Professional Documents
Culture Documents
A Case of Choroidal Neovascularization Secondary To Unilateral Retinal Pigment Epithelium Dysgenesis
A Case of Choroidal Neovascularization Secondary To Unilateral Retinal Pigment Epithelium Dysgenesis
Uploaded by
dedypurnamaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Case of Choroidal Neovascularization Secondary To Unilateral Retinal Pigment Epithelium Dysgenesis
A Case of Choroidal Neovascularization Secondary To Unilateral Retinal Pigment Epithelium Dysgenesis
Uploaded by
dedypurnamaCopyright:
Available Formats
Case Rep Ophthalmol 2014;5:3437
DOI: 10.1159/000358426
Published online: January 22, 2014
2014 S. Karger AG, Basel
16632699/14/00510034$39.50/0
www.karger.com/cop
This is an Open Access article licensed under the terms of the Creative Commons
Attribution-NonCommercial 3.0 Unported license (CC BY-NC) (www.karger.com/OA-
license), applicable to the online version of the article only. Distribution permitted for non-
commercial purposes only.
Hisanori Imai, MD, PhD
Department of Ophthalmology
Kobe Kaisei Hospital
3-11-15 Shinoharakitamati, Nada-ku, Kobe 657-0068 (Japan)
E-Mail imai@kobe-kaisei.org
A Case of Choroidal
Neovascularization Secondary to
Unilateral Retinal Pigment
Epithelium Dysgenesis
Tsuyoshi Shimoyama
a, b
Hisanori Imai
a, b
Shigeru Honda
a
Akira Negi
a
a
Division of Ophthalmology, Department of Organ Therapeutics, Kobe University
Graduate School of Medicine, and
b
Department of Ophthalmology, Kobe Kaisei Hospital,
Kobe, Japan
Key Words
Unilateral retinal pigment epithelium dysgenesis Anti-VEGF Bevacizumab Choroidal
neovascularization Triamcinolone Fundus autofluorescence
Abstract
Aim: To report a case of choroidal neovascularization secondary to unilateral retinal pigment
epithelium dysgenesis (URPED), which was resistant to posterior subtenon injection of
triamcinolone acetonide (STTA) and intravitreal bevacizumab injection (IVB). Case Report: An
8-year-old boy was referred to us because of a unilateral unique clinical appearance on
funduscopic examination in his left eye (OS). A geometric lesion at the retinal pigment
epithelium level of the interpapillomacular area was disclosed OS. The optic nerve was
slightly hyperemic OS. Findings from the right fundus examination were normal. Based on
these characteristic findings, he was diagnosed as having URPED. Best corrected Landolt ring
chart visual acuity (BCVA) was 1.0 in both eyes. Twenty-three months after the first visit, the
patient presented with visual disturbance OS. Funduscopic examination showed an
expansion of the geometric lesion and the development of a subfoveal choroidal neovascu-
larization (CNV). BCVA was 0.4 OS. Two-time STTA (40 mg/1 ml) was performed at the onset
of CNV and 6 months later, and additional IVB (1.25 mg/0.05 ml) was done 10 months later
for the treatment of CNV, but the geometric lesion and CNV were resistant to the treatment
and continued to expand. Seven years after the first visit, the geometric lesion and the CNV
kept expanding steadily. Conclusion: URPED is a rare clinical entity, and the prognosis of this
disease is still unclear. The visual prognosis may depend on whether CNV fully develops.
2014 S. Karger AG, Basel
D
o
w
n
l
o
a
d
e
d
b
y
:
2
0
2
.
6
7
.
4
4
.
6
6
-
2
/
1
0
/
2
0
1
4
5
:
0
5
:
3
5
P
M
Case Rep Ophthalmol 2014;5:3437
DOI: 10.1159/000358426
2014 S. Karger AG, Basel
www.karger.com/cop
Shimoyama et al.: A Case of Choroidal Neovascularization Secondary to Unilateral
Retinal Pigment Epithelium Dysgenesis
35
Introduction
Unilateral retinal pigment epithelium dysgenesis (URPED) is a rare clinical entity [13].
