Professional Documents
Culture Documents
Anesthetic Considerations For Dental Practice: A World Without Pain!
Anesthetic Considerations For Dental Practice: A World Without Pain!
Uploaded by
kca15Copyright:
Available Formats
You might also like
- Sensory Processing 101, by Dayna Abraham, Claire Heffron, Pamela Braley, and Lauren DrobnjakDocument191 pagesSensory Processing 101, by Dayna Abraham, Claire Heffron, Pamela Braley, and Lauren Drobnjakmaribel100% (5)
- WD 4 - Seaside FitnessDocument4 pagesWD 4 - Seaside Fitnessnatalie p0% (4)
- Craniosacral BiodynamicsDocument12 pagesCraniosacral Biodynamicsmilero75% (8)
- Sarepta IR Presentation (October 2017)Document45 pagesSarepta IR Presentation (October 2017)medtechyNo ratings yet
- Setting Free The Bears - D. WegnerDocument12 pagesSetting Free The Bears - D. Wegnerrebeca_latorre100% (1)
- Anxiety and Pain Management in DentalDocument7 pagesAnxiety and Pain Management in DentalNoor SolikhahNo ratings yet
- Orofacialpain:: A PrimerDocument10 pagesOrofacialpain:: A Primeranon_768201406No ratings yet
- CholesteatomaDocument13 pagesCholesteatomaKing KaruNo ratings yet
- Atypical Odontalgia Current Knowledge and Implications For Diagnosis and ManagementDocument5 pagesAtypical Odontalgia Current Knowledge and Implications For Diagnosis and ManagementIma ShofyaNo ratings yet
- PDF 20230624 122205 0000Document36 pagesPDF 20230624 122205 0000Maria EvergardenNo ratings yet
- International Archives of MedicineDocument13 pagesInternational Archives of Medicineqwerty150dNo ratings yet
- Dental Office.Document29 pagesDental Office.Maryam KardoustNo ratings yet
- Inferior Alveolar Nerve Injury Associated With Implant SurgeryDocument8 pagesInferior Alveolar Nerve Injury Associated With Implant SurgerynormaleiNo ratings yet
- Newapproachestopain Management: Orrett E. OgleDocument10 pagesNewapproachestopain Management: Orrett E. OgleNajeeb UllahNo ratings yet
- Introduction To Oral Pathology 1Document32 pagesIntroduction To Oral Pathology 1Hoor M TahanNo ratings yet
- Atypical Facial PainDocument5 pagesAtypical Facial PaindamarstationNo ratings yet
- Emergencies in GPDocument29 pagesEmergencies in GPPrashant MathuriaNo ratings yet
- Rajiv RQ3Document6 pagesRajiv RQ3ravi guptaNo ratings yet
- Anglictina - Maturita - Vyssia Uroven (B2)Document23 pagesAnglictina - Maturita - Vyssia Uroven (B2)ENIGMA PUBLISHINGNo ratings yet
- Diabetic Foot KuliahDocument104 pagesDiabetic Foot KuliahTirta Apriandi100% (1)
- Interdisciplinary DentistryDocument32 pagesInterdisciplinary DentistryNikhil Tyagi100% (1)
- Orthodontics Pain 230624 025230Document33 pagesOrthodontics Pain 230624 025230Maria EvergardenNo ratings yet
- Causes - American Tinnitus AssociationDocument8 pagesCauses - American Tinnitus AssociationJames StroupNo ratings yet
- Definition of Oral Medicine: An Effective Approach To The Patient Who Requires Dental Care Entails The Following StepsDocument9 pagesDefinition of Oral Medicine: An Effective Approach To The Patient Who Requires Dental Care Entails The Following StepsYaser JasNo ratings yet
- Texte EnglezaDocument10 pagesTexte EnglezaRuxi UdreaNo ratings yet
- Orofacial Pain: Clin A/Prof Robert DelcanhoDocument48 pagesOrofacial Pain: Clin A/Prof Robert DelcanhoguhanderNo ratings yet
