Professional Documents
Culture Documents
1144 FTP PDF
1144 FTP PDF
Uploaded by
Regina GamezOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1144 FTP PDF
1144 FTP PDF
Uploaded by
Regina GamezCopyright:
Available Formats
DIABETES/METABOLISM RESEARCH AND REVIEWS RESEARCH ARTI CLE
Diabetes Metab Res Rev 2010; 26: 668676.
Published online in Wiley Online Library (wileyonlinelibrary.com) DOI: 10.1002/dmrr.1144
Association of cognitive performance with the
metabolic syndrome and with glycaemia in
middle-aged and older European men: the
European Male Ageing Study
Jos Tournoy
1
* David M. Lee
2
Neil Pendleton
3
Terence W. ONeill
2
Daryl B. OConnor
4
Gyorgy
Bartfai
5
Felipe F. Casanueva
6,7
Joseph D. Finn
8
Gianni Forti
9
Aleksander Giwercman
10
Thang S.
Han
11
Ilpo T. Huhtaniemi
12
Krzysztof Kula
13
Michael E. J. Lean
14
Carly M. Moseley
8
Margus
Punab
15
Alan J. Silman
2
Dirk Vanderschueren
16
Frederick C. W. Wu
8
Steven Boonen
1
and the
EMAS study group
1
Department of Experimental Medicine, Division of
Gerontology and Geriatrics, Katholieke Universiteit
Leuven, Leuven, Belgium;
2
School of Translational
Medicine, Arthritis Research UK Epidemiology Unit,
University of Manchester, Manchester, UK;
3
School
of Community Based Medicine, Neurodegeneration
and Mental Health Research Group, University of
Manchester, Salford Royal NHS Trust, Salford, UK;
4
Institute of Psychological Sciences, University of
Leeds, Leeds, UK;
5
Department of Obstetrics,
Gynaecology and Andrology, Albert Szent-Gyorgy
Medical University, Szeged, Hungary;
6
Department
of Medicine, Santiago de Compostela University,
Complejo Hospitalario Universitario de Santiago
(CHUS), Spain;
7
CIBER de Fisiopatologa Obesidad
y Nutricion (CB06/03), Instituto Salud Carlos III;
Santiago de Compostela, Spain;
8
Department of
Endocrinology, Andrology Research Unit,
Manchester Royal Inrmary, University of
Manchester, Manchester, UK;
9
Andrology Unit,
Department of Clinical Physiopathology, University
of Florence, Florence, Italy;
10
Reproductive Medicine
Centre, Malmo University Hospital, University of
Lund, Malmo, Sweden;
11
Department of
Endocrinology, Royal Free and University College
Hospital Medical School, University College London,
London, UK;
12
Department of Reproductive Biology,
Imperial College London, Hammersmith Campus,
London, UK;
13
Department of Andrology and
Reproductive Endocrinology, Medical University of
Lodz, Lodz, Poland;
14
Department of Human
Nutrition, University of Glasgow, Glasgow, UK;
15
Andrology Unit, United Laboratories of Tartu
University Clinics, Tartu, Estonia;
16
Department of
Andrology and Endocrinology, Katholieke
Universiteit Leuven, Leuven, Belgium
*Correspondence to: Jos Tournoy, Department of
Experimental Medicine, Division of Gerontology
and Geriatrics, Katholieke Universiteit Leuven,
Herestraat 49, 3000 Leuven, Belgium.
E-mail: jos.tournoy@uzleuven.be
The EMAS Study Group: Florence (Gianni Forti,
Luisa Petrone, Giovanni Corona); Leuven (Dirk
Vanderschueren, Steven Boonen, Herman
Borghs); Lodz (Krzysztof Kula, Jolanta
Slowikowska-Hilczer, Renata Walczak-
Jedrzejowska); London (Ilpo Huhtaniemi); Malm o
(Aleksander Giwercman); Manchester (Frederick
Wu, Alan Silman, Terence ONeill, Joseph Finn,
Philip Steer, Abdelouahid Tajar, David Lee,
Stephen Pye); Santiago (Felipe Casanueva, Marta
Ocampo, Mary Lage); Szeged (Gyorgy Bartfai,
Imre F oldesi, Imre Fejes); Tartu (Margus Punab,
Paul Korrovitz); Turku (Min Jiang).
Received: 19 May 2010
Revised: 5 October 2010
Accepted: 6 October 2010
Abstract
Background and aims Metabolic syndrome has been reported to have
adverse effects on cognition although the results are conicting. We
investigated the association between metabolic syndrome and cognitive
function in a population sample of middle-aged and older European men
and whether any observed association could be explained by lifestyle or other
confounding factors.
Methods A total of 3369 men in the 40- to 79-year age group were recruited
from population registers in eight centres for participation in the European
Male Ageing Study. The subjects completed a questionnaire instrument and
several cognitive function tests including the ReyOsterrieth Complex Figure
test, the Camden Topographical Recognition Memory test and the Digit
Symbol Substitution Test. Metabolic syndrome data were assessed at an
invited visit and metabolic syndrome was dened by the National Cholesterol
Education Programs Adult Treatment Panel-III criteria.
Associations between cognitive performance and metabolic syndrome were
explored using linear regression.
Results Complete cognitive and metabolic syndrome data from 3152 sub-
jects were included in the analysis, of whom 1007 (32%) fullled criteria for
metabolic syndrome. After adjustment for putative health and lifestyle con-
founders, no signicant associations were found between any of the cognitive
function scores and metabolic syndrome or between cognitive performance
and high-sensitivity C-reactive protein. Analysis of the individual metabolic
syndrome factors, however, revealed an inverse association between the level
of glucose and cognitive performance.
Conclusions Metabolic syndrome was not associated with cognitive impair-
ment in this population. Of the individual components of the syndrome,
diabetes was associated with poorer performances in memory, executive func-
tions and processing speed, associations that warrant further investigation.
Copyright 2010 John Wiley & Sons, Ltd.
Keywords metabolic syndrome X; cognition; diabetes mellitus; men
Introduction
Ageing is associated with a loss of cognitive performance and increased
risk of dementia. The aetiology is likely to be multi-factorial and pre-
cise mechanisms are unknown, although cardiovascular risk factors have
been implicated. Metabolic syndrome refers to a cluster of cardiovascular
risk factors which include abdominal obesity, hypertriglyceridaemia, low
high-density lipoprotein-cholesterol (HDL-c) levels, high blood pressure and
elevated blood glucose levels [1]. The presence of the syndrome has been
linked with the occurrence of cardiovascular events [2] and also other
Copyright 2010 John Wiley & Sons, Ltd.
Association of Cognitive Performance With the Metabolic Syndrome 669
adverse effects including fatty liver disease and polycystic
ovarian syndrome. Cognitive impairment has been
reported to be associated with the syndrome; however,
data is limited and sometimes conicting. Thus, some
studies have demonstrated an inverse association between
the metabolic syndrome and cognition [3] or cognitive
decline [48], while other studies have not been able
to conrm these ndings [9,10]. Both age [10,11] and
gender [5,11] may also play a role; it has been suggested
that older women with metabolic syndrome may be less
vulnerable to develop cognitive decline than younger
women [12] and men [5,11]. Higher high-sensitivity C-
reactive protein (hs-CRP) levels have been associated
with metabolic syndrome and also an increased risk of
cardiovascular events [13]. In one study, inammation
was found to be negatively associated with cognition in
the presence of metabolic syndrome [7]. Further data are,
however, needed to better dene the relationship between
the metabolic syndrome, cognition and the inammatory
response. Our objectives in this analysis were to
investigate the association between cognitive function
and the metabolic syndrome in a representative sample of
middle-aged and older European men [14] and explore
whether any of the associations were inuenced by
putative confounding factors. A secondary objective was
to study the inuence of the individual components of the
metabolic syndrome on cognitive performance. Thirdly,
we explored if there was any association between hs-CRP
and cognition and the inuence of the presence or absence
of metabolic syndrome on any putative association.
