Professional Documents
Culture Documents
Coronary Angiographic Morphology in Myocardial Infarction: A Link Between The Pathogenesis of Unstable Angina and Myocardial Infarction
Coronary Angiographic Morphology in Myocardial Infarction: A Link Between The Pathogenesis of Unstable Angina and Myocardial Infarction
Uploaded by
Sabila RosyidaCopyright:
Available Formats
You might also like
- FCCS - Pediatric Vs Adult ConsiderationDocument13 pagesFCCS - Pediatric Vs Adult ConsiderationludiNo ratings yet
- Eriksen Et Al-2002-Clinical Cardiology PDFDocument5 pagesEriksen Et Al-2002-Clinical Cardiology PDFmedskyqqNo ratings yet
- 2000 - Stamm Et Al. - Surgery For Bilateral Outflow Tract Obstruction in Elastin ArteriopathyDocument9 pages2000 - Stamm Et Al. - Surgery For Bilateral Outflow Tract Obstruction in Elastin ArteriopathybanupluNo ratings yet
- Circulation 1973 ALONSO 588 96Document10 pagesCirculation 1973 ALONSO 588 96Jessica ARNo ratings yet
- 29 Full PDFDocument7 pages29 Full PDFDHIVYANo ratings yet
- Tortuosity,: Coiling, and Kinking of Internal Carotid ArteryDocument13 pagesTortuosity,: Coiling, and Kinking of Internal Carotid ArteryRoberto AmayaNo ratings yet
- Acosta 2003Document5 pagesAcosta 2003Mihaela MocanNo ratings yet
- BR Heart J 1985 Hartnell 392 5Document5 pagesBR Heart J 1985 Hartnell 392 5phng77No ratings yet
- Acs 03 03 234Document13 pagesAcs 03 03 234IwanNo ratings yet
- Jurnal Coronary Artery FistulaDocument3 pagesJurnal Coronary Artery FistulaRistinyaUnuyNo ratings yet
- Discrete Atherosclerotic Coronary Artery Aneurysms: A Study of 20 PatientsDocument4 pagesDiscrete Atherosclerotic Coronary Artery Aneurysms: A Study of 20 PatientsaudiNo ratings yet
- Scientific Letters: Rev Esp Cardiol. 2016 69 (3) :337-349Document2 pagesScientific Letters: Rev Esp Cardiol. 2016 69 (3) :337-349luisNo ratings yet
- Disseccao Tipo b2Document6 pagesDisseccao Tipo b2coopervascba.diradmNo ratings yet
- Cell Therapy in Patients With Left Ventricular Dysfunction Due To Myocardial InfarctionDocument10 pagesCell Therapy in Patients With Left Ventricular Dysfunction Due To Myocardial InfarctionMrityunjay PathakNo ratings yet
- The Fate of The Distal Aorta After Repair of Acute Type A Aortic DissectionDocument10 pagesThe Fate of The Distal Aorta After Repair of Acute Type A Aortic Dissectionapi-160333876No ratings yet
- Circulation 1975 Burggraf 146 56Document12 pagesCirculation 1975 Burggraf 146 56Zikri Putra Lan LubisNo ratings yet
- Anatomic Features and Surgical Strategies in Double-Outlet Right VentricleDocument18 pagesAnatomic Features and Surgical Strategies in Double-Outlet Right VentriclesuckeydluffyNo ratings yet
- Principles in The Management of Arterial Injuries Associated With Fracture DislocationsDocument5 pagesPrinciples in The Management of Arterial Injuries Associated With Fracture DislocationsJohannes CordeNo ratings yet
- Pi Is 0003497505012002Document5 pagesPi Is 0003497505012002Tri RachmadijantoNo ratings yet
- Ect AsiaDocument4 pagesEct Asiajessik zavalaNo ratings yet
- s0735 1097 (85) 80117 0Document8 pagess0735 1097 (85) 80117 0John DoeNo ratings yet
- Echocardiographic Features of Total Anomalous Pulmonary: VenousDocument8 pagesEchocardiographic Features of Total Anomalous Pulmonary: VenousTanuj VermaNo ratings yet
- Revisión de Disección Celíaca y EsplénicaDocument5 pagesRevisión de Disección Celíaca y EsplénicaLuis AlfonsoNo ratings yet
- Short-And Long-Term Outcomes of Acute Upper Extremity Arterial ThromboembolismDocument4 pagesShort-And Long-Term Outcomes of Acute Upper Extremity Arterial ThromboembolismWilhelm HeinleinNo ratings yet
- Delayed Pericardial Effusion Following Stab Wounds To The ChestDocument4 pagesDelayed Pericardial Effusion Following Stab Wounds To The Chestapi-541676441No ratings yet
- Atrial Hemangioma A Case Report and Review of The LiteratureDocument11 pagesAtrial Hemangioma A Case Report and Review of The LiteratureSaya MenarikNo ratings yet
- 1 s2.0 S0929664608602041 MainDocument9 pages1 s2.0 S0929664608602041 MainEko SiswantoNo ratings yet
- ICA AneurismDocument6 pagesICA AneurismnaimNo ratings yet
- Paracardiac Masses Caused A Right Coronary Artery Aneurysm and A Saphenous Vein Graft AneurysmDocument3 pagesParacardiac Masses Caused A Right Coronary Artery Aneurysm and A Saphenous Vein Graft AneurysmSheikh Mizanur RahmanNo ratings yet
- Angiography 50%Document17 pagesAngiography 50%Nova SipahutarNo ratings yet
- Open Fixation in Flail Chest: Review of 64 Patients: Riginal OntributionDocument6 pagesOpen Fixation in Flail Chest: Review of 64 Patients: Riginal OntributionDian PermatasariNo ratings yet
- Anilllo VascularDocument5 pagesAnilllo VascularKendy LópezNo ratings yet
- Left Hemothorax: Unusual Manifestation of Aortic DissectionDocument5 pagesLeft Hemothorax: Unusual Manifestation of Aortic DissectionIJAR JOURNALNo ratings yet
- Predictive Value of Angiographic Testing For Tolerance To Therapeutic Occlusion of The Carotid ArteryDocument4 pagesPredictive Value of Angiographic Testing For Tolerance To Therapeutic Occlusion of The Carotid ArteryCarol ArtigasNo ratings yet
- Effect of Left Ventricular Outflow Tract Obstruction On Clinical Outcome in Hypertrophic CardiomyopathyDocument9 pagesEffect of Left Ventricular Outflow Tract Obstruction On Clinical Outcome in Hypertrophic CardiomyopathyAstrid Noviera IksanNo ratings yet
- Cairns 1976Document14 pagesCairns 1976Direvald WesterosNo ratings yet
- Duplex Guided Balloon Angioplasty and Subintimal DDocument8 pagesDuplex Guided Balloon Angioplasty and Subintimal DJose PiulatsNo ratings yet
- CoronariesDocument9 pagesCoronariesbanzicaaNo ratings yet
- Cardiac ValveDocument9 pagesCardiac Valveikbal rambalinoNo ratings yet
- Angeborene Koronarfisteln - Die Häufigste Angeborene KoronaranomalieDocument8 pagesAngeborene Koronarfisteln - Die Häufigste Angeborene KoronaranomalieCHENo ratings yet
- Aortic Regurgitation: Clinical PracticeDocument8 pagesAortic Regurgitation: Clinical PracticeChintya Fidelia MontangNo ratings yet
- Bmjcred00241 0003Document2 pagesBmjcred00241 0003Shafa AudryNo ratings yet
