Professional Documents
Culture Documents
tmpA9F9 TMP
tmpA9F9 TMP
Uploaded by
FrontiersOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
tmpA9F9 TMP
tmpA9F9 TMP
Uploaded by
FrontiersCopyright:
Available Formats
Open Access
Original Article
Primary effects of intravitreal bevacizumab in
patients with diabetic macular edema
Iftikhar-ul-Haq Tareen1, Azizur Rahman2,
P.S Mahar3, Muhammad Saleh Memon4
ABSTRACT
Objective: To evaluate the efficacy of primary intra vitreal bevacizumab (IVB) injection on macular edema
in diabetic patients with improvement in best corrected visual acuity (BCVA) and central macular thickness
(CMT) on optical coherence tomography (OCT).
Methods: This prospective interventional case series study was conducted at Retina Clinic, Al-Ibrahim Eye
Hospital, and Isra Postgraduate Institute of Ophthalmology Karachi. Between December 2010 to June 2012.
BCVA measurement with Early Treatment in Diabetic Retinopathy Study (ETDRS) charts and ophthalmic
examination, including Slit-lamp bio microscopy, indirect ophthalmoscopy, Fundus fluorescein angiography
(FFA) and OCT were done at the base line examination. At monthly interval all patients were treated with
3 injections of 0.05 ml intra vitreal injection containing 1.25 mg bevacizumab. Patients were followed up
for 6 months and BCVA and OCT were taken at the final visit at 6 month.
Results: The mean BCVA at base line was 0.420.14 Log Mar units. This improved to 0.340.13, 0.250.12,
0.170.12 and 0.160.14 Log Mar units at 1 month after 1st, 2nd 3rd injections and at final visit at 6 months
respectively, a difference that was statistically significant (P > 0.0001) from base line. The mean 1mm CMT
measurement was 452.9 143.1 m at base line, improving to 279.8 65.2 m (P < 0.0001) on final visit.
No serious complications were observed.
Conclusions: Primary IVB at a dose of 1.25 mg on monthly interval seems to provide stability and
improvement in BCVA and CMT in patient with DME.
KEY WORDS: Best Corrected Visual Acuity (BCVA), Central Macular Thickness (CMT), Diabetic Macular
Edema (DME), Intra Vitreal Bevacizumab (IVB).
doi: http://dx.doi.org/10.12669/pjms.294.3735
How to cite this:
Tareen IH, Rahman A, Mahar PS, Memon MS. Primary effects of intravitreal bevacizumab in patients with diabetic macular edema.
Pak J Med Sci 2013;29(4):1018-1022. doi: http://dx.doi.org/10.12669/pjms.294.3735
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0),
which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
1.
2.
3.
4.
1-4:
INTRODUCTION
Dr. Iftikhar-ul-Haq Tareen, FCPS,
Prof. Azizur Rahman, MCPS, FCPS,
Prof. P.S Mahar, FRCS, FRCOphth,
Prof. Muhammad Saleh Memon, DO, FRCS,
Al-Ibrahim Eye Hospital,
Isra Postgraduate Institute of Ophthalmology,
Karachi - Pakistan.
With the increasing prevalence of diabetes in the
world wide, Diabetic retinopathy (DR) remains the
major threat to sight in the working-age population.
It remains as a major cause of blindness in developing
countries.1 According to the Diabetic Association of
Pakistan World Health Organization (DAP-WHO)
survey (1994-1998), overall prevalence of Diabetes
is 11.47% in Pakistani population.2 Another study
has revealed that 25% of those patients, that present
to the health care facilities in Pakistan with diabetes
suffered from retinal complications.3 The Wisconsin
study4 reported that 9% of diabetic population had
macular edema with in 1 disc diameter of the fovea.
Correspondence:
Dr. Iftikhar Tareen,
House No. 1, Street 5, Faisal Town,
Brewery Road,
Quetta, Pakistan.
