Professional Documents
Culture Documents
Nec PDF
Nec PDF
Uploaded by
dr.mahensOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nec PDF
Nec PDF
Uploaded by
dr.mahensCopyright:
Available Formats
Journal of Neonatal Surgery 2014;3(3):27
EL-MED-Pub Publishers.
*
Corresponding Author
ORIGINAL ARTICLE
Characteristic Radiological findings in Preterm Infants with Missed
Intestinal Perforation
Sivasankar Jayakumar, Nitin Patwardhan*
Department of Paediatric surgery, University Hospitals of Leicester Infirmary road, Leicester,
United Kingdom LE1 5WW
ABSTRACT
BACKGROUND: Pneumoperitoneum on radiological imaging is typical in intestinal perforation
in necrotizing enterocolitis [NEC]. However, it is not seen in all cases and intestinal
perforation is missed on occasions. We present a series of preterm infants with
characteristic x-ray findings that on exploration revealed missed intestinal perforation.
METHODS: Retrospective review of neonates with intra-operative diagnosis of intestinal
perforation which was missed on x-ray abdomen over a period of 6 months is being
presented here.
RESULTS: Three neonates born at 24 (24-30) weeks of gestation were identified. PDA was
noted in all 3 patients and they required ventilator and inotropic support. Feeds were
commenced at 5 (2-7) days of life. All three patients were treated for NEC. Surgical opinion
was sought in view of localized gas shadow in a fixed position seen on repeated x-rays in all
three patients. All three patients had laparotomy and small bowel resection with ileostomy
formation at a mean age of 26 (24-46) days. Intra-operatively, small bowel perforation and
adjacent pseudocysts filled with air and intestinal contents were noted in all 3 patients.
Post-operatively full feeds were established in all patients.
CONCLUSION: In premature infants with NEC, intestinal perforation can be missed on
occasions. Our patients interestingly, developed characteristic abdominal x-ray findings that
in our experience should prompt for surgical intervention.
Key words: Missed intestinal perforation, Pseudocyst, Necrotizing enterocolitis, Preterm, Neonate
INTRODUCTION
Necrotizing enterocolitis (NEC) is a severe
inflammatory process of the gastrointestinal
tract in neonates and is associated with a
significant morbidity and mortality. Despite
advances in neonatal care, NEC still remains as
one of the most common causes of surgical
intervention in the neonate. In NEC, the extent
of disease could be focal [Isolated], multifocal or
pan-intestinal. In a retrospective study on 32
patients with NEC, isolated NEC was present in
8 (25%), multifocal NEC in 19 (59%) and pan
intestinal NEC in 5 (16%) of the operated cases
[1]. Abdominal x-ray [AXR] is an important
component of the assessment of infants with
suspected NEC. AXR findings in NEC ranges
from dilated bowel loops in suspected NEC to
pneumatosis intestinalis, portal venous gas
shadows and pneumoperitoneum in cases of
definite NEC [2]. Pneumoperitoneum is widely
accepted as an indication for surgical
intervention. Very rarely, such a
pneumoperitoneum secondary to intestinal
perforation could be missed. We present a
series of three preterm neonates who had initial
treatment for NEC and later developed
characteristic AXR findings that on surgical
intervention were noted to be pseudocysts
adjacent to bowel perforation. The details of
presentation of these cases along with intra-
Characteristic Radiological findings in Preterm Infants with Missed Intestinal Perforation
Journal of Neonatal Surgery Vol. 3(3); 2014
operative findings and outcomes are presented
and discussed in this article.
MATERIALS AND METHODS
Retrospective review of neonates with intra-
operative diagnosis of intestinal perforation
which was missed on x-ray abdomen over a
period of 6 months is being presented here.
RESULTS
Three neonates, with a median gestational age
of 24 (24-30) weeks with pseudocyst formation
[noted at laparotomy] were identified over a
period of 6 months. Antenatal scans did not
reveal any bowel abnormality and antenatal
serology was negative for HIV, Hepatitis B,
VDRL and Rubella was immune in all 3
patients. PDA was noted in all 3 patients and
they required inotropic support. Feeds were
commenced at 5 [2, 5 & 7] days of life.
Intravenous antibiotics for suspected NEC were
commenced at 18 [14, 18 & 37] days of life.