- Managing The Diabetic FootDocument45 pagesManaging The Diabetic FootArio SabrangNo ratings yet
- Sample Research Paper On Rheumatoid ArthritisDocument8 pagesSample Research Paper On Rheumatoid Arthritisgw32pesz100% (1)
- H. Gremillion-Temporomandibular Disorders and Orafacial Pain, An Issue of Dental Clinics (The Clinics - Dentistry) - Saunders (2007) PDFDocument274 pagesH. Gremillion-Temporomandibular Disorders and Orafacial Pain, An Issue of Dental Clinics (The Clinics - Dentistry) - Saunders (2007) PDFSamuel Flores CalderonNo ratings yet
- Atypical OdontalgiaDocument5 pagesAtypical OdontalgiaMaria Putri NasutionNo ratings yet
- Temporomandibular Joint Disorder ThesisDocument5 pagesTemporomandibular Joint Disorder Thesisheatherdionnemanchester100% (2)
- OSTEOARTHRITISDocument2 pagesOSTEOARTHRITISAssasination ClassroomNo ratings yet
- Osteoarthritis Thesis PDFDocument8 pagesOsteoarthritis Thesis PDFjeanniesuttonminneapolis100% (2)
- Argument SynthesisDocument7 pagesArgument Synthesisapi-309603847No ratings yet
- JurnalDocument12 pagesJurnalRestia07RahmaNo ratings yet
- Homeopathy and DentistryDocument3 pagesHomeopathy and DentistrynadiidaNo ratings yet
- Current Concepts: Review ArticleDocument7 pagesCurrent Concepts: Review ArticleMia Mia MiaNo ratings yet
- 2008-0510 - Otitis Eksterna (Diffusa) PDFDocument14 pages2008-0510 - Otitis Eksterna (Diffusa) PDFEka 'Percival' AnggrainiNo ratings yet
- Ortho Wertz Operative ConsentDocument2 pagesOrtho Wertz Operative ConsentHicham GawishNo ratings yet
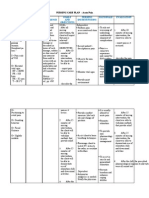
- 1200 Walker MelissaDocument55 pages1200 Walker Melissazano_adamNo ratings yet
- General Medicine ScenarioDocument8 pagesGeneral Medicine ScenarioHayley WelshNo ratings yet
- POK Exam QuestionsDocument6 pagesPOK Exam QuestionsBosco AinaniNo ratings yet
- EAOM HandbookDocument249 pagesEAOM HandbookmadhaNo ratings yet
- Minimally Invasive Surgery for Chronic Pain Management: An Evidence-Based ApproachFrom EverandMinimally Invasive Surgery for Chronic Pain Management: An Evidence-Based ApproachGiorgio PietramaggioriNo ratings yet
- Dissertation Psoriasis ArthritisDocument7 pagesDissertation Psoriasis ArthritisWriteMyPaperOnlineCanada100% (1)
- Common Medical History QuestionsDocument4 pagesCommon Medical History QuestionsvelangniNo ratings yet
- Rheumatoid Arthritis ThesisDocument8 pagesRheumatoid Arthritis ThesisTracy Morgan100% (2)
- Arthritis: 30 Natural Remedies for Treating Arthritis Pain Osteoarthritis, Rheumatoid Arthritis, Gout, Back Pain, Arthritis in Hands & Knees, Arthritis Diet and More!From EverandArthritis: 30 Natural Remedies for Treating Arthritis Pain Osteoarthritis, Rheumatoid Arthritis, Gout, Back Pain, Arthritis in Hands & Knees, Arthritis Diet and More!No ratings yet
- Headache - 2013 - Shephard - Orofacial Pain A Guide For The Headache PhysicianDocument18 pagesHeadache - 2013 - Shephard - Orofacial Pain A Guide For The Headache PhysicianNatalie JaraNo ratings yet
- Encountering Odontogenic PainDocument18 pagesEncountering Odontogenic PainGiTa TAriganNo ratings yet
- All About Arthritis- Find Updated Causes, Symptoms, Diagnostic Tests, New Alternative Treatments, Cures and BreakthroughsFrom EverandAll About Arthritis- Find Updated Causes, Symptoms, Diagnostic Tests, New Alternative Treatments, Cures and BreakthroughsNo ratings yet
