Professional Documents
Culture Documents
Al Ahmad 2014 Journal of Endodontics
Al Ahmad 2014 Journal of Endodontics
Uploaded by
survivor1998Copyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5835)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (350)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- ptw1 Assesment QuestionDocument6 pagesptw1 Assesment Questionharis100% (2)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Patterns of Language Comprehension Deficit in Abused and Neglected Children - Fox Et Al. 53 (3) : 239 - Journal of Speech and Hearing DisordersDocument3 pagesPatterns of Language Comprehension Deficit in Abused and Neglected Children - Fox Et Al. 53 (3) : 239 - Journal of Speech and Hearing DisordersGabriel RendonNo ratings yet
- HYEN-RFQ-ME-004 - RFQ For FET - Rev.C - 210218Document22 pagesHYEN-RFQ-ME-004 - RFQ For FET - Rev.C - 210218MouiciNo ratings yet
- n119 So Kunjungan BP SPV Maulana Mulya Ke 3 22-10-2022 (Template Form So)Document260 pagesn119 So Kunjungan BP SPV Maulana Mulya Ke 3 22-10-2022 (Template Form So)niceso 21No ratings yet
- Mouth Preparation For RPDDocument45 pagesMouth Preparation For RPDArbaz SajjadNo ratings yet
- National Professional Practice Examination (NPPE) Candidate GuideDocument13 pagesNational Professional Practice Examination (NPPE) Candidate Guidedemet cioncaNo ratings yet
- Kuliah Radiologi Emergensi - Maret 2020 - PlainDocument67 pagesKuliah Radiologi Emergensi - Maret 2020 - PlainArief VerditoNo ratings yet
- Respiratory AssessmentDocument27 pagesRespiratory AssessmentAinaB ManaloNo ratings yet
- Zeniton 70 IFUDocument292 pagesZeniton 70 IFUyoelalperinbackupNo ratings yet
- PUSH UP PFT JOSEPH L. CELICIOUS JR. 1Document12 pagesPUSH UP PFT JOSEPH L. CELICIOUS JR. 1Arnelson DerechoNo ratings yet
- Ota Go Correctional FacilityDocument14 pagesOta Go Correctional FacilityKier Marcial V. Collao IVNo ratings yet
- Bionic Eye - An Artificial Vision & Comparative Study Based On Different Implant TechniquesDocument9 pagesBionic Eye - An Artificial Vision & Comparative Study Based On Different Implant TechniquesGabi BermudezNo ratings yet
- Transitional Housing ListDocument27 pagesTransitional Housing ListA IDOHERBALIFE IDOHERBABBASLIFENo ratings yet
- Ethics Review E1 FormDocument3 pagesEthics Review E1 FormShivali RS SrivastavaNo ratings yet
- Chapter 02 - Diversity On OrganizationsDocument29 pagesChapter 02 - Diversity On OrganizationsAsra AliNo ratings yet
- Aip Budget 2024 Needed DataDocument22 pagesAip Budget 2024 Needed Datamoox TVNo ratings yet
- Block 1Document47 pagesBlock 1Yashwant ChauhanNo ratings yet
- Rockwell Maintenance Manual 4B Auto Slack Adjuster 1998Document26 pagesRockwell Maintenance Manual 4B Auto Slack Adjuster 1998ScottNo ratings yet
- 20220206542333tangazo La Kazi La Mkataba Rea 1Document3 pages20220206542333tangazo La Kazi La Mkataba Rea 1SABATO HARUNI (neGro)No ratings yet
- AkQuire HDCDocument1 pageAkQuire HDCBrgy Sta. CruzNo ratings yet
- Tugas Matriks JurnalDocument24 pagesTugas Matriks JurnalEti NurmahdaniNo ratings yet
- Pragati Life Insurance Limited Network Hospitals & Diagnostic Centres For Discount CardDocument9 pagesPragati Life Insurance Limited Network Hospitals & Diagnostic Centres For Discount CardImran SikderNo ratings yet
- Strategic Management (Assignment) HMSM 4032Document6 pagesStrategic Management (Assignment) HMSM 4032MOZAIDNo ratings yet
- RU - Trauma and Emergency CareDocument32 pagesRU - Trauma and Emergency CareryanNo ratings yet
- Girdle Stone Procedure in Bilateral Rheumatoid Hip: A Case ReportDocument2 pagesGirdle Stone Procedure in Bilateral Rheumatoid Hip: A Case Reportumer ilyasNo ratings yet
- Proofex Torchseal 3PDocument4 pagesProofex Torchseal 3PFZweiNo ratings yet
- Getting Out of My BoxDocument4 pagesGetting Out of My Boxapi-532881677No ratings yet
- Learning and Teaching in The Clinical EnvironmentDocument4 pagesLearning and Teaching in The Clinical EnvironmentDaniel Alejandro Lozano MorenoNo ratings yet
- Fowler, Gasiorek, & Giles (2015) - Don't Talk Yourself Into An Early Grave! The Role of Communication in Aging WellDocument2 pagesFowler, Gasiorek, & Giles (2015) - Don't Talk Yourself Into An Early Grave! The Role of Communication in Aging WellCraig FowlerNo ratings yet
- Nasal TumorDocument20 pagesNasal TumorMahmoud ElsherbenyNo ratings yet
Al Ahmad 2014 Journal of Endodontics
Al Ahmad 2014 Journal of Endodontics
Uploaded by
survivor1998Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Al Ahmad 2014 Journal of Endodontics
Al Ahmad 2014 Journal of Endodontics
Uploaded by
survivor1998Copyright:
Available Formats
Antibiotic Resistance and Capacity for Biolm Formation
of Different Bacteria Isolated from Endodontic
Infections Associated with Root-lled Teeth
Ali Al-Ahmad, PD,* Hawnaz Ameen,* Klaus Pelz, MD,
Lamprini Karygianni, DMD,*
Annette Wittmer,
Annette C. Anderson, Dr hum med,* Bettina Spitzm uller,*
and Elmar Hellwig, DMD*
Abstract
Introduction: To date, a variety of microbial species
have been isolated from endodontic infections.
However, endodontic clinical bacterial isolates have
not been sufciently characterized with regard to their
capacity for antibiotic resistance and biolm formation.
In this study, antibiotic resistance and biolm formation
of 47 different aerobic and anaerobic bacterial isolates,
belonging to 32 different species previously isolated
from infected lled root canals, were studied. Methods:
Antibiotic sensitivity to 11 antibiotics including penicillin
G, amoxicillin, clindamycin, gentamicin, vancomycin,
tetracycline, doxycycline, fosfomycin, rifampicin, cipro-
oxacin, and moxioxacin was tested using the stan-
dardized Etest method (Bio Merieux, Marcy-1Etoile,
France). The antibiotic sensitivity of 4 control strains
was also estimated in parallel. Additionally, the capacity
to form biolms was quantied using the microtiter
plate test. Results: Different aerobic and anaerobic
bacterial species were either resistant against a number
of antibiotics or showed high minimal inhibitory concen-
trations against clinically relevant antibiotics. Five
aerobic and 2 anaerobic isolates, including Entero-
coccus faecalis, Streptococcus mutans, Lacto-
bacillus fermentum, Actinomyces naeslundii,
Actinomyces viscosus, Prevotella buccae, and
Propionibacterium acidifaciens, were character-
ized as being high biolm producers, whereas 8 aerobic
and 3 anaerobic isolates were found to be moderate bio-
lm producers. Most isolates with resistance or mark-
edly high minimal inhibitory concentration values were
also either moderate biolm producers or high biolm
producers. Conclusions: These results suggest that
the clinical signicance of endodontic infections could
include that they serve as a reservoir for antibiotic resis-
tance. Furthermore, endodontic treatment should
consider the adhesion and biolm formation by a variety
of bacteria. (J Endod 2014;40:223230)
Key Words
Antibiotic resistance, apical periodontitis, biolm, endodontic infection
T
he persistence of microorganisms in root canal infections is the most widely
accepted cause of endodontic treatment failure and is accompanied by the
continuing presence of periradicular lesions (1, 2). In cases of endodontic
retreatment, microorganisms have been isolated from 35%100% of the root canal
treated teeth after removal of the obturation material (313). Many studies have
highlighted the diversity of the microbial populations isolated from secondary
endodontic infections as described in an earlier report from our group (13). However,
very few studies have characterized the recovered clinical bacterial isolates from
secondary endodontic infections with regard to their antibiotic resistance or capacity
to form biolm. Both characteristics are of major clinical concern. Preethee et al
(14) recently found evidence that efaA, a potent Enterococcus faecalis virulence
gene associated with infective endocarditis, can be found in E. faecalis strains detected
in therapy-resistant infected root canals. Because E. faecalis has been frequently recov-
ered from persistent and secondary endodontic infections (13) and microorganisms
such as streptococci found in infected root canals are known to be potential agents
of endocarditis, the characterization of antibiotic resistance of endodontic bacteria
remains an important focus of microbiological research.
