Professional Documents
Culture Documents
Pattern of Ocular Injuries in Owo, Nigeria: Original Article
Pattern of Ocular Injuries in Owo, Nigeria: Original Article
Uploaded by
paulpiensaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pattern of Ocular Injuries in Owo, Nigeria: Original Article
Pattern of Ocular Injuries in Owo, Nigeria: Original Article
Uploaded by
paulpiensaCopyright:
Available Formats
Original Article
Pattern of Ocular Injuries in Owo, Nigeria
Charles Oluwole Omolase1, FWACS, FMCOphth; Ericson Oluseyi Omolade1, MBBS
Olakunle Tolulope Ogunleye1, MBBS; Bukola Olateju Omolase2, MBBS
Chidi Oliver Ihemedu1, MBBS; Olumuyiwa Adekunle Adeosun1, MBBS
1
Department of Ophthalmology, Federal Medical Center, Owo, Ondo State, Nigeria
2
Department of Radiology, Federal Medical Center, Owo, Ondo State, Nigeria
Purpose: To determine the pattern of ocular injuries in patients presenting to the
eye clinic and the accident and emergency department of Federal Medical Center,
Owo, Ondo State, Nigeria.
Methods: This prospective study was conducted between January and December 2009.
Federal Medical Center, Owo is the only tertiary hospital in Ondo State, Nigeria.
The eye center located at this medical center was the only eye care facility in the
community at the time of this study. All patients were interviewed with the aid of an
interviewer-administered questionnaire and underwent a detailed ocular examination.
Results: Of 132 patients included in the study, most (84.1%) sustained blunt eye
injury while (12.1%) had penetrating eye injury. A considerable proportion of patients
(37.9%) presented within 24 hours of injury. Vegetative materials were the most
common (42.4%) offending agent, a minority of patients (22%) was admitted and
none of the patients had used eye protection at the time of injury.
Conclusion: In the current series, blunt eye injury was the most common type of
ocular trauma. The community should be educated and informed about the importance
of preventive measures including protective eye devices during high risk activities.
Patients should be encouraged to present early following ocular injury.
Keywords: Eye Injuries, Pattern; Vegetative Matter; Nigeria
J Ophthalmic Vis Res 2011; 6 (2): 114-118.
Correspondence to: Charles Oluwole Omolase, FWACS, FMCOphth. Consultant Ophthalmologist, Department
of Ophthalmology, Federal Medical Centre, P.M.B 1053, Owo, Ondo State, Nigeria; Tel: +23408033788860;
e-mail: omolash2000@yahoo.com
Received: May 27, 2010
Accepted: March 9, 2011
INTRODUCTION
Trauma is an important cause of ocular
morbidity. The pattern of ocular injuries tends
to vary from one location to another and is
affected by the activities of residents in a
particular location.1 Many eye injuries are related
to particular occupations and certain cultures. 2
Some individuals by virtue of their job are
prone to ocular injuries and certain activities
of daily living increase the risk of eye trauma
due to exposure to hazards.3 Despite the fact
that the eyes represent only 0.27% of the total
114
body surface area and 4% of the facial area, they
are the third most common organ affected by
injuries after the hands and feet.4 Ocular trauma
is an avoidable cause of blindness and visual
impairment. Ocular trauma may be caused by
various objects used in different settings. 5 Male
subjects are at higher risk of ocular trauma. 6
Even though ocular trauma has been described
as a neglected issue,7 it was highlighted as a
major cause of visual morbidity more recently.8
Worldwide there are approximately 1.6
million people blind from eye injuries, 2.3
million bilaterally visually impaired and 19
JOURNAL OF OPHTHALMIC AND VISION RESEARCH 2011; Vol. 6, No. 2
Ocular Injuries in Nigeria; Omolase et al
million with unilateral visual loss; these facts
make ocular trauma the most common cause
of unilateral blindness. 9 The age distribution
for serious ocular trauma is bimodal with the
maximum incidence in young adults and a
second peak in the elderly. 10,11 Studies have
shown that approximately one half of patients
who present to an eye casualty department are
cases of ocular trauma.12,13 Direct and indirect
costs of ocular trauma are known to run into
millions of dollars annually. 14 Ocular trauma
occurs frequently in developing countries and
constitutes a major health problem. 15 Even
though developing countries carry the largest
burden of ocular trauma, they are the least able
to afford the costs.16,17 Recognition of the public
health importance of ocular trauma has sparked
growing interest in studies on eye injuries.18 The
execution of this study became imperative in
view of an increasing number of ocular trauma
at the only eye center in the community. We
designed this study to determine the pattern
of ocular injuries in patients presenting to the
eye clinic and the accident and emergency
department of Federal Medical Center, Owo,
Ondo State, Nigeria.
