Professional Documents
Culture Documents
Pulmonary Hemorrhage in Henoch-Schönlein Purpura: Case Report and Systematic Review of The English Literature
Pulmonary Hemorrhage in Henoch-Schönlein Purpura: Case Report and Systematic Review of The English Literature
Uploaded by
Iwan MiswarOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pulmonary Hemorrhage in Henoch-Schönlein Purpura: Case Report and Systematic Review of The English Literature
Pulmonary Hemorrhage in Henoch-Schönlein Purpura: Case Report and Systematic Review of The English Literature
Uploaded by
Iwan MiswarCopyright:
Available Formats
Pulmonary Hemorrhage in Henoch-Schnlein Purpura:
Case Report and Systematic Review of the English Literature
Srinivas Rajagopala, MD, DM,* Vineeta Shobha, MD, DM,
Uma Devaraj, DNB,
George DSouza, MD, DNB,
and Isha Garg, MD
Background: Diffuse alveolar hemorrhage (DAH) is a rare complication of Henoch-Schnlein
purpura (HSP) and data on its prevalence, management, and outcomes are scant.
Objectives: To enable evidence-based management of DAH in HSP.
Methods: A case report and a systematic review were conducted of all reported cases of DAH
complicating HSP in the English literature.
Results: DAH predominantly affects older male children and adults with HSP. The occurrence of
DAHin HSP is rare and the reported prevalence ranged from0.8%to 5%. DAHoccurred variably
after the diagnosis of HSP, ranging from 2 days to 18 years. Hemoptysis (75%), drop in hemo-
globin (74%), and chest inltrates (94%) were the most common clinical ndings. Lung biopsy
showed leukocytoclastic vasculitis with alveolar hemorrhage (69.2%) or only alveolar hemorrhage
(31.8%) with variable IgA staining by immunouorescence. DAHwas frequently severe and 50%
of the patients required mechanical ventilation. Cyclophosphamide and pulse methylprednisolone
for DAH was associated with better outcomes, particularly in patients who were already receiving
steroids at the time of DAH. Steroids and immunosuppressants were administered for a median
duration of 9 and 4.5 months, respectively. Systemic recurrences (27.7%) and recurrences of DAH
(8.3%) were frequent. DAHwas associated with high mortality (27.6%) and morbidity (persistent
urinary abnormalities, 12%; chronic renal failure, 9%; complications of therapy, 27%).
Conclusions: DAH is a life-threatening complication in HSP. Current protocols use pulse meth-
ylprednisolone and cyclophosphamide for 6 months.
2013 Elsevier Inc. All rights reserved. Semin Arthritis Rheum 42:391-400
Keywords: diffuse alveolar hemorrhage, Henoch-Schnlein purpura, hemoptysis, respiratory failure
H
enoch-Schnlein purpura (HSP) is a small-ves-
sel vasculitis presenting with a tetrad of cutane-
ous purpura, arthritis, abdominal pain, and
nephritis. HSP usually affects children and is an acute,
self-limited illness that lasts about 4 weeks with recur-
rences in 25%. Diffuse alveolar hemorrhage (DAH) is an
unusual complication of HSP and data on its frequency,
management, and outcomes are scant. We describe a clas-
sic case of DAHoccurring in HSP and reviewall reported
cases of DAHcomplicating HSP in the English literature.
CASE REPORT
A 55-year-old man presented with a rash over his legs and
back, abdominal pain, joint pain, and hematochezia of 15
days duration. He was a farmer by occupation, did not
smoke or drink alcohol, and did not have any signicant
past medical history. On examination he was afebrile,
normotensive, with respiratory rate of 16 breaths/min
and a pulse rate of 100 beats/min. He had extensive non-
palpable purpura over the legs and back, pedal edema, and
joint tenderness in the knee, ankle, and interphalangeal
joints of both upper limbs. The rest of the physical exam-
ination was unremarkable. Investigations showed a he-
moglobin count of 11.3 g/dl (normal 12 to 14) and a
platelet count of 2.34 10
5
/l (normal 1.5 to 4.5 10
5
)
*Department of Pulmonology, St Johns Medical College Hospital, Sarjapur Road,
Bangalore, India.
Department of Medicine, St Johns Medical College Hospital, Sarjapur Road,
Bangalore, India.
Department of Pathology, St Johns Medical College Hospital, Sarjapur Road,
Bangalore, India.
The authors have no conicts of interest to disclose.
Address reprint requests to Srinivas Rajagopala, MD, DM, Consultant, Department
of Pulmonary Medicine, Liver Intensive Care, Global Hospitals and Health City,
Perumbakkam, Chennai, India 600100. E-mail: visitsrinivasan@gmail.com.
VASCULITIS
391 0049-0172/13/$-see front matter 2013 Elsevier Inc. All rights reserved.
http://dx.doi.org/10.1016/j.semarthrit.2012.07.004
with normal leukocyte counts. Urine examination re-
vealed 10 to 12 leukocytes/hpf (normal 2 to 3/hpf), 6 to 8
erythrocytes/hpf with albuminuria; no casts were ob-
served. Serum creatinine was 0.9 mg/dl (normal 0.6 to
1.0). Ultrasound of the abdomen showed wall thickening
of the jejunum and minimal ascites. Stool occult blood
was positive. Human immunodeciency virus enzyme-
linked immunosorbent assay, antinuclear antibody,
antineutrophil cytoplasmic antibody by immunouores-
cence, andn antiglomerular basement antibody enzyme-
linked immunosorbent assay tests were all negative.
Twenty-four-hour urine protein was 3.94 g/24 h/m
2
(normal 30 g). Liver function tests, electrocardio-
gram, and chest radiographs were normal. Skin biopsy
showed evidence of leukocytoclastic vasculitis; immuno-
uorescence showed pericapillary IgA and C3 deposition
(Fig. 2). Renal biopsy showed evidence of focal prolifera-
tive glomerulonephritis and IgA/C3 deposition (Fig. 3).
Colonoscopy was normal. A diagnosis of HSP with focal
segmental glomerulonephritis and gastrointestinal bleed
was made. He was started on 1 mg/kg prednisolone, and
pantoprazole on day 4 of admission; his joint pains and
gastrointestinal bleed subsided. On day 7 of admission, he
developed sudden breathlessness, hemoptysis, and cough.
Chest radiographs showed bilateral consolidation (Fig. 1,
left) with a drop in hemoglobin (7.6 g/dl). Arterial blood
gas analysis showed PaO
2
/FiO
2
of 325 (normal 450 to
500), PaCO
2
of 30 mmHg (normal 40 4), HCO
3
of 22
mm Hg (normal 24 4), and pH 7.48 (normal, 7.40
0.04). Repeat electrocardiogramwas normal and echocar-
diography conrmed normal ejection fraction with no
valvular defects or evidence of infective endocarditis.
Bronchoscopy was normal; bronchoalveolar lavage uid
showed numerous hemosiderin-laden macrophages. Adi-
agnosis of DAH was made, and oxygen at 2 l/min, 1 g/d
pulse methylprednisolone for 3 days, and pulse cyclo-
phosphamide 750 mg/m
2
were administered; 1 mg/kg
prednisolone was continued after 3 days. He became
asymptomatic with normalization of ndings on Chest
Radiography (Fig. 1, right) and was discharged on day 21
of admission. However, his course was complicated by
recurrent gastrointestinal bleed, worsening edema, and a
urinary tract infection. He was initiated on diuretics, enal-
april and levooxacin. Cyclophosphamide was subse-
quently changed to azathioprine because of persistent
neutropenia. He remains asymptomatic at 6 months of
follow-up on 10 mg prednisolone and azathioprine but
has persistent albuminuria.
MATERIALS AND METHODS
Literature Search and Study Selection
Two of the authors (RS and VS) conducted a systematic
search of the literature independently in MEDLINE,
OVID, and CINAHL databases using the terms He-
noch-Schnlein purpura AND alveolar hemorrhage,
lung, and pulmonary hemorrhage. A second search
was then performed using the terms anaphylactoid pur-
pura AND alveolar hemorrhage, lung, and pulmo-
nary hemorrhage. In addition, another search was per-
formed using the term Henoch-Schnlein purpura and
abstracts were searched for possible cases of alveolar hem-
orrhage secondary to HSP. Only those articles that were
reported in English literature and included patients with
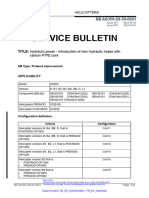
Figure 1 Composite gure shows bilateral alveolar inltrates
with air bronchograms (left) at the time of diagnosis of
alveolar hemorrhage. Chest radiograph (right) after treat-
ment with pulse methylprednisolone and cyclophosphamide
shows normalization of radiologic ndings.