Methods
Study participants
Our analyses are based on the cross-sectional base-
line data from the European Male Ageing Study,
a non-interventional cohort study of male ageing in
Europe. Details regarding recruitment, response rates
and assessments have been described [14]. In brief,
8416 community-dwelling men in the 40- to 79-year
age group were invited to attend the study from munic-
ipal or population registers in eight centres: Florence,
Italy; Leuven, Belgium; Lodz, Poland; Malm o, Swe-
den; Manchester, UK; Santiago de Compostela, Spain;
Szeged, Hungary and Tartu, Estonia. Of these, 3369
agreed to participate in the full study. Stratied ran-
dom sampling was used for the baseline survey to
obtain an equal distribution in four age bands (4049,
5059, 6069 and 7079 years). The letter of invita-
tion sent to the subjects had questions about smoking,
frequency of alcohol consumption, comorbidity includ-
ing diabetes and hypertension, and age leaving educa-
tion. Those who agreed to participate were seen at an
assessment facility where they completed an interviewer-
assisted questionnaire and a number of cognitive func-
tion tests. A fasting blood sample was also taken. The
study was funded by the European Union and ethical
approval was obtained in agreement with local institu-
tional requirements.
Interviewer-assisted questionnaire
The interviewer-assisted questionnaire included questions
about physical activity and depressive symptoms. Physical
activity was assessed using the Physical Activity Scale
for the Elderly [15] and depressive symptoms using the
Beck Depression Inventory [16]. Current prescription and
non-prescription medication use was also documented.
Assessment of cardiovascular risk
factors
Seated pulse and blood pressure [Omron 500I, Omron
Healthcare (UK) Ltd, Milton Keynes, UK] was recorded
after a 5-min rest period. Waist circumference was
measured using anthropometric tape, and the median
of three measurements was used as the recorded
value. Fasting blood samples were taken by morning
phlebotomy before 10 AM either when subjects attended
the clinic or alternatively at their homes if they had
difculty attending. Glucose and lipid measurements were
undertaken in each centre and assessed at the local health
care facility.
The presence of the metabolic syndrome was dened
according to the National Cholesterol Education Pro-
gram Adult Treatment Panel-III denition [17]. Three
or more of the following ve criteria had to be
met: waist circumference 102 cm, fasting triglyceride
1.7 mmol/L, fasting HDL-c <1.03 mmol/L, blood pres-
sure 130/85 mmHg or currently using anti-hypertensive
medication, fasting glucose 5.6 mmol/L or using anti-
diabetic medication.
Assessment of cognitive function
Several cognitive domains were assessed in this study:
visuo-constructional ability, visual memory, executive
function, attention and processing speed. The test battery
included the ReyOsterrieth Complex Figure (ROCF) to
test visuo-constructional ability and memory, the Camden
Topographical Recognition Memory (CTRM) to test
topographical memory and the Digit Symbol Substitution
Test (DSST) to assess attention and processing speed. This
battery was specically selected to minimize the inuence
of language and culture, facilitating standardization
across different centres. Further details of the tests are
outlined below.
The copying and delayed reproduction of the ROCF is
a measure of visual perception, memory and executive
function [18]. Subjects were instructed to complete the
copy and, without being pre-informed, asked to reproduce
the gure after 30 min. The applied ROCF scoring criteria
were based on the original test procedure, which denes
18 units of the drawing and assigns point values of 02
Copyright 2010 John Wiley & Sons, Ltd. Diabetes Metab Res Rev 2010; 26: 668676.
DOI: 10.1002/dmrr
670 J. Tournoy et al.
to each unit dependent upon the degree to which the
units are correctly drawn and placed. Both ROCF tests
had a maximum score of 36. The CTRM test measures
the recognition component of visual memory retrieval,
tapping into the cortical component of visual memory
[19]. The CTRM test involves the presentation of 30
coloured photographs of outdoor topographical scenes,
each shown for 3 s, followed by a three-way forced
recognition component. The CTRM had a maximum score
of 30. The DSST is a subtest adopted from the Wechsler
Adult Intelligence Scales and provides a reliable measure
of psychomotor speed and visual scanning [20]. Within
a 1-min time frame, participants were asked to make as
many correct symbol-for-digit substitutions as possible.
Higher scores for each test indicate better cognitive
performance.
Measurement of hs-CRP
hs-CRP levels were determined using a solid-phase,
chemiluminescent immunometric assay (Immulite 2000
hs-CRP assay; Diagnostics Products Corporation, Siemens,
Deereld, IL, USA) with a sensitivity of 0.01 mg/dL. The
mean replicate coefcient of variation was less than 3%.
All measurements were made at a central laboratory
facility in Santiago.
Analysis
Cognitive scores, individual components of the metabolic
syndrome, age, age leaving education, the Physical Activ-
ity Scale for the Elderly and Beck Depression Inventory
score and hs-CRP were treated as continuous variables,
while the metabolic syndrome (absent versus present),
smoking (non-smoking versus currently smoking) and
alcohol consumption (<1 day/week versus 1 day/week)
as categorical variables.
Linear regression was used to determine the association
of the cognitive test scores (dependent variables)
with the metabolic syndrome and its components
(independent variables). Adjustments were made for age,
age leaving education, smoking, alcohol consumption,
physical activity, depression and hs-CRP. To allow
for the likelihood that observations are independent
across centres, but not necessarily within centres, robust
standard errors were requested using Statas cluster
subcommand with centre as the clustering variable.
Results are expressed as beta coefcients () and 95%
condence intervals. Statistical analyses were undertaken
using Intercooled STATA version 9.2 (StataCorp, College
Station, TX, USA).
Results
Subject characteristics
In total, 3369 men participated in the full study,
corresponding to a response rate of 41%. A total of
217 subjects with incomplete cognitive and/or metabolic
syndrome data were excluded and 3152 subjects
were included in the analysis. Of the latter, baseline
characteristics are shown in Table 1. Metabolic syndrome
was present in 1007 (32%) of the subjects. Among those
with metabolic syndrome, 981 (97%) had high blood
pressure, 775 (77%) had abdominal obesity, 725 (72%)
had high fasting glucose or were taking anti-diabetic
medication, 663 (66%) had hypertriglyceridaemia and
303 (30%) had low HDL-c. Subjects with metabolic
syndrome were slightly older (61.0 10.4 versus 59.3
11.2), had higher body mass indexes (30.7 4.1
versus 26.3 3.3) and had higher scores for depressive
symptoms as measured by the Beck Depression Inventory
(7.8 6.9 versus 6.4 6.1). Furthermore, participants
fullling the metabolic syndrome criteria were less
physically active as measured by the Physical Activity
Scale for the Elderly (188 96 versus 200 89) and had
higher hs-CRP levels (5.5 8.3 versus 3.9 7.9). In the
group without metabolic syndrome, signicantly fewer
subjects suffered a heart condition (15 versus 20%). There
were no signicant differences regarding age leaving
education, alcohol consumption and current smoking.
Cognitive performance and metabolic
syndrome
Men without the metabolic syndrome performed signi-
cantly better on all cognitive tests compared with men
having the syndrome (Table 1). After adjustment for
age, the metabolic syndrome was associated with lower
scores on the ROCF copy ( = 0.608, p < 0.001) and
DSST ( = 0.813, p < 0.01). No signicant differences
were observed for ROCF recall ( = 0.381, p > 0.05)
and CTRM ( = 0.228, p > 0.05) scores (Table 2). The
association with ROCF copy and DSST disappeared after
adjustment for various lifestyle factors and depressive
symptoms (all p > 0.05).