E-mail: iftikhartareen@yahoo.com
*
*
*
*
Received for Publication:
April 22, 2013
1st Revision Received:
May 13, 2013
2nd Revision Received:
June 7, 2013
Final Revision Accepted:*
June 9, 2013
1018 Pak J Med Sci 2013 Vol. 29 No. 4
www.pjms.com.pk
Primary effects of IVB in DME
A study carried out at Al Ibrahim Eye Hospital
(2011) showed that 39.8% of patients registered at
retinal clinic were suffering from DR, out of which
45% were having Clinically Significant Macular
Edema (CSME).5
Retinal hypoxia is the primary cause of DR which
increases the expression of vascular endothelial
growth factor (VEGF). It is an endothelial cellspecific mitogen which induces angiogenesis
and increase vascular permeability by affecting
endothelial tight-junction protein.6 In ocular
vascular disease such as DME, VEGF levels has
been found considerably higher in macular region.7
The Early Treatment Diabetic Retinopathy (ETDRS)
shows 3-year risk of moderate visual loss due to
macular edema was 32%, and focal macular laser
photocoagulation was effective in the treatment of
DME. ETDRS demonstrated that immediate focal
laser photocoagulation reduced the risk of moderate
visual loss by 50% (from 24% to 12%, 3 year after
initiation of treatment). However, 12% of treated
eyes still lost 15 ETDRS letters at 3-year followup interval. Furthermore, only 3% of laser-treated
eyes experienced a gain of 3 lines of vision.8 The
failure of laser photocoagulation in these eyes has
prompted interest in other treatment modalities
such as Anti-VEGF agents9, intravitreal triemcinolon
acetonide (IVTA),10 pars plana vitrectomy (PPV)11
or treatment with protein Kinase C inhibitors.12
Food and Drug Administration (FDA) has
approved bevacizumab (Avastin, Genentech
Inc. South San Francisco, CA, USA) a fusion
protein with human antibody backbone against
VEGF, it binds and inhibits all the active forms of
VEGF and is used in the treatment of metastatic
colorectal cancer. Some studies had found it useful
in the reduction of macular edema secondary to
central retinal vein Occlusion (CRVO),13 vascular
permeability and neovascularization secondary to
age-related macular degeneration (AMD).14
The purpose of this study was to evaluate the
best corrected visual acuity (BCVA) measured on
ETDRS chart and central macular thickness (CMT)
carried out on optical coherence tomography (OCT)
after a series of 3 injection of IVB at interval of one
month and at mean follow up of 6 months after 1st
injection.
METHODS
All patients were followed up for 6 months.
Approval of the study was obtained from the
institutional ethical committee, and informed
consent was obtained from all patients. The
study followed the principles of Declaration of
Helsinki.
Patients with evidence of DME were included
in this study. DME is defined as the evidence
of diffuse retinal thickening, hard exudates
(with out a circinate ring pattern) involving
the center of the macula (clinically significant
diabetic macular edema as defined by ETDRS),
or both and Diffuse fluorescin leakage involving
the center of the macula on FFA, and Central
Macular Thickening (CMT) on Optical Coherence
Tomography (OCT).
The exclusion criteria included patients with
DME who had been treated previously with laser
photocoagulation, intra vitreal triamcinolone or
any Anti-VEGF therapy elsewhere. The patients
with Macular ischemia, uncontrolled intraocular
pressure, intra ocular surgery within past 6 months,
history of vitreo retinal surgery of the study
eye, or any evidence of epiretinal membrane or
vitreomacular traction were excluded.
After detailed history each patient underwent
baseline examination which included BCVA measurement with ETDRS charts and ophthalmic examination, including slit lamp bio microscopy and dilated fundus examination with +90 diopter lens and
indirect ophthalmoscopy. All patients had fundus
fluorescien angiography (FFA).Baseline CMT was
analyzed by OCT using 6 diagonal slow 6mm radial
line scan on Topcon analyzer (Tokyo, Japan).
Procedure: All eyes had several drops of local
anesthetic (Alcaine Alcon, Belgium) with dilatation
of pupil (Mydriacyl 1% - Alcon, Belgium) before
the procedure. After the eye had been prepped in
standard fashion using 5% povidoniodine, an eye
lid speculum was used to stabilize the eyelids and
the injection of 1.25 mg (0.05 ml), bevacizumab was
performed at 3.5 to 4mm posterior to the limbus
through the inferiotemporal pars plana with a
tuberculin syringe and 30 gauge needle After
injection, retinal artery perfusion was checked
with the indirect ophthalmoscopy. A single drop of
antibiotic (Vigamox Alcon, Belgium) is instilled
and patients were instructed to administer topical
antibiotics for one week.
All patients were examined at one week and
one month after the first injection. At 1st month
visit BCVA was recorded and 2nd injection was
administered and the same was repeated after one
month and the 3rd injection was administered .The
patients were followed-up for 6 months and final
Pak J Med Sci 2013 Vol. 29 No. 4
www.pjms.com.pk 1019
Iftikhar-ul-Haq Tareen et al.
Table-I: Mean Log Mar value for the BCVA 1 month
after each injection & at 6 month follow up examination.
BCVA
Mean Log
Std
Snellen
Mar Unit Deviation equivalent
At baseline
0.42
0.14
20/50
After 1st injection
0.34
0.13
20/40
After 2nd injection
0.25
0.12
20/30
After 3rd injection
0.17
0.12
20/25
At 6 month Follow up
0.16
0.14
20/25
BCVA and CMT were taken at the final visit at 6
month after the first injection.
RESULTS
A total of 49 diabetic patients were enrolled in this
study. Seven of our patients were lost the follow-up
or were excluded due to exclusion criteria from the
study. The final data of 78 eyes of 42 patients with
a minimum follow up of 6 months after 1st injection
of bevacizumab were included for analysis. The
patients had a mean age of 53.5 11.4 years, and
25(59.52%) were male, 17(40.47%) were female.