It is characterized by a unilateral occurrence in young patients and consists of a round
affected area with a distinct scalloped margin of reticular retinal pigment epithelium (RPE)
hyperplasia, mid-lesion lacunae of RPE hyperplasia, central thinning and atrophy of RPE. The
findings of fundus autofluorescence (FAF) and fluorescein angiography (FA) are the most
important when diagnosing URPED. The visual prognosis of URPED is still unclear, but it
may depend on whether choroidal neovascularization (CNV) will develop [1].
In this report, we present a case of CNV associated with URPED, which was resistant to
the treatment with posterior subtenon injection of triamcinolone acetonide (STTA) and
intravitreal bevacizumab injection (IVB).
Case Report
An 8-year-old boy was referred to us because of a unilateral unique funduscopic ap-
pearance in the left eye (OS). Funduscopic findings revealed a geometric lesion at the RPE
level of the interpapillomacular area, contiguous with the slightly hyperemic optic nerve (fig.
1). The lesion was composed of marginal RPE hyperplasia and atrophic RPE in its center.
Findings from the right fundus examination were normal. Based on these characteristic
findings, the patient was diagnosed with URPED. Best corrected Landolt ring chart visual
acuity (BCVA) was 1.0 in both eyes. Twenty-three months after the first visit, he presented
with visual disturbance OS. Funduscopic examination showed enlargement of the lesion and
development of subfoveal CNV (fig. 2). FA findings revealed hypofluorescence from RPE
hyperplasia, hyperfluorescence from RPE atrophy and dye leakage from the optic nerve and
CNV (fig. 2). Optical coherence tomography (OCT) revealed type 2 CNV, but the exudative
change was not obvious (fig. 2). The patients BCVA was 0.4 OS. Two-time STTA (40 mg/1
ml) was performed at the onset of CNV and 6 months later. Additional IVB (1.25 mg/0.05 ml)
was performed 10 months later for the treatment of CNV. Both STTA and IVB were
performed with the written informed consent from both the patient and his father as well as
with an approval of the institutional review board of Kobe University of Medicine and the
Tenets of the Declaration of Helsinki. Despite the treatment, the geometric lesion and CNV
were resistant to the treatment and expanded gradually. Seven years after the first visit, the
geometric lesion and the CNV kept expanding steadily, and new CNV developed at the
inferior retina (fig. 3).
Discussion
Cohen et al. [2] first reported 4 cases of this unique fundus lesion in 2002. In their study,
2 of 4 cases were complicated by CNV. Finally, in 2009, they proposed naming this disorder
URPED and reported that 2 of 9 cases were affected by CNV [1]. We believe that this is the
first follow-up report which can provide new clinical information about this disease because
Cohen et al. [1, 2] did not mention the course of CNV treatment.
In our case, CNV did not respond to both STTA and IVB. Systemic steroids, immunosup-
pressants or additional STTA and IVB might be effective to achieve the quieting effect of this
highly active CNV, but we did not impose them because the patient was still experiencing
periods of growth. Generally, regardless of the treatment, CNV suppresses eventually with
D
o
w
n
l
o
a
d
e
d
b
y
:
2
0
2
.
6
7
.
4
4
.
6
6
-
2
/
1
0
/
2
0
1
4
5
:
0
5
:
3
5
P
M
Case Rep Ophthalmol 2014;5:3437
DOI: 10.1159/000358426
2014 S. Karger AG, Basel
www.karger.com/cop
Shimoyama et al.: A Case of Choroidal Neovascularization Secondary to Unilateral
Retinal Pigment Epithelium Dysgenesis
36
RPE proliferation, which is one of the remodeling processes of wound repairing. In our case,
we could not observe RPE proliferation around CNV during the follow-up period. On the
contrary, new CNV developed at the inferior retina. Furthermore, the geometric lesion was
significantly enlarged over the RPE hyperplasia. These findings may suggest that the
congenital RPE malfunction, which spreads across a wide area of the fundus, is the
underlying reason for the development of this disease.