Figure 2 Photomicrograph of low-power view of the skin
biopsy (10, left) shows neutrophilic inltration into the
dermis and brinoid vasculitis. Immunouorescence micros-
copy (right, arrow) of the skin biopsy shows deposition of IgA
and C3 and absence of IgG and IgM in the same areas. (Color
version of gure is available online.)
Figure 3 Photomicrograph of high-power view of the kidney
biopsy (40, PAS stain) showing evidence of focal prolifera-
tive glomerulonephritis. Immunouorescence shows deposi-
tion of IgA and C3 and absence of IgG and IgM. (Color
version of gure is available online.)
392 Diffuse alveolar hemorrhage in Henoch-Schnlein purpura
diagnosed HSP fullling the 1990 criteria of the Ameri-
can College of Rheumatology (1) or the HSP EULAR/
PRINTO/PRES Ankara 2008 classication (2) and (1)
alveolar hemorrhage documented by at least 2 of the fol-
lowing (a) drop in hemoglobin, (b) hemoptysis, (c) new
pulmonary inltrates, (d) hemosiderin-laden macro-
phages on bronchoalveolar lavage uid, or (2) surgical or
autopsy specimens showing alveolar hemorrhage with or
without leukocytoclastic vasculitis were included for anal-
ysis. The study was approved by the institutions ethics
board.
Data Extraction
Both abstracts and full text articles, where available, were
reviewed. Data were extracted in a predesigned data ex-
traction form regarding the age, sex, clinical features,
mode of diagnosis of diffuse alveolar hemorrhage, time to
diagnosis of DAH after diagnosis of HSP, comorbidities,
kidney, skin, and lung biopsy ndings, treatment before
DAH and after the onset of alveolar hemorrhage, the
duration of immunosuppressant administered, and out-
comes. Data were extracted and expressed in a descriptive
fashion (mean, SD).
RESULTS
Our search yielded 3662 references. This included 36
cases of diffuse alveolar hemorrhage in Henoch-Schnlein
purpura (Table 1) in 28 published reports. Full text or
abstracts were available for all 36 cases (3-30) in the arti-
cles reviewed. An additional 20 reports were excluded
because they reported cases in other languages (31-38)
or did not include patients with alveolar hemorrhage
(39-50).
The median age of DAH in HSP was 16.5 years (4
months to 78 years). Fifty percent (n 32)
(3,6,9,10,12,14,21,22,24,25,27-30) were older than 20
years at presentation. Male patients were affected more
frequently (M:F, 20:12). The occurrence of alveolar hem-
orrhage in HSP is rare and the reported prevalence ranged
from 0.8% to 5% (4,11,19,22). Several large series of
patients with HSP, both in children (51,52) and in adults
(53,54), have not reported any case of DAH.
Alveolar hemorrhage occurs in the setting of extensive
systemic vasculitis due to HSP. The organs involved were
kidney (94.4%), skin (86.1%), gastrointestinal tract
(75%), and joints (72.7%). Patients without cutaneous
involvement at presentation had documented rash either
previously (14) or later in the disease course (18). One-
fourth of the patients had other organ involvement, com-
monly neurologic (5,6,11,17,30) (13.8%), upper respira-
tory tract (3,8,17,18) (11.1%), or cardiac (11,23) (5.5%).
Overlap with microscopic polyangiitis, as demonstrated
by brinoid necrosis in subcutaneous vessels, medium-
sized arteries, and positive antineutrophil cytoplasmic an-
tibody, was reported in 2 patients (12,30) (5.5%). Most
patients did not have other comorbid illnesses (88.9%).
The diagnosis of HSP was based on the characteristic
clinical syndrome in most patients. Leukocytoclastic vas-
culitis was demonstrated in most patients in whom a skin
biopsy was performed (6,9,11-14,17,18,21-25,27-30)
(n 21), even when normal areas were biopsied (14).
However, IgA positivity was seen in 57% (n 21) only
(6,12-14,17,22,23,25,28-30), especially when biopsy was
attempted later in the disease course. Renal vasculitis was
very common (94.4%, n 31/33); hematuria and/or
proteinuria (33%, n 12/33) and renal failure in 47%
(n 17/33) (7,9,11-13,15-17,19,20,22,23,27,29,30)
were the most common manifestations. The mean serum
creatinine was 3.2 0.57 mg/dl at presentation and
5.6% were on hemodialysis (n 2/33) (14,25). Ne-
phrotic syndrome was seen in 8.3% (n 3/36)
(14,20,27). Biopsy commonly demonstrated mesangio-
proliferative glomerulonephritis (44.4%, n 8/18)
(8,9,12,15,18,24,26,29) but a wide variety of other le-
sions were observed (Table 2). Immunouorescence was
obtained in 44.4% (n 16/36) and demonstrated IgA
and C3 in 93.7% (n 15/16) of these patients (6,8-
10,12,13,15,17-19,21,26,27,29,30). Concurrent gastro-
intestinal vasculitis was seen in 75%(n 27/36); abdom-
inal pain (42.7%, n 15/36) and malena (25%, n
9/36) were most common but gastroenteropathy (5.6%,
n 2/36) and intestinal obstruction (2.8%, n 1/36)
were also seen.
Alveolar hemorrhage occurred variably after other or-
gan involvement, ranging from2 days to 18 years after the
diagnosis of HSP. Hemoptysis (75%), drop-in hemoglo-
bin (74%), and chest inltrates (94%) were present in
most patients, suggesting the late recognition of alveolar
hemorrhage. Bronchoalveolar lavage for hemosiderin-
laden macrophages was attempted in 16.7% only. The
chest radiograph commonly demonstrated alveolar inl-
trates or ground-glass opacities (80.6%); however, reticu-
lonodular inltrates mimicking interstitial lung disease
were seen in 13.9% (11,14). Pleural effusions were also
observed in 16.7%and were often massive, requiring tube
thoracostomy (4,9,12,16,18,30).
Lung biopsy was available in 36.1% (n 13/36) and
showed leukocytoclastic vasculitis with alveolar hemor-
rhage (69.2%, n 10/13) (3,5,6,10,12,13,15,23,25,27)
or only alveolar hemorrhage without capillaritis (31.8%,
n 3/13) (7,17,30). IgA was positive in only 50% (n
3/6) (6,10,12) of these lesions. Electron microscopic ex-
amination was reported in 2 cases (12,13) and one of
them demonstrated electron-dense deposits in the capil-
lary basement membrane and the interstitium of the alve-
olar walls (12).
Overall, 27.8% of HSP patients who experienced
DAH died (n 10/36) (3,5,6,10-12,17,23,25,30). Un-
treated alveolar hemorrhage was rapidly fatal (10,17).
Most of the patients (61%) were on treatment with ste-
roids for systemic vasculitis at the time of onset of alveolar
hemorrhage (47%). DAHwas frequently severe and 50%
(n 18/36) of the patients required mechanical ventila-
S. Rajagopala et al. 393
Table 1 Summary of All Reported Cases of Henoch-Schnlein Purpura with Diffuse Alveolar Hemorrhage in English Literature
References No.
Age/
Sex
Clinical Features
Kidney
Biopsy IF
Diagnosis of DAH
Time to
Lung
Regimen
of MP
Prior to
DAH
Regimen After DAH
Outcomes Skin Arthritis Kidney GI Others
Drop
in
Hb Hemoptysis Radiology BALF Others MP CYC
Jacome et
al.
1 45/F Proteinuria;
hematuria
Melena Epistaxis Not done NA Alveolar NA Lung Bx LCV
neg; DAH
IgA NA
NA Steroids Steroids?
Dose
None Died of DAH
Cream et
al.
5% (4/77) NA Proteinuria Pain NA Not done NA Consolidation
PE (75%)
NA Pleurisy Several
weeks
Steroids 4/77 patients
had DAH;
individual
data NA
Alive;
recurrence
1/4
Weiss et al. 1 8/M Proteinuria Pain Neurological Not done NA Alveolar NA Lung Bx
LCV;
IgA NA
NA Steroids Prednisolone
2 mg/
kg/d
None Died of DAH
Kathuria et
al.
1 57/M Proteinuria;
ESRD
Pain Neurological CGN IgA; no
C3
NA Consolidation NA LCV, DAH
IgA; no
C3 lung,
skin Bx
5 yr Steroids 1
mg/kg
None; oral
steroids
None Renal
recurrence;
pseudotumor
cerebri/died
DAH
Leatherman
et al.
1 10/F Proteinuria;
Cr 5.2
Pain No FSGN; IgA;
C3 neg
NA Alveolar NA Lung Bx
done;
DAH, LCV
neg;
IgA
8 wk Steroids Prednisolone?
dose
AZA?
duration
Alive;
recurrence
4; alive 10
yr
Payton et
al.
