidone
and aripiprazole have received U.S. FDA approval for aggression in autism, yet their side effects,
particularly of weight gain, is often prohibitive in longterm use. Evidence exists supporting stimulants
and noradrenergic agents in co-occurring ADHD symptoms. Frequent comorbidity with epilepsy has led
to an abundance of data on the use of anti-seizure medicines, such as valproic acid.
In his 1998 article, Carlsson proposes a role for glutamate in the pathophysiology of autism (2), noting
that glutamatergic neurons originate in the amygdala and hippocampus, implicated in autism. Early
evidence exists for a number of glutamate modulators in the treatment of autism, among them: n-
acetylcysteine (3), riluzole (4), the uncompetitive NMDA antagonists amantadine (5) and memantine
(6).
Finally, Modi, et al. (7) demonstrated in prairie voles that d-cycloserine (an NMDA partial agonist that
promotes learning) enhances socially reinforced learning. This suggests that NMDA enhancement may
be useful in combination with behavioral therapies for enhancing social functioning in ASD.
Bibliography
1. Williams K, Wheeler DM, Silove N, Hazell P. Selective serotonin reuptake inhibitors (SSRIs) for
autism spectrum disorders (ASD). Cochrane Database Syst Rev. 2010(8):CD004677.
2. Carlsson ML. Hypothesis: is infantile autism a hypoglutamatergic disorder? Relevance of glutamate
- serotonin interactions for pharmacotherapy. J Neural Transm. 1998;105(4-5):525-35.
3. Hardan AY, Fung LK, Libove RA, Obukhanych TV, Nair S, Herzenberg LA, et al. A randomized
controlled pilot trial of oral N-acetylcysteine in children with autism. Biological psychiatry.
2012;71(11):956-61.
4. Wink LK, Erickson CA, Stigler KA, McDougle CJ. Riluzole in autistic disorder. Journal of child and
adolescent psychopharmacology. 2011;21(4):375-9.
5. King BH, Wright DM, Handen BL, Sikich L, Zimmerman AW, McMahon W, et al. Double-blind,
placebo-controlled study of amantadine hydrochloride in the treatment of children with autistic
disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(6):658-65.
6. Owley T, Salt J, Guter S, Grieve A, Walton L, Ayuyao N, et al. A prospective, open-label trial of
memantine in the treatment of cognitive, behavioral, and memory dysfunction in pervasive
developmental disorders. Journal of child and adolescent psychopharmacology. 2006;16(5):517-24.
7. Modi ME, Young LJ. D-cycloserine facilitates socially reinforced learning in an animal model
relevant to autism spectrum disorders. Biological psychiatry. 2011;70(3):298-304.
126
127
ORAL PRESENTATIONS
128
OP 1
Low Striatal Dopamine and Comorbid Substance Abuse in
Schizophrenia
A.George Awad*, Lakshmi Voruganti
Professor, Emeritus, University Of Toronto And The Institute Of Medical Science, toronto, Ontario,
Canada*, Department Of Psychiatry, Oakville General Hospital, Oakville, Ontario, Canada
One of the prominent hypothesis that explain the high comorbid substance abuse in schizophrenia has
been the self medication hypothesis. According to such hypothesis, persons with schizophrenia take
to drug abuse as a direct consequence of dealing with aspects of their illness experience or to alleviate
medication side effects notably dysphoric states. In our previous studies we demonstrated the high
association of drug abuse with the unpleasant dysphoric reactions. In subsequent neuroimaging
dopamine depletion SPECT studies, we reported that dysphoric responses to antipsychotics are
associated with consistent low striatal dopamine binding ratios. More recently experimental evidence
has indicated that low striatal dopamine binding ratios are a contributor to cocaine use in rhesus
monkey, as well enhancing impulsivity. Such new data for the first time provides a possible link
between our data of low striatal dopamine, dysphoria and comorbid substance abuse. Such new data
revives interest in the old self-medication hypothesis and likely explain in part why some persons with
schizophrenia take to drug abuse: only those who develop dysphoria and have low striatal dopamine.
This presentation will review not only the new data but will also deal with the implications of such
information.
129
OP 2
Is it Time to Recognize Co-morbid Substance Abuse in
Schizophrenia as New Dimension and Indication for
Antipsychotic Drug Development?
A. George Awad*, Lakshmi Voruganti
Professor, Emeritus, University Of Toronto And The Institute Of Medical Science, toronto, Ontario,
Canada* department Of Psychiatry, Oakville General Hospital, Oakville, Ontario, Canada
Background: Comorbid drug abuse in schizophrenia has been estimated as ranging between 10% -
70% and can have significant impact on the course of the illness and its response to treatment. Most
prominent among the explanation given has been the self medication hypothesis which eventually
proved based on our research as well as others to be inadequate to explain the total and varied picture
of comorbid substance abuse. Although it is accepted that substance abuse is likely multifactorial in its
genesis, the most compelling recent information has been the elucidation of the neurobiological
pathways implicated in the development and maintenance of comorbid addictive states in
schizophrenia. The new neurobiological information raises the notion of whether comorbid addictive
states can be related to the disease itself. Both drug abuse and schizophrenia share a common
neurobiological circuit that involves dopamine and which mediate, rewards and reinforcement
behaviour. Hyperdopaminergic states as proposed in schizophrenia can disrupt the adaptive
mechanism of the dopamine neurons in response to novel rewards. Historically persons with
schizophrenia and comorbid substance abuse has been treated with antipsychotics, yet recent data
also raises the concern about whether first generation antipsychotics in long term use can conversely
lead to enhancement of the abused substances reinforcing properties. The recent demonstration that
Clozapine can provide more benefits in the treatment of comorbid substance abuse, raises the
question of whether there exists a differential role of antipsychotics not only between first and second
generation but also between second generation antipsychotics themselves.
Conclusion: Even though the state of knowledge is not yet conclusive we are raising the question
supported by current evidence, of whether comorbid substance abuse needs to be recognized as a
dimension and new a indication for antipsychotics drug development. It is our hope that the recognition
of comorbid substance abuse as a new indication for antipsychotic drug development or add on
medications can accelerate clinical research in this area which is lagging behind the significant basic
science developments. (Awad AG, Journal of psychopharmacology in press)
130
OP 3
A Survey on Pain Assessment for Cancer Patients in Shaheed Ghazi
Hospital- Iran, Tabriz Hematology & Oncology Research Center-2010
Herizchi.S. Assistant Professor of Psychiatry
Ershadmanesh.M. GP of Social Security Found
Mousavi. S.M. Assistant Professor of Social Medicine.
Asvadi.I. Professor of Hematology & Oncology.
Somi .M. Professor of Internal Medicine
Golchin.M. Educational Nurse of Hematology & Oncology Research Center
Introduction:
Cancer is a worldwide problem these days. Also it is the second reason of mortality in the west north
regions of Iran. Pain is one of the most important problems in patients with cancer. Patients with all
stages and types of cancer and underling different methods of treatment, suffer from pain. Pain affects
the patients` Quality Of Life strongly and Pain relieving is a major part of the palliative care medicine.
Material and Methods
101 patients with different cancers in the oncology ward of Shaheed Ghazi hospital in Iran, Tabriz were
studied about their pain severity and its agents and the ways that decrease it after a written consent.
Results:
The pain was sever and intolerable in 55% of patients. Near 41% of the patients suffered from
moderate pain. There was not any significant relationship within severity of pain and sex or type of
cancer. The most usual drug for pain relief was Petedin. Other analgesic drugs were Methadone,
Morphine, Acetaminophen and Ibuprofen.
Conclusion:
Many pain relief drugs are used for cancer patients; however pain is an important problem that should
be more attention to it in therapy plans.
Introduction:
According several reference, pain is an inconvenience feeling and experience probably refers to some
damages in tissues or stimulations in pain sensory terminals. In cancer patients Pain is one of the
most important problems.
Pain may be caused with several agents, for example, poor circulation in blood and lymph,
inflammation, bone fractures due to metastasis, infections, pressure on nerves by tumor, chemotherapy
side effect and psychological problems.
However the pain perception in cancer patients depends in some factors like the type and stage of
cancer and tolerance in patients.
Cancer is a worldwide problem these days. Also it is the second reason of mortality in the west north
regions of Iran. Pain is one of the most important problems in patients with cancer. Patients with all
stages and types of cancer and underling different methods of treatment, suffer from pain. Pain affects
the patients` Quality Of Life strongly and Pain relieving is a major part of the palliative care medicine.
Perfect understanding pain and the patients experiences is needed for controlling it. The incidence of
pain has been studied in different researches. The results were different in the range of 30 to 90
percent in end stage cancer patients. The areas of pain were also different. In one research 08 - 08
percent of patients with bone metastases were suffering pain; 80% of patients were complaining pain in
2 different areas and 30% of them had pain in 3 areas of body. 08 % of patients with breast cancer had
pain in several sites without any relationship with injured part (2). A review article believed 24- 60
percent of patients in treatment period and 00 - 06 percent of patients in sever progressing period
have pain(3). Another A review article believed the range of pain were 11- 84 percent of patients have
pain with no relation of the type of cancer. (4)
In a broad survey in UK there were a remarkable relationship between Quality Of Life and pain and
insomnia. (5) In a review article
By Montazery IRAN, patients with breast cancer, had generalized pain, arm problems and menopauses
induced signs. (6)
131
Material and Methods:
101 patients with different cancers in the oncology ward of Shaheed Ghazi hospital in Iran, Tabriz were
interred in research. After signing an informed consent, they completed a valued questionnaire about
their pain severity and its agents and the ways that decrease it. Some data like type and stage of
cancer and pain release drugs was gathered from documents. Then data were interred spss17
software and analyzed.
Results:
Demographic characteristics:46 patients were male and 55 were female. Oldest was 84 years old
and the youngest was 15,the mean age of patients was 44.3.
Pain perception in patients:44 percent of patients had less pain. 43 percent had pain in abdomen
and low back. 12 percent complained all body pain. Other had pain in head, neck, chest, shoulder and
legs. 30 percent had painless drugs, 30 percent denied them. Others hadnt known about any
prescription pain relief drugs. 45 percent of patients didnt complete the item of pain severity. 2 percent
record the severity of pain as mild, 22 percent assigned this item as moderate, in 21 percent pain was
very sever, 7 percent said pain severity as non controllable and in 3 percent sever pain had prevented
routine life activities. According patients data files, the most usual painless drug was Petedin; less
usual drugs were Methadone, Morphine, Acetaminophen and Ibubrophene. There were not any
significant differences between patients age and type of cancer and pain severity.
Discussion:
In a research by Teunissen 50 percent of patients had complained about fatigue, pain, weakness and
anorexia that could not be treated. This rang is near to this research results.(7) In a review article 59
percent of patients with cancer had pain and 1/3 of them were moderate to severe. This subject is
similar to recent study(8). But in this article type of cancer affected the pain severity, but in our recent
study results is apposite to them. According a study in Germany the pain incidence was 55 percent and
44 percent were severe(9). The more pain was seen in the cancers of digestive system, lung, blood
and breast. This article had an important comment to an emergency need to more notice for pain
treatment. The pain was sever and intolerable in 55% of patients. Near 41% of the patients suffered
from moderate pain. There was not any significant relationship within severity of pain and sex or type of
cancer. The most usual drug for pain relief was Petedin. Other analgesic drugs were Methadone,
Morphine, Acetaminophen and Ibuprofen.
Conclusion:
Many pain Analgesic drugs are used for cancer patients; however pain is an important problem that
should be more attention to it in therapy plans.
132
OP 4
Evaluation of Psychiatric Illness in Iranian Stoma Patients
Bahar Mahjoubi, Homa Mohammad-sadeghi*, Mastoureh Mohammadipour, Rezvan
Mirzaei, Reyhanebh Moini
Tehran University Of Medical Sciences, Tehran Institute Of Psychiatry
Introduction and Aims: The objective of this study was to assess the nonpsychotic psychiatric
disorders of stoma patients in Iran. The only study that evaluated stoma patients in Iran indicated that
postoperative problems, especially psychosocial ones, have a rather high frequency in comparison with
other reports, but since no standardized questionnaire was applied for the evaluation of psychosocial
problems and their severity, further studies were needed.
Methods: In this cross-sectional study, patients referred to the Iranian Ostomy Association from 2005
to 2006 filled the 28-item General Health Questionnaire (GHQ) in Farsi as a screening instrument to
identify cases of nonpsychotic psychiatric morbidity.
Results: A total of 155 patients participated in the study, of whom 79 (51%) were female and 76 (49%)
were male. Fifty-five percent of the patients (n=86) had psychiatric problems. The females' mean GHQ
score was significantly higher than that of males (P=.001). Psychiatric disorder was significantly more
frequent among patients with the following specifications: educational level of high school or lower
(P=.001), mucosal hemorrhage of the ostomy (P=.03), stomal stenosis (P=.012), and history of
psychiatric drug consumption (P=.000). GHQ score decreased as stoma age increased (P=.032;
r=.177).
Discussion: Similar to other complications, psychiatric problems are prevalent in Iranian stoma
patients. Our findings highlight the need for special support.
133
OP 5
Which Clinical Observations are Leading Further Psychiatric
Evaluations?
M. Alper nar*, K. Nahit zmenler
*Department Of Consultation-liaison Psychiatry, Taf Rehabilitation Center, Ankara, Turkey department
Of Psychiatry, Glhane Military Medical Faculty, Ankara, Turkey
Introduction and objectives: There are few studies focusing on psychiatric consultation decision-
making processes based on clinical observations in consultation-liaison psychiatry settings.
Aim: We want to explore whether the clinical staff respond to the major psychiatric symptoms by
requesting psychiatric consultation.
Method: This study was conducted in university hospital inpatient settings. A survey that consists of
index symptoms including psychosis, depression, anxiety disorders and eating disorders were
distributed to the clinical staff. Another part was added to assess clinical staffs opinions on their
psychiatric evaluation skills and psychiatric education needs.
Results: A total of 436 surveys were distributed and 328 of them were collected with a response rate
of 75,2 %. While suicidal ideation, hostility and self-harming behavior (83.3% to 83.5%; 80.6% to 65.9;
75.0% to 76.9% for physicians and nurses respectively) are the most acknowledged observations;
refusal of the treating physician and the hospital and not to sign the consent form are the least
acknowledged observations (29.2% to 25.3%; 29.2% to 23.1; 29.2% to 26.4% for physicians and
nurses respectively) for the psychiatric assessment referral. Physicians (72.2%) as well as nurses
(69.2%) think that their current psychiatry knowledge is inadequate and they are aware that they need
to refine their knowledge on psychiatry (75% for physicians and 86.8% for nurses).
Conclusion: Physicians and nurses are facing psychiatric management problems during their clinical
practice. Decision of psychiatric assessment referral is affected by the profession and the type of clinic.
Expressed learning needs thought to be welcomed by academic psychiatrists.
134
OP 6
Examination of Consultation Liaison Psychiatry Referrals at
Rehabilitation Setting; 5 Months Experience
M. Alper nar1, Eda Aslan karde2
1 Consultation-liasion Department, Taf Rehabilitation Center, Ankara, Turkey
2 Department Of Psychiatry, Gediz State Hospital, Gediz, Ktahya, Turkey
Objective: Rehabilitation settings include patients with comorbid psychiatric disorders. Turkish Armed
Forces Rehabilitation Center is a flagship center, specialized in orthopedic, spinal injury, and traumatic
brain injury rehabilitation in Turkey. A diversity of psychiatric symptoms are substantially encountered
during the rehabilitation programme. Thus, we aimed to examine the consultation liaison psychiatry
department referrals in a relatively short time period.
Methods: Referrals to consultation liaison psychiatry department were examined retrospectively
between November 2011 and March 2012. Age, sex, marital status, referring clinic, major complaint,
primary and comorbid psychiatric diagnoses, and given treatment data were collected from the patient
records.
Results: A total of 255 patients were admitted to the consultation liaison psychiatry department.
Seventy-one percent (n=181) of them were male, and 29 % of them (n=74) were female (n=255). The
mean patient age was 41.920.1 years (meanSD). Major complaint of the referrals was anxiety (39.6
%, n=101) and three most common psychiatric diagnoses were anxiety (44.5 %, n=113), depression
(19.7 %, n=50), and post- traumatic stress disorder (11.8 %, n=30).
Conclusion: By its nature, rehabilitation setting consist mostly traumatized patients. There is also a
substantial caregiver burden. Responsible physician must take into account that psychiatric comorbidity
rates are high in rehabilitation center patients and in their family members.
135
OP 7
Trauma Symptomatology of the Trauma Survivors in the
Rehabilitation Setting: 5 Moths Experience
M. Alper nar*, Eda Aslan karde**
*Consultation-liasion Department, Taf Rehabilitation Center, Ankara, Turkey
** Department Of Psychiatry, Gediz State Hospital, Gediz, Ktahya, Turkey
Objective: Turkish Armed Forces (TAF) Rehabilitation Center is the flagship rehabilitation center in
Turkey; specialized in orthopedic, spinal injury, traumatic brain injury rehabilitation and provides health
service for wounded soldiers particularly, service members, and civilians. The patients treated at TAF
Rehabilitation Center with traumatic injuries due to combat or accidents were monitored for post-
traumatic symptoms during their rehabilitation process. The data were analyzed to demonstrate the
symptomology of traumatized patients.
Methods: Sociodemographic features of the patients referred to consultation liaison psychiatry
department with traumatic experience were assessed. Their psychometric evaluation was done using
CAPS, HAM-A, HAM-D, IES-R, DES and STAI.
Results: There were total 30 patients with traumatic experience. A ninety percent of them were male
(n=27), and 10% of them (n=3) were female. The mean age of patients with traumatic experiences was
25.85.13 years old (meanSD). Assessments were done at 5.66.2 moths (meanSD) after the
traumatic experience. Fifty percent of the patients (n=15) were diagnosed as PTSD. Total CAPS scores
were found as 65.241.9, CAPS B subscale scores were 16.313.1, CAPS C subscale scores were
18.211.7 and CAPS C subscale scores were 12.99.2 (meanSD) among PTSD patients. Among
patients without PTSD, total CAPS scores were found as 74.347.6, CAPS B subscale scores were
1710.5, CAPS C subscale scores were 18.614.2 and CAPS C subscale scores were 16.210.3
(meanSD).
Conclusions: Patients with traumatic experience constitutes a vulnerable group of patients with
regards to their traumatic symptoms. These symptoms require careful and early assessment to prevent
PTSD development.
136
OP 8
The Impact of Work on Mothers Psychological Elements in
Ardebil Province (Iran)
Nasimifar Hojjat*, Khalafi Ali, Hashemimehr Azimeh
Peyamenoor University Of Meshkin Shahr- Iran
This paper analyses research on the impact of work on mothers psychological elements in Ardebil
province (Iran). A survey was conducted of a representative sample of working and non-working
mothers in Ardebil province in 2011 (N=450, 225 working mothers, and 225 non-working mothers).
Four main explanatory factors were examined (self esteem, self concept, self efficacy & depression).
The study is a descriptive, co relational design. Significant differences between working and non-
working women were found in Ardebil. It is argued that this is a result of the counter-balance of the
positive and negative factors associated with paid work, such as increased stress on one hand and self
esteem, self concept, self efficacy on the other. Iranian society's particular socio-cultural climate has
contributed to this finding, with its dominant gender-role ideology; the priority and extra weight placed
on women's traditional roles as wives and mothers, and the remarkably influential impact of husbands
attitudes on women's psychological factors.
Key words: self esteem, self concept, self efficacy ,depression, working , non-working mothers
137
OP 9
Interleukin-6 Reflects Trait Impulsivity in Suicide Attempters
Jussi Jokinen
Karolinska Institutet, Stockholm, Sweden
Aim: High CSF and plasma interleukin-6 (IL-6) levels have been reported in suicide attempters.
Features of the suicidal temperament include such personality traits as anger and aggression,
impulsivity, anxiety proneness and low socialization. High levels of neuroticism, and low levels of
conscientiousness assessed with structured personality inventories have previously been associated to
increased levels of IL-6, in population based samples. The aim of this study was to assess whether
plasma levels of IL-6 were associated to specific personality traits in suicide attempters. Methods
Plasma concentration of IL-6 was measured in 58 suicide attempters with a high throughput automated
biochip immunoassay system. Patients were evaluated using the Karolinska Scale of Personality
(KSP). A standard multiple regression analysis was performed with IL-6 as the dependent variable and
KSP factors Neuroticism, Nonconformity, Psychoticism and Extraversion as independent variables
adjusted for age, gender and BMI.
Results: The regression model was significant and the results suggested that high scores on
Extraversion were associated with high levels of IL-6. IL-6 levels showed a significant positive
correlation with trait impulsivity (r=0.39, p=0.003).
Conclusions: In suicide attempters, IL-6 may be related to trait impulsivity, a key feature of the suicidal
temperament. This study motivates further studies on cytokine activity and their involvement in
behavioural development. The study adds further support on biological involvement in suicidal
behaviour.
138
OP 10
Using Oxytocin to Modify Callous Unemotional Traits in Children
Diagnosed with Conduct Disorder, Subtype Significant Callous
Unemotional Traits
Robin Mackenzie
University Of Kent, Canterbury, United Kingdom
Introduction: Oxytocin may hold potential as an effective treatment for children diagnosed with
conduct disorder, subtype significant callous unemotional [CU] traits
Aim: To assess the potential of oxytocin to modify CU traits and enhance empathy
Method: Evaluative review of research in cognitive/affective neuroscience, genetics and psychiatry to
assess the potential of oxytocin to treat CU traits
Results: Current conduct disorder treatments seldom modify CU traits. Oxytocin, a neuropeptide
associated with social bonds in mammals, holds promise as a treatment as its receptor distribution is
atypical in children with CU traits, together with specific atypical amygdala and superior temporal
sulcus formations and genetic markers. Discussion: administration is problematic. Ongoing treatment
entails means involving nasal sprays or injections being replaced by approved intrathecal devices
delivering targeted regular precise doses. Ethical issues centre upon theories of affective empathy as
essential for moral socialisation. Evidence suggests experiencing affective empathy underpins moral
decision making by alleviating harmful actions towards others. Children diagnosed with CU traits do not
feel affective empathy, fear, guilt or remorse, engage in instrumental aggression towards others, are
insensitive to negative reinforcement and resistant or immune to moral socialisation. They tend not to
focus on others eyes to identify their emotions, fail to identify fearful faces and regard actions which
frighten others as acceptable. Administering oxytocin may help to alleviate their atypical oxytocin
receptor distribution to promote social bonds and enhance affective empathy. Yet atypical
neurochemistry and general insensitivity to their own emotions mean they do not feel fearful. Thus, if
they cannot identify fear as one of their own emotions, they cannot identify when another is feeling it
and on that basis refrain from frightening or harming that other. Hence, while oxytocin fosters greater
eye contact, it may not promote affective empathy, guilt or remorse. Programs identifying children with
CU traits as suitable for compulsory treatment on the basis of the risk of future psychopathy may be
unethical because of stigma and labelling. As oxytocin is associated with the formation of ingroups and
the exclusion of outgroup members, ensuring appropriate social bonds form after oxytocin treatment
may prove problematic. Caution is warranted and further research is needed.
139
OP 11
Rational-choice Theory of Neurosis: Development and Treatment
Yacov Rofe
Bar Ilan University Faculty Of Social Sciences
Freud's psychoanalytical theory of neurosis has encountered serious problems, whereby the term
neurosis was excluded by the DSM for the lack of empirical criteria and research that challenges the
existence of repression, the "cornerstone on which the whole structure of psychoanalysis rests" (see
review by Rof, 2008). Moreover, rival theories, including psychoanalysis, are incapable of accounting
for fundamental issues, such as high prevalence of neuroses among women, the profound difference
between Western and non-Western, and the fluctuation of prevalence over different time periods (e.g.,
the striking increase in eating disorders, dissociative identity disorder). Another fundamental issue is
the inability to integrate the various therapeutic interventions into one model. The Rational-Choice
Theory of Neurosis (Rof, 2000, 2010) redefines neurosis by providing five objective criteria and claims
that neuroses are consciously and deliberately adopted to cope with intolerable levels of stress. The
main function of neurosis is a form of repression, redefined as intentional distraction. Patients
consciously and deliberately choose specific neurotic disorders in order to eliminate stress related
thoughts that currently dominate their attention. Thus contrary to Freud, repression is the consequence,
rather than the cause of neurosis. Patients create unawareness by unique psychological processes
which cause the forgetting of the knowledge of self-involvement and the development of self-deceptive
beliefs, which rationalize the maintenance of the symptoms. RCTN accounts for all aforementioned
problems, including the integration of all therapeutic interventions. This revolutionary approach not only
has important implications for the psychological sciences, but also for the legal system, as it implies
that people are responsible for their behaviors, which seemingly appear to be outside their conscious
control.
References Rof, Y. (2000). The Rationality of Psychological Disorders: Psychobizarreness Theory.
New York, NY: Kluwer Academic Publishers Rof, Y. (2002). Psychobizarreness theory: A response to
Lester's review. Contemporary Psychology, 47, 632. Rof, Y. (2008). Does repression exist? Memory,
pathogenic, unconscious, and clinical evidence. Review of General Psychology, 12, 63-85. Rof, Y.
(2010). The rational-choice theory of neurosis: Unawareness and an integrative therapeutic approach.
Journal of Psychotherapy Integration, 20, 152-202.
140
OP 12
The Effect of Alexithymia on Treatment Response in Patients
with Major Depressive Disorder
Mehmet Inta, Cemal Onur Noyan*
Diyarbakr Military Hospital, Department Of Psychiatry, Diyarbakr. gmsuyu Military Hospital,
Department Of Psychiatry, Istanbul*.
Introduction: A relationship between alexithymia and depression is described in several studies but
information about the effect of alexithymia on treatment response in major depressive disorder (MDD)
is limited.
Aim: The aim of the study is to define the effect of alexithymia on treatment response in patients with
MDD. Method: The study population comprised 45 outpatients diagnosed as major depressive
disorder. Structured Clinical Interview (SCID-I) for DSM-IV was used for diagnosis of MDD. Hamilton
Rating Scale for Depression (HAM-D) and the Turkish version of the 20-item Toronto Alexithymia Scale
(TAS-20) were administered to patients before and after treatment with sertraline (50-200 mg/day) for
12 weeks. The response criterion was defined as a 50% or greater decrease in the total HAM-D score.
The sample was classified as alexithymic (n=20, 44,4 %) and non-alexithymic (n=25, 55,6%) in terms
of TAS-20 scores. HAM-D scores, TAS-20 scores and response rate of two groups were compared.