- Juliana AuditoryDocument10 pagesJuliana Auditoryomar franklin molina tinocoNo ratings yet
- Jurnal - Relief of PainDocument6 pagesJurnal - Relief of PainChandra NepaNo ratings yet
- Differential Diagnosis For Orofacial Pain, Including Sinusitis, TMD, Trigeminal NeuralgiaDocument10 pagesDifferential Diagnosis For Orofacial Pain, Including Sinusitis, TMD, Trigeminal Neuralgiasiska tiaraNo ratings yet
- Phantom Tooth PainDocument31 pagesPhantom Tooth PainMuchlis Fauzi ENo ratings yet
- Thesis About ArthritisDocument5 pagesThesis About ArthritisVicki Cristol100% (2)
- Psoriatic Arthritis enDocument5 pagesPsoriatic Arthritis enFebrian LodewijkNo ratings yet
- Ijsrp p1486Document6 pagesIjsrp p1486Sandeep KumarNo ratings yet
- OPERATORIA. Henry A. Gremillion Multidisciplinary Diagnosis and Management of Orofacial PainDocument13 pagesOPERATORIA. Henry A. Gremillion Multidisciplinary Diagnosis and Management of Orofacial PainKenigal14No ratings yet
- OsteoporosisDocument39 pagesOsteoporosisSri MahadhanaNo ratings yet
- Computers in MedicineDocument3 pagesComputers in Medicineapi-270568774No ratings yet
- 3 Emergency NursingDocument38 pages3 Emergency NursingDennis N. MuñozNo ratings yet
- Diabetic Foot, Diabetic Foot Ulcer & Diabetic Foot Care: Prepared by Munirah Supervised by DR NaqibDocument49 pagesDiabetic Foot, Diabetic Foot Ulcer & Diabetic Foot Care: Prepared by Munirah Supervised by DR NaqibAfifah SelamatNo ratings yet
- Handbook of Oral Diseases 1 Edition PDFDocument449 pagesHandbook of Oral Diseases 1 Edition PDFEdgar Trujillo Benítez88% (8)
- National Health MissionDocument31 pagesNational Health MissionAlpana Rani DasNo ratings yet
- Research Paper Topics Music TherapyDocument5 pagesResearch Paper Topics Music Therapyjbuulqvkg100% (1)
- Cesarean Delivery Technique Evidence or Tradition A Review of The Evidence-Based DeliveryDocument12 pagesCesarean Delivery Technique Evidence or Tradition A Review of The Evidence-Based DeliveryKrizt Denisse LedezmaNo ratings yet
- USC Fistula Consult LetterDocument4 pagesUSC Fistula Consult LetterDr Rene SoteloNo ratings yet
- 3 NsaidsDocument23 pages3 NsaidsHagai MagaiNo ratings yet
- Nature Deficit DisorderDocument9 pagesNature Deficit Disorderapi-302555293No ratings yet
- Sustenna AntipsikotikDocument31 pagesSustenna Antipsikotiktitik dyahNo ratings yet
- Electrolyte Quintet Potassium PDFDocument6 pagesElectrolyte Quintet Potassium PDFMaria Guadalupe Hernandez Jimenez100% (1)
- Drug Interactions and Hormonal ContraceptionDocument2 pagesDrug Interactions and Hormonal ContraceptionDimpaNo ratings yet
- NCP 28Document9 pagesNCP 28Leanne Joie Lozano100% (1)
- Article 2Document9 pagesArticle 2105070201111009No ratings yet
- 100 Item Exam On Fundamentals of NursingDocument54 pages100 Item Exam On Fundamentals of NursingYen Valien Cugay100% (1)
- Eaclipt Cpe 2019Document9 pagesEaclipt Cpe 2019inas zahraNo ratings yet
- ILS 2014 Final Year Revision LectureDocument54 pagesILS 2014 Final Year Revision LectureokaberntrNo ratings yet
- Biliary Ascariasis 2Document17 pagesBiliary Ascariasis 2Joanna Marie Panganiban100% (1)
- Common Medical AbbreviationsDocument2 pagesCommon Medical AbbreviationsShahad HakimuddinNo ratings yet
- Resolution of Pinguecula-Related Dry Eye Disease ADocument4 pagesResolution of Pinguecula-Related Dry Eye Disease ASylvia MtrianiNo ratings yet