1 17/M Proteinuria;
hematuria,
RF
No Nasal
stufness
MPGN IgA,
IgM C3
NA No NA No Bx done NA Steroids Prednisolone?
dose
CYC?dose,
AZA
Alive; persistent
proteinuria
Shichiri et
al.
1 53/F Proteinuria;
hematuria,
RF Cr 1.4
Bleed Diabetes,
urinary
tract
infection
MPGN IgA,
IgM C3
Consolidation
PE (R)
NA Skin Bx: LCV
IgA NA
2 wk None Prednisolone
50 mg/d
None Alive; persistent
proteinuria
3 yr
Markus et
al.
1 78/M No Melena;
ulcer
1 previous
episode
of DAH
CGN; IgA Consolidation NA DAH, LCV,
IgA-Intra-
alveolar
IgA
3 wk None None None Died of DAH
References No. (If Series)
Age/
Sex
Clinical Features
Kidney
biopsy IF
Diagnosis of DAH
Time to
Lung
Involvement
Treatment
Prior to DAH
Regimen After DAH
Outcome Skin
Arthritis/
Arthralgia
NephritisCr
(mg/dl) GI Others
Drop
in
Hb Hemoptysis Radiology BALF Others MP CYC
Olson et
al.
4/169 (2.3%) 14/F Hematuria,
Cr NA
Pain None Not done Alveolar Yes No lung biopsy; skin
biopsy IgA-
leukocytoclastic
vasculitis (75%);
IgA-FSGN (1),
IgA-CGN (1); IgA
DPGN (1), NA
(1)
15 wk None Pulse MP 1
g/d 3
doses,
then oral
5 mo
None; cutaneous
recurrence
Alive 18 mo;
recurrence
4.5/F Hematuria;
RF Cr 2.1
Pain None Reticulonodular No 28 wk N None Prednisolone
2 mg/kg/
d 5
mo
CYC 3.3 mg/kg/
d 2.5 mo
Alive; sys
recurrence,
proteinuria
15/M Hematuria;
RF Cr 1.9
Pain/
blood
No Alveolar;
interstitial
No 3.5 wk N None MP 500 mg/
d 1
day
None Died 24 h;
DIC
16/M RF Cr 3.8;
hematuria
Pain Neurological/
cardiac
Alveolar;
interstitial
No 7 wk Prednisolone
60 mg/d
Prednisolone
60 mg/d
14 mo
Oral CYC 1 mg/
kg/d 3 mo
Alive 14 mo;
proteinuria,
zoster
3
9
4
D
i
f
f
u
s
e
a
l
v
e
o
l
a
r
h
e
m
o
r
r
h
a
g
e
i
n
H
e
n
o
c
h
-
S
c
h
n
l
e
i
n
p
u
r
p
u
r
a
Table 1 Continued
References No. (If Series)
Age/
Sex
Clinical Features
Kidney
biopsy IF
Diagnosis of DAH
Time to
Lung
Involvement
Treatment
Prior to DAH
Regimen After DAH
Outcome Skin
Arthritis/
Arthralgia
NephritisCr
(mg/dl) GI Others
Drop
in
Hb Hemoptysis Radiology BALF Others MP CYC
Yokose et
al.
1 77/M Hematuria;
RF; Cr
6.5
No Fibrinoid
necrosis?
MPN
MPGN
IgA
C3
Alveolar; large
PE
NA Skin Bx LCV IgA,
autopsy lung
LCV, DAH IgA
2 d None Pulse MP 30
mg/kg/d
x? doses
None Died at 51 d
Wright et
al.
1 14/F Hematuria;
RF; Cr
2.2
Melena Lung biopsy
LCV, DAH
IgM,
C3,
IgA
DPGN;
IgA,
IgM,
C3
Alveolar NA Skin Bx LCV; IgA 3 wk Pulse MP Repeat pulse
MP 30
mg/kg/d
3
doses,
then oral
2 mg/kg/
d
None Alive 7 mo;
duodenal
ulcer
Mallat et
al.
1 29/M Nephrotic
syndrome;
ESRD on
dialysis
No Diagnosed
HSP 11 yr;
recurrent
bouts 4
No Reticulonodular Yes IgA C3 skin Bx
LCV of normal
skin
11 yr None Pulse MP
3 doses
None Alive no
recurrence;
ESRD
Reznik et
al.
1 14/F RF; CR NA Pain No MPGN;
IgA,
C3
Alveolar NA Lung biopsy LCV,
DAH; IgA NA
1 wk Recurrence
of DAH 3
yr later;
none
Pulse MP
? doses
Pulse CYC? dose,
PE? sessions
Alive; normal
Carter et
al.
1 15/M Nephritis;
Cr 1.3
Pain/
blood
None;
intercostal
tube
drainage
No Alveolar;
massive
transudative
PE
NA No skin, renal, or
lung biopsy done
1 wk None Pulse MP
500 mg/
d 4,
then 300
mg
4 d, then
160 mg
1 d
None Alive 18 mo;
recurrence
of PH
References No. (If Series)
Age/
Sex
Clinical Features
Kidney Biopsy
IF
Diagnosis of DAH
Time to
Lung
Involvement
Treatment
Prior to DAH
Regimen After DAH
Outcome Skin Arthritis Nephritis GI Others
Drop
in
Hb Hemoptysis Radiology BALF Others MP CYC
Paller et
al.
2 12/M Hematuria;
RF; Cr
1.7
No Epistaxis;
stroke,
seizures
CGN; IgA _ Alveolar NA Skin Bx LCV
IgA
1.5 wk Prednisolone
2 mg/kg/
d
Prednisolone
2 mg/kg/
d
Pulse CYC 750
mg/m
2
, then 3
mo
Alive at 2 yr;
CYC
anaphylaxis
0.4/F Hematuria;
Cr NA
No None NA Alveolar NA Skin Bx LCV IgA
NA; autopsy
lung Bx
DAH; no
LCV
64 wk None None None Multiple
recurrences;
died
Vats et al. 1 7/M Not at
onset;
day
4
Hematuria;
Cr 0.5
Colicky
pain;
bleed
Sinus
involvement;
surgery
MPGNIgA,
C3
Alveolar;
pleural
effusions
NA Skin Bx: IgA-
LCV; sinus,
jejunum
LCV-
1 wk None Pulse MP 30
mg/kg/d
3
doses,
then 2
mg/kg/d
None Alive;
hematuria
6 wk
Besbas et
al.
1/550 (0.18%) 6/M Hematuria;
RF Cr 2.8
No None DPGN; IgA,
C3
Alveolar NA None 1 wk Pulse MP 30
mg/kg/d
3
doses
Pulse MP 15
mg/kg/d
2, then
2 mg/kg/
d
Pulse CYC 250
mg/d, then
oral 2 mg/kg/d
? months
Alive 18
mo,
neutropenia
Al-Harbi et
al.
1 9/F Nephrotic
syndrome;
RF Cr 5.4
Pain;
bleed
None No biopsy Alveolar NA None 1.5 wk Prednisolone
30 mg/d
Pulse MP 30
mg/kg/d
3
doses,
then oral
6 mo
Worsening on MP;
CYC pulse 750
mg/m
2
, then
750 mg/m
2
6
Alive at 1 yr
Teixeira et
al.
1 45/M Nephritis; Cr
1.0
Pain Occult alveolar
hemorrhage;
previous
pulmonary
tuberculosis
FPGN IgA, C3
mesangium
Normal Yes Skin Bx normal;
no lung Bx
3 mo Occult DAH;
none
Prednisone 1
mg/kg/d
None Alive at 1 yr
S
.
R
a
j
a
g
o
p
a
l
a
e
t
a
l
.
3
9
5
Table 1 Continued
References No. (If Series)
Age/
Sex
Clinical Features
Kidney Biopsy
IF
Diagnosis of DAH
Time to
Lung
Involvement
Treatment
Prior to DAH
Regimen After DAH
Outcome Skin Arthritis Nephritis GI Others
Drop
in
Hb Hemoptysis Radiology BALF Others MP CYC
Nadrous
et al.
2/124 (1.6%) 20/M RF Cr 2.0 No None Not done Alveolar NA Skin Bx: IgA
deposition
2 wk Parenteral
prednisolone?
dose
Pulse MP
500 mg/
d 2;
then 60
mg/d 10
d
None Alive
76/F RF Cr 1.2 Pain Systemic
recurrences
multiple;
2nd
episode of
DAH
Not done Alveolar NA Skin Bx: IgA
deposition
18 yr One prior
DAH on
3 mg/d
prednisone
Parenteral
prednisolone
60
mg/d
2; then
30 mg/d
None Recurrence of
PH; alive
Kalyoncu
et al.