METHODS
This prospective study was performed at the
eye clinic and the accident and emergency
department of Federal Medical Center, Owo,
Ondo State, Nigeria between January and
December 2009. The hospital was the only
tertiary medical center in Ondo State at the
time of the study. The eye center is patronized
by patients from Ondo State, Nigeria and some
other neighboring states.
The patients either presented directly to the
hospital or were referred from other public or
private hospitals. Approval was obtained from
the Ethical Review Committee of the hospital
prior to commencement of this study. Informed
consent was obtained from each participant.
All consenting patients with varying degrees of
ocular injuries were enrolled in this study. The
respondents were interviewed with the aid of
semi-structured questionnaire by the authors.
All patients underwent a comprehensive ocular
examination including visual acuity (using
Snellen chart), penlight, slit lamp biomicroscopy
and direct ophthalmoscopy. Data were analyzed
using SPSS 15.0.1 statistical software package
(SPSS Inc., Chicago, IL, USA). Chi-square test
was employed with statistical significance set
at 0.05.
RESULTS
One hundred and thirty-two patients including
102 male (77.3%) and 30 female (22.7%) subjects
1 to 70 years of age participated in the study.
Ethnicity of the patients was Yorubas in 68.2%,
Ibos in 7.6% and Hausas in 3%. The majority
of the patients (82.6%) were Christian and the
remaining (17.4%) were Muslim. Few patients
(13.3%) had no formal education, 53 (40.2%)
had primary education, 33 (25%) had secondary
education, and 28 (21.2%) had tertiary education.
Most patients (51.5%) were single, 47.7% were
married and one subject (0.8%) was widowed.
The occupation of the patients is detailed in Table
1, most of the patients (36.4%) were students.
The right eye was involved in 60 (45.5%)
subjects, the left eye in 59 (44.7%) cases and the
injury was bilateral in 13 (9.9%) cases. Injury
occurred at home in 40 individuals (30.3%), on
the road in 37 (28%), at school in 28 (21.2%), at
work in 11 (8.3%), during a party in 8 (6.1%),
on a farm in 7 (5.3%) and in church in 1 (0.8%).
Age and sex did not affect the location at which
injury was sustained (P=0.698 and 0.072,
respectively), but occupation was significantly
associated with the place of injury (P<0.001).
Most injuries (84.1%) were blunt, 6 (12.1%)
were due to penetrating trauma, 2 (1.5%) eyes
sustained perforating injury and 3 (2.3%)
were affected by chemical burns. Age, sex
and occupation did not significantly affect
Table 1. Patients occupation
Occupation
Schooling
Farming
Artisan
Trading
Civil Servant
Unemployed
Total
Frequency
48
24
24
17
16
3
132
JOURNAL OF OPHTHALMIC AND VISION RESEARCH 2011; Vol. 6, No. 2
Percentage
36.4
18.2
18.2
12.9
12.1
2.3
100
115
Ocular Injuries in Nigeria; Omolase et al
the type of injury (P=0.396, 0.481 and 0.946,
respectively).
The offending agents are summarized in
Table 2, 42.4% were vegetative materials. Age
and sex were not correlated with the type of
the agent (P=0.976 and 0.528, respectively),
however occupation was significantly associated
with the causal agent (P=0.016).
A considerable proportion of patients
(37.9%) presented within 24 hours, 8.3% after
48 hours, 6.8% after 72 hours, 17.4% between
3 and 7 days, and 29.5% after one week. The
anatomical site of injury and level of education
significantly affected the time of presentation
(P=0.007 and 0.002, respectively) but age, sex
and occupation did not (P=0.334, 0.818 and
0.287, respectively). The distance travelled by
the patients to the eye center was less than
20km in 61.4%, 20-50 km in 21.2%, 50-100km
in 12.9% and more than 100km in 4.5%. This
variable however did not significantly affect
the time of presentation (P=0.7).
Only 32 (24.2%) patients had occupational
eye injury, no subject used protective eyewear
at the time of injury. Only 29 (22%) cases were
admitted. Most patients (51.5%) sought some
form of treatment prior to presentation: 31
patients (45.6%) self administered medication,
5 (7.4%) received traditional treatment and
the remaining 1 (1.5%) used a combination of
treatments.