- Pathophysiology, Diagnosis, and Medical Management of Nonsurgical PatientsDocument14 pagesPathophysiology, Diagnosis, and Medical Management of Nonsurgical PatientsVanitha Ratha KrishnanNo ratings yet
- tmp53D3 TMPDocument8 pagestmp53D3 TMPFrontiersNo ratings yet
- Shaggy Aorta 8Document1 pageShaggy Aorta 8Eghet SilviuNo ratings yet
- 45 1057Document5 pages45 1057Gabriela PinticanNo ratings yet
- Hollehorst PlaquesDocument3 pagesHollehorst PlaquesErick Roa GandicaNo ratings yet
- Jurnal Astra ACSDocument30 pagesJurnal Astra ACSEta EtiiNo ratings yet
- 405 2013 Article 2598Document5 pages405 2013 Article 2598M Shiddiq GhiffariNo ratings yet
- Aranda 1998Document5 pagesAranda 1998Sarly FebrianaNo ratings yet
- Adult Choroidal Vein of Galen MalformationDocument5 pagesAdult Choroidal Vein of Galen MalformationSonia Prima Arisa PutriNo ratings yet
- Wa0005Document7 pagesWa0005nandawahyuseptiaNo ratings yet
- Ekim, H. y Tuncer, M. (2009) - Manejo de Lesiones Traumáticas de La Arteria Braquial Informe de 49 PacientesDocument5 pagesEkim, H. y Tuncer, M. (2009) - Manejo de Lesiones Traumáticas de La Arteria Braquial Informe de 49 PacientesEdgar Geovanny Cardenas FigueroaNo ratings yet
- Frequency of Coronary Artery Disease in Valvular Aortic Stenosis :experience of The Cardiology Center of Mohamed V Military Hospital About 148 CasesDocument5 pagesFrequency of Coronary Artery Disease in Valvular Aortic Stenosis :experience of The Cardiology Center of Mohamed V Military Hospital About 148 CasesIJAR JOURNALNo ratings yet
- Percutaneous Transluminal Angioplasty and Stenting As First-Choice Treatment in Patients With Chronic Mesenteric IschemiaDocument6 pagesPercutaneous Transluminal Angioplasty and Stenting As First-Choice Treatment in Patients With Chronic Mesenteric IschemiaCotaga IgorNo ratings yet
- Aortic D RefferatDocument5 pagesAortic D RefferatRachman IbrahimNo ratings yet
- Echo Case Ao RegurgDocument3 pagesEcho Case Ao Regurgdgina8800No ratings yet
- Spon Artery DissceDocument6 pagesSpon Artery DissceMuhammad JunaidNo ratings yet
- Griffith 1996Document10 pagesGriffith 1996Sowmya ANo ratings yet
- Intrinsic Third Ventricular Craniopharyngiomas: Report On Six Cases and A Review of The LiteratureDocument8 pagesIntrinsic Third Ventricular Craniopharyngiomas: Report On Six Cases and A Review of The LiteratureAmina GoharyNo ratings yet
- Advancements in Acute Aortic Syndrome: From Pathophysiology to Personalized TherapeuticsFrom EverandAdvancements in Acute Aortic Syndrome: From Pathophysiology to Personalized TherapeuticsNo ratings yet
- Follow Up Pasien (29 Juli-11 Agustus 2017) : S o Demam (+)Document6 pagesFollow Up Pasien (29 Juli-11 Agustus 2017) : S o Demam (+)Sabila RosyidaNo ratings yet
- Daftar Pustaka: Universitas Lambung MangkuratDocument3 pagesDaftar Pustaka: Universitas Lambung MangkuratSabila RosyidaNo ratings yet
- Acute Renal Failure: Definitions, Diagnosis, Pathogenesis, and TherapyDocument10 pagesAcute Renal Failure: Definitions, Diagnosis, Pathogenesis, and TherapySabila RosyidaNo ratings yet
- Mekanisme:: Types of VomitingDocument3 pagesMekanisme:: Types of VomitingSabila RosyidaNo ratings yet
- Proposal Kegiatan Bakti Sosial " ": Asam-Asam Sehat Bersama FK UnlamDocument1 pageProposal Kegiatan Bakti Sosial " ": Asam-Asam Sehat Bersama FK UnlamSabila RosyidaNo ratings yet
- Anorectal MalformationDocument4 pagesAnorectal MalformationSabila RosyidaNo ratings yet
- Table 1Document1 pageTable 1Sabila RosyidaNo ratings yet
- 年 1 月 TOEFL 试题: Section One: Listening ComprehensionDocument16 pages年 1 月 TOEFL 试题: Section One: Listening ComprehensionSabila RosyidaNo ratings yet
- New England Journal Medicine: The ofDocument11 pagesNew England Journal Medicine: The ofnenda nurfendaNo ratings yet
- Chronic Total Occlusions: Emmanouil S. Brilakis, MD, PHDDocument69 pagesChronic Total Occlusions: Emmanouil S. Brilakis, MD, PHDсергейNo ratings yet
- TachycardiaDocument12 pagesTachycardiaPuskesmas Pinang JayaNo ratings yet
- PWKI Art 23954-10Document5 pagesPWKI Art 23954-10Oeij Henri WijayaNo ratings yet
- CV Template TeachingDocument3 pagesCV Template Teachingmohammadrezahajian12191No ratings yet
- An Assignment On Surgery subject:-SHOCK (Definition, Classification and Pathophysiology of Shock)Document8 pagesAn Assignment On Surgery subject:-SHOCK (Definition, Classification and Pathophysiology of Shock)manish soniNo ratings yet
- Quiz Results: NURS 502 Med / Surg Cardiovascular System Correct Answers: 7Document7 pagesQuiz Results: NURS 502 Med / Surg Cardiovascular System Correct Answers: 7Moshi LoveNo ratings yet
- Pharma Q From BooksDocument6 pagesPharma Q From BooksJhayneNo ratings yet
- US Hypertension Review GuidelinesDocument12 pagesUS Hypertension Review Guidelinesmefav7778520100% (1)
- Appeal Chaitanya Ashok Chate - Y PDFDocument1 pageAppeal Chaitanya Ashok Chate - Y PDFrahulsaini855No ratings yet
- Human Cardiovascular PhysiologyDocument5 pagesHuman Cardiovascular PhysiologyKirsten CruzadoNo ratings yet
- Cardioversion of Atrial Fibrillation in Obese Patients: Results From The Cardioversion-BMI Randomized Controlled TrialDocument22 pagesCardioversion of Atrial Fibrillation in Obese Patients: Results From The Cardioversion-BMI Randomized Controlled TrialAttilio Del RossoNo ratings yet
- 15-Lead ECG PowerpointDocument20 pages15-Lead ECG Powerpointgillian102290No ratings yet
- AED PowerPointDocument78 pagesAED PowerPointPetar RajicNo ratings yet
- HPNDocument32 pagesHPNkaren GoNo ratings yet
- Picco Technology Clinical Evidence Brochure en Non - UsDocument25 pagesPicco Technology Clinical Evidence Brochure en Non - UsRichard DaiNo ratings yet
- Aortic GuidelinesDocument62 pagesAortic GuidelinesAmy Hoo Hui MayNo ratings yet
- Cardiology Clinical CasesDocument13 pagesCardiology Clinical CasesKareem Waleed Ibrahim Hamimy100% (1)
- Bls QuestionDocument7 pagesBls Questionmonir61100% (2)
- Arm Blood Pressure Differences 'Predict Death RiskDocument2 pagesArm Blood Pressure Differences 'Predict Death RiskCarolina RusselNo ratings yet
- Echo Guidelines For Chamber QuantificationDocument24 pagesEcho Guidelines For Chamber QuantificationOnon EssayedNo ratings yet