1 13/M Not at
onset;
nephritis
later Cr
3.6
Severe
pain
Rheumatic (?)
carditis 6-yr
autopsy,
DAH IgA-
brinoid
necrosis
Not done Alveolar
opacities
NA Skin biopsy LCV
IgA C3
autopsy
lungs LCV;
IgA NA
3 Prednisolone
2 mg/kg
Pulse MP 30
mg/kg/d
CYC 2 mg/kg/d
26 d
Died at 4 wk;
massive
PH
References
No./
Series
Age/
Sex
Clinical Features
Kidney
Biopsy IF
Diagnosis of DAH Time to
Lung
Involvement
(wk)
Treatment
Prior to DAH
Regimen After DAH
Outcome Skin
Arthritis
Arthralgia
Nephritis Cr
mg/dl GI Others HbDrop Hemoptysis Radiology BALF Others MP CYC
Tiryaki et al. 1 78/F Hematuria,
proteinuria
Cr 0.7
No None MPGN IgA
NA
Alveolar
opacities
Yes Skin biopsy:
LCV Ig A
Na
12 Pulse MP
?Doses,
then 48
mg/d
Pulse MP
1.5 g
3, then 1
mg/kg/d
3 mo
None Alive; tapered
3 mo
Usui et al. 1 69/M ESRD; Cr
8.73
Gastroenteropathy ESRD 18 yr Hyalinized
glomeruli;
IgA NA
GGO/
consolidation
NA IgA C3 skin
biopsy;
autopsy-
LCV, DAH
IgA
2 100 mg
prednisolone
Pulse MP
3, then
125 mg/
d;
recurrence
26th day
MP 3
None Died at 5 wk
Matsubayashi
et al.
1 6/M Hematuria;
Cr 0.3
Protein-losing
enteropathy,
colonic blebs,
hemorrhage
None MPGNIg A GGO/
consolidation
NA No 2.5 Prednisolone 2
mg/kg/d
Pulse MP
?doses
Cyclosporine
A;
abdominal
recurrence
MP 2
Mizoribine?
duration
Renal
recurrence;
alive-
mizoribine
started
Touissant et
al.
1 54/M Nephrotic
syndrome;
Cr 3.9
Intestinal
obstruction
Trans-bronchial
Bx LCV;
alveolar
hemorrhage
IgA NA
FPGN with
mesangial
IgA, C3
Alveolar
opacities;
GGO on CT
Yes; also
on
biopsy
Skin Bx: LCV
IgA NA
3 Parenteral MP Pulse MP
3
CYC 2 mg/
kg/d 4
mo; MMF
later
Alive; dialysis
independent
at 3 yr
Oto et al. 1 33/F No No Kabuki
syndrome
No biopsy GGO/
consolidation
NA Skin biopsy
LVC IgA
1.5 None Prednisolone
20 mg
None Alive at 2 mo
Goel et al. 1 72/M Nephritis; Cr
1.6
No Multiple
comorbidities
MPGN Ig
A
GGO/nodular
inltrates
Yes IgA renal/
skin
biopsy; no
lung
biopsy
2 Prednisolone
40 mg/d
PE-1 session;
pulse MP
?doses
CYC 175 mg/
d 3 mo;
AZA until
6 mo
Alive at 6 mo;
Cr 1.6 mg/
dl
Nagasaka et
al.
1 74/M Hematuria;
Cr 2.4
Duodenal ulcers Intracranial
bleed; MPO-
ANCA
CGN; IgA,
C3
Consolidation/
pleural
effusion
No IgA skin
biopsy
autopsy:
DAH, no
LCV
8 Pulse MP 3 None None Died 4 wk
later
The numerator is the number of cases in males and the denominator is the total number of cases reported.
3
9
6
D
i
f
f
u
s
e
a
l
v
e
o
l
a
r
h
e
m
o
r
r
h
a
g
e
i
n
H
e
n
o
c
h
-
S
c
h
n
l
e
i
n
p
u
r
p
u
r
a
tion (3,5,6,10-13,15-20,25,28,29) for a mean duration
of 26 4.8 days (n 10). Continuation of oral steroids,
often at higher doses, was associated with a mortality rate
of 27. 2% (n 3/11) (3,5,6,11). Pulse methylpred-
nisolone, at a varying number of boluses, was adminis-
tered after the occurrence of DAH in 11 patients (mor-
tality 27.2%, n 3/11). Pulse methylprednisolone along
with cyclophosphamide (11,17,19,20,23), pulse cyclo-
phosphamide followed by azathioprine (7,8,29), or my-
cophenolate mofetil (27) and cyclosporine A (26) were
administered in 11 patients and had the least mortality
rate observed (9%, n 1/11). Untreated DAH had a
uniformly fatal outcome (n 3/3, 100%) (6,17,30). Ste-
roids and immunosuppression were administered for a
median duration of 9 months (range, 10 days to 36
months) and 4.5 months (2.5 to 36 months), respectively.
The total duration of reported follow-up (mean, SE)
was 1.6 (0.5) months (n 19). Recurrence of vasculitis
was seen in 27.7%, including 4 patients (11.1%) with
recurrent DAH (7,16,22,25). Morbidity due to DAH
was also common and persistent urinary abnormalities
(8,9,11,18) (12%), chronic renal failure (9%) (14,25),
Table 2 Summary Findings of All Reported Cases of Henoch-Schnlein Purpura with Diffuse Alveolar Hemorrhage in the
English Literature
Parameter Value
Age (median, range) 16.5 (4 mo to 78 yr), N 32
Kidney biopsy (50%, N 18/36) MPGN (44.4%, N 8/18), FSGN (16.7%, N 3/18), DPGN (5.5%,
N 1/18), CGN (27.8%, N 5/18)
Hyalinized glomeruli (5.5%, N 1/18)
Kidney biopsy immunouorescence
(44.4%, N 16/36)
IgA, C3 positive (93.75%, N 15/16), IgA, C3 negative (6.3%,
N 1/16)
Time to lung involvement from onset
of illness (mean, range)
3 wk (2 d to 18 yr) (N 29)
Diagnosis of diffuse alveolar
hemorrhage
Drop in hemoglobin (74%, N 27), hemoptysis (75%, N 36), chest
radiology nding (94.4%, N 36), bronchoalveolar lavage (16.7%,
N 36)
Chest radiology ndings Consolidation/ground glass opacity (80.6%, N 36)
Reticulonodular opacity (13.9%, N 36)
Normal (5.6%, N 36)
Pleural effusions (16.7%, N 36)
Leukocytoclastic vasculitis (LCV) on
lung biopsy
69.2% (N 9/13); DAH alone 31.8% (N 4/13)
Immunoglobulin A positive on lung
biopsy
Surgical or autopsy (N 6/13); 50% (N 3/6)
Treatment before DAH None 38.9% (N 14/36)
Oral steroids 50% (N 18/36)
Pulse methylprednisolone 11% (N 4/36)
Treatment after onset of DAH None 8.3% (N 3/36)
Oral steroids alone 30.5% (N 11/36)
Methylprednisolone pulse alone 30.5% (N 11/36)
Steroids and immunosuppression 30.5% (N 11/36)
Mechanical ventilation 50% (N 36)
Duration of mechanical ventilation
(mean, SE)
26 4.8 d (N 10)
Duration of steroid therapy median,
range
9 mo (10 d to 36 mo, N 11)
Duration of immunosuppression
(median, range)
4.5 mo (2.5-36 mo, N 6)
Recurrences of vasculitis 27.7%
(N 10)
None 72.2% (N 36), all systemic 19.4% (N 7/36), PH alone
11.1% (N 4/36)
Complications of
immunosuppression 27% (N 11)
Zoster 9% (N 11), neutropenia 9% (N 11), anaphylaxis 9%
(N 11)
Mortality 27.8% (N 10/36)
Morbidity Persistent hematuria, albuminuria 12% (N 33), chronic renal failure
9% (N 33)
M, Male; F, Female; NA, not available; , present; absent; Cr, creatinine; DAH, diffuse alveolar hemorrhage; GN, glomerulonephritis;
MPGN, Mesangioproliferative glomerulonephritis; FSGN, Focal segmental glomerulonephritis; CGN, Cresentric glomerulonephritis; DPGN,
diffuse proliferative glomerulonephritis; PE, pleural effusions; R, right-sided; Bx, biopsy; LCV, leukocytoclastic vasculitis; IgA, Immunoglobulin
A; C3, complement 3; CYC, cyclophosphamide; AZA, azathioprine; MP, methylprednisolone; MV, mechanical ventilation; ESRD, end stage
renal disease; MPN, microscopic polyangiitis; PH, pulmonary hemorrhage.