Another clinically important property of endodontic microorganisms is their
ability to form biolms. In treated and untreated root canals, apical periodontitis
can be classied as a biolm-induced disease (15, 16). To the best of our
knowledge, among different clinical bacterial isolates recovered from endodontic
infections, E. faecalis is the only species that has been widely studied for its capacity
to form biolm (17, 18). If bacteria participate in gene exchange within a biolm
via horizontal gene transfer, processes leading to a spread of antibiotic resistance
genes between different clinically relevant species can be accelerated. As
summarized by Madson et al (19), horizontal gene transfer rates are typically higher
in biolm communities compared with those in planktonic niches. Thus, there is
a connection between biolm formation and horizontal gene transfer. In addition to
this, the persistence of endodontic bacteria via biolm formation underlines the neces-
sity for more effective methods not only to completely eliminate bacteria during
endodontic retreatment but also to isolate all of the existing microorganisms during
the microbiological sampling from infected root canals. It should also be kept in
mind that the complex anatomy of the root canal poses further difculties because bio-
lms of persistent microorganisms within root canals may also be located on the walls of
From the Departments of *Operative Dentistry and Periodontology and
Hygiene and Microbiology, Albert-Ludwigs-University, Freiburg, Germany.
Address requests for reprints to Dr Ali Al-Ahmad, Department of Operative Dentistry and Periodontology, University School and Dental Hospital, Hugstetter Strae
55, D-79106 Freiburg, Germany. E-mail address: ali.al-ahmad@uniklinik-freiburg.de
0099-2399/$ - see front matter
Copyright 2014 American Association of Endodontists.
http://dx.doi.org/10.1016/j.joen.2013.07.023
Basic ResearchBiology
JOE Volume 40, Number 2, February 2014 Antibiotic Resistance and Capacity of Bacteria 223
ramications and isthmuses (15). The aim of the present study was to
analyze the capacity for biolm formation and a broad pattern of anti-
biotic sensitivity for a diverse array of clinical bacterial isolates obtained
from patients with secondary endodontic infections in asymptomatic
teeth with apical periodontitis.
Material and Methods
Clinical Bacterial Isolates and Strain Maintenance
A total of 21 patients were referred to the University Clinic and
Dental Hospital, University of Freiburg, Freiburg, Germany, for
endodontic retreatment over a period of 2 years. After microbiolog-
ical sampling, 47 different bacterial isolates belonging to 32 different
species were isolated from the infected root canals. All patients gave
their written informed consent to the study protocol, which had been
approved by the Ethics Committee (no. 140/09, University of Frei-
burg). During the pretreatment examination, the following clinical
parameters were evaluated by an endodontist: sex and age of the
patient, endodontic history, tooth type (ie, incisor, premolar, or
molar in upper/lower jaw), clinical signs (ie, the presence of sinus
tract and pus), type of previous endodontic treatment, and radio-
graphic appearance. Indeed, preoperative radiographs were taken,
all radiographs were digitized, and the radiographic quality of the
pre-existing obturation was estimated. Endodontic treatment of all
teeth had been completed at least 2 years before the study, and all
of the teeth exhibited apical periodontitis on radiographic examina-
tion. In each of the cases, retreatment was indicated, and previous
root canal treatment was considered a failure. In our attempt to
focus on bacterially induced apical infections and to eliminate other
causative factors, we assumed that mechanical microbial access to
the apex is a prerequisite for the contamination of periapical tissues.
In this context, teeth with obturation material that did not reach
within 4 mm of the radiographic apex or that could not be isolated
with a rubber dam were excluded from the study. No direct exposure
of the root canal lling material to the oral cavity was evident. All of
the teeth were asymptomatic. Patients who used antibiotics within the
last 30 days before commencement of the study were excluded. A
detailed description of the patients collective characteristics, the
sampling procedure used, the isolation, and the identication of
the recovered clinical isolates has been reported in earlier studies
(1113). Briey, the tooth and surrounding area were cleaned
with 30% hydrogen peroxide (H
2
O
2
) and swabbed with a 3%
sodium hypochlorite solution (NaOCl). Endodontic access was
achieved with a sterile high-speed carbide bur until the root lling
was exposed. Subsequently, the tooth and the adjacent rubber dam
were disinfected a second time using 30% H
2
O
2
and 3% NaOCl.
The cavity was swabbed with a 5% sodium thiosulfate solution to
inactivate the NaOCl. To assess the efcacy of the disinfection, a sterile
foam pellet was moistened in a sterile 0.9% NaCl solution and was
used to swab the access cavity and the tooth surface. If bacterial
growth occurred in these quality control samples, the tooth was
excluded from the study.
Coronal gutta-percha was removed with Gates Glidden drills. The
working length was established radiographically and with the aid of an
electronic apex locator (Raypex 5; VDW, Munich, Germany). The canal
was enlarged from 0.52 mm from the radiographic apex with Pro-
Taper NiTi instruments (Dentsply Maillefer, Ballaigues, Switzerland).
Teeth that could not be instrumented to this length were excluded
from the study. No solvent was used at any time. After introducing
approximately 40 mL sterile saline solution (0.9% NaCl) into the canal
with a sterile syringe, 3 sequential sterile paper points (ISO25, taper 04;
ROEKO, Langenau, Germany) were placed to the working length to soak
up the uid. Each paper point was kept inside the canal for 1 minute and
then transferred into a sterile vial containing 0.75 mL reduced transfer
uid. Finally, conventional retreatment was nished after root canal
disinfection, and the root canal was lled by using vertical compaction.
The long-term storage of all clinical isolates was accomplished at
80
C in basic growth medium containing 15% (v/v) glycerol as
described by Jones et al (20).
Testing Antibiotic Sensitivity Using the Etest
The testing of antibiotic sensitivity using the Etest method (Bio Mer-
ieux, Marcy-1Etoile, France) was conducted according to the manufac-
turers instructions and as described in an earlier report (3). The
standardized Etest was applied to reveal any antibiotic sensitivity for
the different clinical bacterial isolates recovered from the infected
root canals. Thus, the antibiotic sensitivity of aerobic and facultative
anaerobic bacterial isolates was tested against 11 antibiotics including
penicillin G, amoxicillin, clindamycin, gentamicin, vancomycin, tetracy-
cline, doxycycline, fosfomycin, rifampicin, ciprooxacin, and moxiox-
acin. The antibiotic sensitivity of anaerobic bacteria was tested using 12
antibiotics, including those previously mentioned and metronidazole.
