Professional Documents
Culture Documents
Seizure: Soheila Zareifar, Hamid Reza Hosseinzadeh, Nader Cohan
Seizure: Soheila Zareifar, Hamid Reza Hosseinzadeh, Nader Cohan
Uploaded by
Firda PotterOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Seizure: Soheila Zareifar, Hamid Reza Hosseinzadeh, Nader Cohan
Seizure: Soheila Zareifar, Hamid Reza Hosseinzadeh, Nader Cohan
Uploaded by
Firda PotterCopyright:
Available Formats
Seizure 21 (2012) 603605
Contents lists available at SciVerse ScienceDirect
Seizure
journal homepage: www.elsevier.com/locate/yseiz
Association between iron status and febrile seizures in children
Soheila Zareifar *, Hamid Reza Hosseinzadeh, Nader Cohan
Hematology Research Center, Nemazee Hospital, Shiraz University of Medical Sciences, Shiraz, Iran
A R T I C L E I N F O
A B S T R A C T
Article history:
Received 20 September 2011
Received in revised form 16 June 2012
Accepted 18 June 2012
Objectives: The aim of this study was to determine the association between iron status and febrile
seizures in children aged 6 months to 5 years.
Methods: This prospective casecontrol study enrolled 300 children who presented with febrile seizures
(case group) and 200 children who presented with a febrile illness without seizures (control group) from
March 2007 to January 2009. Hemoglobin, mean corpuscular volume and serum ferritin concentration
were compared in the two groups in relation to age, sex and use of iron supplementation.
Results: Patients with febrile seizures were more frequently iron decient as dened by a serum ferritin
level below 20 ng/dl (56.6% vs. 24.8%, P = 0.0001). Mean hemoglobin concentration was 10.8 g/dl in the
control group and 11.7 g/dl in the case group (P < 0.05). The difference between groups in mean
corpuscular volume was not statistically signicant (75.5 vs. 74.4 , P < 0.130).
Conclusion: Low serum ferritin concentration and low iron status may be risk factors for the development
of febrile seizures.
2012 British Epilepsy Association. Published by Elsevier Ltd. All rights reserved.
Keywords:
Iron
Febrile seizure
Ferritin
Children
1. Introduction
Simple febrile seizures (SFSs) are the most common type of
seizure during childhood. The peak incidence is at the age of
approximately 18 months, occurring in 25% of all children.1
Because of their association with later epilepsy, many independent
risk factors (genetic factors, age, gender, fever, type and duration of
seizure, family and developmental history, multiple seizures,
perinatal exposure to antiretroviral drugs, history of maternal
smoking and alcohol consumption during pregnancy) have been
studied as potential predictors of recurrent febrile seizures.25
However, the data available in the literature are inconsistent.69
Iron plays a critical role in the metabolism of several
neurotransmitters, and in low iron status, aldehyde oxidases
and monoamine are reduced. In addition, the expression of
cytochrome C oxidase, a marker of neuronal metabolic activity, is
decreased in iron deciency.10 In developing countries, iron
deciency is one of the most prevalent nutritional problems,11
especially among infants aged between 6 and 24 months.1216 In
developing countries 4666% of all children under 4 years of age
are anemic, with half of the prevalence attributed to irondeciency anemia. Many studies have clearly demonstrated the
effect of iron on development, cognition, behavior and neurophysiology, and especially on brain metabolism, neurotransmitter
function and myelination.17 Iron-deciency anemia is common
* Corresponding author. Tel.: +98 7116473239; fax: +98 7116473239.
E-mail address: zareifars@sums.ac.ir (S. Zareifar).
during the second and third years of life and has been variably
associated with developmental and behavioral impairments,
hence it can inuence motor and cognitive skills.10,11 Because
iron is important for the function of various enzymes and
neurotransmitters in the central nervous system, low serum levels
of ferritin may lower the seizure threshold.18,19
We compared iron status in children with febrile seizures and a
control group in order to determine the relationship between iron
status and febrile seizures in pediatric patients in southern Iran.