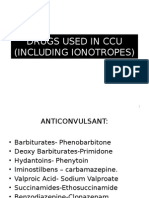
- Drugs Used in CcuDocument169 pagesDrugs Used in CcuAnusha Verghese100% (3)
- Common Emergency DrugsDocument58 pagesCommon Emergency Drugshatem alsrour85% (20)
- Chest TraumaDocument47 pagesChest Traumafrenee aradanasNo ratings yet
- 468-Article Text-964-1-10-20171113Document3 pages468-Article Text-964-1-10-20171113ahmadalipoland25No ratings yet
- Practice/monograph/70/basics/classification - HTML) : DVT: Lower ExtremityDocument2 pagesPractice/monograph/70/basics/classification - HTML) : DVT: Lower ExtremityAyu Putri Firda NNo ratings yet
- Bader Madoukh, Ayman Battisha, Henry Ukwu, Mohammed Al-Sadawi, Shakil ShaikhDocument4 pagesBader Madoukh, Ayman Battisha, Henry Ukwu, Mohammed Al-Sadawi, Shakil ShaikhputriayuratnasariNo ratings yet
- Blood Pressure Solution The Step by Step Guide To Lowering HighDocument112 pagesBlood Pressure Solution The Step by Step Guide To Lowering HighMostafa SayedNo ratings yet
- Chapter 4 - Mixed Venous Oxygen SaturationDocument3 pagesChapter 4 - Mixed Venous Oxygen SaturationJamesNo ratings yet
Coronary Angiographic Morphology in Myocardial Infarction: A Link Between The Pathogenesis of Unstable Angina and Myocardial Infarction
Coronary Angiographic Morphology in Myocardial Infarction: A Link Between The Pathogenesis of Unstable Angina and Myocardial Infarction
Uploaded by
Sabila RosyidaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Coronary Angiographic Morphology in Myocardial Infarction: A Link Between The Pathogenesis of Unstable Angina and Myocardial Infarction
Coronary Angiographic Morphology in Myocardial Infarction: A Link Between The Pathogenesis of Unstable Angina and Myocardial Infarction
Uploaded by
Sabila RosyidaCopyright:
Available Formats
lACC Vol. 6, No.
1233
December 19X5:1233-X
CLINICAL STUDIES
Coronary Angiographic Morphology in Myocardial Infarction:
A Link Between the Pathogenesis of Unstable Angina and
Myocardial Infarction
JOHN A, AMBROSE, MD, FACC,* STEPHEN L.WINTERS, MD,* ROHIT R, ARORA, MD,*
JACOB I. HAFT, MD, FACC,t JONATHAN GOLDSTEIN, MD, FACC,t
K, PETER RENTROP, MD, FACC,* RICHARD GORLIN, MD, FACC,*
VALENTIN FUSTER, MD, FACC*
New York, New York and Newark, New Jerse\'
It has previously been shown that analysis of coronary
morphology can separate unstable from stable angina.
An eccentric stenosis with a narrow neck or irregular
borders, or both, is very common in patients who present
with acute unstable angina, whereas it is rare in patients
with stable angina. To extend these observations to myo
cardial infarction, the coronary morphology of 41 pa
tients with acute or recent infarction and nontotally oc
cluded infarct vessels was studied. For all patients, 27
(66%) of 41 infarct vessels contained this eccentric nar
rowing, whereas only 2 (11 %) of 18 noninfarct vessels
with narrowing of 50 to less than 100% had this lesion
(p < 0.001). In addition, a separate group of patients
with acute myocardial infarction who underwent intra
coronary streptokinase infusion were also analyzed in
similar fashion. Fourteen (61 %) of 23 infarct vessels
contained this lesion after streptokinase infusion com-
Acute coronary occlusion is the usual cause of transmural
myocardial infarction. Angiography at the time of infarction
has demonstrated thrombotic occlusion of a stenotic artery
in 70 to 90% of infarct vessels. whereas in the remaining
cases a severely stenotic artery without total occlusion is
found (1,2). Pathologic studies (3,4) in patients whose death
was due to infarction or sudden, or both, have shown that
a thrombus is usually superimposed on a ruptured athero
sclerotic plaque. Although the appearance of these compli-
From the *Department of Medicine. Division of Cardiology. Mount
Sinai Medical Center. New York. New York and tDivision of Cardiology.
St. Michael's Hospital. Newark. New Jersey. Manuscript received January
10. 1985; revised manuscript received February 20. 1985. accepted May
8. 1985.
Address for reprints: John A. Ambrose. MD. Division of Cardiology,
Mount Sinai Medical Center. One Gustave L. Levy Place. New York.
New York 10029.
(<)
19X5 by the American College of Cardiology
Downloaded From: http://content.onlinejacc.org/ on 12/08/2014
pared with 1 (9%) of 11 non infarct vessels with narrow
ing of 50 to less than 100% (p < 0.01).
Therefore, an eccentric coronary stenosis with a nar
row neck or irregular borders, or both, is the most coni
mon morphologic feature on angiography in both acute
and recent infarction as well as unstable angina. This
lesion probably represents either a disrupted athero
sclerotic plaque or a partially occlusive or lysed throm
bus, or both. The predominance of this morphology in
both unstable angina and acute infarction suggests a
possible link between these two conditions. Unstable an
gina and myocardial infarction may form a continuous
spectrum with the clinical outcome dependent on the
subsequent change in coronary supply relative to myo
cardial demand.
(J Am Coil CardioI1985;6:1233-8)
cated atherosclerotic lesions has been described by Levin
and Fallon (5) at postmortem angiography, the qualitative
appearance of coronary lesions at routine angiography in
patients with acute myocardial infarction has not been reported.
We have previously shown (6) in a consecutive series of
patients evaluated because of angina that patients presenting
with acute unstable angina often have a characteristic coro
nary lesion. An eccentric stenosis with a narrow neck due
to one or more overhanging edges or irregular borders, or
both. was found in the majority of these patients. In patients
whose presumed "angina-producing" vessel could be iden
tified, this lesion was found in 71 % of vessels in patients
with unstable angina, compared with only 16% of vessels
in patients with stable angina (p < 0.001). Not only was
this lesion a sensitive indicator of unstable angina, it was
infrequent in obstructed arteries that were not "angina-pro
ducing" vessels. It was postulated that these lesions possibly
0735-1097/85/$3.30
1234
AMBROSE ET AL.