For aerobic and facultative anaerobic bacteria, the Etest was conducted
on Mueller-Hinton agar for E. faecalis isolates and the control strain E.
faecalis (American Type Culture Collection [ATCC] 29212) or on
Mueller-Hinton agar containing 5%horse blood for Streptococcus mu-
tans, Streptococcus oralis, Streptococcus sanguinis, Streptococcus
constellatus, Lactobacillus fermentum, Lactobacillus rhamnosus,
Lactobacillus casei, Lactobacillus gasseri, Actinomyces naeslundii,
Actinomyces viscosus, Moraxella osloensis, Eikenella corrodens,
and both control strains Haemophilus inuenzae (National Collection
of Type Cultures [England] [NCTC] 8468) and Streptococcus pneumo-
niae (ATCC 49619). Colonies of each isolate were picked froman over-
night agar plate and suspended in sterile saline (0.9%) to an inoculum
turbidity of McFarland 0.5. Using sterile nontoxic spun swabs, each
isolate was streaked on agar plates. The Etest strip was then applied
to the agar surface using sterile tweezers.
The anaerobic isolates belonged to the following species: Prevo-
tella intermedia, Prevotella buccae, Fusobacterium nucleatum,
Tannerella forsythia, Porphyromonas gingivalis, Campylobacter
rectus, Campylobacter gracilis, Veillonella dispar, Dialister
pneumosintes, Parvimonas micra, Atopobiumrimae, Propionibac-
terium propionicum, Propionibacterium acidifaciens, Pseudora-
mibacter alactolyticus, Solobacterium moorei, Mogibacterium
pumilum, Mogibacterium timidum, Bidobacterium sp, and the
control strain Bacteroides fragilis (ATCC 25285). For P. gingivalis,
the Etest was conducted on yeast cysteine blood agar. For all other
anaerobic isolates, Wilkins-Chalgren agar with 5% horse blood was
used (anaerobic jar [AnaeroCultA; Merck, Darmstadt, Germany]).
Colonies of each isolate were picked from a 48-hour subculture and
suspended in sterile saline (0.9%) to an inoculum turbidity of 0.51
McFarland. Four milliliters of each suspended isolate were pipetted
on the agar plate, excessive solution was then removed, and the plates
were dried. The Etest strip was then applied to the agar surface using
sterile tweezers. Nitrocen discs (Becton Dickinson, Sparks, MD)
were used for the detection of beta-lactamases. If available, the break-
points according to the European Committee on Antimicrobial Suscep-
tibility Testing and the epidemiologic cut-off values were used to
compare the results. When European Committee on Antimicrobial
Susceptibility Testing and epidemiologic cut-off values did not exist,
minimal inhibitory concentration (MIC) values for similar strains
were derived from the literature and used to compare the antibiotic
sensitivity of the endodontic clinical isolates.
Basic ResearchBiology
224 Al-Ahmad et al. JOE Volume 40, Number 2, February 2014
Biolm Plate Assay
The biolm formation test was conducted as previously described
(21). In brief, aerobic bacterial strains were grown in tryptic soy broth
(Merck, Darmstadt, Germany) overnight at 37
C under aerobic condi-
tions with 5% CO
2
(capnophilic conditions), whereas anaerobic
bacteria were grown in gas chromatography Hewlett-Packard (GC-
HP, Wilmington, DE) broth overnight under anaerobic conditions
(anaerobic jars [GENbox anaer; bioMerieuxsa, Marcy lEtoile,
France]). The log10 of the colony-forming unit of each overnight
culture as determined on Columbia blood agar or yeast cysteine blood
agar was in the range of 10
8
colony-forming unit/mL. Polystyrene 96-
well tissue culture plates (Greiner Bio-One, Frickenhausen, Germany)
were lled with either 180 mL fresh tryptic soy broth for aerobic bacteria
or with GC-HP broth for anaerobic bacteria; afterward, 20 mL of the
overnight culture were added to each well. The plates were incubated
for 48 hours at 37
C in an aerobic atmosphere with 5% CO
2
to cultivate
biolms of aerobic bacteria or under anaerobic conditions in anaerobic
jars (AnaeroCult A) for biolm formation of the anaerobic isolates. The
culture medium was discarded, and the wells were washed 3 times with
300 mL phosphate-buffered saline to remove nonadherent bacteria.
The plates were air dried and stained with 0.1% crystal violet (Median
Diagnostics GmbH, Dunningen, Switzerland) for 10 minutes. Excess
stain was removed by washing 3 times with 200 mL distilled water.
The plates were dried for 10 minutes at 60
C. Fifty microliters of alcohol
(99.9%, absolute for analysis, Merck) were added to each well for re-
solubilization of the dye. The optical density was measured at 595 nm
with a Tecan Innite 200 plate reader (Tecan, Crailsheim, Germany).
All tests were performed in quadruplicate, whereas the experiments
were conducted twice, and the mean values were determined. Three
biolm-forming categories were established according to 2 different
cut-off values, which were xed to dene the following categories: bio-
lmnonproducer or C1, biolm moderate producer or C2, and biolm
high producer or C3. A low cut-off value was xed by adding 3 standard
deviations of the blank to the negative control. The high cut-off value was
dened as 3 times the low cut-off value.
Results
Antibiotic Sensitivity Testing
A total of 47 different bacterial isolates belonging to 32 different
species were screened for antibiotic sensitivity. Table 1 shows the values
of antibiotic sensitivity of all 4 control strains (E. faecalis, S. pneumo-
niae, H. inuenzae, and B. fragilis) tested in parallel.
The results of antibiotic sensitivity testing of aerobic, facultative
anaerobic, and anaerobic bacteria are depicted in Tables 2 and 3,
respectively. Only 2 E. faecalis isolates (nos. 3 and 6 in Table 2) showed
MICs of 64 mg/L for tetracycline and 12 mg/L for doxycycline and can
therefore be considered resistant to these antibiotics. Attention should
be paid to S. mutans (no. 8 in Table 2) exhibiting high MIC (256 mg/L)
for fosfomycin. All other Streptococcus strains as well as A. naeslundii
and Actinomyces viscosus showed high MIC values in the range of
24192 mg/L for fosfomycin. Lactobacilli presented high antibiotic
resistance against fosfomycin (MIC >1024 mg/L). With an MIC higher
than 256 mg/L, L. fermentum, L. rhamnosus, and L. casei also showed
high antibiotic resistance against vancomycin. L. gasseri showed inter-
mediary MIC values in the range of 11.5 mg/L for vancomycin but was
resistant to ciprooxacin (MIC >32 mg/L).
Taking a look at the anaerobic isolates (Table 3), P. intermedia
proved to be penicillin resistant (MIC 16 mg/L) and showed a positive
beta-lactamase result. However, P. intermedia and Prevotella buccae
revealed high MIC values for tetracycline and doxycycline. Compared
with the break points found for aerobic bacteria, these 2 species could T
A
B
L
E
1
.
A
n
t
i
b
i
o
t
i
c
S
e
n
s
i
t
i
v
i
t
y
o
f
A
l
l
T
e
s
t
e
d
C
o
n
t
r
o
l
S
t
r
a
i
n
s
S
p
e
c
i
e
s
P
e
n
i
c
i
l
l
i
n
G
C
l
i
n
d
a
m
y
c
i
n
A
m
o
x
i
c
i
l
l
i
n
G
e
n
t
a
m
i
c
i
n
F
o
s
f
o
m
y
c
i
n
V
a
n
c
o
m
y
c
i
n
C
i
p
r
o
o
x
a
c
i
n
T
e
t
r
a
c
y
c
l
i
n
e
D
o
x
y
c
y
c
l
i
n
e
R
i
f
a
m
p
i
c
i
n
M
o
x
i
o
x
a
c
i
n
M
e
t
r
o
n
i
d
a
z
o
l
E
.
f
a
e
c
a
l
i
s
A
T
C
C
2
9
2
1
2
2
.
0
0
0
6
.
0
0
0
0
.
5
0
0
8
.
0
0
0
3
2
.
0
0
0
4
.
0
0
0
0
.
3
8
0
1
6
.
0
0
0
4
.