- Virginia HendersonDocument15 pagesVirginia HendersonryanNo ratings yet
- Rheannah Kaitlen WendelDocument2 pagesRheannah Kaitlen Wendelapi-706427623No ratings yet
- Unicool R-404A: Catalogue Number: 905623 Version No: 4.4Document14 pagesUnicool R-404A: Catalogue Number: 905623 Version No: 4.4asdfasdfNo ratings yet
- Deep Vein ThrombosisDocument4 pagesDeep Vein ThrombosisAgatha FeliciaNo ratings yet
- The Biology of CancerDocument20 pagesThe Biology of CancerAlishka Garg59% (22)
- Grant Et Al (2017) Community Psychology Approaches To Intervention With Children and Adolescents.Document17 pagesGrant Et Al (2017) Community Psychology Approaches To Intervention With Children and Adolescents.LocoderemanteNo ratings yet
- Pre and Post Operative ManagementDocument3 pagesPre and Post Operative Managementdrsb54No ratings yet
- 42 Respiratory Insufficiency-Pathophysiology, Diagnosis, Oxygen TherapyDocument73 pages42 Respiratory Insufficiency-Pathophysiology, Diagnosis, Oxygen TherapyLaila AcehNo ratings yet
Anesthetic Considerations For Dental Practice: A World Without Pain!
Anesthetic Considerations For Dental Practice: A World Without Pain!
Uploaded by
kca15Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anesthetic Considerations For Dental Practice: A World Without Pain!
Anesthetic Considerations For Dental Practice: A World Without Pain!
Uploaded by
kca15Copyright:
Available Formats
3/19/2013
Anesthetic
Considerations
for
Dental Practice
A World Without Pain!
Edward P. Heinrichs, D.M.D.
University of Pittsburgh
School
of
Dental Medicine
CIPA
(Congenital Insensitivity to Pain with Anhidrosis)
Rare inherited disorder of the nervous system
which prevents the sensation of pain, heat,
and cold or any real nerve-related sensation.
Can feel pressure.
Anhidrosis body does not sweat
Hyperthermia
Mental Retardation
Infections
Teething
Self-mutilation
Infants rarely survive beyond age 3
Surviving infants do not often survive
beyond age 25
Lip & Tongue Scarring
Fractures
Eye Injuries
3/19/2013
Pain
A World Without Pain????
-Necessary
-Protective
-Can and Must be
Controlled
Public Speaking
Mice
Heights
Common Fears
Typical dental patient of 2013
Dentistry =
Pain
Anxiety
Flying
No fears
Going to the dentist
PAIN!!!!!!!!!!!!!
Phobias
Special Needs
LOCAL ANESTHESIA
in
DENTISTRY
3/19/2013
Emphasis on Pharmacologic
Techniques
How do we overcome pain
and anxiety in the dental office?
Safe and Effective
Behavioral Techniques
-Pharmacology
-Effect on Physiology
-Adverse Effects & Management
Hypnosis
Pharmacologic Approaches
(local anesthetics)
Science Based
Successful Dental
Practice
Spectrum of Pain Control
No
Meds
Nitrous
Oxide
Enteral
+
Nitrous
Gen
Anes
Local Anesthesia
Enteral
I.V.
Complications & Training
Delivery of Treatment
Successful Dental
Practice
(most important)
PLEASANT
Location
Surgical Skills & Outcomes
Interaction with Specialists
Interaction with Patients (Dr. & Staff)
Variety of Procedures Available
Educational Materials
Newsletters
Comfortable Atmosphere
Comfortable Treatment
(hospital or surgicenter)
Surgeon
Assisting Staff
Anesthesiologist
PAINLESS
3/19/2013
Roles of Each
SURGEON
Anesthesiologist
Surgical Procedure
Post-operative instructions
Post-operative prescriptions
Discharge
Follow-up call to patient?