As detailed in Table 3, the most common
site of injury (43.9%) was the cornea. Age and
sex did not significantly affect the anatomical
site of injury (P=0.573 and 0.302, respectively)
while occupation did (P=0.027). Few patients
(21.2%) had sustained injury to other parts of
the face.
Table 2. Offending agents
Metallic object
Finger, elbow, fist
Insect
Stone
Glass
Bullet
Chemical
Ball
Total
116
Frequency
28
21
11
8
3
2
2
1
132
Percentage
21.2
15.9
8.3
6.1
2.3
1.5
1.5
0.8
100
Table 3. Anatomical site of eye injury
Lid
Conjunctiva
Cornea
Iris
Lens
Anterior/posterior segment
Cornea and lens
Total
Frequency
27
16
58
15
6
5
5
132
Percentage
20.5
12.1
43.9
11.4
4.5
3.8
3.8
100
Table 4. Visual acuity at presentation and after treatment
Visual acuity
6/5-6/18
6/18-6/60
3/60-6/60
<3/60
Total
Frequency (%)
At presentation
After treatment
67 (50.8)
102 (77.3)
16 (12.1)
6 (4.5)
6 (4.5)
1 (0.8)
43 (32.6)
23 (17.4)
132 (100)
132 (100)
The majority of patients (95.5%) had good
vision prior to the injury. Table 4 summarizes
visual acuities of the patients at presentation
and after treatment. Patient age was significantly
associated with visual outcomes (P=0.019),
however sex and occupation were not (P=0.925
and 0.169, respectively). Prognosis for restoration
of vision was good in most patients (62.9%),
fair in 21.2%, and poor in 15.9%.
DISCUSSION
The predominance of Yorubas and Christians
in our study is not surprising in view of
their predominance in the community. There
was a preponderance of male subjects in our
study which is in accordance with some other
reports. 3,19-21 The predominance of ocular
injuries in male subjects may be related to their
aggressive and adventure seeking behavior. As
reported by some other studies,3,12 most of our
patients belonged to a young and active age
group. This finding is understandable as such
people are likely to engage in risky behaviours
and activities which may predispose to ocular
injuries.
The particular function of the eye has
mandated an exposed location which increases
the possibility of injury.22 The type and extent of
damage sustained by the eye depends on both
JOURNAL OF OPHTHALMIC AND VISION RESEARCH 2011; Vol. 6, No. 2
Ocular Injuries in Nigeria; Omolase et al
the mechanism and force of injury. Laterality
in ocular injuries also tends to vary. There was
a slight predominance of injury to the right
eye (45.5%) in this study which is similar to
a report by Mallika et al 21 in Malaysia. This
predominance was higher (58.5%) in a study
by Okoye3 in Enugu, Nigeria. The reason may
be the fact that most people are right handed.
Almost one third of our patients sustained
injury at home. This finding is similar to the
study by Mallika et al.21 Most of our respondents
had blunt trauma which is different from the
report by Okoye, 3 stating a preponderance
of penetrating trauma. Another study has
reported changing patterns of eye injuries in
Nigeria over the past decades during which a
preponderance of war-related injuries in the
early 70s was replaced by home and school
related injuries as well as industrial trauma.
Furthermore with the rising incidence of
armed robbery and civilian-armed combats in
Nigeria, gun shot injuries are becoming more
common.23 Our study included only two cases
of gun shot eye injuries. This finding may be
attributed to the fact that the study population
and neighboring communities enjoyed peaceful
co-existence at the time of the study.
Remarkably, a significant proportion
of our patients presented to the eye clinic
within 24 hours of eye injury which may have
contributed to the favorable outcome in most
of them. Proximity to the eye center may have
contributed to early presentation. Awareness
of the services offered at our eye center is also
likely to have prompted early presentation.
The importance of increasing awareness about
existing eye facilities in the populace cannot
be overemphasized as this is likely to promote
the utilization of such health facilities. Our
findings are somehow in contrast to those
reported by Babar et al24 in Pakistan; over 60%
of their patients presented one week after eye
injury. Late presentation following eye injuries
has also been reported in other studies.25-27 A
study by Qureshi 28 reported that the farther
the victims lived from an eye care facility, the
later they presented after injury. The findings
of the latter report are at variance with the
current study because the distance travelled
by our patients did not significantly affect the
time of presentation.
It is disturbing that none of our respondents
utilized protective devices at the time of
injury. This finding underscores the need for
educating people regarding the use of protective
eyewear which may significantly decrease the
magnitude of visual loss due to trauma. The
impact of ocular trauma in terms of medical
care, loss of income and cost of rehabilitation
services clearly highlights the importance of
preventive strategies.19
In summary there was a preponderance of
eye injuries among male subjects in our study.