0
0
0
0
.
5
0
0
0
.
1
2
5
N
D
S
.
p
n
e
u
m
o
n
i
a
e
A
T
C
C
4
9
6
1
9
0
.
3
8
0
.
0
9
4
0
.
0
4
7
1
2
8
0
.
5
0
.
2
5
0
.
0
9
4
0
.
0
6
4
0
.
0
3
2
0
.
0
6
4
N
D
H
.
i
n
u
e
n
z
a
e
N
C
T
C
8
4
6
8
0
.
3
8
4
0
.
1
9
3
0
.
1
2
5
1
9
2
0
.
0
0
4
0
.
0
9
4
0
.
3
8
0
.
2
5
0
.
0
0
6
N
D
B
.
f
r
a
g
i
l
i
s
A
T
C
C
2
5
2
8
5
8
0
.
7
5
6
>
1
0
2
4
>
1
0
2
4
1
6
1
0
.
0
3
2
0
.
0
2
3
0
.
0
1
6
0
.
0
9
4
0
.
1
9
N
C
T
C
,
N
a
t
i
o
n
a
l
C
o
l
l
e
c
t
i
o
n
o
f
T
y
p
e
C
u
l
t
u
r
e
s
(
E
n
g
l
a
n
d
)
;
N
D
,
n
o
t
d
e
t
e
r
m
i
n
e
d
f
o
r
f
a
c
u
l
t
a
t
i
v
e
a
n
a
e
r
o
b
i
c
b
a
c
t
e
r
i
a
l
i
s
o
l
a
t
e
s
.
Basic ResearchBiology
JOE Volume 40, Number 2, February 2014 Antibiotic Resistance and Capacity of Bacteria 225
be considered resistant to tetracycline and doxycycline. Tannerella
forsythia exhibited resistance against ciprooxacin (MIC >32 mg/
mL) and rifampicin (MIC = 32 mg/mL). Veillonella spp and Dialister
spp showed typical resistance to gentamycin and vancomycin. P. alac-
tolyticus and Mogibacterium timidum were resistant to tetracycline
(MIC 8 and 4 mg/L, respectively) and doxycycline (MIC = 6 and 3
mg/mL, respectively). Solobacterium moorei presented a noticeably
high MIC (32 mg/L) for rifampicin.
Biolm Formation
Besides testing the antibiotic sensitivity patterns for all of the
aerobic and facultative anaerobic isolates and the anaerobic endodontic
isolates, their capacity for biolm formation was also examined. The
different clinical isolates were divided into 3 categories including non-
producers of biolm or C1, moderate biolm producers or C2, and
high biolm producers or C3. The corresponding optical density
(OD) cut-off values varied between 0.086 and 0.258. OD values lower
than 0.086 represented biolm nonproducers, values ranging between
0.0860.258 were associated with moderate biolm producers, and
OD values higher than 0.258 corresponded to high biolm producers.
Figures 1 and 2 show the results concerning biolm formation by
aerobic and anaerobic bacteria, respectively.
Among the aerobic bacteria (Fig. 1), 7 isolates comprising the
species E. faecalis, S. anginosus, S. oralis, M. osloensis, and E. cor-
rodens failed to form biolms. Eight isolates belonging to the species
E. faecalis, S. mutans, S. constellatus, L. rhamnosus, L. casei, and
Lactobacillus gasseri were found to be biolm moderate producers.
Five isolates of the species E. faecalis. S. mutans, L. fermentum, A.
naeslundii, and A. viscosus were characterized as biolm high
producers.
Considering the anaerobic isolates (Fig. 2), 2 isolates comprising
the species P. buccae and Propionibacterium acidifaciens were
found to be high biolm producers. Three isolates of the species F. nu-
cleatum, V. dispar, and Propionibacterium propionicum were char-
acterized as moderate biolm producers. All other anaerobic bacterial
isolates depicted in Figure 2 failed to form biolms and were catego-
rized as biolm nonproducers. However, 1 isolate (no. 14) of the
species Parvimonas micra tended to be a moderate biolm producer.
Discussion
In various recent reports, a variety of bacteria have been isolated
and identied from secondary endodontic infections. However, consid-
ering the broad assortment of bacterial species that are causing
endodontic infections, very few reports have depicted their capacity
for biolm formation or sensitivity to different antibiotics. Both topics
are of major clinical signicance for general oral health and particularly
for the prognosis of endodontic treatment. In this study, we present for
the rst time a characterization of the capacity of 47 clinical isolates
belonging to 32 different species, which were gained entirely from
secondary/persistent endodontic infections to form biolms as well
as their antibiotic sensitivity patterns.
Antibiotic sensitivity testing not only constitutes an essential
requirement for the treatment of infectious bacteria but is also an effec-
tive method to characterize them. The Etest is a standard test widely used
in medical microbiology and shows acceptable antibiotic sensitivity
results for most medically important antimicrobial drugs as well as
different pathogens (2224). For aerobic bacteria, a total of 11
different antibiotics were tested, whereas 12 were used for the
anaerobic bacterial isolates. Furthermore, the comparison of
antimicrobial susceptibility of different strains using this test was T
A
B
L
E
2
.
A
n
t
i
b
i
o
t
i
c
S
e
n
s
i
t
i
v
i
t
y
o
f
A
l
l
T
e
s
t
e
d
A
e
r
o
b
i
c
a
n
d
F
a
c
u
l
t
a
t
i
v
e
A
n
a
e
r
o
b
i
c
E
n
d
o
d
o
n
t
i
c
B
a
c
t
e
r
i
a
l
I
s
o
l
a
t
e
s
N
o
.
S
p
e
c
i
e
s
P
e
n
i
c
i
l
l
i
n
G
C
l
i
n
d
a
m
y
c
i
n
A
m
o
x
i
c
i
l
l
i
n
G
e
n
t
a
m
i
c
i
n
F
o
s
f
o
m
y
c
i
n
V
a
n
c
o
m
y
c
i
n
C
i
p
r
o
o
x
a
c
i
n
T
e
t
r
a
c
y
c
l
i
n
e
D
o
x
y
c
y
c
l
i
n
e
R
i
f
a
m
p
i
c
i
n
M
o
x
i
o
x
a
c
i
n
1
E
.
f
a
e
c
a
l
i
s
0
.
5
0
0
6
.
0
0
0
0
.
0
9
4
3
.
0
0
0
6
.
0
0
0
1
.
5
0
0
0
.
7
5
0
0
.
1
9
0
0
.
1
2
5
1
.
0
0
0
0
.
1
2
5
2
E
.
f
a
e
c
a
l
i
s
4
.
0
0
0
1
6
.
0
0
0
1
.
0
0
0
8
.
0
0
0
4
8
.
0
0
0
2
.
0
0
0
0
.
7
5
0
0
.
3
8
5
0
.
1
9
0
1
.
5
0
0
0
.
1
9
0
3
E
.
f
a
e
c
a
l
i
s
4
.
0
0
0
6
.
0
0
0
0
.
7
5
0
6
.
0
0
0
2
4
.
0
0
0
1
.
5
0
0
0
.
5
0
0
6
4
.
0
0
0
1
2
.
0
0
0
2
.
0
0
0
0
.
1
9
0
4
E
.
f
a
e
c
a
l
i
s
3
.
0
0
0
2
.
0
0
0
0
.
7
5
0
8
.
0
0
0
4
8
.
0
0
0
2
.
0
0
0
0
.
5
0
0
1
.
0
0
0
0
.
1
9
0
1
.
5
0
0
0
.
1
2
5
5
E
.
f
a
e
c
a
l
i
s
3
.
0
0
0
3
.
0
0
0
1
.
0
0
0
4
.
0
0
0
4
8
.
0
0
0
1
.
0
0
0
0
.
5
0
0
0
.
5
0
0
0
.
7
5
0
0
.
3
8
0
0
.