Surgeon
ANESTHESIOLOGIST
Private Practice
Youre on your own
Review health History & vital signs
Determine level of anxiety
Decision on Pre-medication (anxiety)
Explain anesthetic procedure (consent)
Deliver appropriate anesthetic care
Continuous Monitoring & Recording of Data
Post-op Recovery, Instructions, Discharge
Follow-up call to patient?
What makes a good
Anesthesiologist?
Dentist
Anesthesiologist
Surgeon
YOU
Well educated
Well trained
Experienced
Confident
Ability to manage procedures, problems
and/or emergencies to the highest levels
3/19/2013
Patient
(never treat a stranger)
Local Anesthesia
Pharmacology
Toxic doses (one drug vs. two)
Agent (duration to match procedure)
Technique (Infiltration, block, wand, other)
Side-effects
Escort needed?
Health History
Vital Signs
Surgical History (anes & surg)
Bleeding, Infection, others
Anesthetic reactions and/or abnormalities
No history is significant
Chart Stamp
Date _______
Date _______
BP _____
BP _____
Pulse/O2 _______ Wt ____
Pulse/O2 _______ Wt ____
Meds:
Meds:
Allerg:
Allerg:
ROS
ROS:
3/19/2013
Mechanisms of Orofacial Pain & Analgesia
Mechanisms of
Orofacial Pain &
Analgesia
Peripheral Pain Mechanisms
Cutaneous Pain
Dentinal Pain
Inflammatory Pain
Central Pain Mechanisms
Rostral transmission of Pain
Endogenous Pain Suppression
Systems
Mechanisms of Orofacial Pain & Analgesia
Peripheral Pain
(mediated by nociceptors)
Skin, oral mucosa, pulp
A delta fibers
-fast conduction
- response to mechanical stimuli
- not chemical or thermal conductive
- responsible for first pain
- sharp pain
More C fibers than A delta fibers,
however, A delta fibers cover more
overall surface areas.
Skin, oral mucosa, pulp
C fibers
-slow conduction
- thermal, chemical, (mechanical)
- responsible for second pain
- dull, aching, burning (inflammatory)
The trigeminal system is the primary
conveyor of oral-facial pain.
Fifth cranial nerve
Largest of cranial nerves
Opthalmic, maxillary, and mandibular branches
Innervates face, anterior scalp, gingiva, oral
mucous membranes, teeth, anterior tongue,
nasal cavities, sinuses, jaw and tongue
musculature
3/19/2013
Trigeminal Nerve (5th)
Facial Nerve (7th)
taste sensation
Contributors to cutaneous
& orofacial pain
Vagus (10th)
Glossopharyngeal Nerve (9th)
larynx
posterior tongue, oronasal pharynx
Mechanisms of Orofacial Pain & Analgesia
Dental Pain (Peripheral)
Apical foramen of the adult bicuspid
700 - A delta fibers
1800 - C fibers
Pure pain transmission via thermal,
chemical, mechanical stimulation
Electro-pulp testing uses A delta fibers
Transmission of Pain
(pain perception)
Point of Origin
Local Anesthesia
Trigeminal Nucleus Caudalis in Medulla
Local
Anesthesia
Thalamus
Cerebral Cortex
(pain reaction)
END
You might also like
- Sensory Processing 101, by Dayna Abraham, Claire Heffron, Pamela Braley, and Lauren DrobnjakDocument191 pagesSensory Processing 101, by Dayna Abraham, Claire Heffron, Pamela Braley, and Lauren Drobnjakmaribel100% (5)
- WD 4 - Seaside FitnessDocument4 pagesWD 4 - Seaside Fitnessnatalie p0% (4)
- Craniosacral BiodynamicsDocument12 pagesCraniosacral Biodynamicsmilero75% (8)
- Sarepta IR Presentation (October 2017)Document45 pagesSarepta IR Presentation (October 2017)medtechyNo ratings yet
- Setting Free The Bears - D. WegnerDocument12 pagesSetting Free The Bears - D. Wegnerrebeca_latorre100% (1)