S. Rajagopala et al. 397
and complications of therapy (27%) (11,13,17,19) were
frequently observed.
DISCUSSION
HSP is an acute, self-limited small-vessel vasculitis char-
acterized by deposition of immunoglobulin A (IgA) im-
mune complexes (55,56). It is predominantly a disease of
children, with the highest prevalence between 4 and 7
years (70 per 100,000) (55).
Age at onset and nephritis at presentation in HSP are
important determinants of severity (57,58). The older age
of this cohort and high prevalence of nephritis suggest
DAH occurs in patients at risk of recurrence of systemic
vasculitis.
DAH is exceedingly rare in HSP and large series have
often not reported any cases of DAH (52,53). Data from
the retrospective studies of Cream et al. (4) and Nadrous
et al. (22) have suggested a prevalence of 1.6% to 5% for
overt alveolar hemorrhage. Differences in reported prev-
alence are probably due to case selection bias.
The high frequency of clinically evident alveolar hem-
orrhage and the use of bronchoscopy in only 16.7% of
patients with DAH related to HSP suggest late clinical
recognition. In alveolar hemorrhage, clinically evident he-
moptysis is present in only 33% of patients at presenta-
tion because the total alveolar volume is large and can
accommodate bleeding without apparent symptoms;
early bronchoscopy is recommended for diagnosis (59).
Recurrent unrecognized DAH may be associated with
reticular inltrates mimicking an interstitial lung disease
and was observed in 13.9% of patients (11,22). Subclin-
ical reductions of transfer factor of the lung for carbon
monoxide (TLCO) with active vasculitis (60), the associ-
ation of reduced TLCO with systemic relapses (60,61),
and the nding of hemosiderin-laden macrophages in the
absence of pulmonary symptoms and normal radiographs
(21) suggest that incipient alveolar hemorrhage may be
more common than is clinically evident. The prognostic
implication of subclinical alveolar hemorrhage, however,
remains unclear.
Corticosteroids are not recommended in patients with
uncomplicated HSP (62,63); however, in patients with
nephritis, pulse methylprednisolone followed by oral cor-
ticosteroids plus azathioprine or cyclophosphamide is ef-
fective in reversing clinical nephritis and preventing dis-
ease progression (55,64). Patients with DAH secondary
to HSP capillaritis are treated with a similar regimen (59).
Given the severity of DAH, it is unlikely that signicant
delays existed after the diagnosis of DAH was made.
However, delays of 2 to 3 weeks after onset of DAH
(9,28) to the administration of steroids were seen, sug-
gesting that the recognition of DAH was delayed. Most
patients were on oral steroids for systemic vasculitis before
the onset of DAH, indicating that steroids alone are inef-
fective. At least 11% of patients had already received 3
doses of pulse methylprednisolone just before the onset of
DAH for systemic vasculitis. Also, patients had a recur-
rence of DAH with pulse methylprednisolone alone (25)
and responded to cyclophosphamide pulse after failing
pulse methylprednisolone for DAH (20). In patients on
steroids at the time of DAH, pulse methylprednisolone
followed by cyclophosphamide for a median duration of 6
months was the most commonly reported treatment reg-
imen and was associated with a mortality rate of 9% (n
1/11). A high frequency of vasculitis recurrence (27.7%)
and morbidity (27%) was seen.
DAHis a rare complication of HSP and often occurs in
adults. Clinical recognition is delayed, with high morbid-
ity and mortality. DAH is frequently severe, requiring
mechanical ventilation. Pulse methylprednisolone and
cyclophosphamide are associated with the least mortality,
particularly in patients on steroids at the time of DAH.
Further multicentric observational studies are required to
dene the optimal regimen and duration of treatment in
DAH related to HSP.
REFERENCES
1. Mills JA, Michel BA, Bloch DA, Calabrese LH, Hunder GG,
Arend WP, et al. The American College of Rheumatology 1990
criteria for the classication of Henoch-Schnlein purpura. Ar-
thritis Rheum 1990;33:1114-21.
2. Ozen S, Pistorio A, Iusan SM, Bakkaloglu A, Herlin T, Brik R, et
al. EULAR/PRINTO/PRES criteria for henoch-schonlein pur-
pura, childhood polyarteritis nodosa, childhood wegener granu-
lomatosis and childhood takayasu arteritis: Ankara 2008. Final
classication criteria. Part ii. Ann Rheum Dis;69:798-806.
3. Jacome AF. Pulmonary hemorrhage and death complicating ana-
phylactoid purpura. South Med J 1967;60:1003-4.
4. Cream JJ, Gumpel JM, Peachey RD. Schnlein-Henoch purpura
in the adult. A study of 77 adults with anaphylactoid or Schn-
lein-Henoch purpura. Q J Med 1970;39:461-84.
5. Weiss VF, Naidu S. Fatal pulmonary hemorrhage in Henoch-
Schnlein purpura. Cutis 1979;23:687-8.
6. Kathuria S, Cheifec G. Fatal pulmonary Hench-Schonlein syn-
drome. Chest 1982;82:654-6.
7. Leatherman JW, Sibley RK, Davies SF. Diffuse intrapulmonary
hemorrhage and glomerulonephritis unrelated to anti-glomerular
basement membrane antibody. Am J Med 1982;72:401-10.
8. Payton CD, Allison ME, Boulton-Jones JM. Henoch Schonlein
purpura presenting with pulmonary haemorrhage. Scott Med J
1987;32:26-7.
9. Shichiri M, Tsutsumi K, Yamamoto I, Ida T, Iwamoto H. Diffuse
intrapulmonary hemorrhage and renal failure in adult Henoch-
Schnlein purpura. Am J Nephrol 1987;7:140-2.
10. Markus HS, Clark JV. Pulmonary haemorrhage in Henoch-
Schnlein purpura. Thorax 1989;44:525-6.
11. Olson JC, Kelly KJ, Pan CG, Wortmann DW. Pulmonary disease
with hemorrhage in Henoch-Schenlein purpura. Pediatrics
1992;89:1177-81.
12. Yokose T, Aida J, Ito Y, Ogura M, Nakagawa S, Nagai T. A case
of pulmonary hemorrhage in Henoch-Schnlein purpura accom-
panied by polyarteritis nodosa in an elderly man. Respiration
1993;60:307-10.
13. Wright WK, Krous HF, Griswold WR, Billman GF, Eicheneld
LF, Lemire JM, et al. Pulmonary vasculitis with hemorrhage in
anaphylactoid purpura. Pediatr Pulmonol 1994;17:269-71.
14. Mallat BS, Teitel AD. Apurpuric henoch-schnlein vasculitis.
J Clin Rheumatol 1995;1:347-9.
15. Reznik VM, Griswold WR, Lemire JM, Mendoza SA. Pulmonary
398 Diffuse alveolar hemorrhage in Henoch-Schnlein purpura
hemorrhage in children with glomerulonephritis. Pediatr
Nephrol 1995;9:83-6.
16. Carter ER, Guevara JP, Moftt DR. Pulmonary hemorrhage in an
adolescent with Henoch-Schnlein purpura. West J Med 1996;
164:171-3.
17. Paller AS, Kelly K, Sethi R. Pulmonary hemorrhage: An often fatal
complication of Henoch-Schoenlein purpura. Pediatr Dermatol
1997;14:299-302.
18. Vats KR, Vats A, Kim Y, Dassenko D, Sinaiko AR. Henoch-
Schnlein purpura and pulmonary hemorrhage: A report and lit-
erature review. Pediatr Nephrol 1999;13:530-4.
19. Besbas N, Duzova A, Topaloglu R, Gok F, Ozaltin F, Ozen S, et
al. Pulmonary haemorrhage in a 6-year-old boy with Henoch-
Schnlein purpura. Clin Rheumatol 2001;20:293-6.
20. Al-Harbi NN. Henoch-Schnlein nephritis complicated with
pulmonary hemorrhage but treated successfully. Pediatr Nephrol
2002;17:762-4.
21. Teixeira A, Genereau T, Sutton L, Herson S, Cherin P. Implica-
tion of occult alveolar hemorrhage in Henoch-Schonlein purpura.
J Clin Rheumatol 2002;8:287-8.
22. Nadrous HF, Yu AC, Specks U, Ryu JH. Pulmonary involvement
in Henoch-Schnlein purpura. Mayo Clin Proc 2004;79:1151-7.
23. Kalyoncu M, Cakir M, Erduran E, Okten A. Henoch-Schnlein
purpura: A case with atypical presentation. Rheumatol Int 2006;
26:669-71.
24. Tiryaki O, Buyukhatipoglu H, Karakok M, Usalan C. Successful
treatment of a rare complication of Henoch-Schnlein purpura in
advanced age: Pulmonary hemorrhage. Intern Med 2007;46:
905-7.