2. Patients and methods
The study group consisted of 300 children with a rst febrile
seizure admitted to the pediatric emergency departments of Shiraz
University of Medical Sciences, Shiraz, southern Iran, between
March 2007 and January 2009. Written informed consent was
obtained from the parents of all patients for inclusion in the study,
which was approved by the Shiraz University of Medical Sciences
Ethics Committee. Simple febrile seizures were dened as seizure
occurring between the ages of 6 months and 5 years, associated
with a rectal temperature of at least 38.3 8C or an axillary
temperature of at least 37.8 8C documented either in the
emergency department or in the medical record, <15 min
duration, without evidence of central nervous system infection,
focal neurological signs or history of seizure, and occurring once in
the previous 24 h. The seizure was dened as complex if it lasted
>15 min, occurred more than once in 24 h or had focal features.
Children with developmental delay, denite neurological illness,
or a history of proved iron-deciency anemia, regular blood
1059-1311/$ see front matter 2012 British Epilepsy Association. Published by Elsevier Ltd. All rights reserved.
http://dx.doi.org/10.1016/j.seizure.2012.06.010
S. Zareifar et al. / Seizure 21 (2012) 603605
604
transfusion or regular therapeutic doses of iron supplements were
excluded. A control group (n = 200) was selected randomly from
children admitted for febrile illnesses such as gastroenteritis, otitis
media or respiratory tract infections without seizure, previous
history of seizure or anticonvulsant therapy. Case and control
groups were comparable for age, gender, normal growth and
development, family history of febrile seizures, temperature at
presentation, white blood cell count and differential, and use of
iron supplementation. Age, sex, underlying illness, frequency and
duration of seizures were recorded for both groups. Because
ferritin is an acute-phase reactant protein in inammatory and
infectious processes, serum ferritin (SF) concentration was
measured by ELISA and double-checked 72 h after the onset of
the febrile illness. Anemia was dened as a decrease in mean
hemoglobin (Hb) level below 2 standard deviations of the normal
values for age, i.e. Hb < 10.5 g/dl for ages 624 months and
<11.5 g/dl for ages 25 years. Hemoglobin, mean corpuscular
volume (MCV), and SF concentration were compared in the case
and control groups.
3. Statistical analysis
The data were analyzed with the SPSS version 15 software
package for Windows (Chicago, IL, USA) by two-sample t-test.
Pearsons chi-squared test was used to calculate the differences in
proportions. Discrete variables are expressed as counts and
percentages. P values < 0.05 were considered signicant.
4. Results
Our results were based on 300 children with SFS (158 boys, 142
girls) and a control group of 200 children (72 boys, 128 girls). Table
1 shows the mean values of Hb, MCV and SF in case and control
groups. For this study we divided the sample into two age
subgroups of 6 months to 2 years (Table 2) and 25 years (Table 3).
The proportion of children with Hb < 10.5 g/dl was higher in both
control subgroups (P = 0.0001, Tables 2 and 3). Serum ferritin
concentration was signicantly lower in both case subgroups
(57.5% vs. 22% and 55.7% vs. 27.6%, P = 0.0001). The differences in
MCV were not signicant in either age subgroup. In children aged
6 months to 2 years (Table 2) and 25 years (Table 3), SF was
signicantly lower (P = 0.0001) in the SFS group.
In both age subgroups, the use of nontherapeutic doses of iron
supplements was more frequent in children with febrile illness
without seizure than in the case group with SFS (Tables 2 and 3).
5. Discussion
This study showed that patients with febrile seizures were
more frequently iron decient as dened by below-normal SF
levels. There is controversy regarding the role of iron status in
febrile convulsions, which are considered a benign seizure
syndrome distinct from epilepsy.1 Previous studies have reported
a relationship between iron-deciency anemia and convulsions in
patients with malaria.19 In addition, iron-deciency anemia can
cause developmental delay and behavioral disturbances early in
life, and correcting anemia early may reverse these processes.2022
Naveed and Billo showed that SF levels were signicantly lower in
children with febrile seizure compared to controls, and suggested
that children with iron deciency are more prone to febrile
seizures.23 Another study found that the incidence of febrile
seizures in patients with thalassemia was much lower than among
children in the general population.24 Thus, iron overload may be a
major factor in the brain metabolism that prevents febrile seizures.
Kobrinsky et al. also suggested that iron-deciency anemia raises
the threshold for febrile seizure,19 whereas Daoud et al. showed
that SF levels were signicantly lower in patients with a rst febrile
seizure than in patients with febrile illness without convulsions.18
Pisacane et al. reported an association between iron-deciency
anemia and febrile convulsions in Neapolitan children.2 In
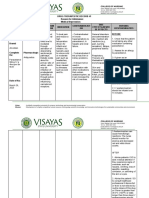
Table 1
Mean age, hemoglobin, mean corpuscular volume and serum ferritin in children with simple febrile seizure (cases) and febrile illness without seizure (controls).