Table 3 summarizes the results from the regression
models of the ve individual components accounting
for the metabolic syndrome and cognitive test scores.
After adjusting for age, education, smoking, alcohol
consumption, physical activity, depressive symptoms and
centre, glucose levels were negatively associated with
all cognitive test scores: ROCF copy ( = 0.261, p <
0.05), ROCF recall ( = 0.175, p < 0.05), CTRM ( =
0.254, p < 0.05) and DSST ( = 0.552, p < 0.01).
Diastolic blood pressure was positively associated with
ROCF recall score ( = 0.025, p < 0.05) and HDL-c with
ROCF copy ( = 0.581, p < 0.05) and recall ( = 0.922,
p < 0.05) scores. After additional analysis adjusting for
hs-CRP, the associations between glucose levels and
ROCF recall ( = 0.156, p > 0.05) and CTRM scores
( = 0.246, p > 0.05) and between diastolic blood
pressure and ROCF recall ( = 0.026, p > 0.05) were
no longer signicant (Table 4). Additional analyses of the
number of added individual components of the metabolic
syndrome and cognitive scores in subjects with metabolic
Copyright 2010 John Wiley & Sons, Ltd. Diabetes Metab Res Rev 2010; 26: 668676.
DOI: 10.1002/dmrr
Association of Cognitive Performance With the Metabolic Syndrome 671
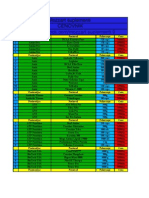
Table 1. Baseline characteristics
Metabolic syndrome
Absent (n = 2145) Present (n = 1007)
Mean (SD) p-Value
a
Age (years) 59.3 (11.2) 61.0 (10.4) <0.001
Age leaving education 20.7 (7.4) 21.1 (8.1) 0.15
Beck Depression Inventory (BDI) 6.4 (6.1) 7.8 (6.9) <0.001
Body mass index (kg/m
2
) 26.3 (3.3) 30.7 (4.1) <0.001
Physical activity (Physical Activity Scale for the Elderly) 200 (89) 188 (96) <0.001
High-sensitivity C-reactive protein (mg/L)
b
3.9 (7.9) 5.5 (8.3) <0.001
Metabolic syndrome criteria
Waist circumference (cm) 94.4 (8.9) 107 (9.8) <0.001
Systolic blood pressure (mmHg) 143 (20) 152 (20) <0.001
Diastolic blood pressure (mmHg) 86 (12) 90 (12) <0.001
High-density lipoprotein-cholesterol (mmol/L) 1.5 (0.3) 1.2 (0.3) <0.001
Triglycerides (mmol/L) 1.3 (0.7) 2.2 (1.4) <0.001
Glucose (mmol/L) 5.3 (0.9) 6.4 (1.8) <0.001
Cognitive test scores
ReyOsterrieth Complex Figure copy 33.6 (4.2) 32.8 (5.0) <0.001
ReyOsterrieth Complex Figure recall 17.2 (6.7) 16.4 (6.5) 0.002
Camden Topographical Recognition Memory 22.9 (4.7) 22.4 (4.7) 0.006
Digit Symbol Substitution Test 28.1 (8.6) 26.6 (9.2) <0.001
Number (%)
Adult Treatment Panel-III metabolic syndrome 2145 (68) 1007 (32)
Waist circumference >102 cm 334 (16) 775 (77) <0.001
Blood pressure >= 130/85 mm Hg and/or using anti-hypertensive drugs 1701 (79) 981 (97) <0.001
High-density lipoprotein-cholesterol <1.03 mmol/L 98 (5) 303 (30) <0.001
Triglycerides 1.7 mmol/L 298 (14) 663 (66) <0.001
Measured blood glucose 5.6 mmol/L and/or using anti-diabetic drugs 412 (19) 725 (72) <0.001
Depressive symptoms
None (BDI 10) 1691 (79) 748 (75) <0.001
Mild-borderline (BDI 1120) 375 (18) 189 (19)
Moderate-extreme (BDI 21) 63 (3) 59 (6)
Self-reported diabetes and/or using anti-diabetic drugs 72 (3) 169 (17) <0.001
Obese (body mass index 30) 238 (11) 540 (54) <0.001
Current smoker 459 (21) 196 (19) 0.21
Alcohol (1 day/week) 1232 (58) 539 (54) 0.04
Heart condition 317 (15) 201 (20) <0.001
Stroke 70 (3) 43 (4) 0.16
a
T-test or rank sum test for continuous variables and
2
test for categorical variables: between metabolic syndrome groups.
b
Distribution very positively skewed, median (interquartile range): absent = 0.20 (0.29); present = 0.33 (0.43).
syndrome revealed no signicant association (p > 0.05,
data not shown).
The association between glucose levels and cognition
was further explored according to diagnostic categories
(Table 5). Therefore, diabetic men had signicantly lower
scores on all cognitive tests except for CTRM( = 1.111,
p > 0.05). The latter was negatively associated with
impaired fasting glucose ( = 0.778, p < 0.01). We
found no signicant association between anti-diabetic or
anti-hypertensive drug use and cognition.
Cognition, hs-CRP and metabolic
syndrome status
We assessed for a possible association between hs-
CRP levels as a marker of inammation and cognitive
performance (Table 6). In the adjusted model for age
alone, a signicant inverse association was observed
between hs-CRP levels and DSST scores. This association
persisted after additional adjustment for education,
smoking, alcohol consumption, physical activity, centre
and depression (data not shown). However, when this
model was analysed with adjustment for metabolic
syndrome, no signicant association was found. There
was no evidence that the association of hs-CRP with any
of the cognitive outcomes was modied by metabolic
syndrome status (metabolic syndrome hs-CRP)] (all
p
interaction
> 0.05, data not shown).
Discussion
In this cross-sectional study of middle-aged and older
European men, the prevalence of the metabolic syndrome
was 32%. The prevalence of the metabolic syndrome
reported in previous studies varied between 5 and
53% in men, depending on the population, age and
applied criteria [ [2] and references herein], making
direct comparisons difcult. Our prevalence rate of
metabolic syndrome is in agreement with a median
Copyright 2010 John Wiley & Sons, Ltd. Diabetes Metab Res Rev 2010; 26: 668676.
DOI: 10.1002/dmrr
672 J. Tournoy et al.
Table 2. Multi-variable linear regression of cognitive test scores on presence of metabolic syndrome (absent = reference group):
covariates in the model
Cognitive test
ReyOsterrieth
Complex
Figure copy
ReyOsterrieth
Complex
Figure recall
Camden Topographical
Recognition
Memory
Digit Symbol
Substitution Test
Covariates in
the model -coefcient (95% condence interval)
Age
a
0.608 (0.929, 0.288)
0.381 (0.842, 0.080) 0.228 (0.558, 0.103) 0.813 (1.379, 0.248)
Age, lifestyle,
depression
b
0.673 (1.411, 0.065) 0.442 (1.233, 0.348) 0.190 (0.817, 0.437) 0.612 (1.347, 0.123)
p < 0.001.
a
Adjusted for age alone.
b
Adjusted for age, education, smoking (non-smoking versus currently smoking), alcohol consumption (<1 day/week versus 1 day/week), physical
activity (Physical Activity Scale for the Elderly), centre and depressive symptoms (Beck Depression Inventory score).