Result: HAM-D scores did not differ between groups. Response rate was 25% in the alexithymic group
and 64% in the non-alexithymic group. HAM-D scores after treatment were significantly correlated with
the TAS-20 scores. Discussion: These findings indicate that alexithymic features have negative effect
on treatment response in patients with MDD.
141
OP 13
Event Related Potentials in Major Depressive Disorder: The
Relationship Between P300 and Treatment Response
Mehmet Inta, Cemal Onur Noyan*
Diyarbakr Military Hospital, Department of Psychiatry, Diyarbakr. gmsuyu Military Hospital
Department of Psychiatry, stanbul*.
Introduction: In the literature, although there are conflicting results about P300 amplitude and latency
in major depressive patients, most of the studies reported that major depressive patients have smaller
P300 amplitude and longer latencies than healthy people.
Aim: In this study we aimed to investigate the relationship between P300 and treatment response in
Major Depressive Disorder. Method: 28 patients suffering from major depression who completed 12
weeks follow up period and 28 healthy people whose age and gender were matched with patients were
included in the study. Event related potentials (P300) were recorded in patients before and after
treatment with sertraline (50-200 mg/day) for 12 weeks. The response criterion was defined as a 50%
or greater decrease in the total Hamilton Depression Rating Scale score. Pretreatment and post
treatment P300 values of the responders (n=18) and nonresponders (n=10) are compared within
themselves and with those of healthy subjects.
Result: No significant difference was found in the P300 amplitudes of responders, nonresponders and
healthy groups before and after treatment. Nonresponders had significantly longer pretreatment P300
latencies than responders and healthy subjects. After treatment of depression, delayed P300 latencies
in the responder group were normalized, but nonresponders still had longer P300 latencies than
responders and healthy subjects.
Discussion: According to these findings, delayed P300 latency may predict a nonresponse to
sertraline treatment; but no relation was found between P300 amplitude and treatment response in
Major Depressive Disorder.
142
OP 14
Oxcarbazepine for Compulsive Water Drinking
C. Onur Noyan*, Mehmet Inta**
*Psychiatry Department Of Gumussuyu Military Hospital **Psychiatry Department Of Diyarbakr Military
Hospital
Objective: Compulsive water drinking(CWD) is well-recognized and unusual clinical disorder
characterized by excessive water-drinking in the absence of a physiologic stimulus to drink. CWD has
several subtypes and multifactorial etiology. There is no pharmacological treatment that has
consistently been demonstrated efficacy of compulsive water drinking, although in some case reports
antidepressants, atypical antipsychotics and other drugs such as pindolol have been reported.
Case: In this case report a 60-year-old woman patient is presented with a diagnosis of CWD in
comorbidity with depressive disorder(without any psychotic and manic symptoms) who was treated
ineffectively with antidepressants and atypical antipsychotics for 3 years. After administration of
oxcarbazepine at a dosage of 600 mg/d, CWD improved within 10 days and no relapse for 12 months.
Conclusions: The oxcarbazepine has also been used as mood stabilizer and for impulse control
disorders, but there is no report of oxcarbazepine in CWD. This is the first cases of CWD treated with
oxcarbazepine. With regard to symptoms of patient and reports on usage of oxcarbazepine for
treatment of impulse control disorders, it has been suggested that some cases with CWD may take part
in obsessive-compulsive disorders or impulse control disorders spectrum. This relationship should also
be investigated.
143
OP 15
Antisocial Personality Disorder: Theory of Mind Disability
C. Onur Noyan*, Mehmet Inta**
*Psychiatry Department Of Gumussuyu Military Hospital **Psychiatry Department Of Diyarbakr Military
Hospital
Introduction: Theory of Mind(ToM) also referrred as mind reading, mentalising or social intelligence is
the ability to identify of others mental state to make sense of or predict others behaviour. There have
been suggestions that this process is disrupted in individuals with Antisocial Personality Disorder(APD)
who tend to misinterpret others emotion. The Reading the Mind in the Eyes Test(RMET) is one of the
most widely used tasks for examining the ToM. The aim of this study is comparing ToM by using the
RMET among subjects with APD and healthy control.
Methods: 30 male subjects with APD and 30 age and sex matched healthy control assessed by a
semistructured sociodemographic form, SCID-II and the Turkish version of the RMET. Results: APD
subjects RMET scores(12,903,27 ) were significantly lower(p=0,000) than the control subjects
scores(17,203,43). The results could not be accounted for by demographics, co-occurring Axis I or II
conditions, medication status, abuse history. These finding suggest that individuals with APD show
significant impairment on identifying of othersemotion.
Conclusion: The results of current study does not confirm the previous studies that revealing the
absence of ToM impairment in APD. Further and larger sample size studies needed to confirm ToM
disabilities in the APD subjects.
144
OP 16
Molecular Genetics of Autosomal Recessive Mental Disorders in
Consanguineous Pakistani Families.
Shoaib Ur Rehman**, Lars Hansen*, Syeda Marriam Bakhtiar, Muhammad Tariq,
Ilyas Ahmad, Saeed Anwar**, Niels Tommerup*, Shahid Mahmood Baig
Institution: National Institute For Biotechnology And Genetic Engineering (nIBGE) P.o.box-577, Jhang
Road, Faisalabad, Pakistan. institution*:wilhelm Johansen Centre For Functional Genome Research
department Of Cellular Andmolecularmedicine the Panum Institute. University Of Copenhagen 3
Blegdamsvej.dk-2200 Copenhagen N Denmark. institution**:department Of Biotechnology Abdul Wali
Khan University Palosa Campus Charsada, Kpk, Pakistan.
Mental disorder or mental illness is a complex term which is a behavioral or psychological pattern
associated with disability that occurs in an individual and is not a part of normal development or culture.
Mental disorders are generally classified into neurological disorders and learning disabilities or mental
retardation. Incidence of mental disorders is relatively high in Pakistan because of high consanguinity.
Hallervorden-Spatz syndrome (HSS) also called neurodegeneration with brain iron accumulation
(NBIA) encompasses a group of progressive extrapyramidal disorders characterized by iron
accumulation in the brain. In the present study, we identified five large consanguineous Pakistani
families with autosomal recessive mental retardation and one with autosomal recessive Hallervorden-
Spatz syndrome (HSS) having multiple affected births. Purpose of the study was to improve the
understanding on protective measurements for mental disorders. Nucleic acid (DNA) was extracted
and subjected to STS (Single tagged sequence) marker analyses for mapping of homozygosity in
known genes and known loci regions using a fluorescence three primer method. All families were
excluded for all known genes and loci regions. For HSS family (consists of three loops), detailed clinical
examination including brain MRI was made for two affected from two loops. Both affected individuals
showed phenotype of HSS. Further its three loops were subjected to the Genome wide scanning using
SNP6.0 array for detection of homozygous regions. No shared homozygous region was found for all
three loops and even for any two loops while five homozygous regions were found for a single central
loop. By checking genotypes for these three loops, no match was found for compound heterozygosity.
PANK2 gene was sequenced as a candidate for this family but no mutation was found. All these
analyses made the molecular genetics of MR6 very complicated and suggest several possible
molecular etiologies; it could be compound heterozygous, have three different mutations or be digenic.
This complexity of HSS needs advanced molecular studies including exome sequencing and next
generation sequencing using DNA capture enrichment to understand the molecular genetics of this
disease phenotype.
145
OP 17
The Relationship of Cognitive Impairment With Neurological and
Psychiatric Variables
Hsna Karaday, zden Arsoy, Burcu Altunrende, Mehmet Hamid Bozta
yrtaihcysP fO tnemtrapeD ytlucaF lacideM ytisrevinU lasyaB tezzI tnabA- Bolu abant Izzet Baysal
University Medical Faculty Department Of Neurology-Bolu/Turkey
Introduction: Cognitive impairment (CI) is an important feature of multiple sclerosis (MS) that affects
up to 50% of patients. It can develop any time during the course of the disease and can even be the
first symptom of the illnesss. Severity of CI seems to be primarily associated with the degree of specific
neuronal loss but factors like disease progression, duration of disease, fatigue, comorbid affective
disorder or drug side effects may also affect cognitive function.
Aim: To assess cognitive function in MS patients and demographically matched healthy controls to see
if there is a difference between these two groups. Method: 31 MS patients diagnosed according to
McDonald criteria and 31 age-sex-education matched healthy controls were included in the study.
Neurological evaluation and disability scoring was made by a neurologist. Standardized psychiatric
evaluation with SCID-I, Standardized Mini Mental Test application, evaluation of depression, anxiety
and functioning with Hamilton Depression and Anxiety Scales (HAM-D, HAM-A) and Global Assesment
of Funcitonality Scale was done by the investigator. Fatigue was assesed by self rating Fatigue
Severity Scale. Cognitive functions were assesed by Serial Digit Learning Test, Verbal and Nonverbal
Cancellation Test, Stroop Test and Rey Auditory Verbal Learning Test.
Results: We found no difference in terms of sociodemographic variables between patients and healthy
controls except for working status. The percent of jobless people were higher in the patient group. Also,
psychiatric comorbidity, especially depressive and anxiety disorders, were higher among MS patients.
As for the cognitive tests, retrieval from long term memory and psychomotor speed were signiticantly
worse in the MS group. CI showed a positive correlation with duration of disease, number of attacks
and physical disability though there were no correlation between CI and depression/anxiety severity.
The duration of disease predicted disturbances in recall and psychomotor speed, whereas severity of
fatigue and disablity predicted depression.
Discussion: Psychomotor speed, attention and memory were primarily imparied in MS patients and CI
was closely associated with clinical aspects of MS rather than depression and anxiety. This CI seen in
a patient population with mild degree of disability and a relatively short duration of disease indicates
that CI can be seen even in early stages of disease before advanced neurological dysfunction sets in.
146
OP 18
QEEG-Neurometric Analysis Guided Neurofeedback (Nf)
Treatment in Dementia: 23 Cases. How Neurometric Analysis is
Important for the Treatment of Dementia As Well As Diagnosis?
Tanju Srmeli
Living Health Outpatient Clinic, Istanbul
Introduction: According to DSM-IV, Dementia requires the development of multiple cognitive deficits
manifested by both 1- memory impairment (impaired ability to learn new information or to recall
previously learned information) and 2-one or more of the cognitive disturbances such as aphasia,
apraxia, agnosia and disturbance in executive functioning. In thisstudy we wanted to show the
outcomes of clinical case series using QEEG and NF in the assessment and treatment of dementia.
Methods: We studied 23 patients ( 10 male and 13 female) with ages ranging between 42 - 86. Before
coming us half of the subjects were taking an an antidementia drug and some of them were on more
than one simultaneously. Additionally of those patients were also administered an antidepressant and
an antipsychotic concurrently. Evaluation measures included drug free QEEG analysis with the NX-
LINK data base, the Mini Mental State Exam, Clinical Global Impressions scale (CGI)
Neuropsychological tests and interviews with the patients family . Our hypothesis was that
neurofeedback treatment that will most benefit those patients who normalize the z score on their
QEEG. Sixty-minute Neurofeedback sessions were administered and each subject completed in
between 20-80 sessions.
Results: All of them showed improvement based on the CGI, Mini Mental State Exam, QEEG-
Neurometric Analysis and the interviews with the patients families. This is a study provides the first
clinical evidence that NF treatment can produce improvements in patients with Dementia. Based on
these positive results, it is recommended that further controlled studies with additional outcome
measures to be conducted.
Discussion: Dementia patients may have mood problems, sleep problems or agitation. They may
need extra psychotropics to address those problems. But an effective non-drug alternative may be
useful in this population to cover all those problems.
Key words: QEEG, Dementia, Neurofeed
147
POSTER PRESENTATIONS
148
P 1
Life Satisfaction Among Iranian Elderly
Aazam Asadollahikordkandi
Health Of Office, Shahed Beheshti University Of Medical Science. Tehran- Iran
Background: life satisfaction among elderly is becoming a important issue with increasing aging
population in the world. The factors such as physical activity, social support, medical conditions or
diseases may affect life satisfaction among elderly. The objective of this study was to examine
relationship between physical activity, social support, medical conditions or diseases Iranian elderly
living in community.
Methods: this study was in a cross-sectional research design. Interviews were conducted among 103
of elderly ( 43 male and 60 female).aged 60 years and over that living in community in Karaj province.
Life satisfaction was examined by LSI A life satisfaction index .medical conditions was assesd by a list
of 25 specific disease such as arthritis, gout, glaucoma,cataract,asthma,hypertension,heart disease,
numbness at extremities,diabetes, gastritis, kidney isease, prostate problem, cancer
,anaemia,stroke,,tuberculosis,breathing difficulties, bedsore, fall, head injury, fracture, memory
problem, uninary incontinence, faecal incontinence. physical activeity consist of ADL and IADL that
covered by Barthel and lawton index. Also social support was measured by Lubben social sacle. The
final questionaire consisted of a demographic characteristic.
Results: The findings showed that the respondents were lower life saitisfaction about 8%. Life
sationfaction was associated with low level of physical activity, low income and marital status
Conclusion: The factors of physical activity income and marital status are important factor that
influence on life satisfaction among elderly.
149
P 2
Does the Presence of a Psychiatrist or a Psychiatric Outpatient
Clinic Prevent the Attempted Suicide?
Abdullah Akpinar(1), Hseyin Yumrukcal (2)
(1)assistant Professor, Deparment Of Psychiatry, Sleyman Demirel University Medical School,
Isparta, Turkey. (2)physician In Psychiatry, Erzincan University Mengucek Gazi Education And
Research Hospital, Erzincan, Turkey.
1.Introduction Psychiatric disorders and specific psychiatric symptoms within or outside of the context
of a psychiatric disorder, have been associated with increased suicide risk [1-4]. Suicide risk is higher
for individuals who have experienced significant personal, academic, vocational or financial loss; who
have maladaptive coping skills; who have become dependent on others, or have lost social or familial
role [5-7]. 1.1
Aim: This research was conducted in a district area with a single hospital. The hospital had no
psychiatrist before September 2009, at which time the psychiatry clinic opened and began accepting
outpatients. In this study, we aimed to determine whether having a psychiatric outpatient clinic has a
significant effect on the emergency admission rates of attempted suicides. We compared attempted
suicide rates (emergency admissions) and associated factors specified for the first year of the
psychiatric outpatient clinic, to the attempted suicide rates and associated factors specified for the
previous year. 2.
Methods 2.1. Local information Terme is a district of Samsun Province of The Republic of Turkey
which is located in Black Sea Region of Northern Anatolia. Terme has a population of 82.621 as of
2010 [8]. 2.2 Measures We compared attempted suicide rates (emergency admissions) and associated
factors specified for the first year of the psychiatric outpatient clinic (September 2009- August 2010) to
the attempted suicide rates and associated factors specified for the previous year (September 2008-
August 2009). 2.3 Statistical Analysis SPSS for Windows 17.0 was used for statistical analysis.Chi
square and fisher exact test were used to determine the significance of differences between
percentages. 3.Results Of all attempted suicides between September 2008 and August 2010, 54%
(n=115) were admitted within the first year before the openening of the psychiatry outpatient clinic,
while 46% (98) were admitted in the second year of that period, namely the first year of the psychiatry
outpatient clinic. The mean age of suicide attempters was 22.98.2 years (range: 12-48). Of those 104
(49.7 %) were teenagers. 97.2 % (n=207) of the patients had overdosed on prescribed drugs and 2.8%
had employed other methods (eg. wrist cutting, hanging, drowning in the sea). Of the 41 people who
were referred to the psychiatry outpatient clinic for suicide, 4 have attempted suicide within a year.
However, of a total of 213 cases, 8 had attempted suicide again within a year. 4.Discussion We aimed
to determine whether the presence of a psychiatry clinic or a psychiatrist, has any effect on the rate of
attempted suicide admissions in the emergency department. Our results showed that 54 % (n=115) of
the cases had attempted suicide in the one-year period prior to the opening of psychiatry outpatient
clinic and 46 % (n=98) cases had attempted suicide in the one-year period beginning with the opening
of the psychiatric outpatient clinic. The number of suicides (17 cases/year) decreased by 8 % in one-
year period beginning with the opening of the psychiatric outpatient clinic. Decrease in the rate of
attempted suicides indicated that the presence of the psychiatric outpatient clinic is a protective factor
for suicide. According to some researchers, up to 98 % of patients who commit suicide may suffer from
at least one major psychiatric disorder [9-12]. Therefore, recognizing and treating psychiatric disorders
has special importance. Also psychiatric disorders could be a preventable risk factor for suicide. The
most frequently reported suicide motive was the situation was so unbearable that I could not think of
any other alternative. The common purpose of suicide is to seek a solution. Presence of a psychiatry
clinic in the district allows patients to seek treatment of psychiatric disorders and stimulate patients to
learn to cope with unbearable psychological pain such as guilt, fear, defeat, shame, humiliation,
disgrace, grief, loneliness, hopelessness, frustrated love, rage and hostility and to learn the
psychological nature of suicide [13,14]. Therefore, the first approach for suicide attempts in the
emergency department should be referral to psychiatry departments. Of a total of 213 cases, 8 (3.8 %)
had repeated suicidal behaviour during the first year after a first suicide attempt. 4 (9.8%) of the
suiciders who applied to the psychiatric outpatient clinic (n=41) attempted suicide again within a year.
Repeated suicide in these four cases suggest that a multidisiplinary approach is necessary for suicide
[15]. The risk of repeated suicidal behaviour is highest during the first year after a suicide attempt. In
150
the WHO/EURO Multi-Centre Study on Suicidal Behaviour it was found that 29 % made another
attempt in a one-year follow-up [16]. 49.7 % of all suicide were commited by teenagers. The highest
rates of suicidal behaviour are among younger people. Due to this high rate of teenage suicide rate;
suicide prevention for teenage group has to be comprehensive, multidisciplinary and involve different
aspects of life as well as different sectors of society, and national strategies and policies should to be
developed [17,18]. In conclusions, a psychiatry oupatient clinic is a protective factor in terms of suicide.
Psychiatric disorders may be preventable risk factors for suicide. Training of emergency physicians is
effective in prevention of suicide. Discharge decision of the patient from emergency department should
be carefully evaluated against involved risks. The size of the problem of suicidal behaviour, means that
provision of aftercare is of major importance. In order to develop preventive measures, specific national
and cultural factors should also be taken into consideration.
References
1. Bertolote JM, Fleischmann A, De Leo D, Wasserman D. Psychiatric diagnoses and suicide: revisiting
the evidence. Crisis. 2004;25(4):147-55.
2. Cheng ATA, Chen THH, Chen CC, Jenkins R. Psychosocial and psychiatric risk factors for suicide.
Br J Psychiatry 2000; 177:360-5.
3. Garlow SJ. Age, gender, and ethnicity differences in patterns of cocaine and ethanol use preceding
suicide. Am J Psychiatry 2002; 159:615-9.
4. Bertolote J, Fleischmann A, De Leo D, Wassserman D. Suicide and mental disorders: do we know
enough? Br J Psychiatry. 2003;183:382-3.
5. Phillips MR, Yang G, Zhang Y, Wang L, Ji H, Zhou M. Risk factors for suicide in China:a national
case-control psychological autopsy study. Lancet 2002;360:1728-36.
6. Johnson JG, Cohen P, Gould MS, Kasen S, Brown J, Brook JS. Childhood adversities, interpersonal
difficulties, and risk for suicide attempts during late adolescence and early adulthood. Arch Gen
Psychiatry 2002;59:741-9.
7. Stack S. Media coverage as a risk factor in suicide. J Epidemiol Community Health 2003; 57:238-40.
8. Information About to Terme: avaliable: http:// www. Terme.bel.tr/ilce_tanitim.asp Accessed 20
January 2012
9. Suominen K, Henrikson M, Suokas J, Isometsa E, Ostamo A, Lnnqvist J. Mental disorders and
comorbidity in attempted suicide. Acta Psyhiatrica Scandinavica. 1996;94:234-240
10. Ferreira de Castro E, Cunha MA, Pimenta F, Costa I. Parasuicide and mental disorders. Acta
Psychiatr Scand. 1998 Jan;97(1):25-31
11. Balazs J, Bitter I, Lecrubier Y, Csiszer N, Ostorharics G. Prevalence of subthreshold forms of
psychiatric disorders in persons making suicide attempts in Hungary. Eur Psychiatry. 2000
Sep;15(6):354-61.
12. Baxter AJ, Charlson FJ, Somerville AJ, Whiteford HA. Mental disorders as risk factors: assessing
the evidence for the global burden of disease study. BMC Med. 2011 Dec 16;9(1):134.
13. Shneidman ES. Perspectives on suicidology. Further reflections on suicide and psychache.Suicide
Life Threat Behav. 1998;28(3):245-250.
14. Shneidman ES. Suicide as psychache. J Nerv Ment Dis. 1993;181(3):145-7
15.Wasserman D, Rihmer Z, Rujescu D, Sarchiapone M, Sokolowski M, titelman D, Zalsman G,
Zemishlany Z, Carli V. The European Psychiatric Association (EPA) guidance on suicide treatment and
prevention. Eur Psychiatry. 2012;27(2):129-141.
16. Arensman E, Kerkhof A, Dirkzwager A, Verduin C, Bille-Brahe U, Crepet P, De Leo D, Hawton K,
Hjelmeland H, Lnnqvist J, Michel K, Querejeta I, Salander-Renberg E, Schmidtke A, Temesvary B,
Wasserman D. Prevalence and risk factors for repeated suicidal behaviour: Results from the
WHO/EURO Multicentre Study on Parasuicide, 1989-1992.
17. Payci SO, Ergin A, Saatci E, Bozdemir N, Akpinar E, Ergun G.Suicidal thought and behavior in high
school students in Adana, Turkey. Coll Antropol. 2005;29(2):527-31.
18. Yasan A, Danis R, Tamam L, Ozmen S, Ozkan M.Socio-cultural features and sex profile of the
individuals with serious suicide attempts in southeastern Turkey: a one-year survey. Suicide Life Threat
Behav. 2008;38(4):467-80.
151
P 3
The Presence or Absence of a Psychiatry Clinic and a
Psychiatrist in the District: Can it Change the Number of
Diazepam Injections for to Psychiatric Symptoms in the
Emergency Department?
Abdullah Akpinar
Assistant Professor, Suleyman Demirel University Medical Faculty And Department Of Psychiatry-
Isparta, Turkey
Introduction: On many occasions acutely psychiatric patients are treated with injections of diazepam.
Benzodiazepines may slow down recovery from psychoneurotic stress, can produce dependence, and
tend to be prescribed indiscriminately in many emergencies (1). Precautions should be taken to prevent
the routine prescription of benzodiazepines to people experiencing distress in emergencies (2). One-
third of the General Practitioners seems to prescribe only anxiolytics for anxiety and depression
symptoms and the most frequently prescribed anxiolytic drug seems to be diazepam (3-5).
Objective: Our research was conducted in a district which has only one hospital. There was no
psychiatrist in this hospital before the September of 2009, since when the hospitals psychiatry clinic
has been accepting patients. We aimed to investigate the frequency of i.m. diazepam administration by
general practitioners in the emergency department in the absence of psychiatry specialist and after the
presence of a psychiatry specialist in the hospital (district).
Method: In this study, emergency departments green prescription registry book was analyzed.
Number of diazepam injections by psychoneurotic disorder were determined. We compared the
number of diazepam injections made in the emergency department of the hospital, in the one-year
period before the opening of the psychiatry outpatient clinic (September 2008 - August 2009) and in the
one-year period after the opening of the psychiatry clinic (September 2009-August 2010). Diazepam
injections were administered by general practitioners in the emergency department.
Results: Our results revealed that in the one year period prior to the establishment of the psychiatry
outpatient clinic, the number of diazepam injections was 6604, while after the psychiatry outpatient
clinic this number decreased to 5467 in the emergency department in one year, which points to a net
decrease of 1137 (17.2 %). In the one-year period before the opening of the psychiatry clinic; 379 units
of diazepam were used in September 2008, this number increased to 682 in August 2009 and
decreased back again to 383 in August 2010. The number of diazepam injections in August 2010 was
44 % (n=299) less than the number of diazepam injections in August 2009.
Discussion: There was a reduction in the number of psychiatric admissions in the emergency
department in the first year of the psychiatry clinic, attributable to the alleviation of the burden of
psychiatric patients. Psychiatric patients tended towards the psychiatry outpatient clinic instead of using
the emergency to seek treatment. Psychiatry patients did not prefer to admit to the emergency clinic for
treatment. Routine diazepam injections pose a lot of risks. Psychiatric patients may not be properly
diagnosed. Patients conception of psychiatric illness and psychiatric interventions may become
distorted, causing them to seek help only in moments of crisis at the emergency department, which
would inevitably lead to an increased burden for emergency departments and patients alike. In a
vicious cycle of this type; psychiatric disorders are not carefully evaluated by the emergency physician.
Patients on the other hand, are deprived of the benefits of a follow up at the outpatient psychiatry clinic
with proper and effective treatment. Thus, the patients daily, occupational, educational, familial, social
functioning are distrupted. Psychiatric disorder become chronic. Patients and relatives become
depressed, anxious, resentful, angry and pessimistic. The vital issues of self mutilation, harm to others,
suicide and homicide may arise (6,7). People presenting with acute anxiety are numerous in the early
phases of all emergencies. Non-pharmacological measures (e.g. psychological first aid) can be used.
(8) There are occasions when pharmacological interventions are indicated. For example, they are
appropriate in cases of severe agitation, sleeplessness, anxiety, dysphoria, somatization that interfere
with a person's ability to address their own and their family's survival needs, and that do not respond to
non-pharmacological interventions. If patients have a psychotic reaction, an injectable antipsychotic
(such as the combination of haloperidol and biperidene) can be administered. Antidepressant tablets
152
with sedative effects (amitriptyline, trazodone, mirtazapine) are a treatment option (9,10). Oral forms of
benzodiazepines (alprozolam, lorezepam, diazepam) can be used. Routine injections can thus be
avoided. Conclusions: Diazepam injections for pscyhoneurotic symptoms are common in emergency
departments. Mental disorders make a substantial independent contribution to the burden of disease in
the emergency departments. It is also necessary to improve emergency professionals skills regarding
the diagnosis and management of psychiatric emergencies.
References:
1. Freeman C. Drugs and physical treatment after trauma. In: rner R, Schnyder U, editors.
Reconstructing early intervention after trauma. Oxford: Oxford University Press; 2003:169-76.