Within one month after the initial bevacizumab
injection improvements in BCVA were observed,
and these significant changes continued throughout
the 6 months follow up period. The mean BCVA at
baseline was 0.42 0.14 Log Mar units. At one month
after the 1st injection BCVA improved to 0.340.13
Log Mar unit, a difference that was statistically
significant (P<0.0001). This improvement in BCVA
was maintained after 2nd and 3rd injections which
were 0.250.12 Log Mar units and 0.170.12 Log Mar
units respectively. In addition the mean BCVA at 6
month follow up examination was 20/25 (0.160.14
Log Mar units), a statistically significant difference
from baseline BCVA (P<0.0001).(Table-I)
Further subgroups analysis demonstrated that
after 1st injection, 49(62.8%) eyes improved one or
more ETDRS line of BCVA,27(34.6%) eyes remained
stable and 2(2.5%) decreased one or more ETDRS
lines of BCVA. This trend continued after 2nd and
3rd injection, and at 6 month follow up examination,
16(20.5%) eyes remained stable, 57(73.0%) eyes
improved one or more ETDRS lines and 5(6.4%)
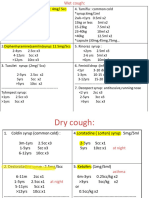
Fig.1: Optical Coherence tomography (OCT) imaging of a
52 years old diabetic male with a history of loss of vision
in both eyes to 20/160, Right eye (a) Left eye (b), in which
diabetic macular edema had developed. The OCT shows
a marked resolution in macular edema and improvement
of Central Macular Thickness (CMT) after treatment.
eyes had decreased one or more ETDRS lines of
BCVA. (Table-II)
Optical Coherence tomography results were
available for all 78 eyes at baseline and at 6 months
follow up examination. At baseline the mean
1-mm CMT measurements was 452.9143.1 m,
improving to 279.865.2 m at 6 month follow up
examination, which was significantly different from
baseline (P<0.0001).(Fig.1)
A mild anterior chamber cellular reaction was
observed in 9 (11.5%) eyes, but the condition
improved with use of topical corticosteroid and
antibiotic combination drops (Tobradex Alcon,
Belgium). No other injection or drug related
complications were observed.
DISCUSSION
This study reports on 78 consecutive eyes with
DME treated with Intravitreal Bevacizumab,
which resulted in both anatomic and functional
improvement. In most of patients improvement of
Table-II: Best Corrected Visual Acuity (BCVA) analysis by subgroups (78 eyes).
After 1st Injection
No of eyes Percentage No of eyes Percentage No of eyes Percentage No of eyes Percentage
Improved 1 ETDRS lines
Remained stable
Decreased 1 ETDRS lines
49
27
2
1020 Pak J Med Sci 2013 Vol. 29 No. 4
62.8%
34.6%
2.5%
After 2nd Injection
53
22
3
www.pjms.com.pk
67.9%
28.2%
3.8%
After 3rd injection
54
21
3
69.2%
26.9%
3.8%
At 6 month follow up
57
16
5
73.0%
20.5%
6.4%
Primary effects of IVB in DME
Fig.2: Changes in best corrected visual acuity (BCVA) after
intravitrealbevacizumab (IVB). BCVA improved after 1st
injection from 0.42 Log Mar (baseline) to 0.34 Log Mar, a
difference that was statistically significant (P<.0001), this
improvement of BCVA was maintained throughout after
2nd and 3rd injections and final visit at 6 months.
BCVA were detected with in the first month after
the 1st injection and continued throughout the study
period. (Fig.2)
The
exact
pathophysiologic
mechanism
responsible for DME remains uncertain, retinal
hypoxia and various rheological disturbances play
a role in the disruption of the inner blood-retinal
barrier associated with metabolic alterations.6
The long term circulatory disturbance may lead
to functional vascular obstruction, relative retinal
ischemia, and release of cytokines such as VEGF.
Funatsuet al7 reported that level of VEGF was
elevated in vitreous fluid of subjects with DME.
VEGF causes conformational changes in the tight
junctions of retinal endothelium and plays a major
role in increasing vascular permeability in the
progression of DME.
Several treatment methods for DME are under
investigation. ETDRS has demonstrated that, the
risk of visual loss from DME can be reduced by laser
photocoagulation.8 However, in some eyes macular
edema may persist despite laser photocoagulation.
Therefore clinicians had developed interests in
other treatment methods such as pharmacologic
therapies. Intravitreal triamicinilone acetonide
(IVTA) injection has some promising results but
this treatment modality is not without its risks and
complication.10 These complications were related
to the injection procedure or to the corticosteroid
suspension.15 Oral protein Kinase C inhibitors had
demonstrated efficacy in prevention of visual loss
from DME.12 Currently Fluocinolon Acetonide
vitreous inserts are under investigations showing
some promising results.16
The important role of VEGF in the breakdown of
the blood-retinal barrier and vascular permeability
resulting in retinal edema is clear. Therefore, the
rationale for use of anti-VEGF agents for treatment
of DME is significant. Bevacizumab (Avastin;
Genentech, Inc) is a fusion protein with human
antibody backbone that binds to all sub types of
VEGF and used successfully in tumor therapy as a
systemic drug. Recently off label use of IVB injection
has been presented in small cohorts of patients with
macular edema from various causes like CRVO13,
AMD14 and Proliferative Diabetic Retinopathy
(PDR).17 As VEGF disrupts the inner blood-retinal
barrier and causes exravasation of fluids by
affecting endothelial tight junctions. Therefore,
VEGF inhibition by IVB has been emerged as a
target molecule for the treatment of DME.