Surgical opinion was sought in view of
persistent abdominal distention and ongoing
sepsis. AXR at the time of referral did not show
any definite signs of NEC in all 3 cases. Case 1,
demonstrated a gas filled blister on the anterior
abdominal wall [Fig. 1] at the time of referral.
AXR in Case 2 showed persistent fixed loop
surrounding a cyst like space in the abdomen
[Fig. 2]. In Case 3, persistent localized gas
shadow was seen on subsequent x-rays [Fig. 3].
Fig. 1(A): Photograph of case 1 on day 23 of life, showing
right peri-umbilical swelling;(B): AXR of Case 1 on day 23 of
life showing localized gas shadow at the site of peri-
umbilical swelling; (C): Lateral x-ray of the abdomen of case
1 on day 23 of life showing dilated bowel and air filled cyst
at the site of peri-umbilical swelling.
All the three neonates underwent laparotomy
and small bowel resection with ileostomy
formation. The age of the patients at the time of
laparotomy was 26 (24, 26 & 46) days. The
individual patient characteristics of all 3
patients are summarized in Table 1. Intra-
operatively, small bowel perforation along with
pseudocyst containing air and intestinal
contents was noted. No intestinal atresia or
other bowel pathology was noted.
Histopathological examination of the resected
cysts and adjacent small bowel were consistent
with NEC in all the three cases. Subsequent
cystic fibrosis screening was negative in all
three patients. Post-operatively full feeds were
established in all 3 patients after stoma
reversal and have been discharged home.
Figure 2: (A): AXR of Case 2 on day 44 of life, showing
dilated bowel loop surrounding a cyst like appearance in
the central abdomen; (B): Lateral shoot through x-ray of the
abdomen of case 2 on day 44 of life showing dilated bowel
in the central abdomen. No free air is seen; (C): AXR of
Case 2 on day 46 of life, showing fixed dilated bowel loop
surrounding a cyst like appearance in the central abdomen.
Figure 3: (A): AXR of case 3 done on day 14 of life, taken at
the referring hospital showing free air in the abdomen. This
finding was missed at the referring hospital; (B): AXR of
case 3 done on day 24 of life, showing localized gas shadow
in the right upper quadrant; (C): AXR of case 3 done on 26
of life, showing persistent localized gas shadow in the right
upper quadrant.
DISCUSSION
Necrotizing enterocolitis (NEC) is diagnosed in
6% of very low birth weight (VLBW; <1500 g)
and 8% of extremely low birth weight (ELBW;
<1000 g) infants [3]. Very few clinical studies
have examined surgical findings in ELBW
neonates with NEC. Earlier series on 50 ELBW
patients showed focal NEC in 52% and pan
involvement in 28%, but no cysts were reported
in their study [1]. In a recent study on 158
ELBW neonates, the incidence of perforated
NEC in ELBW premature infants was reported
as 5.1% and the average age at onset of
perforated NEC was 26 days [4]. In this study,
dilated and fixed bowel loops, bowel wall
Characteristic Radiological findings in Preterm Infants with Missed Intestinal Perforation
Journal of Neonatal Surgery Vol. 3(3); 2014
thickening and ascites with brown stool-like
substance on percutaneous drainage were the
predominant signs at the time of diagnosis of
perforated NEC and these signs may be
considered as a significant sign of perforated
NEC despite the absence of free air on
radiography [4]. However, in the absence of free
air on radiography and prior to percutaneous
drainage, it is extremely difficult to know if
bowel perforation has occurred.
Table 1: Tabular column showing individual patient characteristics in all the three cases noted in our series.
Although absolute evidence of bowel
perforation/pneumoperitoneum was not
evident in all our patients at the time of
presentation to us, one of our patients [Case 3]
had an AXR sent to us from the referring
hospital that clearly revealed a
pneumoperitoneum on day 14 of life [Fig. 3].
This patient was referred to us on day 24 of life
after the above finding was missed at the
referring hospital. The subsequent AXR taken
on day 24 of life showed a cystic appearance
but no obvious pneumoperitoneum. As similar
findings were noted intra-operatively in the
other 2 cases in our series with the background
of NEC, it is likely that they also had a missed
intestinal perforation and subsequent
pseudocyst formation.