MORPHOLOGY IN MYOCARDIAL INFARCTION
lACC Vol. 6. No.6
December 1985: 1233-8
represent disrupted plaques or partially occlusive or lysed
thrombi, or both. Unstable angina is often a precursor of
myocardial infarction and both conditions may present acutely
and suddenly. Therefore, morphologic analysis of coronary
lesions in myocardial infarction may show similarities to
the coronary lesions in unstable angina.
CONCENTRIC LESIONS
TYP',(R>'([D
ECCENTRIC LESIONS
Methods
Patients. Angiographic data were reviewed in all pa
tients with acute or recent 3 months) infarction referred
for cardiac catheterization to Mount Sinai Hospital between
September 1981 and April 1984. In all patients myocardial
infarction was documented by a characteristic history of
prolonged chest pain, by diagnostic electrocardiographic
changes and by elevated serum cardiac enzymes. Only pa
tients in whom characteristic electrocardiographic changes
or wall motion abnormalities, or both, could confidently
localize a nontotally occluded infarct vessel at angiography
were stUdied. Totally occluded infarct vessels were elimi
nated because of inability to assess morphology.
Series J. Of the 50 angiograms that fulfilled these cri
teria, seven were eliminated because of inadequate visual
ization of the coronary lesion in the infarct vessel and two
because of inability to characterize the lesion. The remaining
41 films represent approximately 33% of all patients with
acute or recent infarction who underwent catheterization at
t/lis institution. The remaining patients either had an infarct
vessel that was totally occluded at the time of angiography
or were part of an ongoing randomized trial on the effects
of intracoronary streptokinase and were therefore not in
cluded in the analysis.
Three groups of patients were identified in the 41 study
patients. Group I comprised 13 patients who underwent
angiography within 12 hours of acute infarction. Although
all patients in Group I received intracoronary streptokinase,
only the pre intervention angiograms were analyzed. These
patients were part of a completed pilot trial at Mount Sinai
Hospital on the effects of intracoronary streptokinase in
acute myocardial infarction and the final report of this study
has been published (7). Group II comprised II patients
studied 1 to 2 weeks after infarction, all of whom had been
treated with full dose anticoagulation therapy. This group
included patients in the medically treated control group of
this same pilot trial who underwent routine catheterization
I to 2 weeks after infarction. Group III comprised 17 pa
tients with recent infarction (2 to 10 weeks) referred for
catheterization because of postinfarction chest pain, young
age or a positive exercise test. The mean age of patients
was 53 years and there were no significant differences among
the three groups. Of the 28 patients in Groups II and III,
23 had severe hypokinesia or akinesia in the distribution of
the infarct vessel as assessed by left ventricular angiography.
Downloaded From: http://content.onlinejacc.org/ on 12/08/2014
T,,,n
(]~>,
MULTI PLE IRREGULARITIES
CD
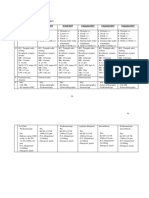
Figure 1. Schematic drawings of the morphologic findings in
coronary artery disease. Concentric lesions were symmetric and
usually smooth. Type I eccentric lesions were asymmetric and
smooth. Most type I lesions were like those depicted on the right
side of the diagram. Type II eccentric lesions either were smooth
with a narrow neck (left side) or had irregular borders (right side).
Multiple irregularities included vessels with serial lesions or severe
diffuse disease.
Series 2. After the initial analysis of these data, a second
series of angiograms was analyzed. The data on 36 patients
with acute infarction and intracoronary streptokinase infu
sion were reviewed. All films were analyzed as described
by the same angiographers who reviewed the first set of
films. These patients represented a consecutive series of
Table 1. Coronary Morphology of the Infarct Vessel in Acute
or Recent Myocardial Infarction (Series 1,41 Cases)
Coronary Morphology
Conc
Type II
Group I
(n = 13)
Group II
(n = II)
Group III
(n = 17)
Total
12
27 (66%)
9 (22%)
Stenosis
Other
(%)*
83 8
84 10
87 9
5 (12%)
*Mean
SD. Conc
concentric lesions; Other
phologies: Type II = type II eccentric lesions.
other mor-
patients with acute infarction admitted to a single hospital
(St. Michael's Hospital) who underwent angiography within
12 hours of the onset of chest pain, From the group of 36
patients, 4 were eliminated because of inadequate films, In
all patients the infarct vessel was localized at angiography
and a loading dose of 10,000 U of streptokinase was directly
infused into the coronary artery followed by a continuous
infusion of 4,000 U/min for a total of 35 to 120 minutes.
In 26 of the 32 patients, the infarct vessel was initially totally
occluded and 17 of these arteries were reperfused (Group I
SK), In the other six patients the infarct vessel was not
totally occluded before streptokinase infusion (Group II SK).
The mean dose of streptokinase was 308,000 U (range 135,000
to 500,000) and dosages were similar among patient groups.
Coronary arteriography. All coronary angiographic
studies were performed from either the brachial or femoral
approach using standard catheters and techniques. All coro-
Figure 2. Selected angiographic images from two patients with a
type II lesion. Top, The arrow points to the type II lesion in the
proximal left anterior descending artery as seen in the right anterior
oblique projection. Bottom, The arrow points to the type II lesion
in the mid right coronary artery as seen in the left anterior oblique
projection.
1235
AMBROSE ET AL.
MORPHOLOGY IN MYOCARDIAL INFARCTION
lACC Va!. 6, No.6
December 1985: 1233~8
Table 2. Coronary Morphology of the Infarct Vessel in
Myocardial Infarction Before and After Reperfusion With
Streptokinase (Series 2, 23 Cases)
Prestreptokinase
Coronary
Morphology
Poststreptokinase
Coronary
Morphology
Type II Cone Other Type II
Group I SK
(n = 17)
Group II SK
(n = 6)
Total
10
4
Cone
Other
Stenosis
(%)
83 II
83 8
4
14
(61%)
4
5
(22%) (17%)
Abbreviations as in Table I.
nary obstructions greater than 50% occlusive were traced
on transparent paper in two views by the same angiographer
and each obstruction was measured with a millimeter rule
and compared with the "normal" proximal juxtaposed seg
ment. Coronary lesions were morphologically classified by
a consensus of three angiographers based on qualitative
analysis of each lesion (Fig. 1), The details of the quanti
tative and qualitative analyses have been previously de
scribed (6).