Data
Age (months)
Hb (g/dl)
MCV ()
SF (ng/dl)
Cases (n = 300)
Controls (n = 200)
P value
Mean
SD
Mean
SD
26.4
11.7
74.4
28.7
13.8
1.16
6.95
10.7
25.6
10.8
75.5
32.98
18.3
1.8
7.53
8.6
0.62
0.0001
0.13
0.0001
Table 2
Characteristics of cases and controls at ages 6 months to 2 years.
Characteristic
Hb < 10.5 (g/dl)
MCV < 70 ()
SF < 30 (ng/dl)
Nontherapeutic iron supplement
Cases (n = 139)
Controls (n = 88)
P value
Male (%)
Female (%)
Male (%)
Female (%)
36.1
34.8
51
71
30.4
17.9
64.1
66.7
65.2
34.1
13
87.9
50.7
19
31
86.2
<0.0001
0.15
<0.0001
<0.05
Table 3
Characteristics of cases and controls at ages 25 years.
Characteristic
Hb < 11.5 (g/dl)
MCV < 75 ()
PF < 30 (ng/dl)
Nontherapeutic iron supplement
Cases (n = 151)
Controls (n = 112)
P value
Male (%)
Female (%)
Male (%)
Female (%)
36.7
32.2
50.8
83.1
47.6
45.5
60.6
75.8
44.6
31.9
25.5
93.6
71.7
16.2
29.7
86.5
<0.0001
<0.05
<0.0001
<0.05
S. Zareifar et al. / Seizure 21 (2012) 603605
contrast, Momen and Hakimzadeh reported no relationship
between iron-deciency anemia and rst febrile convulsion in
children younger than 5 years of age in Iran.25 In another study in
Iran, Bidabadi and Mashouf reported that iron-deciency anemia
was less frequent among patients with febrile seizure than in
controls, and found no protective effect of iron deciency against
febrile convulsions.26 Pisacane et al., in their comparative study of
age- and sex-matched children, reported a signicantly higher
rate of iron-deciency anemia, dened on the basis of low serum
iron concentration, among children with febrile seizure than in
the control group.2 In children younger than 2 years of age, 30% of
those with febrile seizures had anemia compared to 14% in the
control group. However, SF levels were not measured in that
study.
In the present study the difference in MCV between the case
and control group overall and between children aged 6 months
to 2 years with and without SFS was not signicant, but it was
signicant in the 2-to-5 year old age group. Kobrinsky et al. also
reported that patients with febrile seizures were less frequently
iron decient as dened by elevated free erythrocyte protoporphyrin, but in their study, SF levels were not measured.19 Of the
indices of body iron status measured in the present study, SF
level was the only value that was signicantly lower in children
with SFS than in the control group a nding also reported by
Daoud et al.18 Although fever was present in all of our patients
in both groups, SF levels were measured 72 h after the onset of
the febrile illness. None of the patients in either group were
being treated for iron-deciency anemia on presentation, but
signicant numbers of patients in both groups sometimes used
non-therapeutic doses of iron supplements. We did not evaluate
the response to iron therapy in children in whom febrile
seizures recurred. Our results suggest that low SF levels may
play a role in febrile seizures.
6. Limitations
The main limitation of this study was the potential confounding
effect of ferritin as an acute-phase reactant agent, which can
interfere with the inuence of iron status on febrile seizures. This
limitation could be overcome by predicting the time when ferritin
level returned to its baseline value after the acute-phase reaction.
7. Conclusion
Low body iron status may decrease the threshold of seizure and
be a risk factor for the development of febrile seizures.
Conict of interest
None.
Acknowledgments
This study was supported by Shiraz University of Medical
Sciences research committee. We thank Shirin Parand and K.
605
Shashok (author AID in the Eastern Mediterranean) for improving
the use of English in the manuscript.
References
1. Berg AT. Febrile seizures and epilepsy: the contribution of epidemiology.
Paediatric and Perinatal Epidemiology 1992;6:14552.
2. Pisacane A, Sansone R, Impagliazzo N, Coppola A, Rolando P, DApuzzo A, et al.
Iron deciency anemia and febrile convulsions: casecontrol study in children
under 2 years. British Medical Journal 1996;313:343.