There are several studies in the literature on the
intravitreal administration of anti-VEGF for DME.
Recently Khan et al18 published a report of 26 eyes,
followed up for 3 months after IVB injection. The
mean BCVA at baseline 0.726 Log Mar was improved
to 0.452 Log Mar at 3rd month. Flourescien leakage
stopped in 25 (96.15%) eyes. Kumar and Sinah19
reported results of 20 eyes with DDME treated with
IVB at a dose of 1.25mg that had not responded to
previous photocoagulation. They concluded that
IVB resulted in a significant decrease in macular
thickness and improvement in BCVA at 3 month.
Ozkiris A20 presented results of 30 eyes, out of
which 24 (80%) eyes showed increased visual acuity
after mean, follow up time of 5.6 months after IVB
injection. BCVA improved from 1.090.23 Log Mar
(at baseline) to 0.900.17 Log Mar at 1st month and
0.770.26 Log Mar at the last visit. The mean edema
map values significantly decreased by 33.3%.
Arevalo et al21 published a report of 24-month
anatomic and visual acuity response after primary
intravitreal bevacizumab in patients with Diffuse
Diabetic Macular Edema (DDME). They compared
2 different doses of intravitreal bevacizumab,
1.25mg and 2.5 mg respectively. They found that
primary IVB at doses of 1.25 or 2.5 mg seem to
provide stability and improvement in BCVA, OCT,
and FA results in DME at 24 months.
The results of our study compare favorably with
these reports and confirm their findings. In our
study, we found that improvement in BCVA was
achieved within a month after 1st IVB injection.
A further improvement was achieved after each
injection of bevacizumab and was maintained at 6
months follow up. BCVA in our study improved
from 0.420.14 Log Mar unit at base line to mean
Pak J Med Sci 2013 Vol. 29 No. 4
www.pjms.com.pk 1021
Iftikhar-ul-Haq Tareen et al.
0.340.13 Log Mar unit after one month of 1st IVB
injection and further improvement to 0.250.12
Log Mar unit after one month of 2nd injection and
this trend continued to the final visit at 6 month
with BCVA improving to 0.160.14 Log Mar unit.
The mean central 1mm CMT improved from
452.9143.1 m at base line to 279.865.2 m at 6
month visit. This confirms the finding of previous
studies which shows that the eyes with DME treated
with IVB result in both anatomic and functional
improvement.
The results of our and other above mentioned
studies indicate that IVB injection may have a
beneficial effect on macular thickness and BCVA
in DME. In future this new treatment method
may replace or compliment focal or grid laser
photocoagulation.
Our study has some limitations. First, the follow
up time was relatively short, but visual and
anatomical responses were apparent during the
follow-up time. Second, there is no control group
in this study as randomization was not possible.
Third, this study was carried out in a single center
so results cannot be generalized.
CONCLUSION
This study demonstrated that IVB injection
is an effective approach with promising results
for the primary treatment of DME. IVB at a dose
of 1.25mg on at least monthly interval seems to
provide stability and improvement in BCVA and
CMT in DME at 6 moths. However evaluation in
a multicenter, randomized, controlled clinical trial
comparing IVB with other treatment modalities is
needed to evaluate the safety and efficacy of this
treatment method.
Conflict of Interest: The authors have no conflict
of interest and is not supported or funded by any
Drug company or any other source.
REFERENCES
1.
Zimmet P, Alberti KG, Shaw J. Global and social implication of the
diabetes epidemic. Nature. 2001;414:782-787. doi:10:1038/414782a.
2. Iqbal F, Naz R. Patterns of diabetes mellitus in Pakistan: An
overview of the problem. Pak J Med Res. 2005;44:86-89.
3. Khan AJ. Prevalence of diabetic retinopathy in Pakistani Subjects:
A pilot study. J Pak Med Assoc. 2004;54:60-66.
4. Klein R, Klein BE, Moss SE, Mathew DD, DcMet DL, et al. the
Wisconsin Epidemiologic Study of Diabetic retinopathy. iv.
Diabetic macular edema. Ophthalmology. 1984;91:1464-1474.
PMID: 6521986
5. Khan A, Qidwai U. Frequency and patterns of eye diseases in
retina clinic of a tertiary care hospital in Karachi. Pak J Ophthalmol.
2011;27:155-159.