Lesions were classified into one of four categories: 1)
concentric stenosis-symmetric and smooth narrowing of
the coronary artery; 2,3) eccentric stenosis-asymmetric
narrowing of the coronary artery, with two subgroups cat
egorized: type I eccentric lesion (asymmetric stenosis with
smooth borders and a broad neck) and type II eccentric
lesion (asymmetric stenosis in the form of a convex intra
luminal obstruction with a narrow base due to one or more
overhanging edges or extremely irregular or scalloped bor
ders, or both); 4) multiple irregularities-three or more se
rial and closely spaced severe obstructions or severe diffuse
irregularities in a coronary artery. Intra- and interobserver
variability for categorizing a lesion into its morphologic
subset was 95 and 88%, respectively. All quantitative and
qualitative analyses in patients given streptokinase were per
formed at the end of the streptokinase infusion. In patients
given streptokinase whose infarct vessel was not totally
occluded, lesions were compared before and at the end of
the infusion.
Statistical analyses. All analyses between groups were
performed using the two-tailed Student's t test or the chi
square test. Significance was defined as a probability (p)
value less than 0.05.
Results
In the 41 patients with acute or recent infarction analyzed
in the first part of this study, the infarct vessel was the left
Downloaded From: http://content.onlinejacc.org/ on 12/08/2014
1236
AMBROSE ET AL.
MORPHOLOGY IN MYOCARDIAL INFARCTION
anterior descending artery in 18, the right coronary artery
in 13 and the left circumflex artery in 10. One vessel disease
was present in 26 patients, and 15 had multivessel disease.
Series 1. Coronary anatomy and morphology.
Quantitative and qualitative analyses of the coronary lesions
in the infarct vessel are contained in Table 1. In each group
the type II eccentric lesion was the most common coronary
morphology and its prevalence in the various subgroups was
similar. Therefore, the time from infarction to angiography
did not influence the prevalence of the type II lesion. Two
type II lesions from different patients are shown in Figure
2. For all patients, 27 (66%) of 41 infarct vessels contained
a type II lesion, whereas only 2 (11 %) of 18 noninfarct
vessels with obstruction of 50 to less than 100% had a type
II lesion (p < 0.00 1). The percent stenosis of infarct vessels
was similar among the three groups.
Figure 3. Selected angiographic frames from two patients with a
type II lesion after infusion of streptokinase. Top, The arrow
points to the type II lesion in the midright coronary artery of a
patient from Group I SK. Bottom, The arrow points to the type
II lesion in the proximal right coronary artery of a patient from
Group II SK. Both frames were filmed in the left anterior oblique
projection. See text for definition of Groups I SK and II SK.
lACC Vol. 6, No.6
December 1985:1233-8
100
(j')
INCIDENCE OF TYPE IT LESIONS
IN MYOCARDIAL INFARCTION
I-
~
a..
I.J,..
(.!)
c:(
I-
80
60
40
a: 20
w
a..
(.)
< 12 hours
1-2 wks
2-IOwks
Reperfused
tolal
occlusions
1SK
Reperfused
<totally
occluded
nSK
GROUP
Figure 4. Bar diagram depicting the incidence of type II lesions
within the five different subgroups from both parts of the study
(Series 1 and 2).
Series 2. Coronary anatomy and morphology after
streptokinase. Quantitative and qualitative analyses of the
patients receiving streptokinase infusion in the second part
of this study are contained in Table 2. The left anterior
descending coronary artery was involved in nine patients,
whereas the left circumflex and right coronary arteries were
the infarct vessels in six and eight patients, respectively.
Eleven patients had one vessel disease and the remainder
had multivessel disease. The angiographic findings after
streptokinase infusion from a typical patient in Group I SK
(total occlusion and reperfusion) and another from Group
II SK (nontotal occlusion) are shown in Figure 3. In Group
I SK, 10 (59%) of 17 reperfused arteries contained a type
II lesion compared with 4 (67%) of 6 in Group II SK (p =
NS). For both groups, 14 (61%) of 23 infarct vessels con
tained a type II lesion, whereas only 1 (9%) of 11 noninfarct
vessels with obstruction of 50 to less than 100% had a type
II lesion (p < 0.01). After streptokinase, no Group II SK
lesion had a changed morphology. The percent stenosis of
the infarct vessel before and after streptokinase infusion in
Group II SK did not change significantly, but in three pa
tients distal flow in the obstructed vessel visually improved
after streptokinase. In addition, the percent stenosis of in
farct vessels in Group I SK and Group II SK was also
similar.
Discussion
Type II eccentric coronary lesion. Quantitative anal
ysis of the degree of obstructive coronary artery disease
often shows no difference among the various clinical coro
nary artery syndromes (8-10). Qualitative analysis of coro
nary morphology may provide a foundation for the angio-
Downloaded From: http://content.onlinejacc.org/ on 12/08/2014
JACC Vol. 6, NO.6
December 1985: 1233-8
graphic stratification of patients with various clinical
presentations in coronary artery disease. The type II eccen
tric lesion (smooth with narrow neck or irregular borders)
is found in the majority of patients with an acute presentation
of unstable angina but is infrequent in stable angina pectoris
(6), The present study also indicates that a similar appearing
lesion is found in the majority of patients with acute or
recent myocardial infarction and nontotally occluded ves
sels, The type II lesion is also the most frequent morphologic
finding in infarct vessels after reperfusion with streptokinase
(Fig. 4), Though the pathologic significance of the type II
lesion is unknown, eccentric and irregular lesions on post
mortem angiography have been shown to manifest plaque
rupture, plaque hemorrhage, superimposed partially occlu
sive thrombus or recanalized thrombus (5). The acute pre
sentation of unstable angina with the type II lesion, the
angiographic appearance of this lesion and the postmortem
angiographic data of Levin and Fallon (5) suggest that the
type II lesion may represent a disrupted atherosclerotic plaque
or a partially occlusive or lysed thrombus, or both. Recently
the appearance of intracoronary thrombus has been de
scribed at angiography in patients with unstable angina and
nontotally occluded vessels (11-14). Such thrombus has
been visualized as a filling defect usually noted just distal
to the obstruction in a region of diminished flow. A similar
appearance was noted in six patients from our entire study.
Spectrum of unstable angina and myocardial infarc
tion. Both unstable angina and acute myocardial infarction
often present acutely and suddenly. This suggests that an
acute process within the coronary artery is causing a de
crease in coronary blood flow relative to oxygen demand.
The predominance of the type II lesion in both conditions
implies that unstable angina and acute infarction may form
a continuous spectrum. If plaque disruption occurs within
an artery, a superimposed thrombus may form. The degree
of anterograde obstruction, the time course of development
of this obstruction as well as the collateral flow and myo
cardial oxygen demand determine whether unstable angina
or myocardial infarction ensues. Therefore, the presence of
this lesion may warrant special consideration. When found
in patients with unstable angina, a type II lesion may rep
resent :l coronary plaque in evolution and it could be the
precursor of impending infarction. This change, if it occurs,
probably involves additional thrombus formation or vaso
spasm, or both (15,16).
Study limitations. Our analysis of coronary morphol
ogy is purely descriptive. Although we believe that the type
II lesion represents a ruptured plaque or a partially lysed
thrombus, or both, we have no definite pathologic confir
mation of this finding and we do not know the pathologic
significance of the other coronary lesions. However, the
postmortem angiographic data of Levin and Fallon (5) sup
port our hypothesis concerning the pat.hologic significance
Downloaded From: http://content.onlinejacc.org/ on 12/08/2014
AMBROSE ET AL.