25. Usui K, Ochiai T, Muto R, Abe I, Aikawa M, Kikushima K, et al.
Diffuse pulmonary hemorrhage as a fatal complication of Schn-
lein-Henoch purpura. J Dermatol 2007;34:705-8.
26. Matsubayashi R, Matsubayashi T, Fujita N, Yokota T, Ohro Y,
Enoki H. Pulmonary hemorrhage associated with Henoch-
Schnlein purpura in a child. Clin Rheumatol 2008;27:803-5.
27. Toussaint ND, Desmond M, Hill PA. A patient with Henoch-
Schonlein purpura and intra-alveolar haemorrhage. Nephrol Dial
Transpl Plus 2008;3:167-70.
28. Oto J, Mano A, Nakataki E, Yamaguchi H, Inui D, Imanaka H, et
al. An adult patient with Kabuki syndrome presenting with He-
noch-Schnlein purpura complicated with pulmonary hemor-
rhage. J Anesth 2008;22:460-3.
29. Goel SS, Langford CA. A 72-year-old man with a purpuric rash.
Cleve Clin J Med 2009;76:353-60.
30. Nagasaka T, Miyamoto J, Ishibashi M, Chen KR. MPO-ANCA-
and IgA-positive systemic vasculitis: A possibly overlapping syn-
drome of microscopic polyangiitis and Henoch-Schoenlein pur-
pura. J Cutan Pathol 2009;36:871-7.
31. Zollinger HU, Hegglin R. [Idiopathic pulmonary hemosiderosis
as a pulmonary form of Schnlein-Henoch purpura]. Schweiz
Med Wochenschr 1958;88:439-43.
32. Storch H, Weidenbach H. [schonlein-henoch purpura, glomeru-
lonephritis and pulmonary hemosiderosis, Goodpastures syn-
drome]. Z Gesamte Inn Med 1970;25:406-12.
33. Fiegler W, Siemoneit KD. [Pulmonary manifestations in anaphy-
lactoid purpura (Henoch-Schnlein Syndrome) (authors transl)].
Rofo 1981;134:269-72.
34. Marandian MH, Ezzati M, Behvad A, Moazzami P, Rakhchan M.
[Pulmonary involvement in schonlein-henochs purpura]. Arch
Fr Pediatr 1982;39:255-7.
35. Boskovic S, Suskovic T. [Henoch-Schoenlein purpura with pul-
monary inltration]. Plucne Boles 1989;41:173-7.
36. Stienstra Y, Fijen JW, Tervaert JW, Dankbaar H, Zijlstra JG, van
der Werf TS. [Pulmonary hemorrhage with respiratory insuf-
ciency in Henoch-Schoenlein purpura]. Ned Tijdschr Geneeskd
2000;144:617-22.
37. Ros S, Martnez Ara J, Garca de Miguel MA, Olea T, de Alvaro F.
[Familial Henoch-Schnlein purpura manifested with lung hem-
orrhage]. Nefrologia 2004;24:499-502.
38. de la Prada Alvarez FJ, Prados Gallardo AM, Tugores Vazquez A,
Uriol Rivera M, Saus Sarrias C, Morey Molina A. [Shonlein-
henoch nephritis complicated with pulmonary renal syndrome].
An Med Int 2005;22:441-4.
39. Clark JH, Fitzgerald JF. Hemorrhagic complications of Henoch-
Schnlein syndrome. J Pediatr Gastroenterol Nutr 1985;4:311-5.
40. Veale D, Venning MC, Quinn A. Pulmonary haemorrhage in
Henoch-Schonlein purpura. Thorax 1990;45:496.
41. Case records of the Massachusetts General Hospital weekly clin-
icopathological exercises. Case 42-1992. A 59-year-old woman
with severe, progressive dyspnea. N Engl J Med;1992(327):
1226-33.
42. Green RJ, Ruoss SJ, Kraft SA, Duncan SR, Berry GJ, Rafn TA.
Pulmonary capillaritis and alveolar hemorrhage. Update on diag-
nosis and management. Chest 1996;110:1305-16.
43. Eicheneld LF, Wright WK. Pulmonary hemorrhage associated
with Henoch-Schonlein purpura. Pediatr Dermatol 1998;15:
143.
44. Agraharkar M, Gokhale S, Le L, Rajaraman S, Campbell GA.
Cardiopulmonary manifestations of Henoch-Schnlein purpura.
Am J Kidney Dis 2000;35:319-22.
45. Srensen SF, Slot O, Tvede N, Petersen J. A prospective study of
vasculitis patients collected in a ve year period: Evaluation of the
Chapel Hill nomenclature. Ann Rheum Dis 2000;59:478-82.
46. von Vigier RO, Trummler SA, Laux-End R, Sauvain MJ, Trutt-
mann AC, Bianchetti MG. Pulmonary renal syndrome in child-
hood: A report of twenty-one cases and a review of the literature.
Pediatr Pulmonol 2000;29:382-8.
47. Manganelli P, Fietta P, Carotti M, Pesci A, Salaf F. Respiratory
systeminvolvement in systemic vasculitides. Clin Exp Rheumatol
2006;24:S48-59.
48. Soloukides A, Moutzouris DA, Metaxatos G, Hadjiconstantinou
V. Pulmonary involvement in henoch-schonlein purpura. Emerg
Med J 2006;23:886.
49. Shin JI, Lee JS. Could intravenous cyclosporin A be an effective
therapeutic strategy in pulmonary hemorrhage associated with
Henoch-Schnlein purpura? Comment on: Pulmonary hemor-
rhage associated with Henoch-Schnlein purpura in a child [Clin
Rheumatol 27(6):803-805]. Clin Rheumatol 2008;27:1475.
50. Shin JI, Lee JS, Sohn MH, Kim KE. Fatal pulmonary renal syn-
drome and treatment in adults with schonlein-henoch purpura:
Comment. J Dermatol 2008;35:252; Author reply 253.
51. Trapani S, Micheli A, Grisolia F, Resti M, Chiappini E, Falcini F,
et al. Henoch schonlein purpura in childhood: Epidemiological
and clinical analysis of 150 cases over a 5-year period and reviewof
literature. Semin Arthritis Rheum 2005;35:143-53.
52. Soylemezoglu O, Ozkaya O, Ozen S, Bakkaloglu A, Dusunsel R,
Peru H, et al. Henoch-Schnlein nephritis: A nationwide study.
Nephron Clin Pract 2009;112:c199-204.
53. Saulsbury FT. Henoch-Schnlein purpura in children. Report of
100 patients and review of the literature. Medicine (Baltimore)
1999;78:395-409.
54. Pillebout E, Thervet E, Hill G, Alberti C, Vanhille P, Nochy D.
Henoch-Schnlein Purpura in adults: Outcome and prognostic
factors. J Am Soc Nephrol 2002;13:1271-8.
55. Saulsbury FT. Henoch-Schnlein purpura. Curr Opin Rheuma-
tol 2001;13:35-40.
56. Saulsbury FT. Clinical update: Henoch-Schnlein purpura. Lan-
cet 2007;369:976-8.
57. Hung S-P, Yang Y-H, Lin Y-T, Wang L-C, Lee J-H, Chiang B-L.
Henoch-Schnlein purpura: Comparison between adults and
children. Pediatr J Neonatol 2009;50:162-8.
58. Ronkainen J, Nuutinen M, Koskimies O. The adult kidney 24
years after childhood Henoch-Schnlein purpura: A retrospective
cohort study. Lancet 2002;360:666-70.
S. Rajagopala et al. 399
59. Ioachimescu OC, Stoller JK. Diffuse alveolar hemorrhage: Diag-
nosing it and nding the cause. Cleve Clin J Med 2008;75:
258-80.
60. Chaussain M, de Boissieu D, Kalifa G, Epelbaum S, Niaudet P,
Badoual J, et al. Impairment of lung diffusion capacity in Schn-
lein-Henoch purpura. J Pediatr 1992;121:12-6.
61. Cazzato S, Bernardi F, Cinti C, Tassinari D, Canzi A, Berga-
maschi R, et al. Pulmonary function abnormalities in children
with Henoch-Schnlein purpura. Eur Respir J 1999;13:597-
601.
62. Ronkainen J, Koskimies O, Ala-Houhala M, Antikainen M, Me-
renmies J, Rajantie J, et al. Early prednisone therapy in Henoch-
Schnlein purpura: A randomized, double-blind, placebo-con-
trolled trial. J Pediatr 2006;149:241-7.
63. Chartapisak W, Opastiraku S, Willis NS, Craig JC, Hodson EM.
Prevention and treatment of renal disease in Henoch-Schnlein
purpura: A systematic review. Arch Dis Child 2009;94:132-7.