Most patients sustained blunt eye injury and
only few of them required admission. A sizeable
proportion of patients presented within 24 hours
after injury. Occupation and the anatomical
site of injury significantly affected the time
of presentation. Some respondents sustained
ocular injury in their school environment. None
of the patients used protective eyewear at the
time of injury. The age of patients significantly
affected visual outcomes. We reccomend mass
education to encourage early presentation
following eye injury and believe that school
authorities should regulate recreational activities
in school and prevent injuries to the eye and
other parts of the body.
Acknowledgements
We are grateful to the respondents for accepting
to participate in this study. Support by the
Management of Federal Medical Center, Owo,
Ondo State, Nigeria is hereby acknowledged.
Conflicts of Interest
None.
REFERENCES
1. Parmar NRC, Sunandan S. Pattern of ocular injuries
in Haryana. Ind J Ophthalmol 1985;33:141-144.
2. Mulugeta A, Bayu S. Pattern of perforating ocular
injuries at Manelik 11 hospital, Addis Ababa. Ethiop
J Health Dev 2001;15:131-137.
3. Okoye OI. Eye injury requiring hospitalization in
JOURNAL OF OPHTHALMIC AND VISION RESEARCH 2011; Vol. 6, No. 2
117
Ocular Injuries in Nigeria; Omolase et al
Enugu, Nigeria. A one-year survey. Niger J Surg Res
2006;8:34-37.
17. Ilsar M, Chirambo M, Belkin M. Ocular injuries in
Malawi. Br J Ophthalmol 1982;66:145-148.
4. Nordber E. Injuries as a public health problem in
sub-Saharan Africa: Epidemiology and prospects for
control. East Afr Med J 2000;77:1-43.
18. Woo JH, Sundar G. Eye injuries in Singapore-Dont
risk it. Do more. A prospective study. Ann Acad Med
Singapore 2006;35:706-718.
5. AdemolaPopoola DS, Owoeye JFA. Gunshot
related binocular injuries. W J Med Sci 2006;1:65-68.
19. Thylefors B. Epidemiological patterns of ocular
trauma. Aust N Z J Ophthalmol 1992;20:95-98.
6. Olurin O. Eye injuries in Nigeria: A review of 433
cases. Am J Ophthalmol 1971;72:159-166.
20. Soliman MM, Macky TA. Pattern of ocular
trauma in Egypt. Graefes Arch Clin Exp Ophthalmol
2008;246:205-212.
7. Parver L. Eye trauma. The neglected disorder. Arch
Ophthalmol 1986;104:1452-1453.
8. Macewen CJ. Ocular injuries. J R Coll Surg Edinb
1999;44:317-323.
9. Negrel AD, Thylefors B. The global impact of eye
injuries. Ophthalmic Epidemiol 1998;5:143-169.
10. Glynn RJ, Seddon JM, Berlin BM. The incidence
of eye injuries in New England. Arch Ophthalmol
1988;106:785-789.
11. Desai P, MacEwen CJ, Baines P, Minaissian DC.
Epidemiology and implications of ocular trauma
admitted to hospital in Scotland. J Epidemiol Comm
Health 1996;50:436-441.
12. Chiapella AP, Rosenthal AR. One year in an eye
casualty clinic. Br J Ophthalmol 1985;69:865-870.
13. Vernon SA. Analysis of all new cases seen in a busy
regional ophthalmic casualty department during a
24-week period. J R Soc Med 1983;76:279-282.
14. Teilsch JM, Parver LM. Determinants of hospital
charges and length of stay for ocular trauma.
Ophthalmology 1990;97:231-237.
15. Michael I, Moses CH, Michael B. Ocular injuries in
Malawi. Br J Ophthalmol 1982;66:145-148.
16. Umeh RE, Umeh OC. Causes and visual outcome
of childhood eye injuries in Nigeria. Eye (Lond)
1997;11:489-495.
118
21. Mallika PS, Tan AK, Asok T, Faisal HA, Aziz S,
Intan G. Pattern of ocular trauma in Kuching,
Malaysia. Malaysia Fam Phys 2009;3:140-145.
22. Steven S. Primary care of eye injuries. J Comm Eye
Health 1997;10:59-60.
23. AdemolaPopoola DS, Odebode TO, Adigun AI.
Intentional enucleation of the eyes: an unusual cause
of binocular blindness. World J Med Sci 2006;1:158161.