3. Huang CC, Wang ST, Chang YC, Huang MC, Chi YC, Tsai JJ. Risk factors for a rst
febrile convulsion in children: a population study in southern Taiwan. Epilepsia
1999;40(6):71925.
4. Landreau-Mascaro A, Barret B, Mayaux MJ, Tardieu M, Blanche S. Risk of early
febrile seizure with perinatal exposure to nucleoside analogues. Lancet
2002;359(9306):5834.
5. Berg AT, Shinnar S, Shapiro ED, Salomon ME, Crain EF, Hauser WA. Risk factors for a
rst febrile seizure: a matched casecontrol study. Epilepsia 1995;36(4):33441.
6. Shinnar S. Febrile seizures. In: Swaiman KF, Ashwal S, Ferriero DM, editors.
Pediatric neurology principles and practice. 4th ed. City: Mosby Elsevier; 2006. p.
107989.
7. Hampers LC, Thompson DA, Bajaj L, Tseng BS, Rudolph JR. Febrile seizure:
measuring adherence to AAP guidelines among community ED physicians.
Pediatric Emergency Care 2006;22(7):4659.
8. Annegers JF, Blakely SA, Hauser WA. Recurrence of febrile convulsions in a
population-based cohort. Epilepsy Research 1990;66:1009.
9. Berg AT. The epidemiology of seizures and epilepsy in children. In: Shinnar S,
Amir N, Branski D, editors. Childhood seizures. Basel, Switzerland: Karger; 1995.
10. DeUngria M, Rao R, Wobken JD, Luciana M, Nelson CA, Georgieff MK. Perinatal
iron deciency decreases cytochrome c oxidase (CytOx) activity in selected
regions of neonatal rat brain. Pediatric Research 2000;48:16976.
11. Beard JL, Erikson KM, Jones BC. Neurobehavioral analysis of developmental iron
deciency in rats. Behavioural Brain Research 2002;134(12):51724.
12. Angulo-Kinzler RM, Peirano P, Lin E, Algarin C, Garrido M, Lozoff B. Twenty fourhour motor activity in human infants with and without iron deciency anemia.
Early Human Development 2002;70(12):85101.
13. DeMaeyer E, Adiels-Tegman M. The prevalence of anemia in the world. World
Health Statistics Quarterly 1985;38:30216.
14. Florentino RF, Guirriec RM. Prevalence of nutritional anemia in infancy and
childhood with emphasis on developing countries. In: Stekel A, editor. Iron
nutrition in infancy and childhood. New York: Raven Press; 1984. p. 6174.
15. Freire W. Strategies of the Pan American Health OrganizationWorld Health
Organization for the control of iron deciency in Latin America. Nutrition
Reviews 1997;55:1838.
16. Stoltzfus R. Dening iron-deciency anemia in public health terms: a time for
reection. Journal of Nutrition 2001;131(2S-2):565S7S.
17. Madan N, Rusia U, Sikka M, Sharma S, Shankar N. Developmental and neurophysiologic decits in iron deciency in children. Indian Journal of Pediatrics
2011;78(1):5864.
18. Daoud AS, Batieha A, Abu-Ekteish F, Gharaibeh N, Ajlouni S, Hijazi S. Iron status:
a possible risk factor for the rst febrile seizure. Epilepsia 2002;43(7):7403.
19. Kobrinsky NL, Yager JY, Cheang MS, Yatscoff RW, Tenenbein M. Does iron
deciency raise the seizure threshold? Journal of Child Neurology 1995;10(March
(2)):1059.
20. Parks YA, Wharton BA. Iron deciency and the brain. Acta Paediatrica Scandinavica 1989;55(suppl. 361):717.
21. Lozoff B, Beard J, Connor J, Barbara F, Georgieff M, Schallert T. Long-lasting
neural and behavioral effects of iron deciency in infancy. Nutrition Reviews
2006;64(5 Pt 2):S3443 [discussion S72-91].
22. Idjradinata P, Pollitt E. Reversal of developmental delays in iron decient
anemic infants treated with iron. Lancet 1993;341:14.
23. Naveed-Ur-Rehman. Billo AG. Association between iron deciency anemia and
febrile seizures. Journal of College of Physicians and Surgeons Pakistan
2005;15(6):33840.