Our case is unique because we observed the hyperemic optic nerve OS at the first visit.
In the previous report, Cohen et al. [1] stated that the affected area is usually contiguous
with the optic nerve, but they did not mention the condition of the optic nerve itself. It is
possible that the inflammation of the optic nerve is one of the triggers in the development of
this unique pattern of the fundus.
To summarize, we propose that patients who develop CNV secondary to URPED should
be informed carefully and always be followed up for treatment-resistant CNV.
References
1 Cohen SY, Fung AE, Tadayoni R, Massin P, Barbazetto I, Berthout A, Gayet P, Meunier I, Yannuzzi LA:
Unilateral retinal pigment epithelium dysgenesis. Am J Ophthalmol 2009;148:914919.
2 Cohen SY, Massin P, Quentel G: Clinicopathologic reports, case reports, and small case series: unilateral,
idiopathic leopard-spot lesion of the retinal pigment epithelium. Arch Ophthalmol 2002;120:512516.
3 Berthout A, Malthieu D, Taboureau E, Milazzo S: Unilateral idiopathic leopard-spot lesion of the retinal
pigment epithelium: a fibroglial tractional complication (in French). J Fr Ophtalmol 2008;31:716.
Fig. 1. Funduscopic findings at the first visit. Funduscopic findings OS revealed a geometric lesion at the
RPE level of the interpapillomacular area, contiguous with the slightly hyperemic optic nerve. The lesion
was composed of marginal RPE hyperplasia and atrophic RPE in its center. Findings from the right fundus
examination were normal.
D
o
w
n
l
o
a
d
e
d
b
y
:
2
0
2
.
6
7
.
4
4
.
6
6
-
2
/
1
0
/
2
0
1
4
5
:
0
5
:
3
5
P
M
Case Rep Ophthalmol 2014;5:3437
DOI: 10.1159/000358426
2014 S. Karger AG, Basel
www.karger.com/cop
Shimoyama et al.: A Case of Choroidal Neovascularization Secondary to Unilateral
Retinal Pigment Epithelium Dysgenesis
37
Fig. 2. Twenty-three months after the first visit, the enlargement of the lesion and the development of
subfoveal CNV were observed (upper left: funduscopic findings, lower left: OCT findings). FA findings
revealed dye leakage from the optic nerve and CNV (upper right: early-phase image, upper left: late-phase
image).
Fig. 3. Seven years after the first visit, the geometric lesion and CNV kept expanding steadily and new CNV
developed at the inferior retina (upper: panoramic funduscopic findings, bottom: panoramic FA findings).
D
o
w
n
l
o
a
d
e
d
b
y
:
2
0
2
.
6
7
.
4
4
.
6
6
-
2
/
1
0
/
2
0
1
4
5
:
0
5
:
3
5
P
M
You might also like
- High Myopia and Glaucoma Susceptibility The Beijing Eye StudyDocument5 pagesHigh Myopia and Glaucoma Susceptibility The Beijing Eye StudyDickyStevanoZukhriNo ratings yet
- THE EIGHT PRINCIPLES OF TAI CHI CHUAN - Energy Arts - Learn Tai (PDFDrive - Com) (1) 8885162263945383523 PDFDocument47 pagesTHE EIGHT PRINCIPLES OF TAI CHI CHUAN - Energy Arts - Learn Tai (PDFDrive - Com) (1) 8885162263945383523 PDFTakis Abatzopoulos100% (1)
- ACCP - Comprehensive Medication Management in Team-Based CareDocument8 pagesACCP - Comprehensive Medication Management in Team-Based CareThuane SalesNo ratings yet
- GastroenteritisDocument29 pagesGastroenteritisKatherine 'Chingboo' Leonico Laud100% (8)