Lorimer and Ellis classified meconium
peritonitis resulting from antenatal perforation
into generalized, fibro-adhesive, cystic, and
healed types. In the cystic type, the perforation
site does not heal effectively, and a thick-walled
cyst forms by fixation of bowel loops [5]. Such
cysts are usually referred as meconium
pseudocysts. Although, in our series of three
patients similar types of cysts were noted, none
of these patients had an antenatal diagnosis of
meconium cysts or any bowel abnormality
suggesting a postnatal and not antenatal event
in formation of the cysts. All patients had
received a full course of triple antibiotics with
presumed diagnosis of NEC prior to surgical
referral. It is likely that the antibiotic support
prevented generalized sepsis and may have
contributed to localized pseudocyst formation
that is similarly seen in antenatal meconium
pseudocysts.
Wexler, in 1978, first described five cases of
NEC with persistent dilated loop sign noted in
plain abdominal x-rays. The position of dilated
Characteristic Radiological findings in Preterm Infants with Missed Intestinal Perforation
Journal of Neonatal Surgery Vol. 3(3); 2014
bowel loops in these cases remained
unchanged in the abdominal x-rays over a
period of 24 to 36 hours and he suggested that
fixed loop of bowels should be surgically
intervened [6]. However, a review of the records
and radiographs of 21 newborn infants with
NEC and 10 control infants performed by
Leonard et al, to test the significance of the
persistent loop sign in NEC did not support the
use of a persistent segmental loop of bowel as a
single criterion for surgical intervention [7].
Interestingly, all of our 3 patients had
persistent fixed bowel loops with abnormal gas
shadows on AXR which intra-operatively were
confirmed to be extra intestinal.
It is well known that neonatal intestinal
perforation may heal spontaneously with or
without a drain insertion [8], however, in all
other cases intervention is needed due to
continued clinical deterioration of the patient.
Our series highlights a third possible outcome
for neonatal intestinal perforation. The cysts
noted in our patients intra-operatively seem to
be a rare occurrence and although we are
unable to describe the exact pathogenesis
behind them, they are most likely to represent
a concealed intestinal perforation. However,
such characteristic x-ray findings in premature
neonates treated for NEC should prompt a
caring physician/surgeon for surgical
intervention.
CONCLUSION
To conclude, intestinal perforation in
premature infants with NEC is a well-known
occurrence. This may be missed occasionally.
The patient may continue to deteriorate or may
have the perforation sealed. Our patients
interestingly, developed pseudocysts localized
at the site of perforation with characteristic
abdominal x-ray findings that in our experience
should prompt for surgical intervention.
REFERENCES
1. Rowe MI, Reblock KK, Kurkchubasche AG, Healey
PJ. Necrotizing enterocolitis in the extremely low
birth weight infant. J Pediatr Surg. 1994; 29:987-
90.
2. Tam AL, Camberos A, Applebaum H. Surgical
decision making in necrotizing enterocolitis and
focal intestinal perforation: predictive value of
radiologic findings. J Pediatr Surg. 2002; 37:1688-
91.
3. Blakely ML, Tyson JE, Lally KP, et al McDonald S,
Stoll BJ, Stevenson DK, Poole WK, Jobe AH,
Wright LL, Higgins RD. NICHD Neonatal Research
Network. Laparotomy versus peritoneal drainage
for necrotizing enterocolitis or isolated intestinal
perforation in extremely low birth weight infants:
outcomes through 18 months adjusted age.
Pediatrics 2006; 117:680-7.
4. Wu CH, Tsao PN, Chou HC, et al Tang JR, Chan
WK, Tsou KI. Necrotizing enterocolitis complicated
with perforation in extremely low birth-weight
premature infants. Acta Paediatr Taiwan. 2002;
43:127-32.
5. Lorimer WS Jr, Ellis DG. Meconium peritonitis.
Surgery. 1966; 60:470-5.
6. Wexler HA: The persistent loop sign in neonatal
necrotizing enterocolitis: a new indication for
surgical intervention? Radiology. 1978;126:201-4.
7. Leonard T Jr, Johnson JF, Pettett PG. Critical
evaluation of the persistent loop sign in
necrotizing enterocolitis. Radiology.