2. Van Ommeren M, Saxena S, Saraceno B (2005) Mental and social health during and after acute
emergencies: emerging consensus? Bull World Health Organ 83: 7175.e1001030
3. Lotrakul M, Saipanish R. How do general practitioners in Thailand diagnose and treat patients
presenting with anxiety and depression? Psychiatry Clin Neurosci. 2009;63(1):37-42.
4. Morgan JD, Wright DJ, Chrystyn H. Pharmacoeconomic evaluation of a patient education letter
aimed at reducing long-term prescribing of benzodiazepines. Pharm World Sci. 2002;24(6):231-5.
5. Gask L, Dixon C, May C, Dowrick C. Qualitative study of an educational intervention for GPs in the
assessment and management of depression. Br J Gen Pract. 2005;55(520):854-9.
6. Jones L, Asare JB, El Masri M, Mohanraj A, Sherief H, Van Ommeren M. Severe mental disorders in
complex emergencies. Lancet 2009;374: 654661.
7. Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, Rahman A. No health without mental
health. Lancet 2007;370: 859877
8. Inter-Agency Standing Committee (IASC) Guidelines on mental health and psychosocial support in
emergency settings. Geneva: IASC. 2007.
9. Uok A. Acute exabations of schizophrenia treatment. The Psychiatric Association of Turkey
Treatment Guidelines of Schizophrenia. Ed.K Alptekin, C Atbasoglu. The Psychiatric Association of
Turkey publications. 2005, p:1-7
10. Walsh JK. Drugs used to treat insomnia in 2002: regulatory-based rather than evidence-based
medicine. Sleep, 2004;27:1441-1442.
153
P 4
Evaluation of the Treatment Compliances for Illegal Drug Users
Who Has Under the Probations Treatment in Samsun-turkey
Abdullah Akpinar(1), Osman al(2) , Umut Mert Aksoy(3)
(1)assistant Professor, Suleyman Demirel University Medical Faculty Department Of Psychiatry-isparta
(2)md. Phd., Samsun Mental Hospital-samsun , (3) Bakrkoy Research and Training Hospital for
Psychiatry
Introduction: Individual and community problems are increasingly spreading for illegal drug users,
thus some new legislative approaches are applied for necessity (1). Probation system allows an
opportunity to be a treat in hospital instead of prison for illegal drug users. The probation system is
applied in many countries over the world, is been carried out in our country since 2006 (1-3). There
were a few data on treatment compliances for probation in our country (4-5).
Objective: In this study we evaluated treatment compliances to who applied by probation in Samsun
Mental Hospital at 2010. Method: This data were collected a retrospective way. This study data
included in 2010. In datas ncluded ; ages, sex, persons treatment compliance. Treatment compliances
were approved by board of health committee who hadnt got in order to four negative urine results and
regularly continued the psychiatric interviews. Results: Total 491 persons were establish who
applicants for probation at 2010. Only 4 (0.9 %) were female and 487 (99.1 %) were male. The mean
ages of the subjects was 32.59.8 years (range: 17-70). 376 (77.6 %) were compliance to treatment
and 115 (22.4 %) were uncompliated.
Discussion: 77.6 % of all had treatment compliance. These persons didnt punish the prison and
completed their treatment in the community. Probation has contributed that was apparent for freedom.
22.4 % of all hadnt got treatment compliance. This reason should be investigated that why some of
them become uncompliance. Person must be detail informed who has probation under treatment.
There is a training program for it (6)
Conclusion: Probation has contributed that was apparent. However existing deficiences must be
determined. New methods can be developped for despite the implementation of training programs who
are uncompliance.
References:
1. Altntoprak AE, Akgr SA, Cokunol H. Yasa D Madde Kullanm Nedeniyle Denetimli Serbestlik
Tedbiri Uygulanan Kiilerde Tedavi Uygulamalar ve Toksikolojik Analiz. Trkiye'de Psikiyatri 2007;
9(3):166-172.
2.Belenco S. The impact of drug offenders on the criminal justice system. Drugs, crime and the criminal
justice system, Weighteid R.(ed), Anderson Publishing Co. Cinninati, 1990, p:27-78
3.Larsson-Kronberg M, Ojehagen A, Berglund M. Experiences of coercion during investigation and
treatment. Int J Law Psychiatry 2005; 28(6):613-621
4. Balc engl C, engl C, Dndolu S, Kaya K. Denizli AMATEM kliniinde denetimli serbestlik
uygulamalar. 6. Ulusal Alkol va Madde Bamll Kongresi, Poster Bildiri, 3-6 Aralk 2009, Belconti
Resort Hotel, Antalya.
5.Evren C. Yasa d madde kullananlarda denetimli serbestlik: Psikiyatrik izleme sreci. 2011;1:1-14.
6.gel K, Karada F, Can Y, Altntoprak E, Cokunol H. Denetimli serbestlik bamllk program.
Trkiye Psikiyatri Dernei Yaynlar; 2010.
154
P 5
Is There Any Risk on Leukocyte with Combination of Clozapine and
Amilsulpride in the Treatment for Schizophrenia
Abdullah Akpinar(1), Osman al(2)
(1)assistant Proffessor, Suleyman Demirel University Medical Faculty And Department Of Psychiatry-isparta
(2)md, Phd. Samsun Mental Hospital - Samsun
Introduction: Clozapine is the gold standard treatment for resistant schizophrenia; however, there are still
patients who are non-responsive or partially responsive to treatment. Although a lack of evidence exists in
reality, these patients are treated with a combination of another pharmacological agents in addition to
Clozapine(1). Co-administration of amisulpride, in a group of patients partially or non-responsive to
clozapine, may lead to a substantial improvement in symptoms, without worsening the side effect burden
(2,3). Also beneficial effect of short term amilsulpiride augmentation of clozapine therapy for schizophrenia
patients is enhanced by its antisalivatory effect on clozapine induced hypersalivation (4). The cumulative
incidence of agranulocytosis in patients treated with clozapine is approximately 0.8 % after. Benign
neutropenia occurs more frequently than agranulocytosis (5,6). Combination of amilsulpride and clozapine
administrated in clinical practise but inadequate data for its effects on leukocyte.
Aim: Is there any risk for leukopenia or agranulocytosis with combination of clozapine and amilsulpride in
the treatment for schizophrenia Method: Twenty-seven consecutive case series with combination of
clozapine and amilsulpride in the treatment for schizophrenia were included in the current study. The group
consisted of patients seen in the inpatient clinic at Samsun Mental Hospital between January 2011 and
January 2012. White blood cell count less than 3500 cells/L was referred as leukopenia
Results: *The mean ages of the patients were 4112 (range: 21-68). *9 (33.3 %) were female and 18 (66.7
%) were male. *The mean length of follow-up was 10 weeks (range 2-60 weeks). *Clozapine mean dose,
combination arm: 440180 mg/d (range:100-700 mg/d) and Amilsulpride mean dose, combination arm:
637184 mg/d (range: 400-800mg/d). *During the follow up period the lowest leukocyte count were
65331360x103 /L (range 4200-8800). *Drugs doses reduction or discontinuation was not for necessary to
worrying about leukopenia in any patient.
Discussion: Clozapine is a well-known drug that is used in treatment-resistant schizophrenia, but
granulocytopenia, which may lead to a potentially fatal condition as agranulocytosis, limit its use.The
incidence of granulocytopenia related to clozapine use was about 0.8% (5-7). Benign neutropenia occurs
more frequently than agranulocytosis. In sample of 68 patients receiving clozapine, transient neutropenia
was found in 22% of the patients (6). In this study the mean time of white blood cell count was found to be
10 weeks. None of the patients treated with combined of clozapine and amisulpride showed leukopenia.
Also none of the patients drug doses were changed for leukopenia fear. Coar et all. showed that
Amilsulpride used after a diagnosis of clozapineassociated granulocytopenia in six patient and none of the
patients treated with amisulpride showed prolonged low white blood cell count (7).
Conclusion: Combination of clozapine and amilsulpride is seems not to adverse affected for leukocyte
(agranulocytsos) is at least in the short term. Long-term follow up with larger samples is needed before firm
conclusions can be drawn.
References:
1. Pai NB, Laidlaw M, Vella SC.Augmentation of clozapine with another pharmacological agent: treatment
for refractory schizophrenia in the 'real world'. Acta Psychiatr Scand. 2012:20. doi: 10.1111/j.1600-
0447.2012.01854.x. [Epub ahead of print]
2.Gen Y. Taner E, Candansayar S. Comparison of clozapine-amisulpride and clozapine-quetiapine
combinations for patients with schizophrenia who are partially responsive to clozapine: a single-blind
randomized study. Adv Ther. 2007;24(1):1-13.
3.Knopf U, Henn FA, Thome J.Combination of clozapine and amisulpride in treatment-resistant
schizophrenia--case reports and review of the literature. Pharmacopsychiatry. 2004;37(1):26-31.
4.Kreinin A, Novitski D, Weizman A. Amisulpride treatment of clozapine-induced hypersalivation in
schizophrenia patients: a randomized, double-blind, placebo-controlled cross-over study. Int Clin
Psychopharmacol. 2006;21(2):99-103.
155
5. Herceg M, Muzinic L, Jukic V. Can we prevent blood dyscrasia (leucopenia, thrombocytopenia) and
epileptic seizures induced by clozapine.Psychiatr DanubP.2010;22(1):85-9.
6.Hummer M, Kurz M, Barnas C, Saria A, Fleischhacker WW. Clozapineinduced transient white blood count
disoreders. J Clin Psychiatry 1994;55:429-32.
7. Coar B, Taner ME, Eser HY, Altnz AE, Tarhan R. Does switching to another antipsychotic in patients
with clozapine-associated granulocytopenia solve the problem? Case series of 18 patients. J Clin
Psychopharmacol. 2011;31(2):169-73.
156
P 6
Rtms Augmentation in Treatment Resistant Depression Patients
(preliminary Report)
Ali Bozkurt*, Sleyman zselek**, Mehmet Ak**, zlem Hekim Bozkurt***
* Near East University School Of Medicine Department Of Psychiatry ** Glhane School Of Medicine
Department Of Psychiatry *** Dkap Children Hospital Department Of Child Psychiatry
Introduction: Almost 50% of Major Depressive Disorder (MDD) patients are not responding to their
first treatment (1,2). Treatment resistant depression (TRD) has been described as partial or none
response to efficient treatment (3). We still need alternative treatments in TRD patients and researches
have shown that repetitive transcranial magnetic stimulation (rTMS) can be an effective treatment
alternative (4).
Aim: The aim of this study was to investigate the response, tolerability and side effects of
augmentation of rTMS in TRD patients. Method: Twenty seven TRD patients (15 female and 12 male)
have been included in the study. They have been interviewed before treatment and end of week 1, 2, 4,
and 8. They clinical outcome has been analyzed by HAM D-17, BDI, and CGI scores. They have
received high frequency (20Hz) rTMS for 10 days, 2 seconds and 40 trains per treatment which means
1600 pulses. None of the patients were psychotic and none of them changed their medications that
they were using before rTMS implication.
Result: Three out of 27 patients has been switched to ECT during treatment due to suicidal ideations
and 1 could not tolerate the side effect of treatment. So 23 of 27 have completed the study. At the end
of week 8 the mean HAM-D scores have declined from 27,88 6,43 to 22,398,71 (t=3.71, P<0.001)
and BDI scores declined from 39,489,15 to 32,0811,73 (t=3.44, P<0.001). 11 of 23 patients did get
partial response and 3 remitted but 9 did not respond at all.
Discussion: The results have shown that rTMS can be a treatment alternative at least in some TRD
patients.
References:
1) Sackeim HA. 2001. The definition and meaning of treatment- resistant depression. J Clin Psychiatry
62(Suppl 16):1017.
2) Fava M. 2003. Diagnosis and definition of treatment-resistant depression. Biol Psychiatry 53:649
659.
3) Nierenberg AA, Dececco LM. Definitions of antidepressant treatment response, remission,
nonresponse, partial response, and other relevant outcomes: A focus on treatment-resistant
depression. J Clin Psychiatry. 2001;62:59.
4) Bernardo DellOsso, Giulia Camuri, Filippo Castellano, Vittoria Vecchi, Matteo Benedetti, Sara
Bortolussi and A. Carlo Altamura. Meta-Review of Metanalytic Studies with Repetitive Transcranial
Magnetic Stimulation (rTMS) for the Treatment of Major Depression. Clinical Practice & Epidemiology
in Mental Health, 2011, 7, 167-177
157
P 7
Tdo2 Gene Polymorphism in Turkish Children With Autism
zlem Hekim Bozkurt*, Tezan Bildik, Afik Berdeli, Ali Bozkurt
Ankara Childrens' Hematology Oncology Research Hospital
Introduction: Tryptophan 2,3-dioxygenase (TDO2) is a rate-limiting enzyme in the metabolism of
tryptophan, the precursor of serotonin. A polymorphism that results in decreased activity of TDO2 could
decrease the metabolism of tryptophan through the kynurenine pathway, causing a shift toward
increased levels serotonin.
Aim: To examine the relationship between autism and polymorphisms in the TDO2 gene in Turkish
population. Method: We have used a casecontrol study. We analyzed DNA samples from77 children
with autism and in 156 age- and race- matched controls, for two TDO2 gene polymorphisms using
PCR-RFLP method. The genotype distribution and allele frequency among groups was compared
using 2, Mann-Whitney test and logistic regression analysis.
Result: There was not found a significant difference between children with autism and healthy controls
for the TDO2 gene C18339241A genotype distribution and allele frequency (p>.05). In contrast, a
significant difference in the TDO2 gene A18340462C genotype distribution and allele frequency was
found between autistic children compared to the healthy controls (p<.001). Genotype-phenotype
correlations indicated that there was no evidence for a significant association between the TDO2 gene
C18339241A polymorphism and autistic symptom profile. For the TDO2 gene A18340462C
polymorphism, there was only found a significant association (p<.05) between 18340462C allele and
subscale of body use on the Childhood Autism Rating Scale (Schopler et al., 1980).
Discussion: It was determined that the TDO2 gene A18340462C polymorphism was associated with
autism in Turkish population (OR=5.797; 95% CI 3.101- 10.838; p<.001). Furthermore, carriers of C
alleles at position of 18340462 nucleotide strongly associated with stereotypic behaviors in children
with autism.
KEY WORDS: autism; TDO2; polymorphism.
158
P 8
An Epileptic Psychosis Case Seen in Childhood
zlem Hekim Bozkurt*, Ali Bozkurt**
*Ankara Pediatric&pediatric Hematology Oncology Training And Research Hospital Child Psychiatry
Departman
**near East Unversty Psychiatry Departman
Introduction: Epilepsy is one of common chronic disorders. Epilepsy can be concurrent with cognitive
and behavioral disorders. It can also be comorbid with psychiatric disorders (Torta and Keller 1999,
Kwan and Brodie 2001). In this case report we wanted to discuss a child who had a psychotic episode
with visual and auditory hallucinations and active partial epilepsy findings in sleep induced EEG. In this
rare case we also wanted to discuss the diagnosis and treatment procedures and the importance of
psychiatric and neurological interview.
Case: O.. Male, born in 2001. He has been diagnosed as epilepsy when he was 8 and had started to
use antiepileptic medications. He had been brought to the outpatient child psychiatry clinic by his
parents and was complaining from irritability, loss of pleasure, unhappiness and defieing parents,
teachers and other supervisorsat school. The psychiatric examination was as following: He was
conscious, his orientation and cooperation was intact. He had depressive and dysphoric mood and was
irritable. His thought process and content, judgment, verbal communication, eye contact, perception
was normal. Medical treatment has been initiated but after an epilepsy episode this treatment has been
stopped. For his depressive mood an irritability he has been consultated with neurology department
and sertraline with atomoxetine has been prescribed. At the first day of this treatment the patient has
reported visual and auditory hallucinations. He reported hearing screaming and crying people and
seeing people without limbs which were bleeding from their eyes. He was also seeing burning
skeletons. His WISC'R test has been scored 75. His EEG had a pathological focus which was
concordant with active partial epilepsy. The MR scan has been reported as normal. His medications
have switched to antiepileptic medications. After 3 weeks his depression an psychotic symptoms
declined.
Discussion: Epileptic seizures may resemble psychiatric signs and symptoms. This may cause
problems in diagnosis and treatment. It's important to evaluate patients detailed and use both
psychiatric and neurological evaluation for differential diagnosis.
159
P 9
Tbars and Lipid Profile in Tunisian Bipolar I Patients
Asma Ezzaher 1,2, Dhouha Haj Mouhamed 1,2, Anwar Mechri 2, Fadoua Neffati 1,
Ilhem Hellara 1, Wahiba Douki 1,2, Lotfi Gaha 2, Mohamed Fadhel Najjar 1
1biochemistry And Toxicology Laboratory, Monastir University Hospital, 5000 Tunisia 2research
Laboratory "vulnerability To Psychotic Disorders Lr 05 Es 10", Department Of Psychiatry, Monastir
University Hospital, Tunisia.
Introduction: Several recent studies reported that patients with bipolar disorder have significant
alterations in antioxidant enzymes. The-end products of lipid peroxidation, especially malondialdehyde
(MDA) evaluated by thiobarbituric acid reactive substances (TBARS) are considered a direct index of
cell lipid peroxidation.
Aims: We aim to investigate the variations of TBARs values, to explore their association with
perturbations in lipid profile in Tunisian bipolar I patients and to explore the association of TBARs to
clinical and therapeutic characteristics of this population.
Patients and methods: Our study included 90 patients with bipolar I disorder, diagnosed according to
the DSM IV, and 92 controls aged respectively 37.211.8 and 34.113.9 years. TBARs concentrations
were determined by enzymatic method. Total cholesterol, triglycerides, c-LDL and c-HDL were
determined by enzymatic colorimetric methods and ApoA1, ApoB and Lp(a) by immunoturbidimetric
techniques on Konelab 30TM. Results and discussion: Compared with controls, patients had
significantly higher TBARs (8.82.5 vs 7.12.8; p<0 ,0001), total cholesterol (4.44 1.05 Vs 3.540.96
mmol/L; p<10-3), c-LDL (2.021.10 Vs 1.010.35 mmol/L; p<10-3 ), Lp(a) (23 211 Vs 148212 mg/L;
p=0.01) levels and ApoB/ApoA1 ratio (0.710.26 Vs 0.580.35 g/L; p=0.009), and significantly lower
ApoA1 level (1.190.25 Vs 1.440.39 g/L; p<10-3). Furthermore, TBARs were significantly correlated
with cholesterol values (r=0.302; p=0.007). Moreover, Bipolar I disorder was significantly associated
with hyperTBARs (OR, 2.23; 95%CI: 1.23-4.03; p=0.008). Depressive patients had the highest levels of
TBARs (p=0.02). Moreover, TBARs were significantly correlated with the illness duration (r=0.356;
P=0.001) and the total number of illness episodes (r=0.247; p=0.02). However, any significant
association was found between this parameter and drug use.
Conclusion: Bipolar patients had a significant increase in TBARs values and perturbations in their lipid
profile that contribute to increased risk of oxidative stress and cardiovascular disease. TBARs were
significantly positively correlated with cholesterol, with the illness duration, and the total number of
illness episodes, but not associated with treatment.
160
P 10
The Impact of Attention Deficit Hyperactivity Disorder on Sleep
and Screen Exposure Among School Children
Ayse Rodopman Arman *, A. Bkmazer, B. Acar, F. Husrevoglu, A. Slocum,
B. Turan, P. Ay
Marmara University Child And Adolescent Psychiatry Department marmara University Public Health
Department marmara University Medical Faculty
Introduction: Attention Deficit Hyperactivity Disorder (ADHD) is a multifactorial disease of genetic
origin that often affects the academic and social functions of children. The relationship of ADHD with
socioeconomic status (SES), sleep problems and the exposure to screen (TV, internet, video games)
has not been researched adequately. The purpose of this study is to further define the relationship
between ADHD, sleep problems, and patterns of electronic device usage in primary schoolchildren.
Methods: A high SES private school and a low SES public school were selected as locations to
implement the study. DSM IV-ADHD Rating Scale was introduced to determine students with potential
ADHD. A mean item response of the scale greater than 1.25 was accepted as possible ADHD. A
sociodemographic questionnaire was also filled out by the parents of all 2-4th grade students at the
selected schools.
Results: Response rates were 369 (73.8%) and 175 (35%) at the public school and the private school,
respectively. Mean age was 9.13 0.93 and 262 (48.2%) were females. The prevalence rate of ADHD
was 9.0%. Potential presence of ADHD did not show variance according to SES variables. Existence of
sleep talking, bruxism, night terror, difficulty awakening from sleep in the morning (p<0.05), and
restless sleep (p<0.001) were significantly higher in ADHD group. 25.6% of ADHD group watched more
than 6 hours of television dail in contrast to10.1% controls. Parents of ADHD group complained more
about convincing their children to stop spending time on the computer (25.8% vs. 7.4%; p=0.001).
Discussion: This study demonstrates that 1 out of 10 primary school students potentially suffers from
ADHD. A two-sided relationship appears to exist between potential ADHD occurrence and both sleep
disorders and television - computer usage patterns. While research so far has shown the prevalence of
ADHD to be higher among males and individuals of lower SES, a statistically significant relationship
was not observed in this study.
161
P 11
Association of the VAMP2, Synapsin 3 and Syntaxin 1A Genes
With Adult Attention Deficit Hyperactivity Disorder
Aye Nur Inci Kenar*, Hasan Herken, M. Emin Erdal, Tuba Gkdoan Edgnl
Denizli State Hospital Psychiatry Clinic-denizli *pamukkale University Faculty Of Medicine And
Department Of Psychiatry-denizli **mersin University Faculty Of Medicine Department Of Medical
Biology And Genetics-mersin ***mula University School Of Health-mula
Introduction: Attention deficit hyperactivity disorder (ADHD) is a disorder that begins in childhood and
has main symptoms of inattention, overactivity and impulsivity. The etiology of ADHD has not been
entirely clarified yet. Structural and metabolic differences at the prefrontal striatal cerebellary system
and the interaction of gene and environment are the main factors thought to play a role in the etiology.
Genetic investigations are performed especially about the dopamine pathways and receptors.
Aim: In this study; it was aimed to investigate the association of the synaptobrevin-2 (VAMP2),
synapsin III and syntaxin 1A genes, which take place in encoding presynaptic proteins, with adult
attention deficit hyperactivity disorder.
Method: One hundred thirty-nine patients, having ADHD aging between 18 and 60 years and 106
healthy people as controls were included into the study. Blood samples were taken from the
participants and genetic analysis were performed.
Result: A significant difference was determined between ADHD and VAMP2Ins/Del polymorphism,
synapsin III-631 C>G polymorphism and syntaxin 1A intron 7 polymorphism according to the control
group. No significant difference was determined between ADHD and synapsin III-196 G>A
polymorphism.
Discussion: It is believed that dopaminergic genes together with synaptic protein genes might have
roles in the etiology of ADHD and functional defects at the parietal cortex and frontostriatal pathways
might interfere in this disorder.
162
P 12
Is Maternal Depressive Symptomatology Effective on Exclusive
Breastfeeding During Postpartum 6 Weeks?
Bilge Burak Annagur*, Ali Annagur, Akkz ahin, Rahmi rs, Fatih Kara
Seluk University, Faculty Of Medicine, Department Of Psychiatry- Konya
Introduction: Mood changes are common in the early postpartum period. The prevalence of
postpartum depression (PPD) ranges from 10% to 15% among women. However, depressive
symptoms may occur more than Major Depressive Disorder in postpartum period. PPD is significant
mental health problems that can have negative effects on mother-infant interactions. Researchers
show that depressed mothers are more likely to express behaviors that have a negative impact on their
children. Depressed mothers are also less sensitively attuned to their infants needs. Many authors
suggest that correlation between depressive symptoms and early termination of breastfeeding.
Researchers said that woman who were depressed prenatally were less likely to attempt to breastfeed
and to persist lactation.
Aim: The aim of this prospective study was to examine the relationship between exclusive
breastfeeding and postpartum depressive symptomatology. Our hypothesis was that mothers with
depressive symptoms initially, fail exclusive breastfeeding.
Methods: One hundred ninety seven mothers attended the study. The participants were interviewed
two times. The first visit was within the first 48 hours after birth. The Edinburgh Postnatal Depression
Scale (EPDS) was completed by the participants. The second interview performed 6 weeks.
Participants answered methods of breastfeeding for 6 weeks, any methodological problems and nipple
pain. EPDS was completed by the participants in 6 weeks. Newborns were term infant.
Results: All the participants divided into two groups as exclusive breastfeeding and mix-feeding (partial
breastfeeding and/or bottle feeding). Both groups were compared in terms of features, such as mode of
delivery, parity, prevalence of depressive symptomatology (at 48-h and 6 wk) and delayed onset of
lactation within first 48. Statistical significance was found for only two variables which delayed onset of
lactation within first 48-h and gestational age.
Discussion: Contrary to our expectation, effect of higher maternal depressive symptomatology was
not demonstrated on exclusive breastfeeding during 6 weeks after delivery. However, the important
finding of this study that delayed onset of nutrition within the first 48 hours affects negatively exclusive
breastfeeding during 6 weeks after delivery.
Conclusion: Clinicians especially should pay attention that lactation difficulty during the first week
postpartum. Early lactation difficulties are associated with greater risk of early termination of
breastfeeding and lower breastfeeding success.
163
P 13
Role of Mood and Impulsivity in Obese People With Binge Eating
Disorder
Bilge Burcak Annagur*, Fatma zlem Orhan, Ali zer, Nur Yaln Yetiir,
Lut Tamam
Seluk University, Faculty Of Medicine, Department Of Psychiatry- Konya
Intraduction: The incidence of obesity has increased dramatically in the past few decades. In addition
to genetic tendency, social, cultural, emotional and diet-related factors play important role in the
development of obesity. There are also high comorbidity rate between obesity and psychiatric
comorbidities. Especially, depression is well described in the literature. Moreover, Patients with
personality disorder, substance abuse, and attention deficit hyperactivity disorder (ADHD) are reported
to have higher prevalence rate of obesity. Characteristics related with eating disorders such as low self-
esteem, body dissatisfaction, perfectionistic attitude, impulsivity and disinhibition have also been
observed in obese patients.
Aim: The aim of study was to evaluate mood and impulsivity in obese people with binge eating
disorder. Method: A total of 149 obese subjects [71 with Binge Eating Disorder (BED) and 78 without
BED] were included in the study and compared to 151 non-clinical populations. They were assessed
with the Structured Clinical Interview (SCID-I), Eating Attitudes Test (EAT), Beck Depression Inventory
(BDI), and Barrat Impulsiveness Scale-11 (BIS-11).