6. Ferrara N. Vascular endothelial growth factor: basic science and
clinical progress. Endocrine Review. 2004;25:581-611. doi: 10.1210/
er.2003-0027
1022 Pak J Med Sci 2013 Vol. 29 No. 4
www.pjms.com.pk
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
Funatsu H, Yamashita H, Sakata k, Noma H, Mimura T, Suzuki
M, et al. Vitreaous levels of vascular endothelial growth factor
and intracellular adhesion molecule 1 are related to diabetic
macular edema. Ophthalmology. 2005;112:806-816. doi:10.1016/j.
ophtha.2004.11.045.
Early Treatment Diabetic Retinopathy Study Research Group.
Treatment technique and clinical guidelines for photocoagulation
of diabetic macular edema; Early Treatment Diabetic Retinopathy
Study report No 2. Ophthalmology. 1987;94:761-774.
Heritoglou C, Kook D, Neubauer A, Wolf A, Priglinger S, Strauss
R, et al. Intravitreal bevacizumab (Avastin) therapy for persistent
diffuse diabetic macular edema. Retina. 2006;26:999-1005.
Gillies MC, Sutter FK, Simppson JM, Simpson JM, Larsson J, Ali
H, et al. Itravitreal triamcinolon for refractory diabetic macular
edema: tow-year results of a double-masked, placebo-controlled,
randomized clinical trial. Ophthalmology. 2006;113:1533-1538.
doi:101016/j.ophtha.2006.02.065.
Pendergast SD, Hussan TS, William GA, Cox MS, Margherio
RR, Ferrone PJ, et al. Vitrectomy for diffuse diabetic macular
edema associated with a taut premacular posterior hyloid. Am J
Ophtalmol. 2000;130:178-186.
Campochiaro PA, C99-PKC412-003 Study Group. Reduction of
diabetic macular edema by oral administration of the Protein
Kinase C inhibitor PKC 412. Invest Ohthalmol Vis Sci. 2004;45:922931. doi:10.1167/ivos.03-0955
Thapa R, Poudyal G. Short term results of Intravitreal bevacizumab
for the treatment of macular edema secondary to retinal vein
occlusion. Nepal J Ophthalmol. 2013;5:63-68. doi.org/10.3126/
nepjop.v5il.7824.
Robert L, Avery MD, Dante J, Reramici MD, Melvin D, Rabena BS,
et al. Intravitreal bevacizumab (Avastin) for neovascular AgeRelated Macular Degeneration. Ophthalmology. 2006;113:363-372.
doi:10.1016/j.optha.2005.11.019.
Ozkiris A, Erkilic K. Complication of intravitreal injection of
triamcinolone acetonide. Can J Ophthalmol. 2005;40:63-68.
doi:10.1038/eye.2008.40.
Campochiaro PA, Brown DM, Pearson A, Chen S, Boyer D,
Morono JR, et al. Sustained
delivery fluocinolone Acetonide
vitreous inserts provide benefit for at least 3 years in patients with
Diabetic macular edema. Ophthalmology. 2012:119:2125-2132.
doi:10.1016/j.ophtha.2012.04.030
Avery RL, Pearlman J, Pieramici DJ. Intravitreal bevacizumab
(Avastin) in the treatment of proliferative diabetic retinopathy.
Ophthalmology. 2006;113:1695-1705.
Khan A, Amir AC, Zahid C. Intravitreal bevacizumab for treatment
of diabetic macular edema. Pak J Ophthalmol. 2012;28:3-9.
Kumar A, SinahS. Intravitreal bevacizumab (Avastin) treatment of
diffuse diabetic macular edema in an Indian population. Indian J
Ophthalmol. 2007;55:451-455.
Ozkiris A. Intravitrel bevacizumab (Avastin) for primary treatment
of diabetic macular edema. Eye. 2009;23:616-620. doi:10.1038/
eye.2008.40.
Arevalo JF, Fromow G, Quiroz MH, Sanchez JG, wu L, Maia M,
et al. Pan-American collaborative Retina Study Group. Primary
intravitreal bevacizumab (Avastin) for diabetic macular edema:
results from Pan-American Collaborative Retina Study group at
24 months. Ophthalmology. 2009;116:1488-1497. doi:10.1016/j.
ophtha.2009.03.016.
Authors Contribution:
IT: Conceived and designed the protocol, did
data collection and statistical analysis, manuscript
writing and editing.
AR: was involved in clinical management of
patients.
P.SM and SM: Critically reviewed the manuscript
for final publication.