MORPHOLOGY IN MYOCARDIAL INFARCTION
1237
of the type II lesion. Additionally, approximately one-third
of infarct patients did not have this lesion. Whether patients
without a type II lesion have a different mechanism for
infarction is also unknown. Conceivably, a minute area of
plaque disruption could also be present. This could serve
as a nidus for thrombus formation, yet the irregularities of
this lesion may not be visible because of the limited reso
lution of the X-ray equipment. Pathologic analysis of coro
nary lesions in patients who died suddenly has shown that
small areas of plaque disruption with superimposed thrombi
are frequently present (4).
Another potential limitation involves patient selection.
The patients analyzed in this study represent only a fraction
of those catheterized with acute infarction. However, be
cause the same predominant morphology was present in all
groups of patients analyzed, this sample is probably rep
resentative of the majority of patients with acute infarction,
Clinical implications. In conclusion, the type II lesion
is the predominant obstructive coronary morphology in acute
myocardial infarction as well as in unstable angina. How
ever, the clinical significance of this finding is unclear. The
anatomy and morphology of coronary lesions before the
onset of unstable angina or infarction are unknown, as is
the clinical outcome of the type II eccentric lesion in un
stable angina. If it can be shown that the type II lesion in
a patient with unstable angina is likely to progress and cause
myocardial infarction, then aggressive therapy would be
indicated when this lesion is demonstrated. The predomi
nance of this lesion in both unstable angina and myocardial
infarction suggests a link between these two disorders. How
ever, further study will be necessary to validate this
association.
References
I. Rentrop P, Blanke H, Karsch KR, Kaiser H, Kostering H, Leitz K.
Selective intracoronary thrombolysis in acute myocardial infarction
and unstable angina pectoris. Circulation 1981 ;63:307-17.
2. Merx W, Dorr R, Rentrop P, et al. Evaluation of the effectiveness of
intracoronary streptokinase infusion in acute myocardial infarction:
postprocedure management and hospital course in 204 patients. Am
Heart J 1981;102:1181-7.
3. Chapman I. Morphogenesis of occluding coronary artery thrombosis.
Arch Pathol 1965;80:256-61.
4. Davies MJ, Thomas A. Thrombosis and acute coronary artery lesions
in sudden cardiac ischemic death. N Engl J Med 1984;310:1137-40.
5. Levin DC, Fallon JT. Significance of the angiographic morphology
of localized coronary stenoses. Histopathologic correlations. Circu
lation 1982;66:316-20.
6. Ambrose JA, Winters SL, Stem A, et al. Angiographic morphology
and the pathogenesis of unstable angina pectoris. J Am Coll Cardiol
1985;5:609-16.
7. Rentrop KP, Feit F, Blanke H, et al. Effects of intracoronary strep
tokinase and intracoronary nitroglycerine infusion on coronary angio
graphic patterns and mortality in patients with acute myocardial in
farction. N Engl J Med 1984;311:1457-63.
1238
AMBROSE ET AL.
MORPHOLOGY IN MYOCARDIAL INFARCTION
8. Alison HW, Russell RO Jr, Mantle JA, Kouchoukos NT, Moraski
RE, Rackley CEo Coronary anatomy and arteriography in patients with
unstable angina pectoris. Am J Cardiol 1978;41:204-9.
9. Rafftenbeul W, Smith LR, Rogers WT, Mantle JA, Rackley CE,
Russell RO. Qualitative coronary arteriography. Coronary anatomy
of patients with unstable angina pectoris reexamined I year after op
timal medical therapy. Am J Cardiol 1979;43:699-707.
10. Fuster V, Frye RL, Connolly DC, Danielson MA, Elveback LR,
Kurkland LT. Arteriographic patterns early in the onset of the coronary
syndromes. Br Heart J 1975;37:1250-5.
11. Vetrovec GW, Cowley MJ, Overton H, Richardson DW. Intracoro
nary thrombus in syndromes of unstable myocardial ischemia. Am
Heart J 1981;102:1202-8.
Downloaded From: http://content.onlinejacc.org/ on 12/08/2014
JACC Vol. 6, No.6
December 1985:1233-8
12. Holmes DR Jr, Hartzler GO, Smith HC, Fuster V. Coronary artery
thrombus in patients with unstable angina. Br Heart J 1981;45:411-6.
13. Mandelkorn lB, Wolf MN, Singh S, et al. Intracoronary thrombus in
nontransmural myocardial infarction and in unstable angina pectoris.
Am J Cardiol 1983;52:1-6.
14. Capone GT, Meyer BB, Wolf NM, Meister SG. Incidence of intra
coronary thrombi in patients with active unstable angina pectoris.
Circulation 1984;70(suppl II):II-415.
J
15. Fuster V, Chesebro JH. Current concepts of thrombogenesis. Role of
platelets. Mayo Ciin Proc 1981;56:102-8.
16. Hirsh PD, Hillis LD, Campbell WB, Firth BG, Willerson JT. Release
of prostaglandins and thromboxane into the coronary circulation in
patients with ischemic heart disease. N Engl J Med 1981;304:685-91.