64. Oner A, Tinaztepe K, Erdogan O. The effect of triple therapy on
rapidly progressive type of Henoch-Schnlein nephritis. Pediatr
Nephrol 1995;9:6-10.
400 Diffuse alveolar hemorrhage in Henoch-Schnlein purpura
You might also like
- Environmental Impact Assessment ModuleDocument39 pagesEnvironmental Impact Assessment ModuleJoshua Landoy100% (2)
- COPD ExacerbationDocument12 pagesCOPD ExacerbationJeffrey ShermanNo ratings yet
- Pandemic H1N1 Influenza A Viral Infection Complicated by Atypical Hemolytic Uremic Syndrome and Diffuse Alveolar HemorrhageDocument5 pagesPandemic H1N1 Influenza A Viral Infection Complicated by Atypical Hemolytic Uremic Syndrome and Diffuse Alveolar HemorrhageDavidNo ratings yet
- 1271 HSP .FullDocument8 pages1271 HSP .FulldonkeyendutNo ratings yet
- A Case of Lupus Pneumonitis Mimicking As Infective PneumoniaDocument4 pagesA Case of Lupus Pneumonitis Mimicking As Infective PneumoniaIOSR Journal of PharmacyNo ratings yet
- Clinical Profile, Etiology, and Management of Hydropneumothorax: An Indian ExperienceDocument5 pagesClinical Profile, Etiology, and Management of Hydropneumothorax: An Indian ExperienceSarah DaniswaraNo ratings yet
- Hypereosinophilic Syndrome: C. Venkatesh, E. Mahender, S. Janani, S. MalathiDocument3 pagesHypereosinophilic Syndrome: C. Venkatesh, E. Mahender, S. Janani, S. MalathialaaNo ratings yet
- Chronic Cor-Pulmonale in Adults: An Experience From A Tertiary Teaching Hospital in DharwadDocument4 pagesChronic Cor-Pulmonale in Adults: An Experience From A Tertiary Teaching Hospital in DharwadThariq Mubaraq DrcNo ratings yet
- Neurology and Neurotherapy: ClinmedDocument4 pagesNeurology and Neurotherapy: ClinmedChristian Hasudungan NainggolanNo ratings yet
- Case Report: Henry G Cheng, Caitlin Gomez, Sarah Khan, Soma WaliDocument1 pageCase Report: Henry G Cheng, Caitlin Gomez, Sarah Khan, Soma WaliYe HtunNo ratings yet
- 2014 Kabir Et Al. - Chronic Eosinophilic Leukaemia Presenting With A CDocument4 pages2014 Kabir Et Al. - Chronic Eosinophilic Leukaemia Presenting With A CPratyay HasanNo ratings yet
- The Use of Sildenafil in Persistent Pulmonary Hypertension of The Newborn PDFDocument6 pagesThe Use of Sildenafil in Persistent Pulmonary Hypertension of The Newborn PDFmaciasdrNo ratings yet
- Nej M CPC 0900643Document10 pagesNej M CPC 0900643Adina OlteanuNo ratings yet
- A Case of HypercalcemiaDocument7 pagesA Case of HypercalcemiaWitrisyah PutriNo ratings yet
- Efusi Pleural in MassDocument4 pagesEfusi Pleural in MassRofi IrmanNo ratings yet
- Alveolar Hemorrhage in SLE0Document10 pagesAlveolar Hemorrhage in SLE0Fabian Aguilar CastilloNo ratings yet
- Dengue Perimyocarditis: A Case Report: PL GohDocument3 pagesDengue Perimyocarditis: A Case Report: PL GohDenny IntanNo ratings yet
- Crim Em2013-948071Document2 pagesCrim Em2013-948071m.fahimsharifiNo ratings yet
- Bilateral Massive Pulmonary Embolism Secondary To Decompression Sickness: A Case ReportDocument4 pagesBilateral Massive Pulmonary Embolism Secondary To Decompression Sickness: A Case ReportPatricio Toledo FuenzalidaNo ratings yet
- Claudia Craven VENTRICULOMEGALY CLASSIFICATIONDocument17 pagesClaudia Craven VENTRICULOMEGALY CLASSIFICATIONGUI VINCENo ratings yet
- Aair 6 454270Document3 pagesAair 6 454270tomasjohn123No ratings yet
- Henoch-Schonlein Purpura Associated With Bee Sting Case Report PDFDocument7 pagesHenoch-Schonlein Purpura Associated With Bee Sting Case Report PDFjoshkelNo ratings yet
- Summary of Summary 5Document36 pagesSummary of Summary 5anon-265120100% (2)
- Dubin Johnson SyndromeDocument4 pagesDubin Johnson SyndromeAustine OsaweNo ratings yet
- Letter To The Editor Henoch-Schönlein Purpura in Adults: Clinics 2008 63 (2) :273-6Document4 pagesLetter To The Editor Henoch-Schönlein Purpura in Adults: Clinics 2008 63 (2) :273-6donkeyendutNo ratings yet
- Pleural Effusion in A Patient With End-Stage Renal Disease - PMCDocument5 pagesPleural Effusion in A Patient With End-Stage Renal Disease - PMCCasemix rsudwaledNo ratings yet
- A Treacherous Course: Clinical Problem-SolvingDocument6 pagesA Treacherous Course: Clinical Problem-SolvingMorocco CandycatyNo ratings yet
- An Etiological Reappraisal of Pancytopenia - LargestDocument9 pagesAn Etiological Reappraisal of Pancytopenia - LargestKaye Antonette AntioquiaNo ratings yet
- Allopurinol-Induced Drug Reactions With Eosinophilia and Systemic Symptoms Syndrome With Interstitial NephritisDocument12 pagesAllopurinol-Induced Drug Reactions With Eosinophilia and Systemic Symptoms Syndrome With Interstitial NephritisJoc HerreraNo ratings yet
- Invasive Aspergillosis in A Patient With End StageDocument8 pagesInvasive Aspergillosis in A Patient With End StageDhurgham QuasimNo ratings yet
- Septic ShockDocument2 pagesSeptic ShockLatifah LàNo ratings yet
- Penyakit DalamDocument2 pagesPenyakit DalamMade NoprianthaNo ratings yet
- 54 Shivraj EtalDocument3 pages54 Shivraj EtaleditorijmrhsNo ratings yet
- Brief CommunicationDocument3 pagesBrief CommunicationanrihmNo ratings yet
- Prophylaxis and Treatment For AspirationDocument19 pagesProphylaxis and Treatment For Aspirationbalab2311No ratings yet
- Paediatrica Indonesiana: Case ReportDocument5 pagesPaediatrica Indonesiana: Case Reportsarliance letteNo ratings yet
- A Severe Asphyxiated Newborn: A Case ReportDocument13 pagesA Severe Asphyxiated Newborn: A Case ReportEeeeeeeeeNo ratings yet
- COPD and Pulmonary Thromboembolism (For Galley Proof)Document6 pagesCOPD and Pulmonary Thromboembolism (For Galley Proof)Ram AdhikariNo ratings yet
- Oxford University PressDocument9 pagesOxford University PresssarafraunaqNo ratings yet
- Uk HSP1Document3 pagesUk HSP1Ery RadiyantiNo ratings yet
- Study of Spectrum of Hemoglobinopathies in Adult Age Group Diagnosed On High Performance Liquid Chromatography in Tertiary Care HospitalDocument9 pagesStudy of Spectrum of Hemoglobinopathies in Adult Age Group Diagnosed On High Performance Liquid Chromatography in Tertiary Care HospitalIJAR JOURNALNo ratings yet
- Pancytopenia Secondary To Bacterial SepsisDocument16 pagesPancytopenia Secondary To Bacterial Sepsisiamralph89No ratings yet
- BlablaDocument3 pagesBlablaRosdiana Elizabeth SiburianNo ratings yet
- BMC Dermatology: Schönlein-Henoch Purpura During Pregnancy With Successful Outcome For Mother and NewbornDocument5 pagesBMC Dermatology: Schönlein-Henoch Purpura During Pregnancy With Successful Outcome For Mother and NewbornteguhNo ratings yet
- A Study of 50 Cases of Hepatorenal: Syndrome and Its OutcomeDocument16 pagesA Study of 50 Cases of Hepatorenal: Syndrome and Its OutcomeRishabh GuptaNo ratings yet
- Antiphospholipid Syndrome in Pediatrics. Rheum Dis Clin N Am 33. 2007Document25 pagesAntiphospholipid Syndrome in Pediatrics. Rheum Dis Clin N Am 33. 2007sprnv2No ratings yet
- Sarcoidosis Review. JAMADocument9 pagesSarcoidosis Review. JAMARafael ReañoNo ratings yet