You might also like
- ABSTRACT - BOOK - 10th IcgsDocument135 pagesABSTRACT - BOOK - 10th Icgsd_kourkoutasNo ratings yet
- Retina Clinica Trials Update - 0813 - Supp2Document16 pagesRetina Clinica Trials Update - 0813 - Supp2cmirceaNo ratings yet
- Well Being: Striving For Good Health in Tribal CommunitiesDocument39 pagesWell Being: Striving For Good Health in Tribal CommunitiesRose Weeks100% (1)
- PDFDocument367 pagesPDFBenazir Amrinnisa YusufNo ratings yet
- A Collaborative Retrospective Study On The Efficacy and Safety of Intravitreal Dexamethasone Implant (Ozurdex) in Patients With Diabetic Macular EdemaDocument17 pagesA Collaborative Retrospective Study On The Efficacy and Safety of Intravitreal Dexamethasone Implant (Ozurdex) in Patients With Diabetic Macular EdemaJosé Díaz OficialNo ratings yet
- Comparison of Intravitreal Bevacizumab (Avastin) With Triamcinolone For Treatment of Diffused Diabetic Macular Edema: A Prospective Randomized StudyDocument9 pagesComparison of Intravitreal Bevacizumab (Avastin) With Triamcinolone For Treatment of Diffused Diabetic Macular Edema: A Prospective Randomized StudyBaru Chandrasekhar RaoNo ratings yet
- Ischemia Modified Albumin As A Useful Marker For Diagnoses and Management of Diabetic RetinopathyDocument5 pagesIschemia Modified Albumin As A Useful Marker For Diagnoses and Management of Diabetic RetinopathyMarcellia AngelinaNo ratings yet
- Vukicevic Et Al 2021 Wfksizpmfaet PDFDocument5 pagesVukicevic Et Al 2021 Wfksizpmfaet PDFMeri VukicevicNo ratings yet
- MataDocument5 pagesMatavikrizkaNo ratings yet
- Review Article JhaveriDocument2 pagesReview Article JhaveriNikhilNo ratings yet
- Uveitis 3Document12 pagesUveitis 3srihandayaniakbarNo ratings yet
- Intraocular Pressure-Lowering Efficacy and Safety of Bimatoprost 0.03% Therapy For Primary Open-Angle Glaucoma and Ocular Hypertension Patients in ChinaDocument9 pagesIntraocular Pressure-Lowering Efficacy and Safety of Bimatoprost 0.03% Therapy For Primary Open-Angle Glaucoma and Ocular Hypertension Patients in ChinaAyu Ersya WindiraNo ratings yet
- tmpF7AC TMPDocument4 pagestmpF7AC TMPFrontiersNo ratings yet
- Retina 2012 Sep 32 (Suppl 2) S225-31Document7 pagesRetina 2012 Sep 32 (Suppl 2) S225-31roro207No ratings yet
- Clinical Science Efficacy and Safety of Trabeculectomy With Mitomycin C For Childhood Glaucoma: A Study of Results With Long-Term Follow-UpDocument6 pagesClinical Science Efficacy and Safety of Trabeculectomy With Mitomycin C For Childhood Glaucoma: A Study of Results With Long-Term Follow-UphusnioneNo ratings yet
- Comparing The Ef Ficacy of Bevacizumab and Ranibizumab in Patients With Diabetic Macular Edema (BRDME) The BRDME Study, A Randomized TrialDocument12 pagesComparing The Ef Ficacy of Bevacizumab and Ranibizumab in Patients With Diabetic Macular Edema (BRDME) The BRDME Study, A Randomized Trialkoas mataNo ratings yet
- Ahmadieh 2007Document7 pagesAhmadieh 2007Ruby KumarNo ratings yet
- MainDocument7 pagesMainiSee ClinicNo ratings yet
- None 3Document11 pagesNone 3Yehiel FlaviusNo ratings yet
- Intravitreal Bevacizumab (Avastin) Therapy For Persistent Diffuse Diabetic Macular EdemaDocument7 pagesIntravitreal Bevacizumab (Avastin) Therapy For Persistent Diffuse Diabetic Macular EdemaJose Antonio Fuentes VegaNo ratings yet
- tmp1BE0 TMPDocument4 pagestmp1BE0 TMPFrontiersNo ratings yet
- Lutfi-Full Paper-Pit 2024Document6 pagesLutfi-Full Paper-Pit 2024Lutfi MaulanaNo ratings yet
- Rise and Ride - 2012Document13 pagesRise and Ride - 2012Alv JDNo ratings yet
- 1 s2.0 S2667376223000148 MainDocument7 pages1 s2.0 S2667376223000148 MainviramonicaNo ratings yet
- 14 FullDocument7 pages14 FullalexanderplNo ratings yet
- Aflibercept Monotherapy or Bevacizumab First For Diabetic Macular EdemaDocument12 pagesAflibercept Monotherapy or Bevacizumab First For Diabetic Macular EdemaLee Foo WengNo ratings yet
- PTVT Gedde2019Document13 pagesPTVT Gedde2019Ahmed NahrawyNo ratings yet