Table 3. Multi-variable linear regression of cognitive test scores on components of the metabolic syndrome
Cognitive test
ReyOsterrieth
Complex Figure
copy
ReyOsterrieth
Complex Figure
recall
Camden
Topographical
Recognition
Memory
Digit Symbol
Substitution Test
Components of the
metabolic syndrome -coefcient (95% condence interval)
a
Waist circumference
(cm)
0.017 (0.039, 0.004) 0.011 (0.040, 0.019) 0.008 (0.039, 0.023) 0.027 (0.058, 0.005)
Systolic blood
pressure (mmHg)
0.001 (0.014, 0.011) 0.007 (0.006, 0.019) 0.004 (0.019, 0.011) 0.014 (0.039, 0.010)
Diastolic blood
pressure (mmHg)
0.012 (0.005, 0.030) 0.025 (0.001, 0.049)
0.004 (0.019, 0.027) 0.022 (0.068, 0.025)
High-density
lipoprotein-
cholesterol
(mmol/L)
0.581 (0.047, 1.114)
0.922 (0.054, 1.789)
0.274 (0.637, 1.184) 0.355 (1.462, 2.172)
Triglycerides (mmol/L) 0.104 (0.269, 0.061) 0.019 (0.244, 0.282) 0.078 (0.240, 0.085) 0.061 (0.310, 0.187)
Glucose (mmol/L) 0.261 (0.458, 0.064)
0.175 (0.343, 0.007)
0.254 (0.484, 0.022)
0.552 (0.855, 0.248)
Although the distribution of triglycerides was positively skewed, using log transformed triglycerides in the above regressions did not substantively
change the associations (all p > 0.05) from those using the untransformed variable.
p < 0.05,
p < 0.01.
a
Adjusted for age, education, smoking (non-smoking versus currently smoking), alcohol consumption (<1 day/week versus 1 day/week), physical
activity (Physical Activity Scale for the Elderly), depressive symptoms (Beck Depression Inventory score) and centre.
prevalence of 31% in elderly populations [21]. Among
those with the metabolic syndrome, the prevalence of
individual metabolic syndrome criteria was consistent
with ndings in similar studies, with hypertension and
waist circumference being the most frequent components
[7,22]. However, large variations between different
studies have been reported [21] due to differences
in age, population and lifestyle factors. We found
a signicantly higher percentage of participants with
either hyperglycaemia or taking anti-diabetic medication
compared with other studies [21], most likely because
we used the proposed lowered criterion of normal
fasting plasma glucose of 5.6 mmol/L, while a limit of
6.1 mmol/L was used in other studies [21].
In general, no association was observed in our
cohort between the presence of metabolic syndrome and
cognition after adjustment for confounders. Our data
agree with previous cross-sectional data reports of a lack
of association between metabolic syndrome and baseline
cognitive performance [6,7] or dementia [9]. In contrast,
several other studies did observe an association with
cognitive impairment [3,23] or dementia [4,5]. Available
evidence had several reasons that could explain some
of the inconsistencies. Differences in study population
may have in part explained the discrepant ndings.
Second, relationships between metabolic syndrome and
cognitive decline or the development of dementia over
time have been primarily reported in longitudinal studies
[6,8,24,25]. Some of these studies showed no signicant
association at baseline but accelerated cognitive decline in
subjects with metabolic syndrome [6]. Lack of evidence of
an association between metabolic syndrome and cognitive
impairment at baseline, as in our current analysis, does
not exclude the potential for such a relationship during
follow-up. Third, our cross-sectional results are based
on static data, while factors that dene the metabolic
Copyright 2010 John Wiley & Sons, Ltd. Diabetes Metab Res Rev 2010; 26: 668676.
DOI: 10.1002/dmrr
Association of Cognitive Performance With the Metabolic Syndrome 673
Table 4. Multi-variable linear regression of cognitive test scores on components of the metabolic syndrome
Cognitive test
ReyOsterrieth
Complex Figure
copy
ReyOsterrieth
Complex Figure
recall
Camden
Topographical
Recognition
Memory
Digit Symbol
Substitution
Test
Components of the
metabolic syndrome -coefcient (95% condence interval)
a
Waist circumference
(cm)
0.021 (0.046, 0.004) 0.009 (0.042, 0.023) 0.016 (0.048, 0.017) 0.029 (0.068, 0.010)
Systolic blood
pressure (mmHg)
0.001 (0.012, 0.015) 0.008 (0.006, 0.023) 0.001 (0.019, 0.016) 0.013 (0.044, 0.018)
Diastolic blood
pressure (mmHg)
0.016 (0.002, 0.034) 0.026 (0.002, 0.054) 0.005 (0.025, 0.035) 0.020 (0.078, 0.036)
High-density
lipoprotein-
cholesterol
(mmol/L)
0.736 (0.130, 1.342)
1.007 (0.212, 1.801)
0.341 (0.734, 1.416) 0.255 (1.964, 2.475)
Triglycerides (mmol/L) 0.093 (0.290, 0.105) 0.040 (0.257, 0.337) 0.033 (0.193, 0.127) 0.091 (0.387, 0.204)
Glucose (mmol/L) 0.242 (0.448, 0.036)
0.156 (0.316, 0.004) 0.246 (0.496, 0.004) 0.530 (0.858, 0.203)
p < 0.05,
p < 0.01.
a
Adjusted for the same variables as the model in Table 3, plus high-sensitivity C-reactive protein.
syndrome are dynamic and their modulating effect on
the risk of developing cognitive impairment might change
over time. In a recent longitudinal study by Akbaraly et al.
[26], no differences in cognitive function were observed
in participants with non-persistent metabolic syndrome,
but the opposite was found if metabolic syndrome
persisted over time. Our current baseline analysis did
not allow assessment of the duration of risk factors that
could modify the risk of cognitive impairment. Fourth,
because of our study design, allowing standardization
across centres independent of culture and language, only
certain cognitive domains were assessed, including visuo-
constructional ability, visual memory, executive function,
attention and processing speed. Several studies have
reported that the metabolic syndrome, or its individual
components, may be associated with specic areas of
cognition that we did not assess, such as verbal learning
and semantic memory [27,28].
Analyzing the potential effect of individual components
of the metabolic syndrome on cognition revealed that
blood glucose levels were inversely associated with all
cognitive scores. To further explore this association,
we discriminated subjects with normal fasting glucose,
impaired fasting glucose and subjects with diabetes. Here,
we found inverse associations between the presence of
diabetes and ROCF copy and recall and DSST scores.
These data are largely consistent with published evidence
for a role of (pre)diabetes in cognitive impairment [29,30]
and the risk of developing dementia [30,31]. Also,
in studies where metabolic syndrome was associated
with cognitive decline, hyperglycaemia was the main
contributor [3,25]. Specic cognitive functions that were
associated with diabetes included verbal and non-verbal
memory, executive functioning and processing speed
[32]. These cognitive domains may be impaired as
a consequence of hypo- and hyperglycaemia, vascular
disease and insulin resistance [33]. Also, diabetes
may interfere with A and tau metabolism, the main
components of the pathological hallmarks of Alzheimers
disease, plaques and tangles, respectively [34].
Our nding of a relation between high serum HDL-c
levels and cognitive performance is in agreement with
previous observations, where higher HDL-c levels were
associated with reduction of cognitive decline among
older participants [11,35] and lower HDL-c levels with
impaired memory [8,36]. Several plausible explanations
might account for this association. First, HDL is the main
carrier of cholesterol in the brain and enhances synaptic
growth and regeneration [37]. Second, low HDL-c is a
known risk factor for cardiovascular disease, which in
turn can lead to dementia. Third, HDL plays an important
role in A metabolism by preventing its aggregation [38].
However, not all data support the association between
HDL-c and cognitive function [39], and the absence of
any association has specically been reported in older
women [40,41].
Although subjects with metabolic syndrome had higher
levels of inammation, we did not demonstrate any
association between hs-CRP and cognition either in the
presence or absence of metabolic syndrome. This is in
contrast to other ndings, where metabolic syndrome
was negatively associated with cognition especially
in subjects with high inammation [3,6,7]. Again,
study population differences might account for these
differences or associative effects could depend on follow-
up observations.