- A Case of Mushroom Poisoning With Russula Subnigricans: Development of Rhabdomyolysis, Acute Kidney Injury, Cardiogenic Shock, and DeathDocument4 pagesA Case of Mushroom Poisoning With Russula Subnigricans: Development of Rhabdomyolysis, Acute Kidney Injury, Cardiogenic Shock, and DeathsuserNo ratings yet
- Significado Clinico de Impactacion Mucosa de Alta Atenuacion en ABPADocument10 pagesSignificado Clinico de Impactacion Mucosa de Alta Atenuacion en ABPAGonzalo LealNo ratings yet
- Alveolar Hemorrhage in Systemic Lupus Erythematosus: An OverviewDocument11 pagesAlveolar Hemorrhage in Systemic Lupus Erythematosus: An OverviewHaider AlshomraniNo ratings yet
- Jurnal InternationalDocument6 pagesJurnal InternationalLeonal Yudha PermanaNo ratings yet
- Evans Syndrome - A Study of Six Cases With Review of LiteratureDocument6 pagesEvans Syndrome - A Study of Six Cases With Review of Literaturedrrome01No ratings yet
- Northrop 2015Document4 pagesNorthrop 2015Annisa Badriyyah HakimahNo ratings yet
- Edisi 2 Artcl 6Document4 pagesEdisi 2 Artcl 6jackbayNo ratings yet
- Pulmonary Tuberculosis and Its Haematological Correlates-1Document8 pagesPulmonary Tuberculosis and Its Haematological Correlates-1mentari_64No ratings yet
- LepsDocument4 pagesLepslynharee100% (1)
- Late Complications of Biliary Atresia: Hepatopulmonary Syndrome and Portopulmonary HypertensionDocument6 pagesLate Complications of Biliary Atresia: Hepatopulmonary Syndrome and Portopulmonary HypertensionAnisa GayatriNo ratings yet
- Ariculo MauDocument2 pagesAriculo MauMerpi Alvarez GorisNo ratings yet
- Epidemiology and Risk Factors in CKD Patients With Pulmonary HypertensionDocument8 pagesEpidemiology and Risk Factors in CKD Patients With Pulmonary HypertensionshaheershayanqaziNo ratings yet
- Diagnosis and Treatment of Chronic CoughFrom EverandDiagnosis and Treatment of Chronic CoughSang Heon ChoNo ratings yet
- CDC GrafikDocument26 pagesCDC GrafikIwan MiswarNo ratings yet
- chp:10.1007/978 1 84996 247 6 - 12Document9 pageschp:10.1007/978 1 84996 247 6 - 12Iwan MiswarNo ratings yet
- Molecular Basis of Lithium Action: Integration of Lithium-Responsive Signaling and Gene Expression NetworksDocument10 pagesMolecular Basis of Lithium Action: Integration of Lithium-Responsive Signaling and Gene Expression NetworksIwan MiswarNo ratings yet
- Mood-Stabilizing Drugs: Mechanisms of Action: Robert J. Schloesser, Keri Martinowich and Husseini K. ManjiDocument11 pagesMood-Stabilizing Drugs: Mechanisms of Action: Robert J. Schloesser, Keri Martinowich and Husseini K. ManjiIwan MiswarNo ratings yet
- Art:10.1007/s12098 013 1010 2Document2 pagesArt:10.1007/s12098 013 1010 2Iwan MiswarNo ratings yet
- 1 s2.0 S019096221200864X MainDocument8 pages1 s2.0 S019096221200864X MainIwan MiswarNo ratings yet
- Art:10.1007/s12098 013 1013 ZDocument2 pagesArt:10.1007/s12098 013 1013 ZIwan MiswarNo ratings yet
- Dietetics: Health Technologies II Mr. KestnerDocument14 pagesDietetics: Health Technologies II Mr. KestnerIwan MiswarNo ratings yet
- Iridium Satellite System (Iss) : Wireless CommunicationDocument11 pagesIridium Satellite System (Iss) : Wireless CommunicationSmrithi K MNo ratings yet
- Decision Trees and Boosting: Helge Voss (MPI-K, Heidelberg) TMVA WorkshopDocument30 pagesDecision Trees and Boosting: Helge Voss (MPI-K, Heidelberg) TMVA WorkshopAshish TiwariNo ratings yet
- Simulation and ModulationDocument89 pagesSimulation and ModulationGuruKPO67% (6)
- Adamco BIFDocument2 pagesAdamco BIFMhie DazaNo ratings yet
- Writing Home, Painting Home: 17th Century Dutch Genre Painting and The "Sailing Letters"Document17 pagesWriting Home, Painting Home: 17th Century Dutch Genre Painting and The "Sailing Letters"María MazzantiNo ratings yet
- The Price of SilenceDocument9 pagesThe Price of Silencewamu885100% (1)
- STEWART Briony Kumiko and The Dragon FINAL2010Document8 pagesSTEWART Briony Kumiko and The Dragon FINAL2010Tahnee HallNo ratings yet
- Sony Kdl-40xbr9 Kdl-46xbr9 Kdl-52xbr9 Ex2m ChassisDocument118 pagesSony Kdl-40xbr9 Kdl-46xbr9 Kdl-52xbr9 Ex2m ChassisAndy WilsonNo ratings yet
- Shattered Reflections A Journey Beyond The MirrorDocument13 pagesShattered Reflections A Journey Beyond The MirrorSweetheart PrinceNo ratings yet
- DAPA Teams Spider DiagramDocument2 pagesDAPA Teams Spider DiagramEduardoJaimeNo ratings yet
- Laboratory For Energy and The Environment: HighlightsDocument14 pagesLaboratory For Energy and The Environment: HighlightsZewdu TsegayeNo ratings yet
- Yamabe Flow On Nilpotent Lie GroupsDocument20 pagesYamabe Flow On Nilpotent Lie GroupsEnzo RicNo ratings yet
- $50SAT - Eagle2 - Communications - Release Version V1 - 2Document25 pages$50SAT - Eagle2 - Communications - Release Version V1 - 2Usman ShehryarNo ratings yet
- Case-Study & Lessons From Nokia DownfallDocument2 pagesCase-Study & Lessons From Nokia Downfallromesh911100% (1)
- Optimal Design of Low-Cost and Reliable Hybrid Renewable Energy System Considering Grid BlackoutsDocument7 pagesOptimal Design of Low-Cost and Reliable Hybrid Renewable Energy System Considering Grid BlackoutsNelson Andres Entralgo MaldonadoNo ratings yet
- Biogas ProductionDocument7 pagesBiogas ProductionFagbohungbe MichaelNo ratings yet
- Tuyển Sinh 10 - đề 1 -KeyDocument5 pagesTuyển Sinh 10 - đề 1 -Keynguyenhoang17042004No ratings yet
- 2021-01-01 Good Organic GardeningDocument110 pages2021-01-01 Good Organic GardeningValéria GarcezNo ratings yet
- StatementOfAccount 6316692309 21072023 222045Document17 pagesStatementOfAccount 6316692309 21072023 222045Asekar AlagarsamyNo ratings yet
- Vernacular Terms 2 PDFDocument3 pagesVernacular Terms 2 PDFsmmNo ratings yet
- Chaliyama Steel Plant-Rungta Mines Limited Hazard Identification & Risk AssessmentDocument3 pagesChaliyama Steel Plant-Rungta Mines Limited Hazard Identification & Risk AssessmentCPP EI DSpNo ratings yet
- Miller PreviewDocument252 pagesMiller PreviewcqpresscustomNo ratings yet
- SBAS35029500001ENED002Document20 pagesSBAS35029500001ENED002unklekoNo ratings yet
- A Short Version of The Big Five Inventory (BFI-20) : Evidence On Construct ValidityDocument22 pagesA Short Version of The Big Five Inventory (BFI-20) : Evidence On Construct ValidityBagas IndiantoNo ratings yet
- Blue Yellow Playful Illustration Self Care Infographic PosterDocument7 pagesBlue Yellow Playful Illustration Self Care Infographic PosterAin NurasyikinNo ratings yet
- In Re Plagiarism Case Against Justice Del CastilloDocument112 pagesIn Re Plagiarism Case Against Justice Del CastilloRaffyLaguesmaNo ratings yet
- Biology: NO Judul PengarangDocument5 pagesBiology: NO Judul Pengarangkartini11No ratings yet
- Hell by D.L. MoodyDocument7 pagesHell by D.L. MoodyLisaNo ratings yet
- Papper Referensi 2 - Using Warmth As The Visual Design of A Store - Intimacy, Relational Needs, and Approach IntentionsDocument11 pagesPapper Referensi 2 - Using Warmth As The Visual Design of A Store - Intimacy, Relational Needs, and Approach IntentionsBergodo PrajuritNo ratings yet