Results: The ratio of obese subjects with BED is 47,6%. Obesity and BED prevalence was higher in
female patients. Childhood obesity was significantly more frequent in obese subjects with BED
(p<0.05). The history of admission to psychiatry clinics and the ratio of suicide attempt were more
frequent in obese group. The ratio sixty one of the 146 (41,2%) subjects with obesity had diagnosed as
depressive disorder according to DSM-IV criteria. Thirty three of 71 BED (46,5%) had diagnosed as
depressive disorder. There are no significant differences between BED(+) and BED(-) groups for
depression (p>0.05). Cognitive impulsivity and nonplanning activity scores of depressive group were
significantly higher than the subjects without depression. (p<0.05). Cognitive impulsivity scores of
depressive obese were significantly higher than the obese without depression (p<0.05).
Discussion: Obesity is strongly related with depression and impulsivity. Impulsivity was significantly
higher in depressive obese subjects than non-depressive ones. Futhermore, impulsivity was a
prominent feature in obese subjects with BED. This also provides clues for influences of each of these
two characteristics on obesity.
164
P 14
Intoxication With an Extreme Overdose of Extended-Release
Quetiapine
Mehmet Inta, Cemal Onur Noyan*
Diyarbakr Military Hospital, Department of Psychiatry, Diyarbakr. gmsuyu Military Hospital
department of Psychiatry, stanbul*.
Introduction: Quetiapine is an atypical antipsychotic with well established efficacy in the treatment of
patients with psychotic disorders. Quetiapine overdose is thought to be safer than other antipsychotics
but information about intoxications with extreme overdose of quetiapine is limited.
Aim: It's aimed to define effects of massive quetiapin XR overdose.
Method: In this article we report a case of intoxication with 36 g of extended-release (XR) quetiapine
ingested by a 21 year old male with a history of psychotic attacks due to substance abuse. He was
admitted to the Emergency Department because of unconsciousness due to intoxication and was taken
to the intensive care unit (ICU) after intubation for ventilatory support. Spontaneous breathing was
restored in 12 hours but he had tachycardia, hypotension, QT prolongation and hypothermia during the
next 3 days in the ICU. After 3 days of management with maintenance of hydration status and
electrolytic balance, he was fully recovered and taken to psychiatric service on the forth day without
any residual symptom.
Discussion: This report helps to define the effects of intoxication with an extreme overdose of
quetiapine XR and underlines the importance of close monitoring of these patients .
165
P 15
Ego-dystonic Auditory and Visual Hallucinations During
Isoretinonin Therapy
C. Onur Noyan*, Mehmet Inta**
*psychiatry Department Of Gumussuyu Military Hospital **psychiatry Department Of Diyarbakr Military
Hospital
INTRODUCTION: Isotretinoin, a vitamin A derivative, is a synthetic oral retinoid that has been widely
being used against severe, resistant and nodulocystic acne. Although the pharmacological mechanism
of isotretinoin is still dubious, its hypothesised that isotretinoin which binding to retinoid receptors that
concentrated in limbic areas including the amygdala, prefrontal cortex, and hippocampus has impact on
neurotransmitter systems that have been implicated in depression in particular dopamine but also
serotonin and norepinephrine. There have been numerous reports of adverse reactions that can be
severe and limit its use. Although preliminary reports revealed that isotretinoin significantly worsened
depression, subsequent researches indicates that isotretinoin carries out no further risk for depression
and anxiety. There is no consensus on a causal relationship between Isotretinoin therapy and mental
health problems.
CLINICAL PRESENTATION: A 21-year-old woman presented with ego-dystonic auditory and visual
hallucinations during the course of isotretinoin therapy (20-mg twice daily for 5 months) for severe,
nodulocystic acne. The patient admitted to our clinic for anhedonia, depressed mood and anxiety. After
detailed evaluation its understood that auditory and visual hallucinations are ego- dystonic and
appeared subsequently with initiation of isoretinoin, meanwhile depressive symptoms has begun at
fourth month of treatment. She has not any explicit complaining about hallucinations. The patient
indicated that she does not care about hallucinations because of there is written on the prospectus that
hallucinations may be seen during treatment. Isotretinoin was discontinued and both auditory and
visual hallucinations has disappeared.
CONCLUSION: Although there is not any report on pubmed about purely hallucinations associated
isoretinoin treatment, but there are also many comments of patients about hallucinations on the internet
health forum sites. This side effect arises probably due to impact of isotretinoin on neurotransmitter
system. When evaluating patients taking isotretinoin, clinicians should be cautious especially for
unspecified psychiatric symptoms like mood and behavioral changes which may not be reported by the
patient. Detailed anamnesis and use of psychometric scales can facilitate the identification of
individuals prone to mental health problems during isotretinoin therapy.
166
P 16
Restless Legs Syndrome Induced By Quetiapine
C. Onur Noyan*, Gener Gen
*Psychiatry Department Of Gumussuyu Military Hospital **Neurology Department Of Mareal akmak
Military Hospital
OBJECTIVE Restless legs syndrome (RLS) is a sensory motor disorder characterized by irresistible
urge to move and unpleasant sensations in the legs. The RLS symptoms begin or worsen during
inactivity periods, especially in the night, and a temporary relief occurs by limb movements. Its
hypothesized that RLS is associated with central dopaminergic dysfunction. We report a case of drug
induced RLS caused by quetiapine. The objective of this case report is attracting attention to the
differentiation of psychotropic drug induced RLS from akathisia
CLINICAL CASE: A 35-year-old woman patient taking escitalopram 20 mg/d for 10 months admitted to
the psychiatry service for her depressed mood and sleep problems. After assessments quetiapine 12,5
mg/d added to the antidepressant therapy for augmentation. After initiation of quetiapine patient
complained of uncomfortable and irritated sensations in both legs that relieving with moving the legs.
RLS arised within 24 hours and resolved after immediately ceasing quetiapine.
CONCLUSION: RLS treatment begins with the elimination of triggering factors. Dopaminergic
dysfunction is considered to be a pathophysiologic mechanism of RLS. Drugs that block dopamine
receptors are likely to induce RLS. Patients taking psychotropic drugs and have complaint for sleep
disturbances and discomfort in the lower limbs should be carefully investigated for RLS and should be
differentiated from akathisia that there is an urge to move the whole body without uncomfortable
sensations.
167
P 17
Hyponatremia During Clozapine Treatment in Schizophrenia: A
Case Report
C. Onur Noyan*, Levent Emirzeolu**
*psychiatry Department Of Gumussuyu Military Hospital **Oncology Department Of haydarpasa
Military Hospital
INTRODUCTION: Hyponatraemia defined as a decrease in serum sodium below 136 mmol/L is rarely
seen but clinically important entity that can cause severe complications. Most of the patients with
serum sodium level above 125 mmol/L are asymptomatic and do not require treatment. There have
been many reports that psychotropic drugs including antipsychotic, antidepressant and antiepileptics
can cause hyponatremia. Hyponatremia accompanying psychiatric patients almost always occurs in the
presence of primary polydipsia. Its assumed that Clozapine is the only antipsychotic that reduces the
risk of hyponatremia. It is unclear whether clozapine improves water excretion or just diminishes intake.
Our case represents clinically asymptomatic hyponatremia observed in schizophrenic patient taking
clozapine.
CLINICAL CASE: We report a 40-year-old male patient suffering with schizophrenia for twenty years
and taking clozapine 300 mg/d for approximately 12 years without any complications. During the
haematologic evaluation routinely being carried out when prescribing clozapine, hyponatremia
(Sodium:128 mmmol/L) observed and confirmed by repeated measurements. Lability in blood pressure
was the only clinical symptom. The patient referred to the internal medicine specialist and thereafter
any possible aetiological factors to explain hyponatremia could not be shown. For lability in blood
pressure antihypertensive medication was started but serum sodium level did not change remarkably.
After the detailed interview with caregivers, information about the increase in water intake for last one
year was striking. As a result, we decided that excessive water intake was the only cause of
hyponatremia with no known medical conditions in the aetiological background. With restriction of fluid
intake and new antihypertensive medication serum sodium level has been normalised within 2 months
and any decrease did not be observed during the subsequent measurements for one year.
CONCLUSION: We think that in our case report, hyponatremia was induced by increase in water
intake. Effects of clozapine in our case which reported previously as the only antipsychotic reducing the
risk of hyponatremia is controversial. Clinicians must carefully evaluate the patient with hyponatremia
associating clozapine use for especially excessive water intake with information obtained from
caregivers. Further studies are required to establish the risk factors associated with antipsychotic-
induced hyponatremia.
168
P 18
The Importance of Pseudocholinesterase Deficiency in
Electroconvulsive Therapy (ect)
Cagatay Karsidag, GokselYuksel, Nihat Alpay
Bakirkoy Mental Hospital For Psychiatry And Neurological Science
Aim: Unlike the common belief, the modified ECT (ECT madeunderanestheasia)is safe, effective and
well tolareted. In this treatment complications are rare. In the literatre the rate of the complications in
ECT is %0.09. One of these important complications is prolonged apnea. Most of the complications are
also composed of prolonged apnea. In the modified ECT the prolonged apneas can results from
conjenital or acquired seudocholines the rasedeficiency, as well as the int ake of drugs or substances
with or without homisidal, suisidalintention.
Result: In this review we evaluated there as on and results of pseudocholinesterased eficiency.
169
P 19
Neurobiology of Violence Behavior
Cagatay Karsidag*, Armagan Ozdemir*, Nihat Alpay*, Nesrin B. Tomruk*,
Umut Mert Aksoy*
* Bakirkoy Mental Hospital For Psychiatry And Neurological Science stanbul/Turkey
Violence is kind of behavior which intended to harm another person by verbay, physical or indirectly
ways. Aggression located in the basis of violence. When a person feel him or herself in danger,
naturally runs away or attact. In other words, violence have a definite function for the survival of human
beings. Violence is generally the final product. It needs to a stimulus for initiation; a mind for processing
and a body for implement it. According to experimental research and case examples functional
problems in the area of frontal lobe, hypothalamus, limbic system brain structures, neuromediator such
as serotonin, dopamine, noradrenalin and hormonal factors such as natural opioids, cortizone and
testosterone may take parts the violence behavior. Emotions and behavior which related with
aggression seem to be associated with the limbic system. It is considered that repertoire of emotional
behavior, including anger and aggression in human beings, programming by genetic basis. However,
the interaction between the prefrontal cortex, amygdala and hypothalamus shows great influence on
the social behavior. Yet in violent behaviors, it is seen deterioration in the balance between these
systems
170
P 20
Functional Connectivity Via FMRI in Response to High-Calorie
Food Cues in Obese Persons With Binge Eating Disorder
Deniz Atalayer,
1,2
Spiro Pantazatos,
1
Lauren Puma,
2
Allan Geliebter
1,2
1
Columbia University, New York, NY;
2
St. Luke's-Roosevelt Hospital, New York, NY
Background: Binge eating disorder (BED) is described as consumption of excessive food quantities in
short time periods, with loss of control and lack of compensatory behaviors which may lead obesity.
Although the psychological, physiological and behavioral aspects of binge eating have been
investigated to a great extent, the neural underpinnings of BED are yet to be studied.
Methods: In this study, we examined the functional neural connectivity with amygdala --a key
emotional processing area, in response to high energy-dense (ED) vs. low-ED visual (pictures) and
auditory (spoken word) food cues in obese subjects with BED vs. obese healthy controls in both fasted
and fed states. Functional magnetic resonance imaging (fMRI) was used to determine functional neural
connectivity A psychophysiological interaction analysis was conducted using a amygdala as the seed
region. Obese (BMI=36.55; mSD) subjects (BED=17; control=14) participated in the study.
Results: When fasted, in response to visual cues for high-ED vs. low-ED foods, obese subjects with
BED showed greater functional connectivity with amygdala in bilateral supplementary frontal motor
areas, bilateral primary motor areas, and posterior cingulate compared to obese controls. During the
fed state, in response to auditory cues for high-ED vs. low-ED foods, obese subjects with BED showed
greater functional connectivity with amygdala in middle cingulate gyrus.
Conclusion: These results suggest that, when fasted, in response to high-ED vs. low-ED food cues,
obese persons with BED have greater functional interactivity between motor planning/execution
regions with emotion-related areas than obese persons without BED. These findings may begin to
elucidate the neural substrates of the emotional component of binge eating in obese individuals.
However, the directionality of the association will require further investigation.
171
P 21
Nasu Hakola Disease : A Case Report Which is Characterized By
Presenil Dementia and Bone Fractures
Derya Ipekiolu, Nesrin Karamustafalolu, Nazan Karagz Sakall, zlem
etinkaya, Mehmet Cem Ilnem
Bakirky Mental Hospital
Introduction: Nasu-Hakola Disease is a rare autosomal ressesive disease. It is described by Nasu
and Hakola separately in 1970s. It is mostly seen in Japanesee and Finns populations. It is a genetic
disease which causes presenil dementia. Its characterized with progressive frontal dementia and
systemic bone cysts. The clinical progress is divided into 4 stages. 1- Latent stage: asymptomatic until
early adulthood 2- Osseos stage: 2. and 3. decads in which sensitiveness, eudemia and pain occur in
wrists and ankles after hard physical exercise. Fractures can occur after minor traumas. 3-Early
Neurologic stage (Neuropsychiatric stage) : Signs of disease begin to appear in 3. and 4. decads.
Progressive frontal dementia becomes clear in this stage. Euforia, loss of social inhibition, personality
alterations, behavioral disorders, loss of insight, memory losses, agnosia,apraxia and broca afazia can
be seen. 4-Late Neurologic stage (Dementia Stage): characterized with late stage dementia and loss of
mobility. Mostly patients die before 50. Pathogenesis is unknown. There are some hypothesis about
vascular damage and systemic lipid metabolism abnormallities. Dap 12 and TREM2 are genes which
are associated with the disease. Case report: We report a man with progressive dementia and bone
fractures. Bilateral putaminal calsifications in Cranial CT, enlargement in cerebral cortical sulcuses and
lateral ventricules in brain MRI, loss of trabecular bone and cystic areas in bilateral knee CT are
determited. n Neuropsychological tests there is widespread cognitive decline which is characterized
with findings asossiated with frontal axle. After imaging, laboratuary and clinical findings the cases is
diagnosid as Naku-Hakola Disease.
Discussion: Diagnosing this disease which is rare and cause presenil dementia, help clinician to solve
social and economical problems during the course of disease.
172
P 22
Effect of Cigarette Smoking on Insulin Resistance Risk
Haj Mouhamed D1,2, Ezzaher A1,2, Neffati F, Douki W1,2, Gaha L2, Najjar Mf1
1- Laboratory Of Biochemistry-toxicology, Monastir University Hospital, Monastir 5000, Tunisia 2-
Research Laboratory "vulnerability To Psychotic Disorders Lr 05 Es 10", Department Of Psychiatry,
Monastir University Hospital, Tunisia.
Introduction: Smoking is one of the main risk factors for cardiovascular disease (CVD). The
mechanism(s) for the effects of smoking on CVD are not clearly understood; however, a number of
atherogenic characteristics such as insulin resistance have been reported.
Aims: We aims to investigate the effects of cigarette smoking on insulin resistance and to determine
the correlation between this parameter with smoking status characteristics (number of cigarettes
smoked/day and consumption duration) and the biological tobacco markers, plasma thiocyanate and
urinary cotinine.
Methods: This study was conducted on 138 nonsmokers and 162 smokers aged respectively
35.5516.03 and 38.4721.91 years. All subjects are not diabetics. Fasting glucose was determined by
enzymatic methods and insulin by chemiluminescence method (Elecsys 2010TM Roche diagnostics).
Insulin resistance (IR) was estimated using the Homeostasis Model of Assessment equation: HOMA-IR
= [fasting insulin (mU/L) fasting glucose (mmol/L)] /22.5. IR was defined as the upper quartile of
HOMA-IR. Values above 2.5 were taken as abnormal and reflect insulin resistance.
Results and Discussion: compared to non-smokers, smokers had significantly higher levels of fasting
glucose (6.17 0.9 Vs 4.2 1.5 mmol/L; p =0.001), fasting insulin (24.19 2.26 Vs 14.30 1.17
mUI/L; p < 10-3) and HOMA-IR index (5.1 4.9 Vs 2.6 1.1; p < 10-3). A statistically significant
association was noted between the smoking status parameters, including both the number of cigarettes
smoked/day (F3161 = 7.5; p = 0.001) and the duration of smoking (F3161 = 1.87; p = 0.04), and
fasting insulin levels as well for HOMA-IR index (F3161 = 7.5; p < 10-3; F3161 = 1.87; p = 0.04;
respectively). Among smokers, we noted a positive correlation between HOMA-IR index and both
plasma thiocyanates (r = 0.437) and urinary cotinine (r = 0.580). Conclusion: The findings show that
smokers have a high risk to developing an insulin resistant, hyperinsulinaemic, compared with a
matched group of non-smokers, and may help to explain the high risk of cardiovascular diseases in
smokers.
173
P 23
Music and Dementia Patients: The Effects on Agitated
Behaviors: A Review of The Litareture
Elcin Babaoglu Akdeniz
Maltepe University health Sciences Institute school Of Nursing
INTRODUCTION Dementia is a form of Alzheimers disease is estimated to effect approximately over
24 million people on the world. Dementia is associated with behavioral symptoms as well as cognitive
impairment. Dementias may affect a large number of functions. Those are emotional state and
perception; cognition, memory and linguistic capacities; and level of anxiety and agitated behaviors.(1,
2) Agitation has been defined as an inappropriate verbal, vocal or motor activity that is not explained by
needs or confusion. Agitation is caused by neurological, physical, psychological, functional,
interpersonal relation, environmental and restraints factors. Pharmacological interventions are
commonly provided to decrease the agitation of older adults with dementia. Some pharmacological
interventions are reported to precipitate agitation in this populationthose interventions are reported to
have adverse effects such as worsening of cognitive function, extra-pyramidal symptoms. Therefore,
non pharmacological interventions have fewer risks. Many researchers have explored the effects of
non pharmacological interventions on decreasing agitation in dementia. Those interventions are
aromatherapy, thermal bath, hand massage, pet therapy, rocking chair therapy, therapeutic
recreational activities, light therapy, behavior management therapy and music (3, 4, 5, 6, 7, 8). Three
dominant groups of symptoms of dementia, which have been suggested to be positively influenced by
music, form the focus of the current discussion: autobiographical memory and language retention;
mood and depression; and aggression and agitation (3, 8, 9, 10).
AIM: The purpose of this study was so systematically review the literature regarding the effectiveness
of music for agitation in older adults with dementia.
METHOD: 3 electronic databases were searched and randomized clinical trials employing
nonpharmacologic interventions for agitation in dementia. The computerized CD-ROM indexes of allied
health (CINAHL), medical (MEDLINE) and psychological (PSYCHLIT) literature from 1980 to 2011
were searched and using the keywords Music and Music Therapy, Dementia and Agitation. The
database searches were limited to articles published in English or Turkish. Abstracts of potentially
eligible studies were reviewed and full text papers were pulled to determine eligibility. The main
outcome was the study specific measure of the effects of music on agitation of dementia patients.
RESULTS: About 35 of 253 articles were identified as eligible. This articles presents the use of music
listening as an effective, noninvasive intervention designed to assist in creating healing environment to
promote health and well being, music has demonstrated effectiveness in reducing pains, decreasing
anxiety, and increasing relaxation. The purposes of these studies are to examine by the use of music
affects agitated behavior in persons with dementia. Music and music therapy may benefit patients
physiologically, psychologically and socio emotionally. Direct physiological effects, in animals, music
changes neuronal activity with entrainment to musical rhythms in the lateral temporal lobe and in
cortical areas devoted to movement. Steady rhythms entrain respiratory patterns. Listening to classical
music increases heart rate variability, a measure of cardiac autonomic balance. In students engaged in
stressful tasks, lower salivary cortisol levels are noted in listening to noise or rock music compared with
control subjects, whose cortisol levels increased. Music affects mu opiate receptor expression,
morphine-6 glucuronide, and interleukin-6 levels in healthy volunteers (11, 12, 13). Human
neuroimaging studies have demonstrated that musical stimuli elicit strong positive or negative
emotional responses activate limbic and paralimbic areas involved in affective processing. In one
study, non-musicians listened to simple, experimenter designed chordal melodies that varied
parametrically in the degree of harmonic dissonance and unpleasentness and rated the emtotional
valence and intensitiy of their response subject dissonance ratings correlated positively with activations
in the parahippocampal gyrus and precuneus and correlated negatively with activations in the
orbifrontal cortex, subcallosal cingulated and ventromedial prefrontal cortex . In a second study,
subjects listened passively to well-loved music that they had slected for their shiever-inducing
properties. The intensitiy of subjects chills while listening to their favorites, when contrasted with
listening to other pieces of music, was correlated with brain activations in the nucleus accumbens,
orbifrontal cortex, and ventromedial prefrontal cortex, areas involved in the processing of rewarding
174
emotions. There was activations in bilateral insula, anter,or cerebellum, anterior cingulated, midbrain,
ventral striatum, thalamus, bilateral amgydala, hippocampus, visual cortex and supplemanetary motor
area. (14, 15)
DISCUSSION An explanatory framework for the development of agitation in persons with dementia has
been proposed in the Progressive Lowered Stress Threshold model (hall, buckwalter). This model
showed that as the level of dementia increases, the threshold between baseline behavior and agitated
behavior decreases. Incremental mpairment of brain areas that integrate sensory and cerebral input
places the person at greater risk for agitated behaviors. The amount and intensity of stressors
contribute to the overall risk for agitated behavior. According those model predicts despite impaired
brain function, calm, baseline behavior can be maximized by modifying environmental stimuli and
controlling for factors that correlate with the perception of stressors. The stress response can be
altered to achieve functionally adaptive behavior by structuring a more supportive environment that
compensates for the decreased cognitive abilities of persons with dementia. This model suggests
Music may be effective calming strategies in the face of progressive cognitive impairment resulting
from dementia. Music could be a modality useful in reducing negative environmental stimuli, which are
perceived as stressful and can lead to agitated behaviors in persons with dementia. Music may alter an
individuals perception of environmental stressors by redirecting attention from multiple environmental
stimuli to a soothing tactile stimulus. Although the areas of the brain that integrate sensory and cerebral
input are affected early in the disease, the amygdale, which is located in the limbic system and
regulates perceptions and responses to emotion, remains intact until late in the course of dementia.
Music has been proposed to alter the stress response by two mechanisms: an endocrine response or a
sympathetic neural response. In the first mechanism, corticotrophin releasing hormone is secreted from
the hypothalamus, which decreases adrenocorticotropic hormone release and results in a decrease in
plasma cortisol levels.when the sympathetic nervous system responds to stress, the locus ceruleus
stimulates norepinephrine release from nerve terminals and epinephrine release from the adrenal
medulla, with resultant increases in blood pressure, heart rate, and anxiety. Neural impulses initiated
by music may mediate the release of stress hormones or decrease neural activity in the sympathetic
nervous system (16, 17, 18, 19). In regard to practice, this systematic review suggested sensory
interventions might be important practical interventions for agitation in older adults with dementia in
terms of significant effect, ease of performance, low cost and safety. Given that agitation is the most
frequently manifested behavioral symptom of elders with dementia and increases with the progress of
dementia, effective nonpharmachological interventions may contribute to the improvement of the
quality of life of these elders and their caregivers.
REFERENCES
1. Ballard, C.G., Margallo-Lana, M.,Fossey, J., Reichelt, K.,Myint, P.,Potkins, D., et al. (2001). A 1-year
follows up study of behavioral and psychological symptoms in dementia among people in care
environments. Journal of Clinical Psychiatry, 62 (8), 631-636
2. Omar, R.,Hailstone, J.C., Warren, J.E., Crutch, S.,J., &Warren, J.D. (2010).The cognitive
organization of music knowledge: A clinical analysis. Brain, 133, 1200-1213
3.Kong. E.(2005). Agitation in dementia: Concept clarification. Journal of Advanced Nursing, 52 (5),
526-536
4. Ryden, M.B., Feldt, K.S., Oh, H.L., Brand, K.,Warne, M.,Weber, E., et al. (1999). Relationship
between aggressive behavior in cognitively impaired nursing home residents and use of restraints,
psychoactive drugs and secured units. Achieves of Psychiatric Nursing, 13 (4), 170-178
5. Talerico, K.A., Evans, L.K.,&Strumpf, N.E. (2002). Mental Health correlates of aggression in nursing
home residents with dementia. The Gerontologist, 42 (2), 169-177
6. Schneider, L.S., Dagerman K., & Insel, P.S. (2006). Efficacy and adverse effects of atypical
antipsychotics for dementia: Meta-analysis of randomized, placebo controlled trials. American Journal
of Geriatric Psychiatry. 14 (3), 191-210
7. Livingston, G., Johnston, K., Katano, C., Paton, J., &Lyketsos, C.G. (2005). Systematic review of
Psychological approaches to the management of neuropsychiatric symptoms of dementia. The
American Journal of Psychiatry, 162 (11), 1996-2021
8. Mc Gonigal-Kenney, M.L.,& Schutte, D.L. (2006). Nonpharmacologic management of agitated
behaviors in persons with Alzheimer disease and other chronic dementing conditions. Journal of
Gerontological Nursing, 32 (2), 9-14
9. Cohen-Mansfield, J. (2001). Nonpharmacological interventions for inappropriate behaviors in
dementia: a review, summary, and critique. American Journal of Geratric Psychiatry, 9(4), 361-381.
10. Cohen-Mansfield, J., & Billig, N. (1986). Agitated behaviors in elderly. I.A. conceptual review.
Journal of the American Geriatrics Society, 34 (10), 711-721.
11. Umemura M, Honda K.(1998). Influence of music on heart rate variability and comfort: a
consideration through comparison of music and noise. J Hum Ergol , 27:30-38
175
12.White JM. (1999). Effects of relaxing music on cardiac autonomic balance and anxiety after acute
mycordial infarction. Am J Crit Care, 8:220-230
13. Khalfa S., Bella SD, Roy M, et al. (2003) effects of relaxing music on salivary cortisol levels after
psychological stress. Ann N Y Acad Sci, 999:374-376.