1982;142:385-6.
8. Khan RA, Mahajan JK, Rao KL. Spontaneous
intestinal perforation in neonates: is surgery
always indicated? Afr J Paediatr Surg. 2011;
8:249-51.
Address for correspondence
Mr. N Patwardhan,
Department of Paediatric surgery, University Hospitals Leicester, Infirmary road, Leicester,
United Kingdom LE1 5WW
E mail: nvpats@gmail.com
Submitted on: 31-05-2014
Accepted on: 29-06-2014
Conflict of interest: None
Source of Support: Nil
You might also like
- Contamination Control Strategy DevelopmentDocument75 pagesContamination Control Strategy DevelopmentArnaldo García100% (9)
- Enthesopathies Knowledge Update - Dreisilker, Ulrich, Dr. MedDocument164 pagesEnthesopathies Knowledge Update - Dreisilker, Ulrich, Dr. MedMarco100% (1)
- Jurnal FixDocument5 pagesJurnal FixHana MitayaniNo ratings yet
- Esophageal Atresia and Tracheoesophageal FistulaDocument28 pagesEsophageal Atresia and Tracheoesophageal FistulaarifNo ratings yet
- 201 203 AbdominalDocument3 pages201 203 AbdominalManal Salah DorghammNo ratings yet
- 014 - The Value of Ileoscopy With Biopsy in The Diagnosis of Intestinal Crohn's DiseaseDocument6 pages014 - The Value of Ileoscopy With Biopsy in The Diagnosis of Intestinal Crohn's DiseaseVân NguyễnNo ratings yet
- Brisbune, Queenslund Summary: Twenty-Seven Patients With Ovarian Remnant Syndrome WereDocument3 pagesBrisbune, Queenslund Summary: Twenty-Seven Patients With Ovarian Remnant Syndrome WereFlaviu TabaranNo ratings yet
- Intestinal Tuberculosis With Abdominal ComplicationsDocument7 pagesIntestinal Tuberculosis With Abdominal ComplicationsTheodelinda Andreea DumitriuNo ratings yet
- Noncommunicating Isolated Enteric Duplication Cyst in The Abdomen in Children: Report of One Case and Review of The LiteratureDocument3 pagesNoncommunicating Isolated Enteric Duplication Cyst in The Abdomen in Children: Report of One Case and Review of The Literatureallan felipeNo ratings yet
- Laparoscopic Appendectomy During PregnancyDocument4 pagesLaparoscopic Appendectomy During PregnancypsychobillNo ratings yet
- Adult Intussussception Int J Student Res 2012Document3 pagesAdult Intussussception Int J Student Res 2012Juan De Dios Diaz-RosalesNo ratings yet
- International Journal of Surgery Case Reports: Adenocarcinoma in An Ano-Vaginal Fistula in Crohn's DiseaseDocument4 pagesInternational Journal of Surgery Case Reports: Adenocarcinoma in An Ano-Vaginal Fistula in Crohn's DiseaseTegoeh RizkiNo ratings yet
- Rectal Prolapse: Rare Presentation and Complication: Case ReportDocument3 pagesRectal Prolapse: Rare Presentation and Complication: Case Reportadi tiarmanNo ratings yet
- Capsula EndoscopicaDocument4 pagesCapsula EndoscopicaYuu DenkiNo ratings yet
- Annrcse01521 0053Document1 pageAnnrcse01521 0053Muhammad Fiqhi HardiansyahNo ratings yet
- Analysis of The Use of Upright Abdominal Radiography For Evaluating Intestinal Perforations in Handlebar TraumasDocument8 pagesAnalysis of The Use of Upright Abdominal Radiography For Evaluating Intestinal Perforations in Handlebar TraumasNur AzizaNo ratings yet
- Acute Appendicitis of The Appendiceal StumpDocument3 pagesAcute Appendicitis of The Appendiceal StumpXavier JarrínNo ratings yet
- Complicated AppendicitisDocument4 pagesComplicated AppendicitisMedardo ApoloNo ratings yet