To our knowledge, we report the rst study to
specically analyse the association between cognitive
function and metabolic syndrome in a large sample of
middle-aged and older European men and demonstrated
no specic association. The key strengths of our study
are that it is based on a representative population-
based framework and that it used uniform methods to
evaluate biophysical and laboratory parameters and a
Copyright 2010 John Wiley & Sons, Ltd. Diabetes Metab Res Rev 2010; 26: 668676.
DOI: 10.1002/dmrr
674 J. Tournoy et al.
Table 5. Multi-variable linear regression of cognitive test scores on fasting glucose and on use of anti-diabetic and anti-hypertensive
medications
Cognitive test
ReyOsterrieth
Complex Figure
copy
ReyOsterrieth
Complex Figure
recall
Camden
Topographical
Recognition
Memory
Digit Symbol
Substitution
Test
Diagnostic
categories -coefcient (95% condence interval)
a
Glycaemia group
Normal fasting glucose Reference Reference Reference Reference
(glucose <5.6 mmol/L and not
using anti-diabetic medication)
Impaired fasting glucose 0.610 (1.694, 0.475) 0.553 (1.635, 0.526) 0.778 (1.277, 0.278)
0.814 (2.076, 0.447)
(glucose 5.6 mmol/L and
<7.0 mmol/L)
Diabetic 1.278 (1.993, 0.563)
1.023 (1.498, 0.548)
1.111 (2.423, 0.200) 2.810 (4.608, 1.012)
(glucose 7.0 mmol/L or using
anti-diabetic medication)
Anti-diabetic/anti-hypertensive drugs
No usage Reference Reference Reference Reference
Any usage 0.196 (1.037, 0.645) 0.005 (0.718, 0.707) 0.049 (0.671, 0.573) 0.144 (0.476, 0.763)
p < 0.01.
a
Adjusted for age, education, smoking (non-smoking versus currently smoking), alcohol consumption (<1 day/week versus 1 day/week), physical
activity (Physical Activity Scale for the Elderly), depressive symptoms (Beck Depression Inventory score), high-sensitivity C-reactive protein and centre.
Table 6. Multi-variable linear regression of cognitive test scores on high-sensitivity C-reactive protein
Cognitive test
ReyOsterrieth
Complex Figure
copy
ReyOsterrieth
Complex Figure
recall
Camden
Topographical
Recognition
Memory
Digit Symbol
Substitution
Test
Covariates in
the model -coefcient (95% condence interval)
Age
a
0.086 (0.289, 0.117) 0.187 (0.475, 0.101) 0.160 (0.368, 0.047) 0.650 (1.006, 0.293)
Age, lifestyle,
depression and
metabolic syndrome
b
0.021 (0.147, 0.188) 0.081 (0.498, 0.336) 0.066 (0.383, 0.252) 0.360 (0.724, 0.005)
p < 0.001.
a
Adjusted for age alone.
b
Adjusted for age, education, smoking (non-smoking versus currently smoking), alcohol consumption (<1 day/week versus 1 day/week), physical
activity (Physical Activity Scale for the Elderly), centre, depressive symptoms (Beck Depression Inventory score) and metabolic syndrome.
battery of cognitive tests easily applicable across different
cultures and languages. In addition, we assessed a large
variety of potential confounders, such as education,
depressive symptoms, smoking and physical activity.
Nevertheless, the ndings have to be interpreted in the
context of the study design which was not without
limitations, including some general methodological
limitations [14]. First, the overall response rate for the
study (41%) could have created a selection bias. Although
the general characteristics of responders versus non-
responders were reported to be largely similar [14], some
observed differences, including smoking prevalence or
socioeconomic status, could have created a response bias,
where those who responded may have differed regarding
the association between metabolic syndrome status and
overall cognitive ability compared with those who did
not respond. Second, survival bias or reverse causality,
the latter in which lower cognitive skills could lead to a
higher risk of diabetes, may bias the observed association,
but the magnitude of these effects is unknown. Third,
specic cognitive domains like verbal memory or semantic
functions were not assessed for their association with the
metabolic syndrome in this study. Fourth, we did not
evaluate subsyndromal cognitive defects and impairment,
so the current data cannot be extrapolated to specic
diseases or conditions. Fifth, the National Cholesterol
Education Program criteria are not the only standardized
denition for metabolic syndrome. Using other denitions
might well inuence the observed effects. However, the
National Cholesterol Education Program denition was
chosen because it better predicts outcome in elderly
subjects than other metabolic syndrome criteria [42].
Copyright 2010 John Wiley & Sons, Ltd. Diabetes Metab Res Rev 2010; 26: 668676.
DOI: 10.1002/dmrr
Association of Cognitive Performance With the Metabolic Syndrome 675
Sixth, conditions contributing to the metabolic syndrome
may change over time. Since the duration of specic
conditions was not assessed at baseline, the potential
inuence of their persistence in time on our results could
not be analysed. However, longitudinal European Male
Ageing Study data will become available and will allow
more in-depth cause-and-effect analyses.
In conclusion, prevalent metabolic syndrome was
not associated with cognitive impairment in a large
community-dwelling sample of middle-aged and older
European men. When analyzing individual components
of the syndrome, those with diabetes were found to
have poorer performance with respect to memory,
executive functions and processing speed. The nature
of this association remains unclear and requires further
investigation.
Acknowledgements
The European Male Aging Study is funded by the Commission
of the European Communities Fifth Framework Programme
Quality of Life and Management of Living Resources Grant
QLK6-CT-2001-00258. Additional support was also provided
by Arthritis Research UK. The authors thank the men who
participated in the eight countries, the research/nursing staff in
the eight centres: C. Pott (Manchester), E. Wouters (Leuven),
M. Nilsson (Malm o), M. del Mar Fernandez (Santiago de
Compostela), M. Jedrzejowska ( odY), H.-M. Tabo (Tartu),
A. Heredi (Szeged) for their data collection and C. Moseley
(Manchester) for data entry and project co-ordination. Dr S.
Boonen is senior clinical investigator of the Fund for Scientic
Research, Flanders, Belgium (F.W.O. Vlaanderen) and holder
of the Novartis Leuven University Chair in Gerontology and
Geriatrics.
Conflict of interest
The authors have no nancial arrangements or conict of
interest to disclose concerning this manuscript.
References
1. Alberti KG, Zimmet PZ. Denition, diagnosis and classication
of diabetes mellitus and its complications. Part 1: diagnosis and
classication of diabetes mellitus provisional report of a WHO
consultation. Diabet Med 1998; 15(7): 539553.
2. Qiao Q, Gao W, Zhang L, Nyamdorj R, Tuomilehto J. Metabolic
syndrome and cardiovascular disease. Ann Clin Biochem 2007;
44(Pt 3): 232263.
3. Dik MG, Jonker C, Comijs HC, et al. Contribution of metabolic
syndrome components to cognition in older individuals. Diabetes
Care 2007; 30(10): 26552660.
4. Razay G, Vreugdenhil A, Wilcock G. The metabolic syndrome
and Alzheimer disease. Arch Neurol 2007; 64(1): 9396.
5. Vanhanen M, Koivisto K, Moilanen L, et al. Association of
metabolic syndrome with Alzheimer disease: a population-based
study. Neurology 2006; 67(5): 843847.
6. Yaffe K, Haan M, Blackwell T, Cherkasova E, Whitmer RA,
West N. Metabolic syndrome and cognitive decline in elderly
Latinos: ndings from the Sacramento Area Latino Study of
Aging study. J Am Geriatr Soc 2007; 55(5): 758762.
7. Yaffe K, Kanaya A, Lindquist K, et al. The metabolic syndrome,
inammation, and risk of cognitive decline. JAMA 2004;
292(18): 22372242.