14. BloodA.J., Zatorre R.J., Bermudez, P &E vans A.C. (1999) Emotional responses to pleasant and
unpleasant music correlate with activity in paralimbic brain regions. Nature Neuroscience, 2:382-387
15. Peretz, I., Blood A.J.,Penhune V.,& Zatorre R.J. (2001) Corticol deafness to dissonance,
Brain:124:928-940
16. Hall, G.R. (1994). Caring for people with Alzheimer disease using the conceptual model of
progressively lowered stress threshold in the clinical settings. Nurisng Clinics of North America, 29,
129-141
17. Hall, G.R.,&Buckwalter, K.C. (1987). Progressively lowered stress threshold: a conceptual for care
of adults with Alzheimers disease. Archieves of Psychiatric Nursing, 1, 399-406
18. Hall, G.R.,&Buckwalter, K.C., Stolley, J.M.,Gerdner, L.A., Garand, L., Rideway, S. et al. (1995).
Standardized care plan: managing Alzheimers disease at home. Journal of Gerontological Nursing, 21
(1), 37-47
19. Zeisel, J.&Raira, p. (2000). Nonpharmacological treatment for Alzheimers disease: a mind-brain
approach. American Journal of Alzheimers Disease and other dementias, 15, 331-340
176
P 24
Phenotype-genotype and Conventional Therapeutic Doze
Monitoring (tdm) Relationship: A Case Report.
Esra Saglam *, Selma zilhan *, Fadime Canbolat *, Nevzat Tarhan *
* Uskudar University, Neuro-psychiatry Istanbul (npi) Hospital, Department Of Pharmacogenetics-
istanbul
ntroduction: Three clinical techniques are still in use to optimize the patients pharmacotherapy.
These techniques are genotyping, phenotyping and Therapeutic Dose Monitoring (TDM). The
development and prospects of TDM and genotype, phenotype analysis as aids in personalized
treatment with antidepressants and antipsychotics are described. Emphasis is put on the usefulness of
TDM combined with genotype, phenotype analysis of cytochrome P450 2D6 (CYP2D6), the key
enzyme involved in the polymorphic metabolism of the majority of antidepressants (both tricyclics and
selective serotonin reuptake inhibitors) and antipsychotic drugs. This combination of methods is
particularly useful in verifying concentration-dependent adverse drug reactions (ADRs) due to poor
metabolism, 'and diagnosing pharmacokinetic reasons (ultrarapid metabolism (UM)) for drug failure.
This is because ADRs may mimic the psychiatric illness itself and therapeutic failure due to UM may be
mistaken for poor compliance with the prescription.
Aim: To with three clinical techniques genotyping, phenotyping and TDM to a psychytric patient.
Method: A 25-yr-old man was hospitalized psychosis. His body weight was 75 kg and he was 175 cm in
height Results of routine laboratory tests were normal. Supportive psychotherapy was also provided.
CYP2D6 genotype was determined with real-time and conventional PCR CYP2D6 fenotype was
determined with dextromethorphan test. Serum concentrations were measured with Liquid
chromatographyMass Spectrometry (LLC-MS/MS )
Results: CYP2D6 genotype was extensive drug metabolizing (EM) CYP2D6 fenotype was ultrarapid
drug metabolizing (UM) The plasma drug concentrations: after 10 days of treatment, mirtazapin 20
mg/day was 14.08 ng/mL (therapeutic range: 40-80 ng/mL), paroksetin 120 mg/day was BQL (<6.22 9
ng/mL) (therapeuticrange: 70-120 ng/mL), poliperidon 40 mg/day was BQL (<5.94 ng/mL) (
therapeuticrange: 20-60 ng/mL). The plasma drug concentrations were fit with fenotype, but the plasma
drug concentrations and fenotype were discordant genotype.
Discussion: The present study demonstrates that serum concentrations of antidepressants and
antipsychotic drugs in psychiatric patients were significantly affected by CYP2D6 fenotype. Detecting
genetic variations by genotyping in drug metabolizing enzymes, is useful to determine enzyme activity
but not efficient alone because the enzyme activity is affected by other factors as environment, diet,
smoking. Fenotyping provides an important advantage for investigations of the influence of CYP2D6
activity on drug therapy and its association with certain diseases. A patient with a CYP2D6 ultrarapid-
metabolism phenotype supports the potential usefulness of the drug therapy. Determination of
phenotype in elucidating serious adverse drug reactions and in preventing subsequent inappropriate
selection or doses of drugs.
177
P 25
Phenotype Compare With Conventional Therapeutic Doze
Monitoring (tdm) at Psychiatric Patients
Esra Saglam*, Selma zilhan*, Fadime Canbolat*, Nevzat Tarhan*
*uskudar University, Neuro-psychiatry Istanbul (npi) Hospital, Department Of Pharmacogenetics-
Istanbul
Introduction: Psychiatric disorders contribute significantly to worldwide morbidity and mortality.
Forecasts to 2020 rank depression second only to ischemic heart disease. Pharmacotherapy is the
mainstay of antidepressants and antipsychotics treatment, but it is often associated with inadequate
response and severe side effects. Since the identification of all the major drug-metabolising
cytochrome P450 (CYP) enzymes and their major gene variants, pharmacogenetics has had a major
impact on psychotherapeutic drug therapy. Variability in CYP activity may be caused by various factors,
including endogenous factors such as age, gender and morbidity as well as exogenous factors such as
co-medication, food components and smoking habit. CYP2D6 is one the most important member of
Cytochrome P450 family which catalyses the metabolism of a large number of clinically important drugs
including antidepressants, neuroleptics, antiarrhythmics, lipophilic beta-adrenoceptor blockers and
opioids. TDM is a valid tool to optimise pharmacotherapy. TDM allows the prediction of the
metabolising phenotypes with high accuracy. Therefore, in our psychiatric clinic TDM is routinely
performed for all our hospitalised patients, and patients would benefit from a tailor made dosage.
Aim: To compare with the patient's drug serum concentrations with CYPD6 fenotypes
Method: In 49 patients treated with antipsychotics and antidepressants that to metabolised CYP2D6.
CYP2D6 genotype was determined with real-time and conventional PCR CYP2D6 fenotype was
determined with dextromethorphan test. Serum concentrations were measured with Liquid
ChromatographyMass Spectrometry (LLC-MS/MS ) Results: CYP2D6 fenotype and plazma
concentrations studied 49 psychiatric patients. At 44 patiens, plazma concentrations were fit with
fenotype, but 5 patiens, plazma concentrations were not fit fenotype.
Discussion: The present study demonstrates that serum concentrations of antipsychotics and
antidepressants drugs, that to metabolised CYP2D6, in psychiatric patients are significantly associated
with CYP2D6 fenotype. .Further prospective studies, showing a direct correlation between predictive
fenotyping and serum concentrations of antipsychotics and antidepressants drugs.
178
P 26
Clinical Efficacy of Hydroethanolic Extract of Hypericum
Perforatum in Patients With Hypertension and Concomitant
Depression
Fatemeh Ranjbar *, Fatemeh Fathi Azad, Fariborz Akbarzadeh, Keivan Shirzadi,
Amirhossein Akbarzadeh, Fahimeh Kazemi Nava
Tabriz University Of Medical Sciences, Clinical Psychiatry Research Center*, Tabriz, Iran
Introduction: Hydroethanolic extract of hypericum perforatum (HEE) has antidepressant effect with
low side effect.
Aim: The aim of this research was to study the clinical efficacy of HEE in patients with hypertension
and concomitant depression.
Method: In this double blind randomized control trial study 60 mild to moderate hypertensive patients
with concomitant mild to moderate depression in beck depression inventory enrolled. The patients were
randomly divided into two intervention and comparison groups. For 4-6 weeks the intervention group
was given HEE 200 mg/day and comparison group was given placebo. The patients were evaluated
with beck depression inventory and tonoport the end of 6th week. Then the results were analyzed
statistically.
Result: There was no significant difference between intervention and comparison groups between
systolic and diastolic blood pressure respectively Pv= 0.796, Pv= 0.654, but there was significant
difference between two groups considering beck depression inventory on depression Pv= 0.004.
Discussion: HEE can improve mild to moderate depression in hypertensive patients but no effect on
mild to moderate hypertension in depressive patients.
179
P 27
Night Eating Syndrome Among Patients With Depression
Fatma zlem Orhan, Ufuk Gney zer, Ali zer, zlem Altunren,
Mustafa elik, Mehmet Fatih Karaaslan
* Kahramanmaras Sutcuimam University Medical Faculty, Psychiatry Department, Kahramanmaras,
Turkey
** Anatolian Medical Centre, Family Medicine, stanbul, Turkey
*** Inonu University Medical Faculty, Department of Public Health Malatya, Turkey ****
Kahramanmaras State Hospital, Psychiatry Department, Kahramanmaras, Turkey
***** Kahramanmaras Sutcuimam University Medical Faculty, Family Medicine, Kahramanmaras,
Turkey
Introduction: Night eating syndrome (NES) is emerging as a potential candidate for a new eating
disorder diagnosis. It is characterized by a delay in the circadian pattern of food intake that is
manifested by evening hyperphagia (i.e., the consumption of 25% of the total daily food intake after
the evening meal) and nocturnal awakenings accompanied by the ingestion of food (2). The defining
features of NES have been identified as evening hyperphagia, morning anorexia, and sleep
disturbance (3). Aim: Symptoms of depression have been more frequent among individuals with NES
and the rate of NES in a population seeking treatment for psychiatric disorders is of interest. However,
as there is presently no study regarding the rate of NES in depressive patients, this descriptive study
was conducted to fill that research gap. The purpose of this study was to identify the rate of night eating
syndrome (NES) in a depressed population.
Method: The study sample was composed of 162 depressed patients and 172 healthy control
participants. Results: The rates of night eating in our sample with depression (35.2%) was higher as
compared with healthy control participants (19.2%) (p < .05). In addition, in the depression group, the
rate of NES-positive patients did not differ in accordance with body mass index (BMI) classification (p >
.05). However, in the control group, the rate of NES- positive patients was significantly different with
regard to BMI classification, and NES diagnosis was highest in the obese members of the control group
(p < .05). Multiple logistic regression analysis was then used to evaluate the relationships of four
variables depression, gender, education status and BMI with the diagnosis of NES. Results showed
that significant independent predictors of NES were depression ( = 2.64; p = .001; 95% confidence
interval = 1.52-4.57); male gender ( = 2.34; p = .002, 95% confidence interval = 1.37-4.03); and a BMI
of 25 or greater ( = 1.83; p = .022; 95% confidence interval = 1.09- 3.08). Discussion: This is the first
study to assess the rate of NES among individuals with depression in Turkey. The rate of night eating
in our sample with depression (35.2%) was higher as compared with previous studies that involved
psychiatric patients. Future studies are needed to replicate these findings, to understand why this
population is at increased risk for NES, and to determine the effects of NES on health outcomes among
individuals with depression.
References: 1. Stunkard AJ, Grace WJ, Wolf HG. The night eating 1. syndrome. JAMA 1955;19:78. 2.
OReardon JP, Ringel BL, Dinges DF, Allison KC, Rogers NL, Martino NS, et al. Circadian eating and
sleeping patterns in the night eating syndrome. Obes Res 2004;12:1789-1796. 3. Striegel-Moore RH,
Franko DL, Thompson D, Affenito S, May A, Kraemer HC. Exploring the typology of night eating
syndrome. Int J Eat Disord 2008;41:411-41
180
P 28
Sociodemographic Variables and Depression in Turkish Women
From Polygamous Versus Monogamous Families
Ali zer, Fatma zlem Orhan, Hasan etin Ekerbier
Malatya Inonu University Medical Faculty, Public Health, kahramanmaras Sutcuimam University
Medical Faculty, Psychiatry, kahramanmaras Sutcuimam University Medical Faculty, Public Health
Introduction: Polygamy has been defined as a marital relationship involving multiple wives.(1) A
senior wife is defined as any married woman who was followed by another wife in the polygamous
marriage. A junior wife is the most recent wife joining a marriage. (2) Polygamous marriage is often
associated with stress, tension, conflict, and disequilibrium in the family structure. Women in
polygamous marriages often experience various degrees of emotional difculties, including anger,
jealousy, pain, emotional distress, competition, loneliness, emptiness, unhappiness, and a lack of
intimacy with their spouse.
Aim: In this study, the authors aimed to determine the difference between the sociodemographic
variables of polygamous and monogamous wives and the extent of the relationship between
depression and polygamous marriage.
Methods: Seventy-nine polygamous wives and 73 monogamous wives were included in
Kahramanmaras, located in southern Turkey.
Results: The participants mean age was 40.310.4 years. The Beck Depression scores were above
17 in one third of the participants. About 8.2% of women from monogamous families, 58.1% of senior
wives, and 41.7% of junior wives had Beck Depression scores above 17; the scores were statistically
lower in women from monogamous families than the scores for the other two groups (p<0.05).The
women from polygamous families were 2.23 times more likely to have BDI scores of 17 or more than
women from monogamous families (OR=2.23, p<0.05). Additionally, women with a chronic disease
were 1.25 times more likely to have BDI scores of 17 or more (OR=1.25, p<0.05).
Discussion: The authors found significant differences in the Beck Depression scores between wives
in polygamous marriages and wives in monogamous marriages. In a recent Turkish study Ozkan (3)
found that participants from polygamous families, especially senior wives, reported more psychological
distress. Different from the previous studies, our findings indicate that senior and junior wives have
higher BDI scores than monogamous wives. Because there is no research on the depression scores of
Turkish women in polygamous and monogamous marriages and the role polygamous marriage plays in
depression, the results highlighted many implications for clinical practice for future research. It is
essential to increase awareness of the signicance of polygamous family structures among
psychiatrists and other therapists. References: 1. Low, B.S. (1988). Measurement of polygamy in
humans. Current Anthropology, 29, 189194. 2. Chaleby, K. (1985). Women of polygamous marriages
in inpatient psychiatric service in Kuwait. Journal of Nervous and Mental Disease, 173, 56-58. 3.
Ozkan, M., Altindag, A., Oto, R. and Sentunali E. (2006). Mental Health Aspects of Turkish Women
from Polygamous Versus Monogamous families. The international Journal of Social Psychiatry, 52,
214-220.
181
P 29
Anxiety And Serum Vitamin B12, Folate, TSH, And Ferritin Levels
in Telogen Alopecia Patients With Trichodynia
Perihan ztrk, Fatma zlem Orhan*, Ali zer, Yasemin Akman
Kahramanmaras Sutcuimam University, Medical Faculty, Department Of Dermatology,
Kahramanmaras kahramanmaras Sutcuimam University, Medical Faculty, Department Of Psychiatry,
Kahramanmaras inonu University, Medical Faculty, Department Of Public Health, Malatya
Introduction: Telogen alopecia is a common complaint and cause of significant emotional distress,
particularly in women. The best way to alleviate the anxiety is to treat hair loss effectively. It is critical to
address the symptoms systematically. Trichodynia (cutaneous dysaesthesia syndrome) is the term
given to the burning or stinging of the scalp related to diffuse alopecia. Increased rates of psychiatric
problems have been reported in patients with trichodynia.
Aim: The aim of this study is to measure the levels of serum ferritine, vitamin B12, zinc, folate, and
TSH and to evaluate the levels of anxiety of telogen alopecia patients with trichodynia.
Method: The study included 31 telogen alopecia patients who complained of trichodynia and 30
telogen alopecia patients without trichodynia. Their serum zinc, folate, ferritine, TSH, and vitamin B12
levels were assessed andtheir anxiety levels were evaluated using the Beck Anxiety Inventory (BAI)
and the State-Trait Anxiety Inventory (STAI).
Results: The mean age of the participants was 27.329.39 years for the patient group and 26.068.74
years for the control group. All participants were female. There was no significant difference between
the patient and control groups in terms of their serum folate, TSH, ferritine, zinc, and vitamin B12 levels
(P >0.05). There was also no significant difference in the BAI or the STAI form STAI-S and STAI-T
between the patient and controls groups (P>0.05). There was no statistically significant difference
(p>0.05) when comparing the anxiety scores of the patient and control groups. Severe anxiety was not
statistically significant, although in trichodynia higher than control group (P>0.05). There was no
correlation between serum ferritin, zinc, vitamin B12, and TSH levels and anxiety scores of the patient
and control groups.
Discussion: In this study, we found that trichodynia was not associated with serum levels of vitamin
B12, ferritine, folate, zinc, or TSH. Trichodynia was also not associated with anxiety. This result was
inconsistent with the results of other studies that found trichodynia was associated with anxiety. Our
experiment included homogeneous groups of females and studied telogen alopecia (excluding other
types of hair loss, such as androgenetic alopecia). Our results indicate trichodynia is not associated
with anxiety, serum zinc, ferritin, vitamin B12, folate, or TSH levels. More comprehensive, case-
controlled studies are needed to determine the other factors associated with trichodynia.
182
P 30
Assesment of Temperament and Character Profile in Patients
With Acne
Perihan Ozturk**, Fatma Ozlem Orhan*, Tugba karakas**, Ali Nuri Oksuz*, Nur
Yalcin Yetisir*
*Sutcuimam University, Medicine Faculty, Psychiatry Department.Kahramanmaras
**Sutcuimam University, Medicine Faculty, Dermatology Department.Kahramanmaras
Aim: Acne is the most common skin disease, affecting nearly 85% of the population as well as their
lives. Acne can severely affect social and psychological functioning. Patients with acnes may have
anxiety, depression, decreased self-esteem, interpersonal difficulties, unemployment, social withdrawal
and even suicidal intent. The aim of this study was to evaluate the temperament and character
inventory (TCI) of patients with acne and to compare the results with those of healthy controls. Material
metod: The study population consisted of 47 patients with acne (39 female,8 male), and 40 healthy
control subjects (18 female, 22 male). All participants were instructed to complete a self-administered
240-item TCI and the Hospital Anxiety and Depression Scale (HADS).
Findings: In this study, among the temperament properties HA, HA1, RD4 and among the character
properties C1, C5 scores were found to be higher in acne patients than in healthy controls (p<0,05).
There was no significant change in the other scales (p>0,05).Compared to the control group, in the
patients with acne, depression and anxiety scores, were found to be markedly higher. Acne type
correlated positively with Disorderliness (NS4) subscale of Novelty seeking and anxiety. Additionally
acne type correlated negatively with Reward Dependence (RD) and Attachment (RD3) subscale of
Reward Dependence (RD); Self-Trancendence (ST), Transpersonal identification (ST2) and Spiritual
acceptance (ST3) subscale of Self-Trancendence; Cooperativeness (C), Compassion (C4) subscale of
C.
Conclusion: Studies in this area may lead to the development of specific and focused interventions for
TCI in patients with acne vulgaris. We suggest that evaluation and treatment of acne should also
include psychosomatic approaches in clinical practice.
183
P 31
Dependence to Ketamine and Suicidal Behavior
Vsquez F*., Paima R, Crdova R., Nicols Y. Falcon S. Vite V.
National Institute of Mental Health Honorio Delgado-_Hideyo Noguchi / Lima- Peru
Introduction: Legal drugs are being used most frequently each time with recreative purposes to get
euphoric states by psychiatric patients , included those intravenous, like ketamine (local anesthetic) ,
with different consequences, not only dependence , but also suicidal behavior.
Aim: To study prevalence of dependents to Ketamine amongst suicide attempters assisted at NIHM
along 3 years.
Methods: Descriptive and prospective trial in suicide attempter patients who reported dependence to
ketamine, assessed by Suicide Prevention Programme team at National Institute of Mental Health,
following DSM IV- TR diagnostic criteria and also an Inventory for Substance Abuse, along 2009 to
2011.
RESULTS: From 2000 assessed patients presenting suicide attempt, 6 of them filled criteria for
ketamine dependence (0,3 %). These were only women, 3 of them (50 %) aged between 18 to 25
years old, and other 3 (50 %) between 26 to 33 years old; more than half self-administered
intravenous ketamine for at least 5 years. Most frequent diagnosis associated to ketamine dependence
was Major Depression Disorder in 5 of patients (83,3 %) and Bipolar Disorder in other one (16,6 %).
One of patients was diagnosed as Pott Disease of long lasting. In 5 patients they were found criteria
for Borderline Personality Disorder (83.3 %) ,also with Marijuana and alcohol dependence in 2 of them
(33,3 %). Previous suicide attempt was reported in 5 patients (83,3 %). Amongst these 6 patients with
ketamine dependence and suicidal behavior, most prevalent methods were: overdose of
benzodiazepines in 3 of them (50.0 %), wounds made by knives in 2 of them (33,3 %) and poisoning
in latter (16,6 %). One of patients (16,6 %) , finally died by suicide, while abstinence period to
ketamine, by jumping to a river.
Discussion: In this trial , prevalence of dependence to ketamine amongst suicide attempters looks
relatively low, although its occurrence carried out serious troubles, mostly in females, with early
beginning and fast association to great disorder like Major Depression, also to Borderline Personality
Disorder, and other psychoactive substance abuse. These magnitude of comorbidity increased suicide
risk and became lethal for one of them , specifically during abstinence period. Authors recommend
obligatory assessment of any substance abuse while evaluating whole suicide behavior.
References:
1. Vasquez F. et al (2007) Designing a profile of suicide attempter in National Institute of Mental
Health Lima Peru The Journal of the European Collegium of Neuropsychopharmacology Vol
17 Suppl 4 p.8.a O 19 Elsevier.
2. Morgan C., et al (2010) Consequences of chronic ketamine self-administration upon
neurocognitive function and psychological wellbeing: a 1-year longitudinal study, Addiction,
105 (1): 121-136
184
P 32
Transcranial Direct Current Stimulation in a Patient With
Shizoaffective Disorder Manic Episode
Gkben Hzl Sayar *, Celal Salcini, Ali Bayram, Gaye Kagan, Nevzat Tarhan
Uskudar University
AIM: Transcranial direct current stimulation is a noninvasive brain stimulation technique in which a
weak current is applied through the scalp to produce changes in neuronal excitability in the underlying
cerebral tissue. Recent clinical trials have shown promising results with left anodal prefrontal tDCS in
treating depression. The report investigates the answer for the question of whether tDCS can be
administered to manic episode patients
METHODS: Here we report the case of a 68-year-old female patient suffering from schizoaffective
disorder manic episode who underwent cathodal tDCS of the right dorsolateral PFC over 3 weeks as
an add-on treatment to a stable antipsychotic and mood stabiliser medication
RESULTS: tDCS over 4 weeks did exert clinically meaningful antimanic effects in this case. The
cathodal montage to right prefrontal area and anodal montage to left deltoid muscle appeared to be the
main contributory factor in the remission of manic symptoms.
DISCUSSION: This is the first report of tDCS treatment in manic episode and future studies need to
further explore this approach.
185
P 33
Transcranial Magnetic Stimulation During Pregnancy
Gkben Hzl Sayar*, Eylem Ozten, Emine Satmis, Gaye Kagan, Nevzat Tarhan
Uskudar University, Neuropsychiatry Istanbul Hospital
Transcranial magnetic stimulation (TMS) therapy is a non-invasive technique that delivers highly
focused magnetic field pulses to a specific portion of the brain. While TMS has its own limitations, it can
be quite effective for those of you who don't tolerate treatment with medications and aren't willing to
consider electroconvulsive therapy. The study population consisted of 7 pregnant females diagnosed
as major depressive disorder. The treatment schedule was six days in a week, with a total of 20
sessions. 25 Hz stimulation with the duration of 2 seconds was delivered 20 times with 30-second
intervals. A full course comprised 1000 magnetic pulses. The mean HAMD score for the study group
decreased from 22.595.92 to 10.505.83 (p<0.001) after 20 sessions of rTMS. Of these 7 patients, 5
demonstrated significant mood improvements and were classified as responders while 2 patients
reached remission status, with HAMD-17 scores less than 8, after rTMS. The newborns revealed no
abnormalities. Complete physical and neurologic examination, screening tests for phenylketonuria and
hypothyroidism, and hearing assessment was normal. None had congenital hip dysplasia, congenital
cardiac disease, cleft lip, or cleft palate. There were no gastrointestinal, pulmonary, or muscular
abnormalities. The proper treatment of mood disorders occurring during pregnancy is a major
therapeutic problem since no antidepressant medications have been established as safe for the
developing fetus. Apart from antidepressants, the most commonly used biological therapeutic method
is ECT (electroconvulsive therapy). We believe that similar efficacy can be achieved using rTMS as a
safer option with substantially less side effects.
186
P 34
Inutero Psychiatric Drug Exposure Resulted as Brachydactyly
Gken Yksel, aatay Karda
Bakirkoy Mental Hospital-istanbul
Introduction The possible teratogenic risks due to the medications used in the perinatal period
especially during pregnancy is still a big controversy. The use of antiepileptic drugs have the potential
to effect fetal development from the beginning of the fist trimester through birth. The exposure to
valproic acid during pregnancy especially in the first trimester is known to increase risk of spina bifida.
But when it comes to the risks of other congenital malformations the data is still limited and growing
evidence of adverse outcomes such as case reports make us understand the overall picture.
Case report Here in this case report we present a 24 years old mother known to have bipolar disorder
for five years and took valproic acid and aripiprazole until 6 weeks gestation when she realised and
ceased her medication. Hospitalised with the exacerbation of mania with psychotic features in 33
weeks gestation and gave birth to a babygirl with brachidactily in one hand in 39 weeks gestation with
C/S. The teratogenicity of drug exposure especially to VPA is discussed.
Discussion Contraception is also vital among these women to avoid the risk of unplanned and high
risk pregnancies. Clinicians must avoid polypharmacy and pay attention to the possibility of pregnancy
of the chronic psychiatric patients. The patients must be informed about the safety of the mood
stabilizers and antipsychotic drugs during pregnancy and breastfeeding. Although case reports
indicated that aripiprazole was not assosiated with teratogenicity it may cause lactation failure and
should be used carefully. VPA poses a higher risk of anatomic teratogenesis than other commonly
used antiepileptic and antipsychotic drugs. VPA should not be thought as the first line treatment for
women of child-bearing potential. If it is necessary to use it, dose should be limited as possible to avoid
the risks. Tapering the dose of any drugs to the minimum dose before delivery will be safe not only for
the mother but also for the baby
187
P 35
Tbars and Non-Enzymatic Antioxidants Markers in Schizophrenic
Patients
Hajer Mabrouk*, Ikram Houas, Haithem Mechria, Anouar Mechri, Wahiba Douki,
Lotfi Gaha,, Mohamed Fadhel Najjar
* Biochemistry-toxicology Laboratory. University Hospital Of Monastir. Tunisia, 5000.
** Research Laboratory vulnerability To Psychotic Disorders Lr 05 Es 10, Psychiatry Department.
University Hospital Of Monastir. Tunisia, 5000.
*** Psychiatry Department. University Hospital Of Monastir. Tunisia, 5000.
Objective: This study aimed to investigate the variations of the plasma TBARS levels (lipid
peroxidation marker) and of the non-enzymatic antioxidants (uric acid, bilirubin and albumin) and their
associations with the clinical and therapeutic characteristics in schizophrenic patients.