24. Auvichayapat P, Auvichayapat N, Jedsrisuparp A, Thinkhamrop B, Sriroj S,
Piyakulmala T<ET AL>. Incidence of febrile seizures in thalassemic patients.
Journal of the Medical Association of Thailand 2004;87(8):9703.
25. Momen AA, Hakimzadeh M. Casecontrol study of the relationship between
anemia and febrile convulsion in children between 9 months and 5 years of age.
Scientic Medical Journal of Ahwaz University of Medical Sciences 2003;1(4):504.
26. Bidabadi E, Mashouf M. Association between iron deciency anemia and rst
febrile convulsion: a casecontrol study. Seizure 2009;18(June (5)):34751.
You might also like
- Nursing Care Plan FeverDocument9 pagesNursing Care Plan FeverVincent Quitoriano85% (48)
- NCP FeverDocument3 pagesNCP Feversinister1785% (48)
- Nursing Care PlansDocument48 pagesNursing Care PlansJuliantiMamangkey86% (7)
- NCPDocument13 pagesNCPLee Da HaeNo ratings yet
- 1 s2.0 S1059131111003268 MainDocument4 pages1 s2.0 S1059131111003268 MainAbdul Ghaffar AbdullahNo ratings yet
- The Relationship Between Iron Deficiency and Febrile Seizure in A Group of Children in Al-Zahraa Teaching Hospital in Al-Najaf GovernorateDocument12 pagesThe Relationship Between Iron Deficiency and Febrile Seizure in A Group of Children in Al-Zahraa Teaching Hospital in Al-Najaf GovernorateCentral Asian StudiesNo ratings yet
- Status Gizi KD Case ControlDocument4 pagesStatus Gizi KD Case Controlwimakrifah istiqomahNo ratings yet
- 6 PBDocument7 pages6 PBLinda AyuNo ratings yet
- Jurnal Reading Iron Deficiency Fakotor Resiko Kejang DemamDocument9 pagesJurnal Reading Iron Deficiency Fakotor Resiko Kejang Demamrizqiahmad33No ratings yet
- Jurnal Besi2Document3 pagesJurnal Besi2Firda PotterNo ratings yet
- Hubungan Anemsia Defisiensi Besi Dengan Kejang Demam Pada Anak BalitaDocument10 pagesHubungan Anemsia Defisiensi Besi Dengan Kejang Demam Pada Anak BalitaAulia ChoirunnisaNo ratings yet
- Kasus Neuro (Saraf)Document10 pagesKasus Neuro (Saraf)ardyan tejaNo ratings yet
- Contoh Majalah PIDocument6 pagesContoh Majalah PIajescoolNo ratings yet
- Iron Deficiency Anemia Among Preschooi Children (2-5) Years in Gaza StripDocument17 pagesIron Deficiency Anemia Among Preschooi Children (2-5) Years in Gaza StripMohammedAAl-HaddadAbo-alaaNo ratings yet
- Psychomotor DevelopmentDocument5 pagesPsychomotor DevelopmentAde RezekiNo ratings yet
- Anemia InsomniaDocument6 pagesAnemia InsomniaBalqis SafariNo ratings yet
- Jurnal AnemiaDocument6 pagesJurnal AnemiamarselyagNo ratings yet
- Prevalence and Causes of Iron Deficiency Anemias in Infants Aged 9 To 12 Months in EstoniaDocument6 pagesPrevalence and Causes of Iron Deficiency Anemias in Infants Aged 9 To 12 Months in EstoniamuarifNo ratings yet
- Prevalence and Risk Factors of Anemia in Under Five-Year-Old Children in Children's HospitalDocument4 pagesPrevalence and Risk Factors of Anemia in Under Five-Year-Old Children in Children's Hospitalindahsarizahab 28No ratings yet
- Endocrine Abnormalities in Children With Beta Thalassaemia MajorDocument6 pagesEndocrine Abnormalities in Children With Beta Thalassaemia MajorKrisbiyantoroAriesNo ratings yet
- Clinical Pediatrics: Impact of Vegetarian Diet On Serum Immunoglobulin Levels in ChildrenDocument7 pagesClinical Pediatrics: Impact of Vegetarian Diet On Serum Immunoglobulin Levels in ChildrenAldy RinaldiNo ratings yet
- Selenium and Leptin Levels in Febrile Seizure: A Case-Control Study in ChildrenDocument6 pagesSelenium and Leptin Levels in Febrile Seizure: A Case-Control Study in ChildrenDyah Gaby KesumaNo ratings yet