24. Babar TF, Khan MT, Marwat MZ, Shah SA, Murad
Y, Khan MD. Patterns of ocular trauma. J Coll
Physicians Surg Pak 2007;17:148-153.
25. Mackiewicz J, Machowicz-Matejko E, Saaga-Pylak
M, Piecyk-Sidor M, Zagrski Z. Work-related,
penetrating eye injuries in rural environments. Ann
Agric Environ Med 2005;12:27-29.
26. Yaya G, Bobossi Serengbe G, Gaudeuille A. Ocular
injuries in children aged 0-15 years: epidemiological
and clinical aspects at Bangui National Teaching
Hospital. J Fr Ophtalmol 2005;28:708-712.
27. Nwosu SN. Domestic ocular and adnexal injuries in
Nigerians. West Afr J Med 1995;14:137-140.
28. Qureshi MB. Ocular injury pattern in Turbat,
Baluchistan, Pakistan. J Comm Eye Health 1997;10:
57-58.
JOURNAL OF OPHTHALMIC AND VISION RESEARCH 2011; Vol. 6, No. 2
You might also like
- Newborn Physical AssessmentDocument3 pagesNewborn Physical AssessmentFateaNo ratings yet
- Case Study On Ford MotorsDocument8 pagesCase Study On Ford Motorsabhishek_awasthi_150% (2)
- Gyorgy Cziffra - MemoirsDocument113 pagesGyorgy Cziffra - MemoirsLuis Miguel Gallego OntilleraNo ratings yet
- Retrospective Study of The Pattern of Eye Disorders Among Patients in Delta State University Teaching Hospital, OgharaDocument6 pagesRetrospective Study of The Pattern of Eye Disorders Among Patients in Delta State University Teaching Hospital, OgharaHello PtaiNo ratings yet
- Pattern of Ocular Trauma Seen in Grarbet Hospital, Butajira, Central EthiopiaDocument6 pagesPattern of Ocular Trauma Seen in Grarbet Hospital, Butajira, Central Ethiopiatrisya putri meliaNo ratings yet
- Etiological Factors of Ocular Trauma in Children and Adolescents Based On 200 Cases at The Pediatric Ophthalmology Unit of The Bouake University HospitalDocument7 pagesEtiological Factors of Ocular Trauma in Children and Adolescents Based On 200 Cases at The Pediatric Ophthalmology Unit of The Bouake University HospitalAthenaeum Scientific PublishersNo ratings yet
- Knowlegde and Willingness To Donate Eye Among Medical Doctors in Delta StateDocument7 pagesKnowlegde and Willingness To Donate Eye Among Medical Doctors in Delta StateInternational Organization of Scientific Research (IOSR)No ratings yet
- Pattern of Ocular Diseases Among Patients Attending Ophthalmic Outpatient Department - A Cross-Sectional StudyDocument11 pagesPattern of Ocular Diseases Among Patients Attending Ophthalmic Outpatient Department - A Cross-Sectional StudyDr. Abhishek OnkarNo ratings yet
- Changes of Patterns and Outcomes of Ocular and Facial Trauma Among Children in JordanDocument11 pagesChanges of Patterns and Outcomes of Ocular and Facial Trauma Among Children in JordanMoiz AhmedNo ratings yet
- International Glaucoma Association: Abebe Bejiga MDDocument2 pagesInternational Glaucoma Association: Abebe Bejiga MDDhika KusumaNo ratings yet
- Trau 1Document3 pagesTrau 1manognaaaaNo ratings yet
- Prevalenceand Associated Ffactorsof Visual Impairment Among School Age ChildrenDocument10 pagesPrevalenceand Associated Ffactorsof Visual Impairment Among School Age ChildrenDaniel AsmareNo ratings yet
- ManuscriptDocument11 pagesManuscriptsarjak shahNo ratings yet
- Dhaiban 2021Document7 pagesDhaiban 2021Eric PavónNo ratings yet
- Nigeria Jenis Penyebab TraumaDocument5 pagesNigeria Jenis Penyebab TraumaMahdiahNo ratings yet
- Provisional PDF Published Jan 26, 2010: Adeyi Adoga, Tonga Nimkur and Olugbenga SilasDocument10 pagesProvisional PDF Published Jan 26, 2010: Adeyi Adoga, Tonga Nimkur and Olugbenga SilasTeddy AttondeNo ratings yet
- Chemical Eye Injuries: Presentation and Management DifficultiesDocument5 pagesChemical Eye Injuries: Presentation and Management DifficultiesMuhammad SubhanNo ratings yet