- Journal Casereport 1Document5 pagesJournal Casereport 1Arif MohammadNo ratings yet
- Shin2016 Retinal Pigment Epithelium Wound Healing After Traumatic Choroidal RuptureDocument5 pagesShin2016 Retinal Pigment Epithelium Wound Healing After Traumatic Choroidal RuptureMilzan MurtadhaNo ratings yet
- Behcet DiseaseDocument6 pagesBehcet DiseasejbahalkehNo ratings yet
- Spectral-Domain Optical Coherence Tomographic Findings at Each Stage of Punctate Inner Choroidopathy Zhang2013Document6 pagesSpectral-Domain Optical Coherence Tomographic Findings at Each Stage of Punctate Inner Choroidopathy Zhang2013kubi.ilskiNo ratings yet
- Laporan Kasus NeurooftalmologiDocument12 pagesLaporan Kasus NeurooftalmologiPradistya Syifa YudiasariNo ratings yet
- 2023 Article 32184Document10 pages2023 Article 32184Diana TricoracheNo ratings yet
- Alsberg 1 s2.0 S2451993621002279 MainDocument5 pagesAlsberg 1 s2.0 S2451993621002279 MainDoug PulaNo ratings yet
- Orbital Apex Syndrome Secondary To Herpes Zoster OphthalmicusDocument4 pagesOrbital Apex Syndrome Secondary To Herpes Zoster OphthalmicusYosiita KartinaaNo ratings yet
- EED Uveitis 4 Get - FileDocument3 pagesEED Uveitis 4 Get - FileAmirahShalehaNo ratings yet
- Ophthal Notes PGDocument6 pagesOphthal Notes PGSwati TyagiNo ratings yet
- Ni Hms 12505Document10 pagesNi Hms 12505noorhadi.n10No ratings yet
- A Case of Angle-Closure Glaucoma, Cataract, Nanophthalmos and Spherophakia in Oculo-Dento-Digital SyndromeDocument3 pagesA Case of Angle-Closure Glaucoma, Cataract, Nanophthalmos and Spherophakia in Oculo-Dento-Digital SyndromeSriana K. LaliyoNo ratings yet
- Moon2019 PDFDocument7 pagesMoon2019 PDFGusti Zidni FahmiNo ratings yet
- Parade Wspos Tipe 2Document3 pagesParade Wspos Tipe 2irwan_201291No ratings yet
- Masquerade SyndromesDocument10 pagesMasquerade Syndromestony_chrisNo ratings yet
- Esferofauia Aislada y GlaucomaDocument3 pagesEsferofauia Aislada y GlaucomaManuel VasquezNo ratings yet
- Classification of Visual Field Abnormalities in Highly Myopic Eyes Without Pathologic ChangeDocument26 pagesClassification of Visual Field Abnormalities in Highly Myopic Eyes Without Pathologic Change钟华No ratings yet
- Herpes Zoster OphthalmicusDocument12 pagesHerpes Zoster OphthalmicusGio Vano NaihonamNo ratings yet
- Choroidal and Retinal Thickening in Severe Preeclampsia: RetinaDocument7 pagesChoroidal and Retinal Thickening in Severe Preeclampsia: RetinaAssifa RidzkiNo ratings yet
- Sympathetic Ophthalmia After Vitreoretinal Surgery: A Report of Two CasesDocument11 pagesSympathetic Ophthalmia After Vitreoretinal Surgery: A Report of Two CasesAlexander RezaNo ratings yet
- The Ocular Biometric and Corneal Topographic Characteristics of High-Anisometropic Adults in TaiwanDocument6 pagesThe Ocular Biometric and Corneal Topographic Characteristics of High-Anisometropic Adults in TaiwanNurul Falah KalokoNo ratings yet
- Neuroretinitis Syphilis in Human Immunodeficiency Virus-Infected PatientDocument6 pagesNeuroretinitis Syphilis in Human Immunodeficiency Virus-Infected PatientAnindya AgrasidiNo ratings yet