- Effectiveness of Iron Therapy On Breath Holding Spells in The ChildrenDocument7 pagesEffectiveness of Iron Therapy On Breath Holding Spells in The ChildrenLetícia SpinaNo ratings yet
- PDF TJP 2149Document12 pagesPDF TJP 2149Imam SabarudinNo ratings yet
- Original Article: Comparative Evaluation of Iron Deficiency Among Obese and Non-Obese ChildrenDocument7 pagesOriginal Article: Comparative Evaluation of Iron Deficiency Among Obese and Non-Obese ChildrenKurnia pralisaNo ratings yet
- TMP AE98Document5 pagesTMP AE98FrontiersNo ratings yet
- Profile of Severe Nutritional Anemia in Children at A Tertiary Care Hospital, South IndiaDocument8 pagesProfile of Severe Nutritional Anemia in Children at A Tertiary Care Hospital, South IndiaDr. Krishna N. SharmaNo ratings yet
- Original Article: AbstractDocument3 pagesOriginal Article: AbstractSeptiani HasibuanNo ratings yet
- 2 Haematological Profile in Children With Protein PDFDocument7 pages2 Haematological Profile in Children With Protein PDFAma BeluNo ratings yet
- RA Iron Deficiency AnemiaDocument6 pagesRA Iron Deficiency Anemiainggrit06No ratings yet
- Impairment of Bone Health in Pediatric Patients With Hemolytic AnemiaDocument7 pagesImpairment of Bone Health in Pediatric Patients With Hemolytic AnemiaMarifer EstradaNo ratings yet
- Anemia and NutrientDocument4 pagesAnemia and NutrientrosaliaNo ratings yet
- Estimating The Prevalence of Iron Deficiency in The First TwoDocument8 pagesEstimating The Prevalence of Iron Deficiency in The First TwoJavier LunaNo ratings yet
- Association Between Helicobacter Pylori Infection and Iron DeficiencyDocument4 pagesAssociation Between Helicobacter Pylori Infection and Iron Deficiencydaiana.diazNo ratings yet
- Iron Deficiency Anaemia in Reproductive Age Women Attending Obstetrics and Gynecology Outpatient of University Health Centre in Al-Ahsa, Saudi ArabiaDocument4 pagesIron Deficiency Anaemia in Reproductive Age Women Attending Obstetrics and Gynecology Outpatient of University Health Centre in Al-Ahsa, Saudi ArabiaDara Mayang SariNo ratings yet
- Iron Def IJPDocument5 pagesIron Def IJPPrahbhjot MalhiNo ratings yet
- The Relationship Between Depression and Serum Ferritin Level - Shariatpanaahi 2007Document4 pagesThe Relationship Between Depression and Serum Ferritin Level - Shariatpanaahi 2007Julio JuarezNo ratings yet
- HemaDocument10 pagesHemadrkhengkiNo ratings yet
- Iron Deficiency in Young Children: A Risk Marker For Early Childhood CariesDocument6 pagesIron Deficiency in Young Children: A Risk Marker For Early Childhood Carieswahyudi_donnyNo ratings yet
- 2023 Anemia and Associated Factors Among Internally Displaced Children at Debark...Document21 pages2023 Anemia and Associated Factors Among Internally Displaced Children at Debark...Olga CîrsteaNo ratings yet
- Determinants of Nutritional Anaemia in Children Less Than Five Years AgeDocument6 pagesDeterminants of Nutritional Anaemia in Children Less Than Five Years AgeBaiiqDelaYulianingtyasNo ratings yet
- Iron DefDocument5 pagesIron DefchristieNo ratings yet
- Association of Elevated Serum Ferritin Concentration With Insulin Resistance and Impaired Glucose Metabolism in Korean Men and WomenDocument7 pagesAssociation of Elevated Serum Ferritin Concentration With Insulin Resistance and Impaired Glucose Metabolism in Korean Men and WomenMakbule ERÇAKIRNo ratings yet
- EJMCM - Volume 7 - Issue 11 - Pages 4739-4745Document7 pagesEJMCM - Volume 7 - Issue 11 - Pages 4739-4745Myo KoNo ratings yet