- Anxiety and Pain Management in DentalDocument7 pagesAnxiety and Pain Management in DentalNoor SolikhahNo ratings yet
- Orofacialpain:: A PrimerDocument10 pagesOrofacialpain:: A Primeranon_768201406No ratings yet
- CholesteatomaDocument13 pagesCholesteatomaKing KaruNo ratings yet
- Atypical Odontalgia Current Knowledge and Implications For Diagnosis and ManagementDocument5 pagesAtypical Odontalgia Current Knowledge and Implications For Diagnosis and ManagementIma ShofyaNo ratings yet
- PDF 20230624 122205 0000Document36 pagesPDF 20230624 122205 0000Maria EvergardenNo ratings yet
- International Archives of MedicineDocument13 pagesInternational Archives of Medicineqwerty150dNo ratings yet
- Dental Office.Document29 pagesDental Office.Maryam KardoustNo ratings yet
- Inferior Alveolar Nerve Injury Associated With Implant SurgeryDocument8 pagesInferior Alveolar Nerve Injury Associated With Implant SurgerynormaleiNo ratings yet
- Newapproachestopain Management: Orrett E. OgleDocument10 pagesNewapproachestopain Management: Orrett E. OgleNajeeb UllahNo ratings yet
- Introduction To Oral Pathology 1Document32 pagesIntroduction To Oral Pathology 1Hoor M TahanNo ratings yet
- Atypical Facial PainDocument5 pagesAtypical Facial PaindamarstationNo ratings yet
- Emergencies in GPDocument29 pagesEmergencies in GPPrashant MathuriaNo ratings yet
- Rajiv RQ3Document6 pagesRajiv RQ3ravi guptaNo ratings yet
- Anglictina - Maturita - Vyssia Uroven (B2)Document23 pagesAnglictina - Maturita - Vyssia Uroven (B2)ENIGMA PUBLISHINGNo ratings yet
- Diabetic Foot KuliahDocument104 pagesDiabetic Foot KuliahTirta Apriandi100% (1)
- Interdisciplinary DentistryDocument32 pagesInterdisciplinary DentistryNikhil Tyagi100% (1)
- Orthodontics Pain 230624 025230Document33 pagesOrthodontics Pain 230624 025230Maria EvergardenNo ratings yet
- Causes - American Tinnitus AssociationDocument8 pagesCauses - American Tinnitus AssociationJames StroupNo ratings yet
- Definition of Oral Medicine: An Effective Approach To The Patient Who Requires Dental Care Entails The Following StepsDocument9 pagesDefinition of Oral Medicine: An Effective Approach To The Patient Who Requires Dental Care Entails The Following StepsYaser JasNo ratings yet
- Texte EnglezaDocument10 pagesTexte EnglezaRuxi UdreaNo ratings yet
- Orofacial Pain: Clin A/Prof Robert DelcanhoDocument48 pagesOrofacial Pain: Clin A/Prof Robert DelcanhoguhanderNo ratings yet
- Managing The Diabetic FootDocument45 pagesManaging The Diabetic FootArio SabrangNo ratings yet
- Sample Research Paper On Rheumatoid ArthritisDocument8 pagesSample Research Paper On Rheumatoid Arthritisgw32pesz100% (1)
- H. Gremillion-Temporomandibular Disorders and Orafacial Pain, An Issue of Dental Clinics (The Clinics - Dentistry) - Saunders (2007) PDFDocument274 pagesH. Gremillion-Temporomandibular Disorders and Orafacial Pain, An Issue of Dental Clinics (The Clinics - Dentistry) - Saunders (2007) PDFSamuel Flores CalderonNo ratings yet
- Atypical OdontalgiaDocument5 pagesAtypical OdontalgiaMaria Putri NasutionNo ratings yet
- Temporomandibular Joint Disorder ThesisDocument5 pagesTemporomandibular Joint Disorder Thesisheatherdionnemanchester100% (2)
- OSTEOARTHRITISDocument2 pagesOSTEOARTHRITISAssasination ClassroomNo ratings yet
- Osteoarthritis Thesis PDFDocument8 pagesOsteoarthritis Thesis PDFjeanniesuttonminneapolis100% (2)