- PIIS0002939422003890Document9 pagesPIIS0002939422003890Anca Florina GaceaNo ratings yet
- Neurosyphilis Masquerading As An Acute Adie's Tonic Pupil: Report of A CaseDocument6 pagesNeurosyphilis Masquerading As An Acute Adie's Tonic Pupil: Report of A CaseOlvaria MisfaNo ratings yet
- Francisco Trincão, João Feijão, Vítor Maduro, Nuno Alves, Carlos Batalha, Pedro Candelária, José Pita-NegrãoDocument1 pageFrancisco Trincão, João Feijão, Vítor Maduro, Nuno Alves, Carlos Batalha, Pedro Candelária, José Pita-NegrãoVitor MaduroNo ratings yet
- Pi Is 0161642022006923Document12 pagesPi Is 0161642022006923Anca Florina GaceaNo ratings yet
- The Pathogenesis of Optic Neuritis Caused by Angiostrongylus Cantonensis in BALB/c MiceDocument12 pagesThe Pathogenesis of Optic Neuritis Caused by Angiostrongylus Cantonensis in BALB/c Miceracut_khansatraNo ratings yet
- Bilateral Congenital Toxoplasmosis Complicated by Choroidal Neo-Vessels A Case ReportDocument3 pagesBilateral Congenital Toxoplasmosis Complicated by Choroidal Neo-Vessels A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Staphylococcus Epidermidis End PDFDocument4 pagesStaphylococcus Epidermidis End PDFNisaNo ratings yet
- Steptoe Et Al. - 2020 - Evolving Longitudinal Retinal Observations in A CoDocument9 pagesSteptoe Et Al. - 2020 - Evolving Longitudinal Retinal Observations in A Copaul steptoeNo ratings yet
- BR J Ophthalmol-2014-Chan-79-81 PDFDocument4 pagesBR J Ophthalmol-2014-Chan-79-81 PDFRomi Mauliza FauziNo ratings yet
- 1 s2.0 S1350946217300599 MainDocument15 pages1 s2.0 S1350946217300599 MainPatricia RodriguesNo ratings yet
- Case Report Diabetic Retinopaty in EnglishDocument13 pagesCase Report Diabetic Retinopaty in Englishsasha anka DilanNo ratings yet
- American Journal of Ophthalmology Case ReportsDocument3 pagesAmerican Journal of Ophthalmology Case ReportsElison Jaya PanggaloNo ratings yet
- Acute Retinal Necrosis Following Contralateral Herpes Zoster OphthalmicusDocument4 pagesAcute Retinal Necrosis Following Contralateral Herpes Zoster Ophthalmicusnurul_sharaswatiNo ratings yet
- Granuloma Epididimitisarticle-2Document4 pagesGranuloma Epididimitisarticle-2Feby Kurnia PutriNo ratings yet
- Management of Double-Penetrating Ocular Injury With Retained Intraorbital Metallic Foreign BodyDocument4 pagesManagement of Double-Penetrating Ocular Injury With Retained Intraorbital Metallic Foreign BodyShirakawa AlmiraNo ratings yet
- Bjophthalmol 2019 315520.fullDocument5 pagesBjophthalmol 2019 315520.fullRemNo ratings yet
- Management of Submacula Bleeding With Pneumatic DisplacementDocument8 pagesManagement of Submacula Bleeding With Pneumatic DisplacementNaufal Hilmi MarzuqNo ratings yet
- Is Episcleritis Associated To Glaucoma?Document3 pagesIs Episcleritis Associated To Glaucoma?Alvin JulianNo ratings yet
- 1600-Article Text-5930-1-10-20231002Document12 pages1600-Article Text-5930-1-10-20231002Yunisa astiaraniNo ratings yet
- 100152-Article Text-841-1-10-20210226Document5 pages100152-Article Text-841-1-10-20210226Rachel DenonaNo ratings yet
- Faure 2017Document8 pagesFaure 2017zazaza94No ratings yet