- 227 Manuscript 538 1 10 20210129Document5 pages227 Manuscript 538 1 10 20210129Ayele BizunehNo ratings yet
- Most Common Ophthalmic Diagnoses in Eye Emergency Departments: A Multicenter StudyDocument8 pagesMost Common Ophthalmic Diagnoses in Eye Emergency Departments: A Multicenter StudyAlba García MarcoNo ratings yet
- Results of Surgery For Congenital Esotropia: Original ResearchDocument6 pagesResults of Surgery For Congenital Esotropia: Original ResearchkarenafiafiNo ratings yet
- Amj 06 560Document5 pagesAmj 06 560paulpiensaNo ratings yet
- Emergency Department Visits Related To Eye InjryDocument10 pagesEmergency Department Visits Related To Eye InjryHectorNo ratings yet
- Nurdin Zuhri Ocular Trauma 1Document14 pagesNurdin Zuhri Ocular Trauma 1Farid NurdiansyahNo ratings yet
- Eye Health Seeking Behavior and Its Associated Factors Among Adult Population in Mangu LGA Plateau State NigeriaDocument9 pagesEye Health Seeking Behavior and Its Associated Factors Among Adult Population in Mangu LGA Plateau State NigeriaAthenaeum Scientific PublishersNo ratings yet
- Theoretical and Conceptual FrameworkDocument14 pagesTheoretical and Conceptual FrameworkJelshan BawogbogNo ratings yet
- The Relation of Onset of Trauma and Visual Acuity On Traumatic PatientDocument6 pagesThe Relation of Onset of Trauma and Visual Acuity On Traumatic PatientNurlaila IshaqNo ratings yet
- Refractive Errors in Children With Autism in A Developing CountryDocument4 pagesRefractive Errors in Children With Autism in A Developing CountryAnifo Jose AntonioNo ratings yet
- Clinical Profile and Visual Outcome of Ocular Injuries in Tertiary Care Rural HospitalDocument8 pagesClinical Profile and Visual Outcome of Ocular Injuries in Tertiary Care Rural HospitalIJAR JOURNALNo ratings yet
- Emergency Department Visits Related Eye Injuries 2008Document10 pagesEmergency Department Visits Related Eye Injuries 2008Nguyễn HữuNo ratings yet
- Should We Say NO To Body Piercing in Children? Complications After Ear Piercing in ChildrenDocument3 pagesShould We Say NO To Body Piercing in Children? Complications After Ear Piercing in ChildrenGhalyRizqiMauludinNo ratings yet
- Amhsr 2 14Document5 pagesAmhsr 2 14Archana KrishnaNo ratings yet
- Ear Syringing - Trends From A Young Ent Practice in Nigeria: Original ResearchDocument4 pagesEar Syringing - Trends From A Young Ent Practice in Nigeria: Original ResearchnavnaNo ratings yet
- Celulitis PeriorbitariaDocument4 pagesCelulitis PeriorbitariaJose Carlos Guerra RangelNo ratings yet
- Adesunkanmi2021 Article ImpactOfTheCOVID-19PandemicOnSDocument8 pagesAdesunkanmi2021 Article ImpactOfTheCOVID-19PandemicOnSCarlosA.DíazNo ratings yet
- Jurnal MataDocument7 pagesJurnal Mataokky_rahmatNo ratings yet
- Dry Eye - WordDocument39 pagesDry Eye - WordJan IrishNo ratings yet
- Intracranial Tumors: An Ophthalmic Perspective: DR M Hemanandini, DR P Sumathi, DR P A KochamiDocument3 pagesIntracranial Tumors: An Ophthalmic Perspective: DR M Hemanandini, DR P Sumathi, DR P A Kochamiwolfang2001No ratings yet
- 34tupe EtalDocument5 pages34tupe EtaleditorijmrhsNo ratings yet
- Risk Factors For Myopia in Inner Mongolia Medical Students in ChinaDocument7 pagesRisk Factors For Myopia in Inner Mongolia Medical Students in ChinaChristabella Natalia WijayaNo ratings yet
- Ophthalmogenetic and Epidemiological Studies of Egyptian Children With Mental RetardationDocument8 pagesOphthalmogenetic and Epidemiological Studies of Egyptian Children With Mental Retardationray m deraniaNo ratings yet