Patients and methods: Our case controls study included 121 schizophrenic patients and 88 control
subjects aged respectively 37.3 10.3 and 33.5 13,9 years. Lipid peroxidation was determined by
spectrophotometric method based on the reaction between malonedialdehyde (MDA) and thiobarbituric
acid (TBA). Plasma uric acid (UA) and total bilirubin (TB) concentrations were determined using Cobas
6000TM (Roche Diagnostics) and albumin levels were determined using Konelab 30TM equipment
(Thermo Electron Corporation).
Results: Compared to controls, patients had a not significantly increase in TBARS levels, significantly
higher levels of UA (270 68 vs. 220 73; p < 0.0001) and lower levels of TB (4.74 3.58 vs. 14.67
8.01; p < 0.0001). Furthermore, TBARS levels were significantly correlated with albumin. The highest
TBARS levels were noted in paranoid sub-type and in patients treated with typical antipsychotics, but
without significant differences. Moreover, the increase in UA was significantly more frequent in
schizophrenic patients than controls with a doubled risk.
Conclusion: considering increase of TBARS levels, UA and TB, schizophrenic patients have higher
risk of oxidative stress without association between these parameters and any clinical or therapeutic
characteristics. Therefore, such patients require specific care, particularly with regard to their
antioxidant status.
188
P 36
Homocysteine in Epileptic Patients
Saadaoui Mohamed Hachem*, Mabrouk Hajer, Chebel Saber, Hellara Ilhem, Neffati
Fadoua, Douki Wahiba, Frih-ayed Mahbouba, Najjar Mohamed Fadhel
* Biochemistry And Toxicology Laboratory, University Hospital Of Monastir ** Department Of
Neurology, University Hospital Of Monastir
Introduction Hyperhomocysteinemia is an independent cardiovascular risk factor and is implicated in
neurological and psychiatric diseases. However, several medical and nutritional factors can influence it.
We propose to study homocysteine levels in treated epileptic patients and the factors that may explain
its increase.
Patients and methods 103 epileptic patients (14 to 75 years, 61 women), treated with sodium
valproate (VPA) and/or carbamazepine (CBZ) and/or phenobarbital (PB), were recruited from
Neurology Department. 100 healthy controls were involved in the study. Homocysteine was determined
by fluorescence immunopolarisation (FPIA). Vitamin B12 and plasma folates were measured by MEIA
(Microparticular Enzymatic Immuno-Assay).
Results Homocysteine was significantly higher in patients than in controls (13,5 11,3 mmol/L Vs. 8,7
3,8 mmol/L, p < 0,001). No significant difference was demonstrated with folates and vitamin B 12.
Homocysteine was significantly increased in patients over 30 years (31 to 40 years: 14,0 11,1 mmol/L
and patients older than 40 years: 20,1 16,9 mmol/L Vs. 8,7 3,8 mmol/L, p < 0,01).
Hyperhomocysteinemia and lower plasma folates are more pronounced in smoking patients than in
smoking controls (p < 0,01). However, no significant difference was observed between smoking
patients and nonsmokers. In addition, subjects treated with enzyme-inducing antiepileptic drugs (CBZ
and/or PB) have higher homocysteine concentrations (16,8 14,1 mmol/L Vs. 8,7 3,8 mmol/L, p <
0,01) and lower folates (5,4 2,7 ng/ml Vs. 8,0 4,1 ng/ml, p < 0,01), while those treated only by
enzyme inhibitor drugs (VPA) have comparable values to controls.
Conclusion Homocysteine levels tend to increase in treated epileptic patients. Hyperhomocysteinemia
has been confirmed in patients treated with enzyme-inducing antiepileptic drugs. Antiepileptic treatment
may need to be added to other conventional parameters causing hyperhomocysteinemia.
189
P 37
Shared Obsessive Compulsive Disorder: A Case Report
Hakan Balibey*, Recep Tutuncu, Huseyin Gunay
Ankara Asker Hastanesi Psikiyatri Klinii, Etimesgut Asker Hastanesi Psikiyatri Klinii- Ankara
ntroduction: Folie a deux (shared psychotic disorder) is often described in the context of
schizophrenia. In this case report we present this syndrome in a non psychotic context. Shared
Obsessive-Compulsive Disorder (SOCD) is a group of diagnosis which controversial by their existence.
Method:. OCD is sometimes difficult to diagnose because of its phenomenological similarities with
other diseases. There are very few articles about SOCD in the literature while it is a rare condition in
which same features of delusions are transmitted and shared by the individuals.
Result: We will discuss over our cases of identical twins (male) the diagnosis of shared psychotic
disorder (folie a deux) and SOCD and treatment follow up . We highlight the uncommon phenomenon
of shared psychiatric disorder occurring in the context of OCD. In the current psychiatric diagnostic
nomenclature, (DSM IV-R and ICD ), there is no category for a non-psychotic shared psychiatric
disorder. We raise the question of broadening the concept of shared disorder so as to include shared
OCD and perhaps other shared psychiatric syndromes.
Discussion: More controlled studies are required in order to better understand the psychopathology
and mechanisms of psychotic and non-psychotic shared disorders in psychiatry. We believe there are
important treatment implications of such an understanding. At the end, our case is comply with SOCD,
meanwhile we think that SOCD can be a new diagnosis group, yet existence of this diagnosis group
must be investigated and discussed, meticulously.
Key words: Folie deux, Obsessive-compulsive disorder, Shared obsessions, diagnosis. References
1. Grover S, Gupta N. Shared obsessive-compulsive disorder. Psychopathology.2006;39 (2):99-101.
Epub 2006 Jan 17. 2. Torch EM. Shared obsessive-compulsive disorder in a married couple: a new
variant of folie deux? J Clin Psychiatry. 1996 Oct;57(10):489. 3. Mergui J, Sol Jaworowski S,
Greenberg D, Lerner V. Shared obsessive compulsive disorder: broadening the concept of shared
psychotic disorder. Australian and New Zealand Journal of Psychiatry 2010; 44:859862 4. Silveira JM,
Seeman MV. Shared psychotic disorder: a critical review of the literature. Can J Psychiatry 1995;
40:389-395
190
P 38
A Case Report of Tardive Dyskinesia and Tremor Due to Use of
Aripiprazole
Hakan Balibey*, Halit Yaar, Hseyin Gnay
Ankara Military Hospital Department Of Psychiatry etimesgut Military Hospital Department Of
Psychiatry
Introduction: Aripiprazole is one of the atypical antipsychotics with lower frequency of extrapramidal
side effects and tardive dyskinesia (TD). On the other hand TD cases related to the use of aripiprazole
have been increasingly reported recently. Method: In the present case we report a female 63-year old
single patient with schizophrenia who has used antipsychotics irregularly for 15 years and aripiprazole
regularly for the last year.
Result: Clinical presentation and follow up of the tremor and TD in the patient were reported and the
importance of consideration of side effects of antipsychotics were discussed.
Discussion: Our opinion is further studies are needed to find out TD risk due to aripiprazole use. In
case of risk factors, TD could be seen even if the drug dose is low or treatment duration is short.
Unvoluntary movements should be screened besides clinical features.
Key words: Aripiprazole, Tardive dyskinesia, Tremor
References:
1. Cetin M, Turgay A. Antpsychotic treatment in The fiftieth year of modern psychopharmacology: an
update. Bull Clin Psychopharmacol 2002; 12: 211-226.
2. Pena MS, Yaltho TC, Jankovic J. Tardive dyskinesia and other movement disorders secondary to
aripiprazole. Mov Disord 2011; 26: 147-152.
3. Ozturk O, Kurt E, Oral T. Delayed-onset drug-induced movement disorders. Bull Clin
Psychopharmacol 2006; 16: 263-273.
4. Ozel A, Turkcapar H, Guriz O, Karaoglan A, Kuru T. Tardive dyskinesia after short term atypical or
antipsychotic drug use. Bull Clin Psychopharmacol 2003; 13: 179-182.
5. Lungu C, Aia PG, Shih LC, Esper CD, Factor SA, Tarsy D. Tardive dyskinesia due to aripiprazole:
report of 2 cases. J Clin Psychopharmacol 2009; 29: 185-186.
6. Evcimen YA, Evcimen H, Holland J. Aripiprazole-induced tardive dyskinesia: the role of tamoxifen.
Am J Psychiatry 2007; 164: 1436-1437.
191
P 39
An Obsessive Compulsive Patient With Increased Serum
Prolactin Levels and Galactorrhea
Hakan Balibey*, Hseyin Gnay, Recep Ttnc
Ankara Military Hospital Department Of Psychiatry etimesgut Military Hospital Department Of
Psychiatry
ntroduction: The prevalance of obsessive compulsive disorder is between 1.9% and 3.3%. Its
etiology has been still investigated beyond biological basis (1). Serotonin specific reuptake inhibitors
(SSRI) are often used in the treatment ( 2 ). Increased levels of prolactin and galactorrhea are adverse
effects of antipsychotics, and it is rarely seen with SSRIs. In the the literature mild increase has been
reported with monoamine oxidase inhibitors, tricyclic antidepressants and SSRIs (3,4). There are some
papers reporting hyperporlactinemia and galactorrhea after treatment with sertraline, fluvoxamine,
paroxetine, citalopram and escitalopram (5,6).
Method: A patient with sexual erotomanic obsessions, anxiety, discomfort, insomnia, feelings of guilt
was referred to our department. Herein clinical features and observed galactorrhea are discussed.
Result: Increased serum prolactin levels and galactorrhea are found after citalopram and fluvoxamine
treatment. Discussion: In our case fluvoxamine and citalopram were combined. This might lead to
higher impact on physiological processes and cause hyperprolactinemia and galactorrhea. As a
conclusion, detailed studies are required investigating the relationship between SSRIs and increased
levels of prolactin. Combined SSRI treatment should be avoided and clinicians should be cautious
about adverse effects and drug-drug combinations.
References:
1. Rasmussen SA,Eisen JL. Clinical Features and Phenomenology of Obsessive Compulsive disorder.
Psychiatric Annals 1989; 19:2:67-73.
2. Hirschfeld RMA: Antidepressants in the USA Current Status and Future Needs. In: Weissman
MM(ed) Treatment of Depression Bridging the 21st Century. Washington.American Psychiatric Press;
2001: 123-128
3. Checkley S. Neuroendocrine effects of psychotropic drugs. Baillire's Clinical Endocrinology and
Metabolism 1991;5;15-33
4. Wieck A, Haddad PM. Antipsychotic-induced hyperprolactinaemia in women: pathophysiology,
severity and consequences. Br J Psychiatry 2003;182:199-204
5. Betl Okat Girayalp. Pititer adenomu olan depresif bir hastada fluoksetine bal galaktore: Olgu
sunumu. Klinik Psikofarmakoloji Blteni 2009;19:159-163
6. Glsn M, Evrensel A, Verim S. Essitalopram tedavisi srasnda gelien galaktore: Olgu sunumu
Klinik Psikofarmakoloji Blteni 2006;16:39-41
192
P 40
The Relationship of Incarceration, Past Suicide Attempts,
Depression, Anxiety and Attention Deficit Disorder/hyperactivity
in Cases of Anti-social Personality Disorder.
Hakan Balbey*, Trker Trker, M. Boran Evren, Nalan Bayar.
Anlara Military Hospital Psychiatry Clinic,glhane Military Academy Of Medicine, Department Of Public
Health
Introduction: Even though attention deficit/hyperactivity disorder (ADHD) has been evaluated as a
childhood disorder for a long time, currently it is widely accepted that this is a disorder that continues
well into adulthood. Attention deficit hyperactivity disorder (ADHD) is a chronic developmental
psychiatric disorder, which starts in early childhood, and primary symptoms of which can be observed
in adulthood. The main symptoms are attention loss, impulsiveness and hyperactivity and results in
mental, social and educational/occupational problems in adulthood (1). The current study is aimed at
studying the relationship of incarceration, suicide attempts, depression, anxiety, attention deficit
hyperactivity disorder in men who have been diagnosed with antisocial personality disorder (APD).
There are previous studies in the literature for equivalent diagnoses (2,3).
Method: A total of 80 subjects, 44 of whom have been diagnosed with Antisocial personality disorder
according to DSM-IV-TR diagnostic criteria in Ankara Military Hospital psychiatry polyclinic and 36 of
whom do not have a psychiatric diagnosis have been included in the study. The subjects have been
administered a semi-structured interview form for identifying their demographic properties, criminal
history and past suicide attempts. The subjects have also been administered Wender-Utah rating
scale, Beck Anxiety scale and Beck depression scale. The diagnosis of anti-social personality disorder
has been corroborated by a second mental health professional for all such cases. All subjects were
selected from among patients who had asked for consultation from Ankara Military Hospital Psychiatry
Polyclinic. Results: There is a strong association between ADHD, anxiety, depression, incarceration
and suicide attempts among subjects who have APD (p<.001).
Discussion: The current study shows that adult ADHD is a significant, life-long risk factor for
psychiatric co-morbidity. Overlooking comorbidities because of confusion with the symptoms of ADHD,
may worsen symptoms and result in resistance to treatment and thus worsen prognosis. Better
understanding of related factors in APD cases which make up a significant portion of those who have
been incarcerated and have past suicide attempts may lead to more effective treatments. It is important
that patients with anti social personality disorder are evaluated according to comorbidity and that those
patients should not go untreated for ADHD, anxiety and depression. We are of the opinion that in order
to demonstrate the relationship between ADHD and APD a cohort study needs to be conducted.
References
1. Wender PH. Attention deficit hyperactivity disorder in adults. New York, Oxford University Press,
1995, p.122-43.
2. Ekinci S, nc H, Canat S. Erikin dikkat eksiklii ve hiperaktivite bozukluu: E tan ve ilevsellik.
Anadolu Psikiyatri Dergisi 2011;12:185-91.
3. Sevin E, engul C, akaloz B, Herken H. Psikiyatri Polikliniinde Erikin Dikkat Eksiklii
Hiperaktivite Bozukluu Tans Konan Hastalarda Etan. Klinik Nropsikiyatri Arivi 2010;47:139-43.
4. Turgay A Erikinlerde dikkat eksiklii hiperaktivite bozukluu (DEHB): Snflandrma, tan ve tedavi
de yenilikler. Dikkat eksiklii hiperaktivite bozukluu. Ege Psikiyatri Srekli Yaynlar 1998; 459-494.
193
P 41
Eye Movement Desensitization and Reprocessing (emdr)
Treatment in a Patient With Posttraumatic Stress Disorder: Case
Report
Hakan Balibey*, Adem Balikci
Ankara Military Hospital Department Of Psychiatry, Samsun Military Hospital Department Of Psychiatry
Introduction: Post-traumatic stress disorder (PTSD), is a mental disorder characterised by re-
experiencing traumatic events with distress, avoidance pattern, restricted affect as well as presence of
varying degrees of autonomic, dysphoric and cognitive symptoms after exposure, encounter or hearing
an excessive traumatic stressor. (1) Eye Movement Desensitization and Reprocessing (EMDR) method
of psychotherapy that brings together elements of different well-known approaches such as
psychodynamic, cognitive, behavioral, and client-centered approaches which are used to treat stress of
war, abuse, traumatic events experienced during childhood, such as natural disasters or caused by
disturbing life experiences as well as emotional problems, phobias, performance anxiety, panic
disorder, body dysmorphic disorder, trauma symptoms in children, grief, chronic pain, abuse, rape and
other problems (3). Incidence of trauma and post-traumatic disorders are extremely high. However, the
Turkish publications related to these disorders treatment options are very limited (4-6).
Method: Treatment process of a male patient with EMDR who admitted to our outpatient clinic by
complaint of witnessing the death of his father by his head being crushed in a traffic accident about a
year ago and who was diagnosed with Post Traumatic Stress Disorder according to the DSM-IV-R
criteria will be discussed. Six sessions of EMDR therapy has been applied and besides clinical
observation for clinical evaluation, Clinician-Administered PTSD (CAPS scale) was used before and
after treatment. Result:. EMDR therapy has been effective in our case. A significant reduction of
symptoms was observed at CAPS scale applied before and after treatment, at clinical observations and
in the patient's own expressions.
Discussion: Although our results needs to be supported by recurrent clinical trials and the literature
findings, we suggest that clinicians should use this method more often for post-traumatic stress
disorder cases. As a result, trauma, EMDR seems to be a good choice for mental health professionals
who want to work about trauma in terms of learning and applying in a very short time and taking quick
results. More applications of this technique into mental health professionals applications will enhance
the competencies of practitioners on psychiatric disorders as well as give a chance for faster recovery
to patients who are suffering from disorders associated with trauma.
References:
1. Sadock BJ, Sadock VA. Kaplan & Sadockss Synopsis of Psychiatry: Behavioral Sciences, Clinical
Psychiatry. Ninth Ed. Philadelphia: Lippincott Williams & Wilkins Publishing, 2003, 623 - 631.
2. Amerikan Psikiyatri Birlii. Psikiyatride Hastalklarn Tanmlanmas ve Snflandrlmas El Kitab
Yeniden gzden geirilmi drdnc bask (DSM-IV-TR),Washington DC, E Krolu (eviri Ed.),
Ankara: Hekimler Yayn Birlii, 2001.
3. Shapiro F. Eye Movement Desensitization and Reprocessing: Basic Principles, Protocols and
Procedures, 2nd Edition, Newyork: Guilford Press, 2001; 4-126.
4. Kavakc , Doan O, Kuu N. EMDR (Gz Hareketleri le Duyarszlatrma ve Yeniden leme):
Psikoterapide Farkl Bir Seenek. Dnen Adam Psikiyatri ve Nrolojik Bilimler Dergisi 2010;23:195-
205.
5. Hocaolu , Salam D. Yalda Travma Sonras Stres Bozukluu: Bir Olgu Sunumu. Klinik Psikiyatri
2007;10:223-227.
6. Kavak , Yldrm O, Kuu N. Travma Sonras Stres Bozukluu ve Snav Kaygs iin EMDR: Olgu
Sunumu. Klinik Psikiyatri 2010;13:42-47.
194
P 42
A Case Series of Hwa-byung Patients Using Instrument of
Pattern Identification for Hwa-byung and Instrument of Oriental
Medical Evaluation for Hwa-byung
Dae-myung Park, Sang-ryong Lee, In-chul Jung*
Dept. Of Oriental Neuropsychiatry, College Of Oriental Medicine, Daejeon University, Daejeon, Korea
Objectives: This case series was conducted to report the efficacy of traditional Korean medicine
treatments for Hwa-Byung.
Methods: Patients were diagnosed with Hwa-byung through Hwa-Byung diagnostic interview
schedule(HBDIS). Instrument of pattern identification for Hwa-Byung was applied to develop an
individualized traditional Korean medicine treatment plan. SCL-90-R, STAI, STAXI, BDI, and instrument
of oriental medical evaluation for Hwa-Byung were measured. After 2 weeks of tradiational Korean
medicine treatments and K-MBSR practice, STAI, STAXI, BDI, and instrument of oriental medical
evaluation for Hwa-Byung were re-assessed to determine the progress of Hwa-Byung.
Result: After treatments, chief complaints have improved. STAI, STAXI, BDI and instrument of oriental
medical evaluation for Hwa-Byung score have decreased.
Conclusions: According to the study, traditional Korean medicine treatments using instrument of
pattern identification for Hwa-Byung have shown positive results in managing Hwa-Byung symptoms
evaluated by instrument of oriental medical evaluation for Hwa-Byung.
Key words: Hwa-Byung, Instrument of Pattern Identification for Hwa-Byung, Instrument of Oriental
Medical Evaluation for Hwa-Byung.
Acknowledgements: This study was supported by a grant of the Oriental Medicine R&D Project,
Ministry for Health & Welfare & Family Affairs, Republic of Korea.(B082005)
195
P 43
Immunology and Alzheimer - State of the Art
Joana Andrade*, Horacio Firmino, Joo Relvas
Hospitais Da Universidade De Coimbra
The immune system serves to protect the organism from external and internal danger by using an
elaborate network of immune sensors. Despite the little attention on immune responses in
neurodegeneration seen a few decades ago, now it is becoming a nuclear interest in these group of
diseases. Factors driving this movement include the recognition that most of the relevant immune
molecules are produced within the brain, that microglia are proficient immune cells shaping neuronal
circuitry and fate, and that systemic immune responses affect brain function. The authors present an
extensive review of this field with particular focus in Alzheimer disease and recent findings regarding
the role of immunity in its pathobiology.
196
P 44
Functional MRI and Obsessive-Compulsive Disorder
Joana Andrade*, Paula Banca, Susan Santo, Nuno Madeira, Flavia Polido,
Fernando Pocinho, Miguel Castelo-branco, Joo Relvas
Hospitais Da Universidade De Coimbra*; University of Coimbra
Obsessivecompulsive disorder (OCD) is a clinically heterogeneous disorder characterized by multiple,
temporally stable symptom dimensions. Preliminary functional neuroimaging studies suggest that these
symptom dimensions may have distinct neural substrates. Fourteen patients diagnosed with OCD were
recruited from the Psychiatry Department of the Hospitais da Universidade de Coimbra. Diagnoses
were established using the Structured Clinical Interview for the Diagnosis of DSM-IV psychiatric
disorders and the Anxiety Disorders Interview Schedule for DSM-IV: Lifetime Version. To assess the
severity and characteristics of OCD symptoms, each patient completed the Yale- Brown Obsessive-
Compulsive Scale, the symptom Checklist and the Padua Inventory, Washington State University
Revision. Depression scores were obtained with Beck Depression Inventory. Patients also completed
the Edinburgh Handedness Inventory to assess handedness. Exclusion criteria included the presence
of comorbidity with other Axis I diagnosis, neurological disorder, history of drug or alcohol addiction or
serious medical condition. All the participants had normal or corrected-to-normal visual acuity. All the
patients underwent functional MRI in our department in the Faculty of Medicine, and data were
addressed according to OCD subtypes. The study was conducted in accordance with the Declaration
of Helsinki and all procedures were approved by the Ethics Commissions of the Faculty of Medicine of
the University of Coimbra. All the patients received cognitive-behavioural therapy at the time of the
study. Written informed consent was obtained from all patients in advance. All subjects demonstrated a
clear understanding of the experimental procedures, risks and the intent of the study. At this moment,
statistical analysis is being performed, aiming to be able to present our first results in the congress.
197
P 45
Internet Addiction Among University Students
Eda Aslan karde, Aylin Yazc* Kemal Yazc
Department Of Psychiatry, Gediz State Hospital, Gediz, Ktahya, Turkey, Department Of Psychiatry,
Medical School Of Mersin University, Mersin, Turkey
Introduction: Internet addiction is a disorder which includes excessive preoccuping with online
activities, tolerance (e.g., spending increased amounts of time in chat rooms), symptoms of withdrawal
when not online (e.g., anxiety, depression) and making unsuccessful efforts to control internet use. It
causes impairment in global functioning of life. In our study, we aimed to find out the percentage of
internet addiction, also to compare the features of sociodemographic data and internet use between
internet addicts and non-addicts among university students.
Method: Participants were 910 students of Mersin University. Socio- demographic data scale and
Young Internet Addiction Scale was used. Young Internet Addiction Scale is a validated tool for
assessment of Internet Addiction.
Results: In our study, the percentage of internet addiction was %2 (n=18) among university students.
No differences were found between average internet use and internet addiction in terms of socio-
demographic data (age, gender, marital status, faculty, class, people living with, financial income and
spent hours for internet per week). Its determined that internet addicts use internet over 40 hours per
week, significantly (p<0.05). The most frequent used internet activities were chat, e-mail and visual talk
for internet addiction.
Discussion: These results suggest that the percentage of Internet addiction among university students
(2%) is considerable. Internet addicts use internet for social internet activities mostly and spend most of
their time using internet. Clinicians should be careful about this new clinical disorder.
198
P 46
Outcomes of a Smoking Cessation Outpatient Clinic
Hatice Kaya, M. Alper nar
Taf Rehabilitation Center, Ankara, Turkey
Introduction: A number of patients and hospital staff and seeking help to quit smoking. A smoking
cessation outpatient clinic fulfills this need. Patient education, nicotine replacement therapy (NRT), and
pharmacotherapy are common methods that are using to help these patients. We evaluated the
outcomes of smoking cessation outpatient clinic to find out its success rate.
Methods: Data of the patients who admitted to smoking cessation outpatient clinic at Turkish Armed
Forces (TAF) Rehabilitation Center between October 2010 and March 2012 were analyzed
retrospectively. Patients who quit smoking for a year accepted as successful quitter.
Results: 64 patients admitted to the outpatient clinic within 18 months. Thirty-four percent (n=22) of
them were female The mean age was 38.17.5 (meanSD) years. The mean smoking duration was
18.36.9 (meanSD) years. Patient education about withdrawal symptoms and coping strategies with
these symptoms were given to all the patients. Twenty-nine (45.3%) patients had pharmacotherapy;
12.5% (n=8) of them had NRT and 4.7% (n=3) of them had pharmacotherapy+NRT. Patients who didnt
have medication followed-up with frequent visits focusing on coping strategies. Out of 20 patients who
quit smoking, nine (42.8%) of them had pharmacotherapy, 14.4% (n=3) of them had NRT, and 42.8%
(n=9) of them had patient education and close follow-up only.
Discussion: Patients who want to quit smoking should be supported with close follow-up and have to
be followed closely. If they are experiencing difficulties to cope with smoking cessation symptoms
should be supported by pharmacotherapy and NRT.
199
P 47
Thyroxine Induced Mania in a Case With Thyroidectomy
Eda Aslan karde* , M. Alper inar**
*Department Of Psychiatry, Gediz State Hospital, Gediz, Ktahya, Turkey
**consultation-liasion Department, Taf Rehabilitation Center, Ankara, Turkey
Introduction: Clinical thyroid functional disorders are frequently accompanied by psychiatric
symptoms. There are evidences that thyroid hormones play a crucial role in the development of
affective psychopathology. We report a patient who presented with features of manic epizode
precipitated by thyroid replacement treatment after thyroidectomy surgery.
Case Presentation: A 58 year old woman was brought to our psychiatric clinic for exhibiting
talkativeness, decreased need for sleep, hearing voices that say she can do anything she want with
just a handclip. Mental status examination determined that she appeared stated age, well dressed with
causal dresses. She made fair eye contact, was alert, oriented to time-place and person. She was
easily distracted. She talked rapidly, had flight of ideas. Her mood was elevated. She had grandiosity
deluisions and auditory hallucinations. She had poor insight. Decreased need for sleep is noted. Her
score on the Young Mania Rating Scale (YMRS) was 31. The patient and her family members didn't
have any significant past psychiatric problems. After the thyroidectomy operation 7 months ago,
replacement of thyroid hormone thyroxine was given to the patient at low doses (12.5 mcg) and was
increased to 50 mcg per day within 1 week. She maintained the same treatment for 6 months. After the
doses were increased to 75 mcg per day last week, the patient underwent a manic state within 3 days.