- Cap Polyposis in Children: Case Report and Literature ReviewDocument6 pagesCap Polyposis in Children: Case Report and Literature ReviewLuis ArrietaNo ratings yet
- Clinical Study: Adhesive Intestinal Obstruction in Infants and Children: The Place of Conservative TreatmentDocument5 pagesClinical Study: Adhesive Intestinal Obstruction in Infants and Children: The Place of Conservative TreatmentOdiet RevenderNo ratings yet
- Upper Gastrointestinal Endoscopy in Turkey: A Review of 5,000 CasesDocument2 pagesUpper Gastrointestinal Endoscopy in Turkey: A Review of 5,000 CasesEnderson MedeirosNo ratings yet
- Gastroenterology Cases PracticeDocument19 pagesGastroenterology Cases PracticeIbtissame BadadNo ratings yet
- Abstract ReferenceDocument10 pagesAbstract ReferenceOvamelia JulioNo ratings yet
- Radiology: World Journal ofDocument7 pagesRadiology: World Journal ofWenny EudensiaNo ratings yet
- 4 - Clinical Patterns in Crohn's Disease - A Statistical Study of 615 CasesDocument9 pages4 - Clinical Patterns in Crohn's Disease - A Statistical Study of 615 CasesVân NguyễnNo ratings yet
- Colovesical FistulaDocument4 pagesColovesical FistulaNisaNo ratings yet
- Kayatsha - Gastroschisis and Omphalocele A Case ReportDocument4 pagesKayatsha - Gastroschisis and Omphalocele A Case ReportAffannul HakimNo ratings yet
- Triple GallbladerDocument12 pagesTriple GallbladerRudy Arindra WijayaNo ratings yet
- Abdominal Tuberculosis in Nepal Medical College Teaching Hospital, KathmanduDocument4 pagesAbdominal Tuberculosis in Nepal Medical College Teaching Hospital, KathmanduSavitri Maharani BudimanNo ratings yet
- Uterine Adherence To Anterior Abdominal Wall After Caesarean SectionDocument3 pagesUterine Adherence To Anterior Abdominal Wall After Caesarean SectionGladstone AsadNo ratings yet
- Adult Intussusception: A Retrospective ReviewDocument5 pagesAdult Intussusception: A Retrospective ReviewkameliasitorusNo ratings yet
- IdiopathicDocument3 pagesIdiopathicAulya ArchuletaNo ratings yet
- Retroperitoneal Appendicitis: A Surgical DilemmaDocument2 pagesRetroperitoneal Appendicitis: A Surgical DilemmaputraNo ratings yet
- Wound: Abdominal DehiscenceDocument5 pagesWound: Abdominal DehiscencesmileyginaaNo ratings yet
- 2017-05 Norfolk and Waveney CPDG Policy Briefing Paper - Capsule EndoscoDocument4 pages2017-05 Norfolk and Waveney CPDG Policy Briefing Paper - Capsule EndoscoAlessioNavarraNo ratings yet
- Small Bowel Obstruction-RcnaDocument21 pagesSmall Bowel Obstruction-RcnaAL MARIA MEDNo ratings yet
- Aipm 17 71Document4 pagesAipm 17 71Iful SaifullahNo ratings yet
- 1 s2.0 S0929644108600089 MainDocument5 pages1 s2.0 S0929644108600089 Maineva kacanjaNo ratings yet
- MRI Sumber 1Document9 pagesMRI Sumber 1Novrizawijaya2No ratings yet
- Guidelines On Small Bowel Enteroscopy and Capsule Endoscopy in AdultsDocument12 pagesGuidelines On Small Bowel Enteroscopy and Capsule Endoscopy in Adultssaeed5198No ratings yet
- Role of Laparoscopic Cholecystectomy in The Early Management of Acute Gallbladder DiseaseDocument6 pagesRole of Laparoscopic Cholecystectomy in The Early Management of Acute Gallbladder DiseaseHoracio ChaconNo ratings yet
- Posterior Sagittal Anorectoplasty in Anorectal MalformationsDocument5 pagesPosterior Sagittal Anorectoplasty in Anorectal MalformationsmustikaarumNo ratings yet
- Huang 1984Document4 pagesHuang 1984vinicius.alvarez3No ratings yet