You might also like
- FCCS - Pediatric Vs Adult ConsiderationDocument13 pagesFCCS - Pediatric Vs Adult ConsiderationludiNo ratings yet
- Eriksen Et Al-2002-Clinical Cardiology PDFDocument5 pagesEriksen Et Al-2002-Clinical Cardiology PDFmedskyqqNo ratings yet
- 2000 - Stamm Et Al. - Surgery For Bilateral Outflow Tract Obstruction in Elastin ArteriopathyDocument9 pages2000 - Stamm Et Al. - Surgery For Bilateral Outflow Tract Obstruction in Elastin ArteriopathybanupluNo ratings yet
- Circulation 1973 ALONSO 588 96Document10 pagesCirculation 1973 ALONSO 588 96Jessica ARNo ratings yet
- 29 Full PDFDocument7 pages29 Full PDFDHIVYANo ratings yet
- Tortuosity,: Coiling, and Kinking of Internal Carotid ArteryDocument13 pagesTortuosity,: Coiling, and Kinking of Internal Carotid ArteryRoberto AmayaNo ratings yet
- Acosta 2003Document5 pagesAcosta 2003Mihaela MocanNo ratings yet
- BR Heart J 1985 Hartnell 392 5Document5 pagesBR Heart J 1985 Hartnell 392 5phng77No ratings yet
- Acs 03 03 234Document13 pagesAcs 03 03 234IwanNo ratings yet
- Jurnal Coronary Artery FistulaDocument3 pagesJurnal Coronary Artery FistulaRistinyaUnuyNo ratings yet
- Discrete Atherosclerotic Coronary Artery Aneurysms: A Study of 20 PatientsDocument4 pagesDiscrete Atherosclerotic Coronary Artery Aneurysms: A Study of 20 PatientsaudiNo ratings yet
- Scientific Letters: Rev Esp Cardiol. 2016 69 (3) :337-349Document2 pagesScientific Letters: Rev Esp Cardiol. 2016 69 (3) :337-349luisNo ratings yet
- Disseccao Tipo b2Document6 pagesDisseccao Tipo b2coopervascba.diradmNo ratings yet
- Cell Therapy in Patients With Left Ventricular Dysfunction Due To Myocardial InfarctionDocument10 pagesCell Therapy in Patients With Left Ventricular Dysfunction Due To Myocardial InfarctionMrityunjay PathakNo ratings yet
- The Fate of The Distal Aorta After Repair of Acute Type A Aortic DissectionDocument10 pagesThe Fate of The Distal Aorta After Repair of Acute Type A Aortic Dissectionapi-160333876No ratings yet
- Circulation 1975 Burggraf 146 56Document12 pagesCirculation 1975 Burggraf 146 56Zikri Putra Lan LubisNo ratings yet
- Anatomic Features and Surgical Strategies in Double-Outlet Right VentricleDocument18 pagesAnatomic Features and Surgical Strategies in Double-Outlet Right VentriclesuckeydluffyNo ratings yet
- Principles in The Management of Arterial Injuries Associated With Fracture DislocationsDocument5 pagesPrinciples in The Management of Arterial Injuries Associated With Fracture DislocationsJohannes CordeNo ratings yet
- Pi Is 0003497505012002Document5 pagesPi Is 0003497505012002Tri RachmadijantoNo ratings yet
- Ect AsiaDocument4 pagesEct Asiajessik zavalaNo ratings yet
- s0735 1097 (85) 80117 0Document8 pagess0735 1097 (85) 80117 0John DoeNo ratings yet
- Echocardiographic Features of Total Anomalous Pulmonary: VenousDocument8 pagesEchocardiographic Features of Total Anomalous Pulmonary: VenousTanuj VermaNo ratings yet
- Revisión de Disección Celíaca y EsplénicaDocument5 pagesRevisión de Disección Celíaca y EsplénicaLuis AlfonsoNo ratings yet
- Short-And Long-Term Outcomes of Acute Upper Extremity Arterial ThromboembolismDocument4 pagesShort-And Long-Term Outcomes of Acute Upper Extremity Arterial ThromboembolismWilhelm HeinleinNo ratings yet
- Delayed Pericardial Effusion Following Stab Wounds To The ChestDocument4 pagesDelayed Pericardial Effusion Following Stab Wounds To The Chestapi-541676441No ratings yet
- Atrial Hemangioma A Case Report and Review of The LiteratureDocument11 pagesAtrial Hemangioma A Case Report and Review of The LiteratureSaya MenarikNo ratings yet
- 1 s2.0 S0929664608602041 MainDocument9 pages1 s2.0 S0929664608602041 MainEko SiswantoNo ratings yet
- ICA AneurismDocument6 pagesICA AneurismnaimNo ratings yet
- Paracardiac Masses Caused A Right Coronary Artery Aneurysm and A Saphenous Vein Graft AneurysmDocument3 pagesParacardiac Masses Caused A Right Coronary Artery Aneurysm and A Saphenous Vein Graft AneurysmSheikh Mizanur RahmanNo ratings yet
- Angiography 50%Document17 pagesAngiography 50%Nova SipahutarNo ratings yet
- Open Fixation in Flail Chest: Review of 64 Patients: Riginal OntributionDocument6 pagesOpen Fixation in Flail Chest: Review of 64 Patients: Riginal OntributionDian PermatasariNo ratings yet
- Anilllo VascularDocument5 pagesAnilllo VascularKendy LópezNo ratings yet
- Left Hemothorax: Unusual Manifestation of Aortic DissectionDocument5 pagesLeft Hemothorax: Unusual Manifestation of Aortic DissectionIJAR JOURNALNo ratings yet
- Predictive Value of Angiographic Testing For Tolerance To Therapeutic Occlusion of The Carotid ArteryDocument4 pagesPredictive Value of Angiographic Testing For Tolerance To Therapeutic Occlusion of The Carotid ArteryCarol ArtigasNo ratings yet
- Effect of Left Ventricular Outflow Tract Obstruction On Clinical Outcome in Hypertrophic CardiomyopathyDocument9 pagesEffect of Left Ventricular Outflow Tract Obstruction On Clinical Outcome in Hypertrophic CardiomyopathyAstrid Noviera IksanNo ratings yet
- Cairns 1976Document14 pagesCairns 1976Direvald WesterosNo ratings yet
- Duplex Guided Balloon Angioplasty and Subintimal DDocument8 pagesDuplex Guided Balloon Angioplasty and Subintimal DJose PiulatsNo ratings yet
- CoronariesDocument9 pagesCoronariesbanzicaaNo ratings yet
- Cardiac ValveDocument9 pagesCardiac Valveikbal rambalinoNo ratings yet
- Angeborene Koronarfisteln - Die Häufigste Angeborene KoronaranomalieDocument8 pagesAngeborene Koronarfisteln - Die Häufigste Angeborene KoronaranomalieCHENo ratings yet
- Aortic Regurgitation: Clinical PracticeDocument8 pagesAortic Regurgitation: Clinical PracticeChintya Fidelia MontangNo ratings yet
- Bmjcred00241 0003Document2 pagesBmjcred00241 0003Shafa AudryNo ratings yet
- Pathophysiology, Diagnosis, and Medical Management of Nonsurgical PatientsDocument14 pagesPathophysiology, Diagnosis, and Medical Management of Nonsurgical PatientsVanitha Ratha KrishnanNo ratings yet
- tmp53D3 TMPDocument8 pagestmp53D3 TMPFrontiersNo ratings yet
- Shaggy Aorta 8Document1 pageShaggy Aorta 8Eghet SilviuNo ratings yet
- 45 1057Document5 pages45 1057Gabriela PinticanNo ratings yet
- Hollehorst PlaquesDocument3 pagesHollehorst PlaquesErick Roa GandicaNo ratings yet
- Jurnal Astra ACSDocument30 pagesJurnal Astra ACSEta EtiiNo ratings yet
- 405 2013 Article 2598Document5 pages405 2013 Article 2598M Shiddiq GhiffariNo ratings yet
- Aranda 1998Document5 pagesAranda 1998Sarly FebrianaNo ratings yet