1
2
5
6
E
.
f
a
e
c
a
l
i
s
3
.
0
0
0
8
.
0
0
0
0
.
7
5
0
8
.
0
0
0
2
4
.
0
0
0
3
.
0
0
0
0
.
5
0
0
6
4
.
0
0
0
1
2
.
0
0
0
1
.
0
0
0
0
.
1
2
5
7
S
.
m
u
t
a
n
s
0
.
0
0
8
0
.
0
2
3
0
.
0
2
3
2
9
4
0
.
7
5
0
.
3
8
0
.
2
5
0
.
2
5
0
.
0
4
7
0
.
0
6
4
8
S
.
m
u
t
a
n
s
0
.
0
1
2
0
.
0
2
3
0
.
0
1
6
0
.
7
5
2
5
6
0
.
5
1
0
.
5
0
.
5
0
.
0
1
2
0
.
1
2
5
9
S
.
m
u
t
a
n
s
0
.
0
4
7
0
.
0
9
4
0
.
0
6
4
4
6
4
1
0
.
7
5
0
.
2
5
0
.
2
5
0
.
0
1
2
0
.
1
9
1
0
S
.
o
r
a
l
i
s
0
.
0
3
2
0
.
0
3
2
0
.
0
3
2
4
2
4
0
.
7
5
1
0
.
3
8
0
.
1
2
5
0
.
0
6
4
0
.
0
9
4
1
1
S
.
a
n
g
i
n
o
s
u
s
0
.
0
1
6
0
.
0
3
2
0
.
0
4
7
0
.
7
5
2
4
1
0
.
1
2
5
0
.
1
9
<
0
.
0
1
6
0
.
0
6
4
0
.
0
2
3
1
2
S
.
c
o
n
s
t
e
l
l
a
t
u
s
0
.
0
1
6
<
0
.
0
1
6
0
.
0
2
3
0
.
5
6
4
1
0
.
1
2
5
0
.
0
9
4
0
.
0
6
4
0
.
0
0
3
0
.
0
2
3
1
3
L
.
f
e
r
m
e
n
t
u
m
0
.
2
5
0
.
0
1
2
0
.
1
2
5
0
.
1
2
5
>
1
0
2
4
>
2
5
6
6
1
1
.
5
0
.
0
4
7
0
.
5
1
4
L
.
r
h
a
m
n
o
s
u
s
2
0
.
1
2
5
2
2
>
1
0
2
4
>
2
5
6
0
.
7
5
0
.
2
5
0
.
3
8
0
.
3
8
0
.
1
2
5
1
5
L
.
r
h
a
m
n
o
s
u
s
0
.
5
0
.
0
4
7
0
.
5
3
>
1
0
2
4
>
2
5
6
0
.
5
0
.
1
9
0
.
2
5
0
.
0
6
4
0
.
1
2
5
1
6
L
.
c
a
s
e
i
0
.
0
9
4
0
.
0
6
4
0
.
0
6
4
0
.
5
>
1
0
2
4
>
2
5
6
0
.
2
5
0
.
3
8
0
.
3
8
0
.
0
9
4
0
.
0
2
3
1
7
L
.
g
a
s
s
e
r
i
0
.
0
9
4
2
0
.
2
5
3
>
1
0
2
4
1
>
3
2
1
1
.
5
0
.
1
9
0
.
7
5
1
8
A
.
n
a
e
s
l
u
n
d
i
i
0
.
0
1
6
0
.
1
2
5
0
.
0
3
2
0
.
3
8
6
4
0
.
5
1
.
5
0
.
0
6
4
0
.
0
6
4
0
.
0
0
2
0
.
3
8
1
9
A
.
v
i
s
c
o
s
u
s
0
.
0
0
6
0
.
0
3
2
0
.
0
1
6
0
.
1
2
5
1
9
2
0
.
1
9
1
0
.
0
3
2
0
.
0
4
7
0
.
0
0
2
0
.
1
2
5
2
0
M
.
o
s
l
o
e
n
s
i
s
0
.
5
2
0
.
0
4
7
0
.
0
4
7
2
4
3
0
.
0
3
2
0
.
1
9
0
.
0
6
4
0
.
1
2
5
0
.
0
3
2
2
1
E
.
c
o
r
r
o
d
e
n
s
2
>
2
5
6
0
.
2
5
3
>
1
0
2
4
4
8
0
.
0
3
2
0
.
5
0
.
3
8
0
.
5
0
.
0
3
2
R
e
s
i
s
t
a
n
t
b
a
c
t
e
r
i
a
a
r
e
m
a
r
k
e
d
i
n
b
o
l
d
.
Basic ResearchBiology
226 Al-Ahmad et al. JOE Volume 40, Number 2, February 2014
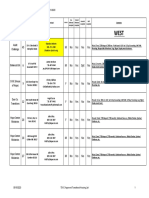
TABLE 3. Antibiotic Sensitivity of All Tested Anaerobic Endodontic Bacterial Isolates
No. Species Penicillin G Clindamycin Amoxicillin Gentamicin Fosfomycin Vancomycin Ciprooxacin Tetracycline Doxycycline Rifampicin Moxioxacin Metronidazol
1 P. intermedia 16 0.008 1 256 >1024 128 0.5 3 3 0.047 0.25 0.094
2 P. buccae 0.047 0.012 0.064 128 >1024 48 0.75 8 3 0.125 0.25 0.19
3 F. nucleatum 0.064 0.016 0.38 96 0.5 >256 1.5 0.25 0.19 0.5 0.094 0.012
4 F. nucleatum 0.016 0.016 0.032 256 0.5 48 0.5 0.064 0.047 0.125 0.032 0.008
5 F. nucleatum 0.008 0.016 0.032 384 0.5 64 0.38 0.047 0.047 0.125 0.023 0.008
6 F. nucleatum 0.002 0.016 0.016 192 0.38 24 0.5 0.016 0.012 0.047 0.047 <0.016
7 T. forsythia 0.002 0.016 <0.016 64 1 >256 >32 0.32 0.32 32 0.064 <0.016
8 P. gingivalis 0.002 0.008 0.012 48 >1024 1 0.25 0.047 0.094 0.003 0.004 <0.016
9 C. rectus 0.008 <0.016 0.064 >1024 0.125 0.125 0.047/0.25 0.023 0.023 <0.002 0.012 <0.016
10 V. dispar 0.125 0.094 0.032 32 0.064 >256 0.064 0.064 0.094 0.75 0.094 0.5
11 Dialister
pneumisintes
0.19 0.094 0.047 16 2 >256 0.047 0.064 0.094 1 0.125 2
12 P. micra 0.006 0.5 0.032 3 0.064 0.75 0.5 0.047 0.047 0.003 0.125 0.125
13 P. micros 0.003 0.5 0.016 2 0.064 0.5 0.5 0.023 0.023 0.002 0.125 0.064
14 P. micros 0.008 0.064 0.032 1 0.064 0.75 0.75 0.023 0.023 0.002 0.125 0.064
15 Atopobium
rimae
0.023 1 0.023 0.5 1 2 0.19 0.125 0.125 0.001 0.047 0.125
16 A. rimae 0.047 0.008 0.064 1 2 2 0.5 0.38 0.5 0.002 0.125 0.25
17 P. alactolyticus 0.002 <0.008 <0.016 >1024 2 0.5 0.125 0.023 0.023 0.001 0.032 <0.016
18 P. alactolyticus 0.004 0.008 0.008 >1024 6 0.75 0.25 0.032 0.047 0.002 0.094 0.016
19 P. alactolyticus 0.002 <0.016 <0.016 12 1.5 0.5 0.25 8 6 0.002 0.064 0.032
20 S. moorei 0.004 0.016 <0.016 16 <0.064 0.19 0.38 0.19 0.125 32 0.064 0.016
21 M. pumilum 0.006 <0.016 0.023 0.125 12 0.38 0.25 0.023 0.023 <0.002 0.064 0.023
22 M. timidum 0.016 0.032 0.064 48 48 0.5 0.38 4 3 0.002 0.064 0.016
23 C. gracilis 0.002 <0.016 0.016 128 0.064 0.064 0.008 0.38 0.25 <0.002 0.006 <0.016
24 Bidobacterium
sp
0.032 0.016 0.016 0.19 0.19 0.5 0.094 0.064 0.064 <0.002 0.016 <0.016
25 P. propionicum 0.016 0.094 0.032 64 >1024 0.75 0.19 0.094 0.094 <0.002 0.064 >256
26 P. acidifaciens 0.064 2 0.094 0.5 48 1.5 0.125 0.19 0.125 0.008 0.094 >256
Resistant bacteria are marked in bold.