- Tonic Pupil and Corneal Anesthesia After Vitrectomy and Encircling Band For Retinal Detachment in An Ex-Premature ChildDocument5 pagesTonic Pupil and Corneal Anesthesia After Vitrectomy and Encircling Band For Retinal Detachment in An Ex-Premature ChildOlvaria MisfaNo ratings yet
- Opth 9 1041Document7 pagesOpth 9 1041petrarizkyNo ratings yet
- Tumor OrbitaDocument4 pagesTumor OrbitaIda Bagus Deny PrayudiNo ratings yet
- Ojoph 2022111815222395Document12 pagesOjoph 2022111815222395budi rahmawatiNo ratings yet
- None 3Document11 pagesNone 3Yehiel FlaviusNo ratings yet
- White Dot Syndromes Harvey S. Uy, M.DDocument11 pagesWhite Dot Syndromes Harvey S. Uy, M.DShimaa MersalNo ratings yet
- Rapidly Progressive Severe Proptosis Esthesioneuroblastoma Case ReportDocument5 pagesRapidly Progressive Severe Proptosis Esthesioneuroblastoma Case ReportSSR-IIJLS JournalNo ratings yet
- Perilimbal Conjunctival Pigmentation in Chinese Patients With Vernal KeratoconjunctivitisDocument4 pagesPerilimbal Conjunctival Pigmentation in Chinese Patients With Vernal KeratoconjunctivitisDwi HardiyantiNo ratings yet
- Highlights in Neuro OphthalmologyDocument2 pagesHighlights in Neuro OphthalmologyShruthi VMNo ratings yet
- Jurnal Mata 5Document6 pagesJurnal Mata 5Dahru KinanggaNo ratings yet
- Journal Pre-Proof: Annals of Medicine and SurgeryDocument23 pagesJournal Pre-Proof: Annals of Medicine and SurgeryDaniel GuevaraNo ratings yet
- Retinal Pigment Epithelium Tear in VKH DiseaseDocument3 pagesRetinal Pigment Epithelium Tear in VKH DiseasePhilip McNelsonNo ratings yet
- Retina 39 426Document9 pagesRetina 39 426ryaalwiNo ratings yet
- IndianJOphthalmol632164-4403297 121352Document3 pagesIndianJOphthalmol632164-4403297 121352Mohammad Abdullah BawtagNo ratings yet
- Fungal Keratitis and Ocular Surface Squamous Neoplasia in A HIV Positive PatientDocument4 pagesFungal Keratitis and Ocular Surface Squamous Neoplasia in A HIV Positive PatientSherly AsrianiNo ratings yet
- Ijeb 48 (7) 642-650Document9 pagesIjeb 48 (7) 642-650dedypurnamaNo ratings yet
- Intoxication GuidelinesDocument3 pagesIntoxication GuidelinesdedypurnamaNo ratings yet
- Special TopicDocument7 pagesSpecial TopicdedypurnamaNo ratings yet
- (Melastoma Malabathricum L.), Moist Exposed Burn Ointment (MEBO) andDocument2 pages(Melastoma Malabathricum L.), Moist Exposed Burn Ointment (MEBO) anddedypurnamaNo ratings yet
- A Toolkit For Women's Empowerment and Leadership in Health and WelfareDocument56 pagesA Toolkit For Women's Empowerment and Leadership in Health and WelfarededypurnamaNo ratings yet
- Corneal Transplantation at An Ophthalmological Referral Center in Colombia: Indications and Techniques (2004-2011)Document4 pagesCorneal Transplantation at An Ophthalmological Referral Center in Colombia: Indications and Techniques (2004-2011)dedypurnamaNo ratings yet
- Refractive Surgery: The Never Ending Task of Improving Vision CorrectionDocument2 pagesRefractive Surgery: The Never Ending Task of Improving Vision CorrectiondedypurnamaNo ratings yet
- Pharma ExamDocument10 pagesPharma Examteabagman0% (1)