- Adult Choroidal Vein of Galen MalformationDocument5 pagesAdult Choroidal Vein of Galen MalformationSonia Prima Arisa PutriNo ratings yet
- Wa0005Document7 pagesWa0005nandawahyuseptiaNo ratings yet
- Ekim, H. y Tuncer, M. (2009) - Manejo de Lesiones Traumáticas de La Arteria Braquial Informe de 49 PacientesDocument5 pagesEkim, H. y Tuncer, M. (2009) - Manejo de Lesiones Traumáticas de La Arteria Braquial Informe de 49 PacientesEdgar Geovanny Cardenas FigueroaNo ratings yet
- Frequency of Coronary Artery Disease in Valvular Aortic Stenosis :experience of The Cardiology Center of Mohamed V Military Hospital About 148 CasesDocument5 pagesFrequency of Coronary Artery Disease in Valvular Aortic Stenosis :experience of The Cardiology Center of Mohamed V Military Hospital About 148 CasesIJAR JOURNALNo ratings yet
- Percutaneous Transluminal Angioplasty and Stenting As First-Choice Treatment in Patients With Chronic Mesenteric IschemiaDocument6 pagesPercutaneous Transluminal Angioplasty and Stenting As First-Choice Treatment in Patients With Chronic Mesenteric IschemiaCotaga IgorNo ratings yet
- Aortic D RefferatDocument5 pagesAortic D RefferatRachman IbrahimNo ratings yet
- Echo Case Ao RegurgDocument3 pagesEcho Case Ao Regurgdgina8800No ratings yet
- Spon Artery DissceDocument6 pagesSpon Artery DissceMuhammad JunaidNo ratings yet
- Griffith 1996Document10 pagesGriffith 1996Sowmya ANo ratings yet
- Intrinsic Third Ventricular Craniopharyngiomas: Report On Six Cases and A Review of The LiteratureDocument8 pagesIntrinsic Third Ventricular Craniopharyngiomas: Report On Six Cases and A Review of The LiteratureAmina GoharyNo ratings yet
- Advancements in Acute Aortic Syndrome: From Pathophysiology to Personalized TherapeuticsFrom EverandAdvancements in Acute Aortic Syndrome: From Pathophysiology to Personalized TherapeuticsNo ratings yet
- Follow Up Pasien (29 Juli-11 Agustus 2017) : S o Demam (+)Document6 pagesFollow Up Pasien (29 Juli-11 Agustus 2017) : S o Demam (+)Sabila RosyidaNo ratings yet
- Daftar Pustaka: Universitas Lambung MangkuratDocument3 pagesDaftar Pustaka: Universitas Lambung MangkuratSabila RosyidaNo ratings yet
- Acute Renal Failure: Definitions, Diagnosis, Pathogenesis, and TherapyDocument10 pagesAcute Renal Failure: Definitions, Diagnosis, Pathogenesis, and TherapySabila RosyidaNo ratings yet
- Mekanisme:: Types of VomitingDocument3 pagesMekanisme:: Types of VomitingSabila RosyidaNo ratings yet
- Proposal Kegiatan Bakti Sosial " ": Asam-Asam Sehat Bersama FK UnlamDocument1 pageProposal Kegiatan Bakti Sosial " ": Asam-Asam Sehat Bersama FK UnlamSabila RosyidaNo ratings yet
- Anorectal MalformationDocument4 pagesAnorectal MalformationSabila RosyidaNo ratings yet
- Table 1Document1 pageTable 1Sabila RosyidaNo ratings yet
- 年 1 月 TOEFL 试题: Section One: Listening ComprehensionDocument16 pages年 1 月 TOEFL 试题: Section One: Listening ComprehensionSabila RosyidaNo ratings yet
- New England Journal Medicine: The ofDocument11 pagesNew England Journal Medicine: The ofnenda nurfendaNo ratings yet
- Chronic Total Occlusions: Emmanouil S. Brilakis, MD, PHDDocument69 pagesChronic Total Occlusions: Emmanouil S. Brilakis, MD, PHDсергейNo ratings yet
- TachycardiaDocument12 pagesTachycardiaPuskesmas Pinang JayaNo ratings yet
- PWKI Art 23954-10Document5 pagesPWKI Art 23954-10Oeij Henri WijayaNo ratings yet
- CV Template TeachingDocument3 pagesCV Template Teachingmohammadrezahajian12191No ratings yet
- An Assignment On Surgery subject:-SHOCK (Definition, Classification and Pathophysiology of Shock)Document8 pagesAn Assignment On Surgery subject:-SHOCK (Definition, Classification and Pathophysiology of Shock)manish soniNo ratings yet
- Quiz Results: NURS 502 Med / Surg Cardiovascular System Correct Answers: 7Document7 pagesQuiz Results: NURS 502 Med / Surg Cardiovascular System Correct Answers: 7Moshi LoveNo ratings yet
- Pharma Q From BooksDocument6 pagesPharma Q From BooksJhayneNo ratings yet
- US Hypertension Review GuidelinesDocument12 pagesUS Hypertension Review Guidelinesmefav7778520100% (1)
- Appeal Chaitanya Ashok Chate - Y PDFDocument1 pageAppeal Chaitanya Ashok Chate - Y PDFrahulsaini855No ratings yet
- Human Cardiovascular PhysiologyDocument5 pagesHuman Cardiovascular PhysiologyKirsten CruzadoNo ratings yet
- Cardioversion of Atrial Fibrillation in Obese Patients: Results From The Cardioversion-BMI Randomized Controlled TrialDocument22 pagesCardioversion of Atrial Fibrillation in Obese Patients: Results From The Cardioversion-BMI Randomized Controlled TrialAttilio Del RossoNo ratings yet
- 15-Lead ECG PowerpointDocument20 pages15-Lead ECG Powerpointgillian102290No ratings yet
- AED PowerPointDocument78 pagesAED PowerPointPetar RajicNo ratings yet
- HPNDocument32 pagesHPNkaren GoNo ratings yet
- Picco Technology Clinical Evidence Brochure en Non - UsDocument25 pagesPicco Technology Clinical Evidence Brochure en Non - UsRichard DaiNo ratings yet
- Aortic GuidelinesDocument62 pagesAortic GuidelinesAmy Hoo Hui MayNo ratings yet
- Cardiology Clinical CasesDocument13 pagesCardiology Clinical CasesKareem Waleed Ibrahim Hamimy100% (1)
- Bls QuestionDocument7 pagesBls Questionmonir61100% (2)
- Arm Blood Pressure Differences 'Predict Death RiskDocument2 pagesArm Blood Pressure Differences 'Predict Death RiskCarolina RusselNo ratings yet
- Echo Guidelines For Chamber QuantificationDocument24 pagesEcho Guidelines For Chamber QuantificationOnon EssayedNo ratings yet
- Drugs Used in CcuDocument169 pagesDrugs Used in CcuAnusha Verghese100% (3)
- Common Emergency DrugsDocument58 pagesCommon Emergency Drugshatem alsrour85% (20)
- Chest TraumaDocument47 pagesChest Traumafrenee aradanasNo ratings yet
- 468-Article Text-964-1-10-20171113Document3 pages468-Article Text-964-1-10-20171113ahmadalipoland25No ratings yet
- Practice/monograph/70/basics/classification - HTML) : DVT: Lower ExtremityDocument2 pagesPractice/monograph/70/basics/classification - HTML) : DVT: Lower ExtremityAyu Putri Firda NNo ratings yet
- Bader Madoukh, Ayman Battisha, Henry Ukwu, Mohammed Al-Sadawi, Shakil ShaikhDocument4 pagesBader Madoukh, Ayman Battisha, Henry Ukwu, Mohammed Al-Sadawi, Shakil ShaikhputriayuratnasariNo ratings yet
- Blood Pressure Solution The Step by Step Guide To Lowering HighDocument112 pagesBlood Pressure Solution The Step by Step Guide To Lowering HighMostafa SayedNo ratings yet
- Chapter 4 - Mixed Venous Oxygen SaturationDocument3 pagesChapter 4 - Mixed Venous Oxygen SaturationJamesNo ratings yet