- ExcelenteDocument6 pagesExcelenteRicardo ColomaNo ratings yet
- Common Cold JournalDocument5 pagesCommon Cold JournalJuwita PratiwiNo ratings yet
- Associations Between Environmental Heavy Metal Exposure and Childhood Asthma: A Population-Based StudyDocument11 pagesAssociations Between Environmental Heavy Metal Exposure and Childhood Asthma: A Population-Based StudyLeidy CarolinaNo ratings yet
- 3 AnemiainPregnancyDocument6 pages3 AnemiainPregnancyGabriela RablNo ratings yet
- Anemi 2Document7 pagesAnemi 2inggrit thalasaviaNo ratings yet
- Am J Clin Nutr 2005 Schneider 1269 75Document7 pagesAm J Clin Nutr 2005 Schneider 1269 75Jony KechapNo ratings yet
- Risk Factor 3Document8 pagesRisk Factor 3ayham luNo ratings yet
- Stunting Dan Stress Oksidatif - Aly 2018Document6 pagesStunting Dan Stress Oksidatif - Aly 2018Emmy KwonNo ratings yet
- Journal Trace Elements in MedicineDocument10 pagesJournal Trace Elements in MedicineOmar ReynosoNo ratings yet
- Iron Deficiency, Cognitive Functions, and Neurobehavioral Disorders in ChildrenDocument10 pagesIron Deficiency, Cognitive Functions, and Neurobehavioral Disorders in ChildrenWahyu RhomadonNo ratings yet
- Serum Ferritin and Amphetamine Response in Youth With Attention-Deficit/Hyperactivity DisorderDocument8 pagesSerum Ferritin and Amphetamine Response in Youth With Attention-Deficit/Hyperactivity DisorderFahmi FachruddinsyahNo ratings yet
- Literature Review On Prevalence of Anemia in PregnancyDocument4 pagesLiterature Review On Prevalence of Anemia in Pregnancyc5pdd0qgNo ratings yet
- Diagnosis and Prevention of Iron Def Anemia in 0-3yoDocument13 pagesDiagnosis and Prevention of Iron Def Anemia in 0-3yorinNo ratings yet
- Diarrhea Dan AnemiaDocument4 pagesDiarrhea Dan AnemiaUnyar LeresatiNo ratings yet
- Anemia Among Adolescents: ArticleDocument7 pagesAnemia Among Adolescents: ArticleEliya eliyaNo ratings yet
- 5-Effect of Low-Dose Ferrous Sulfate Vs Iron Polysaccharide Complex On Hemoglobin Concentration in Young Children With Nutritional Iron-Deficiency AnemiaDocument8 pages5-Effect of Low-Dose Ferrous Sulfate Vs Iron Polysaccharide Complex On Hemoglobin Concentration in Young Children With Nutritional Iron-Deficiency AnemiaMundo Tan PareiraNo ratings yet
- Anemia As Risk Factor For PneumoniaDocument12 pagesAnemia As Risk Factor For PneumoniaEndy Widya PutrantoNo ratings yet
- Research ArticleDocument7 pagesResearch ArticleauliyaNo ratings yet
- Iron Supplementation Improves Iron Status and Reduces Morbidity in Children With or Without Upper Respiratory Tract Infections: A Randomized Controlled Study in Colombo, Sri Lanka1-3Document15 pagesIron Supplementation Improves Iron Status and Reduces Morbidity in Children With or Without Upper Respiratory Tract Infections: A Randomized Controlled Study in Colombo, Sri Lanka1-3nurkasihNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 16: HematologyFrom EverandComplementary and Alternative Medical Lab Testing Part 16: HematologyNo ratings yet
- Tabel 1.16 Hasil Penemuan Penderita Program P2 ISPA Poli MTBS Rawat Inap Cempaka 2014 Periode Januari-Desember 2014Document4 pagesTabel 1.16 Hasil Penemuan Penderita Program P2 ISPA Poli MTBS Rawat Inap Cempaka 2014 Periode Januari-Desember 2014Firda PotterNo ratings yet
- Management For Labiopalatognatoskizis PatientDocument1 pageManagement For Labiopalatognatoskizis PatientFirda PotterNo ratings yet
- 2009 Article 957Document8 pages2009 Article 957Firda PotterNo ratings yet
- Jurnal Besi2Document3 pagesJurnal Besi2Firda PotterNo ratings yet