- BMC OphthalmologyDocument7 pagesBMC OphthalmologyRizki Yuniar WNo ratings yet
- Presentación Edema Macular DiabéticoDocument26 pagesPresentación Edema Macular Diabéticomauricio bayramNo ratings yet
- Jurnal Anti VEFGDocument9 pagesJurnal Anti VEFGFitria Sirr Mu'thiarohmahNo ratings yet
- 2023 Article 740Document13 pages2023 Article 740francescoNo ratings yet
- IBEPE StudyDocument8 pagesIBEPE StudyKaran KumarswamyNo ratings yet
- Pio y AntivegfDocument14 pagesPio y AntivegfBernardo RomeroNo ratings yet
- Corticosteroids For Bacterial Keratitis - The Steroids For Corneal Ulcers Trial (SCUT)Document8 pagesCorticosteroids For Bacterial Keratitis - The Steroids For Corneal Ulcers Trial (SCUT)Bela Bagus SetiawanNo ratings yet
- 015 7851Document6 pages015 7851dradnanahmad82No ratings yet
- Piis0161642014000712 PDFDocument8 pagesPiis0161642014000712 PDFZhakiAlAsrorNo ratings yet
- Analysis of Intraoperative and Postoperative Complications in Pseudoexfoliation Eyes Undergoing Cataract SurgeryDocument4 pagesAnalysis of Intraoperative and Postoperative Complications in Pseudoexfoliation Eyes Undergoing Cataract SurgerymathyasthanamaNo ratings yet
- Usa, 2002Document8 pagesUsa, 2002Maha OmarNo ratings yet
- MataDocument16 pagesMataIslah NadilaNo ratings yet
- Jurnal Reading DR Sofi SiapDocument28 pagesJurnal Reading DR Sofi SiapBima Bayu PutraNo ratings yet
- PJMS 32 1229Document5 pagesPJMS 32 1229Nurvita WidyastutiNo ratings yet
- BR J Ophthalmol 2016 Straub Bjophthalmol 2015 306930Document5 pagesBR J Ophthalmol 2016 Straub Bjophthalmol 2015 306930BillGhoes'toNo ratings yet
- Jurnal Mata 5 KEVIN PDFDocument10 pagesJurnal Mata 5 KEVIN PDFKevinNo ratings yet
- Facoemulsifucacion + Stent TrabecularDocument8 pagesFacoemulsifucacion + Stent TrabecularCarlos VerdiNo ratings yet
- Tugas Akademik 13-Journal Reading 4-Glaukoma-Galuh Yulieta - 240215 - 072026Document8 pagesTugas Akademik 13-Journal Reading 4-Glaukoma-Galuh Yulieta - 240215 - 072026Arina SetyaningrumNo ratings yet
- Combined Intravitreal Ranibizumab and Verteporfin Photodynamic Therapy Versus Ranibizumab Alone For The Treatment of Age-Related Macular DegenerationDocument5 pagesCombined Intravitreal Ranibizumab and Verteporfin Photodynamic Therapy Versus Ranibizumab Alone For The Treatment of Age-Related Macular Degeneration568563No ratings yet
- Retina 39 426Document9 pagesRetina 39 426ryaalwiNo ratings yet
- Jurnal 4Document8 pagesJurnal 4Putri kartiniNo ratings yet
- Journal ReadingDocument21 pagesJournal ReadingRettyNo ratings yet
- Steroid Induced Ocular Hypertension Following Myopic Photorefractive KeratectomyDocument5 pagesSteroid Induced Ocular Hypertension Following Myopic Photorefractive KeratectomyMaria Angelina BunawanNo ratings yet
- Rhegmatogenous Retinal DetachmentDocument6 pagesRhegmatogenous Retinal DetachmentPutri kartiniNo ratings yet
- Rhegmatogenous Retinal DetachmentDocument6 pagesRhegmatogenous Retinal DetachmentPutri kartiniNo ratings yet
- Jurnal EED 6Document10 pagesJurnal EED 6Garsa GarnolNo ratings yet
- LimitedDocument2 pagesLimitedlfathiyahNo ratings yet
- The Effect of Trabeculectomy On Cataract Formation or ProgressionDocument6 pagesThe Effect of Trabeculectomy On Cataract Formation or ProgressionGina Nadia HastarinNo ratings yet
- 050906A Nurse Led Approach To Diabetic Retinal Screening 2Document3 pages050906A Nurse Led Approach To Diabetic Retinal Screening 2anisarahma718No ratings yet
- 8th JC Paper - Un Et Al. Effect of Mirabegron On Intraocular Pressure in Patients With Glaucoma. Journal of Urological Surgery. 2020Document5 pages8th JC Paper - Un Et Al. Effect of Mirabegron On Intraocular Pressure in Patients With Glaucoma. Journal of Urological Surgery. 2020Wai Kit CheongNo ratings yet
- Vitrectomy Results in Proliferative Diabetic RetinopathyDocument3 pagesVitrectomy Results in Proliferative Diabetic RetinopathyRohamonangan TheresiaNo ratings yet
- tmp5FAA TMPDocument4 pagestmp5FAA TMPFrontiersNo ratings yet