- Management of Foreign Bodies in The Ear: A Retrospective Review of 123 Cases in NigeriaDocument5 pagesManagement of Foreign Bodies in The Ear: A Retrospective Review of 123 Cases in NigeriaElrach CorpNo ratings yet
- China Risk FactorsDocument6 pagesChina Risk FactorsNoor MohammadNo ratings yet
- A Cross Sectional Study of Refractive ErDocument6 pagesA Cross Sectional Study of Refractive Er0039 NURUL HANI IZZUANI BINTI AFRIZANNo ratings yet
- Aes 04 9Document6 pagesAes 04 9Ignasius HansNo ratings yet
- Prevalence and Consequence of Customized Ocular Prosthesis in Last 15 Years at Dhaka City, Bangladesh: A Retrospective StudyDocument6 pagesPrevalence and Consequence of Customized Ocular Prosthesis in Last 15 Years at Dhaka City, Bangladesh: A Retrospective Studymohammaddu49No ratings yet
- You Et Al-2014-Acta OphthalmologicaDocument9 pagesYou Et Al-2014-Acta OphthalmologicaviviNo ratings yet
- Prevalence and Associated of Occular Morbidity in Luzira-UgandaDocument8 pagesPrevalence and Associated of Occular Morbidity in Luzira-Ugandadramwi edwardNo ratings yet
- Sciencedirect: Prevalence and Etiology of Midfacial Fractures: A Study of 799 CasesDocument6 pagesSciencedirect: Prevalence and Etiology of Midfacial Fractures: A Study of 799 CasesSuci NourmalizaNo ratings yet
- An Injury Profile of Maxillofacial Trauma in Yaounde An Observational Study in CameroonDocument9 pagesAn Injury Profile of Maxillofacial Trauma in Yaounde An Observational Study in CameroonAthenaeum Scientific PublishersNo ratings yet
- Research Article: Prevalence and Risk Factors For Adult Cataract in The Jingan District of ShanghaiDocument7 pagesResearch Article: Prevalence and Risk Factors For Adult Cataract in The Jingan District of ShanghaiIndermeet Singh AnandNo ratings yet
- Joph2016 1438376 PDFDocument6 pagesJoph2016 1438376 PDFdesytrilistyoatiNo ratings yet
- Journal Pone 0268800Document19 pagesJournal Pone 0268800YAP JOON YEE NICHOLASNo ratings yet
- Epidemiological Study of Ocular Trauma in An Urban Slum Population in Delhi, IndiaDocument4 pagesEpidemiological Study of Ocular Trauma in An Urban Slum Population in Delhi, IndiaSitifa AisaraNo ratings yet
- Femi OgundeleDocument8 pagesFemi OgundeleAbdullahi nurudeenNo ratings yet
- Epidemiology of Ocular Tumors 2013Document230 pagesEpidemiology of Ocular Tumors 2013Ranny LaidasuriNo ratings yet
- Eye Banking and Corneal Transplantation in Tertiary Care Hospital Located in Rural AreaDocument6 pagesEye Banking and Corneal Transplantation in Tertiary Care Hospital Located in Rural AreaIOSR Journal of PharmacyNo ratings yet
- Visual Impairment and Blindness in A Population-Based Study of Mashhad, IranDocument8 pagesVisual Impairment and Blindness in A Population-Based Study of Mashhad, IranSubhan Nur RamadhanNo ratings yet
- Managing Myopia Clinical Guide Dec 2020Document12 pagesManaging Myopia Clinical Guide Dec 2020Jorge Ivan Carcache LopezNo ratings yet
- Relationship of Dissociated Vertical Deviation and The Timing of Initial Surgery For Congenital EsotropiaDocument4 pagesRelationship of Dissociated Vertical Deviation and The Timing of Initial Surgery For Congenital EsotropiaMacarena AlvarezNo ratings yet
- Javed and Kashif Split PDF 1674305144401Document4 pagesJaved and Kashif Split PDF 1674305144401criticseyeNo ratings yet
- Prevalence of Blindness in Patients With Uveitis: Original ResearchDocument4 pagesPrevalence of Blindness in Patients With Uveitis: Original ResearchMuhammad RaflirNo ratings yet
- Journal Reading On Fall InjuryDocument20 pagesJournal Reading On Fall InjuryMAE DEVILLANo ratings yet
- Ajcr 4 47Document2 pagesAjcr 4 47paulpiensaNo ratings yet