- Argument SynthesisDocument7 pagesArgument Synthesisapi-309603847No ratings yet
- JurnalDocument12 pagesJurnalRestia07RahmaNo ratings yet
- Homeopathy and DentistryDocument3 pagesHomeopathy and DentistrynadiidaNo ratings yet
- Current Concepts: Review ArticleDocument7 pagesCurrent Concepts: Review ArticleMia Mia MiaNo ratings yet
- 2008-0510 - Otitis Eksterna (Diffusa) PDFDocument14 pages2008-0510 - Otitis Eksterna (Diffusa) PDFEka 'Percival' AnggrainiNo ratings yet
- Ortho Wertz Operative ConsentDocument2 pagesOrtho Wertz Operative ConsentHicham GawishNo ratings yet
- 1200 Walker MelissaDocument55 pages1200 Walker Melissazano_adamNo ratings yet
- General Medicine ScenarioDocument8 pagesGeneral Medicine ScenarioHayley WelshNo ratings yet
- POK Exam QuestionsDocument6 pagesPOK Exam QuestionsBosco AinaniNo ratings yet
- EAOM HandbookDocument249 pagesEAOM HandbookmadhaNo ratings yet
- Minimally Invasive Surgery for Chronic Pain Management: An Evidence-Based ApproachFrom EverandMinimally Invasive Surgery for Chronic Pain Management: An Evidence-Based ApproachGiorgio PietramaggioriNo ratings yet
- Dissertation Psoriasis ArthritisDocument7 pagesDissertation Psoriasis ArthritisWriteMyPaperOnlineCanada100% (1)
- Common Medical History QuestionsDocument4 pagesCommon Medical History QuestionsvelangniNo ratings yet
- Rheumatoid Arthritis ThesisDocument8 pagesRheumatoid Arthritis ThesisTracy Morgan100% (2)
- Arthritis: 30 Natural Remedies for Treating Arthritis Pain Osteoarthritis, Rheumatoid Arthritis, Gout, Back Pain, Arthritis in Hands & Knees, Arthritis Diet and More!From EverandArthritis: 30 Natural Remedies for Treating Arthritis Pain Osteoarthritis, Rheumatoid Arthritis, Gout, Back Pain, Arthritis in Hands & Knees, Arthritis Diet and More!No ratings yet
- Headache - 2013 - Shephard - Orofacial Pain A Guide For The Headache PhysicianDocument18 pagesHeadache - 2013 - Shephard - Orofacial Pain A Guide For The Headache PhysicianNatalie JaraNo ratings yet
- Encountering Odontogenic PainDocument18 pagesEncountering Odontogenic PainGiTa TAriganNo ratings yet
- All About Arthritis- Find Updated Causes, Symptoms, Diagnostic Tests, New Alternative Treatments, Cures and BreakthroughsFrom EverandAll About Arthritis- Find Updated Causes, Symptoms, Diagnostic Tests, New Alternative Treatments, Cures and BreakthroughsNo ratings yet
- Juliana AuditoryDocument10 pagesJuliana Auditoryomar franklin molina tinocoNo ratings yet
- Jurnal - Relief of PainDocument6 pagesJurnal - Relief of PainChandra NepaNo ratings yet
- Differential Diagnosis For Orofacial Pain, Including Sinusitis, TMD, Trigeminal NeuralgiaDocument10 pagesDifferential Diagnosis For Orofacial Pain, Including Sinusitis, TMD, Trigeminal Neuralgiasiska tiaraNo ratings yet
- Phantom Tooth PainDocument31 pagesPhantom Tooth PainMuchlis Fauzi ENo ratings yet
- Thesis About ArthritisDocument5 pagesThesis About ArthritisVicki Cristol100% (2)
- Psoriatic Arthritis enDocument5 pagesPsoriatic Arthritis enFebrian LodewijkNo ratings yet
- Ijsrp p1486Document6 pagesIjsrp p1486Sandeep KumarNo ratings yet
- OPERATORIA. Henry A. Gremillion Multidisciplinary Diagnosis and Management of Orofacial PainDocument13 pagesOPERATORIA. Henry A. Gremillion Multidisciplinary Diagnosis and Management of Orofacial PainKenigal14No ratings yet
- OsteoporosisDocument39 pagesOsteoporosisSri MahadhanaNo ratings yet