In laboratory evaluation, the thyroid functions revealed normal range. She was diagnosed as thyroxine
induced mania and hospitilized. She was administered with olanzapine 10 mg per day and after 3 days
of initiation of treatment, she had complete recovery. Her score on YMRS was 4 after olanzapine
treatment.
Discussion: Thyroid replacement treatment increases the risk of mania in vulnerable individuals that
even if a direct relationship between levels of psychopathology and thyroid hormones cannot be
demonstrated peripherally. Its postulated that thyroid hormones might act as neuromodulators of
central beta-adrenergic function and such a state is thought to be the neurochemical basis for mania.
200
P 48
Epidemiologic Features of the Psychiatry Outpatient Clinic
Admissions in a County Hospital
Eda Aslan karde, M. Alper inar
Department Of Psychiatry, Gediz State Hospital, Gediz, Ktahya, Turkey consultation-liasion
Department, Taf Rehabilitation Center, Ankara, Turkey
Objective: Epidemiological studies are necessary to determine the etiology and pathogenesis of
psychiatric disorders. The data that reflect the real situation in the best way can be obtained by field
studies. Demographic and social information is determinant for usage of psychiatric clinics. The aim of
this study is to investigate the sociodemographic features and psychiatric diagnosis of the patients who
admitted to Gediz State Hospitals Psychiatry Clinic during a one-month period.
Methods: Admissions to psychiatry clinic during March 2012 were examined retrospectively. Age, sex,
psychiatric diagnosis and comorbid medical diagnoses data were collected from the patient records.
Results: A total of 310 patients were admitted to study. 36,2% of them were male (n=116) and 63,8%
of them were female (n=204). Male patients were 4119 years old, female patents were 3917 years
old. The most common psychiatric diagnoses were found as major depressive disorder (45,9%,
n=147), anxiety disorders (31,2%, n=100), psyhotic disorders (5%, n= 16) and somatoform disorders
(%4,1, n=13). Among anxiety disorders, generalized anxiety disorder (14,7%, n=47); among psychotic
disorders, schizophrenia (%3,1, n=10) and among somatoform disorders, somatization disorder (%3,8,
n=12) were found as the most common psychiatric disorders. 34,1% (n=109) patients had comorbid
medical diagnosis. The most frequent comorbid medical conditions were hipertansion (15,9%, n=51),
diabetes mellitus (7%, n=24) and hypothyroidism ( 2,1%, n= 7).
Conclusion: In this study most of the applicants were female. Major depressive disorder, anxiety
disorders, psychotic disorders and somatoform disorders were determined as the most common
diagnosis. The results suggest that comorbid medical condition rates are high in county hospital.
Clinicians should consider about comorbidity during examination.
201
P 49
Epidemiologic Features of Anxiety Disorders in a County
Hospital
Eda Aslan karde, M. Alper inar*
Department Of Psychiatry, Gediz State Hospital, Gediz, Ktahya, Turkey *consultation-liaison
Department, Taf Rehabilitation Center, Ankara, Turkey
Introduction: Epidemiological studies provide important information about the patterns of disorders in
communities. Anxiety disorders have a high impact on daily life and cause a great deal of suffering for
the individual patient. Anxiety disorders, although as common as depression, has received less
attention and is often undetected and undertreated. Our aim for this study is to determine the
sociodemographic features of patients with anxiety disorders and medical comorbidity of anxiety
disorders in a state hospital of a county.
Method: Admissions to psychiatry clinic in February 2012 were examined retrospectively. Age, sex,
comorbid medical diagnoses data were collected from the records of the patients with anxiety
disorders.
Results: A total of 147 patients with anxiety disorders were admitted to study. 31,3% of them were
male (n= 46), and 68,7% of them were female (n=101). The patients were 43 18 years old; male
patients were 4320 years old, female patents were 4317 years old. Among anxiety disorders,
generalized anxiety disorder (48,3%, n=71) was the most diagnosed psychiatric disorder. The others
were; anxiety disorder NOS (27,2%, n=40), panic disorder (23,1%, n=34) and obsessive- compulsive
disorder (1,4%, n=2). The most common comorbid medical diagnoses were found as hypertension
(19%, n= 27), diabetes mellitus (8,8%, n=13) and hypothyroidism (2,7 %, n=4). Fifty-four percent 54,4%
(n=80) of the patients who admitted to psychiatry clinic were living in the villages and 45,6% (n=67) of
them were living in the county. 79,6% (n=117) of them were married, %13,6 (n= 20) were single and
6,8% (n=10) were divorced/widow.
Discussion: Anxiety disorders are shown to be very common. Women have higher rates of anxiety
disorders than men. The patient with anxiety disorders were admitted to our psychiatric clinic from
villages mostly. The high rates of comorbidity with chronic medical conditions are remarkable and those
medical conditions need additional and close attention to the patients with anxiety disorders.
202
P 50
The Study of Effectiveness Instruction and Counseling
Premarital on Consolidation of Family Basis
Manouchehr Saadatkhah
Master Of Psychological Counseling Center In Welfare (behzisti Organization) In Ardebil Province
Introduction: The most important thing in life is to marry anyone that will affect aspects of his personal
and social issues. With the rising divorce statistics, the experts will gain a suitable solutions to prevent
this pest and provide a successful marriage and life expectancy. The present study have been
conducted the effectiveness of premarital instruction and counseling on consolidation of family basis.
Methods: From among all clients referred to psychological counseling center of Welfare and
psychological counseling center of Raha in Ardabil province that before pre-marriage counseling
services and other counseling services (other than pre-marriage counseling) had received 76
people(38 people recipients counseling services before marriage, and 38 people have not received
counseling services before marriage and that no other instruction in this field) were randomly selected
then both groups responded to dyadic adjustment scale (DAS) . For data analysis was used t
test and multivariate analysis of variance.
Results: With equally demographic characteristics of the subjects that by 'chi-square' was
determined data analysis results (mean differences significant by t-test 5/486 of between the two
compared groups and also sub-scales mean significant by multivariate analysis of variance between
groups) showed the effectiveness of pre-marriage counseling to increase adjustment between the
couple.
Conclusion: This study showed that premarital instruction and counseling enhanced adjustment
between the couple and this results confirmed high confidence.
Key words: pre-marriage counseling, adjustment couple, consolidation of family basis
203
P 51
Preliminary Study Title: Frontal Gamma Activities as a Biomarker
of Family History
Meltem Ballan*
1
, John H. Gilmore
1
, Jessica Beattie
1
Department of Psychiatry, School of Medicine, University of North Carolina-Chapel Hill
Brief Study Synopsis
Recent studies have shown that Schizophrenia has genetic causes; however, there is a large patient
population without a family history of Schizophrenia. The latter challenges the scientists to explore the
other factors. For example (Maki et al., 2010)studied the relationship between environmental factors
and genetic factors on Schizophrenia. They suggested an interaction between the environmental factor
(i.e., maternal depression during pregnancy) and the genetic factor. In this context, (Clarke et al., 2011)
studied the interaction between genetic liability and prenatal exposure to infection. Moreover,
Reichenberg et al (2010)studieddifferent familial onsets of Schizophrenia. Although the actual cause of
Schizophrenia is still not known, an alternative interpretation would be that all these complicated
genetic and environmental factors affect the brain development. For example, prenatal exposure to
maternal stress results in reduced hippocampal volume and reduced neurogenesis in rhesus monkeys
(Coe et al., 2003). In this matter, we want to put forward the studies on Schizophrenia exploring the
infant brain dynamics (e.g., EEG biomarkers, spontaneous brain activities and Visual Evoked
Potentials (VEPs) using high-resolution Electroencephalogram (EEG, >64 channels).
Background and Hypothesis
Visual processing deficits are one of the most common indicators of Schizophrenia. In this context,
recent studies have used high-resolution EEG for identifying the temporal brain dynamics of adult
Schizophrenia patients over the visual pathway. The studies indicated that patients are less sensitive to
identify the difference in spatial frequency (i.e., gabor patch) and contrast (e.g., black and white screen
v.s. gray and white screen) Subcortical visual dysfunction in schizophrenia drives secondary cortical
impairments (Butler et al., 2007). (Butler, et al., 2007) suggested that this insensitivity in contrast and
spatial frequency is a result of pervasive magnocellular dysfunction in dorsal and ventral stream of
visual pathway. In this line of research, we want to increase ourunderstandingof Schizophrenia to
capture the disorder in an early stage of life testing the visual perception. In a longitudinal seminal
study, Conel (1939, 1947, 1951) illustrated the state of cortical development at the birth, at 3 months
and 6 months of ages. This study showed thatthe visual cortex is partially developed at birth; however,
it develops rapidly within 3 months of age and 6 months of age period. During this period, visual acuity
and contrast sensitivity develop rapidly to just below the adult level by the age of 6 months (Pirchio et
al., 1978). At this stage, we hypothesize that the spontaneous reaction to a video would show
significant differences between healthy population and high-risk population infants at 12 months of age.
In order to validate our results we would repeat the test at 2 weeks of age, 12 months of age and 24
months of age.
Briefly, the infant EEG bands are defined as theta band (4-7 Hz) related to emotional development and
learning, alpha band (6-10 Hz) social and emotional development and high frequency activities
between 10 and 50 Hz as beta and gamma activities. These frequencies are related to cognitive
development, language development, familial history of depression and mental disorders (Benasich,
Gou, Choudhury, & Harris, 2008; Haan, 2007). In the current study, we analyzed gamma changes
including whole head activities and focused only on frontal activities as the visual cortex activities are
stimulated passively for newborns.
Results and Discussion
Currently, we are building our control database looking at the spontaneous EEG dynamics over the
frontal and occipital regions. Our first focus is fast gamma activities. Our preliminary results showed
that there is anincrease on the frontal gamma activities by age. Our preliminary results showed that
overall averaged gamma power(5 Hz bins between 30-50 Hz) increased by age. The figures represent
the gamma powers between 36-40 Hz. We expect a delay as well as a hemispheric asymmetry shift
with infants of Schizophrenia patients.
Significance
Our preliminary data a global increase in absolute EEG gamma power and this resulted
change in beta and alpha powers.
204
The gamma power and its frontal-occipital dynamics can be accurate biomarkers to observe
developmental differences
Limitation
The group studied is very small for statistical analysis.
Two weeks old infants are presented lights whereas older subjects watched videos.
The analysis is limited to artifact free regions and infant EEG studies include more artifacts
than adult studies.
The conclusion requires further support:
Increasing the number of participants.
Analyzing the other frequency bands.
Analyzing second to second frequency power changes in individual participants.
Selected References
1. Benasich, A. A., Gou, Z., Choudhury, N., & Harris, K. D. (2008). Early cognitive and language
skills are linked to resting frontal gamma power across the first 3 years. Behav Brain Res,
195(2), 215-222.
2. Butler, P. D., Martinez, A., Foxe, J. J., Kim, D., Zemon, V., Silipo, G., et al. (2007). Subcortical
visual dysfunction in schizophrenia drives secondary cortical impairments. Brain, 130(Pt 2),
417-430.
3. Clarke, M. C., Tanskanen, A., Huttunen, M., Leon, D. A., Murray, R. M., Jones, P. B., et al.
(2011). Increased risk of schizophrenia from additive interaction between infant motor
developmental delay and obstetric complications: evidence from a population-based
longitudinal study. Am J Psychiatry, 168(12), 1295-1302.
4. Coe, C. L., Kramer, M., Czeh, B., Gould, E., Reeves, A. J., Kirschbaum, C., et al. (2003).
Prenatal stress diminishes neurogenesis in the dentate gyrus of juvenile rhesus monkeys. Biol
Psychiatry, 54(10), 1025-1034.
5. Haan, D. (Ed.). (2007). Infant EEG and Event Related Potentials, : Psychology Press.
6. Maki, P., Riekki, T., Miettunen, J., Isohanni, M., Jones, P. B., Murray, G. K., et al. (2010).
Schizophrenia in the offspring of antenatally depressed mothers in the northern Finland 1966
birth cohort: relationship to family history of psychosis. Am J Psychiatry, 167(1), 70-77.
7. Reichenberg, A., Caspi, A., Harrington, H., Houts, R., Keefe, R. S., Murray, R. M., et al.
(2010). Static and dynamic cognitive deficits in childhood preceding adult schizophrenia: a 30-
year study. Am J Psychiatry, 167(2), 160-169.
N Ne ew wb bo or rn n T Tw wo o- -y ye ea ar r o ol ld d
G Ga am mm ma a F Fr re eq qu ue en nc cy y ( (3 36 6- -4 40 0 H Hz z) )
O On ne e- -y ye ea ar r o ol ld d
205
P 52
Biosensors for Clinical Neuropsychopharmacology
Bragazzi Nicola Luigi
University Of Genoa, Italy
Here we present enzyme-based biosensors for Clinical Neuropsychopharmacology, fully characterized
via nanotechnologies (such as UV spectrophotometry, nanogravimetry, AFM, Langmuir-Blodgett p-A
isotherm, amperometric and potentiometric measurements). First we validate them with collected blood
samples from healthy volunteers and then using real blood samples from psychiatric patients. Different
biosensors are compared (based on laccase, lipase, etc) and results are discussed in details. Also
clinical correlations with mind diseases and responder-states are commented.
206
P 53
Three Different Specific Internet Addiction Cases From the
Internet Addiction Clinic of a Training and Research Hospital
mer enormanc, Ramazan Konkan, Oya Gl, Gliz enormanci
Bakirkoy Research And Training Hospital for Psychiatry, Neurology And Neurosurgery
Some people use internet for a particular purpose such as online sex, gaming, gambling, stock tracking
or shopping. This case study includes three different patients their treatment combination with
pharmacotherapy and cognitive behavioral therapy. AG 40 year-old man. Each time he spent at least 3
hours on the Internet, which he was reviewing some items on the shopping sites in extensive detail at
least for 2 hours, finally feeling relief after make purchases in large amounts. He showed
characteristics of ADHD and had high scores on the screening test. HE 16 year-old man. He was
addicted to an interactive online game called 'Massively multiplayer online role-playing game
(MMORPG), He had been using the Internet for the past 7 years, during which he reached to an
addictive level within last 3 years. Before contacting us, he had been on extended-release
risperidone,oral risperidone, atomoxetine, olanzapine, naltrexone and aripiprazole prescribed to control
his internet use. BC 33 year-old man. He moved into a small rental shop that costed him 90 per
month, where he spent his entire day busy on the internet gambling and sex sites. His family and
friends were not aware of this place. He had lost over 20,000. Motivational interviewing is important in
the treatment of Internet addiction as it is in all behavioral dependencies We use motivational
interviewing techniques to ensure their participation to the cognitive behavioral therapy besides
pharmacotherapy.
207
P 54
Two Cases of Generalized Internet Addiction From the Internet
Addiction Clinic of a Training and Research Hospital
mer enormanc, Ramazan Konkan, Oya Gl, Gliz enormanci
Bakirkoy Research And Training Hospital for Psychiatry, Neurology And Neurosurgery
Generalized pathological internet use, involves overuse of internet, either for several purposes or
wasting too much online with no direct purpose. This case study includes two different patients with
specific internet addiction and their treatment combination with pharmacotherapy and cognitive
behavioral therapy UH 16 year-old teenager. His mother reported that he spent all his time after school
on the Internet and his grades had been falling It was determined in his psychiatric evaluation that he
was worried about what he called evil thoughts and he spent at least 6 hours a day on the Internet to
get rid of this state of unrest. He said he wouldnt be using the Internet so heavily if he hadnt had
worries and restlessness. VS is a 52 year-old man. He presented to our clinic complaining about his
aimless Internet use over 10 hours a day for the past 8 years. His psychiatric history revealed that he
had fears of being humiliated and critized in public and crowded places for 20 years. He had automatic
thoughts like What if I make a mistake, humiliate myself and come across as ignorant. Hed been
using almost all antidepressants in their effective doses and durations and seeking treatment for his
social anxiety disorder for approximately 20 years. Cognitive behavioral therapy was used in both
cases, addressing both the Internet addiction and the comorbid anxiety disorder.
208
P 55
Effect of Treatment on Inflammation Biomarkers, Heart Rate
Variability and Arterial Stiffness in Depressed Patients
Angelos Halaris, Edwin Meresh, Ozden Arisoy, Jawed Fareed, Debra Hoppenstead,
Steven Kimmons
Loyola University Strich School Of Medicine, Department Of Psychiatry And Behavioral Sciences,
Chicago-usa * Loyola University Strich School Of Medicine, Department Of Pathology- Chicago-usa
*abant Izzet Baysal University Medical School, Department Of Psychiatry, Bolu- Turkey
Introduction: Depressive illness (MDD) shows high co-morbidity with cardiovascular disease (CVD)
and may contribute to its development. The precise mechanisms underlying this co-morbidity elude us.
Studies have focused on platelet reactivity, endothelial and autonomic nervous system (ANS)
dysfunction and inflammatory processes. But it is still unclear if antidepressant treatment can reverse
this pathology.
Objective: To determine whether depressed patients showed normalization of inflammation, ANS and
endothelial function measures following successful treatment with either escitalopram (ESC) or
quetiapine (QTP), as monotherapeutic agents.
Method: 77 MD patients and 27 HCs were enrolled. 34 patients received escitalopram (ESC) at 10-40
mg/day and 51 patients received quetiapine (QTP) at 25-300 mg/day for 12 weeks. Depression, anxiety
and stress severity were assessed with the Hamilton Depression and Anxiety Scales (HAMD, HAMA),
Beck Depression Inventory (BDI) and Perceived Stress Scale (PSS). Post-treatment HAM-D17 scores
were used to determine treatment response. Arterial stiffness, an index of endothelial dysfunction, was
measured by Augmentation Index (AIx) and Pulse Wave Velocity (PWV). Heart Rate Variability (HRV)
was used as an index of ANS imbalance. Plasma concentrations of C-reactive protein (CRP),
interleukin (IL)-1, 1, 2, 4, 6, 8, 10, vascular endothelial growth factor (VEGF), interferon- (IFN- ),
tumor necrosis factor- (TNF-), monocyte chemotactic protein-1 (MCP-1), and epidermal growth
factor (EGF) were analyzed using a high-sensitivity biochip immunoassay system.
Results: 19 patients from the ESC group and 25 patients from the QTP group completed week 12
assessments. ESC and QTP were equally effective in reducing the symptoms of depression in patients
completing the study with similar response and remission rates. In thel MD cohort, 63.3% experienced
remission, 14.3% were partial responders, and 22.4% were non-responders. After 12 weeks of
treatment, there were significant decreases in HAMD17, HAMA, BDI and PSS14 scores in both MDD
cohorts. Despite these impressive response rates, we did not observe any significant alterations in
cytokine or growth factor levels, HRV and arterial stiffness measures after twelve weeks of treatment.
Baseline CRP, VEGF, IL4, IL1A levels were significantly higher in the responder group, while only IL4
and IL1A were higher in remitter group. Elevated levels of these cytokines appear to be indicative of
therapy response.
Discussion: These findings indicate that antidepressant treatment over a twelve week period is not
sufficient to normalize inflammatory biomarker levels, HRV and arterial stiffness measures despite a
signifiant resolution of depressed symptamotology. But baseline VEGF, CRP, IL4 and IL1A appear to
be predictors of favorable response to therapy.
209
P 56
Inflammation and Heart Rate Variability in Major Depression
Angelos Halaris, Edwin Meresh, Ozden Arisoy**, Jawed Fareed*, Debra
Hoppenstead*, Steven Kimmons
Loyola University Strich School Of Medicine, Department Of Psychiatry And Behavioral Sciences,
Chicago-usa * Loyola University Strich School Of Medicine, Department Of Pathology- Chicago-usa
**abant Izzet Baysal University Medical School, Department Of Psychiatry, Bolu- Turkey
Introduction: Cardiovascular disease (CVD) and major depressive disorder (MDD) are two of the
worlds leading health problems. MDD is associated with increased CVD events. The possible
mechanisms underlying this co-morbidity have focused on platelet reactivity, endothelial and autonomic
nervous system (ANS) dysfunction and inflammatory processes.
Objective: To evaluate plasma cytokine profile, endothelial and ANS dysfunction in MDD patients
versus age-matched healthy controls (HC).
Method: 77 MDD patients and 27 HCs were enrolled. Depression and anxiety severity was assessed
with the Hamilton Depression and Anxiety Scales (HAMD, HAMA) and Beck Depression Inventory
(BDI). The level of perceived stress was evaluated with the Perceived Stress Scale (PSS). Arterial
stiffness, an index of endothelial dysfunction, was measured by Augmentation Index (AIx) and Pulse
Wave Velocity (PWV). Heart Rate Variability (HRV) was assessed as an index of ANS imbalance.
Plasma concentrations of C-reactive protein (CRP), interleukin (IL)-1, 1, 2, 4, 6, 8, 10, vascular
endothelial growth factor (VEGF), interferon- (IFN- ), tumor necrosis factor- (TNF-), monocyte
chemotactic protein-1 (MCP-1), and epidermal growth factor (EGF) were analyzed using a high-
sensitivity biochip immunoassay system. Correlations were sought between cytokines, HRV, AIx, PWV
and various clinical rating scales.
Results: In the MDD group, mean baseline HAMD, HAMA, BDI and PSS14 scores were significantly
higher than the HCs (p=0.005). AIx of the MD group (17.1) was higher than HCs (15.7) but failed to
reach statistical significance. PWV, HRV measures were not different between the two groups. The
MDD cohort expressed higher levels of proinflammatory cytokines compared to HCs, with eight of
them reaching statistical significance (CRP, IL2, 6, 8, VEGF, IFN- , TNF-, MCP-1). Statistically
significant correlations were found between baseline HAMD17 and CRP, IL2, VEGF, TNF- ; between
baseline HAMA and CRP,VEGF; between PSS and CRP,VEGF, IFN- . BDI was positively correlated
with AIx. Parasympathetic measures of HRV were negatively correlated with IL-6, while heart rate was
positively correlated with IL-1A. EGF was negatively correlated with PWV.
Discussion: This study indicates that MDD patients have increased perceived stress, increased
arterial stiffness and increased levels of circulating proinflammatory cytokines providing compelling
evidence that depression, immune dsyregulation and arterial stiffness are intimately linked
210
P 57
The Role of Psychiatrist in a palliative Care Mobile Team"
Tomislav Peharda, Dragan Trivanovic, Krizo Katinic, Dragutin Breski
General Hospital Pula, Pula, Istria, Croatia
INTRODUCTION: In May 2011 a mobile palliative care team of the County of Istria was established as
a model of outpatient palliative care, to assist general practitioners in treatment of intensified symptoms
in critically ill patients. The team (psychiatrist, oncologist, neurologist and psychologist) responds to
emergency health calls within a radius of 70 km.
AIM: The broad aim was the psychological training of GPs in the county, education of community
nursing providers and the palliative care team itself, as well as education of patients and their families.
Specific aim was start-up of psychiatric interventions on a call either from GP or from oncologist of the
palliative team. Interventions included the treatment of patients with delirium, paranoid content, suicidal
thoughts, insomnia, anxiety and depression. This entailed treatment of families' anxious depression,
adjustment disorder including acute stress reactions. Psychiatrist in the team observes emotional
reactions of its members, strengthens the cohesion of the team, encourages support and seeks regular
meetings during which he triggers their unconscious reactions in the field. He also links the hospital
services (psycho-oncological unit) with outpatient services (family and general practitioner).
METHOD: Palliative treatment included a provision of psychopharmacs (1 to 2.5 mg fluphenazine,
risperidone 2 mg, 5 mg olanzapine and clozapine 25mg), antidepressants (sertraline 50mg,
escitalopram 10g, duloxentine 60mg), anxiolytics (alprazolam 0.25 mg) and hypnotics (zolpidem 10
mg), as well as psychotherapy techniques: support, brief focal psychotherapy, CBT. The team used
problem solving, support psychotherapy and identify automatic thoughts techniques.
RESULT: In the frame of the project, within six months period, the psychiatrist examined 76 palliative
patients in the field; two psycho-oncological clinics were established in the County's small towns;
regular monthly meetings of the mobile team with supervision were conducted as well as team training
of general practitioners (6 training sessions) and community nursing providers (5 trainings sessions).
DISCUSSION: Aim of this work was to emphasize that the project of the mobile palliative care team, in
spite of lack of developed national program, offers some concrete outpatient solutions to help terminally
ill patients, where the role of a psychiatrist is complex but unavoidable.
211
P 58
Personality Traits in Schizophrenia Patients at Remission Phase
and Their First Degree Relatives: A Dopaminergic and
Glutamatergic Genes Polymorphism Study
Vesile Altinyazar1, Azad Gnderici2
Md, Assist.prof., Department Of Psychiatry, Faculty Of Medicine, Adnan Menderes University, Aydin,
Turkey.1 md, Tunceli Government Hospital, Tunceli, Turkey.2
Objective: The dopaminergic and glutamatergic systems are major interest in etiology of schizophrenia
and supposed endophenotypes such as personality traits. In the present study we investigated the
association between the catechol-O-methyltransferase (COMT) gene P2 promoter rs2075507
(previously rs2097603), rs4680 (Val/Met), rs165599, the dopamine transporter gene (DAT1) VNTR and
the glutamate transporter gene (SLC1A2) promoter -181A/C polymorphisms, as well as both
symptomatic and personality features in schizophrenia.
Methods: The sample comprised 51 schizophrenic patients in remission, 45 first-degree relatives of
patients and 112 healthy controls. The samples were genotyped for these polymorphisms and
assessed with the Operational Criteria Checklist for Psychotic Illness (OPCRIT) for each of the five
factor-derived scales (negative symptoms, delusions, hallucinations, mania, and depression), and also
evaluated using the Temperament and Character Inventory (TCI).
Results: No significant differences were found between these polymorphism and groups. However,
rs2075507 was associated with delusion and mania scores and Novelty-Seeking in patients. There
were significant effects of DAT1 VNTR and SLC1A2 -181C polymorphisms on Self-Transcendence
scores.
Conclusion: COMT P2 promoter rs2075507 polymorphism may be associated with schizophrenia
symptom dimensions and rs2075507, SLC1A2 promoter -181A/C and DAT1 VNTR polymorphisms
may be associated with both normal and psychopathological aspects of personality.