- DAFTAR PUSTAKA AcccccDocument2 pagesDAFTAR PUSTAKA AcccccFirda PotterNo ratings yet
- Immune Reconstitution Inflammatory Syndrome and Cerebral ToxoplasmosisDocument2 pagesImmune Reconstitution Inflammatory Syndrome and Cerebral ToxoplasmosisFirda PotterNo ratings yet
- BR J Ophthalmol 2004 Stanford 444 5Document4 pagesBR J Ophthalmol 2004 Stanford 444 5Firda PotterNo ratings yet
- 976 FullDocument7 pages976 FullFirda PotterNo ratings yet
- 2008 Article 25Document8 pages2008 Article 25Firda PotterNo ratings yet
- Ijeb 48 (7) 642-650Document0 pagesIjeb 48 (7) 642-650Firda PotterNo ratings yet
- 3.CI - AppendixDocument63 pages3.CI - AppendixFirda PotterNo ratings yet
- Nursing Care PlanDocument3 pagesNursing Care Planagentlara28No ratings yet
- Dmt316 Manual UkDocument12 pagesDmt316 Manual UkCarlos MinayaNo ratings yet
- Protokol SarcomaDocument4 pagesProtokol SarcomaHep PutNo ratings yet
- Drug Study ParacetamolDocument1 pageDrug Study ParacetamolAbigail Basco100% (2)
- Referral Letter - MeningitisDocument3 pagesReferral Letter - MeningitisChristafar RajNo ratings yet
- Homeostasis, Stress and Adaptation - Ppt2aDocument154 pagesHomeostasis, Stress and Adaptation - Ppt2aV_RN100% (2)
- Natural Cancer Remedies That WorkDocument48 pagesNatural Cancer Remedies That WorkAlessio Anam100% (2)
- Effectiveness of Tepid Sponge Compresses and Plaster Compresses On Children'S Fever Temperature TyphoidDocument7 pagesEffectiveness of Tepid Sponge Compresses and Plaster Compresses On Children'S Fever Temperature TyphoidAndri YansyahNo ratings yet
- JD Drug-1-2Document2 pagesJD Drug-1-2RON PEARL ANGELIE CADORNANo ratings yet
- Science Model School: Class: 4 Subject Syllabus Scheme of Papers MarksDocument9 pagesScience Model School: Class: 4 Subject Syllabus Scheme of Papers MarksBest CampusNo ratings yet
- Benign Febrile Convulsions Nursing Care PlansDocument10 pagesBenign Febrile Convulsions Nursing Care PlansMurugesan100% (1)
- Aconitum NapellusDocument18 pagesAconitum Napelluskattarsys1No ratings yet
- How 20to 20perform 20a 20physical 20exam 20in 20your 20horseDocument50 pagesHow 20to 20perform 20a 20physical 20exam 20in 20your 20horseThamil ArasanNo ratings yet
- JP XII Organic Chemistry (23) - 1 PDFDocument7 pagesJP XII Organic Chemistry (23) - 1 PDFAshish RanjanNo ratings yet
- Fever of Unknown OriginDocument26 pagesFever of Unknown OriginFiona Yona Sitali100% (1)
- Physio ThermoregulationDocument9 pagesPhysio ThermoregulationStd DlshsiNo ratings yet
- Standard Treatment ProtocolsDocument663 pagesStandard Treatment Protocolsdrvins1No ratings yet
- End-Stage Renal DiseaseDocument3 pagesEnd-Stage Renal DiseaseAkira Pongchad B100% (1)
- Temperature, Pulse Rate and Inspiration RatesDocument1 pageTemperature, Pulse Rate and Inspiration RatesmvladysemaNo ratings yet
- Engleza Schita-Plan Ingrijire SpecificDocument4 pagesEngleza Schita-Plan Ingrijire SpecificBenterez Ionela BiancaNo ratings yet
- Fever: Clinical DescriptionDocument6 pagesFever: Clinical DescriptionNama ManaNo ratings yet
- Fever Without Source: Dr. Tiroumourougane Serane. VDocument29 pagesFever Without Source: Dr. Tiroumourougane Serane. VTirouNo ratings yet
- IAH AC Introduction To HomotoxicologyDocument60 pagesIAH AC Introduction To HomotoxicologywurtukukNo ratings yet
- Daftar PustakaDocument3 pagesDaftar Pustakahendri najibNo ratings yet
- Nursing Care PlanDocument8 pagesNursing Care Planalexander abasNo ratings yet
- Non Specific HostDocument46 pagesNon Specific HostAdrian BautistaNo ratings yet