B
a
s
i
c
R
e
s
e
a
r
c
h
B
i
o
l
o
g
y
J
O
E
V
o
l
u
m
e
4
0
,
N
u
m
b
e
r
2
,
F
e
b
r
u
a
r
y
2
0
1
4
A
n
t
i
b
i
o
t
i
c
R
e
s
i
s
t
a
n
c
e
a
n
d
C
a
p
a
c
i
t
y
o
f
B
a
c
t
e
r
i
a
2
2
7
shown to be a useful tool to identify the rst oral Vagococcus uvialis
isolate from a root-lled tooth with a periradicular lesion (3).
Among a huge number of experimental systems used to study
biolm formation, including the constant depth fermenter and
chemostat-based models, the microtiter plate assay has been shown
to be a practical test system that is less labor intensive and less chal-
lenging to perform (21, 25). In the present study, crystal violet was
used to stain the biolm, and after drying the stained biolm, the dye
was resolubilized from the biolm using alcohol. This leads to
a homogenous turbidity of the dye and reduces, as suggested by
Stepanovic et al (25), the bias correlating with the measurement of
optical density of dry stained biolm on the bottom of microtiter
plate wells. Such biases could be caused by a heterogeneous
covering grade of microtiter plate bottoms by the biolm. Additionally,
in this study, a high cut-off was used to categorize the ability to form
biolm.
To the best of our knowledge, neither the capacity of endodontic
bacteria to form biolms nor their relative levels of antibiotic resistance
have been satisfactorily studied to date. The resistance and robustness of
endodontic bacteria to withstand the antimicrobials used to treat root
canals such as sodium hypochlorite, alkali, and chlorhexidine have
been emphasized in the literature (26, 27). However, there has been
a focus on the antibiotic susceptibility of endodontic enterococci, in
particular E. faecalis. Pinheiro et al (28) tested the antibiotic sensitivity
of different E. faecalis isolates from root-lled canals with persistent
infections. Most tested antibiotics proved to be effective against
endodontic E. faecalis isolates. However, the capacity of the isolates
to form biolms was not further studied by the authors. Enterococci,
which were recovered from primary endodontic infections, presented
variable antibiotic susceptibility to rifampicin and ciprooxacin as
found by Ferrari et al (29), whereas all were susceptible to ampi-
cillin. Variable antibiotic susceptibility, including 47% reduced
Figure 1. A graphic representation of biolm formation by aerobic endodontic bacterial isolates. Means and standard deviations of 4 repeated measurements are
presented. Biolm nonproducers (category 1), moderate biolm producers (category 2), and high biolm producers (category 3) are depicted by white, gray, and
black bars, respectively.
Figure 2. A graphic representation of biolm formation by anaerobic endodontic bacterial isolates. Means and standard deviations of 4 repeated measurements
are presented. Biolm nonproducers (category 1) and moderate biolm producers (category 2) are depicted by white and gray bars, respectively.
Basic ResearchBiology
228 Al-Ahmad et al. JOE Volume 40, Number 2, February 2014
sensitivity for tetracycline, has also been shown for E. faecalis iso-
lated from periodontitis patients (30). Furthermore, E. faecalis orig-
inating from secondary endodontic infections in Finland and
Lithuania exhibited similar susceptibility patterns, with levels of resis-
tance that were considered typical for the species (31). The only
exception was the high prevalence of rifampicin resistance, an
outcome that contradicts the results of the present study, which dis-
closed 5 rifampicin sensitive strains. It is remarkable that the same
authors described an unusual susceptibility of 4 E. faecalis strains
to cefotaxim and only 1 strain to clindamycin. Additionally, it has
been shown in a root canal model that the presence of the Tn916-
like conjugative transposon containing the tetracycline resistance
gene tet(M) allowed an E. faecalis strain to survive irrigation for 5
minutes using a solution containing a high concentration of tetracy-
cline (32). In our report, the resistance of 2 E. faecalis isolates to
tetracycline is in agreement with the results mentioned earlier.
With the aid of the Etest upon examining 6 different antibiotics,
Gomes et al (33) discovered an increase in anaerobic resistance to
penicillin G and clindamycin. This nding is consistent with the high
resistance of Prevotella intermedia against penicillin G, which was
seen in our report. Jacinto et al (34) revealed that different endodontic
P. gingivalis isolates recovered from infected root canals with periap-
ical abscesses were susceptible to 7 of 9 antibiotics. Endodontic isolates
of F. nucleatum from primary infections were sensitive to amoxicillin,
amoxicillin with clavulanate, benzylpenicillin (penicillin G), cephaclor,
clindamycin, and metronidazole (35). Jungermann et al (36) were not
only able to detect different antibiotic resistance genes in primary and
persistent infections, but they also showed that the antibiotic resistance
gene against tetracycline was not eliminated after endodontic treatment.
In agreement with the results presented here, oral Actinomyces species
including A. naeslundii and A. viscosus proved to be sensitive to amox-
icillin, clindamycin, doxycycline, and moxioxacin (37). Persistent
endodontic Enterococcus isolates were revealed to be resistant to ceph-
alosporins, gentamycin, and polymyxin, with these being related to
intrinsic resistance (38). Furthermore, E. faecalis from persistent
endodontic infections showed erythromycin and azithromycin resis-
tance (20% and 60%, respectively) (39). In a recent report by Skucaite
et al (40), 40% of the endodontic isolates from primary and secondary
infections were resistant to tetracycline, whereas in our study 2 of 6
strains were not susceptible. In an earlier report from Vigil et al
(41), no antibiotic resistance was detected among bacterial isolates
fromrefractory endodontic infections, suggesting a continuous increase
in antibiotic resistance over the last 16 years.
Interestingly, the present study revealed that most isolates with
resistance or markedly high MIC values were also either moderate bio-
lm producers (E. faecalis, Lactobacilli, and Prevotella buccae) or
high biom producers (Actinomyces spp, Streptococcus mutans,
and Pseudoramibacter alactolyticus). This kind of correlation
between capacity for biolm formation and high or low sensitivity to
some antibiotics has not been reported to date. This could possibly
reect the high rate of horizontal gene exchange, which is taking place
in biolms (19). The evidence for this assumption has been found in the
literature where transfer of the conjugative plasmid pAM81 carrying
erythromycin resistance between 2 endodontic infection-associated
species, Streptococcus gordonii and E. faecalis, was shown in an
ex vivo tooth model (42).
Reports about biolm formation of endodontic isolates are scarce
although the existence of biolm is one of the main reasons for
endodontic treatment failure (15, 16). Because E. faecalis is one of
the most frequently isolated endodontic agents in persistent
infections, this is one of the few microorganisms that have been
widely tested for their capacity to form biolms (17, 19). Facts
supporting the hypothesis that E. faecalis can persist in root canals
by forming biolms were delivered by Distel et al (43) who exhibited
typical mushroom-shape E. faecalis biolm in in vitroinfected root
canals. Our group has also shown that endodontic isolates of E. faecalis
can integrate into a biolm formed by salivary bacteria in vitro (18).