8. Komulainen P, Lakka TA, Kivipelto M, et al. Metabolic syndrome
and cognitive function: a population-based follow-up study
in elderly women. Dement Geriatr Cogn Disord 2007;; 23(1):
2934.
9. Muller M, Tang MX, Schupf N, Manly JJ, Mayeux R, Luchsinger
JA. Metabolic syndrome and dementia risk in a multiethnic
elderly cohort. Dement Geriatr Cogn Disord 2007; 24(3):
185192.
10. van den Berg E, Biessels GJ, de Craen AJ, Gussekloo J,
Westendorp RG. The metabolic syndrome is associated with
decelerated cognitive decline in the oldest old. Neurology 2007;
69(10): 979985.
11. Laudisio A, Marzetti E, Pagano F, et al. Association of metabolic
syndrome with cognitive function: the role of sex and age. Clin
Nutr 2008; 27(5): 747754.
12. Yaffe K, Weston AL, Blackwell T, Krueger KA. The metabolic
syndrome and development of cognitive impairment among
older women. Arch Neurol 2009; 66(3): 324328.
13. Devaraj S, Singh U, Jialal I. Human C-reactive protein and the
metabolic syndrome. Curr Opin Lipidol 2009; 20(3): 182189.
14. Lee DM, ONeill TW, Pye SR, et al. The European Male Ageing
Study (EMAS): design, methods and recruitment. Int J Androl
2009; 32(1): 1124.
15. Washburn RA, Smith KW, Jette AM, Janney CA. The Physical
Activity Scale for the Elderly (PASE): development and
evaluation. J Clin Epidemiol 1993; 46(2): 153162.
16. Beck AT, Steer RA, Brown GK. Manual for the Beck Depression
Inventory-II. Psychological Corporation: San Antonio, TX, 1996.
17. Expert Panel on Detection E, and Treatment of High Blood
Cholesterol in Adults. Executive summary of the third report
of the National Cholesterol Education Program (NCEP) expert
panel on detection, evaluation, and treatment of high blood
cholesterol in adults (Adult Treatment Panel III). JAMA 2001;
285(19): 24862497.
18. Osterrieth. Le test de copie dune gure complexe. Arch Psychol
1944; 30: 286356.
19. Warrington E. The Camden memory Test Manual. Psychology
press: Hove, 1996.
20. Uiterwijk J. WAIS-III-NL/V. Lisse. Swets and Zeitlinger: The
Netherlands, 2001.
21. Denys K, Cankurtaran M, Janssens W, Petrovic M. Metabolic
syndrome in the elderly: an overview of the evidence. Acta
Clin Belg 2009; 64(1): 2334.
22. Raffaitin C, Gin H, Empana JP, et al. Metabolic syndrome and
risk for incident Alzheimers disease or vascular dementia: the
three-city study. Diabetes Care 2009; 32(1): 169174.
23. Segura B, Jurado MA, Freixenet N, Albuin C, Muniesa J,
Junque C. Mental slowness and executive dysfunctions in
patients with metabolic syndrome. Neurosci Lett 2009; 462(1):
4953.
24. Kalmijn S, Foley D, White L, et al. Metabolic cardiovascular
syndrome and risk of dementia in Japanese-American elderly
men. The Honolulu-Asia aging study. Arterioscler Thromb Vasc
Biol 2000; 20(10): 22552260.
25. Yaffe K. Metabolic syndrome and cognitive disorders: is the sum
greater than its parts?. Alzheimer Dis Assoc Disord 2007; 21(2):
167171.
26. Akbaraly TN, Kivimaki M, Shipley MJ, et al. Metabolic syndrome
over 10 years and cognitive functioning in late mid life: the
Whitehall II study. Diabetes Care 2009; 33(1): 8489.
27. Gatto NM, Henderson VW, St John JA, McCleary C, Hodis HN,
Mack WJ. Metabolic syndrome and cognitive function in healthy
middle-aged and older adults without diabetes. Neuropsychol Dev
Cogn B Aging Neuropsychol Cogn 2008; 15(5): 627641.
28. Strachan MW, Deary IJ, Ewing FM, Frier BM. Is type II diabetes
associated with an increased risk of cognitive dysfunction? A
critical review of published studies. Diabetes Care 1997; 20(3):
438445.
29. Yaffe K, Blackwell T, Kanaya AM, Davidowitz N, Barrett-
Connor E, Krueger K. Diabetes, impaired fasting glucose, and
development of cognitive impairment in older women. Neurology
2004; 63(4): 658663.
30. Luchsinger JA, Tang MX, Shea S, Mayeux R. Hyperinsulinemia
and risk of Alzheimer disease. Neurology 2004; 63(7):
11871192.
Copyright 2010 John Wiley & Sons, Ltd. Diabetes Metab Res Rev 2010; 26: 668676.
DOI: 10.1002/dmrr
676 J. Tournoy et al.
31. Ott A, Stolk RP, van Harskamp F, Pols HA, Hofman A,
Breteler MM. Diabetes mellitus and the risk of dementia: the
Rotterdam study. Neurology 1999; 53(9): 19371942.
32. S Roriz-Filho J, Sa-Roriz TM, Rosset I, et al. (Pre)diabetes, brain
aging, and cognition. Biochim Biophys Acta 2009; 1792(5):
432443.
33. Kodl CT, Seaquist ER. Cognitive dysfunction and diabetes
mellitus. Endocr Rev 2008; 29(4): 494511.
34. Gasparini L, Xu H. Potential roles of insulin and IGF-1 in
Alzheimers disease. Trends Neurosci 2003; 26(8): 404406.
35. Karlamangla AS, Singer BH, Reuben DB, Seeman TE. Increases
in serum non-high-density lipoprotein cholesterol may be
benecial in some high-functioning older adults: MacArthur
studies of successful aging. J Am Geriatr Soc 2004; 52(4):
487494.
36. Zhang J, McKeown RE, Hajjar I. Serum cholesterol levels are
associated with impaired recall memory among older people.
Age Ageing 2005; 34(2): 178182.
37. Mauch DH, Nagler K, Schumacher S, et al. CNS synaptogenesis
promoted by glia-derived cholesterol. Science 2001; 294(5545):
13541357.
38. Olesen OF, Dago L. High density lipoprotein inhibits assembly of
amyloid beta-peptides into brils. Biochem Biophys Res Commun
2000; 270(1): 6266.
39. Reitz C, Luchsinger J, Tang MX, Manly J, Mayeux R. Impact of
plasma lipids and time on memory performance in healthy
elderly without dementia. Neurology 2005; 64(8): 13781383.
40. Henderson VW, Guthrie JR, Dennerstein L. Serum lipids and
memory in a population based cohort of middle age women. J
Neurol Neurosurg Psychiatry 2003; 74(11): 15301535.
41. Yaffe K, Barrett-Connor E, Lin F, Grady D. Serum lipoprotein
levels, statin use, and cognitive function in older women. Arch
Neurol 2002; 59(3): 378384.
42. Scuteri A, Najjar SS, Morrell CH, Lakatta EG. The metabolic
syndrome in older individuals: prevalence and prediction of
cardiovascular events: the Cardiovascular Health study. Diabetes
Care 2005; 28(4): 882887.
Copyright 2010 John Wiley & Sons, Ltd. Diabetes Metab Res Rev 2010; 26: 668676.