212
P 59
Peripheral Edema Associated with Olanzapine- Valproate
Combination: A Case Report
Leyla Bozatl*, Yasemin Grgl, Rugl Kse nar, M. Blent Snmez,
M. Erdal Vardar
Trakya University, Faculty Of Medicine, Department Of Psychiatry, Edirne *trakya University, Faculty
Of Medicine, Department Of Child And Adolescent Psychiatry, Edirne
Olanzapine is an atypical antypsychotic approved for treatment of schizophrenia and bipolar disorder
(Stahl, 2000). The most frequent side-effects of olanzpine include constipation, dyspepsia, weight gain,
dry mouth, dizziness, somnolence, asthenia and insomnia (Collaborative Working Group on Clinical
Trail Evaluations, 1998). Premarketing trials have reported peripheral edema as an infrequent adverse
event which affected 3% of 532 actively treated subjects, compared to 1% of 294 subjects on placebo
(Zyprexa production leaflet, 2005). Pedaledema has been observed in rare cases using atypical
antipsychotics such as risperidone (Sanders and Lehrer, 1998), olanzapine (Christensen, 2003),
amisulpiride (Chen and Chou, 2004) and ziprasidone (Ku et al., 2006). Herein, we reported a case of
peripheral edema related to depakine and olanzapine. A 48-year- old male diagnosed with bipolar
disorder had been treated for the 3-4 week with depakine and olanzapine. The peripheral edema
developed with this therapy. As a result of the examinations couldnt be found another reason for a
peripheral edema. Treatment has been terminated and peripheral edema decreased.
213
P 60
Quality of Life in Adolescent Epileptic Patients With and Without
Psychiatric Comorbidity
Erdem Beyoglu
1
, Yesim Taneli
1
, zlem zdemir
2
, Mehmet Sait Okan
2
, Suna Taneli
1
1
Uludag University School of Medicine, Dept. of Child and Adolescent Psychiatry, Bursa, Turkey
2
Uludag University School of Medicine, Dept. of Child Neurology, Bursa, Turkey
(yesimtaneli@hotmail.com)
AIM: Epilepsy as well as psychiatric diseases have both a negative impact on quality of life (QoL).
Epilepsy is one of the most common disease during childhood. Epileptic patients show high rates of
psychiatric comorbidity. This study aimed at investigating quality of life in adolescent epileptic patients
with and without psychiatric comorbidity.
METHOD: Forty-two adolescent epileptic patients (52.14% female) with at least one seizure in the past
2 years, able to comply with study procedures, without any known acute or chronic disease affecting
the quality of life were included after IRB approval and informed consent. Severity of epilepsy was
determined by the Department of Paediatric Neurology according to the Clinical Global Impression
Severity Scale (CSI-S). At the Department of Child and Adolescent Psychiatry, psychiatric comorbidity
was assessed according to DSM-IV by psychiatric interview and Brief Symptom Inventory (BSI)
Turkish version; while the Pediatric Quality of Life Inventory (PedsQL) Child Report and Parents
Report Turkish version was applied to determine the impact of epilepsy on quality of life (QoL).
RESULTS: Mean age of patients was 15.31+1.66 years. Rate of partial epilepsy was 76.2% and of
generalized epilepsy was 23.6%. Clinical Global Impression Severity scores did not differ by type of
epilepsy. All patients were on medication and 14.28% took a combination of antiepileptics. Rate of
psychiatric comorbidity was 52.4% and a high rate of depression (26.2%) was noted. Epileptic
adolescents with psychiatric comorbidity (52.4%) did not differ from those without psychiatric
comorbidity (47.6%) in terms of gender, mean age, CGI-S, illness duration, duration of neuropaediatric
follow-up, type of epilepsy, type of antiepileptic agent, time to last seizure or number of in-patient
treatment (all p > 0.05). Mean BSI total score as well as depression, anxiety, negative self and
somatization items were higher in patients with psychiatric comorbidity (all p < 0.05), a difference for
hostility items could not be verified (p > 0.05). PedsQL mean value of patient reports was 77.83+14.68,
and of parent reports was 78.26+13.50. Mean PedsQL patient report score was lower in epileptic
patients with a psychiatric comorbidity than without a psychiatric comorbidity (70.81+15.60 vs.
85.56+8.57; p < 0.05) (Table 1); this result was due to perceived lower psychosocial health (p < 0.05),
whereas perceived physical health did not differ (p > 0.05). Parental assessment of quality of life using
PedsQL did not differ for epileptics patients with or without psychiatric comorbidity (p > 0.05). Mean
PedsQL for epileptic patients with a psychiatric comorbidity was lower in patient reports than in parent
reports (p < 0.05).
CONCLUSION: Psychiatric comorbidity has a significant negative impact on quality of life in epileptic
adolescents, especially in terms of perceived psychosocial health.
Acknowledgements: Presented data are part of Dr. E. Beyoglus thesis, presented at Uludag
University School of Medicine (Advisor Y. Taneli).
214
P 61
Methylenetetrahydropholate Reductase (Mthfr) Gene
Polymorphism in Pediatric Attention Deficit and Hyperactivity
Disorder
Algun Tfekci
1
, Yesim Taneli
1
, Emine Kirhan
2
, Melahat Dirican
2
1
Uludag University School of Medicine, Dept. of Child and Adolescent Psychiatry, Bursa, Turkey;
2
Uludag University School of Medicine, Dept. of Biochemistry, Bursa, Turkey
AIM: The study aimed to investigate 5,10-methylenetetrahydropholate reductase (MTHFR) gene
polymorphism in children and adolescents with attention deficit and hyperactivity disorder (ADHD).
METHOD: Thirty-nine children and adolescents (10.3% female) with a diagnosis of ADHD according to
DSM-IV were included after IRB approval and informed consent. Mean age of the study group was 9.5
years (range 6.4-14 years). Severity of ADHD was assessed with the Clinical Global Impression -
Severity Scale (CGI-S). MTHFR gene polymorphisms were determined for C677T and A1298C via strip
assay based on a PCR - Reverse Hybridization technique. Independent samples t test, Mann Whitney
U test; Fishers Exact test and Pearson chi-square (SPSS Inc, Chicago, Il, USA) were applied with a
statistical treshold of p<0.05.
RESULTS:
A) The combined subtype of ADHD was seen in 84.6% of patients, and the predominantly attention
deficit subtype was seen in 15.4% of patients; but the predominantly hyperactive subtype was not
found in the study group. Clinical Global Impression Severity (CGI-S) scores revealed 74.4% (n:29)
mild/moderate and 25.6% (n:10) marked/severe cases according to ADHD symptom severity.
B) MTHFR C677C (normal homozygotic), C677T and T677T frequencies were 46.2%, 48.7% and
5.1%, respectively. MTHFR A1298A (normal homozygotic), A1298C and C1298C frequencies were
38.5%, 41.0% and %20.5%, respectively. MTFHR C677T distribution was similar to local (Bursa;
n=195) (1) and national (Turkey; n=1684) (2) population samples (both p>0.05). MTFHR A1298C
distribution was similar to a national population sample (Turkey; n=1684) (p>0.05) (2), while local
A1298C distribution data were not available for comparison.
C) Distribution of MTHFR C677T or A1298C polymorphisms did not differ for ADHD subtypes (p>0.05).
Distribution of polymorphisms also did not differ for symptom severity of inattention or hyperactivity
(p<0.05).
CONCLUSION: In conclusion, our preliminary results do not show a distinct pattern of MTHFR gene
polymorphisms in ADHD. Studies with larger samples are needed.
Acknowledgements: 1) Presented data are part of Dr. A. Tufekcis thesis, presented at Uludag
University School of Medicine (Advisor Y. Taneli). 2) This work was supported in part by the
Commission of Scientific Research Projects of Uludag University under Project Number T(U-2009/4).
Literature:
1- Meral A, et al., Turk J Hemat. 2002;19(Suppl.3):111;
2- Sazci A, et al., Cell Biochem Funct. 2005;23:51-4.
215
You might also like
- The Mind in Conflict (Charles Brenner) (Z-Library)Document284 pagesThe Mind in Conflict (Charles Brenner) (Z-Library)zjcashin2857100% (1)
- Wilfred Bion - Learning From Experience (Routledge Classics) - Routledge (2023)Document161 pagesWilfred Bion - Learning From Experience (Routledge Classics) - Routledge (2023)willmetalangelNo ratings yet
- A Karl Abraham - A Short Study of The Development of The Libido (1924)Document86 pagesA Karl Abraham - A Short Study of The Development of The Libido (1924)vanpec100% (1)
- Henri F. Ellenberger EthnopsychiatryDocument381 pagesHenri F. Ellenberger EthnopsychiatryHeráclito Aragão Pinheiro100% (1)
- Trauma Sequelae (Libro)Document537 pagesTrauma Sequelae (Libro)Andrea BautistaNo ratings yet
- The Para-Existential Personality DisorderDocument10 pagesThe Para-Existential Personality DisorderKostas RigasNo ratings yet
- Anthropology and The AbnormalDocument24 pagesAnthropology and The Abnormaldanielschwartz88No ratings yet
- Craig McGarty, Vincent Y. Yzerbyt, Russell Spears Stereotypes As Explanations The Formation of Meaningful Beliefs About Social Groups 2002Document243 pagesCraig McGarty, Vincent Y. Yzerbyt, Russell Spears Stereotypes As Explanations The Formation of Meaningful Beliefs About Social Groups 2002Ardisos ArdisosNo ratings yet
- Jones Sigmund Freud Life and Work Vol 1Document91 pagesJones Sigmund Freud Life and Work Vol 1Ivan DulovNo ratings yet
- Magagna, J. and Pepper Goldsmith, T. (2009) - Complications in The Development of A Female Sexual Identity.Document14 pagesMagagna, J. and Pepper Goldsmith, T. (2009) - Complications in The Development of A Female Sexual Identity.Julián Alberto Muñoz FigueroaNo ratings yet
- Angelo Stagnaro's Something From Nothing - A Guide To Modern Cold ReadingDocument12 pagesAngelo Stagnaro's Something From Nothing - A Guide To Modern Cold ReadingDario KatušićNo ratings yet
- Sigmund Freud The Correspondence of Sigmund Freud and Sandor Ferenczi Volume 1, 1908-1914Document619 pagesSigmund Freud The Correspondence of Sigmund Freud and Sandor Ferenczi Volume 1, 1908-1914myemanation100% (14)
- Lady Feeding The Cats Initial AnalysisDocument3 pagesLady Feeding The Cats Initial Analysisapi-288431060100% (1)
- Lesson Plan 2 RasputinDocument23 pagesLesson Plan 2 Rasputinapi-281357399No ratings yet
- SSymptoms and Symbols A Multiple Code Theory of Somatization Bucciymptoms and Symbols A Multiple Code Theory of Somatization BucciDocument10 pagesSSymptoms and Symbols A Multiple Code Theory of Somatization Bucciymptoms and Symbols A Multiple Code Theory of Somatization BuccishapirafrankNo ratings yet
- Curriculum For Degree in Clinical PsychiatryDocument72 pagesCurriculum For Degree in Clinical PsychiatryEricBoamahNo ratings yet
- Edgerton, R. (1984) Anthropology and Mental Retardation. Research Approaches and OpportunitiesDocument24 pagesEdgerton, R. (1984) Anthropology and Mental Retardation. Research Approaches and Opportunitiesjuanitoendara100% (1)
- York 10 PH DDocument370 pagesYork 10 PH DNAHOMNo ratings yet
- Andreas Hamburger, Camellia Hancheva, Vamık D. Volkan - Social Trauma - An Interdisciplinary Textbook-Springer (2020)Document381 pagesAndreas Hamburger, Camellia Hancheva, Vamık D. Volkan - Social Trauma - An Interdisciplinary Textbook-Springer (2020)Happy_DoraNo ratings yet
- Clinical PsyDocument25 pagesClinical PsyAyesha YaqoobNo ratings yet
- Megill (1987) The Reception of Foucault by HistorianDocument26 pagesMegill (1987) The Reception of Foucault by Historiansashadam815812No ratings yet
- Koehler Interview Gaetano BenedettiDocument15 pagesKoehler Interview Gaetano BenedettijuanpablovildosoNo ratings yet
- LivroDocument256 pagesLivroDaniel Alves De Farias BezerraNo ratings yet
- Madness in Buenos AiresDocument340 pagesMadness in Buenos AiresLaura VanadiaNo ratings yet
- Psychoanalytic Explorations in Music ReviewDocument4 pagesPsychoanalytic Explorations in Music Reviewgonzalovillegas1987No ratings yet
- History of Hypnosis in EUropeDocument5 pagesHistory of Hypnosis in EUropeTom JerryNo ratings yet
- 100 Años de Psiquiatria - KraepelinDocument174 pages100 Años de Psiquiatria - Kraepelinlizardocd100% (2)
- Chapter 02 FreudDocument3 pagesChapter 02 FreudAvtandilGogeshviliNo ratings yet
- FERRO - Clinical Implications of Bion S ThoughtDocument15 pagesFERRO - Clinical Implications of Bion S ThoughtErin SaldiviaNo ratings yet
- Evolutionary Theory, Culture and Psychiatric Diagnosis: Horacio Fabrega JRDocument29 pagesEvolutionary Theory, Culture and Psychiatric Diagnosis: Horacio Fabrega JRPer SabNo ratings yet
- The Body in Adolescence - Psychic Isolation and Physical Symptoms PARTE 2Document16 pagesThe Body in Adolescence - Psychic Isolation and Physical Symptoms PARTE 2vanessa saNo ratings yet
- Ivana S Marková, Eric Chen - Rethinking Psychopathology - Creative Convergences-Springer (2020)Document297 pagesIvana S Marková, Eric Chen - Rethinking Psychopathology - Creative Convergences-Springer (2020)Paco La MadridNo ratings yet
- S Nav Kayg S ProgramDocument43 pagesS Nav Kayg S Programemretaha2424No ratings yet
- (International Perspectives in Philosophy and Psychiatry) Stanghellini, Giovanni - Lost in Dialogue - Anthropology, Psychopathology and Care-Oxford University Press (2017)Document229 pages(International Perspectives in Philosophy and Psychiatry) Stanghellini, Giovanni - Lost in Dialogue - Anthropology, Psychopathology and Care-Oxford University Press (2017)Ignacio VeraNo ratings yet
- Binswanger-Comprendre - IX.7. RovalettiDocument13 pagesBinswanger-Comprendre - IX.7. RovalettimauroNo ratings yet
- Psychosomatic As We KnowDocument5 pagesPsychosomatic As We Knowrqi11No ratings yet
- (Research in Analytical Psychology and Jungian Studies Series) Laner Cassar - Jung's Technique of Active Imagination and Desoille's Directed Waking Dream Method - Bridging The Divide-Routledge (2020)Document233 pages(Research in Analytical Psychology and Jungian Studies Series) Laner Cassar - Jung's Technique of Active Imagination and Desoille's Directed Waking Dream Method - Bridging The Divide-Routledge (2020)novi.2711No ratings yet
- What Is Obsession? Differentiating Obsessive-Compulsive Disorder and The Schizophrenia Spectrum 2022Document8 pagesWhat Is Obsession? Differentiating Obsessive-Compulsive Disorder and The Schizophrenia Spectrum 2022corbanmihai43No ratings yet
- EtikaDocument218 pagesEtikaDragutin PetrićNo ratings yet
- Assister Althusser and FeminismDocument97 pagesAssister Althusser and FeminismfelipeprozasNo ratings yet
- Folk DevilsDocument13 pagesFolk DevilsMatin AgahiNo ratings yet
- Poter, R Whright, D PDFDocument391 pagesPoter, R Whright, D PDFRenan F. NascimentoNo ratings yet
- 7402529Document15 pages7402529Marcus Jason GohmNo ratings yet
- Didier Anzieu Freud's Self-AnalysisDocument329 pagesDidier Anzieu Freud's Self-AnalysisMosica Adela100% (2)
- Compassion and RepressionDocument26 pagesCompassion and RepressionJason DanelyNo ratings yet
- Scharff Sobre FairbairnDocument21 pagesScharff Sobre FairbairnAntonio TariNo ratings yet
- Bourdin, D. (2003) - La Pensée Clinique Clinical Thinking André GreenDocument4 pagesBourdin, D. (2003) - La Pensée Clinique Clinical Thinking André GreenofanimenochNo ratings yet
- BIN Kimura Cogito and I A Bio Logical ApproachDocument7 pagesBIN Kimura Cogito and I A Bio Logical ApproachJorge CarriónNo ratings yet
- Payment PDFDocument35 pagesPayment PDFLauraMariaAndresanNo ratings yet
- Isidor Sadger - Recollecting Freud-The University of Wisconsin Press (2005)Document183 pagesIsidor Sadger - Recollecting Freud-The University of Wisconsin Press (2005)hugoarceNo ratings yet
- J Am Psychoanal Assoc 1999 Mahon 1381 90Document11 pagesJ Am Psychoanal Assoc 1999 Mahon 1381 90Pedro DurãoNo ratings yet
- Psychiatry and Neuroscience UpdateDocument480 pagesPsychiatry and Neuroscience UpdateJessica Silva100% (1)
- Autism: French Psychoanalysis Reported As "Cult-Like" To A French Government's Body by Autism Rights WatchDocument2 pagesAutism: French Psychoanalysis Reported As "Cult-Like" To A French Government's Body by Autism Rights WatchAutismRightsWatchNo ratings yet
- On Certain Similarities Between Spinoza and PsychoanalysisDocument9 pagesOn Certain Similarities Between Spinoza and PsychoanalysisCecilia PaccazochiNo ratings yet
- Hüseyin Köse Torino AtıDocument12 pagesHüseyin Köse Torino AtıAydin KarabulutNo ratings yet
- Franz Alexander, M.D.Document4 pagesFranz Alexander, M.D.زين العابدين فارسNo ratings yet
- Freud Origins of Psychoanalysis Letters To Fliess Part 3Document28 pagesFreud Origins of Psychoanalysis Letters To Fliess Part 3skjfldsfdsdfiojsd100% (1)
- History: 141 True and False Self (1960)Document7 pagesHistory: 141 True and False Self (1960)fazio76No ratings yet
- Volkan, Vamik (2009) - Large-Group Identity, IR and PsychoanalysisDocument8 pagesVolkan, Vamik (2009) - Large-Group Identity, IR and PsychoanalysisADIELruleNo ratings yet
- Freud, Luria and The Clinical Method: Mark SolmsDocument27 pagesFreud, Luria and The Clinical Method: Mark SolmsVALERIA AGUILAR100% (1)
- Journal of the History of the Behavioral Sciences Volume 1 Issue 1 1965 [Doi 10.1002%2F1520-6696%28196501%291%3A1-43%3A%3Aaid-Jhbs2300010107-3.0.Co%3B2-6] George Mora -- The Historiography of Psychiatry and Its DevelopmDocument10 pagesJournal of the History of the Behavioral Sciences Volume 1 Issue 1 1965 [Doi 10.1002%2F1520-6696%28196501%291%3A1-43%3A%3Aaid-Jhbs2300010107-3.0.Co%3B2-6] George Mora -- The Historiography of Psychiatry and Its DevelopmIoanaAlexandraNo ratings yet
- EACME 2011 Conference in Collaboration WDocument329 pagesEACME 2011 Conference in Collaboration WDejan DonevNo ratings yet
- Role of Nutraceuticals in Health Promotion: Swati Chaturvedi, P. K. Sharma, Vipin Kumar Garg, Mayank BansalDocument7 pagesRole of Nutraceuticals in Health Promotion: Swati Chaturvedi, P. K. Sharma, Vipin Kumar Garg, Mayank BansalFree Escort ServiceNo ratings yet
- Inflammation in Schizophrenia and DepressionDocument9 pagesInflammation in Schizophrenia and DepressionFree Escort ServiceNo ratings yet
- Walid Sarhan F. R. C. PsychDocument46 pagesWalid Sarhan F. R. C. PsychFree Escort ServiceNo ratings yet
- ResumeDocument3 pagesResumeFree Escort ServiceNo ratings yet
- Mechanism For The Ability of 5Document2 pagesMechanism For The Ability of 5Free Escort ServiceNo ratings yet
- Nutraceuticals: Let Food Be Your MedicineDocument32 pagesNutraceuticals: Let Food Be Your MedicineFree Escort ServiceNo ratings yet
- Quality by Design On PharmacovigilanceDocument1 pageQuality by Design On PharmacovigilanceFree Escort ServiceNo ratings yet
- Reliability and ValidityDocument15 pagesReliability and Validityapi-260339450No ratings yet
- ABSTRACT (QBD: A Holistic Concept of Building Quality in Pharmaceuticals)Document1 pageABSTRACT (QBD: A Holistic Concept of Building Quality in Pharmaceuticals)Free Escort ServiceNo ratings yet
- Quality Is Built in by Design, Not Tested inDocument1 pageQuality Is Built in by Design, Not Tested inFree Escort ServiceNo ratings yet
- Nutraceutical Role in Health CareDocument1 pageNutraceutical Role in Health CareFree Escort ServiceNo ratings yet
- Reliablity Validity of Research Tools 1Document19 pagesReliablity Validity of Research Tools 1Free Escort Service100% (2)
- Optimizing Quality by Design in Bulk Powder & Solid Dosage: Smt. Bhoyar College of Pharmacy, KamteeDocument3 pagesOptimizing Quality by Design in Bulk Powder & Solid Dosage: Smt. Bhoyar College of Pharmacy, KamteeFree Escort ServiceNo ratings yet
- Bioassay & BiostandardisationDocument51 pagesBioassay & BiostandardisationFree Escort Service100% (1)
- 102i Eng Screen 02Document14 pages102i Eng Screen 02Free Escort ServiceNo ratings yet
- BIOASSAYDocument16 pagesBIOASSAYFree Escort ServiceNo ratings yet
- Tablets:: Tablets May Be Defined As SolidDocument13 pagesTablets:: Tablets May Be Defined As SolidFree Escort ServiceNo ratings yet
- Tablet Coating: Why Coat Tablets?Document12 pagesTablet Coating: Why Coat Tablets?Free Escort ServiceNo ratings yet
- T.Shivakumar: Kottam Institute of Pharmacy Jntu, A.PDocument45 pagesT.Shivakumar: Kottam Institute of Pharmacy Jntu, A.PFree Escort ServiceNo ratings yet
- 2415 14725 4 PBDocument13 pages2415 14725 4 PBFree Escort ServiceNo ratings yet
- The Mysterious Kundalini - TextDocument128 pagesThe Mysterious Kundalini - Textjavierruiz1100% (1)
- Portfolio RubricDocument1 pagePortfolio Rubricpavansohal100% (2)
- Personality Adjectives Lesson PlanDocument5 pagesPersonality Adjectives Lesson PlanMiriam Troya100% (3)
- Spelling Patterns Chart: Pattern: - CeiDocument2 pagesSpelling Patterns Chart: Pattern: - CeiMarko MakovicNo ratings yet
- Chapter 3 RMDocument25 pagesChapter 3 RMfeyisaabera19No ratings yet
- Reflect ls6 Unit Task Rubrics p3 0Document8 pagesReflect ls6 Unit Task Rubrics p3 0Stephen LindhorstNo ratings yet
- Specific Directions For The Administration of The PhilDocument4 pagesSpecific Directions For The Administration of The PhilMELANIE GALSIMNo ratings yet
- Final LEADMGT Research PaperDocument18 pagesFinal LEADMGT Research PaperJosephNo ratings yet
- Life ChangesDocument6 pagesLife Changesmichelenrique20058107No ratings yet
- NCP For CHNDocument2 pagesNCP For CHNJhielo ArambulaNo ratings yet
- Cognitive Behavioral TheoryDocument28 pagesCognitive Behavioral TheoryAngela CabasNo ratings yet
- Unit 4 Text - Flowers For AlgernonDocument116 pagesUnit 4 Text - Flowers For AlgernonJuan-Pablo HernandezNo ratings yet
- Bibliography of Sexuality Studies in Latin AmericaDocument99 pagesBibliography of Sexuality Studies in Latin AmericaivnsmrnwNo ratings yet
- Zhang 2018Document11 pagesZhang 2018Asmadera Mat EsaNo ratings yet
- Syllabus JDM CourseDocument4 pagesSyllabus JDM CourseAlberto ForteNo ratings yet
- The Beginners Guide To Self HypnosisDocument34 pagesThe Beginners Guide To Self Hypnosisdesie100% (7)
- Harish Chander, "Evil and Religion in Langston Hughes' - Tambourines To Glory - "Document22 pagesHarish Chander, "Evil and Religion in Langston Hughes' - Tambourines To Glory - "PACNo ratings yet
- Zeigarnik - 1987 - Loss of SpontaneityDocument13 pagesZeigarnik - 1987 - Loss of SpontaneityHansel SotoNo ratings yet
- The Psychology of Cybercriminals by AbijinNSDocument9 pagesThe Psychology of Cybercriminals by AbijinNSNs AbijinNo ratings yet
- Effectively Manage Workplace DiversityDocument5 pagesEffectively Manage Workplace Diversityrao_pooja13No ratings yet
- Search ResultsDocument2 pagesSearch ResultsM. Najam us Saqib Qadri al HanbliNo ratings yet
- De Thi HSG BC 2021Document5 pagesDe Thi HSG BC 2021Do Minh LoiNo ratings yet
- Hope For The Flowers Reaction PaperDocument1 pageHope For The Flowers Reaction PaperAilendeLunaNo ratings yet
- Sultan Kuradat Islamic Academy Foundation College Bulalo, Sultan Kudarat, MaguindanaoDocument27 pagesSultan Kuradat Islamic Academy Foundation College Bulalo, Sultan Kudarat, MaguindanaoJaharaJaneDacunganKatingNo ratings yet
- Left and Right Brain DominanceDocument34 pagesLeft and Right Brain DominanceCHRISTIAN EANo ratings yet
- Leadership & Organization SyllabusDocument10 pagesLeadership & Organization SyllabusahamiltonscribdNo ratings yet





























































![Journal of the History of the Behavioral Sciences Volume 1 Issue 1 1965 [Doi 10.1002%2F1520-6696%28196501%291%3A1-43%3A%3Aaid-Jhbs2300010107-3.0.Co%3B2-6] George Mora -- The Historiography of Psychiatry and Its Developm](https://imgv2-1-f.scribdassets.com/img/document/267327584/149x198/90a332a96f/1433180658?v=1)