Takemura et al (44) focused on the in vitro biolm formation of
some root canal isolates on gutta-percha points. In an earlier report
from our group, the high afnity of different oral bacteria to adhere
to different root canal lling materials and sealers including gutta-
percha was also highlighted (45).
In conclusion, endodontic infections could be a reservoir for anti-
biotic resistance. Although rinses containing antibiotics such as MTAD
(a mixture of a tetracycline isomer, an acid, and a detergent) were
shown to be effective in eradicating endodontic bacteria (46), the devel-
opment of antibiotic resistance should be considered when there is
a proposal to use them to eradicate endodontic infections. Further-
more, endodontic treatment should consider the characteristics of
adhesion and biolm formation by a variety of bacteria. Taking into
consideration that root canal bacteria potentially develop antibiotic
resistance, their ability to form biolms would facilitate the spread of
antibiotic resistance by horizontal gene transfer.
Acknowledgments
The authors thank Dr Markus Altenburger and Dr Christian
Tennert for the provision of patient samples.
Supported by the German Research Foundation (DFG, AL 1179/
1-1).
The authors deny any conicts of interest related to this study.
References
1. Haapasalo M, Udns T, Endal U. Persistent, recurrent, and acquired infection of the
root canal system post-treatment. Endod Topics 2003;6:2956.
2. Nair PN, Sjogren U, Krey G, et al. Intraradicular bacteria and fungi in root-lled,
asymptomatic human teeth with therapy-resistant periapical lesions; a long-term
light and electron microscopic follow-up study. J Endod 1990;16:5808.
3. Al-Ahmad A, Pelz K, Schirrmeister JF, et al. Characterization of rst oral Vagococcus
isolate froma root-lled tooth with periradicular lesions. Curr Microbiol 2008;57:2358.
4. Cheung GS, Ho MW. Microbial ora of root canal-treated teeth associated with asymp-
tomatic periapical radiolucent lesions. Oral Microbiol Immunol 2001;16:3327.
5. Molander A, Reit C, Dahlen G, et al. Microbiological status of root-lled teeth with
apical periodontitis. Int Endod J 1998;31:17.
6. Peciuliene V, Reynaud AH, Balciuniene I, et al. Isolation of yeasts and enteric
bacteria in root-lled teeth with chronic apical periodontitis. Int Endod J 2001;
34:42934.
7. R^oc as IN, Jung IY, Lee CY, et al. Polymerase chain reaction identication of micro-
organisms in previously root-lled teeth in a South Korean population. J Endod
2004;30:5048.
8. Rolph HJ, Lennon A, Riggio MP, et al. Molecular identication of microorganisms
from endodontic infections. J Clin Microbiol 2001;39:32829.
9. Siqueira JF Jr, R^oc as IN. Polymerase chain reaction-based analysis of microorgan-
isms associated with failed endodontic treatment. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod 2004;97:8594.
10. Sundqvist G, Figdor D, Persson S, et al. Microbiologic analysis of teeth with failed
endodontic treatment and the outcome of conservative re-treatment. Oral Surg
Oral Med Oral Pathol Oral Radiol Endod 1998;85:8693.
11. Schirrmeister JF, Liebenow AL, Braun G, et al. Detection and eradication of micro-
organisms in root-lled teeth associated with periradicular lesions: an in vivo study.
J Endod 2007;33:53640.
12. Schirrmeister JF, Liebenow AL, Pelz K, et al. New bacterial compositions in root-
lled teeth with periradicular lesions. J Endod 2009;35:16974.
13. Anderson AC, Hellwig E, Vespermann R, et al. Comprehensive analysis of secondary
dental root canal infections: a combination of culture and culture-independent
approaches reveals new insights. PLoS One 2012;7:e49576.
14. Preethee T, Kandaswamy D, Hannah R. Molecular identication of an Enterococcus
faecalis endocarditis antigen efaA in root canals of therapy resistant endodontic
infections. J Conserv Dent 2012;15:31922.
15. Ricucci D, Siqueira JF Jr. Biolms and apical periodontitis: study of prevalence and
association with clinical and histopathologic ndings. J Endod 2010;36:127788.
Basic ResearchBiology
JOE Volume 40, Number 2, February 2014 Antibiotic Resistance and Capacity of Bacteria 229
16. Chavez de Paz LE. Redening the persistent infection in root canals: possible role of
biolm communities. J Endod 2007;33:65262.
17. Duggan JM, Sedgley CM. Biolm formation of oral and endodontic Enterococcus
faecalis. J Endod 2007;33:8158.
18. Al-Ahmad A, Muller N, Wiedmann-Al-Ahmad M, et al. Endodontic and salivary
isolates of Enterococcus faecalis integrate into biolm from human salivary
bacteria cultivated in vitro. J Endod 2009;35:98691.
19. Madsen JS, Burmlle M, Hansen LH, et al. The interconnection between biolm
formation and horizontal gene transfer. FEMS Immunol Med Microbiol 2012;65:
18395.
20. Jones D, Pell PA, Sneath PHA. Maintenance of bacteria on glass beads at -60
C to
-76
C. In: Kirsop BE, Doyle AE, eds. Maintenance of Microorganisms and
Cultured Cells: A Manual of Laboratory Methods, 2nd ed. London: Academic
Press; 1991:4550.
21. Al-Ahmad A, Wiedmann-Al-Ahmad M, Auschill TM, et al. Effects of commonly used
food preservatives on biolm formation of Streptococcus mutans in vitro. Arch
Oral Biol 2008;53:76572.
22. Tenover FC, Baker CN, Swenson JM. Evaluation of commercial methods for deter-
mining antimicrobial susceptibility of Streptococcus pneumoniae. J Clin
Microbiol 2008;34:104.
23. Amsler K, Santoro C, Foleno B, et al. Comparison of broth microdilution, agar dilu-
tion, and Etest for susceptibility testing of doripenem against gram-negative and
gram-positive pathogens. J Clin Microbiol 2010;48:33537.
24. Lonsway DR, Urich SK, Heine HS, et al. Comparison of Etest method with reference
broth microdilution method for antimicrobial susceptibility testing of Yersinia pes-
tis. J Clin Microbiol 2011;49:195660.
25. Stepanovic S, Vukovic D, Dakic I, et al. A modied microtiter-plate test for quanti-
cation of staphylococcal biolm formation. J Microbiol Methods 2000;40:1759.
26. Chavez de Paz LE, Bergenholtz G, Svensater G. The effects of antimicrobials on
endodontic biolm bacteria. J Endod 2010;36:707.
27. Kayaoglu G, Erten H, rstavik D. Possible role of the adhesin ace and collagen
adherence in conveying resistance to disinfectants on Enterococcus faecalis.
Oral Microbiol Immunol 2008;23:44954.
28. Pinheiro ET, Gomes BP, Drucker DB, et al. Antimicrobial susceptibility of Entero-
coccus faecalis isolated from canals of root lled teeth with periapical lesions. Int
Endod J 2004;37:75663.
29. Ferrari PH, Cai S, Bombana AC. Effect of endodontic procedures on enterococci,
enteric bacteria and yeasts in primary endodontic infections. Int Endod J 2005;
38:37280.
30. Rams TE, Feik D, Mortensen JE, et al. Antibiotic susceptibility of periodontal Entero-
coccus faecalis. J Periodontol 2013;84:102633.
31. Reynaud af Geijersstam AH, Ellington MJ, Warner M, et al. Antimicrobial suscep-
tibility and molecular analysis of Enterococcus faecalis originating from
endodontic infections in Finland and Lithuania. Oral Microbiol Immunol
2006;21:1648.
32. Rossi-Fedele G, Roberts AP. A preliminary study investigating the survival of tetracy-
cline resistant Enterococcus faecalis after root canal irrigation with high concen-
trations of tetracycline. Int Endod J 2007;40:7727.