DOI: 10.1002/dmrr
You might also like
- PH Red Cross First Aid and BLS (Edited)Document41 pagesPH Red Cross First Aid and BLS (Edited)ctuagent75% (8)
- Association Between A Comprehensive Movement Assesment and MetabolicallyDocument9 pagesAssociation Between A Comprehensive Movement Assesment and MetabolicallyzunigasanNo ratings yet
- Metabolic Syndrome and Quality of Life in The Elderly: Age and Gender DifferencesDocument10 pagesMetabolic Syndrome and Quality of Life in The Elderly: Age and Gender DifferencesThalia KarampasiNo ratings yet
- Metabolic Syndrome and Risk For Incident Alzheimer's Disease or Vascular DementiaDocument6 pagesMetabolic Syndrome and Risk For Incident Alzheimer's Disease or Vascular DementiaadriricaldeNo ratings yet
- Review Article: Overactive Bladder: Is There A Link To The Metabolic Syndrome in Men?Document5 pagesReview Article: Overactive Bladder: Is There A Link To The Metabolic Syndrome in Men?monicamoniccNo ratings yet
- Am J Clin Nutr 2014 Chung Ajcn.114.086314Document17 pagesAm J Clin Nutr 2014 Chung Ajcn.114.086314Daniel Lee Eisenberg JacobsNo ratings yet
- Metabolic Pro Filing of Polycystic Ovary Syndrome Reveals Interactions With Abdominal ObesityDocument10 pagesMetabolic Pro Filing of Polycystic Ovary Syndrome Reveals Interactions With Abdominal ObesityYuniati ValentinaNo ratings yet
- 2015 Sup 11 FullDocument5 pages2015 Sup 11 FullsebastianNo ratings yet
- Risk Factors of Non-Communicable Diseases and Metabolic SyndromeDocument9 pagesRisk Factors of Non-Communicable Diseases and Metabolic SyndromeAseem MohammedNo ratings yet
- Accepted Manuscript: MaturitasDocument26 pagesAccepted Manuscript: MaturitasAlpha17 MedicsteenNo ratings yet
- Healthy Behaviours, Lifestyle Patterns and Sociodemographic Determinants of The Metabolic SyndromeDocument6 pagesHealthy Behaviours, Lifestyle Patterns and Sociodemographic Determinants of The Metabolic SyndromeReynaldo TrianaNo ratings yet
- Jurnal MKMI, Vol 6 No.2, Januari 2011, Hal 7-16: Artikel IIDocument10 pagesJurnal MKMI, Vol 6 No.2, Januari 2011, Hal 7-16: Artikel IIIndra DwinataNo ratings yet
- International Journal of STD & AIDS: Hypogonadism Among HIV-infected Men in ThailandDocument7 pagesInternational Journal of STD & AIDS: Hypogonadism Among HIV-infected Men in ThailandMohankummar MuniandyNo ratings yet
- Write Review On Metabolic Disorders and ManagementDocument9 pagesWrite Review On Metabolic Disorders and ManagementFatima MazharNo ratings yet
- Epidemiology of The Metabolic Syndrome in Hungary: Public HealthDocument7 pagesEpidemiology of The Metabolic Syndrome in Hungary: Public Healthadi suputraNo ratings yet
- A Prospective Study of Obesity and Incidence and Progession of Lower Urinary Tract SymptomsDocument13 pagesA Prospective Study of Obesity and Incidence and Progession of Lower Urinary Tract SymptomssusanaNo ratings yet
- Diabetes & Metabolic Syndrome: Clinical Research & Reviews: Mohsen Janghorbani, Masoud AminiDocument7 pagesDiabetes & Metabolic Syndrome: Clinical Research & Reviews: Mohsen Janghorbani, Masoud AminiAndi SuryawanNo ratings yet
- Effect of Probiotics Therapy On Nonalcoholic Fatty Liver DiseaseDocument15 pagesEffect of Probiotics Therapy On Nonalcoholic Fatty Liver DiseaserachelNo ratings yet
- Cross Sectional 1Document7 pagesCross Sectional 1Ridho KurniaNo ratings yet
- High Prevalence of Metabolic Syndrome Features in Patients Previously Treated For Nonfunctioning Pituitary MacroadenomaDocument7 pagesHigh Prevalence of Metabolic Syndrome Features in Patients Previously Treated For Nonfunctioning Pituitary Macroadenomaseb2008No ratings yet
- PB, Afect, Cardiovasc, Biomark, LDL, CholestDocument6 pagesPB, Afect, Cardiovasc, Biomark, LDL, CholestAna IsaNo ratings yet
- Belsky Daniel Et Al., Quantification of Biological Aging in Young AdultsDocument7 pagesBelsky Daniel Et Al., Quantification of Biological Aging in Young AdultsAristide de BésureNo ratings yet
- Higher Selenium Status Is Associated With Adverse Blood Lipid Profile in British AdultsDocument7 pagesHigher Selenium Status Is Associated With Adverse Blood Lipid Profile in British AdultsHerly Maulida SurdhawatiNo ratings yet
- Downloaded From Uva-Dare, The Institutional Repository of The University of Amsterdam (Uva)Document28 pagesDownloaded From Uva-Dare, The Institutional Repository of The University of Amsterdam (Uva)Indah Putri permatasariNo ratings yet
- Physical Activity and Mortality in Indiv PDFDocument11 pagesPhysical Activity and Mortality in Indiv PDFYudistiraNo ratings yet
- 2017 Article 215Document11 pages2017 Article 215pelinNo ratings yet
- Analysis of Blood Glucose Distribution Characteristics and Its Risk Factors Among A Health Examination Population in Wuhu (China)Document9 pagesAnalysis of Blood Glucose Distribution Characteristics and Its Risk Factors Among A Health Examination Population in Wuhu (China)Aleksa CopicNo ratings yet
- Association Between Dietary Patterns and The Risk of Metabolic Syndrome Among Lebanese AdultsDocument9 pagesAssociation Between Dietary Patterns and The Risk of Metabolic Syndrome Among Lebanese AdultsThalia KarampasiNo ratings yet
- The Association Between Metabolic Syndrome and Biochemical Markers in Beijing AdolescentsDocument10 pagesThe Association Between Metabolic Syndrome and Biochemical Markers in Beijing AdolescentsZhe WangNo ratings yet
- GoutDocument17 pagesGoutnadita erischaNo ratings yet
- Association of E-Cigarettes With Erectile Dysfunction: The Population Assessment of Tobacco and Health StudyDocument13 pagesAssociation of E-Cigarettes With Erectile Dysfunction: The Population Assessment of Tobacco and Health StudyThaynan Filipe TFNo ratings yet
- Aging YeniDocument19 pagesAging YeniDr.Serkan SenerNo ratings yet
- Complex Actions of Sex Steroids in Adipose Tissue, The Cardiovascular System, and Brain: Insights From Basic Science and Clinical StudiesDocument31 pagesComplex Actions of Sex Steroids in Adipose Tissue, The Cardiovascular System, and Brain: Insights From Basic Science and Clinical Studiesgparya009No ratings yet
- Nutrients: Chewing Difficulty Should Be Included As A Geriatric SyndromeDocument12 pagesNutrients: Chewing Difficulty Should Be Included As A Geriatric SyndromeIlmia AmaliaNo ratings yet
- Nonalcoholic SteatohepatitisDocument15 pagesNonalcoholic SteatohepatitisLucas VenturaNo ratings yet
- Nutrients 13 00315Document11 pagesNutrients 13 00315Priscila PintoNo ratings yet
- Age at Menarche and Lung Function: A Mendelian Randomization StudyDocument10 pagesAge at Menarche and Lung Function: A Mendelian Randomization StudySpica RegulusNo ratings yet