- Research ArticleDocument7 pagesResearch ArticlePhei Qing TjangNo ratings yet
- Lerner SFDocument9 pagesLerner SFAdriana FallaNo ratings yet
- Choroidal NeovascularizationFrom EverandChoroidal NeovascularizationJay ChhablaniNo ratings yet
- tmpF178 TMPDocument15 pagestmpF178 TMPFrontiersNo ratings yet
- Tmp1a96 TMPDocument80 pagesTmp1a96 TMPFrontiersNo ratings yet
- tmp998 TMPDocument9 pagestmp998 TMPFrontiersNo ratings yet
- tmpE3C0 TMPDocument17 pagestmpE3C0 TMPFrontiersNo ratings yet
- Tmpa077 TMPDocument15 pagesTmpa077 TMPFrontiersNo ratings yet
- tmp3656 TMPDocument14 pagestmp3656 TMPFrontiersNo ratings yet
- tmp27C1 TMPDocument5 pagestmp27C1 TMPFrontiersNo ratings yet
- tmpA7D0 TMPDocument9 pagestmpA7D0 TMPFrontiersNo ratings yet
- tmp96F2 TMPDocument4 pagestmp96F2 TMPFrontiersNo ratings yet
- tmp97C8 TMPDocument9 pagestmp97C8 TMPFrontiersNo ratings yet
- Buffer Enriched Mineral Lick For Summer Management in RuminantsDocument6 pagesBuffer Enriched Mineral Lick For Summer Management in RuminantsBharathidhasan SelvarasuNo ratings yet
- Psyche 100 ItemsDocument9 pagesPsyche 100 ItemsYaj CruzadaNo ratings yet
- Updated, 01.06.13 RESUME Prof - Tushar T.shelkeDocument9 pagesUpdated, 01.06.13 RESUME Prof - Tushar T.shelketushaarraj4933No ratings yet
- Paracetamol OverdoseDocument1 pageParacetamol OverdoseMilanisti22No ratings yet
- Laporan Pemakaian Obat HarianDocument21 pagesLaporan Pemakaian Obat Harianklinik dr NandoNo ratings yet
- Chapter 1 Foundation of Modern NursingDocument30 pagesChapter 1 Foundation of Modern Nursingteklay100% (2)
- Varcarolis Halter TherCommTechniqDocument5 pagesVarcarolis Halter TherCommTechniqeatthescrollNo ratings yet
- Vda de Canilang Vs CADocument3 pagesVda de Canilang Vs CARegine YuNo ratings yet
- RBDDocument31 pagesRBDAhmadNo ratings yet
- Phrases and Process For HypnosisDocument45 pagesPhrases and Process For HypnosisUmair UsmanNo ratings yet
- Evaluation of Hypoglycemia: & Insulin Autoimmune Syndrome (Hirata Disease)Document15 pagesEvaluation of Hypoglycemia: & Insulin Autoimmune Syndrome (Hirata Disease)Anonymous B3J9sWNo ratings yet
- Atrial Septal Defect PDFDocument4 pagesAtrial Septal Defect PDFTien Chen TuNo ratings yet
- Normal Erythrocyte1Document4 pagesNormal Erythrocyte1RonyArtoKapidaNo ratings yet
- Cruise Ship Safety ConcernsDocument4 pagesCruise Ship Safety ConcernsAnthony Tunying MantuhacNo ratings yet
- Health Centre Stgs - Federal Government of SomaliaDocument102 pagesHealth Centre Stgs - Federal Government of SomaliaAhmed MohamedNo ratings yet
- Outpatient Pediatric Doses by Zhino NajiDocument21 pagesOutpatient Pediatric Doses by Zhino Najiysjkvxcnk9No ratings yet
- Anaesthesia PDFDocument43 pagesAnaesthesia PDFP.G.R. PreethamNo ratings yet
- Ringer Asetat Pada AnakDocument72 pagesRinger Asetat Pada Anaknanda surastyo100% (1)
- Medical Administrative AssistantDocument2 pagesMedical Administrative Assistantapi-77740790No ratings yet
- Closed FOIA Log - October 2021Document120 pagesClosed FOIA Log - October 2021rikinNo ratings yet
- Chlosite LD 1647856024Document8 pagesChlosite LD 1647856024Mai ThúyNo ratings yet
- Factset Interview Questions PDFDocument2 pagesFactset Interview Questions PDFXzavion0% (1)
- BVM Global Bolleneni HillsideDocument23 pagesBVM Global Bolleneni HillsideVictor GhoshNo ratings yet
- Axcent Brochure Patient Monitoring 2018Document12 pagesAxcent Brochure Patient Monitoring 2018harrylukitoNo ratings yet
- Seminiferous TubuleDocument9 pagesSeminiferous TubuleOLASUNMBO OWOLABINo ratings yet
- Case Presentation Calalang General Hospital: Far Eastern University Institute of Nursing Summer 2009Document15 pagesCase Presentation Calalang General Hospital: Far Eastern University Institute of Nursing Summer 2009Bianca de GuzmanNo ratings yet
- LBP (Nyeri Pinggang) Peumonia: Puskesmas Darul Ihsan TAHUN: 2017Document11 pagesLBP (Nyeri Pinggang) Peumonia: Puskesmas Darul Ihsan TAHUN: 2017puskesmas darul ihsanNo ratings yet