33. Gomes BP, Jacinto RC, Montagner F, et al. Analysis of the antimicrobial susceptibility
of anaerobic bacteria isolated from endodontic infections in Brazil during a period
of nine years. J Endod 2011;37:105862.
34. Jacinto RC, Gomes BPFA, Shah HN, et al. Incidence and antimicrobial susceptibility
of Porphyromonas gingivalis isolated from mixed endodontic infections. Int Endod J
2006;39:6270.
35. Jacinto RC, Montagner F, Signoretti FG, et al. Frequency, microbial interactions,
and antimicrobial susceptibility of Fusobacterium nucleatum and Fusobacterium
necrophorum isolated from primary endodontic infections. J Endod 2008;34:
14516.
36. Jungermann GB, Burns K, Nandakumar R, et al. Antibiotic resistance in primary and
persistent endodontic infections. J Endod 2011;37:133744.
37. LeCorn DW, Vertucci FJ, Rojas MF, et al. In vitro activity of amoxicillin, clindamycin,
doxycycline, metronidazole, and moxioxacin against oral Actinomyces. J Endod
2007;33:55760.
38. Noda M, Komatsu H, Inoue S, et al. Antibiotic susceptibility of bacteria detected
from the root canal exudate of persistent apical periodontitis. J Endod 2000;26:
2214.
39. Pinheiro ET, Gomes BP, Ferraz CC, et al. Evaluation of root canal microorganisms
isolated from teeth with endodontic failure and their antimicrobial susceptibility.
Oral Microbiol Immunol 2003;18:1003.
40. Skucaite N, Peciuliene V, Vitkauskiene A, et al. Susceptibility of endodontic patho-
gens to antibiotics in patients with symptomatic apical periodontitis. J Endod 2010;
36:16116.
41. Vigil GV, Wayman BE, Dazey SE, et al. Identication and antibiotic sensitivity of
bacteria isolated from periapical lesions. J Endod 1997;23:1104.
42. Sedgley CM, Lee EH, Martin MJ, et al. Antibiotic resistance gene transfer between
Streptococcus gordonii and Enterococcus faecalis in root canals of teeth
ex vivo. J Endod 2008;34:5704.
43. Distel JW, Hatton JF, Gillespie MJ. Biolm formation in medicated root canals.
J Endod 2002;28:68993.
44. Takemura N, Noiri Y, Ehara A, et al. Single species biolm-forming ability of root
canal isolates on gutta-percha points. Eur J Oral Sci 2004;112:5239.
45. Senges C, Wrbas KT, Altenburger M, et al. Bacterial and Candida albicans
adhesion on different root canal lling materials and sealers. J Endod 2011;37:
124752.
46. Torabinejad M, Shabahang S, Aprecio RM, et al. The antimicrobial effect of MTAD:
an in vitro investigation. J Endod 2003;29:4003.
Basic ResearchBiology
230 Al-Ahmad et al. JOE Volume 40, Number 2, February 2014
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5835)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (350)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- ptw1 Assesment QuestionDocument6 pagesptw1 Assesment Questionharis100% (2)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Patterns of Language Comprehension Deficit in Abused and Neglected Children - Fox Et Al. 53 (3) : 239 - Journal of Speech and Hearing DisordersDocument3 pagesPatterns of Language Comprehension Deficit in Abused and Neglected Children - Fox Et Al. 53 (3) : 239 - Journal of Speech and Hearing DisordersGabriel RendonNo ratings yet
- HYEN-RFQ-ME-004 - RFQ For FET - Rev.C - 210218Document22 pagesHYEN-RFQ-ME-004 - RFQ For FET - Rev.C - 210218MouiciNo ratings yet
- n119 So Kunjungan BP SPV Maulana Mulya Ke 3 22-10-2022 (Template Form So)Document260 pagesn119 So Kunjungan BP SPV Maulana Mulya Ke 3 22-10-2022 (Template Form So)niceso 21No ratings yet
- Mouth Preparation For RPDDocument45 pagesMouth Preparation For RPDArbaz SajjadNo ratings yet
- National Professional Practice Examination (NPPE) Candidate GuideDocument13 pagesNational Professional Practice Examination (NPPE) Candidate Guidedemet cioncaNo ratings yet
- Kuliah Radiologi Emergensi - Maret 2020 - PlainDocument67 pagesKuliah Radiologi Emergensi - Maret 2020 - PlainArief VerditoNo ratings yet
- Respiratory AssessmentDocument27 pagesRespiratory AssessmentAinaB ManaloNo ratings yet
- Zeniton 70 IFUDocument292 pagesZeniton 70 IFUyoelalperinbackupNo ratings yet
- PUSH UP PFT JOSEPH L. CELICIOUS JR. 1Document12 pagesPUSH UP PFT JOSEPH L. CELICIOUS JR. 1Arnelson DerechoNo ratings yet
- Ota Go Correctional FacilityDocument14 pagesOta Go Correctional FacilityKier Marcial V. Collao IVNo ratings yet
- Bionic Eye - An Artificial Vision & Comparative Study Based On Different Implant TechniquesDocument9 pagesBionic Eye - An Artificial Vision & Comparative Study Based On Different Implant TechniquesGabi BermudezNo ratings yet
- Transitional Housing ListDocument27 pagesTransitional Housing ListA IDOHERBALIFE IDOHERBABBASLIFENo ratings yet
- Ethics Review E1 FormDocument3 pagesEthics Review E1 FormShivali RS SrivastavaNo ratings yet
- Chapter 02 - Diversity On OrganizationsDocument29 pagesChapter 02 - Diversity On OrganizationsAsra AliNo ratings yet
- Aip Budget 2024 Needed DataDocument22 pagesAip Budget 2024 Needed Datamoox TVNo ratings yet
- Block 1Document47 pagesBlock 1Yashwant ChauhanNo ratings yet
- Rockwell Maintenance Manual 4B Auto Slack Adjuster 1998Document26 pagesRockwell Maintenance Manual 4B Auto Slack Adjuster 1998ScottNo ratings yet
- 20220206542333tangazo La Kazi La Mkataba Rea 1Document3 pages20220206542333tangazo La Kazi La Mkataba Rea 1SABATO HARUNI (neGro)No ratings yet
- AkQuire HDCDocument1 pageAkQuire HDCBrgy Sta. CruzNo ratings yet
- Tugas Matriks JurnalDocument24 pagesTugas Matriks JurnalEti NurmahdaniNo ratings yet
- Pragati Life Insurance Limited Network Hospitals & Diagnostic Centres For Discount CardDocument9 pagesPragati Life Insurance Limited Network Hospitals & Diagnostic Centres For Discount CardImran SikderNo ratings yet
- Strategic Management (Assignment) HMSM 4032Document6 pagesStrategic Management (Assignment) HMSM 4032MOZAIDNo ratings yet
- RU - Trauma and Emergency CareDocument32 pagesRU - Trauma and Emergency CareryanNo ratings yet
- Girdle Stone Procedure in Bilateral Rheumatoid Hip: A Case ReportDocument2 pagesGirdle Stone Procedure in Bilateral Rheumatoid Hip: A Case Reportumer ilyasNo ratings yet
- Proofex Torchseal 3PDocument4 pagesProofex Torchseal 3PFZweiNo ratings yet
- Getting Out of My BoxDocument4 pagesGetting Out of My Boxapi-532881677No ratings yet
- Learning and Teaching in The Clinical EnvironmentDocument4 pagesLearning and Teaching in The Clinical EnvironmentDaniel Alejandro Lozano MorenoNo ratings yet
- Fowler, Gasiorek, & Giles (2015) - Don't Talk Yourself Into An Early Grave! The Role of Communication in Aging WellDocument2 pagesFowler, Gasiorek, & Giles (2015) - Don't Talk Yourself Into An Early Grave! The Role of Communication in Aging WellCraig FowlerNo ratings yet
- Nasal TumorDocument20 pagesNasal TumorMahmoud ElsherbenyNo ratings yet