- Gastric Volvulus With Hiatal Hernia in A Young Male A Case ReportDocument5 pagesGastric Volvulus With Hiatal Hernia in A Young Male A Case ReportAthenaeum Scientific PublishersNo ratings yet
- Pediatric Surgery: Original ArticleDocument4 pagesPediatric Surgery: Original ArticleRiyadhiErvinNo ratings yet
- Trichobezoar With Large Bowel Obstruction in Children - Case ReportDocument3 pagesTrichobezoar With Large Bowel Obstruction in Children - Case ReportSajag GuptaNo ratings yet
- TR Kelompok 4 AbdomenDocument29 pagesTR Kelompok 4 AbdomenShelly AnggrainiNo ratings yet
- Pi Is 0016508500545053Document5 pagesPi Is 0016508500545053Abdullah KhanNo ratings yet
- Pi Is 0016508500545053Document5 pagesPi Is 0016508500545053Abdullah KhanNo ratings yet
- Gut 1965 James 372 5Document5 pagesGut 1965 James 372 5Agus SyaifudinNo ratings yet
- J Epsc 2015 05 012Document4 pagesJ Epsc 2015 05 012Hanung PujanggaNo ratings yet
- Tuberculous Ileal Perforation in Post-Appendicectomy PeriOperative Period: A Diagnostic ChallengeDocument3 pagesTuberculous Ileal Perforation in Post-Appendicectomy PeriOperative Period: A Diagnostic ChallengeIOSRjournalNo ratings yet
- Management of Rectal Prolapse in ChildrenDocument6 pagesManagement of Rectal Prolapse in ChildrenWaNda GrNo ratings yet
- Choledochal CystDocument5 pagesCholedochal CystZulia Ahmad BurhaniNo ratings yet
- Management of Perforated Appendicitis in Children: A Decade of Aggressive TreatmentDocument5 pagesManagement of Perforated Appendicitis in Children: A Decade of Aggressive Treatmentapi-308365861No ratings yet
- Umbilical Cord Hernias: Prenatal Diagnosis and Natural HistoryDocument4 pagesUmbilical Cord Hernias: Prenatal Diagnosis and Natural HistoryFriska GriffinNo ratings yet
- Laparoscopy in The Acute AbdomenDocument15 pagesLaparoscopy in The Acute AbdomenDragoiu AlexandraNo ratings yet
- An Antenatal Appearance of Megacystis-Microcolon-Intestinal Hypoperistalsis SyndromeDocument8 pagesAn Antenatal Appearance of Megacystis-Microcolon-Intestinal Hypoperistalsis SyndromeserubimNo ratings yet
- Balloon and Bougie Dilation of Benign Esophageal Strictures: Ajay George, Vikas SinhaDocument3 pagesBalloon and Bougie Dilation of Benign Esophageal Strictures: Ajay George, Vikas SinhaAgus KarsetiyonoNo ratings yet
- Infectious IleoceicitisDocument2 pagesInfectious IleoceicitisYandiNo ratings yet
- Superior Vesical Fissure: Variant Classical Bladder ExstrophyDocument3 pagesSuperior Vesical Fissure: Variant Classical Bladder ExstrophyChindia BungaNo ratings yet
- Esophageal Preservation and Replacement in ChildrenFrom EverandEsophageal Preservation and Replacement in ChildrenAshwin PimpalwarNo ratings yet
- Krizzaveronica - Cuevas@deped - Gov.ph: Poblacion, San Jose, Negros Oriental Contact #: 09176276121/ 09276455321Document2 pagesKrizzaveronica - Cuevas@deped - Gov.ph: Poblacion, San Jose, Negros Oriental Contact #: 09176276121/ 09276455321StephanieNo ratings yet
- FrontMatter IndigenousFermentedFoodsfortheTropicsDocument23 pagesFrontMatter IndigenousFermentedFoodsfortheTropicsGustavoTorresNo ratings yet
- Brain Project Explanation and RubricDocument2 pagesBrain Project Explanation and RubricahdyalNo ratings yet
- DM Technical Guideline No.-10-Disposal-of-Unwanted-Materials-September-2020Document8 pagesDM Technical Guideline No.-10-Disposal-of-Unwanted-Materials-September-2020katageriguruNo ratings yet