- Smart Sensor 4 Gases AS8900 - Manual de OperaçãoDocument12 pagesSmart Sensor 4 Gases AS8900 - Manual de OperaçãoRogerioPascualNo ratings yet
- Nasopharyngeal Carcinoma in Children and AdolescentsDocument5 pagesNasopharyngeal Carcinoma in Children and AdolescentsSyifa MunawarahNo ratings yet
- Famco Important ChaptersDocument7 pagesFamco Important ChaptersFiryal BalushiNo ratings yet
- Details of NACO Supported Blood BanksDocument2 pagesDetails of NACO Supported Blood BanksRajeev SinghNo ratings yet
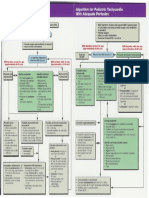
- Pediatric Tachycardia AlgorithmsDocument1 pagePediatric Tachycardia AlgorithmsGalih FatoniNo ratings yet
- Msds Guano DiscsDocument5 pagesMsds Guano Discsapi-289433849No ratings yet
- Top Dental Schools - Admission RequirementsDocument10 pagesTop Dental Schools - Admission RequirementsDental school admission0% (1)
- A Hands-On Guide For Essbase Report ScriptDocument9 pagesA Hands-On Guide For Essbase Report ScriptAmit SharmaNo ratings yet
- Hindu Ast.Document418 pagesHindu Ast.ANANTHPADMANABHAN100% (1)
- Spectrum - Bone Densitometry WOrkshopDocument16 pagesSpectrum - Bone Densitometry WOrkshopanbufelix1939No ratings yet
- Aitecs 3017 DATASHEETDocument2 pagesAitecs 3017 DATASHEETJose Antonio Diaz FierrezNo ratings yet
- Đề Thi Vào 10 Chuyên Anh Đáp Án ĐỀ THI THỬ LẦNDocument7 pagesĐề Thi Vào 10 Chuyên Anh Đáp Án ĐỀ THI THỬ LẦNVân OriNo ratings yet
- Changes in PregnancyDocument13 pagesChanges in PregnancyZarlyn MirafloresNo ratings yet
- ADRnewReporting Form 1.4Document2 pagesADRnewReporting Form 1.4Sourabh kundara50% (2)
- Aroma TherapyDocument14 pagesAroma Therapysandhyapanicker1988No ratings yet
- AGS 2023 BEERS PocketDocument9 pagesAGS 2023 BEERS Pocketerika avelina rodriguez jaureguiNo ratings yet
- JACKSON V AEGLive April 30th RICHARD SENEFF/ Martinez DetectiveDocument208 pagesJACKSON V AEGLive April 30th RICHARD SENEFF/ Martinez DetectiveTeamMichael100% (1)
- Rice Bran Healthy OilDocument25 pagesRice Bran Healthy OilMusheer BashaNo ratings yet
- Digestion Enzyme Practice TestDocument15 pagesDigestion Enzyme Practice TestJila HafiziNo ratings yet
- Iksir-e-Badan (Elixir) : Unique Influence From Unani Medicine - A ReviewDocument6 pagesIksir-e-Badan (Elixir) : Unique Influence From Unani Medicine - A ReviewAmjad NaseerNo ratings yet
- General and Local AnesthesiaDocument1 pageGeneral and Local Anesthesiaahmedhelper300No ratings yet
- Critical Care EnvironmentDocument16 pagesCritical Care EnvironmentJeffrey KauvaNo ratings yet
- Pharmacology Connections To Nursing Practice 3rd Edition Adams Test Bank 1Document32 pagesPharmacology Connections To Nursing Practice 3rd Edition Adams Test Bank 1matthew100% (57)
- Management of Cutaneous ErythrasmaDocument11 pagesManagement of Cutaneous ErythrasmaDesi RatnaningtyasNo ratings yet
- SAI's vs. STD'S: - Syphilis - Chlamydia - Vaginitis - Herpes - GonnorheaDocument25 pagesSAI's vs. STD'S: - Syphilis - Chlamydia - Vaginitis - Herpes - GonnorheaMark CheneyNo ratings yet
- Rajiv Gandhi University of Health Sciences Bangalore, KarnatakaDocument16 pagesRajiv Gandhi University of Health Sciences Bangalore, KarnatakaYadnya SaputraNo ratings yet