- A Case-Comparison Study of Executive Functions in Alcohol-Dependent Adults With Maternal History of AlcoholismDocument6 pagesA Case-Comparison Study of Executive Functions in Alcohol-Dependent Adults With Maternal History of AlcoholismmirymirelaNo ratings yet
- Napping and Prevalence of Metabolic SyndromeDocument13 pagesNapping and Prevalence of Metabolic SyndromeLuisNo ratings yet
- Hypertension, Diabetes and Cognitive Impairment Among ElderlyDocument8 pagesHypertension, Diabetes and Cognitive Impairment Among ElderlyIJPHSNo ratings yet
- Sui&Pasco (2020) Nice ReviewDocument10 pagesSui&Pasco (2020) Nice ReviewFred ThingsNo ratings yet
- Age at Menarche and Type 2 Diabetes Risk 2013Document9 pagesAge at Menarche and Type 2 Diabetes Risk 2013Corin Boice TelloNo ratings yet
- 5 Prevalence and Risk ChinaDocument16 pages5 Prevalence and Risk ChinaM JNo ratings yet
- Ni Hms 400832Document15 pagesNi Hms 400832andinitaaaNo ratings yet
- Active Smoking, Passive Smoking, and Risk of Nonalcoholic Fatty Liver Disease (NAFLD) : A Population-Based Study in ChinaDocument7 pagesActive Smoking, Passive Smoking, and Risk of Nonalcoholic Fatty Liver Disease (NAFLD) : A Population-Based Study in ChinaYelvi Novita RozaNo ratings yet
- GuidliinesDocument13 pagesGuidliinesFaten NajarNo ratings yet
- Recent Advances in Cardiovascular Aspects of Polycystic Ovary SyndromeDocument9 pagesRecent Advances in Cardiovascular Aspects of Polycystic Ovary SyndromeRuth BritoNo ratings yet
- Outcomes/Epidemiology/Socioeconomics: Health Issues of Men: Prevalence and Correlates of Erectile DysfunctionDocument6 pagesOutcomes/Epidemiology/Socioeconomics: Health Issues of Men: Prevalence and Correlates of Erectile Dysfunctionputri windianiNo ratings yet
- 641 FullDocument6 pages641 FullLider Olmen PanggabeanNo ratings yet
- PIIS1059131118301237Document8 pagesPIIS1059131118301237bilal hadiNo ratings yet
- Lichen PlanusDocument7 pagesLichen PlanusHania KhanNo ratings yet
- The Metabolic Syndrome in Healthy, Multiethnic Adolescents in Toronto, Ontario: The Use of Fasting Blood Glucose As A Simple IndicatorDocument5 pagesThe Metabolic Syndrome in Healthy, Multiethnic Adolescents in Toronto, Ontario: The Use of Fasting Blood Glucose As A Simple Indicatordoxy20No ratings yet
- Dyslipidemia and Metabolic Syndrome in Patients With Lichen Planus: A Case-Control StudyDocument8 pagesDyslipidemia and Metabolic Syndrome in Patients With Lichen Planus: A Case-Control StudyPOPA EMILIANNo ratings yet
- KocełakDocument14 pagesKocełaksaifulmangopo123No ratings yet
- PS 305 Milestone 2Document2 pagesPS 305 Milestone 2Ashika LataNo ratings yet
- Plant-Based Dietary Changes May Improve Symptoms in Patients With Systemic Lupus ErythematosusDocument12 pagesPlant-Based Dietary Changes May Improve Symptoms in Patients With Systemic Lupus ErythematosusLucas PedroNo ratings yet
- Insulin Metabolism in Polycystic Ovary Syndrome Secretion, Signaling, and ClearanceDocument14 pagesInsulin Metabolism in Polycystic Ovary Syndrome Secretion, Signaling, and ClearancePatterns of IvyNo ratings yet
- tmpE2CA TMPDocument5 pagestmpE2CA TMPFrontiersNo ratings yet
- Artigo Dieta Anti-Inflamatória No MetabolismoDocument12 pagesArtigo Dieta Anti-Inflamatória No MetabolismoRegiane De Sousa LimaNo ratings yet
- Nama: Desi Indah Sari NIM: 22010117130139 Kelas: CDocument2 pagesNama: Desi Indah Sari NIM: 22010117130139 Kelas: CSariNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 12: NeurologyFrom EverandComplementary and Alternative Medical Lab Testing Part 12: NeurologyNo ratings yet
- P E - Q1-FinalDocument23 pagesP E - Q1-FinalXanderz McBitzNo ratings yet
- Lipoprotein - WikipediaDocument38 pagesLipoprotein - WikipediaTejaswiNo ratings yet
- WEF New Frontiers of Nutrition 2023Document44 pagesWEF New Frontiers of Nutrition 2023Lorena BelloNo ratings yet
- ChlostrolDocument17 pagesChlostrolPooja RanaNo ratings yet
- Basic Principles of GeneticsDocument3 pagesBasic Principles of GeneticsKuoRosalineNo ratings yet
- Jim Sheppard Standard PDFDocument2 pagesJim Sheppard Standard PDFMarco LifemedicsNo ratings yet
- Vegetarian Diets For Children: Right From The StartDocument5 pagesVegetarian Diets For Children: Right From The StartVegan Future100% (5)
- Diabetes Healing SuperfoodsDocument48 pagesDiabetes Healing SuperfoodsTrueVa1ue100% (5)
- ACTIVITY 1: Nursing Care PlanDocument4 pagesACTIVITY 1: Nursing Care PlanChelsea JardelezaNo ratings yet
- Siridhanya Product DetailsDocument22 pagesSiridhanya Product DetailsdileephclNo ratings yet
- Manila Police District (MPD) As of January 2022: Action PNCO, DSTU OIC, Training Section C, DPRMDDocument15 pagesManila Police District (MPD) As of January 2022: Action PNCO, DSTU OIC, Training Section C, DPRMDShan Dave TupasNo ratings yet
- Every Day Nutritionvs Game Day NutritionDocument2 pagesEvery Day Nutritionvs Game Day Nutritionmarin0410No ratings yet
- 12 BibliographyDocument10 pages12 BibliographyPraveena.RNo ratings yet
- Essay 3 BrionesDocument7 pagesEssay 3 Brionesapi-704703402No ratings yet
- Individual Bmi Monitoring FormDocument2 pagesIndividual Bmi Monitoring FormFredimar PatarayNo ratings yet
- Biochemsitry 3304 Midterm 3 - KeyDocument12 pagesBiochemsitry 3304 Midterm 3 - Keyabelopez12No ratings yet
- CenovnikDocument14 pagesCenovnikMozzart SuplementiNo ratings yet
- ChrisPowell SmartFoodsListDocument1 pageChrisPowell SmartFoodsListOum El Ghoul100% (3)
- LANTUS XR Label InformationDocument17 pagesLANTUS XR Label InformationMichaelJonatanNo ratings yet
- Reading Test 2 - Diseases of AffluenceDocument9 pagesReading Test 2 - Diseases of AffluenceOlive GroupNo ratings yet
- Sivakumar Etal 2009Document8 pagesSivakumar Etal 2009mosman5No ratings yet
- Jurnal HipertensiDocument10 pagesJurnal HipertensiUtrihandayaniNo ratings yet
- The of By: Detection Lactose and Maltose Means of MethylamineDocument3 pagesThe of By: Detection Lactose and Maltose Means of MethylamineŠĭlệncěIšmyPŕIdệNo ratings yet
- Stacey Luneke ResearchfinalDocument9 pagesStacey Luneke Researchfinalapi-309088550No ratings yet
- Consistent Carbohydrate Diet For Diabetes MellitusDocument1 pageConsistent Carbohydrate Diet For Diabetes MellitusMuneca IbanezNo ratings yet
- So What Is Juvenile DiabetesDocument6 pagesSo What Is Juvenile Diabetesapi-274083684No ratings yet
- Physical Activity and Resting Metabolic Rate: John R. Speakman and Colin SelmanDocument14 pagesPhysical Activity and Resting Metabolic Rate: John R. Speakman and Colin SelmanPejvak KHorram DinNo ratings yet
- 09 October 2019 CNADocument17 pages09 October 2019 CNAMohit KumarNo ratings yet
- ActivityDocument1 pageActivityEvans Christian Rosal-OfficialNo ratings yet