- Different Types of Bath PresentationDocument55 pagesDifferent Types of Bath PresentationThomas Mathew100% (2)
- Obstetric Abdominal Examination OSCE GuideDocument16 pagesObstetric Abdominal Examination OSCE GuideMuhammad Aamir IqbalNo ratings yet
- AnalgesicDrugs Combinations in Thetreatment of Different Types of PainDocument68 pagesAnalgesicDrugs Combinations in Thetreatment of Different Types of PainAnuj MairhNo ratings yet
- 10 Overtraining SyndromeDocument15 pages10 Overtraining SyndromeTasniiem KhmbataNo ratings yet
- PAR - 4849 - Nitrofurantoin MC Mylan - 9 MRT 2022Document12 pagesPAR - 4849 - Nitrofurantoin MC Mylan - 9 MRT 2022Marcel JinihNo ratings yet
- Body Composition PDFDocument10 pagesBody Composition PDFSiti Fathimah Mohd RidzuanNo ratings yet
- Higher Running Pace Intensity Spectrum ChartDocument1 pageHigher Running Pace Intensity Spectrum Chart23S46 ZHAO TIANYUNo ratings yet
- Fluid Volume Deficient Cues SDocument6 pagesFluid Volume Deficient Cues SjedrickNo ratings yet
- Continuous Passive Motion DeviceDocument3 pagesContinuous Passive Motion DeviceSanny RamosNo ratings yet
- Volume: 04 Issue: 02 - Mar-Apr 2023Document9 pagesVolume: 04 Issue: 02 - Mar-Apr 2023Central Asian StudiesNo ratings yet
- ISAPS 8 2 InteractiveDocument27 pagesISAPS 8 2 Interactivehuyenthanh1807No ratings yet
- Gc-Ms Analysis of Phytochemical Compounds Present in The Rhizomes of NerviliaDocument7 pagesGc-Ms Analysis of Phytochemical Compounds Present in The Rhizomes of NerviliaMd. Badrul IslamNo ratings yet
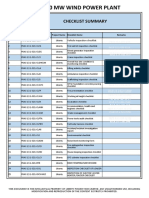
- Act02 50 MW Wind Power Plant: Checklist SummaryDocument54 pagesAct02 50 MW Wind Power Plant: Checklist SummaryRaza Muhammad SoomroNo ratings yet
- Gotu Kola (Centella Asiatica)Document11 pagesGotu Kola (Centella Asiatica)My Pham Thi DiemNo ratings yet
- Pharmaceutical Care v. Rowe, 429 F.3d 294, 1st Cir. (2005)Document27 pagesPharmaceutical Care v. Rowe, 429 F.3d 294, 1st Cir. (2005)Scribd Government DocsNo ratings yet
- WHO EMRO - Tobacco and Waterpipe Use Increases The Risk of Suffering From COVID-19 - Know The Truth - TFIDocument3 pagesWHO EMRO - Tobacco and Waterpipe Use Increases The Risk of Suffering From COVID-19 - Know The Truth - TFIJesse DanzigNo ratings yet
- CPD Re-Orentation & Performance ReviewDocument24 pagesCPD Re-Orentation & Performance ReviewAhmed AdemNo ratings yet
- The Healing Wonders of Honey and CinnamonDocument5 pagesThe Healing Wonders of Honey and CinnamonRonie100% (9)
- Hemoglobina PDFDocument2 pagesHemoglobina PDFDiana LauraNo ratings yet
- Ebm JurnalDocument198 pagesEbm Jurnalcamelia musaadNo ratings yet
- Idioma Moderno I: Inglés Unit 3 Autoevaluación 2013/2014: New Inside Out Upper-Intermediate Unit 3 TestDocument27 pagesIdioma Moderno I: Inglés Unit 3 Autoevaluación 2013/2014: New Inside Out Upper-Intermediate Unit 3 TestAneider Iza ErvitiNo ratings yet
- Biostatistics 203. Survival Analysis: YhchanDocument8 pagesBiostatistics 203. Survival Analysis: YhchanselinblueNo ratings yet
- 2023 IFBB European Bodybuilding ChampionshipsDocument42 pages2023 IFBB European Bodybuilding ChampionshipsbobobiscotteNo ratings yet
- Perdido - Activity 4 Nutri.Document3 pagesPerdido - Activity 4 Nutri.Kariza PerdidoNo ratings yet