- Computers in MedicineDocument3 pagesComputers in Medicineapi-270568774No ratings yet
- 3 Emergency NursingDocument38 pages3 Emergency NursingDennis N. MuñozNo ratings yet
- Diabetic Foot, Diabetic Foot Ulcer & Diabetic Foot Care: Prepared by Munirah Supervised by DR NaqibDocument49 pagesDiabetic Foot, Diabetic Foot Ulcer & Diabetic Foot Care: Prepared by Munirah Supervised by DR NaqibAfifah SelamatNo ratings yet
- Handbook of Oral Diseases 1 Edition PDFDocument449 pagesHandbook of Oral Diseases 1 Edition PDFEdgar Trujillo Benítez88% (8)
- National Health MissionDocument31 pagesNational Health MissionAlpana Rani DasNo ratings yet
- Research Paper Topics Music TherapyDocument5 pagesResearch Paper Topics Music Therapyjbuulqvkg100% (1)
- Cesarean Delivery Technique Evidence or Tradition A Review of The Evidence-Based DeliveryDocument12 pagesCesarean Delivery Technique Evidence or Tradition A Review of The Evidence-Based DeliveryKrizt Denisse LedezmaNo ratings yet
- USC Fistula Consult LetterDocument4 pagesUSC Fistula Consult LetterDr Rene SoteloNo ratings yet
- 3 NsaidsDocument23 pages3 NsaidsHagai MagaiNo ratings yet
- Nature Deficit DisorderDocument9 pagesNature Deficit Disorderapi-302555293No ratings yet
- Sustenna AntipsikotikDocument31 pagesSustenna Antipsikotiktitik dyahNo ratings yet
- Electrolyte Quintet Potassium PDFDocument6 pagesElectrolyte Quintet Potassium PDFMaria Guadalupe Hernandez Jimenez100% (1)
- Drug Interactions and Hormonal ContraceptionDocument2 pagesDrug Interactions and Hormonal ContraceptionDimpaNo ratings yet
- NCP 28Document9 pagesNCP 28Leanne Joie Lozano100% (1)
- Article 2Document9 pagesArticle 2105070201111009No ratings yet
- 100 Item Exam On Fundamentals of NursingDocument54 pages100 Item Exam On Fundamentals of NursingYen Valien Cugay100% (1)
- Eaclipt Cpe 2019Document9 pagesEaclipt Cpe 2019inas zahraNo ratings yet
- ILS 2014 Final Year Revision LectureDocument54 pagesILS 2014 Final Year Revision LectureokaberntrNo ratings yet
- Biliary Ascariasis 2Document17 pagesBiliary Ascariasis 2Joanna Marie Panganiban100% (1)
- Common Medical AbbreviationsDocument2 pagesCommon Medical AbbreviationsShahad HakimuddinNo ratings yet
- Resolution of Pinguecula-Related Dry Eye Disease ADocument4 pagesResolution of Pinguecula-Related Dry Eye Disease ASylvia MtrianiNo ratings yet
- Virginia HendersonDocument15 pagesVirginia HendersonryanNo ratings yet
- Rheannah Kaitlen WendelDocument2 pagesRheannah Kaitlen Wendelapi-706427623No ratings yet
- Unicool R-404A: Catalogue Number: 905623 Version No: 4.4Document14 pagesUnicool R-404A: Catalogue Number: 905623 Version No: 4.4asdfasdfNo ratings yet
- Deep Vein ThrombosisDocument4 pagesDeep Vein ThrombosisAgatha FeliciaNo ratings yet
- The Biology of CancerDocument20 pagesThe Biology of CancerAlishka Garg59% (22)
- Grant Et Al (2017) Community Psychology Approaches To Intervention With Children and Adolescents.Document17 pagesGrant Et Al (2017) Community Psychology Approaches To Intervention With Children and Adolescents.LocoderemanteNo ratings yet
- Pre and Post Operative ManagementDocument3 pagesPre and Post Operative Managementdrsb54No ratings yet
- 42 Respiratory Insufficiency-Pathophysiology, Diagnosis, Oxygen TherapyDocument73 pages42 Respiratory Insufficiency-Pathophysiology, Diagnosis, Oxygen TherapyLaila AcehNo ratings yet