- Negative G-Force Ocular Trauma Caused by A Rapidly Spinning CarouselDocument4 pagesNegative G-Force Ocular Trauma Caused by A Rapidly Spinning CarouselpaulpiensaNo ratings yet
- Amj 06 560Document5 pagesAmj 06 560paulpiensaNo ratings yet
- Cochrane ShowDocument14 pagesCochrane ShowpaulpiensaNo ratings yet
- En V68n5a5Document5 pagesEn V68n5a5paulpiensaNo ratings yet
- A New Ocular Trauma Score in Pediatric Penetrating Eye InjuriesDocument5 pagesA New Ocular Trauma Score in Pediatric Penetrating Eye InjuriespaulpiensaNo ratings yet
- Newsltr Jan 2012Document112 pagesNewsltr Jan 2012paulpiensaNo ratings yet
- Surgical Treatment of Severely Traumatized Eyes With No Light PerceptionDocument6 pagesSurgical Treatment of Severely Traumatized Eyes With No Light PerceptionpaulpiensaNo ratings yet
- Artikel Jurnal KKN PuyantiDocument6 pagesArtikel Jurnal KKN Puyantipuyanti -No ratings yet
- ATR100 Owners Manual PDFDocument20 pagesATR100 Owners Manual PDFHernan Alberto Orozco CastañoNo ratings yet
- AMI System Using DLMS - White PaperDocument6 pagesAMI System Using DLMS - White PaperBijuNo ratings yet
- Sci 9-DLP 2Document5 pagesSci 9-DLP 2elsie tequinNo ratings yet
- Redox Reactions in 1 ShotDocument66 pagesRedox Reactions in 1 ShotBoss mayank100% (1)
- Balancing Chemical Equations HTML Guide - enDocument2 pagesBalancing Chemical Equations HTML Guide - enMiguel ApazaNo ratings yet
- Hero Project Kedar BBADocument49 pagesHero Project Kedar BBAVinod HeggannaNo ratings yet
- AT8611 Lab QuestionsDocument9 pagesAT8611 Lab QuestionsChirpiNo ratings yet
- 非谓语动词练习题(学生)Document2 pages非谓语动词练习题(学生)huangyj970218No ratings yet
- Nakagami Vs Ricean FadingDocument2 pagesNakagami Vs Ricean Fadingdelwar28No ratings yet
- Week 1 - Assessment #1Document2 pagesWeek 1 - Assessment #1elaineNo ratings yet
- Jackman 1996Document66 pagesJackman 199612545343No ratings yet
- Admission Notification: 3 Floor, Composite Arts Building, Golapbag Golapbag, Burdwan: - 713 104 West Bengal, IndiaDocument3 pagesAdmission Notification: 3 Floor, Composite Arts Building, Golapbag Golapbag, Burdwan: - 713 104 West Bengal, IndiaHemnath Patra দর্শনNo ratings yet
- RRN3901 Spare Parts CatalogDocument11 pagesRRN3901 Spare Parts CatalogleonardomarinNo ratings yet
- PDK 025786 Diagnose enDocument296 pagesPDK 025786 Diagnose enMalek KamelNo ratings yet
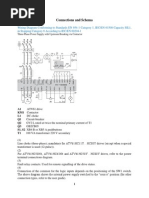
- Connections and SchemaDocument7 pagesConnections and SchemaKukuh WidodoNo ratings yet
- Washing Machine Manual Kenmore HE5tDocument76 pagesWashing Machine Manual Kenmore HE5tmachnerdNo ratings yet
- Flame Tests and Atomic SpectraDocument3 pagesFlame Tests and Atomic SpectraImmanuel LashleyNo ratings yet
- Correlation and RegressionDocument39 pagesCorrelation and RegressionMuhammad Amjad RazaNo ratings yet
- RidleyWorks15 02Document112 pagesRidleyWorks15 02Sergio Omar OrlandoNo ratings yet
- AirValves 2013 PDFDocument268 pagesAirValves 2013 PDFSergio Sebastian Ramirez GamiñoNo ratings yet
- Clinical MedicineDocument18 pagesClinical MedicineRishikesh AsthanaNo ratings yet
- Inquiries Investigation and ImmersionDocument61 pagesInquiries Investigation and Immersionmutsuko100% (4)
- Dec Hanu Tht2 Writing Week 4 - Effect ParagraphDocument11 pagesDec Hanu Tht2 Writing Week 4 - Effect ParagraphHồng BắcNo ratings yet
- Manual Proportional Directional Control Valve (With Pressure Compensation, Multiple Valve Series)Document6 pagesManual Proportional Directional Control Valve (With Pressure Compensation, Multiple Valve Series)Fawzi AlzubairyNo ratings yet
- End Yoke PDFDocument96 pagesEnd Yoke PDFadamtuongNo ratings yet
- Admisie Aer-En 2013Document8 pagesAdmisie Aer-En 2013ionut2007No ratings yet